Role of Neck Dissection for Differentiated Thyroid CA
- Slides: 23
Role of Neck Dissection for Differentiated Thyroid CA Joint Hospital Surgical Grand Round NDH Dr. Alex TSANG
Background l Differentiated Thyroid CA refers to – – – Papillary thyroid CA Follicular thyroid CA Comprises almost 90% of all Thyroid CA
Papillary Thyroid CA l l l Papillary thyroid cancers (PTC) =77% of thyroid malignancies Strong propensity for regional nodal involvement. Recent analysis which included > 33, 000 patients with PTC, reports a 22% incidence of lymphatic involvement at initial operation
Follicular Thyroid CA l l l Follicular thyroid cancers (FTC) less common Lower rate of lymphatic involvement In the same analysis only 2% with lymphatic involvement Zaydfudim V, Feurer ID, Griffin MR, et al. The impact of lymph node involvement on survival in patients with papillary and follicular thyroid carcinoma. Surgery 2008; 144(6): 1070– 7 [discussion: 1077– 8].
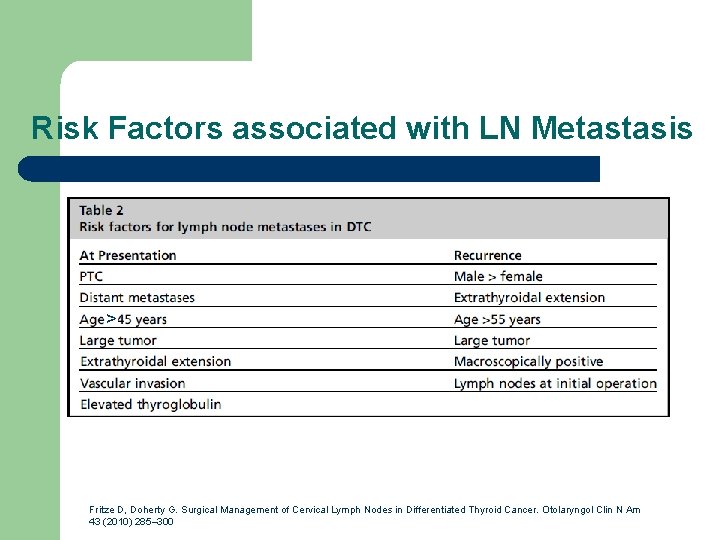
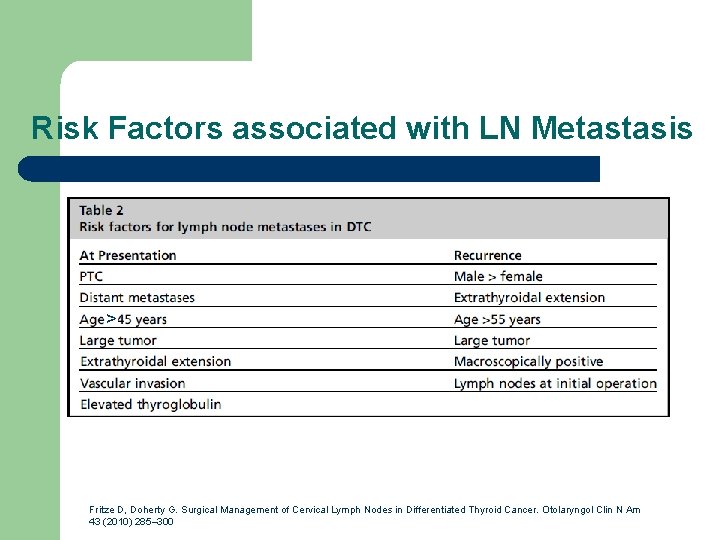
Risk Factors associated with LN Metastasis > Fritze D, Doherty G. Surgical Management of Cervical Lymph Nodes in Differentiated Thyroid Cancer. Otolaryngol Clin N Am 43 (2010) 285– 300
Significance of LN Met l If LN Met +ve in initial OT – Locoregional Recurrence rate: higher l recurrence of DTC in 19% of patients with initially positive nodes and 2% in node-negative patients Loh KC, Greenspan FS, Gee L, et al. Pathological tumor-node-metastasis (p. TNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab 1997; 82(11): 3553– 62. Mc. Henry CR, Rosen IB, Walfish PG. Prospective management of nodal metastases in differentiated thyroid cancer. Am J Surg 1991; 162(4): 353– 6.
Significance of LN Met l If LN Met +ve in initial OT – Distant Met: higher l In a series stratified by tumor size, 0. 7% of patients initially T 1 -T 3 N 0 had distant metastases at diagnosis and 2. 9% eventually developed distant spread. For T 1 T 3 N 1 patients, 8. 5% had systemic involvement at diagnosis, and 15. 1% later developed systemic disease. Loh KC, Greenspan FS, Gee L, et al. Pathological tumor-node-metastasis (p. TNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab 1997; 82(11): 3553– 62. Mc. Henry CR, Rosen IB, Walfish PG. Prospective management of nodal metastases in differentiated thyroid cancer. Am J Surg 1991; 162(4): 353– 6.
Significance of LN Met l If LN Met +ve in initial OT – Survival: inconclusive l l l Some studies showed no significant impact on survival if LN met +ve Some studies showed worse long term survival (at least 14 years) if LN met +ve So, knowing LN status helps to have more accurate staging which affect patients’ further management and prognosis. Loh KC, Greenspan FS, Gee L, et al. Pathological tumor-node-metastasis (p. TNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab 1997; 82(11): 3553– 62. Mc. Henry CR, Rosen IB, Walfish PG. Prospective management of nodal metastases in differentiated thyroid cancer. Am J Surg 1991; 162(4): 353– 6.
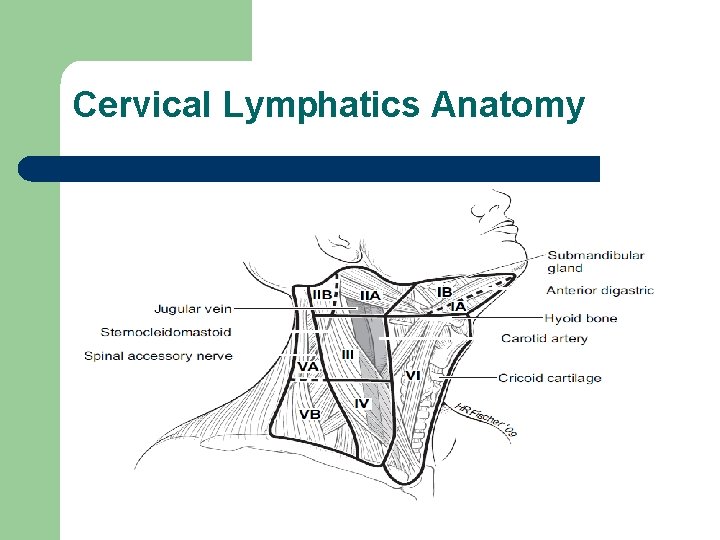
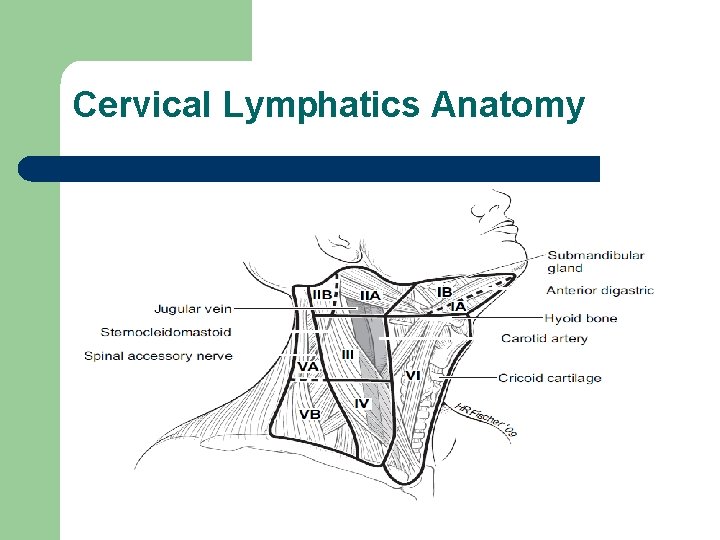
Cervical Lymphatics Anatomy
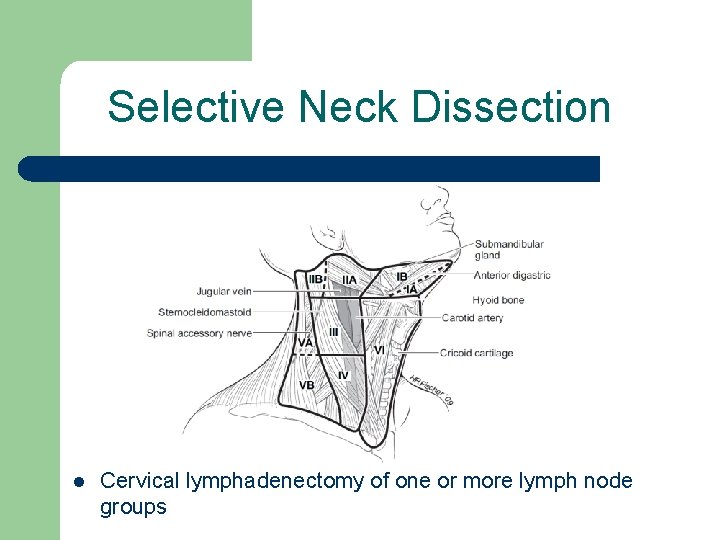
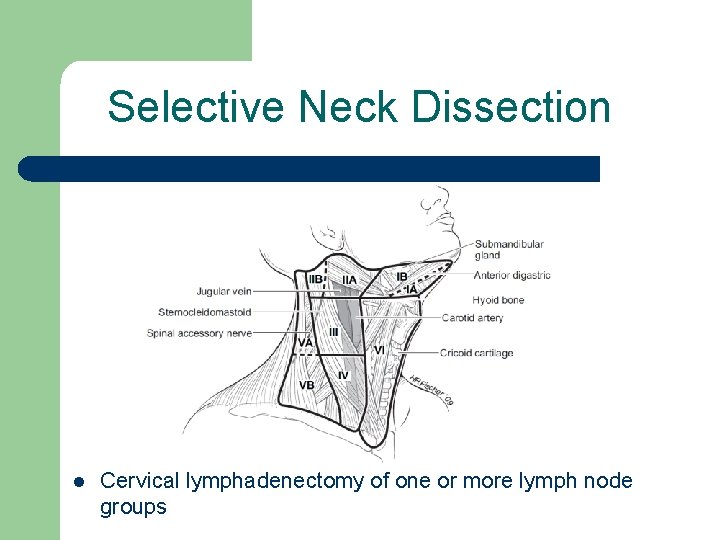
Selective Neck Dissection l Cervical lymphadenectomy of one or more lymph node groups
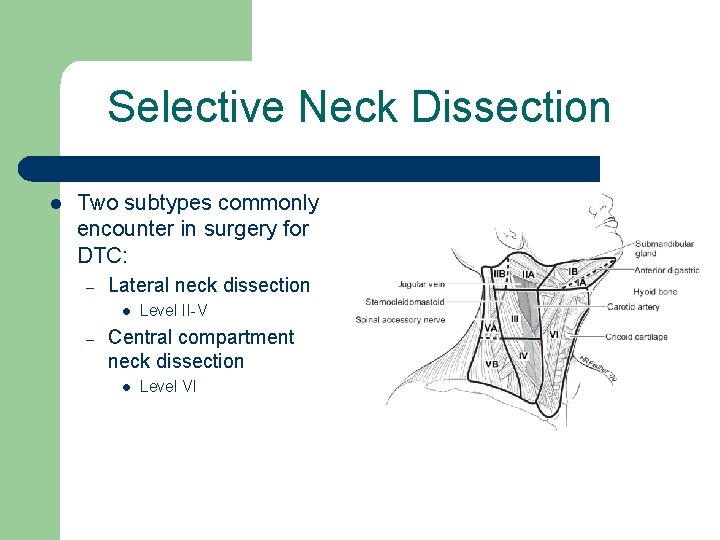
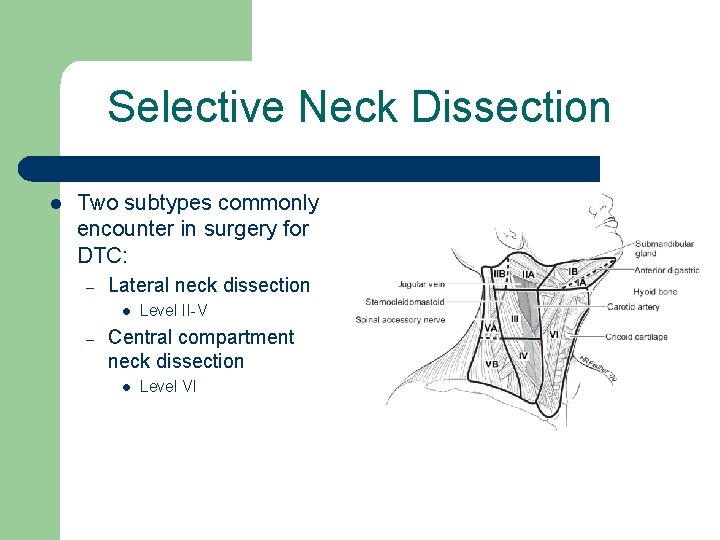
Selective Neck Dissection l Two subtypes commonly encounter in surgery for DTC: – Lateral neck dissection l – Level II-V Central compartment neck dissection l Level VI
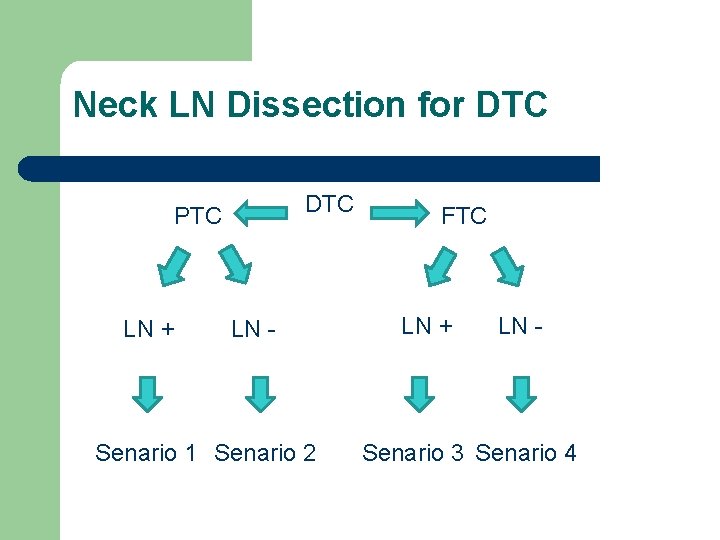
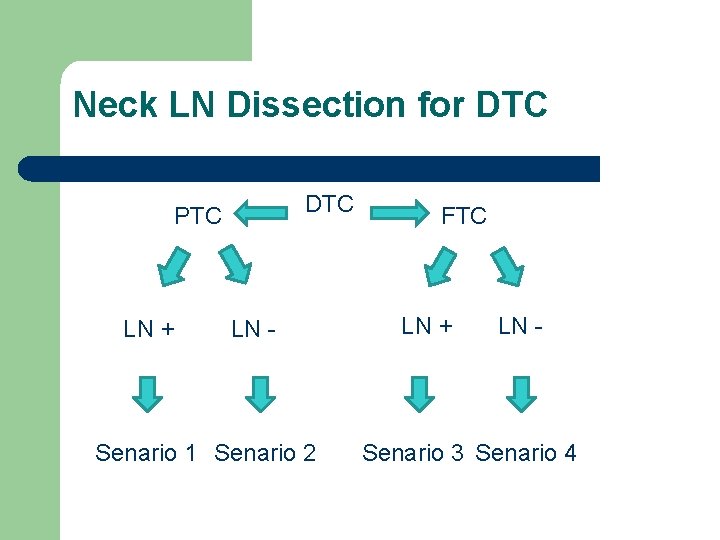
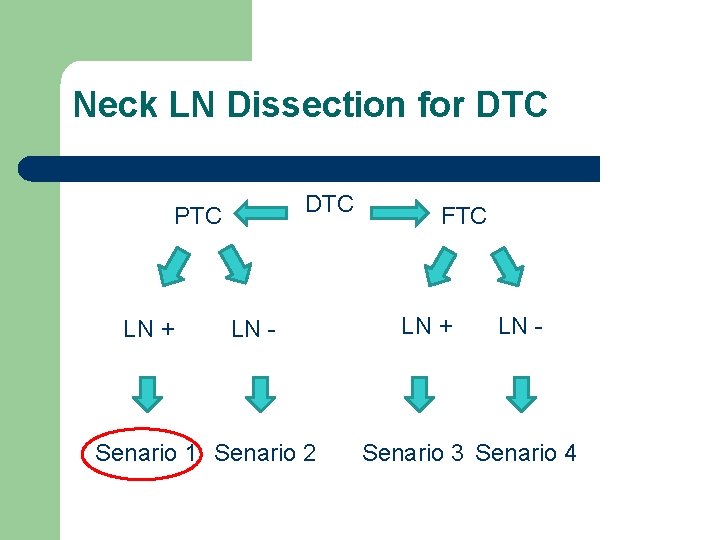
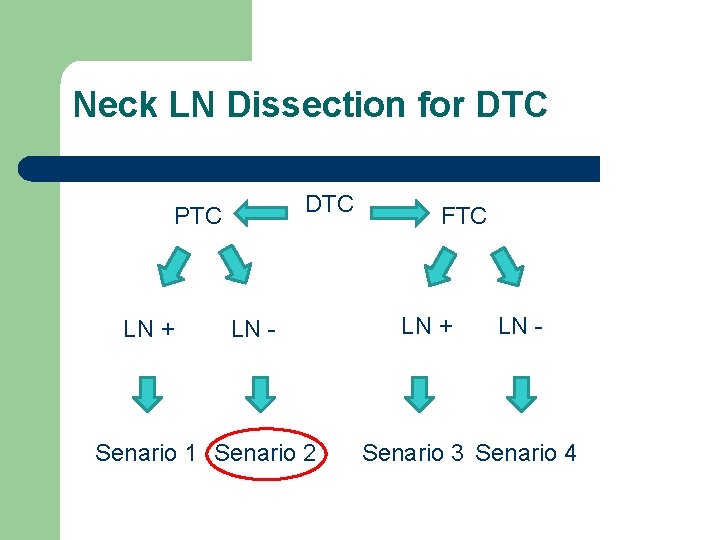
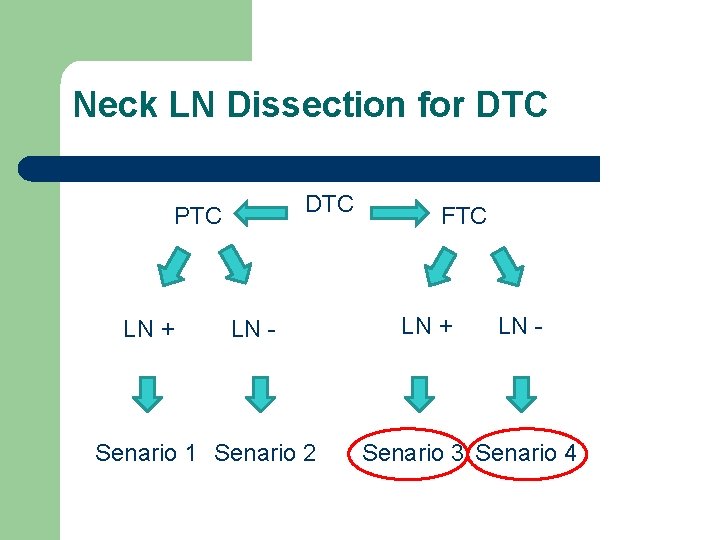
Neck LN Dissection for DTC PTC LN + LN - Senario 1 Senario 2 FTC LN + LN - Senario 3 Senario 4
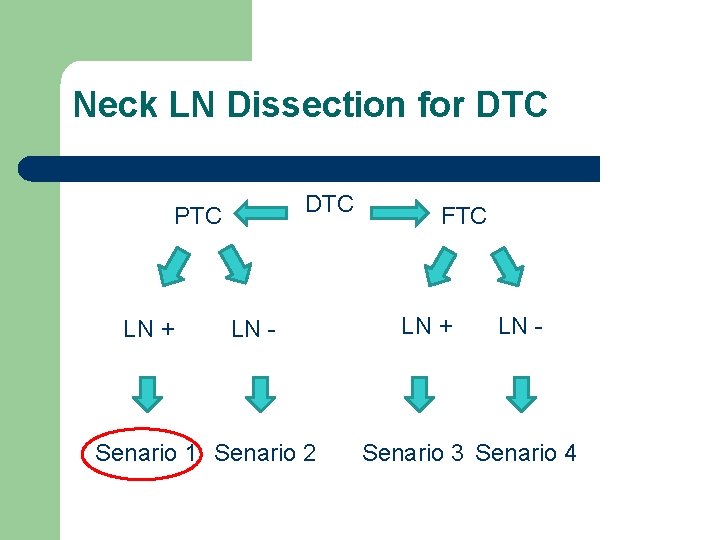
Neck LN Dissection for DTC PTC LN + LN - Senario 1 Senario 2 FTC LN + LN - Senario 3 Senario 4
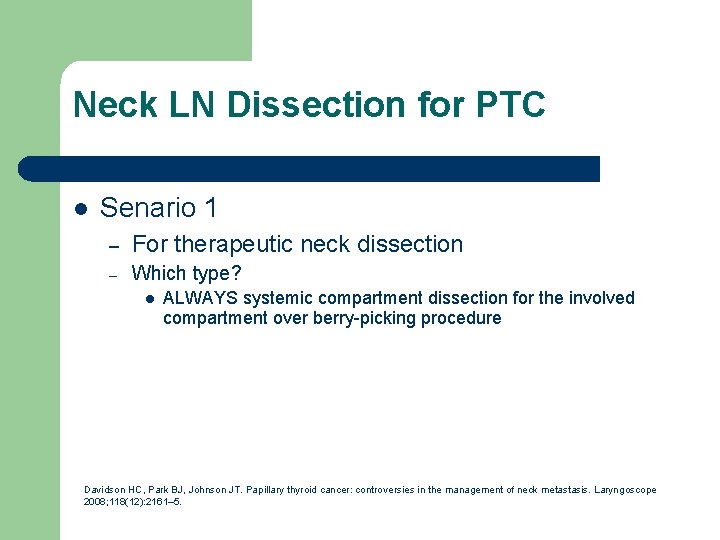
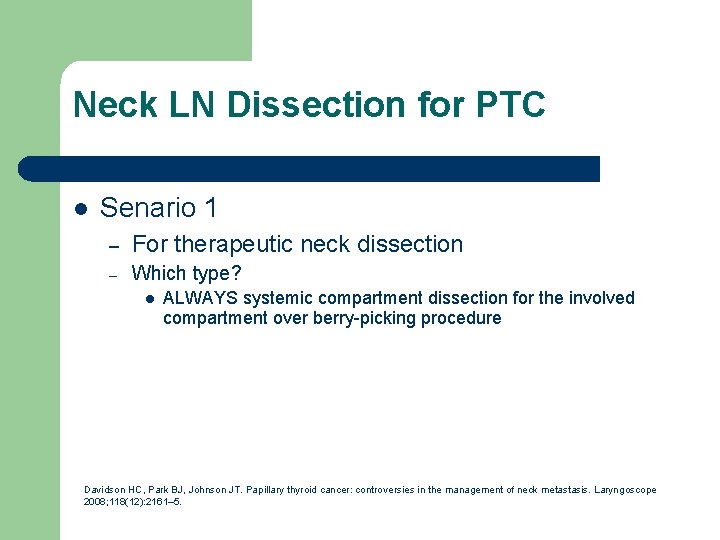
Neck LN Dissection for PTC l Senario 1 – For therapeutic neck dissection – Which type? l ALWAYS systemic compartment dissection for the involved compartment over berry-picking procedure Davidson HC, Park BJ, Johnson JT. Papillary thyroid cancer: controversies in the management of neck metastasis. Laryngoscope 2008; 118(12): 2161– 5.
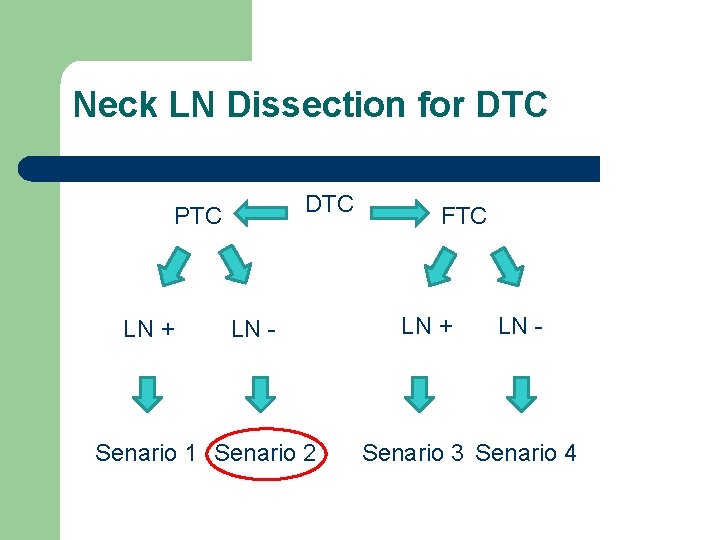
Neck LN Dissection for DTC PTC LN + LN - Senario 1 Senario 2 FTC LN + LN - Senario 3 Senario 4
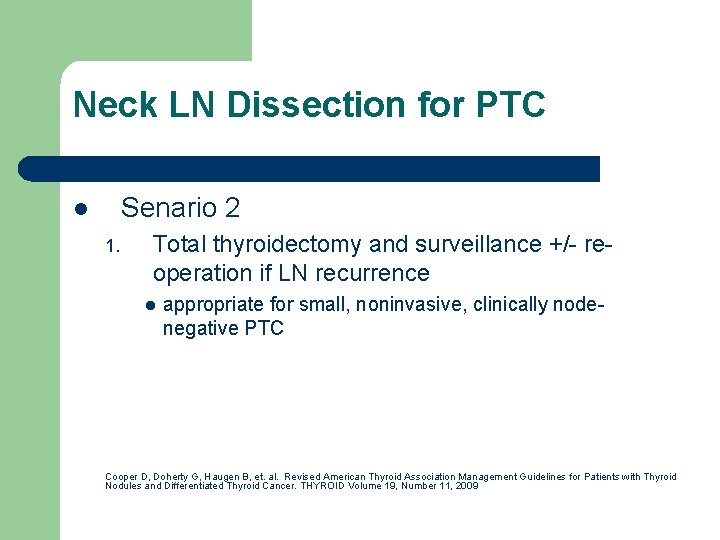
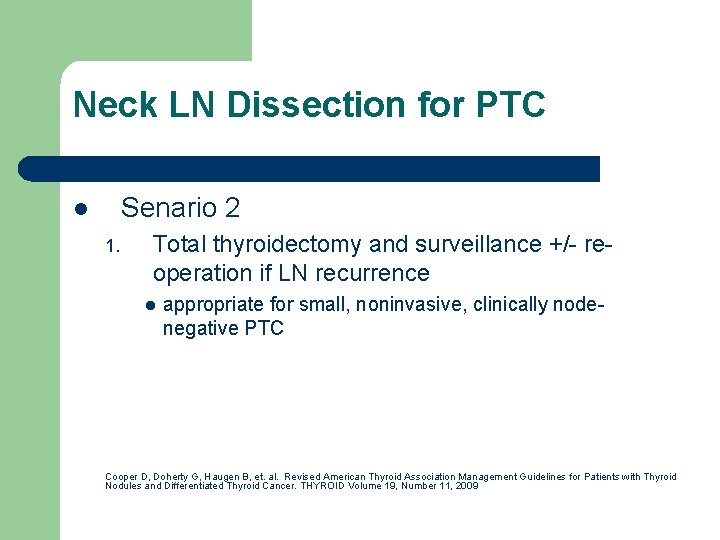
Neck LN Dissection for PTC Senario 2 l 1. Total thyroidectomy and surveillance +/- reoperation if LN recurrence l appropriate for small, noninvasive, clinically nodenegative PTC Cooper D, Doherty G, Haugen B, et. al. Revised American Thyroid Association Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer. THYROID Volume 19, Number 11, 2009
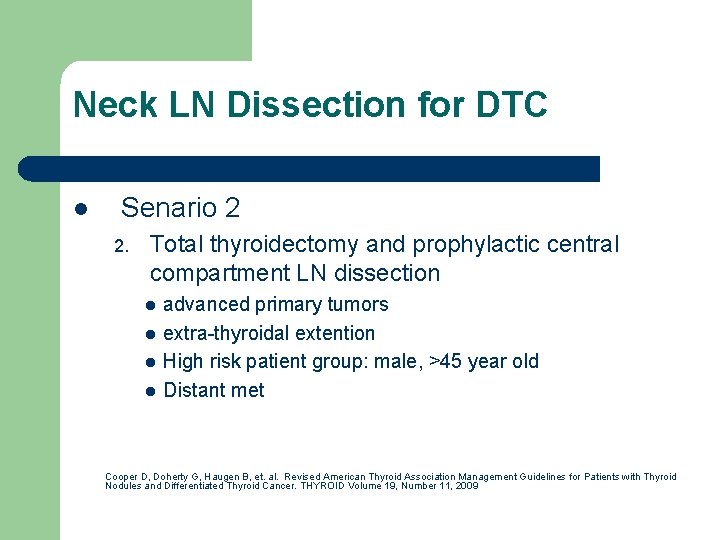
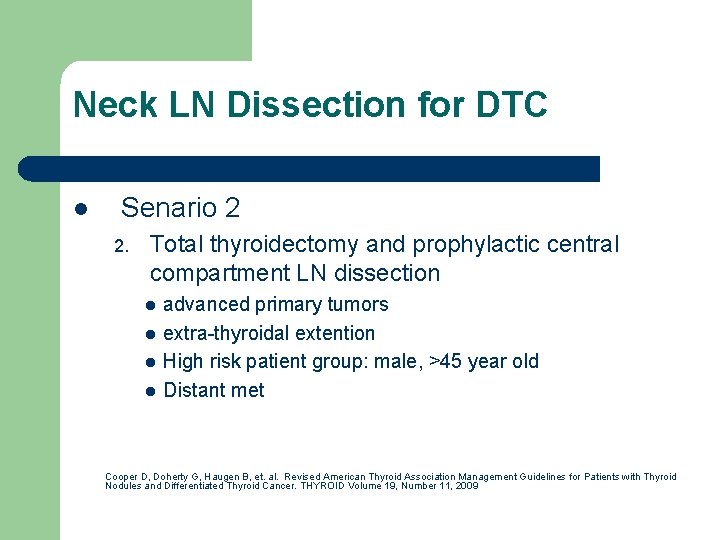
Neck LN Dissection for DTC l Senario 2 2. Total thyroidectomy and prophylactic central compartment LN dissection l l advanced primary tumors extra-thyroidal extention High risk patient group: male, >45 year old Distant met Cooper D, Doherty G, Haugen B, et. al. Revised American Thyroid Association Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer. THYROID Volume 19, Number 11, 2009
Benefits for prophylactic CCLND l l unanticipated central metastases in 38% to 45% of patients with PTC prevents compression or invasion of critical aerodigestive and neural structures decreases lymphatic recurrence low levels of thyroglobulin which may facilitate surveillance for recurrent disease
Drawback for prophylactic CCLND l l Uncertain about effect on overall survival Higher potential surgical complications – – Significantly higher temporary hypo. PTH. When compare with re-op in recurrence patients vs prophylatic CCLND, significantly more permanent RLN palsy. Fritze D, Doherty G. Surgical Management of Cervical Lymph Nodes in Differentiated Thyroid Cancer. Otolaryngol Clin N Am 43 (2010) 285– 300
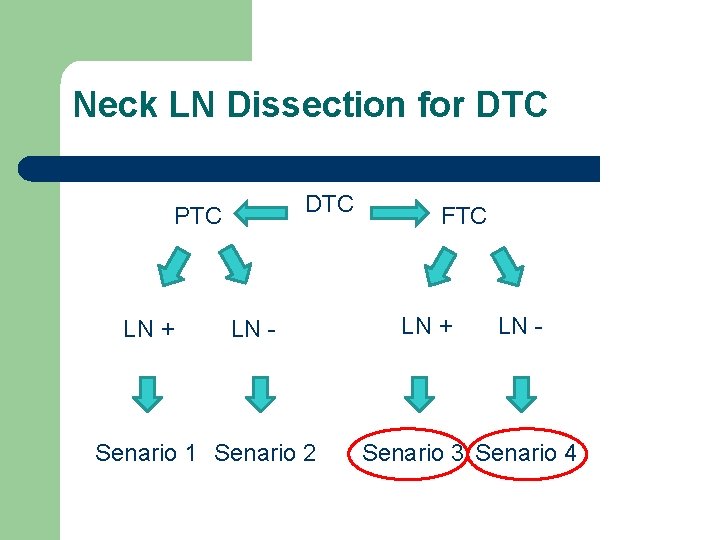
Neck LN Dissection for DTC PTC LN + LN - Senario 1 Senario 2 FTC LN + LN - Senario 3 Senario 4
Neck LN Dissection for FTC? Senario 3 l Therapeutic neck dissection is indicated – Senario 4 l Not for prophylatics neck LN Dissection Observation and re-operate if recurrence – – l as FTC had a lower risk of LN met
Conclusion l PTC – – l Therapeutic systemic functional compartment dissection if LN met is +ve. Prophylactic CCLND in high risk group in expert hands. FTC – – Therapeutic systemic functional compartment dissection if LN met is +ve. NOT for prophylatic neck LN dissection.
The End Questions?