Clinical Obstetric Case Damietta 7 12 2012 Specialized

Clinical Obstetric Case Damietta 7 -12 -2012 Specialized Hospital Dr Mohamed El Sherbiny MD Obstetrics&Gynecology
A-History B-Examination C-Laboratory investigations D- Imaging (U/S color Doppler & MRI) Diagnosis

A-History
History § Personal History § Complaint § Menstrual § Obstetric history § Past history § Family history § Present history
History § Personal History § Complaint § Present history § Menstrual § Obstetric history § Past history § Family history Kaser Aini
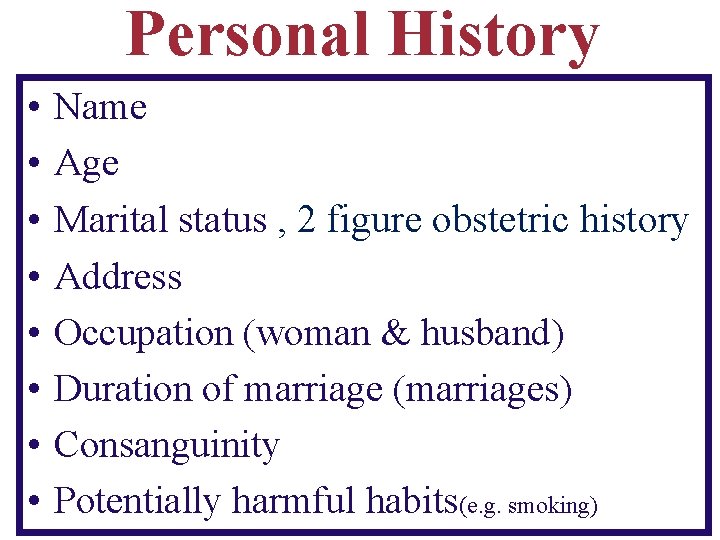
Personal History • • Name Age Marital status , 2 figure obstetric history Address Occupation (woman & husband) Duration of marriage (marriages) Consanguinity Potentially harmful habits(e. g. smoking)
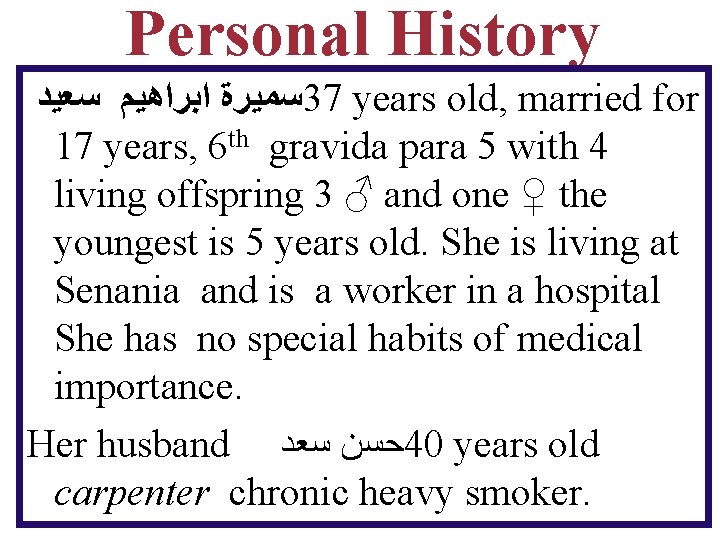
Personal History ﺳﻤﻴﺮﺓ ﺍﺑﺮﺍﻫﻴﻢ ﺳﻌﻴﺪ 37 years old, married for 17 years, 6 th gravida para 5 with 4 living offspring 3 ♂ and one ♀ the youngest is 5 years old. She is living at Senania and is a worker in a hospital She has no special habits of medical importance. Her husband ﺣﺴﻦ ﺳﻌﺪ 40 years old carpenter chronic heavy smoker.
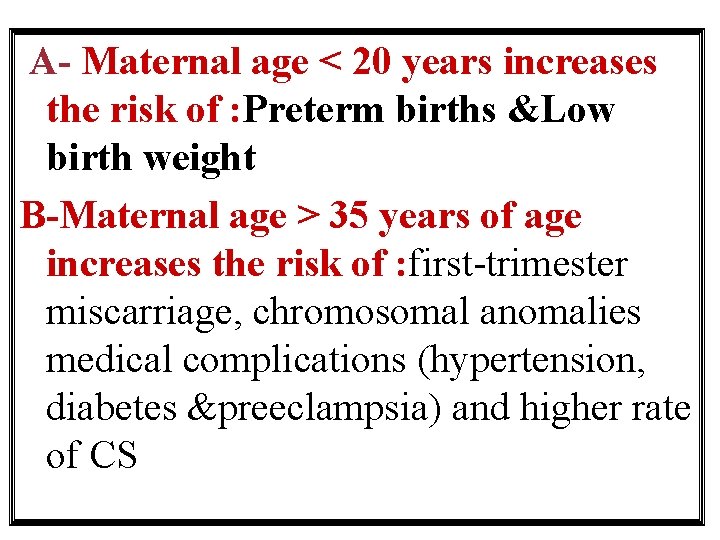
A- Maternal age < 20 years increases the risk of : Preterm births &Low birth weight B-Maternal age > 35 years of age increases the risk of : first-trimester miscarriage, chromosomal anomalies medical complications (hypertension, diabetes &preeclampsia) and higher rate of CS
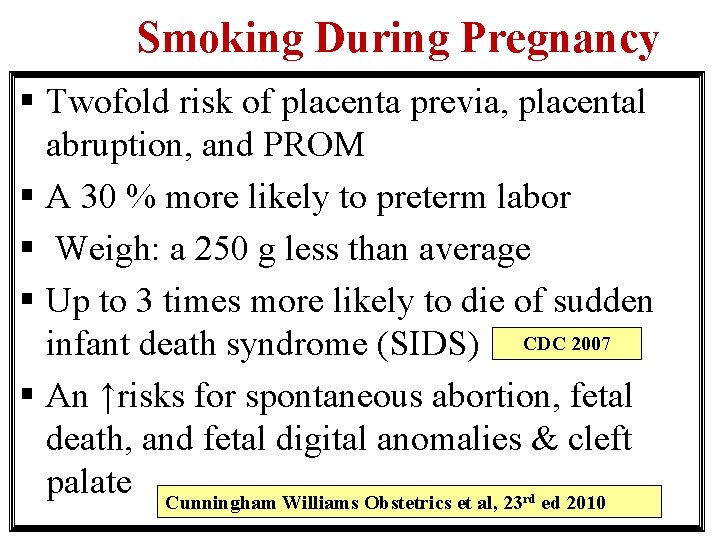
Smoking During Pregnancy § Twofold risk of placenta previa, placental abruption, and PROM § A 30 % more likely to preterm labor § Weigh: a 250 g less than average § Up to 3 times more likely to die of sudden infant death syndrome (SIDS) CDC 2007 § An ↑risks for spontaneous abortion, fetal death, and fetal digital anomalies & cleft palate Cunningham Williams Obstetrics et al, 23 ed 2010 rd
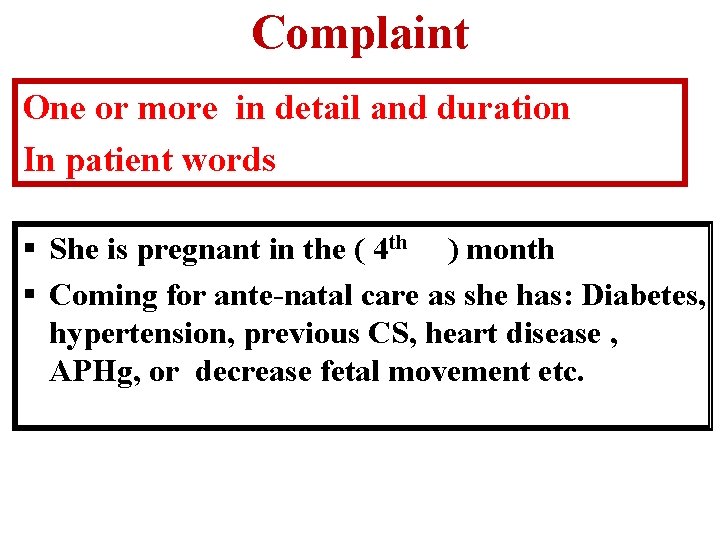
Complaint One or more in detail and duration In patient words § She is pregnant in the ( 4 th ) month § Coming for ante-natal care as she has: Diabetes, hypertension, previous CS, heart disease , APHg, or decrease fetal movement etc.
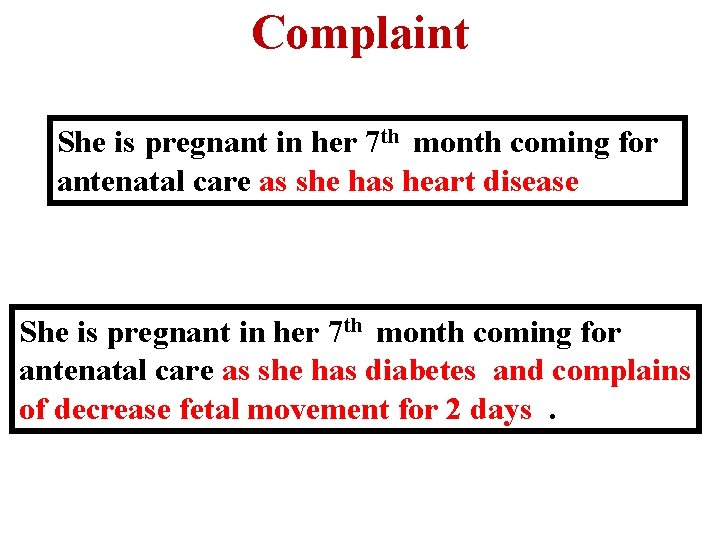
Complaint She is pregnant in her 7 th month coming for antenatal care as she has heart disease She is pregnant in her 7 th month coming for antenatal care as she has diabetes and complains of decrease fetal movement for 2 days.
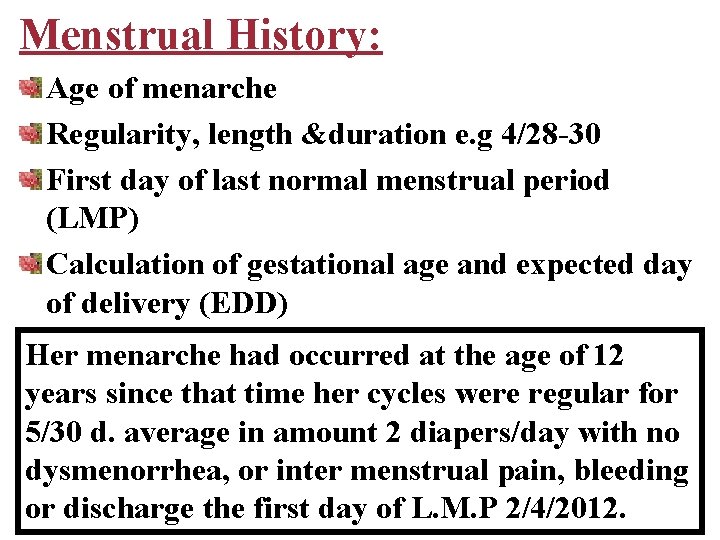
Menstrual History: Age of menarche Regularity, length &duration e. g 4/28 -30 First day of last normal menstrual period (LMP) Calculation of gestational age and expected day of delivery (EDD) Her menarche had occurred at the age of 12 years since that time her cycles were regular for 5/30 d. average in amount 2 diapers/day with no dysmenorrhea, or inter menstrual pain, bleeding or discharge the first day of L. M. P 2/4/2012.
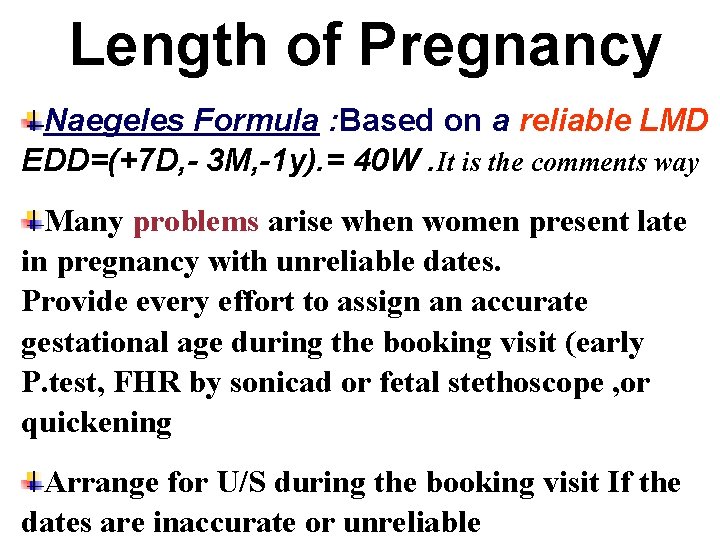
Length of Pregnancy Naegeles Formula : Based on a reliable LMD EDD=(+7 D, - 3 M, -1 y). = 40 W. It is the comments way Many problems arise when women present late in pregnancy with unreliable dates. Provide every effort to assign an accurate gestational age during the booking visit (early P. test, FHR by sonicad or fetal stethoscope , or quickening Arrange for U/S during the booking visit If the dates are inaccurate or unreliable
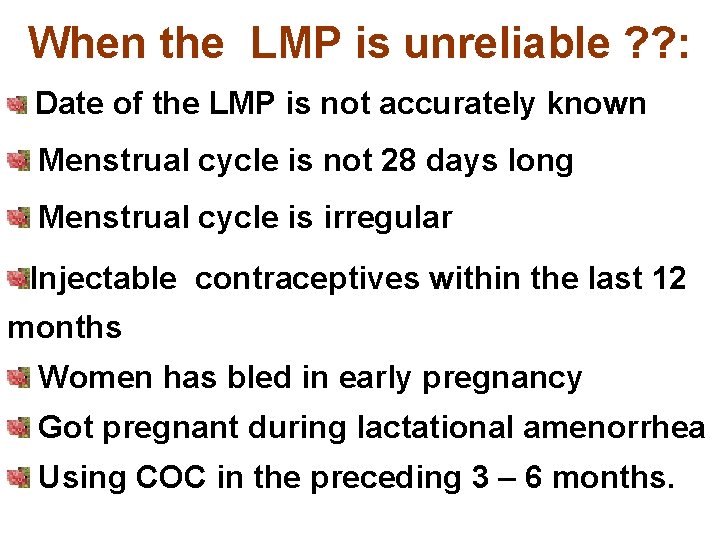
When the LMP is unreliable ? ? : Date of the LMP is not accurately known Menstrual cycle is not 28 days long Menstrual cycle is irregular Injectable contraceptives within the last 12 months Women has bled in early pregnancy Got pregnant during lactational amenorrhea Using COC in the preceding 3 – 6 months.
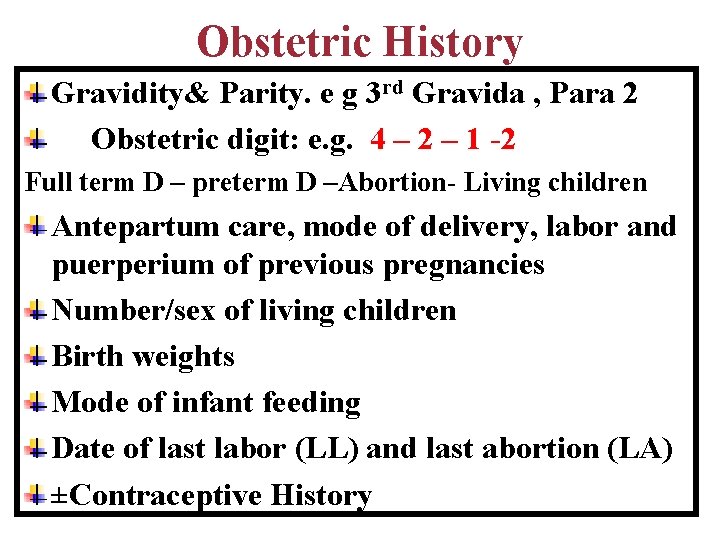
Obstetric History Gravidity& Parity. e g 3 rd Gravida , Para 2 Obstetric digit: e. g. 4 – 2 – 1 -2 Full term D – preterm D –Abortion- Living children Antepartum care, mode of delivery, labor and puerperium of previous pregnancies Number/sex of living children Birth weights Mode of infant feeding Date of last labor (LL) and last abortion (LA) ±Contraceptive History
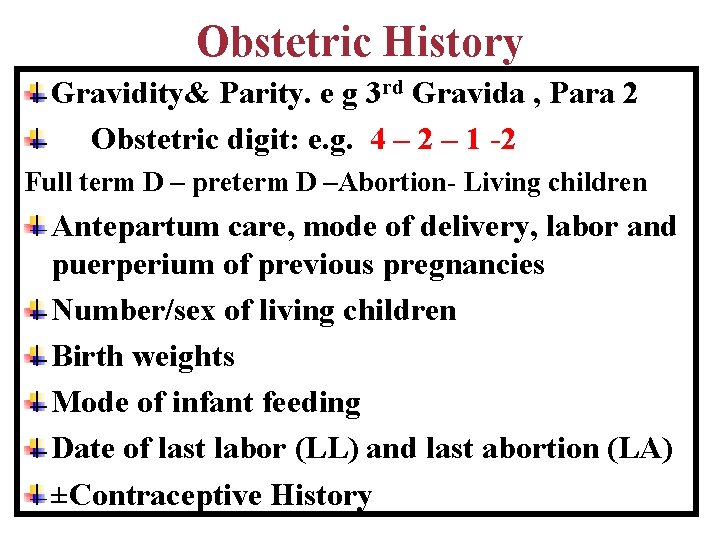
Obstetric History Gravidity& Parity. e g 3 rd Gravida , Para 2 Obstetric digit: e. g. 4 – 2 – 1 -2 Full term D – preterm D –Abortion- Living children Antepartum care, mode of delivery, labor and puerperium of previous pregnancies Number/sex of living children Birth weights Mode of infant feeding Date of last labor (LL) and last abortion (LA) ±Contraceptive History
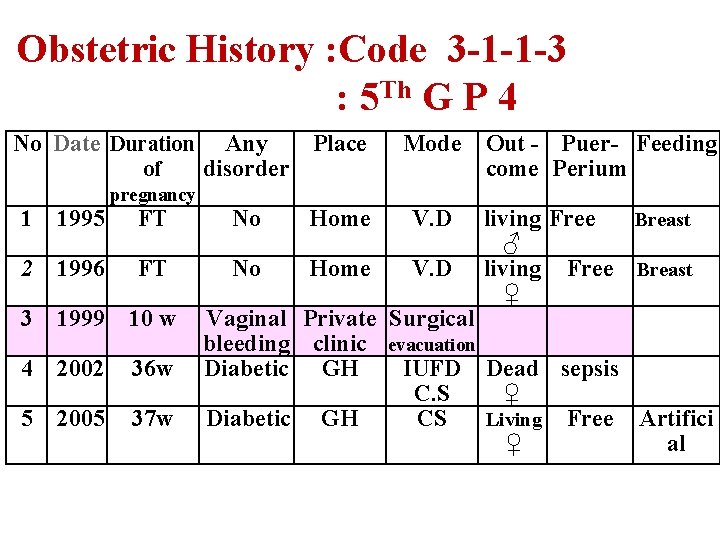
Obstetric History : Code 3 -1 -1 -3 : 5 Th G P 4 No Date Duration of 1 1995 2 pregnancy Any Place disorder Mode FT No Home V. D 1996 FT No Home V. D 3 1999 10 w 4 2002 36 w 5 2005 37 w Out - Puer- Feeding come Perium Breast living Free ♂ living Free Breast ♀ Vaginal Private Surgical bleeding clinic evacuation Diabetic GH IUFD Dead sepsis C. S ♀ Diabetic GH CS Living Free Artifici ♀ al
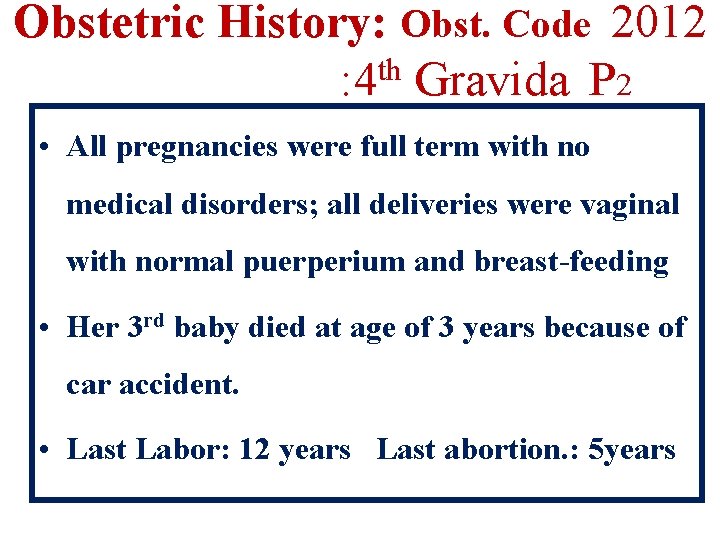
Obstetric History: Obst. Code 2012 : 4 th Gravida P 2 • All pregnancies were full term with no medical disorders; all deliveries were vaginal with normal puerperium and breast-feeding • Her 3 rd baby died at age of 3 years because of car accident. • Last Labor: 12 years Last abortion. : 5 years
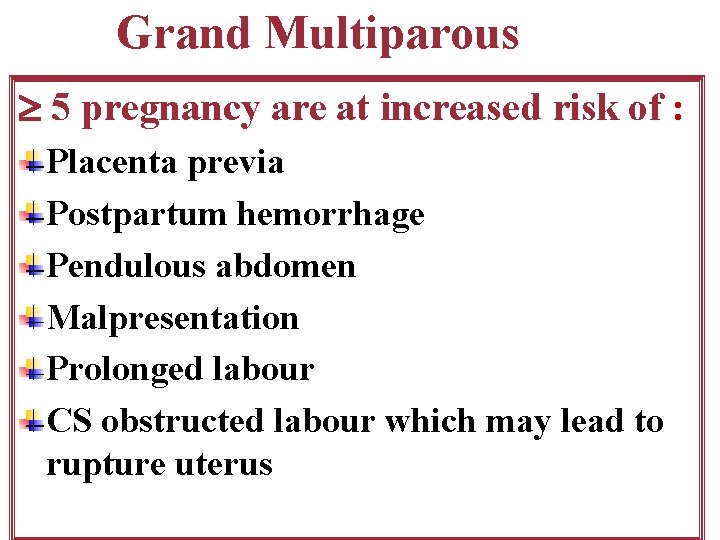
Grand Multiparous 5 pregnancy are at increased risk of : Placenta previa Postpartum hemorrhage Pendulous abdomen Malpresentation Prolonged labour CS obstructed labour which may lead to rupture uterus
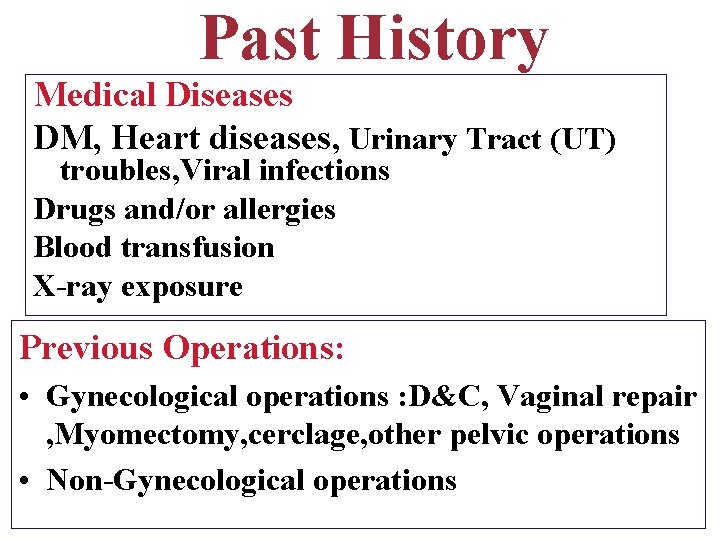
Past History Medical Diseases DM, Heart diseases, Urinary Tract (UT) troubles, Viral infections Drugs and/or allergies Blood transfusion X-ray exposure Previous Operations: • Gynecological operations : D&C, Vaginal repair , Myomectomy, cerclage, other pelvic operations • Non-Gynecological operations
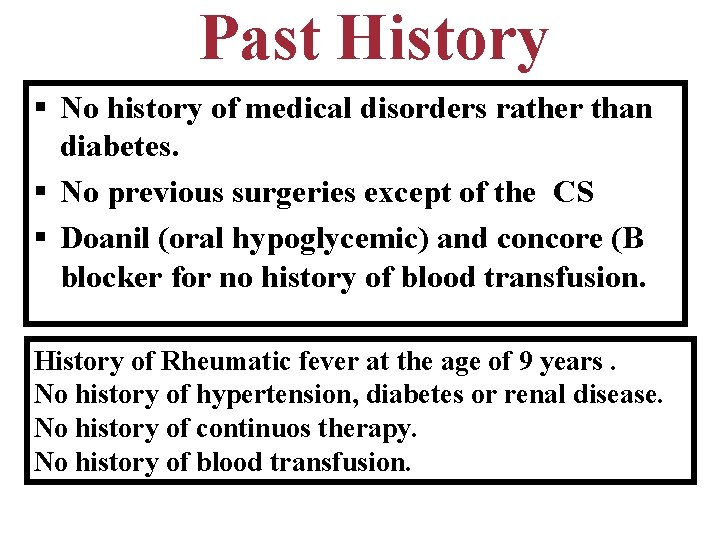
Past History § No history of medical disorders rather than diabetes. § No previous surgeries except of the CS § Doanil (oral hypoglycemic) and concore (B blocker for no history of blood transfusion. History of Rheumatic fever at the age of 9 years. No history of hypertension, diabetes or renal disease. No history of continuos therapy. No history of blood transfusion.
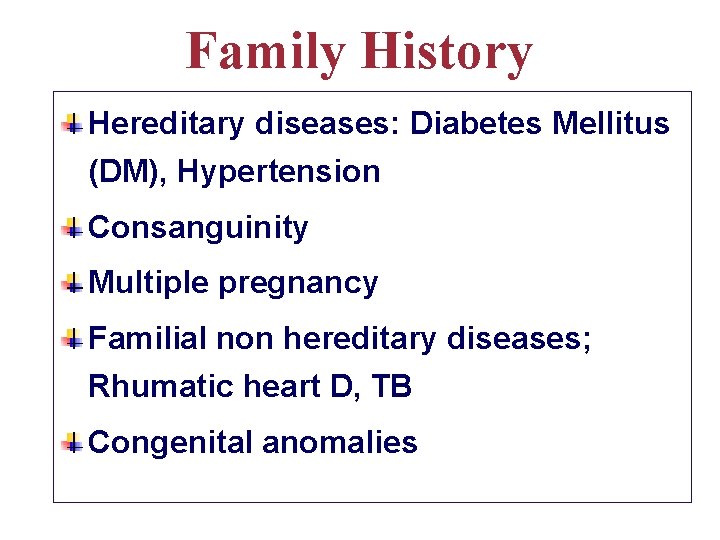
Family History Hereditary diseases: Diabetes Mellitus (DM), Hypertension Consanguinity Multiple pregnancy Familial non hereditary diseases; Rhumatic heart D, TB Congenital anomalies
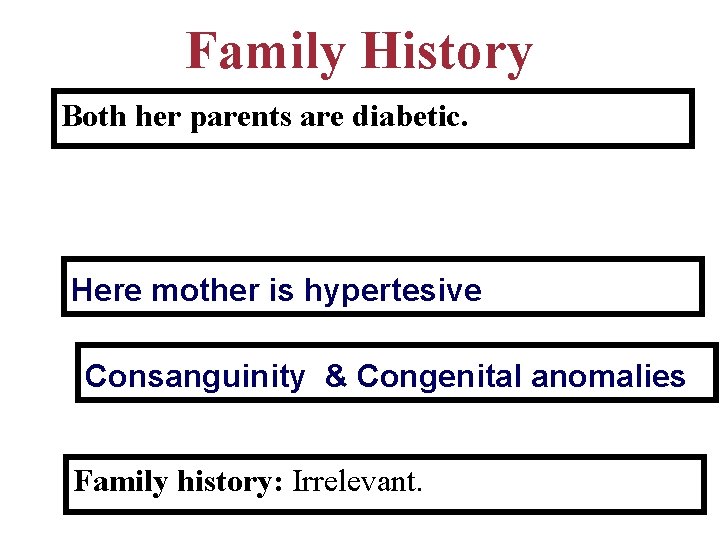
Family History Both her parents are diabetic. Here mother is hypertesive Consanguinity & Congenital anomalies Family history: Irrelevant.

Others History q. Family Planning History Last method used &duration Date and reason of discontinuation q. Immunization History q. Breast-feeding History
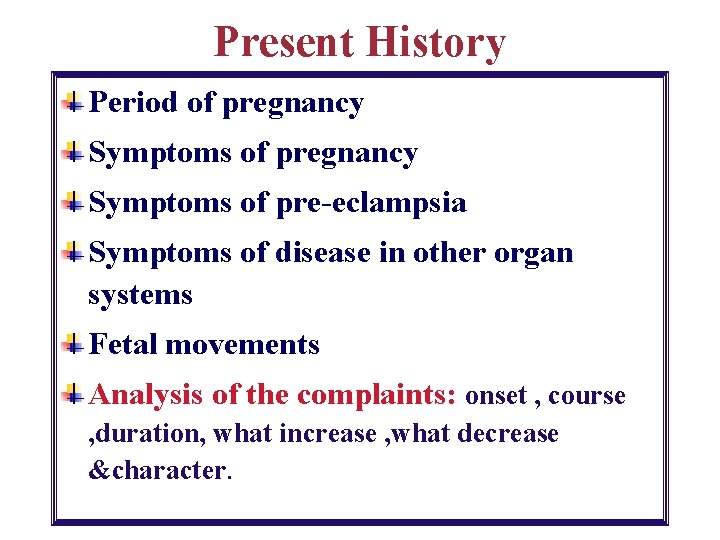
Present History Period of pregnancy Symptoms of pre-eclampsia Symptoms of disease in other organ systems Fetal movements Analysis of the complaints: onset , course , duration, what increase , what decrease &character.
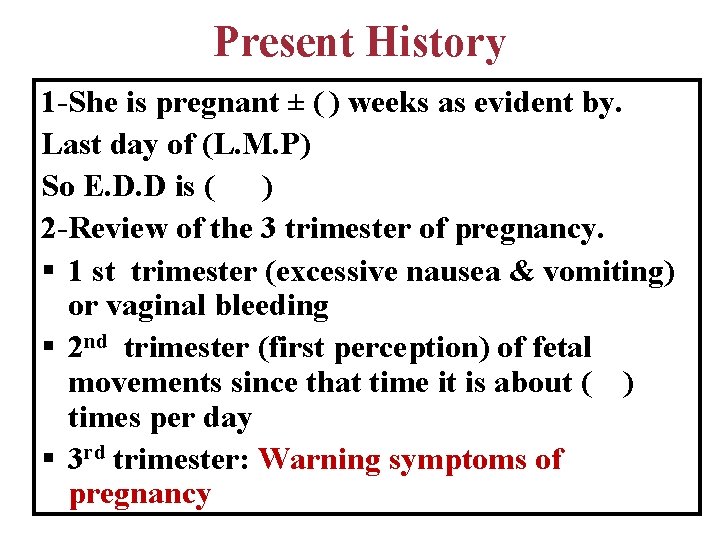
Present History 1 -She is pregnant ± ( ) weeks as evident by. Last day of (L. M. P) So E. D. D is ( ) 2 -Review of the 3 trimester of pregnancy. § 1 st trimester (excessive nausea & vomiting) or vaginal bleeding § 2 nd trimester (first perception) of fetal movements since that time it is about ( ) times per day § 3 rd trimester: Warning symptoms of pregnancy
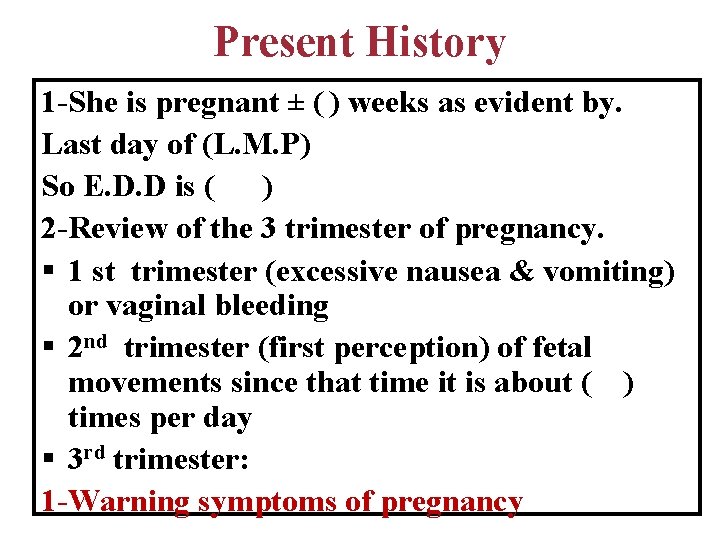
Present History 1 -She is pregnant ± ( ) weeks as evident by. Last day of (L. M. P) So E. D. D is ( ) 2 -Review of the 3 trimester of pregnancy. § 1 st trimester (excessive nausea & vomiting) or vaginal bleeding § 2 nd trimester (first perception) of fetal movements since that time it is about ( ) times per day § 3 rd trimester: 1 -Warning symptoms of pregnancy
Present History 4 - Specific symptoms and history taking related to the complaint & Analysis 5 -Admission 6 -Therapy 7 -Blood and urine analysis Ultrasonography and Its results 8 -Plan of management 9 -Mode and time of delivery 10 - Review of other body systems revealed
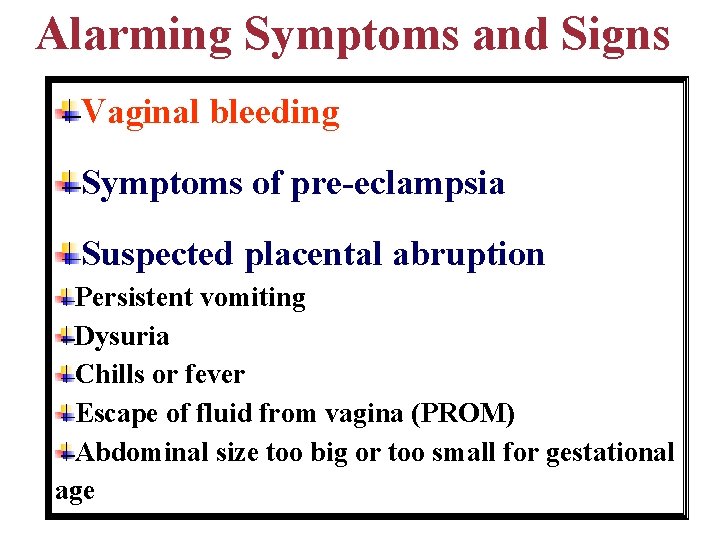
Alarming Symptoms and Signs Vaginal bleeding Symptoms of pre-eclampsia Suspected placental abruption Persistent vomiting Dysuria Chills or fever Escape of fluid from vagina (PROM) Abdominal size too big or too small for gestational age
Vaginal bleeding • < 20 weeks Threatened abortion • >20 weeks Antepartum hemorrhage
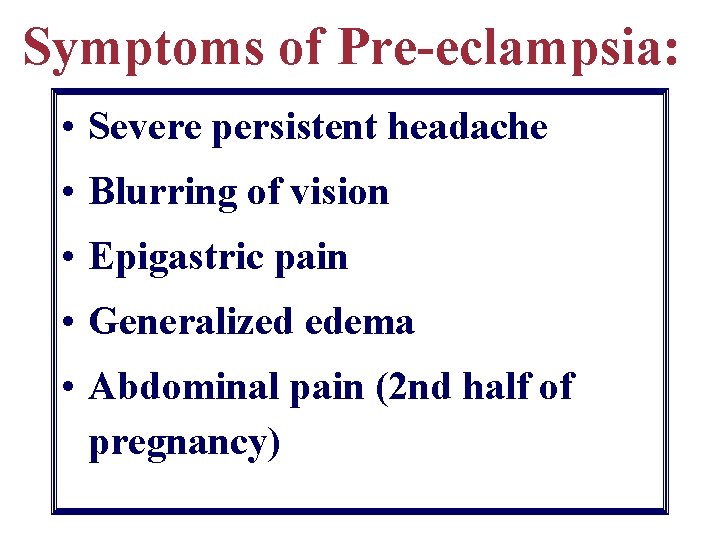
Symptoms of Pre-eclampsia: • Severe persistent headache • Blurring of vision • Epigastric pain • Generalized edema • Abdominal pain (2 nd half of pregnancy)
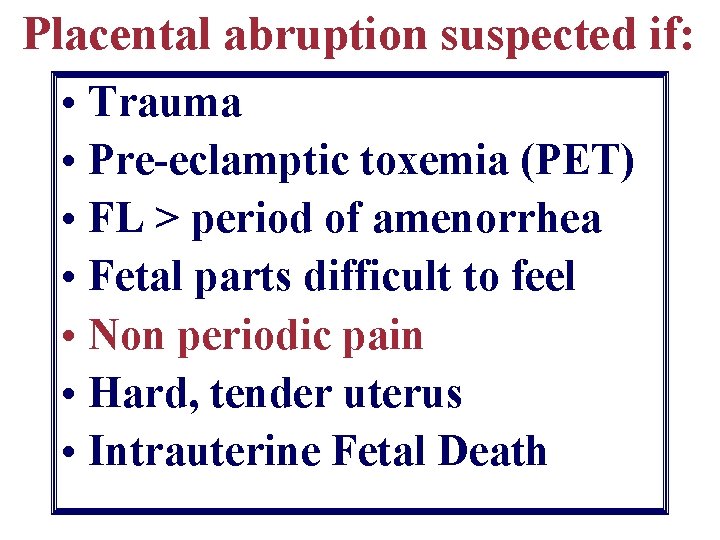
Placental abruption suspected if: • Trauma • Pre-eclamptic toxemia (PET) • FL > period of amenorrhea • Fetal parts difficult to feel • Non periodic pain • Hard, tender uterus • Intrauterine Fetal Death
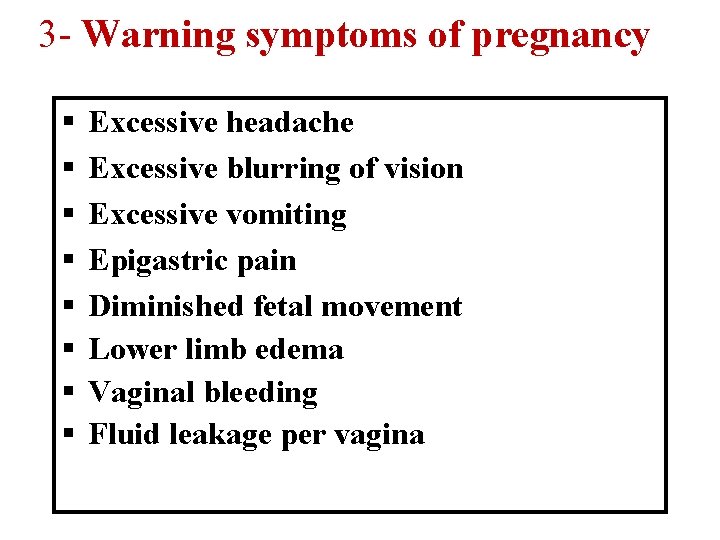
3 - Warning symptoms of pregnancy § § § § Excessive headache Excessive blurring of vision Excessive vomiting Epigastric pain Diminished fetal movement Lower limb edema Vaginal bleeding Fluid leakage per vagina
B. Examination
General (Systemic) Examination Physical signs: P , Temp , Bp& RR, weight, height face &Neck examination Heart and lung examination Breast examination Lower limb: Varicose veins &Edema Skeletal or neurological abnormalities
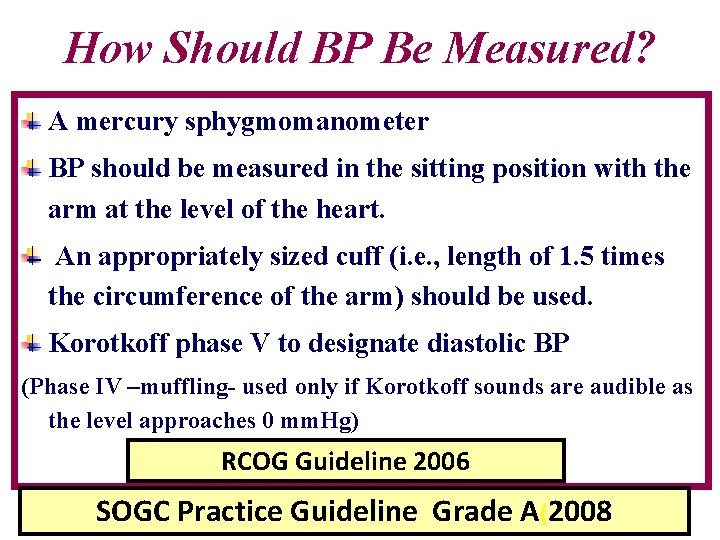
How Should BP Be Measured? A mercury sphygmomanometer BP should be measured in the sitting position with the arm at the level of the heart. An appropriately sized cuff (i. e. , length of 1. 5 times the circumference of the arm) should be used. Korotkoff phase V to designate diastolic BP (Phase IV –muffling- used only if Korotkoff sounds are audible as the level approaches 0 mm. Hg) RCOG Guideline 2006 SOGC Practice Guideline Grade A(2008
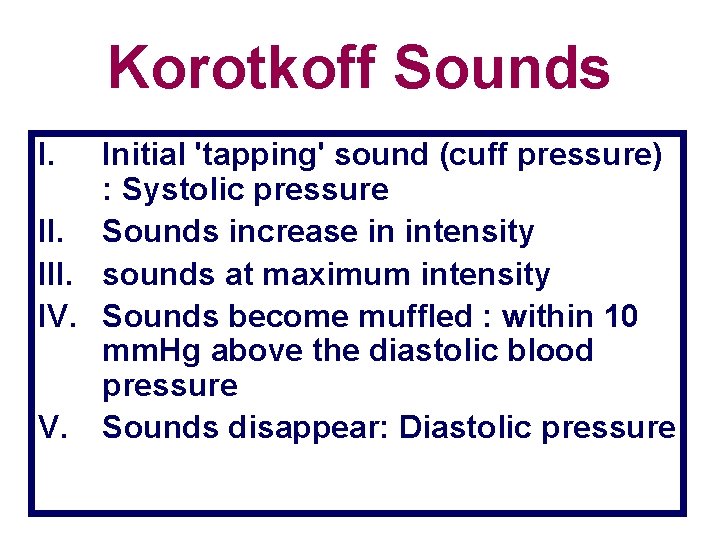
Korotkoff Sounds I. Initial 'tapping' sound (cuff pressure) : Systolic pressure II. Sounds increase in intensity III. sounds at maximum intensity IV. Sounds become muffled : within 10 mm. Hg above the diastolic blood pressure V. Sounds disappear: Diastolic pressure
How Should BP Be Measured? A mercury sphygmomanometer BP should be measured in the sitting position with the arm at the level of the heart. An appropriately sized cuff (i. e. , length of 1. 5 times the circumference of the arm) should be used. Korotkoff phase V to designate diastolic BP (Phase IV –muffling- used only if Korotkoff sounds are audible as the level approaches 0 mm. Hg) RCOG Guideline 2006 SOGC Practice Guideline Grade A(2008
. • Height: should be measured. As short ladies less than 150 cm are having higher incidence of contracted pelvis. • Gait: The way of walking. As limping or waddling gait is usually associated with oblique contracted pelvis. • Built: Under weight, average or obese (dystrophia Dystocia syndrome) [short, muscular, obese, hirshutism with higher incidence of android pelvis and occipto-posterior position).
Face and neck • 3 -Pallor of the mucus membranes (anemia). • Yellowish discoloration of the sclera (in day light) (Jaundice). • Butterfly pigmentation of the nose and cheeks (chloasma gravidarum). • Congested neck veins. • Enlarged thyroid (goiter)
• 4 - Chest and heart examination for any abnormalities. • 5 - Breast for sings of pregnancy, any abnormal masses, discharge or nipple abnormalities. Pregnant • breast ppears enlarged, warm, tender, nodular with colostrums passing out. • 6 -Lower limbs: • Lower limb edema in cases of P. I. H (by pressure at the ankle and lower tibia against a bone [pitting]). • Varicose veins. • ♦ Leg deformities as (bow legs) sings of an old rickets.
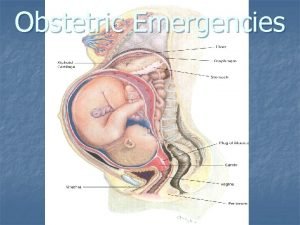
II- Abdominal examination • • • A-Inspection: General abdominal examination. Movements: respiratory or intestinal. In obstetrical examination: fetal movements. Shape and contour of the abdomen. Skin for any pigmentation (linea nigra or striae gravidarum). • Scars of previous operations (type of healing primary or secondary intention)
Midline structures • Subcostal angle: usually obtuse during pregnancy. • Epigastric pulsation. • Divarication of the recti muscles. • Umbilicus: site, discharge or nodules. • Hair distribution. • Hernial orifices. • Flanks.
Back Examination • for Deformities or renal angle tenderness • A- Palpation: • 1 - Superficial palpation: to detect any tenderness, rigidity or superficial masses. • 2 - Deep palpation: to palpate deep (intraperitoneal organs) e. g. liver, spleen or other masses. • 3 - Special obstetric palpation of the gravid uterus to know the presentation, position of the fetus and duration of pregnancy; by the following maneuvers
Fundal level: • -The examiner doctor stands on the right side of the pregnant lady, facing the maternal abdomen. • -The right hand is used to push the pregnant uterus centrally because most of the pregnant uteri ar tilted to the right side (dextro-rotation). • Then the ulnar border of the left hand is used to feel the funds of the uterus by sweeping the ulna border of the left hand till getting the resistance of the convex border of the fundus of the uterus (in midline). • The level of fundus demonstrates the duration of pregnancy. • If the fundus is felt at the upper border of symphysis pubis = 12 weeks. If the fundus is felt at the upper border of the umbilicus = 24 weeks.

Korotkoff Sounds Initial 'tapping' sound (cuff pressure). I : Systolic pressure Sounds increase in intensity. II sounds at maximum intensity. III Sounds become muffled : within 10. IV mm. Hg above the diastolic blood pressure Sounds disappear: Diastolic pressure. V
Why Korotkoff Phase IV Is No Longer Used? Korotkoff phase V is more reliable Use of Korotkoff phase V compared with that of phase IV has similar pregnancy outcome.
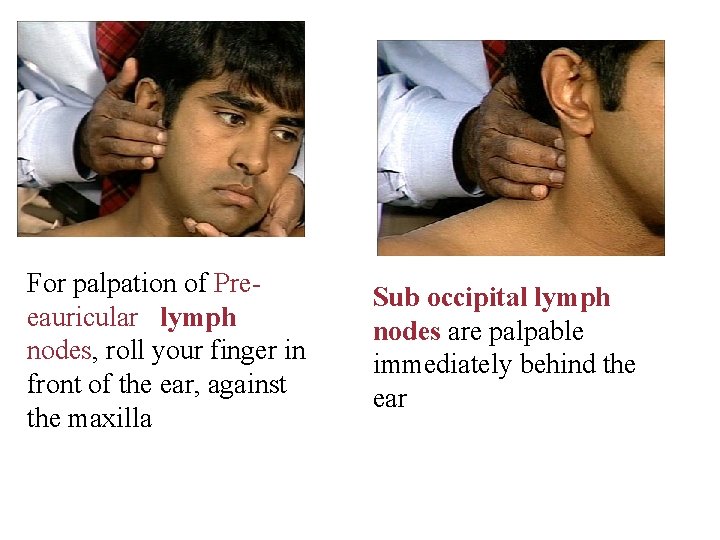
For palpation of Preeauricular lymph nodes, roll your finger in front of the ear, against the maxilla Sub occipital lymph nodes are palpable immediately behind the ear
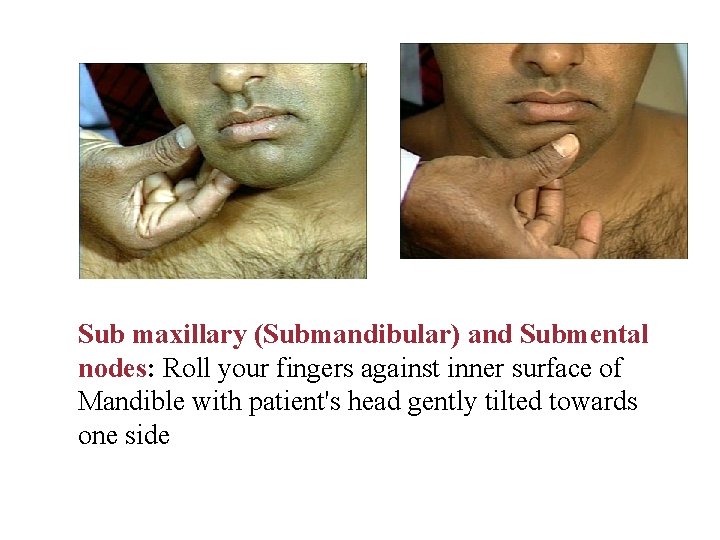
Sub maxillary (Submandibular) and Submental nodes: Roll your fingers against inner surface of Mandible with patient's head gently tilted towards one side

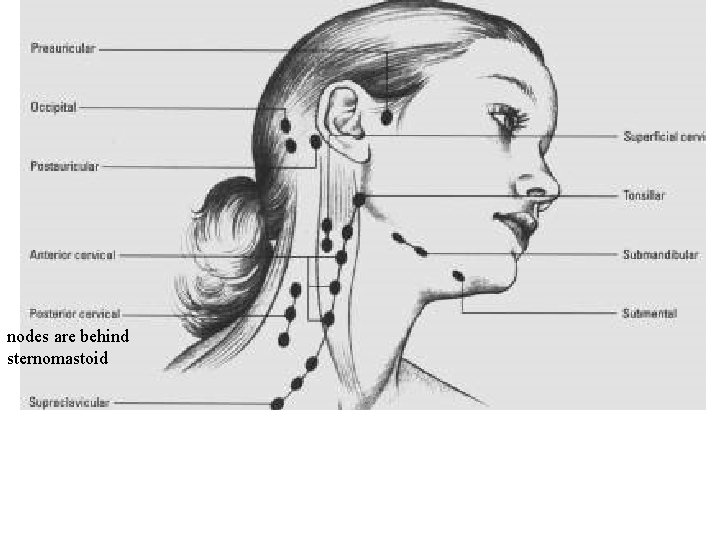
nodes are behind sternomastoid
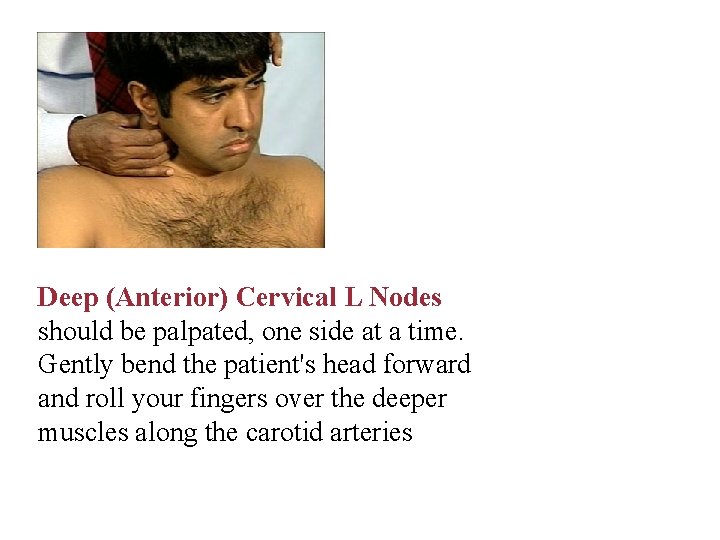
Deep (Anterior) Cervical L Nodes should be palpated, one side at a time. Gently bend the patient's head forward and roll your fingers over the deeper muscles along the carotid arteries
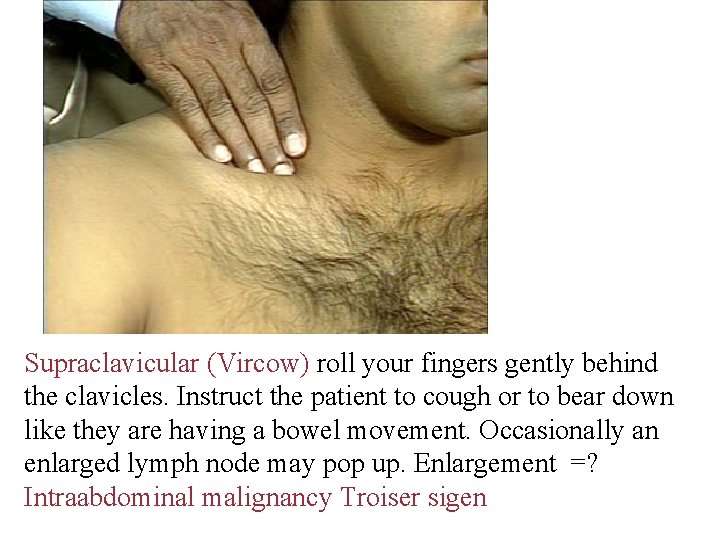
Supraclavicular (Vircow) roll your fingers gently behind the clavicles. Instruct the patient to cough or to bear down like they are having a bowel movement. Occasionally an enlarged lymph node may pop up. Enlargement =? Intraabdominal malignancy Troiser sigen
Abdominal (Obstetric): • Inspection • Palpation • Auscultation
Abdominal (Obstetric): Inspection: Contour and size of abdomen Signs of pregnancy § Breast ( Hyperpigmentation, Dilated veins) § Striae gravidarum § Linea Negra Scars from previous operations Fetal movements Hernial orifices and back

Melanocyte- stimulating placental hormone
Abdominal (Obstetric) (cont. ): Palpation: Tenderness , rigidity& papable organs Fundal Level (height) Fundal grip Umbilical grip 1 st & 2 nd Pelvic Grips
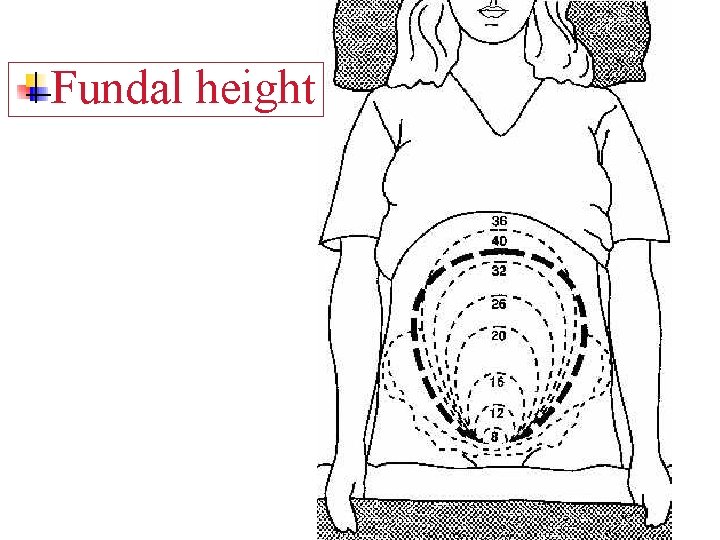
Fundal height
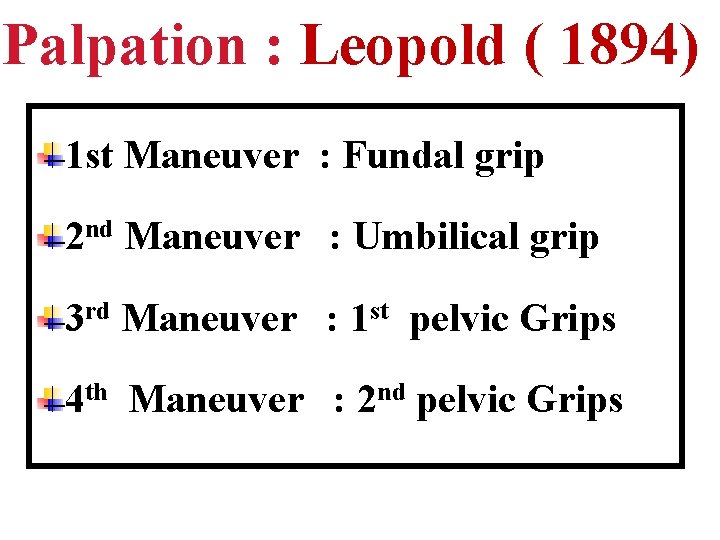
Palpation : Leopold ( 1894) 1 st Maneuver : Fundal grip 2 nd Maneuver : Umbilical grip 3 rd Maneuver : 1 st pelvic Grips 4 th Maneuver : 2 nd pelvic Grips
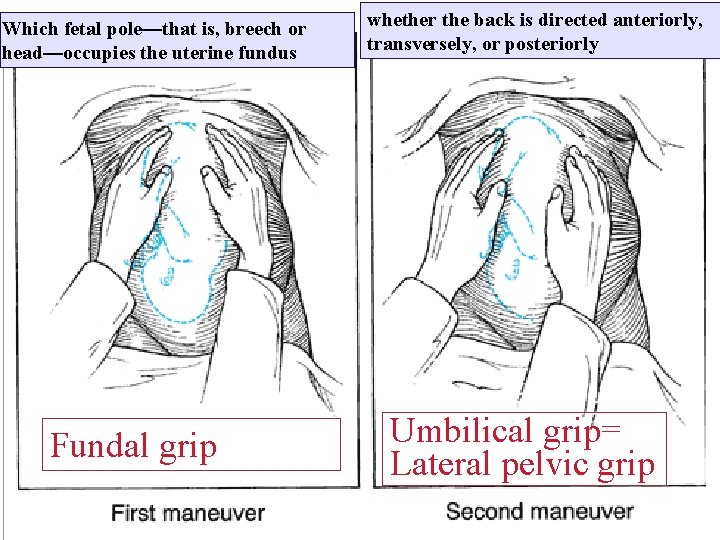
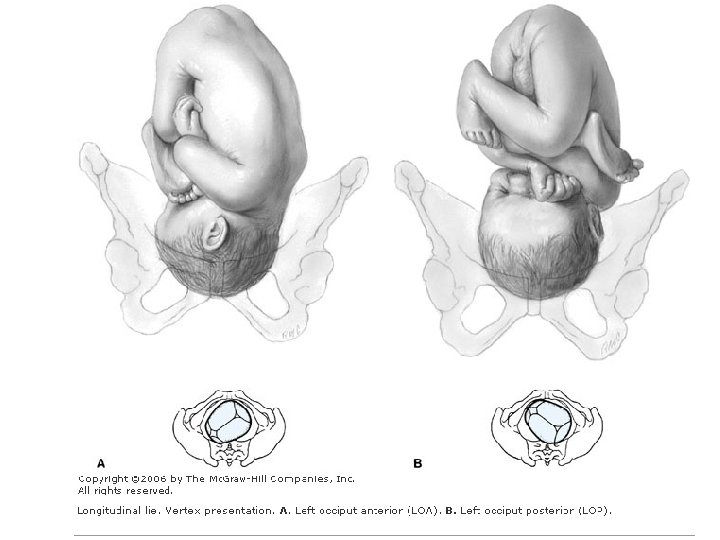
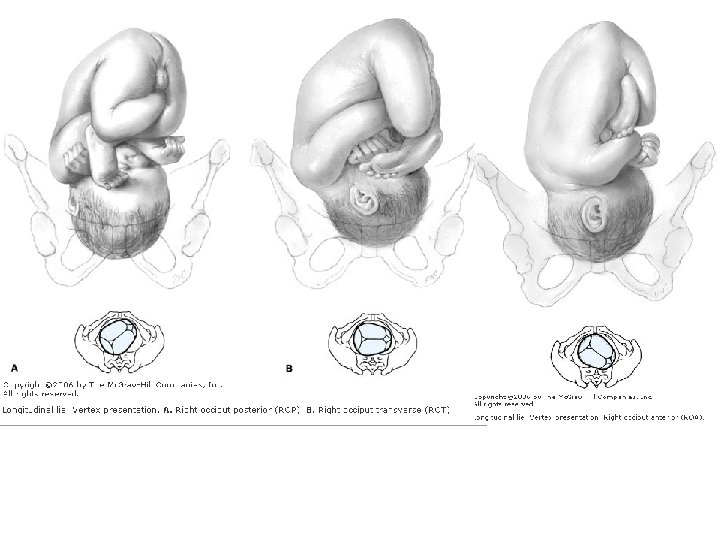
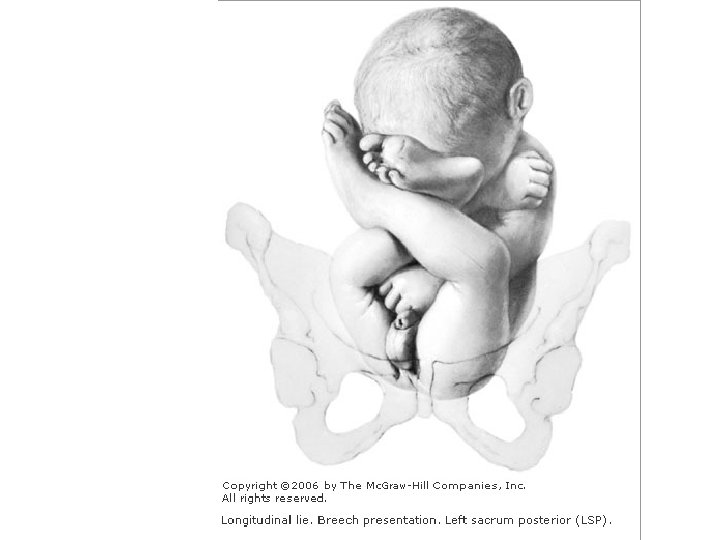
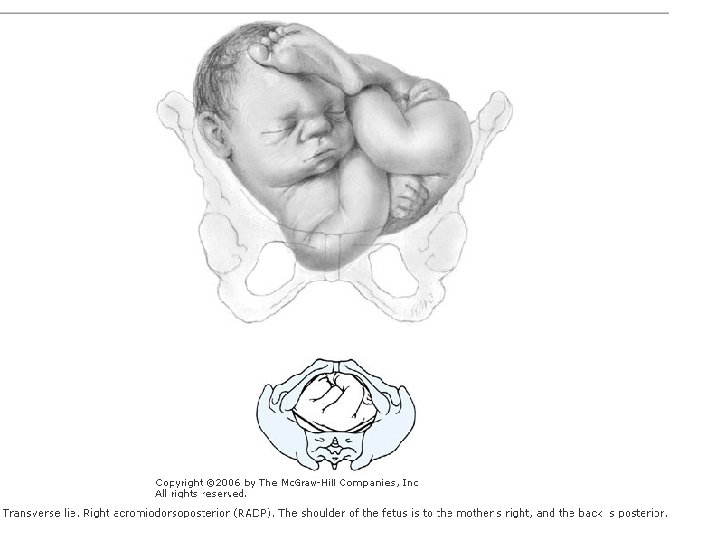
Which fetal pole—that is, breech or head—occupies the uterine fundus Fundal grip whether the back is directed anteriorly, transversely, or posteriorly Umbilical grip= Lateral pelvic grip
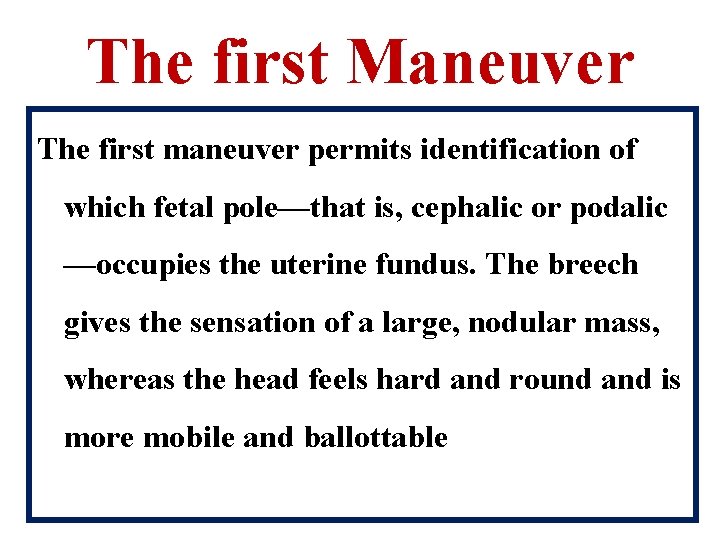
The first Maneuver The first maneuver permits identification of which fetal pole—that is, cephalic or podalic —occupies the uterine fundus. The breech gives the sensation of a large, nodular mass, whereas the head feels hard and round and is more mobile and ballottable
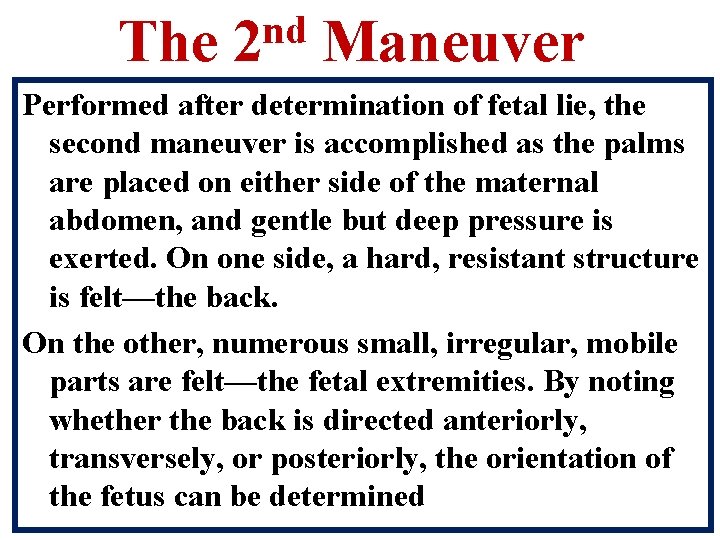
The nd 2 Maneuver Performed after determination of fetal lie, the second maneuver is accomplished as the palms are placed on either side of the maternal abdomen, and gentle but deep pressure is exerted. On one side, a hard, resistant structure is felt—the back. On the other, numerous small, irregular, mobile parts are felt—the fetal extremities. By noting whether the back is directed anteriorly, transversely, or posteriorly, the orientation of the fetus can be determined
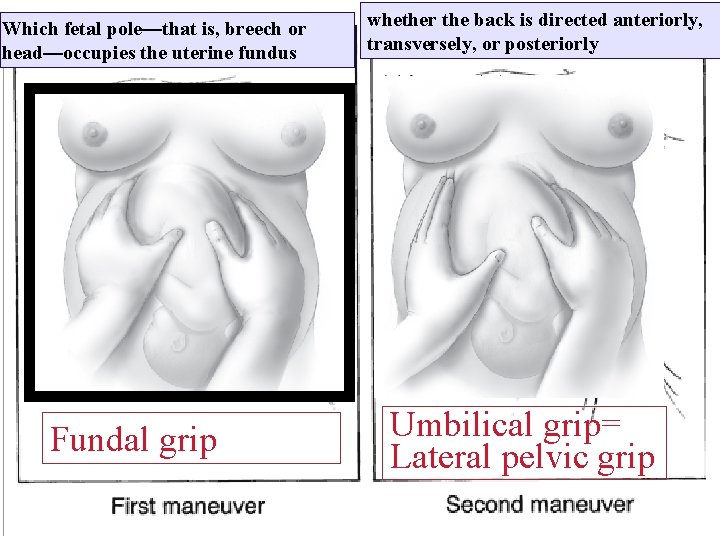
Which fetal pole—that is, breech or head—occupies the uterine fundus Fundal grip whether the back is directed anteriorly, transversely, or posteriorly Umbilical grip= Lateral pelvic grip
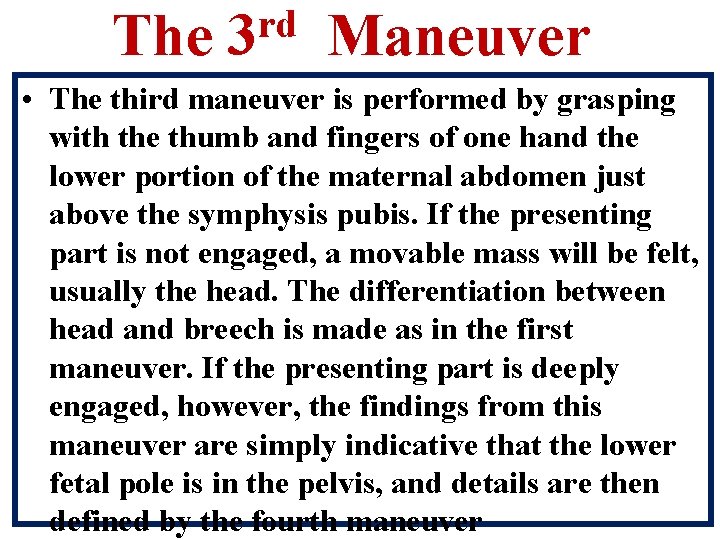
The rd 3 Maneuver • The third maneuver is performed by grasping with the thumb and fingers of one hand the lower portion of the maternal abdomen just above the symphysis pubis. If the presenting part is not engaged, a movable mass will be felt, usually the head. The differentiation between head and breech is made as in the first maneuver. If the presenting part is deeply engaged, however, the findings from this maneuver are simply indicative that the lower fetal pole is in the pelvis, and details are then defined by the fourth maneuver
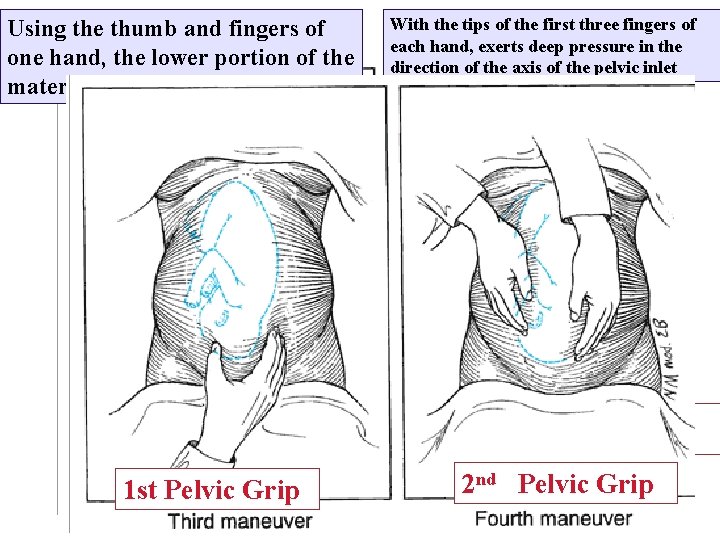
Using the thumb and fingers of one hand, the lower portion of the maternal abdomen is grasped just 1 st pelvic grip 1 st Pelvic Grip With the tips of the first three fingers of each hand, exerts deep pressure in the direction of the axis of the pelvic inlet 2 nd pelvic grip 2 nd Pelvic Grip
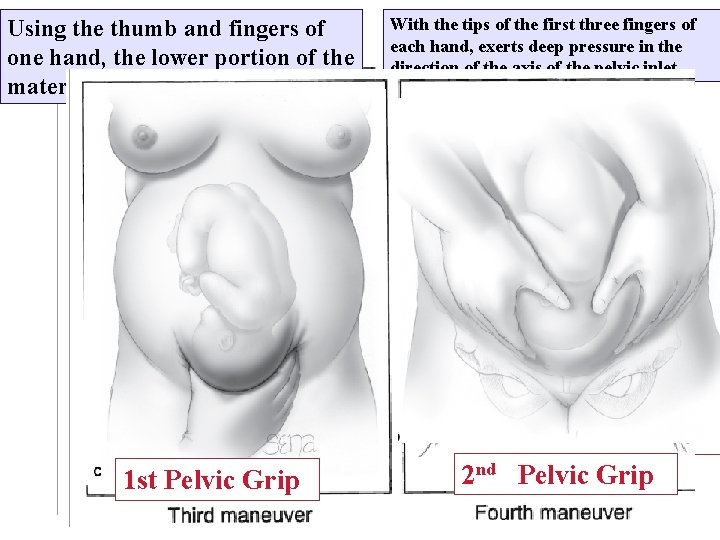
Using the thumb and fingers of one hand, the lower portion of the maternal abdomen is grasped just 1 st pelvic grip 1 st Pelvic Grip With the tips of the first three fingers of each hand, exerts deep pressure in the direction of the axis of the pelvic inlet 2 nd pelvic grip 2 nd Pelvic Grip
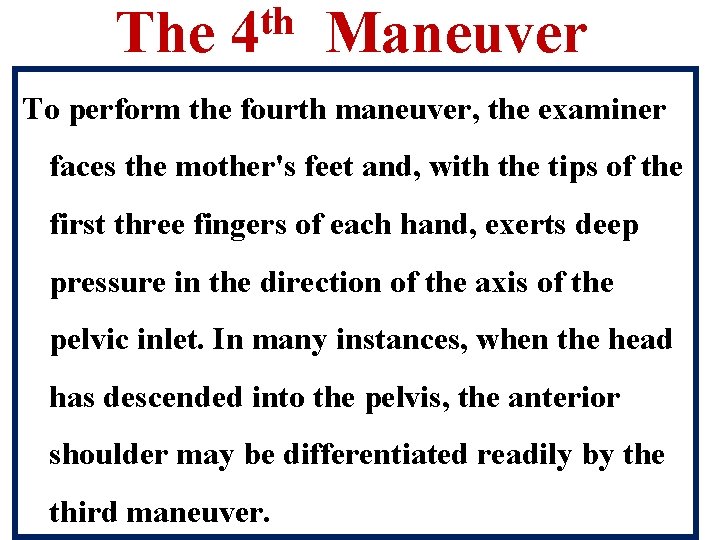
The th 4 Maneuver To perform the fourth maneuver, the examiner faces the mother's feet and, with the tips of the first three fingers of each hand, exerts deep pressure in the direction of the axis of the pelvic inlet. In many instances, when the head has descended into the pelvis, the anterior shoulder may be differentiated readily by the third maneuver.
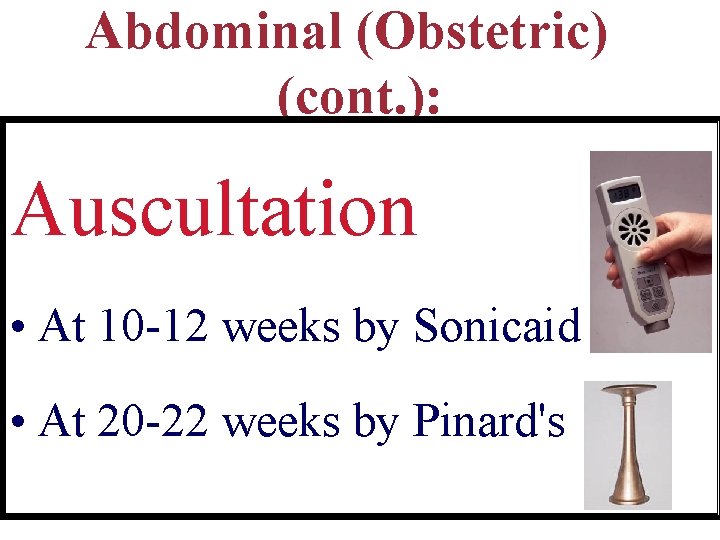
Abdominal (Obstetric) (cont. ): Auscultation • At 10 -12 weeks by Sonicaid • At 20 -22 weeks by Pinard's
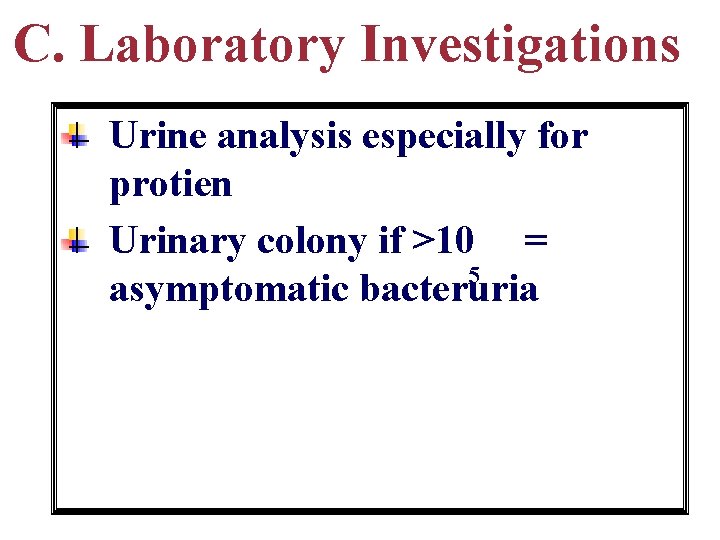
C. Laboratory Investigations Urine analysis especially for protien Urinary colony if >10 = 5 asymptomatic bacteruria
C. Laboratory Investigations Blood analysis Ø Complete blood count (CBC) Ø ABO groupings and RH typing Ø Blood Glucose Level Ø Hepatitis B antigen Ø Wasserman reaction Ø Rubella antibody
C. Laboratory Investigations Blood analysis Ø Complete blood count (CBC) Ø ABO groupings and RH typing Ø Blood Glucose Level Ø Hepatitis B antigen Ø Wasserman reaction Ø Rubella antibody
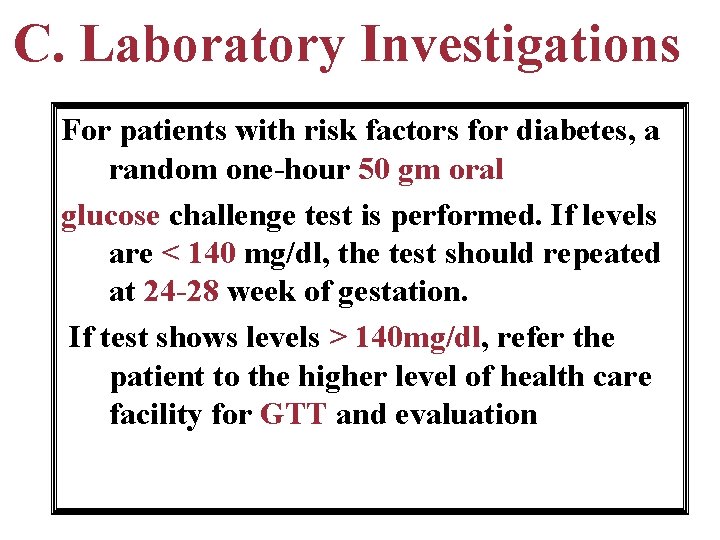
C. Laboratory Investigations For patients with risk factors for diabetes, a random one-hour 50 gm oral glucose challenge test is performed. If levels are < 140 mg/dl, the test should repeated at 24 -28 week of gestation. If test shows levels > 140 mg/dl, refer the patient to the higher level of health care facility for GTT and evaluation
C. Ultrasound (U/S) 1 -First trimester scan 2 -second trimester scan 3 -Third trimester scan 4 - When needed
C. Ultrasound (U/S) 1 -First trimester scan 2 -second trimester scan 3 -Third trimester scan 4 - When needed
C. Ultrasound (U/S) Pregnant women should be offered an early U/S scan to: 1 -Determine gestational age 2 -To detect multiple pregnancies. 3 -To ensure consistency of gestational age assessments 4 -To reduce the need for induction of labour after 41 weeks (10% versus 2%). It has a great value when the LMD is unreliable National Institute for. Clinical Excellence (NICE ) Guideline
At early pregnancy Gestational Sac Crown Rump Length
Diagnosis
Subsequent Antenatal Visits
Subsequent Antenatal Visits ØRecord any new complaints ØPerform examination at each visit ØInvestigation: Urine & Blood ØU/S ØAssessment of Fetal Weil-Being
Subsequent Antenatal Visits • Record any new complaints • Perform examination at each visit: • General: Blood pressure& LL • Abdominal: • Fundal level & Fetal lie • Fetal presentation& Fetal heart sound
Subsequent Antenatal Visits : cont. Request basic investigations v. Urine examination by dipstick for Protein , Glucose &Ketones v. Blood : Hb , screening for GD at 26 -28 week
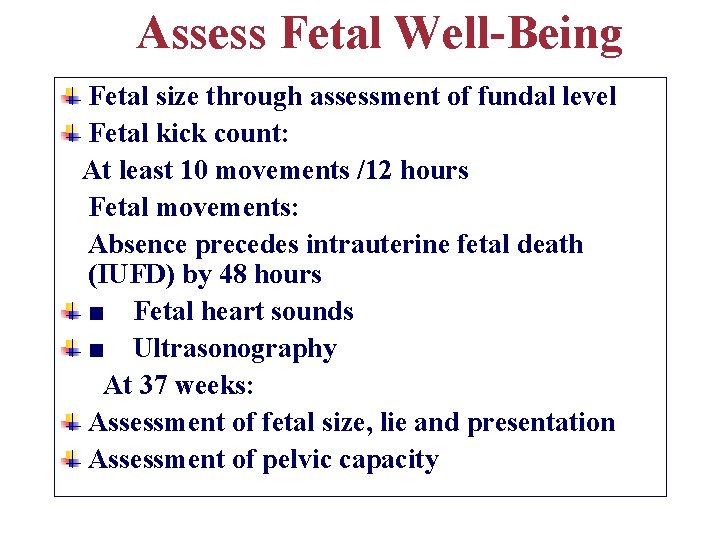
Assess Fetal Well-Being Fetal size through assessment of fundal level Fetal kick count: At least 10 movements /12 hours Fetal movements: Absence precedes intrauterine fetal death (IUFD) by 48 hours ■ Fetal heart sounds ■ Ultrasonography At 37 weeks: Assessment of fetal size, lie and presentation Assessment of pelvic capacity
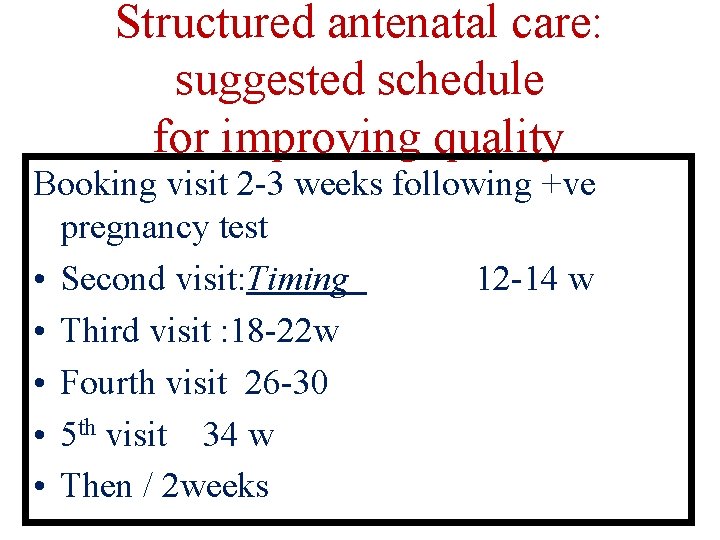
Structured antenatal care: suggested schedule for improving quality Booking visit 2 -3 weeks following +ve pregnancy test • Second visit: Timing 12 -14 w • Third visit : 18 -22 w • Fourth visit 26 -30 • 5 th visit 34 w • Then / 2 weeks
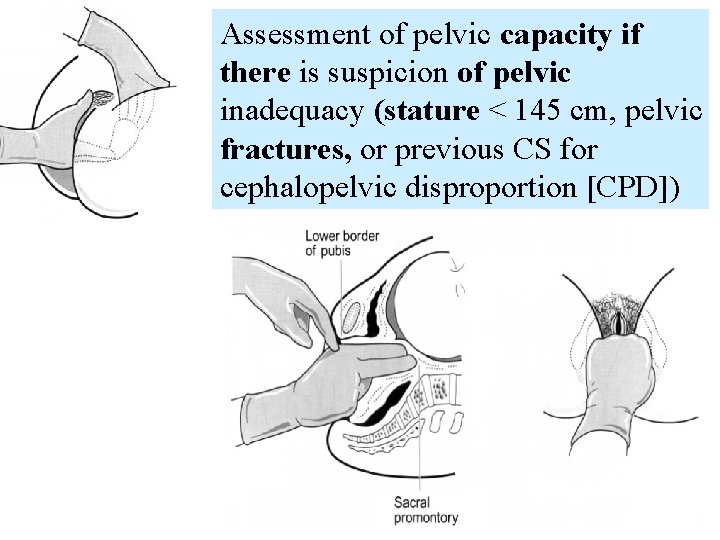
Assessment of pelvic capacity if there is suspicion of pelvic inadequacy (stature < 145 cm, pelvic fractures, or previous CS for cephalopelvic disproportion [CPD])
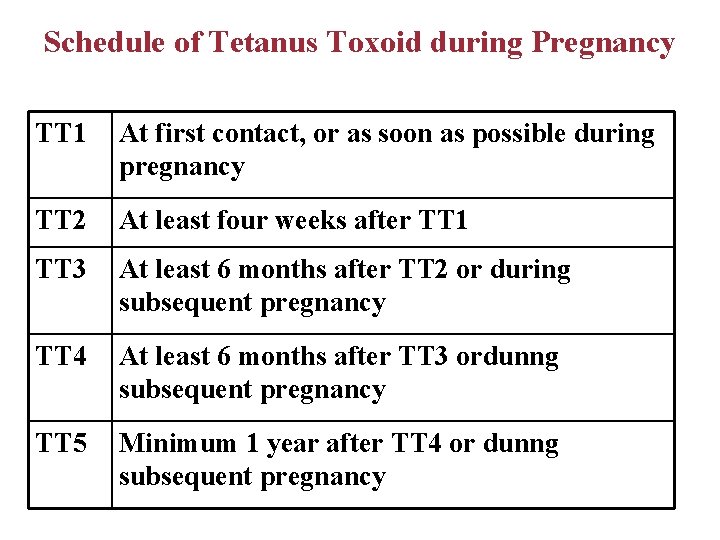
Schedule of Tetanus Toxoid during Pregnancy TT 1 At first contact, or as soon as possible during pregnancy TT 2 At least four weeks after TT 1 TT 3 At least 6 months after TT 2 or during subsequent pregnancy TT 4 At least 6 months after TT 3 ordunng subsequent pregnancy TT 5 Minimum 1 year after TT 4 or dunng subsequent pregnancy


Thank You
- Slides: 92