Oral Cavity Salivery Glands Head Neck Unit Lecture
- Slides: 21
Oral Cavity & Salivery Glands Head & Neck Unit – Lecture 10 ﺍﻷﻌﺴﻢ ﺟﻠﻴﻞ ﺣﻴﺪﺭ. ﺩ
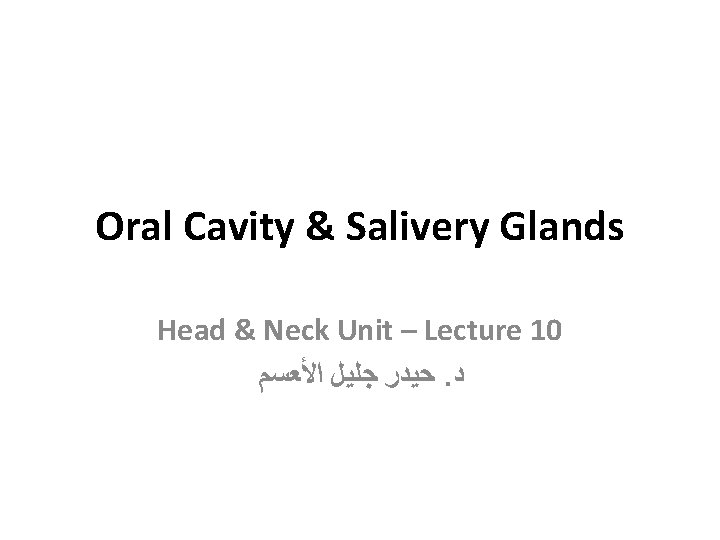
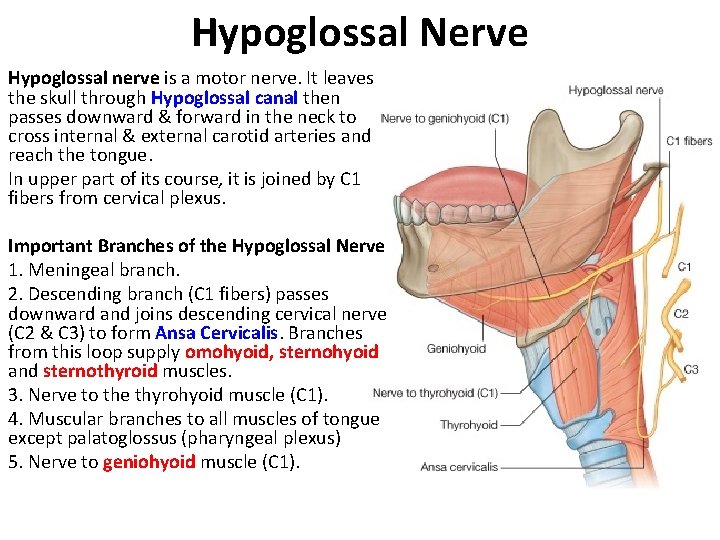
The Lips • They are two fleshy folds surrounding the oral orifice and covered on the outside by skin and lined on the inside by mucous membrane. • The substance of lips is made up by orbicularis oris and muscles that radiate from the lips into the face in addition to vessels and labial salivery gland. • Philtrum is shallow vertical groove seen in midline on outer surface of upper lip. • Labial frenulae are median folds of mucous membrane connecting inner surface of lips to gums.
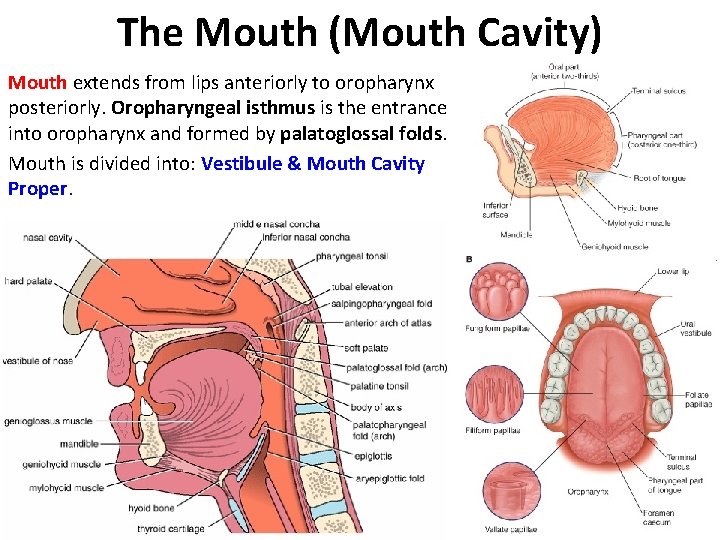
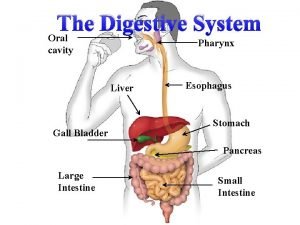
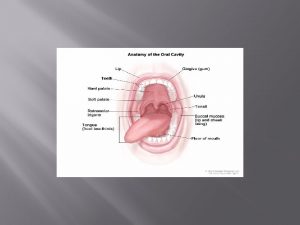
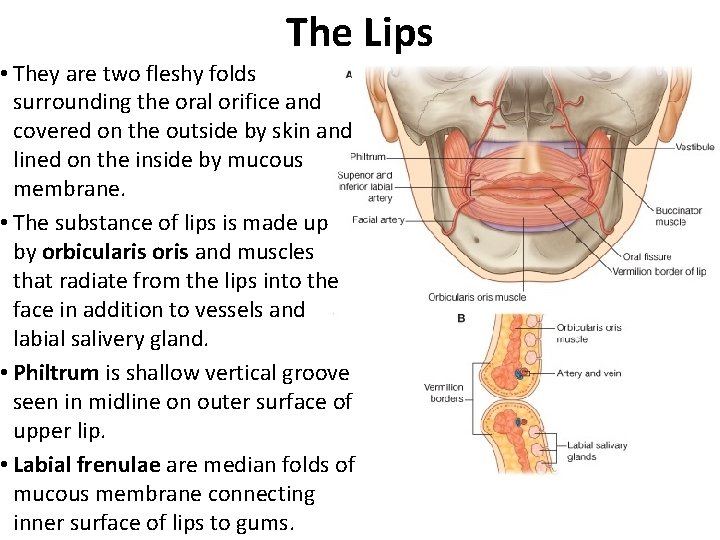
The Mouth (Mouth Cavity) Mouth extends from lips anteriorly to oropharynx posteriorly. Oropharyngeal isthmus is the entrance into oropharynx and formed by palatoglossal folds. Mouth is divided into: Vestibule & Mouth Cavity Proper. Vestibule: The vestibule is a slit like space that lies between lips and cheeks (externally) and gums and teeth (internally). It communicates with exterior through oral fissure & with mouth proper behind the third molar tooth on each side. The lateral walls of vestibule are formed by cheeks, which is made up by Buccinator. Parotid gland duct opens on a small papilla into the vestibule opposite upper 2 nd molar tooth.
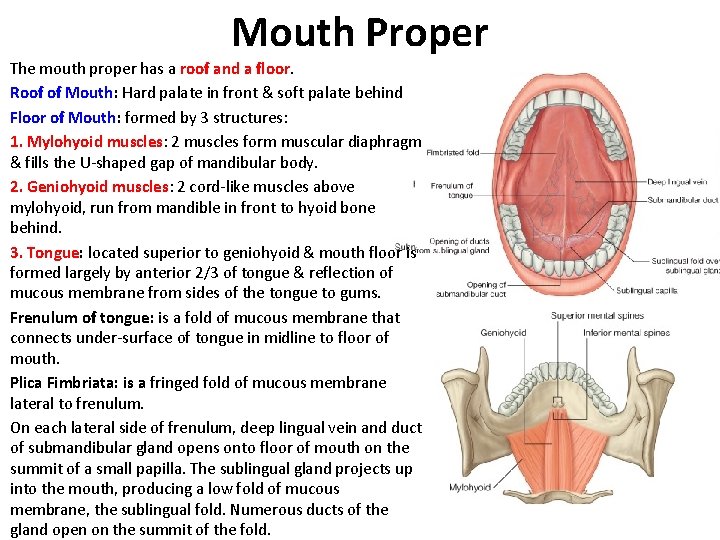
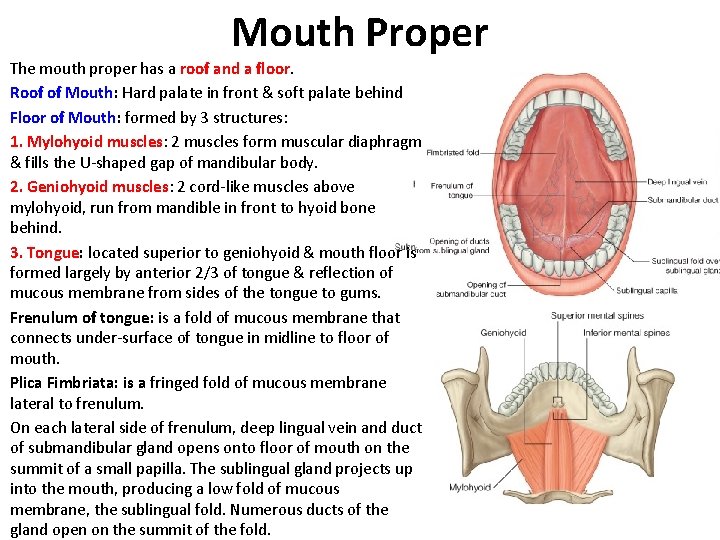
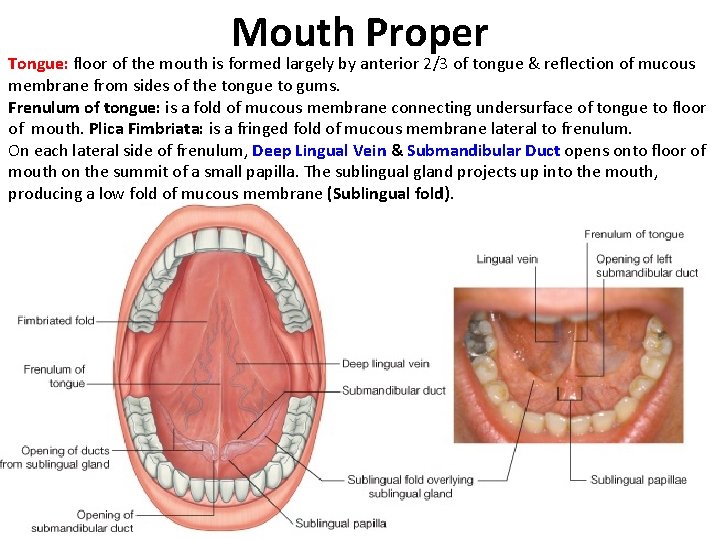
Mouth Proper The mouth proper has a roof and a floor. Roof of Mouth: Hard palate in front & soft palate behind Floor of Mouth: formed by 3 structures: 1. Mylohyoid muscles: 2 muscles form muscular diaphragm & fills the U-shaped gap of mandibular body. 2. Geniohyoid muscles: 2 cord-like muscles above mylohyoid, run from mandible in front to hyoid bone behind. 3. Tongue: located superior to geniohyoid & mouth floor is formed largely by anterior 2/3 of tongue & reflection of mucous membrane from sides of the tongue to gums. Frenulum of tongue: is a fold of mucous membrane that connects under-surface of tongue in midline to floor of mouth. Plica Fimbriata: is a fringed fold of mucous membrane lateral to frenulum. On each lateral side of frenulum, deep lingual vein and duct of submandibular gland opens onto floor of mouth on the summit of a small papilla. The sublingual gland projects up into the mouth, producing a low fold of mucous membrane, the sublingual fold. Numerous ducts of the gland open on the summit of the fold.
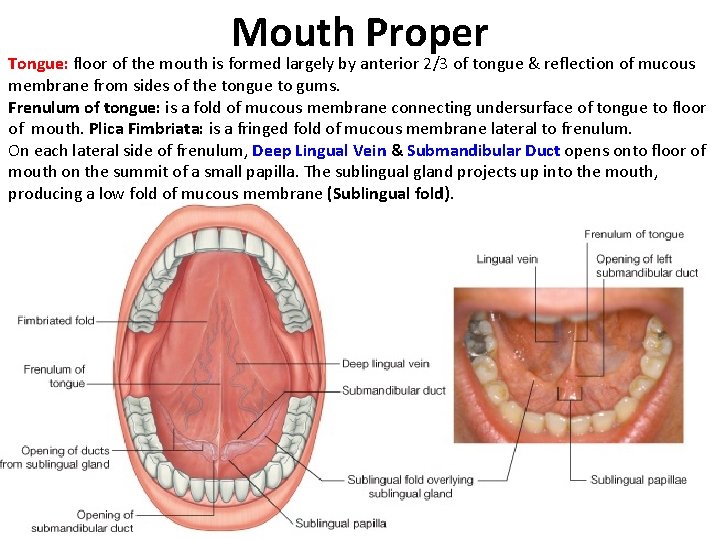
Mouth Proper Tongue: floor of the mouth is formed largely by anterior 2/3 of tongue & reflection of mucous membrane from sides of the tongue to gums. Frenulum of tongue: is a fold of mucous membrane connecting undersurface of tongue to floor of mouth. Plica Fimbriata: is a fringed fold of mucous membrane lateral to frenulum. On each lateral side of frenulum, Deep Lingual Vein & Submandibular Duct opens onto floor of mouth on the summit of a small papilla. The sublingual gland projects up into the mouth, producing a low fold of mucous membrane (Sublingual fold).
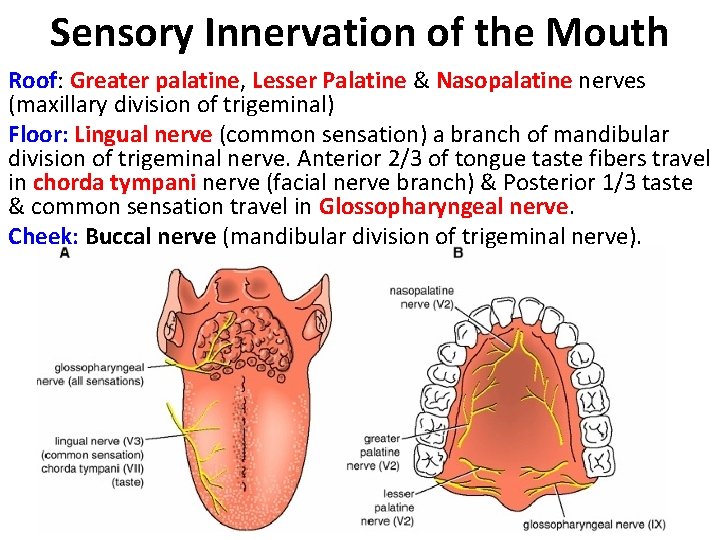
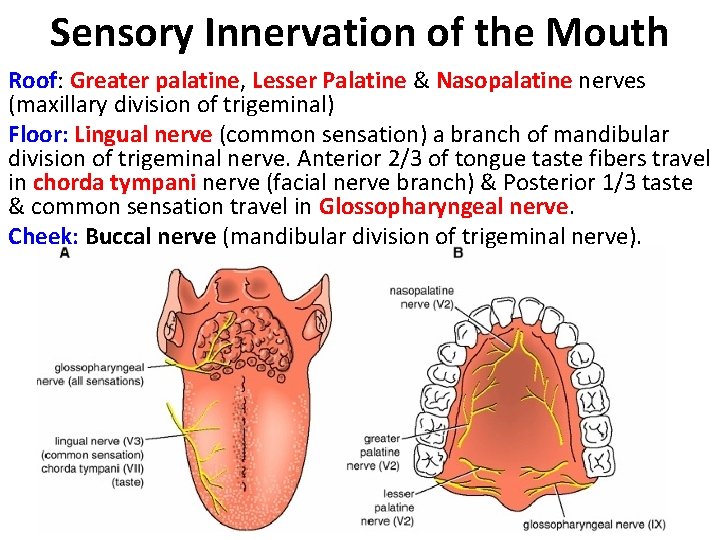
Sensory Innervation of the Mouth Roof: Greater palatine, Lesser Palatine & Nasopalatine nerves (maxillary division of trigeminal) Floor: Lingual nerve (common sensation) a branch of mandibular division of trigeminal nerve. Anterior 2/3 of tongue taste fibers travel in chorda tympani nerve (facial nerve branch) & Posterior 1/3 taste & common sensation travel in Glossopharyngeal nerve. Cheek: Buccal nerve (mandibular division of trigeminal nerve).
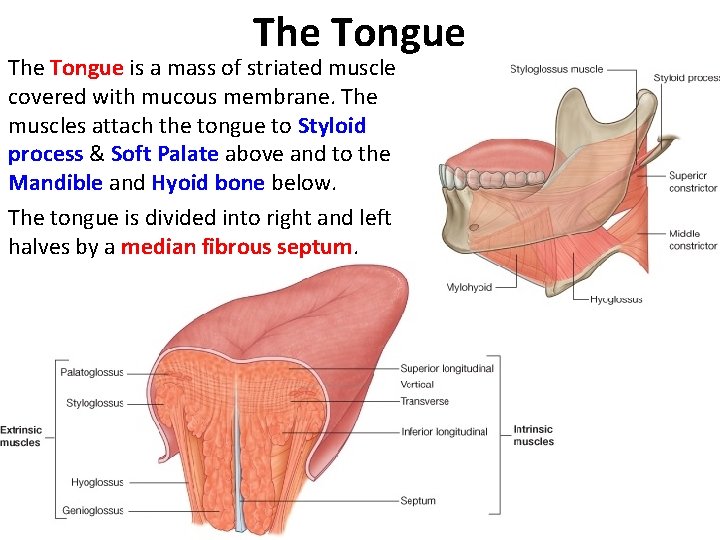
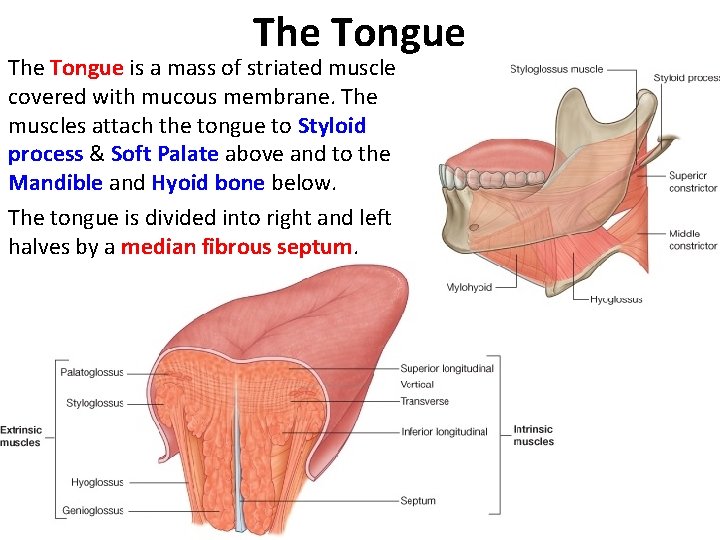
The Tongue is a mass of striated muscle covered with mucous membrane. The muscles attach the tongue to Styloid process & Soft Palate above and to the Mandible and Hyoid bone below. The tongue is divided into right and left halves by a median fibrous septum.
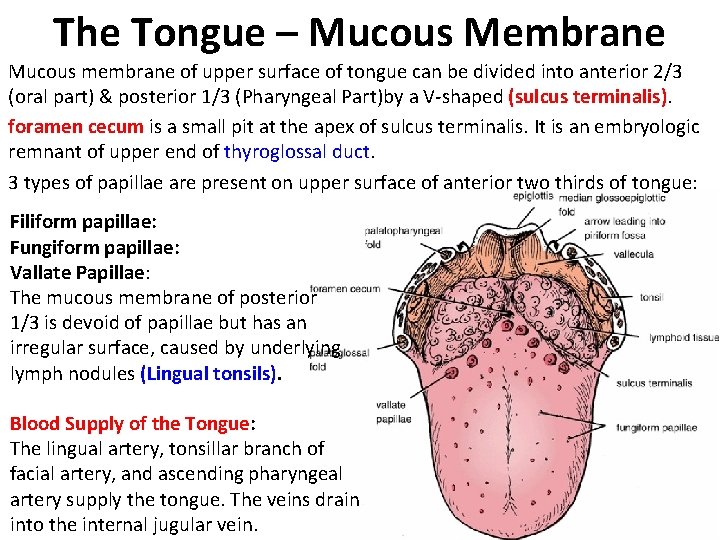
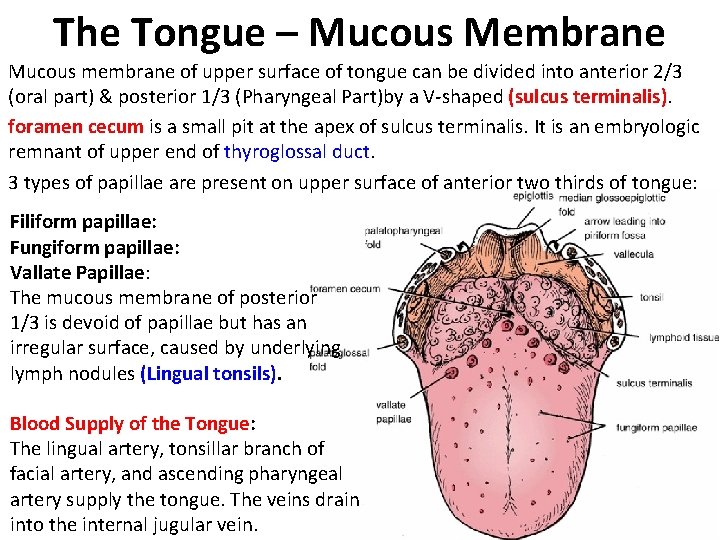
The Tongue – Mucous Membrane Mucous membrane of upper surface of tongue can be divided into anterior 2/3 (oral part) & posterior 1/3 (Pharyngeal Part)by a V-shaped (sulcus terminalis). foramen cecum is a small pit at the apex of sulcus terminalis. It is an embryologic remnant of upper end of thyroglossal duct. 3 types of papillae are present on upper surface of anterior two thirds of tongue: Filiform papillae: Fungiform papillae: Vallate Papillae: The mucous membrane of posterior 1/3 is devoid of papillae but has an irregular surface, caused by underlying lymph nodules (Lingual tonsils). Blood Supply of the Tongue: The lingual artery, tonsillar branch of facial artery, and ascending pharyngeal artery supply the tongue. The veins drain into the internal jugular vein.
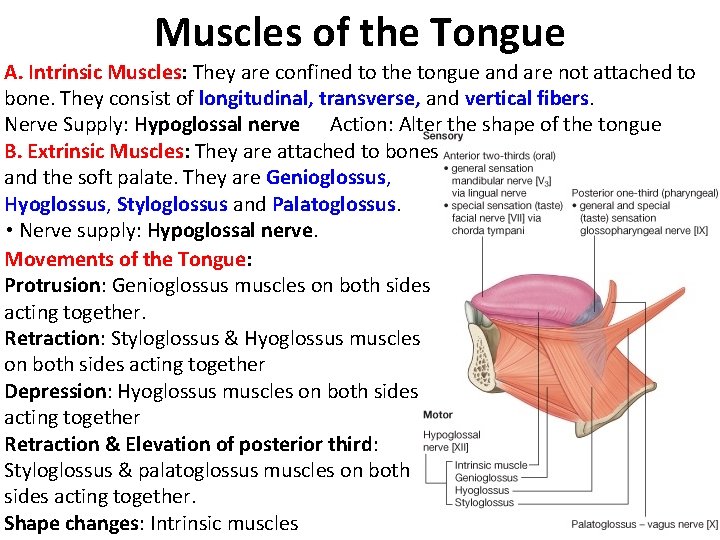
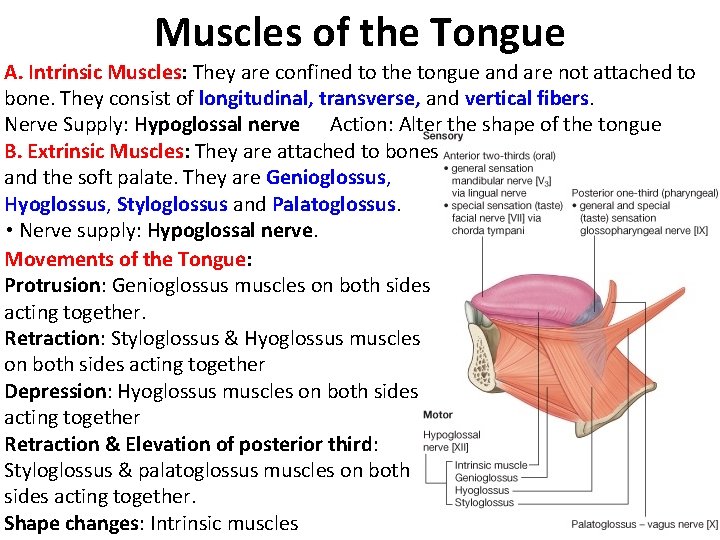
Muscles of the Tongue A. Intrinsic Muscles: They are confined to the tongue and are not attached to bone. They consist of longitudinal, transverse, and vertical fibers. Nerve Supply: Hypoglossal nerve Action: Alter the shape of the tongue B. Extrinsic Muscles: They are attached to bones and the soft palate. They are Genioglossus, Hyoglossus, Styloglossus and Palatoglossus. • Nerve supply: Hypoglossal nerve. Movements of the Tongue: Protrusion: Genioglossus muscles on both sides acting together. Retraction: Styloglossus & Hyoglossus muscles on both sides acting together Depression: Hyoglossus muscles on both sides acting together Retraction & Elevation of posterior third: Styloglossus & palatoglossus muscles on both sides acting together. Shape changes: Intrinsic muscles
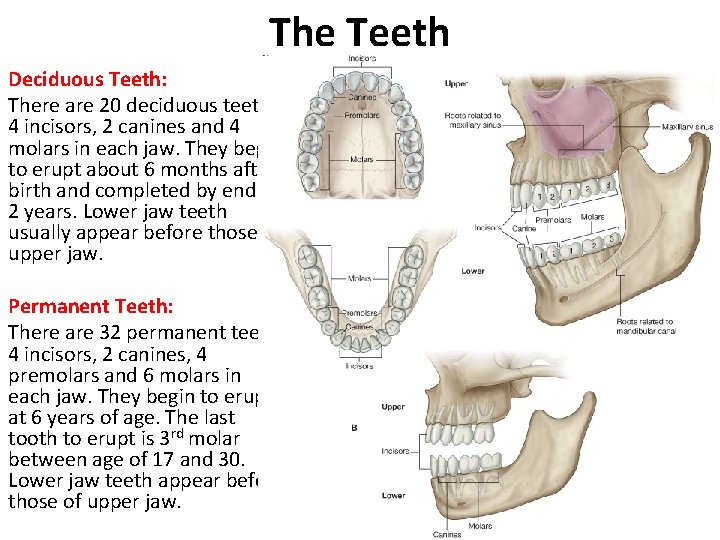
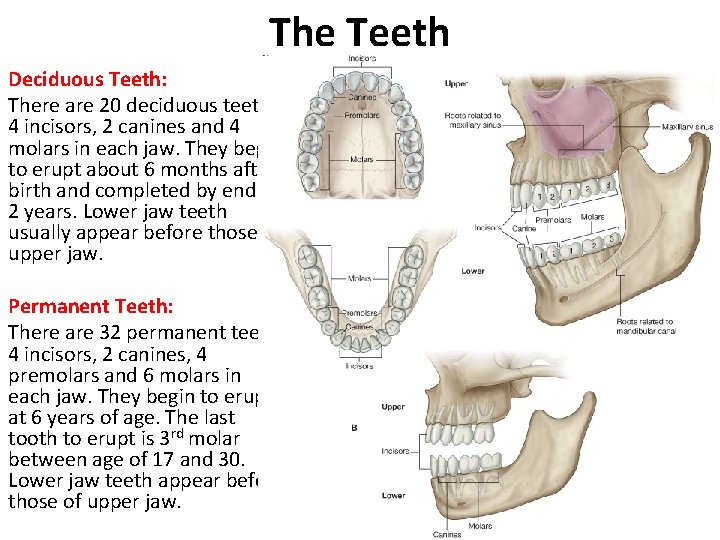
The Teeth Deciduous Teeth: There are 20 deciduous teeth: 4 incisors, 2 canines and 4 molars in each jaw. They begin to erupt about 6 months after birth and completed by end of 2 years. Lower jaw teeth usually appear before those of upper jaw. Permanent Teeth: There are 32 permanent teeth: 4 incisors, 2 canines, 4 premolars and 6 molars in each jaw. They begin to erupt at 6 years of age. The last tooth to erupt is 3 rd molar between age of 17 and 30. Lower jaw teeth appear before those of upper jaw.
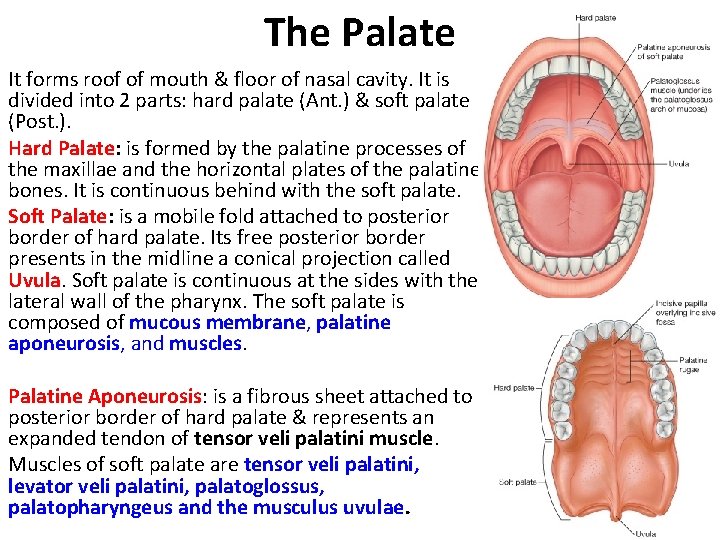
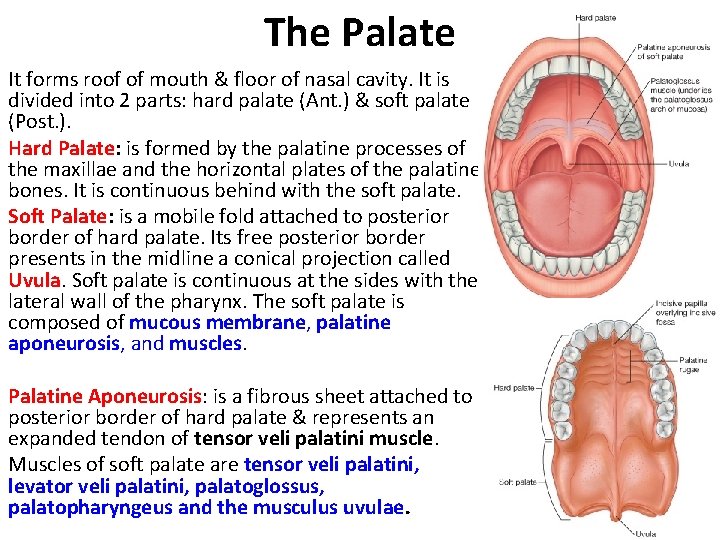
The Palate It forms roof of mouth & floor of nasal cavity. It is divided into 2 parts: hard palate (Ant. ) & soft palate (Post. ). Hard Palate: is formed by the palatine processes of the maxillae and the horizontal plates of the palatine bones. It is continuous behind with the soft palate. Soft Palate: is a mobile fold attached to posterior border of hard palate. Its free posterior border presents in the midline a conical projection called Uvula. Soft palate is continuous at the sides with the lateral wall of the pharynx. The soft palate is composed of mucous membrane, palatine aponeurosis, and muscles. Palatine Aponeurosis: is a fibrous sheet attached to posterior border of hard palate & represents an expanded tendon of tensor veli palatini muscle. Muscles of soft palate are tensor veli palatini, levator veli palatini, palatoglossus, palatopharyngeus and the musculus uvulae.
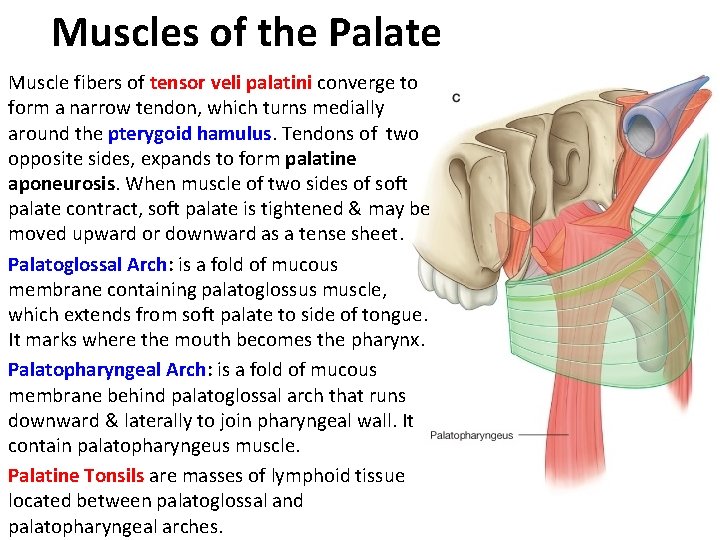
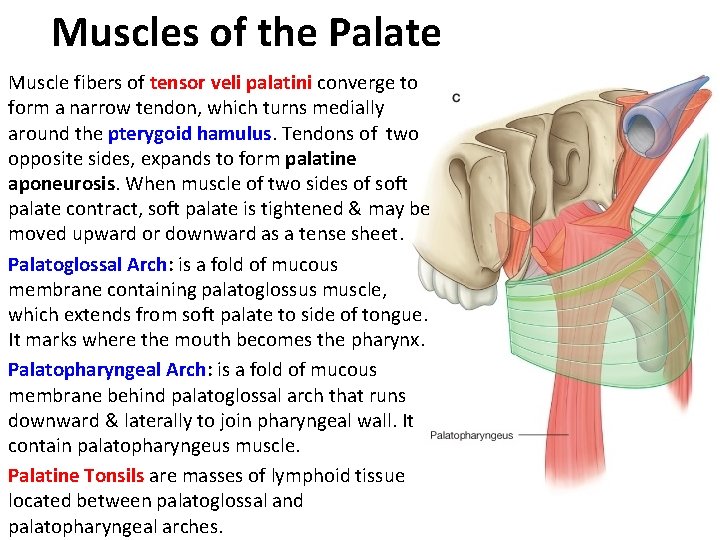
Muscles of the Palate Muscle fibers of tensor veli palatini converge to form a narrow tendon, which turns medially around the pterygoid hamulus. Tendons of two opposite sides, expands to form palatine aponeurosis. When muscle of two sides of soft palate contract, soft palate is tightened & may be moved upward or downward as a tense sheet. Palatoglossal Arch: is a fold of mucous membrane containing palatoglossus muscle, which extends from soft palate to side of tongue. It marks where the mouth becomes the pharynx. Palatopharyngeal Arch: is a fold of mucous membrane behind palatoglossal arch that runs downward & laterally to join pharyngeal wall. It contain palatopharyngeus muscle. Palatine Tonsils are masses of lymphoid tissue located between palatoglossal and palatopharyngeal arches.
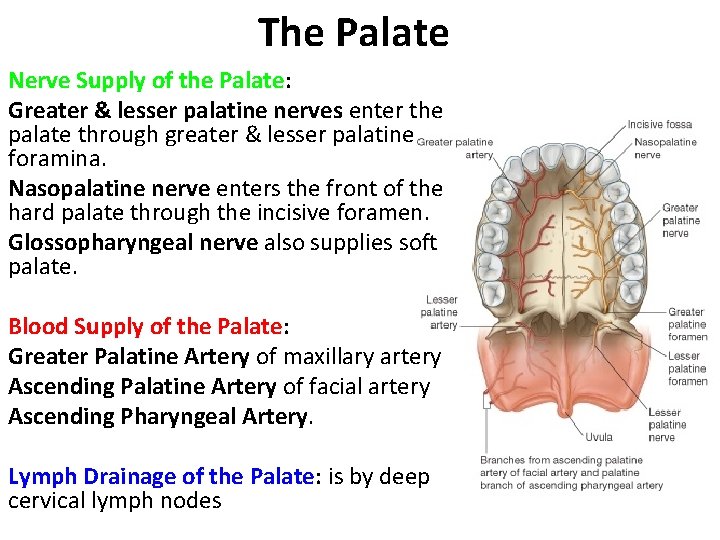
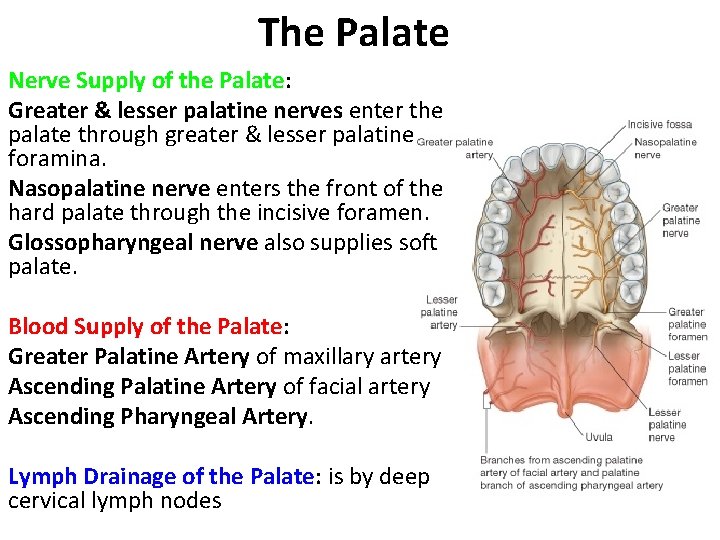
The Palate Nerve Supply of the Palate: Greater & lesser palatine nerves enter the palate through greater & lesser palatine foramina. Nasopalatine nerve enters the front of the hard palate through the incisive foramen. Glossopharyngeal nerve also supplies soft palate. Blood Supply of the Palate: Greater Palatine Artery of maxillary artery Ascending Palatine Artery of facial artery Ascending Pharyngeal Artery. Lymph Drainage of the Palate: is by deep cervical lymph nodes
The Salivary Glands
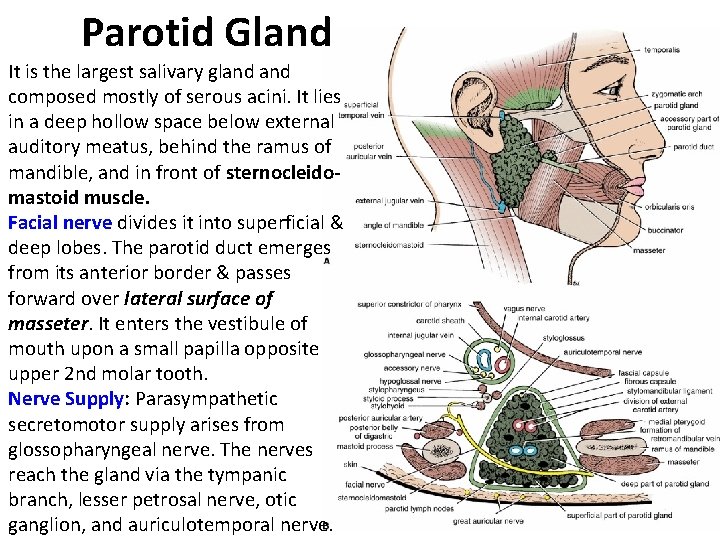
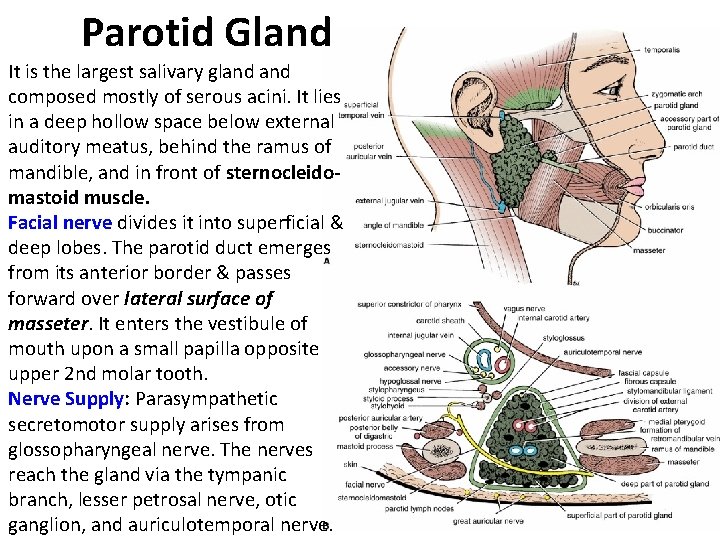
Parotid Gland It is the largest salivary gland composed mostly of serous acini. It lies in a deep hollow space below external auditory meatus, behind the ramus of mandible, and in front of sternocleidomastoid muscle. Facial nerve divides it into superficial & deep lobes. The parotid duct emerges from its anterior border & passes forward over lateral surface of masseter. It enters the vestibule of mouth upon a small papilla opposite upper 2 nd molar tooth. Nerve Supply: Parasympathetic secretomotor supply arises from glossopharyngeal nerve. The nerves reach the gland via the tympanic branch, lesser petrosal nerve, otic ganglion, and auriculotemporal nerve.
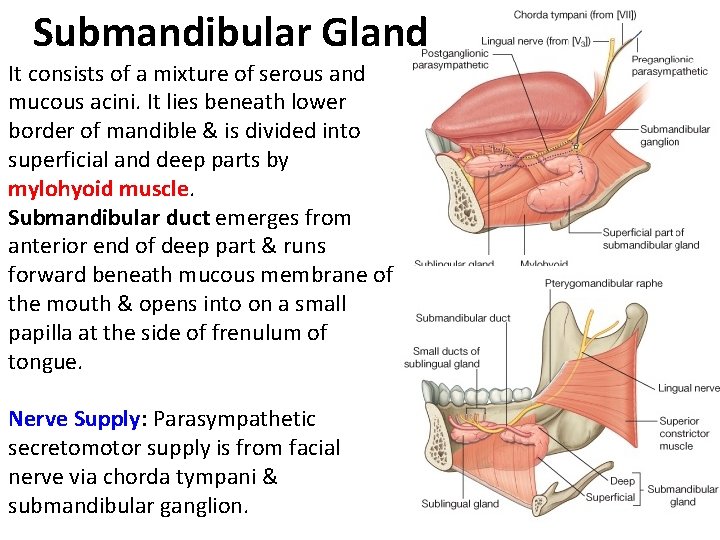
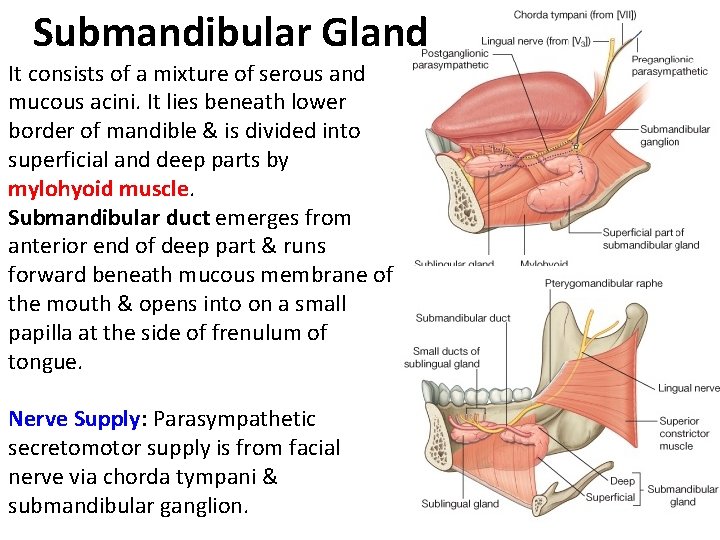
Submandibular Gland It consists of a mixture of serous and mucous acini. It lies beneath lower border of mandible & is divided into superficial and deep parts by mylohyoid muscle. Submandibular duct emerges from anterior end of deep part & runs forward beneath mucous membrane of the mouth & opens into on a small papilla at the side of frenulum of tongue. Nerve Supply: Parasympathetic secretomotor supply is from facial nerve via chorda tympani & submandibular ganglion.
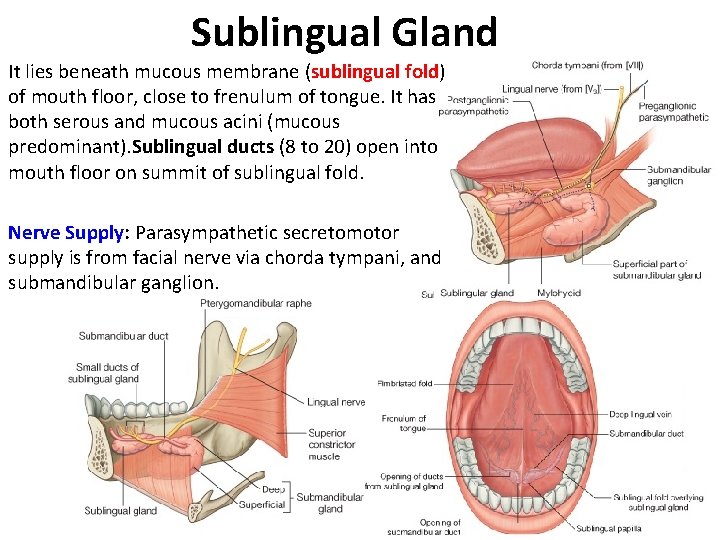
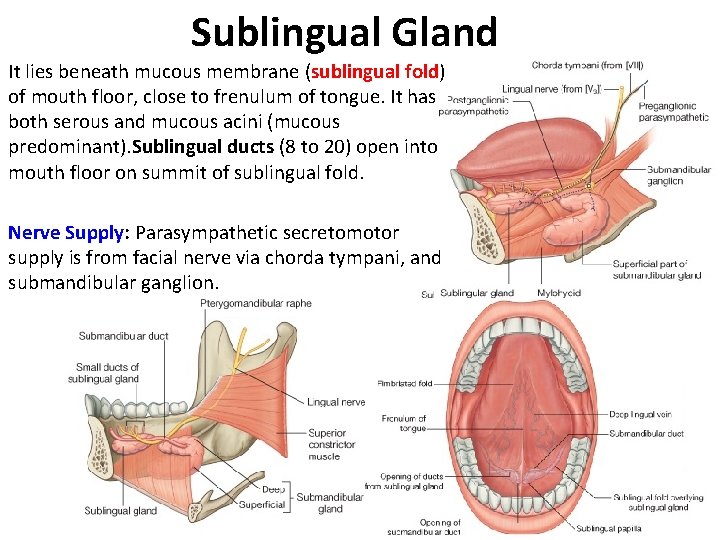
Sublingual Gland It lies beneath mucous membrane (sublingual fold) of mouth floor, close to frenulum of tongue. It has both serous and mucous acini (mucous predominant). Sublingual ducts (8 to 20) open into mouth floor on summit of sublingual fold. Nerve Supply: Parasympathetic secretomotor supply is from facial nerve via chorda tympani, and submandibular ganglion.
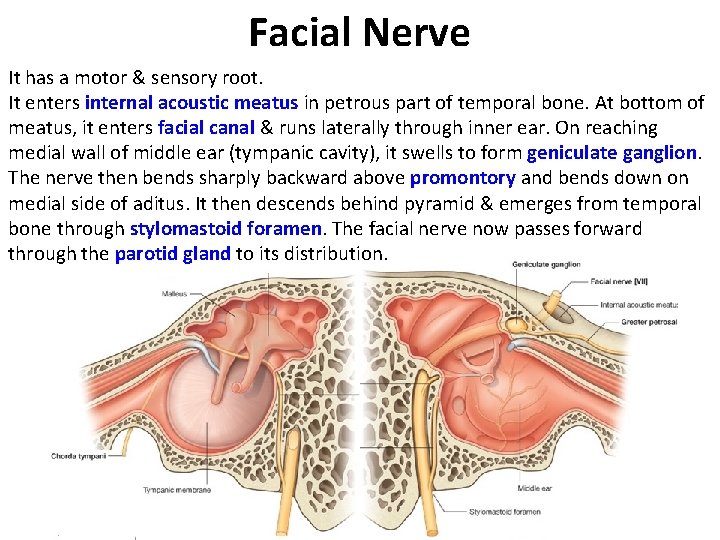
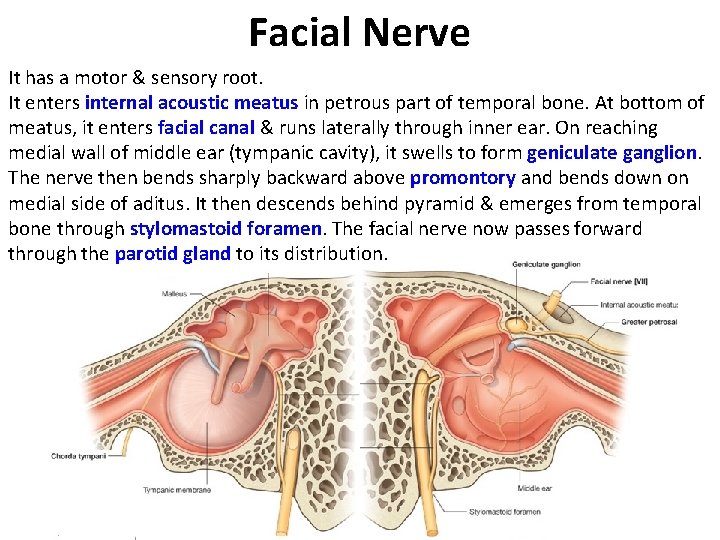
Facial Nerve It has a motor & sensory root. It enters internal acoustic meatus in petrous part of temporal bone. At bottom of meatus, it enters facial canal & runs laterally through inner ear. On reaching medial wall of middle ear (tympanic cavity), it swells to form geniculate ganglion. The nerve then bends sharply backward above promontory and bends down on medial side of aditus. It then descends behind pyramid & emerges from temporal bone through stylomastoid foramen. The facial nerve now passes forward through the parotid gland to its distribution.
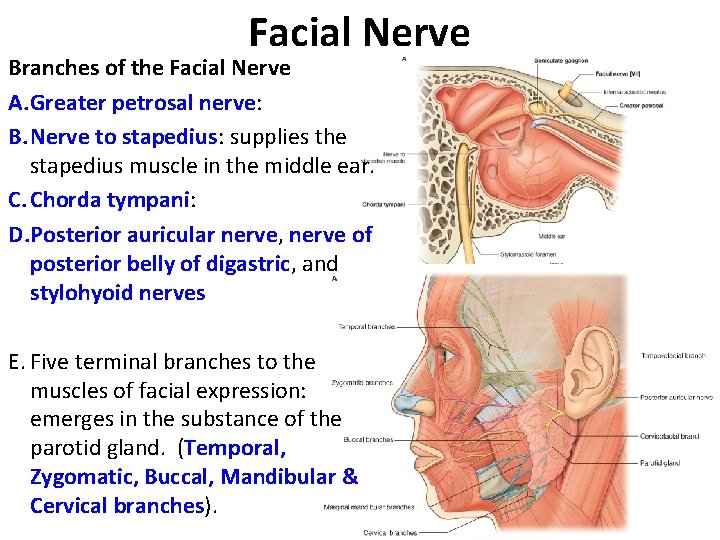
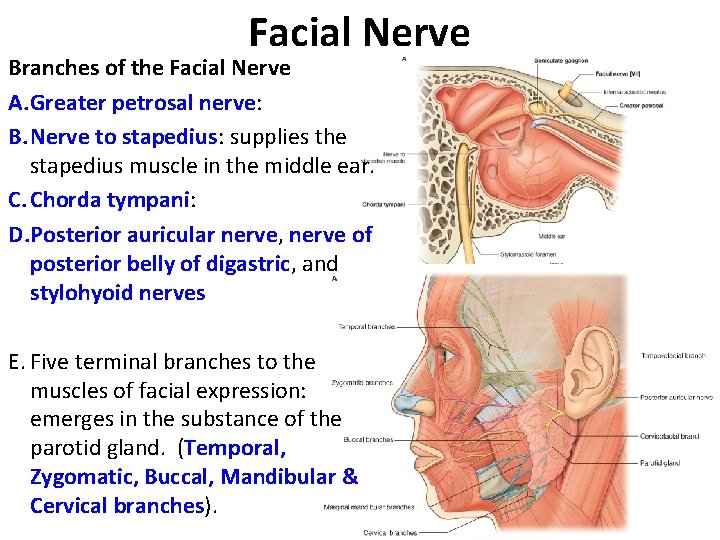
Facial Nerve Branches of the Facial Nerve A. Greater petrosal nerve: B. Nerve to stapedius: supplies the stapedius muscle in the middle ear. C. Chorda tympani: D. Posterior auricular nerve, nerve of posterior belly of digastric, and stylohyoid nerves E. Five terminal branches to the muscles of facial expression: emerges in the substance of the parotid gland. (Temporal, Zygomatic, Buccal, Mandibular & Cervical branches).
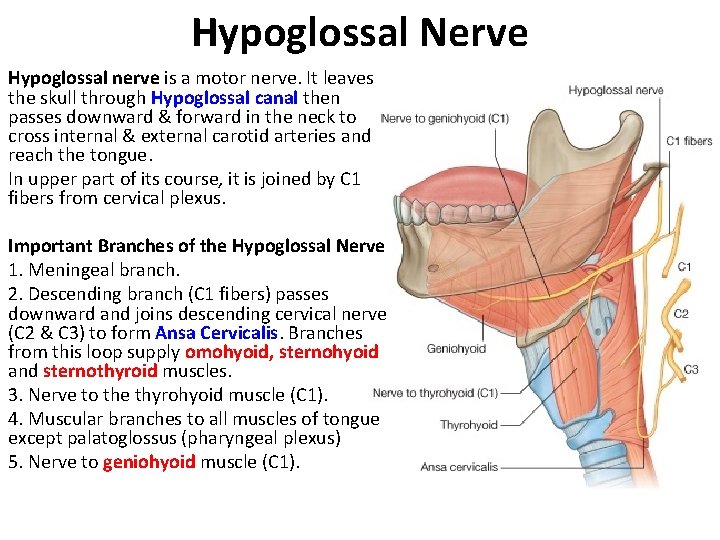
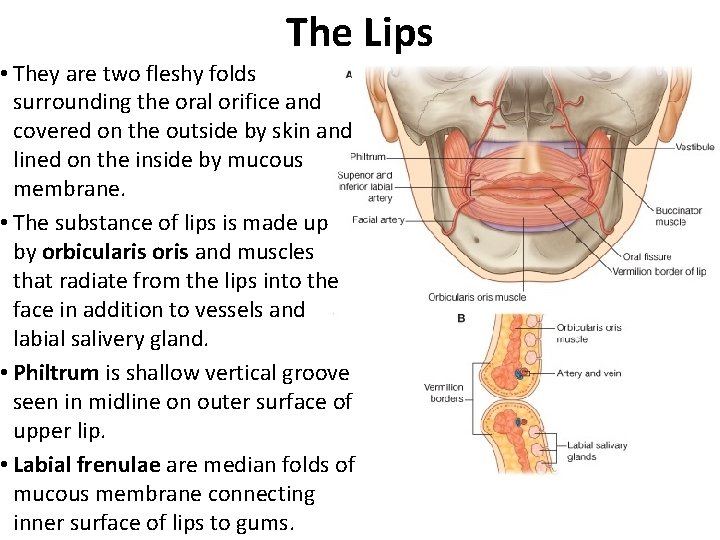
Hypoglossal Nerve Hypoglossal nerve is a motor nerve. It leaves the skull through Hypoglossal canal then passes downward & forward in the neck to cross internal & external carotid arteries and reach the tongue. In upper part of its course, it is joined by C 1 fibers from cervical plexus. Important Branches of the Hypoglossal Nerve 1. Meningeal branch. 2. Descending branch (C 1 fibers) passes downward and joins descending cervical nerve (C 2 & C 3) to form Ansa Cervicalis. Branches from this loop supply omohyoid, sternohyoid and sternothyroid muscles. 3. Nerve to the thyrohyoid muscle (C 1). 4. Muscular branches to all muscles of tongue except palatoglossus (pharyngeal plexus) 5. Nerve to geniohyoid muscle (C 1).
End of the Lecture GOOD LUCK
 Thoracic membranes
Thoracic membranes Floor of mouth anatomy
Floor of mouth anatomy Gianuzzi demilune
Gianuzzi demilune Eccomyosis
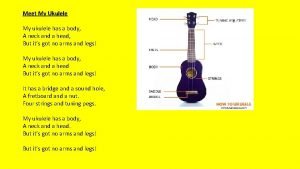
Eccomyosis There once was a man from tennessee ukulele
There once was a man from tennessee ukulele Tnm 8 head and neck
Tnm 8 head and neck Risk factors of head and neck cancer
Risk factors of head and neck cancer Thumb brush strum
Thumb brush strum Muscular system head and neck
Muscular system head and neck Zygomaticus
Zygomaticus Regional write up head face and neck
Regional write up head face and neck What has a neck but no head
What has a neck but no head Body planes directions and cavities worksheet
Body planes directions and cavities worksheet Mental anatomical term
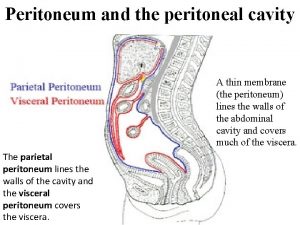
Mental anatomical term What are intraperitoneal organs
What are intraperitoneal organs Greater omentum and lesser omentum
Greater omentum and lesser omentum High-arched palate
High-arched palate Pyloric orifice function
Pyloric orifice function Landmark of the face
Landmark of the face White appearance
White appearance Function of duodenum
Function of duodenum Fovea palatina
Fovea palatina