Clinicalradiographic followup studies of endodontic treatment expectations and







- Slides: 115

Clinical-radiographic follow-up studies of endodontic treatment: expectations and limitations We all strive for excellence, but how well do we do?
Clinical-radiographic follow-up studies of endodontic treatment: expectations and limitations We all strive for excellence, but how well do we do? How can we monitor improvement?
Clinical-radiographic follow-up studies of endodontic treatment: expectations and limitations We all strive for excellence, but how well do we do? How can we monitor improvement? Where do we seek information to support/adjust treatment?
Clinical-radiographic follow-up studies of endodontic treatment: expectations and limitations • Design of follow-up studies: – RCTs, cohort studies, case controls, case series, retro- and prospective, • Critical issues in endodontic clinical research: – Tooth survival, case selection, criteria and harmonization - examples • The fundamental difference between prevention and treatment – When will we ever learn? • Can we cure chronic apical periodontitis? – Histology, experiments, Ricucci, Brynolf, Wu & Wesselink • A change in concept from qualitative to quantitative microbial control • The futility of personal experience – A journey through a hypothetical practice situation • Precision in design – Stiches in embroidery
1 Design of follow-up studies
What do we know? • Technical performance – Length is important in cases of AP – Width is controversial at best(worst), of no consequence at worst (best) – Cultivable bacteria left in the canal at the time of filling are associated with outcome, measured in teeth with AP mainly • Biological and clinical factors – tbd
Clinical-radiographic follow-up studies of endodontic treatment: expectations and limitations • Design of follow-up studies: – RCTs (prosp) – Cohort studies (r&p) – Case controls (r&p) • {Matched pairs} – Case series (r&p) – Case collection (r&p) – Retro- and prospective – drop-outs!
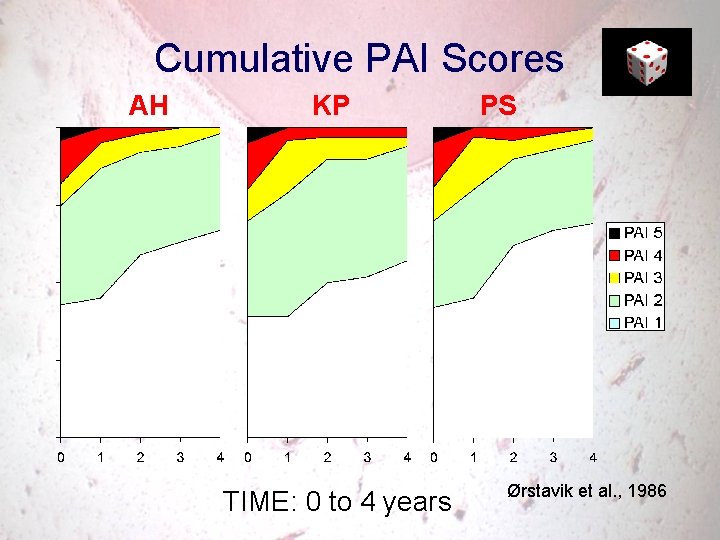
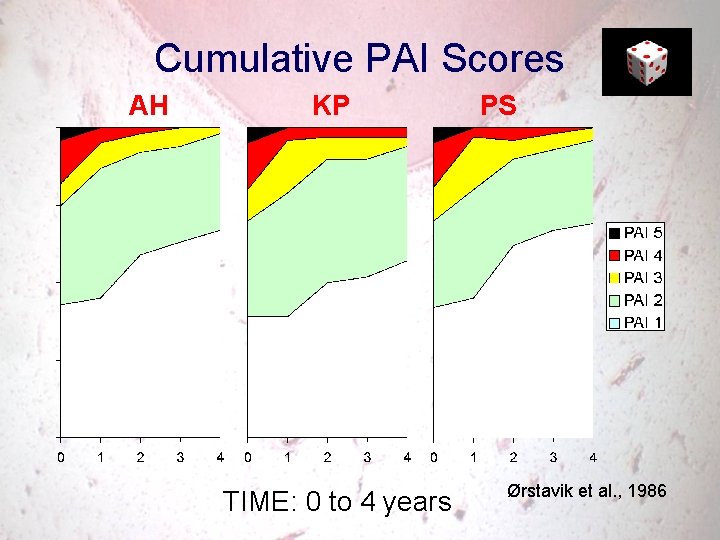
Cumulative PAI Scores AH KP TIME: 0 to 4 years PS Ørstavik et al. , 1986
The single case report: A valuable contribution to the scientific literature Gould 3 x. O September 2001 editorial • ”I wish to advocate for the validity and value of the single case report. I believe that the case report with appropriate content remains an important contribution to the body of clinical and diagnostic information for oral health care providers and researchers. ”
2 Critical issues in endodontic clinical research
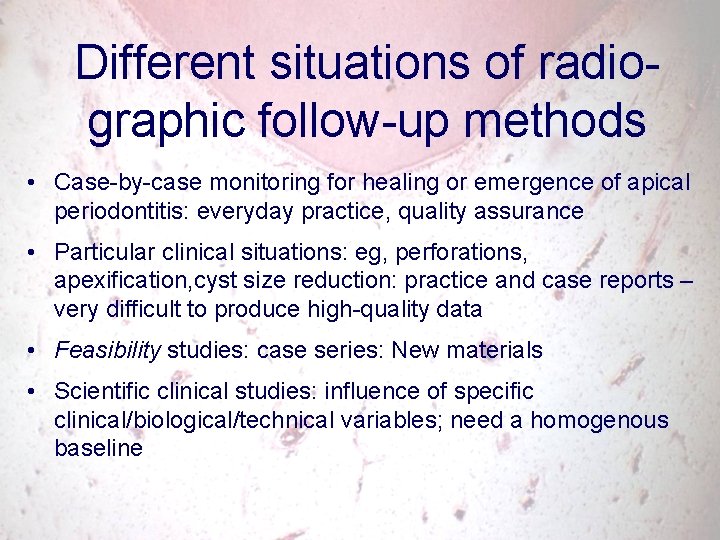
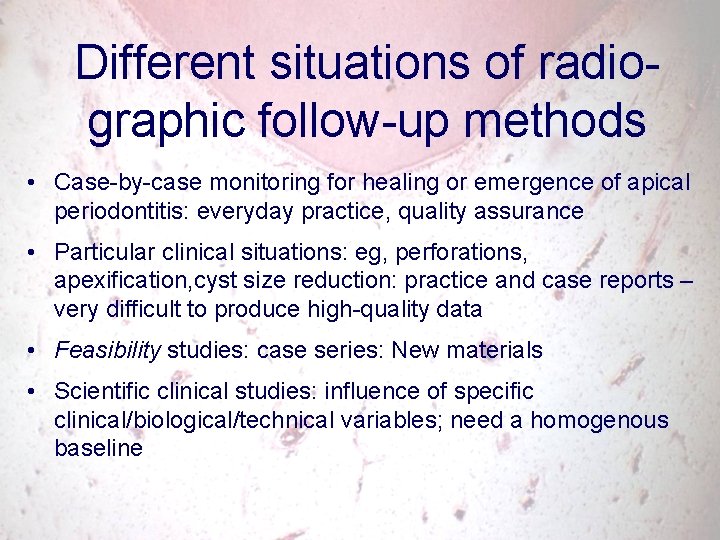
Different situations of radiographic follow-up methods • Case-by-case monitoring for healing or emergence of apical periodontitis: everyday practice, quality assurance • Particular clinical situations: eg, perforations, apexification, cyst size reduction: practice and case reports – very difficult to produce high-quality data • Feasibility studies: case series: New materials • Scientific clinical studies: influence of specific clinical/biological/technical variables; need a homogenous baseline
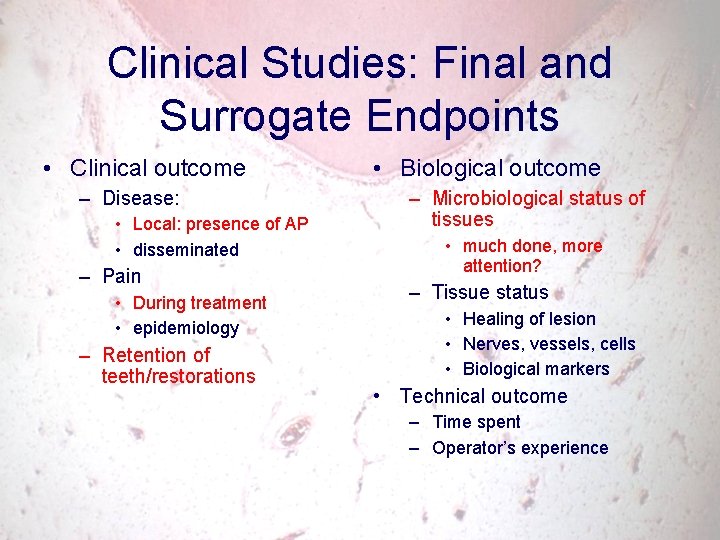
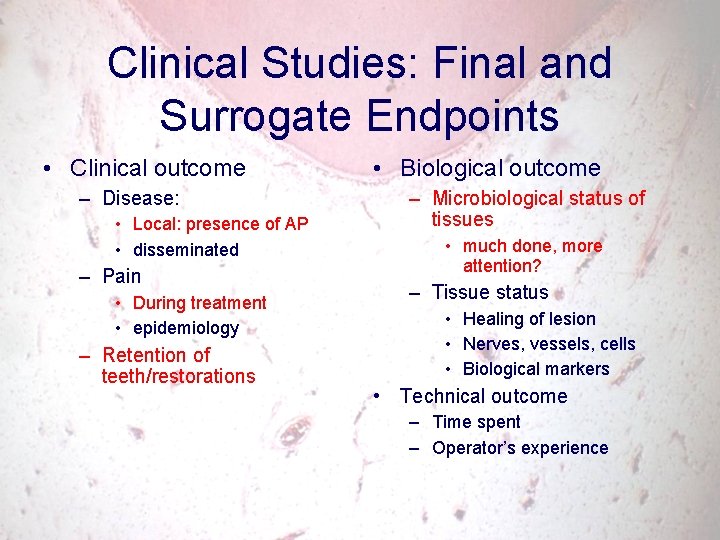
Clinical Studies: Final and Surrogate Endpoints • Clinical outcome – Disease: • Local: presence of AP • disseminated – Pain • During treatment • epidemiology – Retention of teeth/restorations • Biological outcome – Microbiological status of tissues • much done, more attention? – Tissue status • Healing of lesion • Nerves, vessels, cells • Biological markers • Technical outcome – Time spent – Operator’s experience
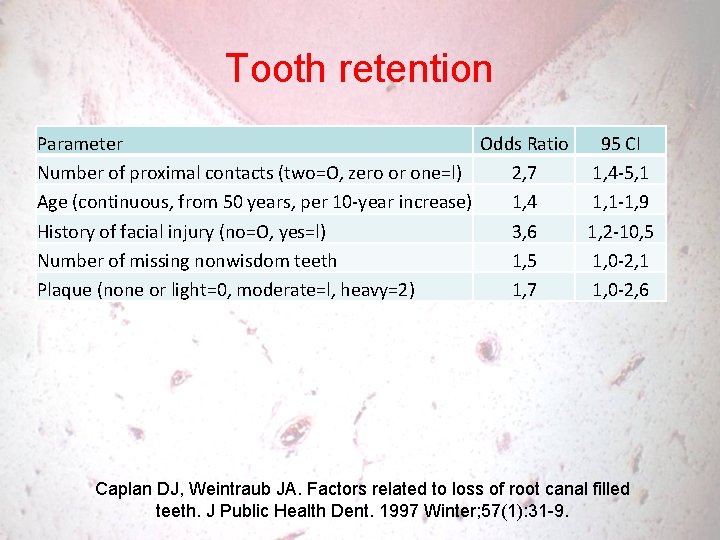
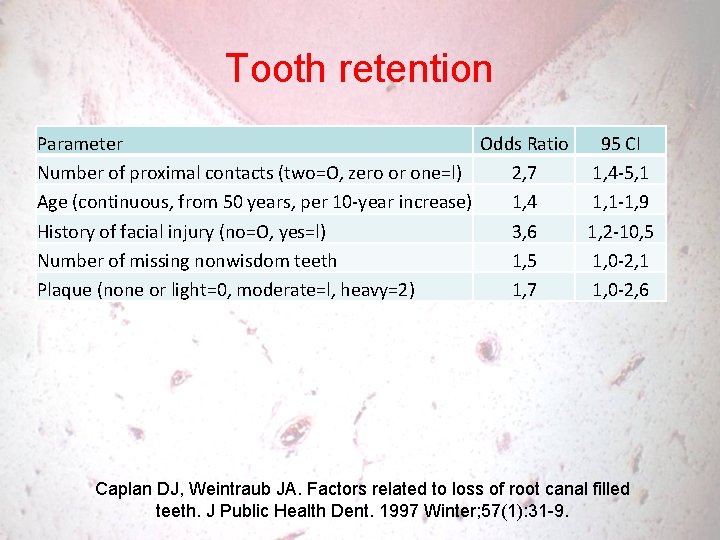
Tooth retention Parameter Odds Ratio 95 CI Number of proximal contacts (two=O, zero or one=l) 2, 7 1, 4 -5, 1 Age (continuous, from 50 years, per 10 -year increase) 1, 4 1, 1 -1, 9 History of facial injury (no=O, yes=l) 3, 6 1, 2 -10, 5 Number of missing nonwisdom teeth 1, 5 1, 0 -2, 1 Plaque (none or light=0, moderate=l, heavy=2) 1, 7 1, 0 -2, 6 Caplan DJ, Weintraub JA. Factors related to loss of root canal filled teeth. J Public Health Dent. 1997 Winter; 57(1): 31 -9.
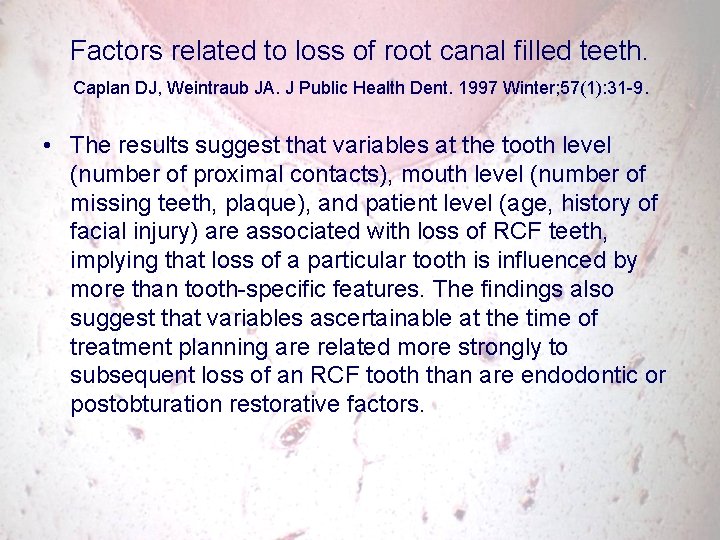
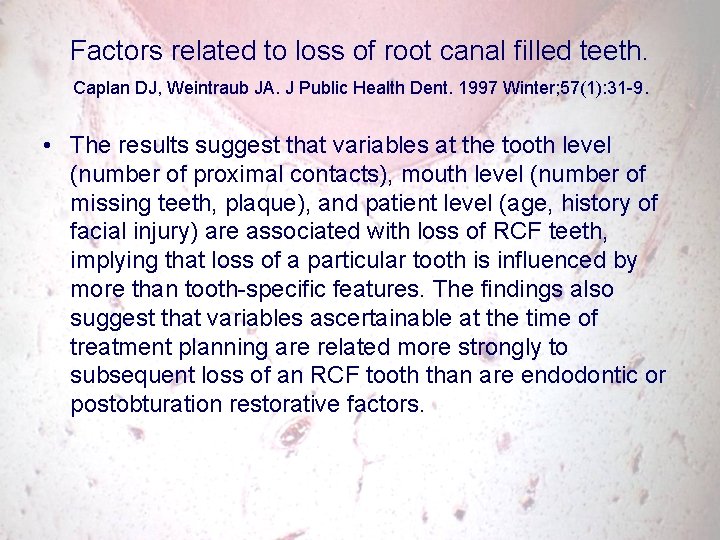
Factors related to loss of root canal filled teeth. Caplan DJ, Weintraub JA. J Public Health Dent. 1997 Winter; 57(1): 31 -9. • The results suggest that variables at the tooth level (number of proximal contacts), mouth level (number of missing teeth, plaque), and patient level (age, history of facial injury) are associated with loss of RCF teeth, implying that loss of a particular tooth is influenced by more than tooth-specific features. The findings also suggest that variables ascertainable at the time of treatment planning are related more strongly to subsequent loss of an RCF tooth than are endodontic or postobturation restorative factors.
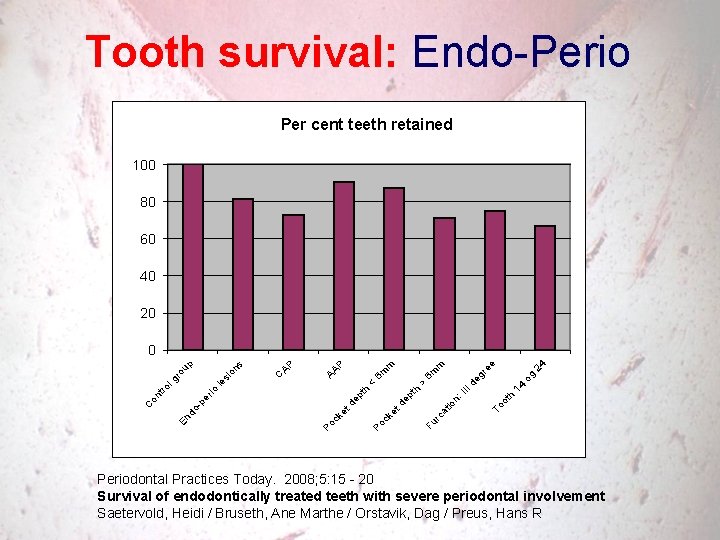
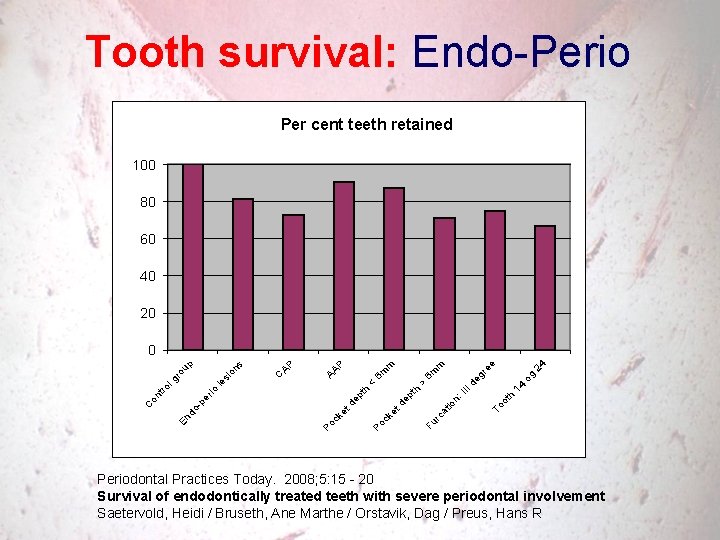
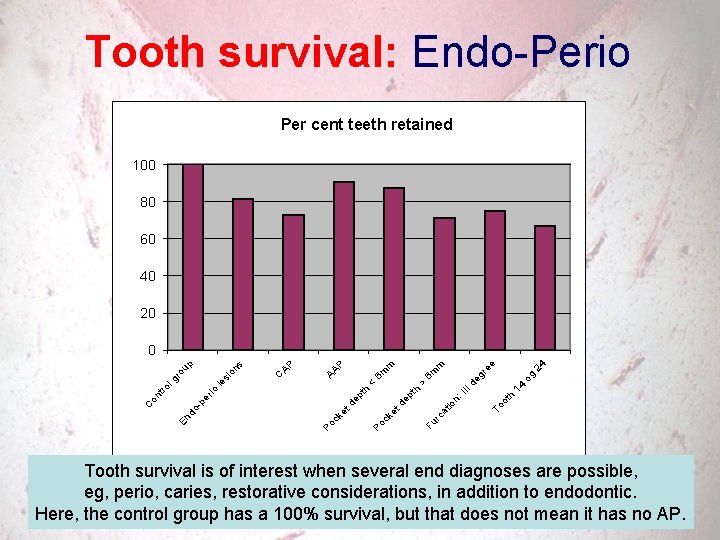
Tooth survival: Endo-Perio Per cent teeth retained 100 80 60 40 20 h ot To II n: io Fu rc at 14 I d o eg g re 24 e m > th t d ke Po c ep th < 6 m m P AA AP er En do -p on C C io tro le l g si ro on s up 0 Periodontal Practices Today. 2008; 5: 15 - 20 Survival of endodontically treated teeth with severe periodontal involvement Saetervold, Heidi / Bruseth, Ane Marthe / Orstavik, Dag / Preus, Hans R
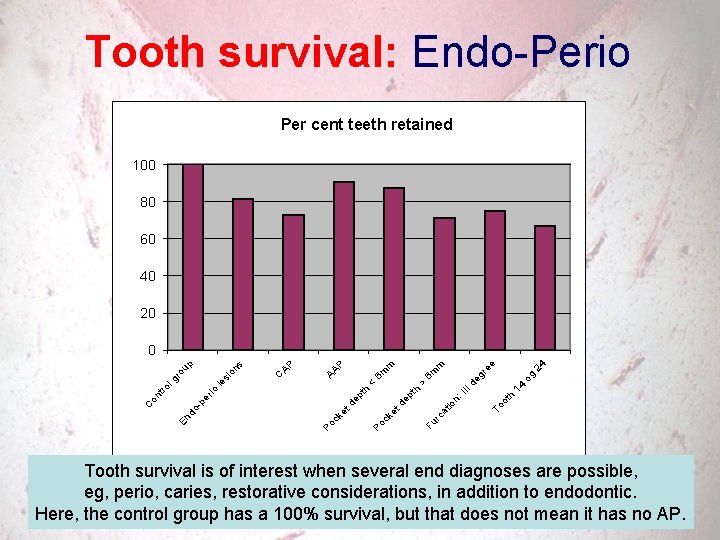
Tooth survival: Endo-Perio Per cent teeth retained 100 80 60 40 20 h ot To II n: io Fu rc at 14 I d o eg g re 24 e m > th t d ke Po c ep th < 6 m m P AA AP er En do -p on C C io tro le l g si ro on s up 0 Tooth survival is of interest when several end diagnoses are possible, Periodontal Practices Today. 2008; 5: 15 - 20 eg, perio, caries, restorative considerations, in addition to endodontic. Survival of endodontically treated teeth with severe periodontal involvement Saetervold, Heidi / Bruseth, Ane Marthe / Orstavik, Dag / Preus, Hans R Here, the control group has a 100% survival, but that does not mean it has no AP.
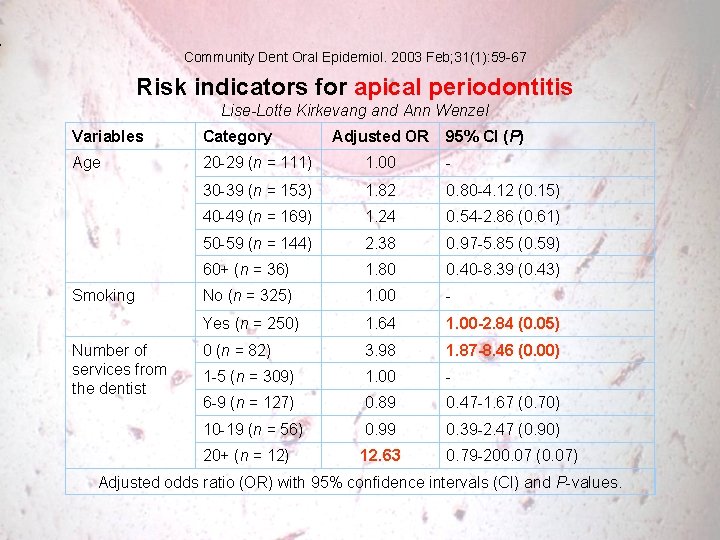
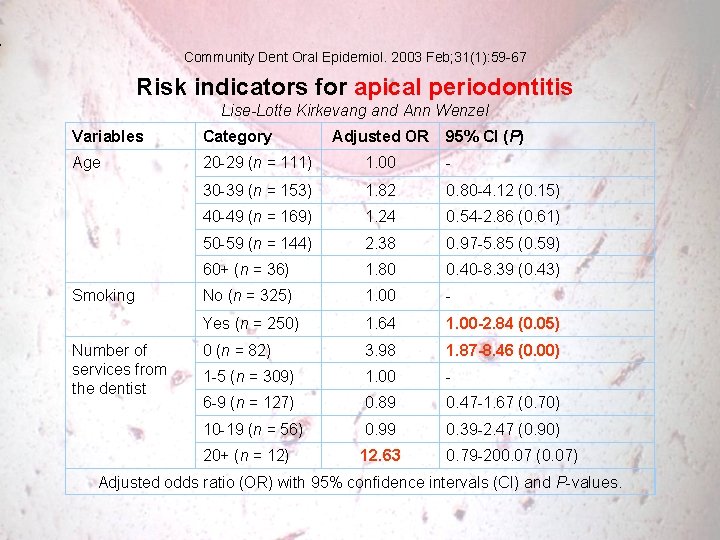
Community Dent Oral Epidemiol. 2003 Feb; 31(1): 59 -67 Risk indicators for apical periodontitis Lise-Lotte Kirkevang and Ann Wenzel Variables Category Age 20 -29 (n = 111) 1. 00 - 30 -39 (n = 153) 1. 82 0. 80 -4. 12 (0. 15) 40 -49 (n = 169) 1. 24 0. 54 -2. 86 (0. 61) 50 -59 (n = 144) 2. 38 0. 97 -5. 85 (0. 59) 60+ (n = 36) 1. 80 0. 40 -8. 39 (0. 43) No (n = 325) 1. 00 - Yes (n = 250) 1. 64 1. 00 -2. 84 (0. 05) 0 (n = 82) 3. 98 1. 87 -8. 46 (0. 00) 1 -5 (n = 309) 1. 00 - 6 -9 (n = 127) 0. 89 0. 47 -1. 67 (0. 70) 10 -19 (n = 56) 0. 99 0. 39 -2. 47 (0. 90) 20+ (n = 12) 12. 63 0. 79 -200. 07 (0. 07) Smoking Number of services from the dentist Adjusted OR 95% CI (P) Adjusted odds ratio (OR) with 95% confidence intervals (CI) and P-values.
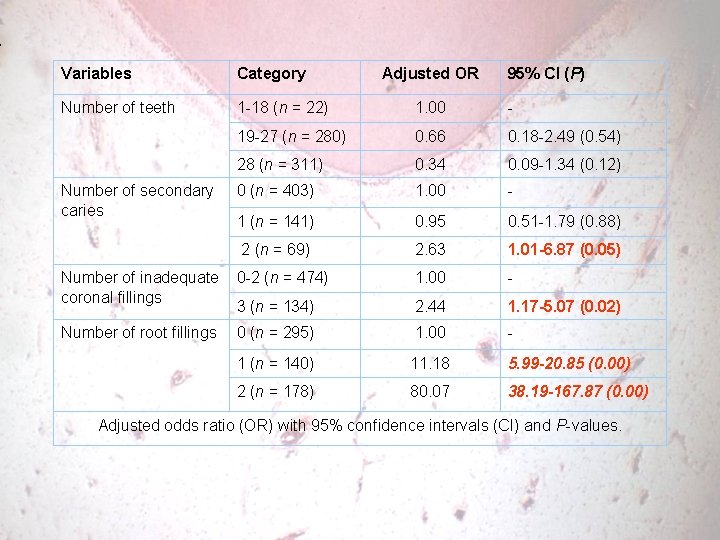
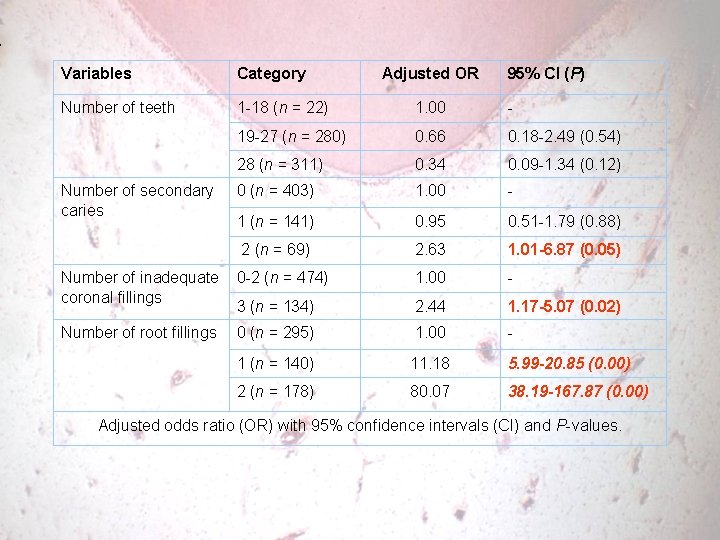
Variables Category Number of teeth 1 -18 (n = 22) 1. 00 - 19 -27 (n = 280) 0. 66 0. 18 -2. 49 (0. 54) 28 (n = 311) 0. 34 0. 09 -1. 34 (0. 12) 0 (n = 403) 1. 00 - 1 (n = 141) 0. 95 0. 51 -1. 79 (0. 88) 2 (n = 69) 2. 63 1. 01 -6. 87 (0. 05) Number of inadequate 0 -2 (n = 474) coronal fillings 3 (n = 134) 1. 00 - 2. 44 1. 17 -5. 07 (0. 02) Number of root fillings 0 (n = 295) 1. 00 - 1 (n = 140) 11. 18 5. 99 -20. 85 (0. 00) 2 (n = 178) 80. 07 38. 19 -167. 87 (0. 00) Number of secondary caries Adjusted OR 95% CI (P) Adjusted odds ratio (OR) with 95% confidence intervals (CI) and P-values.
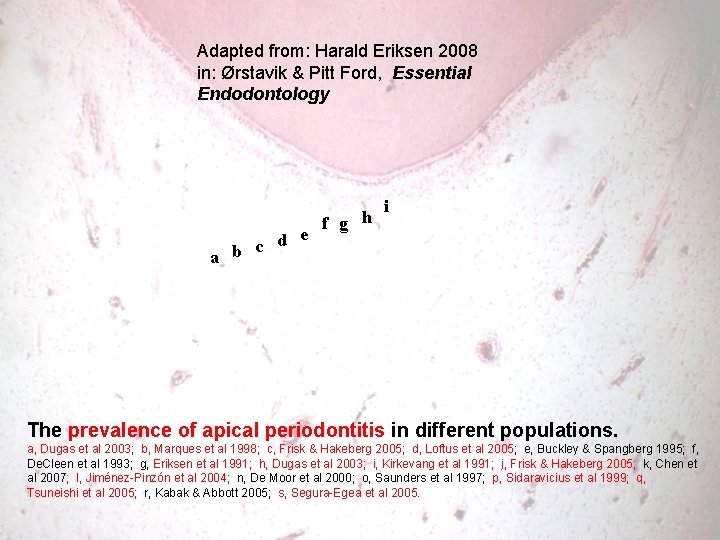
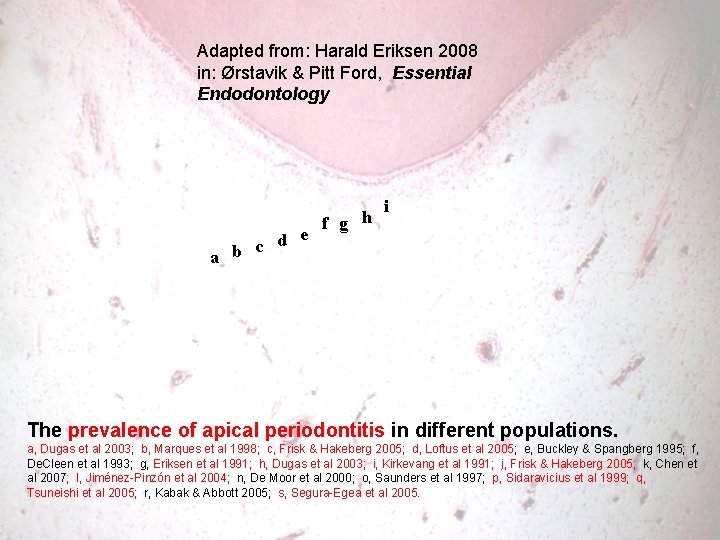
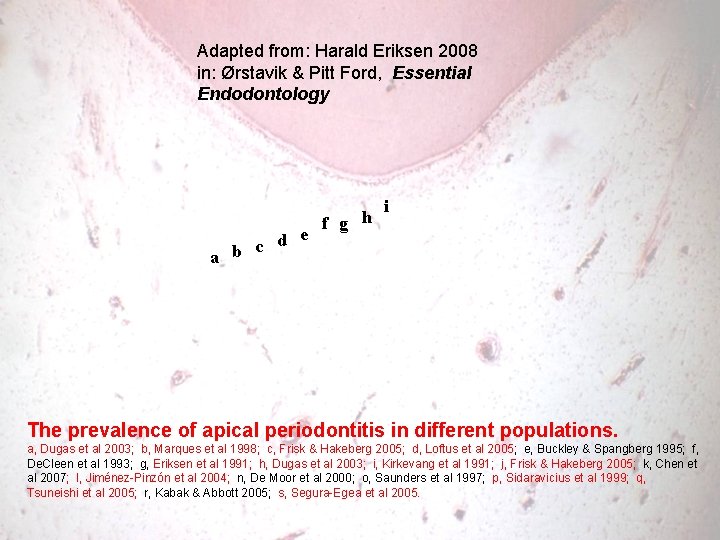
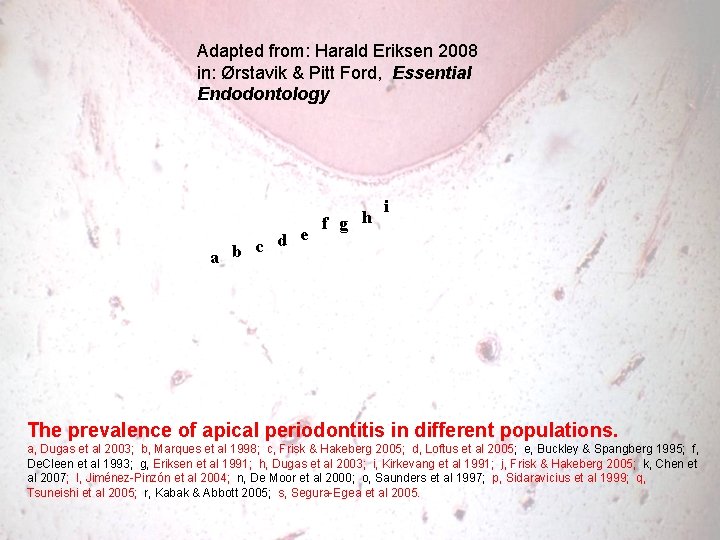
Adapted from: Harald Eriksen 2008 in: Ørstavik & Pitt Ford, Essential Endodontology d e c a b f g h i The prevalence of apical periodontitis in different populations. a, Dugas et al 2003; b, Marques et al 1998; c, Frisk & Hakeberg 2005; d, Loftus et al 2005; e, Buckley & Spangberg 1995; f, De. Cleen et al 1993; g, Eriksen et al 1991; h, Dugas et al 2003; i, Kirkevang et al 1991; j, Frisk & Hakeberg 2005; k, Chen et al 2007; l, Jiménez-Pinzón et al 2004; n, De Moor et al 2000; o, Saunders et al 1997; p, Sidaravicius et al 1999; q, Tsuneishi et al 2005; r, Kabak & Abbott 2005; s, Segura-Egea et al 2005.
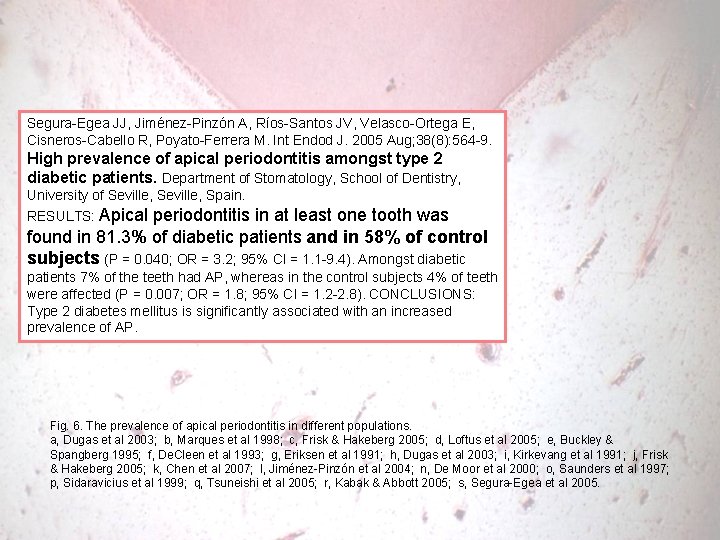
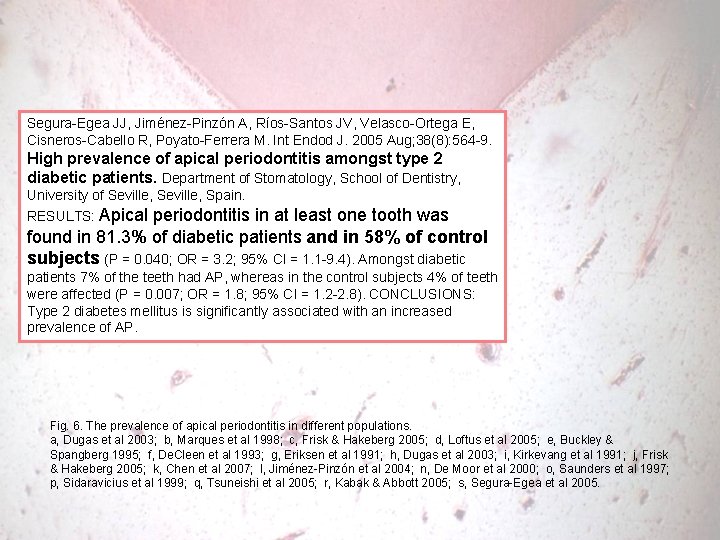
Segura-Egea JJ, Jiménez-Pinzón A, Ríos-Santos JV, Velasco-Ortega E, Cisneros-Cabello R, Poyato-Ferrera M. Int Endod J. 2005 Aug; 38(8): 564 -9. High prevalence of apical periodontitis amongst type 2 diabetic patients. Department of Stomatology, School of Dentistry, University of Seville, Spain. RESULTS: Apical periodontitis in at least one tooth was found in 81. 3% of diabetic patients and in 58% of control subjects (P = 0. 040; OR = 3. 2; 95% CI = 1. 1 -9. 4). Amongst diabetic patients 7% of the teeth had AP, whereas in the control subjects 4% of teeth were affected (P = 0. 007; OR = 1. 8; 95% CI = 1. 2 -2. 8). CONCLUSIONS: Type 2 diabetes mellitus is significantly associated with an increased prevalence of AP. Fig. 6. The prevalence of apical periodontitis in different populations. a, Dugas et al 2003; b, Marques et al 1998; c, Frisk & Hakeberg 2005; d, Loftus et al 2005; e, Buckley & Spangberg 1995; f, De. Cleen et al 1993; g, Eriksen et al 1991; h, Dugas et al 2003; i, Kirkevang et al 1991; j, Frisk & Hakeberg 2005; k, Chen et al 2007; l, Jiménez-Pinzón et al 2004; n, De Moor et al 2000; o, Saunders et al 1997; p, Sidaravicius et al 1999; q, Tsuneishi et al 2005; r, Kabak & Abbott 2005; s, Segura-Egea et al 2005.
Endodontics is: Prevention or treatment of apical periodontitis which in practice means Protection against or elimination(? ) of root canal infection Diagnostics, choice of treatment method, irrigation, medication and root filling are all means towards this end Ørstavik 1988
Endodontics is: Prevention or treatment of apical periodontitis which in practice means Protection against or elimination(? ) of root canal infection How to monitor this disease? Ørstavik 1988
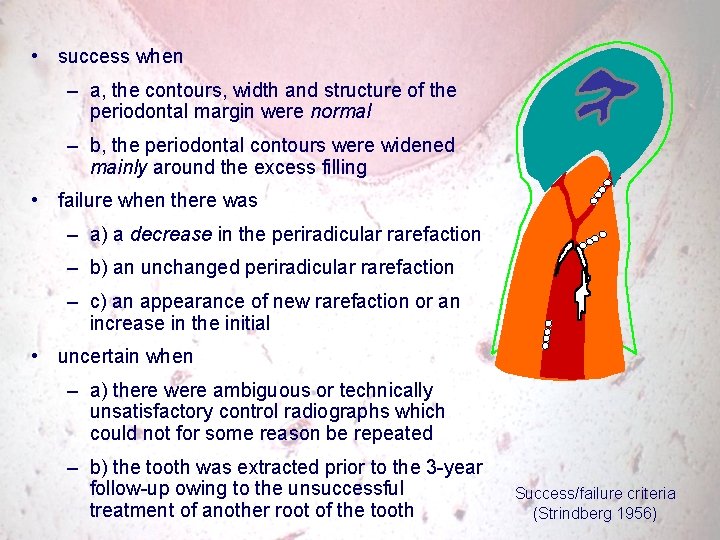
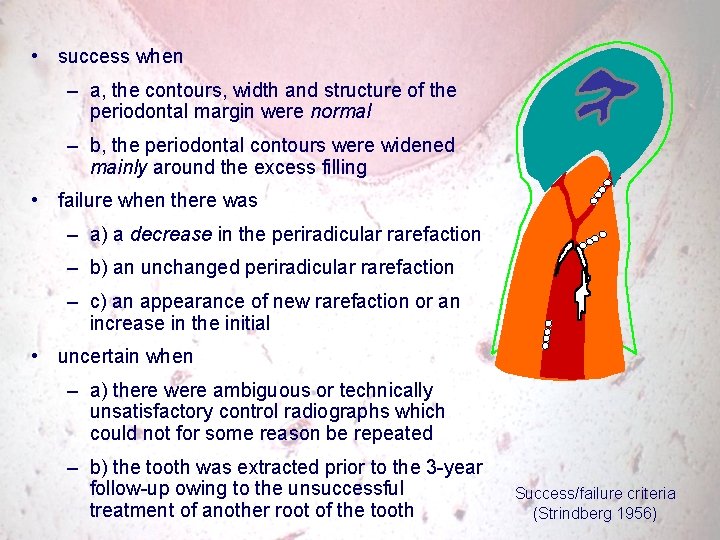
• success when – a, the contours, width and structure of the periodontal margin were normal – b, the periodontal contours were widened mainly around the excess filling • failure when there was – a) a decrease in the periradicular rarefaction – b) an unchanged periradicular rarefaction – c) an appearance of new rarefaction or an increase in the initial • uncertain when – a) there were ambiguous or technically unsatisfactory control radiographs which could not for some reason be repeated – b) the tooth was extracted prior to the 3 -year follow-up owing to the unsuccessful treatment of another root of the tooth Success/failure criteria (Strindberg 1956)
Probability assessments • Definitively no disease 1 • Probably no disease 2 • Uncertain 3 • Probably disease 4 • Definitively disease 5 An attempt to systematize the ”clinical assessment situation”
Scoring Systems in Clinical Dentistry • Caries: limited progress until DMF index was established (1938) • Gingivitis & marginal periodontitis: confusion until indices were applied (1950 -60) • Apical periodontitis: Calibrated indices? Xray digitized measurements? Quantification by (CB)CT?
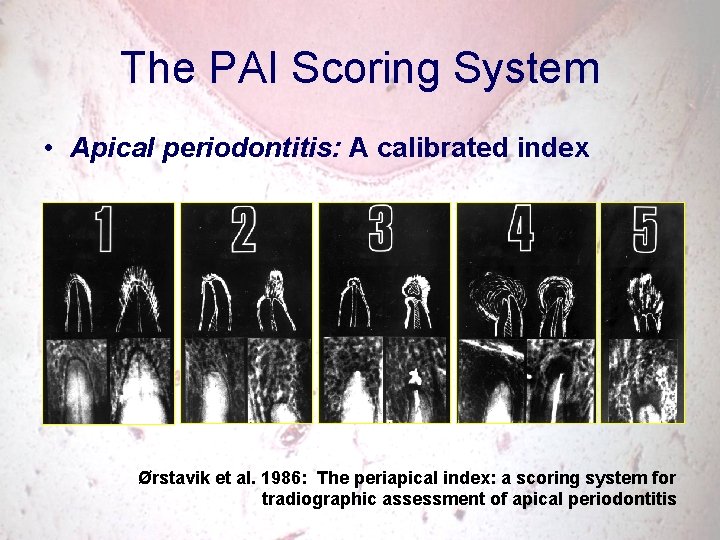
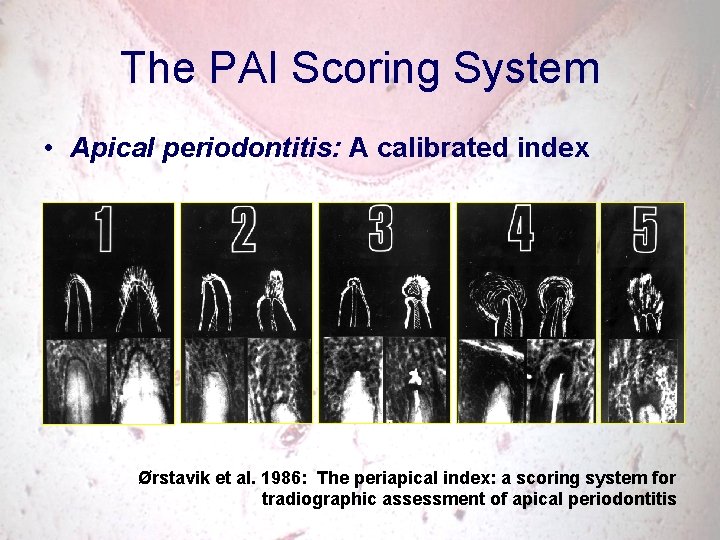
The PAI Scoring System • Apical periodontitis: A calibrated index Ørstavik et al. 1986: The periapical index: a scoring system for tradiographic assessment of apical periodontitis
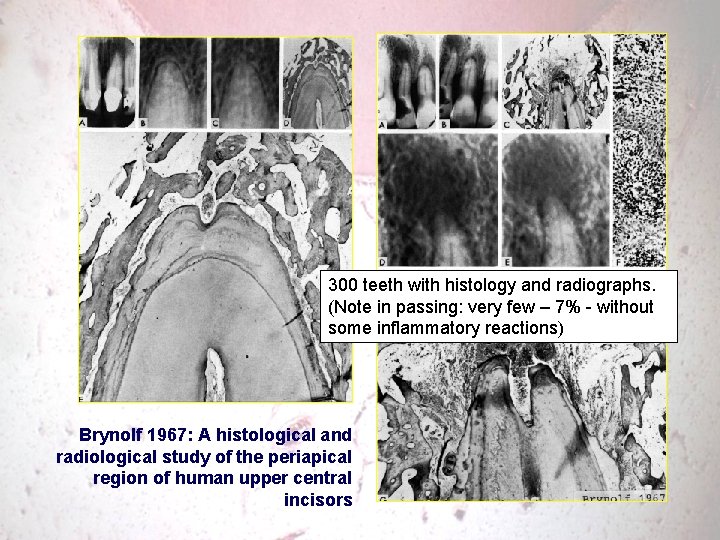
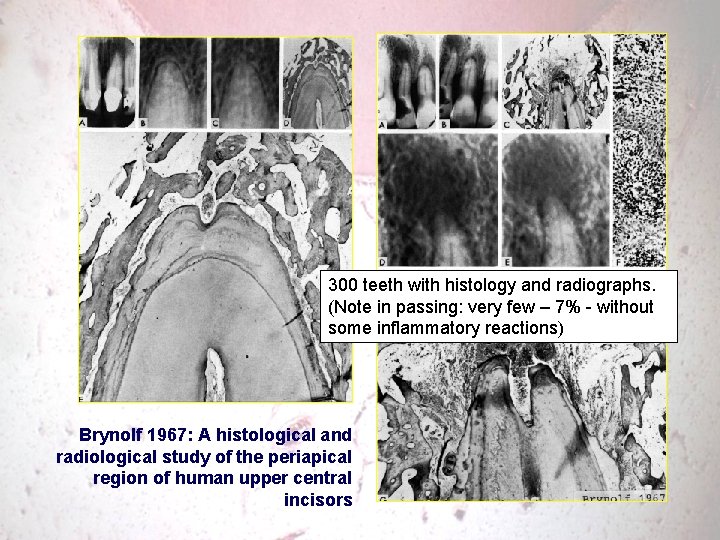
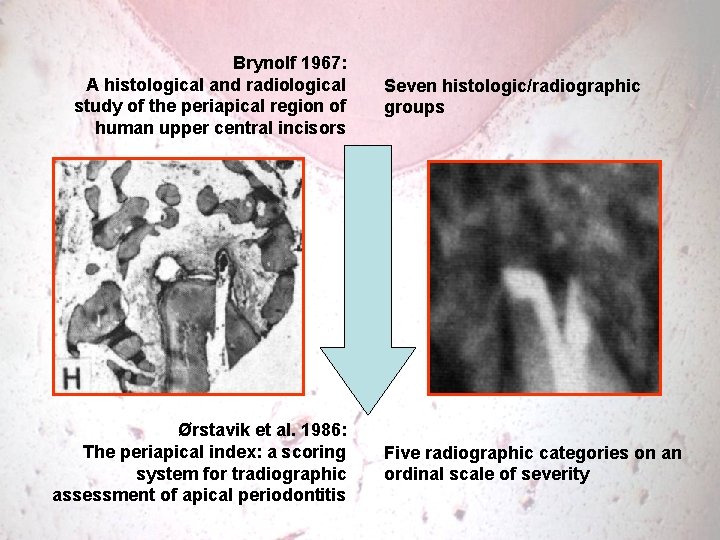
300 teeth with histology and radiographs. (Note in passing: very few – 7% - without some inflammatory reactions) Brynolf 1967: A histological and radiological study of the periapical region of human upper central incisors
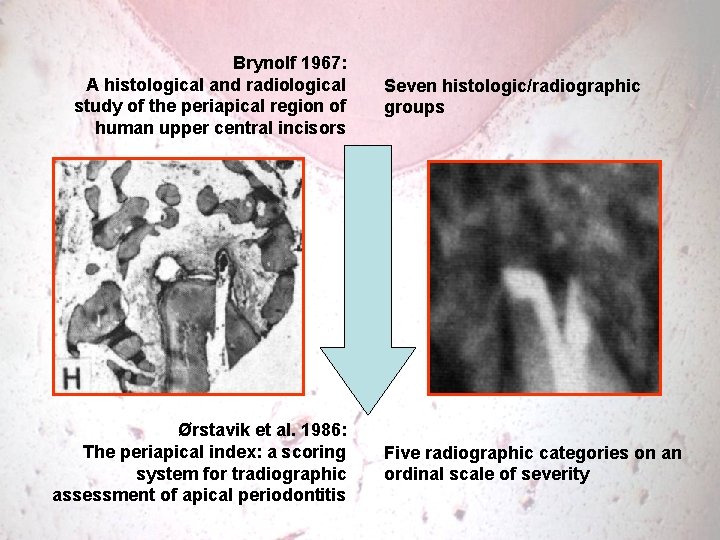
Brynolf 1967: A histological and radiological study of the periapical region of human upper central incisors Ørstavik et al. 1986: The periapical index: a scoring system for tradiographic assessment of apical periodontitis Seven histologic/radiographic groups Five radiographic categories on an ordinal scale of severity
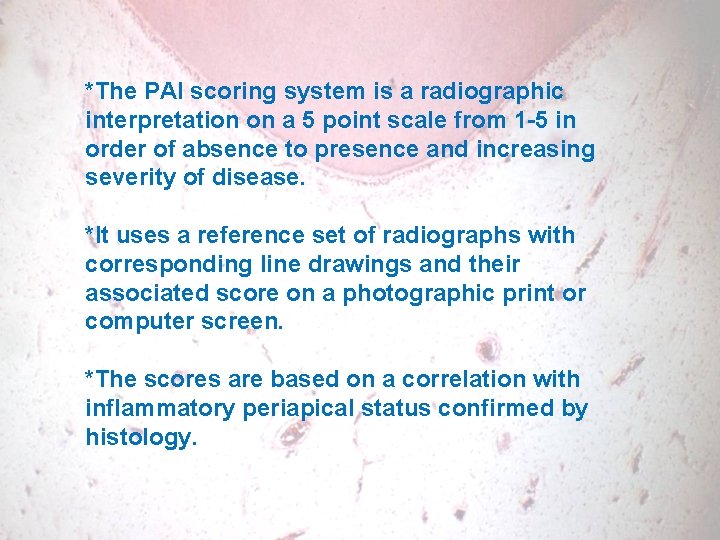
*The PAI scoring system is a radiographic interpretation on a 5 point scale from 1 -5 in order of absence to presence and increasing severity of disease. *It uses a reference set of radiographs with corresponding line drawings and their associated score on a photographic print or computer screen. *The scores are based on a correlation with inflammatory periapical status confirmed by histology.
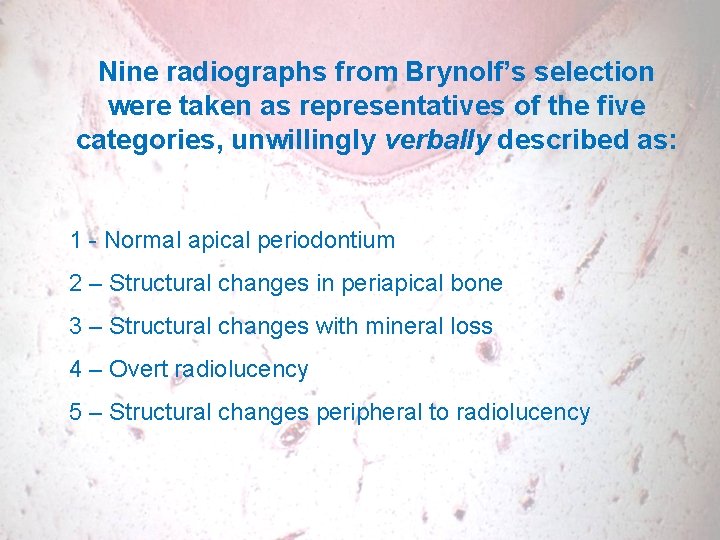
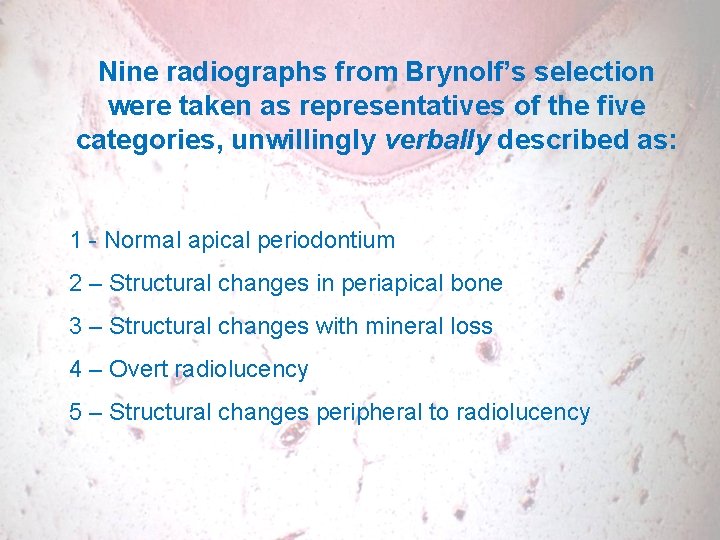
Nine radiographs from Brynolf’s selection were taken as representatives of the five categories, unwillingly verbally described as: 1 - Normal apical periodontium 2 – Structural changes in periapical bone 3 – Structural changes with mineral loss 4 – Overt radiolucency 5 – Structural changes peripheral to radiolucency
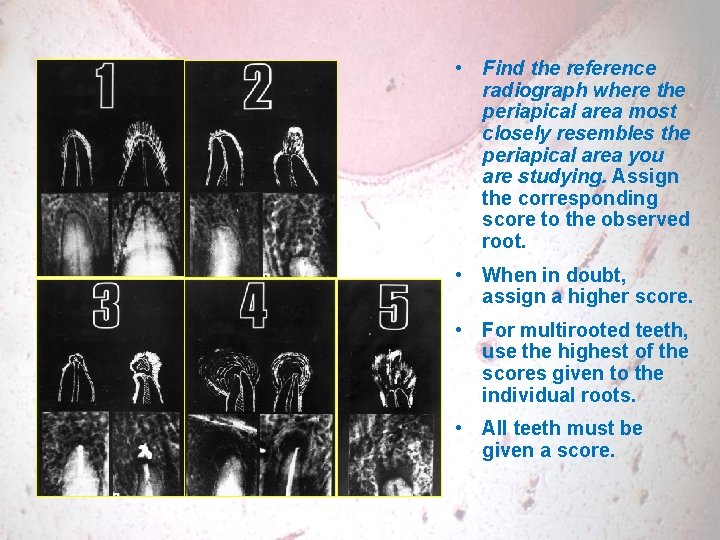
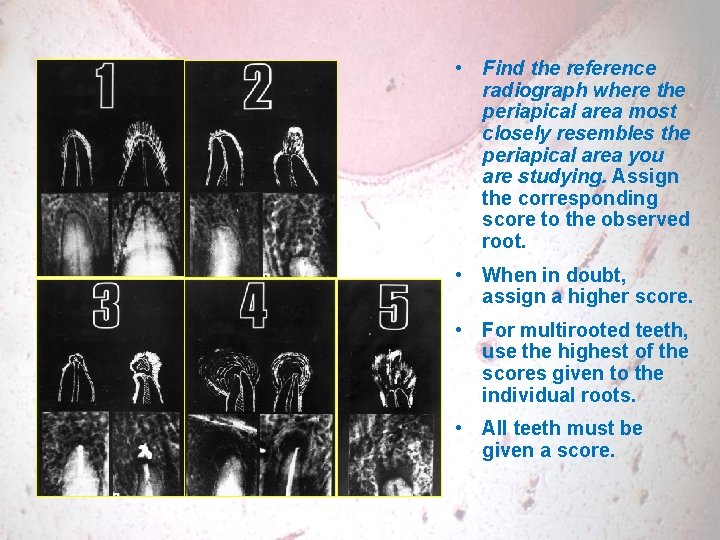
• Find the reference radiograph where the periapical area most closely resembles the periapical area you are studying. Assign the corresponding score to the observed root. • When in doubt, assign a higher score. • For multirooted teeth, use the highest of the scores given to the individual roots. • All teeth must be given a score.
Calibration • Material: • Reference scale • Set of written instructions for scoring • Set of 100 radiographs, one tooth in each is scored. The ’true scores’ have been determined by consensus of two endodontists involved with the development of the system. • Excel file for computation of essential statistical parameters. • 20 calibrated scorers world wide – kappa values from 0. 62 to 0. 80
Usage • 16 countries, 50+ publications • Retrospective clinical follow-ups • Epidemiological studies • Prospective and experimentalstudies
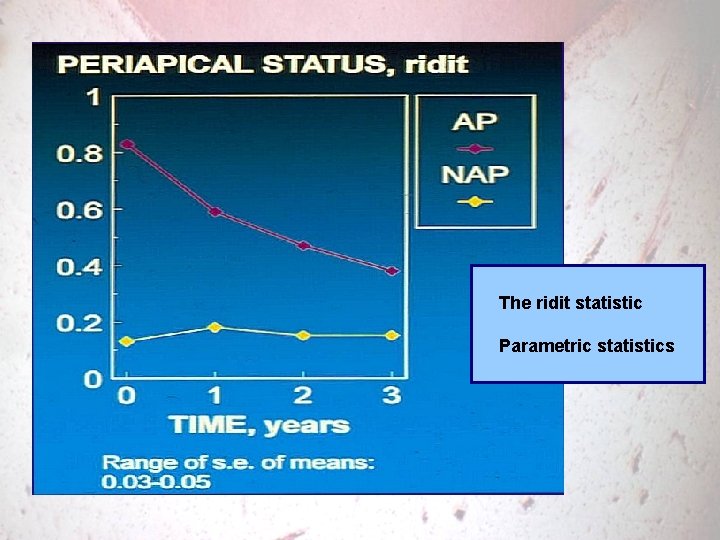
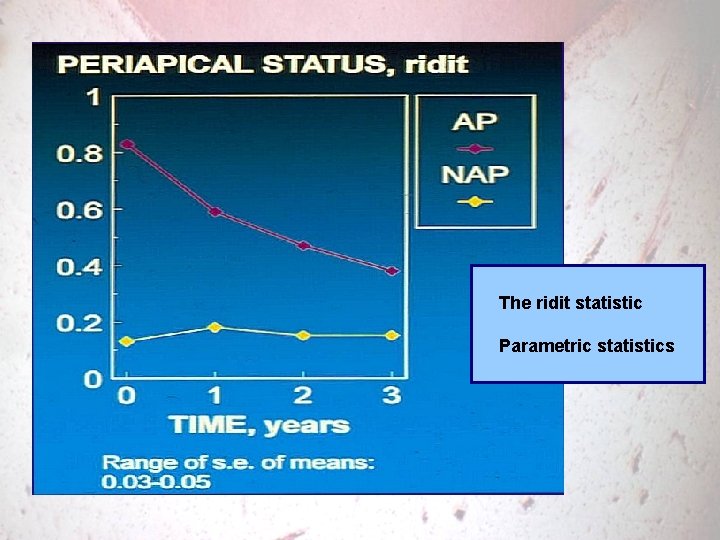
The ridit statistic Parametric statistics
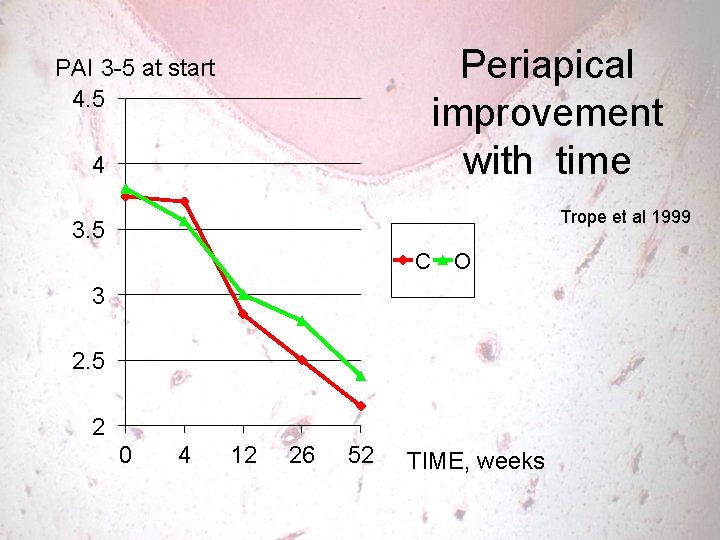
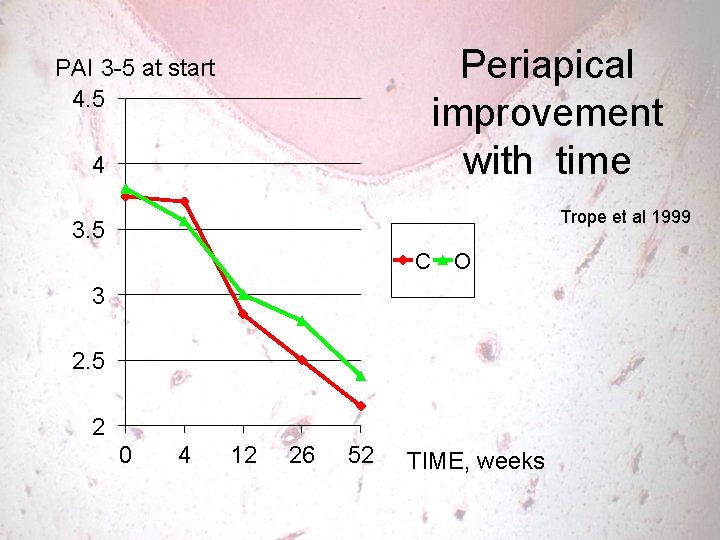
Periapical improvement with time PAI 3 -5 at start 4. 5 4 Trope et al 1999 3. 5 C O 3 2. 5 2 0 4 12 26 52 TIME, weeks
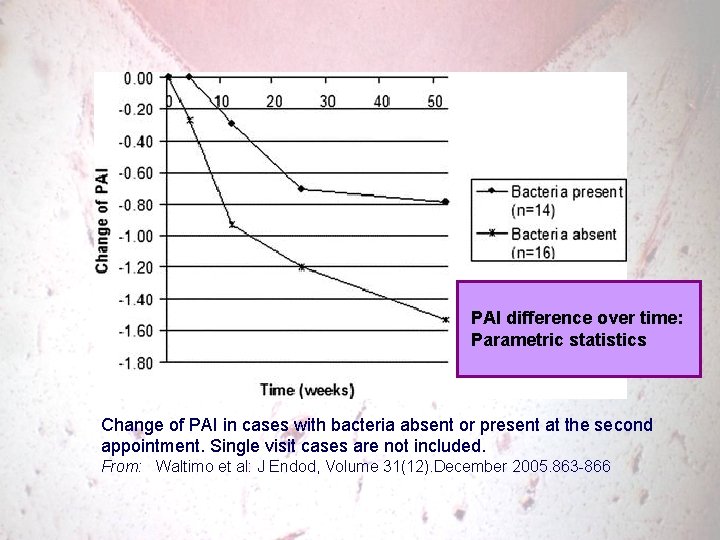
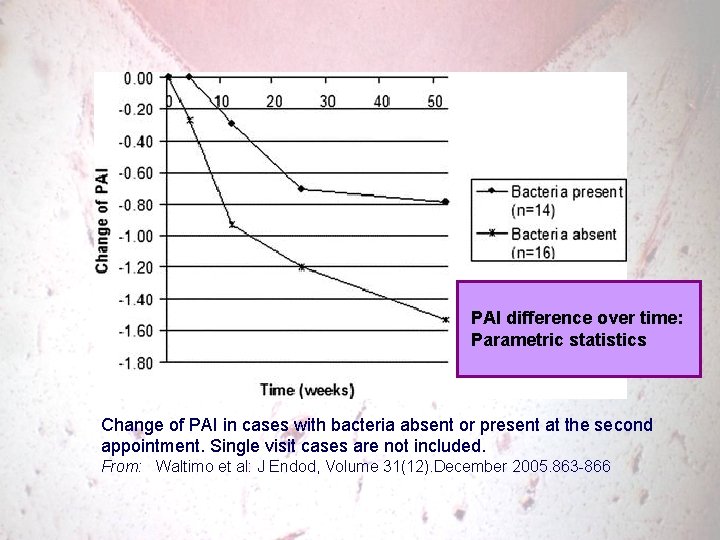
PAI difference over time: Parametric statistics Change of PAI in cases with bacteria absent or present at the second appointment. Single visit cases are not included. From: Waltimo et al: J Endod, Volume 31(12). December 2005. 863 -866
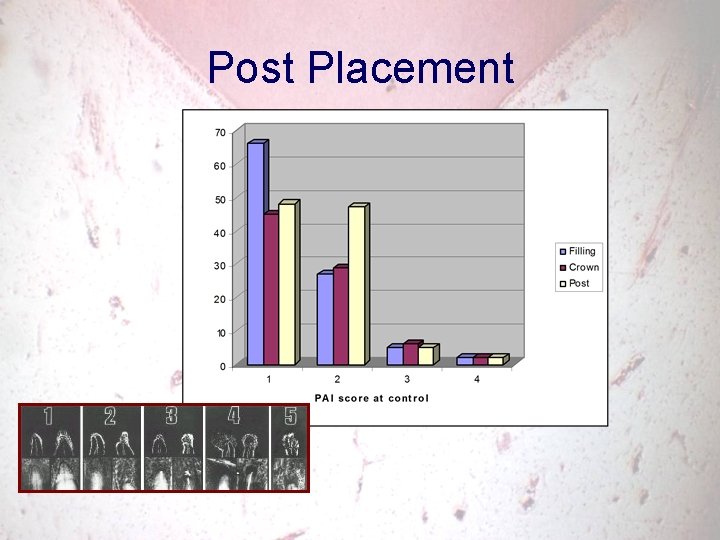
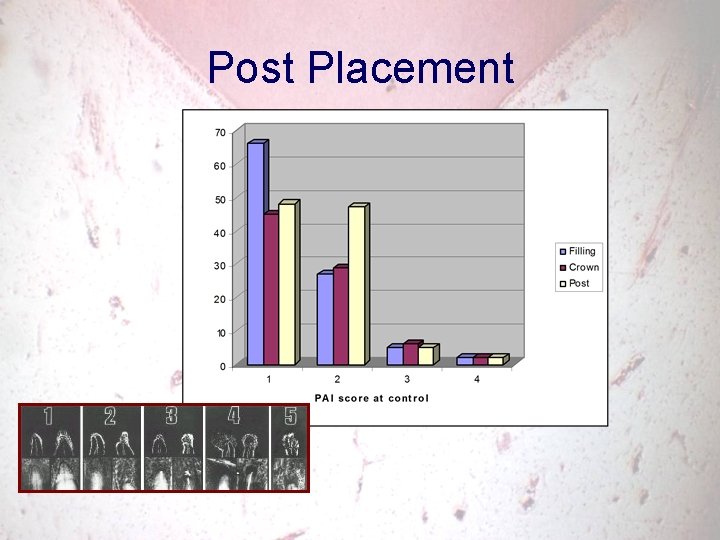
Post Placement
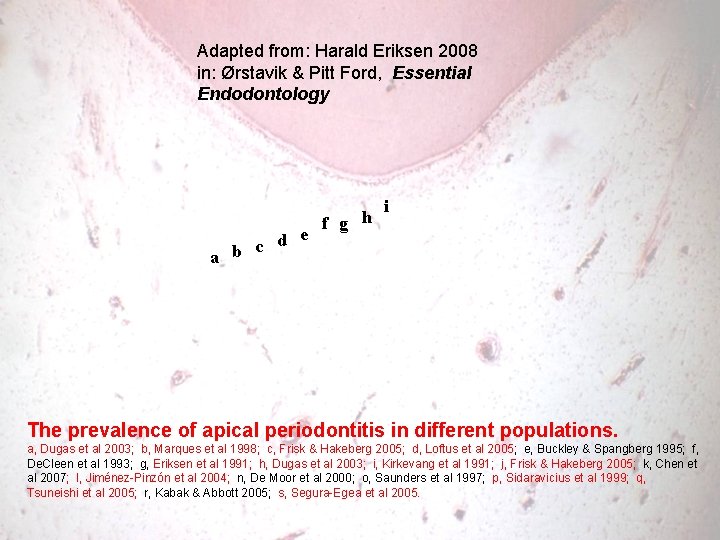
Adapted from: Harald Eriksen 2008 in: Ørstavik & Pitt Ford, Essential Endodontology d e c a b f g h i The prevalence of apical periodontitis in different populations. a, Dugas et al 2003; b, Marques et al 1998; c, Frisk & Hakeberg 2005; d, Loftus et al 2005; e, Buckley & Spangberg 1995; f, De. Cleen et al 1993; g, Eriksen et al 1991; h, Dugas et al 2003; i, Kirkevang et al 1991; j, Frisk & Hakeberg 2005; k, Chen et al 2007; l, Jiménez-Pinzón et al 2004; n, De Moor et al 2000; o, Saunders et al 1997; p, Sidaravicius et al 1999; q, Tsuneishi et al 2005; r, Kabak & Abbott 2005; s, Segura-Egea et al 2005.
Weaknesses of the PAI system • Front tooth reference only • Moderate specifity
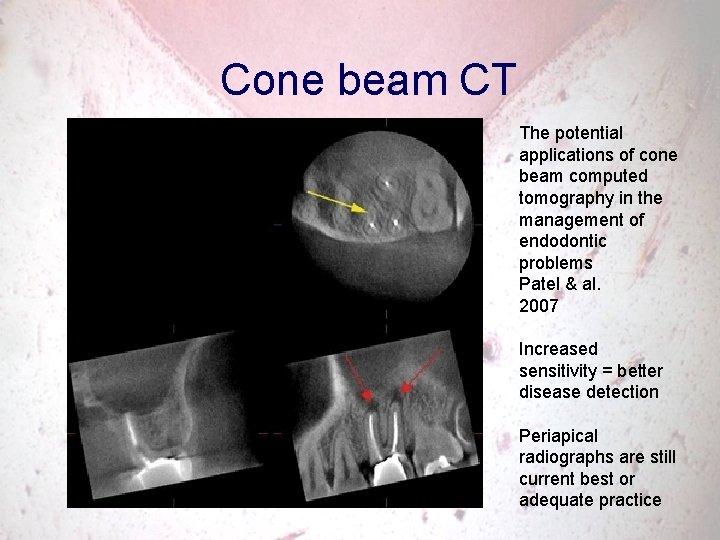
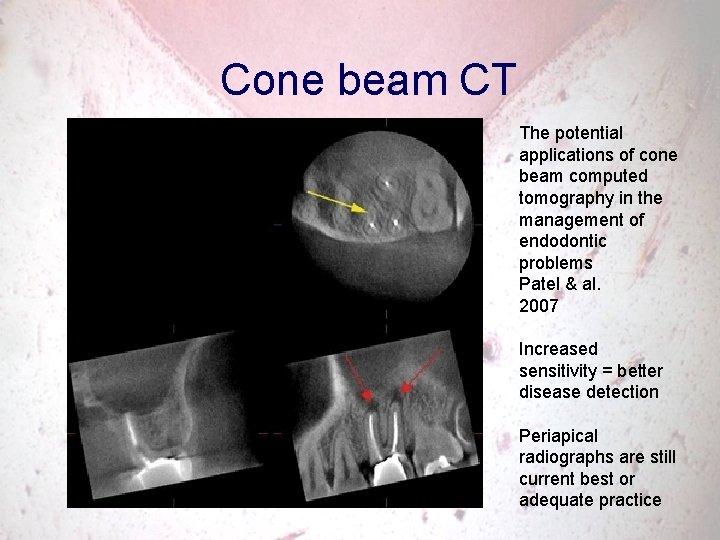
Cone beam CT The potential applications of cone beam computed tomography in the management of endodontic problems Patel & al. 2007 Increased sensitivity = better disease detection Periapical radiographs are still current best or adequate practice
3 The fundamental difference between prevention and treatment
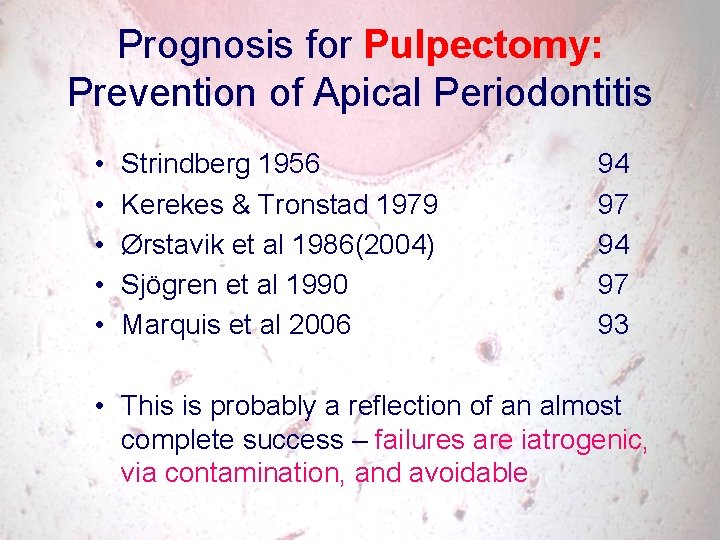
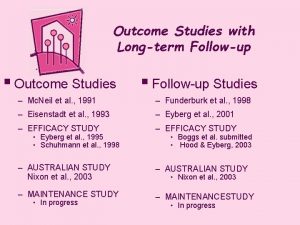
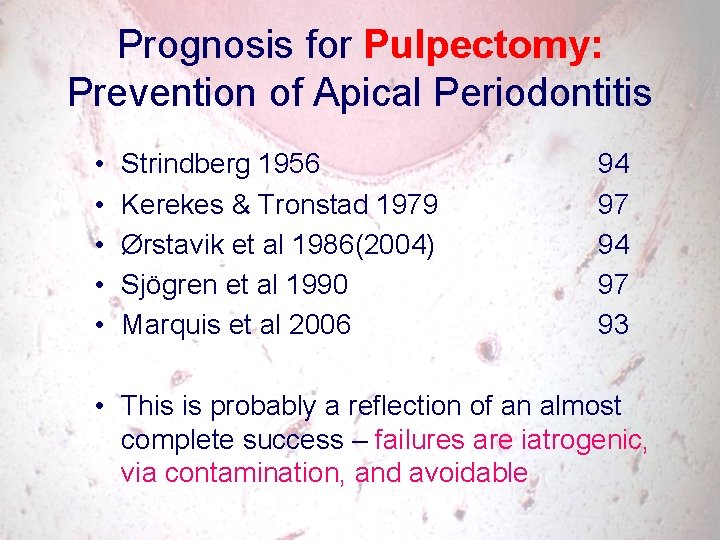
Prognosis for Pulpectomy: Prevention of Apical Periodontitis • • • Strindberg 1956 Kerekes & Tronstad 1979 Ørstavik et al 1986(2004) Sjögren et al 1990 Marquis et al 2006 94 97 93 • This is probably a reflection of an almost complete success – failures are iatrogenic, via contamination, and avoidable
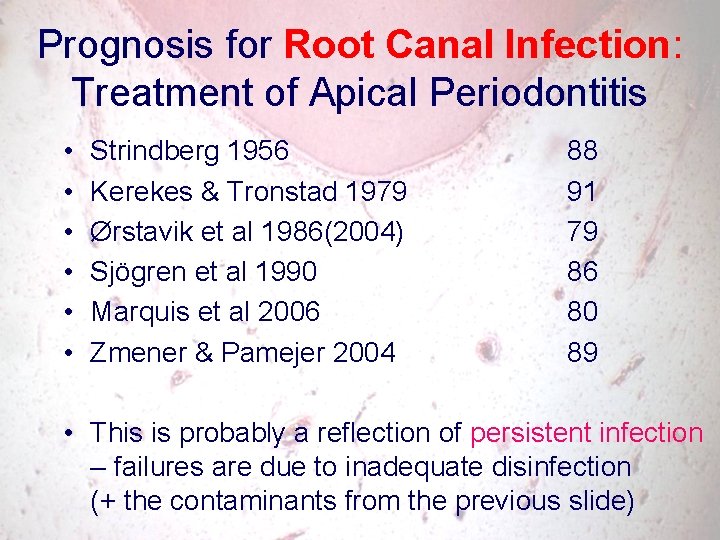
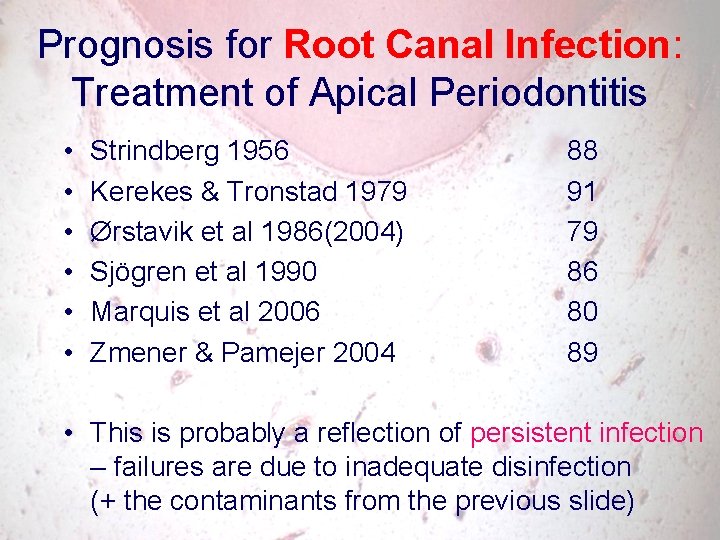
Prognosis for Root Canal Infection: Treatment of Apical Periodontitis • • • Strindberg 1956 Kerekes & Tronstad 1979 Ørstavik et al 1986(2004) Sjögren et al 1990 Marquis et al 2006 Zmener & Pamejer 2004 88 91 79 86 80 89 • This is probably a reflection of persistent infection – failures are due to inadequate disinfection (+ the contaminants from the previous slide)
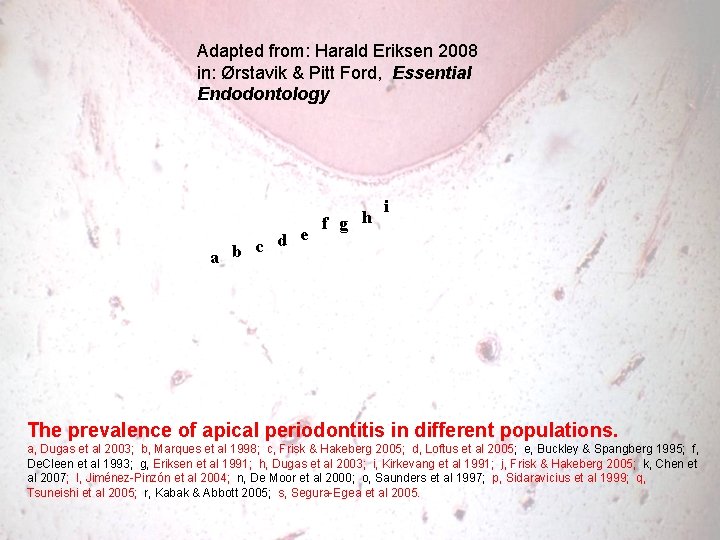
Adapted from: Harald Eriksen 2008 in: Ørstavik & Pitt Ford, Essential Endodontology d e c a b f g h i The prevalence of apical periodontitis in different populations. a, Dugas et al 2003; b, Marques et al 1998; c, Frisk & Hakeberg 2005; d, Loftus et al 2005; e, Buckley & Spangberg 1995; f, De. Cleen et al 1993; g, Eriksen et al 1991; h, Dugas et al 2003; i, Kirkevang et al 1991; j, Frisk & Hakeberg 2005; k, Chen et al 2007; l, Jiménez-Pinzón et al 2004; n, De Moor et al 2000; o, Saunders et al 1997; p, Sidaravicius et al 1999; q, Tsuneishi et al 2005; r, Kabak & Abbott 2005; s, Segura-Egea et al 2005.
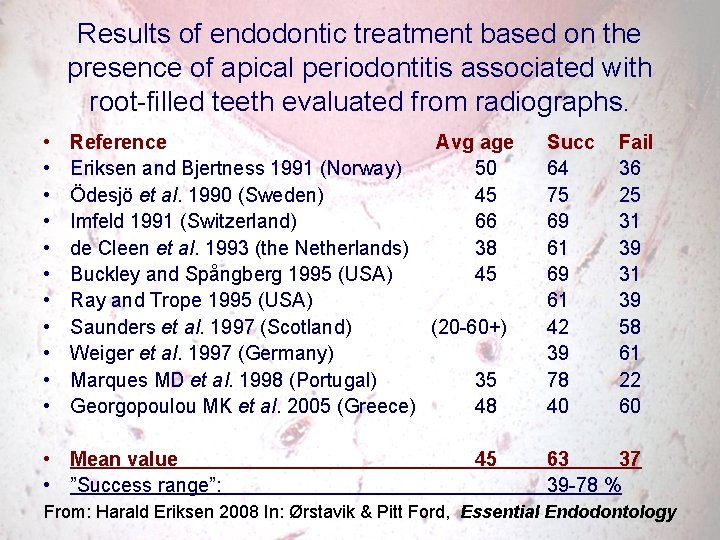
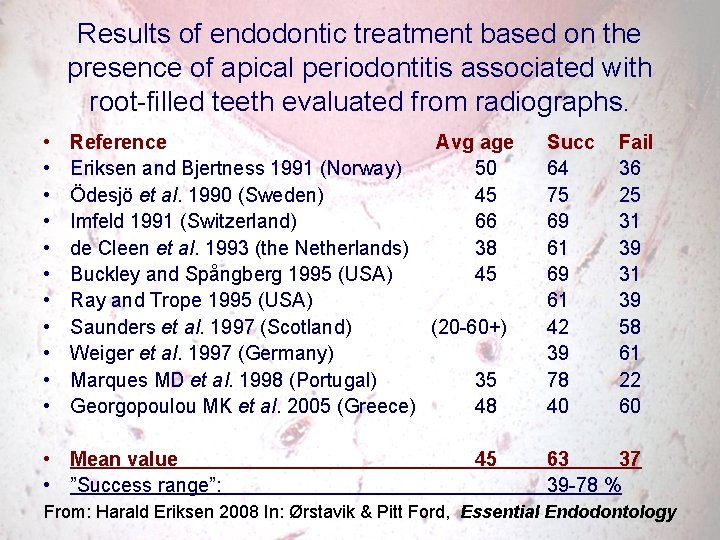
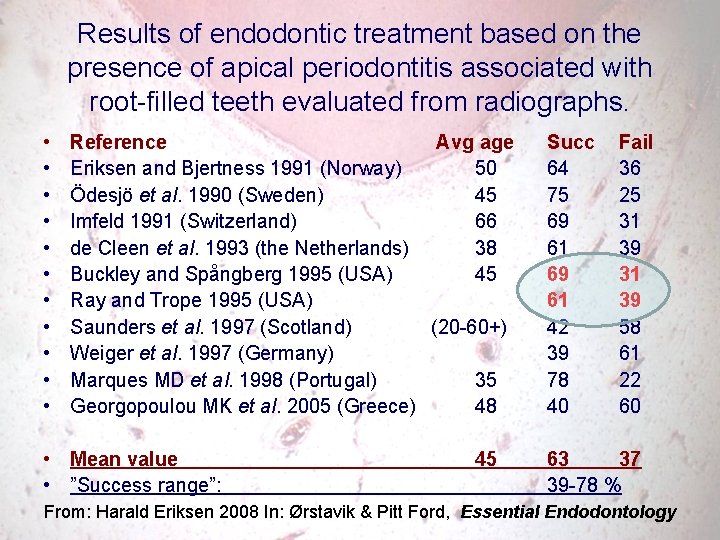
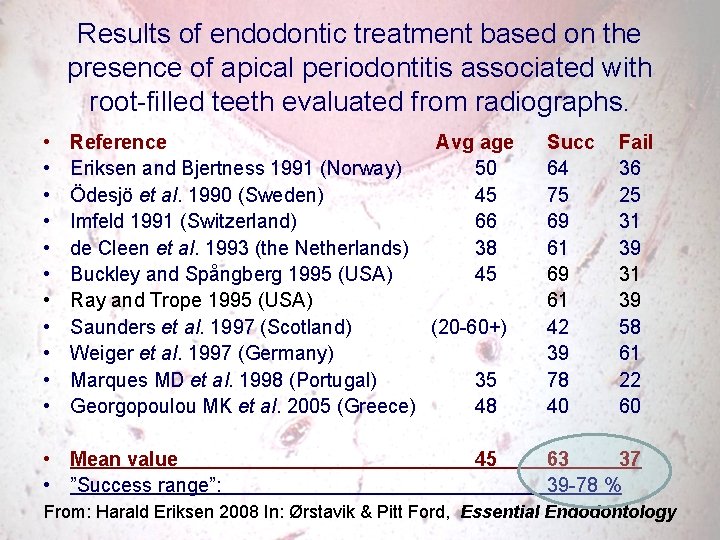
Results of endodontic treatment based on the presence of apical periodontitis associated with root-filled teeth evaluated from radiographs. • • • Reference Avg age Eriksen and Bjertness 1991 (Norway) 50 Ödesjö et al. 1990 (Sweden) 45 Imfeld 1991 (Switzerland) 66 de Cleen et al. 1993 (the Netherlands) 38 Buckley and Spångberg 1995 (USA) 45 Ray and Trope 1995 (USA) Saunders et al. 1997 (Scotland) (20 -60+) Weiger et al. 1997 (Germany) Marques MD et al. 1998 (Portugal) 35 Georgopoulou MK et al. 2005 (Greece) 48 • Mean value • ”Success range”: 45 Succ Fail 64 36 75 25 69 31 61 39 69 31 61 39 42 58 39 61 78 22 40 60 63 37 39 -78 % From: Harald Eriksen 2008 In: Ørstavik & Pitt Ford, Essential Endodontology
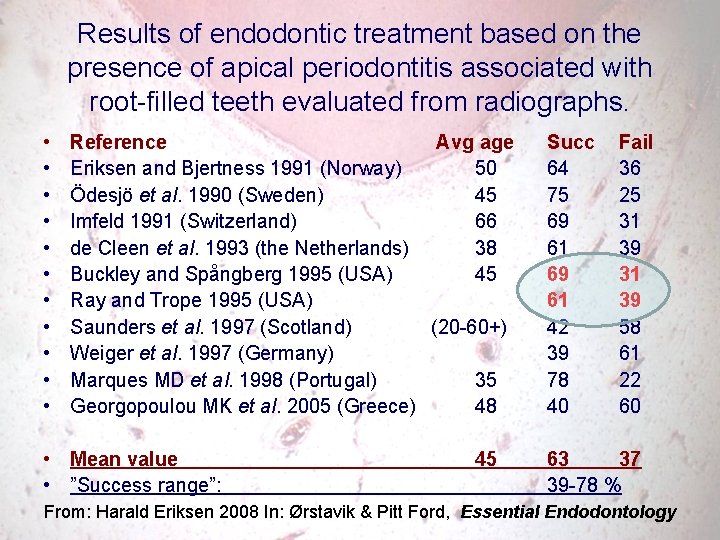
Results of endodontic treatment based on the presence of apical periodontitis associated with root-filled teeth evaluated from radiographs. • • • Reference Avg age Eriksen and Bjertness 1991 (Norway) 50 Ödesjö et al. 1990 (Sweden) 45 Imfeld 1991 (Switzerland) 66 de Cleen et al. 1993 (the Netherlands) 38 Buckley and Spångberg 1995 (USA) 45 Ray and Trope 1995 (USA) Saunders et al. 1997 (Scotland) (20 -60+) Weiger et al. 1997 (Germany) Marques MD et al. 1998 (Portugal) 35 Georgopoulou MK et al. 2005 (Greece) 48 • Mean value • ”Success range”: 45 Succ Fail 64 36 75 25 69 31 61 39 69 31 61 39 42 58 39 61 78 22 40 60 63 37 39 -78 % From: Harald Eriksen 2008 In: Ørstavik & Pitt Ford, Essential Endodontology
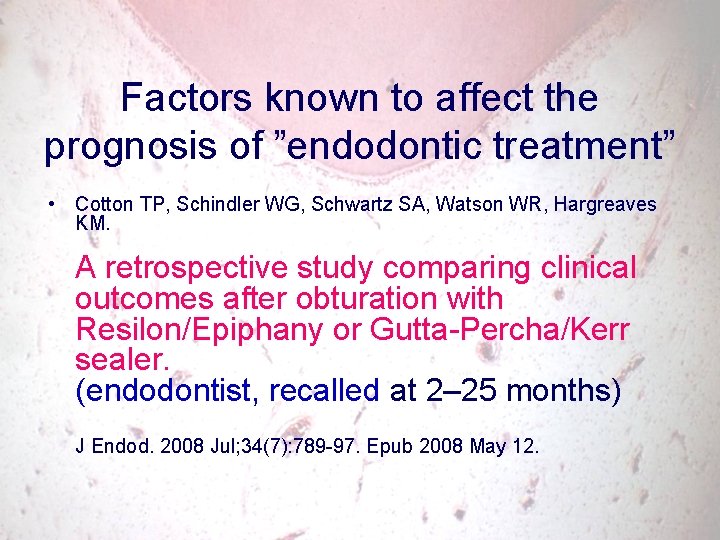
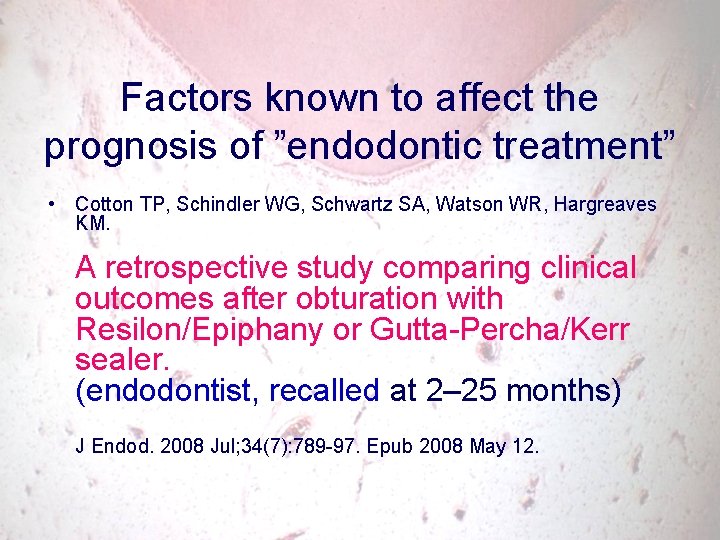
Factors known to affect the prognosis of ”endodontic treatment” • Cotton TP, Schindler WG, Schwartz SA, Watson WR, Hargreaves KM. A retrospective study comparing clinical outcomes after obturation with Resilon/Epiphany or Gutta-Percha/Kerr sealer. (endodontist, recalled at 2– 25 months) J Endod. 2008 Jul; 34(7): 789 -97. Epub 2008 May 12.
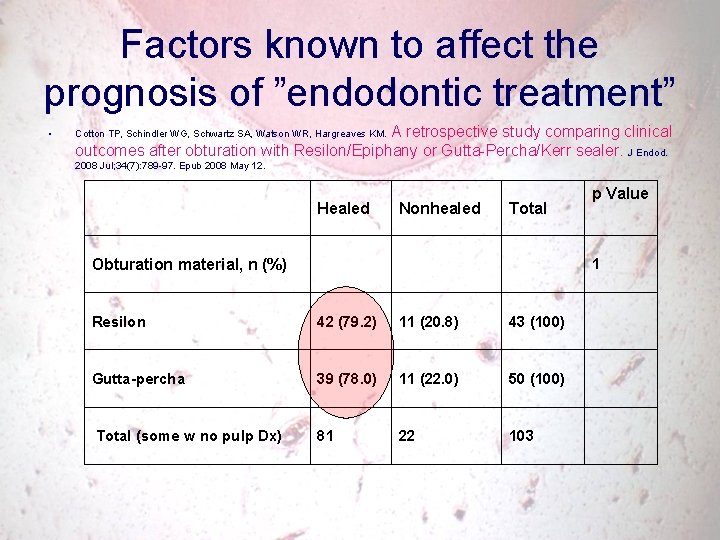
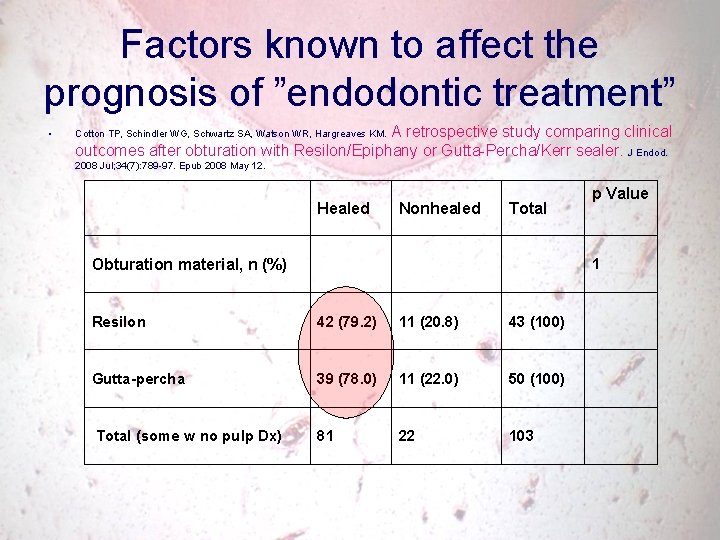
Factors known to affect the prognosis of ”endodontic treatment” • A retrospective study comparing clinical outcomes after obturation with Resilon/Epiphany or Gutta-Percha/Kerr sealer. J Endod. Cotton TP, Schindler WG, Schwartz SA, Watson WR, Hargreaves KM. 2008 Jul; 34(7): 789 -97. Epub 2008 May 12. Healed Nonhealed Total Obturation material, n (%) p Value 1 Resilon 42 (79. 2) 11 (20. 8) 43 (100) Gutta-percha 39 (78. 0) 11 (22. 0) 50 (100) Total (some w no pulp Dx) 81 22 103
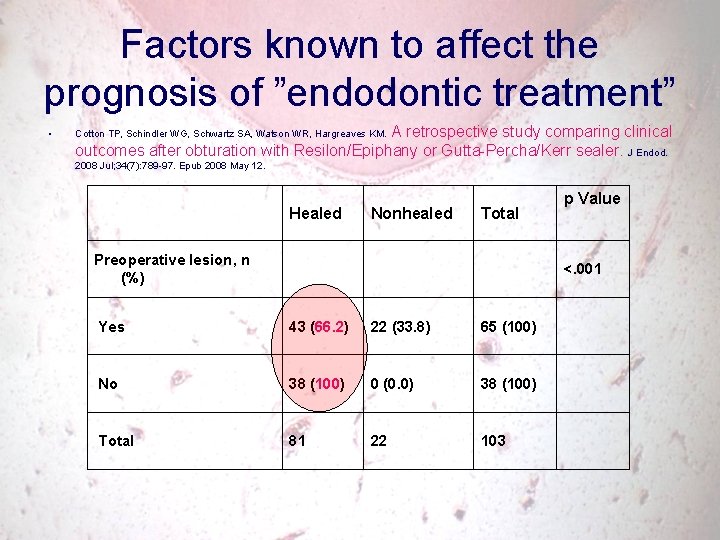
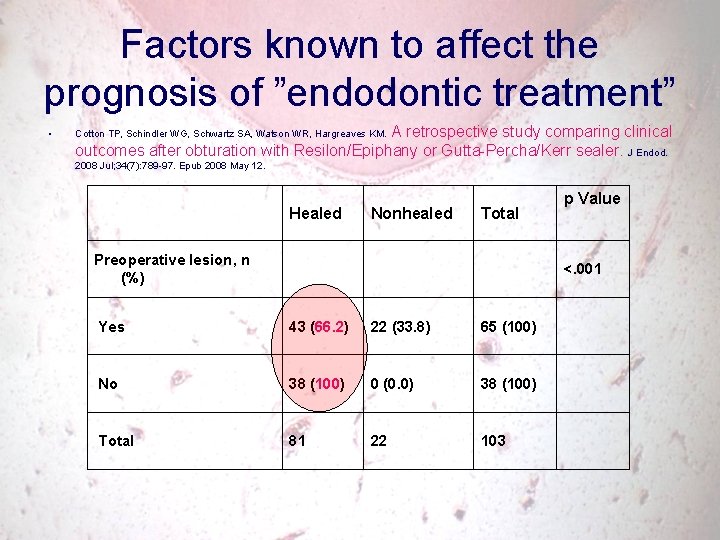
Factors known to affect the prognosis of ”endodontic treatment” • A retrospective study comparing clinical outcomes after obturation with Resilon/Epiphany or Gutta-Percha/Kerr sealer. J Endod. Cotton TP, Schindler WG, Schwartz SA, Watson WR, Hargreaves KM. 2008 Jul; 34(7): 789 -97. Epub 2008 May 12. Healed Nonhealed Total Preoperative lesion, n (%) p Value <. 001 Yes 43 (66. 2) 22 (33. 8) 65 (100) No 38 (100) 0 (0. 0) 38 (100) Total 81 22 103
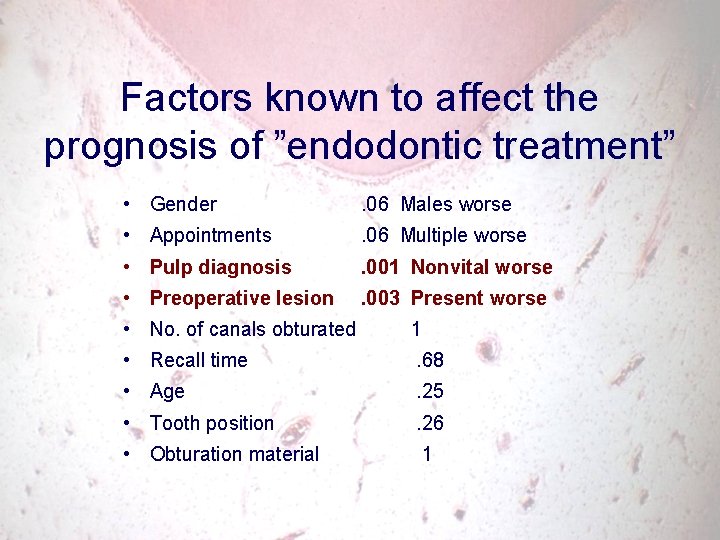
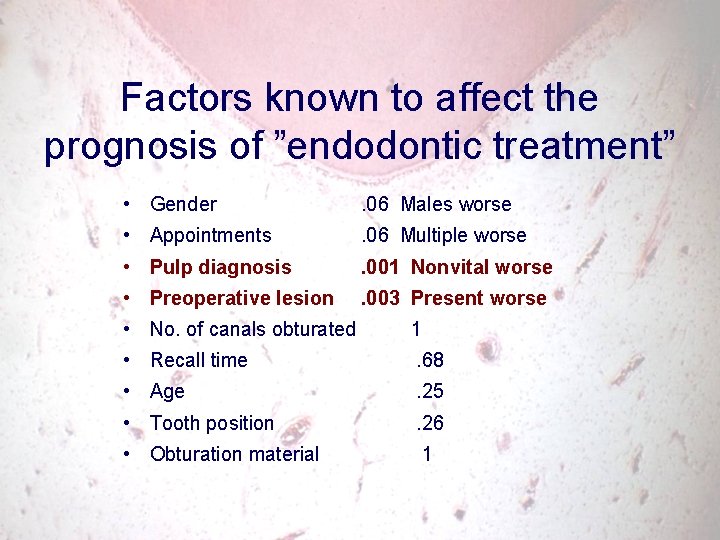
Factors known to affect the prognosis of ”endodontic treatment” • Gender . 06 Males worse • Appointments . 06 Multiple worse • Pulp diagnosis . 001 Nonvital worse • Preoperative lesion . 003 Present worse • No. of canals obturated 1 • Recall time . 68 • Age . 25 • Tooth position . 26 • Obturation material 1
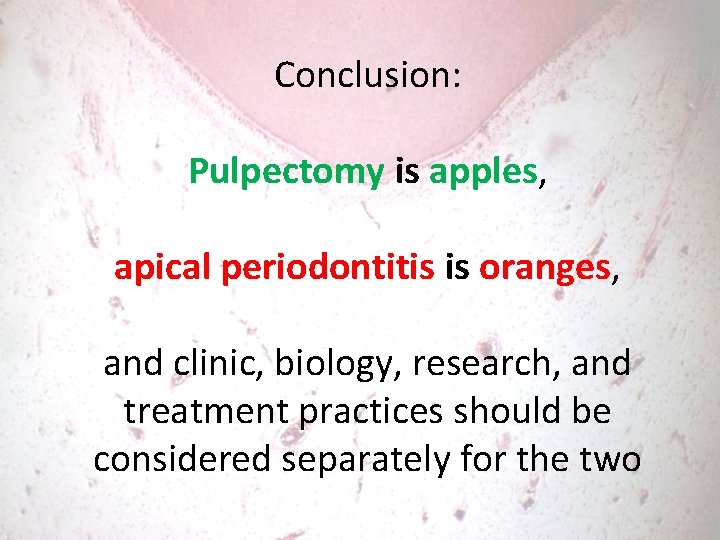
Conclusion: Pulpectomy is apples, apical periodontitis is oranges, and clinic, biology, research, and treatment practices should be considered separately for the two
4 Can we cure chronic apical periodontitis?
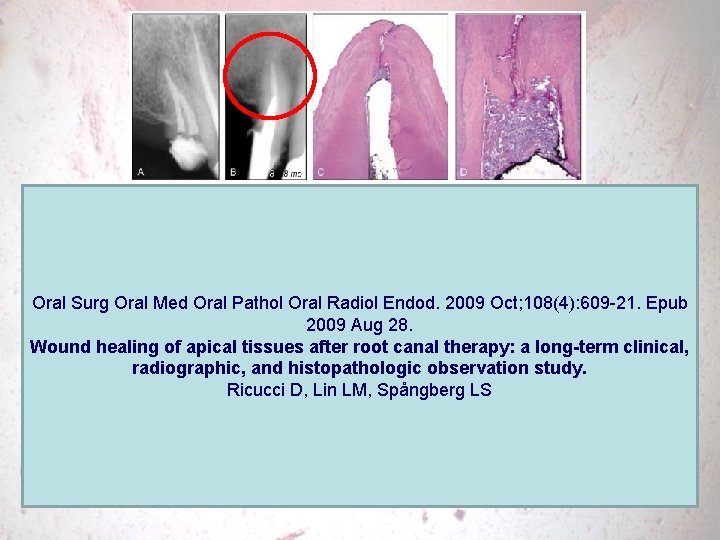
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Oct; 108(4): 609 -21. Epub 2009 Aug 28. Wound healing of apical tissues after root canal therapy: a long-term clinical, radiographic, and histopathologic observation study. Ricucci D, Lin LM, Spångberg LS

Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Oct; 108(4): 609 -21. Epub 2009 Aug 28. Wound healing of apical tissues after root canal therapy: a long-term clinical, radiographic, and histopathologic observation study. Ricucci D, Lin LM, Spångberg LS
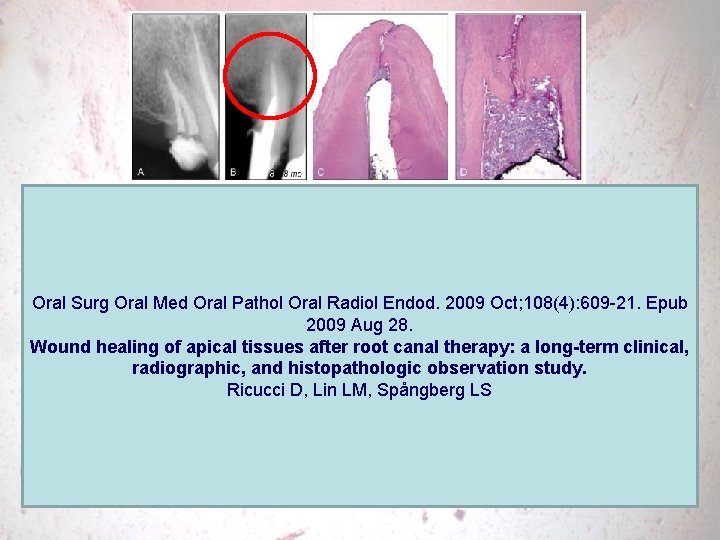
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Oct; 108(4): 609 -21. Epub 2009 Aug 28. Wound healing of apical tissues after root canal therapy: a long-term clinical, radiographic, and histopathologic observation study. Ricucci D, Lin LM, Spångberg LS


J Endod. 2009 Apr; 35(4): 493 -502. Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. Ricucci D, Siqueira JF Jr, Bate AL, Pitt Ford TR. This study intended to examine histologically root canal-treated teeth evincing apical periodontitis lesions and correlate the findings with clinical observations. Specimens were obtained from 24 patients (12 asymptomatic and 12 symptomatic) by extraction or endodontic surgery and consisted of roots or root tips and the associated pathologic lesion. Specimens were processed for histologic analysis, and serial sections were evaluated. Findings were correlated with clinical observations according to the presence or absence of symptoms. The mean period elapsed from treatment to specimen retrieval in the asymptomatic group was 7. 5 years, as compared with 2. 2 years in the symptomatic group.
J Endod. 2009 Apr; 35(4): 493 -502. Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. Ricucci D, Siqueira JF Jr, Bate AL, Pitt Ford TR. All specimens exhibited periradicular inflammation. Bacteria were visualized in all cases, except for 1 specimen from the asymptomatic group in which a foreign body reaction to overfilled material was the probable reason for emergent disease in a previously vital case. Irrespective of the presence of symptoms, bacteria were always located within the root canal system, although they were also observed in the periradicular tissues in 1 asymptomatic and 4 symptomatic teeth. In general, intraradicular bacterial colonization was heavier in symptomatic failed teeth. The present findings support the role of intraradicular infections, usually in the form of biofilms, as the primary cause of endodontic treatment failure.
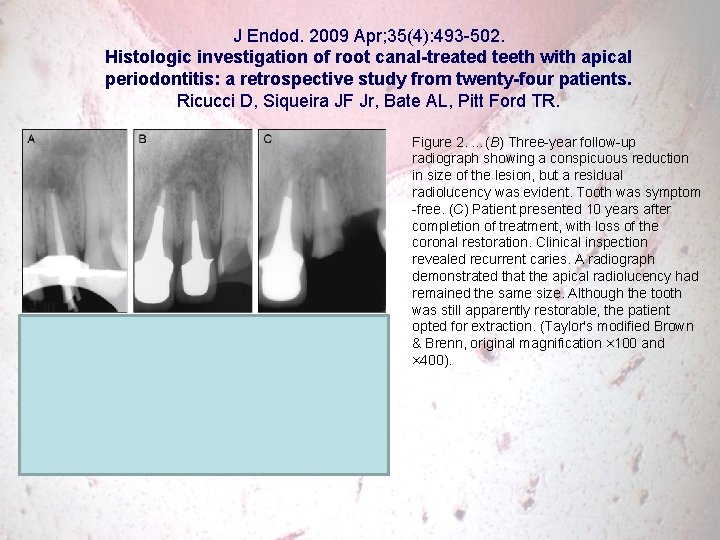
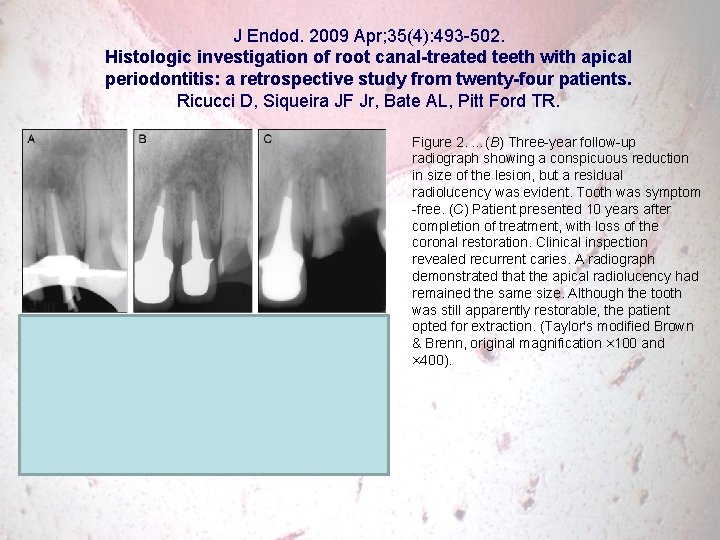
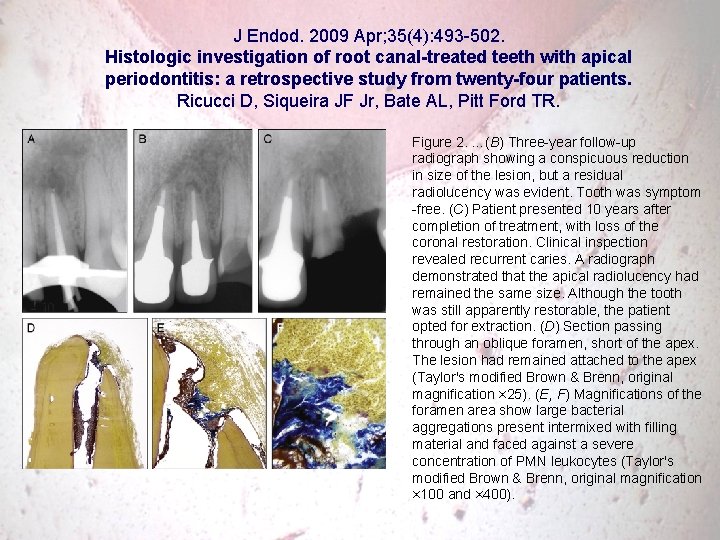
J Endod. 2009 Apr; 35(4): 493 -502. Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. Ricucci D, Siqueira JF Jr, Bate AL, Pitt Ford TR. Figure 2. …(B) Three-year follow-up radiograph showing a conspicuous reduction in size of the lesion, but a residual radiolucency was evident. Tooth was symptom -free. (C) Patient presented 10 years after completion of treatment, with loss of the coronal restoration. Clinical inspection revealed recurrent caries. A radiograph demonstrated that the apical radiolucency had remained the same size. Although the tooth was still apparently restorable, the patient opted for extraction. (Taylor's modified Brown & Brenn, original magnification × 100 and × 400).
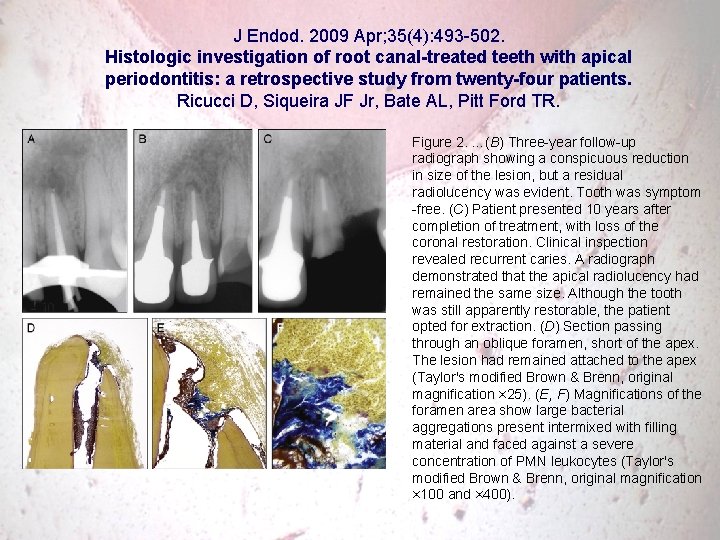
J Endod. 2009 Apr; 35(4): 493 -502. Histologic investigation of root canal-treated teeth with apical periodontitis: a retrospective study from twenty-four patients. Ricucci D, Siqueira JF Jr, Bate AL, Pitt Ford TR. Figure 2. …(B) Three-year follow-up radiograph showing a conspicuous reduction in size of the lesion, but a residual radiolucency was evident. Tooth was symptom -free. (C) Patient presented 10 years after completion of treatment, with loss of the coronal restoration. Clinical inspection revealed recurrent caries. A radiograph demonstrated that the apical radiolucency had remained the same size. Although the tooth was still apparently restorable, the patient opted for extraction. (D) Section passing through an oblique foramen, short of the apex. The lesion had remained attached to the apex (Taylor's modified Brown & Brenn, original magnification × 25). (E, F) Magnifications of the foramen area show large bacterial aggregations present intermixed with filling material and faced against a severe concentration of PMN leukocytes (Taylor's modified Brown & Brenn, original magnification × 100 and × 400).
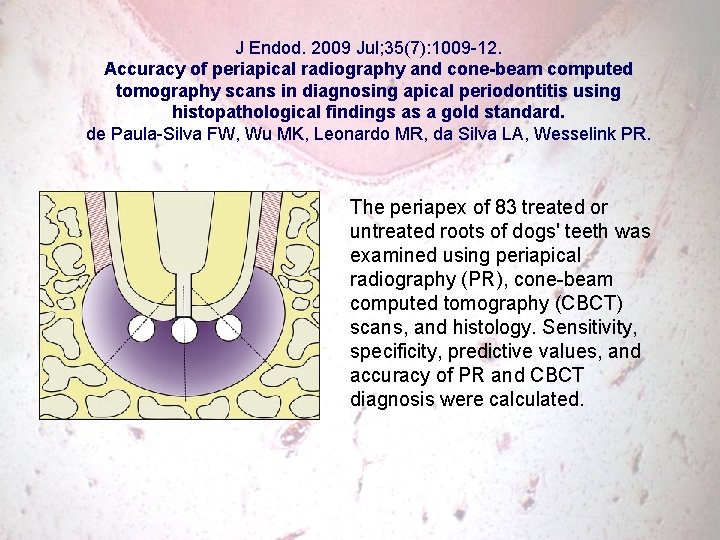
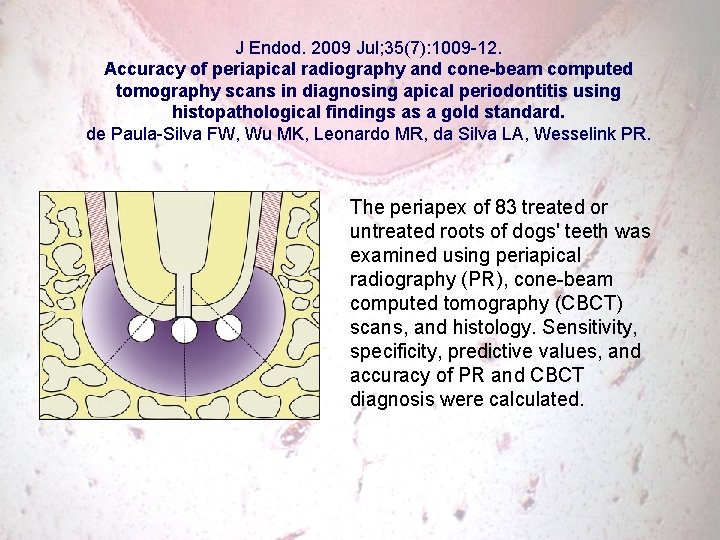
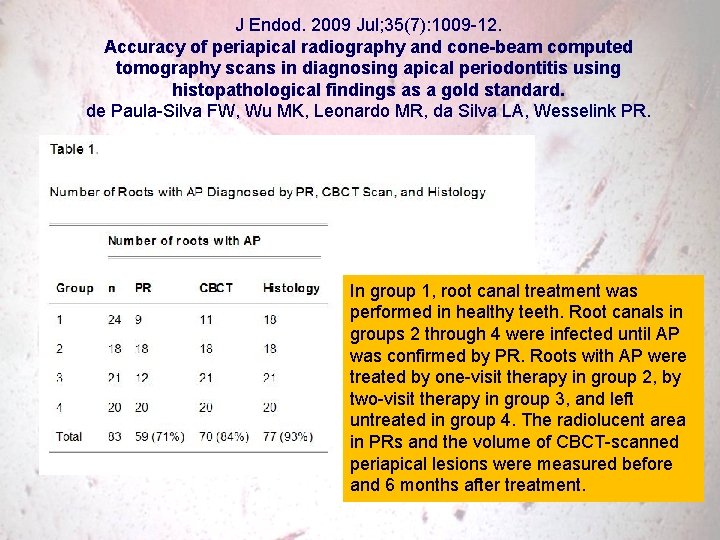
J Endod. 2009 Jul; 35(7): 1009 -12. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. de Paula-Silva FW, Wu MK, Leonardo MR, da Silva LA, Wesselink PR. The periapex of 83 treated or untreated roots of dogs' teeth was examined using periapical radiography (PR), cone-beam computed tomography (CBCT) scans, and histology. Sensitivity, specificity, predictive values, and accuracy of PR and CBCT diagnosis were calculated.
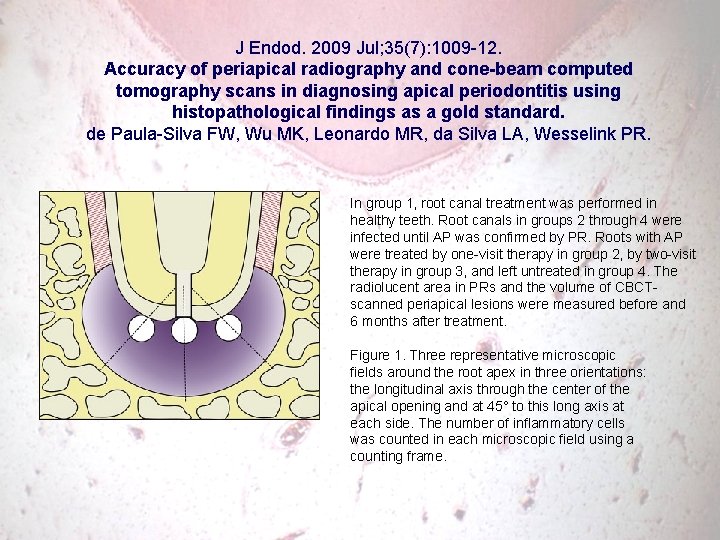
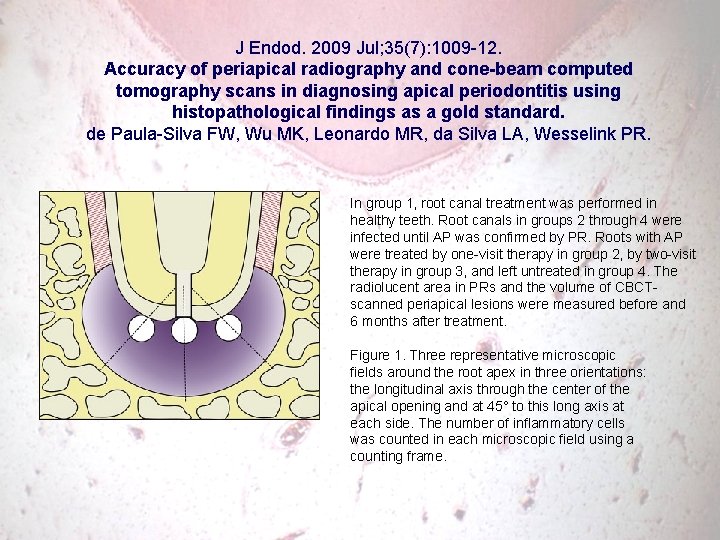
J Endod. 2009 Jul; 35(7): 1009 -12. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. de Paula-Silva FW, Wu MK, Leonardo MR, da Silva LA, Wesselink PR. In group 1, root canal treatment was performed in healthy teeth. Root canals in groups 2 through 4 were infected until AP was confirmed by PR. Roots with AP were treated by one-visit therapy in group 2, by two-visit therapy in group 3, and left untreated in group 4. The radiolucent area in PRs and the volume of CBCTscanned periapical lesions were measured before and 6 months after treatment. Figure 1. Three representative microscopic fields around the root apex in three orientations: the longitudinal axis through the center of the apical opening and at 45° to this long axis at each side. The number of inflammatory cells was counted in each microscopic field using a counting frame.
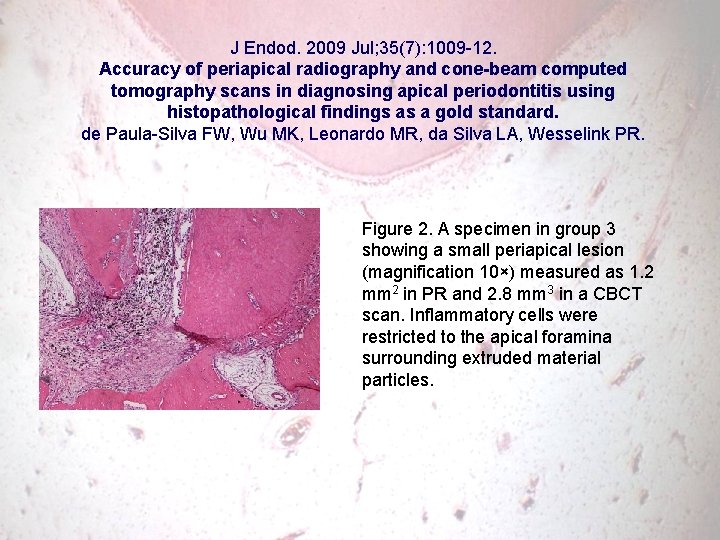
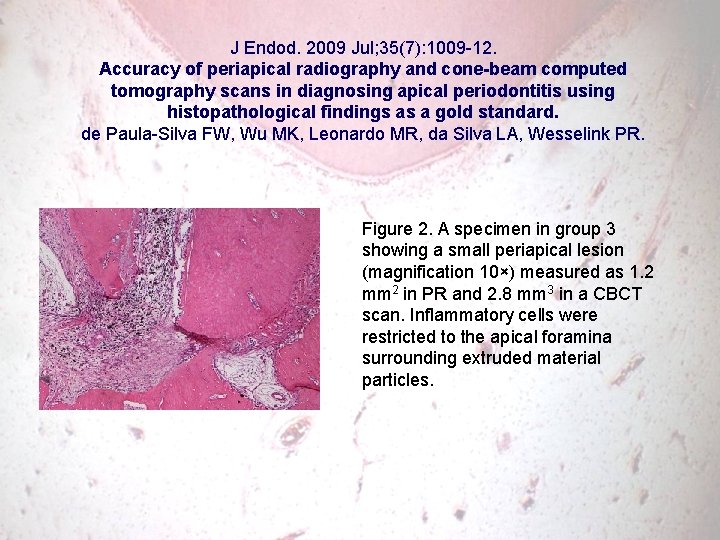
J Endod. 2009 Jul; 35(7): 1009 -12. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. de Paula-Silva FW, Wu MK, Leonardo MR, da Silva LA, Wesselink PR. Figure 2. A specimen in group 3 showing a small periapical lesion (magnification 10×) measured as 1. 2 mm 2 in PR and 2. 8 mm 3 in a CBCT scan. Inflammatory cells were restricted to the apical foramina surrounding extruded material particles.
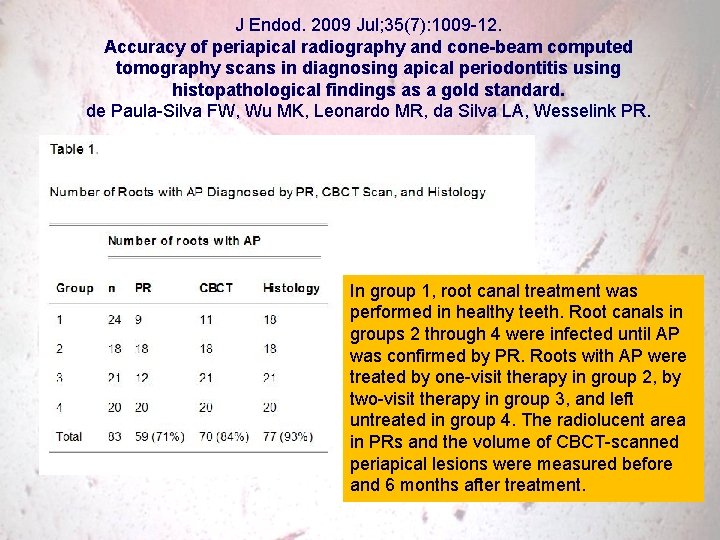
J Endod. 2009 Jul; 35(7): 1009 -12. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. de Paula-Silva FW, Wu MK, Leonardo MR, da Silva LA, Wesselink PR. In group 1, root canal treatment was performed in healthy teeth. Root canals in groups 2 through 4 were infected until AP was confirmed by PR. Roots with AP were treated by one-visit therapy in group 2, by two-visit therapy in group 3, and left untreated in group 4. The radiolucent area in PRs and the volume of CBCT-scanned periapical lesions were measured before and 6 months after treatment.
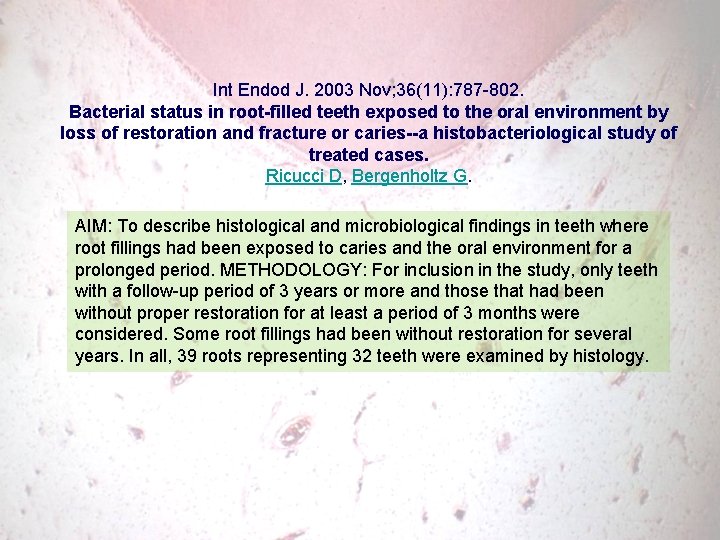
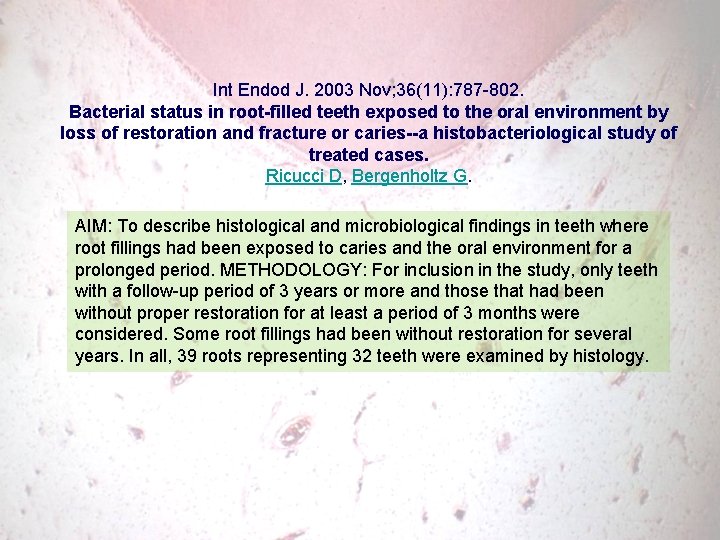
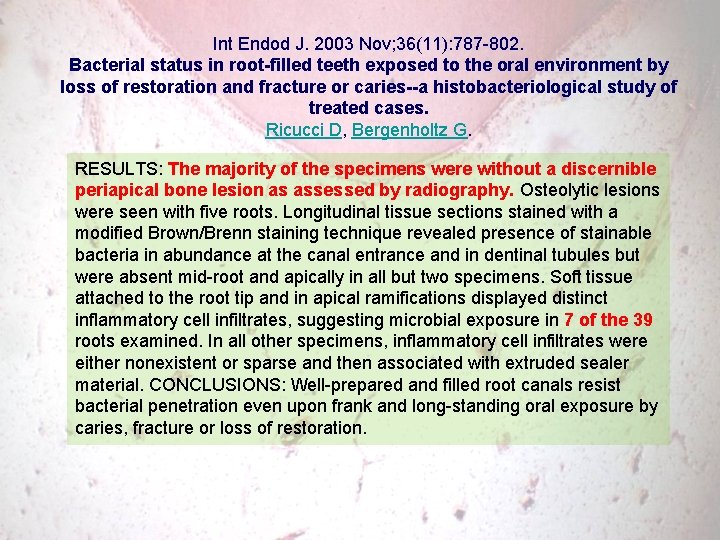
Int Endod J. 2003 Nov; 36(11): 787 -802. Bacterial status in root-filled teeth exposed to the oral environment by loss of restoration and fracture or caries--a histobacteriological study of treated cases. Ricucci D, Bergenholtz G. AIM: To describe histological and microbiological findings in teeth where root fillings had been exposed to caries and the oral environment for a prolonged period. METHODOLOGY: For inclusion in the study, only teeth with a follow-up period of 3 years or more and those that had been without proper restoration for at least a period of 3 months were considered. Some root fillings had been without restoration for several years. In all, 39 roots representing 32 teeth were examined by histology.
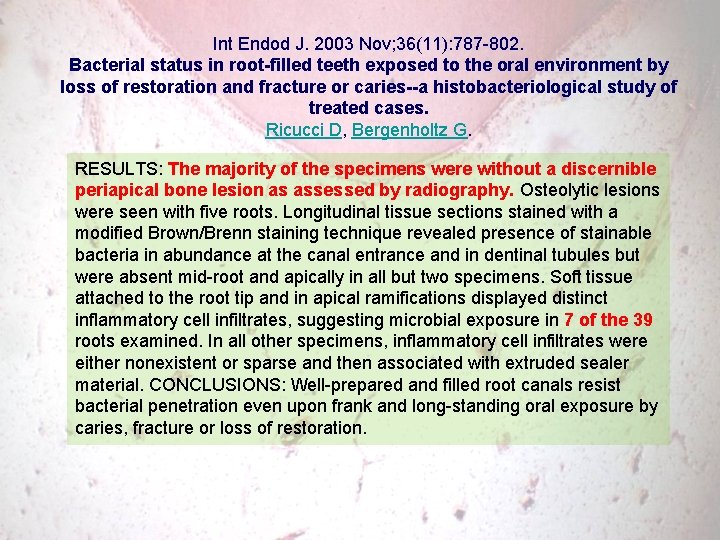
Int Endod J. 2003 Nov; 36(11): 787 -802. Bacterial status in root-filled teeth exposed to the oral environment by loss of restoration and fracture or caries--a histobacteriological study of treated cases. Ricucci D, Bergenholtz G. RESULTS: The majority of the specimens were without a discernible periapical bone lesion as assessed by radiography. Osteolytic lesions were seen with five roots. Longitudinal tissue sections stained with a modified Brown/Brenn staining technique revealed presence of stainable bacteria in abundance at the canal entrance and in dentinal tubules but were absent mid-root and apically in all but two specimens. Soft tissue attached to the root tip and in apical ramifications displayed distinct inflammatory cell infiltrates, suggesting microbial exposure in 7 of the 39 roots examined. In all other specimens, inflammatory cell infiltrates were either nonexistent or sparse and then associated with extruded sealer material. CONCLUSIONS: Well-prepared and filled root canals resist bacterial penetration even upon frank and long-standing oral exposure by caries, fracture or loss of restoration.
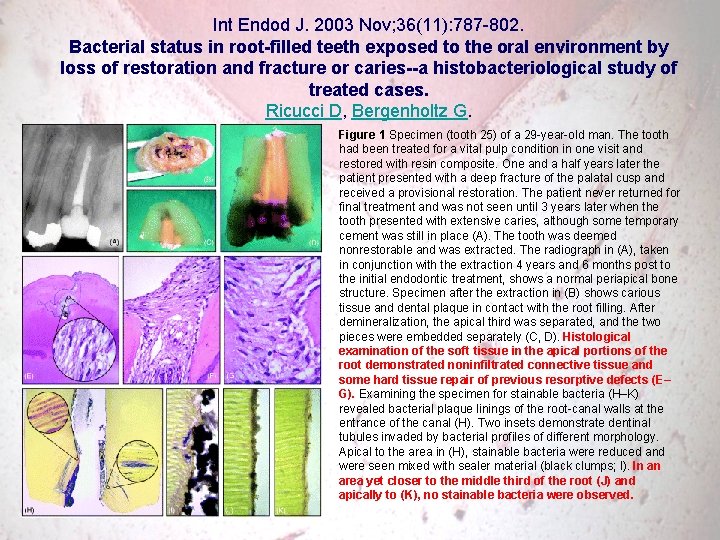
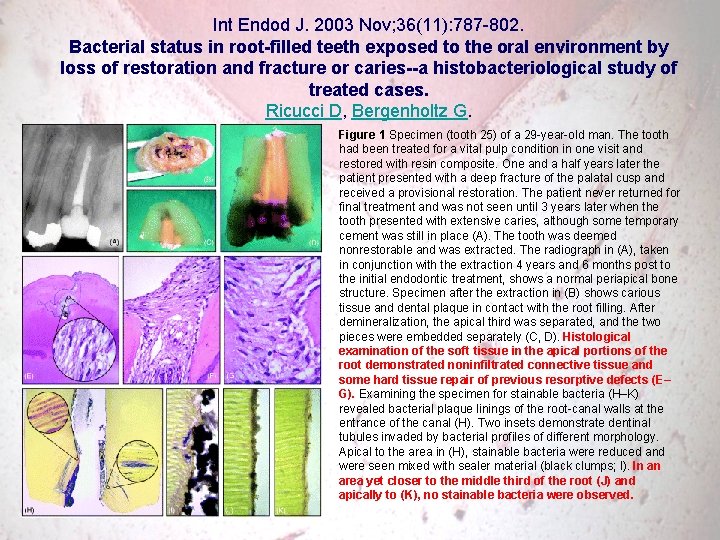
Int Endod J. 2003 Nov; 36(11): 787 -802. Bacterial status in root-filled teeth exposed to the oral environment by loss of restoration and fracture or caries--a histobacteriological study of treated cases. Ricucci D, Bergenholtz G. Figure 1 Specimen (tooth 25) of a 29 -year-old man. The tooth had been treated for a vital pulp condition in one visit and restored with resin composite. One and a half years later the patient presented with a deep fracture of the palatal cusp and received a provisional restoration. The patient never returned for final treatment and was not seen until 3 years later when the tooth presented with extensive caries, although some temporary cement was still in place (A). The tooth was deemed nonrestorable and was extracted. The radiograph in (A), taken in conjunction with the extraction 4 years and 6 months post to the initial endodontic treatment, shows a normal periapical bone structure. Specimen after the extraction in (B) shows carious tissue and dental plaque in contact with the root filling. After demineralization, the apical third was separated, and the two pieces were embedded separately (C, D). Histological examination of the soft tissue in the apical portions of the root demonstrated noninfiltrated connective tissue and some hard tissue repair of previous resorptive defects (E– G). Examining the specimen for stainable bacteria (H–K) revealed bacterial plaque linings of the root-canal walls at the entrance of the canal (H). Two insets demonstrate dentinal tubules invaded by bacterial profiles of different morphology. Apical to the area in (H), stainable bacteria were reduced and were seen mixed with sealer material (black clumps; I). In an area yet closer to the middle third of the root (J) and apically to (K), no stainable bacteria were observed.
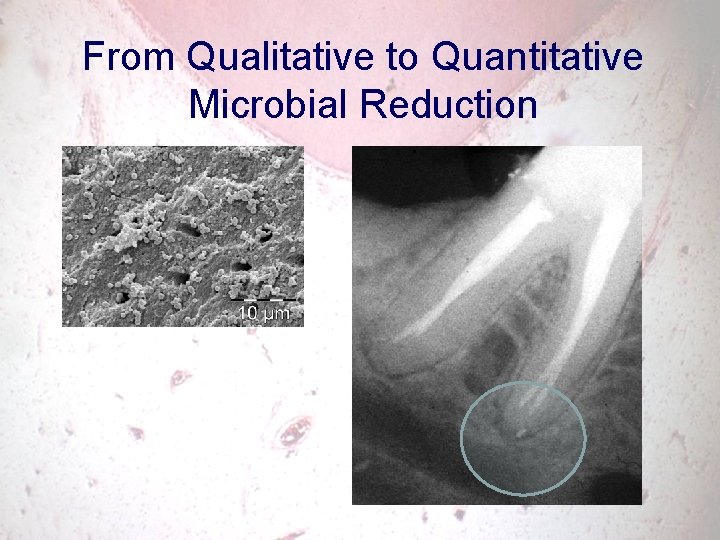
5 From qualitative to quantitative microbial control
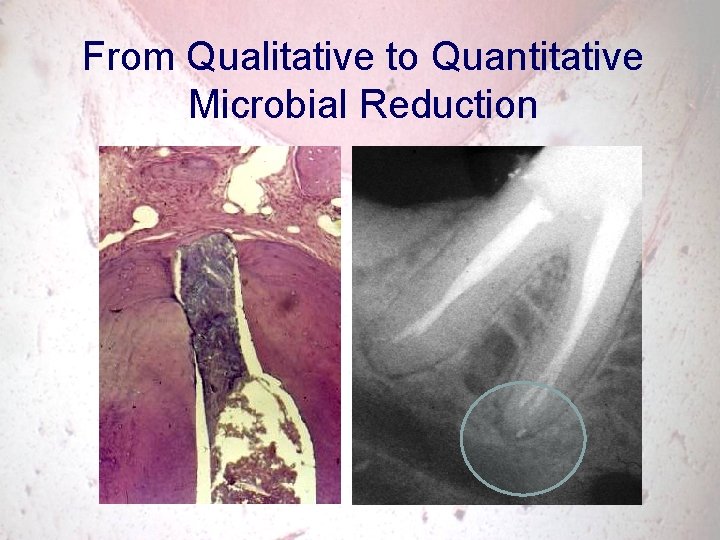
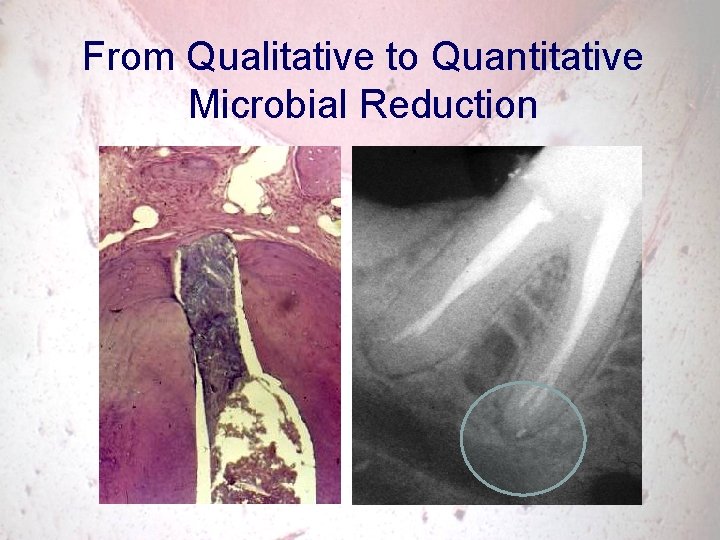
From Qualitative to Quantitative Microbial Reduction
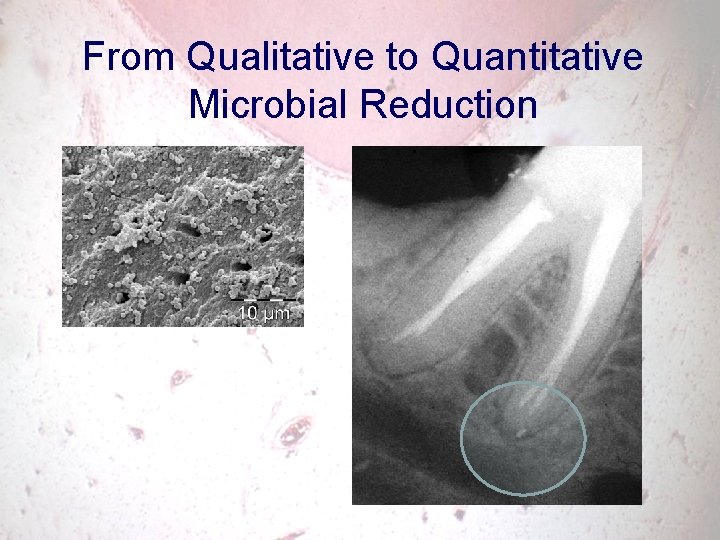
From Qualitative to Quantitative Microbial Reduction
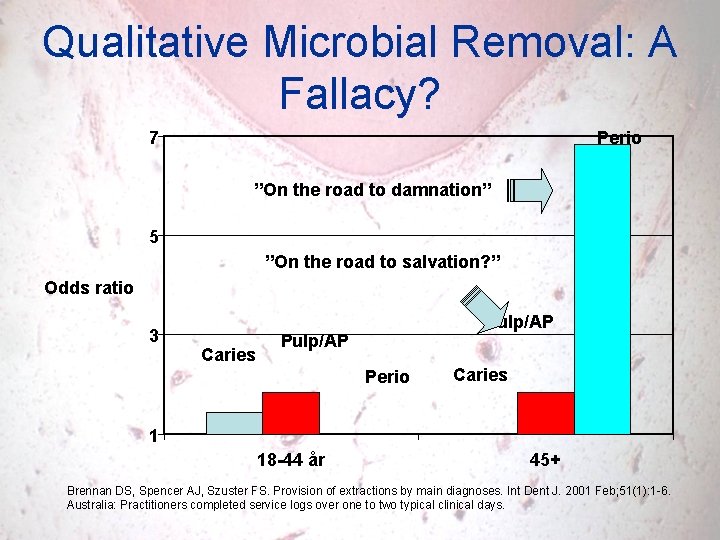
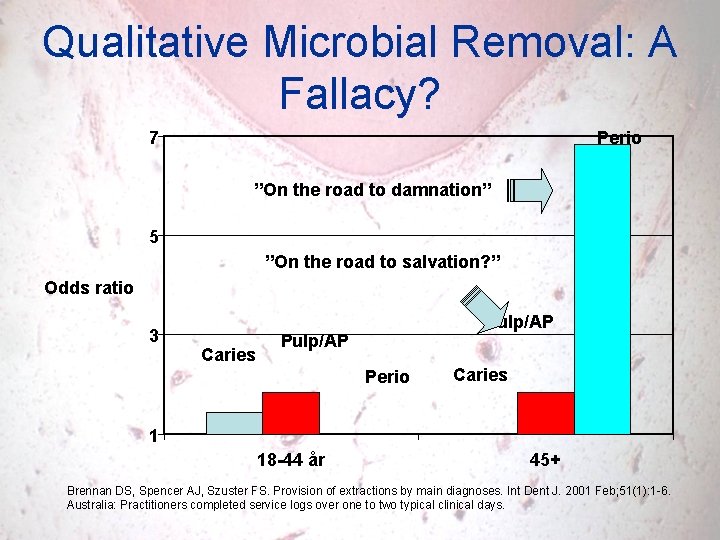
Qualitative Microbial Removal: A Fallacy? 7 Perio ”On the road to damnation” 5 ”On the road to salvation? ” Odds ratio 3 Caries Pulp/AP Perio Caries 1 18 -44 år 45+ Brennan DS, Spencer AJ, Szuster FS. Provision of extractions by main diagnoses. Int Dent J. 2001 Feb; 51(1): 1 -6. Australia: Practitioners completed service logs over one to two typical clinical days.
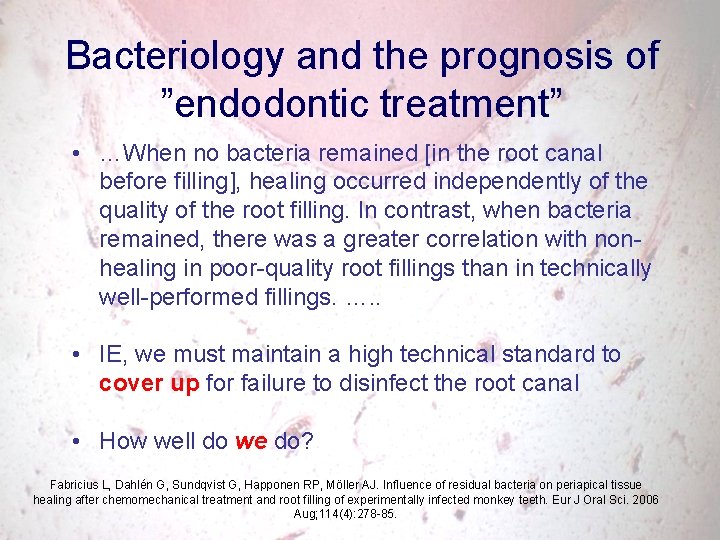
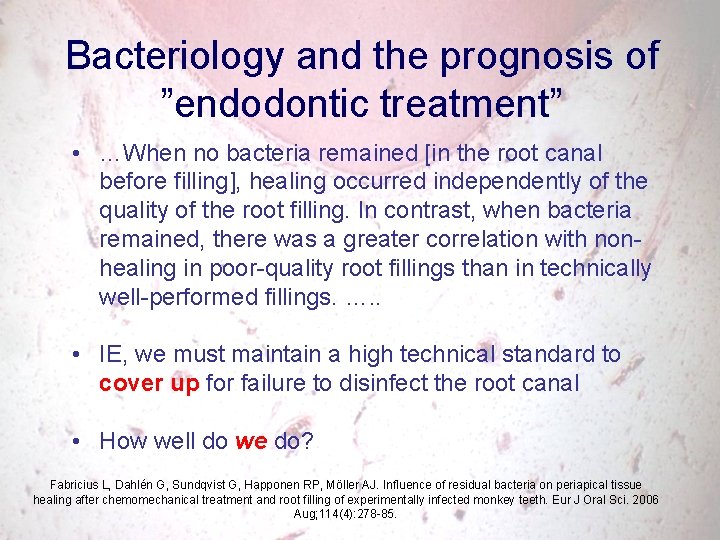
Bacteriology and the prognosis of ”endodontic treatment” • …When no bacteria remained [in the root canal before filling], healing occurred independently of the quality of the root filling. In contrast, when bacteria remained, there was a greater correlation with nonhealing in poor-quality root fillings than in technically well-performed fillings. …. . • IE, we must maintain a high technical standard to cover up for failure to disinfect the root canal • How well do we do? Fabricius L, Dahlén G, Sundqvist G, Happonen RP, Möller AJ. Influence of residual bacteria on periapical tissue healing after chemomechanical treatment and root filling of experimentally infected monkey teeth. Eur J Oral Sci. 2006 Aug; 114(4): 278 -85.
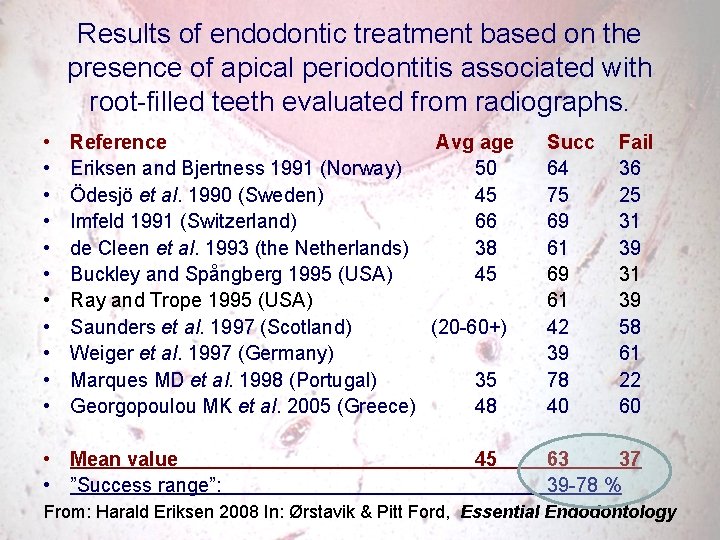
Results of endodontic treatment based on the presence of apical periodontitis associated with root-filled teeth evaluated from radiographs. • • • Reference Avg age Eriksen and Bjertness 1991 (Norway) 50 Ödesjö et al. 1990 (Sweden) 45 Imfeld 1991 (Switzerland) 66 de Cleen et al. 1993 (the Netherlands) 38 Buckley and Spångberg 1995 (USA) 45 Ray and Trope 1995 (USA) Saunders et al. 1997 (Scotland) (20 -60+) Weiger et al. 1997 (Germany) Marques MD et al. 1998 (Portugal) 35 Georgopoulou MK et al. 2005 (Greece) 48 • Mean value • ”Success range”: 45 Succ Fail 64 36 75 25 69 31 61 39 69 31 61 39 42 58 39 61 78 22 40 60 63 37 39 -78 % From: Harald Eriksen 2008 In: Ørstavik & Pitt Ford, Essential Endodontology
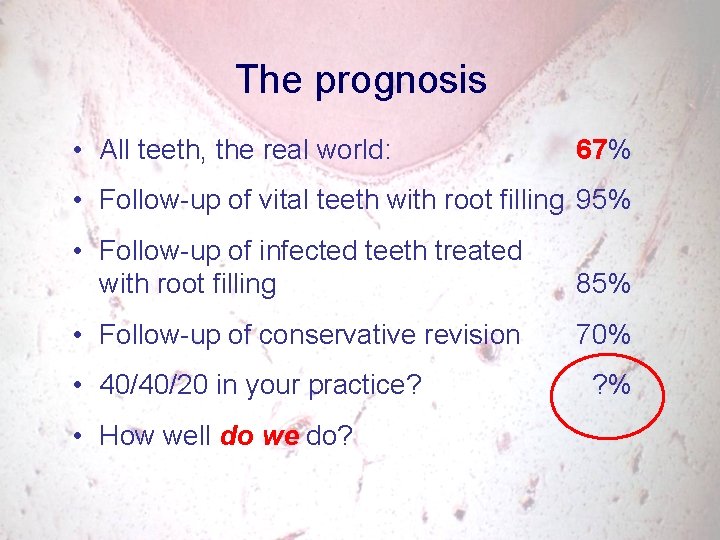
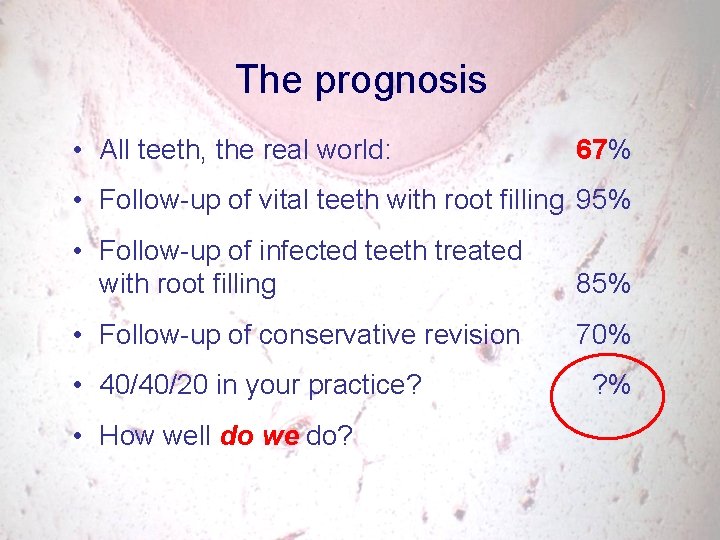
The prognosis • All teeth, the real world: 67% • Follow-up of vital teeth with root filling 95% • Follow-up of infected teeth treated with root filling 85% • Follow-up of conservative revision 70% • 40/40/20 in your practice? ? % • How well do we do?
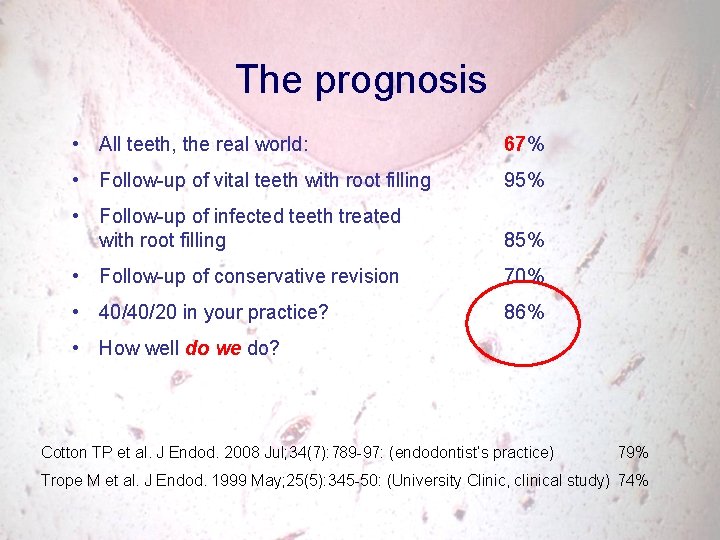
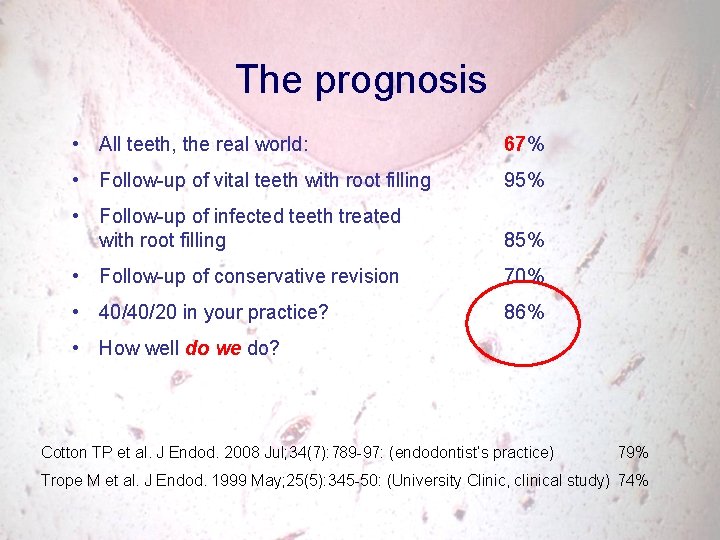
The prognosis • All teeth, the real world: 67% • Follow-up of vital teeth with root filling 95% • Follow-up of infected teeth treated with root filling 85% • Follow-up of conservative revision 70% • 40/40/20 in your practice? 86% • How well do we do? Cotton TP et al. J Endod. 2008 Jul; 34(7): 789 -97: (endodontist’s practice) 79% Trope M et al. J Endod. 1999 May; 25(5): 345 -50: (University Clinic, clinical study) 74%
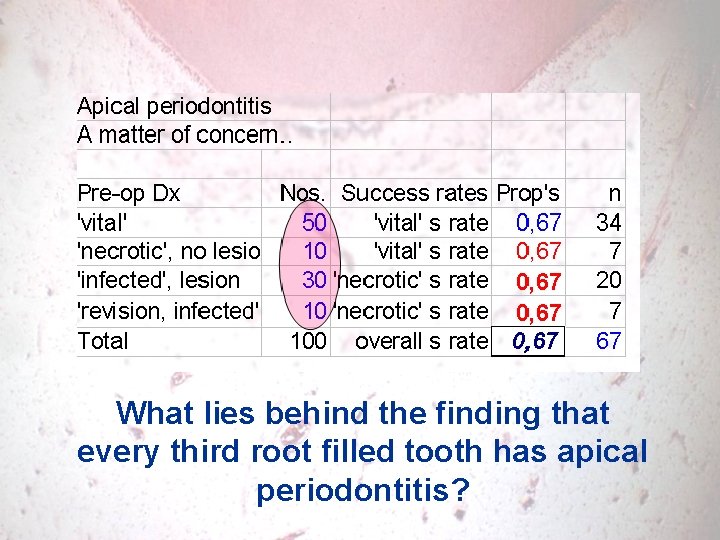
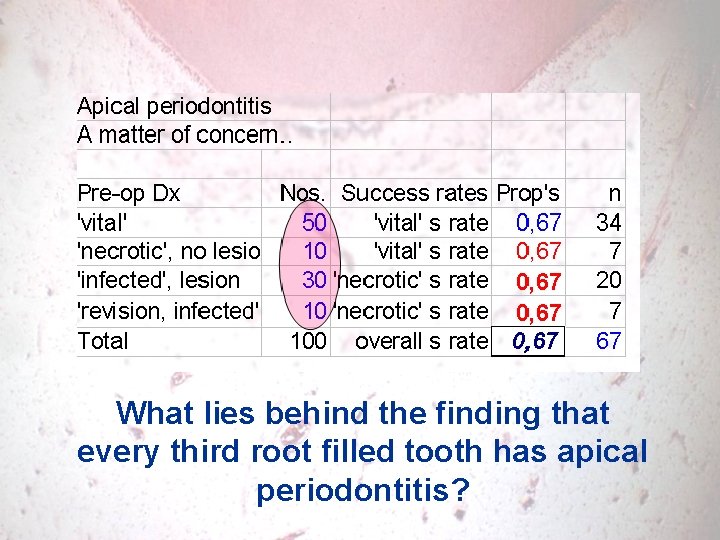
What lies behind the finding that every third root filled tooth has apical periodontitis?
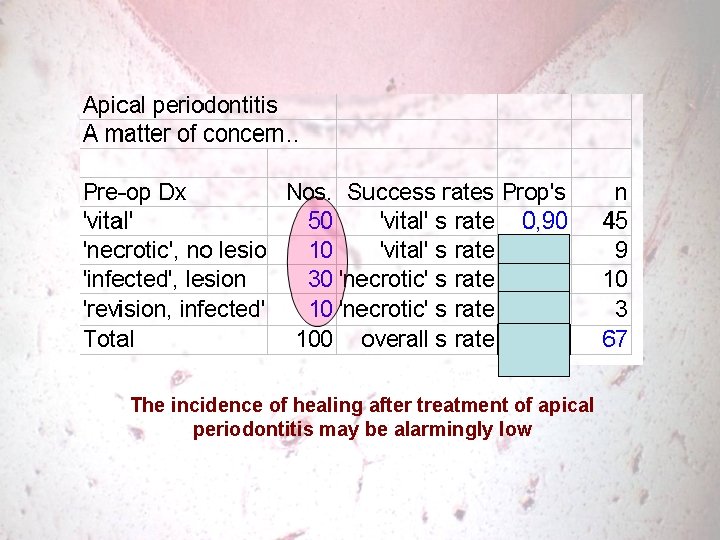
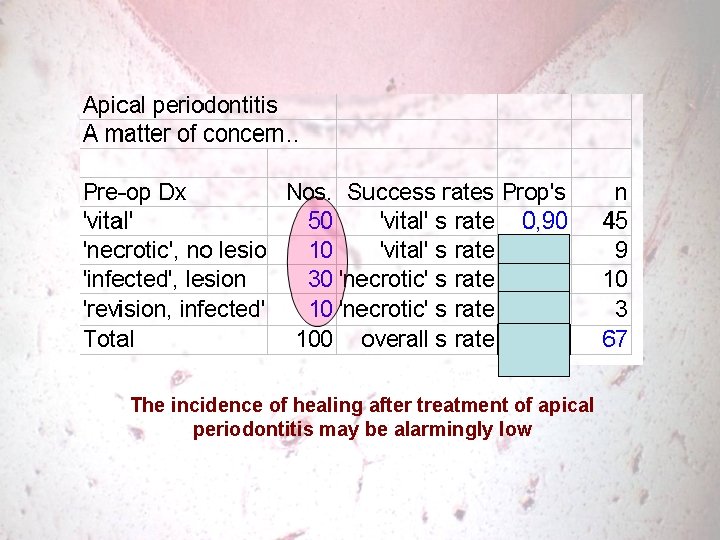
The incidence of healing after treatment of apical periodontitis may be alarmingly low
Arguments suggesting bacterial removal is difficult • Tx results are worse with for AP than for pulpectomy • They are alarmingly low measured with PA radiographs, and even much worse when CBCT is applied • Many more of the successsful vital cases becomes infected and failing with CBCT • Histology reveals microbes in (almost) every case of teeth with inflammatory changes • Inflammatory changes are abundant around root filled teeth
6 The futility of personal experience: the strongest argument for clinical studies
Assessment of one’s own cases • Careful selection of cases for systematic studies: – Preoperative diagnosis AP/NAP – Complications – Technically difficult cases – Surgical variables, if applicable • Limitations of one’s own long-term follow-up experiences
Self-assessment: for practical purposes, we have to og back to the success/failure concept • Suppose 200 patients are seen for control each year (5 per week, 40 wks), • this gives a 95% confidence interval for success rates around 85% of • 80 to 90% • i. e. , there is no way anyone can register a real change in treatment outcome of less than some 10%! • Before that, bias in case selection and uncontrollable drop-outs are inevitable
Self-assessment: example • You want to follow your own experiences with one-step endodontics • Let us suppose that of the 200 patients you get in for recall, 80 had CAP, • of which at least ¼ for various reasons had to be treated in 2 or more appointments anyway, leaving 60, • which gives a conf int of 76 to 94% • i. e. , there is no way anyone can register a real change in therapeutic outcome of less than some 20% on a yearly basis
’It works in my hands’: How many cases does one really need to document a difference in performance? To pursuade a colleague to change his ways?

Even 200 cases are not very discriminating: How many cases are followed systematically in any practice? Moreover, controlling and randomizing the variables influencing bacteria in the canal, and other variables affecting the final outcome are probably never done in any practice – and it is no longer considered ethical
Finally: any new method or new material is correctly applied to simple cases first, recognizing the learning curve. When such cases are retrospectively assessed, they should have a better outcome than the average or complicated case
Conclusion: assessment of one’s own cases • There are serious limitations just by the numbers needed, in one’s own ability to assess outcome • Base-line harmonization is almost impossible and • Case selection is crucial
Conclusion: assessment of one’s own cases • There are serious limitations just by the numbers needed, in one’s own ability to assess outcome • Base-line harmonization is almost impossible and • Case selection is crucial • But: the unusual case will always evade systematic studies, and treatment will still have to be based on hearsay and clinical judgment: cf the plea for the case report
7 Precision in design
Examples by title • 1950: 1000 Fälle von Gangränbehandlung nach der Walkhoffschen Methode. (case series, pro-retro) • 1985: A comparison of antimicrobial effects of calcium hydroxide and iodine-potassium iodide. (cohort study, retro) • 2008: Clinical and radiographic comparison of primary molars after formocresol and electrosurgical pulpotomy: a randomized clinical trial. • 2008: Periapical radiographs overestimate root canal wall thickness during post space preparation. (paraclinical, high precision)
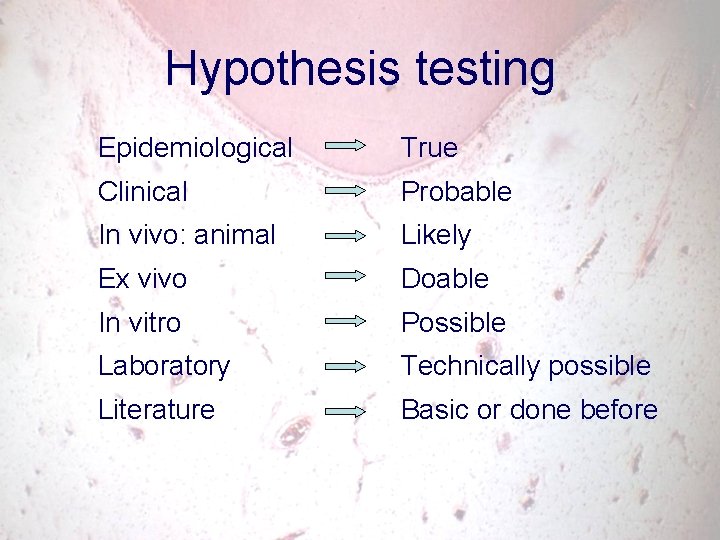
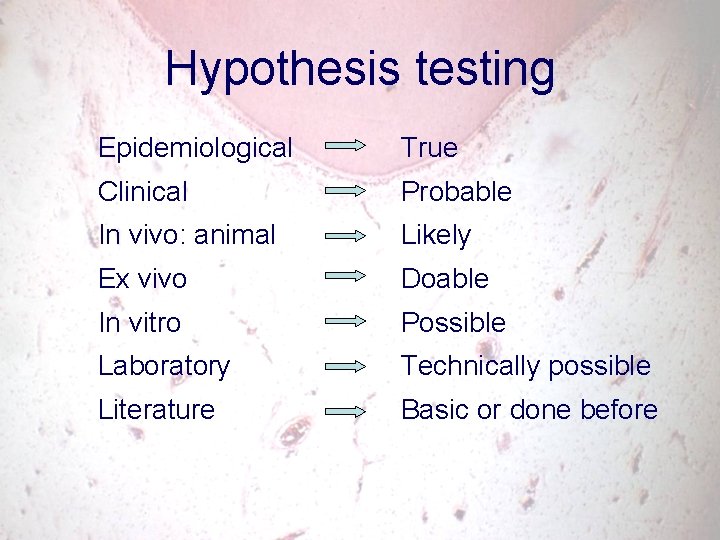
Hypothesis testing Epidemiological True Clinical Probable In vivo: animal Likely Ex vivo Doable In vitro Possible Laboratory Technically possible Literature Basic or done before
Clinical studies: done at chairside • Diagnosis – Xrays, pain • Treatment – Prophylaxis, medicaments, materials, techniques • Disease – Monitoring, criteria • Tooth survival
Ex vivo • Wikipedia: Ex vivo (Latin: out of the living) means that which takes place outside an organism. In science, ex vivo refers to experimentation or measurements done in or on living tissue in an artificial environment outside the organism with the minimum alteration of the natural conditions. • Focus is on re-insertion into the human body/complete organism
In vitro • From Wikipedia, the free encyclopedia • In vitro (Latin for within the glass) refers to the technique of performing a given experiment in a controlled environment outside of a living organism; for example in a test tube.
In vitro – ex vivo • From Wikipedia, the free encyclopedia • In cell biology, ex vivo procedures often involve living cells or tissues taken from an organism and cultured in a laboratory apparatus, usually under sterile conditions with no alterations for up to 24 hrs. Experiments lasting longer than this using living cells or tissue are typically considered to be in vitro. One widely performed ex vivo study is the chick chorioallantoic membrane (CAM) assay. In this assay, angiogenesis is promoted on the CAM membrane of a chick embryo outside the organism (chicken).
Technological experiments • Physical testing: – Materials, techniques • Chemical testing: – Composition, reactions • Manipulative and functional tests: – Bench-top usage tests: working time, setting time, leakage (like ex vivo, but the process is lab defined)
Animal experiments • Biological tests – Toxicity, allergenicity, inflammatory potential • Usage tests – Medicaments and devices applied as suggested for human use
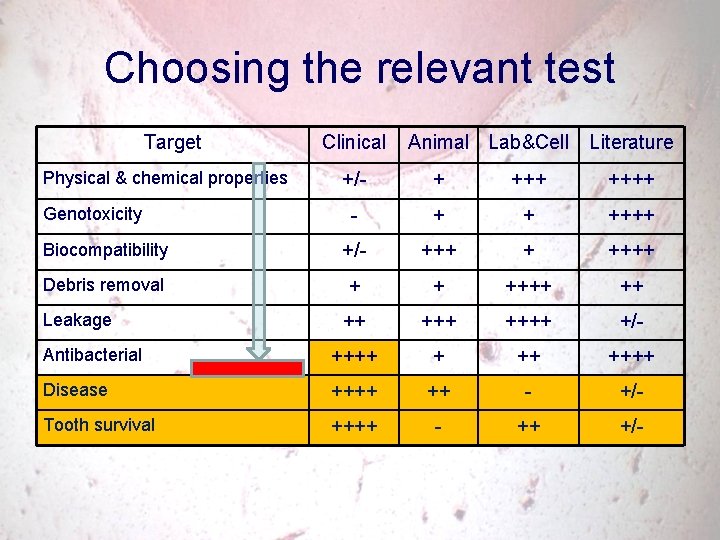
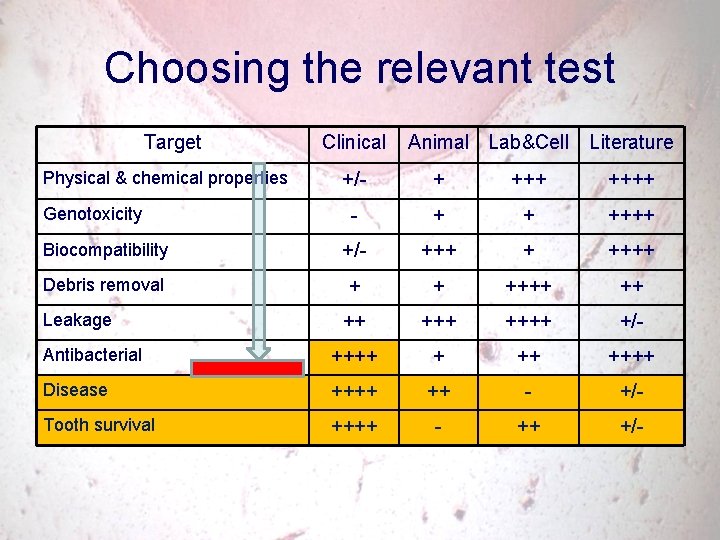
Choosing the relevant test Target Physical & chemical properties Clinical Animal Lab&Cell Literature +/- + ++++ - + + ++++ Biocompatibility +/- +++ + ++++ Debris removal + + ++++ ++++ +/- Antibacterial ++++ ++++ Disease ++++ ++ - +/- Tooth survival ++++ - ++ +/- Genotoxicity Leakage
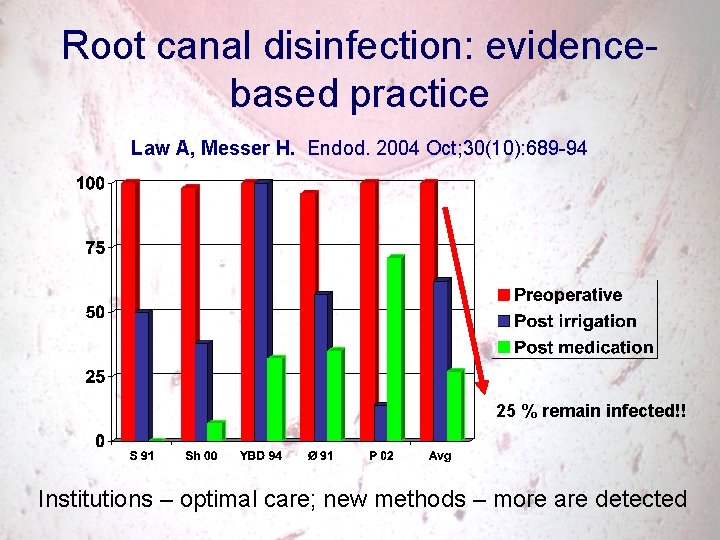
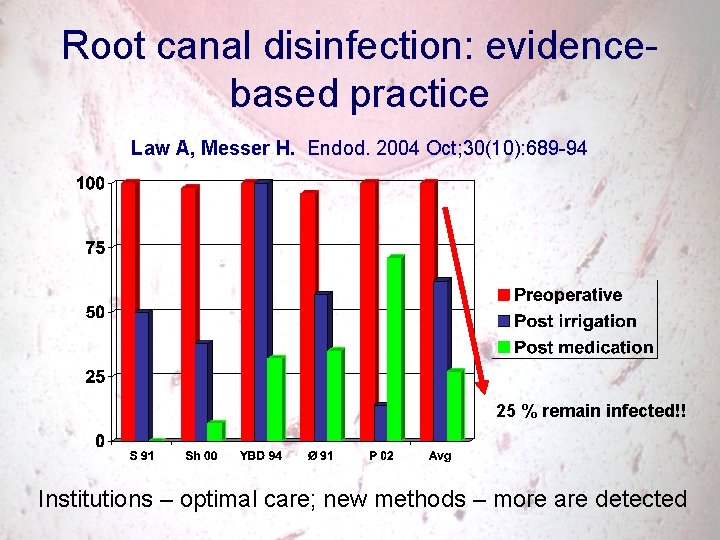
Root canal disinfection: evidencebased practice Law A, Messer H. Endod. 2004 Oct; 30(10): 689 -94 25 % remain infected!! Institutions – optimal care; new methods – more are detected
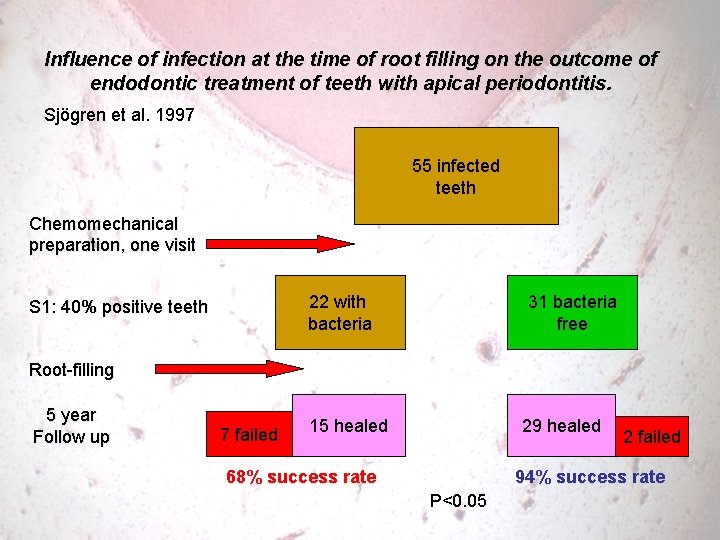
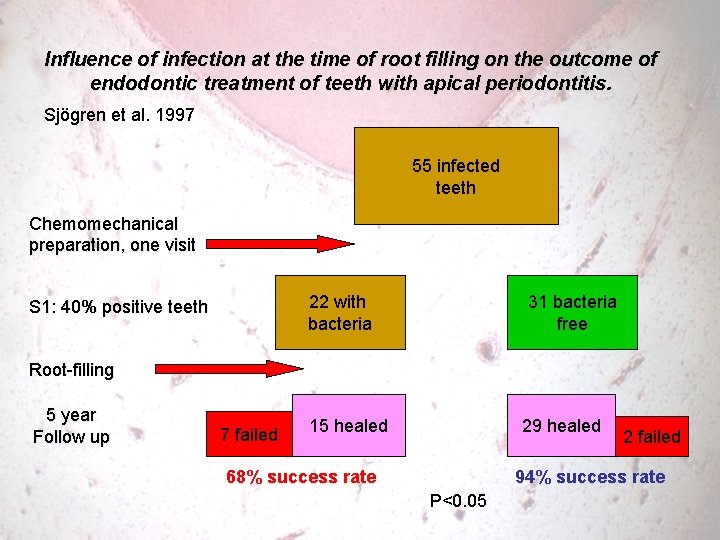
Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Sjögren et al. 1997 55 infected teeth Chemomechanical preparation, one visit 31 bacteria free 22 with bacteria S 1: 40% positive teeth Root-filling 5 year Follow up 7 failed 15 healed 29 healed 68% success rate 2 failed 94% success rate P<0. 05
Thank you!
Different methods of radiographic follow-up methods • Success-failure analysis • Probability assessments • Lesion size monitoring • The PAI scoring system • Quantitative methods • New radiographic techniques
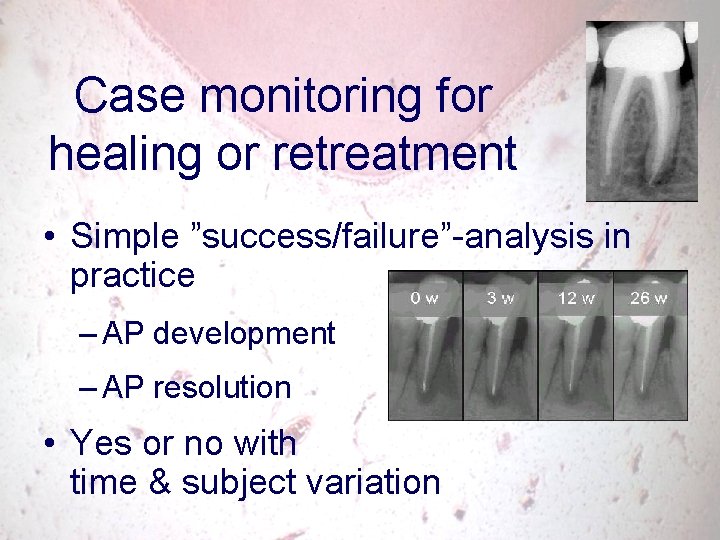
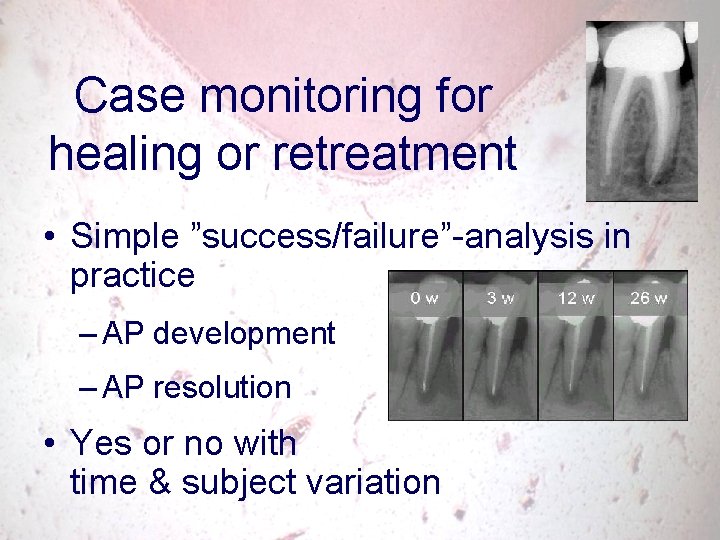
Case monitoring for healing or retreatment • Simple ”success/failure”-analysis in practice – AP development – AP resolution • Yes or no with time & subject variation
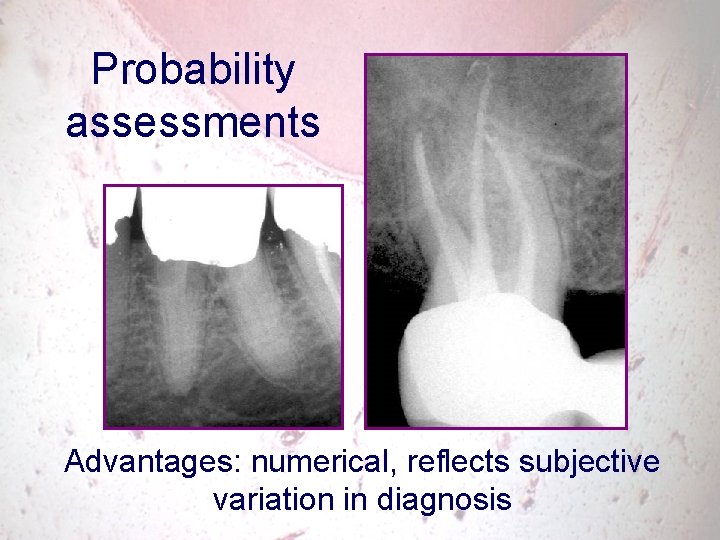
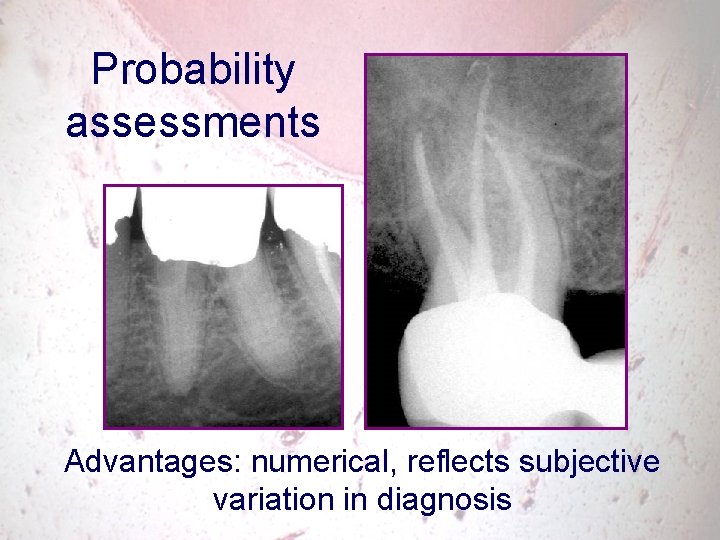
Probability assessments Advantages: numerical, reflects subjective variation in diagnosis
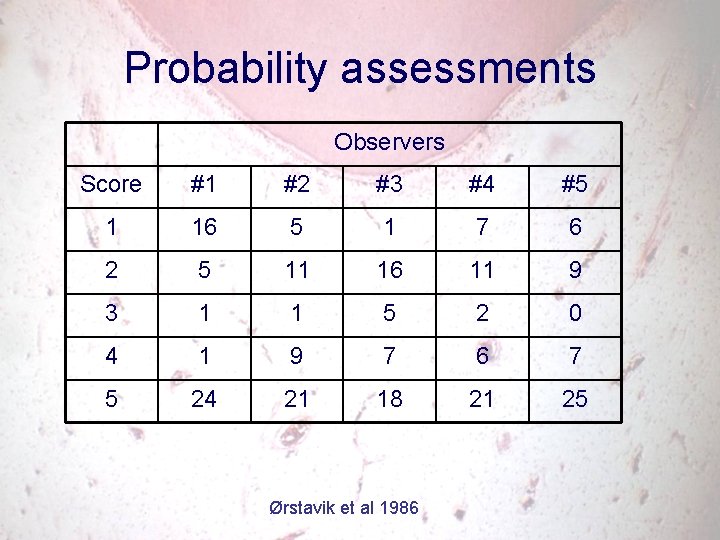
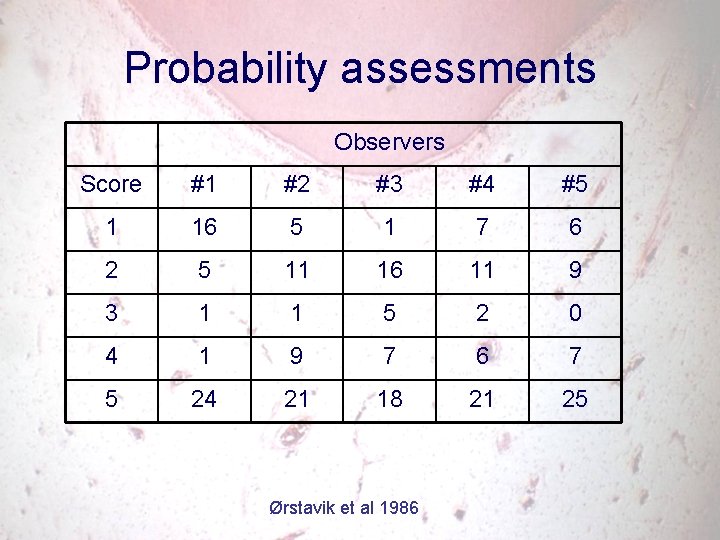
Probability assessments Observers Score #1 #2 #3 #4 #5 1 16 5 1 7 6 2 5 11 16 11 9 3 1 1 5 2 0 4 1 9 7 6 7 5 24 21 18 21 25 Ørstavik et al 1986
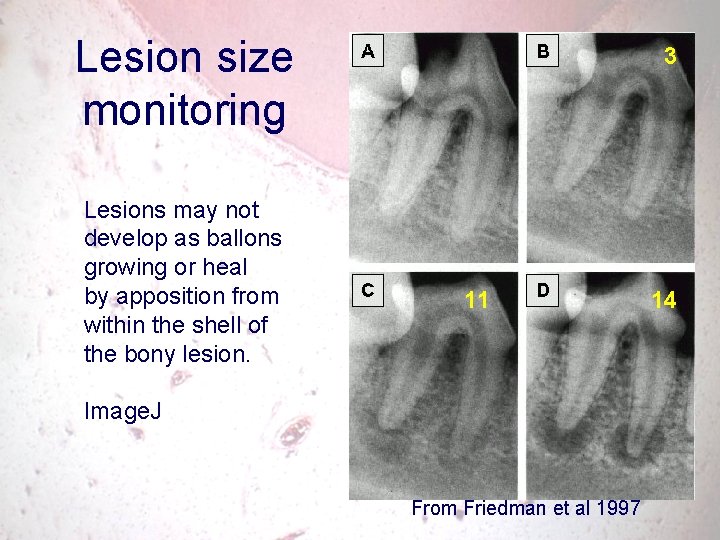
Lesion size monitoring • Quantitative • Numerical, continuous scale • Reflecting the biological process?
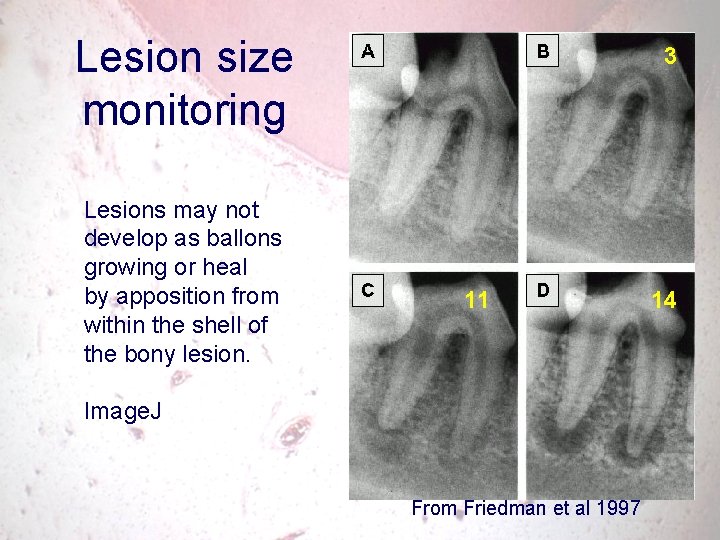
Lesion size monitoring Lesions may not develop as ballons growing or heal by apposition from within the shell of the bony lesion. 3 11 Image. J From Friedman et al 1997 14
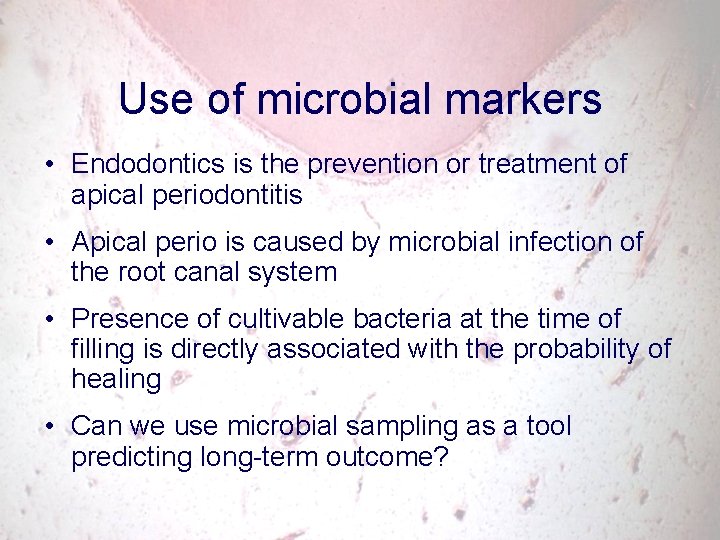
Use of microbial markers • Endodontics is the prevention or treatment of apical periodontitis • Apical perio is caused by microbial infection of the root canal system • Presence of cultivable bacteria at the time of filling is directly associated with the probability of healing • Can we use microbial sampling as a tool predicting long-term outcome?

Bacteriological sampling procedures: Complete vs. discrete
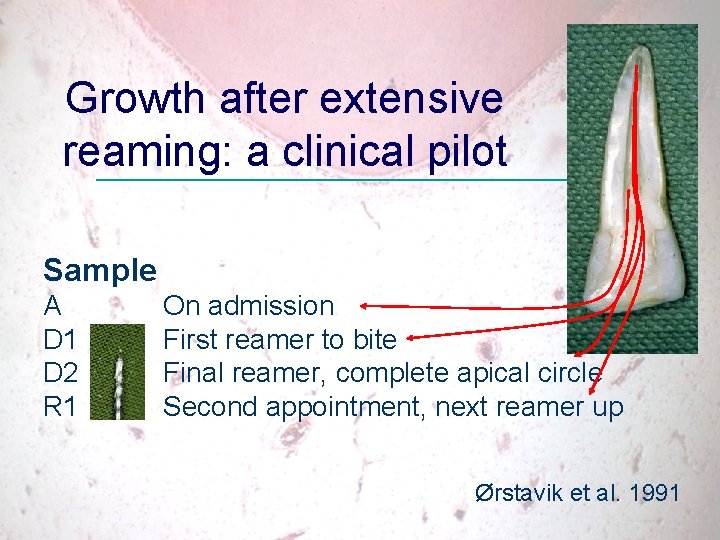
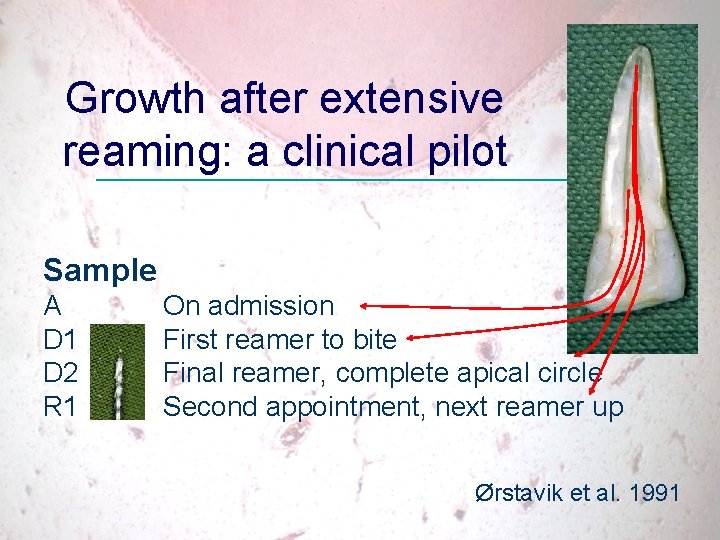
Growth after extensive reaming: a clinical pilot Sample A D 1 D 2 R 1 On admission First reamer to bite Final reamer, complete apical circle Second appointment, next reamer up Ørstavik et al. 1991
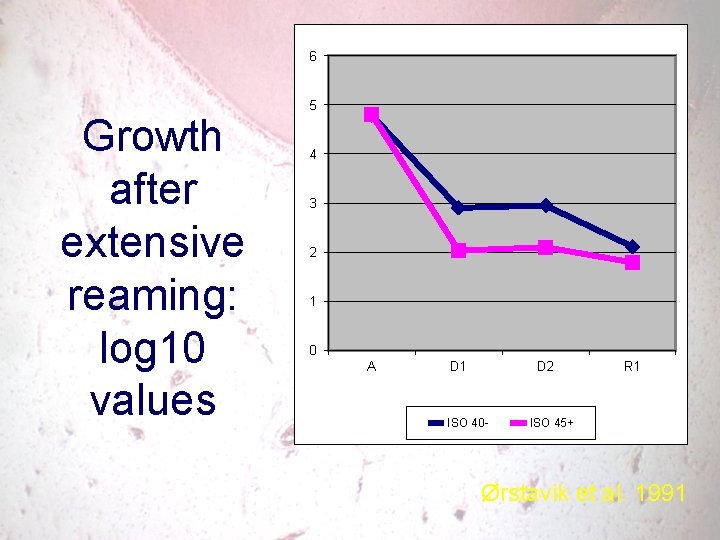
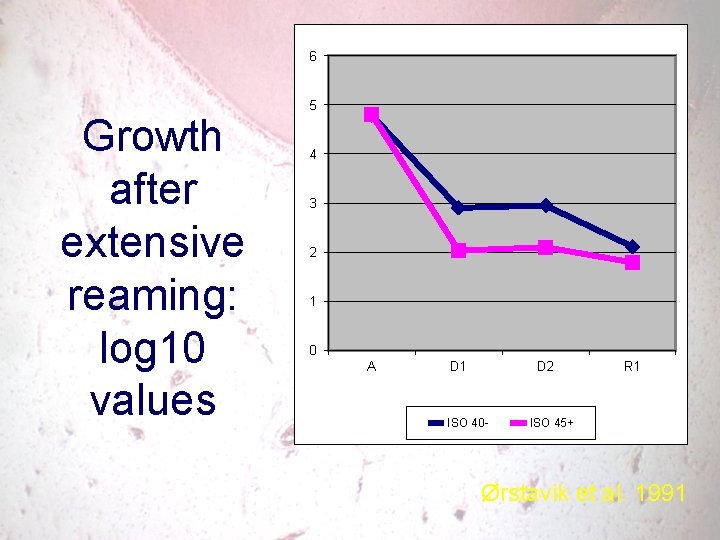
6 Growth after extensive reaming: log 10 values 5 4 3 2 1 0 A D 1 D 2 ISO 40 - R 1 ISO 45+ Ørstavik et al. 1991

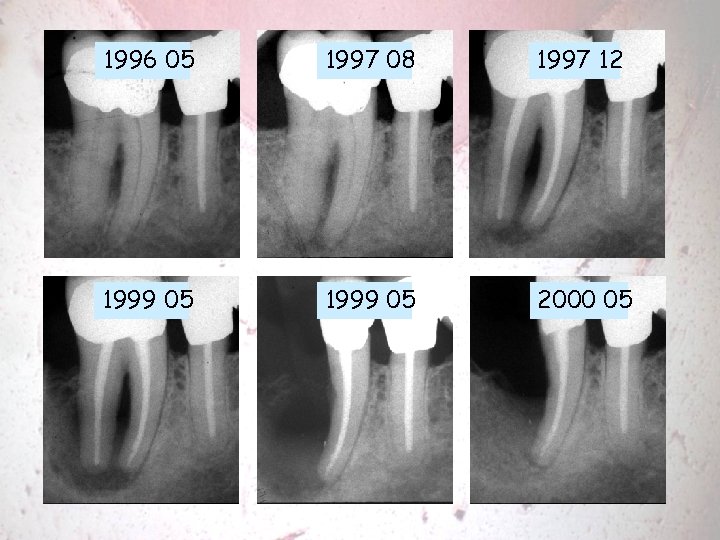
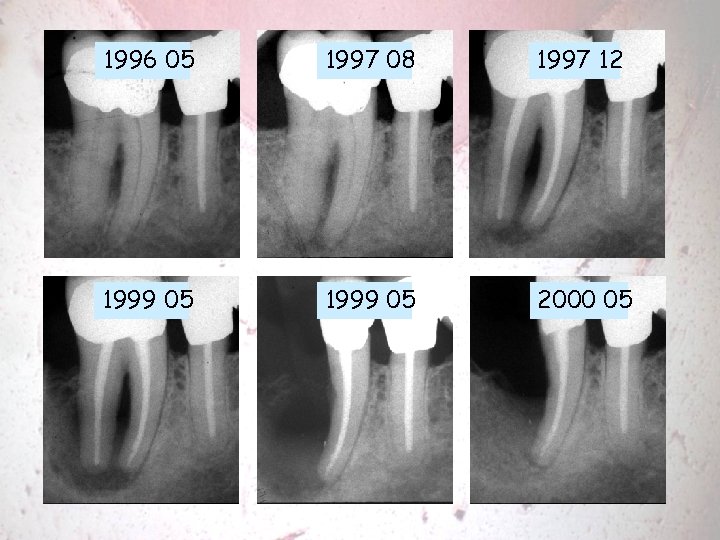
1996 05 1997 08 1997 12 1999 05 2000 05
 Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Followup edge
Followup edge Followup:actionitems
Followup:actionitems Follow-up visits
Follow-up visits Spreaders and pluggers ppt
Spreaders and pluggers ppt Irs kit endo
Irs kit endo Obturating material
Obturating material Silver point obturation disadvantages
Silver point obturation disadvantages Paradigm shift from women studies to gender studies
Paradigm shift from women studies to gender studies Roles, responsibilities and expectations examples
Roles, responsibilities and expectations examples Iso 9001;2015
Iso 9001;2015 Necessity advisability and expectations
Necessity advisability and expectations Team rules and expectations
Team rules and expectations Que es una preposicion en ingles
Que es una preposicion en ingles Team rules and expectations
Team rules and expectations Set high expectations which inspire motivate and challenge
Set high expectations which inspire motivate and challenge Our hopes and expectations
Our hopes and expectations Expectations for unit and ratee examples
Expectations for unit and ratee examples Classroom procedures and expectations
Classroom procedures and expectations Irony vs coincidence
Irony vs coincidence Workplace expectations examples
Workplace expectations examples Quality is meeting or exceeding customer expectations
Quality is meeting or exceeding customer expectations Chapter 20 great expectations
Chapter 20 great expectations Chapter 6 great expectations summary
Chapter 6 great expectations summary Great expectations aa chapters 8-10
Great expectations aa chapters 8-10 Chapter 7 great expectations summary
Chapter 7 great expectations summary Virtual training expectations
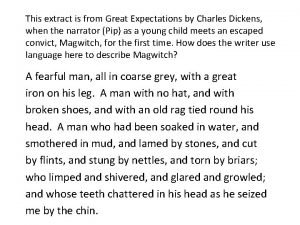
Virtual training expectations A fearful man all in coarse gray
A fearful man all in coarse gray Iterated expectation
Iterated expectation My expectations
My expectations Meeting patient expectations in nursing
Meeting patient expectations in nursing Working below age related expectations
Working below age related expectations Linear regression with one regressor
Linear regression with one regressor Motifs in great expectations
Motifs in great expectations Ross greene plan a b c
Ross greene plan a b c Leader hm
Leader hm Great expectations summary
Great expectations summary Great expectations chapter 18-19 summary
Great expectations chapter 18-19 summary Charles dickens presentation
Charles dickens presentation Great expectations climax
Great expectations climax Michigan grade level content expectations
Michigan grade level content expectations Expectations in probability
Expectations in probability Important clipart
Important clipart Implicit service promises examples
Implicit service promises examples Chapter 37 great expectations
Chapter 37 great expectations Zone of tolerance for different service dimensions
Zone of tolerance for different service dimensions Possible levels of customer expectations
Possible levels of customer expectations Desired and adequate service
Desired and adequate service Great expectations
Great expectations Exceeding expectations realty
Exceeding expectations realty School vs work expectations
School vs work expectations Prayer points for pregnant mothers
Prayer points for pregnant mothers Expectations in personal development
Expectations in personal development Chapter 37 great expectations
Chapter 37 great expectations Hans robert jauss pdf
Hans robert jauss pdf Secondary group
Secondary group Great expectations analysis
Great expectations analysis Character sketch of pip in great expectations
Character sketch of pip in great expectations Literature circle expectations
Literature circle expectations Nyssls
Nyssls Clarity of expectations of students
Clarity of expectations of students Irony in oliver twist
Irony in oliver twist Journal writing expectations
Journal writing expectations Victorian era marriage expectations
Victorian era marriage expectations Behavior that matches group expectations
Behavior that matches group expectations Anguage
Anguage Expectation failure
Expectation failure Expectations for student council
Expectations for student council Examples of community expectations
Examples of community expectations Guest teacher expectations
Guest teacher expectations Expectations graffiti
Expectations graffiti Using champs in the classroom
Using champs in the classroom Middle school cafeteria expectations
Middle school cafeteria expectations Examples of facilitative emotions
Examples of facilitative emotions Four frames of kindergarten
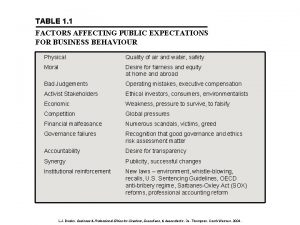
Four frames of kindergarten Public expectations
Public expectations Schoolwide expectations
Schoolwide expectations School expectations
School expectations Homeroom expectations
Homeroom expectations High expectations high support
High expectations high support With great expectations comes great responsibility
With great expectations comes great responsibility School expectations
School expectations Sample expectations in training
Sample expectations in training Whiteboard expectations
Whiteboard expectations Hallway expectations elementary
Hallway expectations elementary School expectations
School expectations Homeroom expectations
Homeroom expectations Workshop expectations
Workshop expectations June budhooram
June budhooram Rational expectations theory
Rational expectations theory Irony of the title great expectations
Irony of the title great expectations Expectations
Expectations Explicit customer expectations
Explicit customer expectations End of reception year expectations
End of reception year expectations Michigan physical education standards
Michigan physical education standards Participant expectations
Participant expectations The seven forms of energy
The seven forms of energy Statuses and their related roles determine
Statuses and their related roles determine Fill expectations
Fill expectations Chapter 36 great expectations
Chapter 36 great expectations Possible levels of customer expectations
Possible levels of customer expectations Trauma awareness and treatment center utah
Trauma awareness and treatment center utah Julie woodside
Julie woodside Charting exercise chapter 28
Charting exercise chapter 28 Class iii
Class iii House classification of denture patients
House classification of denture patients Cbt assessment example
Cbt assessment example Sewage treatment primary secondary and tertiary
Sewage treatment primary secondary and tertiary Oral diagnosis and treatment planning ppt
Oral diagnosis and treatment planning ppt Sample treatment plan for adhd
Sample treatment plan for adhd Ethics and fair treatment at work
Ethics and fair treatment at work Case conceptualization example cbt
Case conceptualization example cbt Care and treatment reviews
Care and treatment reviews Assessment and treatment alternatives
Assessment and treatment alternatives Chapter 1 risk and its treatment
Chapter 1 risk and its treatment Hepatitis b symptoms
Hepatitis b symptoms