Sytemic Lupus Erythematosus SLE Introduction Lupus is classified
- Slides: 10
Sytemic Lupus Erythematosus SLE
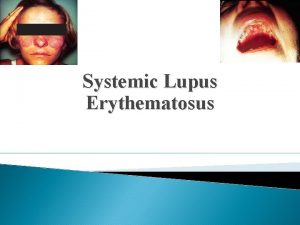
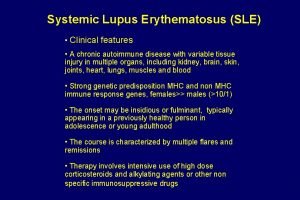
Introduction • Lupus is classified as discoid (skin) , systemic, or drug-induced. • Discoid • Primarily affects the skin. • Erythematosus butterfly rash over nose and cheeks. • Generally self-limiting. • Systemic • Affects the connective tissues of multiple organ systems. • Can lead to major organ failure. • Drug-induced • Drugs: hydralazine, isoniazid • Symptoms resolve when the drug is discontinued. • Does not cause renal or neurological disease.
Key factors • Systemic Lupus Erythematosus (SLE) is a chronic, inflammatory autoimmune disease. • Varies in severity and progression. • Chronic; exacerbations (flares) and remissions. • Lupus may be difficult to diagnose because of the vagueness of early symptoms. • The cause of lupus is unknown. • There is no known cure for discoid or systemic lupus.
Risk Factors • Female gender between the ages of 15 and 40 (drops after menopause) • Diagnostic Procedures and • • • Nursing Interventions Antinuclear Antibody Titer (antibody produced against one’s own DNA) Lupus Antibodies Decreased BUN, Serum Creatinine: Elevated (with renal involvement) Urinalysis: Positive for protein, RBCs (renal involvement) CBC: Pancytopenia
Assessments • • • Monitor for signs and symptoms. Fatigue/malaise Fever (also major symptom of exacerbation) Butterfly rash on face Alopecia Anorexia/weight loss Anemia Lymphadenopathy Depression Joint pain, swelling, tenderness Raynaud’s phenomenon (arteriolar vasospasm in response to cold/stress)
Assess/Monitor • Pain, mobility, and fatigue • Vital signs (especially blood pressure) • For systemic manifestations: • • HTN, edema, Urine output, BUN, serum creatinine (renal compromise) Diminished breath sounds (pleural effusion) Tachycardia, sharp inspiratory chest pain (pericarditis) Rubor, pallor, cyanosis of hands/feet (vasculitis/vasospasm, Raynaud’s phenomenon) Arthralgias, myalgias, polyarthritis (joint, connective tissue involvement) • Psychoses, paresis, seizures (neurologic involvement) • Nutritional status
NANDANursing. Diagnoses • • • Risk for infection Acute pain, chronic pain Deficient knowledge Ineffective coping Risk for altered tissue perfusion (cardiac, renal, peripheral)
Nursing. Interventions • • Teach the client regarding the need to: Avoid UV and sun exposure. Use sunscreen when outside and exposed to sunlight. Use mild protein shampoo and avoid harsh hair treatments. Use steroid creams for skin rash. Report peripheral and periorbital edema promptly. Report signs/symptoms of infection related to immunosuppression.
Medical Management • NSAIDs to reduce inflammation (Gastric ulcer, NSAID-induced • • • hepatitis), contraindicated for clients with renal compromise. Corticosteroids (fluid retention, HTN, and renal dysfunction), weaning Immunosuppressant agents (methotrexate) (bone marrow suppression, increased liver enzymes). Antimalarial for suppression of synovitis, fever, and fatigue. Encourage frequent eye examinations. Provide small, frequent meals if anorexia is a problem. Offer betweenmeal supplements. Encourage the client to limit salt intake for fluid retention secondary to steroid therapy. Provide emotional support to the client and significant others. Refer to support groups as appropriate.
Complicationsand. Nursing Implications • • Renal failure/glomerulonephritis (major cause of death) Pericarditis, myocarditis (instruct client to report chest pain) Vasculitis (major organ ischemia) Osteonecrosis (constriction of small blood vessels supplying hip joint) secondary to corticosteroids • Increased incidence of miscarriage, stillbirth, premature birth, and other pregnancy-related complications (sexual counseling regarding contraception)