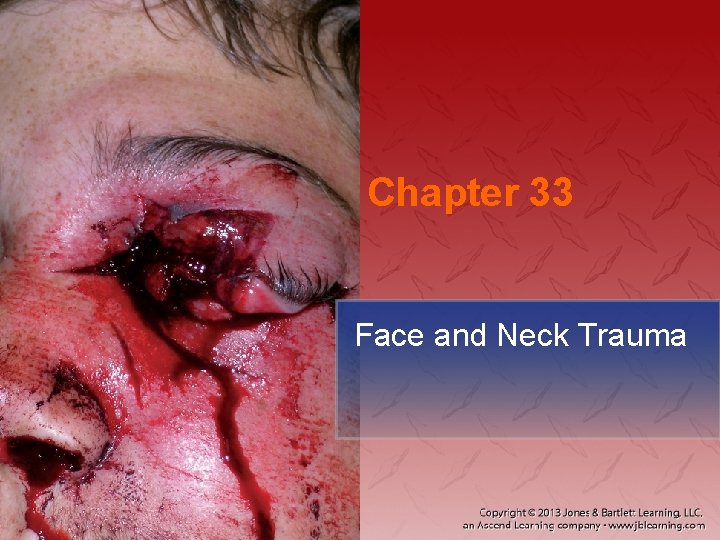
Chapter 33 Face and Neck Trauma National EMS




























- Slides: 110
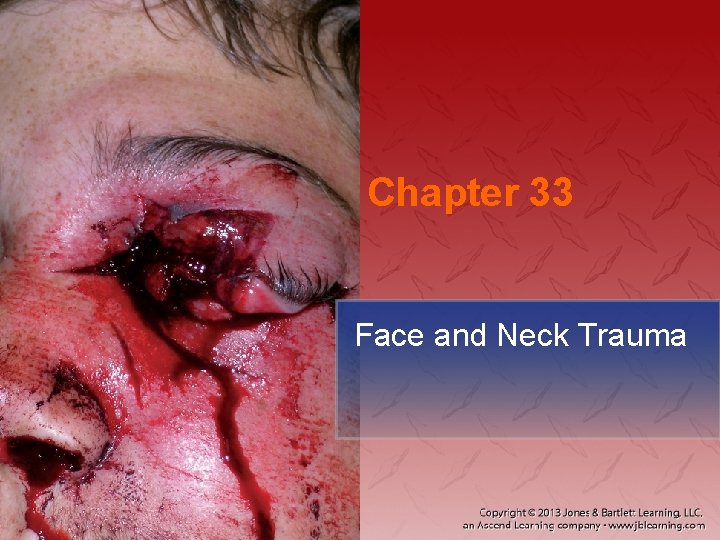
Chapter 33 Face and Neck Trauma

National EMS Education Standard Competencies Trauma Integrates assessment findings with principles of epidemiology and pathophysiology to formulate a field impression to implement a comprehensive treatment/disposition plan for an acutely injured patient.
National EMS Education Standard Competencies Head, Facial, Neck, and Spine Trauma Recognition and management of • Life threats • Spine trauma
National EMS Education Standard Competencies Head, Facial, Neck, and Spine Trauma Pathophysiology, assessment, and management of − Penetrating neck trauma − Laryngotracheal injuries − Spine trauma • Dislocations/subluxations • Fractures • Sprains/strains
National EMS Education Standard Competencies Head, Facial, Neck, and Spine Trauma Pathophysiology, assessment, and management of − − Facial fractures Skull fractures Foreign bodies in the eyes Dental trauma
National EMS Education Standard Competencies Head, Facial, Neck, and Spine Trauma Pathophysiology, assessment, and management of − − Unstable facial fractures Orbital fractures Perforated tympanic membrane Mandibular fractures
Introduction • You will commonly encounter patients with injuries to the face and neck. − These injuries can be some of the most graphic you will see.
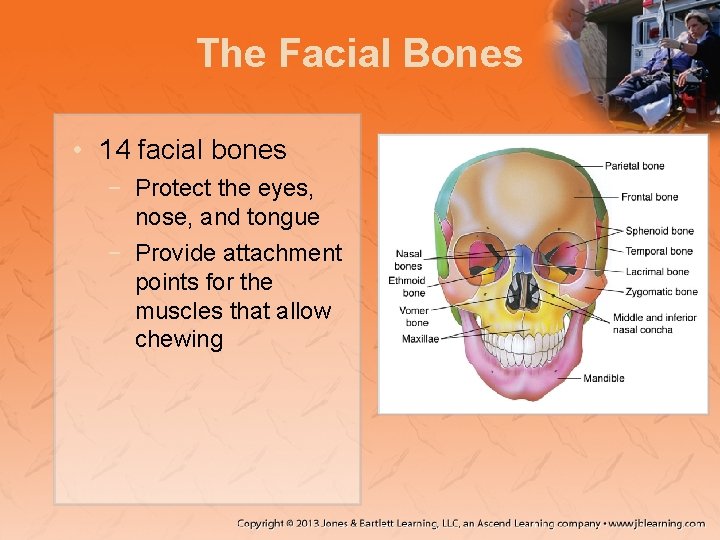
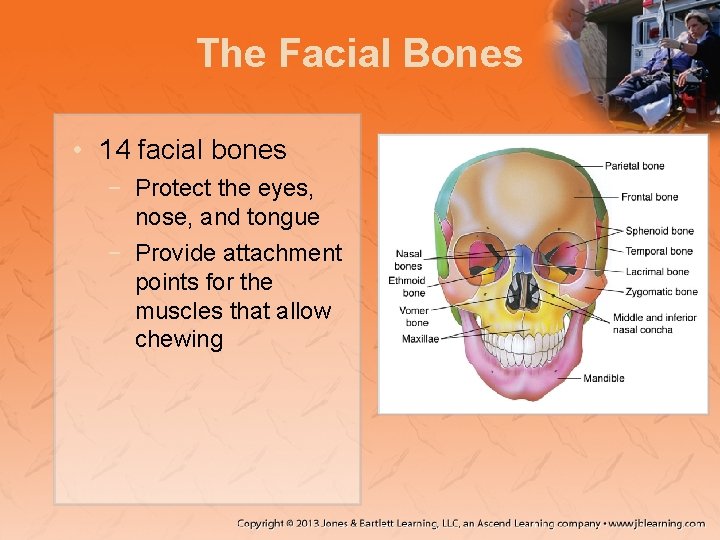
The Facial Bones • 14 facial bones − Protect the eyes, nose, and tongue − Provide attachment points for the muscles that allow chewing
The Facial Bones • Two major nerves provide control: − Trigeminal nerve • Ophthalmic nerve • Maxillary nerve • Mandibular nerve − Facial nerve
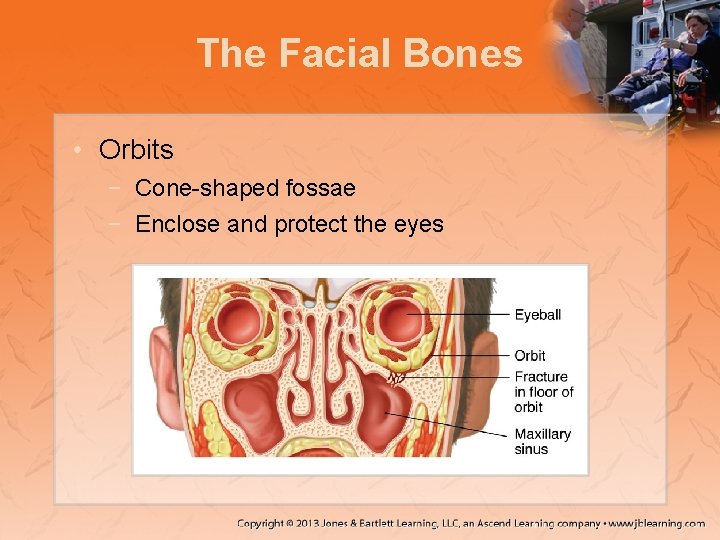
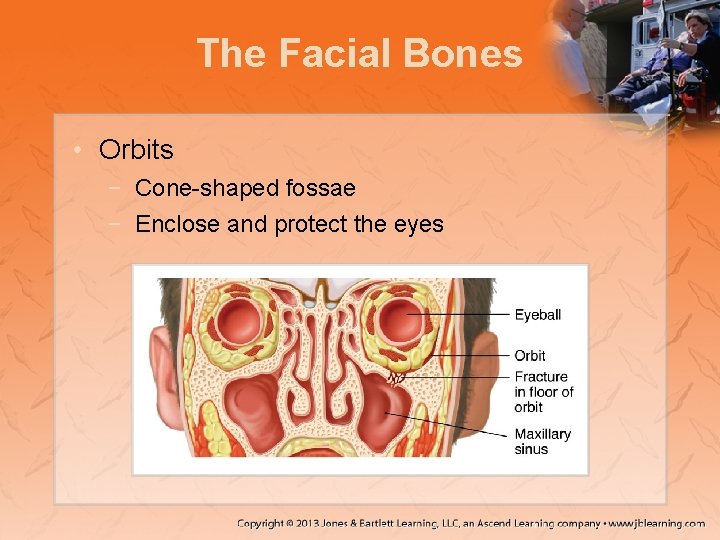
The Facial Bones • Orbits − Cone-shaped fossae − Enclose and protect the eyes
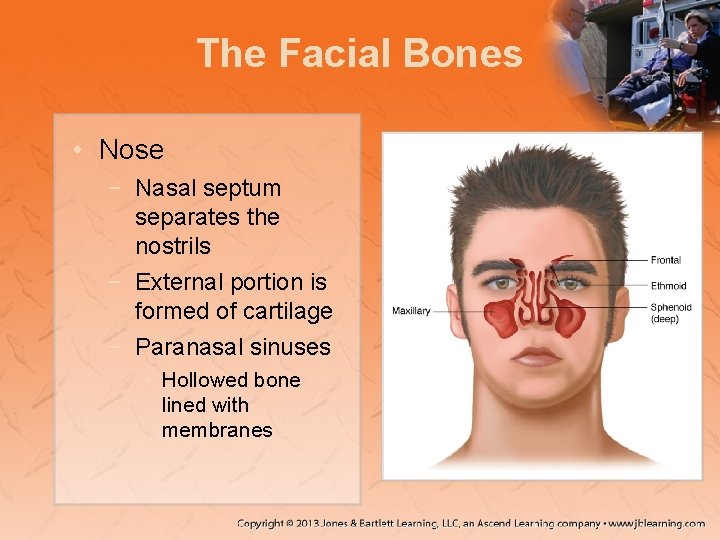
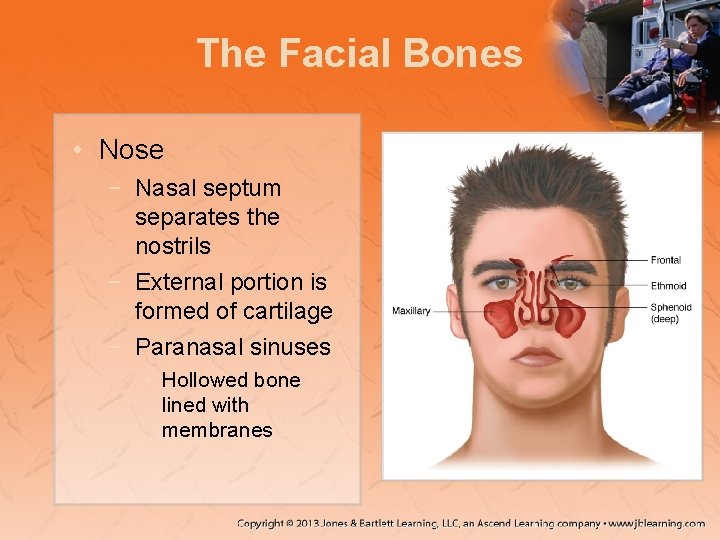
The Facial Bones • Nose − Nasal septum separates the nostrils − External portion is formed of cartilage − Paranasal sinuses • Hollowed bone lined with membranes

The Facial Bones • Mandible − Movable bone forming the lower jaw • Temporomandibular joint (TMJ) − Allows movement of the mandible

The Facial Bones

The Eye • Globe: spherical structure housed within the orbit • Oculomotor nerve − Innervates the muscles that cause motion • Optic nerve − Provides the sense of vision
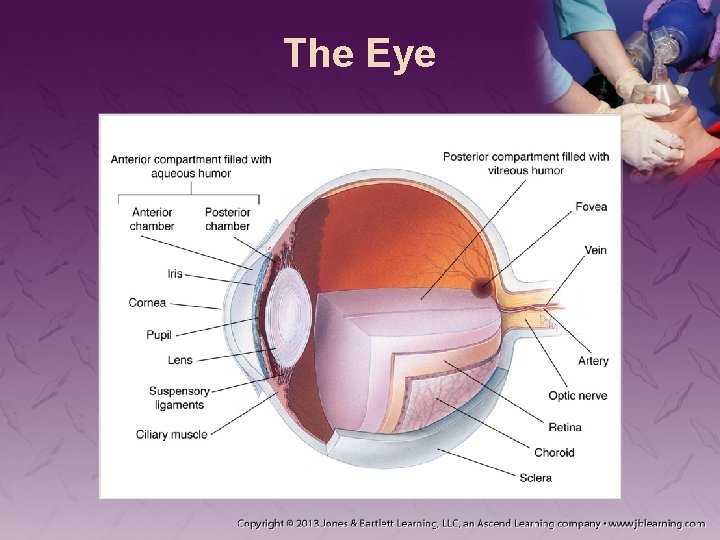
The Eye • Structures of the eye include: − − − − Sclera Cornea Conjunctiva Iris Pupil Lens Retina
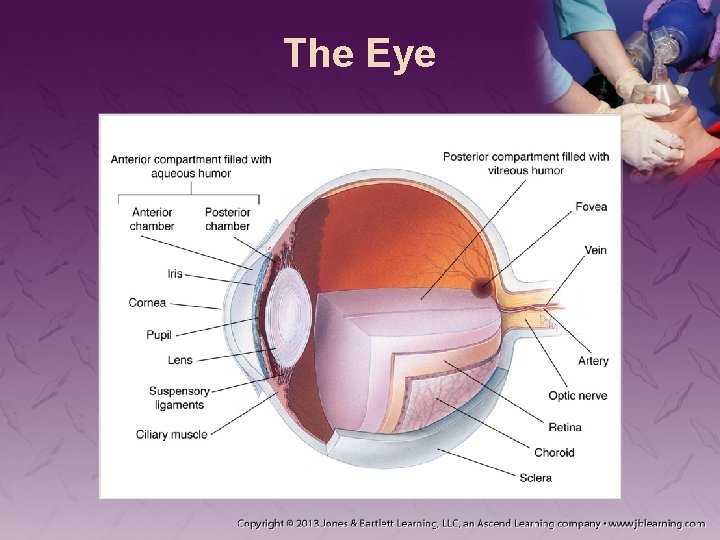
The Eye
The Eye • Anterior chamber is filled with aqueous humor. − If lost, it will be replenished. • Posterior chamber is filled with vitreous humor. − If lost, it cannot be replenished.
The Eye • Two types of vision: − Central vision • Visualization of objects directly in front of you − Peripheral vision • Visualization of lateral objects
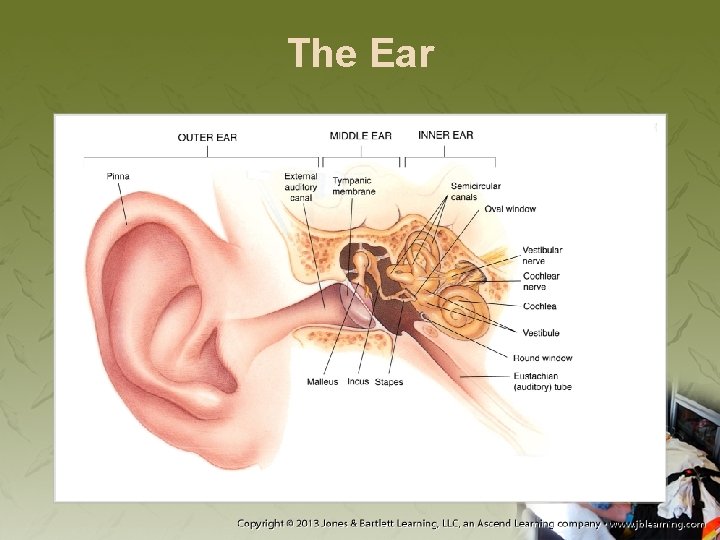
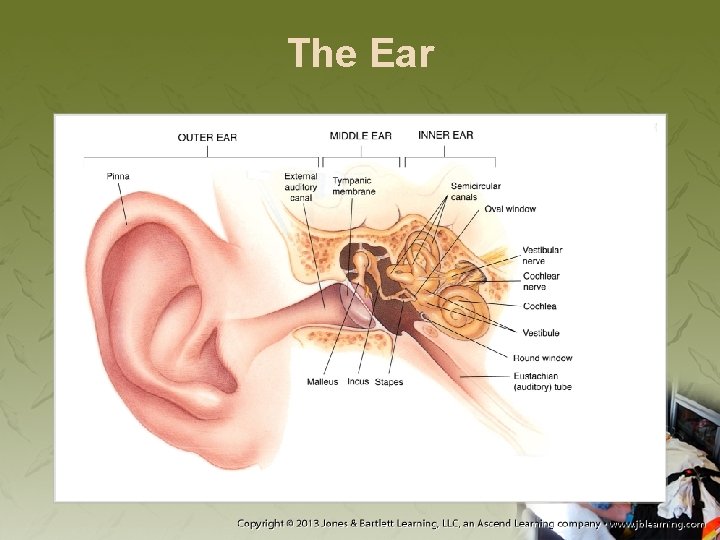
The Ear • Divided into three anatomic parts − External ear − Middle ear − Inner ear
The Ear

The Ear • Sound waves enter through the pinna. − Travel to the tympanic membrane − Vibration is transmitted to the cochlear duct. − At the organ of Corti, vibration forms nerve impulses that travel to the brain.
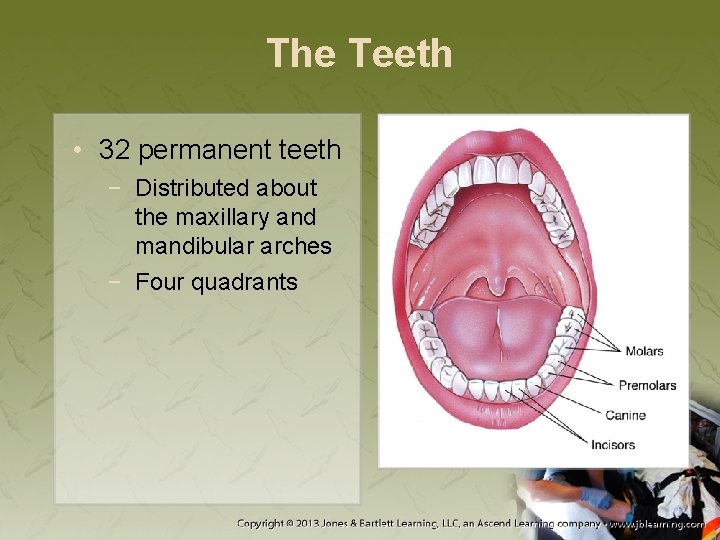
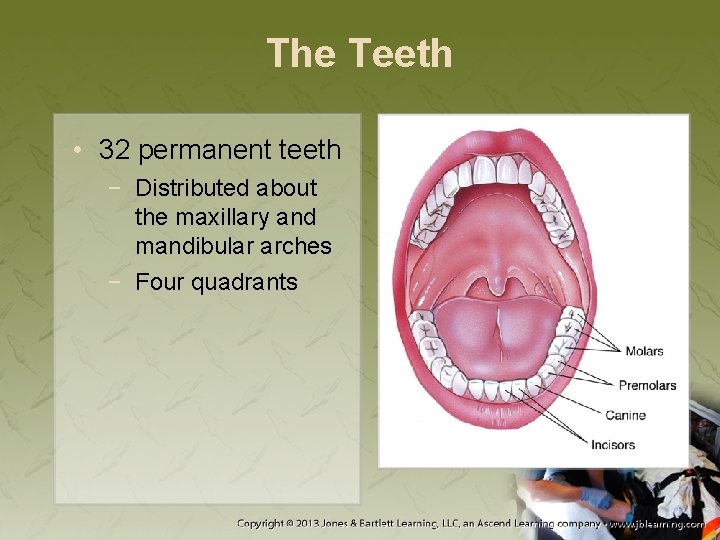
The Teeth • 32 permanent teeth − Distributed about the maxillary and mandibular arches − Four quadrants
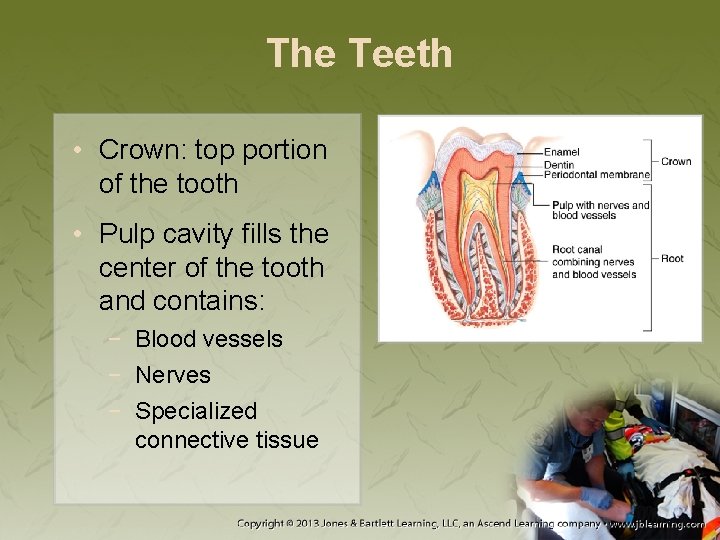
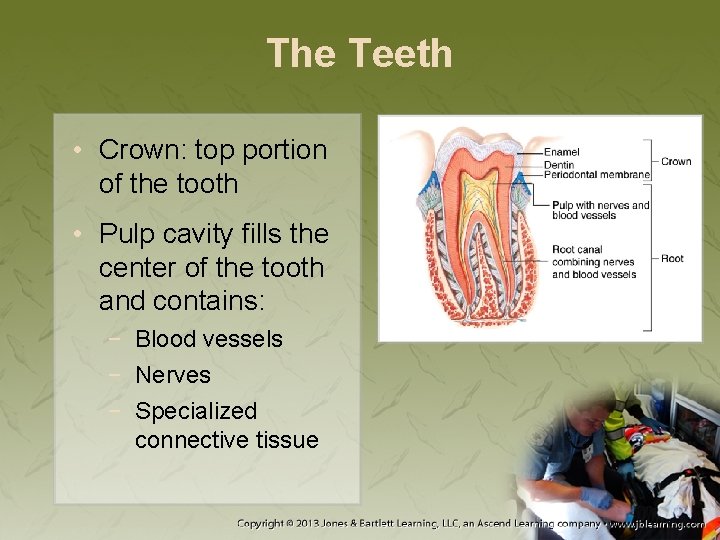
The Teeth • Crown: top portion of the tooth • Pulp cavity fills the center of the tooth and contains: − Blood vessels − Nerves − Specialized connective tissue

The Mouth • Digestion begins with mastication. • Tongue: primary organ of taste
The Mouth • Hypoglossal nerve − Provides motor function to tongue • Glossopharyngeal nerve − Provides taste sensation • Mandibular branch of trigeminal nerve − Provides motor innervation • Facial nerve − Provides taste and sensations
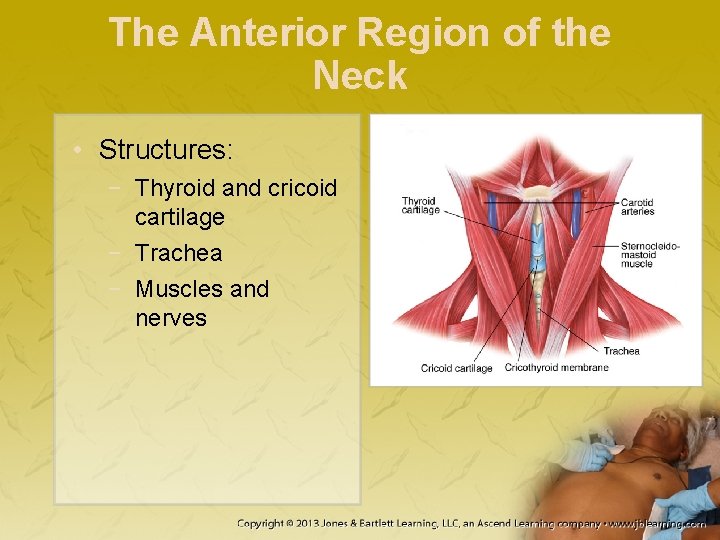
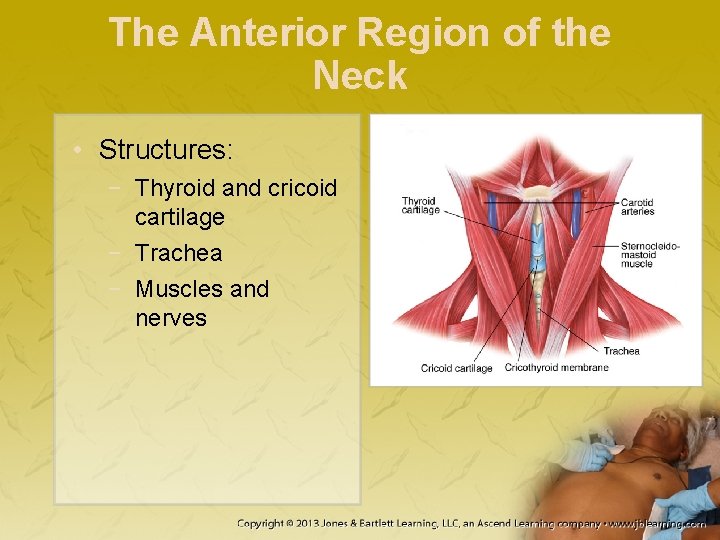
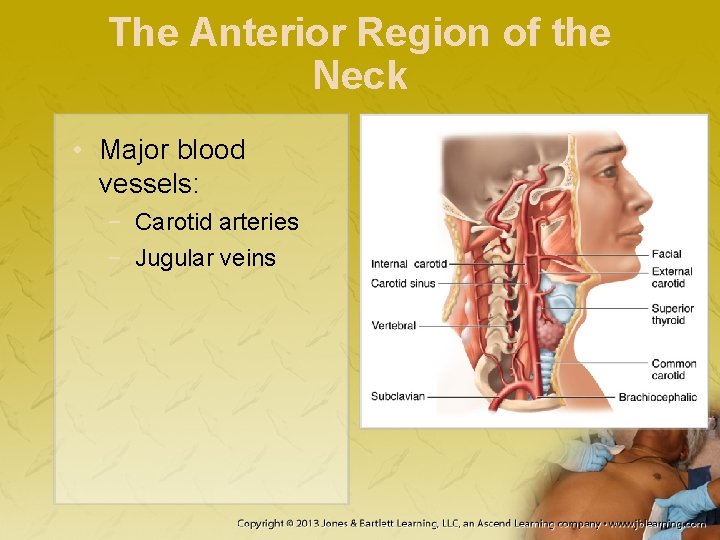
The Anterior Region of the Neck • Structures: − Thyroid and cricoid cartilage − Trachea − Muscles and nerves
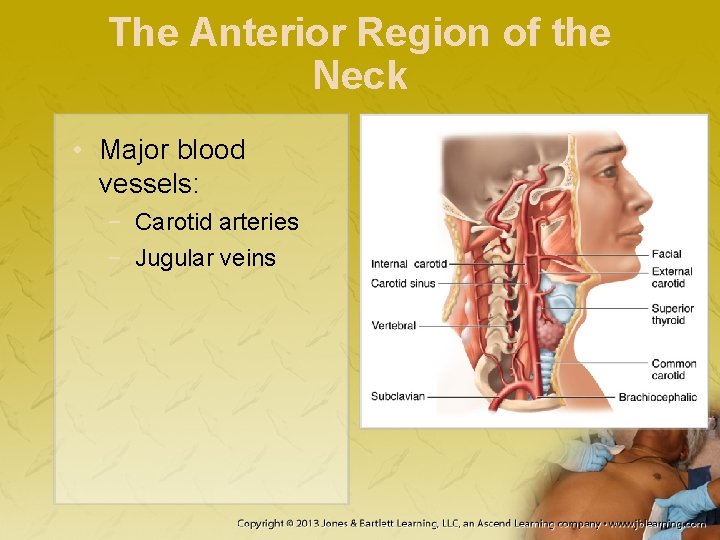
The Anterior Region of the Neck • Major blood vessels: − Carotid arteries − Jugular veins
Scene Size-Up • Assess and address any hazards. • Determine the number of patients. • Consider need for additional resources. • Evaluate the mechanism of injury (MOI).

Primary Assessment • Form a general impression. − Determine whether life threats are present. − If potential for neck or spine injury exists, perform manual immobilization. − Check for responsiveness.
Primary Assessment • Airway and breathing − − Determine whether air is moving. Suction as needed. Correct airway patency. Assess the patient’s breathing.
Primary Assessment • Circulation − − Palpate the pulse. Inspect the skin. Control significant bleeding. If multiple systems are likely affected, perform a rapid exam.
Primary Assessment • Transport decision − The following require immediate transport: • • • Poor initial general impression Altered level of consciousness Dyspnea Abnormal vital signs Shock Severe pain
Primary Assessment • Transport decision (cont’d) − Other signs that require rapid transport: • • Tachycardia Tachypnea Weak pulse Cool, moist, and pale skin
History Taking • Was there a precipitating factor? • Ask about the injury. − Record information on the patient care record. • If unresponsive, your only sources of information may be: − The scene − Medic Alert jewelry
Secondary Assessment • Assess the respiratory system. − Listen for air movement and breath sounds. − Determine the rate and quality of respiration. − Assess for asymmetric chest wall movement.
Secondary Assessment • Assess the neurologic system. − − Level of consciousness Pupil size and reactivity Motor response Sensory response

Secondary Assessment • Assess the musculoskeletal system. − Look for DCAP-BTLS. − Assess the chest, abdomen, and extremities. − Assess the posterior torso.
Secondary Assessment • Assess all anatomic regions. • Record pulse, motor, and sensory function. • Reassess the vital signs.
Reassessment • Obtain and evaluate vital signs. • Check interventions. • Repeat the primary assessment.
Reassessment • Documentation should include: − − Description of the MOI Position in which you found the patient Location and description of injuries Accurate account of treatment
Emergency Medical Care • Focus on airway protection. • Expose wounds, control bleeding, and prepare to treat for shock. − Patients with major closed soft-tissue injury should receive oxygen. − Splint painful, swollen, or deformed extremities.
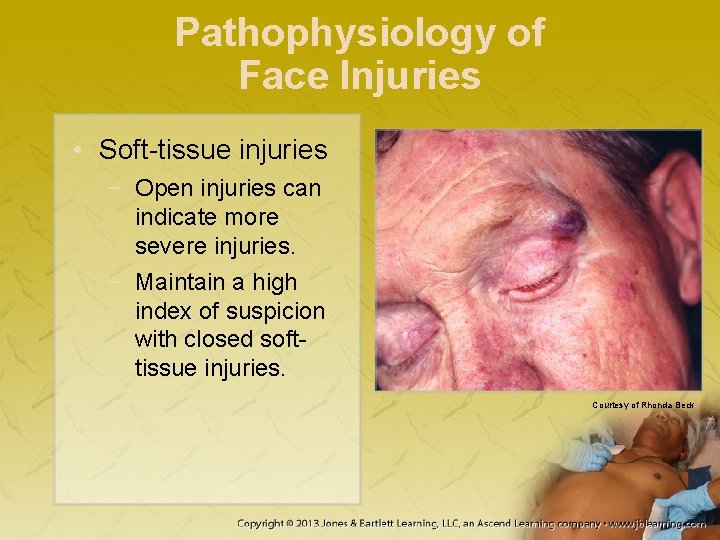
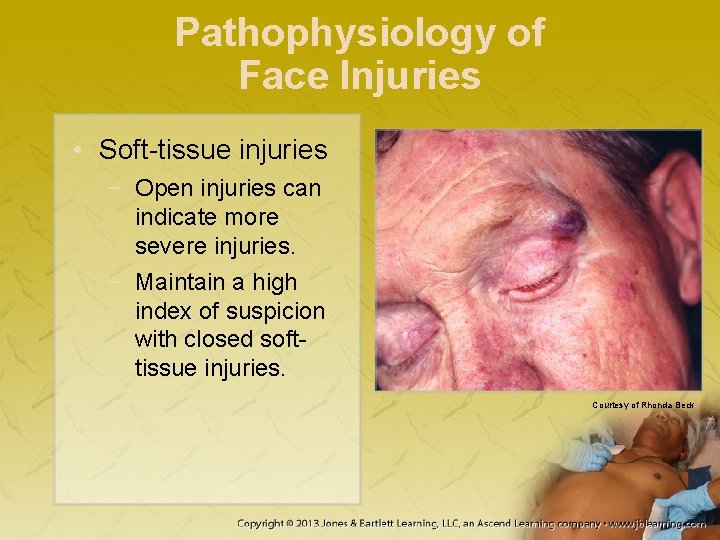
Pathophysiology of Face Injuries • Soft-tissue injuries − Open injuries can indicate more severe injuries. − Maintain a high index of suspicion with closed softtissue injuries. Courtesy of Rhonda Beck

Pathophysiology of Face Injuries • Soft-tissue injuries (cont’d) − Impaled objects present risk of airway compromise. − Massive oropharyngeal bleeding can result in: • Airway obstruction • Aspiration • Ventilator inadequacy
Pathophysiology of Face Injuries • Maxillofacial fractures − Occur when facial bones absorb strong impact − When assessing, protect the cervical spine. − First clue: ecchymosis
Pathophysiology of Face Injuries • Nasal fractures − Nasal bones are not structurally sound. − Characterized by: • Swelling • Tenderness • Crepitus

Pathophysiology of Face Injuries • Mandibular fractures and dislocations − Suspect in patients with blunt force trauma to lower third of face, presenting with: • Dental malocclusion • Numbness of the chin • Inability to open the mouth
Pathophysiology of Face Injuries • Maxillary fractures − Produce: • • Massive facial swelling Instability of the midfacial bones Malocclusion Elongated appearance of the face

Pathophysiology of Face Injuries • Maxillary fractures (cont’d) − Le Fort fractures are classified into: • Le Fort I fracture • Le Fort III fracture
Pathophysiology of Face Injuries • Orbital fractures − Signs and symptoms include: • • • Infraorbital hypoesthesia Enophthalmos traumaticus Massive nasal discharge Impaired vision Paralysis of upward gaze
Pathophysiology of Face Injuries • Zygomatic fractures − Signs and symptoms include: • Flattened appearance on face • Loss of sensation over cheek, nose, and upper lip • Paralysis of upward gaze
Assessment of Face Injuries • It is not important to distinguish among the various fractures in the prehospital setting. • Assessment is primarily clinical. • Pay attention to: − Swelling and deformity − Instability − Blood loss
Assessment of Face Injuries • Evaluate the cranial nerve function. • Visually inspect the oropharynx for signs of posterior epistaxis. − Alert the ED to this situation.
Management of Face Injuries • Protect the cervical spine. • Inspect the mouth for objects that could obstruct the airway. • Suction the oropharynx as needed. • Insert an airway adjunct as needed.
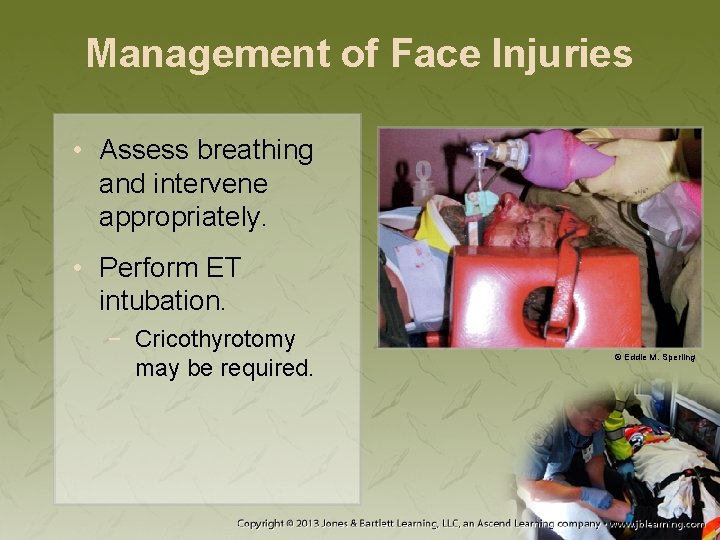
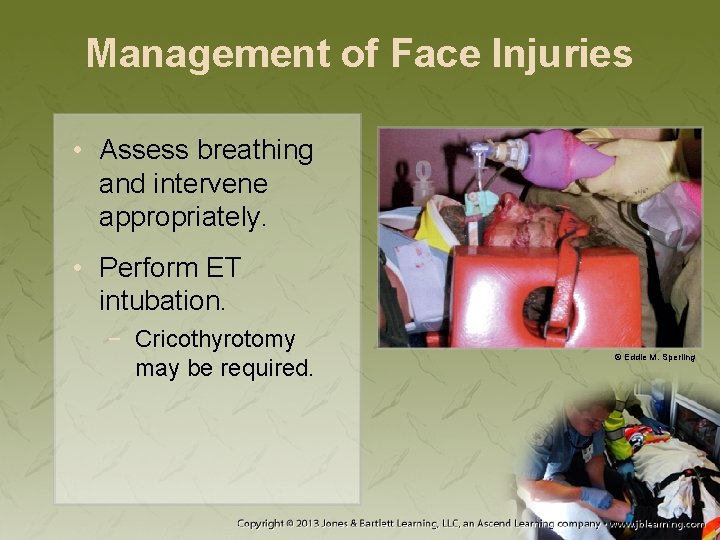
Management of Face Injuries • Assess breathing and intervene appropriately. • Perform ET intubation. − Cricothyrotomy may be required. © Eddie M. Sperling
Management of Face Injuries • Soft-tissue injuries − Control bleeding with direct pressure; apply sterile dressings. − Leave impaled objects in the face unless they pose a threat to the airway

Management of Face Injuries • Soft-tissue injuries (cont’d) − For severe oropharyngeal bleeding with inadequate ventilation: • Suction the airway for 15 seconds. • Provide ventilatory assistance for 2 minutes. • Continue alternating until the airway is cleared or secured.
Management of Face Injuries • Soft-tissue injuries (cont’d) − Epistaxis is most effectively controlled by applying direct pressure to the nares. • Responsive patients should sit up and forward. • Unresponsive patients should be positioned on their side.

Management of Face Injuries • Maxillofacial fractures − Cold compresses may reduce swelling, pain − Determine: • Whether patient has significant medical problems • Approximate time of injury • Any drug allergies and last oral intake
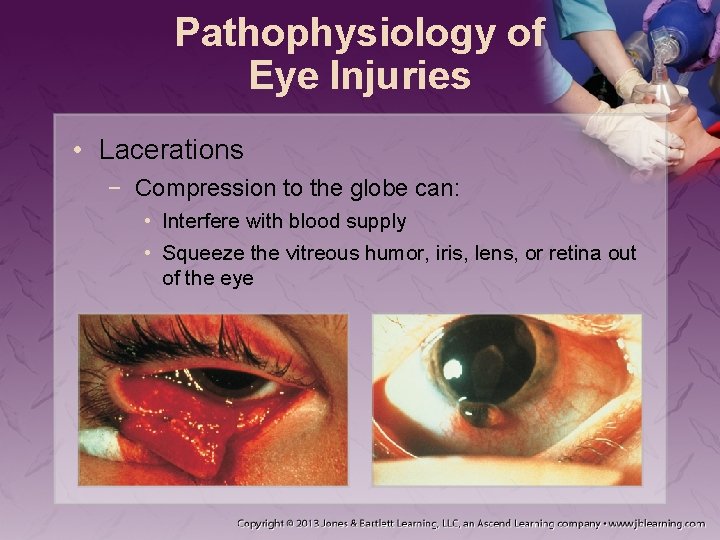
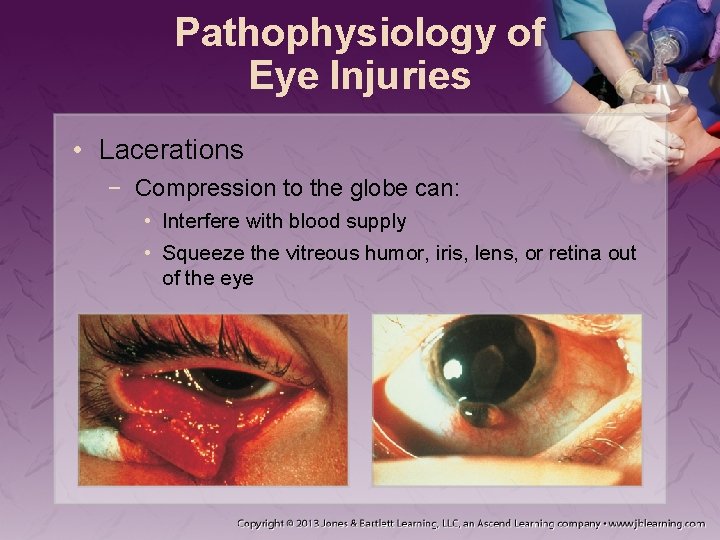
Pathophysiology of Eye Injuries • Lacerations − Compression to the globe can: • Interfere with blood supply • Squeeze the vitreous humor, iris, lens, or retina out of the eye

Pathophysiology of Eye Injuries • Foreign bodies, impaled objects − Foreign objects can produce irritation. • Conjunctivitis: inflamed and red conjunctiva • Eye produces tears.
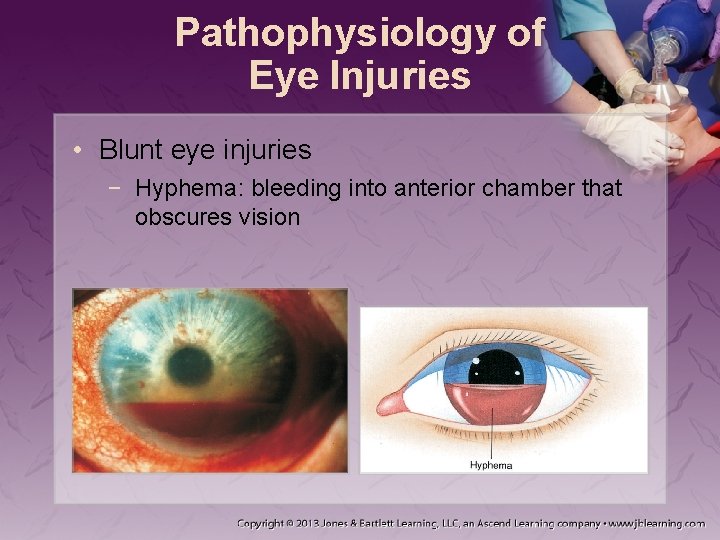
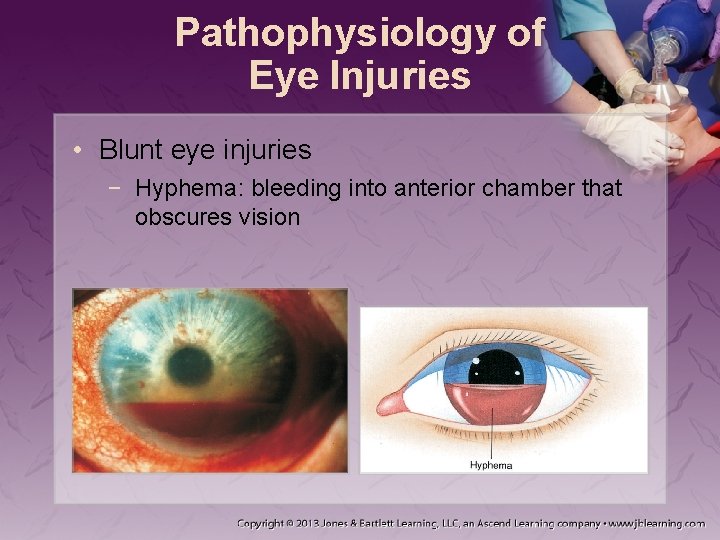
Pathophysiology of Eye Injuries • Blunt eye injuries − Hyphema: bleeding into anterior chamber that obscures vision
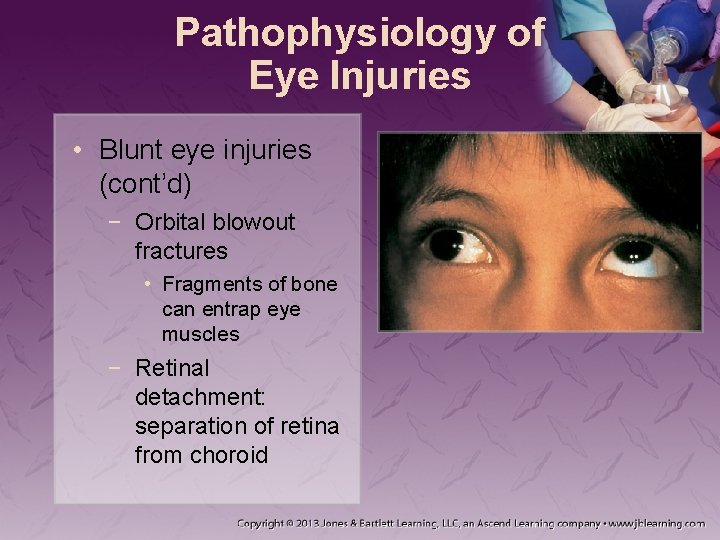
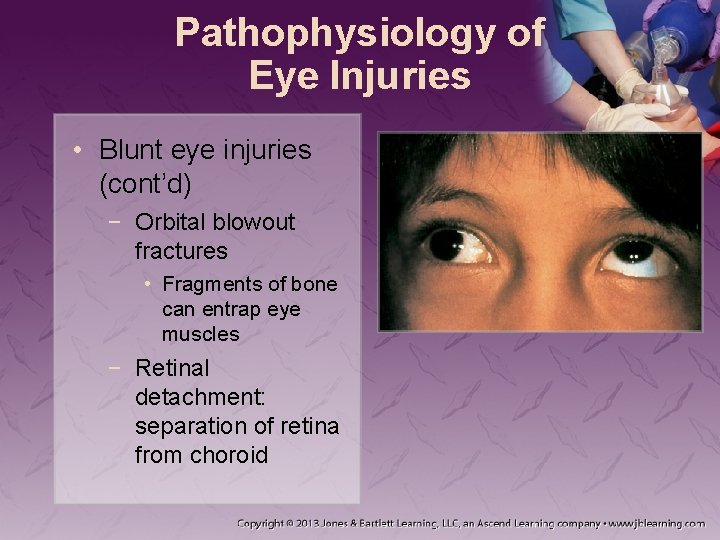
Pathophysiology of Eye Injuries • Blunt eye injuries (cont’d) − Orbital blowout fractures • Fragments of bone can entrap eye muscles − Retinal detachment: separation of retina from choroid
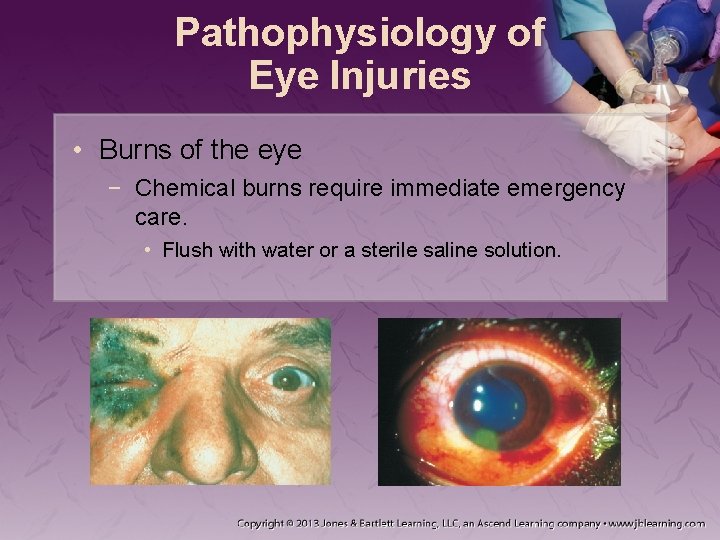
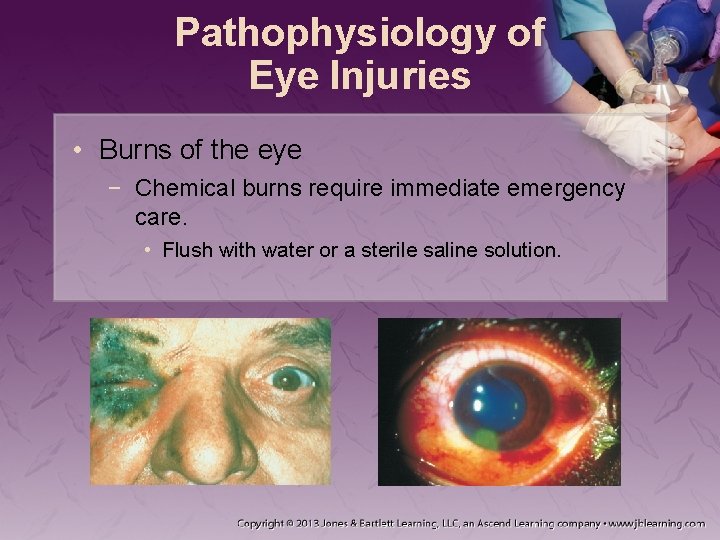
Pathophysiology of Eye Injuries • Burns of the eye − Chemical burns require immediate emergency care. • Flush with water or a sterile saline solution.
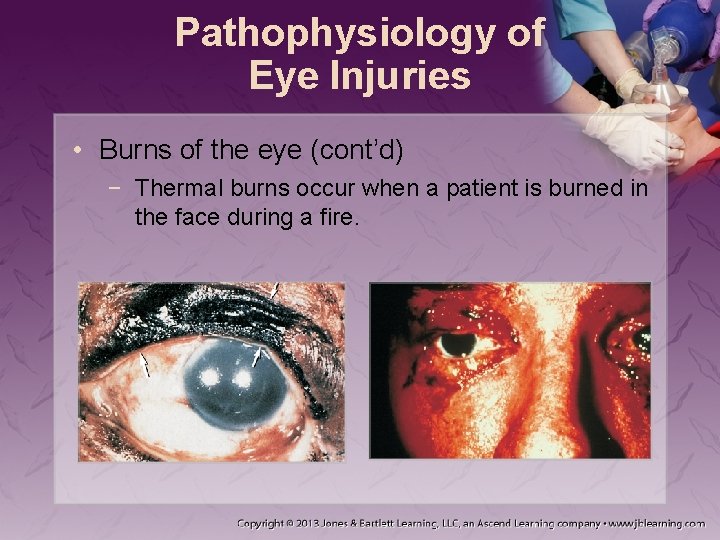
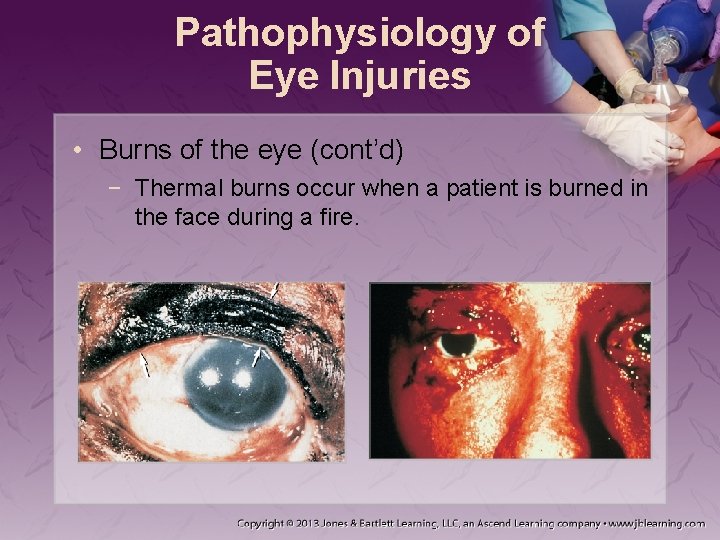
Pathophysiology of Eye Injuries • Burns of the eye (cont’d) − Thermal burns occur when a patient is burned in the face during a fire.

Pathophysiology of Eye Injuries • Burns of the eye (cont’d) − Infrared rays, eclipse light, and laser burns can damage sensory cells. − Superficial burns can result from ultraviolet rays. • May not be painful initially
Assessment of Eye Injuries • Note the MOI. • Ensure a patent airway. • Control any external bleeding. • If appropriate, perform a rapid exam.

Assessment of Eye Injuries • When obtaining the history, determine: − − − How and when did the injury happen? When did the symptoms begin? What symptoms is the patient experiencing? Were both eyes affected? Are there underlying diseases or conditions? Does the patient take medications?
Assessment of Eye Injuries • Symptoms of serious ocular injury: − − Visual loss Double vision Severe eye pain A foreign body sensation
Assessment of Eye Injuries • During physical examination, evaluate: − Orbital rim: ecchymosis, swelling, lacerations, tenderness − Eyelids: ecchymosis, swelling, lacerations − Corneas: foreign bodies − Conjunctivae: redness, pus, inflammation, foreign bodies
Assessment of Eye Injuries • During physical examination, evaluate (cont’d): − Globes: redness, abnormal pigmentation, lacerations − Pupils: size, shape, equality, reaction to light − Eye movements: paralysis of gaze or discoordination between eyes − Visual acuity: ask patient to read a newspaper
Management of Eye Injuries • Lacerations and blunt trauma − Prehospital care of injuries to the eyelids: • Bleeding control • Gentle patching of the eye − Most globe injuries are best treated in the ED.
Management of Eye Injuries • Lacerations and blunt trauma (cont’d) − When treating penetrating injuries of the eye: • Never exert pressure on the injured globe. • If part of the globe is exposed, gently apply a moist, sterile dressing. • Cover with a protective shield, cup, or dressing. • Apply soft dressings; provide transport.
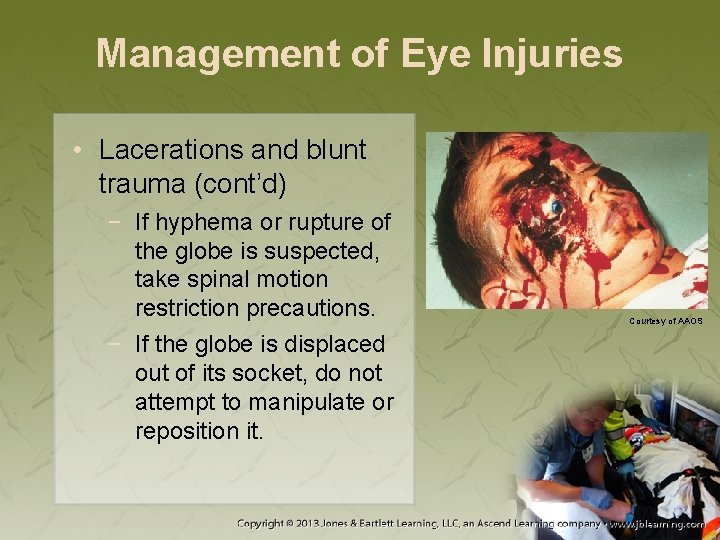
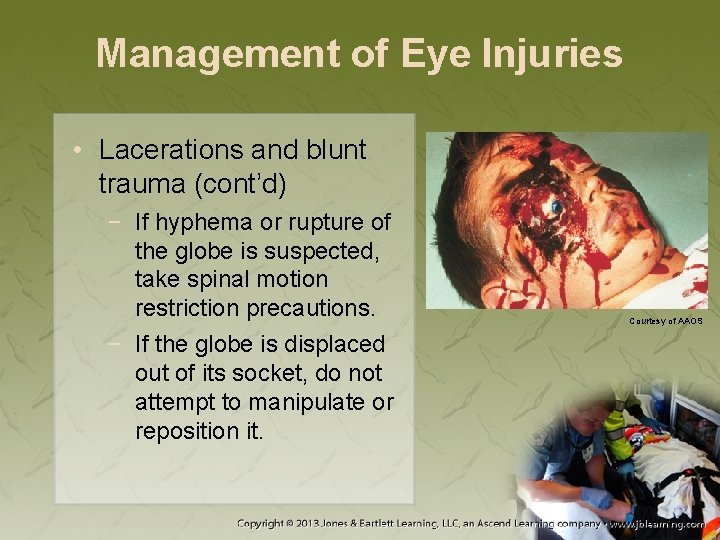
Management of Eye Injuries • Lacerations and blunt trauma (cont’d) − If hyphema or rupture of the globe is suspected, take spinal motion restriction precautions. − If the globe is displaced out of its socket, do not attempt to manipulate or reposition it. Courtesy of AAOS
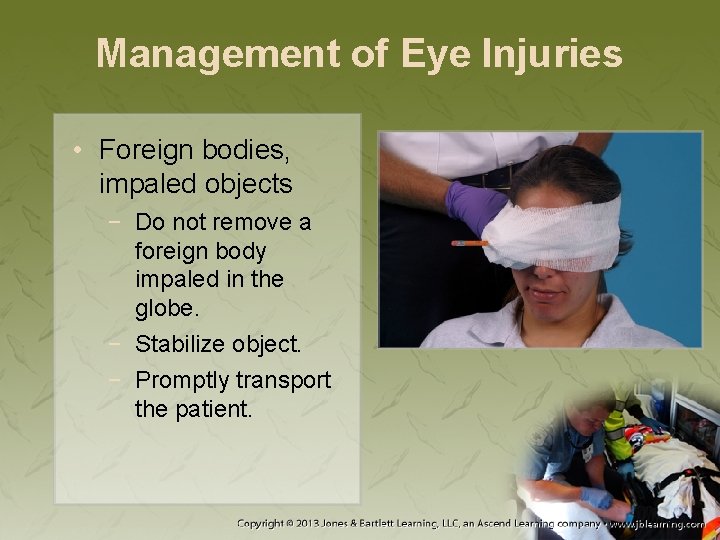
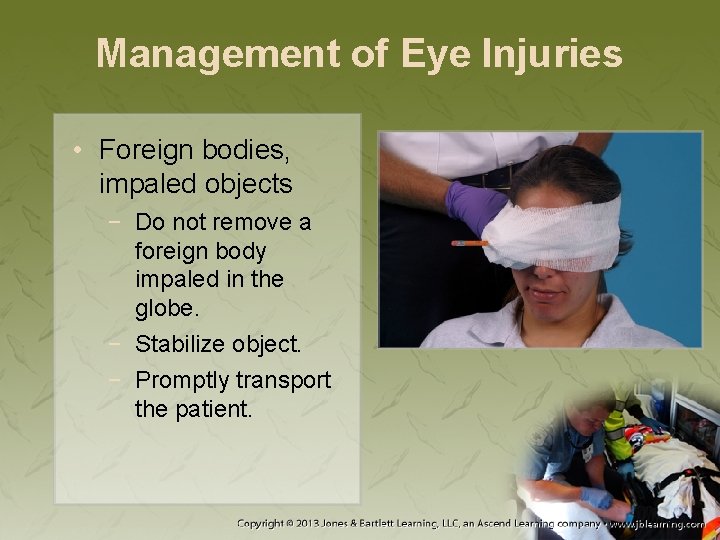
Management of Eye Injuries • Foreign bodies, impaled objects − Do not remove a foreign body impaled in the globe. − Stabilize object. − Promptly transport the patient.
Management of Eye Injuries • Burns caused by ultraviolet light − Cover with a sterile, moist pad and eye shield. − Apply cool compresses if patient is in distress. − Place the patient in a supine position.

Management of Eye Injuries • Chemical burns − Immediately irrigate with water or saline solution. − Avoid contaminated water getting into unaffected eye. − Irrigate for at least 5 minutes.

Management of Eye Injuries Courtesy of AAOS

Management of Eye Injuries • To examine the undersurface of the upper eyelid, pull the lid upward and forward. − If you spot a foreign object, remove it with a moist, sterile, cotton-tipped applicator. • Unless imbedded in the cornea
Pathophysiology of Ear Injuries • Soft-tissue injuries − Pinna has a poor blood supply. • Tends to heal poorly • Healing is often complicated by infection.
Pathophysiology of Ear Injuries • Ruptured eardrum − Signs and symptoms include: • Loss of hearing • Blood drainage from the ear − Typically heals spontaneously
Assessment and Management of Ear Injuries • Ensure breathing adequacy. • If MOI suggests spinal injury, apply full spinal motion restriction precautions.

Assessment and Management of Ear Injuries • If direct pressure does not control bleeding: − Place dressing between ear and scalp. − Apply roller bandage. − Apply ice pack.
Assessment and Management of Ear Injuries • If partially avulsed: − Realign the ear into position. − Gently bandage with padding that has been slightly moistened with normal saline. • If completely avulsed: − Wrap it in salinemoistened gauze. − Place in plastic bag and place bag on ice.
Assessment and Management of Ear Injuries • If blood or CSF drainage is noted: − Apply a loose dressing over the ear. − Assess for basilar skull fracture. • Do not remove an impaled object. − Stabilize the object. − Cover the ear to prevent movement and minimize contamination.
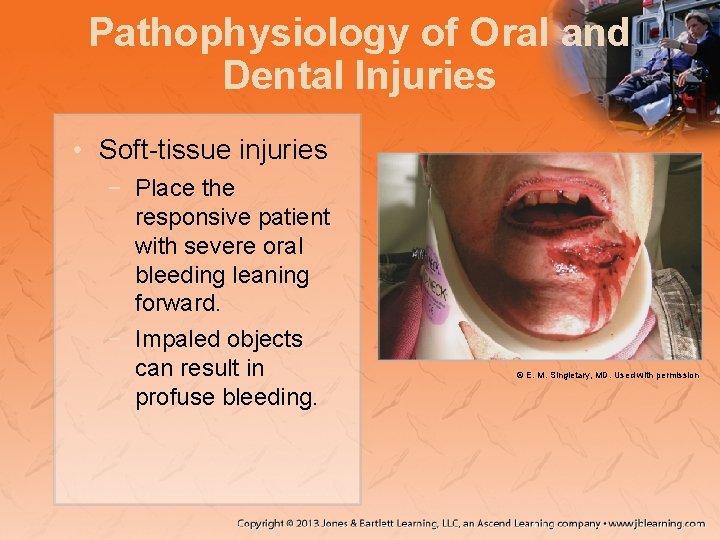
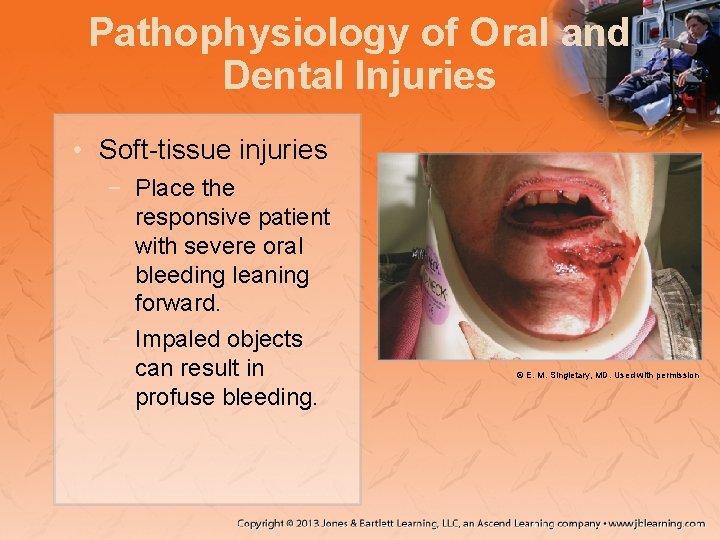
Pathophysiology of Oral and Dental Injuries • Soft-tissue injuries − Place the responsive patient with severe oral bleeding leaning forward. − Impaled objects can result in profuse bleeding. © E. M. Singletary, MD. Used with permission

Pathophysiology of Oral and Dental Injuries • Dental injuries − May be associated with mechanisms that cause severe maxillofacial trauma − Always assess the mouth following facial injury.
Assessment and Management of Oral and Dental Injuries • Ensure adequate breathing. − Suction the oropharynx as needed. − Remove fractured tooth fragments. − Apply spinal motion restriction precautions as dictated by the MOI.
Assessment and Management of Oral and Dental Injuries • Impaled objects should be stabilized. − Unless they interfere with airway • To replant an avulsed tooth: − Place the tooth in its socket. − Hold it in place with or have patient bite down.

Pathophysiology of Injuries to the Anterior Part of the Neck • Soft-tissue injuries − Blunt trauma often results in: • Swelling and edema • Injury to the various structures • Injury to the cervical spine − Be prepared to initiate aggressive management.
Pathophysiology of Injuries to the Anterior Part of the Neck • Soft-tissue injuries (cont’d) − Primary threats from penetrating trauma: • Massive hemorrhage • Airway compromise − Air embolisms are associated with open neck injuries.
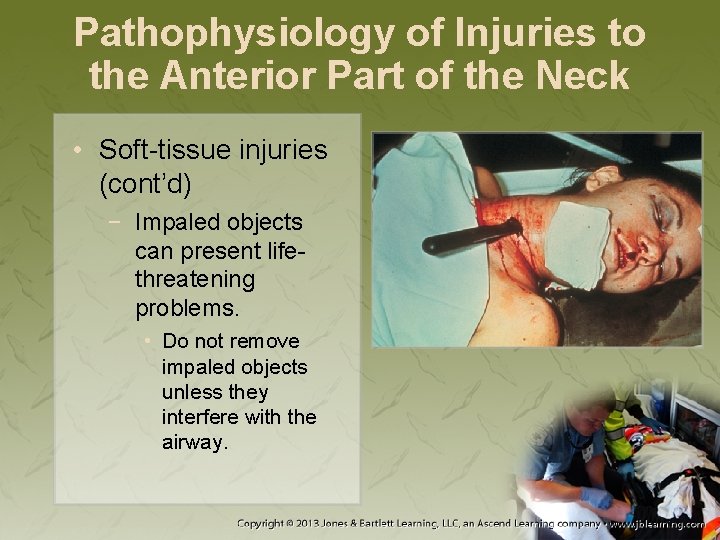
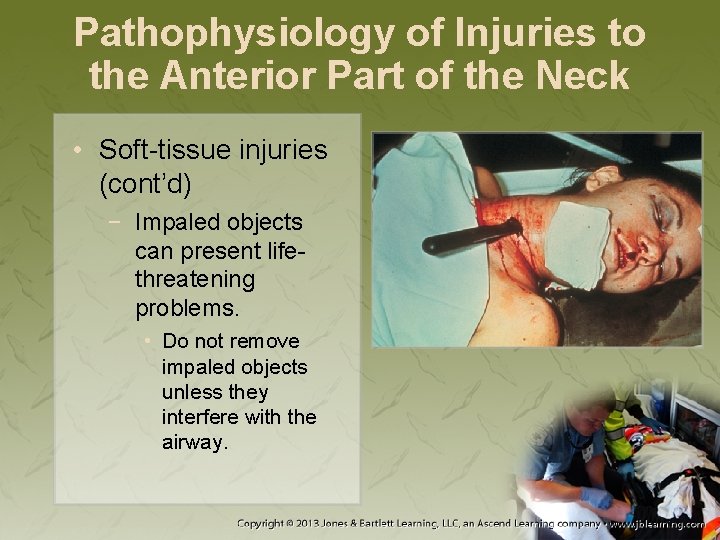
Pathophysiology of Injuries to the Anterior Part of the Neck • Soft-tissue injuries (cont’d) − Impaled objects can present lifethreatening problems. • Do not remove impaled objects unless they interfere with the airway.
Pathophysiology of Injuries to the Anterior Part of the Neck • Injuries to larynx, trachea, and esophagus − Can be easily overlooked − Significant injuries to the larynx and trachea pose risk of airway compromise. − Esophageal perforation can result in mediastinitis.
Assessment of Injuries to the Anterior Part of the Neck • Common signs: − Bruising − Redness to the overlying skin − Palpable tenderness • Note MOI; maintain high index of suspicion
Assessment of Injuries to the Anterior Part of the Neck • If patient is unresponsive: − Stabilize head in a neutral in-line position. − Open airway with the jaw-thrust maneuver. • Assess the patient’s breathing.

Management of Injuries to the Anterior Part of the Neck • To control bleeding from an open neck wound, cover with an occlusive dressing. − Apply direct pressure with a bulky dressing. − Secure by wrapping roller gauze loosely.

Management of Injuries to the Anterior Part of the Neck • Monitor for reflex bradycardia. • Advise the patient to refrain from speaking. • If signs of shock are present: − Keep the patient warm. − Establish vascular access. − Infuse an isotonic crystalloid solution.

Management of Injuries to the Anterior Part of the Neck • Patients may require a surgical or percutaneous airway. − Use multiple techniques for confirming correct ET tube placement.
Pathophysiology of Spine Trauma • Sprain: stretching or tearing of ligaments − Provide cervical spine stabilization. • Strain: stretching or tearing of muscle or tendon − Cervical precautions should be taken.

Assessment of Spine Trauma • Transport to the ED for radiologic studies. • Conduct a visual inspection. • If the patient is symptomatic with pain, maintain spinal stabilization.
Assessment of Spine Trauma • If MOI dictates spinal clearance protocol and examination produces pain: − Stop the examination. − Maintain spinal stabilization. − Transport for further evaluation in the ED.
Management of Spine Trauma • Patients reporting neck pain after injury should be evaluated in the ED. • Address airway, ventilation, and oxygenation considerations. • Prevent further injury with motion restrictions.
Management of Spine Trauma • If your examination reveals no obvious MOI, consider treatment for muscular strain. − Rest, ice, elevation − Soft collar
Injury Prevention • Prevention during activities in which the risk of being hit is high: − − Helmets Face shields Mouth guards Safety glasses

Injury Prevention • Advances in motor vehicle safety include: − Better occupant safety restraints and air bags − Improvements to the headrests
Summary • A strong knowledge of anatomy and physiology of the face, head, and brain is essential to accurately assess and manage patients with injuries to these locations. • Personal safety is your initial primary concern when you are treating any patient with head or face trauma. • Head and face trauma most often result from direct trauma or rapid deceleration.
Summary • Trauma to the face can range from a broken nose to more severe injuries. • Your primary concerns with assessing and managing a patient with facial trauma are to ensure a patent airway and maintain adequate oxygenation and ventilation. • Any patient with head or face trauma should be suspected of having a spinal injury.

Summary • Blind nasotracheal intubation is relatively contraindicated in the presence of midface fracture. • Remove impaled objects in the face or throat only if they impair breathing or if they interfere with your ability to manage the airway. • Injuries to the eye can be varied, including lacerations, blunt trauma, impaled objects, or burns.
Summary • Never remove impaled objects from the eye. • Chemical burns to the eye should be treated with gentle irrigation. • Ear injuries should be realigned and bandaged. If a part is avulsed, transport with the patient if possible. Stabilize an object that is impaled in the ear.
Summary • The primary threat from oral or dental trauma is oropharyngeal bleeding and aspiration of blood or broken teeth. • Aggressively manage injuries involving the anterior neck. • Patients presenting with sprains or strains should be transported for further evaluation at the emergency department.
Credits • Chapter opener: © E. M. Singletary, M. D. Used with permission. • Backgrounds: Orange—© Keith Brofsky/Photodisc/Getty Images; Purple—Jones & Bartlett Learning. Courtesy of MIEMSS; Red—© Margo Harrison/Shutter. Stock, Inc. ; Green—Courtesy of Rhonda Beck. • Unless otherwise indicated, all photographs and illustrations are under copyright of Jones & Bartlett Learning, courtesy of Maryland Institute for Emergency Medical Services Systems, or have been provided by the American Academy of Orthopaedic Surgeons.