Definition n n Jugular Venous Pulse defined as

- Slides: 32
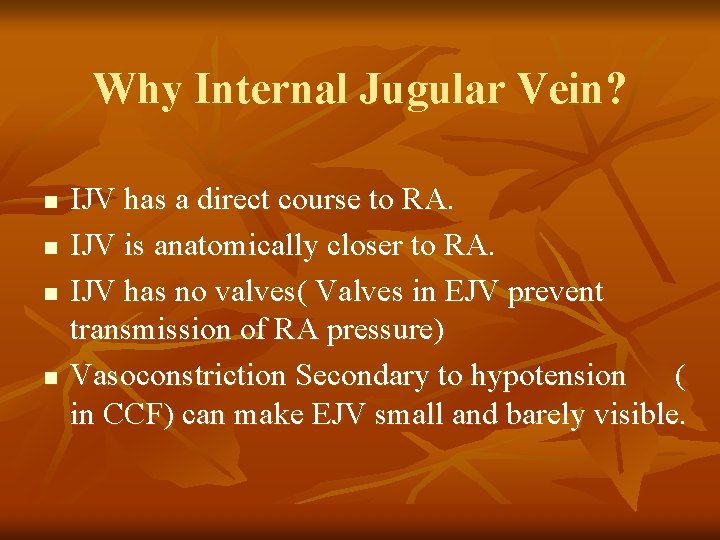
Definition n n Jugular Venous Pulse: defined as the oscillating top of vertical column of blood in right IJV that reflects pressure changes in Right Atrium in cardiac cycle. Jugular Venous Pressure: Vertical height of oscillating column of blood.
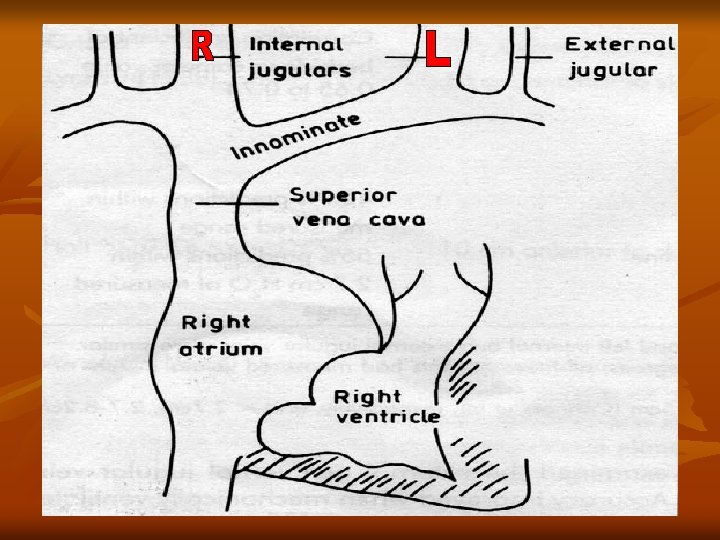
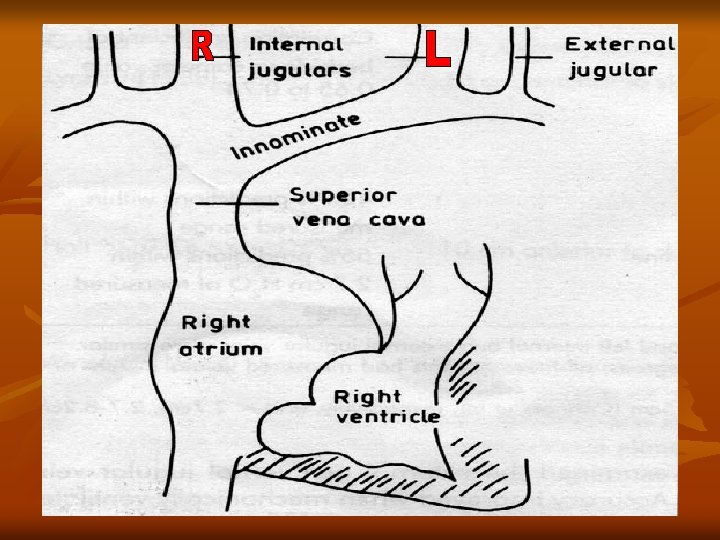
Why Internal Jugular Vein? n n IJV has a direct course to RA. IJV is anatomically closer to RA. IJV has no valves( Valves in EJV prevent transmission of RA pressure) Vasoconstriction Secondary to hypotension ( in CCF) can make EJV small and barely visible.
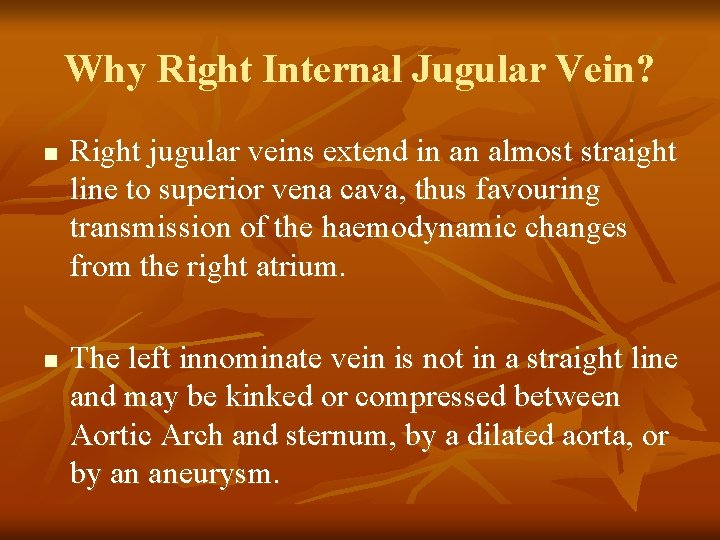
Why Right Internal Jugular Vein? n n Right jugular veins extend in an almost straight line to superior vena cava, thus favouring transmission of the haemodynamic changes from the right atrium. The left innominate vein is not in a straight line and may be kinked or compressed between Aortic Arch and sternum, by a dilated aorta, or by an aneurysm.
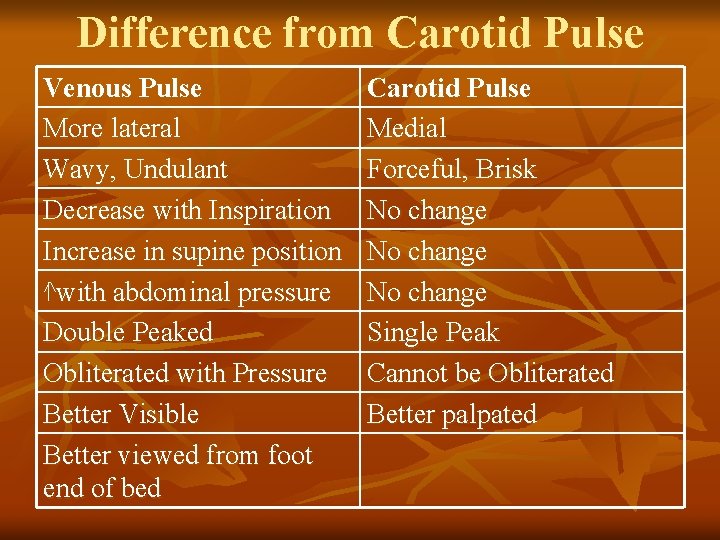
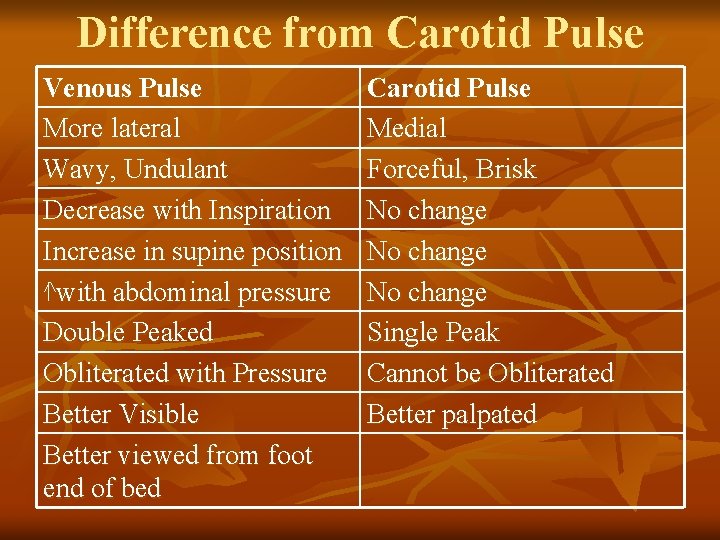
Difference from Carotid Pulse Venous Pulse More lateral Wavy, Undulant Decrease with Inspiration Increase in supine position ^with abdominal pressure Double Peaked Obliterated with Pressure Better Visible Better viewed from foot end of bed Carotid Pulse Medial Forceful, Brisk No change Single Peak Cannot be Obliterated Better palpated
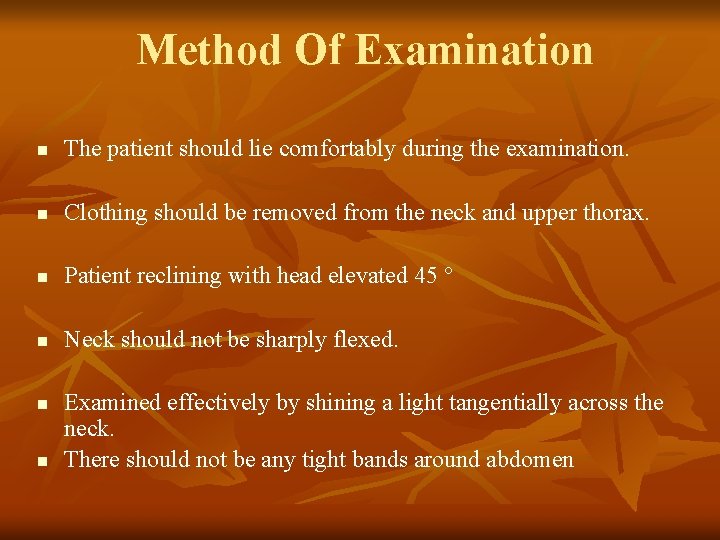
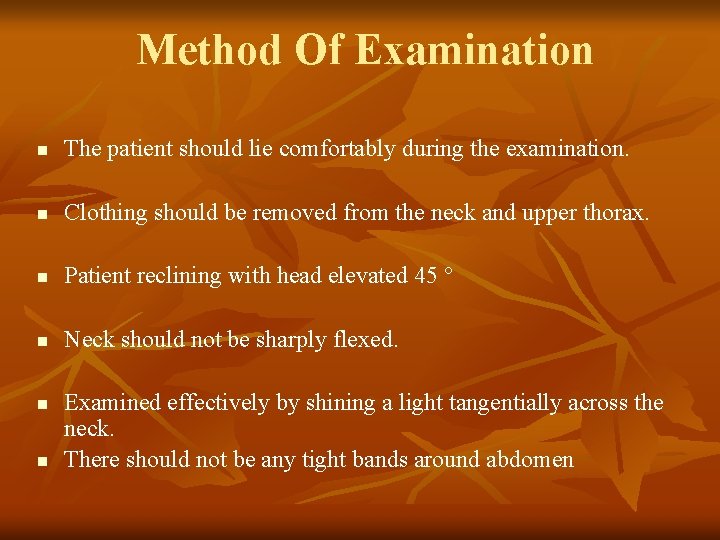
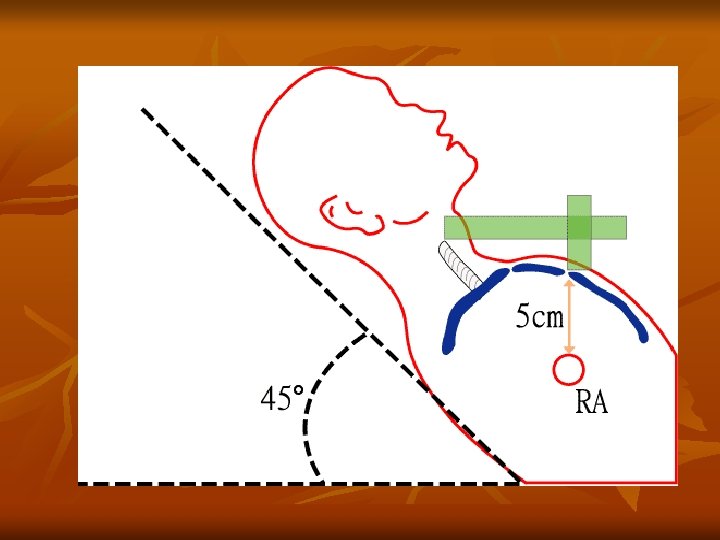
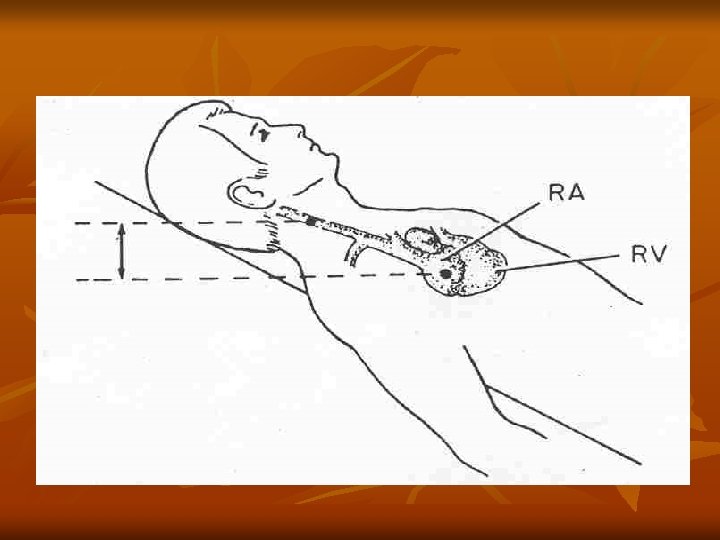
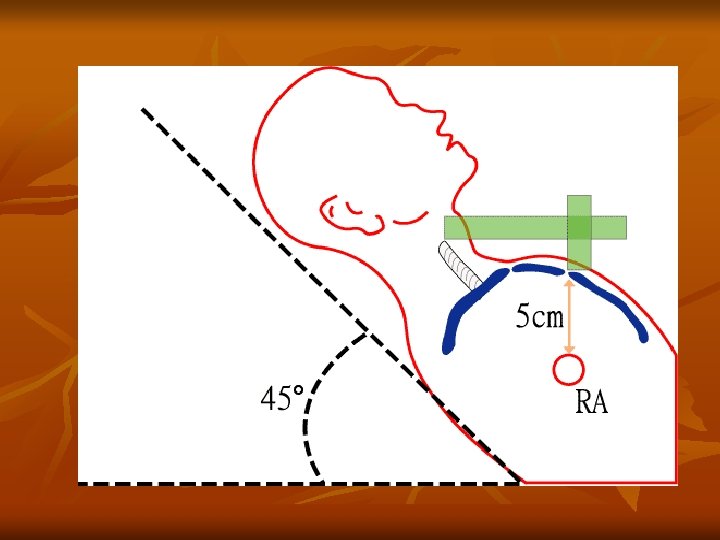
Method Of Examination n The patient should lie comfortably during the examination. n Clothing should be removed from the neck and upper thorax. n Patient reclining with head elevated 45 ° n Neck should not be sharply flexed. n n Examined effectively by shining a light tangentially across the neck. There should not be any tight bands around abdomen
Observations Made n the level of venous pressure. n the type of venous wave pattern.
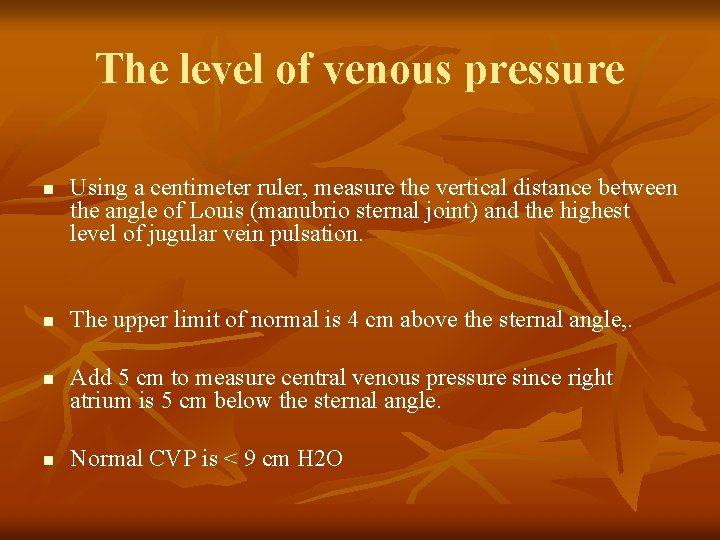
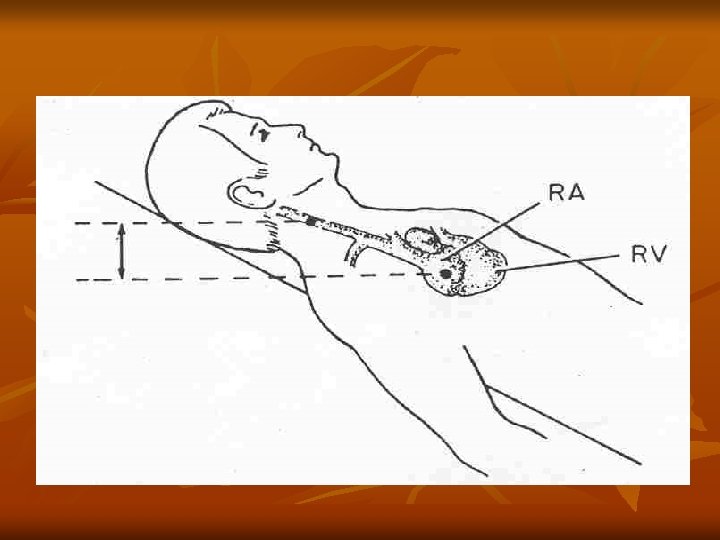
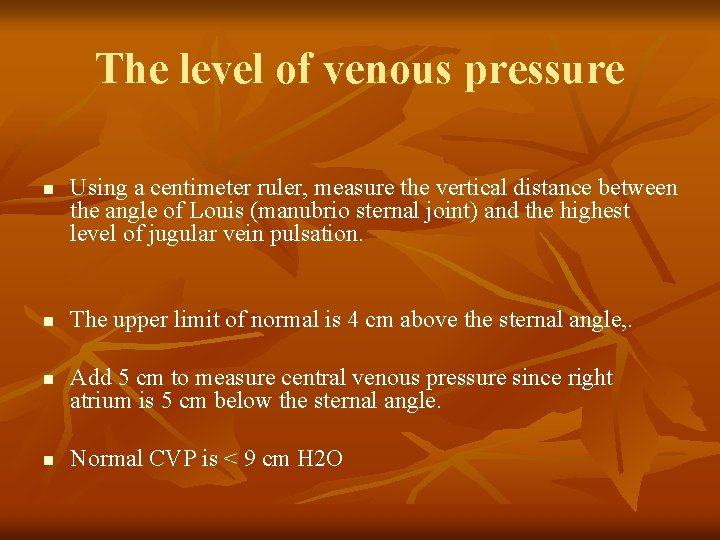
The level of venous pressure n n Using a centimeter ruler, measure the vertical distance between the angle of Louis (manubrio sternal joint) and the highest level of jugular vein pulsation. The upper limit of normal is 4 cm above the sternal angle, . Add 5 cm to measure central venous pressure since right atrium is 5 cm below the sternal angle. Normal CVP is < 9 cm H 2 O
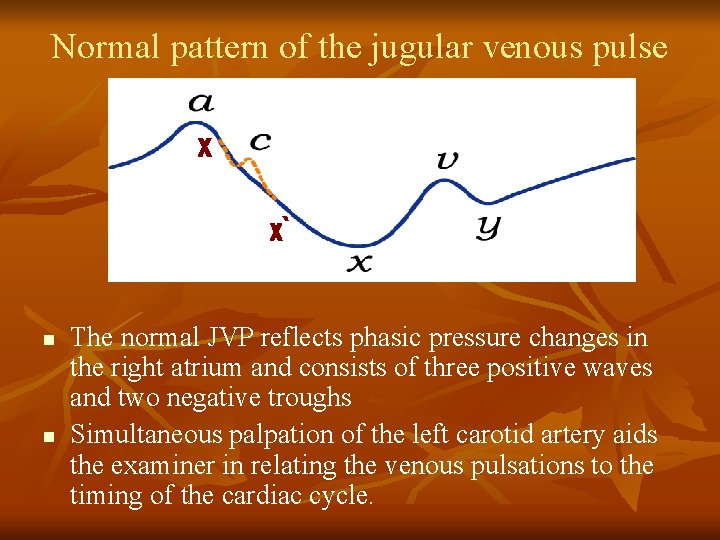
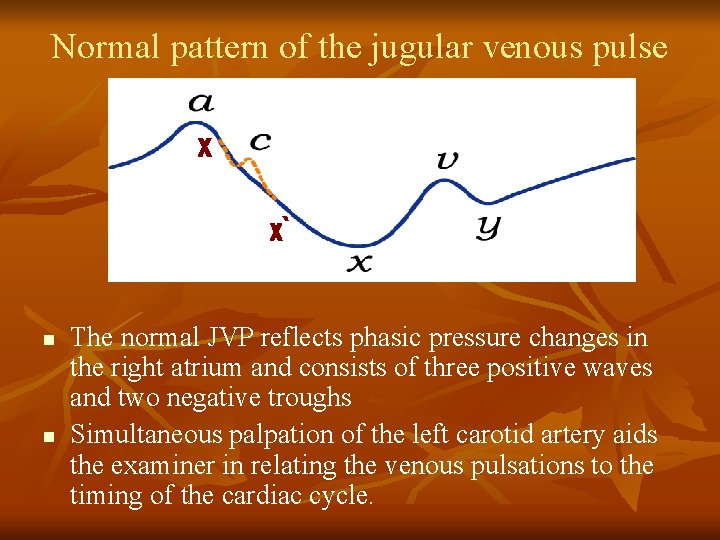
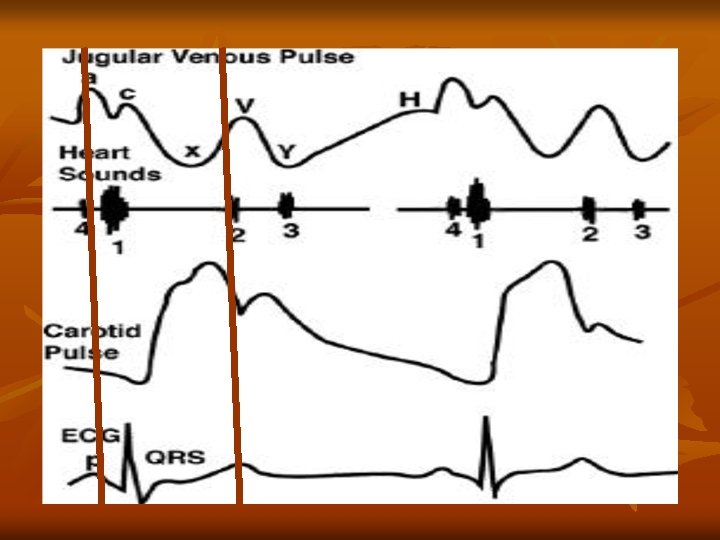
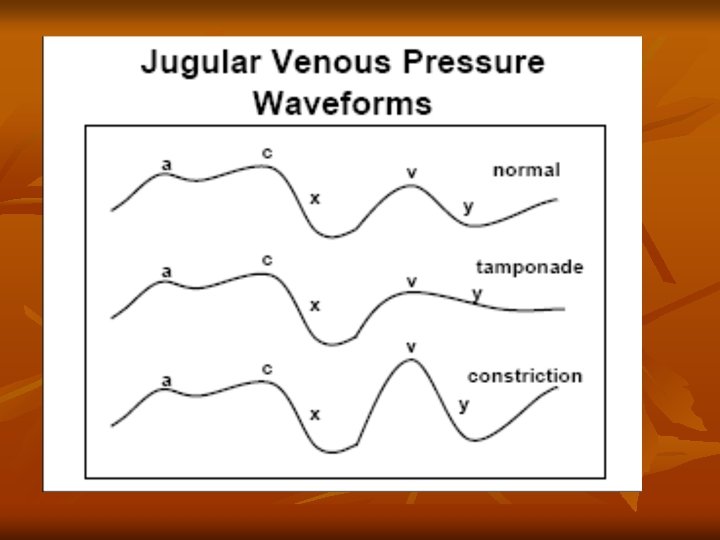
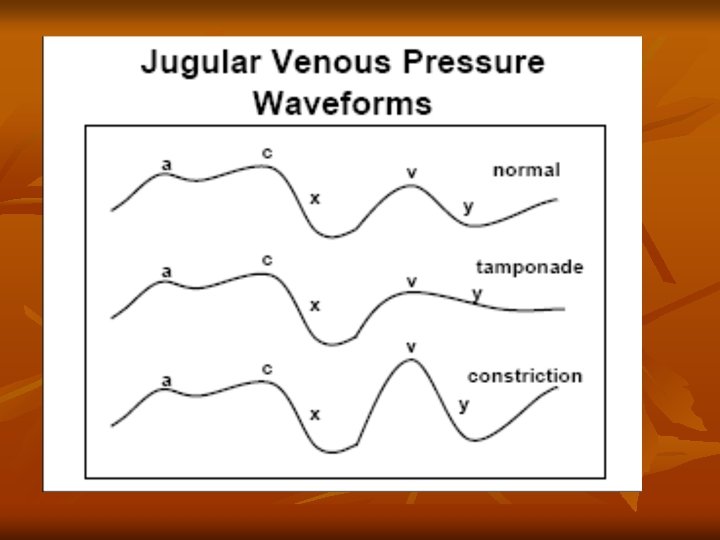
Normal pattern of the jugular venous pulse n n The normal JVP reflects phasic pressure changes in the right atrium and consists of three positive waves and two negative troughs Simultaneous palpation of the left carotid artery aids the examiner in relating the venous pulsations to the timing of the cardiac cycle.
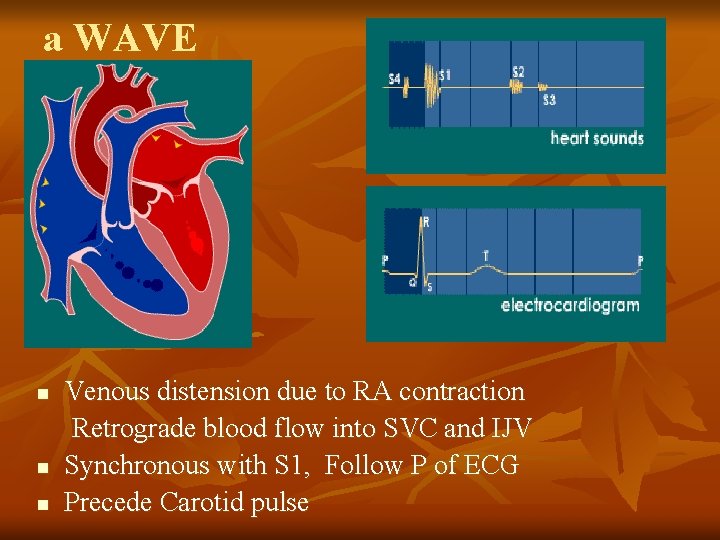
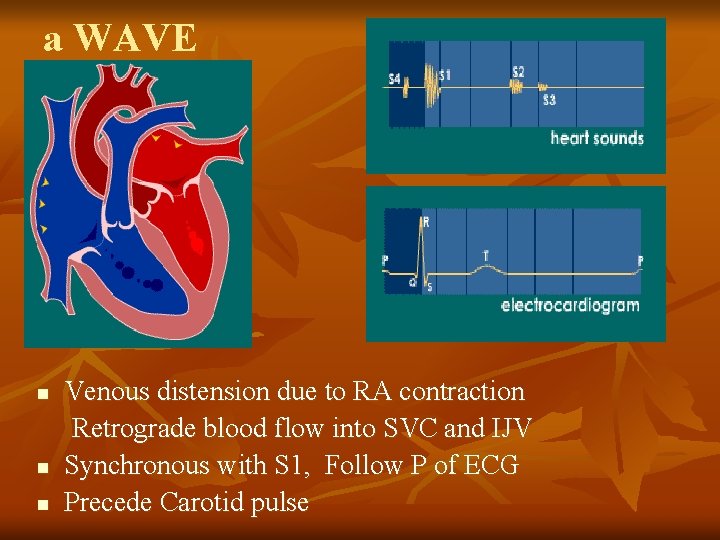
a WAVE n n n Venous distension due to RA contraction Retrograde blood flow into SVC and IJV Synchronous with S 1, Follow P of ECG Precede Carotid pulse
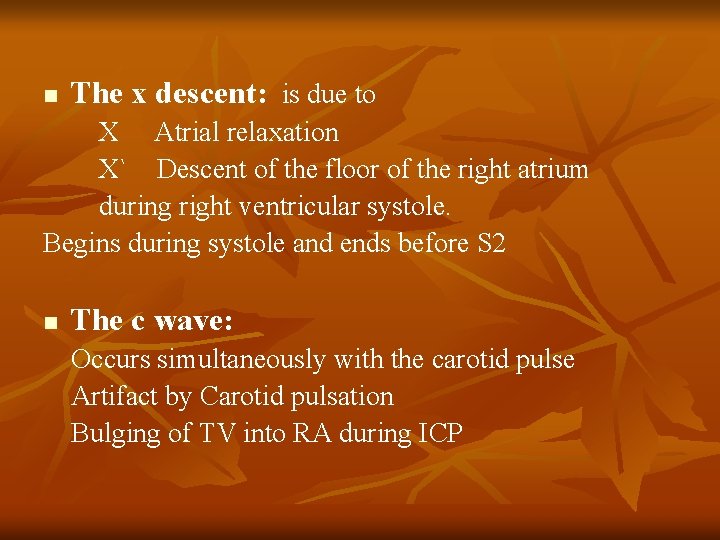
n The x descent: is due to X Atrial relaxation X` Descent of the floor of the right atrium during right ventricular systole. Begins during systole and ends before S 2 n The c wave: Occurs simultaneously with the carotid pulse Artifact by Carotid pulsation Bulging of TV into RA during ICP
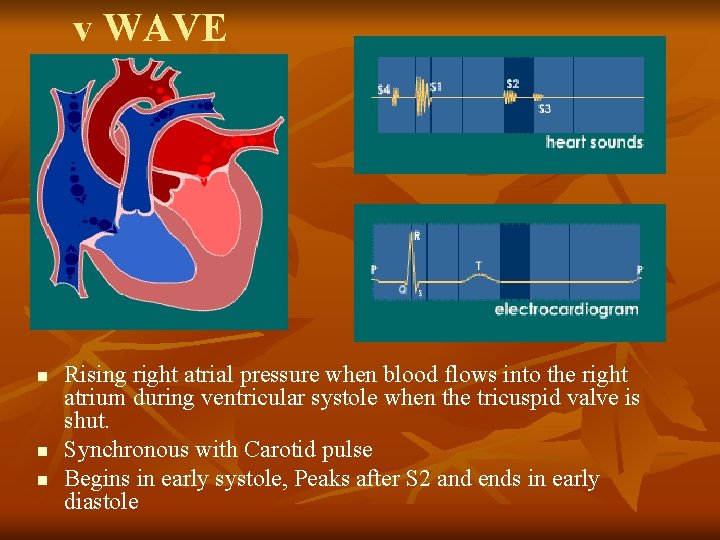
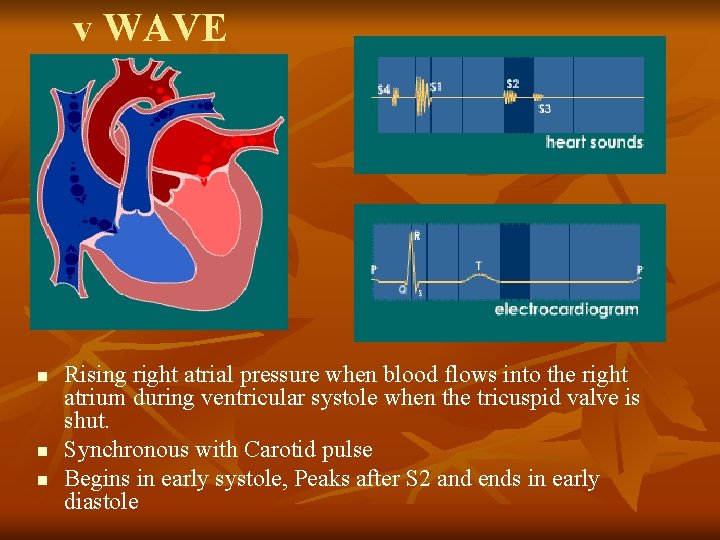
v WAVE n n n Rising right atrial pressure when blood flows into the right atrium during ventricular systole when the tricuspid valve is shut. Synchronous with Carotid pulse Begins in early systole, Peaks after S 2 and ends in early diastole
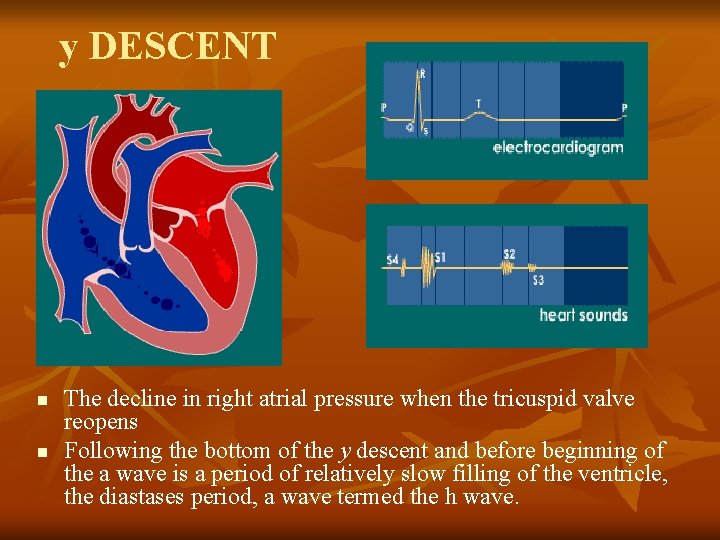
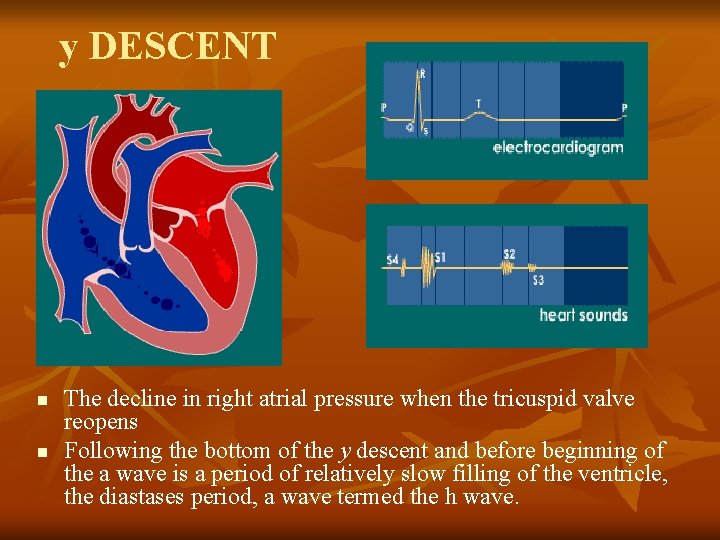
y DESCENT n n The decline in right atrial pressure when the tricuspid valve reopens Following the bottom of the y descent and before beginning of the a wave is a period of relatively slow filling of the ventricle, the diastases period, a wave termed the h wave.
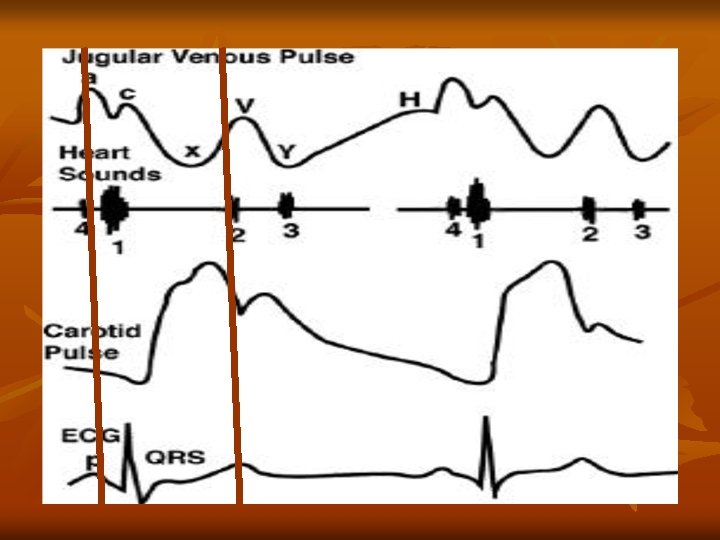
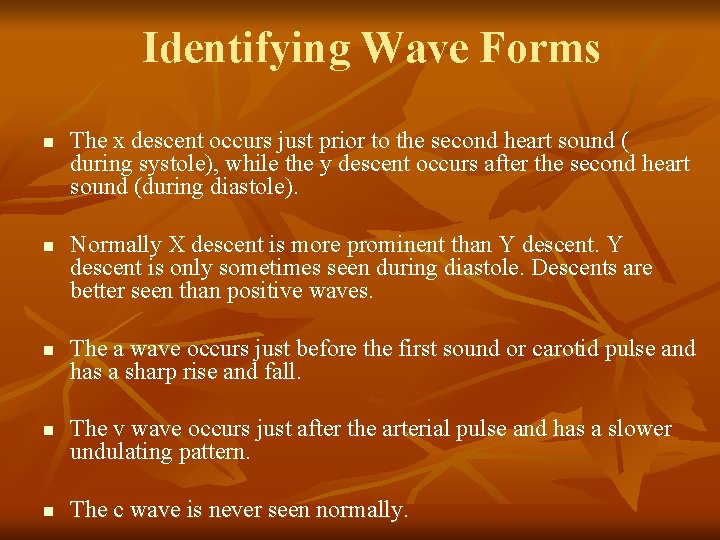
Identifying Wave Forms n n n The x descent occurs just prior to the second heart sound ( during systole), while the y descent occurs after the second heart sound (during diastole). Normally X descent is more prominent than Y descent is only sometimes seen during diastole. Descents are better seen than positive waves. The a wave occurs just before the first sound or carotid pulse and has a sharp rise and fall. The v wave occurs just after the arterial pulse and has a slower undulating pattern. The c wave is never seen normally.
Abnormalities of jugular venous pulse A. Low jugular venous pressure 1. Hypovolaemia.
B. Elevated jugular venous pressure 1. Intravascular volume overload conditions Right ventricular infarction Left heart failure Myocardial infarction. Valvular Heart Disease Cardiomyopathy 2. Constrictive pericarditis. 3. Pericardial effusion with tamponade
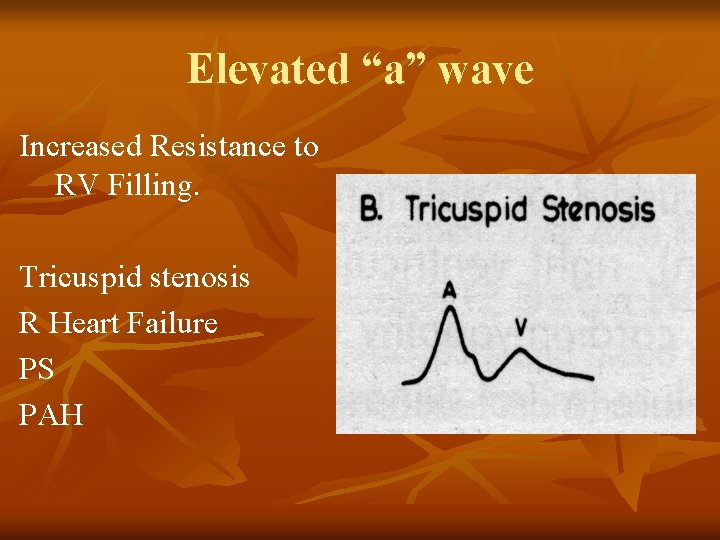
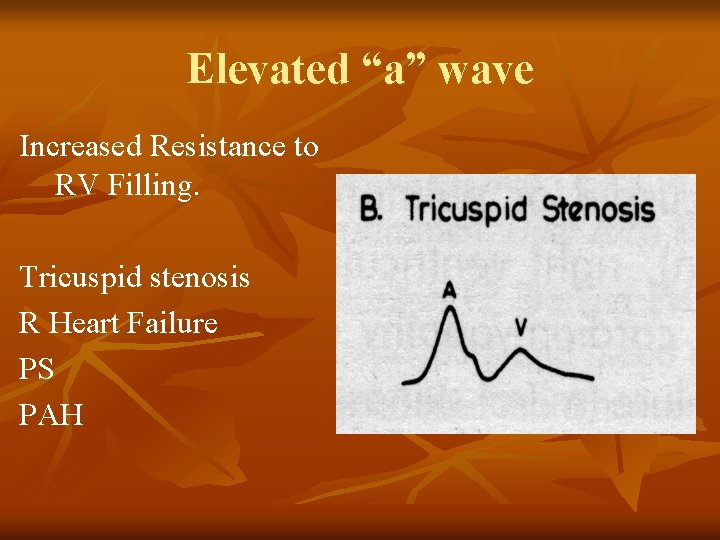
Elevated “a” wave Increased Resistance to RV Filling. Tricuspid stenosis R Heart Failure PS PAH
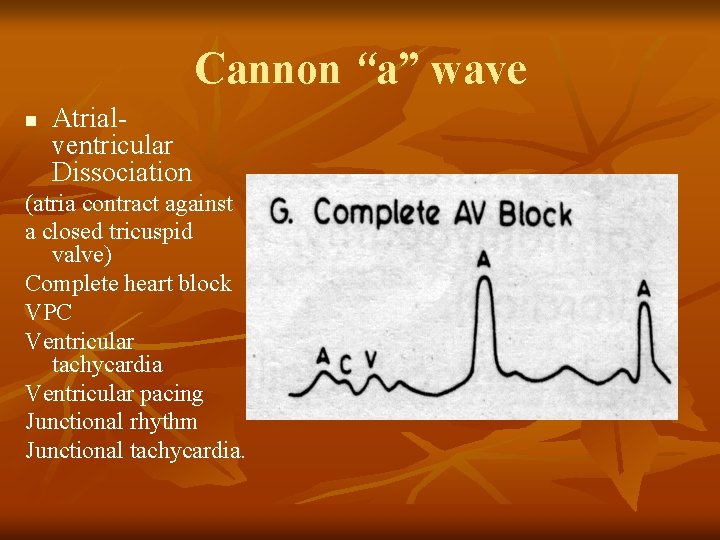
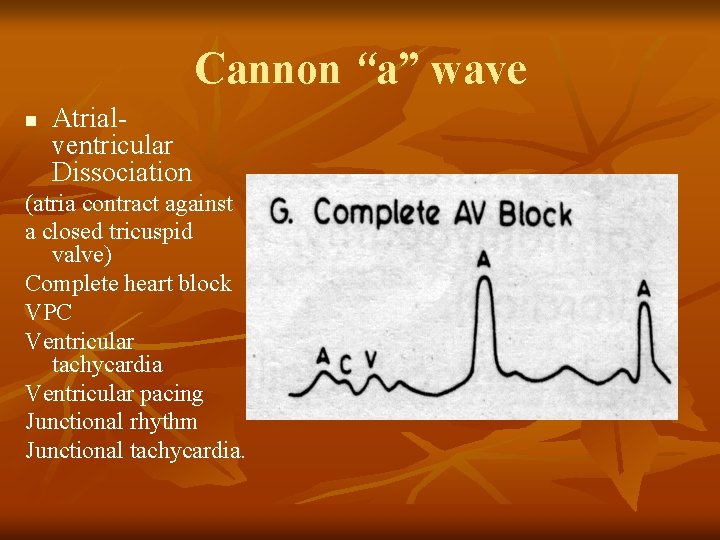
Cannon “a” wave n Atrialventricular Dissociation (atria contract against a closed tricuspid valve) Complete heart block VPC Ventricular tachycardia Ventricular pacing Junctional rhythm Junctional tachycardia.
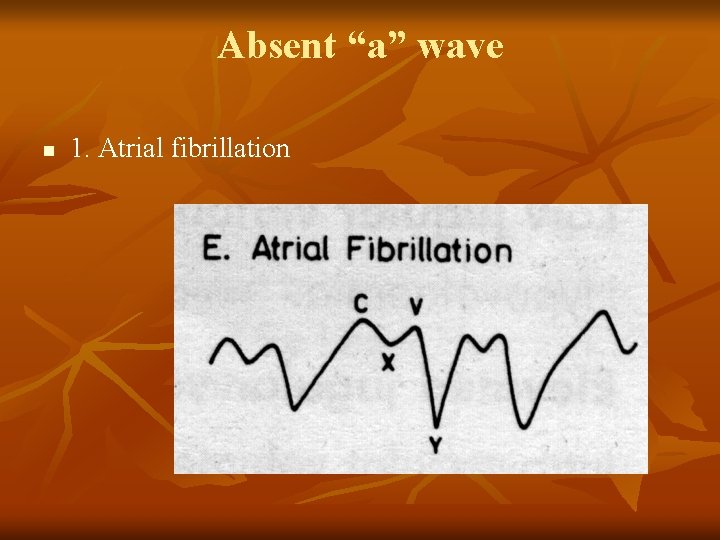
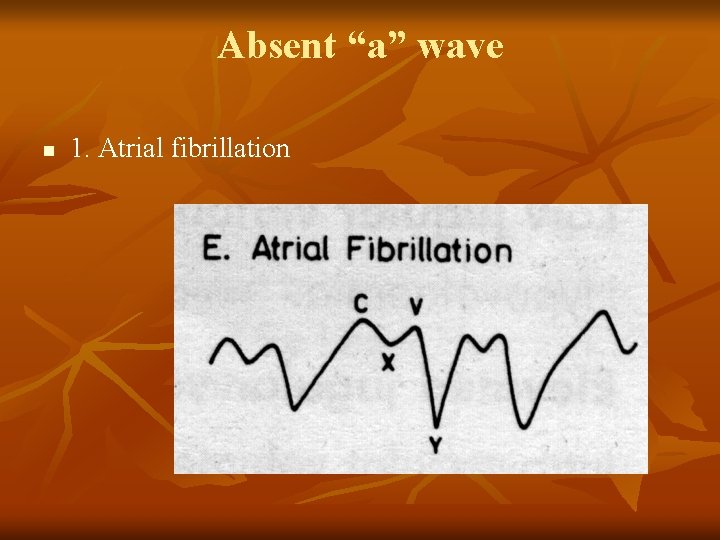
Absent “a” wave n 1. Atrial fibrillation
Elevated “v” wave 1. Tricuspid regurgitation. 2. Right ventricular failure. 3. Restrictive cardiomyopathy. 4. Cor Pulmonale
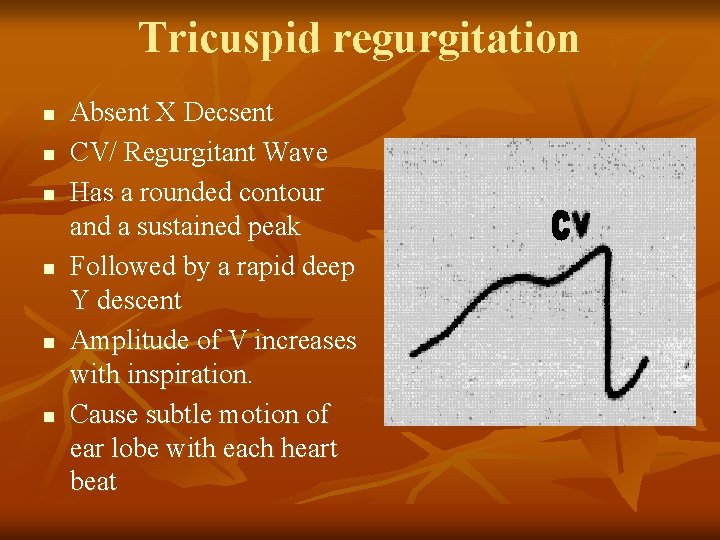
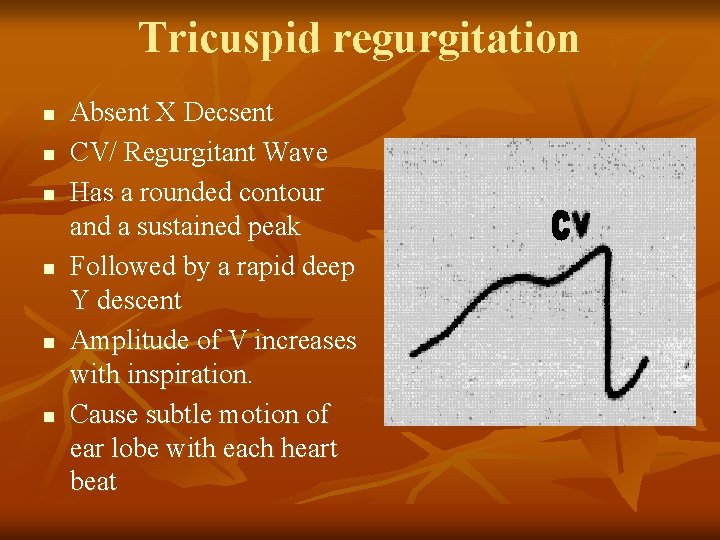
Tricuspid regurgitation n n n Absent X Decsent CV/ Regurgitant Wave Has a rounded contour and a sustained peak Followed by a rapid deep Y descent Amplitude of V increases with inspiration. Cause subtle motion of ear lobe with each heart beat
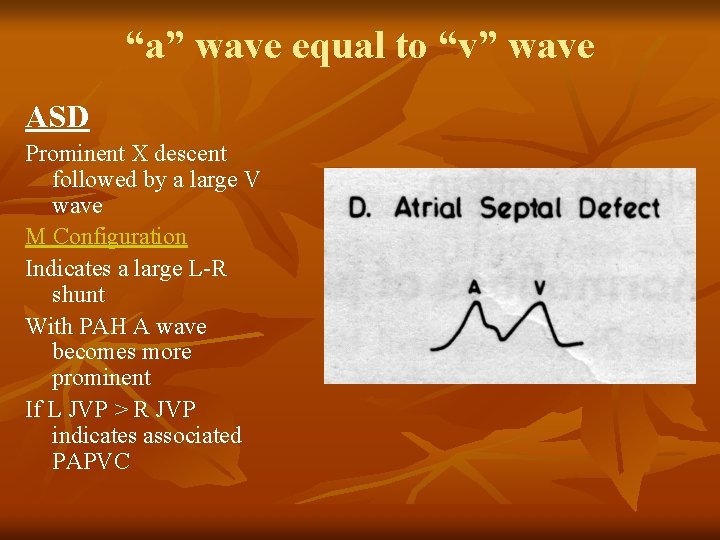
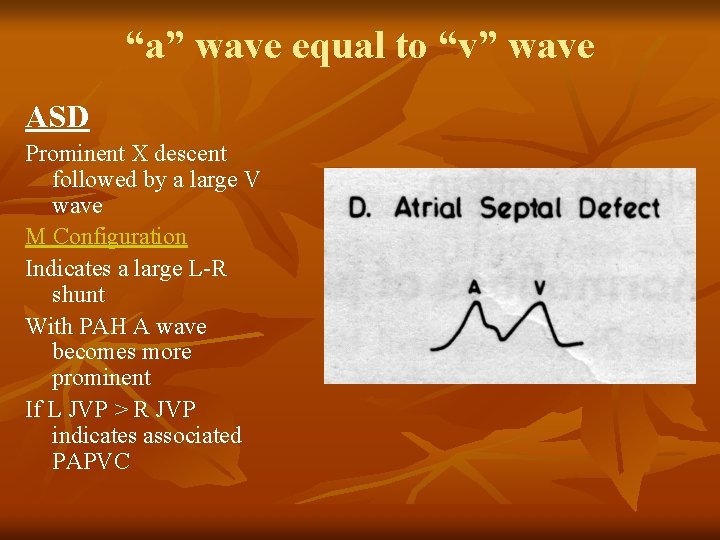
“a” wave equal to “v” wave ASD Prominent X descent followed by a large V wave M Configuration Indicates a large L-R shunt With PAH A wave becomes more prominent If L JVP > R JVP indicates associated PAPVC
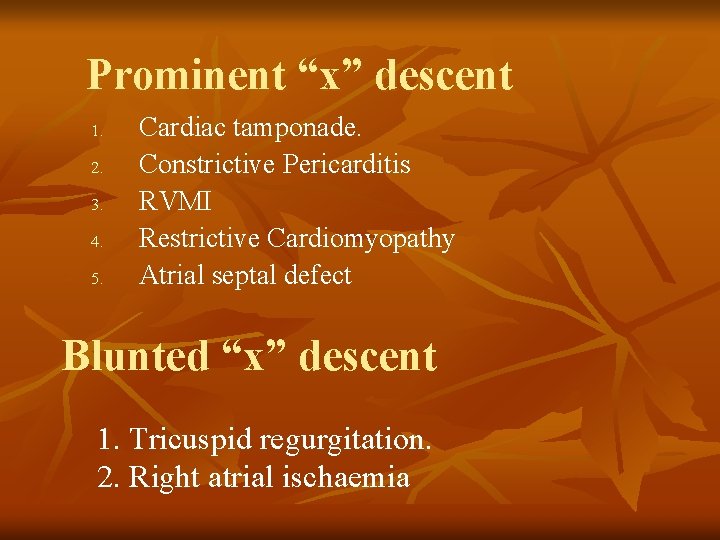
Prominent “x” descent 1. 2. 3. 4. 5. Cardiac tamponade. Constrictive Pericarditis RVMI Restrictive Cardiomyopathy Atrial septal defect Blunted “x” descent 1. Tricuspid regurgitation. 2. Right atrial ischaemia
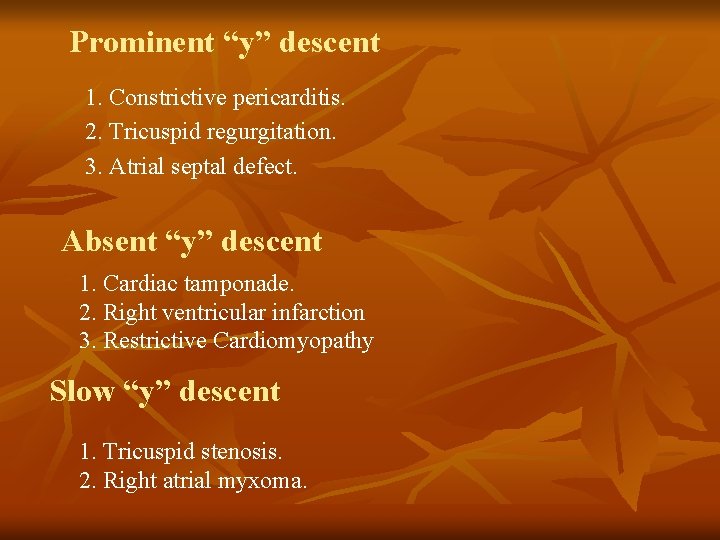
Prominent “y” descent 1. Constrictive pericarditis. 2. Tricuspid regurgitation. 3. Atrial septal defect. Absent “y” descent 1. Cardiac tamponade. 2. Right ventricular infarction 3. Restrictive Cardiomyopathy Slow “y” descent 1. Tricuspid stenosis. 2. Right atrial myxoma.
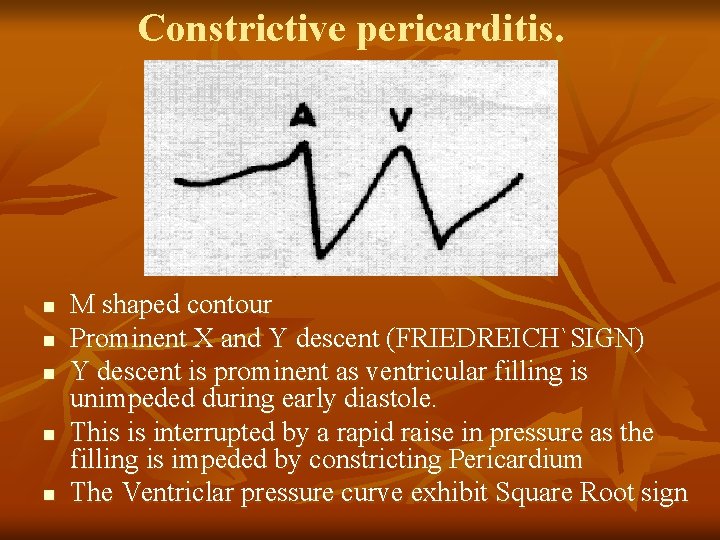
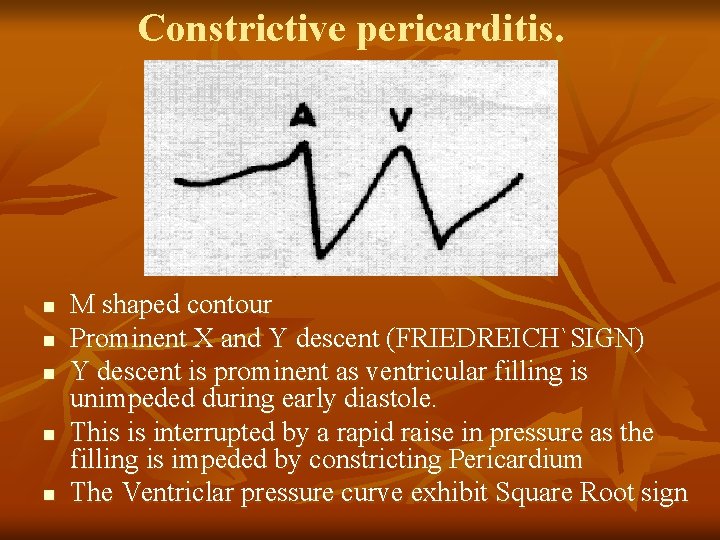
Constrictive pericarditis. n n n M shaped contour Prominent X and Y descent (FRIEDREICH`SIGN) Y descent is prominent as ventricular filling is unimpeded during early diastole. This is interrupted by a rapid raise in pressure as the filling is impeded by constricting Pericardium The Ventriclar pressure curve exhibit Square Root sign
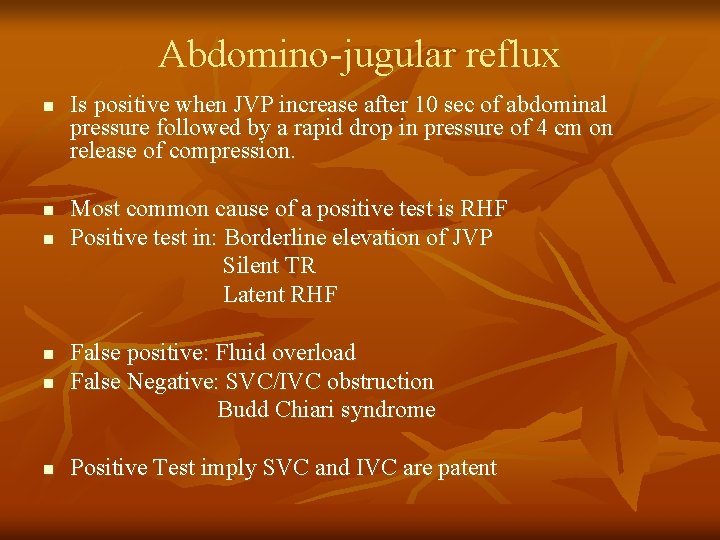
Abdomino-jugular reflux n n n Is positive when JVP increase after 10 sec of abdominal pressure followed by a rapid drop in pressure of 4 cm on release of compression. Most common cause of a positive test is RHF Positive test in: Borderline elevation of JVP Silent TR Latent RHF n False positive: Fluid overload False Negative: SVC/IVC obstruction Budd Chiari syndrome n Positive Test imply SVC and IVC are patent n
Kussmaul sign Failure of decline in JVP occur during inspiration. n n Constrictive Pericarditis Severe RHF Restrictive Cardiomyopathy Tricuspid Stenosis
