Rheumatoid Arthritis Dr M C du Plooy The














- Slides: 44
Rheumatoid Arthritis Dr M C du Plooy The Wits University DGMC
Introduction - Systemic disease - Progressive inflammatory immune mediated disorder. - Affects articular and extra articular structures - Joints pathology characterised by proliferation of synovial membrane - Chronic destructive polyarthritis
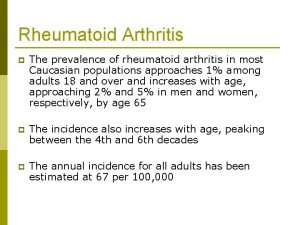
Epidemiology • • • Worldwide distribution Incidence : 4 per 10, 000 Prevalence : 1 -3 % Female : Male ratio - 3: 1 Older age groups - equal Children (UK) prevalence 1 per 1000 Incidence 1 per 10, 000
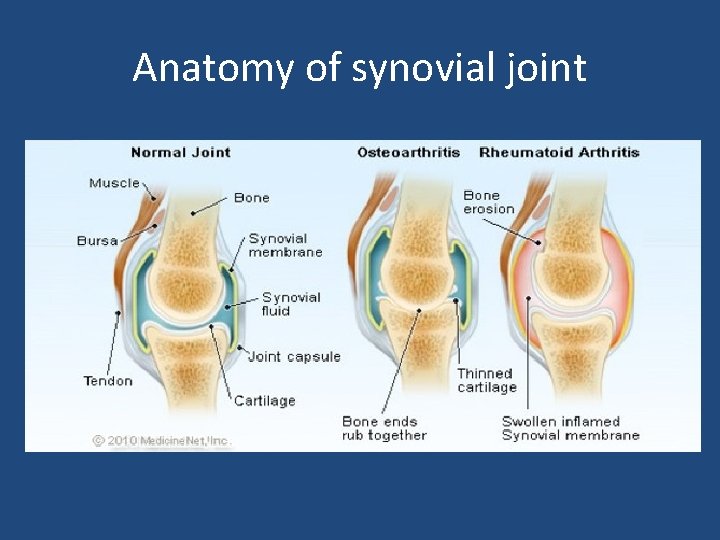
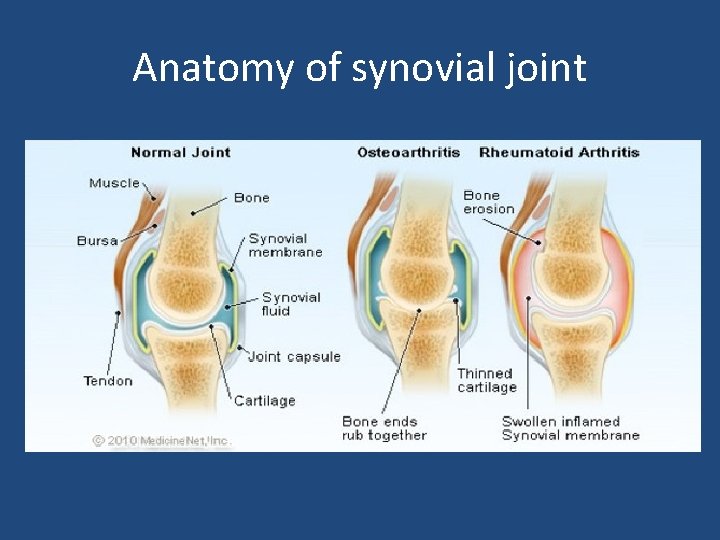
Anatomy of synovial joint
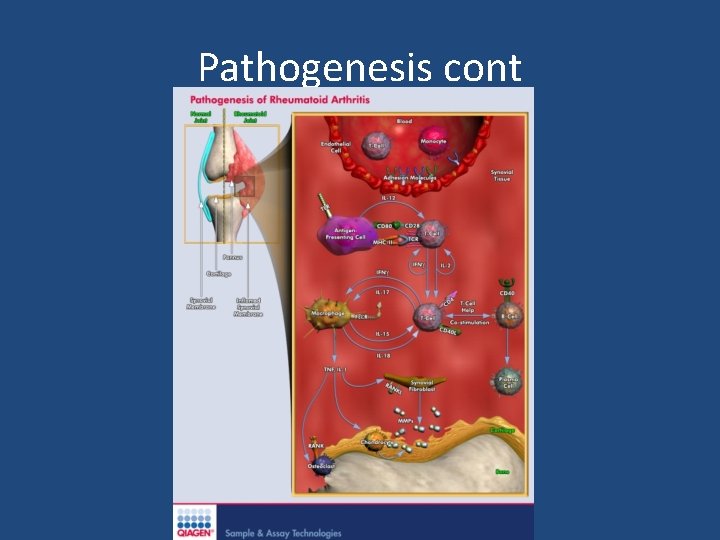
Pathogenesis • Synovial joints affected • Synovial membrane -1 to 3 cells thick • RA- proliferation of synovium - expanding layer of synovial cells - pannus formation ( granulation tissue )
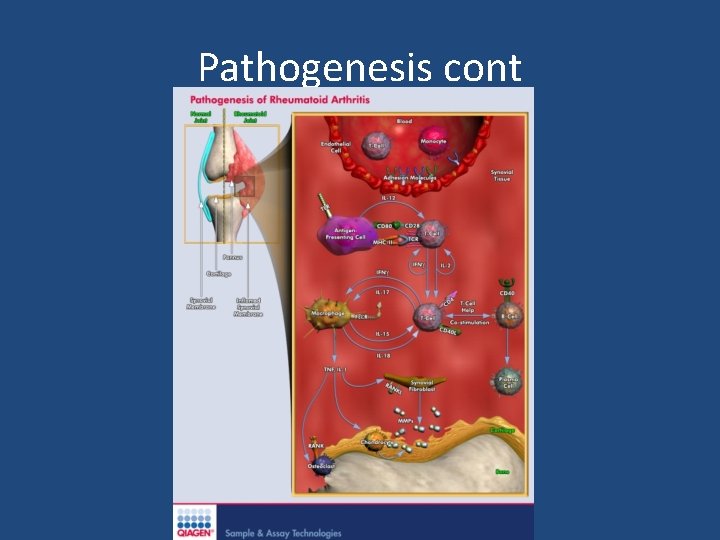
Pathogenesis cont

PANNUS

Clinical Picture Systemic disease • Articular features • Extra articular features
Articular features • Symmetrical • Small joints hands and feet PIPJ MCPJ Wrists • Elbows • Shoulders • Not DIPJ
Articular features cont Lower limbs • • Knees Ankles Midfoot – midtarsal joints Hip Other : • Sternoclacicular joint • TM Joint
Articular features -cont • Cervical Spine esp C 1 and C 2 - radiculopathy - spinal cord involvement • NOT thoracic or lumbar spine • Cricoarytenoid joints : - throat pain - Hoarseness - Stridor

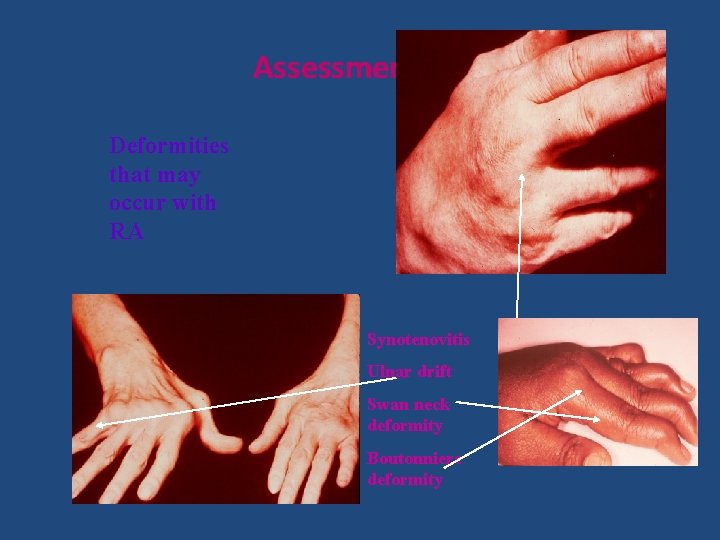
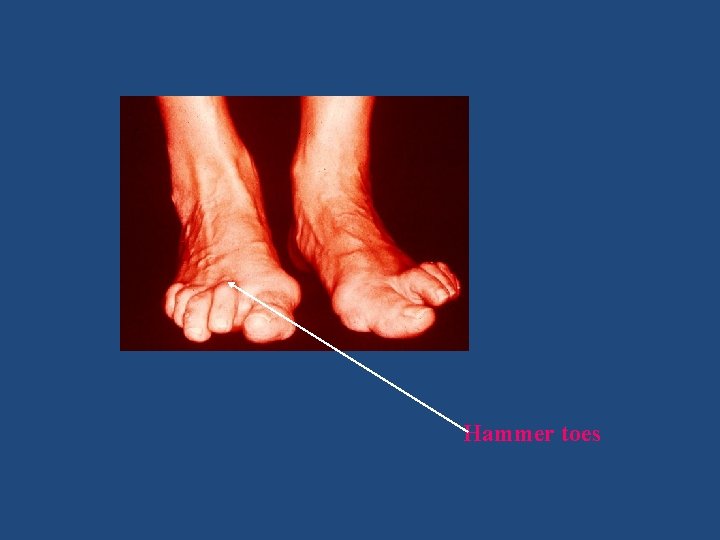
Typical deformities Hands : • Swan neck deformities • Boutonniere • Z deformities thumb • bent fork deformities Feet : • • • Hallux valgus Cock up toes / hammer toes Overriding toes Subluxation of MTPJ Pes planus
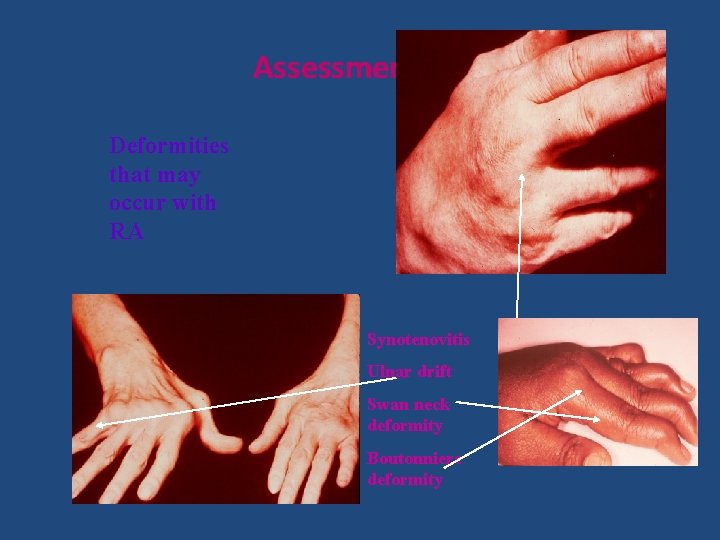
Assessment RA Deformities that may occur with RA Synotenovitis Ulnar drift Swan neck deformity Boutonniere deformity

Subcutaneous nodules (disappear and appear without warning)

Mutlans deformity (rapidly progressing RA) Hitch-hiker thumb Genu valgus
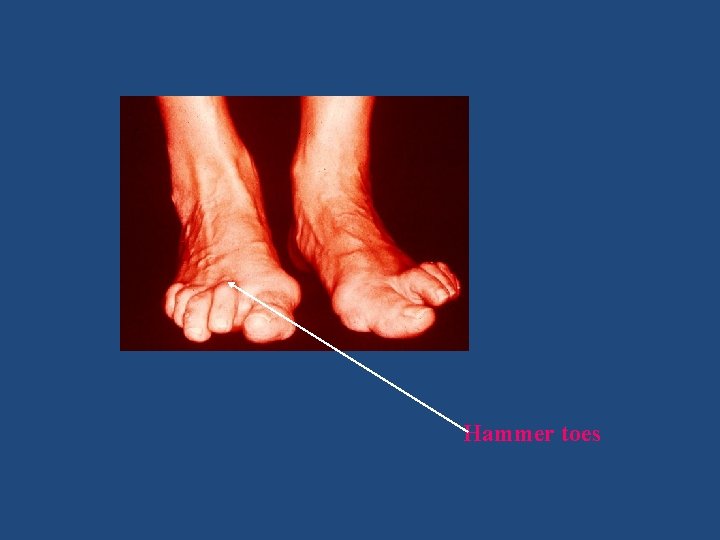
Hammer toes

Extra articular features • Constitutional: - Fever / Weight loss / fatigue • Skin ; - SC Nodules - Vasculitis - Palmar erythema • Pulmonary : - Pleuritis - Pulm nodules - ILD - Bronciolitis obliterans - Pulmonary HPT : ILD / vasculitis of pulmonary vessels
cont • Eyes : - Sjogrens syndrome - Episcleritis - Scleritis - scleromalacia perforans • Haematological: - Anaemia : ACD / Fe deficiency / Folate def - Leucocytosis - Thrombocytosis

cont Renal : - Rarely directly - Amyloidosis or drugs CVS : Increased risk of IHD - Accelerated atherosclerosis - Corticosteroids - Vasculitis Other : MR / AR / TR RA is Independent risk factor for IHD
Cont Vasculitis - Leucocytoclastic vasculitis - Non healing ulcers eg Pyoderma gangrenosa - Neuropathy
cont Nervous system: • Central NS: - brain not affected - spinal cord compression C/Spine • Peripheral NS: - Peripheral neuropathy - Compression neuropathy eg CTS, TTS - Mononeuritis multiples eg wrist or foot drop
COMPLICATIONS MALIGNANCIES: • Increased risk : - Altered immuno surveilance - Immunosuppressive drugs • Types: - NHL - Nonmelanomatous skin cancers • Lower risk: - Breast CA - Colon cancer • ? NSAID Rx
cont INFECTIONS : Increased risk multifactorial : - Activity and severity of RA - GC use - Comorbidities eg DM, CCF - Joint replacement surgery
Investigations Blood tests • • RF Anti CCP ab FBC LFT ESR CRP ANA

Investigations - cont • Imaging : - Xray : hands – AP only C/Spine - Ultrasound - MRI - Bone density • Urine dipstix

Diagnosis • ACR criteria 1987: - EMS > 1 hr Arthritis in > joint areas Small joints : PIPJ / MCPJ /wrists Symmetric Nodules RF and/or Anti CCP positive Xray changes eg typical erosions , PAOP 4/7 present > 6 weeks
Eular –ACR criteria 2010

Subcutaneous nodules (disappear and appear without warning)
Poor prognostic features • • • Smoking Number of swollen joints Socioeconomic status Level of education Lag time from onset sx to diagnosis to initiation of DMARD’s Sustained elevated acute phase reactants Anti CCP positivity High titers of RF and anti CCP ab Genetic background Erosions esp < 2 yrs
Management Non pharmacological : Pharmacological Surgical
Non Pharmacological - Multi disciplinary team • • • OT PT Podiatry Biokinetics Psychologist Social worker
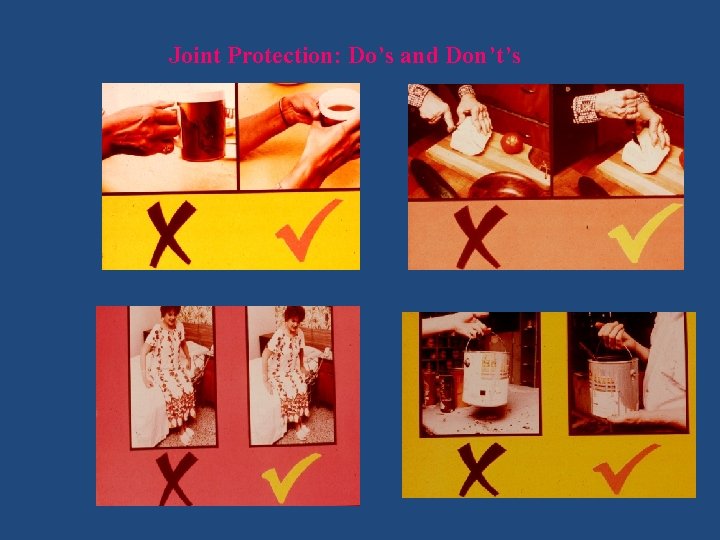
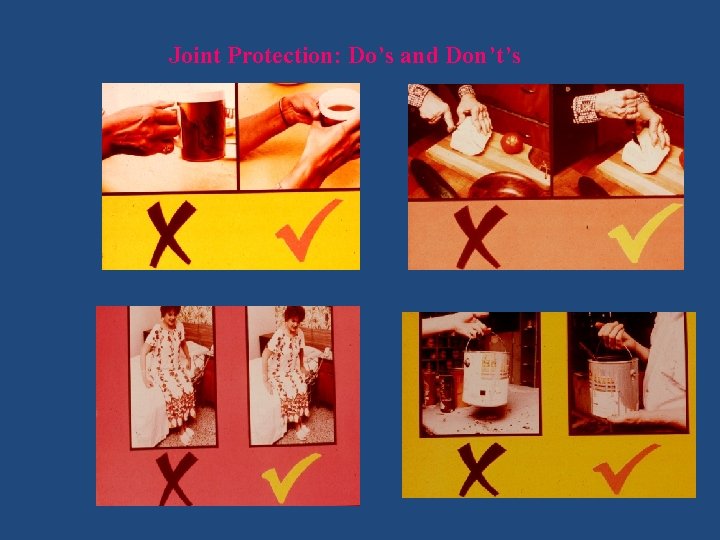
Joint Protection: Do’s and Don’t’s
Management -cont Pharmacological: Pain Relief : - Analgesics : - NSAIDS DMARD’s - Synthetic - Biologic
Mx -cont Synthetic DMARD’s • • • Anti malarials Methotrexate Sulfasalazine Leflunomide Corticosteroids
Mx -cont Biologic DMARD’s: • Cytokine Inhibitors : - Anti –TNF inhibitors : Infliximab; Adalumimab; Etanercept; Golimumab - Anti IL 6 ab ( Actemra ) • T cell co stimulatory pathway modulator: Abatacept – Orencia • B Cell inhibitors Anti CD 20 inhibitor ( Rituximab ) • Intracellular : Small molecules kinase inhibitors eg JAK kinase inhibitors

Management -cont DMARD’s - SLOW ACTING drugs - Explain to patients re A/E - Regular blood tests Corticosteroids: - Bridging period - Beneficial in first 6 months - Vit D and Ca prophylactically with CS > 1/12
Mx -cont • Comorbid diseases: • Depression • Osteoporosis • Traditional risk factors for IHD HPT; Dislipidaemia ; Smoking ; DM
Pregnancy • Which drugs are safe to use ? • • Salazopyrin Hydroxycloroquin Azathioprine Prednisone

Mx - cont Surgical : • • Joint replacement Tenosynovectomy for nerve entrapment Decompression carpal tunnel Corrective arthrotomies of MTJ Stabilisation of C/Spine Tendon release and transfer Arthrodesis of esp ankle joint
Outcome measures • Treat to target : • What is the target ? - Remission (goal) Clinical remission Serological remission Radiographic remission - Low disease activity
cont • How to measure ? Various tools : - SDAI - CDAI - DAS 28 score - HAQ

cont • What parameter to be measured ? • • Duration of EMS Number of tender joints Number of swollen joints Patient global assessment Physicians global assessment Acute phase reactants Ultrasonography
Mortality and Morbidity • Morbidity: Disease of > 10 yrs – 50 -80% unable to work • Mortality: • Causes of death : - IHD - Infections - Fractures with post op complications - Malignancies

THANK YOU
 Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Juvenile rheumatoid arthritis
Juvenile rheumatoid arthritis Haart side effects
Haart side effects Nursing management of gonococcal arthritis
Nursing management of gonococcal arthritis B t cells
B t cells Extra articular manifestations of rheumatoid arthritis
Extra articular manifestations of rheumatoid arthritis Nursing diagnosis for rheumatoid arthritis
Nursing diagnosis for rheumatoid arthritis Pauciarticular juvenile rheumatoid arthritis
Pauciarticular juvenile rheumatoid arthritis Rheumatoid arthritis
Rheumatoid arthritis Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Ra vs oa morning stiffness
Ra vs oa morning stiffness Caplan syndrome
Caplan syndrome Soft tissue rheumatoid arthritis
Soft tissue rheumatoid arthritis Barik meaning
Barik meaning Steinbrocker stage
Steinbrocker stage Rheumatoid factor 10
Rheumatoid factor 10 Anatomi fisiologi asam urat
Anatomi fisiologi asam urat Urethritis reactive arthritis
Urethritis reactive arthritis Viral arthritis
Viral arthritis Reactive arthritis
Reactive arthritis Arthritis foundation indiana
Arthritis foundation indiana Poststreptococcal reactive arthritis
Poststreptococcal reactive arthritis Arthritis in shoulder nhs
Arthritis in shoulder nhs Infusion therapy for arthritis
Infusion therapy for arthritis Septic workup
Septic workup Haemophilus ducreyi culture media
Haemophilus ducreyi culture media Septic arthritis
Septic arthritis Septic arthritis complications
Septic arthritis complications Arthritis and food allergies
Arthritis and food allergies Peripheral arthritis
Peripheral arthritis Acute gout attack treatment
Acute gout attack treatment Septic arthritis complications
Septic arthritis complications Eular recommendations psoriatic arthritis
Eular recommendations psoriatic arthritis Rehaklinik psoriasis arthritis
Rehaklinik psoriasis arthritis Arthritis treatment
Arthritis treatment Coccobacilli
Coccobacilli Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Septic arthritis antibiotics
Septic arthritis antibiotics Psoriasis arthritis nhs
Psoriasis arthritis nhs Kode icd 10 fraktur vertebra thorakal
Kode icd 10 fraktur vertebra thorakal Seronegative arthritis
Seronegative arthritis Caprine arthritis encefalitis
Caprine arthritis encefalitis Septic arthritis gonorrhea
Septic arthritis gonorrhea Narbentypen
Narbentypen Reactive arthritis pathophysiology
Reactive arthritis pathophysiology