Systemic Lupus Erythematosis The Immune System Immunology Connection




- Slides: 31
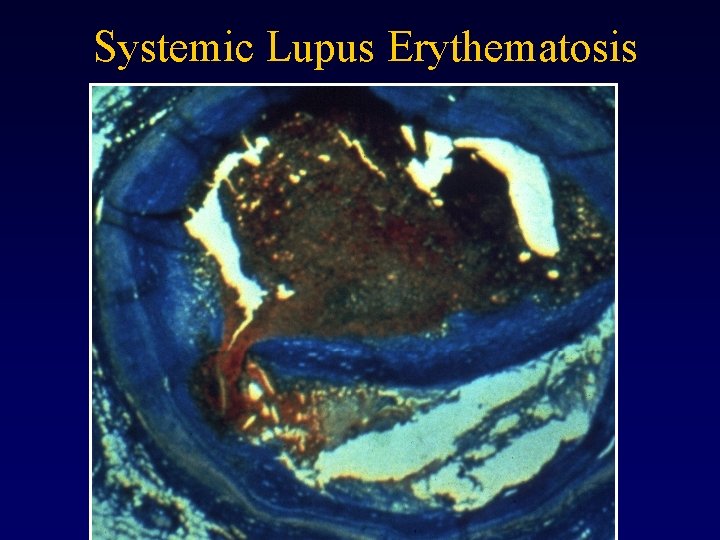
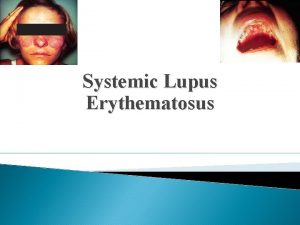
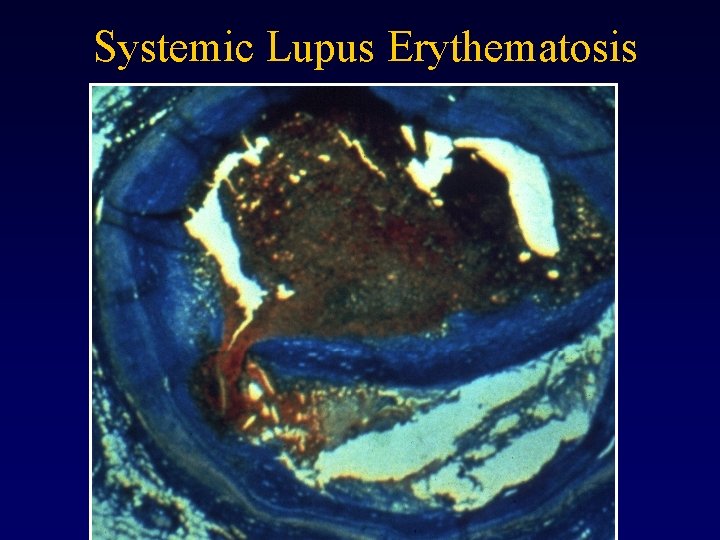
Systemic Lupus Erythematosis
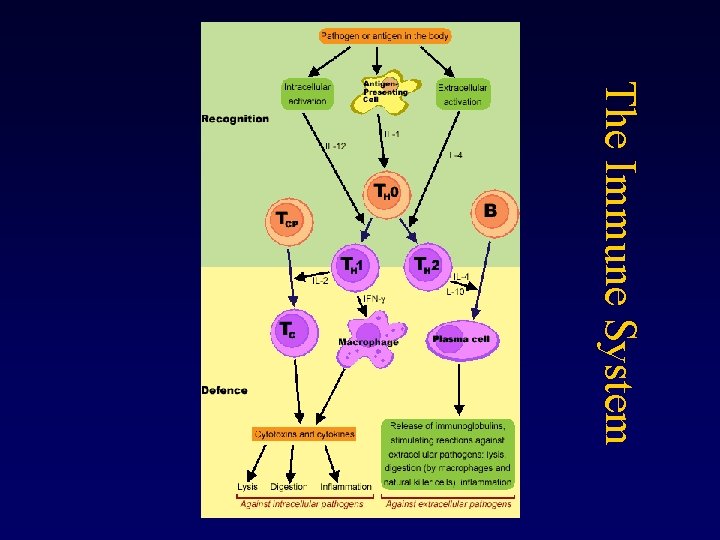
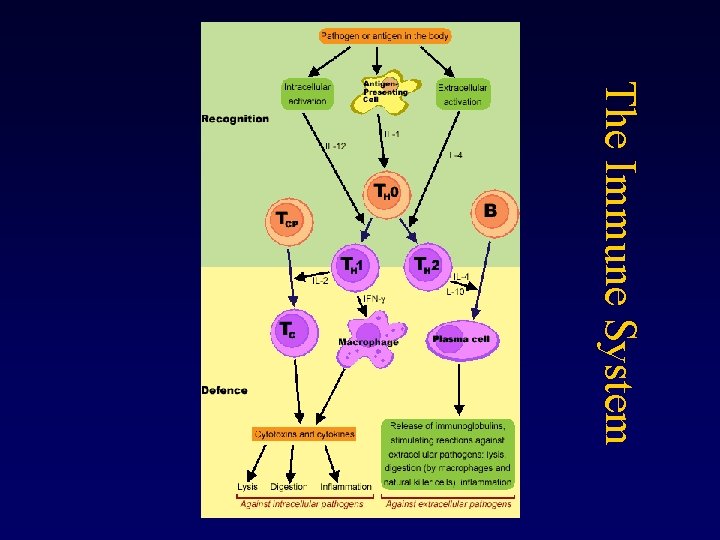
The Immune System
Immunology Connection to Tissue Engineering • Develop methods to selectively block immune response to engineered tissue • Manipulate immune system tissues to prevent autoimmune diseases • Scaffold compatibility
Gender Differences in Immune Response • Females resist a variety of infections better than males • Females may reject transplanted organs more rapidly • Females have a higher frequency of autoimmune diseases
What is Lupus? • An autoimmune disease • Your body can not adequately distinguish between foreign materials (antigens) and its own cells and tissues. • The immune system directs the development of antibodies that target bodily (antigens) components. • The auto-antibodies react with the bodies own antigens, forming immune complexes which can accumulate and cause increasing inflammationrelated damage.
What Causes Lupus? • Cause unknown, but suspect – Genetic factors – Environmental factors
What Causes Lupus? (cont’d) • Genetic causes – – Hereditary, but no single gene known to cause SLE Some people more genetically prone to Lupus 5% of children with parents who have it develop Lupus 10% of Lupus patients also have a close relative with the disease – Chromosomes 1 and 6 associated with Lupus in certain families
Observations to Support Genetic Factors in Lupus Clustering in families Identical twins > fraternal twins
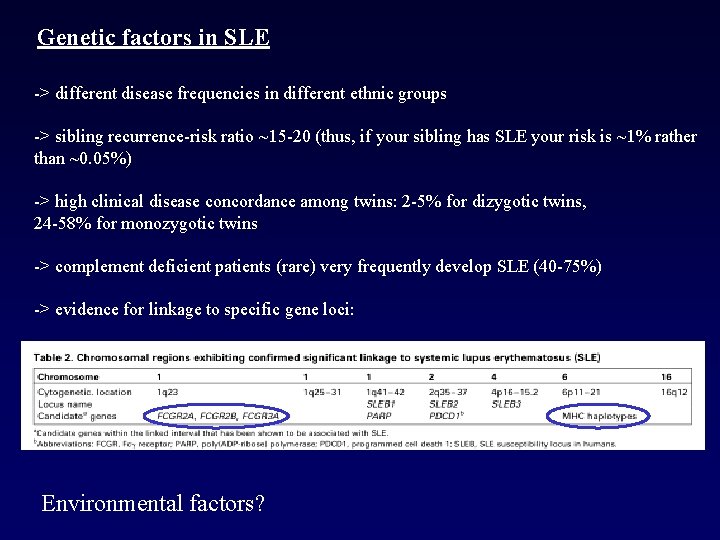
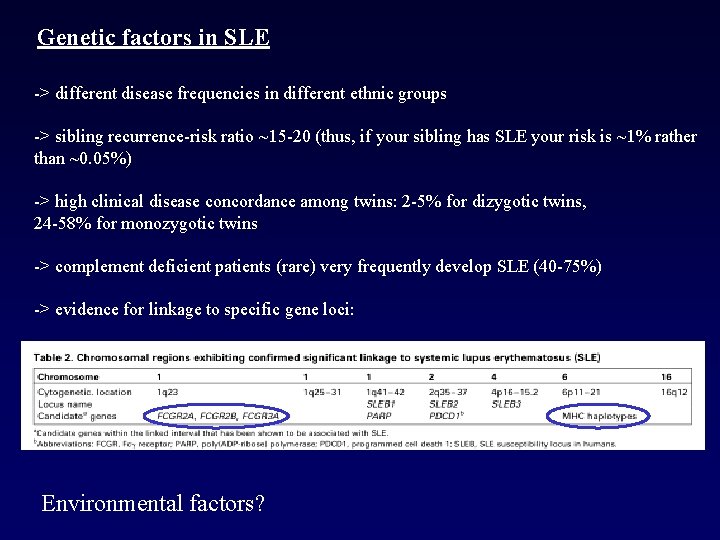
Genetic factors in SLE -> different disease frequencies in different ethnic groups -> sibling recurrence-risk ratio ~15 -20 (thus, if your sibling has SLE your risk is ~1% rather than ~0. 05%) -> high clinical disease concordance among twins: 2 -5% for dizygotic twins, 24 -58% for monozygotic twins -> complement deficient patients (rare) very frequently develop SLE (40 -75%) -> evidence for linkage to specific gene loci: Environmental factors?
What Causes Lupus? (cont’d) • Environmental causes – Infections – Antibiotics – Ultra-violet light – Extreme stress – Certain drugs
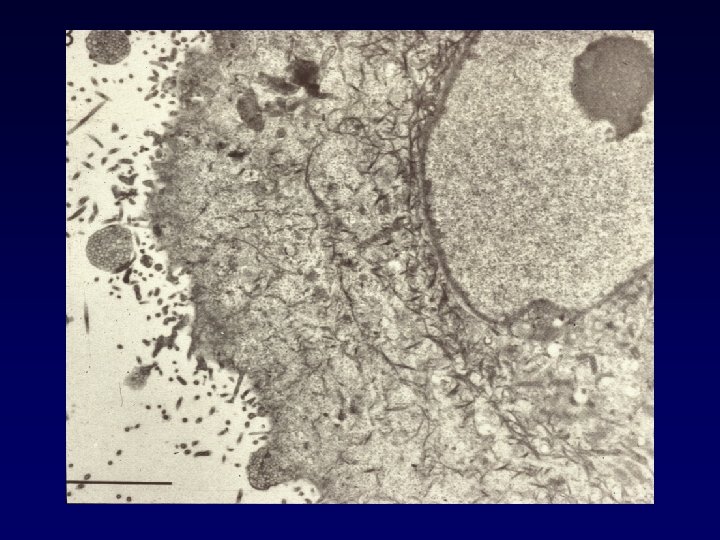
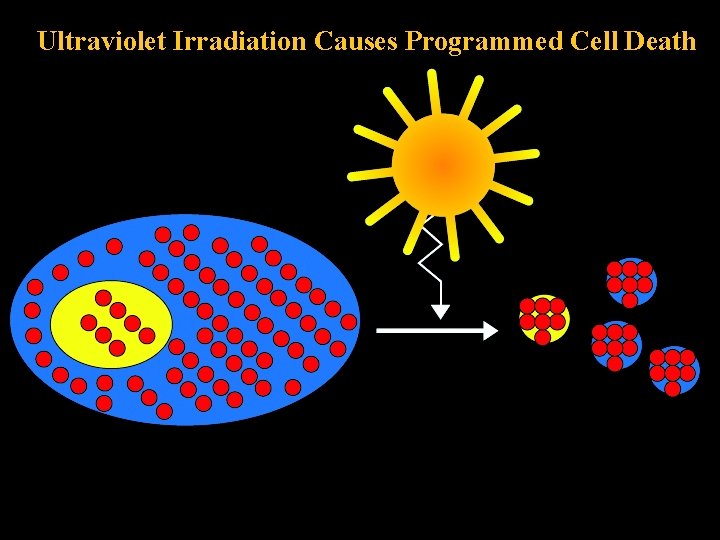
Apoptosis and SLE: Causal Connection? • Delayed clearance of apoptotic cells • Abnormal exposure of intracellular components to immune response, supported by autoantibody findings in Lupus patients
Complement and SLE? • Altered complement system: an SLE correlation? • Reduced levels of C 3 and C 4 components commonly found, those with C 1, C 2, and C 4 gene aberrations at apparent high risk
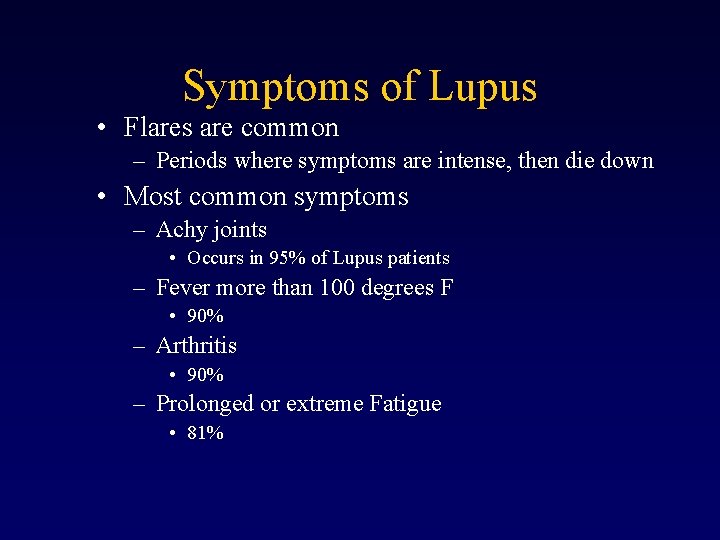
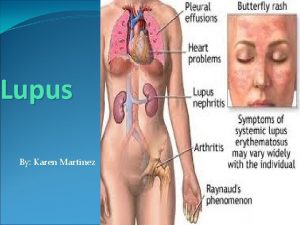
Symptoms of Lupus • Flares are common – Periods where symptoms are intense, then die down • Most common symptoms – Achy joints • Occurs in 95% of Lupus patients – Fever more than 100 degrees F • 90% – Arthritis • 90% – Prolonged or extreme Fatigue • 81%
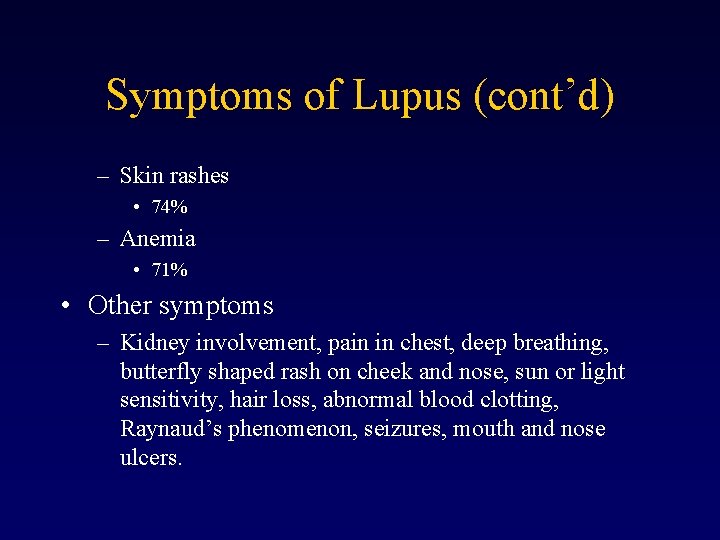
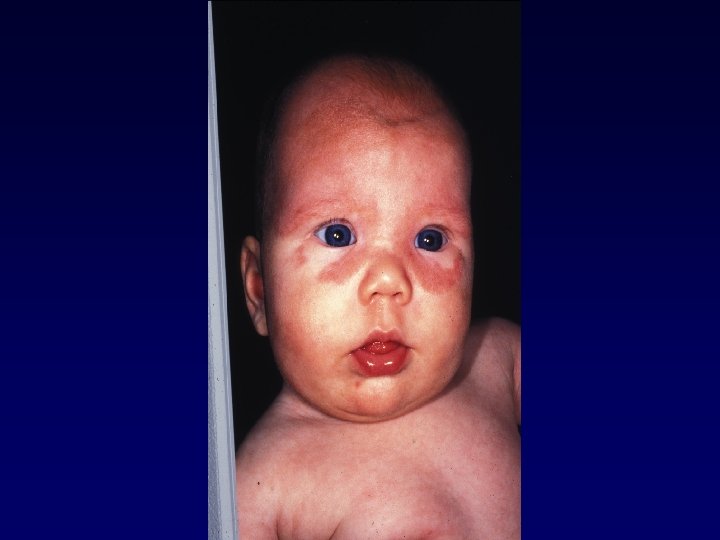
Symptoms of Lupus (cont’d) – Skin rashes • 74% – Anemia • 71% • Other symptoms – Kidney involvement, pain in chest, deep breathing, butterfly shaped rash on cheek and nose, sun or light sensitivity, hair loss, abnormal blood clotting, Raynaud’s phenomenon, seizures, mouth and nose ulcers.
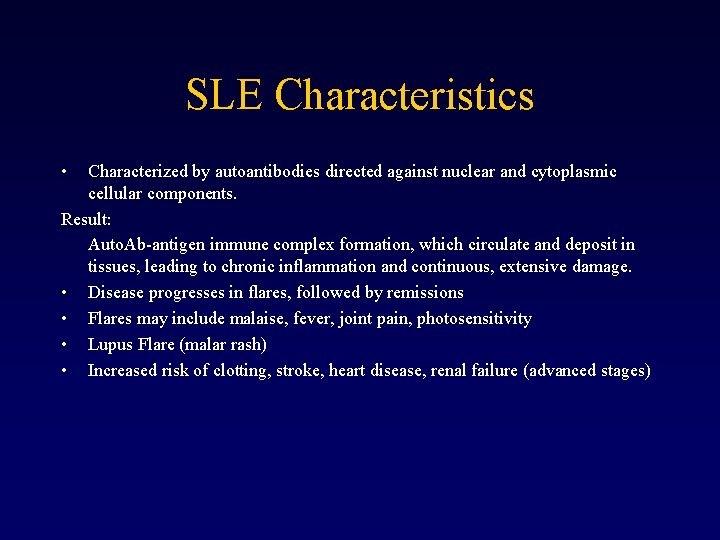
SLE Characteristics • Characterized by autoantibodies directed against nuclear and cytoplasmic cellular components. Result: Auto. Ab-antigen immune complex formation, which circulate and deposit in tissues, leading to chronic inflammation and continuous, extensive damage. • Disease progresses in flares, followed by remissions • Flares may include malaise, fever, joint pain, photosensitivity • Lupus Flare (malar rash) • Increased risk of clotting, stroke, heart disease, renal failure (advanced stages)
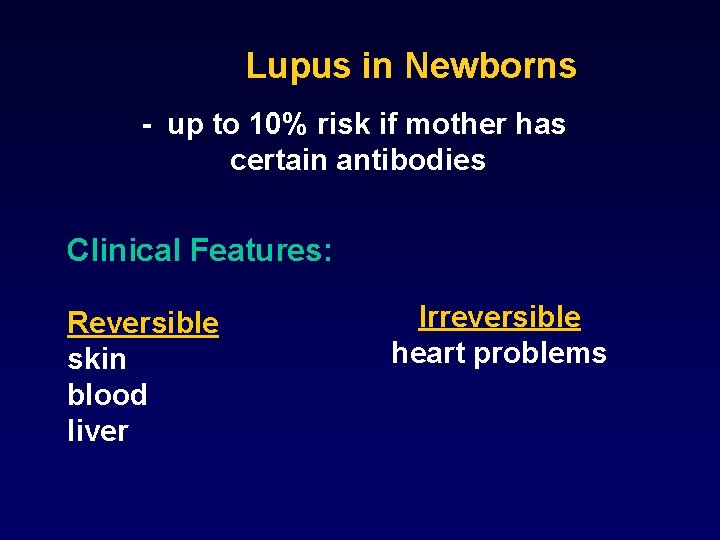
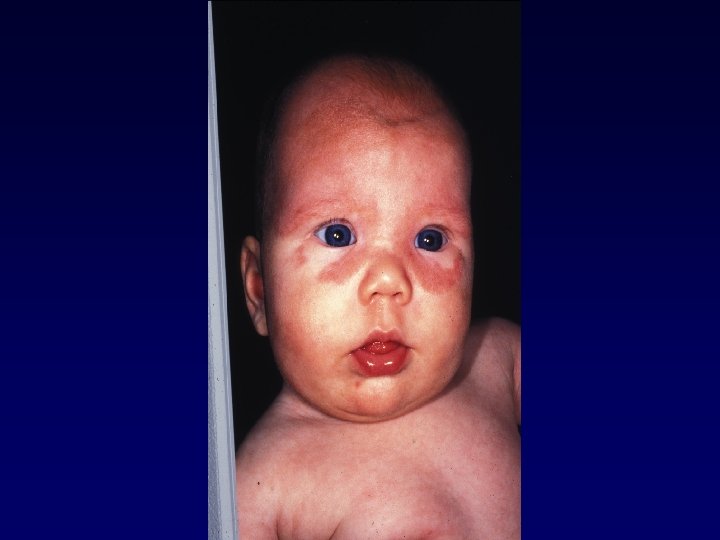
Lupus in Newborns - up to 10% risk if mother has certain antibodies Clinical Features: Reversible skin blood liver Irreversible heart problems
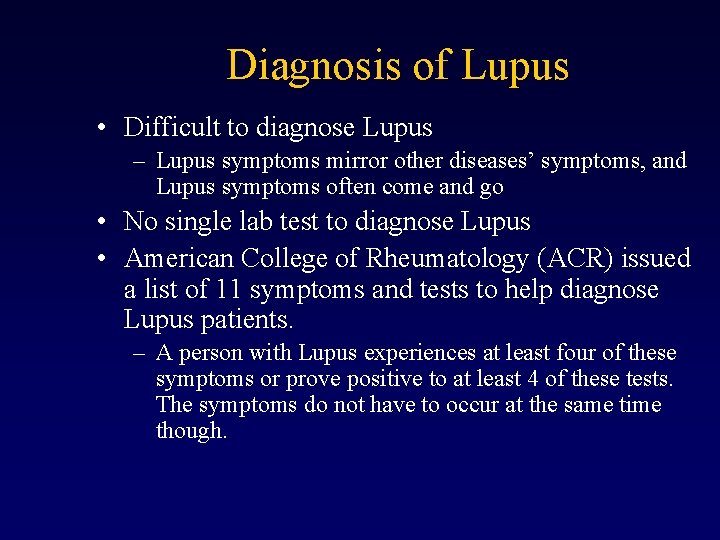
Diagnosis of Lupus • Difficult to diagnose Lupus – Lupus symptoms mirror other diseases’ symptoms, and Lupus symptoms often come and go • No single lab test to diagnose Lupus • American College of Rheumatology (ACR) issued a list of 11 symptoms and tests to help diagnose Lupus patients. – A person with Lupus experiences at least four of these symptoms or prove positive to at least 4 of these tests. The symptoms do not have to occur at the same time though.
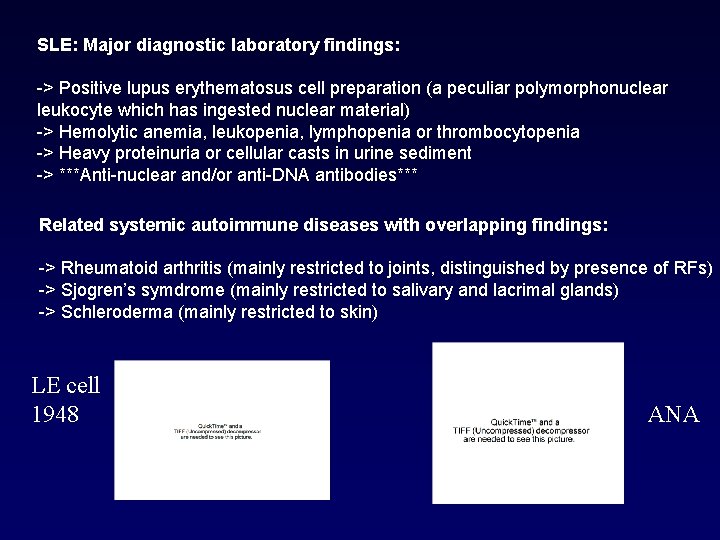
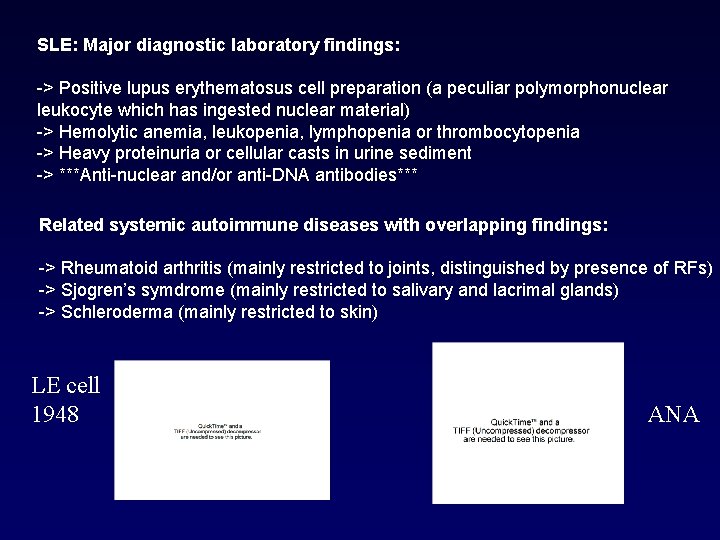
SLE: Major diagnostic laboratory findings: -> Positive lupus erythematosus cell preparation (a peculiar polymorphonuclear leukocyte which has ingested nuclear material) -> Hemolytic anemia, leukopenia, lymphopenia or thrombocytopenia -> Heavy proteinuria or cellular casts in urine sediment -> ***Anti-nuclear and/or anti-DNA antibodies*** Related systemic autoimmune diseases with overlapping findings: -> Rheumatoid arthritis (mainly restricted to joints, distinguished by presence of RFs) -> Sjogren’s symdrome (mainly restricted to salivary and lacrimal glands) -> Schleroderma (mainly restricted to skin) LE cell 1948 ANA
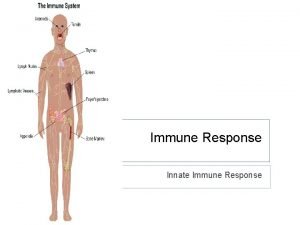
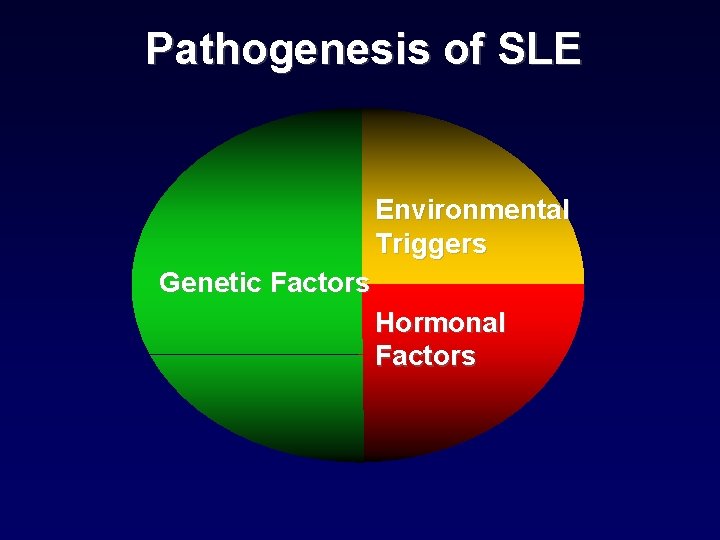
Pathogenesis of SLE Environmental Triggers Genetic Factors Hormonal Factors

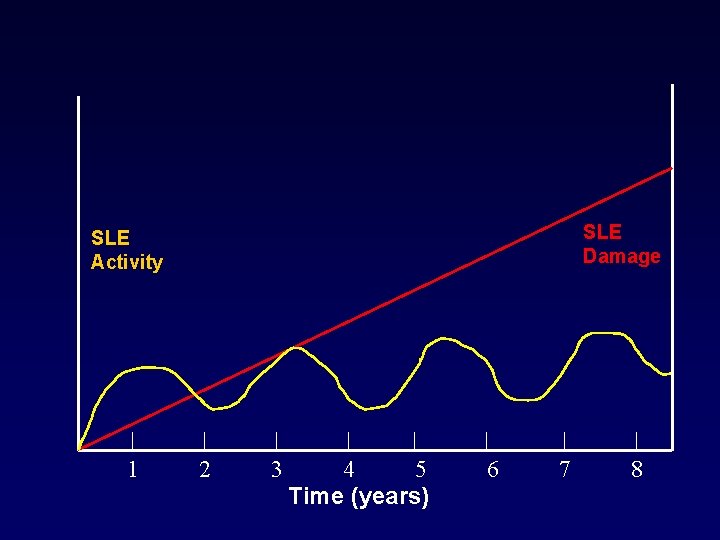
Natural History of SLE • Disease flares/activity (reversible) • Organ damage (irreversible) disease treatment
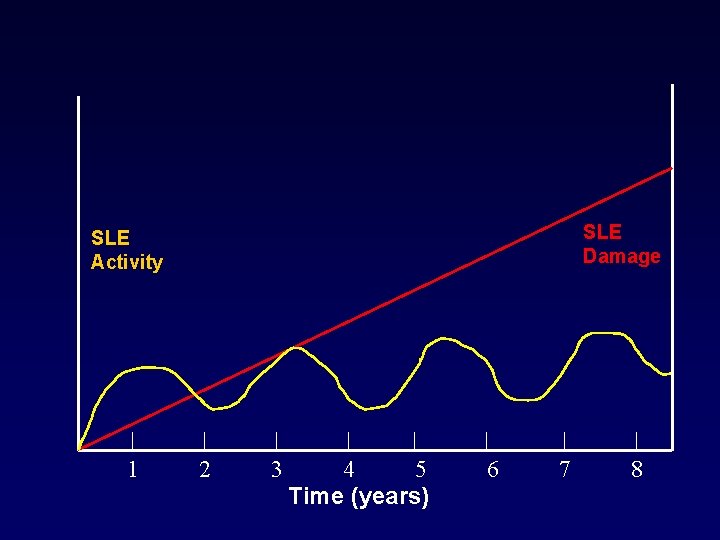
SLE Damage SLE Activity 1 2 3 4 5 Time (years) 6 7 8
Environmental Triggers Sun exposure (photosensitivity) Drug-induced lupus Viral triggers
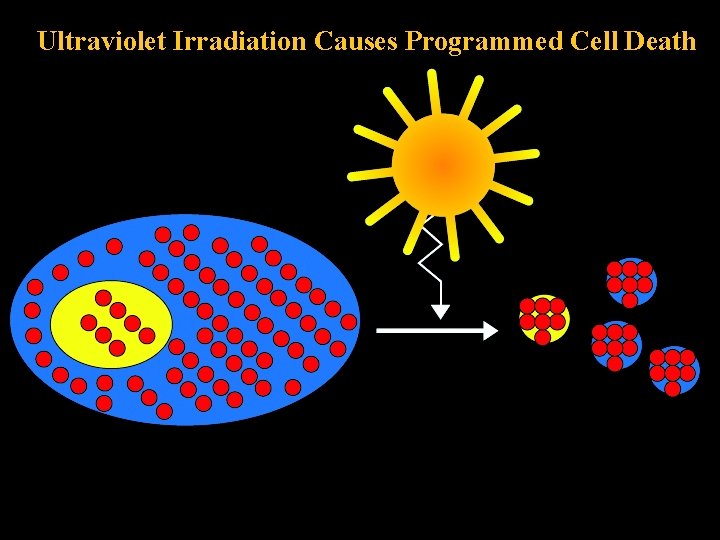
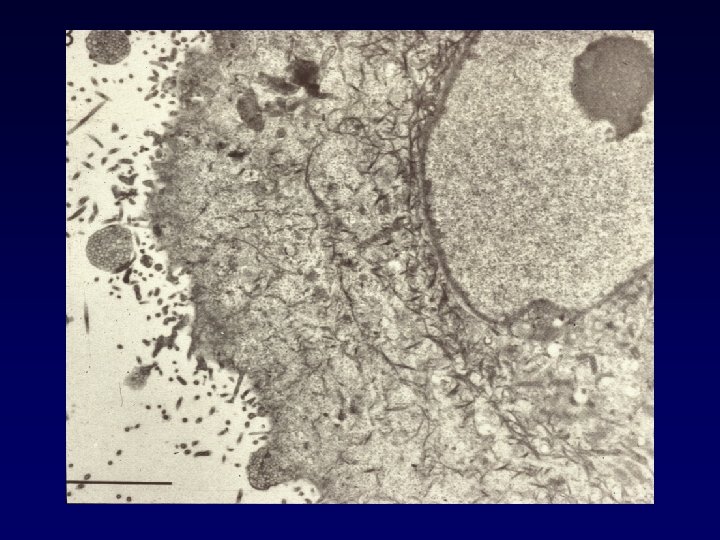
Ultraviolet Irradiation Causes Programmed Cell Death

SLE Treatment • • NSAIDS Antimalarials (HCQ Mepacrine) Corticosteroids (oral/iv/im/intralesional) Immunosuppressives – – – • • Azathioprine Cyclosporin A Methotrexate MMF Cyclophosphamide Biologicals- Rituximab Others- Prasterone, Thalidomide, Acetretin
Interview of a Lupus Patient • What kind of medications do you take? – I take Plaquenil which is an anti-malarial drug that fights fatigue. I also take Advil when I get stiff. I used to take Prednisone, but I don’t have to anymore because my disease isn’t as severe anymore as it used to be. • Is there any research being done to find a cure or better treatment for Lupus? – There are many groups doing research on the immune system which is a link to autoimmune diseases like Lupus. Also, since Lupus seems to attack mostly women, there are many groups trying to find a link between hormones and Lupus.


 A subsequent
A subsequent Case study 87 systemic lupus erythematosus
Case study 87 systemic lupus erythematosus Elsever
Elsever Slip critical connection vs bearing connection
Slip critical connection vs bearing connection Shear plane in bolted connection
Shear plane in bolted connection Slip critical connection vs bearing connection
Slip critical connection vs bearing connection Surface vs deep connections
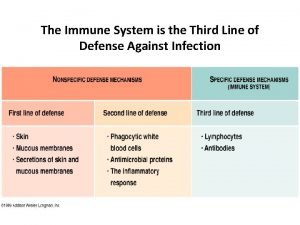
Surface vs deep connections What is the third line of defense in the immune system
What is the third line of defense in the immune system Flow chart
Flow chart Any substance capable of provoking an immune response
Any substance capable of provoking an immune response Second line of defense immune system
Second line of defense immune system Chapter 35 immune system and disease
Chapter 35 immune system and disease 1st 2nd and 3rd line of defense immune system
1st 2nd and 3rd line of defense immune system Ap biology immune system
Ap biology immune system Lesson 12 blood and immune system
Lesson 12 blood and immune system Lesson 12 blood and immune system
Lesson 12 blood and immune system Oobean
Oobean Immunity assignment slideshare
Immunity assignment slideshare Overreactions of the immune system
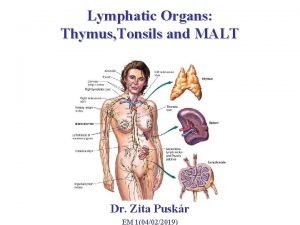
Overreactions of the immune system Lymphatic vs immune system
Lymphatic vs immune system Lymphatic vs immune system
Lymphatic vs immune system Defination of immune system
Defination of immune system 3rd line of defense
3rd line of defense Main function of the immune system
Main function of the immune system Tonsil histology
Tonsil histology Thymus
Thymus Immune complex
Immune complex Thalassemia autosomal recessive
Thalassemia autosomal recessive 1what's the purpose of the body's immune system?
1what's the purpose of the body's immune system? Phagocyte
Phagocyte Precipitation curve immunology
Precipitation curve immunology Central tolerance and peripheral tolerance
Central tolerance and peripheral tolerance