Chapter 15 16 Host Defenses II Specific Immunity

- Slides: 120
Chapter 15 -16 Host Defenses II: Specific Immunity and Immunization
Third Line Of Defense – Adaptive Immunity • When your non specific defenses are breached and our innate immune system can’t control the infection, then we have the other half of our immune system, the adaptive immune system, to help us out. • The adaptive immune system is characterized by extreme specificity and memory • This sets it apart from the other two parts of immunity.
Overview of Adaptive Immunity • Adaptive immunity is the body’s ability to recognize and defend itself against distinct invaders and their products • Five attributes of adaptive immunity – Specificity – Inducibility – Clonality – Unresponsiveness to self – Memory © 2012 Pearson Education Inc.
Thirdline of Defense • Specific immunity is a complex interaction of immune cells (leukocytes) reacting against antigens – Stages – Self and nonself – Clonal selection – Antigens
Adaptive Immunity -the innate system is triggered by general characteristics of invaders. Adaptive immune system detects specific molecular components of specific strains of microorganisms. -You are not born with adaptive immunity, it must be acquired following interaction with a microbe.
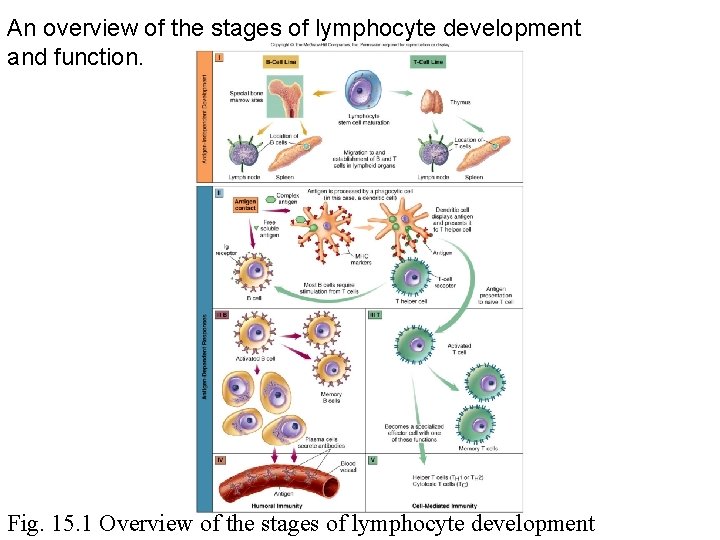
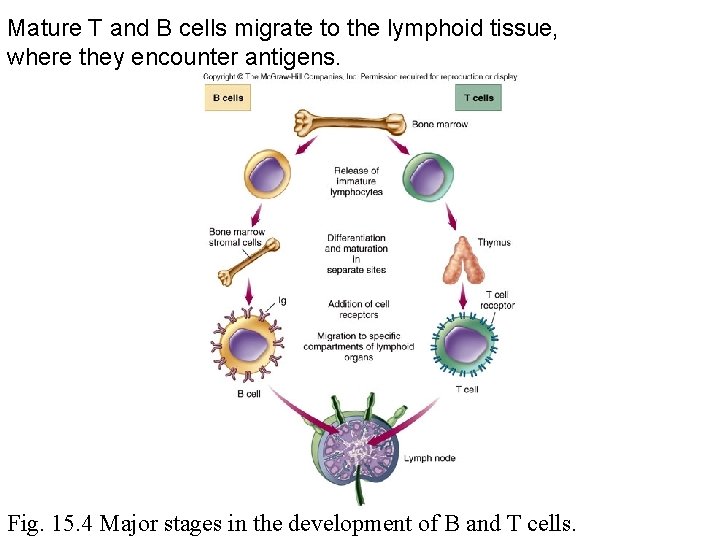
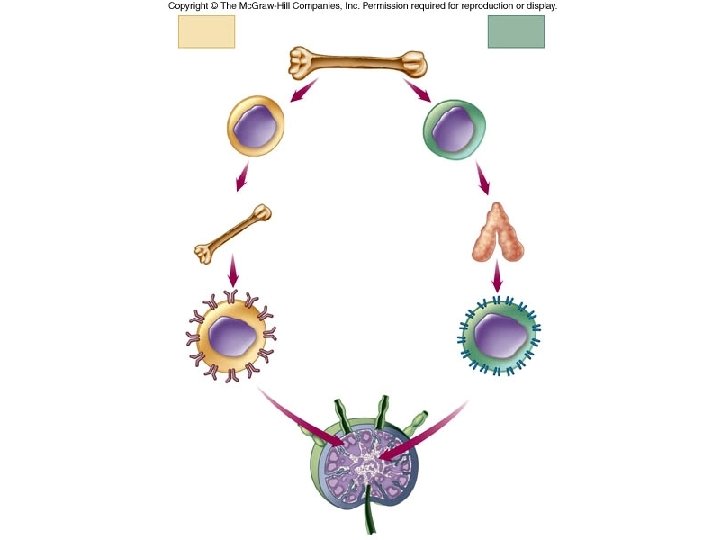
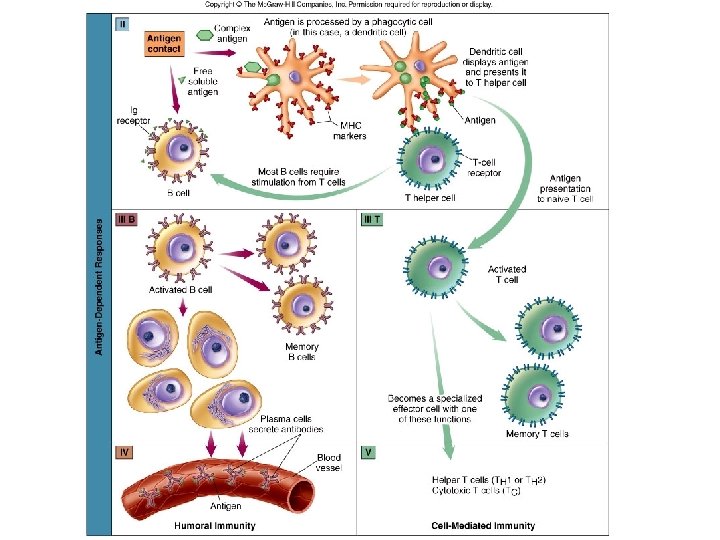
Overview of Adaptive Immunity • Involves activity of lymphocytes • Two main types of lymphocytes – B lymphocytes (B cells) • Mature in the bone marrow – T lymphocytes (T cells) • Mature in the thymus • Two types of adaptive immune responses – Humoral immune responses – Cell-mediated immune responses © 2012 Pearson Education Inc.
Ways to “interact” with a microbe Infection – meeting the microbe in daily life. Results in illness, but the body learns that microbe. Vaccination – a purposeful introduction to a microbe. Some diseases are too dangerous to risk an infection, so we use a vaccination.
Attenuated vaccine- live cells of a pathogen that have been genetically altered. Confers strong, long lasting immunity. Inactivated vaccine- contain cells that have been killed by heat or by chemical means. Very safe but less effective. Necessitates booster. Fears of Jenner’s vaccine
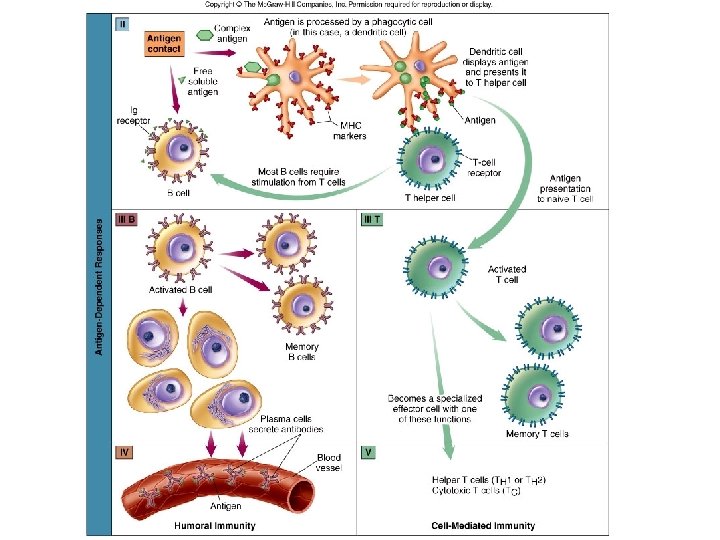
Stages • Dual lymphocyte development and differentiation • Presentation of antigens • Challenge of B and T lymphocytes by antigens • Production of antibodies by B cells (plasma cell) • T lymphocyte responses
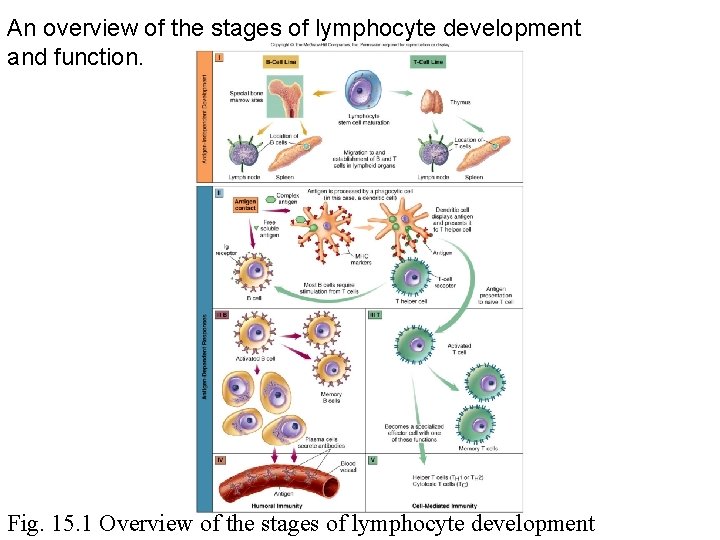
An overview of the stages of lymphocyte development and function. Fig. 15. 1 Overview of the stages of lymphocyte development
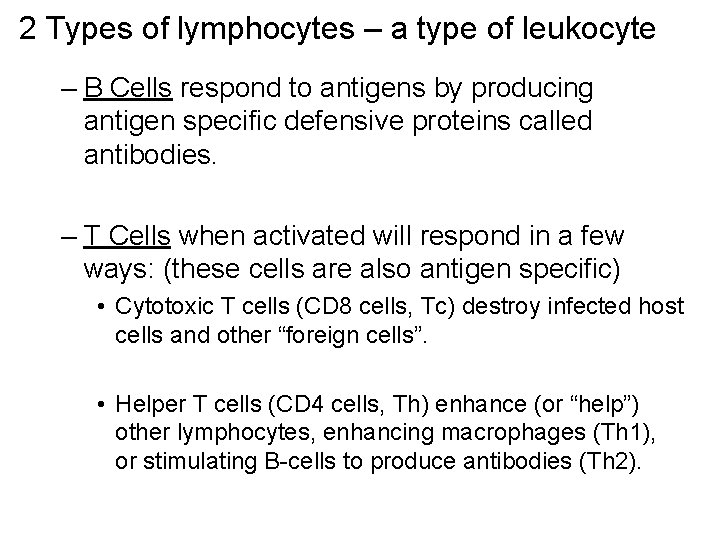
2 Types of lymphocytes – a type of leukocyte – B Cells respond to antigens by producing antigen specific defensive proteins called antibodies. – T Cells when activated will respond in a few ways: (these cells are also antigen specific) • Cytotoxic T cells (CD 8 cells, Tc) destroy infected host cells and other “foreign cells”. • Helper T cells (CD 4 cells, Th) enhance (or “help”) other lymphocytes, enhancing macrophages (Th 1), or stimulating B-cells to produce antibodies (Th 2).
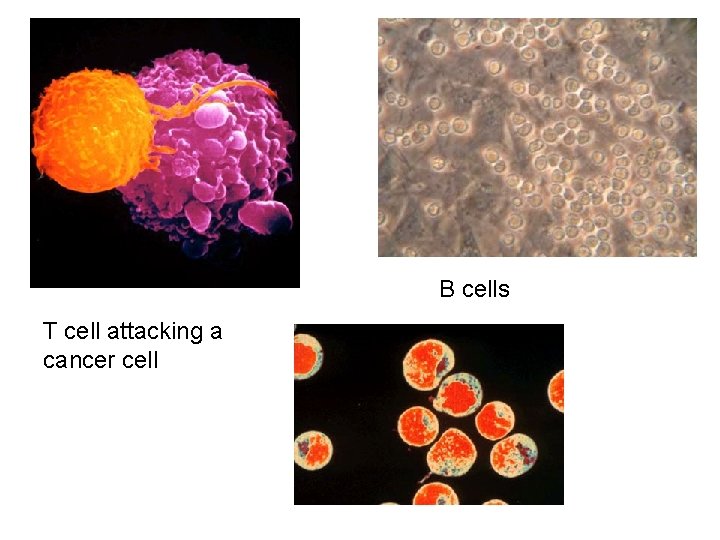
B cells T cell attacking a cancer cell
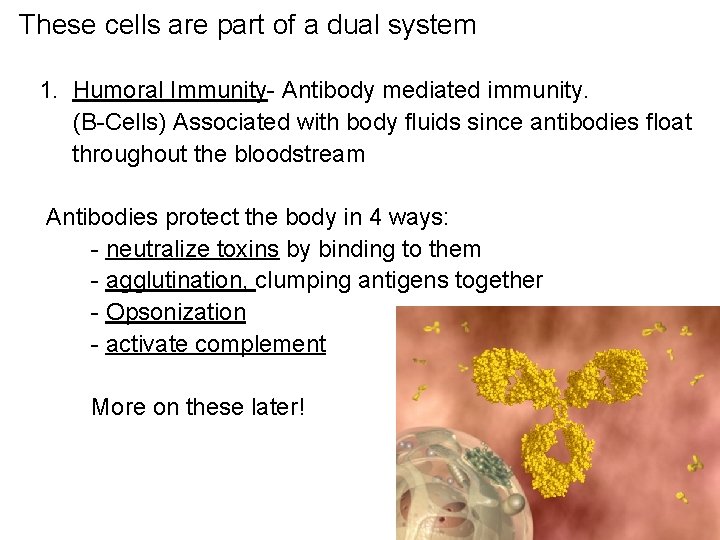
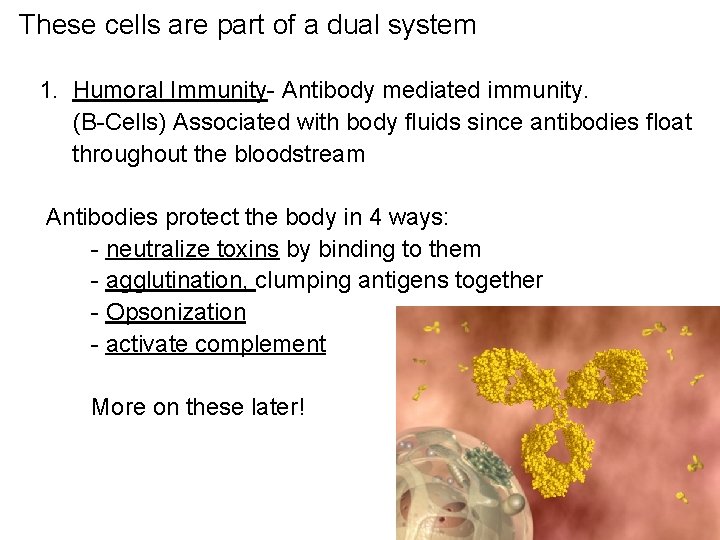
These cells are part of a dual system 1. Humoral Immunity- Antibody mediated immunity. (B-Cells) Associated with body fluids since antibodies float throughout the bloodstream Antibodies protect the body in 4 ways: - neutralize toxins by binding to them - agglutination, clumping antigens together - Opsonization - activate complement More on these later!
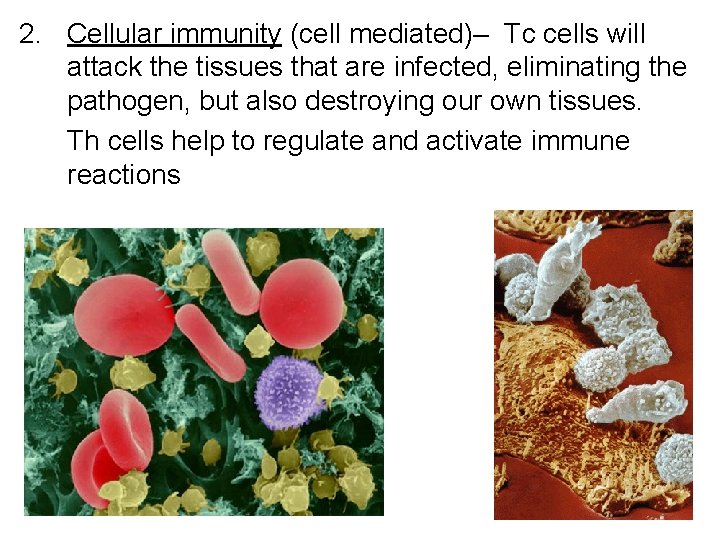
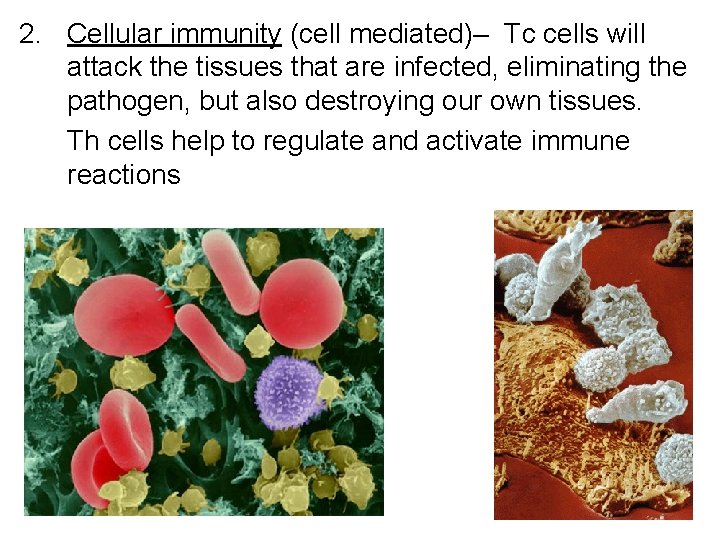
2. Cellular immunity (cell mediated)– Tc cells will attack the tissues that are infected, eliminating the pathogen, but also destroying our own tissues. Th cells help to regulate and activate immune reactions
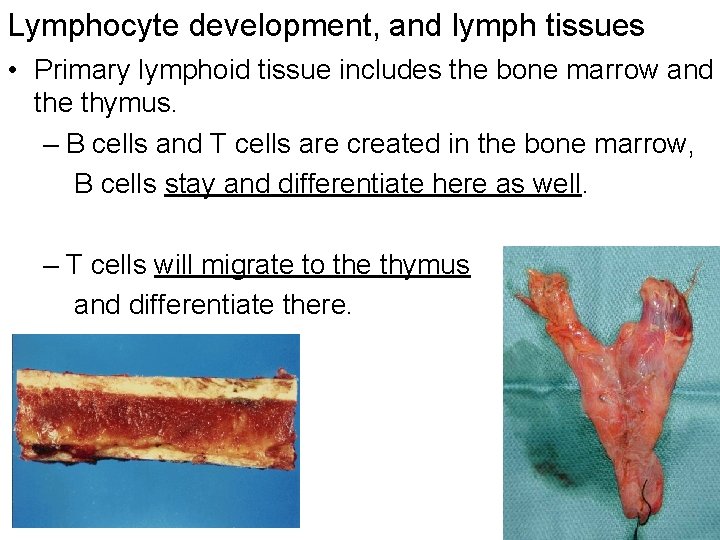
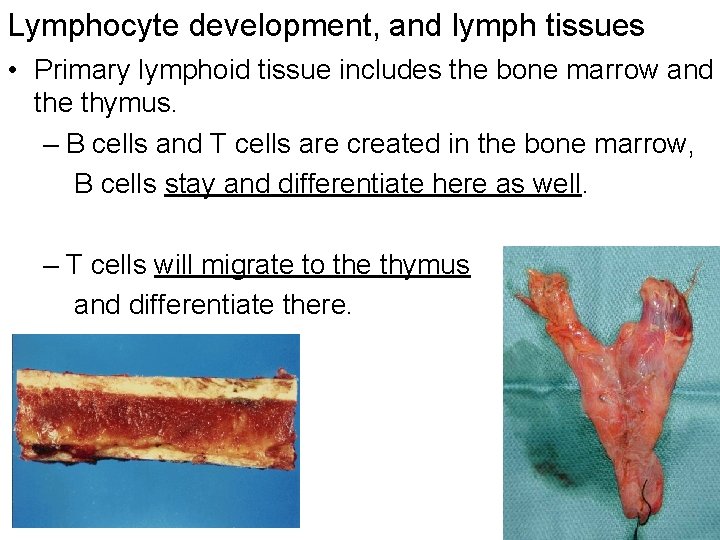
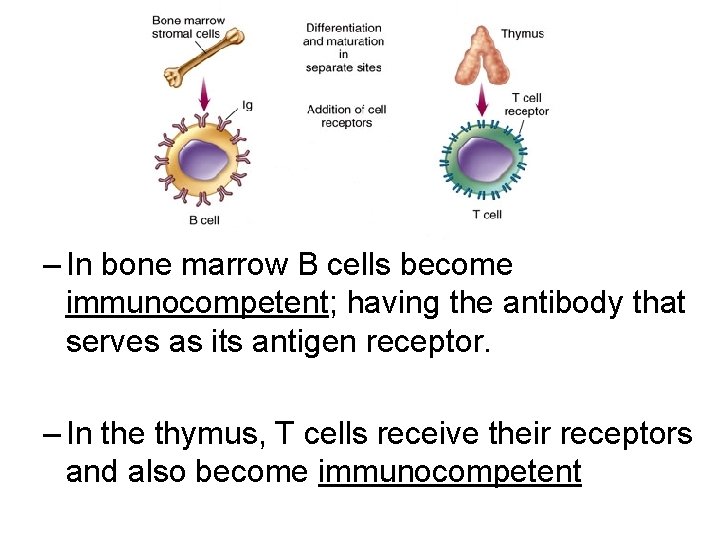
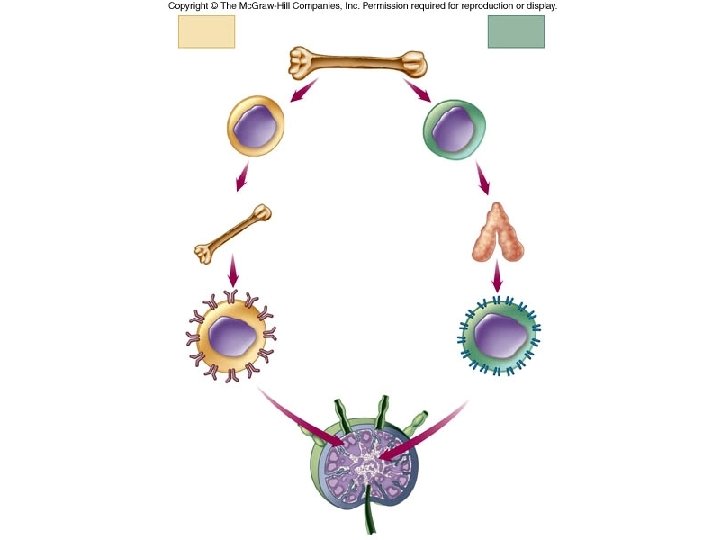
Lymphocyte development, and lymph tissues • Primary lymphoid tissue includes the bone marrow and the thymus. – B cells and T cells are created in the bone marrow, B cells stay and differentiate here as well. – T cells will migrate to the thymus and differentiate there.
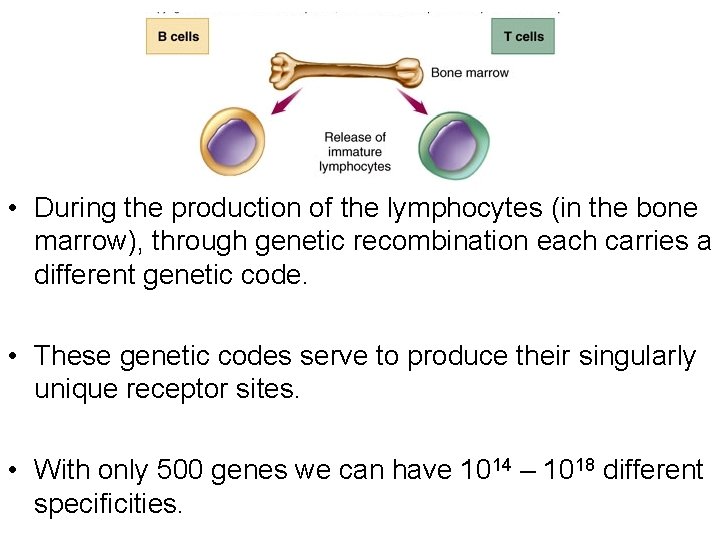
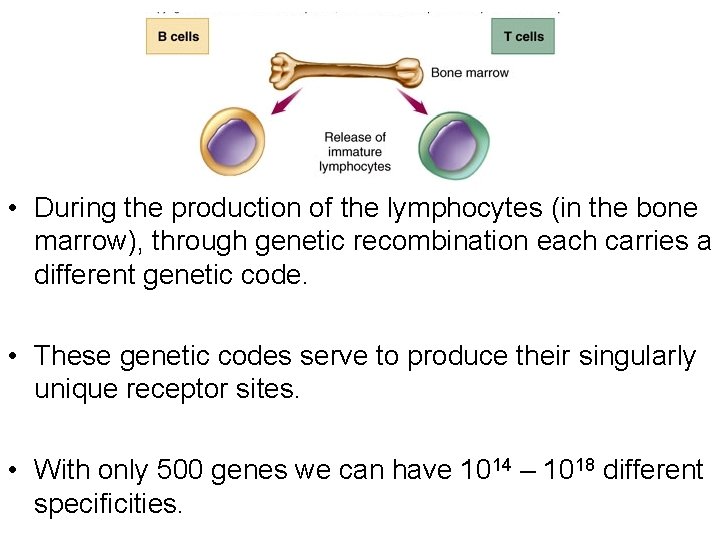
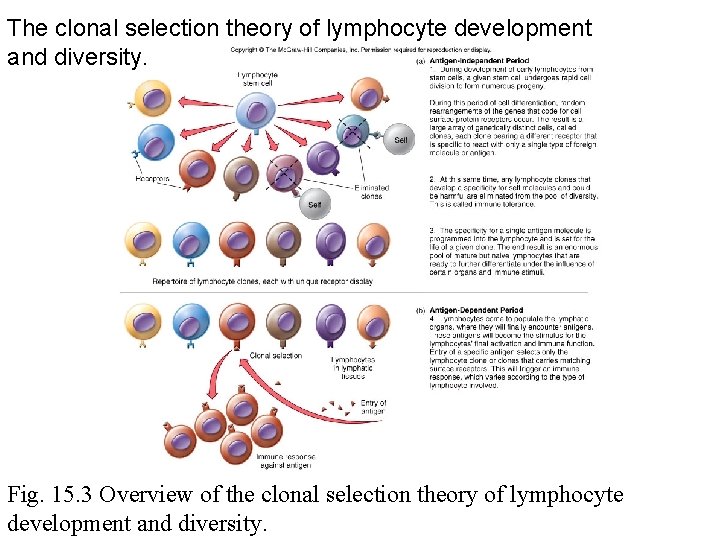
• During the production of the lymphocytes (in the bone marrow), through genetic recombination each carries a different genetic code. • These genetic codes serve to produce their singularly unique receptor sites. • With only 500 genes we can have 1014 – 1018 different specificities.
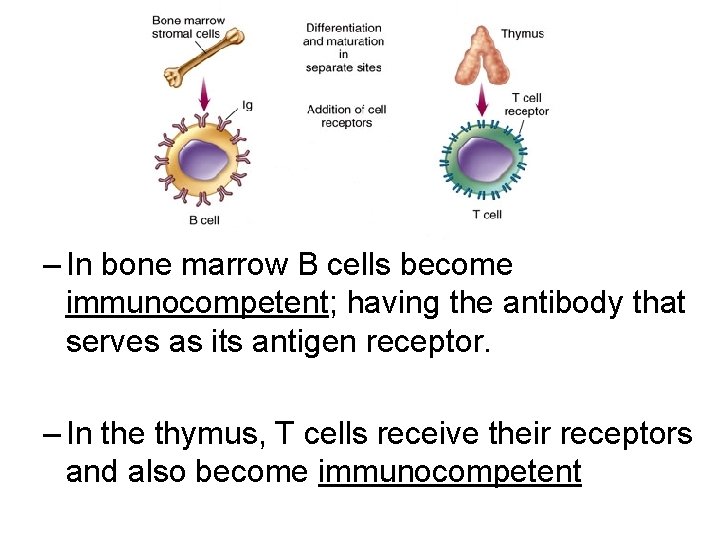
– In bone marrow B cells become immunocompetent; having the antibody that serves as its antigen receptor. – In the thymus, T cells receive their receptors and also become immunocompetent
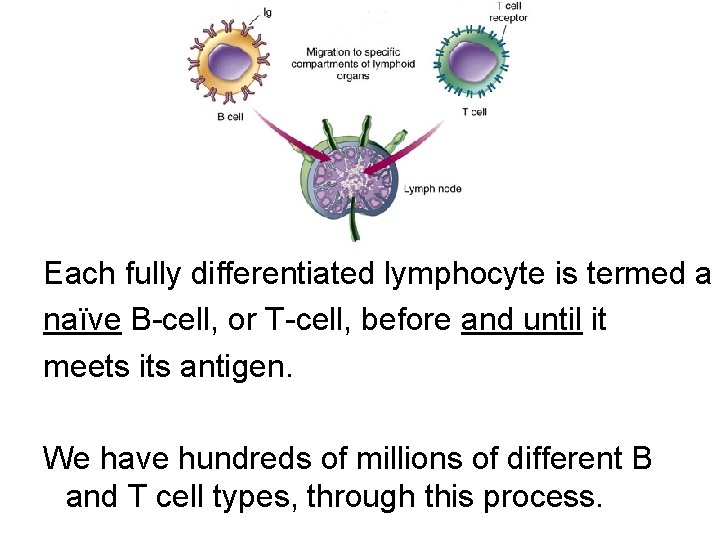
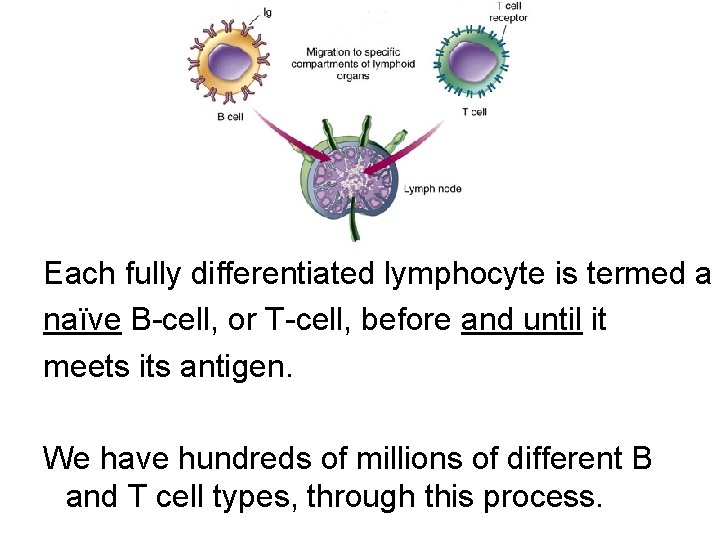
Each fully differentiated lymphocyte is termed a naïve B-cell, or T-cell, before and until it meets its antigen. We have hundreds of millions of different B and T cell types, through this process.
Self and nonself • Markers – glycoprotein – located on the cell surface – Eg. Major histocompatibility complex (MHC)
Markers • Host cells receptors (ex. MHC) confer specificity and identity • Role – detection, recognition, and communication • Lymphocyte cells recognize the host cell receptors as “self” • Lymphocyte cells recognize microbe receptors as ‘nonself’
Major histocompatibility complex (MHC) • • Self receptor Glycoprotein Found on all nucleated cells In humans – Human leukocyte antigen (HLA) is equivalent to the MHC • Classes of MHC
Classes of MHC • Each individual has a unique MHC profile – Expression of a particular combination of MHC genes • Class I – all nucleated cells • Class II – macrophages, dendritic cells, B cells
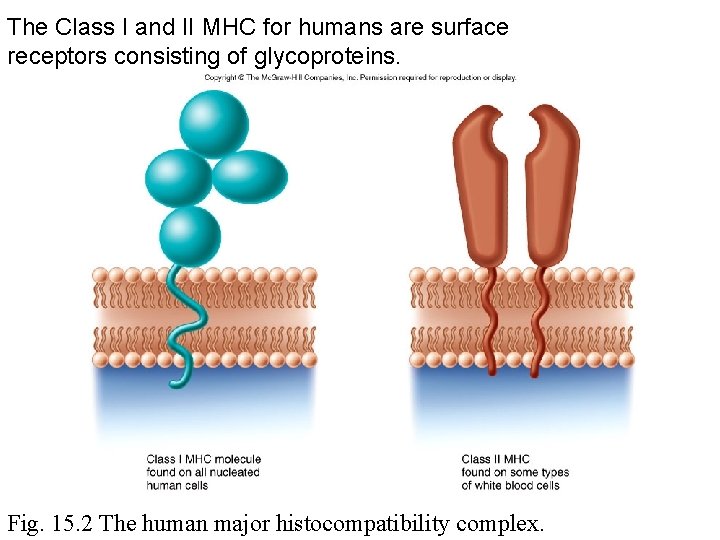
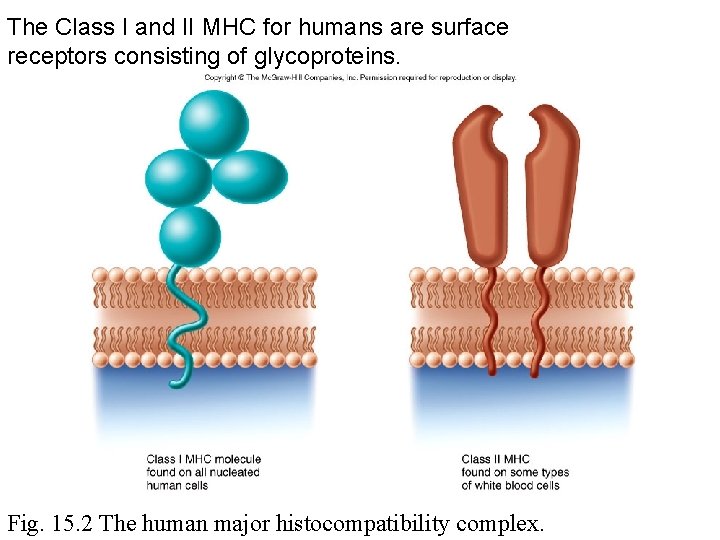
The Class I and II MHC for humans are surface receptors consisting of glycoproteins. Fig. 15. 2 The human major histocompatibility complex.
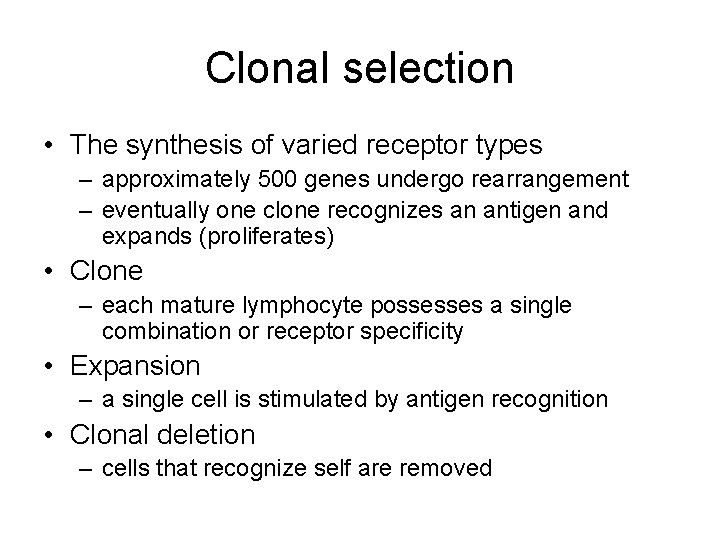
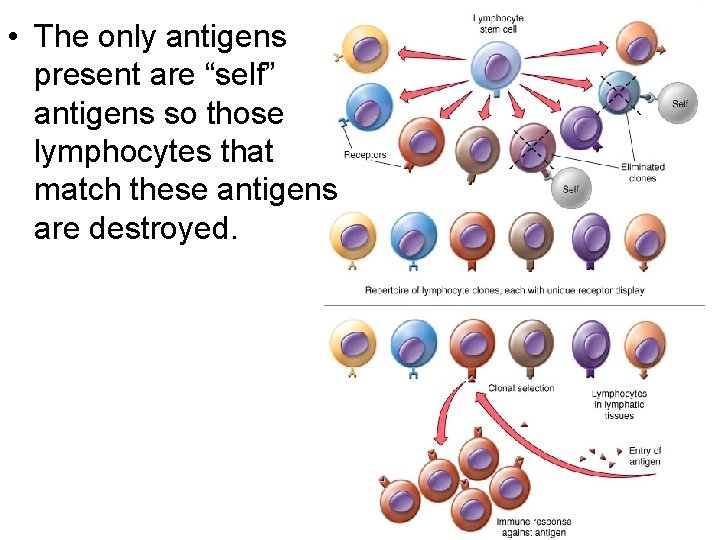
Clonal selection • The synthesis of varied receptor types – approximately 500 genes undergo rearrangement – eventually one clone recognizes an antigen and expands (proliferates) • Clone – each mature lymphocyte possesses a single combination or receptor specificity • Expansion – a single cell is stimulated by antigen recognition • Clonal deletion – cells that recognize self are removed
B cell clone • Application of immunology • Propagate a single clone in order to synthesis monoclonal antibodies • Monoclonal antibody – possess a single specificity for antigen
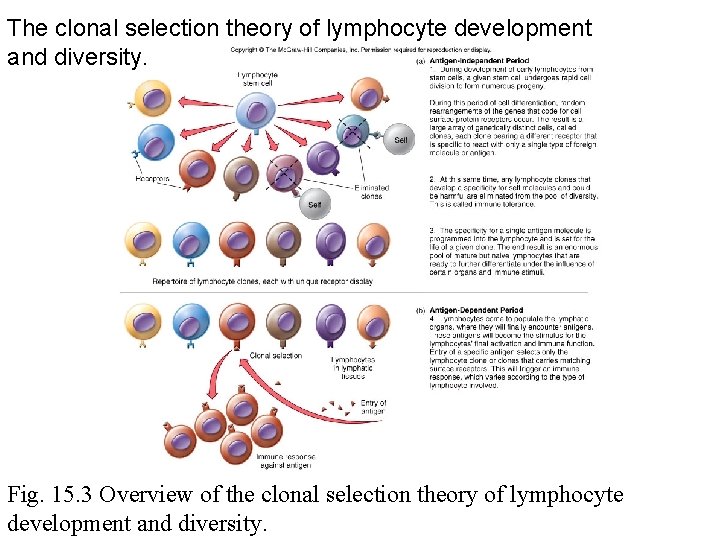
The clonal selection theory of lymphocyte development and diversity. Fig. 15. 3 Overview of the clonal selection theory of lymphocyte development and diversity.
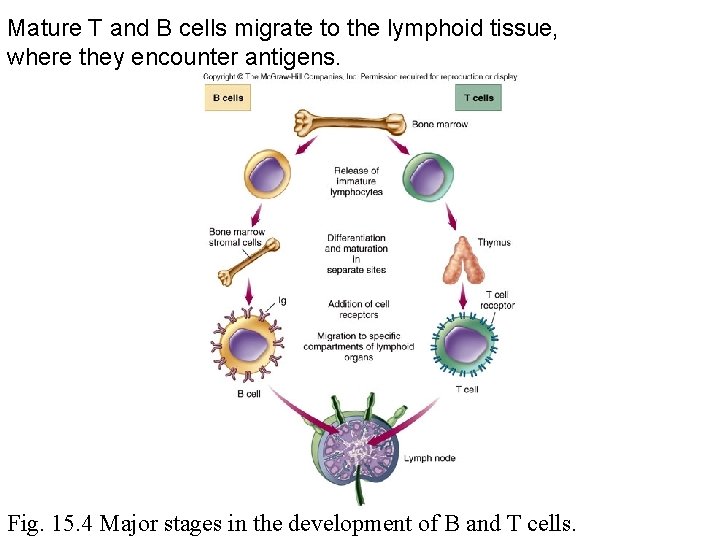
Mature T and B cells migrate to the lymphoid tissue, where they encounter antigens. Fig. 15. 4 Major stages in the development of B and T cells.
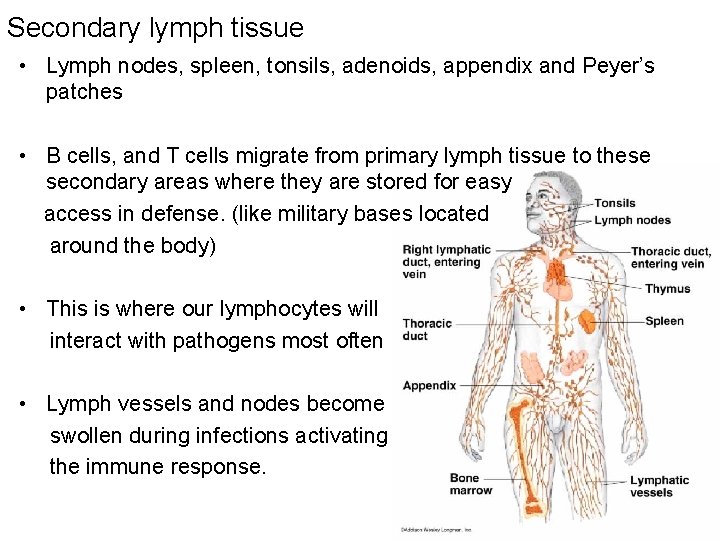
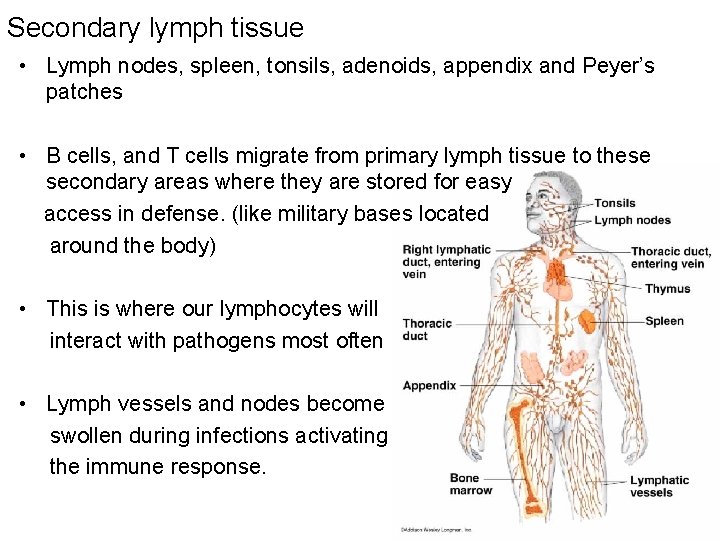
Secondary lymph tissue • Lymph nodes, spleen, tonsils, adenoids, appendix and Peyer’s patches • B cells, and T cells migrate from primary lymph tissue to these secondary areas where they are stored for easy access in defense. (like military bases located around the body) • This is where our lymphocytes will interact with pathogens most often • Lymph vessels and nodes become swollen during infections activating the immune response.
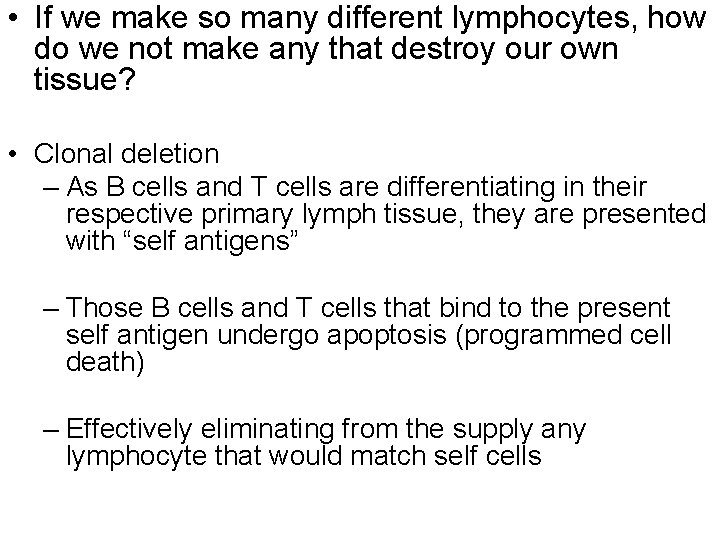
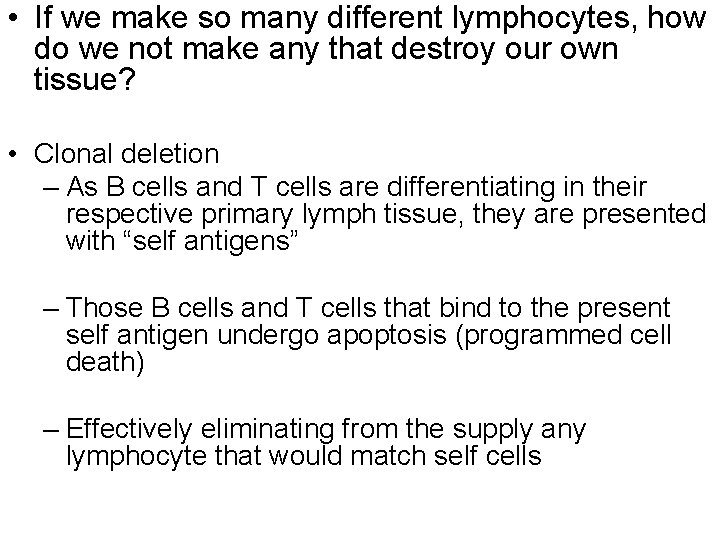
• If we make so many different lymphocytes, how do we not make any that destroy our own tissue? • Clonal deletion – As B cells and T cells are differentiating in their respective primary lymph tissue, they are presented with “self antigens” – Those B cells and T cells that bind to the present self antigen undergo apoptosis (programmed cell death) – Effectively eliminating from the supply any lymphocyte that would match self cells
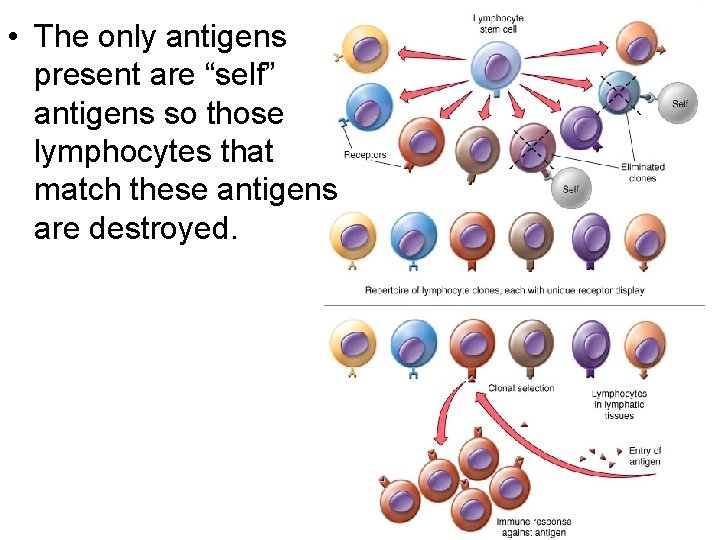
• The only antigens present are “self” antigens so those lymphocytes that match these antigens are destroyed.
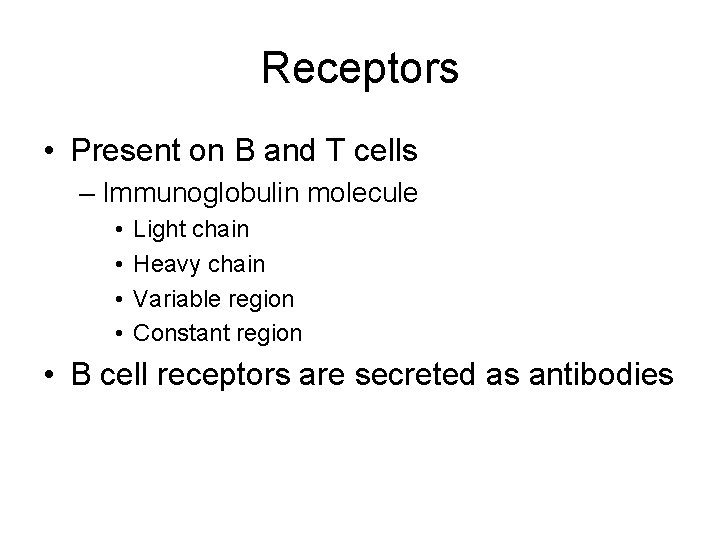
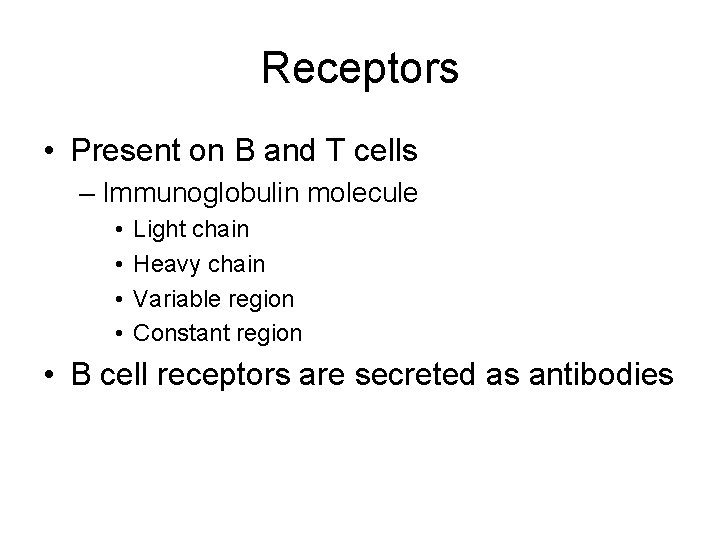
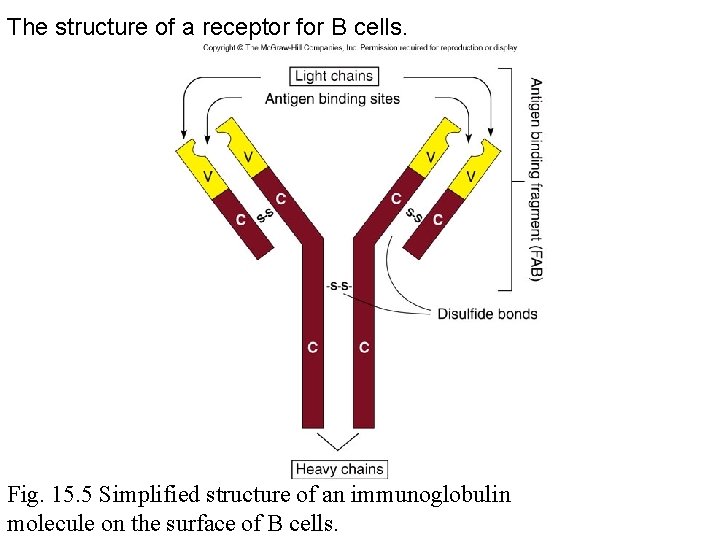
Receptors • Present on B and T cells – Immunoglobulin molecule • • Light chain Heavy chain Variable region Constant region • B cell receptors are secreted as antibodies
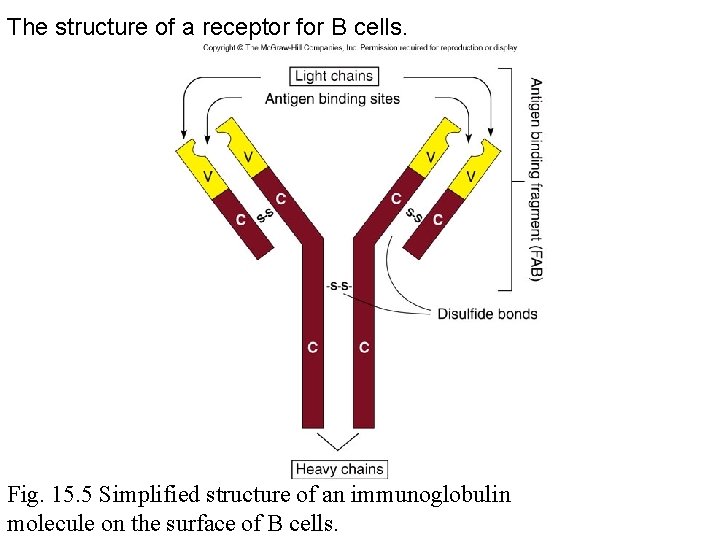
The structure of a receptor for B cells. Fig. 15. 5 Simplified structure of an immunoglobulin molecule on the surface of B cells.
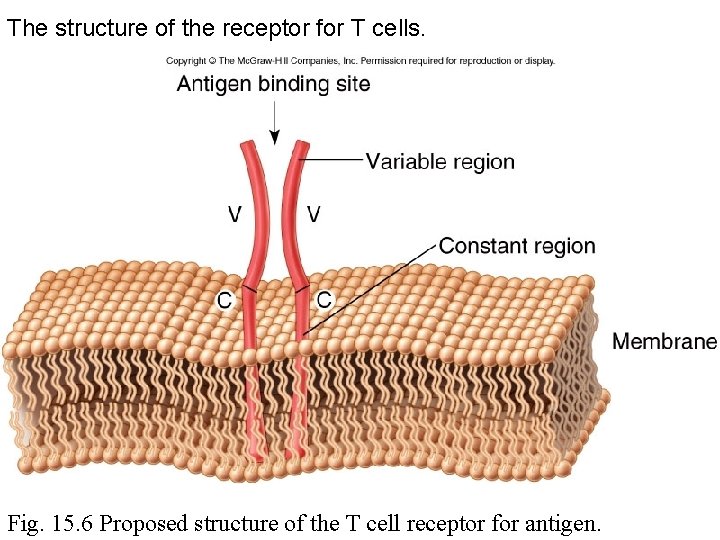
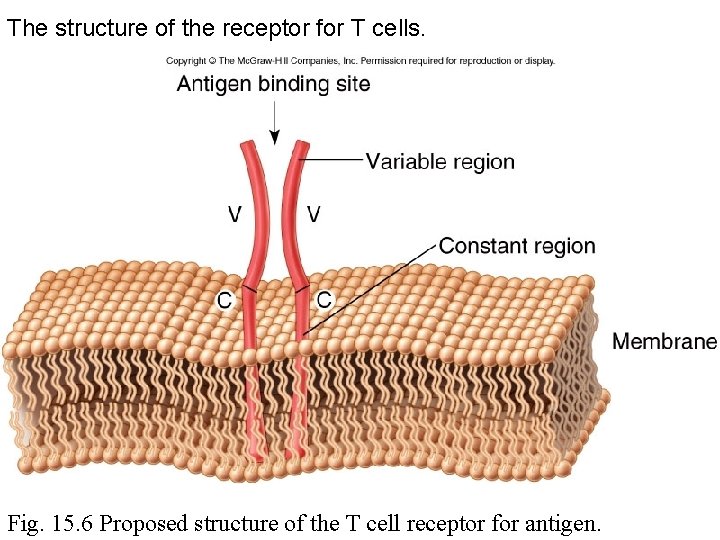
The structure of the receptor for T cells. Fig. 15. 6 Proposed structure of the T cell receptor for antigen.
Antigens • • Foreign material Size and shape Alloantigens Superantigens
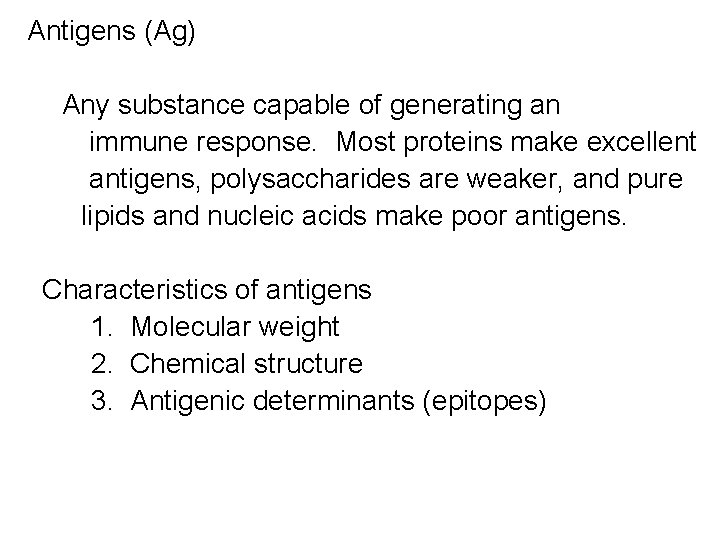
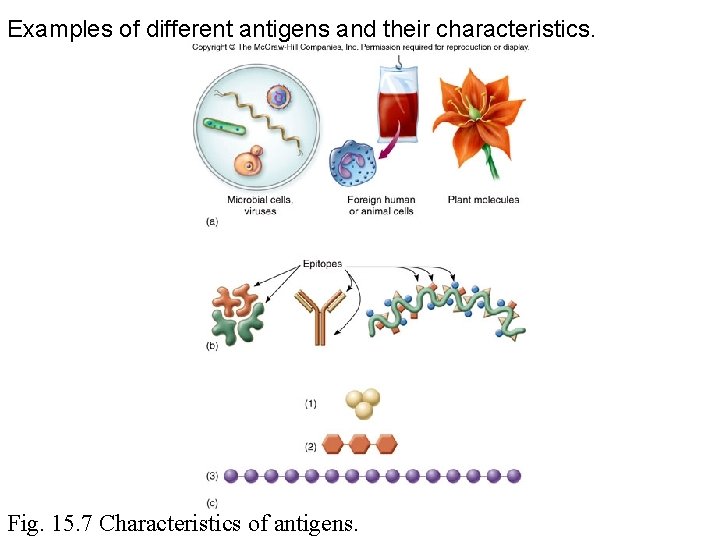
Antigens (Ag) Any substance capable of generating an immune response. Most proteins make excellent antigens, polysaccharides are weaker, and pure lipids and nucleic acids make poor antigens. Characteristics of antigens 1. Molecular weight 2. Chemical structure 3. Antigenic determinants (epitopes)
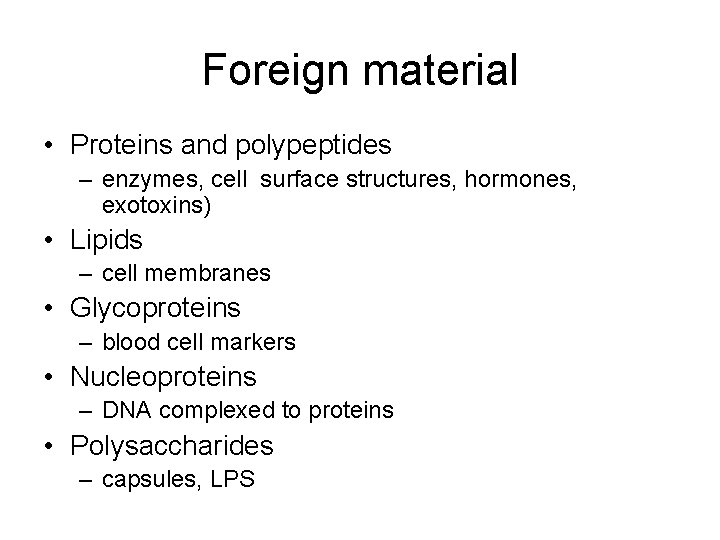
Foreign material • Proteins and polypeptides – enzymes, cell surface structures, hormones, exotoxins) • Lipids – cell membranes • Glycoproteins – blood cell markers • Nucleoproteins – DNA complexed to proteins • Polysaccharides – capsules, LPS
Size and shape • Immunogen – Less than 1000 daltons – no immune recognition – Greater than 1000 daltons – immune recognition – Proteins are better immunogens than polysaccharides • Epitope – portion of the antigen (ex. Amino acids) recognized by lymphocyte receptor • Haptens – antigens that are too small to elicit an immune response
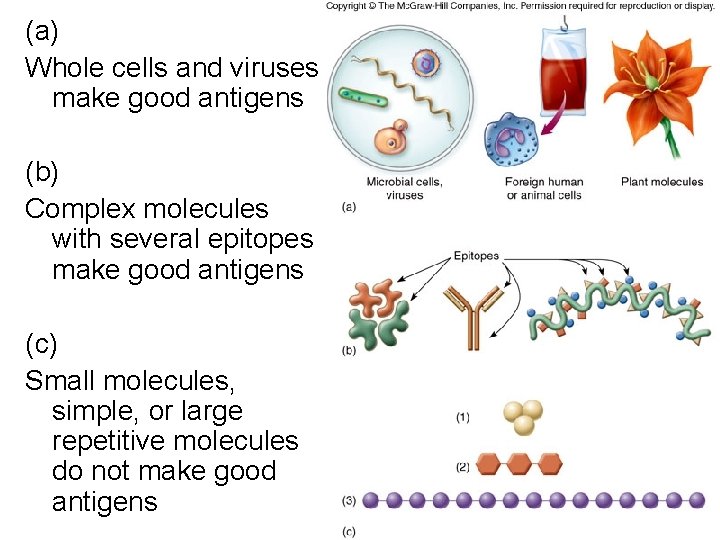
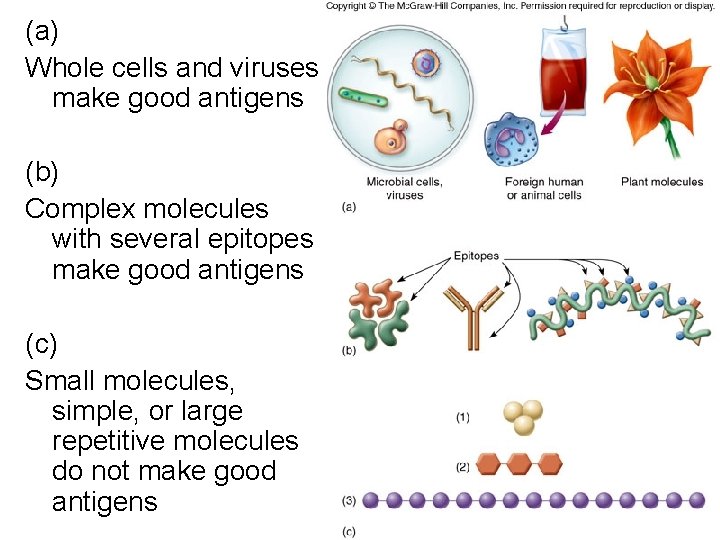
(a) Whole cells and viruses make good antigens (b) Complex molecules with several epitopes make good antigens (c) Small molecules, simple, or large repetitive molecules do not make good antigens
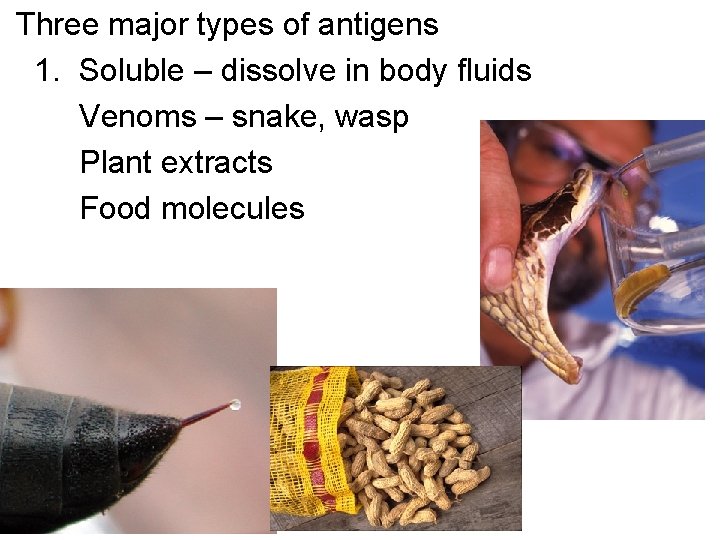
Three major types of antigens 1. Soluble – dissolve in body fluids Venoms – snake, wasp Plant extracts Food molecules
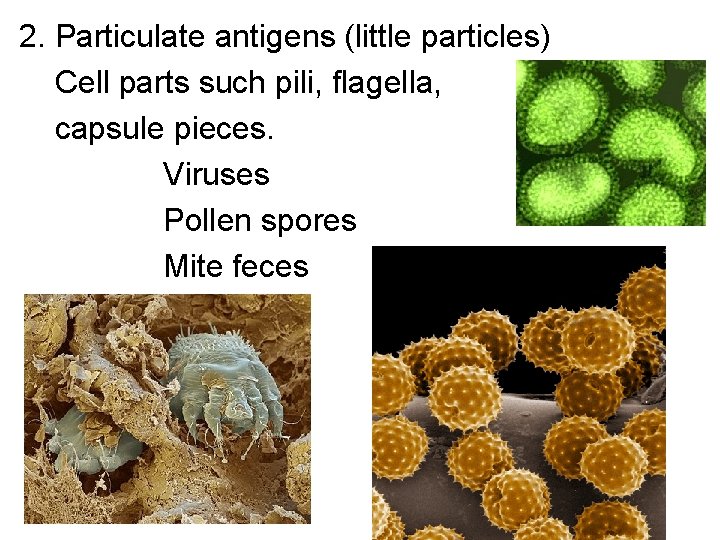
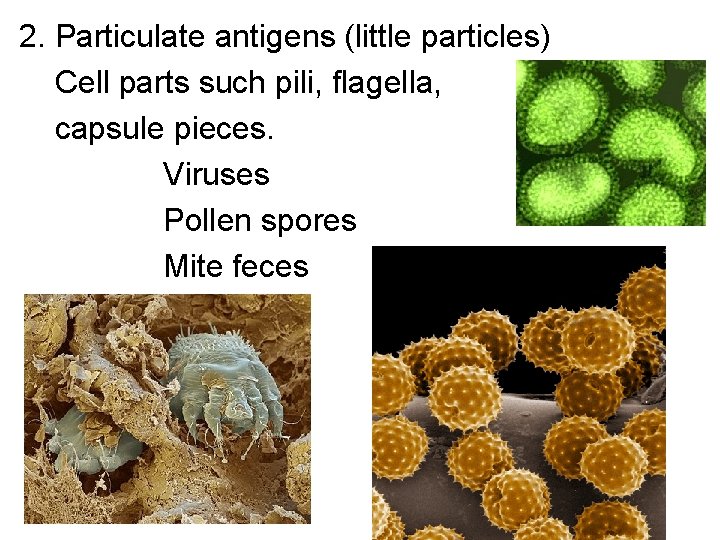
2. Particulate antigens (little particles) Cell parts such pili, flagella, capsule pieces. Viruses Pollen spores Mite feces
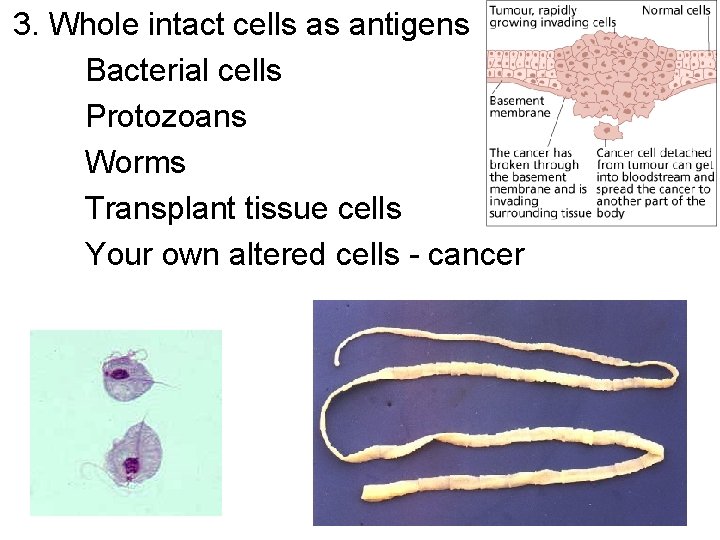
3. Whole intact cells as antigens Bacterial cells Protozoans Worms Transplant tissue cells Your own altered cells - cancer
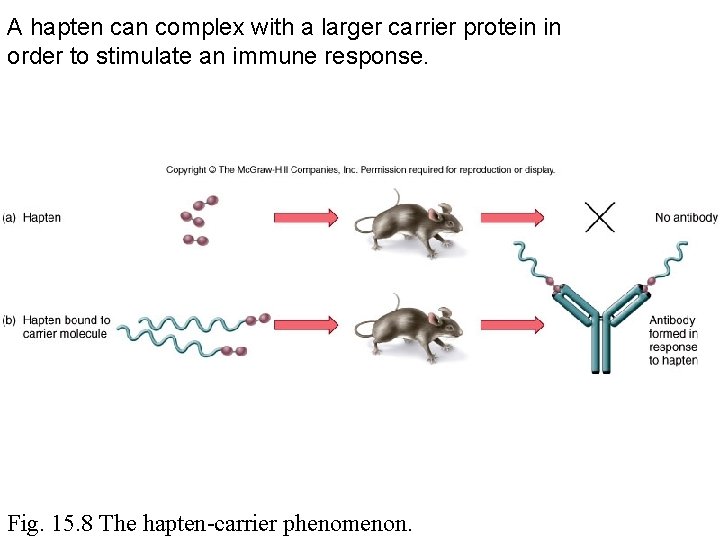
Haptens – an incomplete antigen, has some but not all characteristics of Antigens. - Lacking in size – less than 1, 000 - Not enough antigenic determinants, or epitopes - Will enter the body but must attach to carrier in the body and then becomes a complete antigen.
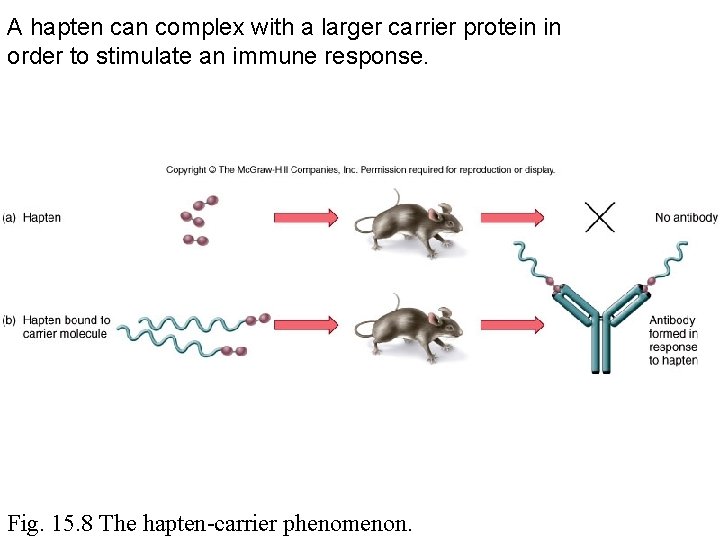
A hapten can complex with a larger carrier protein in order to stimulate an immune response. Fig. 15. 8 The hapten-carrier phenomenon.
Alloantigens • Cell surface markers that occur in some members of the same species – blood typing (transfusion) – MHC profile (organ grafting)
Superantigen • Bacterial toxins • T cell activation much greater than normal antigens • Large release of cytokines • Results in toxic shock syndrome and some autoimmune diseases
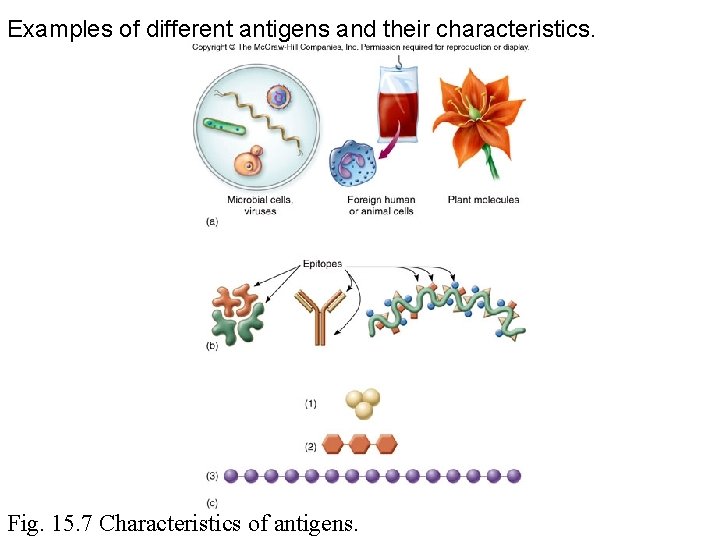
Examples of different antigens and their characteristics. Fig. 15. 7 Characteristics of antigens.
B cells • • Activation Antibody-antigen interaction Response
Activation • • Clonal selection and binding of antigen Instruction by chemical mediators Transmission of signal to the nucleus B cell changes into a plasma cells and begins mitosis • Clonal expansion and memory cell formation • Antibody production and secretion
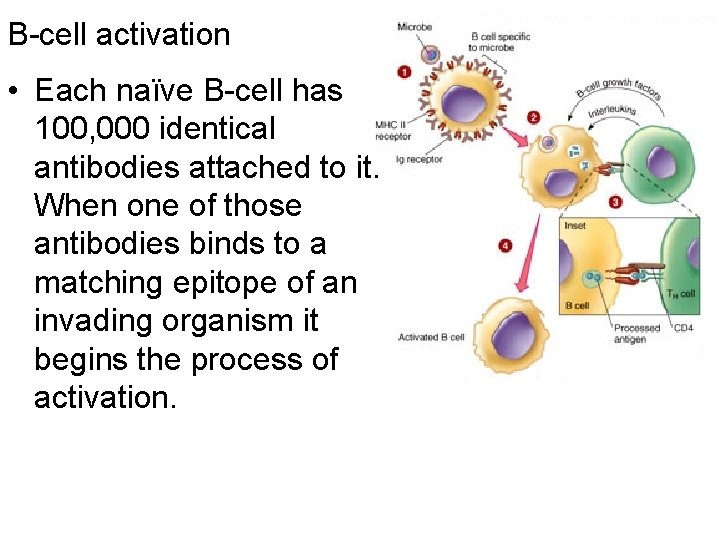
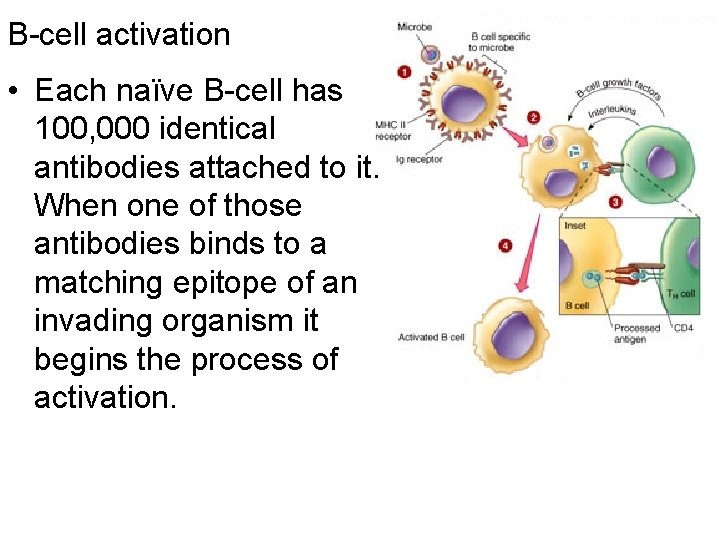
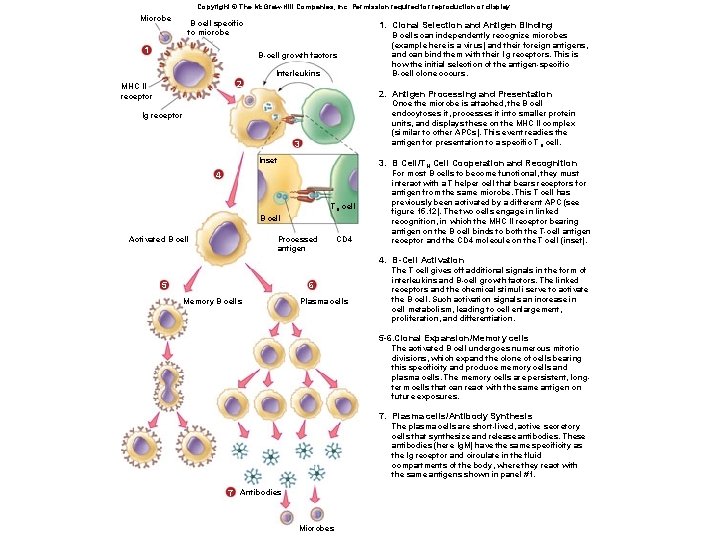
B-cell activation • Each naïve B-cell has 100, 000 identical antibodies attached to it. When one of those antibodies binds to a matching epitope of an invading organism it begins the process of activation.
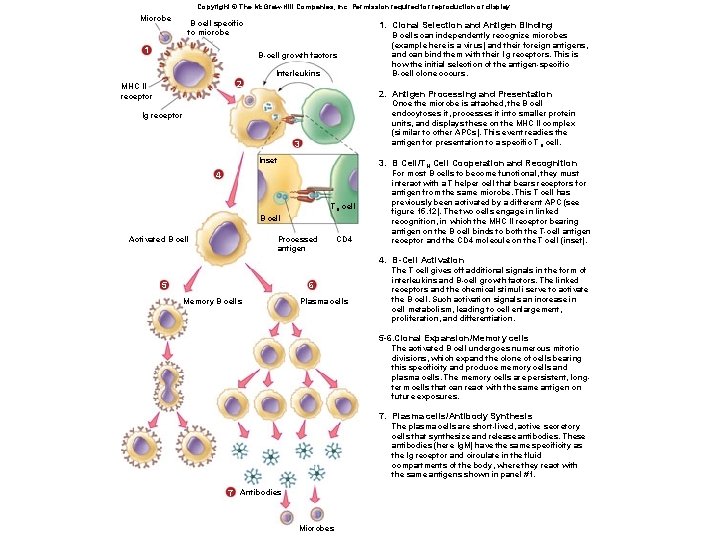
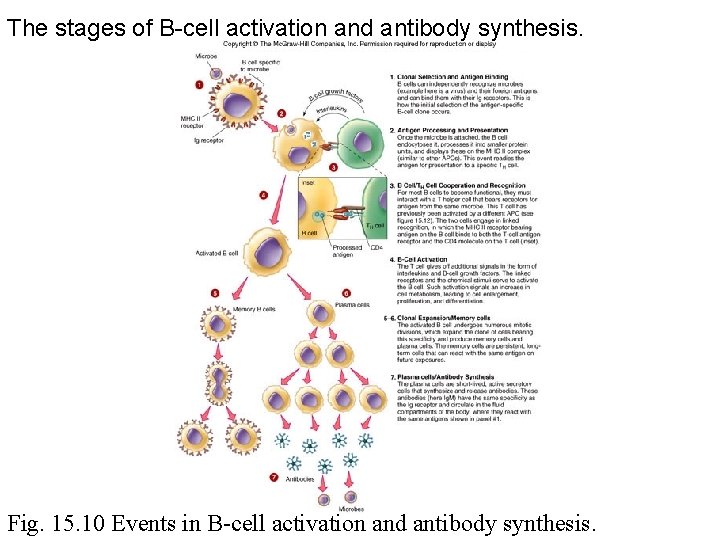
Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Microbe B cell specific to microbe 1 1. Clonal Selection and Antigen Binding B-cell growth factors Interleukins 2 MHC II receptor 2. Antigen Processing and Presentation Once the microbe is attached, the B cell endocytoses it, processes it into smaller protein units, and displays these on the MHC II complex (similar to other APCs). This event readies the antigen for presentation to a specific T H cell. Ig receptor 3 Inset 3. B Cell/TH Cell Cooperation and Recognition 4 TH cell B cell Activated B cells can independently recognize microbes (example here is a virus) and their foreign antigens, and can bind them with their lg receptors. This is how the initial selection of the antigen-specific B-cell clone occurs. Processed antigen CD 4 For most B cells to become functional, they must interact with a T helper cell that bears receptors for antigen from the same microbe. This T cell has previously been activated by a different APC (see figure 15. 12). The two cells engage in linked recognition, in which the MHC II receptor bearing antigen on the B cell binds to both the T-cell antigen receptor and the CD 4 molecule on the T cell (inset). 4. B-Cell Activation 5 6 Memory B cells Plasma cells The T cell gives off additional signals in the form of interleukins and B-cell growth factors. The linked receptors and the chemical stimuli serve to activate the B cell. Such activation signals an increase in cell metabolism, leading to cell enlargement, proliferation, and differentiation. 5 -6. Clonal Expansion/Memory cells The activated B cell undergoes numerous mitotic divisions, which expand the clone of cells bearing this specificity and produce memory cells and plasma cells. The memory cells are persistent, longterm cells that can react with the same antigen on future exposures. 7. Plasma cells/Antibody Synthesis The plasma cells are short-lived, active secretory cells that synthesize and release antibodies. These antibodies (here Ig. M) have the same specificity as the lg receptor and circulate in the fluid compartments of the body, where they react with the same antigens shown in panel #1. 7 Antibodies Microbes
B-cell activation 1. Naïve B-cells tethered antibodies match and bind with the present microbe. 2. B-cell endocytoses the microbe and presents smaller pieces on the MHC II proteins to the Th 2 cell. 3. Previously activated Th 2 (that matches the microbe) links with B-cell and it’s antigen bearing MHC II proteins 4. Th 2 cell chemically signals for the B-cell to proliferate. 5 – 6. Some clones become memory cells to be used later. Other clones go on to produce plasma cells. 7. Plasma cells secrete large amts of antibodies (2000/second) with same specificity as original B-cell
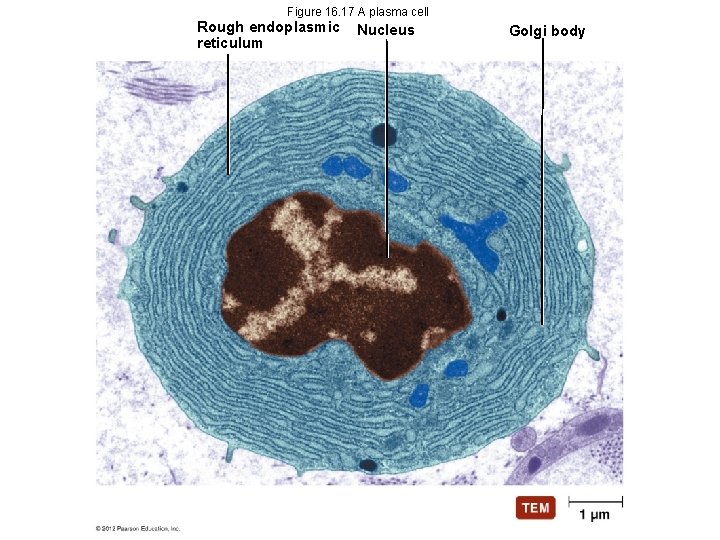
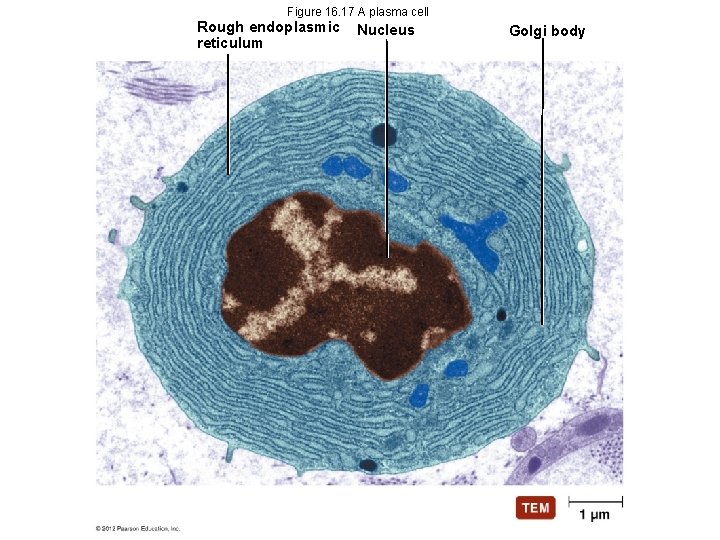
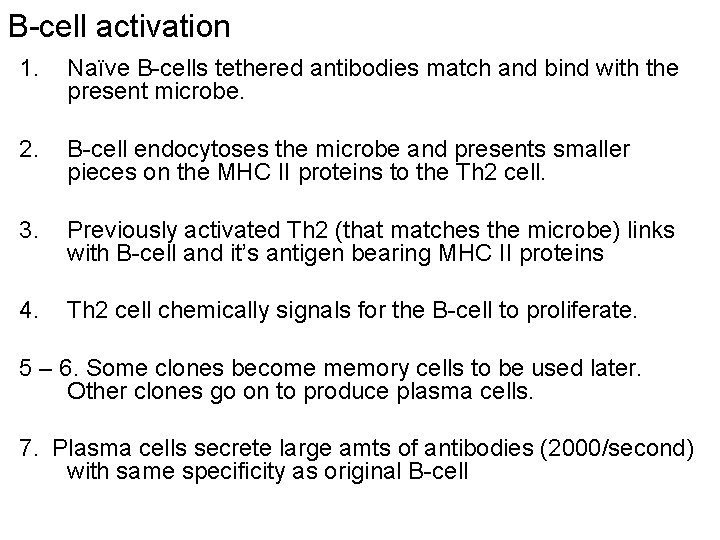
Figure 16. 17 A plasma cell Rough endoplasmic reticulum Nucleus Golgi body
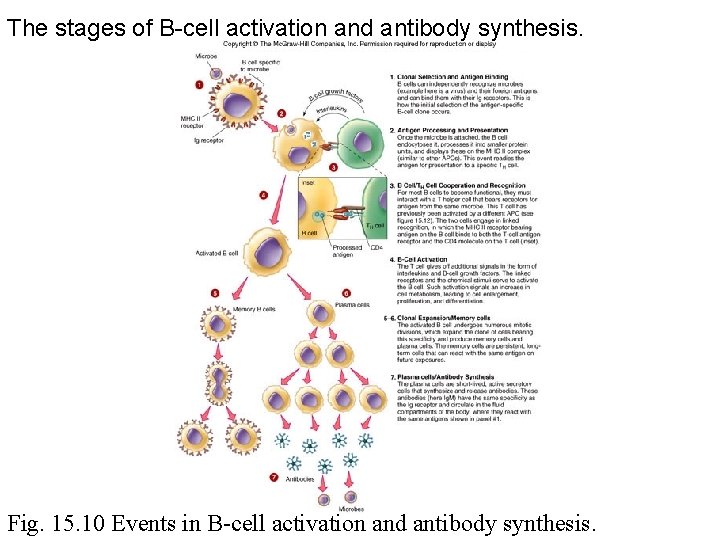
The stages of B-cell activation and antibody synthesis. Fig. 15. 10 Events in B-cell activation and antibody synthesis.
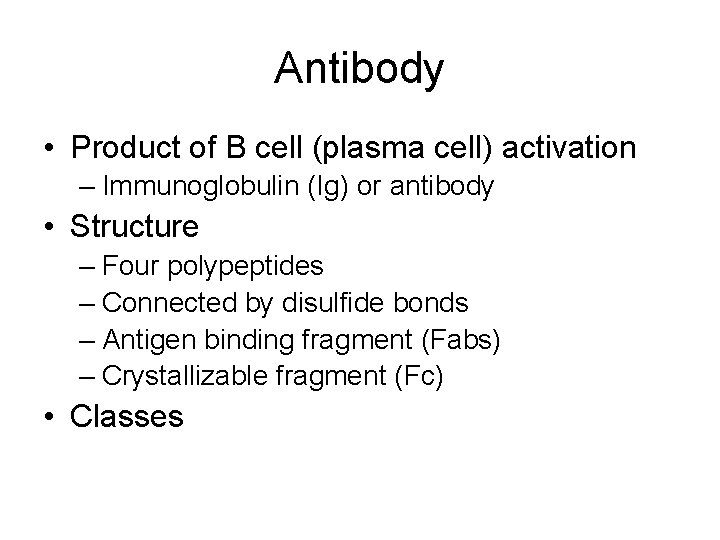
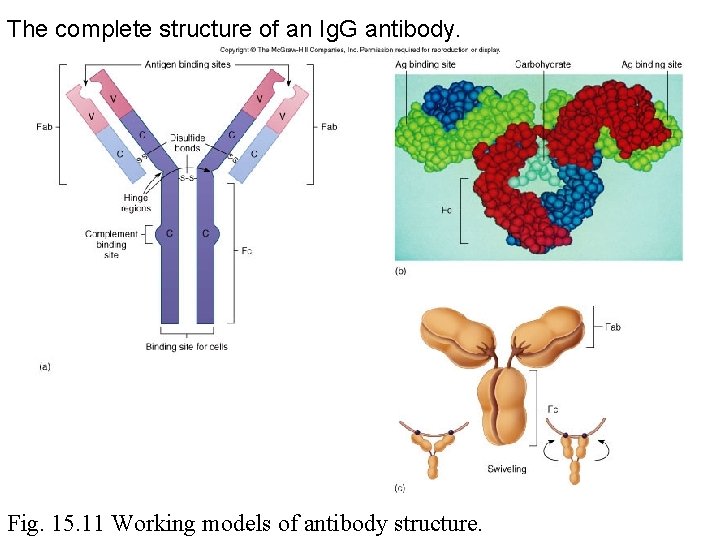
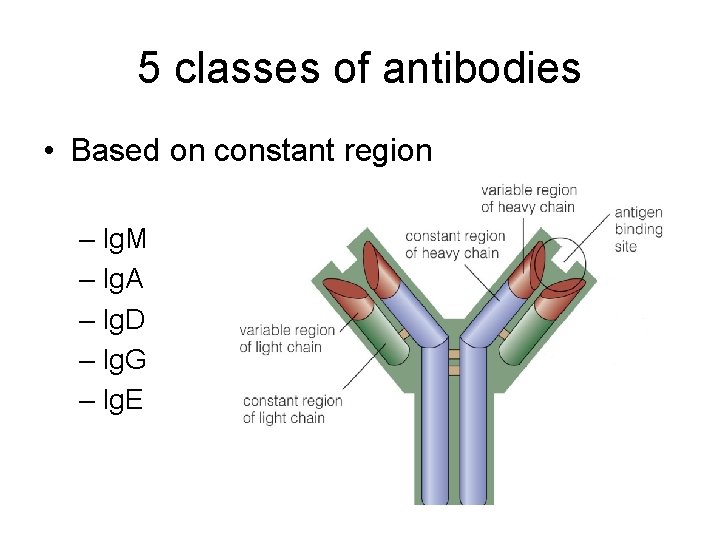
Antibody • Product of B cell (plasma cell) activation – Immunoglobulin (Ig) or antibody • Structure – Four polypeptides – Connected by disulfide bonds – Antigen binding fragment (Fabs) – Crystallizable fragment (Fc) • Classes
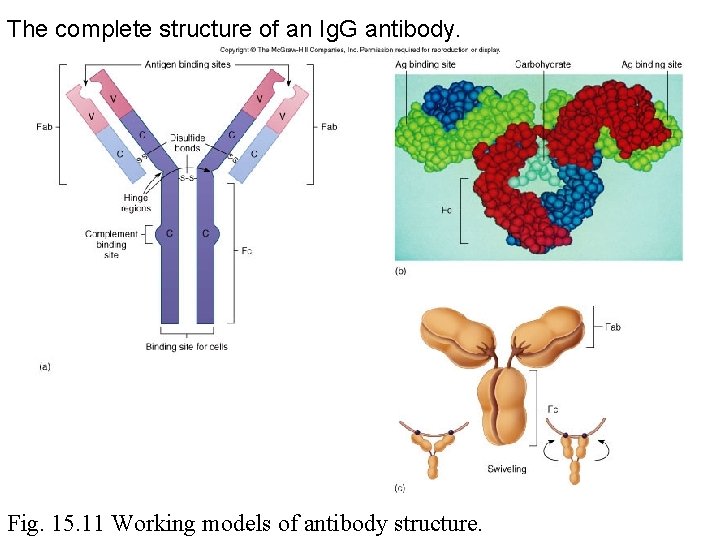
The complete structure of an Ig. G antibody. Fig. 15. 11 Working models of antibody structure.
Fab • Variable (N-terminal of the heavy and light chains) • Binds to the antigenic determinant • Swiveling enables more efficient • Held together by disulfide bonds
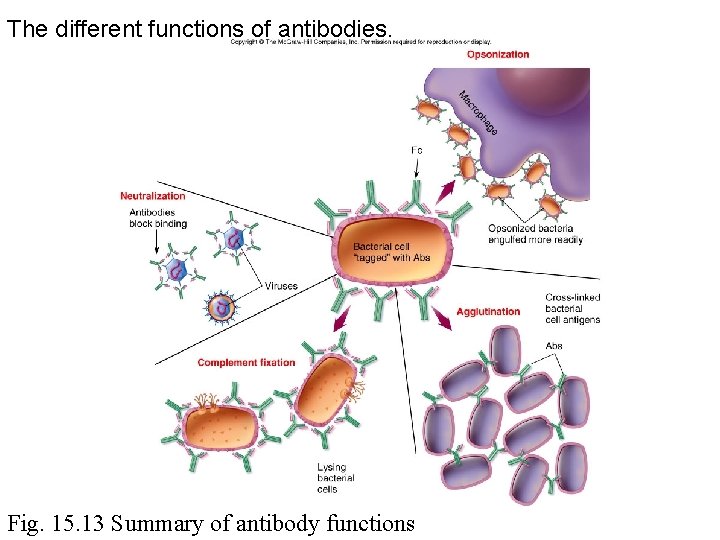
Antibody-antigen interactions • • Opsonization Agglutination Neutralization Complement fixation
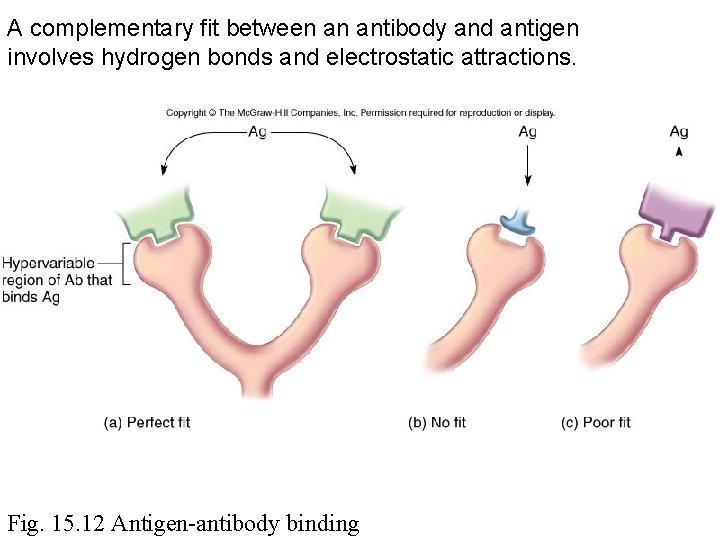
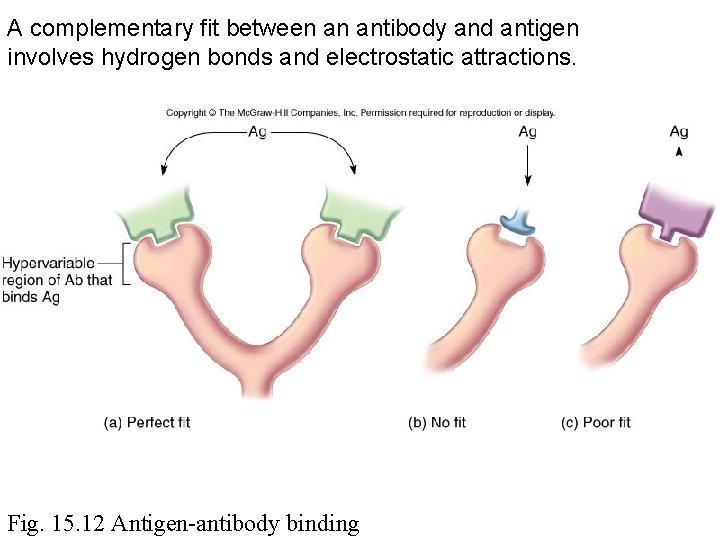
A complementary fit between an antibody and antigen involves hydrogen bonds and electrostatic attractions. Fig. 15. 12 Antigen-antibody binding
Opsonization • Microbes or particles coated with antibodies • Enables macrophages to recognize and phagocytize microbe
Agglutination • Antibodies cross-link cells or particles into clumps • Renders microbes immobile • Enhances phagocytosis • Principle for certain immune tests (RBC typing)
Neutralization • Antibody binds to – The microbe or virus receptor – Antigenic site of a molecule (Eg. Exotoxin) • Prevents further binding of microbe or toxin
Complement fixation • Antibodies interaction with complement proteins (Eg. Classical pathway) • Lysis of microbial cell
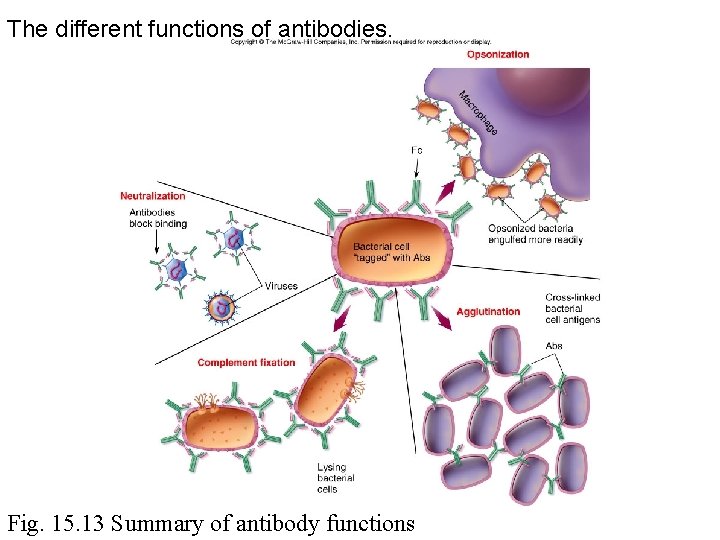
The different functions of antibodies. Fig. 15. 13 Summary of antibody functions
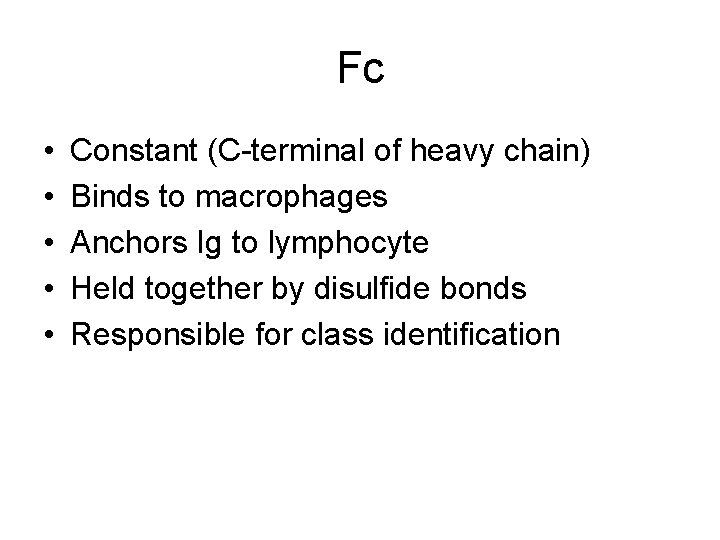
Fc • • • Constant (C-terminal of heavy chain) Binds to macrophages Anchors Ig to lymphocyte Held together by disulfide bonds Responsible for class identification
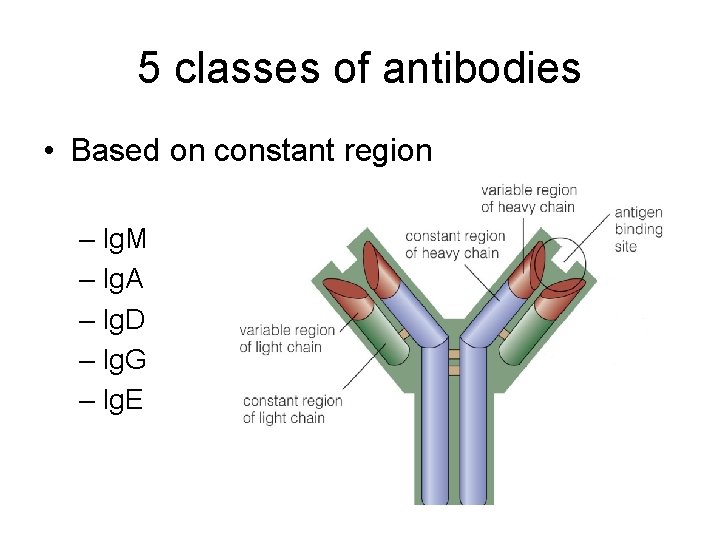
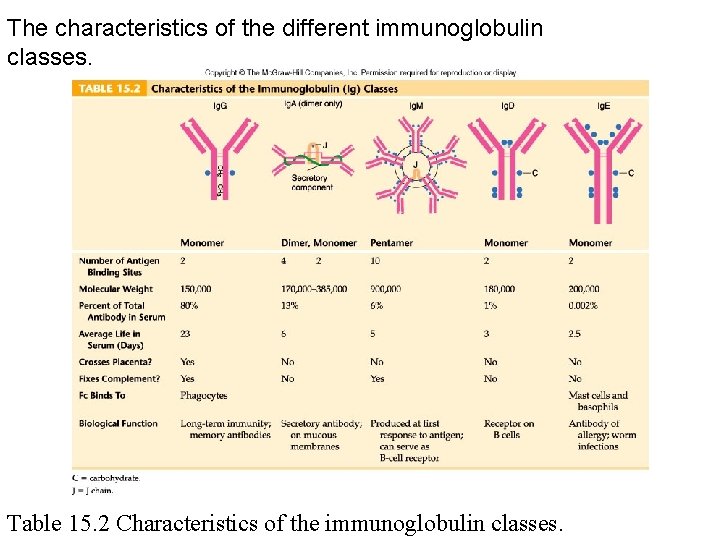
5 classes of antibodies • Based on constant region – Ig. M – Ig. A – Ig. D – Ig. G – Ig. E
Classes • Isotypes – based on the Fc fragment • Immunoglobulin (Ig) – Ig. G – Ig. A – Ig. M – Ig. D – Ig. E
Ig. G • • Monomer Primary response Memory cell response Most prevalent in tissue fluid and blood
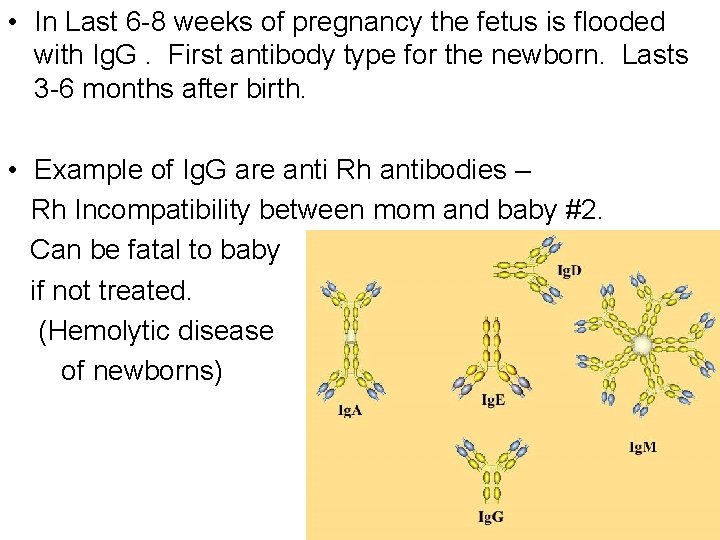
Ig. G • • 75% Most numerous Monomer- single antibody unit Located – blood, extracellular fluid physically smallest Aids in opsonization Activates complement the only antibodies that can cross from blood to tissue, and from mother to baby across placental barrier.
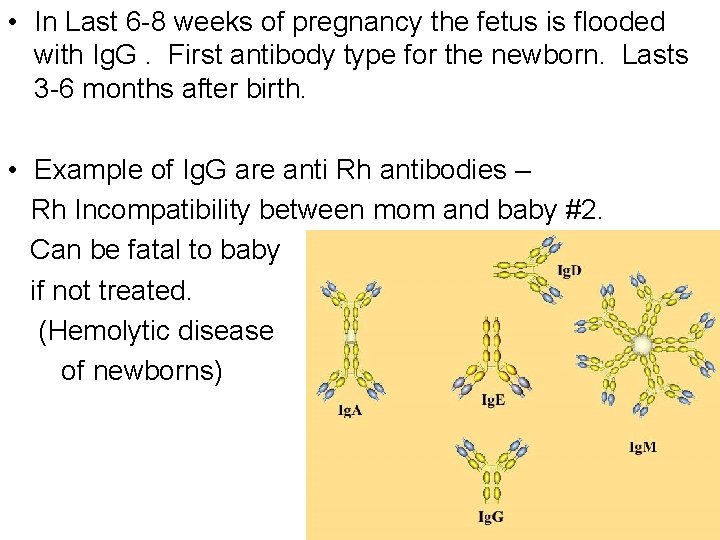
• In Last 6 -8 weeks of pregnancy the fetus is flooded with Ig. G. First antibody type for the newborn. Lasts 3 -6 months after birth. • Example of Ig. G are anti Rh antibodies – Rh Incompatibility between mom and baby #2. Can be fatal to baby if not treated. (Hemolytic disease of newborns)
Ig. A • Monomer or dimer (secretory Ig. A) • Dimer – held together by a J chain • Secretory Ig. A (mucous and serous secretions) – Local immunity – Salivary glands, intestine, nasal membrane, breast, lung, genitourinary tract • Protection for newborns
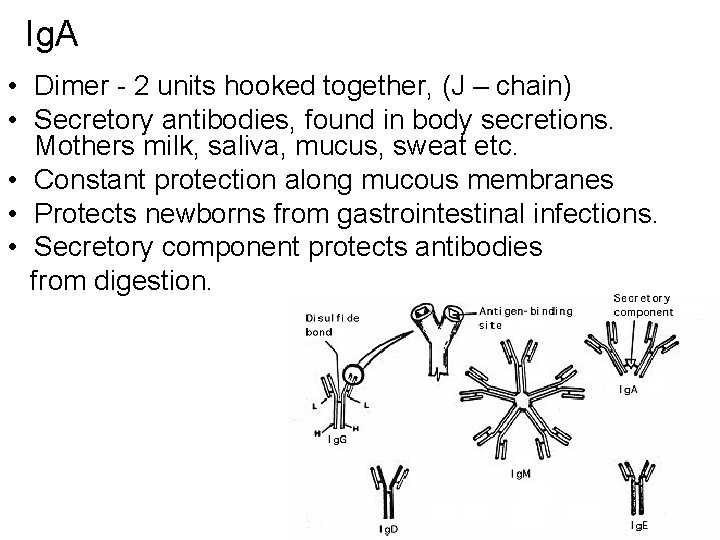
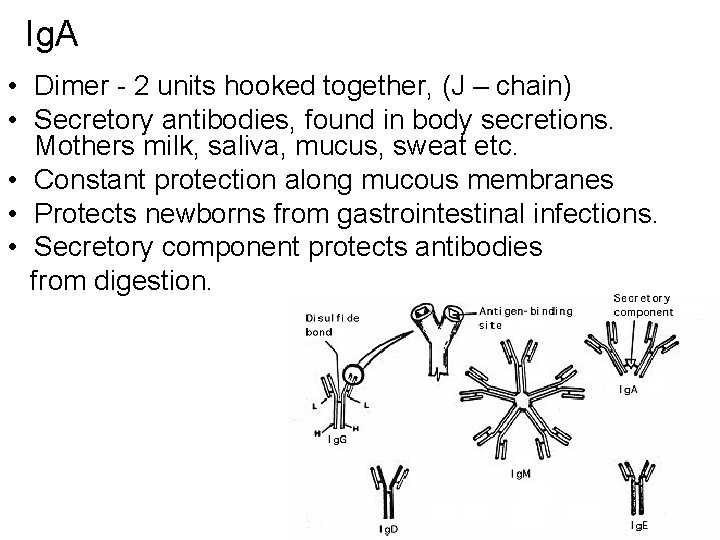
Ig. A • Dimer - 2 units hooked together, (J – chain) • Secretory antibodies, found in body secretions. Mothers milk, saliva, mucus, sweat etc. • Constant protection along mucous membranes • Protects newborns from gastrointestinal infections. • Secretory component protects antibodies from digestion.
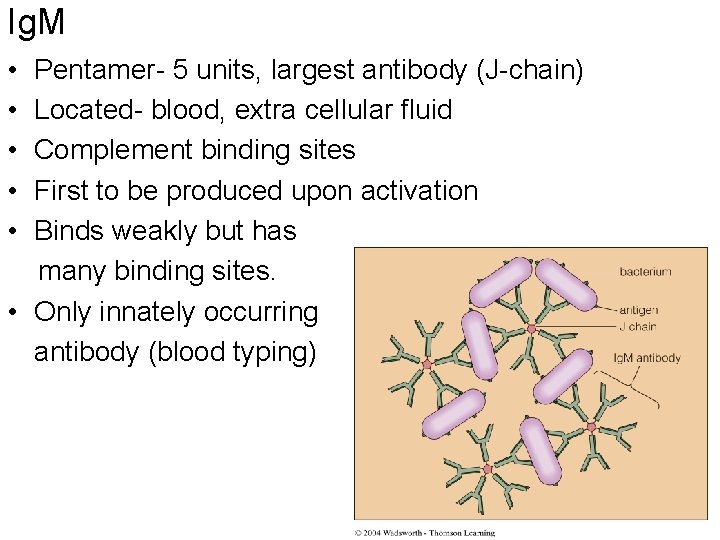
Ig. M • Five monomers • Held together by a J chain • First to be synthesized during primary immune response • Associated with complement fixation • Receptor for antigens on B cells • Circulates in the blood
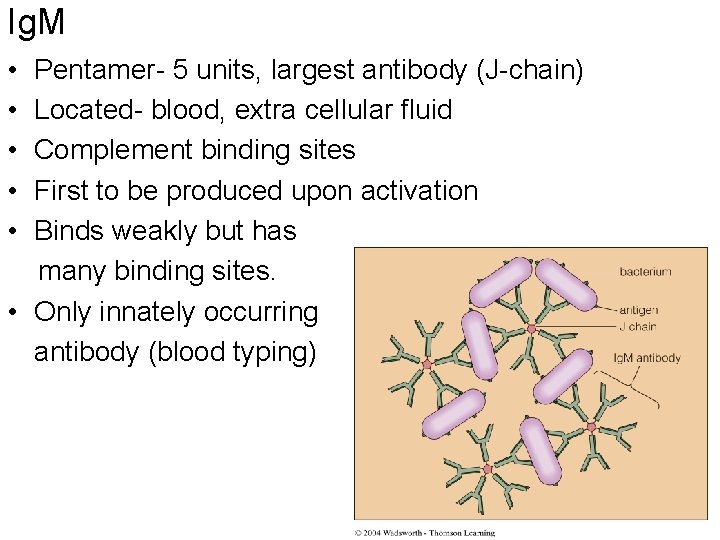
Ig. M • • • Pentamer- 5 units, largest antibody (J-chain) Located- blood, extra cellular fluid Complement binding sites First to be produced upon activation Binds weakly but has many binding sites. • Only innately occurring antibody (blood typing)
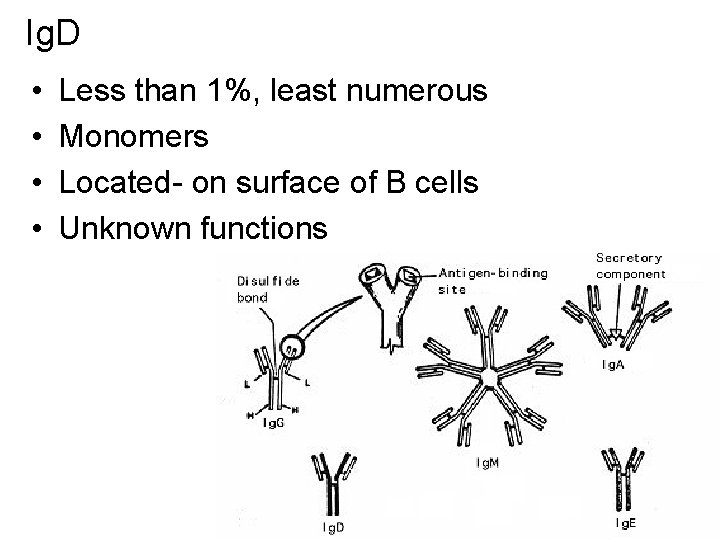
Ig. D • Monomer • Small amounts in the serum • Receptor for antigens on B cells
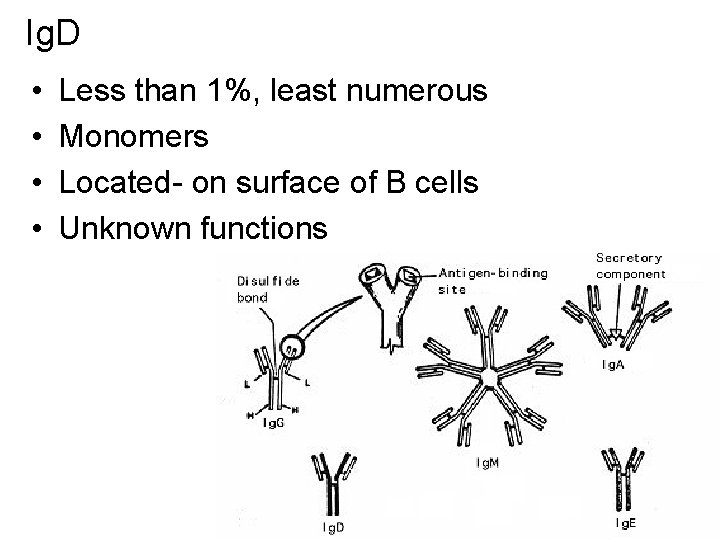
Ig. D • • Less than 1%, least numerous Monomers Located- on surface of B cells Unknown functions
Ig. E • Allergies • Parasite infections • Fc portion binds to mast cells and basophils – release chemical mediators that aid inflammation
Ig. E • Monomer • Located – on surface of mast cells, eosinophils and basophils • Membrane binding site Allergy antibodies, and helps to control worms by bursting the above mentioned cells.
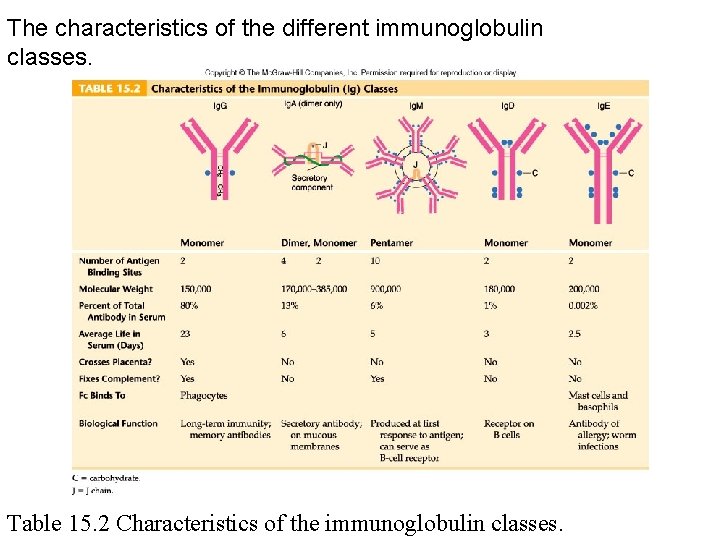
The characteristics of the different immunoglobulin classes. Table 15. 2 Characteristics of the immunoglobulin classes.
Response • Primary • Secondary
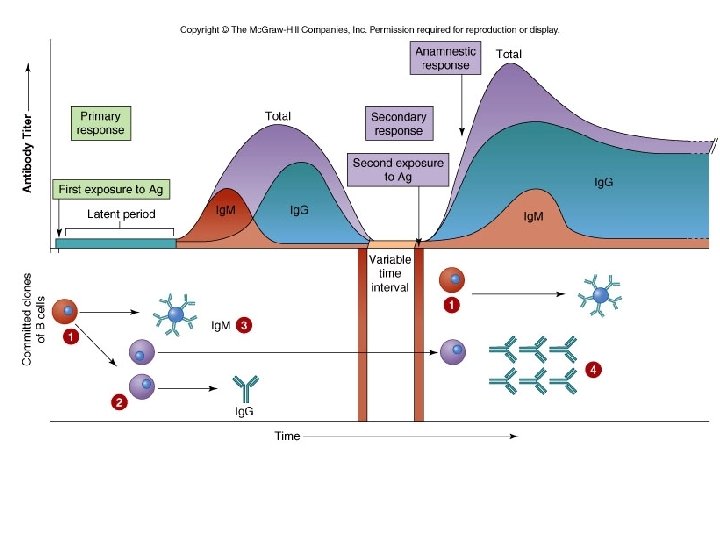
Primary • First exposure – Latent period • Lack of antibodies synthesis – Synthesis of antibodies • Level of synthesis (titer) • Ig. M first • Followed by Ig. G, and some Ig. A and Ig. M
Secondary • Re-exposure to the same immunogen (Anamnestic response) • Antibody synthesis, titer, and length of antibody persistence is rapid and amplified – Primarily due to memory cells
Reactivation: immunological memory • Plasma cells die once the infection is over • Memory cells persist long after the primary infection. They provide immunological memory • Primary response can take 1 to 2 weeks to take real effect. • Secondary response produces antibodies in a few days.
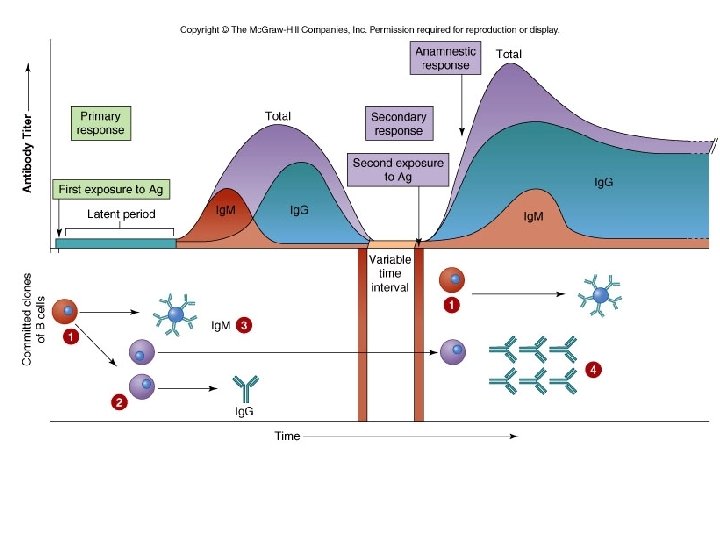
• Memory b-cells – Are more numerous than naïve B cells – Have a higher affinity antibodies due to previous activation Can eliminate pathogens from the body before sign and symptoms. Vaccines confer this type of immunity.
T cell • Activation • Types
Activation • Cell-mediated immunity • Antigen presenting cells • Transformation
Cell-mediated immunity • Direct involvement of T cells • Produce and react to cytokines • Activated simultaneously with B cell activation • Subset of T cells have unique CD receptors (CD 4, CD 8)
Elements of Adaptive Immunity • Immune System Cytokines – Interleukins (ILs) • Signal among leukocytes – Interferons (IFNs) • Antiviral proteins that may act as cytokines – Growth factors • Proteins that stimulate stem cells to divide – Tumor necrosis factor (TNF) • Secreted by macrophages and T cells to kill tumor cells and regulate immune responses and inflammation – Chemokines • Chemotactic cytokines that signal leukocytes to move © 2012 Pearson Education Inc.
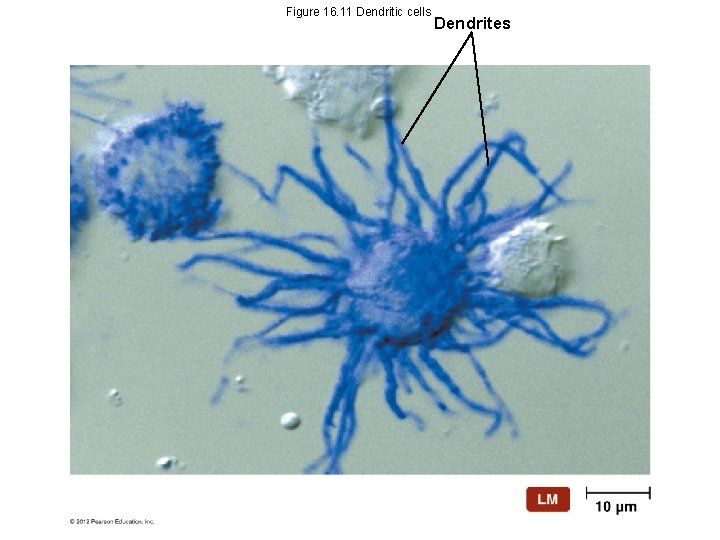
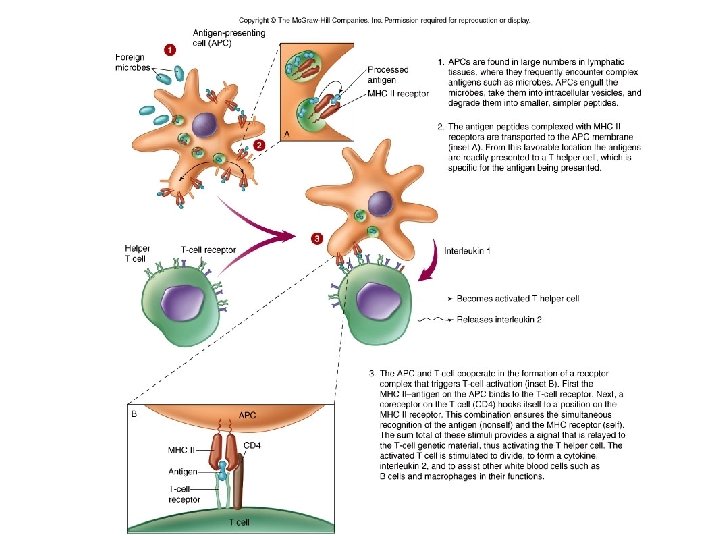
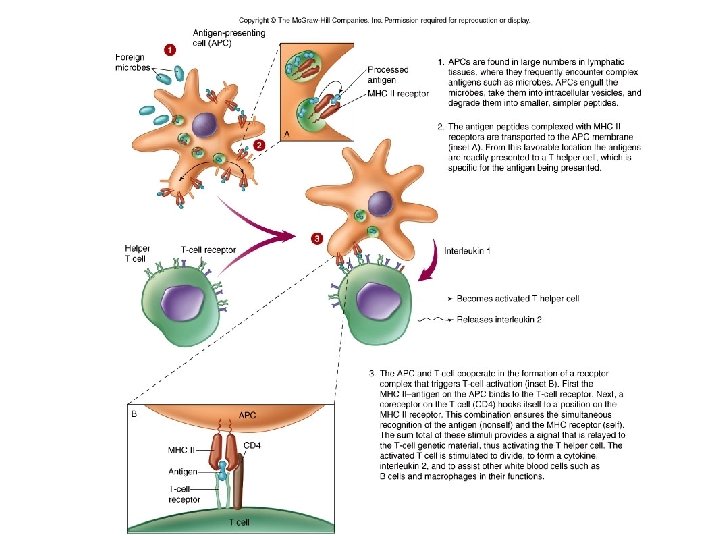
Antigen presenting cells (APC) • Macrophages and dendritic cells – Process and present antigen in association with MHC II – T cell CD receptor recognize antigen/MHC II
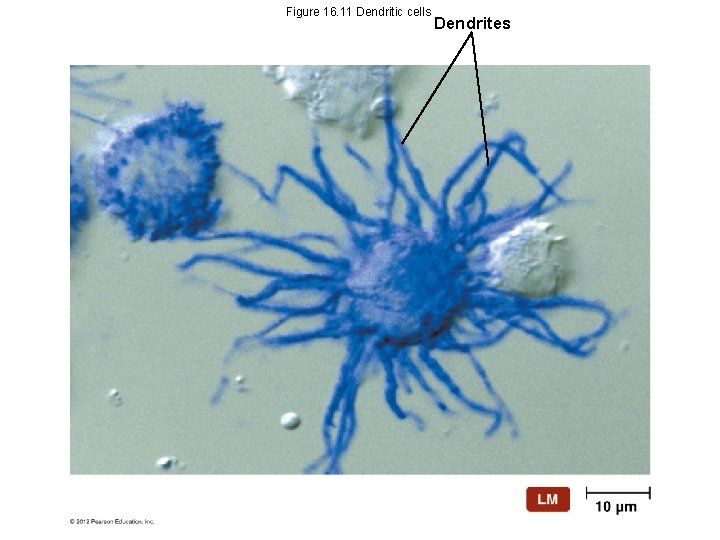
Figure 16. 11 Dendritic cells Dendrites
Transformation • Activated T cells prepare for mitosis • Effectors cells or types (TH, TC) are produced • Memory cells are produced
Types • Helper T cells (TH) • Cytotoxic T cells (TC)
TH • Regulate immune reactions to antigens by releasing cytokines • CD 4 receptor • Type of cytokine will determine subset of TH – TH 1 (activate other T cells, delayed type hypersensitivity) – TH 2 (B cell differentiation) • Cytokines also activate macrophages • Most prevalent in the blood Insert animation. 0083 T helper cell dependent antigen
T Helper (Th cell) • Regulates immune reactions of B cells and T cells • Involved in activating macrophages and improving opsonization • Most prevalent type of T cell in the blood and lymph organs (HIV depresses CD 4 cells) • Th 1 (activates more T cells) and Th 2 (enhance B cell activation) is defined by the type of interleukin released by the APC during activation.
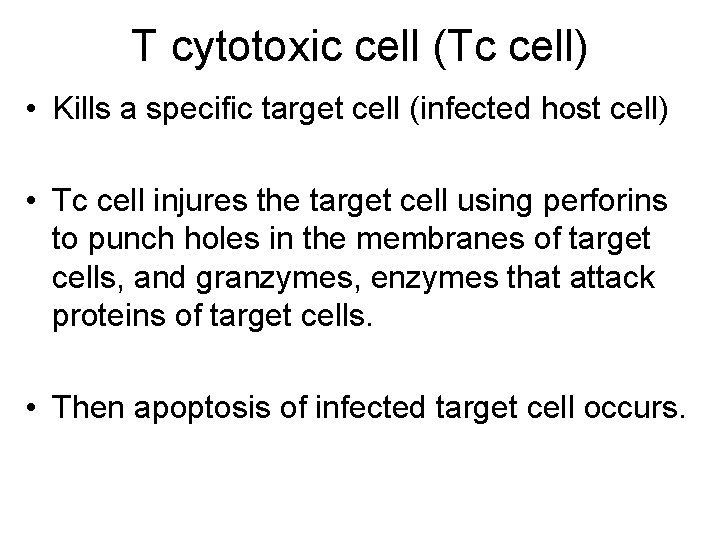
TC • Binds and lyses cells (apoptosis) – microbe, viral infected cells, foreign cells, cancer cells • • CD 8 receptor Perforins – punch holes in the membrane Granzymes – degrade proteins Natural killer (NK) cells – related to TC – attack virus infected cells and cancer cells Insert animation. 0034 Cytotoxic T cell
T cytotoxic cell (Tc cell) • Kills a specific target cell (infected host cell) • Tc cell injures the target cell using perforins to punch holes in the membranes of target cells, and granzymes, enzymes that attack proteins of target cells. • Then apoptosis of infected target cell occurs.
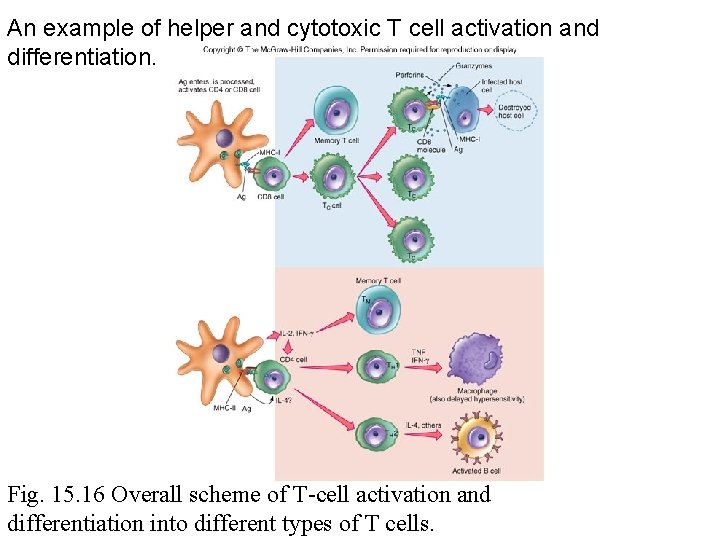
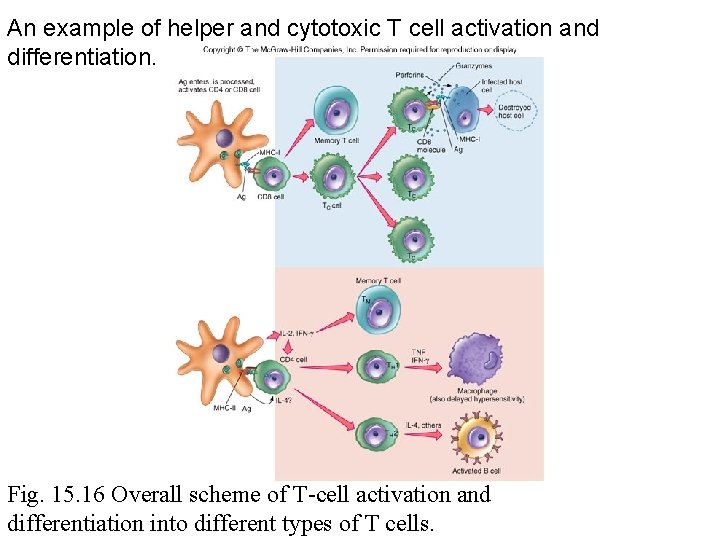
An example of helper and cytotoxic T cell activation and differentiation. Fig. 15. 16 Overall scheme of T-cell activation and differentiation into different types of T cells.
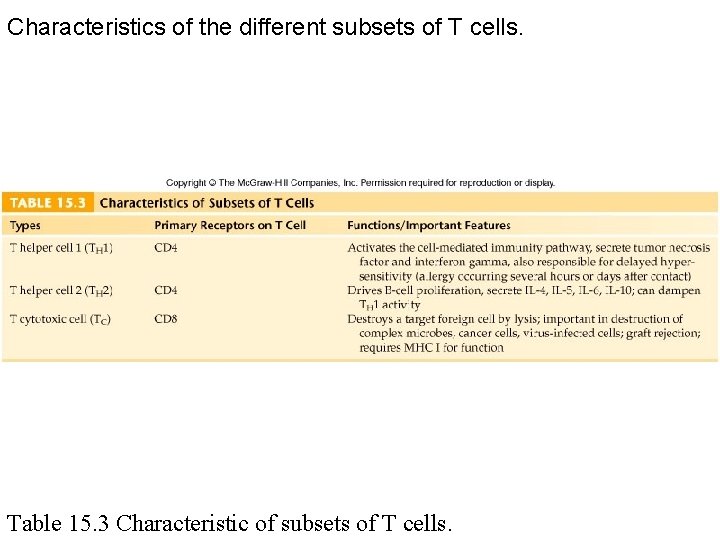
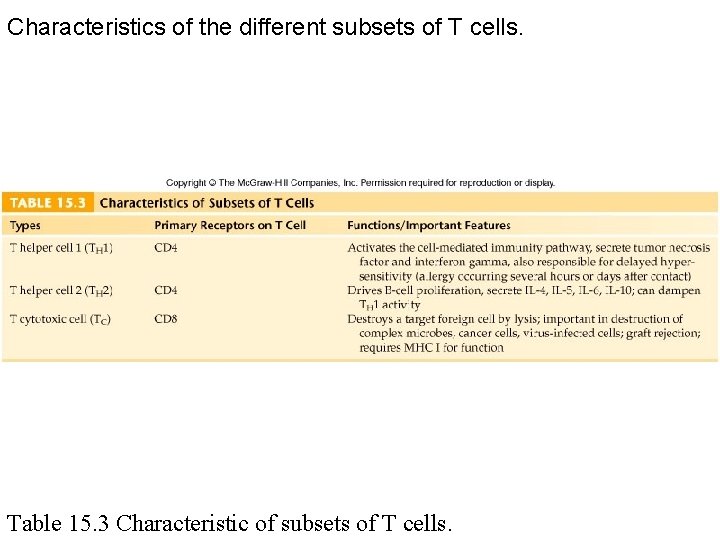
Characteristics of the different subsets of T cells. Table 15. 3 Characteristic of subsets of T cells.
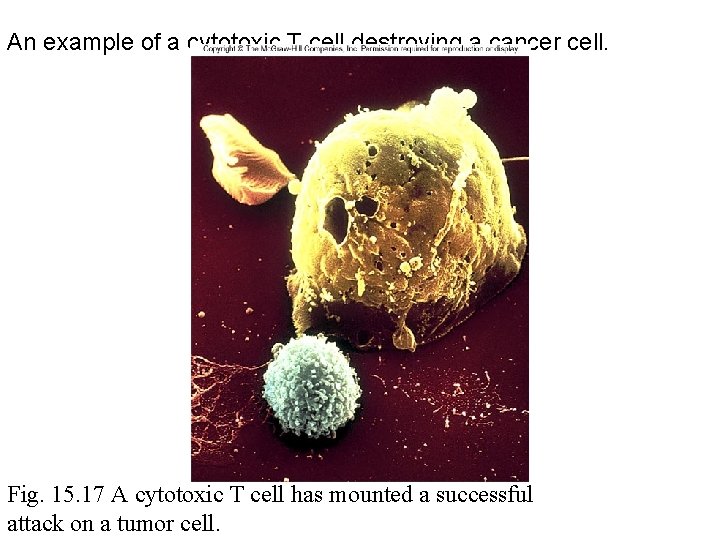
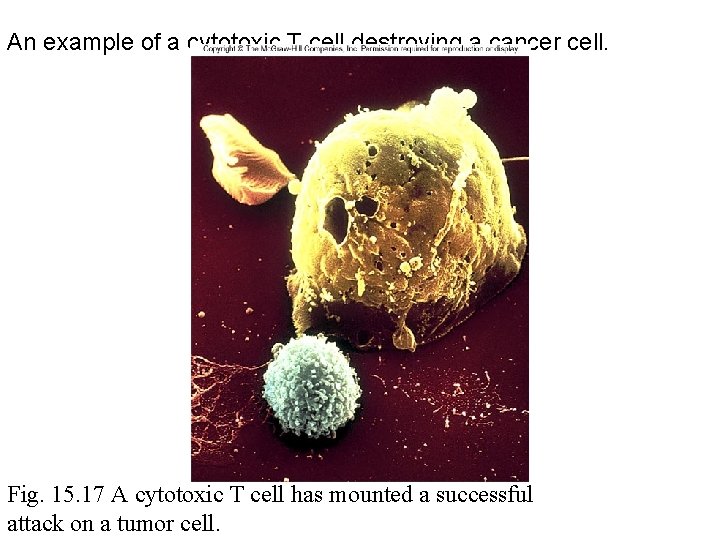
An example of a cytotoxic T cell destroying a cancer cell. Fig. 15. 17 A cytotoxic T cell has mounted a successful attack on a tumor cell.
Chapter 17 - Immunization Specific Immunities • • • Active Passive Natural Artificial Vaccines
Immunization • Brief History of Immunization – Chinese noticed children who recovered from smallpox did not contract the disease again – They infected children with material from a smallpox scab to induce immunity • This process known as variolation – Variolation spread to England America but was stopped because of risk of death © 2012 Pearson Education Inc.
Immunization • Brief History of Immunization – 1796 – Edward Jenner discovered process of vaccination – 1879 – Louis Pasteur developed a vaccine against Pasteurella multocida – Antibody transfer developed when it was discovered vaccines protected through the action of antibodies © 2012 Pearson Education Inc.
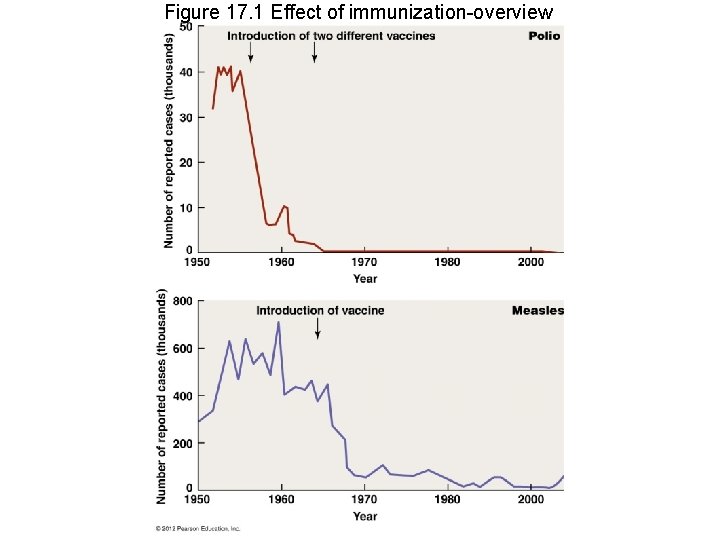
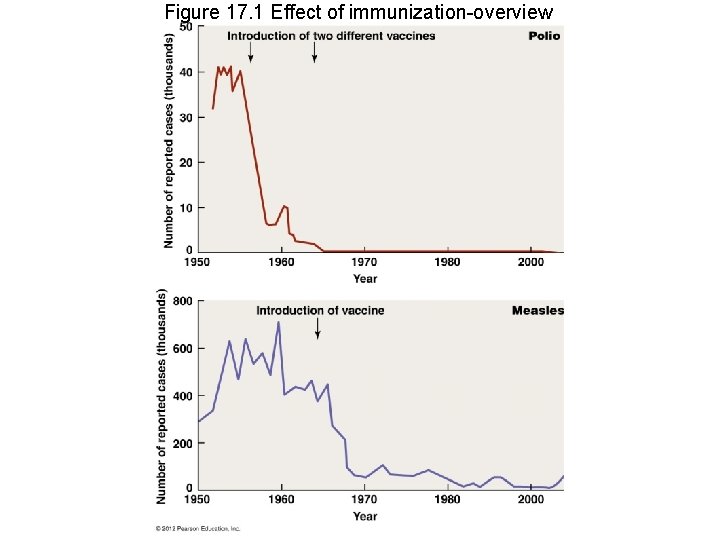
Figure 17. 1 Effect of immunization-overview
Immunization • Brief History of Immunization – Many developing nations do not receive vaccines – Effective vaccines not developed for some pathogens – Vaccine-associated risks discourage investment in developing new vaccines © 2012 Pearson Education Inc.
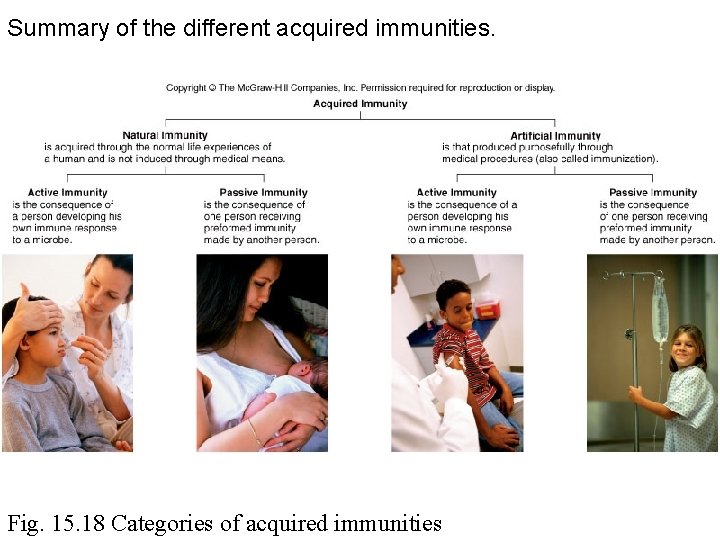
Active • • Natural or artificial Antigen activates B and T cells Memory cells Long-term protection
Passive • Natural or artificial • Receive antibodies from another individual or animal • No memory cells • No antibody production • Short-term protection
Natural • Immunity produced by normal biological experiences, no medical intervention – Natural active • Eg. Infection – Natural passive • Eg. Mother to child
Artificial • Immune protection through medical procedures or intervention – Artificial active • Eg. vaccination – Artificial passive • Eg. immunotherapy
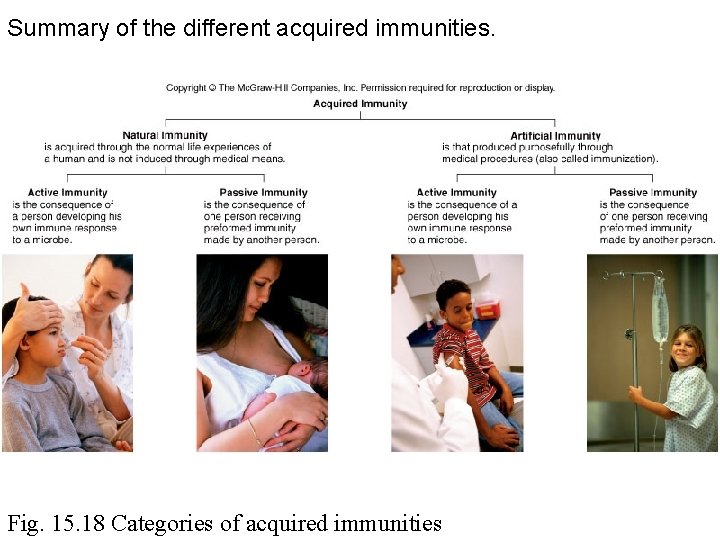
Summary of the different acquired immunities. Fig. 15. 18 Categories of acquired immunities
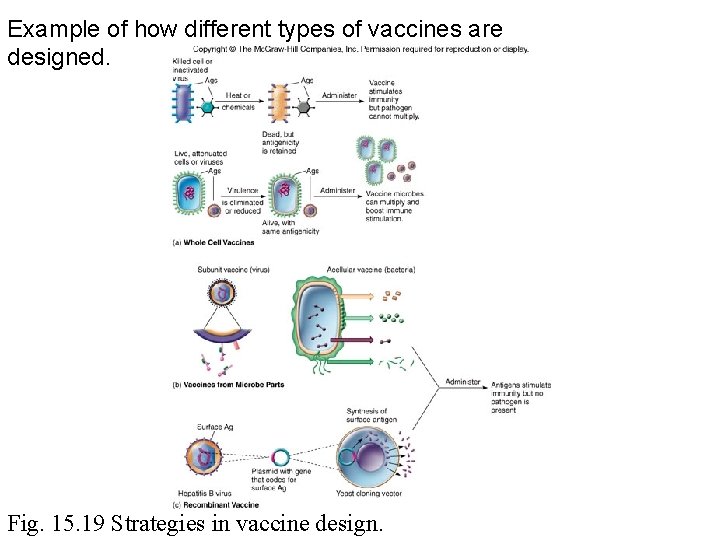
Vaccines • Types – Killed whole cell or inactivated viruses – Live, attenuated cells or viruses – Antigenic molecules from bacteria or viruses – Genetically engineered microbes or microbial antigens
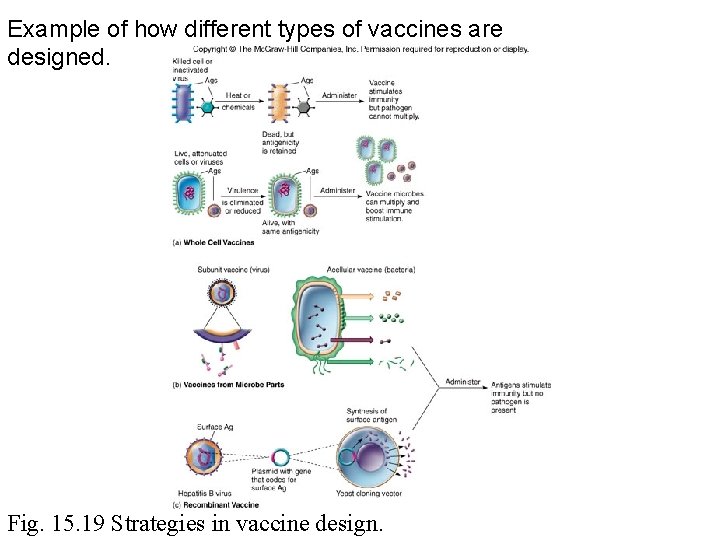
Example of how different types of vaccines are designed. Fig. 15. 19 Strategies in vaccine design.
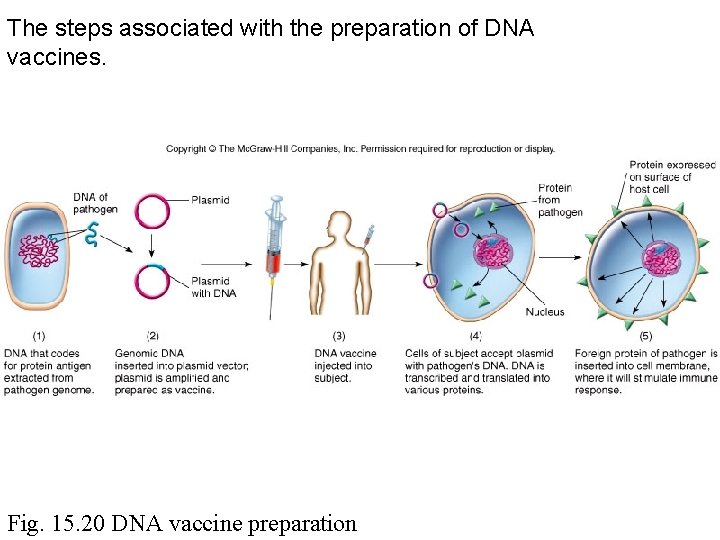
New vaccines • DNA vaccines – Insert microbial DNA into plasmid – Inoculate recipient with plasmid – Host cell expresses microbial DNA – Immune system reacts to microbial antigen expressed on the host cell surface
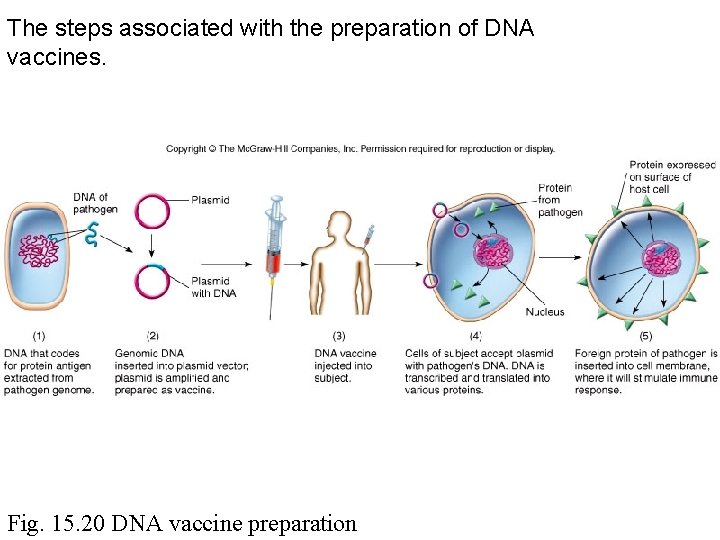
The steps associated with the preparation of DNA vaccines. Fig. 15. 20 DNA vaccine preparation
Benefits of vaccinations • Long-lasting immunity • Herd immunity – Indirect protection of nonimmune – Prevents epidemics
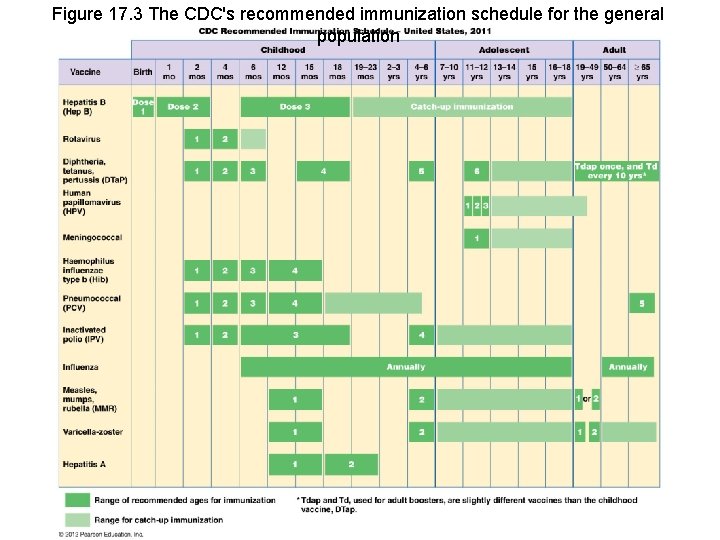
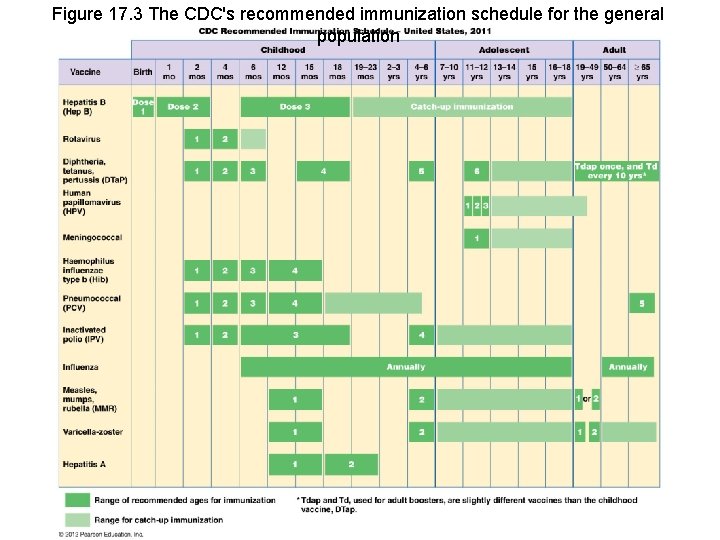
Figure 17. 3 The CDC's recommended immunization schedule for the general population
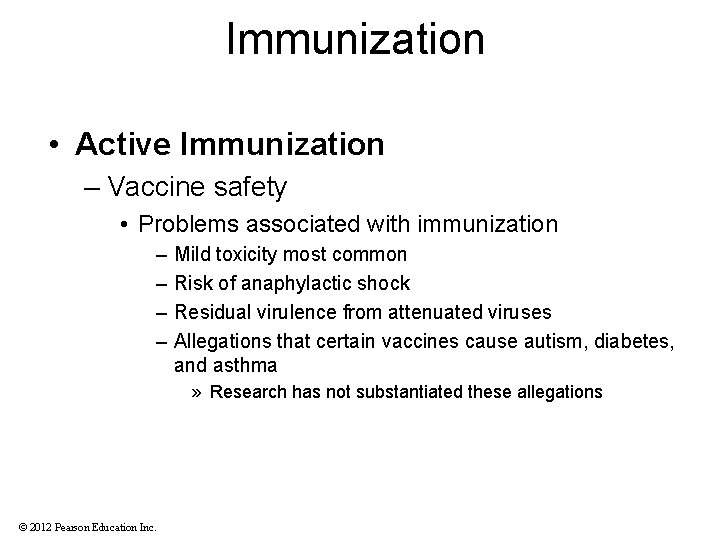
Immunization • Active Immunization – Vaccine safety • Problems associated with immunization – – Mild toxicity most common Risk of anaphylactic shock Residual virulence from attenuated viruses Allegations that certain vaccines cause autism, diabetes, and asthma » Research has not substantiated these allegations © 2012 Pearson Education Inc.
