1909 followup Kirill Lipatov 1909 followup Overview Collection


- Slides: 61

1909 follow-up Kirill Lipatov
1909 follow-up Overview - Collection of topics potentially pertinent to 1909 rotation Obtained from cases previously encountered by residents Accompanied by supplemental reading list PLEASE SEND US CASES FROM YOUR 1909 SHIFTS!
Disclaimer - I claim no expertise on presented topics - Presented information is up for discussion and criticism
Case 1 75 yo M admitted for altered mental status to the general hospital floor. He is disoriented and combative. He is given 4 mg of IV Haldol. Vitals: HR 120, BP 200/100, Temp 96. 9 F, RR 24, Sp. O 2 100%
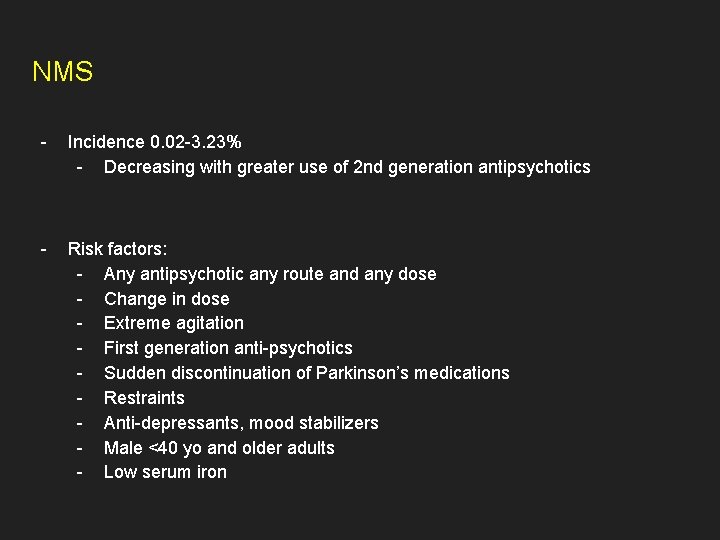
NMS - Incidence 0. 02 -3. 23% - Decreasing with greater use of 2 nd generation antipsychotics - Risk factors: - Any antipsychotic any route and any dose - Change in dose - Extreme agitation - First generation anti-psychotics - Sudden discontinuation of Parkinson’s medications - Restraints - Anti-depressants, mood stabilizers - Male <40 yo and older adults - Low serum iron
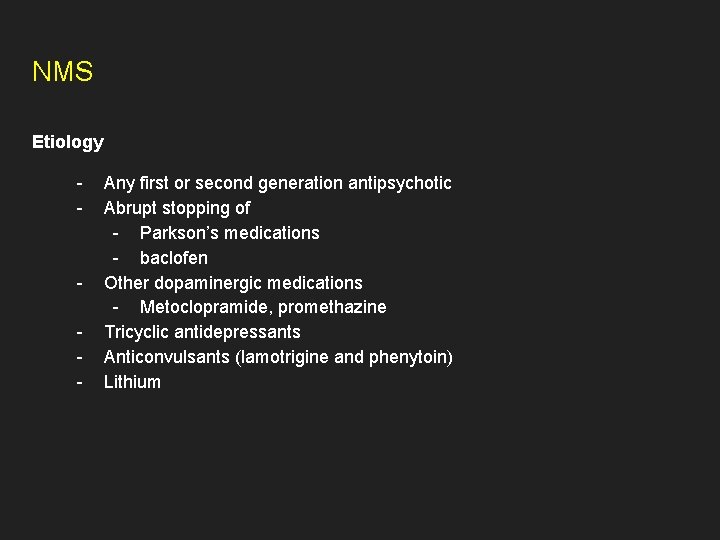
NMS Etiology - - Any first or second generation antipsychotic Abrupt stopping of - Parkson’s medications - baclofen Other dopaminergic medications - Metoclopramide, promethazine Tricyclic antidepressants Anticonvulsants (lamotrigine and phenytoin) Lithium
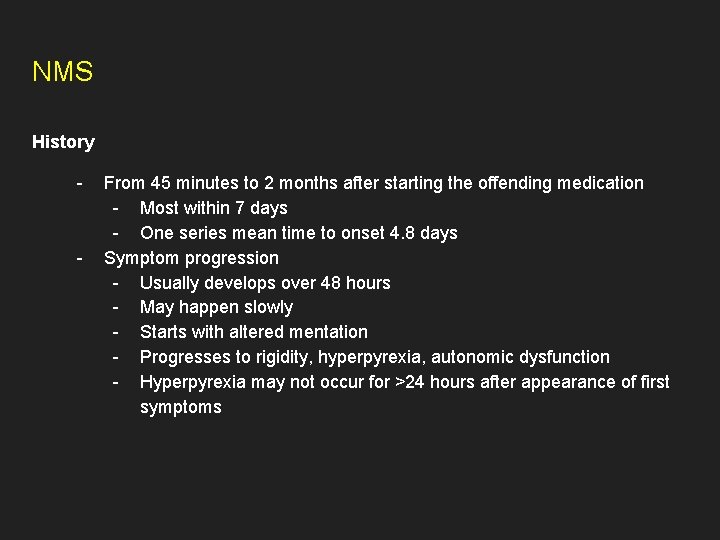
NMS History - - From 45 minutes to 2 months after starting the offending medication - Most within 7 days - One series mean time to onset 4. 8 days Symptom progression - Usually develops over 48 hours - May happen slowly - Starts with altered mentation - Progresses to rigidity, hyperpyrexia, autonomic dysfunction - Hyperpyrexia may not occur for >24 hours after appearance of first symptoms
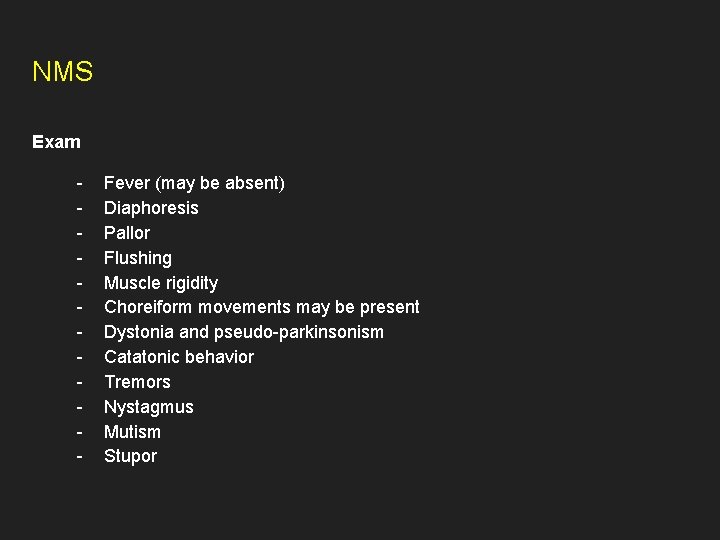
NMS Exam - Fever (may be absent) Diaphoresis Pallor Flushing Muscle rigidity Choreiform movements may be present Dystonia and pseudo-parkinsonism Catatonic behavior Tremors Nystagmus Mutism Stupor
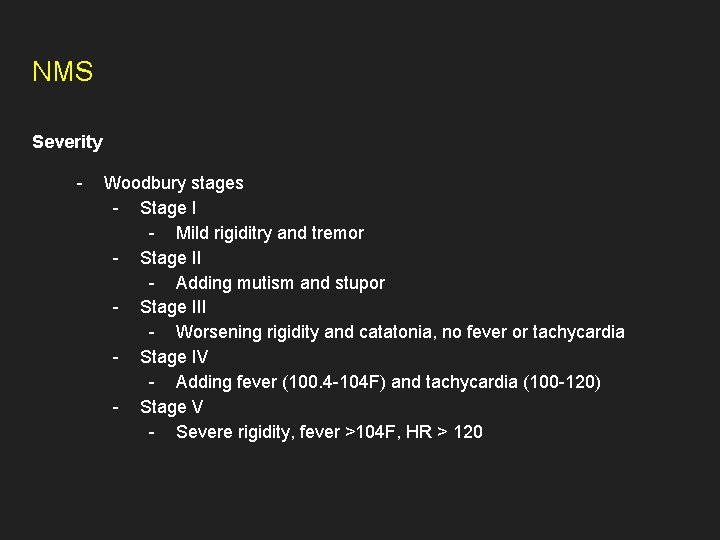
NMS Severity - Woodbury stages - Stage I - Mild rigiditry and tremor - Stage II - Adding mutism and stupor - Stage III - Worsening rigidity and catatonia, no fever or tachycardia - Stage IV - Adding fever (100. 4 -104 F) and tachycardia (100 -120) - Stage V - Severe rigidity, fever >104 F, HR > 120
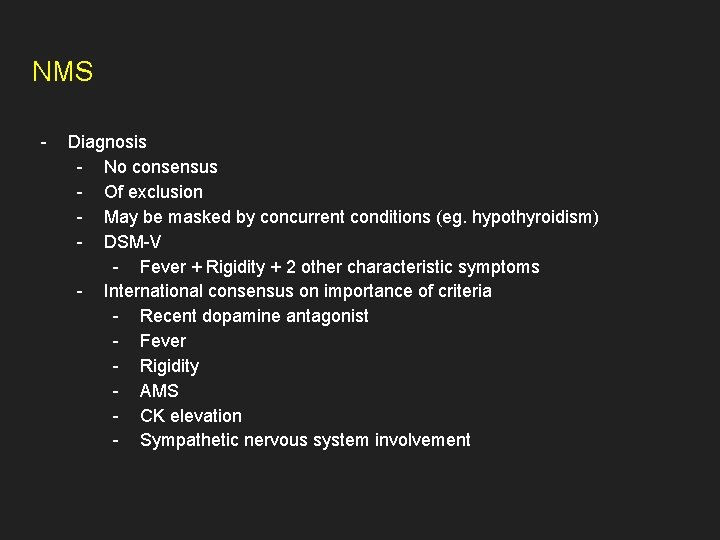
NMS - Diagnosis - No consensus - Of exclusion - May be masked by concurrent conditions (eg. hypothyroidism) - DSM-V - Fever + Rigidity + 2 other characteristic symptoms - International consensus on importance of criteria - Recent dopamine antagonist - Fever - Rigidity - AMS - CK elevation - Sympathetic nervous system involvement
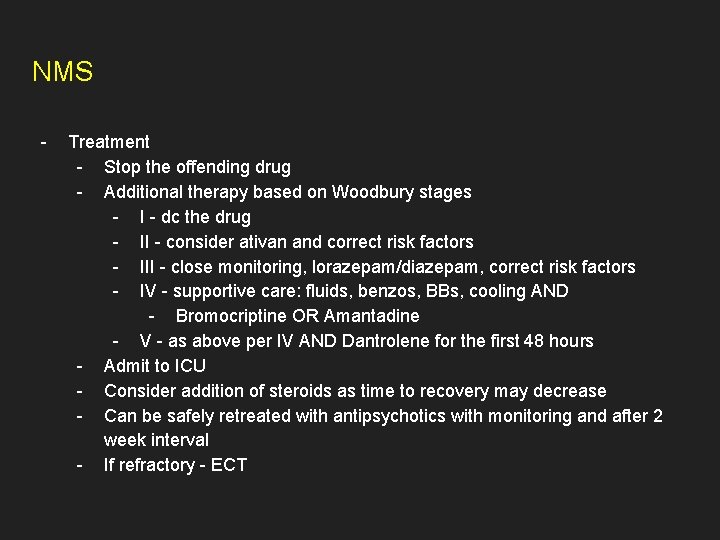
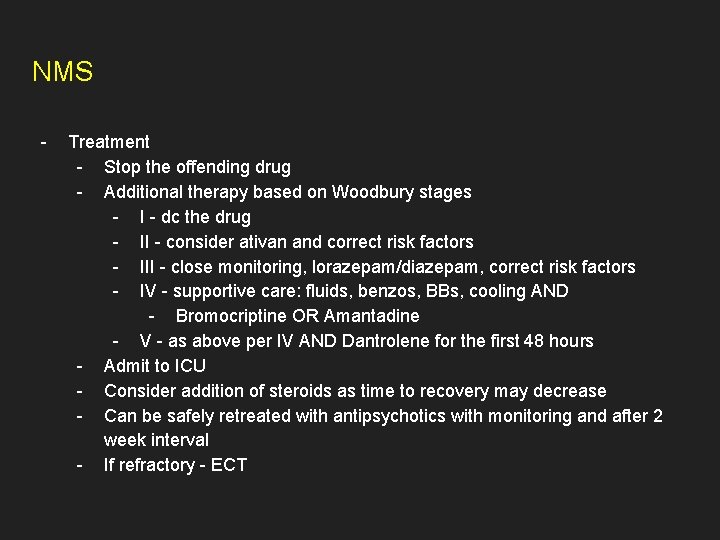
NMS - Treatment - Stop the offending drug - Additional therapy based on Woodbury stages - I - dc the drug - II - consider ativan and correct risk factors - III - close monitoring, lorazepam/diazepam, correct risk factors - IV - supportive care: fluids, benzos, BBs, cooling AND - Bromocriptine OR Amantadine - V - as above per IV AND Dantrolene for the first 48 hours - Admit to ICU - Consider addition of steroids as time to recovery may decrease - Can be safely retreated with antipsychotics with monitoring and after 2 week interval - If refractory - ECT
Case 2 32 yo man with history of IV drug use presented to the hospital with shortness of breath and admitted for bilateral pneumonia. His hypoxemia quickly progresses despite broad spectrum antibiotics, he is intubated and placed on IMV. His initial settings are Vt 400, RR 16, Fi. O 2 0. 9, PEEP 14. Within a few hours post intubation he develops acute desaturations and hypotension.
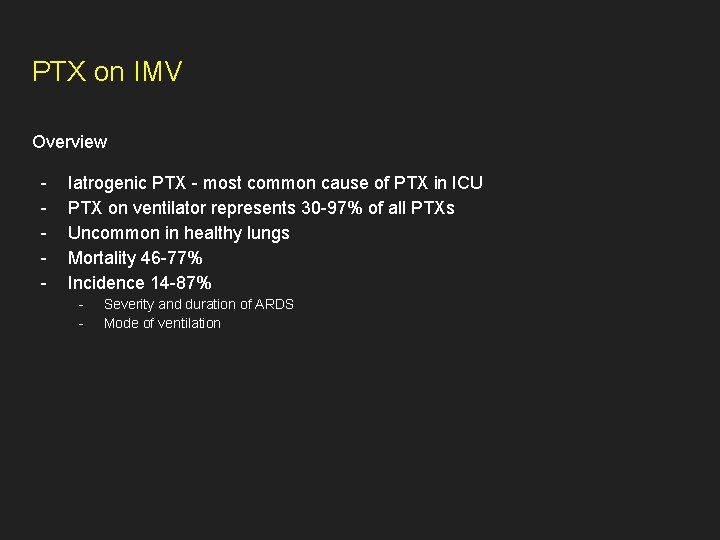
PTX on IMV Overview - Iatrogenic PTX - most common cause of PTX in ICU PTX on ventilator represents 30 -97% of all PTXs Uncommon in healthy lungs Mortality 46 -77% Incidence 14 -87% - Severity and duration of ARDS Mode of ventilation
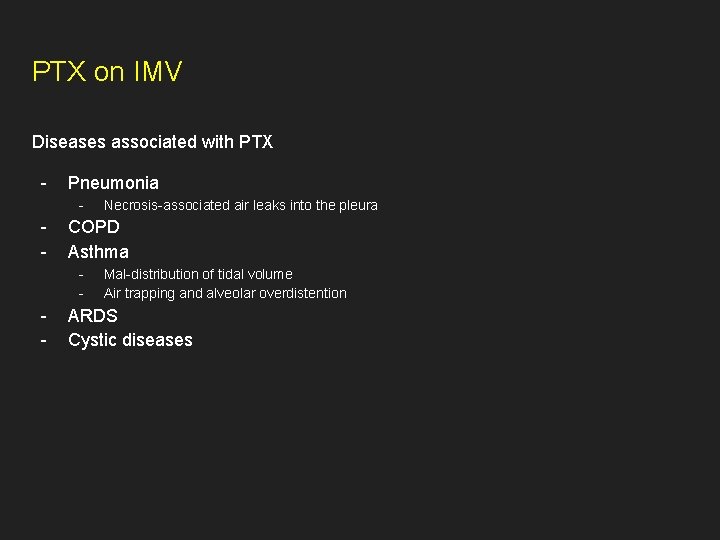
PTX on IMV Diseases associated with PTX - Pneumonia - - COPD Asthma - - Necrosis-associated air leaks into the pleura Mal-distribution of tidal volume Air trapping and alveolar overdistention ARDS Cystic diseases
PTX on IMV Risk factors for PTX on a ventilator - High peak airway pressure (>50 cm. H 2 O) Overdistention Volutrauma > barotrauma - - Higher risk in overdistention than high airway pressures in animal studies May come from higher PEEP (controversial) Almost unavoidable if Pplat > 35 in one study

Title - Text
PTX in IMV Presentation - Chest pain Tachycardia (most common) Agitation Hypotension Interstitial emphysema Pneumomediastinum Pneumoperitoneum Subcutaneous emphysema
PTX in IMV Clinical presentation - Median time to development 4 days since starting IMV 80% develop PTX in the first 3 days In ARDS highest incidence - - Early phase >2 weeks 7. 4 -10% will have recurrence on the other side
PTX in IMV Diagnosis - Clinical - Decreased breath sounds - May not be noted if <15% of hemothorax - Hyperresonant percussion - Decrease in Vt with increase in PAP - Increase in CVP - Pulsus paradoxus (arterial tracing)
PTX in IMV Diagnosis - Radiographic - CXR - Different appearance if supine - Limited by similar appearance of pre-existing lung disease - Visceral gas - Skin folds - Bullous disease - CT scan - Gold standard - Helps avoid complication of thoracostomy without PTX - Impractical and unsafe in most instances of tension
PTX in IMV Transthoracic ultrasonography - - Fast Available bedside Helps rule out PTX - 92% sensitivity in one study - More sensitive than CXR in another study Relies on visualization of: - Respiration-dependant movement of visceral pleura against parietal pleura - AKA “sliding lung sign” - Band-like reverberation echoes at the boundary between pleura and lung - Comet-tail artifacts
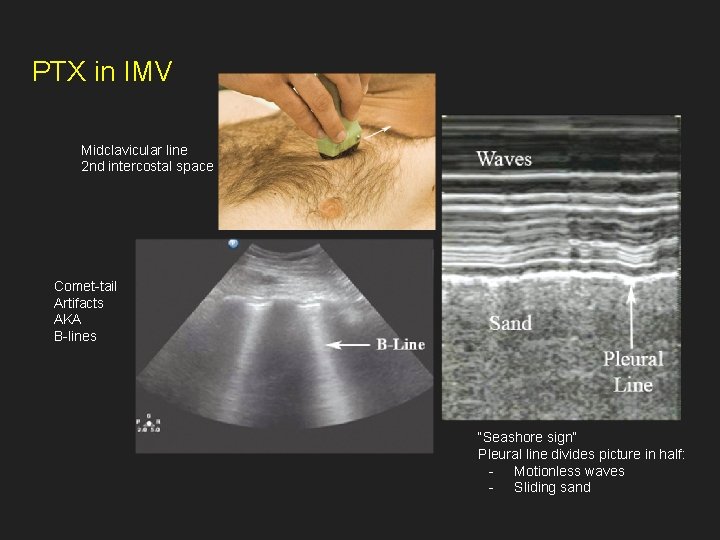
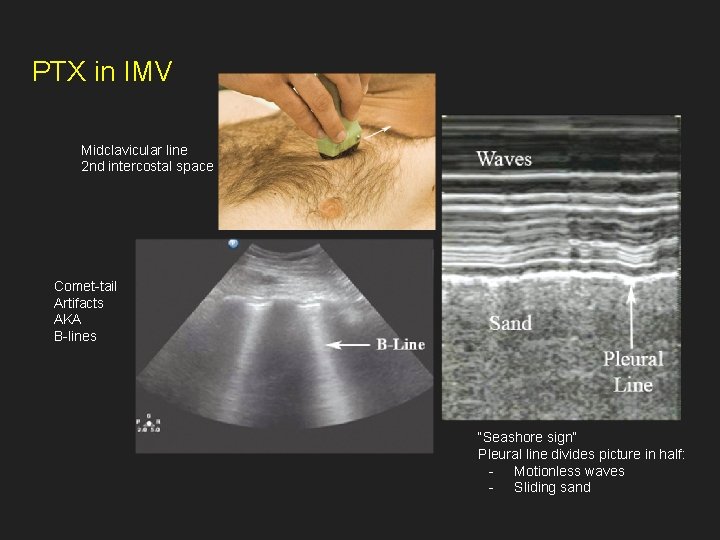
PTX in IMV Midclavicular line 2 nd intercostal space Comet-tail Artifacts AKA B-lines “Seashore sign” Pleural line divides picture in half: - Motionless waves - Sliding sand
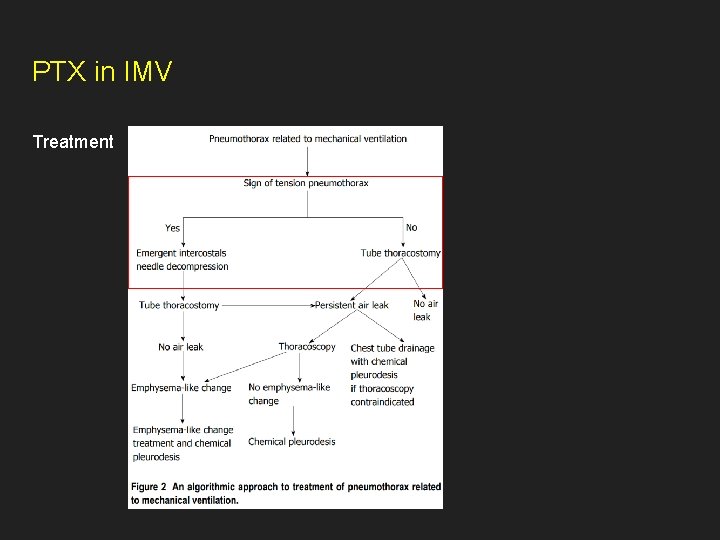
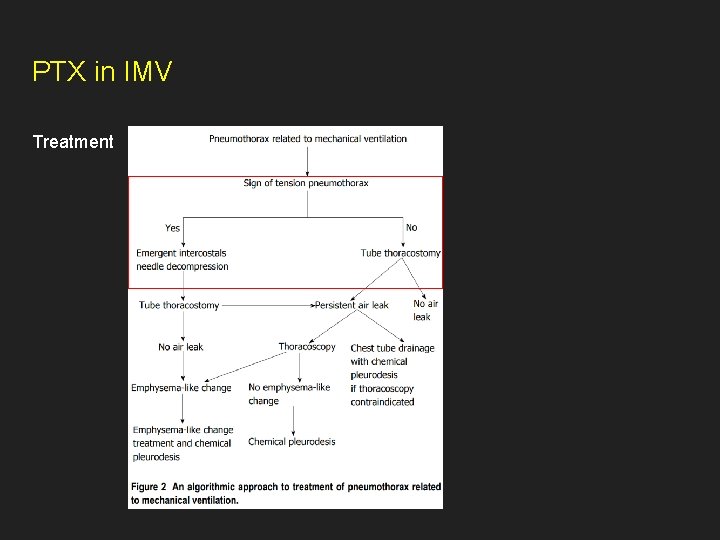
PTX in IMV Treatment
Case 3 54 yo male admitted for ARDS, hospital day #37. He just weaned off of VV ECMO and underwent tracheostomy placement hospital day #12. You are called to bedside overnight because the nurse noticed bleeding around the tracheostomy site. The bleeding is not stopping and the pressor requirement is increasing.
Tracheo-innominate artery fistula Overview - Fistula between trachea and tracheo-innominate artery Rare complication of tracheostomy Incidence 0. 7% Survival 14. 3% Mortality 100% without operative intervention 75% develop within first 3 weeks of tracheostomy
Tracheo-innominate artery fistula Risk factors - Low tracheostomy tube placement Overinflation of the cuff >20 mm. Hg Malpositioned tracheostomy tube tip Anatomical variants Local infection or neoplasm Radiation Steroids Diabetes Malnutrition
TIAF Diagnosis - High index of suspicion - - Sentinel bleed (50% of cases) - may benefit from early evaluation Pulsating tracheostomy tube Bronchoscopy CT angiogram (20 -30% sensitive)
TIAF Management - Hyperinflate the balloon - - If unsuccessful: - - Successful in 85% of cases Intubate past the tracheostomy site Attempt to tamponade the bleeding with a finger Blood Surgery vs IR embolization - Call everyone who has a phone number or a pager
Tracheostomy emergencies - Guidelines slides
Hypothermia slides - Text
Case 5 32 yo M presents to SW MICU for altered mental status. He is an inmate in prison where he was earlier found to be confused, lethargic, and disoriented. There is a concern for ingestion. On arrival he is tachypneic, tachycardic, normotensive. Lipase 5000. Osmolar gap 70. Anion gap 24. Bicarb undetectable. BHB 30. Glucose 467. He is diagnosed with DKA and admitted to MICU. Insulin drip started. 3 hours into his stay in MICU he develops worsening tachypnea breathing 60 times a minute. He is visible uncomfortable and diaphoretic. He continues to not answer any questions.
Hypophosphatemia in DKA Overview - Diabetic ketoacidosis - - Complication of DM 1 and DM 2 Associated with elevated anion gap metabolic acidosis Mortality 1 -5%, depending on age and comorbidities Causes: - New onset DM - Non-compliance - Infection - Pancreatitis - SGLT-2 Treatment: - IVF - Insulin - Electrolyte replacement
Hypophosphatemia in DKA Inorganic phosphorus in DKA - Normal serum concentration Intracellular depletion Insulin causes influx of i. P into the cells - Dose dependant insulin-induced hypophosphatemia - As early as 30 minutes after administration - May last for up to a week
Hypophosphatemia in DKA Hematologic manifestations - - 2, 3 -DPG depletion - Initially balanced by the acidosis - With improvement in acidosis oxygen dissociation curve moved markedly to the left - Takes up to 1 week to recover 2, 3 -DPG levels - Impaired oxygenation of tissues - Most affecting kidneys, brain, retina, pancreas, heart ATP depletion - Increased rigidity of RBC membrane - Trapping of RBCs in spleen - Hemolytic anemia
Hypophosphatemia in DKA Neurologic manifestations - May develop as a result of prolonged post-DKA hypophosphatemia - Encephalopathy - Confusion - Seizures - Hallucinations - Coma
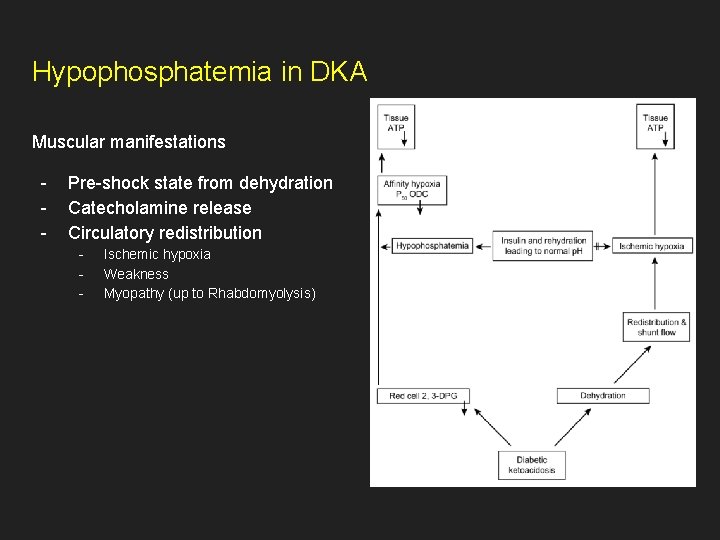
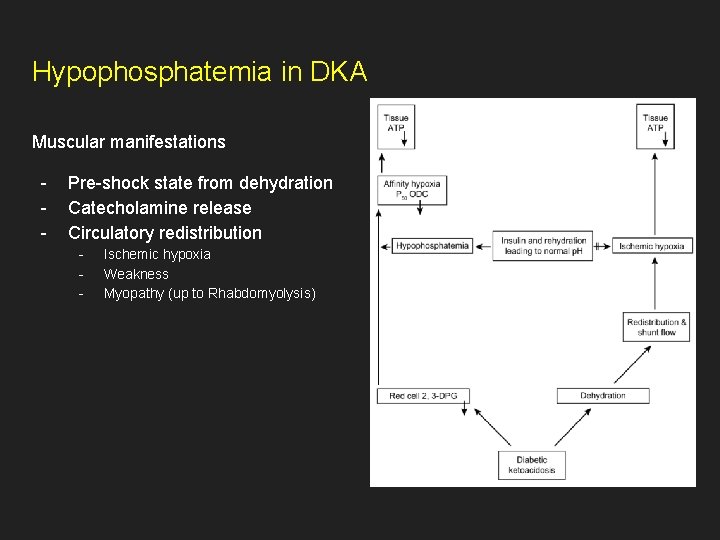
Hypophosphatemia in DKA Muscular manifestations - Pre-shock state from dehydration Catecholamine release Circulatory redistribution - Ischemic hypoxia Weakness Myopathy (up to Rhabdomyolysis)
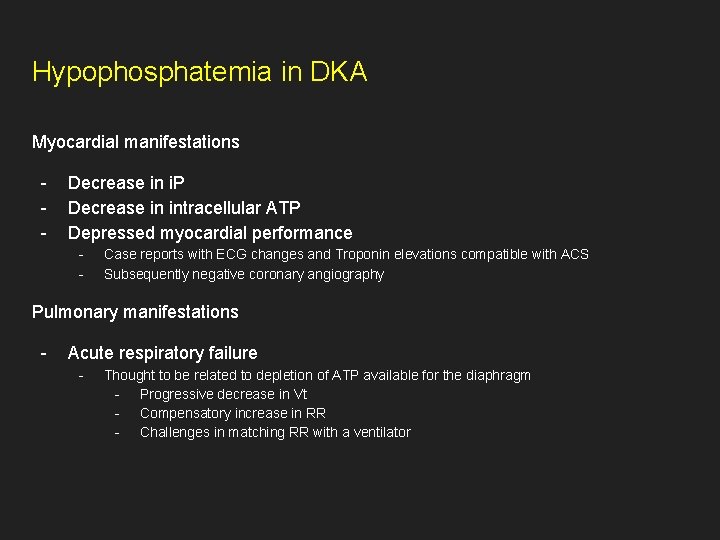
Hypophosphatemia in DKA Myocardial manifestations - Decrease in i. P Decrease in intracellular ATP Depressed myocardial performance - Case reports with ECG changes and Troponin elevations compatible with ACS Subsequently negative coronary angiography Pulmonary manifestations - Acute respiratory failure - Thought to be related to depletion of ATP available for the diaphragm - Progressive decrease in Vt - Compensatory increase in RR - Challenges in matching RR with a ventilator
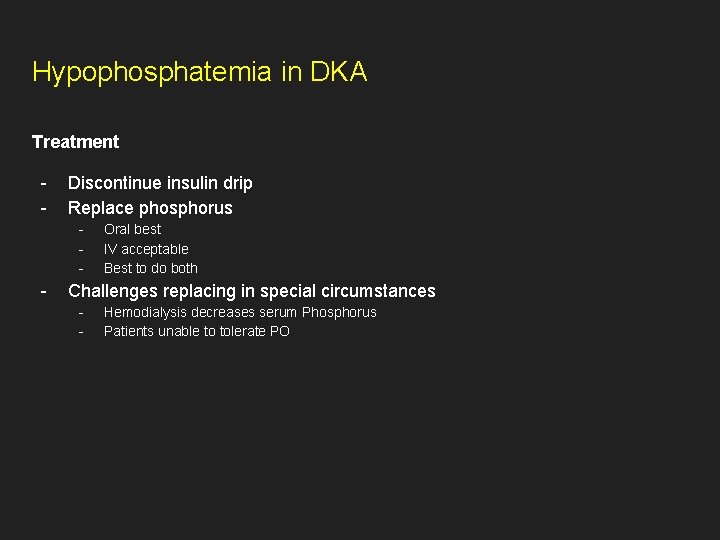
Hypophosphatemia in DKA Treatment - Discontinue insulin drip Replace phosphorus - - Oral best IV acceptable Best to do both Challenges replacing in special circumstances - Hemodialysis decreases serum Phosphorus Patients unable to tolerate PO
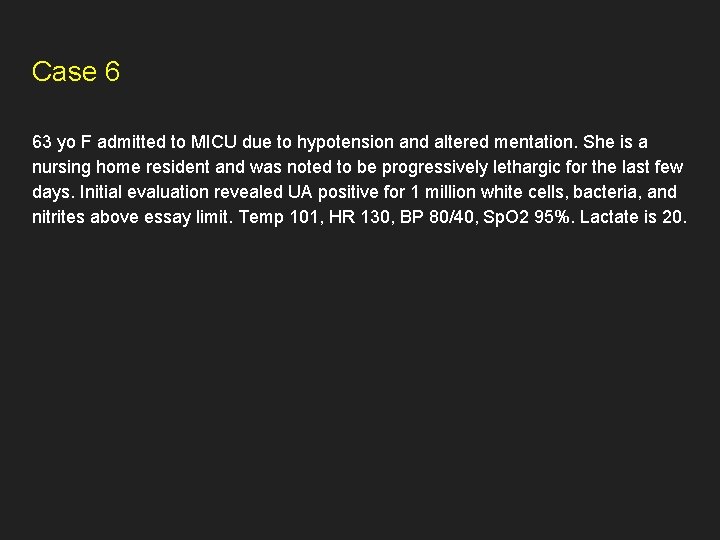
Case 6 63 yo F admitted to MICU due to hypotension and altered mentation. She is a nursing home resident and was noted to be progressively lethargic for the last few days. Initial evaluation revealed UA positive for 1 million white cells, bacteria, and nitrites above essay limit. Temp 101, HR 130, BP 80/40, Sp. O 2 95%. Lactate is 20.
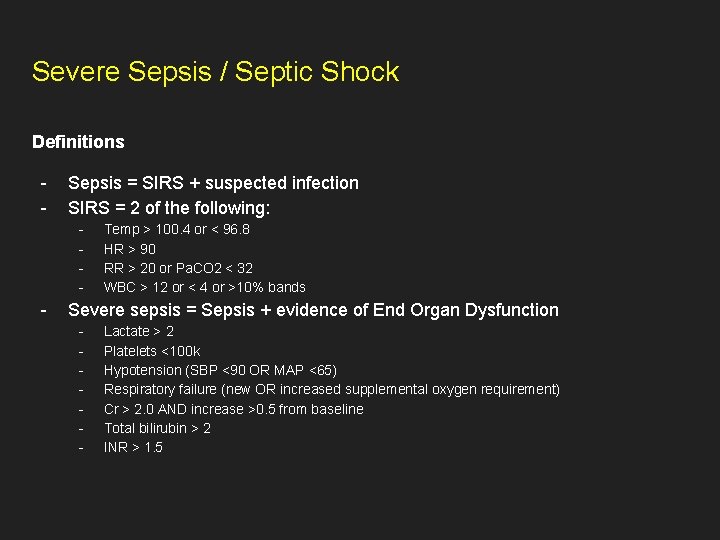
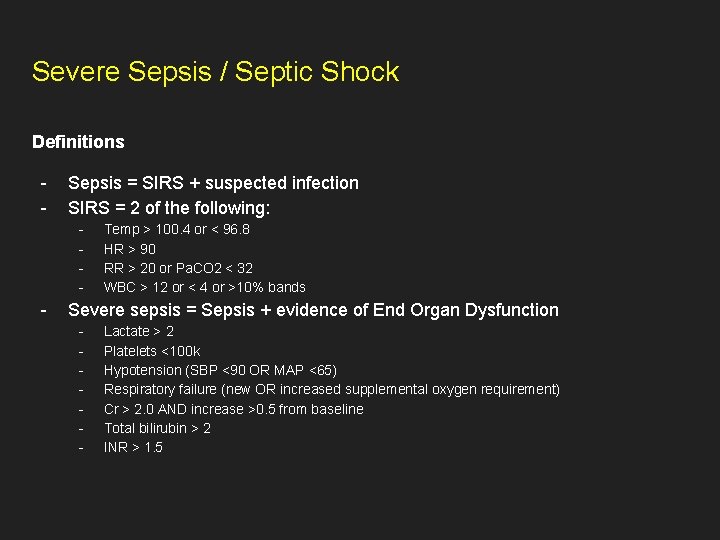
Severe Sepsis / Septic Shock Definitions - Sepsis = SIRS + suspected infection SIRS = 2 of the following: - - Temp > 100. 4 or < 96. 8 HR > 90 RR > 20 or Pa. CO 2 < 32 WBC > 12 or < 4 or >10% bands Severe sepsis = Sepsis + evidence of End Organ Dysfunction - Lactate > 2 Platelets <100 k Hypotension (SBP <90 OR MAP <65) Respiratory failure (new OR increased supplemental oxygen requirement) Cr > 2. 0 AND increase >0. 5 from baseline Total bilirubin > 2 INR > 1. 5
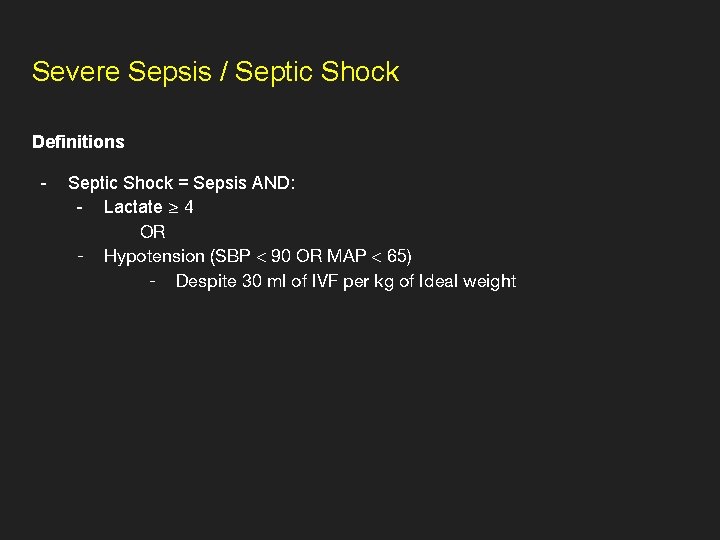
Severe Sepsis / Septic Shock Definitions - Septic Shock = Sepsis AND: - Lactate ≥ 4 OR - Hypotension (SBP < 90 OR MAP < 65) - Despite 30 ml of IVF per kg of Ideal weight
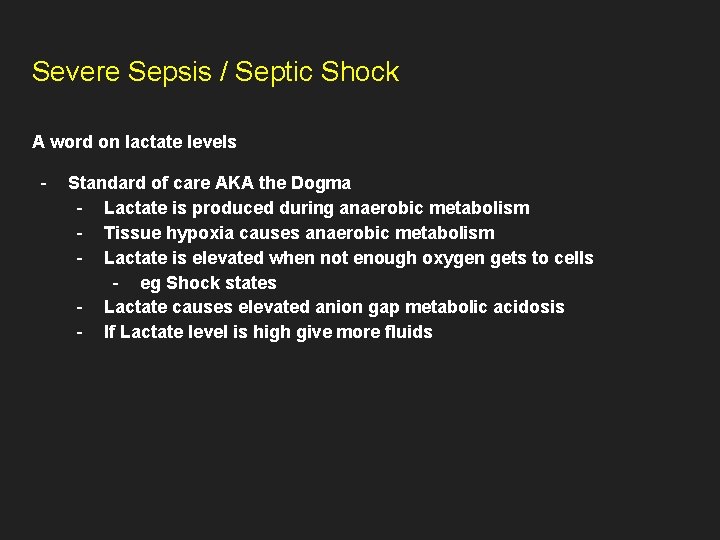
Severe Sepsis / Septic Shock A word on lactate levels - Standard of care AKA the Dogma - Lactate is produced during anaerobic metabolism - Tissue hypoxia causes anaerobic metabolism - Lactate is elevated when not enough oxygen gets to cells - eg Shock states - Lactate causes elevated anion gap metabolic acidosis - If Lactate level is high give more fluids
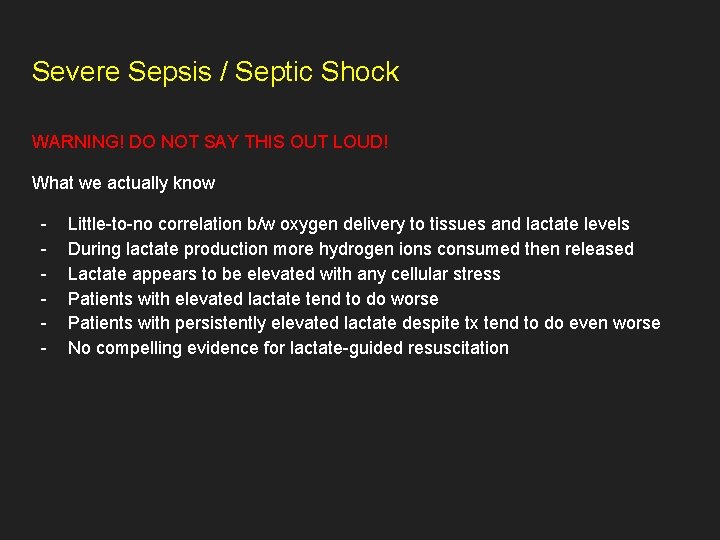
Severe Sepsis / Septic Shock WARNING! DO NOT SAY THIS OUT LOUD! What we actually know - Little-to-no correlation b/w oxygen delivery to tissues and lactate levels During lactate production more hydrogen ions consumed then released Lactate appears to be elevated with any cellular stress Patients with elevated lactate tend to do worse Patients with persistently elevated lactate despite tx tend to do even worse No compelling evidence for lactate-guided resuscitation
Severe Sepsis / Septic Shock Treatment - - Timely antibiotics - Retrospective studies suggest worse outcomes if abx are delayed - Shotgun approach is acceptable Intravenous fluids - 30 cc/kg of ideal weight - Balanced crystalloids preferred (eg LR, PLASMALYTE, NORMOSOL, etc) - There is potential benefit for albumin infusions in specific circumstances
Severe Sepsis / Septic Shock A word on IV fluids WARNING! DO NOT SAY THIS OUT LOUD! - There is no evidence to suggest 30 cc/kg is superior to other doses There is little evidence to suggest IVF is truly beneficial Identically beneficial response to fluids in every patient seems implausible Utility in assessing fluid responsiveness? - No reliable / accurate method Most evidence for passive leg raise and pulse pressure variation Some evidence for Bioreactance (eg NICOM) If fluid responsiveness is proven, what then? - No reliable way of assessing actual fluid status
Severe Sepsis / Septic Shock Things are not looking good… Pressors - Norepinephrine Epinephrine Vasopressor Dopamine Phenylephrine
Case 7 34 yo F presents to the ED complaining she feels unwell. She was noted to have a low grade fever 100. 0 and appeared restless. Before she could provide any more information she had an episode of generalized tonic-clonic seizure. She was given 2 mg of ativan which failed to break the seizure. She underwent rapid sequence intubation and was sedated with propofol. Her seizures visibly stopped and she was brought to MICU under your care. In the interim she is becoming progressively more hypotensive
Thyroid Storm Overview - Rare - - Significant mortality - - 10 -30% Can develop in setting of chronic thyroid conditions - - 0. 2 per 100, 000 per year Graves, toxic goiter, solitary toxic adenoma) Particularly with irregular use or discontinuation of anti-thyroid medications More often precipitated by surgery, trauma, acute iodine load
Thyroid Storm Clinical features - CV - - Fever Altered mentation - - Tachycardia, HF, hypotension, cardiac arrest Often predominate - Majority have tachycardia and/or a-fib Agitation, anxiety, delirium, stupor, coma Associated with higher mortality GI - N/V/D, abdominal pain Hepatic failure and/or jaundice
Thyroid Storm Laboratory findings - Low TSH, high T 4 and/or T 3 - - May have isolated T 3 elevation without significant alterations in TSH or T 4 Usually no worse than uncomplicated thyrotoxicosis Has to be compatible but not necessary for diagnosis of thyroid storm Mild hyperglycemia Mild hypercalcemia Abnormal LFTs Elevated or reduced WBCs
Thyroid Storm Diagnosis - No universally accepted criteria or validated clinical tools 1993 Burch and Wartofsky came up with a handy table (next slide) - Score of 45 or more is highly suggestive of thyroid storm 25 -44 supports the diagnosis <25 Thyroid storm is unlikely
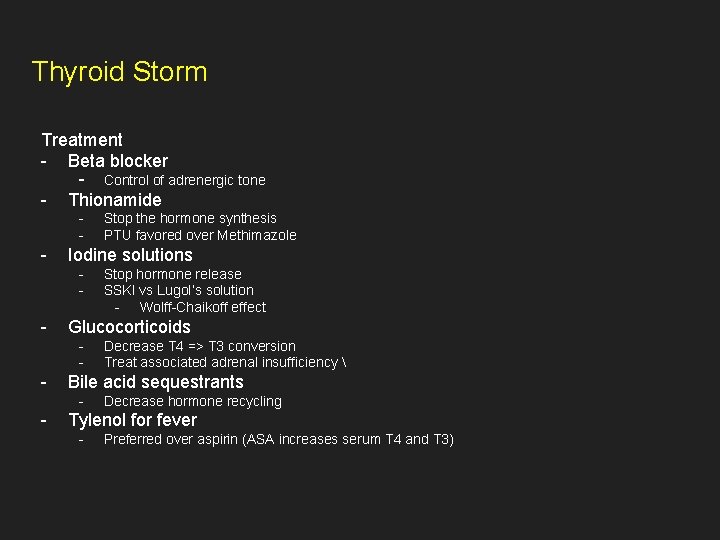
Thyroid Storm Treatment - Beta blocker - Control of adrenergic tone - Thionamide - - Iodine solutions - - Decrease T 4 => T 3 conversion Treat associated adrenal insufficiency Bile acid sequestrants - - Stop hormone release SSKI vs Lugol’s solution - Wolff-Chaikoff effect Glucocorticoids - - Stop the hormone synthesis PTU favored over Methimazole Decrease hormone recycling Tylenol for fever - Preferred over aspirin (ASA increases serum T 4 and T 3)
Case 8 42 yo female presenting after reported seizure. The episode lasted 1 -2 minutes and resolved on its own. Her relatives brought her to the ED and she was ultimately admitted to general hospital floor. Rapid response is called overnight. You arrive to find the patient actively seizing.
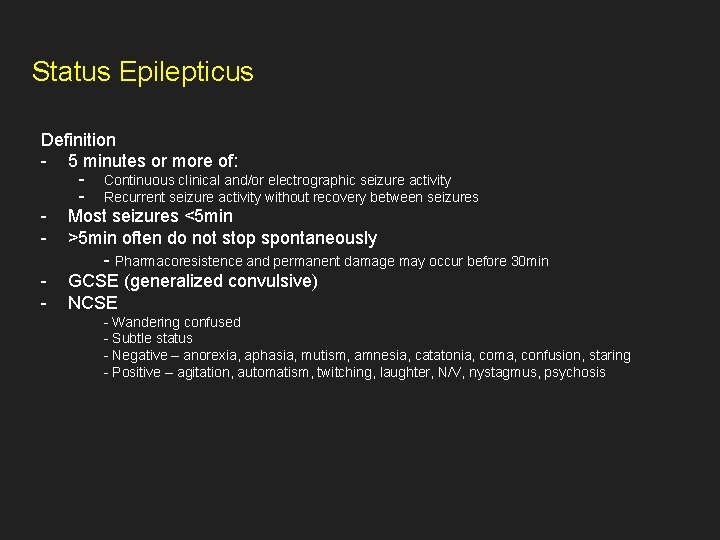
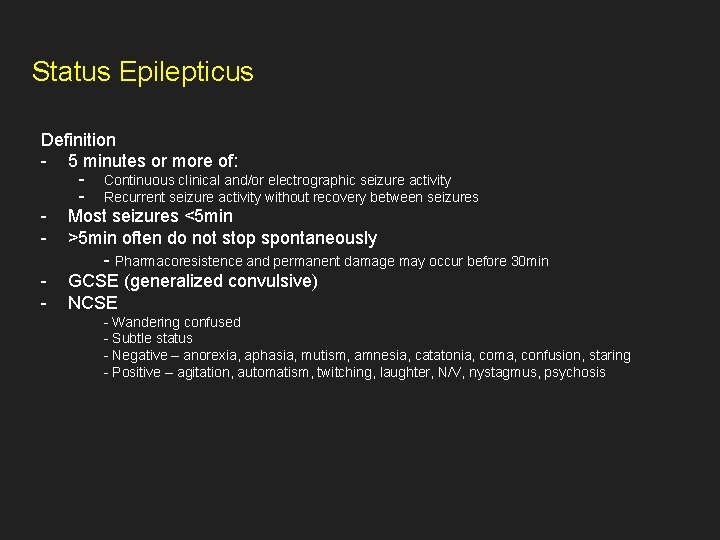
Status Epilepticus Definition - 5 minutes or more of: - Continuous clinical and/or electrographic seizure activity - Recurrent seizure activity without recovery between seizures - Most seizures <5 min - >5 min often do not stop spontaneously - Pharmacoresistence and permanent damage may occur before 30 min - GCSE (generalized convulsive) - NCSE - Wandering confused - Subtle status - Negative – anorexia, aphasia, mutism, amnesia, catatonia, coma, confusion, staring - Positive – agitation, automatism, twitching, laughter, N/V, nystagmus, psychosis
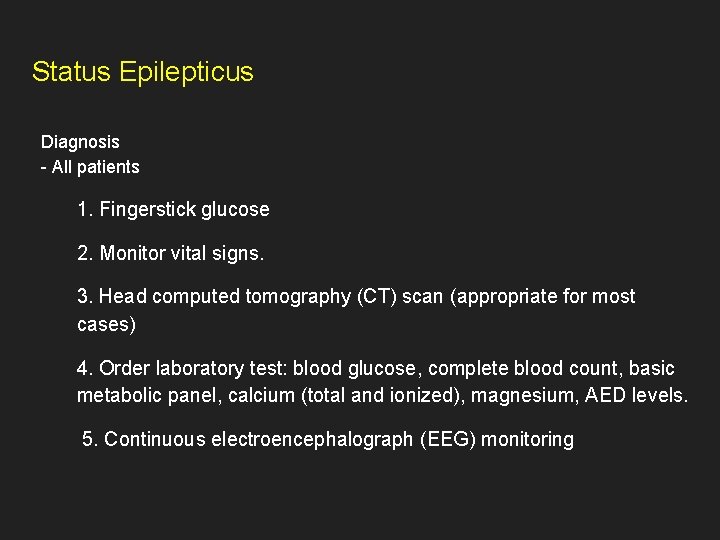
Status Epilepticus Diagnosis - All patients 1. Fingerstick glucose 2. Monitor vital signs. 3. Head computed tomography (CT) scan (appropriate for most cases) 4. Order laboratory test: blood glucose, complete blood count, basic metabolic panel, calcium (total and ionized), magnesium, AED levels. 5. Continuous electroencephalograph (EEG) monitoring
Status Epilepticus Diagnosis - All patients 1. Fingerstick glucose 2. Monitor vital signs. 3. Head computed tomography (CT) scan (appropriate for most cases) 4. Order laboratory test: blood glucose, complete blood count, basic metabolic panel, calcium (total and ionized), magnesium, AED levels. 5. Continuous electroencephalograph (EEG) monitoring
Status Epilepticus - Consider based on clinical presentation 1. Brain magnetic resonance imaging (MRI) 2. Lumbar puncture (LP) 3. Comprehensive toxicology panel including toxins that frequently cause seizures (i. e. isoniazid, tricyclic antidepressants, theophylline, cocaine, sympathomimetics, alcohol, organophosphates, and cyclosporine) 4. Other laboratory tests: liver function tests, serial troponins, type and hold, coagulation studies, arterial blood gas, AED levels, toxicology screen (urine and blood), and inborn errors of metabolism
Status Epilepticus Prognosis - GCSE - - Mortality - At discharge 9 -21% - At 30 days 19 -27% - At 90 days 19% Morbidity - Severe neurologic/cognitive sequelae 11 -16% - Functional deterioration 23 -26%
Status Epilepticus - In patients with adequate therapy, mortality ~8% - 45% mortality with inadequate therapy - Insufficient dose - Wrong route - Delay in treatment - Inadequate ventilation - Medical complications
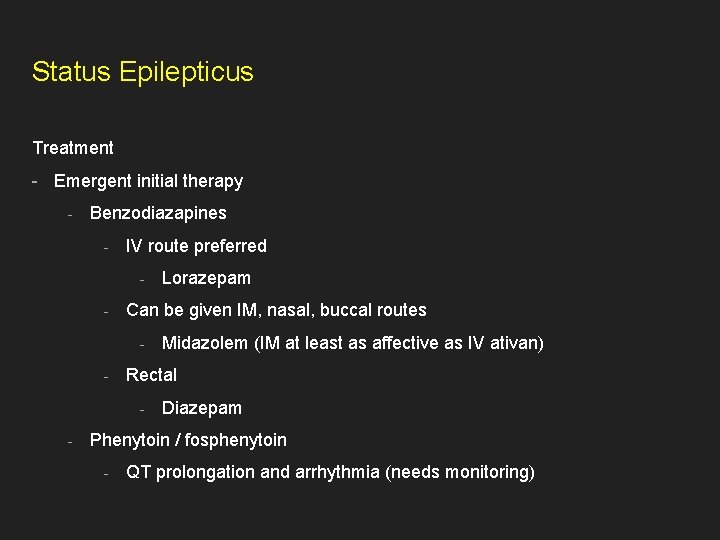
Status Epilepticus Treatment - Emergent initial therapy - Benzodiazapines - IV route preferred - - Can be given IM, nasal, buccal routes - - Midazolem (IM at least as affective as IV ativan) Rectal - - Lorazepam Diazepam Phenytoin / fosphenytoin - QT prolongation and arrhythmia (needs monitoring)
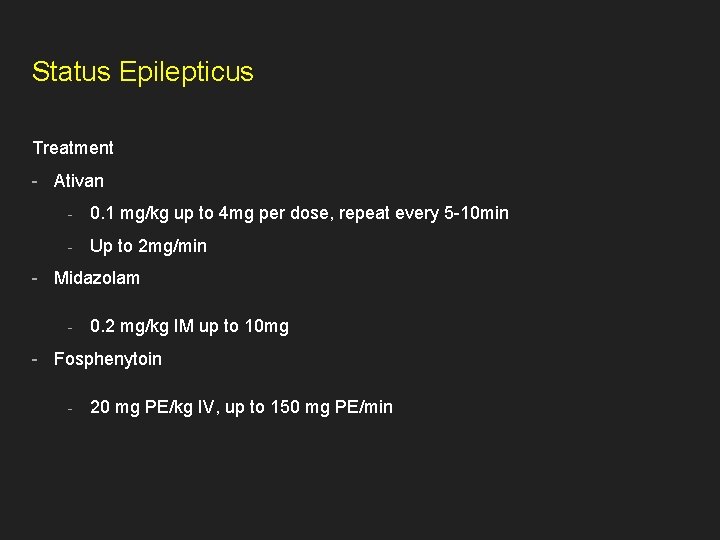
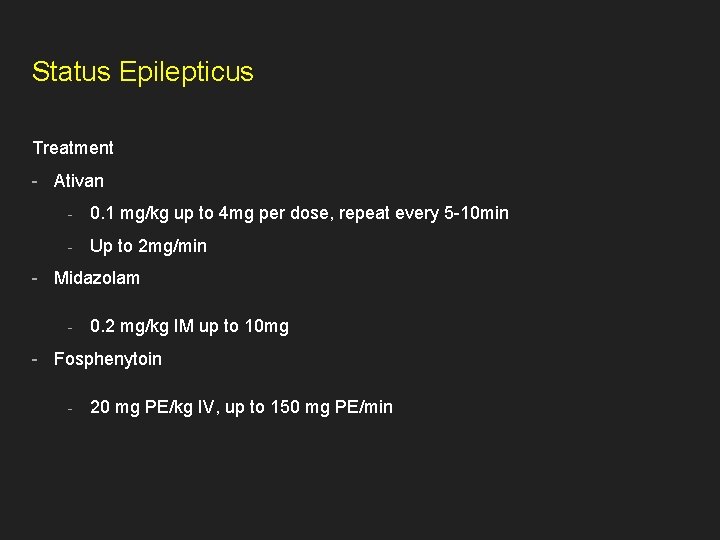
Status Epilepticus Treatment - Ativan - 0. 1 mg/kg up to 4 mg per dose, repeat every 5 -10 min - Up to 2 mg/min - Midazolam - 0. 2 mg/kg IM up to 10 mg - Fosphenytoin - 20 mg PE/kg IV, up to 150 mg PE/min
 Kirill filimonov
Kirill filimonov Kirill belashchenko
Kirill belashchenko Followup:actionitems
Followup:actionitems Follow-up visits
Follow-up visits Followup edge
Followup edge Documentary payment
Documentary payment Landsat collection 1 vs collection 2
Landsat collection 1 vs collection 2 Chapter 27 empire and expansion
Chapter 27 empire and expansion Nata a torino nel 1909
Nata a torino nel 1909 Trait and factor theory steps
Trait and factor theory steps Kip domovine leta 188 likovi
Kip domovine leta 188 likovi The reform discussed by governor johnson in this excerpt
The reform discussed by governor johnson in this excerpt Examples of agency problems
Examples of agency problems Ssrs overview
Ssrs overview Overview of passives
Overview of passives Overview on the national tuberculosis elimination program
Overview on the national tuberculosis elimination program Nims components
Nims components Animal farm overview
Animal farm overview Trajectory data mining an overview
Trajectory data mining an overview Overview manajemen keuangan
Overview manajemen keuangan Onap architecture
Onap architecture Algori
Algori Cell signaling overview
Cell signaling overview Chapter 8 section 2 photosynthesis answer key
Chapter 8 section 2 photosynthesis answer key Introduction product overview
Introduction product overview Overview
Overview Nitrogen group
Nitrogen group Maximo work order priority
Maximo work order priority Gprs overview
Gprs overview Systemic veins
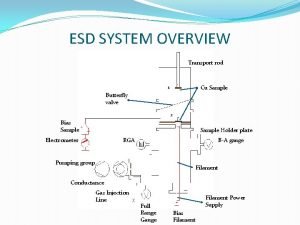
Systemic veins System overview sample
System overview sample Cuda overview
Cuda overview Introduction product overview
Introduction product overview Vpls overview
Vpls overview An overview of data warehousing and olap technology
An overview of data warehousing and olap technology Market overview managed file transfer solutions
Market overview managed file transfer solutions Chapter 1 an overview of financial management
Chapter 1 an overview of financial management What is multinational financial management
What is multinational financial management What is product line depth
What is product line depth British school system
British school system Classification of matter
Classification of matter Introduction to distributed computing
Introduction to distributed computing Overview of financial management
Overview of financial management Solar massachusetts renewable target (smart) program
Solar massachusetts renewable target (smart) program Pulmonary circulation
Pulmonary circulation Introduction to wan
Introduction to wan Dual mode in os
Dual mode in os Iptv technology
Iptv technology Computer system overview
Computer system overview General overview
General overview Mobile commerce overview
Mobile commerce overview Intro to human resource management
Intro to human resource management Brigrance
Brigrance Hyper-v overview
Hyper-v overview Types of investment banks
Types of investment banks Overview of http
Overview of http Overview of cellular respiration
Overview of cellular respiration Overview of grid computing
Overview of grid computing Overview of government accounting
Overview of government accounting Owasp asvs level 2
Owasp asvs level 2 Dna purification overview
Dna purification overview Example of nursing process
Example of nursing process