STUDY OF IMMUNITY NONSPECIFIC RESISTANCE 1 Immunity Types
- Slides: 25
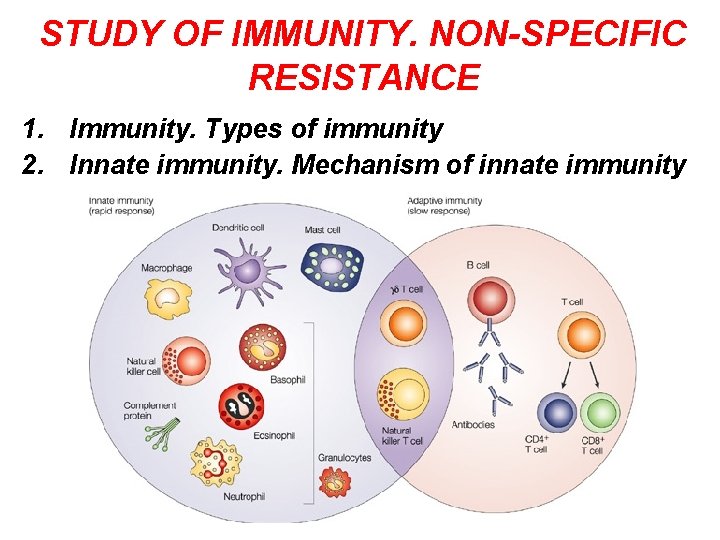
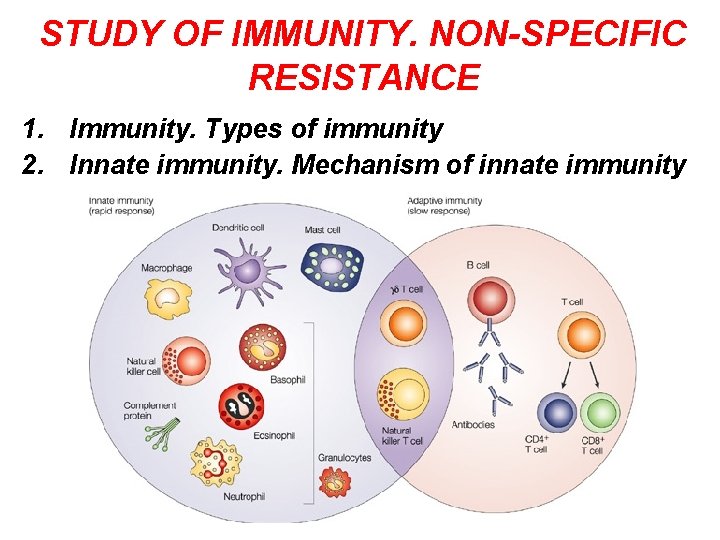
STUDY OF IMMUNITY. NON-SPECIFIC RESISTANCE 1. Immunity. Types of immunity 2. Innate immunity. Mechanism of innate immunity
IMMUNITY • The resistance offered by the host to the harmful effect of pathogenic microbial infection is called immunity. Immunity against infectious diseases is of different types.
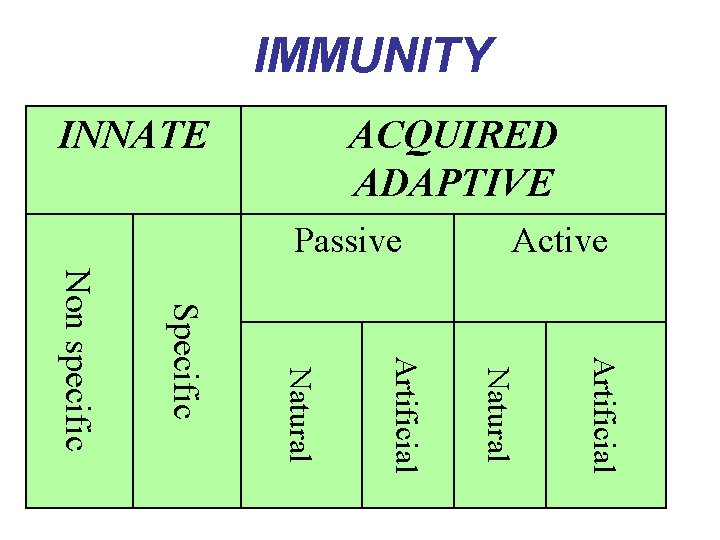
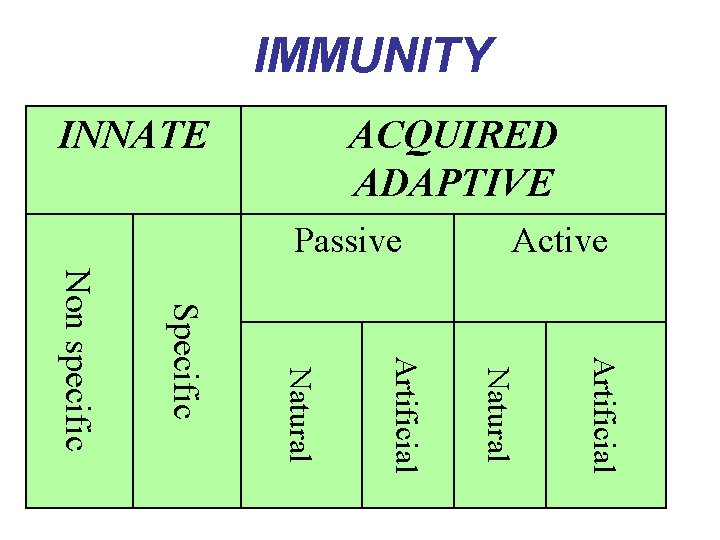
IMMUNITY ACQUIRED ADAPTIVE INNATE Active Passive Artificial Natural Specific Non specific
INNATE IMMUNITY • This is basic immunity, which may be genetically passed on from one generation to other generation • It does not depend on prior contacts with microorganisms • It may be non-specific when it indicates a degree of resistance to all infection • It is specific when it shows resistance to particular pathogens
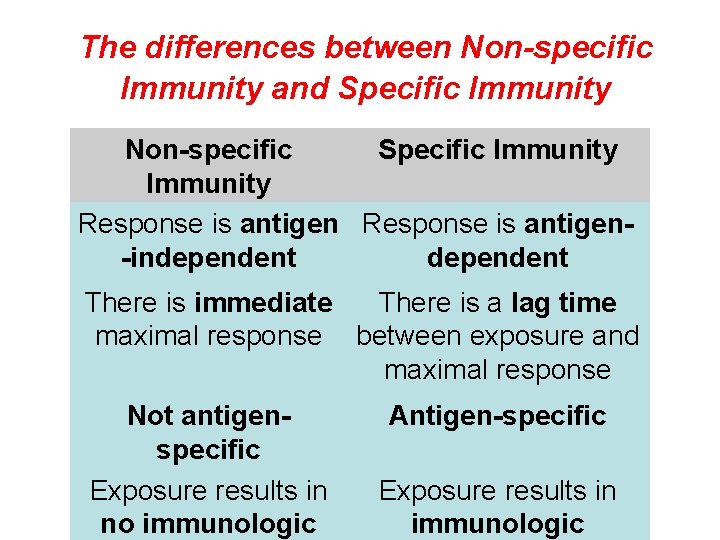
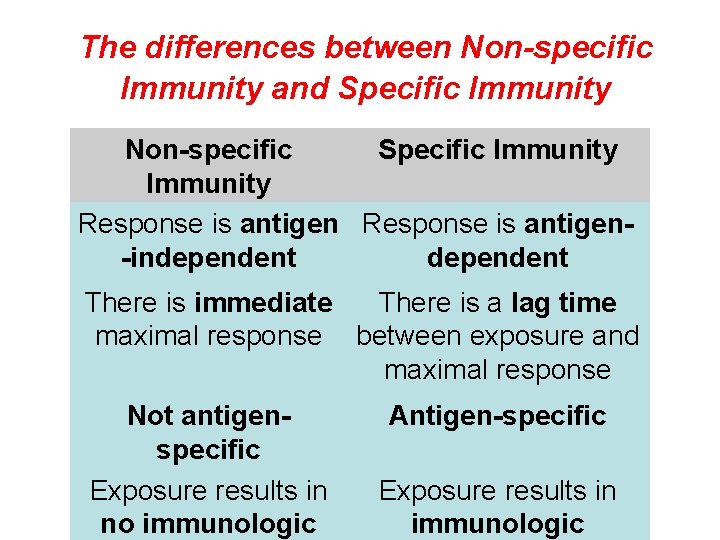
The differences between Non-specific Immunity and Specific Immunity Non-specific Specific Immunity Response is antigen-independent There is immediate There is a lag time maximal response between exposure and maximal response Not antigenspecific Exposure results in no immunologic Antigen-specific Exposure results in immunologic
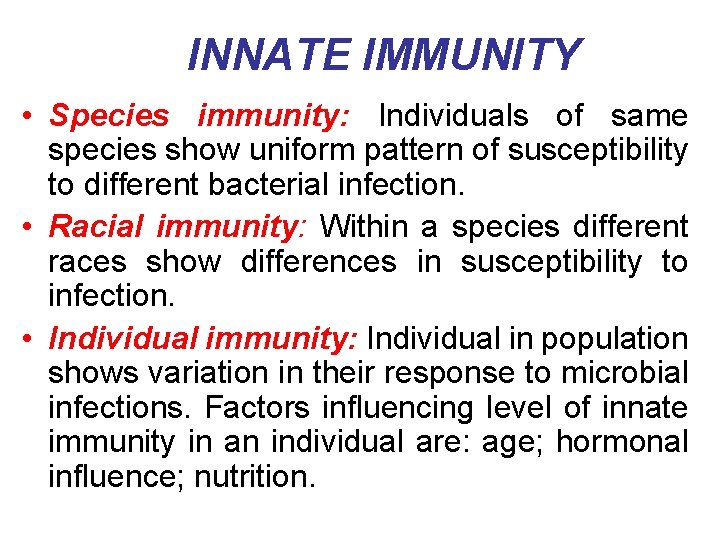
INNATE IMMUNITY • Species immunity: Individuals of same species show uniform pattern of susceptibility to different bacterial infection. • Racial immunity: Within a species different races show differences in susceptibility to infection. • Individual immunity: Individual in population shows variation in their response to microbial infections. Factors influencing level of innate immunity in an individual are: age; hormonal influence; nutrition.
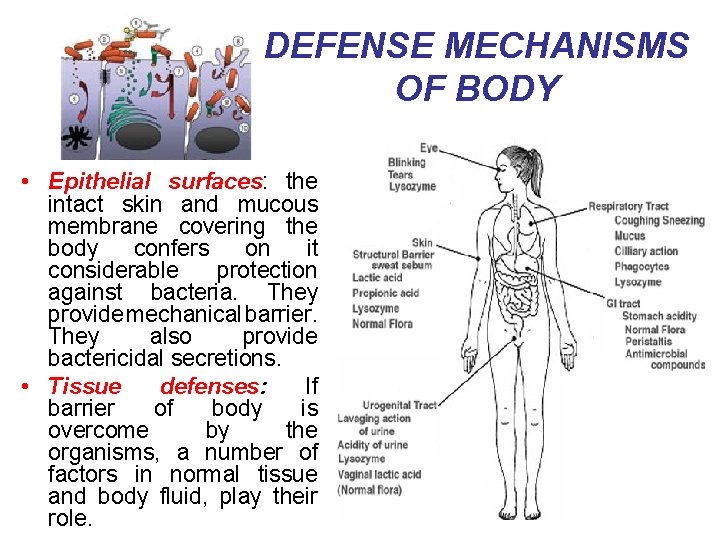
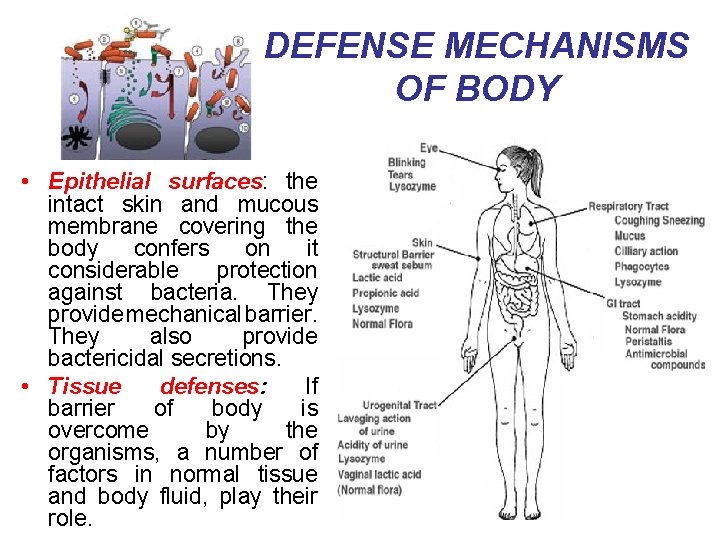
DEFENSE MECHANISMS OF BODY • Epithelial surfaces: the intact skin and mucous membrane covering the body confers on it considerable protection against bacteria. They provide mechanical barrier. They also provide bactericidal secretions. • Tissue defenses: If barrier of body is overcome by the organisms, a number of factors in normal tissue and body fluid, play their role.
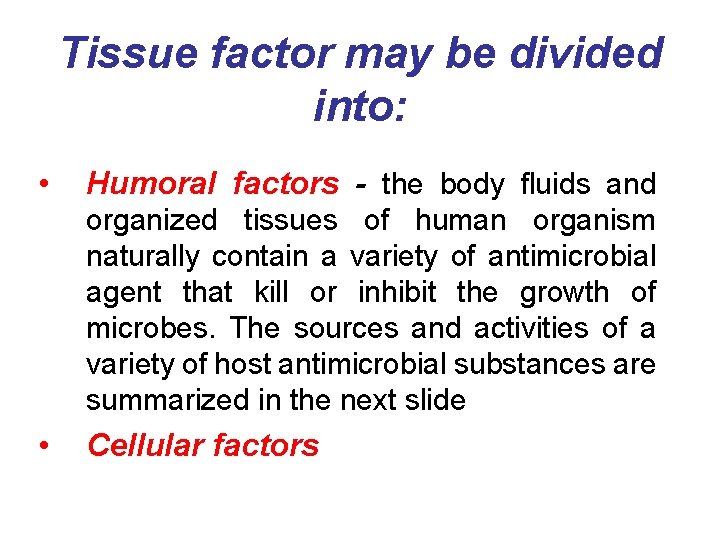
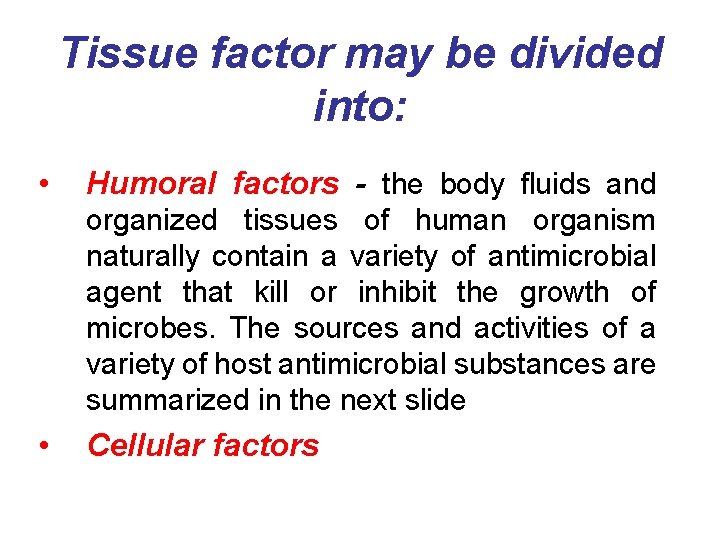
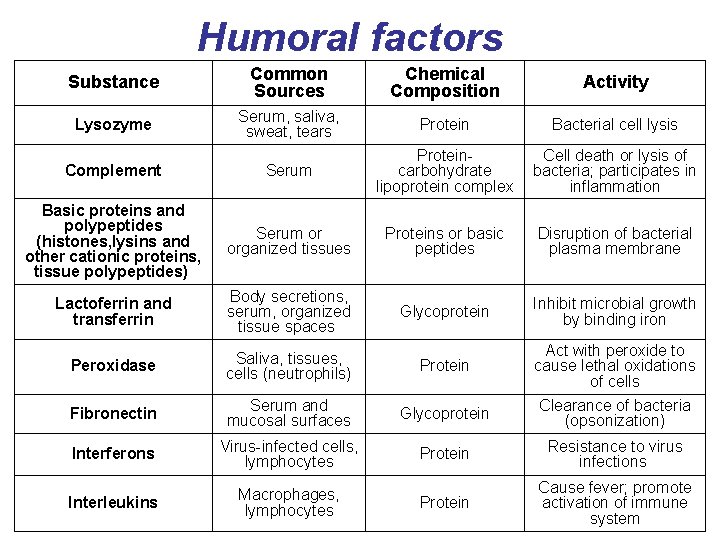
Tissue factor may be divided into: • Humoral factors - the body fluids and organized tissues of human organism naturally contain a variety of antimicrobial agent that kill or inhibit the growth of microbes. The sources and activities of a variety of host antimicrobial substances are summarized in the next slide • Cellular factors
Humoral factors Substance Common Sources Chemical Composition Activity Lysozyme Serum, saliva, sweat, tears Protein Bacterial cell lysis Complement Serum Proteincarbohydrate lipoprotein complex Cell death or lysis of bacteria; participates in inflammation Basic proteins and polypeptides (histones, lysins and other cationic proteins, tissue polypeptides) Serum or organized tissues Proteins or basic peptides Disruption of bacterial plasma membrane Lactoferrin and transferrin Body secretions, serum, organized tissue spaces Glycoprotein Inhibit microbial growth by binding iron Peroxidase Saliva, tissues, cells (neutrophils) Protein Act with peroxide to cause lethal oxidations of cells Fibronectin Serum and mucosal surfaces Glycoprotein Clearance of bacteria (opsonization) Interferons Virus-infected cells, lymphocytes Protein Resistance to virus infections Interleukins Macrophages, lymphocytes Protein Cause fever; promote activation of immune system
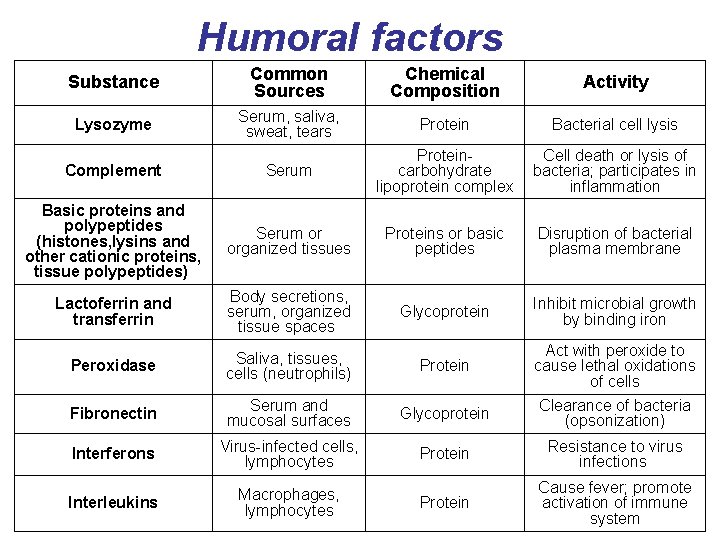
MICROBIAL ANTAGONISM • This refers to the protection of the surfaces afforded by an intact normal flora in a healthy organism E. coli bacteria (yellow) in the gut are part of the normal intestinal flora of humans
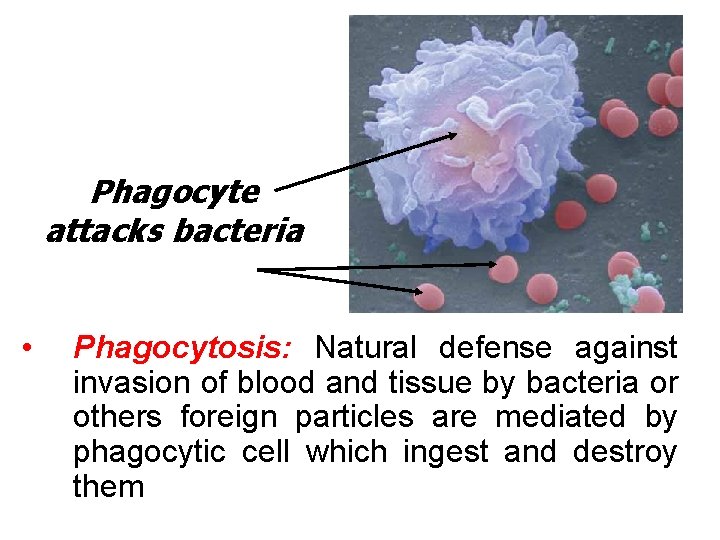
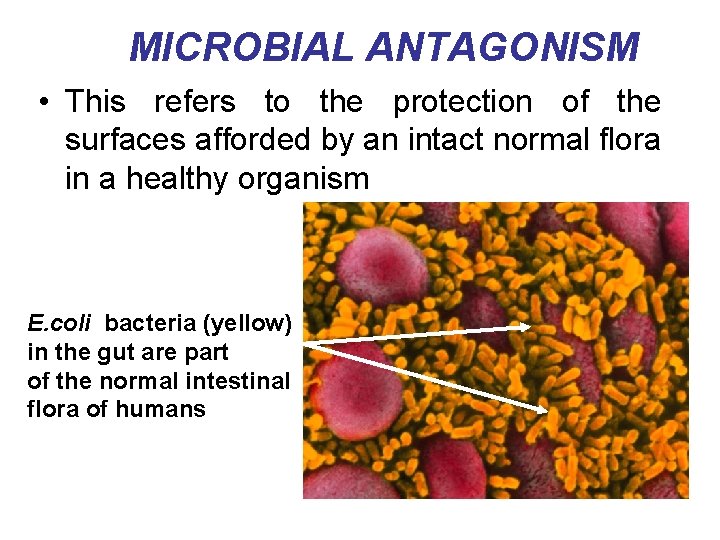
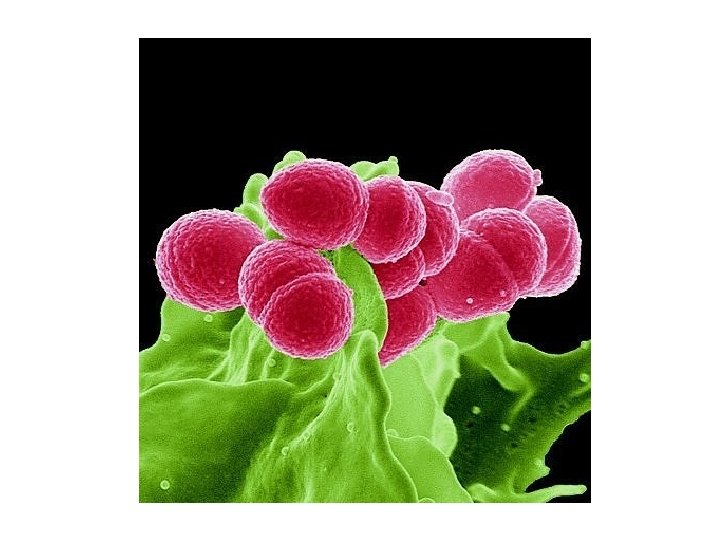
Phagocyte attacks bacteria • Phagocytosis: Natural defense against invasion of blood and tissue by bacteria or others foreign particles are mediated by phagocytic cell which ingest and destroy them
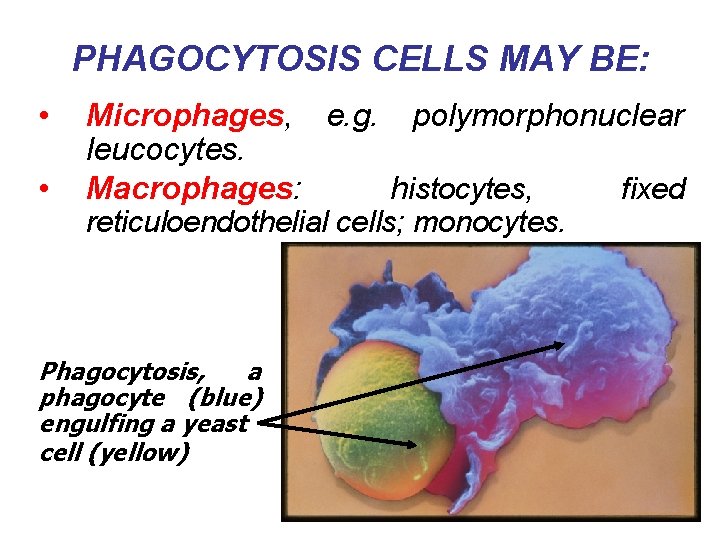
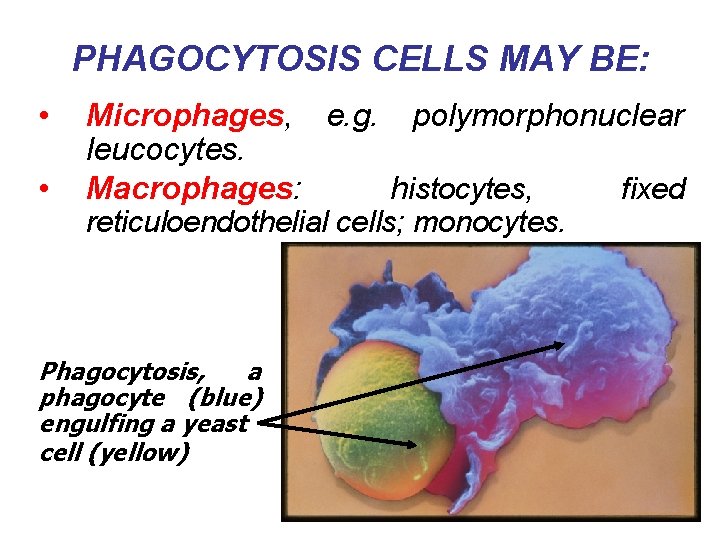
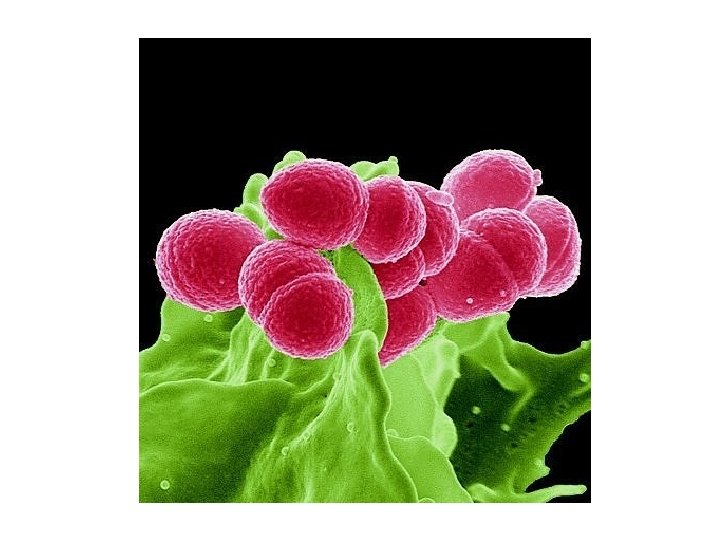
PHAGOCYTOSIS CELLS MAY BE: • • Microphages, e. g. polymorphonuclear leucocytes. Macrophages: histocytes, fixed reticuloendothelial cells; monocytes. Phagocytosis, a phagocyte (blue) engulfing a yeast cell (yellow)
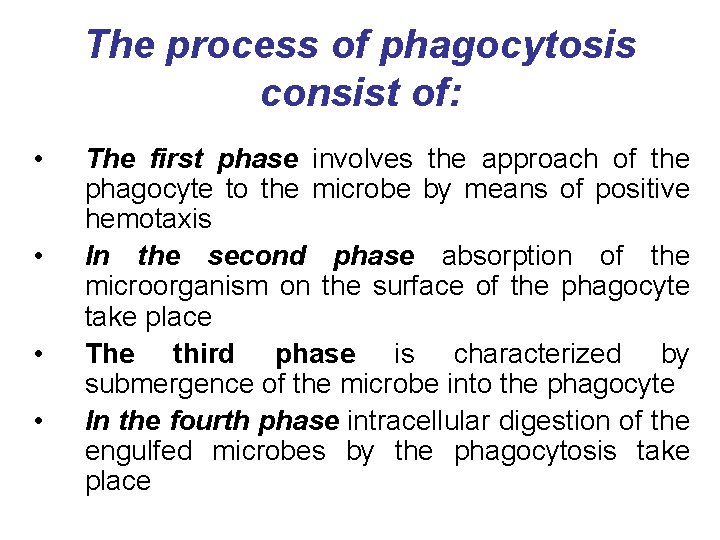
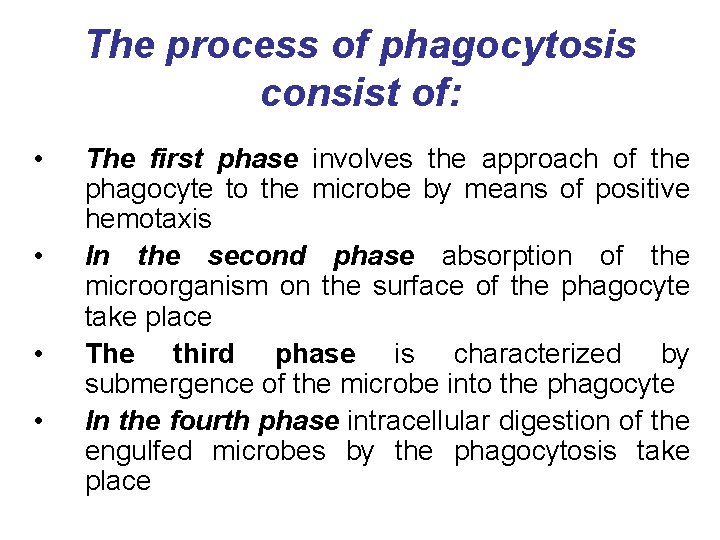
The process of phagocytosis consist of: • • The first phase involves the approach of the phagocyte to the microbe by means of positive hemotaxis In the second phase absorption of the microorganism on the surface of the phagocyte take place The third phase is characterized by submergence of the microbe into the phagocyte In the fourth phase intracellular digestion of the engulfed microbes by the phagocytosis take place
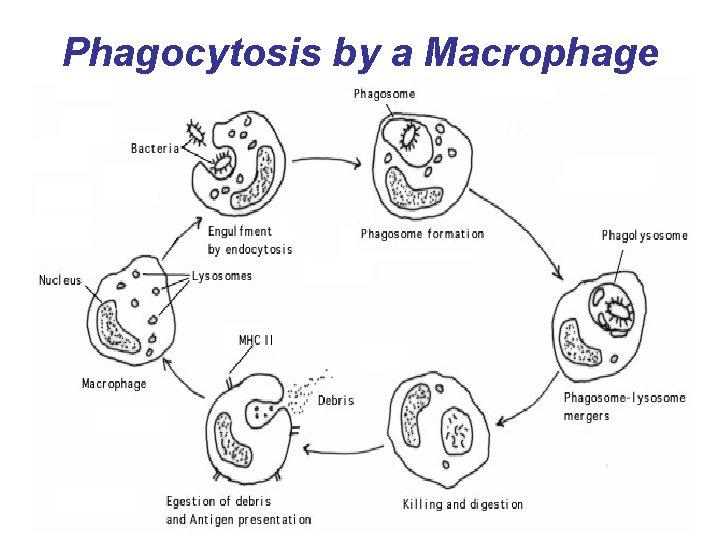
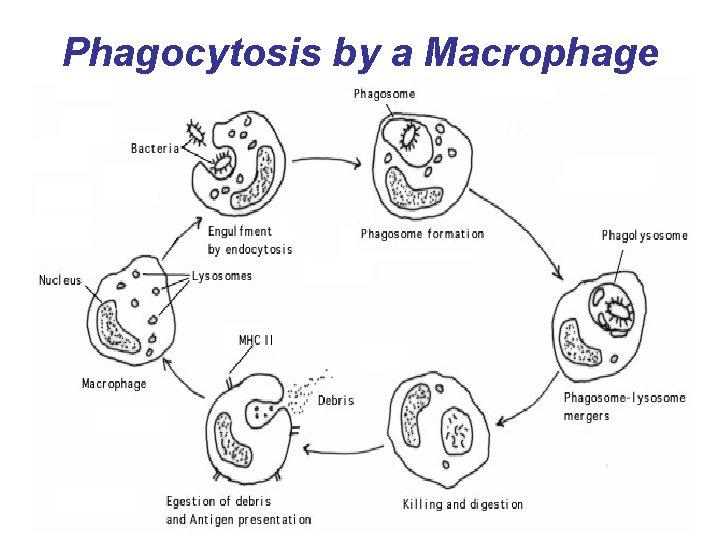
Phagocytosis by a Macrophage
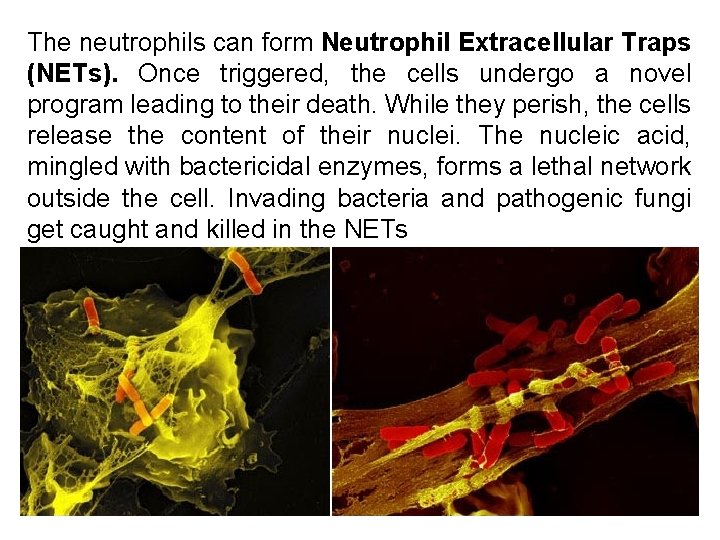
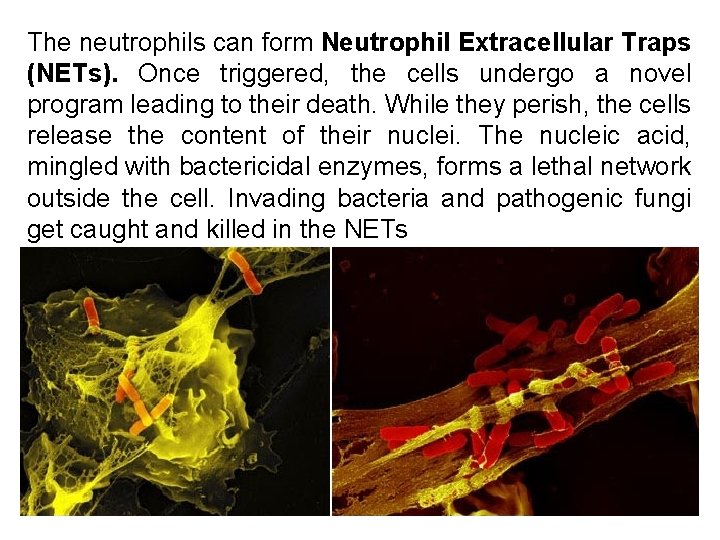
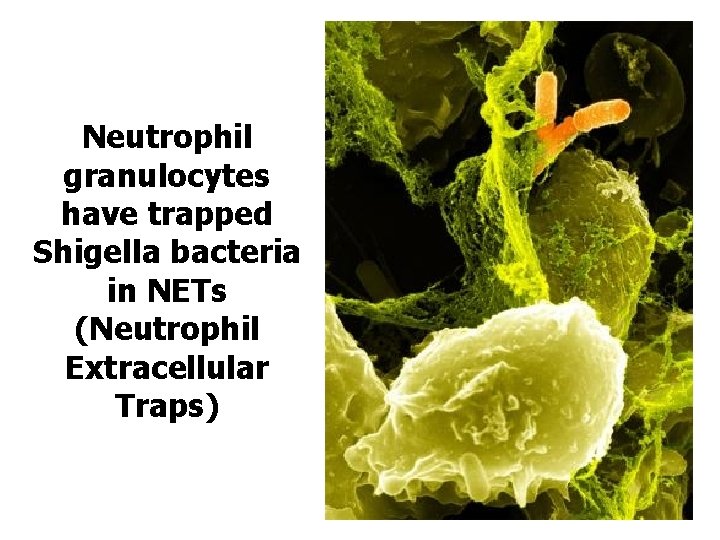
The neutrophils can form Neutrophil Extracellular Traps (NETs). Once triggered, the cells undergo a novel program leading to their death. While they perish, the cells release the content of their nuclei. The nucleic acid, mingled with bactericidal enzymes, forms a lethal network outside the cell. Invading bacteria and pathogenic fungi get caught and killed in the NETs
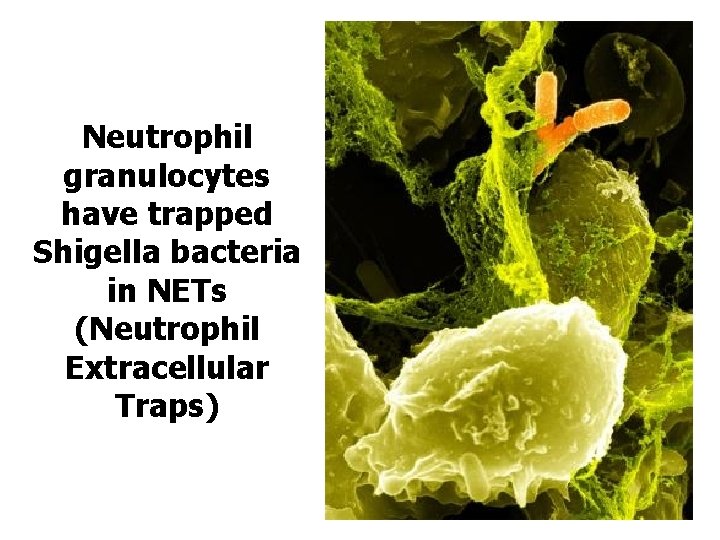
Neutrophil granulocytes have trapped Shigella bacteria in NETs (Neutrophil Extracellular Traps)
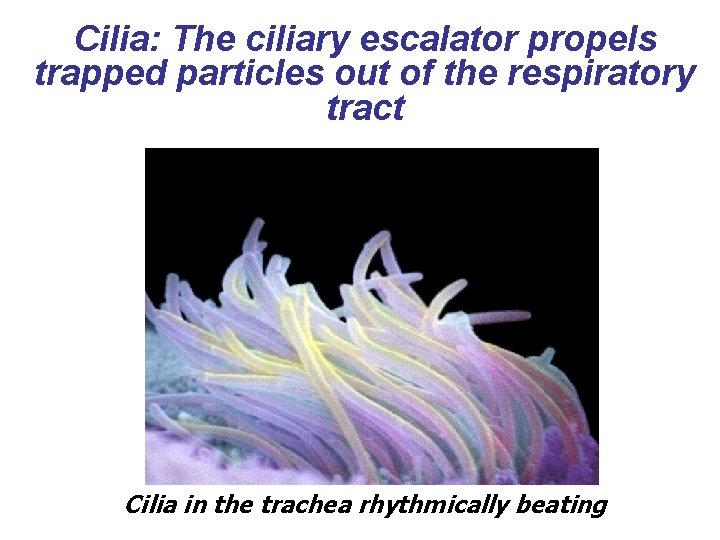
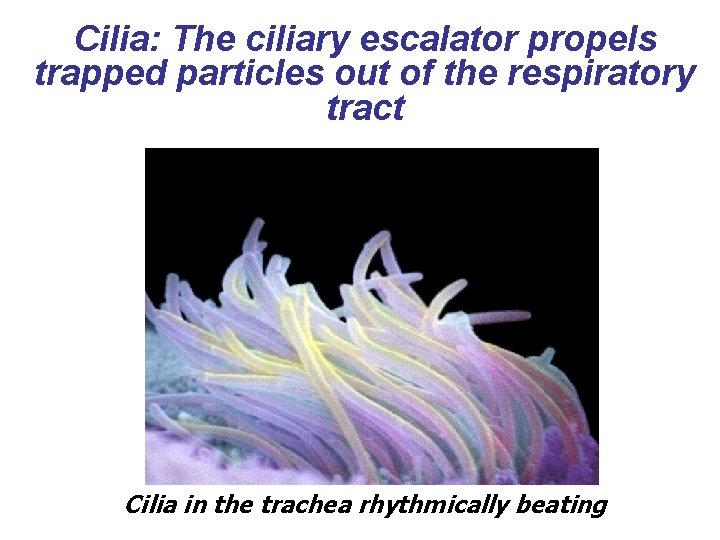
Cilia: The ciliary escalator propels trapped particles out of the respiratory tract Cilia in the trachea rhythmically beating
NON-SPECIFIC IMMUNITY • Inflammation: Tissue injury or irritation initiated by entry of bacteria or of other irritant leads to inflammation • Fever: It is natural defense mechanism. It may actually destroy the infecting organism. Fever stimulates the production of interferon and helps in recovery from virus infections
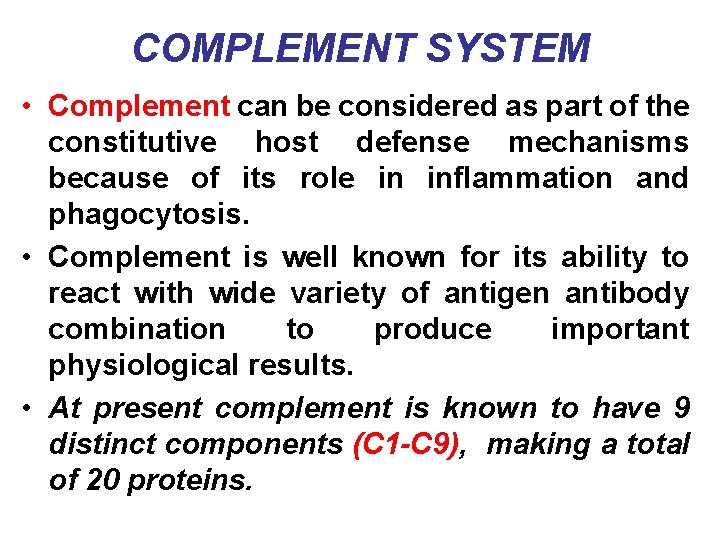
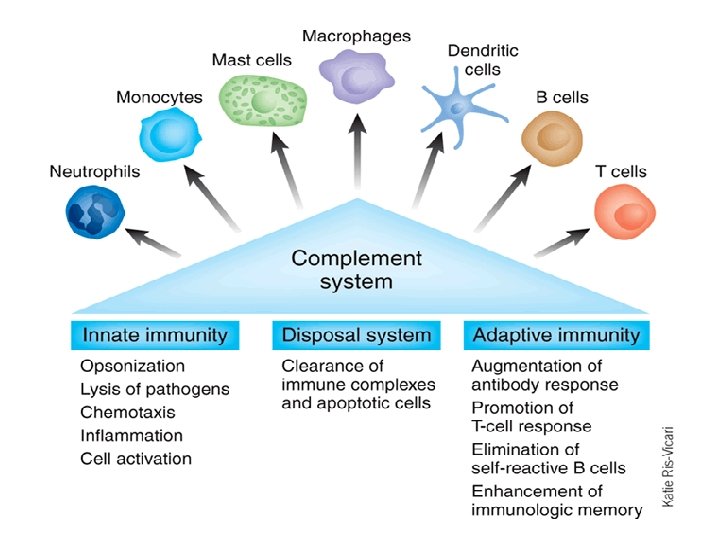
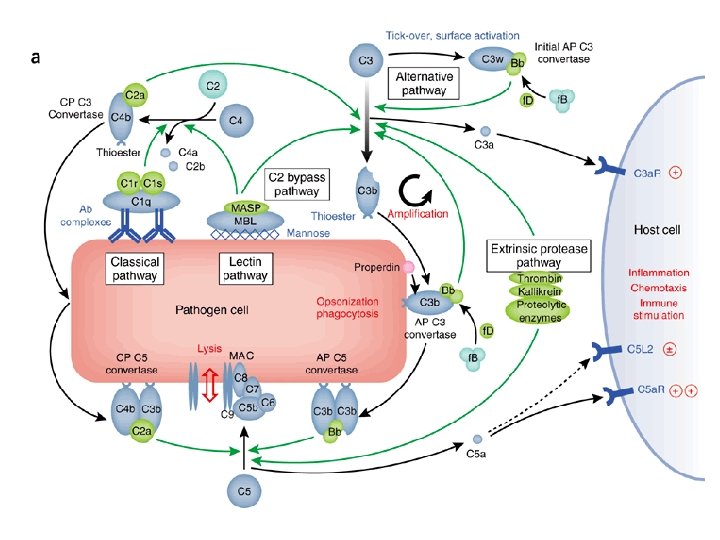
COMPLEMENT SYSTEM • Complement can be considered as part of the constitutive host defense mechanisms because of its role in inflammation and phagocytosis. • Complement is well known for its ability to react with wide variety of antigen antibody combination to produce important physiological results. • At present complement is known to have 9 distinct components (C 1 -C 9), making a total of 20 proteins.
Important physiological effects of complement system • • The destruction of erythrocytes as well as other tissue cells. The initiation of inflammatory changes. The lysis of bacteria cells. Enhancement of phagocytosis involving some opsonized particles.
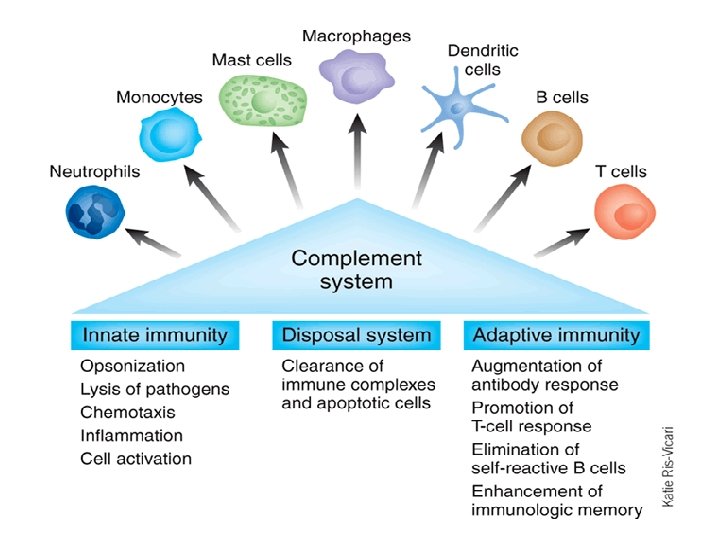
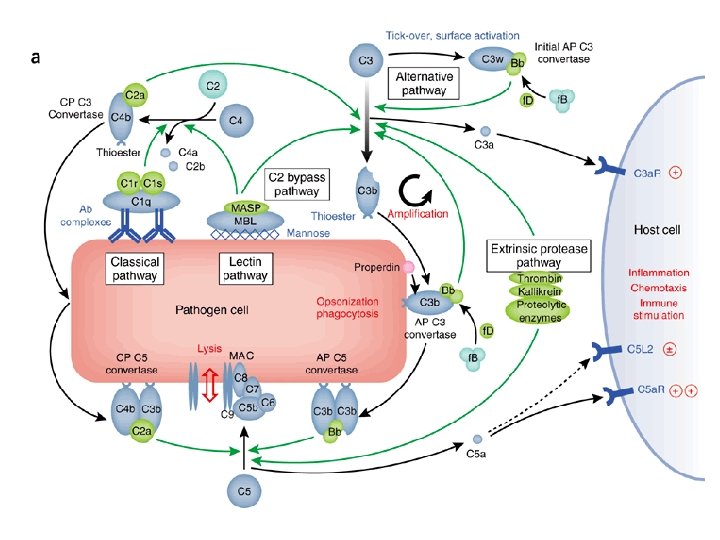
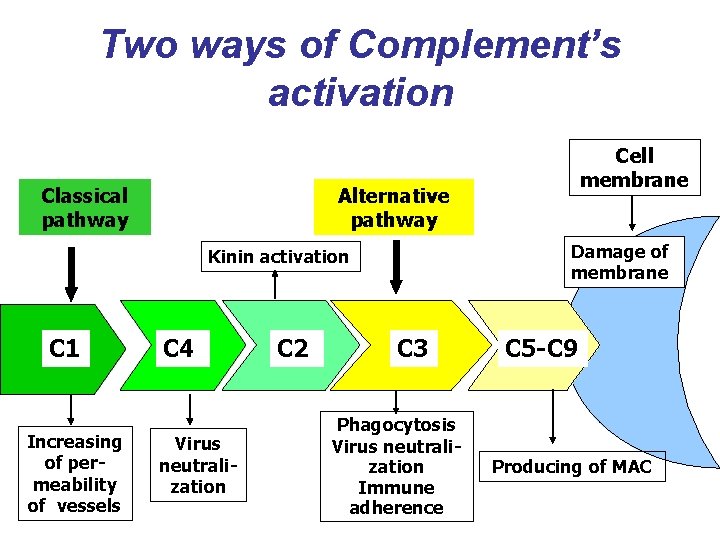
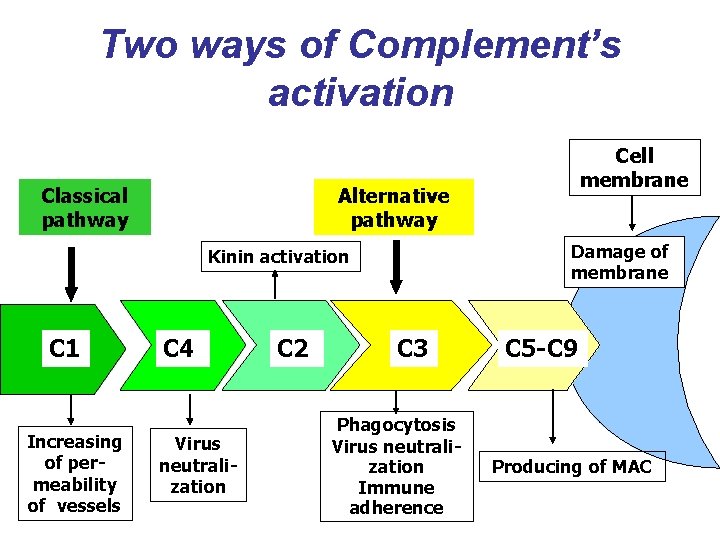
Two ways of Complement’s activation Classical pathway Alternative pathway Damage of membrane Kinin activation С 1 Increasing of permeability of vessels Cell membrane С 4 Virus neutralization С 2 С 3 Phagocytosis Virus neutralization Immune adherence С 5 -С 9 Producing of MAC
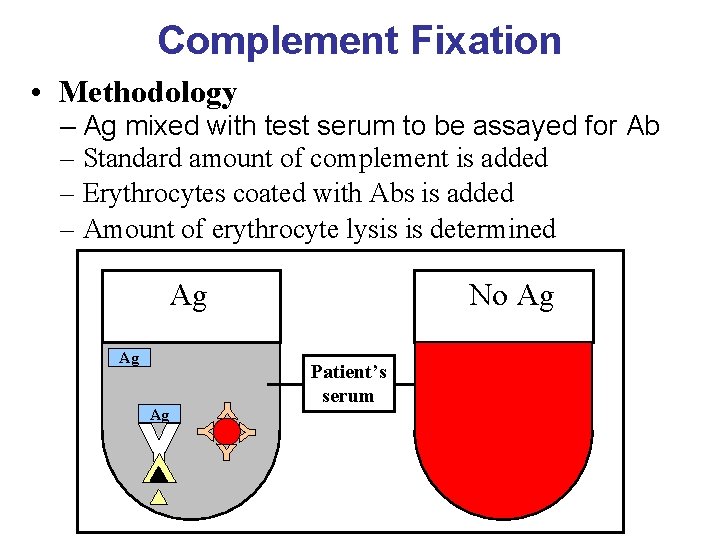
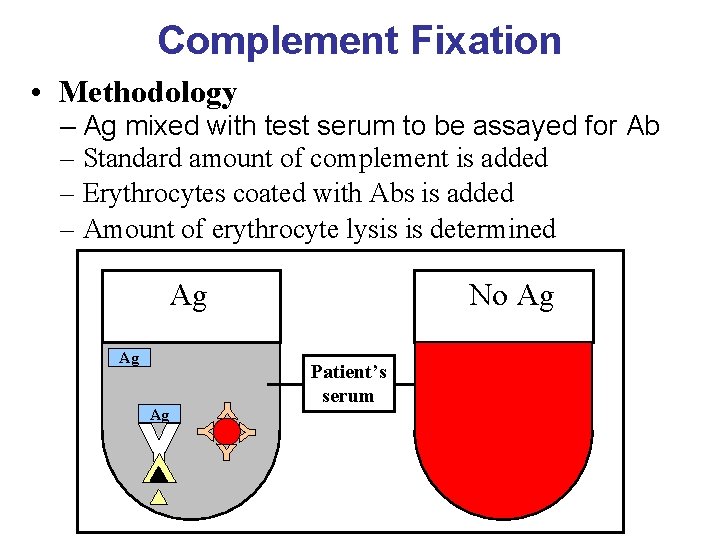
Complement Fixation • Methodology – Ag mixed with test serum to be assayed for Ab – Standard amount of complement is added – Erythrocytes coated with Abs is added – Amount of erythrocyte lysis is determined No Ag Ag Patient’s serum