Lupus erythematosus Definition Lupus erythematosus LE is classified









- Slides: 31
Lupus erythematosus
Definition Lupus erythematosus LE is classified as connective tissue disease. It occurs predominantly in females in the reproductive years. Multiple abnormal immune responses are present. It may involved any organ of the body and is manifested in many forms. It may be lifethreatening when it becomes severe.
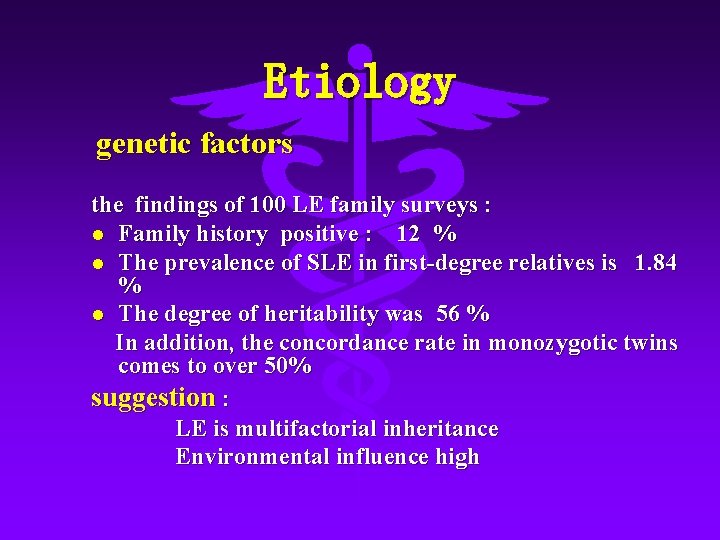
Etiology genetic factors the findings of 100 LE family surveys : l Family history positive : 12 % l The prevalence of SLE in first-degree relatives is 1. 84 % l The degree of heritability was 56 % In addition, the concordance rate in monozygotic twins comes to over 50% suggestion : LE is multifactorial inheritance Environmental influence high
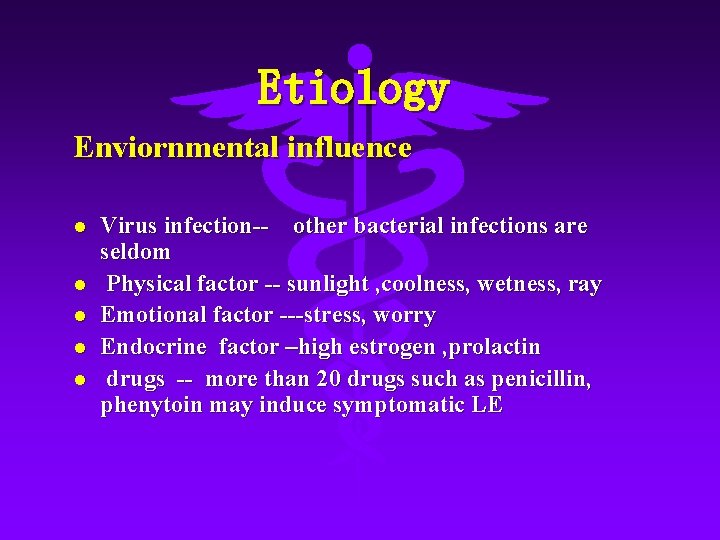
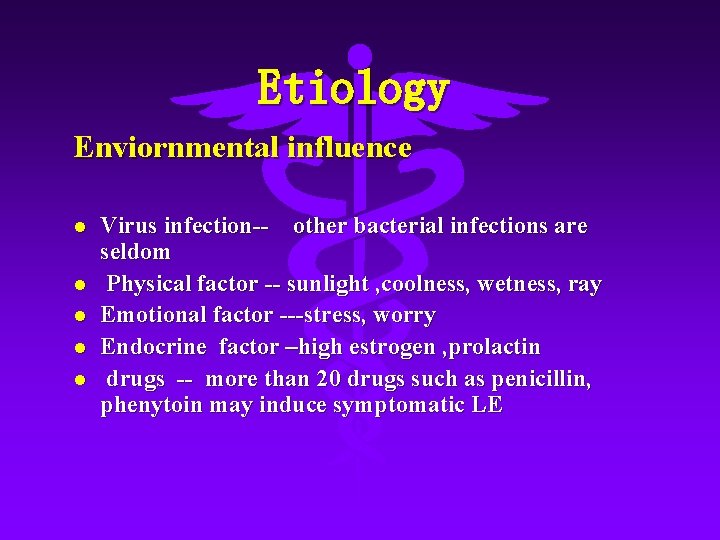
Etiology Enviornmental influence l l l Virus infection-- other bacterial infections are seldom Physical factor -- sunlight , coolness, wetness, ray Emotional factor ---stress, worry Endocrine factor –high estrogen , prolactin drugs -- more than 20 drugs such as penicillin, phenytoin may induce symptomatic LE
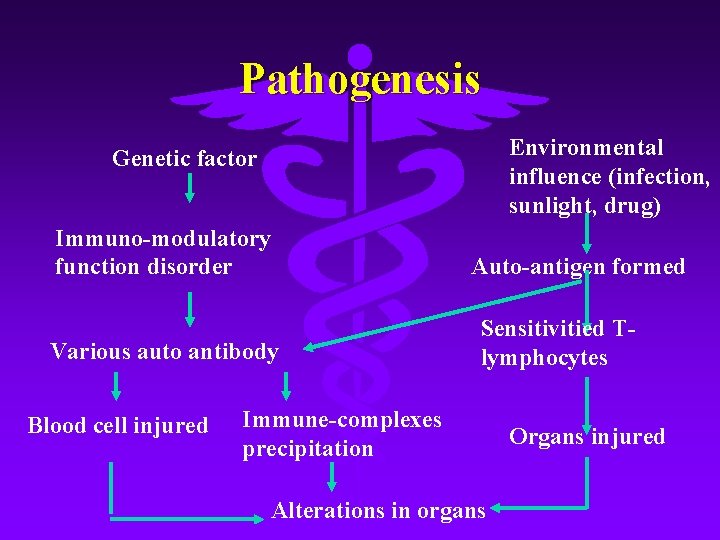
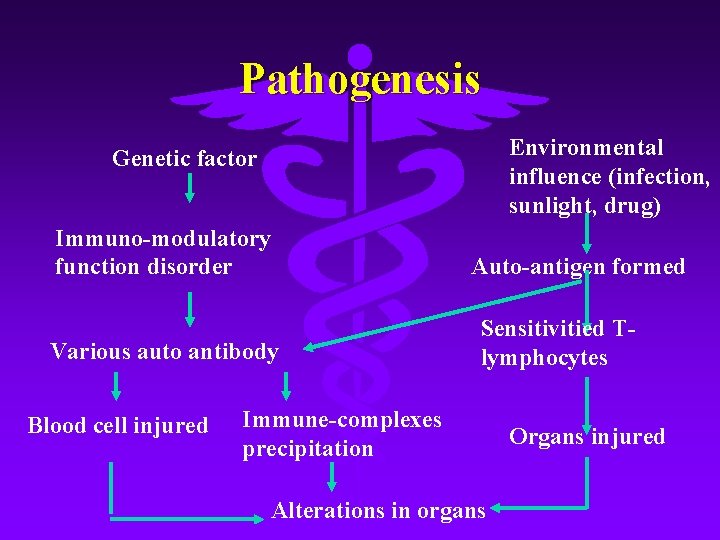
Pathogenesis Environmental influence (infection, sunlight, drug) Genetic factor Immuno-modulatory function disorder Various auto antibody Blood cell injured Auto-antigen formed Sensitivitied Tlymphocytes Immune-complexes precipitation Alterations in organs Organs injured

Clinical manifestation l Discoid LE ←→★ Systemic LE
Discoid lupus erythematosus, DLE l l Skin lesions are predominantly manifested Eruptions may occur singly or be multiple localized DLE Lesions localized on face, dorsa of the hand generalized DLE Lesions widespread on trunk , extremities

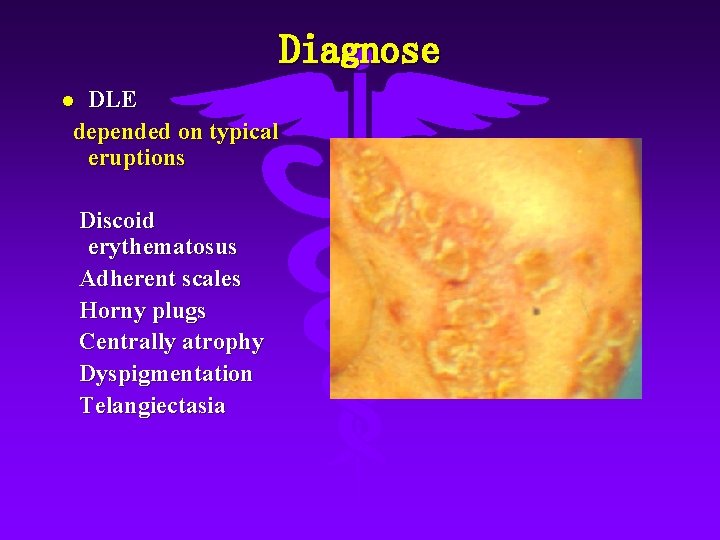
Skin lesions in discoid LE l Red macules or papules associated with edema→→ discoid eyrthematosus with adherent scales, horny plugs—-centrally atrophy, dyspigmentation, telangiectasia



skin lesions in discoid LE Favorite sites are malar areas, bridge of nose, lower lip, ear, scalp and dorsa of the hand

Skin lesions in discoid LE atrophy in the scalp → false alopecia areata lesions on low lip may be eroded
Systemic lupus erythematosus l l SLE may involved any organ of the body and is manifested in many forms. It will be life-threatening when severely. Basic pathology alteration shows necrotizing vasculitis
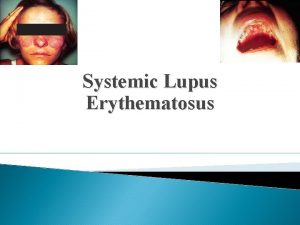
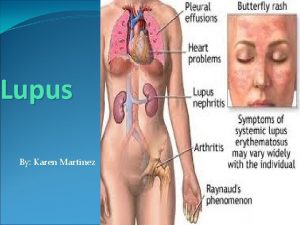
Skin and mucous membrane lesions l l Skin involvement occurs in 80% of cases. It is often the earliest abnormality and predominant symptom. Sunlight may develop the facial eruption and a severe relapse. Mulity form : erythema, papule, blood blister Specific eruption: malar erythema on finger pulp or toe pulp erythema around the nail fold
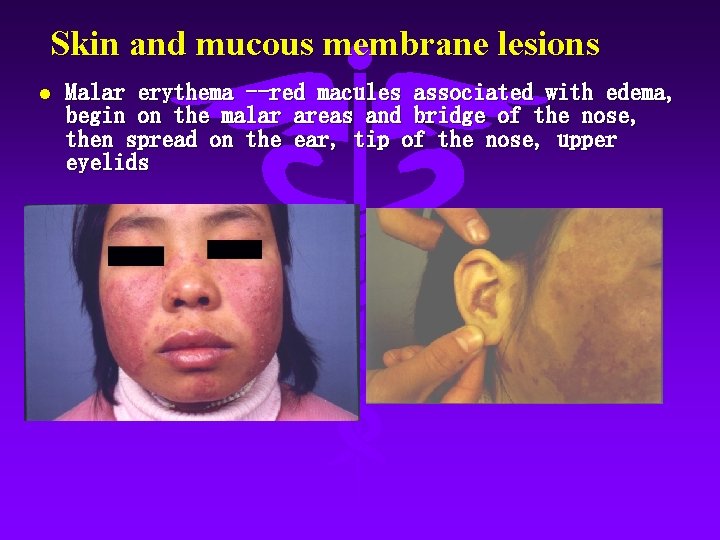
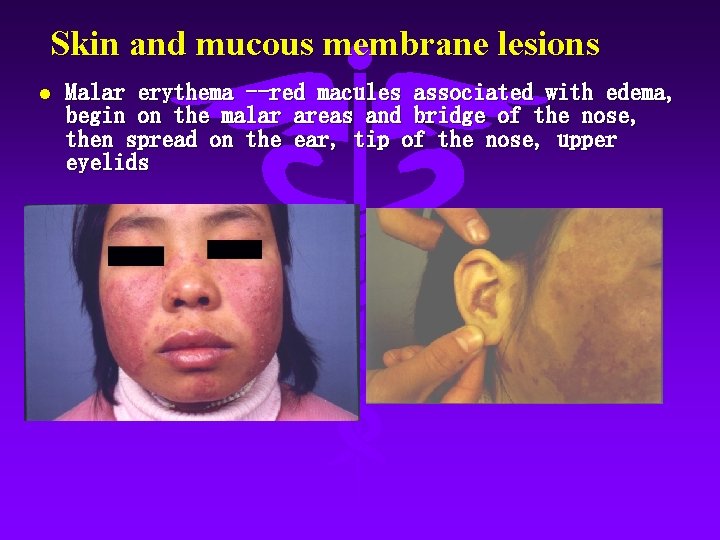
Skin and mucous membrane lesions l Malar erythema --red macules associated with edema, begin on the malar areas and bridge of the nose, then spread on the ear, tip of the nose, upper eyelids

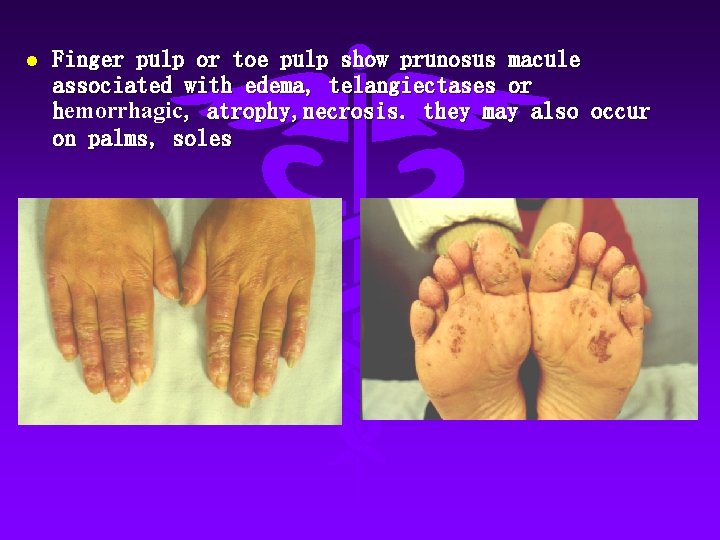
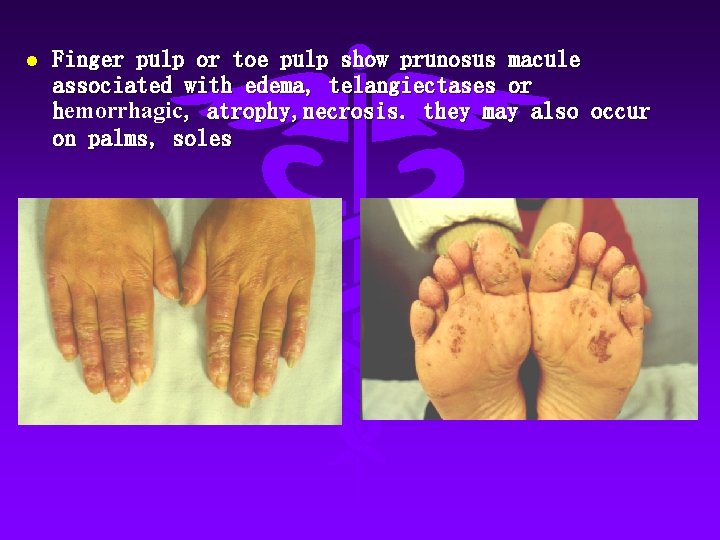
l Finger pulp or toe pulp show prunosus macule associated with edema, telangiectases or hemorrhagic, atrophy, necrosis. they may also occur on palms, soles
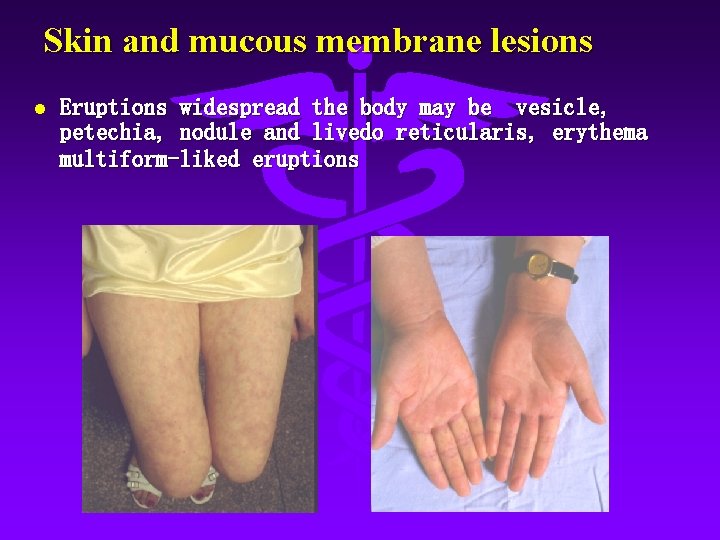
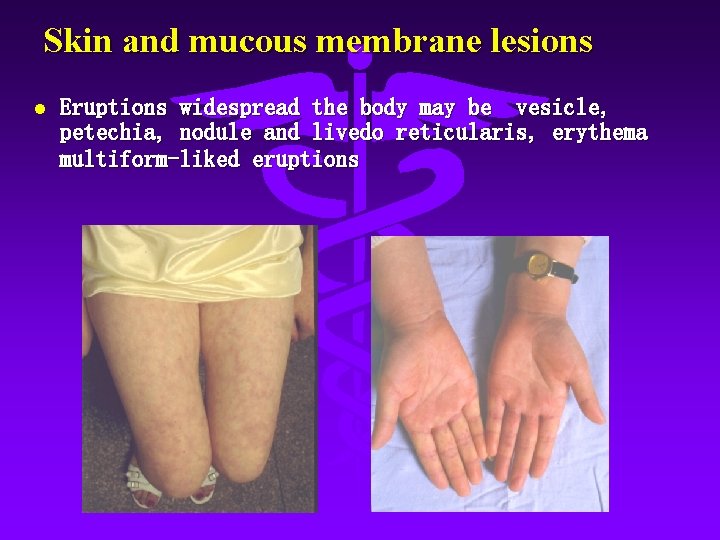
Skin and mucous membrane lesions l Eruptions widespread the body may be vesicle, petechia, nodule and livedo reticularis, erythema multiform-liked eruptions
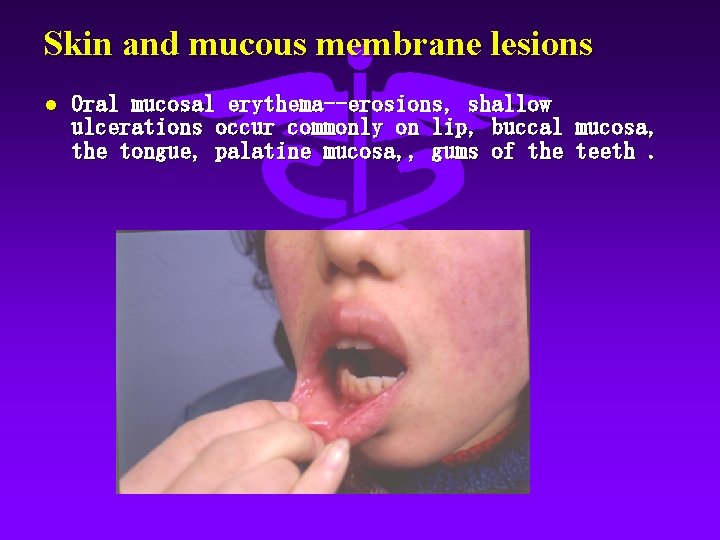
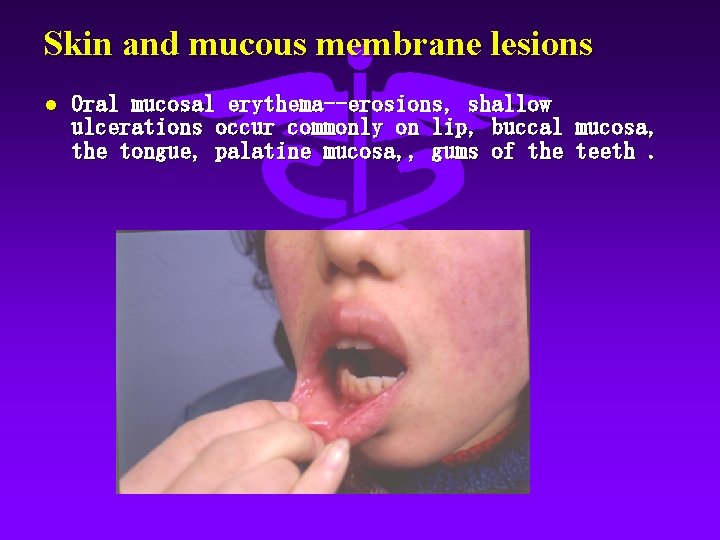
Skin and mucous membrane lesions l Oral mucosal erythema--erosions, shallow ulcerations occur commonly on lip, buccal mucosa, the tongue, palatine mucosa, , gums of the teeth.
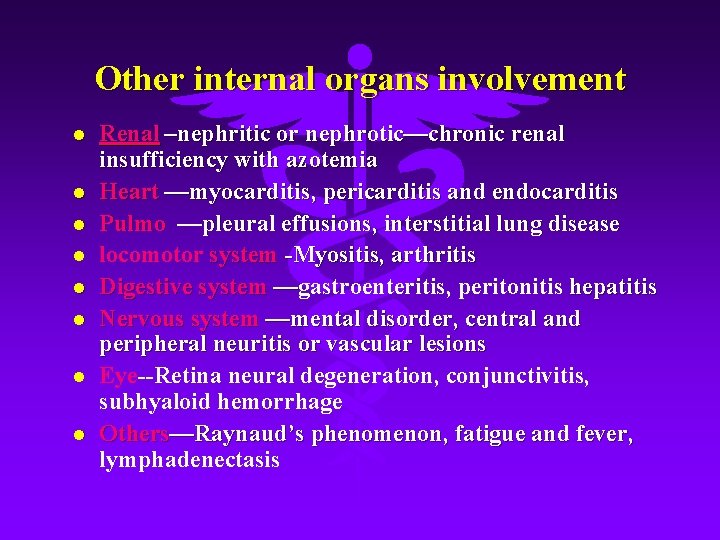
Other internal organs involvement l l l l Renal –nephritic or nephrotic—chronic renal insufficiency with azotemia Heart —myocarditis, pericarditis and endocarditis Pulmo —pleural effusions, interstitial lung disease locomotor system -Myositis, arthritis Digestive system —gastroenteritis, peritonitis hepatitis Nervous system —mental disorder, central and peripheral neuritis or vascular lesions Eye--Retina neural degeneration, conjunctivitis, subhyaloid hemorrhage Others—Raynaud’s phenomenon, fatigue and fever, lymphadenectasis
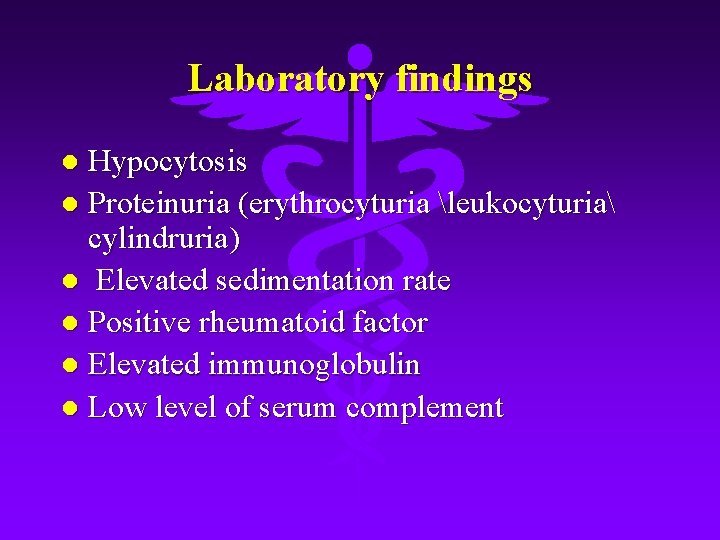
Laboratory findings Hypocytosis l Proteinuria (erythrocyturia leukocyturia cylindruria) l Elevated sedimentation rate l Positive rheumatoid factor l Elevated immunoglobulin l Low level of serum complement l
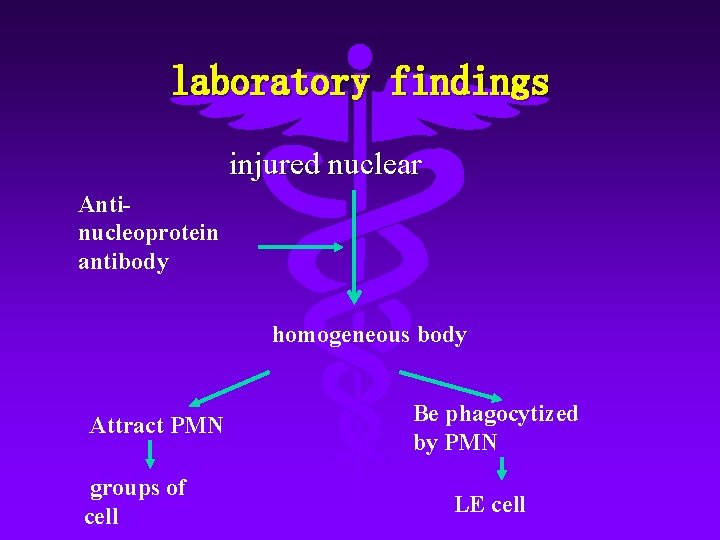
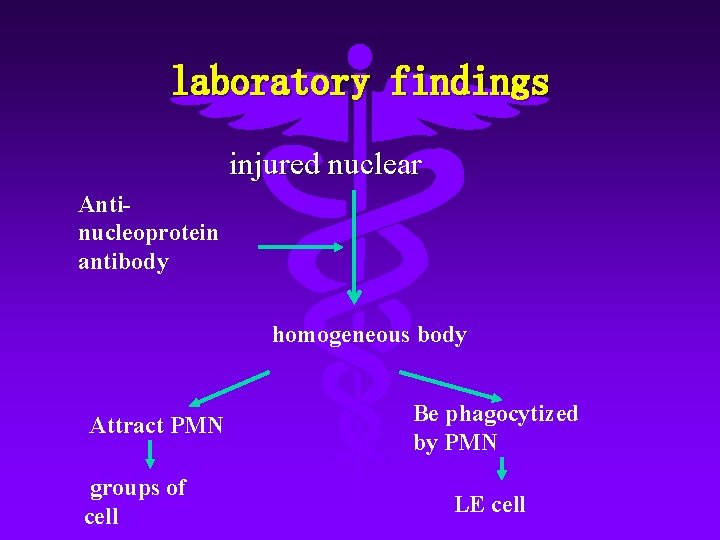
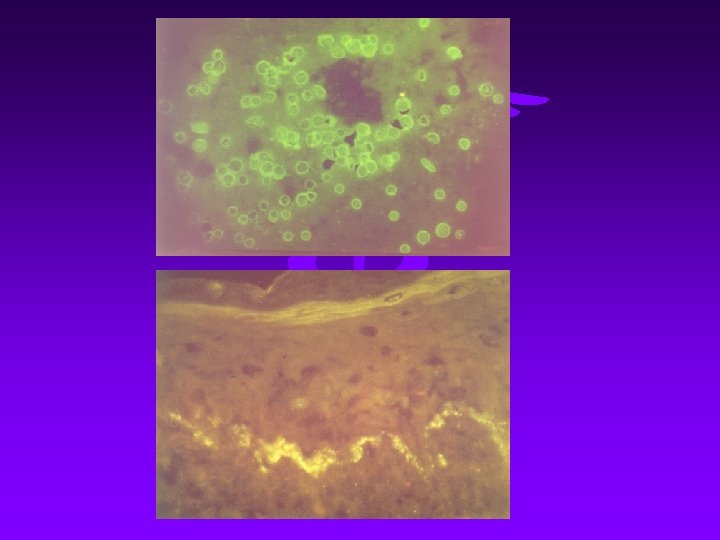
laboratory findings injured nuclear Antinucleoprotein antibody homogeneous body Attract PMN groups of cell Be phagocytized by PMN LE cell

laboratory findings l Special test(1)LE cell( cell smear)
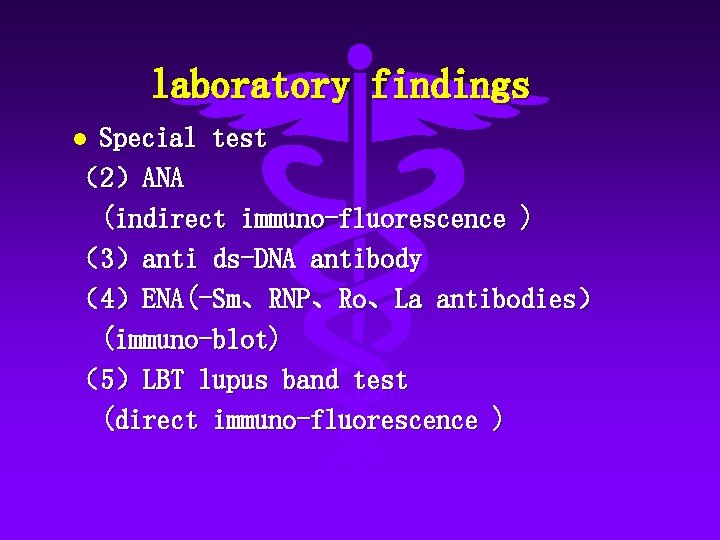
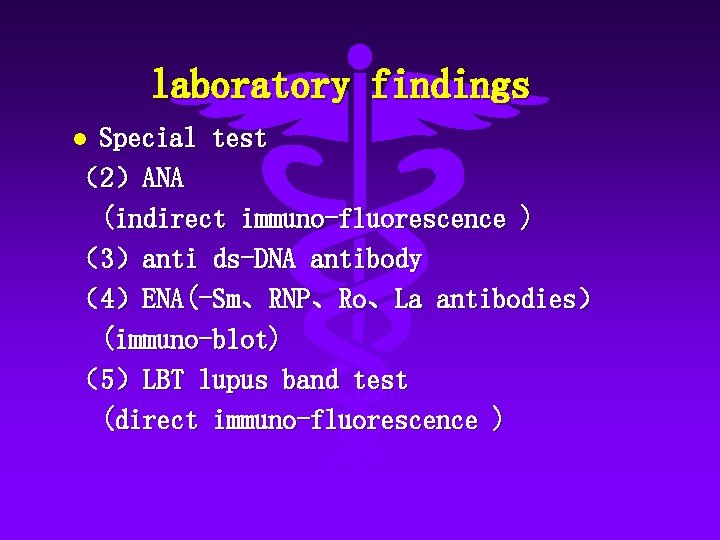
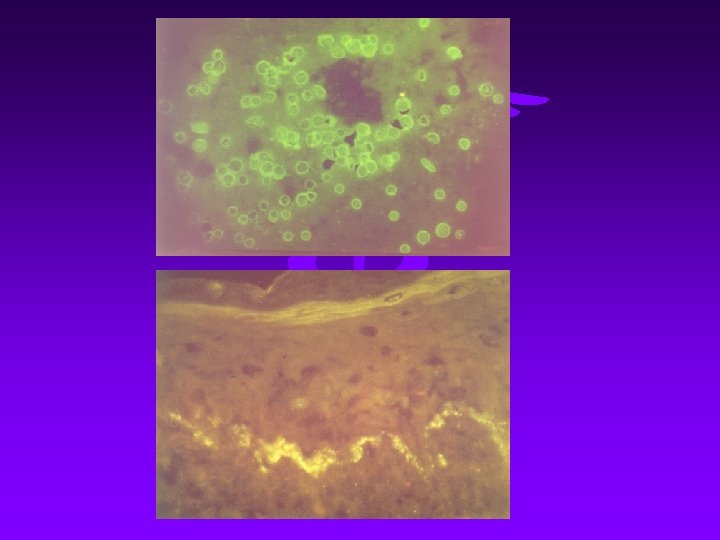
laboratory findings Special test (2)ANA (indirect immuno-fluorescence ) (3)anti ds-DNA antibody (4)ENA(-Sm、RNP、Ro、La antibodies) (immuno-blot) (5)LBT lupus band test (direct immuno-fluorescence ) l
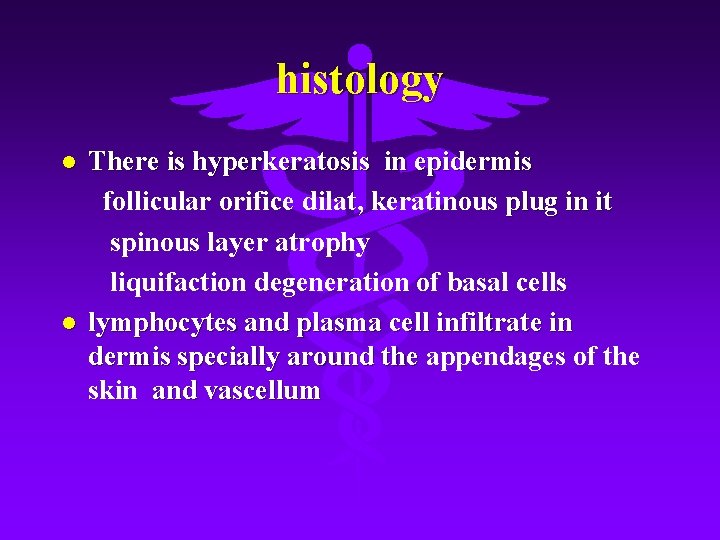
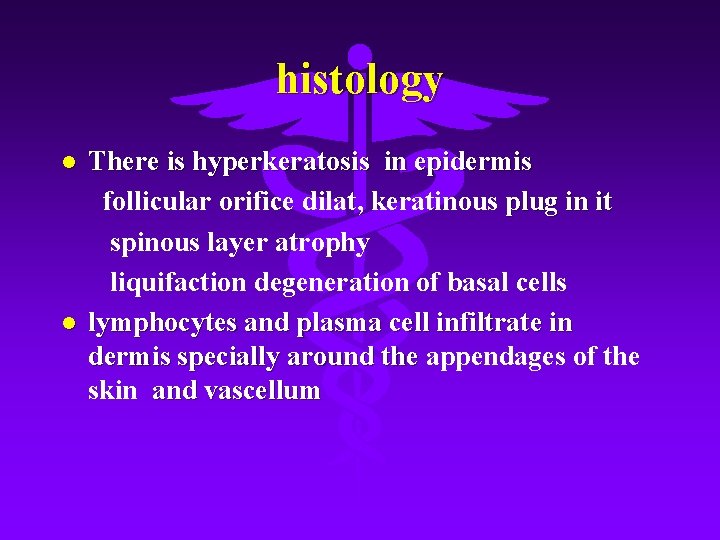
histology l l There is hyperkeratosis in epidermis follicular orifice dilat, keratinous plug in it spinous layer atrophy liquifaction degeneration of basal cells lymphocytes and plasma cell infiltrate in dermis specially around the appendages of the skin and vascellum
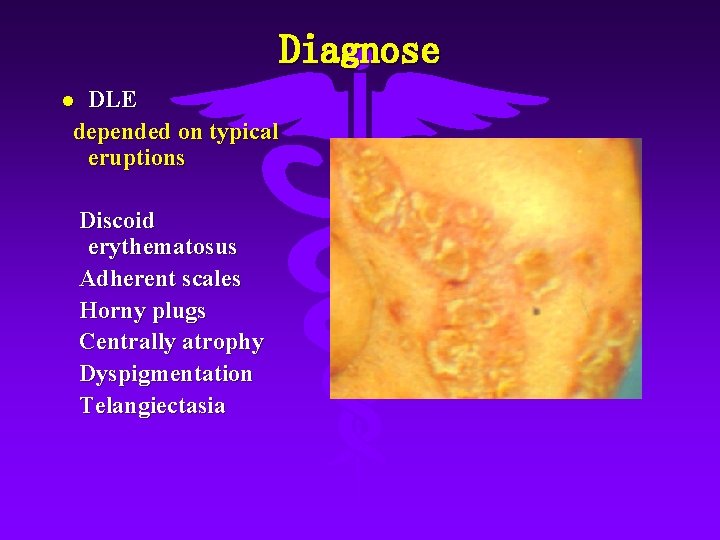
Diagnose DLE depended on typical eruptions l Discoid erythematosus Adherent scales Horny plugs Centrally atrophy Dyspigmentation Telangiectasia
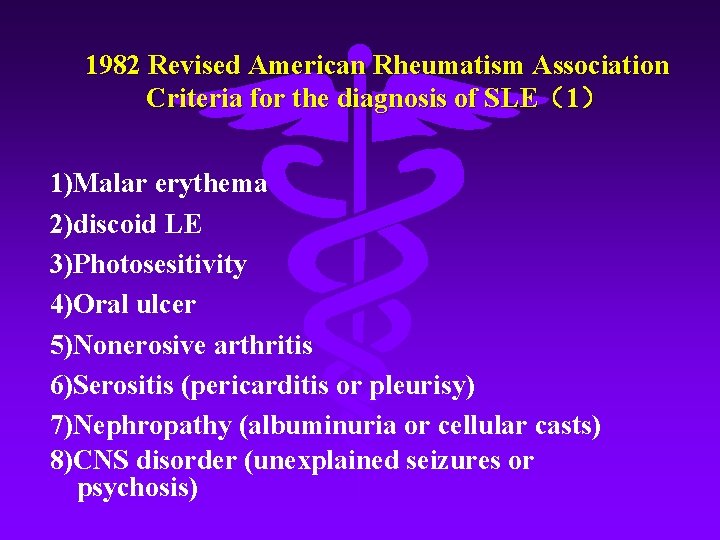
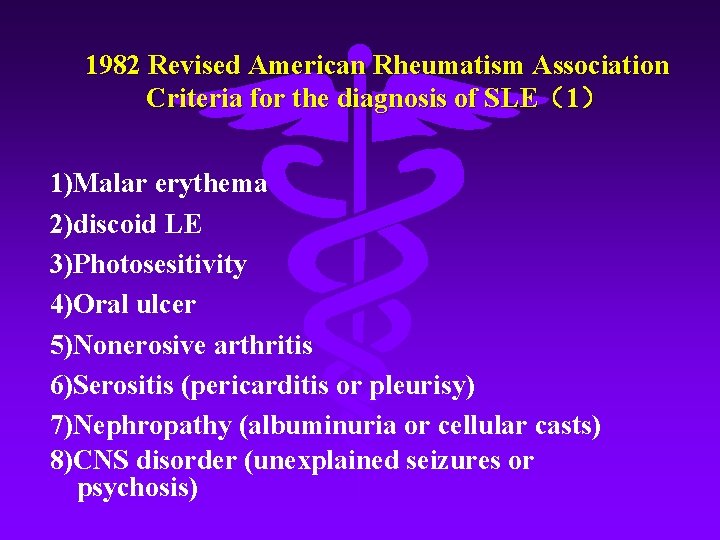
1982 Revised American Rheumatism Association Criteria for the diagnosis of SLE(1) 1)Malar erythema 2)discoid LE 3)Photosesitivity 4)Oral ulcer 5)Nonerosive arthritis 6)Serositis (pericarditis or pleurisy) 7)Nephropathy (albuminuria or cellular casts) 8)CNS disorder (unexplained seizures or psychosis)
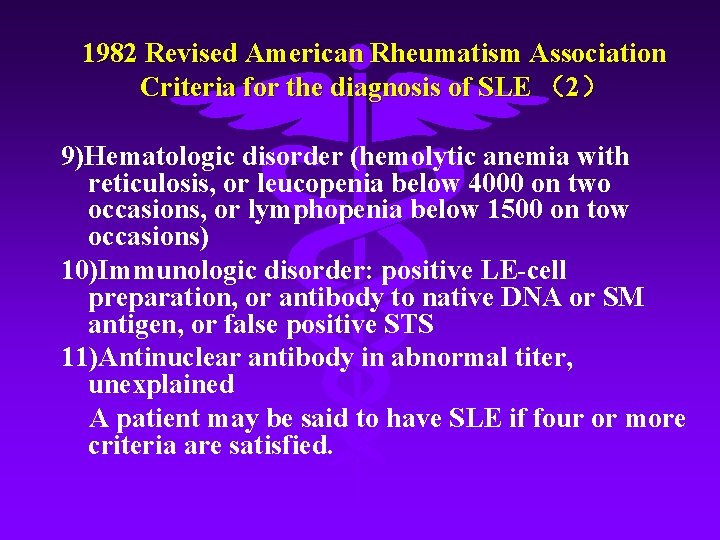
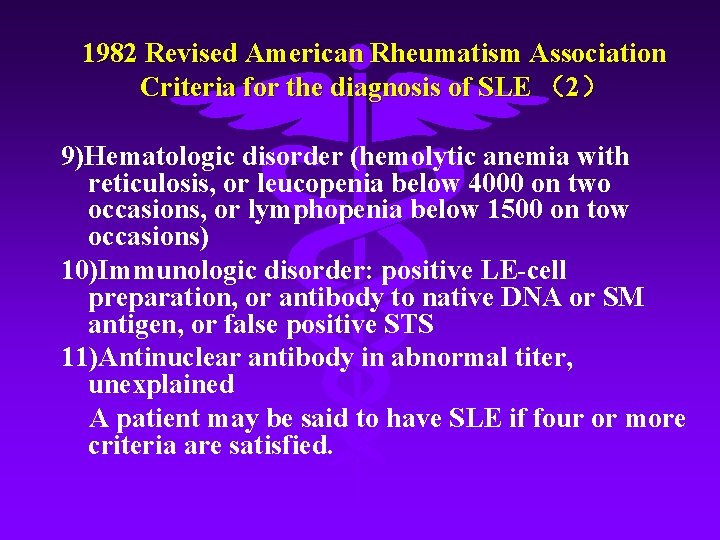
1982 Revised American Rheumatism Association Criteria for the diagnosis of SLE (2) 9)Hematologic disorder (hemolytic anemia with reticulosis, or leucopenia below 4000 on two occasions, or lymphopenia below 1500 on tow occasions) 10)Immunologic disorder: positive LE-cell preparation, or antibody to native DNA or SM antigen, or false positive STS 11)Antinuclear antibody in abnormal titer, unexplained A patient may be said to have SLE if four or more criteria are satisfied.

Treatment l l Avoid exposure to strong sunlight, to excessive cold, heat, tension , tiredness and infection For predominant skin lesion, hydroxychloroquine, thalidomide, tripterygium wilfordii are recommended , topical application of carticosteroid For patients whose organs involved, carticosteroid should be administered, and combinations of steroid with immunosuppressive drugs are recommended when necessary Others : nonsteroidal anti-inflammatory agents, immuno -modulatory drugs and other supportive treatments
 Case study 87 systemic lupus erythematosus
Case study 87 systemic lupus erythematosus Systemic lupus
Systemic lupus Lupus definition
Lupus definition Genus and species examples
Genus and species examples Raynaud's disease lupus
Raynaud's disease lupus Antifosfolipid sendromu
Antifosfolipid sendromu Slicc kriterleri
Slicc kriterleri Keberadaan hukum ketika homo homini lupus
Keberadaan hukum ketika homo homini lupus Iud and lupus
Iud and lupus Soap brain md
Soap brain md Michelle petri md
Michelle petri md Lupus nefriti sınıflaması
Lupus nefriti sınıflaması Uveiitis
Uveiitis Declinazione lupus
Declinazione lupus Ad rivum eundem lupus et agnus venerant
Ad rivum eundem lupus et agnus venerant Declinazione lupus
Declinazione lupus Asuhan keperawatan sle pada anak
Asuhan keperawatan sle pada anak Wat is sle
Wat is sle Padrao full house lupus
Padrao full house lupus Matchstick sign lupus vulgaris
Matchstick sign lupus vulgaris Lupus eritematoso sistémico
Lupus eritematoso sistémico Lupus research alliance
Lupus research alliance Lupus eritematoso sistémico
Lupus eritematoso sistémico Lupus eritematoso sistémico
Lupus eritematoso sistémico Canis lupus familiaris classification
Canis lupus familiaris classification Dentista fernando ramos
Dentista fernando ramos Adaptive immunity
Adaptive immunity Lupus immagini
Lupus immagini Lupus presentation powerpoint
Lupus presentation powerpoint Complemento lupus
Complemento lupus Dr elizabeth haryanti
Dr elizabeth haryanti Roman hakl
Roman hakl