Systemic Lupus Erythematosus History of Lupus Lupus means

- Slides: 48
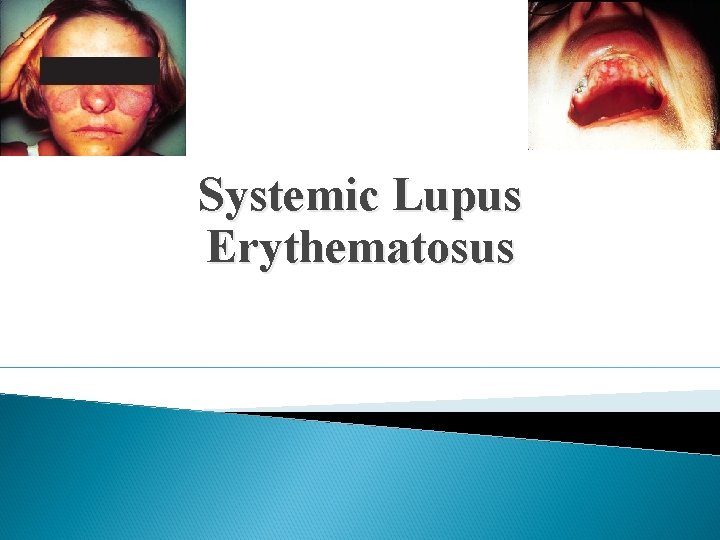
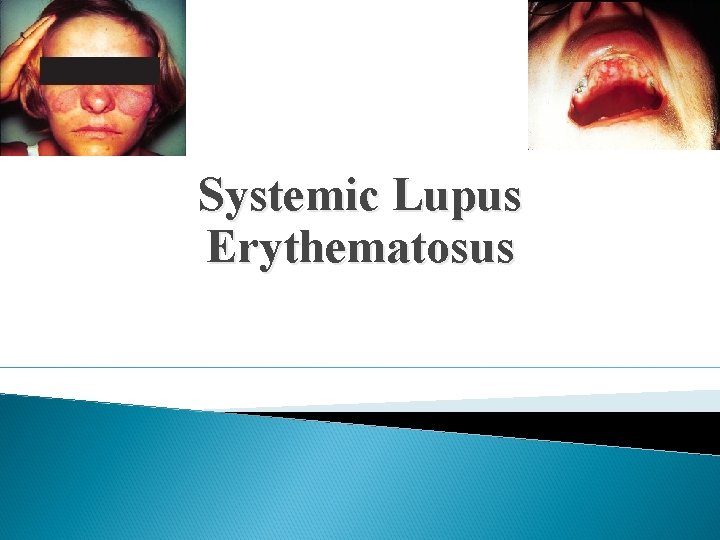
Systemic Lupus Erythematosus
History of Lupus Lupus means “wolf” in Latin 10 th century- case reports appeared in writings Late 1800 s- Sir William Osler initially described the systemic nature and linked rashes to organ involvement 1949 - LE cell described by Malcolm Hargraves at Mayo Clinic 1954 - ANA described 1971 - First set of classification criteria proposed for Lupus 1983 - Antiphospholipid antibody syndrome described
What exactly is Lupus? Autoimmune disease where one’s immune system attacks itself Autoantibody production -> immune complex deposition -> inflammation -> damage Chronic disease, characterized by flares and remission Pleomorphic with different phenotypic expressions Multisystem involvement
Types Of Lupus Drug Induced Lupus Neonatal Lupus Cutaneous Lupus Systemic Lupus Erythematosus
Who get’s Lupus? Prevalence is over 1. 5 million Americans Incidence difficult due to lack of strict definition Bimodal peak presentation: ages 20 -40 and again after age 60 Prevalence is higher in African Americans, Asians, Hispanics Female to male predominance
Does your gender really matter? 90% of patients with lupus are female Before puberty F: M ratio is 2: 1 During reproductive years ratio 8: 1 Post-menopausal ratio 2. 3: 1 Increased frequency in women attributed to the hormonal effect of estrogen
Does your gender really matter? Nurses Health Study use of estrogen-containing contraceptive agents associated with an 50 percent increase in risk of developing SLE either early onset of menarche (age ≤ 10 years) or administration of estrogen to postmenopausal women doubles their risk Treatment of clinically stable SLE with oral contraceptives for one year does not increase disease flares
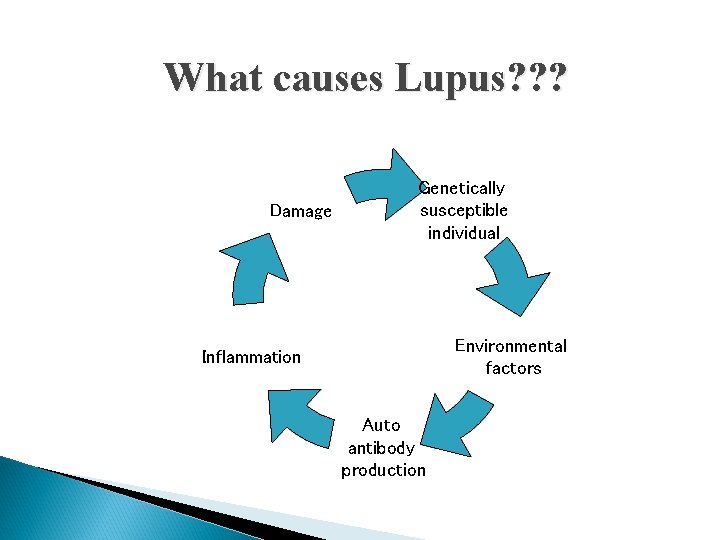
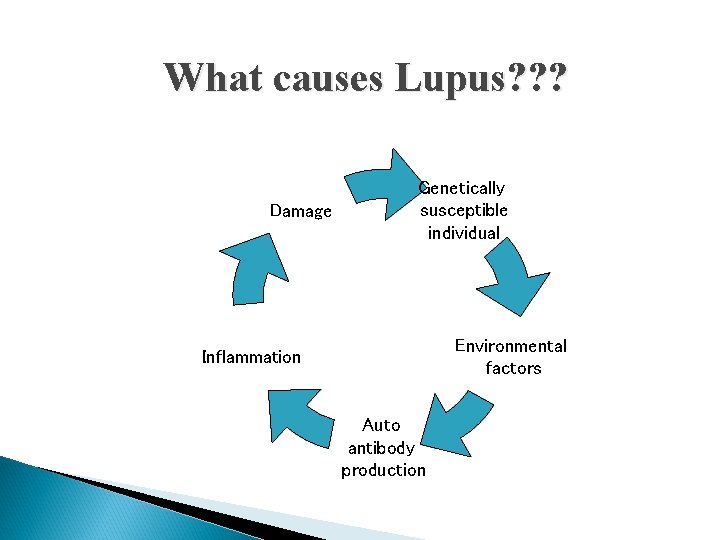
What causes Lupus? ? ? Damage Genetically susceptible individual Environmental factors Inflammation Auto antibody production
Genetics of Lupus High concordance in monozygotic twins 5 -12% or relatives with lupus have the disease No single lupus gene Disease is polygenic At least 30 susceptiblility genes identified HLADR 2, HLADR 3, HLADR 4, HLADR 8 (present in 75%) Homozygous deficiency of C 1 q complement
Environmental Factors UVA and UVB light can stimulate/ up-regulate autoimmunity stimulating keratinocytes to produce cytokines -> activate B cells to produce ab Viruses/Bacteria: molecular mimicry SLE patients have higher titers of antibodies to Epstein-Barr virus (EBV), increased circulating EBV viral loads; SSA ab has a sequence similar to EBV nuclear ag 1 Parvovirus B 19 Drugs Silica exposure, tobacco smoke, emotional stress
Immune dysregulation Upregulation of innate immunity Delayed clearance of apoptotic cells, resulting in antigenic stimulation Loss of tolerance via failed elimination of autoreactive T lymphocytes Abnormalities in B cells Abnormalities in T regulatory cells (CD 4+/CD 25+ cells down regulate immune system responses)
Autoantibodies in Lupus Study of US army recruits revealed lupus autoab present for up to 9 years prior to dx in 85% ANA ds. DNA Anti-Smith Anti-RNP Anti-SSA, anti-SSB Anticardiolipin Anti B 2 glycoprotein
Meaning of ANAs What exactly are they? Antibodies that bind to various antigens in the nucleus of a cell How is it measured? Indirect Immunofluorescence
ANA and Aging For every year after age 50, percentage of ANA positivity increases 1%/year For example Age 50 1% Age 55 5% Age 60 10%
ANA in Lupus Sensitivity 93 -99% in SLE Sensitivity 95 -100% in drug induced Lupus Specificity is not great Higher the titer, higher the specificity 1: 40 - 30% normal population 1: 160 - seen in 5% of the population
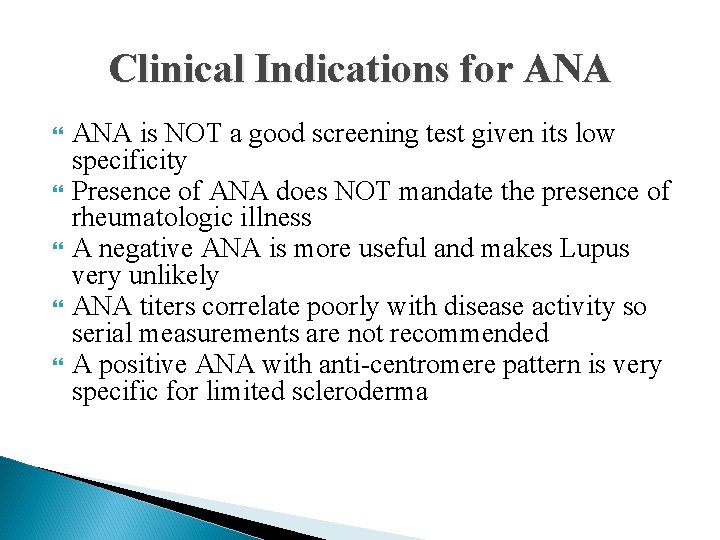
Clinical Indications for ANA is NOT a good screening test given its low specificity Presence of ANA does NOT mandate the presence of rheumatologic illness A negative ANA is more useful and makes Lupus very unlikely ANA titers correlate poorly with disease activity so serial measurements are not recommended A positive ANA with anti-centromere pattern is very specific for limited scleroderma
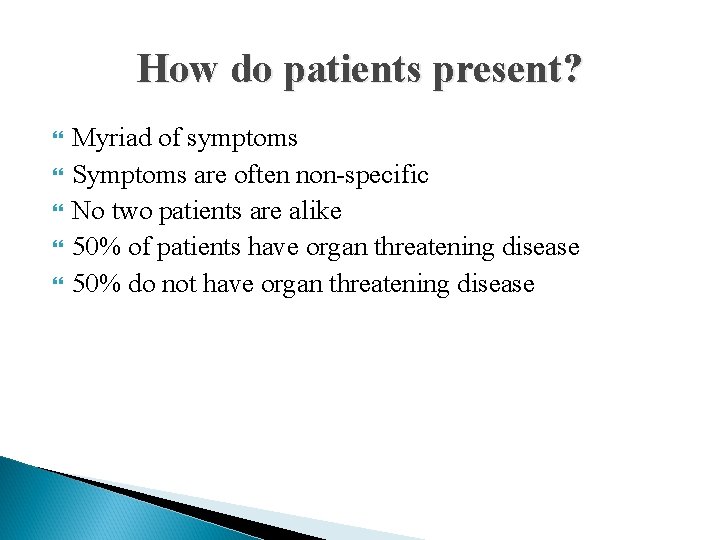
How do patients present? Myriad of symptoms Symptoms are often non-specific No two patients are alike 50% of patients have organ threatening disease 50% do not have organ threatening disease
Question What is the most common organ system involvement in lupus?
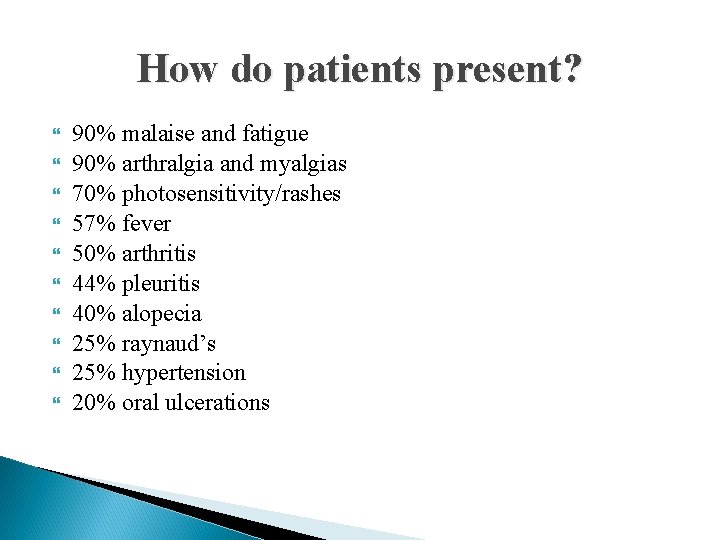
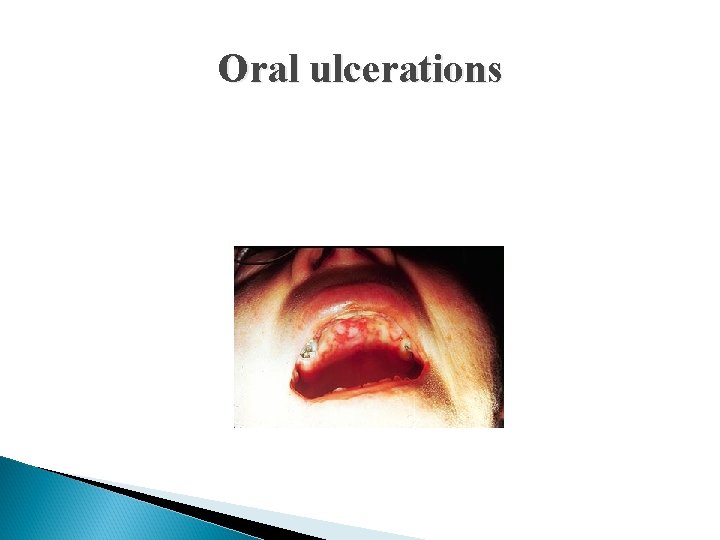
How do patients present? 90% malaise and fatigue 90% arthralgia and myalgias 70% photosensitivity/rashes 57% fever 50% arthritis 44% pleuritis 40% alopecia 25% raynaud’s 25% hypertension 20% oral ulcerations
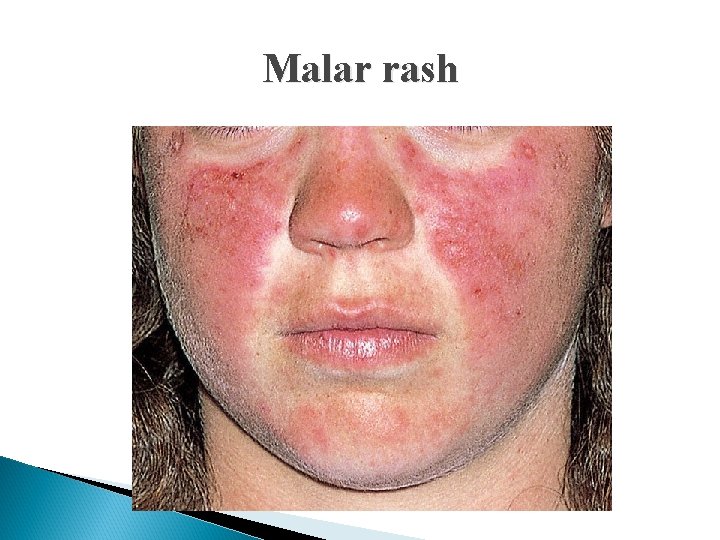
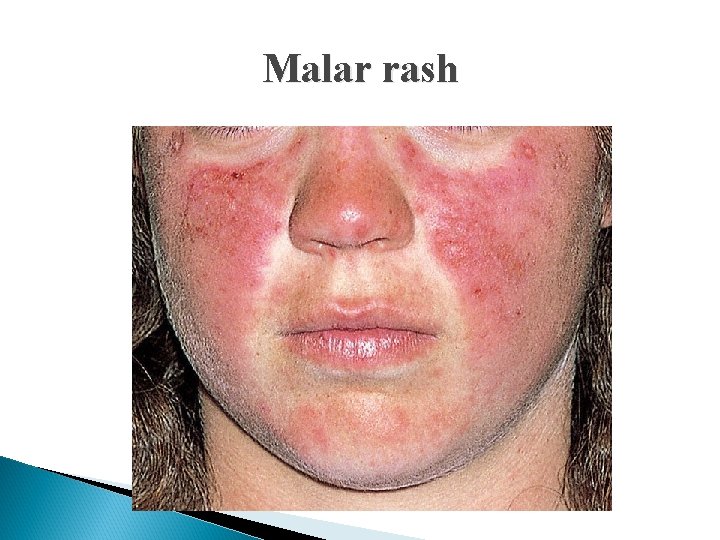
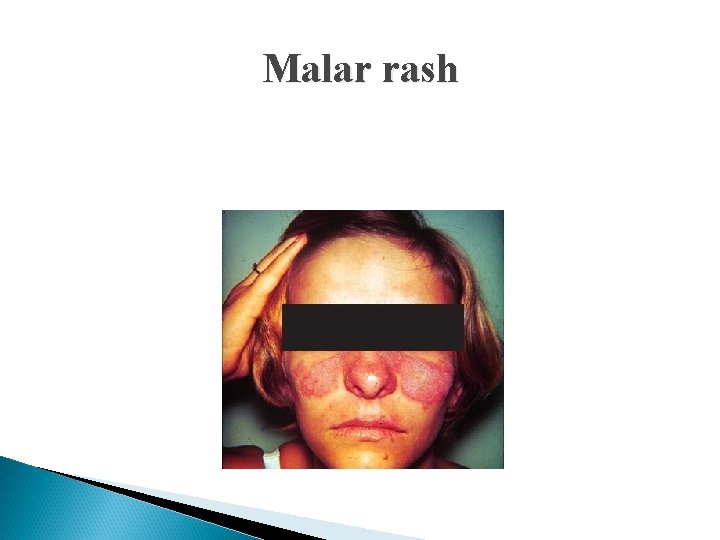
Malar rash
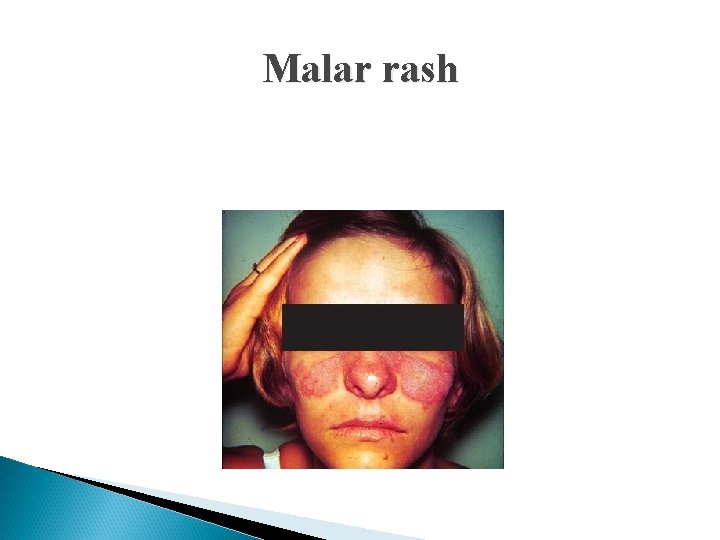
Malar rash
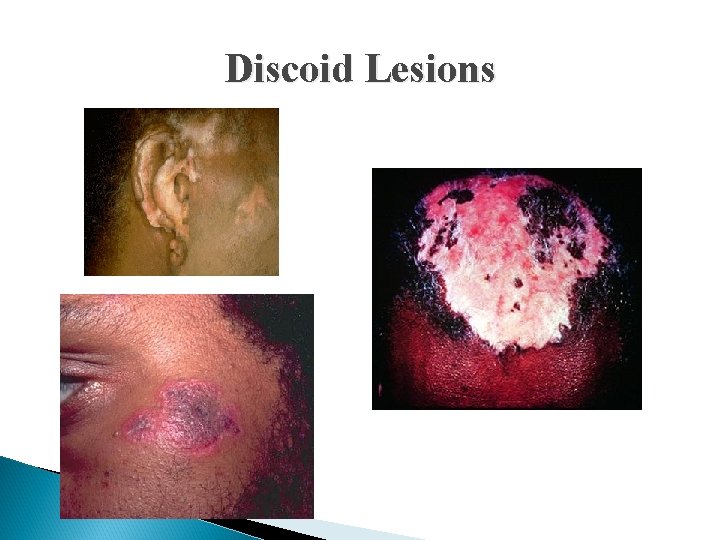
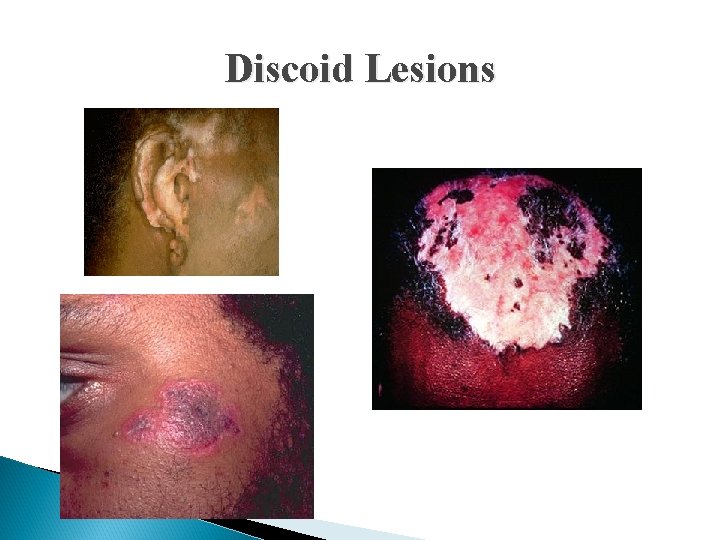
Discoid Lesions
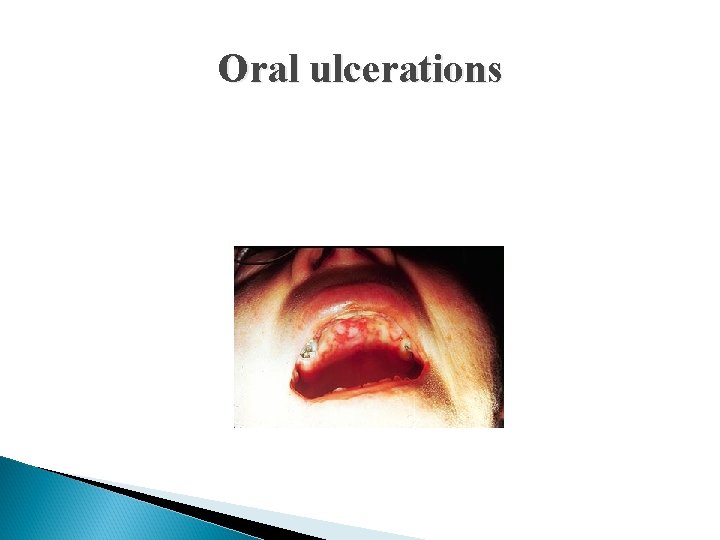
Oral ulcerations
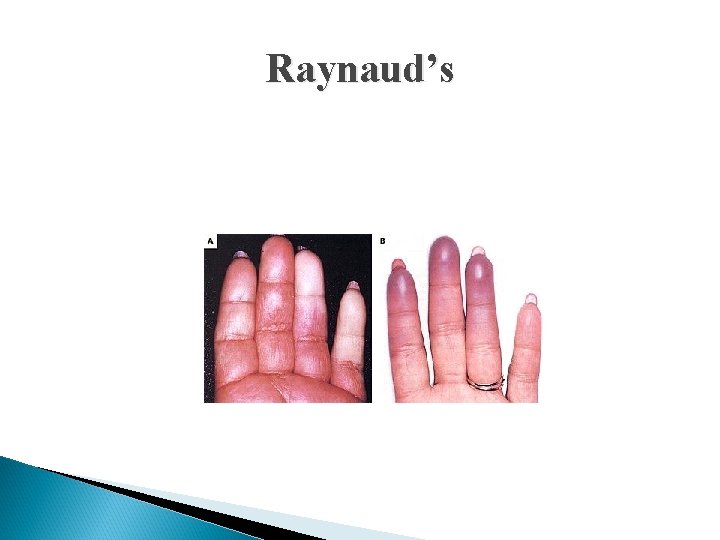
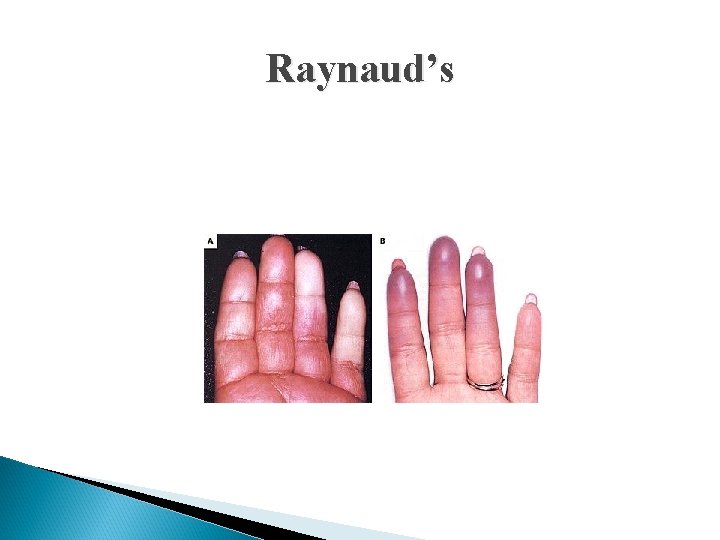
Raynaud’s
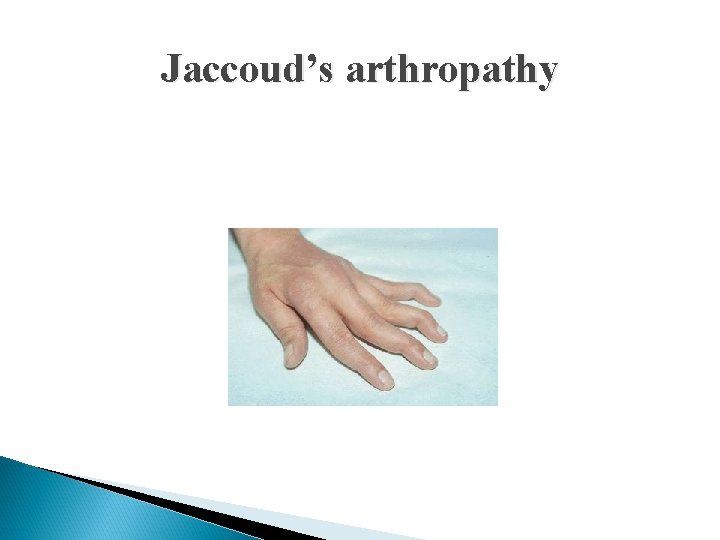
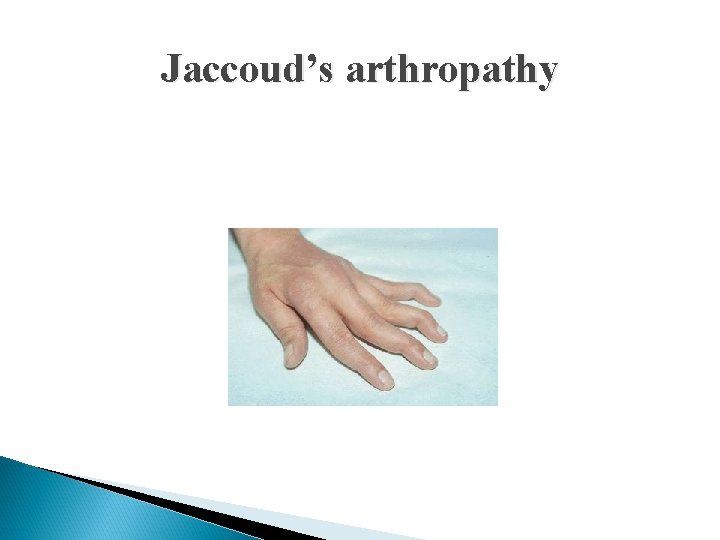
Jaccoud’s arthropathy
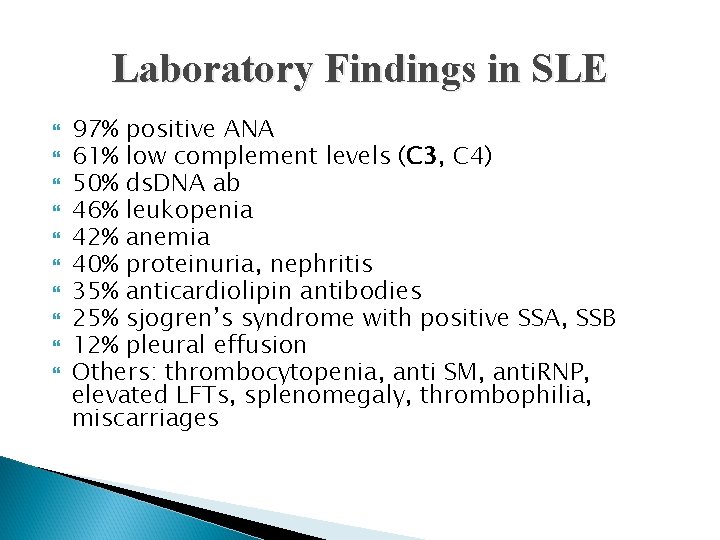
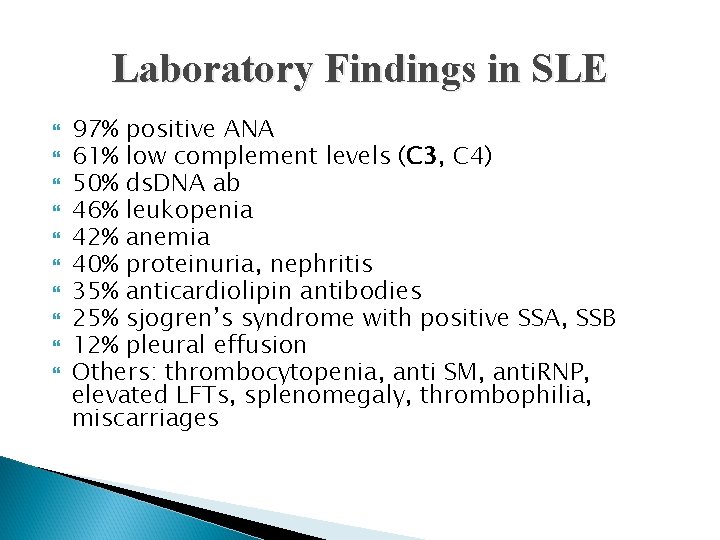
Laboratory Findings in SLE 97% positive ANA 61% low complement levels (C 3, C 4) 50% ds. DNA ab 46% leukopenia 42% anemia 40% proteinuria, nephritis 35% anticardiolipin antibodies 25% sjogren’s syndrome with positive SSA, SSB 12% pleural effusion Others: thrombocytopenia, anti SM, anti. RNP, elevated LFTs, splenomegaly, thrombophilia, miscarriages
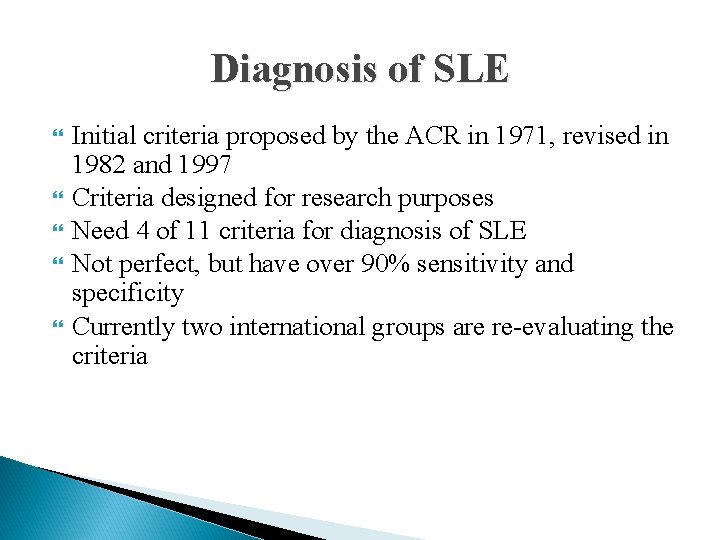
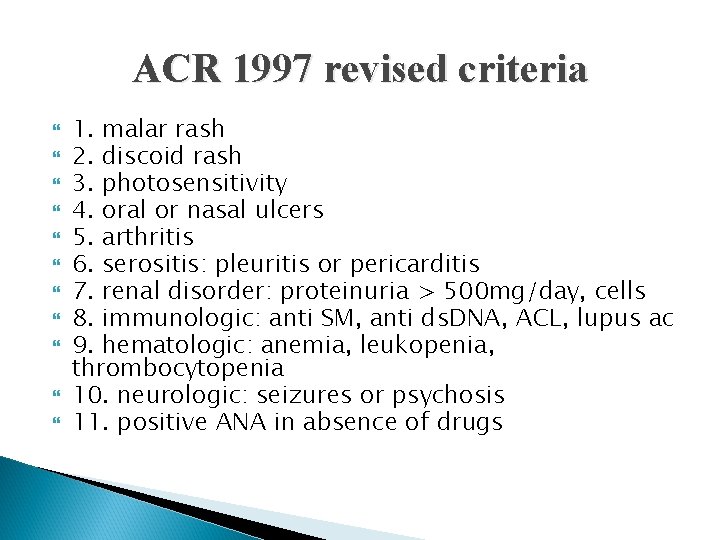
Diagnosis of SLE Initial criteria proposed by the ACR in 1971, revised in 1982 and 1997 Criteria designed for research purposes Need 4 of 11 criteria for diagnosis of SLE Not perfect, but have over 90% sensitivity and specificity Currently two international groups are re-evaluating the criteria
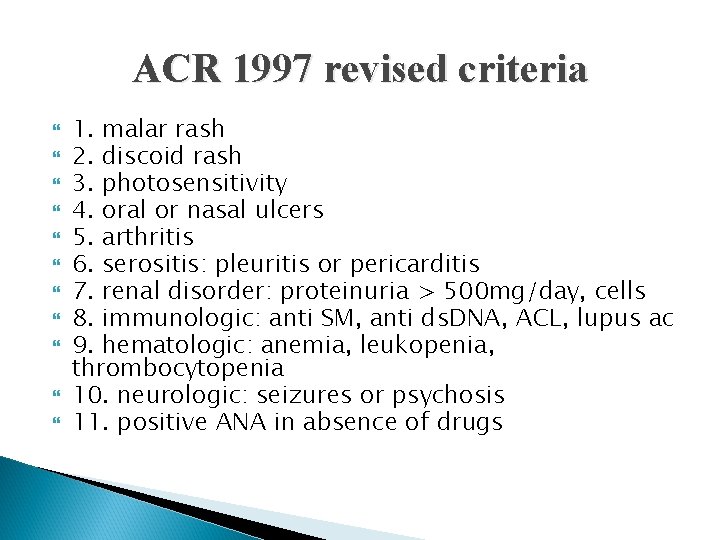
ACR 1997 revised criteria 1. malar rash 2. discoid rash 3. photosensitivity 4. oral or nasal ulcers 5. arthritis 6. serositis: pleuritis or pericarditis 7. renal disorder: proteinuria > 500 mg/day, cells 8. immunologic: anti SM, anti ds. DNA, ACL, lupus ac 9. hematologic: anemia, leukopenia, thrombocytopenia 10. neurologic: seizures or psychosis 11. positive ANA in absence of drugs
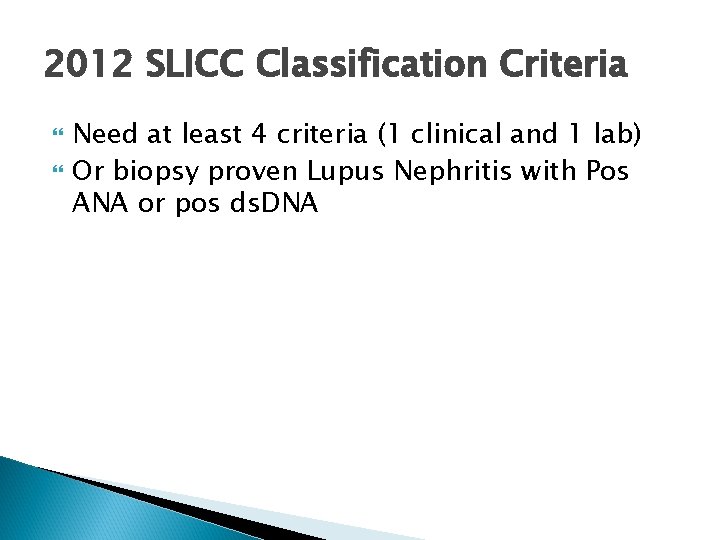
2012 SLICC Classification Criteria Need at least 4 criteria (1 clinical and 1 lab) Or biopsy proven Lupus Nephritis with Pos ANA or pos ds. DNA
Case #3 A newly diagnosed patient with lupus asks you what her lifetime prognosis is. What do you say?
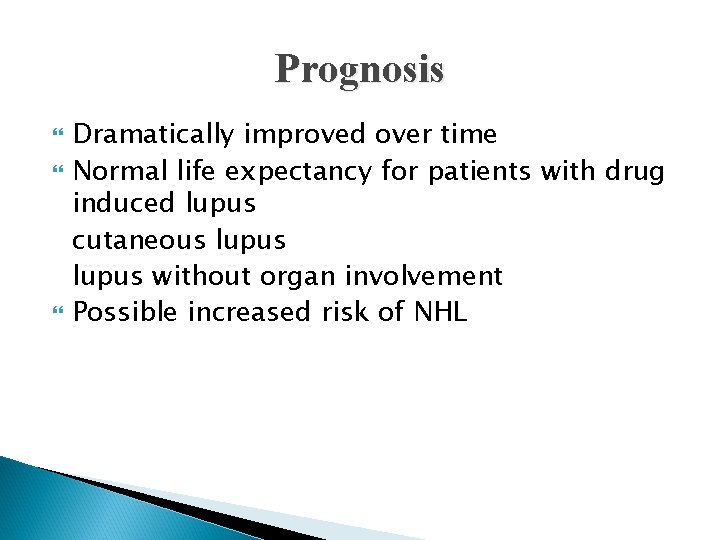
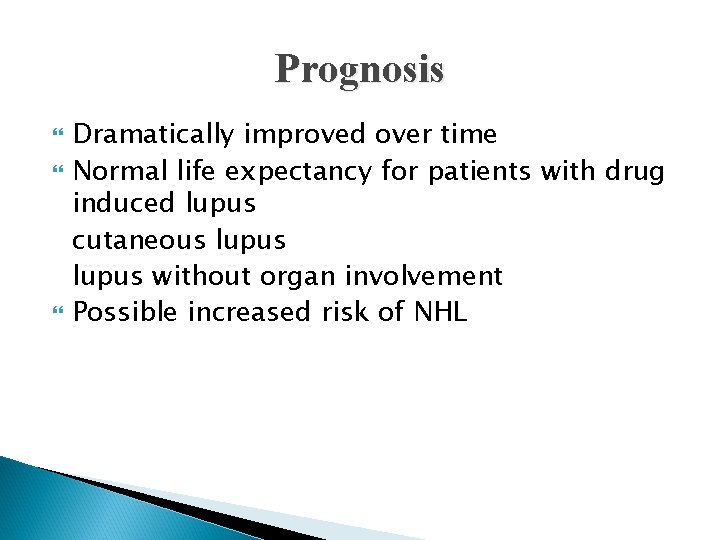
Prognosis Dramatically improved over time Normal life expectancy for patients with drug induced lupus cutaneous lupus without organ involvement Possible increased risk of NHL
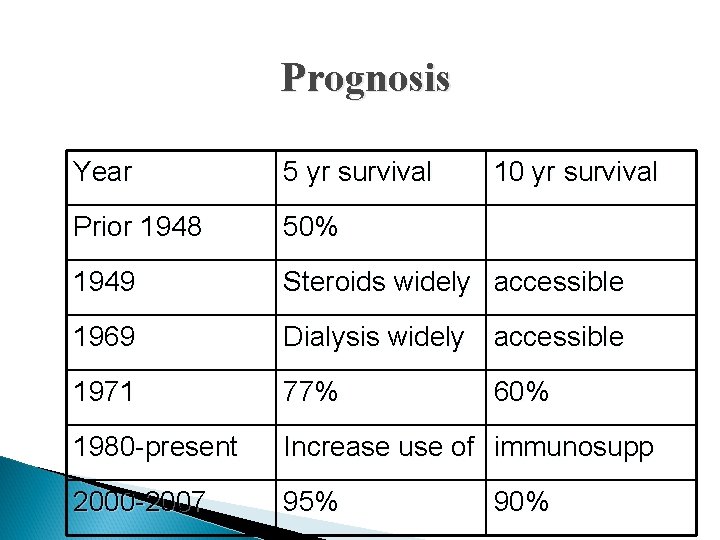
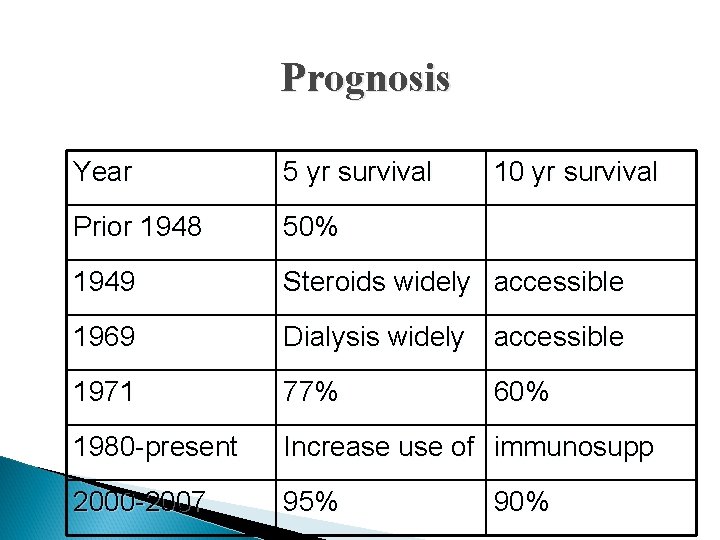
Prognosis Year 5 yr survival 10 yr survival Prior 1948 50% 1949 Steroids widely accessible 1969 Dialysis widely accessible 1971 77% 1980 -present Increase use of immunosupp 2000 -2007 95% 60% 90%
Poor Prognostic Factors Renal disease (esp DPGN) Hypertension Male sex Young age Older age at presentation Poor socioeconomic status Black race, which may primarily reflect low socioeconomic status Presence of antiphospholipid antibodies Antiphospholipid syndrome High overall disease activity
Mortality Bimodal mortality Early deaths: infection and renal involvement Later deaths: atherosclerotic disease Premenopausal women with lupus have 3050 x higher risk of CAD than their non-lupus counterparts
Treatment Individualized Evaluate their risks for organ involvement ds. DNA ab: renal and neurologic SSA/SSB ab: rashes, pregnancy risks APL ab: clotting RNP ab: may develop overlap diseases
Treatment: Patient Education 1. Avoidance sun 2. Use of SPF > 35 sunblocks UVA and UVB 3. Sun-protective clothing 4. Promote exercise 5. Healthy diet (low chol, low sugar, low salt) 6. Smoking cessation 7. Avoidance of stress (animal models) 8. Good sleep hygiene
Treatment: Antimalarials hydroxychloroquine, quinacrine (available compounded), chloroquine Prevent activation of toll like receptors 7 & 9 Used in lupus over 50 years FDA approved indication Mildest immunosuppressant Very safe, risk of retinal toxicity low Eye exam once yearly
Hydroxychlorquine Takes 6 weeks to kick in, up to 6 months for maximal effect Dose maximum is *** mg/kg/day Reduces intensity of flares Increases time to flare Treats skin and joint manifestations May prevent renal disease Mortality benefit Safe in pregnancy
Treatment: Steroids Mainstay for organ threatening disease Work quickly and effectively dose of 1 mg/kg/day taper over 4 -6 weeks, by 10% q week Long term AE: hyperglycemia, hyperlipidemia, accelerated atherosclerosis, bone demineralization, AVN, cataracts, glaucoma, PUD, skin thinning, emotional lability Add a steroid sparing imunosuppresant
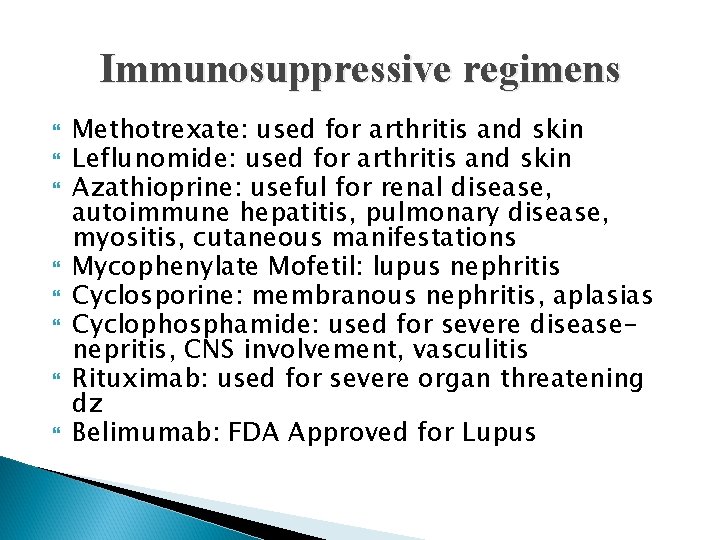
Immunosuppressive regimens Methotrexate: used for arthritis and skin Leflunomide: used for arthritis and skin Azathioprine: useful for renal disease, autoimmune hepatitis, pulmonary disease, myositis, cutaneous manifestations Mycophenylate Mofetil: lupus nephritis Cyclosporine: membranous nephritis, aplasias Cyclophosphamide: used for severe diseasenepritis, CNS involvement, vasculitis Rituximab: used for severe organ threatening dz Belimumab: FDA Approved for Lupus
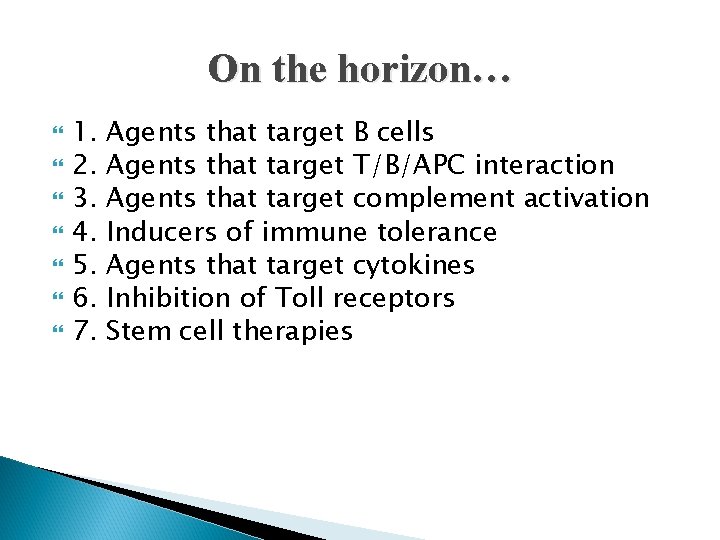
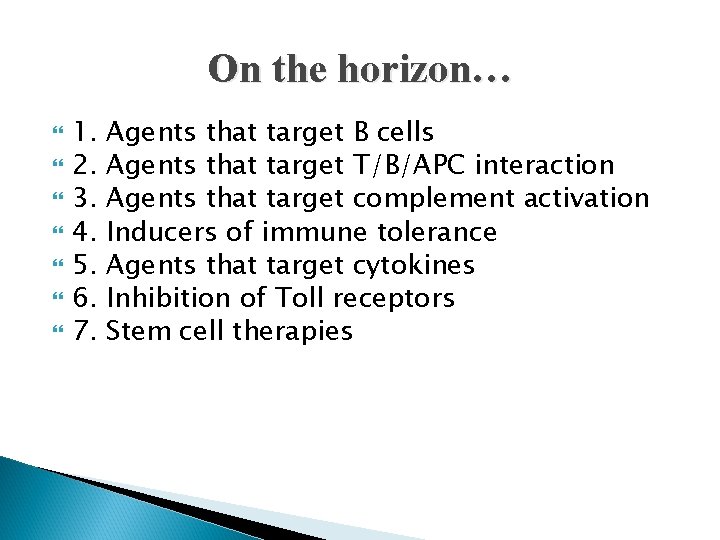
On the horizon… 1. 2. 3. 4. 5. 6. 7. Agents that target B cells Agents that target T/B/APC interaction Agents that target complement activation Inducers of immune tolerance Agents that target cytokines Inhibition of Toll receptors Stem cell therapies
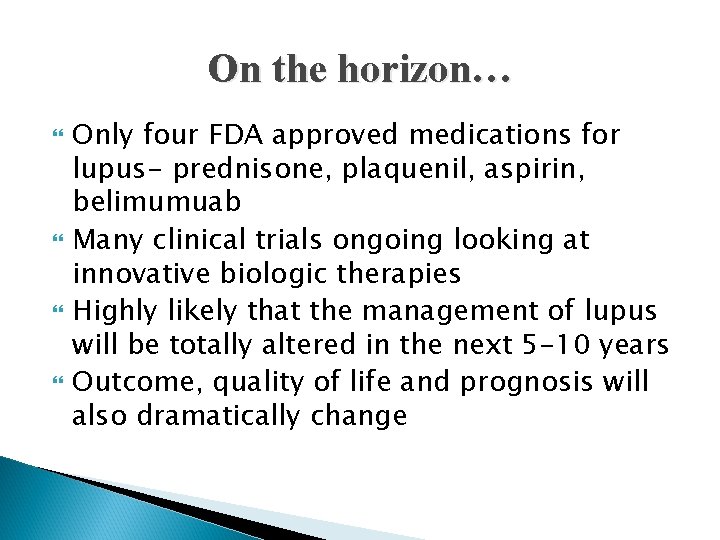
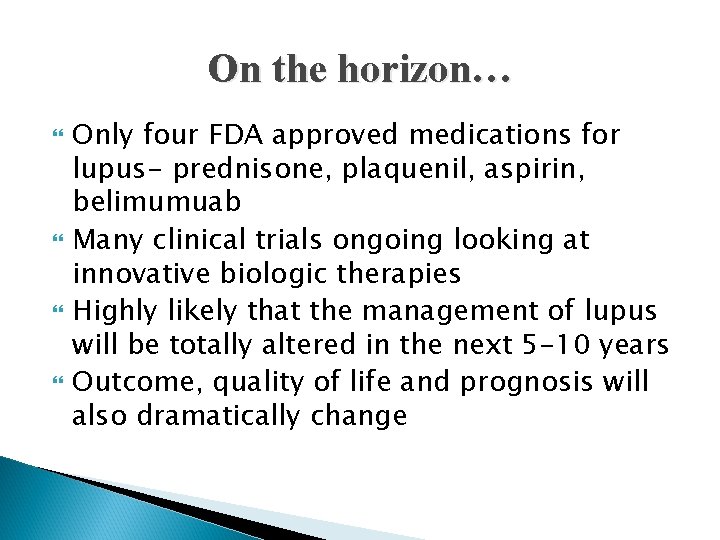
On the horizon… Only four FDA approved medications for lupus- prednisone, plaquenil, aspirin, belimumuab Many clinical trials ongoing looking at innovative biologic therapies Highly likely that the management of lupus will be totally altered in the next 5 -10 years Outcome, quality of life and prognosis will also dramatically change
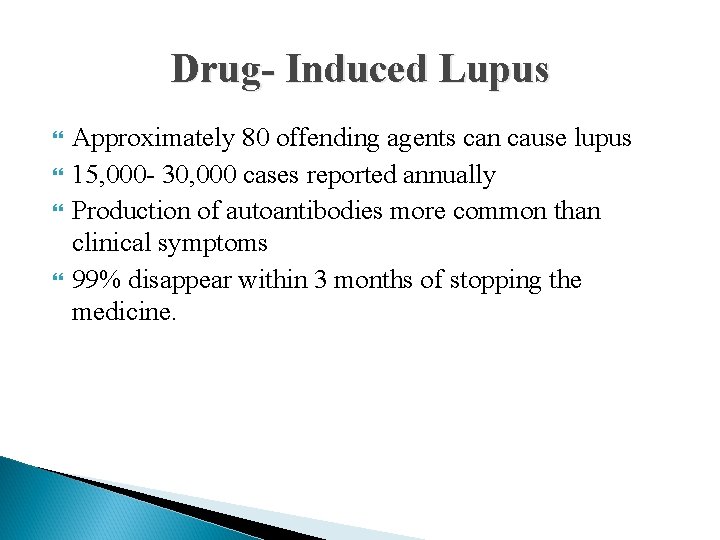
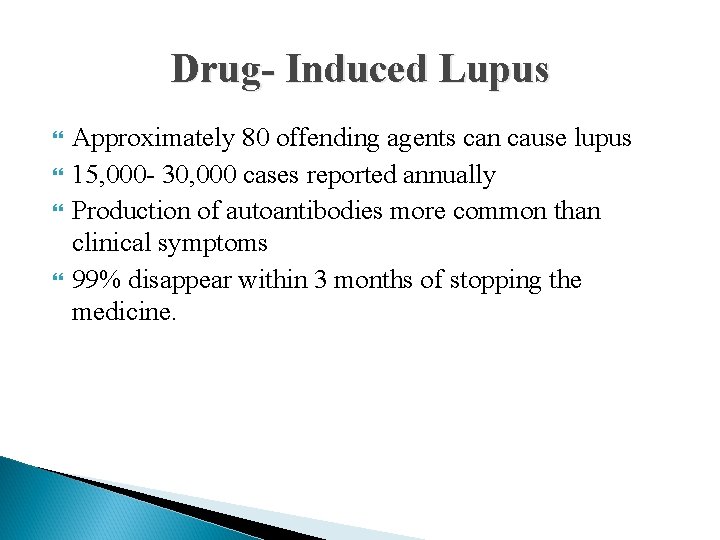
Drug- Induced Lupus Approximately 80 offending agents can cause lupus 15, 000 - 30, 000 cases reported annually Production of autoantibodies more common than clinical symptoms 99% disappear within 3 months of stopping the medicine.
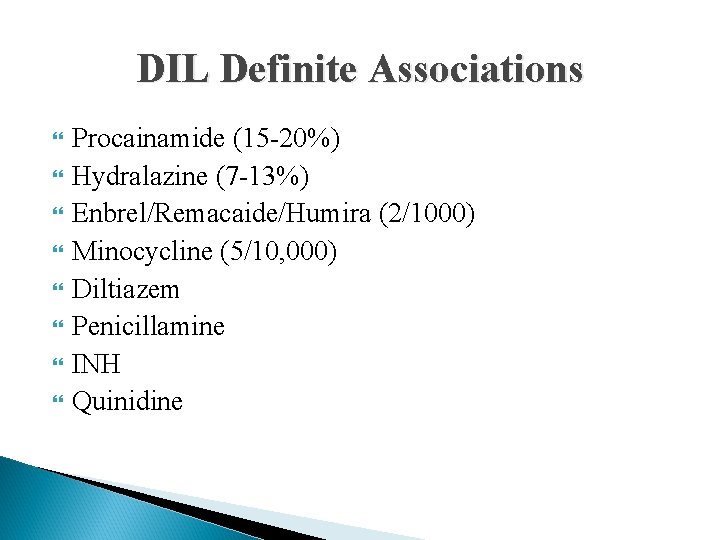
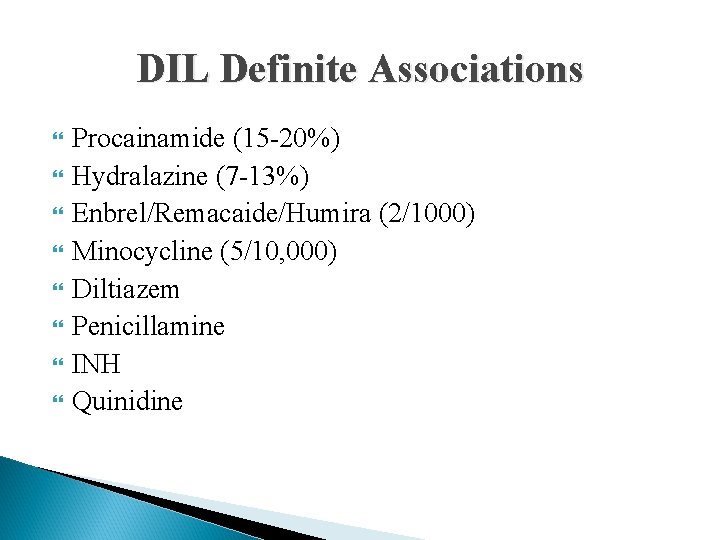
DIL Definite Associations Procainamide (15 -20%) Hydralazine (7 -13%) Enbrel/Remacaide/Humira (2/1000) Minocycline (5/10, 000) Diltiazem Penicillamine INH Quinidine
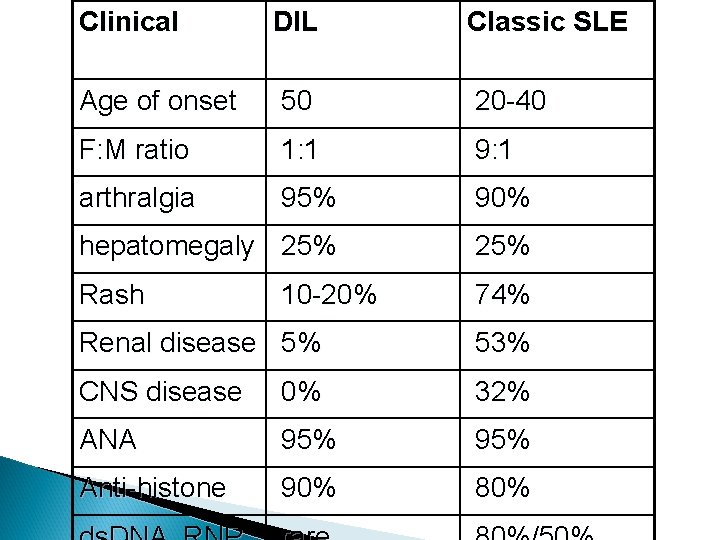
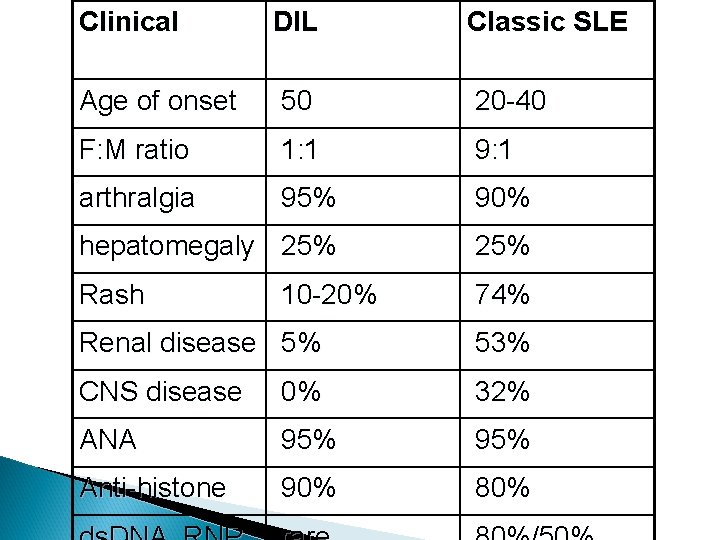
Clinical DIL Classic SLE Age of onset 50 20 -40 F: M ratio 1: 1 9: 1 arthralgia 95% 90% hepatomegaly 25% Rash 74% 10 -20% Renal disease 5% 53% CNS disease 0% 32% ANA 95% Anti-histone 90% 80%
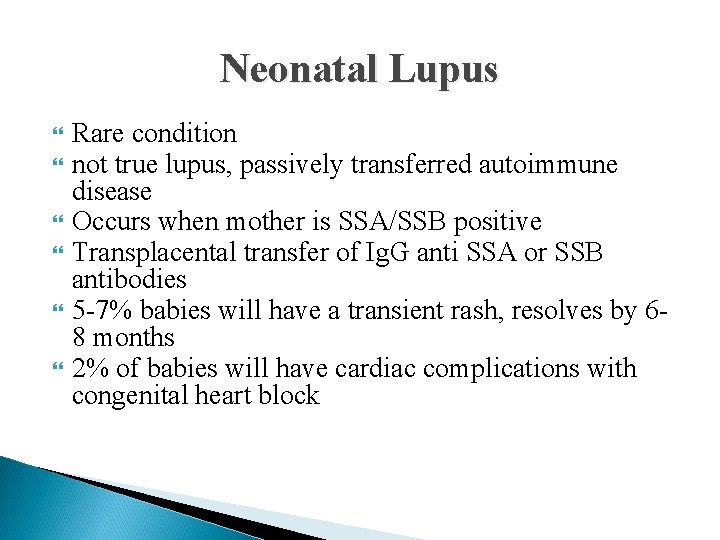
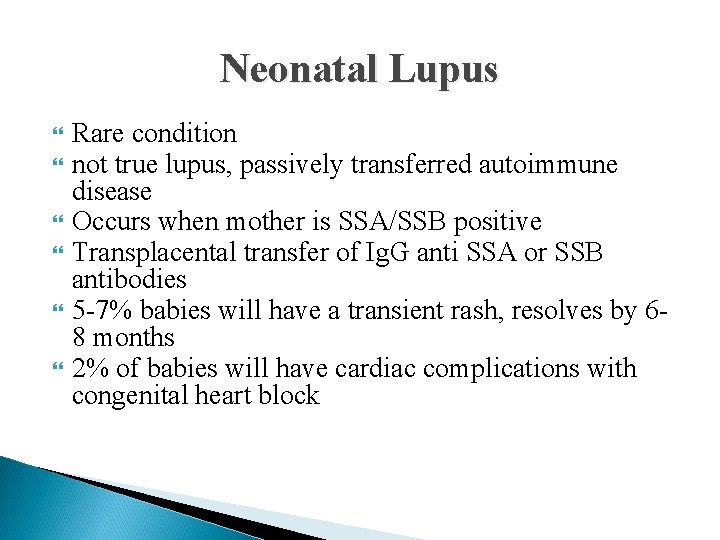
Neonatal Lupus Rare condition not true lupus, passively transferred autoimmune disease Occurs when mother is SSA/SSB positive Transplacental transfer of Ig. G anti SSA or SSB antibodies 5 -7% babies will have a transient rash, resolves by 68 months 2% of babies will have cardiac complications with congenital heart block
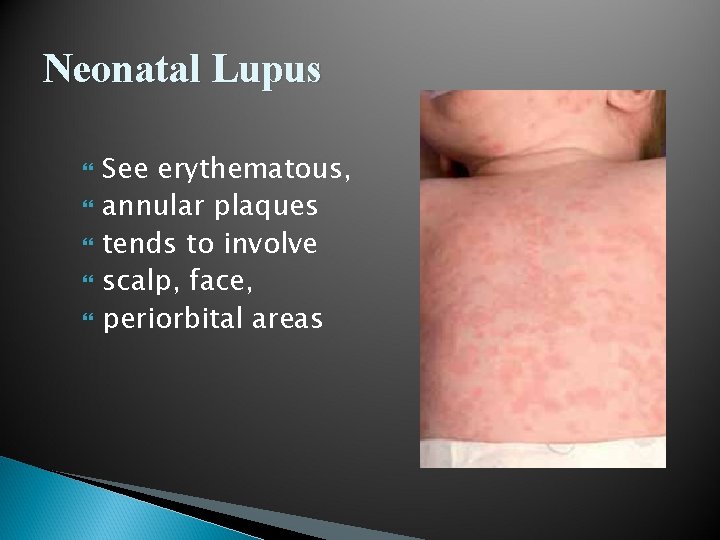
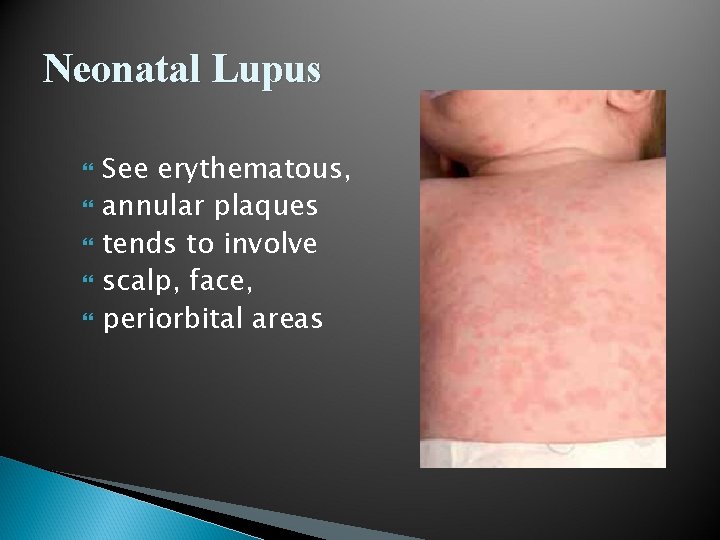
Neonatal Lupus See erythematous, annular plaques tends to involve scalp, face, periorbital areas

 Case study 87 systemic lupus erythematosus
Case study 87 systemic lupus erythematosus Sle criteria
Sle criteria Quadrilateral pentagon hexagon octagon
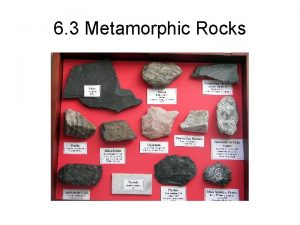
Quadrilateral pentagon hexagon octagon Meta means in metamorphism
Meta means in metamorphism Meta means change and morph means heat
Meta means change and morph means heat Ex situ conservation definition
Ex situ conservation definition Bio means life
Bio means life How much kontos per gallon
How much kontos per gallon Mycoses
Mycoses Local and systemic difference
Local and systemic difference Systemic effects of immobility
Systemic effects of immobility Major veins of the body
Major veins of the body Ion storm
Ion storm Svr calculation
Svr calculation Chapter 15 preventive dentistry
Chapter 15 preventive dentistry Blood supply of stomach flowchart
Blood supply of stomach flowchart Systemic acquired resistance in plants
Systemic acquired resistance in plants Systemic pathology exam questions pdf
Systemic pathology exam questions pdf Systemic acquired resistance in plants
Systemic acquired resistance in plants Indications and contraindications of tooth extraction
Indications and contraindications of tooth extraction Hypertension medical definition
Hypertension medical definition Human diseases a systemic approach
Human diseases a systemic approach Figure 11-4
Figure 11-4 Local factor affecting wound healing
Local factor affecting wound healing Pulmonary systemic
Pulmonary systemic Overview of the major systemic arteries
Overview of the major systemic arteries Vasoreflexes
Vasoreflexes Systemic barriers examples
Systemic barriers examples Blood supply of heart
Blood supply of heart Overview of the major systemic arteries
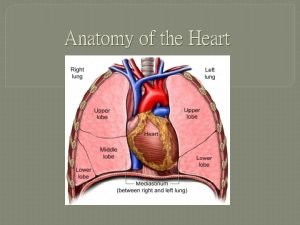
Overview of the major systemic arteries Correctly label the following internal anatomy of the heart
Correctly label the following internal anatomy of the heart Systemic sustainability education
Systemic sustainability education Systemic social work
Systemic social work Systemic error
Systemic error Systemic examination of respiratory system
Systemic examination of respiratory system Portacaval anastomosis
Portacaval anastomosis Hepatic portal system diagram
Hepatic portal system diagram Alhashli
Alhashli Applied anthropology's systemic perspective recognizes that
Applied anthropology's systemic perspective recognizes that Sfl
Sfl Arteries of the thorax
Arteries of the thorax Ncf curriculum framework 2005
Ncf curriculum framework 2005 Extravasation vs phlebitis
Extravasation vs phlebitis Arteries of the systemic circulation
Arteries of the systemic circulation Arteries of the systemic circulation
Arteries of the systemic circulation Respiratory zone structures
Respiratory zone structures Inscryption ringworm card
Inscryption ringworm card Systemic family therapy techniques
Systemic family therapy techniques Di syston systemic insecticide
Di syston systemic insecticide