Innate and adaptive immunity Assis Prof Dr Suhad
- Slides: 19
Innate and adaptive immunity Assis. Prof. Dr. Suhad Faisal Hatem
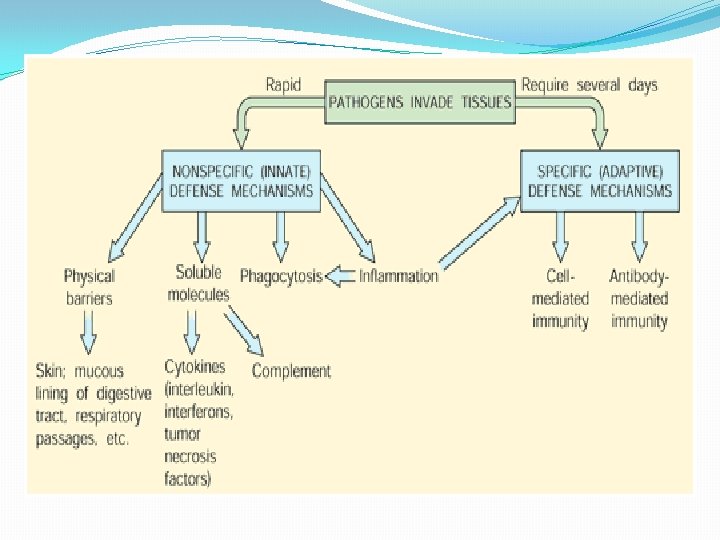
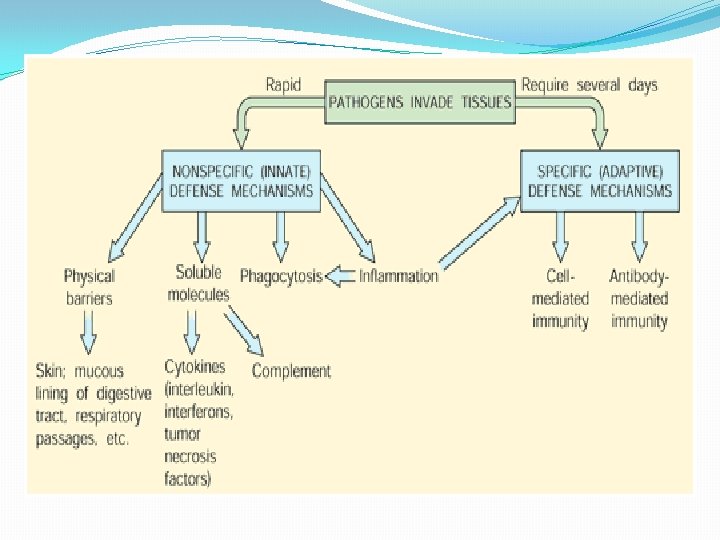
Innate immunity is considering first line of defense, an immediate response to a pathogen that does not confer lifelong protective immunity. It is includes : ürapidly mobilized at the initial site of infection but lacks immunologic memory cells. üNon specific übarriers to infectious agents, such as the skin (epithelium) and mucous membranes. üIt also includes many immune components important in the innate including phagocytic cells, natural killer (NK) cells, Toll-like receptors (TLR ), cytokines and complement.
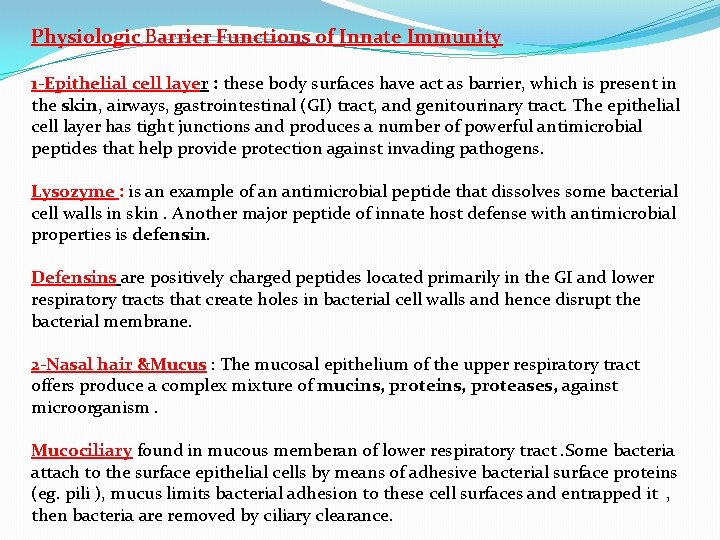
Physiologic Barrier Functions of Innate Immunity 1 -Epithelial cell layer : these body surfaces have act as barrier, which is present in the skin, airways, gastrointestinal (GI) tract, and genitourinary tract. The epithelial cell layer has tight junctions and produces a number of powerful antimicrobial peptides that help provide protection against invading pathogens. Lysozyme : is an example of an antimicrobial peptide that dissolves some bacterial cell walls in skin. Another major peptide of innate host defense with antimicrobial properties is defensin. Defensins are positively charged peptides located primarily in the GI and lower respiratory tracts that create holes in bacterial cell walls and hence disrupt the bacterial membrane. 2 -Nasal hair &Mucus : The mucosal epithelium of the upper respiratory tract offers produce a complex mixture of mucins, proteases, against microorganism. Mucociliary found in mucous memberan of lower respiratory tract. Some bacteria attach to the surface epithelial cells by means of adhesive bacterial surface proteins (eg. pili ), mucus limits bacterial adhesion to these cell surfaces and entrapped it , then bacteria are removed by ciliary clearance.
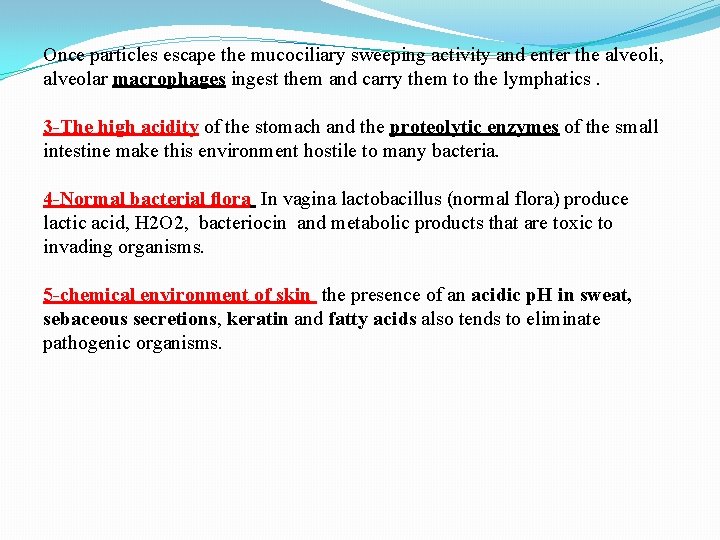
Once particles escape the mucociliary sweeping activity and enter the alveoli, alveolar macrophages ingest them and carry them to the lymphatics. 3 -The high acidity of the stomach and the proteolytic enzymes of the small intestine make this environment hostile to many bacteria. 4 -Normal bacterial flora In vagina lactobacillus (normal flora) produce lactic acid, H 2 O 2, bacteriocin and metabolic products that are toxic to invading organisms. 5 -chemical environment of skin the presence of an acidic p. H in sweat, sebaceous secretions, keratin and fatty acids also tends to eliminate pathogenic organisms.
Mechanisms of Innate Immunity When the pathogen penetrate the body by wound or burn , the innate system has both 1 -cells (neutrophils or called PMNCs, and macrophages along with NK cells) and 2 -proteins complement and numerous cytokines. . Many of these cytokines are proinflammatory molecules such as: üInterleukin-1 (IL-1) üTumor necrosis factor-alpha (TNF-α) üInterleukin-6 (IL-6) üInterferons, and are induced through Toll-like receptors (TLR ) interactions. Interferons: is protein realase in innate response by lymphocytes against virus infection and cancer lead to elevate the fever. Mechanisms steps : A. Microbial Sensors When a pathogen enters the skin , it is confronted by macrophages and other phagocytic cells possessing “microbial sensors. ” There are three major groups of microbial sensors: (1) Toll-like receptors (TLRs) (2) NOD-like receptors (NLRs) (3) RIG-1–like helicases
TLRs are type 1 transmembrane proteins with an extracellular domain, and a cytoplasmic domain. TLR recognition of these specific microbial patterns leads to a rapid and strong inflammatory response marked by cellular activation and cytokine release. B. Cellular Components and Phagocytosis Any antigen (microorganism) that enters the body through the lymphatics, lung, or blood stream is engulfed by phagocytic cells. Øeffective innate immunity are responses that are rapid, nonspecific, and of short duration. ØDuring infection, circulating phagocytic cells increase and can participate in chemotaxis migration ingestion and microbial killing. Øphagocytic cells include (1) monocytes and macrophages; (2) granulocytes including neutrophils, eosinophils, and basophils; and (3) dendritic cells. Dendritic cells are also phagocytic and can degrade pathogens; however, their main role is to activate T cells in the adaptive immune response by acting as APCs and by producing regulatory cytokines (eg, IFN-α).
Phagocytosis steps is a multistep process whereby a phagocytic cell, like a neutrophil, recognizes the pathogen, ingests it, and then destroys the engulfed organism. Once a pathogen enters the blood or tissue, the phagocytic cell migrates to that site. This migration is dependent on the release of chemo attractant signals produced by either the cells of the host or the pathogen. chemo attractant are IL-8 & IL-17 that attracts neutrophils which attach to the endothelial cell surface, the site of infection. neutrophil recognizes, engulfs, and digestion the pathogen into an endocytic vesicle called a phagosome then killed. When the neutrophil completes its mission, it undergoes apoptosis and dies
There are several antimicrobial mechanisms used by phagocytes to remove the pathogen: (1) Acidifcation occurs within the phagosome. The phagosome p. H is 3. 5– 4. 0, and this level of acidity is bacteriostatic or bactericidal. (2) Toxic oxygen-derived products are generated and include superoxide O 2 -, hydrogen peroxide H 2 O 2. (3) Toxic nitrogen oxides are also produced , and nitric oxide NO is formed. (4) Phagocytic cells generate antimicrobial peptides (enzymes)that participate in pathogen killing. The innate immune response is effective and eliminating most pathogens. If this initial mechanism fails, the adaptive immune response is induced. Thus both systems interact and collaborate to achieve the final goal of destroying the pathogen.
Adaptive Immunity The second line of defense, It is specific for the pathogen and confers protective immunity to reinfection with that pathogen. Adaptive immunity can specifically recognize and destroy the pathogen because lymphocytes carry specialized cellular receptors and produce specific antibodies. adaptive immunity is : ØHighly specific Øhas immunologic memory cells , Development of immunological memory, in which pathogens are "remembered" through memory B cells and memory T cells Øtake many days to induce to the first antigen exposure Øcan respond rapidly to a second antigen exposure ØThe adaptive immune response involves: antibody-mediated and cell mediated immune responses.
1 -Cell mediated immunity response Cell differentiated Lymphoid cells play a significant role in the adaptive immune response. During embryonic development, blood cell precursors (hematopoietic stem cells) originate in the fetal liver and other tissues; in postnatal life, the stem cells reside in the bone marrow. Stem cells may differentiate into cells of the myeloid or lymphoid series. The lymphoid progenitor cells develop into two main lymphocyte populations: B cells and T cells. B cells differentiation Stem cells destined to become B lymphocytes develop in the bone marrow. They rearrange their immunoglobulin genes and express a unique receptor for antigen on their cell surface. Following this step, they migrate to a secondary lymphoid organ (eg, the spleen) and may be activated by an encounter with antigen to become antibody-secreting plasma cells. B cells Plasma cells Some of the plasma cells Antibodies memory B cells
T cells differentiation T cells are lymphocytes that are produced in the bone marrow but travel to the thymus to mature. Once T cell receptors ( TCR) rearrangement has occurred and positive and negative selection has terminated, these cells form T cell subclasses with specific functions 1 -CD 4 T cells, also called helper cells (Th) 2 -CD 8 T cells, called Cytotoxic T L ymphocyte (CTL) 3 -Regulatory (suppressor T cells) , Regulatory T cells (T reg cells) are crucial for the maintenance of immunological tolerance. Their major role is to shut down T cell-mediated immunity and to suppress autoreactive T cells. Helper T cells express T cell receptors (TCR) that recognize antigen (toxin or microbial pathogen) bound to Class II MHC molecules. It include many subtyps : including Th 1, Th 2 , Th 3. Th 17. Th 9 4 -Memory T cells : Like cytotoxic T cells, most of the CD 4+ helper cells die on resolution of infection, with a few remaining as CD 4+ memory cells.
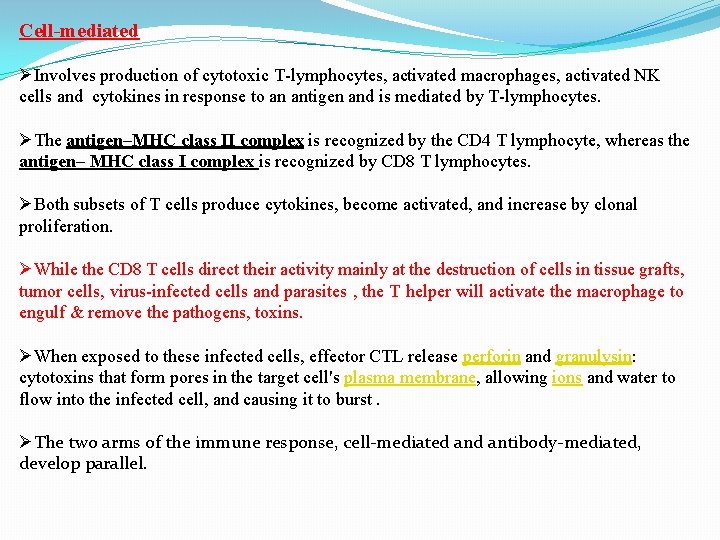
Cell-mediated ØInvolves production of cytotoxic T-lymphocytes, activated macrophages, activated NK cells and cytokines in response to an antigen and is mediated by T-lymphocytes. ØThe antigen–MHC class II complex is recognized by the CD 4 T lymphocyte, whereas the antigen– MHC class I complex is recognized by CD 8 T lymphocytes. ØBoth subsets of T cells produce cytokines, become activated, and increase by clonal proliferation. ØWhile the CD 8 T cells direct their activity mainly at the destruction of cells in tissue grafts, tumor cells, virus-infected cells and parasites , the T helper will activate the macrophage to engulf & remove the pathogens, toxins. ØWhen exposed to these infected cells, effector CTL release perforin and granulysin: cytotoxins that form pores in the target cell's plasma membrane, allowing ions and water to flow into the infected cell, and causing it to burst. ØThe two arms of the immune response, cell-mediated antibody-mediated, develop parallel.
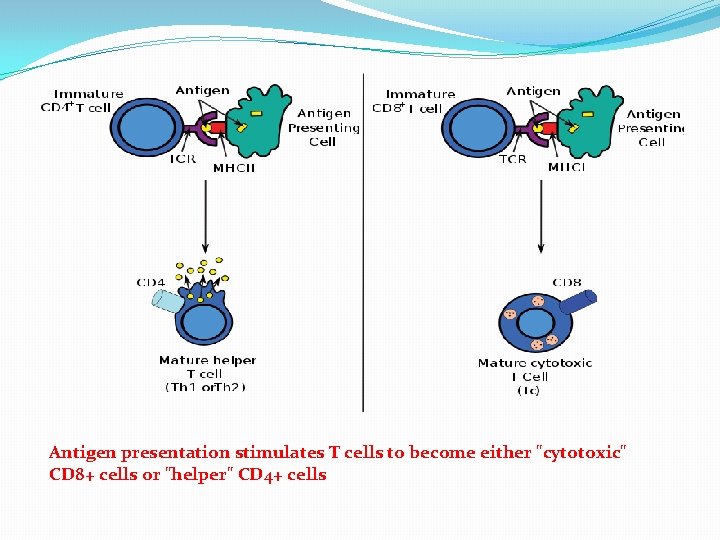
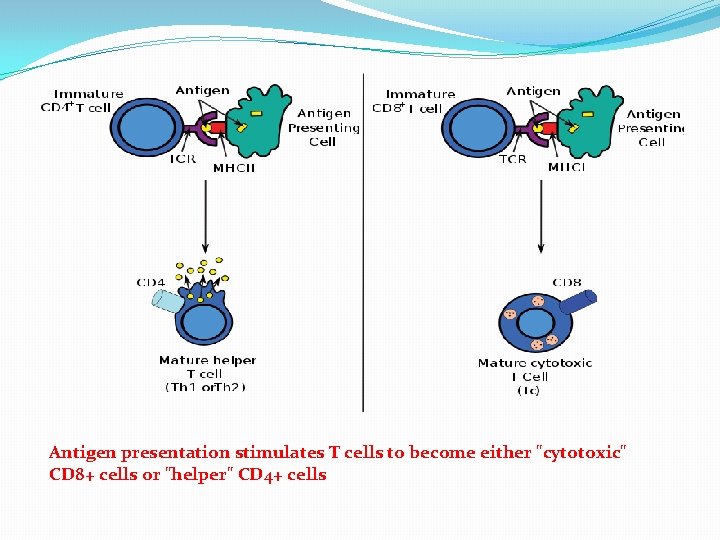
Antigen presentation stimulates T cells to become either "cytotoxic" CD 8+ cells or "helper" CD 4+ cells
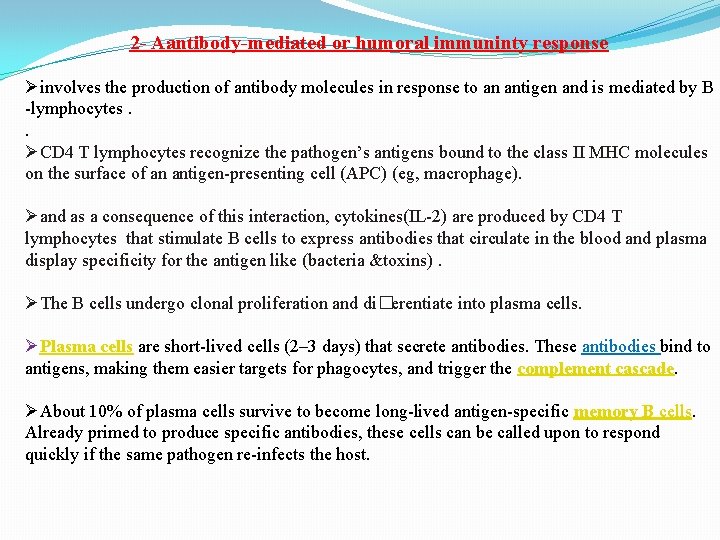
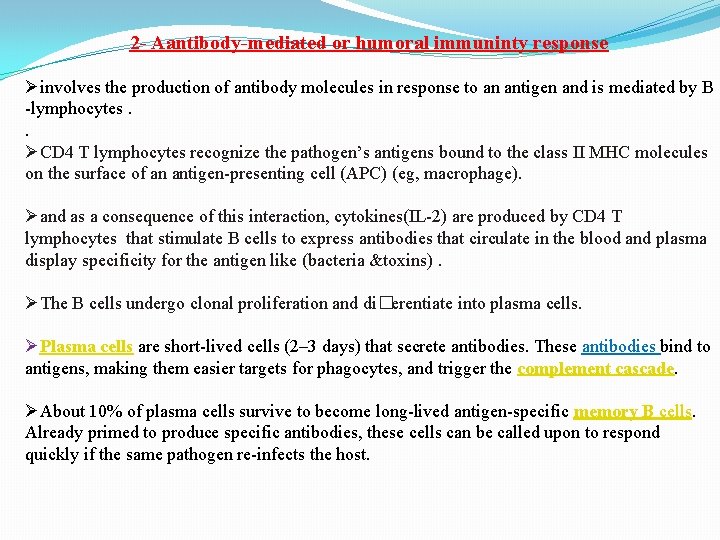
2 - Aantibody-mediated or humoral immuninty response Øinvolves the production of antibody molecules in response to an antigen and is mediated by B -lymphocytes. . ØCD 4 T lymphocytes recognize the pathogen’s antigens bound to the class II MHC molecules on the surface of an antigen-presenting cell (APC) (eg, macrophage). Øand as a consequence of this interaction, cytokines(IL-2) are produced by CD 4 T lymphocytes that stimulate B cells to express antibodies that circulate in the blood and plasma display specificity for the antigen like (bacteria &toxins). ØThe B cells undergo clonal proliferation and di�erentiate into plasma cells. ØPlasma cells are short-lived cells (2– 3 days) that secrete antibodies. These antibodies bind to antigens, making them easier targets for phagocytes, and trigger the complement cascade. ØAbout 10% of plasma cells survive to become long-lived antigen-specific memory B cells. Already primed to produce specific antibodies, these cells can be called upon to respond quickly if the same pathogen re-infects the host.
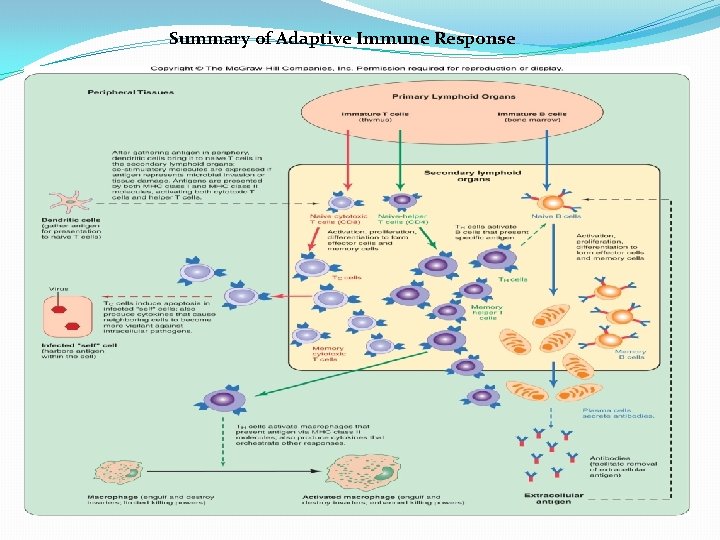
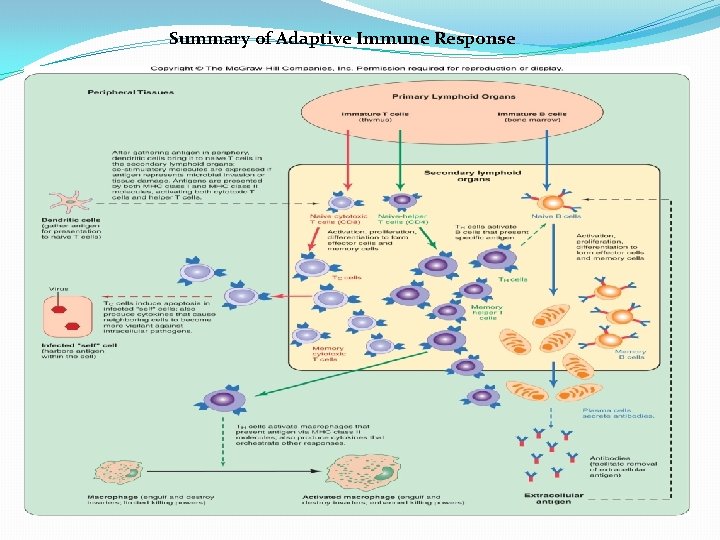
Summary of Adaptive Immune Response
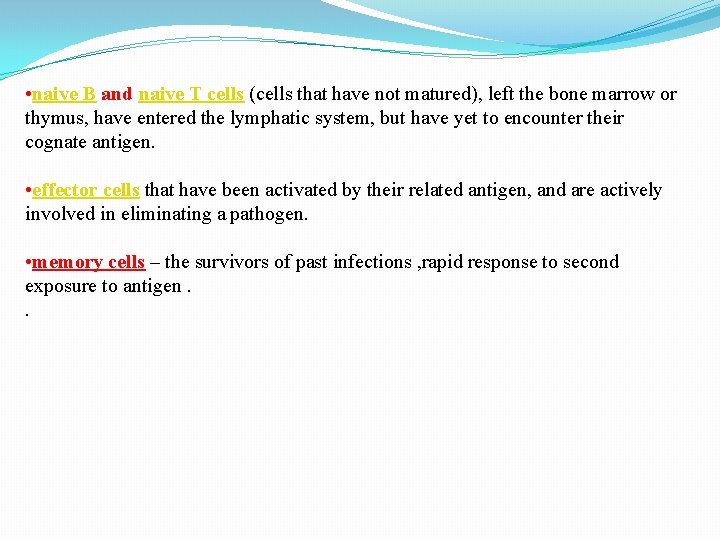
• naive B and naive T cells (cells that have not matured), left the bone marrow or thymus, have entered the lymphatic system, but have yet to encounter their cognate antigen. • effector cells that have been activated by their related antigen, and are actively involved in eliminating a pathogen. • memory cells – the survivors of past infections , rapid response to second exposure to antigen. .
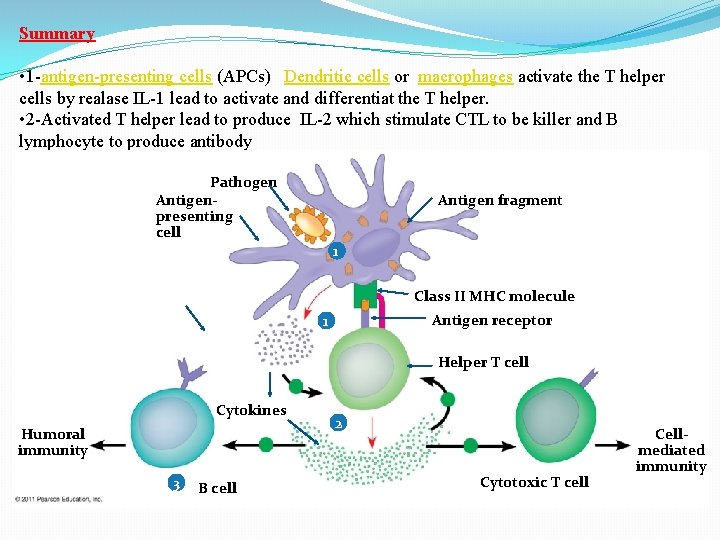
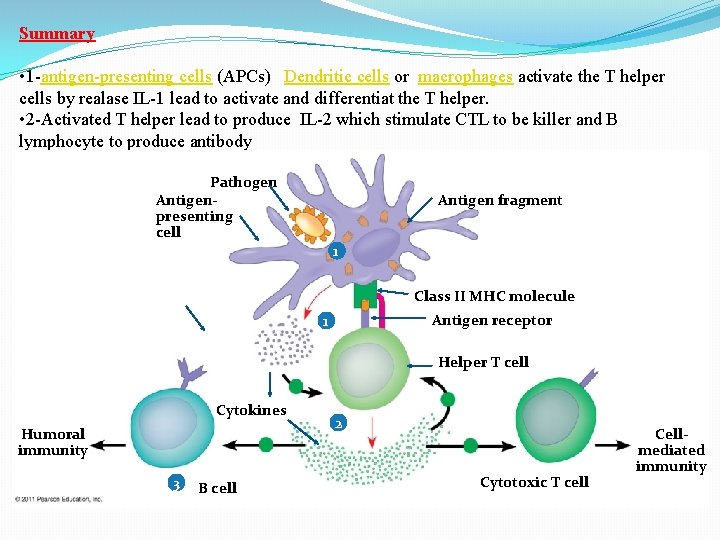
Summary • 1 -antigen-presenting cells (APCs) Dendritic cells or macrophages activate the T helper cells by realase IL-1 lead to activate and differentiat the T helper. • 2 -Activated T helper lead to produce IL-2 which stimulate CTL to be killer and B lymphocyte to produce antibody Pathogen Antigenpresenting cell Antigen fragment 1 Class II MHC molecule Antigen receptor 1 Helper T cell Cytokines Humoral immunity 3 B cell 2 Cytotoxic T cell Cellmediated immunity
THANK YOU