Chapter 1 EMS Systems National EMS Education Standard









- Slides: 79
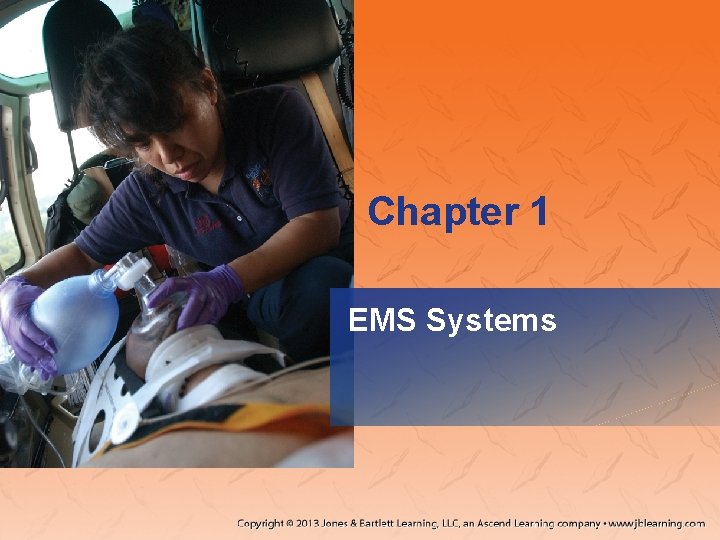
Chapter 1 EMS Systems
National EMS Education Standard Competencies Preparatory Integrates comprehensive knowledge of the EMS system, safety/well-being of the paramedic, and medical/legal and ethical issues, which is intended to improve the health of EMS personnel, patients, and the community.
National EMS Education Standard Competencies Emergency Medical Services (EMS) Systems – EMS systems – History of EMS – Roles/responsibilities/professionalism of EMS personnel – Quality improvement – Patient safety
National EMS Education Standard Competencies Research – Impact of research on emergency medical responder (EMR) care – Data collection – Evidence-based decision making – Research principles to interpret literature and advocate evidence-based practice
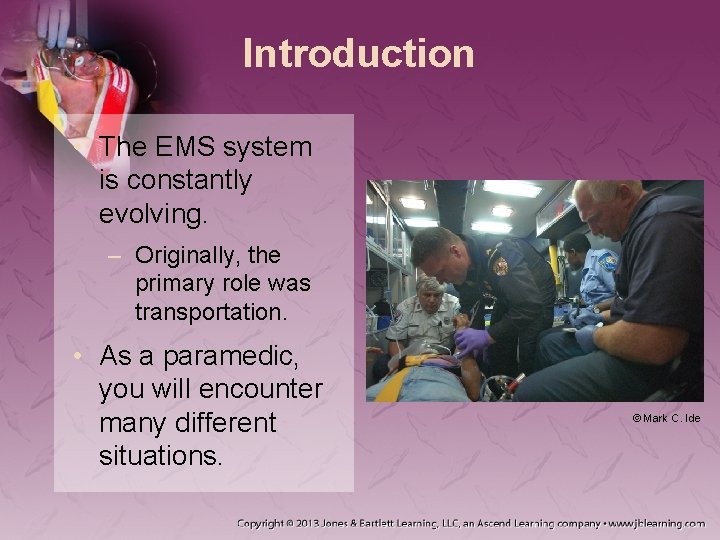
Introduction • The EMS system is constantly evolving. – Originally, the primary role was transportation. • As a paramedic, you will encounter many different situations. © Mark C. Ide
Introduction • The public’s perception of you is based on: – TV and articles – Your treatment of their loved ones • Continued education is a must. • Treat everyone with respect and dignity.
The History of EMS • 1485 – First use of an ambulance – Transport only • 1800 s – First use of ambulance/ attendant to care for injuries on site • 1926 – Service started similar to present day • 1940 s – EMS turned over to fire and police departments – No standards set
© National Library of Medicine The 20 th Century and Modern Technology • EMS made major strides after WWII. – Bringing hospital to field gave patients a better chance for survival – Korean War • First use of a helicopter • M*A*S*H units
The 20 th Century and Modern Technology • 1956 – Mouth-to-mouth resuscitation developed • Late 1950 s/early 1960 s – Focus shifted to bringing hospital to patients – MICUs developed
The 20 th Century and Modern Technology • 1965: “The White Paper” released – Findings included: • Lack of uniform laws and standards • Poor-quality equipment • Lack of communication • Lack of training
The 20 th Century and Modern Technology • “The White Paper” findings outlined 10 critical points for EMS system – Led to National Highway Safety Act – Created US Department of Transportation • 1968 – Training standards implemented – 9 -1 -1 created
The 20 th Century and Modern Technology • 1969 – First true paramedic program – Standards for ambulance design and equipment • 1970 s – NREMT began Courtesy of Eugene L. Nagel and the Miami Fire Department
The 20 th Century and Modern Technology • 1970 s (cont’d) – 1971: Emergency Care and Transportation of the Sick and Injured published by the AAOS – 1973: Emergency Medical Services System Act – 1977: First National Standard Curriculum for Paramedics developed by US DOT
The 20 th Century and Modern Technology • 1980 s/1990 s – Number of trained personnel grew – NHTSA developed 10 system elements to help sustain EMS system – Responsibility for EMS transferred to the states – Major legislative initiatives

Licensure, Certification, and Registration • Certification examination: – Ensures all health care providers have the same basic level of knowledge and skill – Once you pass certification you can apply for state licensure.
Licensure, Certification, and Registration • Licensure: – How states control who practices – Also known as certification or credentialing – Unlawful to practice without licensure • Holding a license shows you: – Completed initial education – Met the requirements to achieve the license • Paramedics are required to receive medical direction.

Licensure, Certification, and Registration • You may be required to be registered and licensed. – Board of registration holds your: • Education records • State or local licensure • Recertification

Licensure, Certification, and Registration • Reciprocity – Certification granted from another state/agency – Requirements: • Hold a current state certification. • Be in good standing. • National Registry certification.
The EMS System • A complex network of coordinated services that provides care to the community • The public needs to be taught how to: • Recognize emergencies. • Activate the EMS system. • Provide basic care.
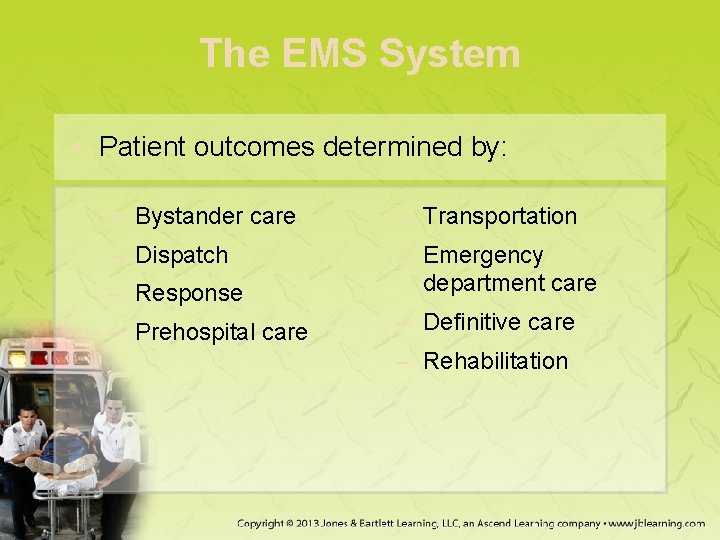
The EMS System • Patient outcomes determined by: – Bystander care – Transportation – Dispatch – Response – Emergency department care – Prehospital care – Definitive care – Rehabilitation

The EMS System • Dispatchers – Usually the public’s first contact – Training level varies by state • Scene may differ from what dispatcher relays
The EMS System • As a paramedic, you must: – Develop care plan – Decide on transport method – Determine receiving facility – Be active in your community.
Levels of Education • EMS system functions from a federal to local level – Federal: National EMS Scope of Practice Model – State: Licensure – Local: Medical director decides day-to-day limits
Levels of Education • The national guidelines designed to create more consistent delivery of EMS nationally – Medical director can only limit scope of practice • 2009: National EMS Education Standards – NREMT provides a national standard for testing and certification
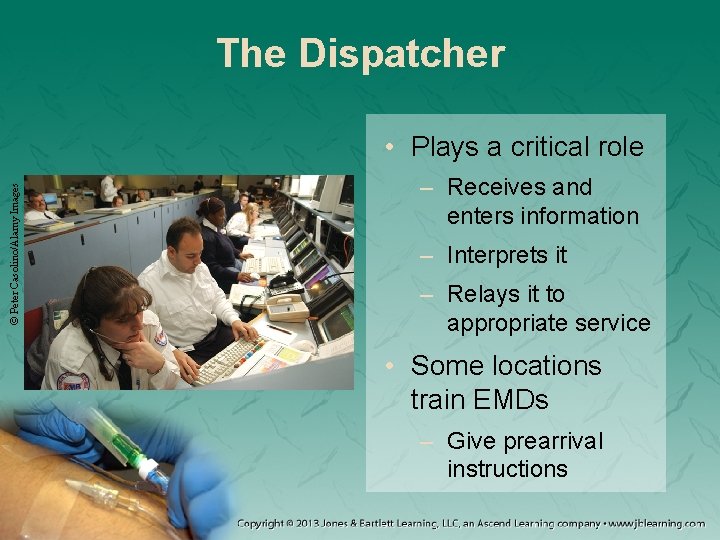
The Dispatcher © Peter Casolino/Alamy Images • Plays a critical role – Receives and enters information – Interprets it – Relays it to appropriate service • Some locations train EMDs – Give prearrival instructions
Emergency Medical Responder (EMR) • Formerly “first responder” • Requirements vary by state • Should be able to: – Recognize seriousness of condition. – Provide basic care. – Relay information. © Matt Dunham/AP Photosages
EMT © Amanda Herron, The Jackson Sun/AP Photos • Formerly EMT-B • Primary provider level in many EMS systems • EMT certification precedes paramedic education • Most populous level in the system
Advanced EMT (AEMT) • Formerly EMT-I • Initially developed in 1985 – Major revision in 1999 • Trained in: • More advanced pathophysiology • Some advanced procedures
Paramedic • Highest level to be nationally certified – 1999: Major revisions to curriculum greatly increased level of training and skills • Even if independently licensed, you must: – Function under guidance of physicians. – Be affiliated with a paramedic-level service.
Paramedic Education • Initial education – Most states base education programs on the National EMS Education Standards. • Outline minimum knowledge needed for practice – States require varying hours of education. • National average: 1, 000 -1, 500 hours
Paramedic Education • Continuing education – Most states require proof of hours. – Attend conferences and seminars. – Read EMS journals. – Get everyone involved in postrun critiques. • The responsibility for continuing education rests with you.
Additional Types of Transports • Specialty center – Require in-house staffs of specialists – Transport time can be slightly longer. – Know: • Location of centers • Protocol for direct transport • Interfacility – Use for: • Nonambulatory patients • Patients who require medical monitoring – Other medical professionals may accompany patient.
Working With Other Professionals • Hospital staff – Become familiar with the hospital. – You may consult with staff by using the radio through established procedures. – The best patient care occurs when emergency care providers have close rapport.
Working With Other Professionals • Public safety agents – Some have EMS training • Can better perform certain functions than you © Mark C. Ide – Interagency cooperation benefits patient
Working With Other Professionals • Continuity of care – The community has expectations of EMS – Focus on prevention – You will interact with many professional groups • Understand your role, as well as theirs.
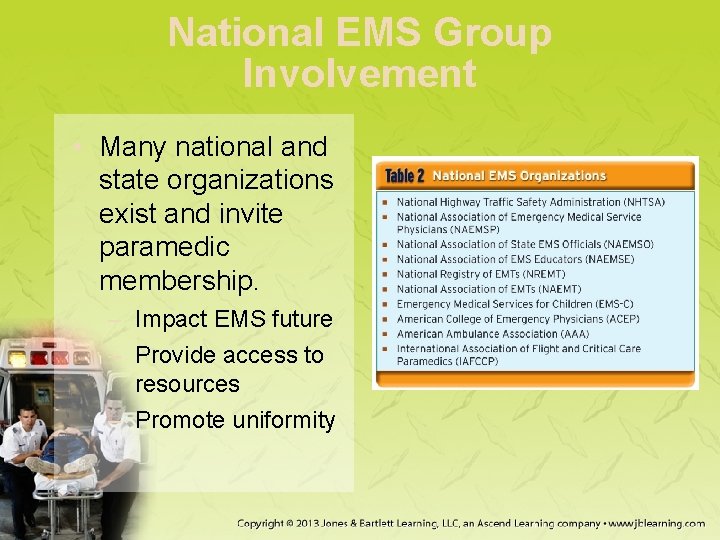
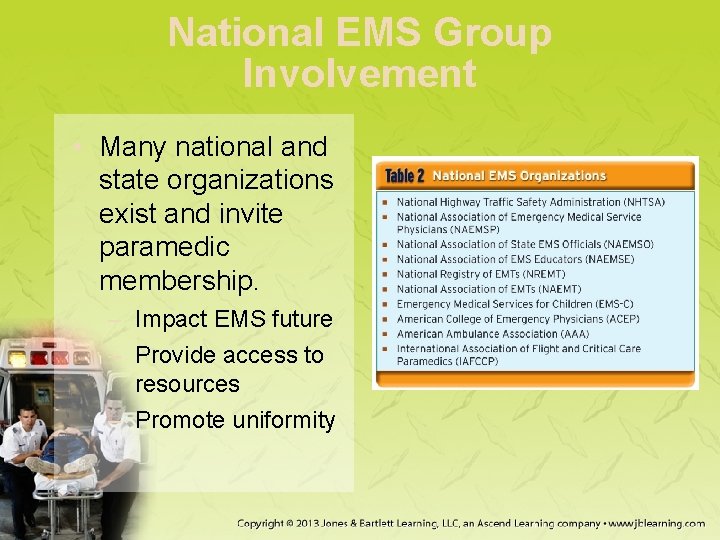
National EMS Group Involvement • Many national and state organizations exist and invite paramedic membership. – Impact EMS future – Provide access to resources – Promote uniformity

Professionalism • You have responsibilities as a health care professional. • You will be measured by: – Standards, competencies, and education requirements – Performance parameters – Code of ethics

Professionalism • You are in a highly visible role in your community. • You must: – Instill confidence. – Establish and maintain credibility. – Show concern for your patients.
Professionalism • Your appearance is of utmost importance. – Has more impact than you may think • Present a professional image and treat colleagues with respect. – Arguing with colleagues is inappropriate. – Raise issues at the appropriate time and place.

Professionalism • Attributes of professionalism: – Integrity – Empathy – Self-motivation • Have an internal drive for excellence – Confidence • Strive to be the best paramedic you can. – Communications • Express and exchange ideas, thoughts, findings • Listen well. • Documentation is important.
Professionalism • Attributes of professionalism (cont’d): – Teamwork and respect • Work together – Patient advocacy • Act in the patient’s best interest – Injury prevention – Careful delivery of service • Deliver the highestquality care – Time management • Prioritize your patient’s needs – Administration
Professionalism • More health care locations are using paramedic services, including: – Administering vaccinations – Serving as home health nurses – Performing special transports
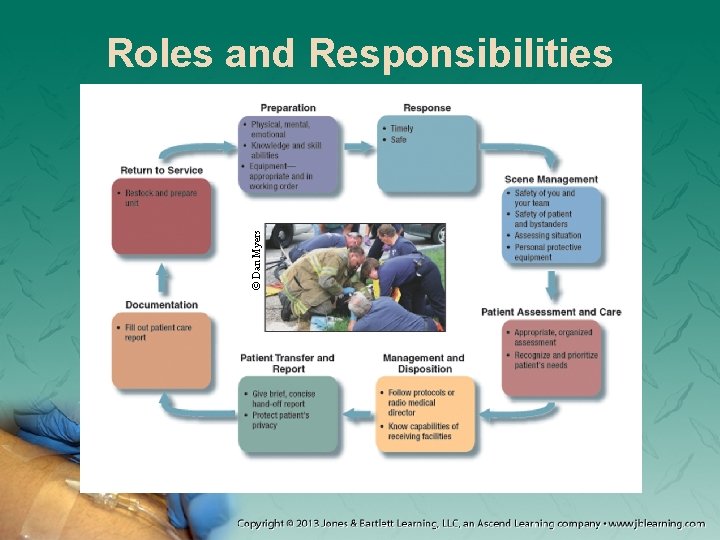
© Dan Myers Roles and Responsibilities
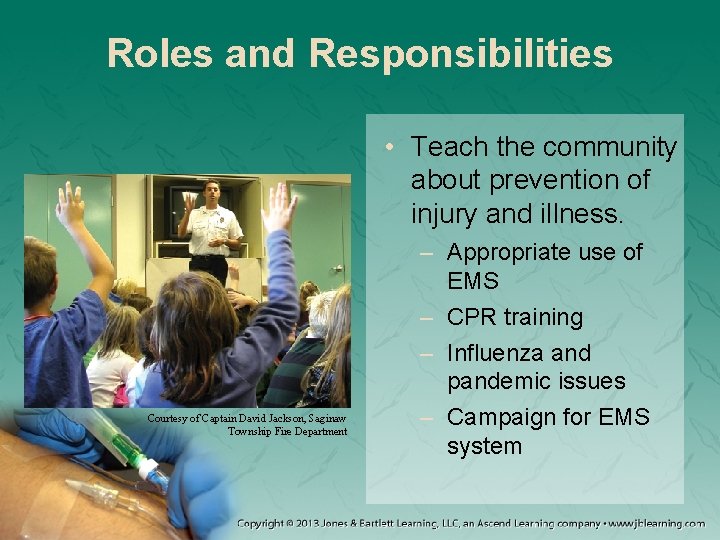
Roles and Responsibilities • Teach the community about prevention of injury and illness. Courtesy of Captain David Jackson, Saginaw Township Fire Department – Appropriate use of EMS – CPR training – Influenza and pandemic issues – Campaign for EMS system
Medical Direction • Paramedics carry out advanced skills – Must take direction from medical directors • Medical directors may perform many roles: – Educate and train – Recommend new personnel or equipment – Develop protocols, guidelines, and quality improvement programs
Medical Direction • Roles of the medical director (cont’d): – – Provide input for patient care Interface between EMS and other agencies Advocate for EMS Serve as “medical conscience”
Medical Direction • Medical directors also provide online and off -line medical control. • Online – Provides immediate and specific patient care resources – Allows for continuous quality improvement – Can render on-scene assistance • Offline – Allows for the development of: • Protocols or guidelines • Standing orders • Procedures • Training
Improving System Quality • Continuous quality improvement (CQI) – Tool to continually evaluate care – Quality control – Process of assessing current practices, looking for ways to improve – Dynamic process
Improving System Quality • Review ambulance runs when possible. • Focus of CQI is improving care • CQI can be a peer review. – Be professional – Should be a constructive process
Improving System Quality • CQI programs help prevent problems by: – Evaluating day-today operations – Identifying possible stress points • Look for ways to eliminate human error. – Ensure adequate lighting – Limit interruptions – Store medications properly
Improving System Quality • Ways to eliminate human error (cont’d) – Be careful when handing patients off. – Three main sources of errors: • Rules-based failure • Knowledge-based failure • Skills-based failure
Improving System Quality • Ways to eliminate human error (cont’d) – – – Agencies need clear protocols. Be aware of your environment. Ask yourself “Why am I doing this? ” Use cheat sheets. Be conscientious of protocols.
EMS Research • EMS has been drawn toward evidencebased practice. – Protocols should be based on scientific findings. • Research should be performed by properly educated researchers. – More education centers now offer an EMS track.

The Research Process • Identify problem, procedure, or question. • Develop research agenda by specifying: – Questions to be answered – Methods to gather data • Stick to the research agenda.
The Research Process • Determine the research domain. – Area of research – Domains: clinical, systems, or education • Research may be performed within a research consortium.
Funding • Researchers should use an IRB when a project begins. • All research requires funding. – Any type of support is considered funding. • Researchers must: – Disclose sources of funding. – Maintain transparency of research methods.
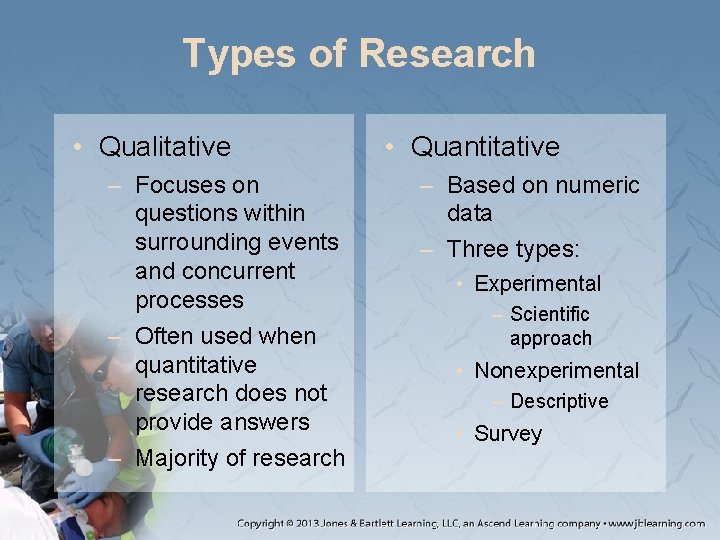
Types of Research • Qualitative – Focuses on questions within surrounding events and concurrent processes – Often used when quantitative research does not provide answers – Majority of research • Quantitative – Based on numeric data – Three types: • Experimental – Scientific approach • Nonexperimental – Descriptive • Survey
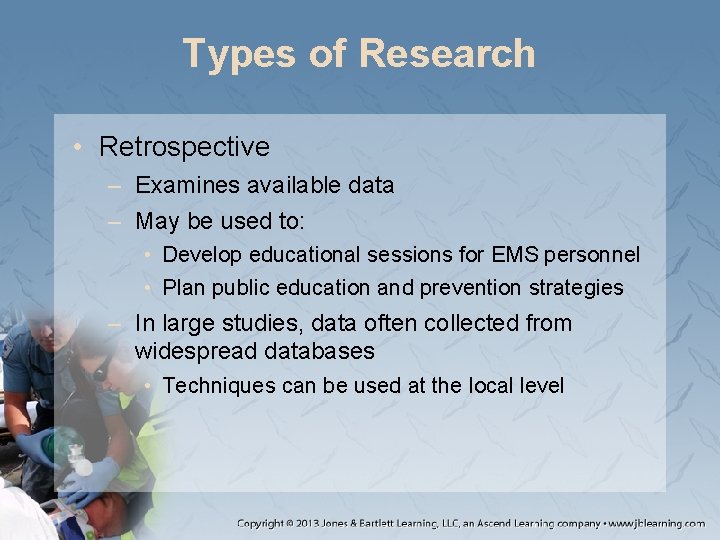
Types of Research • Retrospective – Examines available data – May be used to: • Develop educational sessions for EMS personnel • Plan public education and prevention strategies – In large studies, data often collected from widespread databases • Techniques can be used at the local level

Types of Research • Other types of research: – – – Prospective Cohort Case study Cross-sectional design Longitudinal design Literature review
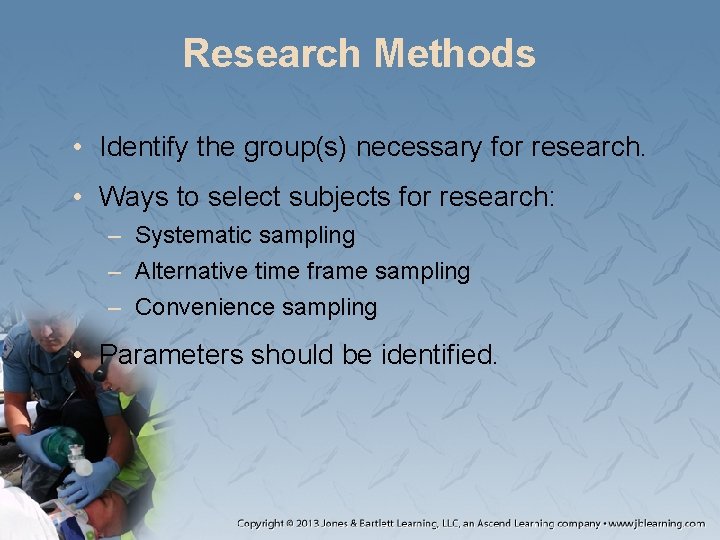
Research Methods • Identify the group(s) necessary for research. • Ways to select subjects for research: – Systematic sampling – Alternative time frame sampling – Convenience sampling • Parameters should be identified.
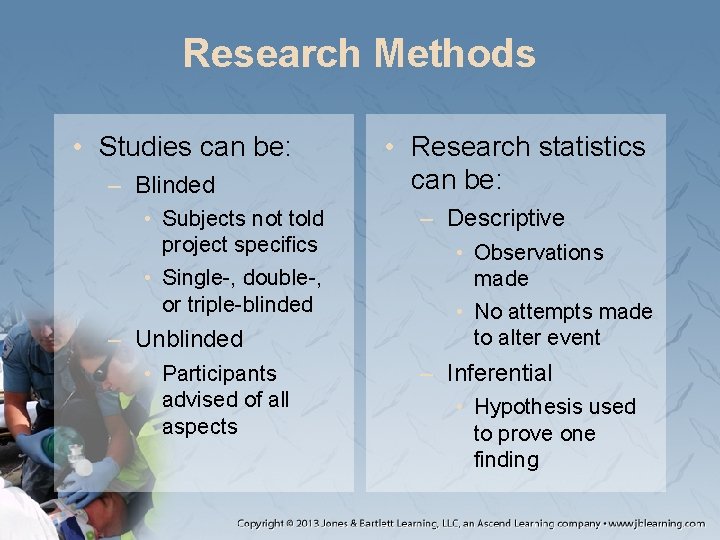
Research Methods • Studies can be: – Blinded • Subjects not told project specifics • Single-, double-, or triple-blinded – Unblinded • Participants advised of all aspects • Research statistics can be: – Descriptive • Observations made • No attempts made to alter event – Inferential • Hypothesis used to prove one finding
Ethical Considerations • The IRB monitors whether a study is conducted ethically and ensures: – Protection of participants – Appropriate conduct • Benefits must outweigh risks. • Conflicts of interest must be identified.
Ethical Considerations • All subjects must: – Give consent. – Know their rights will be protected. – Participate voluntarily. – Be informed of all potential risks. – Be free to withdraw at any time.
Evaluating Medical Research • When evaluating research, look for certain criteria to determine the research quality. – Know what questions to answer. • Read every part of the research. • Consider the type of journal.
Evaluating Medical Research • Peer review helps ensure quality. – Subject-matter experts review material prior to publication • Internet sites can be valid tools. • Studies must follow a structured process. • There will always be limitations.
Evidence-Based Practice • Care should focus on procedures that have proven useful in improving patient outcomes. – Evidence-based practice will have a growing role in EMS. • Stay up to date on health care advances. – Make sure you understand new research results.
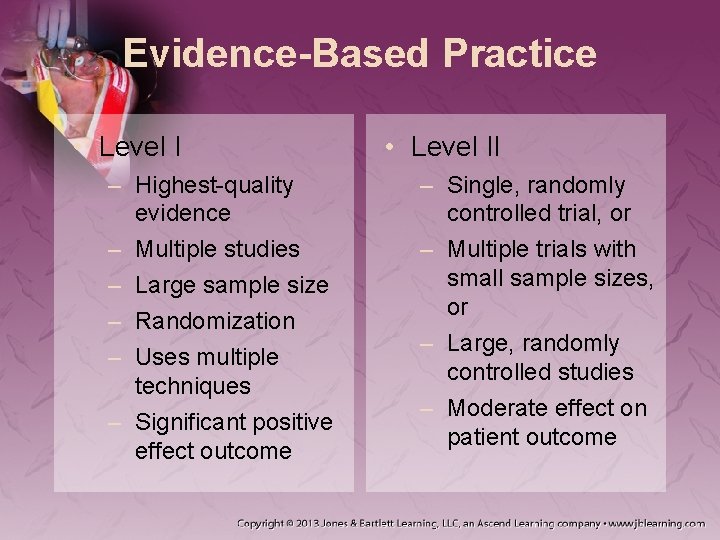
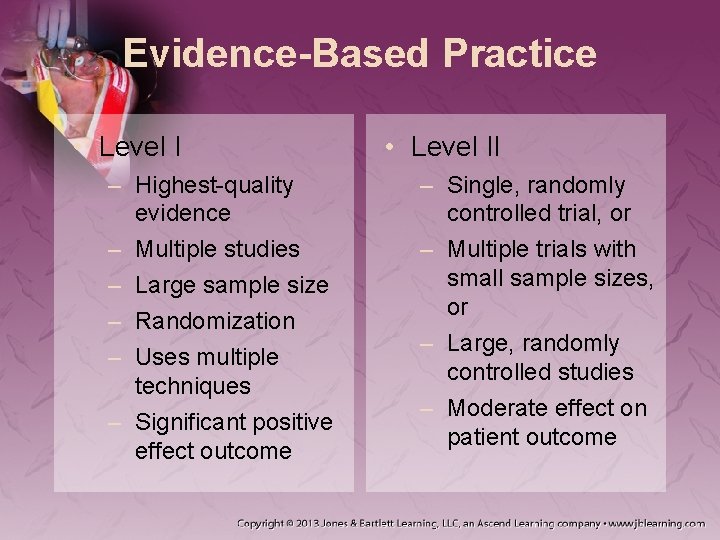
Evidence-Based Practice • Level I – Highest-quality evidence – Multiple studies – Large sample size – Randomization – Uses multiple techniques – Significant positive effect outcome • Level II – Single, randomly controlled trial, or – Multiple trials with small sample sizes, or – Large, randomly controlled studies – Moderate effect on patient outcome
Evidence-Based Practice • Level III – Level IIIA: Well-designed trial without randomization – Level IIIB: Evidence from causal comparison and case or cohort studies – Level IIIC: Evidence gathered from single experiments
Evidence-Based Practice • Level IV – Lowest level – Reviews of: • Descriptive studies • Expert opinion • Uncontrolled studies
Evidence-Based Practice • Research determines the effectiveness of treatment. – Can help identify which procedures, medications, and treatments do and do not work • When following a new study, measure the results with your CQI program.
Summary • Ambulance corps were developed during World Wars I and II to transport and rapidly care for soldiers. • Helicopters were used to rapidly remove soldiers from the battlefield during the Korean and Vietnam Wars.
Summary • In 1966 the National Academy of Science and the National Research Council released “The White Paper” outlining 10 points. – The National Highway Safety Act and the US Department of Transportation were created as a result. • Paramedics must be licensed (also known as certification or credentialing) before performing any functions.
Summary • Standards for prehospital emergency care, and the people who provide it, are regulated under state law by a state office of EMS. • There are four levels of training: emergency medical responder, emergency medical technician, advanced emergency medical technician, and paramedic. • Paramedics may be involved in interfacility transports and transports to specialty centers.
Summary • Paramedics should be familiar with the roles and responsibilities of other health care providers and public safety agencies. • Continuing education programs expose paramedics to new research findings and refresh their skills and knowledge. • A physician medical director authorizes EMS providers to provide care in the field through off-line or online medical direction.
Summary • There are expected standards and a code of ethics for all paramedics. • There are many professional attributes that a paramedic is expected to have, including but not limited to integrity, empathy, teamwork, patient advocacy, and time management skills.
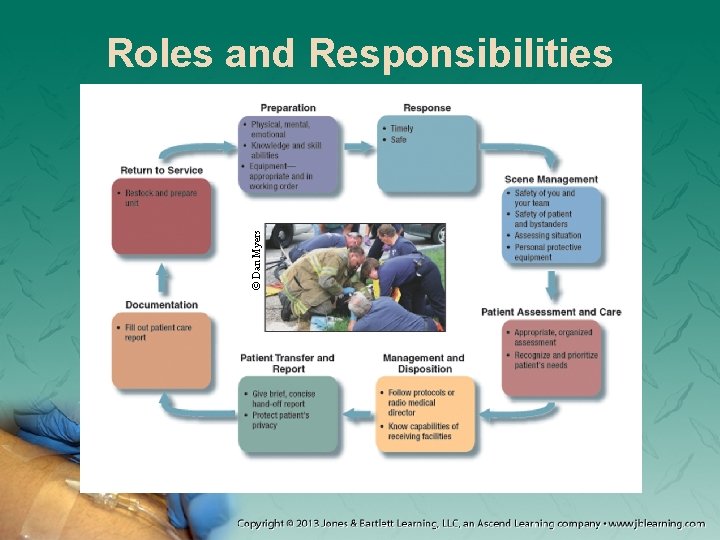
Summary • Some of the primary paramedic responsibilities include preparation, response, scene management, patient assessment and care, management and disposition, patient transfer and report, documentation, and return to service. • Paramedics evaluate their care through quality control and continuous quality improvement.
Summary • Research establishes a consensus of what EMS personnel should or should not do. Research may be quantitative or qualitative. • There are many ethical considerations when conducting research. Researchers must always obtain consent from subjects, inform them of the research parameters, and protect their rights and welfare.
Summary • Paramedics should know how to evaluate the quality of research, including how to recognize peer-reviewed literature and how to find quality research on the Internet. • Review medical literature as it becomes available, and stay up to date on changing guidelines.
Credits • Chapter opener: © Mark C. Ide • Backgrounds: Purple – Courtesy of Rhonda Beck; Green – Jones & Bartlett Learning; Blue – Courtesy of Rhonda Beck; Lime – © Photodisc • Unless otherwise indicated, all photographs and illustrations are under copyright of Jones & Bartlett Learning, courtesy of Maryland Institute for Emergency Medical Services Systems, or have been provided by the American Academy of Orthopaedic Surgeons. • ,