The Urinary System Chapter 18 Waste Products Chemical



- Slides: 69
The Urinary System Chapter 18
Waste Products • Chemical reactions in the body result in waste products that may be potentially harmful. • Must be eliminated from the body. • Examples of metabolic waste products: – Urea – Salts – Water
The Urinary System • Most important route of waste-product removal in the body. • Removes nearly all the soluble waste products from blood and transports out of the body. • Removes excess water from the body.
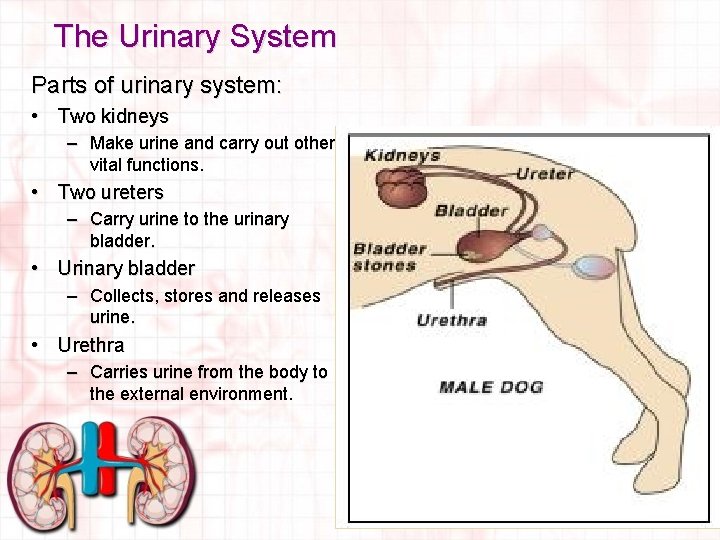
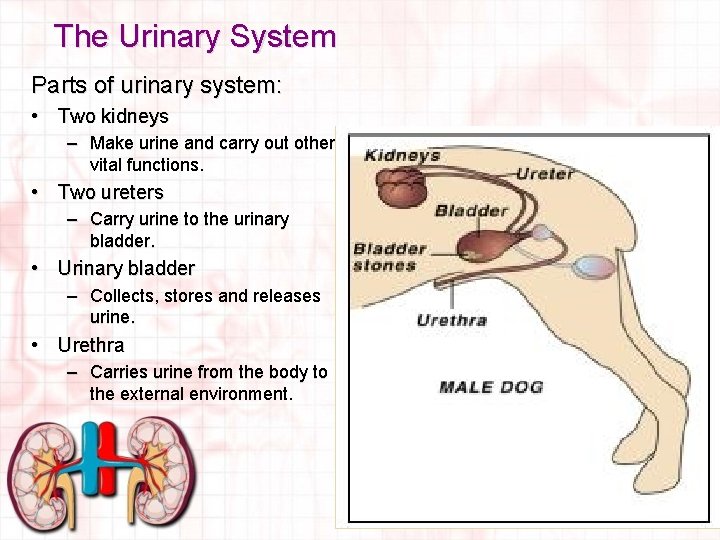
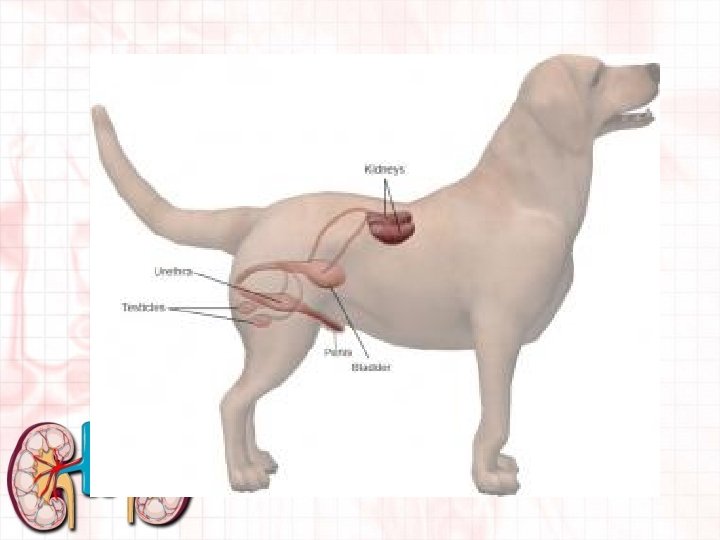
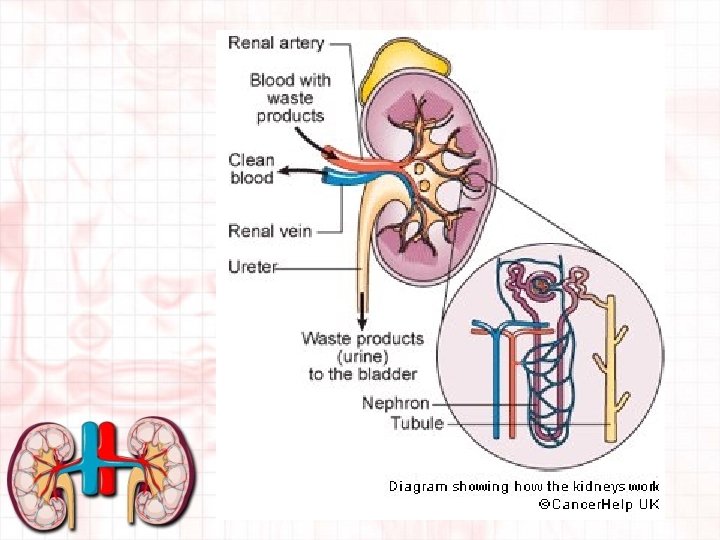
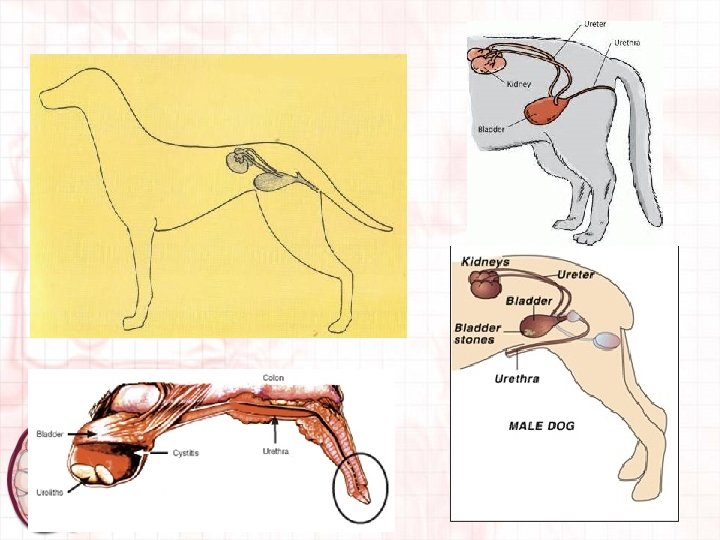
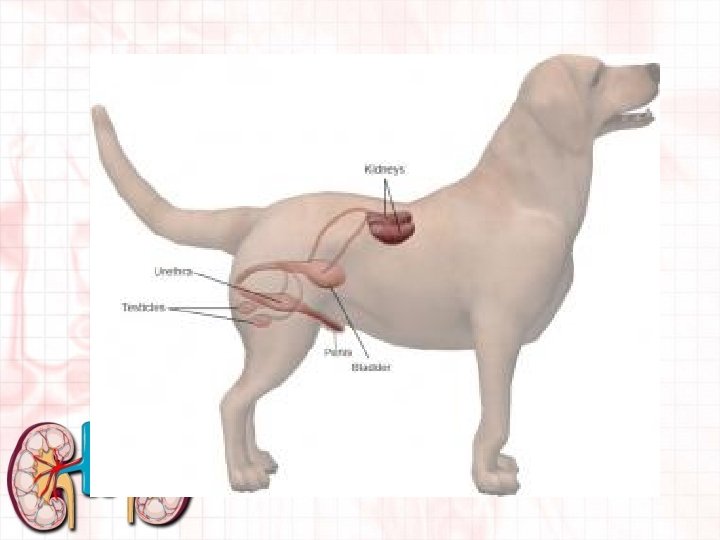
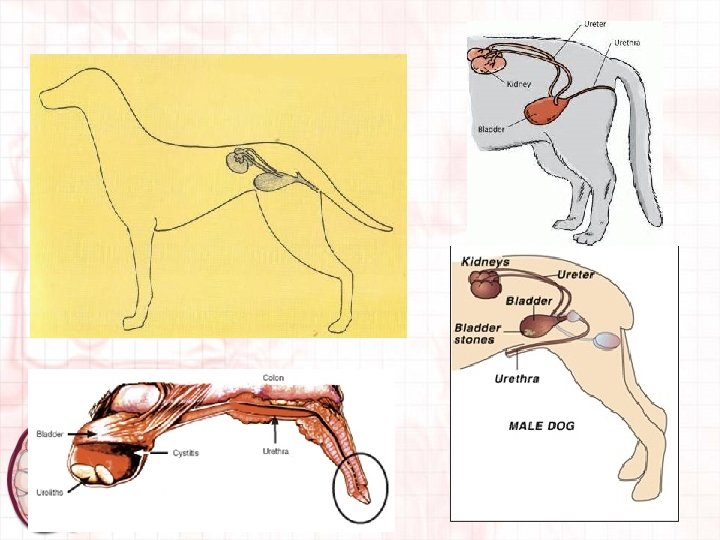
The Urinary System Parts of urinary system: • Two kidneys – Make urine and carry out other vital functions. • Two ureters – Carry urine to the urinary bladder. • Urinary bladder – Collects, stores and releases urine. • Urethra – Carries urine from the body to the external environment.
Terminology • • Nephrology- The study of the kidney. Diuresis- Body has excess formation of urine Oliguria- Little urine is formed and passed Anuria- No urine is formed or passed Dysuria- Difficult urination Hematuria- Blood in urine Polyuria- Increased urine volume. Antidiuretic Hormone (ADH)- (may also be referred to as Vasopressin) promotes water conservation by reabsorbing urine from collecting ducts. • Aldosterone-mineralcorticoid hormone secreted by cortex of adrenal gland. Stimulates kidney to conserve sodium ions and water and eliminate potassium and hydrogen ions.
Kidney Function • Must maintain homeostasis through a variety of processes. – Blood filtration, reabsorption, and secretion • Blood is filtered, useful substances are returned to circulation (reabsorption) and waste products are secreted. – Fluid balance regulation • Makes sure body has enough water to maintain healthy environment. – Acid-base regulation • Ability to remove hydrogen and bicarbonate ions from blood. – Hormone production • Produce and regulate hormones. – ADH from posterior pituitary gland. – Kidneys produce erythropoietin- necessary for red blood cell production and some prostaglandins – Aldosterone- secreted by adrenal glands
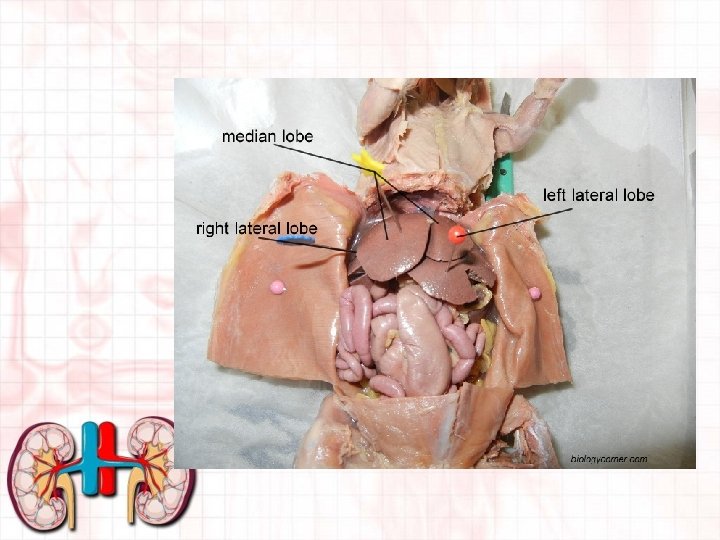
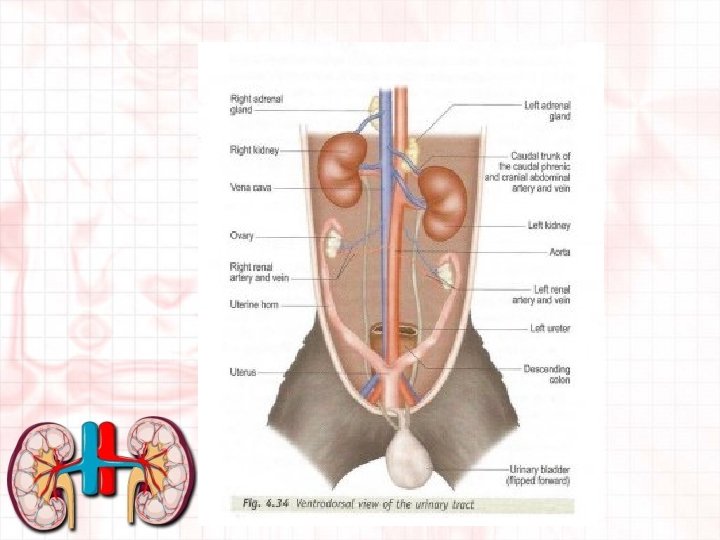
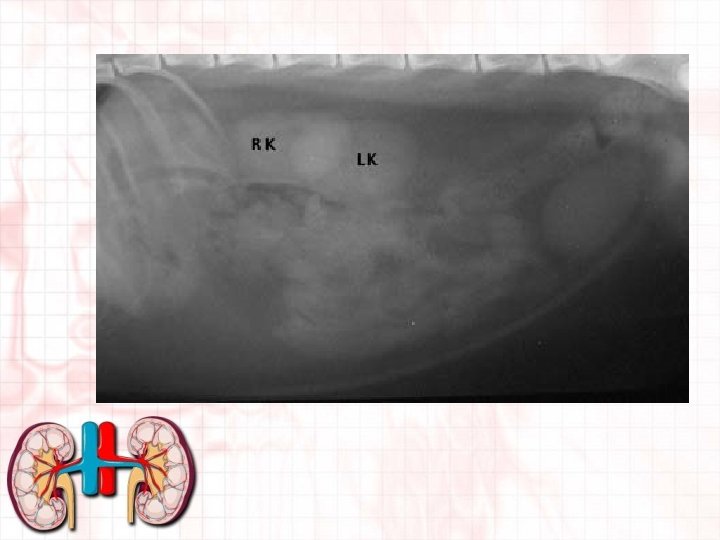
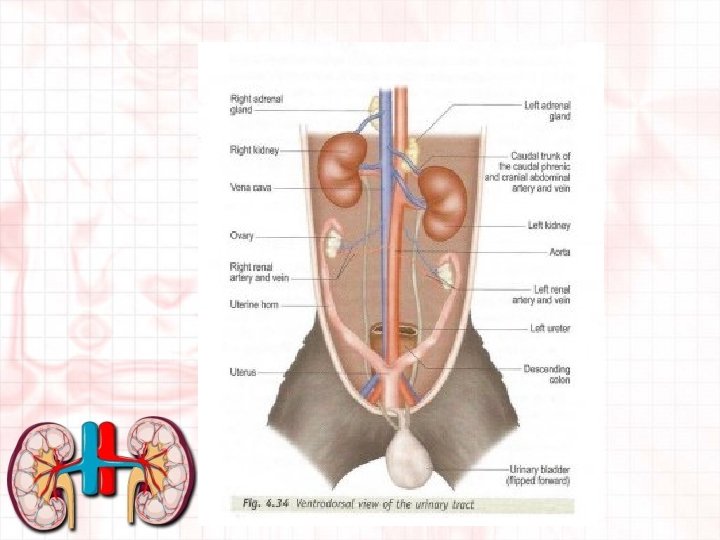
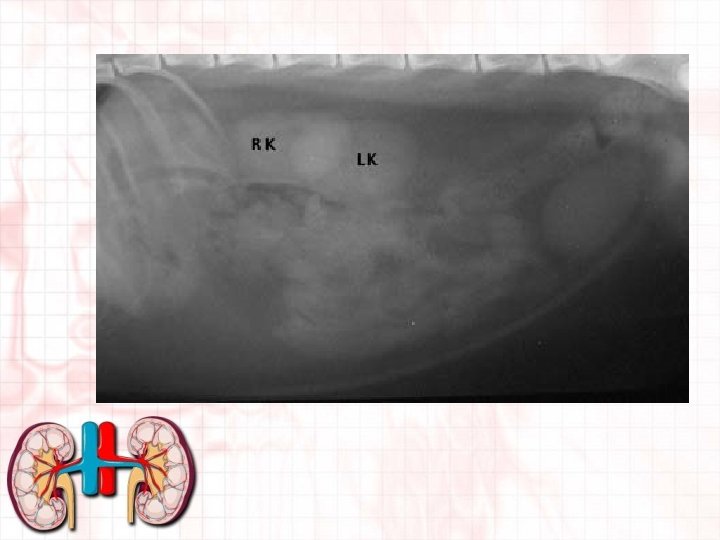
Location of the kidneys • In dorsal part of abdomen • Ventral to and on either side of first few lumbar vertebrae. • In most domestic animals, right kidney is slightly more cranial than left. • Perirenal fat surrounds and helps protect from exertion from other organs. • Are retroperitoneal to the abdominal cavity and so are considered outside abdominal cavity. • Move somewhat with the movement of the diaphragm • Position may vary with species.
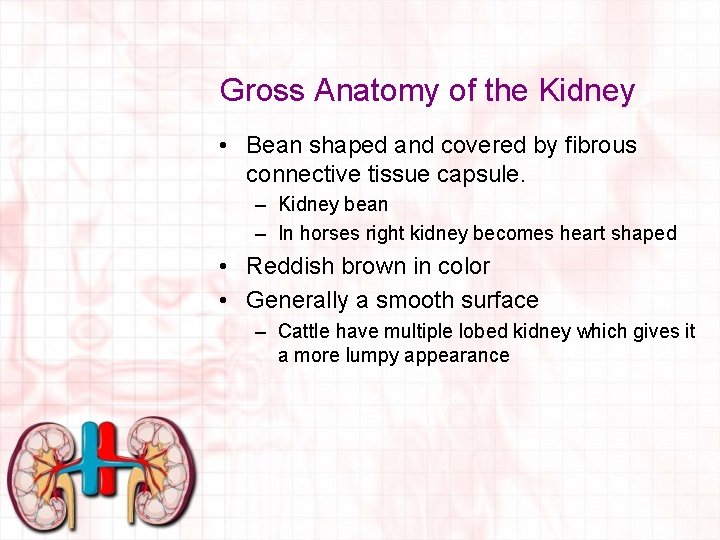
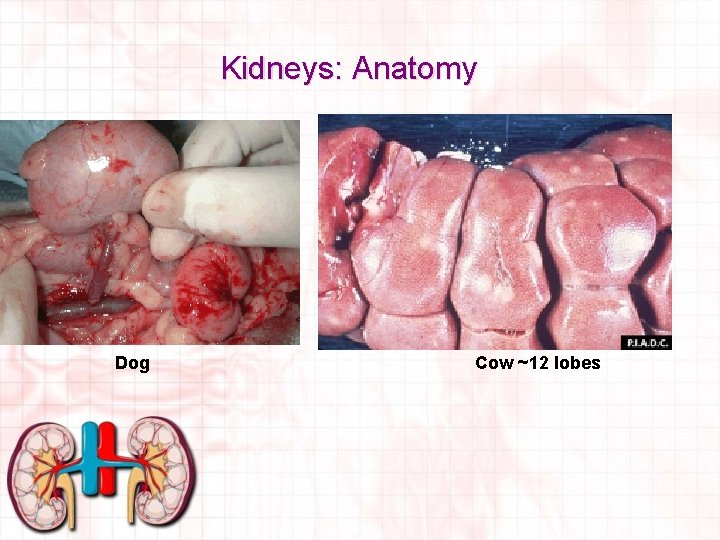
Gross Anatomy of the Kidney • Bean shaped and covered by fibrous connective tissue capsule. – Kidney bean – In horses right kidney becomes heart shaped • Reddish brown in color • Generally a smooth surface – Cattle have multiple lobed kidney which gives it a more lumpy appearance
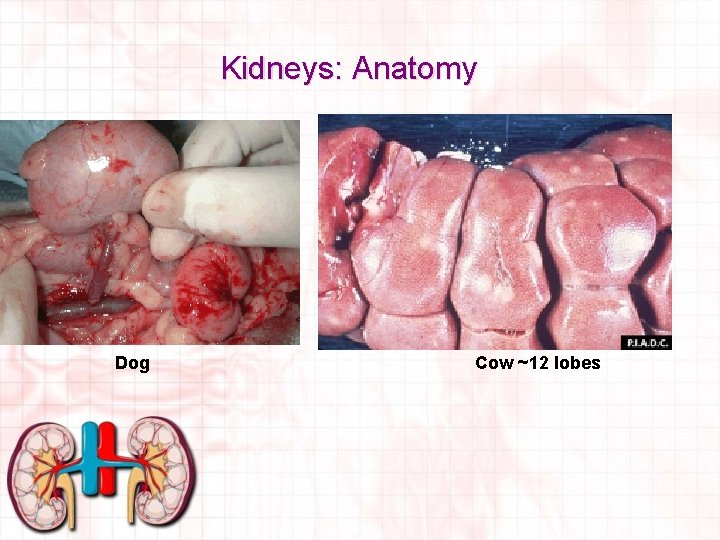
Kidneys: Anatomy Dog Cow ~12 lobes
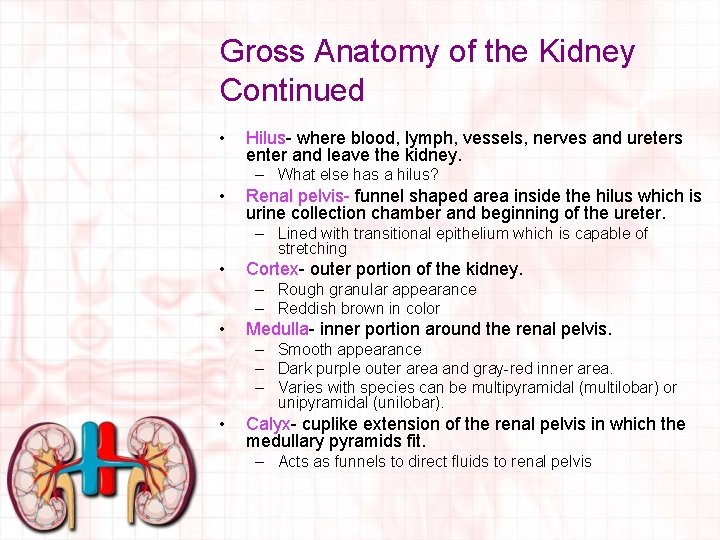
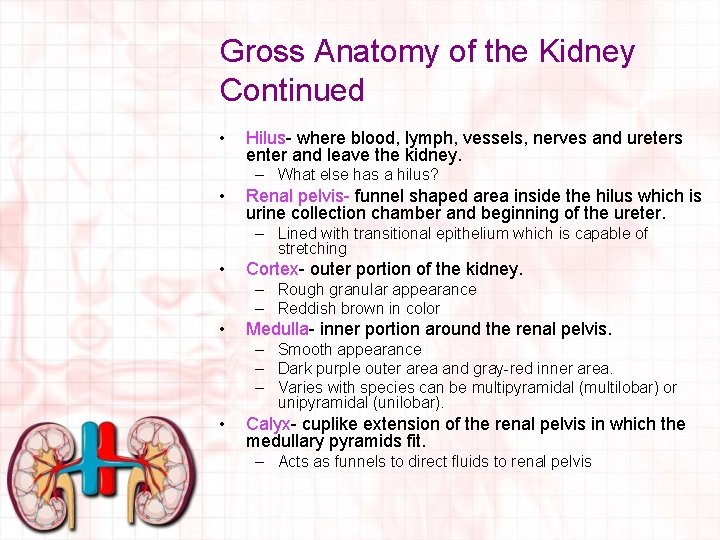
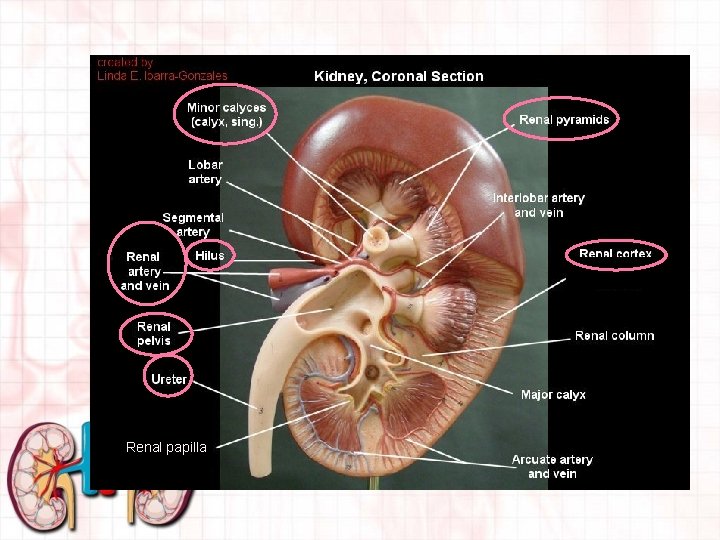
Gross Anatomy of the Kidney Continued • Hilus- where blood, lymph, vessels, nerves and ureters enter and leave the kidney. – What else has a hilus? • Renal pelvis- funnel shaped area inside the hilus which is urine collection chamber and beginning of the ureter. – Lined with transitional epithelium which is capable of stretching • Cortex- outer portion of the kidney. – Rough granular appearance – Reddish brown in color • Medulla- inner portion around the renal pelvis. – Smooth appearance – Dark purple outer area and gray-red inner area. – Varies with species can be multipyramidal (multilobar) or unipyramidal (unilobar). • Calyx- cuplike extension of the renal pelvis in which the medullary pyramids fit. – Acts as funnels to direct fluids to renal pelvis
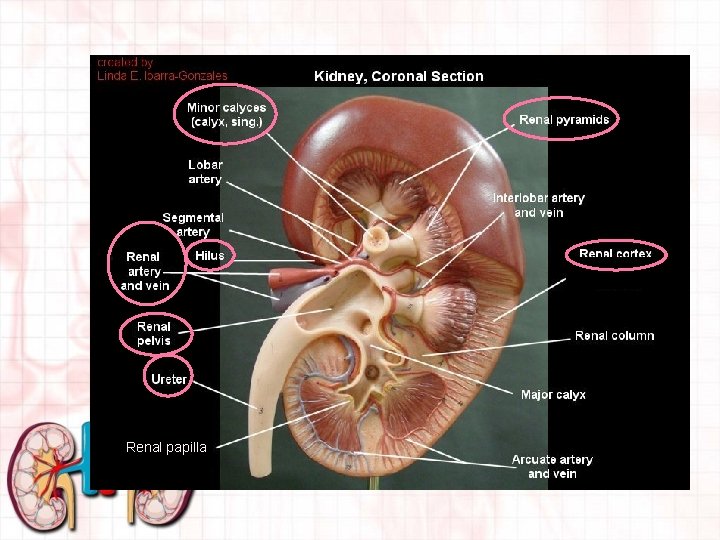
Renal papilla
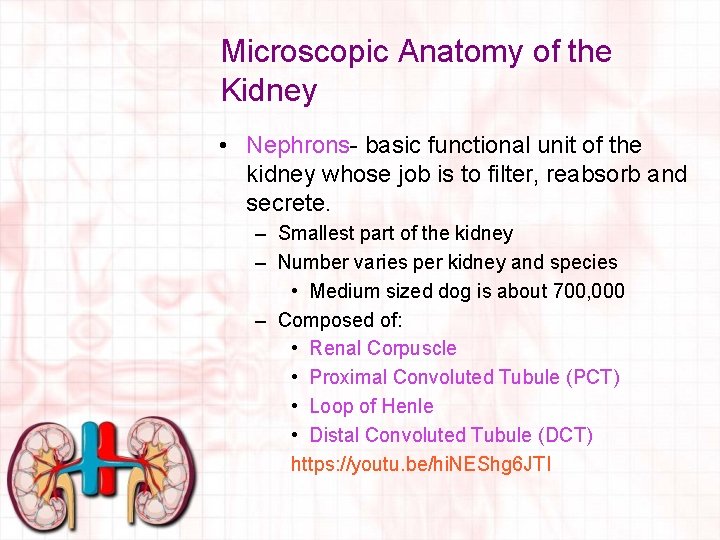
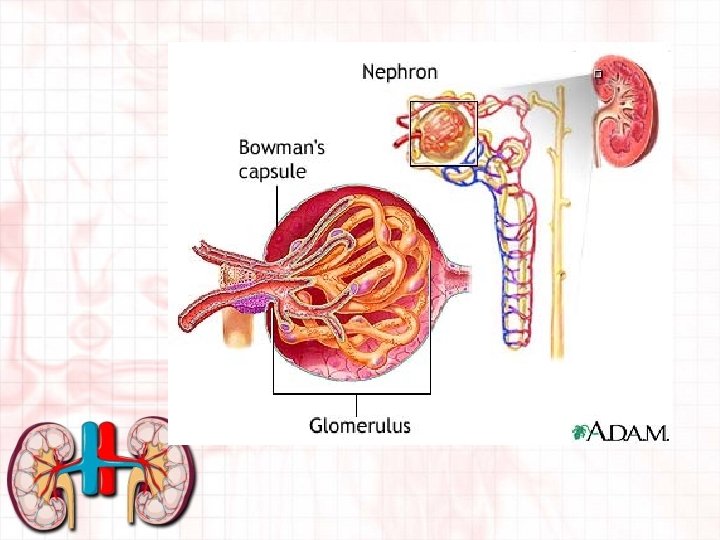
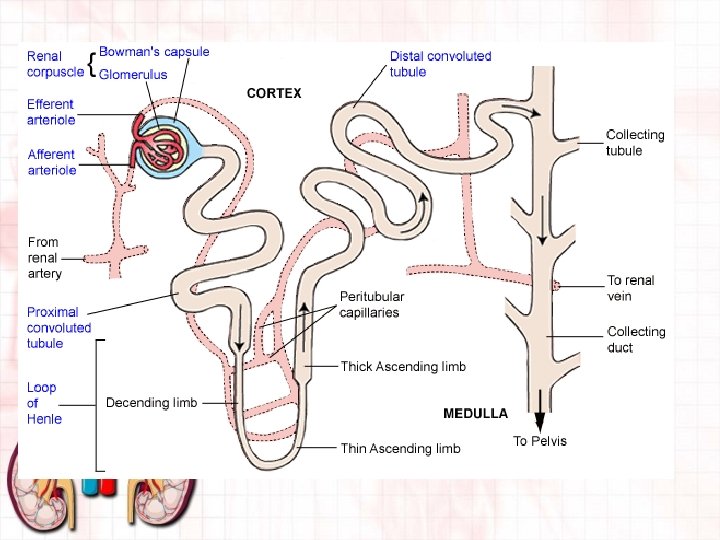
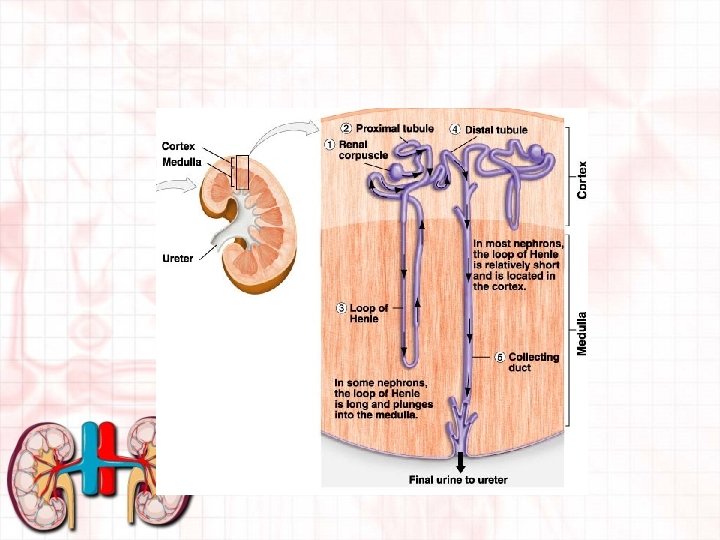
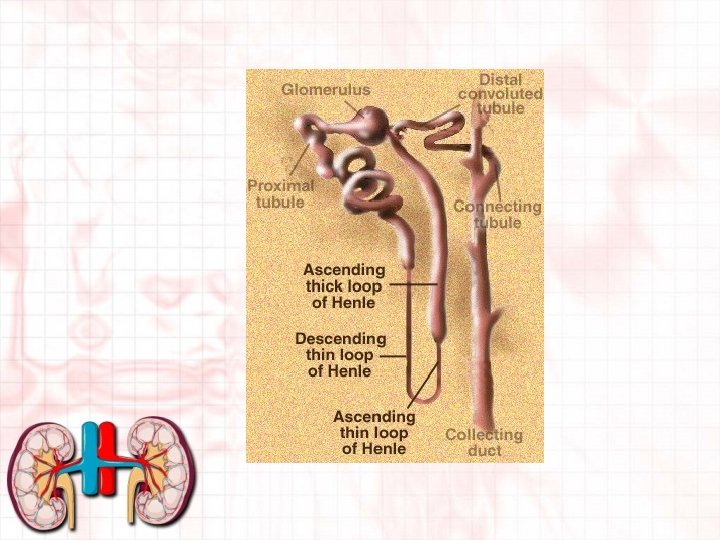
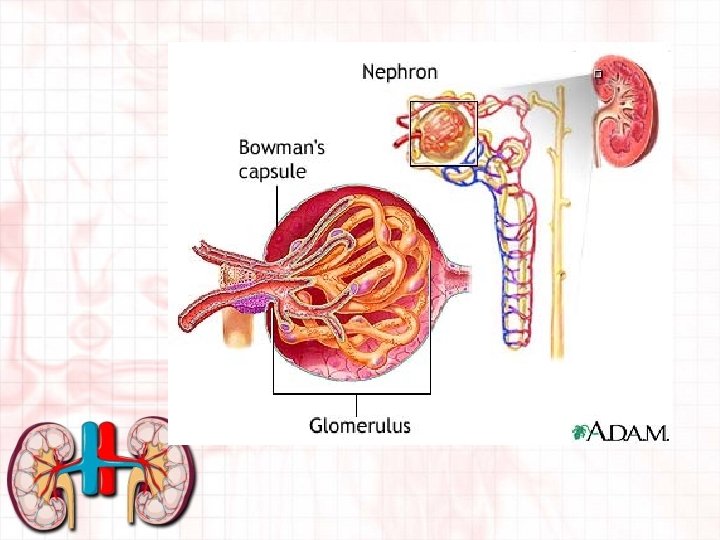
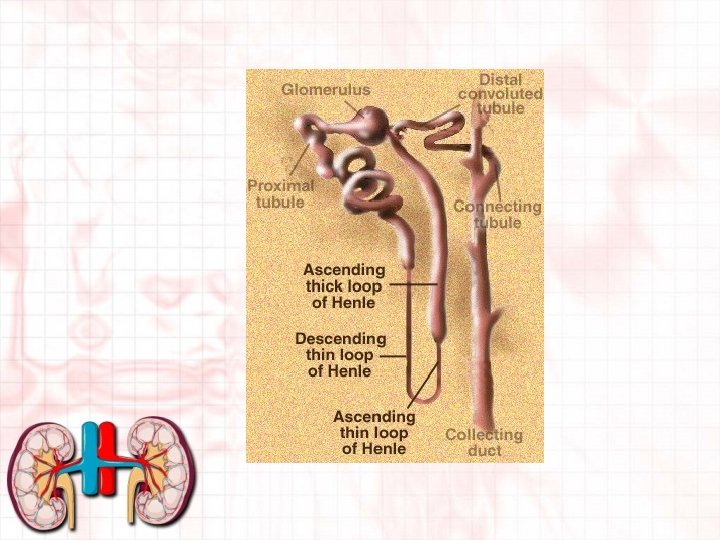
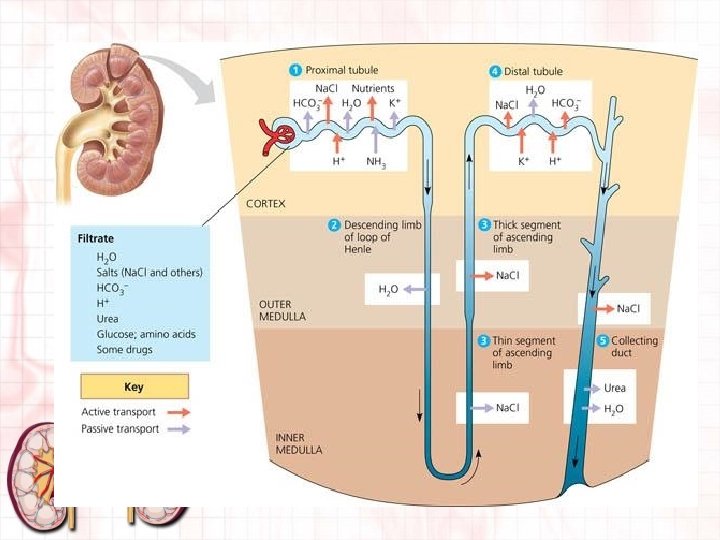
Microscopic Anatomy of the Kidney • Nephrons- basic functional unit of the kidney whose job is to filter, reabsorb and secrete. – Smallest part of the kidney – Number varies per kidney and species • Medium sized dog is about 700, 000 – Composed of: • Renal Corpuscle • Proximal Convoluted Tubule (PCT) • Loop of Henle • Distal Convoluted Tubule (DCT) https: //youtu. be/hi. NEShg 6 JTI
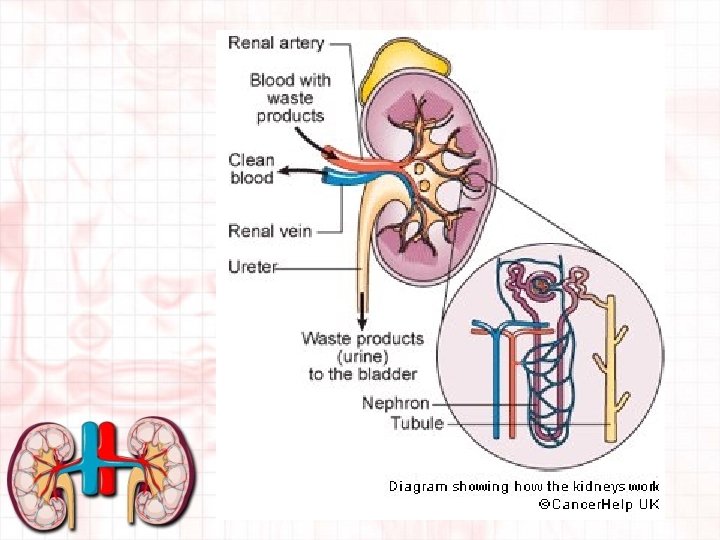
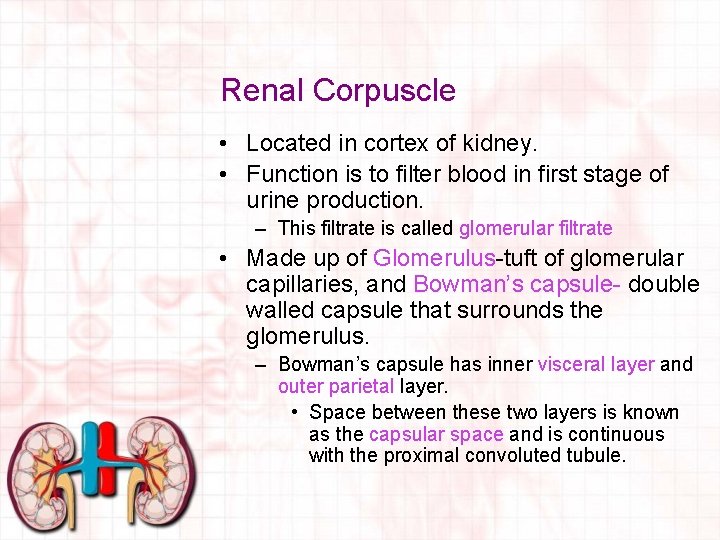
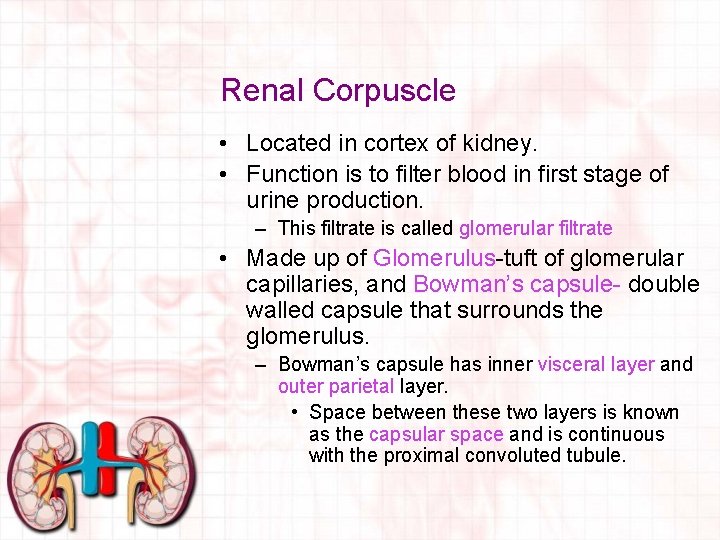
Renal Corpuscle • Located in cortex of kidney. • Function is to filter blood in first stage of urine production. – This filtrate is called glomerular filtrate • Made up of Glomerulus-tuft of glomerular capillaries, and Bowman’s capsule- double walled capsule that surrounds the glomerulus. – Bowman’s capsule has inner visceral layer and outer parietal layer. • Space between these two layers is known as the capsular space and is continuous with the proximal convoluted tubule.
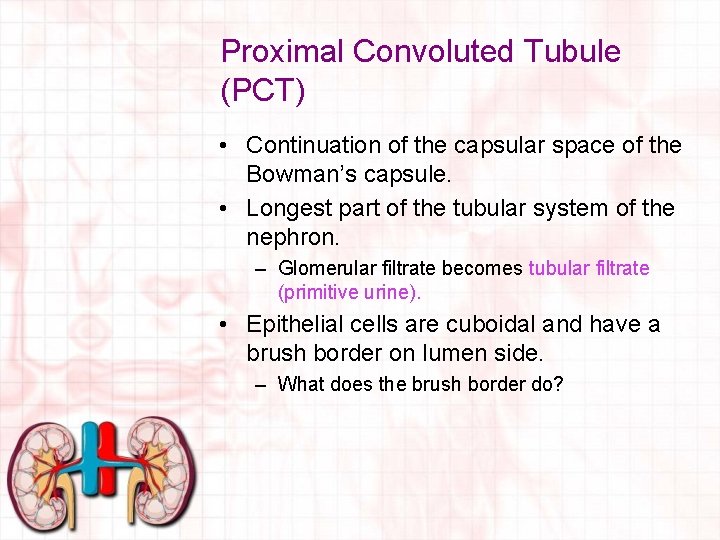
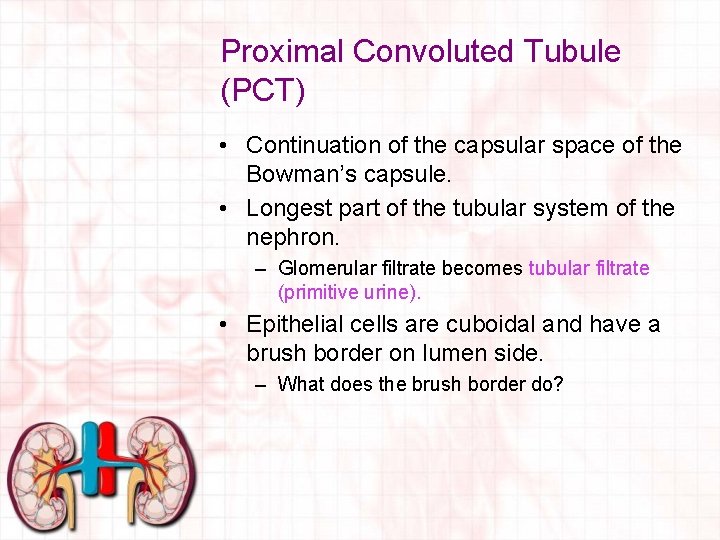
Proximal Convoluted Tubule (PCT) • Continuation of the capsular space of the Bowman’s capsule. • Longest part of the tubular system of the nephron. – Glomerular filtrate becomes tubular filtrate (primitive urine). • Epithelial cells are cuboidal and have a brush border on lumen side. – What does the brush border do?
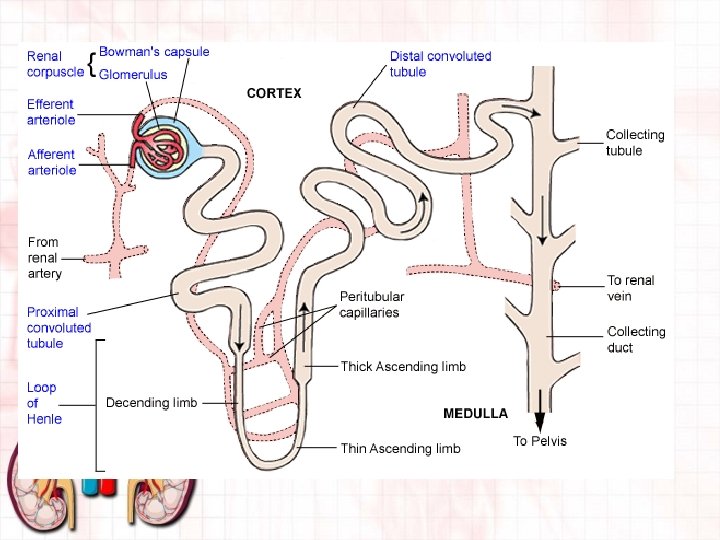
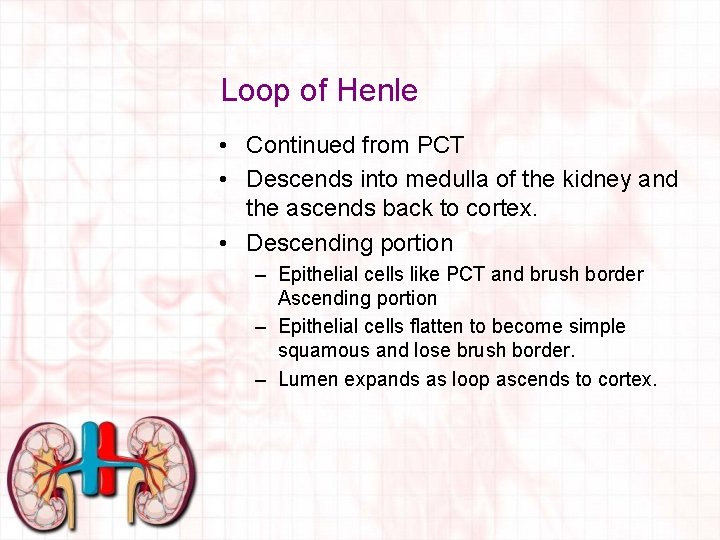
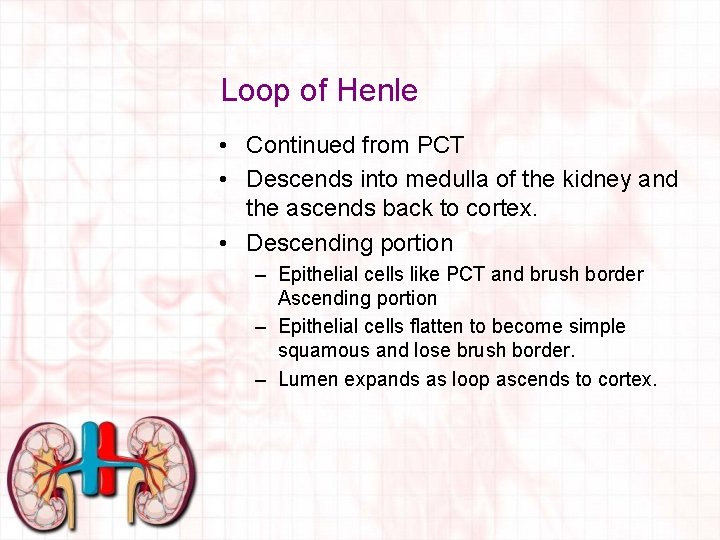
Loop of Henle • Continued from PCT • Descends into medulla of the kidney and the ascends back to cortex. • Descending portion – Epithelial cells like PCT and brush border Ascending portion – Epithelial cells flatten to become simple squamous and lose brush border. – Lumen expands as loop ascends to cortex.
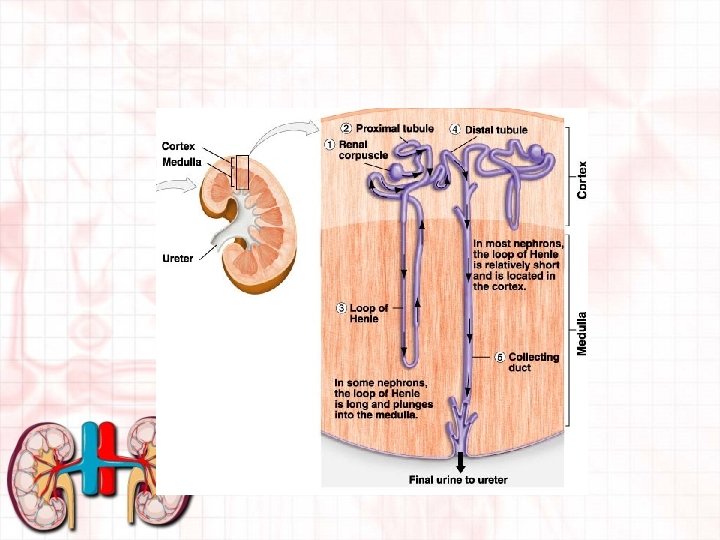
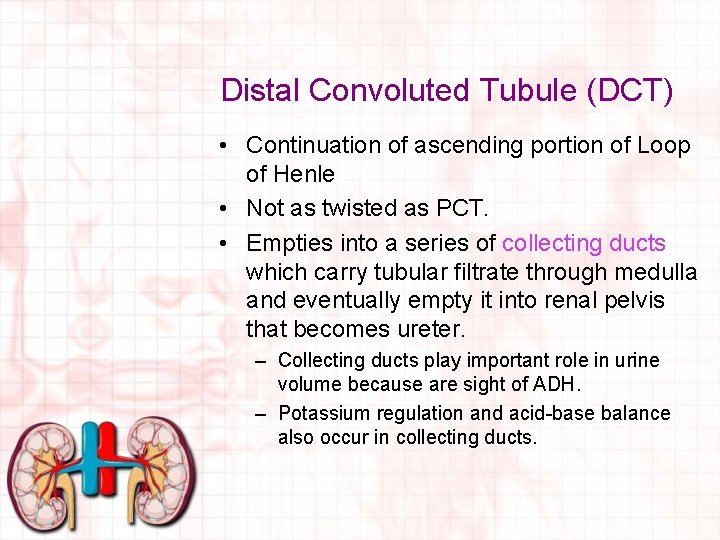
Distal Convoluted Tubule (DCT) • Continuation of ascending portion of Loop of Henle • Not as twisted as PCT. • Empties into a series of collecting ducts which carry tubular filtrate through medulla and eventually empty it into renal pelvis that becomes ureter. – Collecting ducts play important role in urine volume because are sight of ADH. – Potassium regulation and acid-base balance also occur in collecting ducts.
Nerve Supply to the Kidneys • Supplied by sympathetic portion of autonomic nervous system. • Is not essential for kidney function. – Why transplanted kidneys will work.
Blood Supply to the Kidneys • Kidneys have very large blood supply. • All circulating blood passes through kidney every 4 or 5 minutes. • Up to 25% of all blood that heart pumps goes to the kidneys. • Composed of: – – – Renal artery Afferent glomerular arterioles Glomerular capillaries Efferent Glomerular arterioles Peritubular capillaries Renal vein
Blood Supply Continued • Composed of: – Renal artery • Branches off of aorta and enters kidney at hilus • Divides smaller and smaller until becomes afferent glomerular arterioles – Afferent glomerular arterioles • Carry blood into the glomerular capillaries of the renal corpuscle. – Glomerular capillaries • Continuation of afferent glomerular arterioles. • Filter plasma from blood and in capsular space called glomerular filtrate. • Only place in body where capillary blood that enters and leaves capillaries is still oxygenated blood.
• Blood supply continued – Efferent Glomerular arterioles • Divide into capillaries that surround nephron- called peritubular capillaries – Peritubular capillaries • Surround nephron and converge to form venules then become renal vein. • Oxygen transfer occurs here. • Usable substances are removed from tubular filtrate and reabsorbed. • Other waste substances are secreted into filtrate here as well. – Renal vein • Leaves kidney at hilus and joins abdominal portion of the caudal vena cava. • Purest blood in body. – Why?
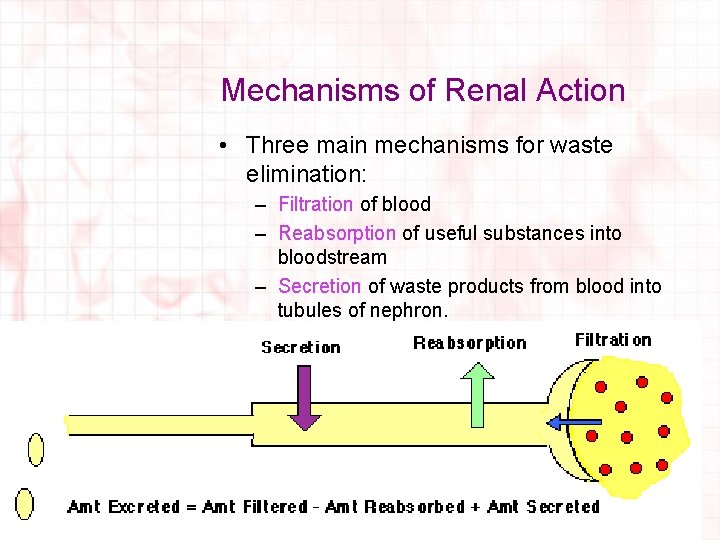
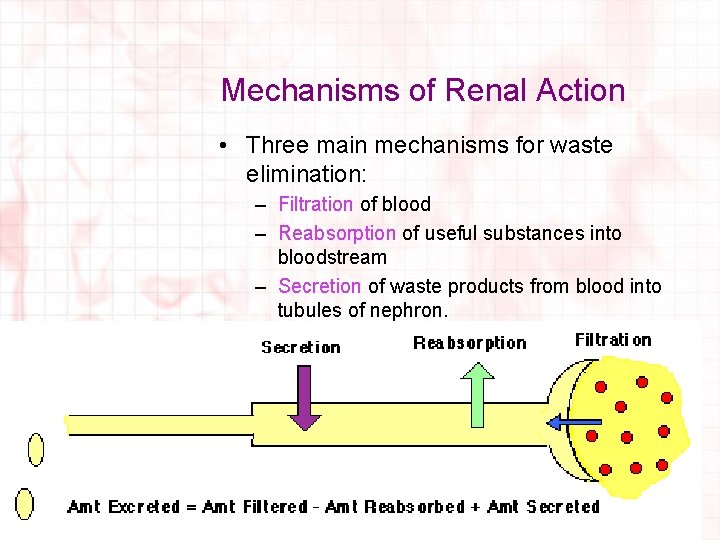
Mechanisms of Renal Action • Three main mechanisms for waste elimination: – Filtration of blood – Reabsorption of useful substances into bloodstream – Secretion of waste products from blood into tubules of nephron.
Terminology • Osmosis- passage of water from weaker to a stronger solution across a semi-permeable membrane. • Diffusion- passage of a substance from a high concentration to a low concentration. • Reabsorption-passage of a substance from the lumen of the renal tubules into the renal capillaries and so back into circulation; this is an active process and requires energy. • Secretion- passage of a chemical substance from the renal capillaries into the lumen of the tubules and out of the body in the urine; this is an active process and requires energy.
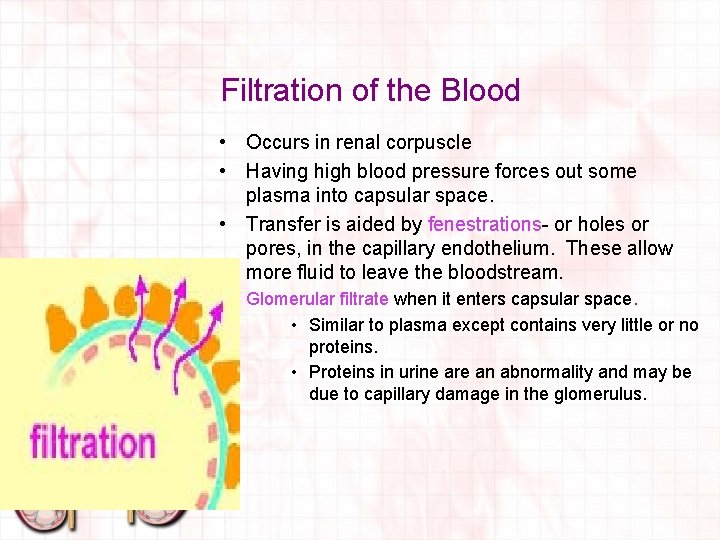
Filtration of the Blood • Occurs in renal corpuscle • Having high blood pressure forces out some plasma into capsular space. • Transfer is aided by fenestrations- or holes or pores, in the capillary endothelium. These allow more fluid to leave the bloodstream. • Glomerular filtrate when it enters capsular space. • Similar to plasma except contains very little or no proteins. • Proteins in urine are an abnormality and may be due to capillary damage in the glomerulus.
Filtration of the Blood • Glomerular Filtration Rate (GFR) – Describes how fast plasma is filtered as it passes through the glomerulus. – Depends on rate of blood flow to the kidneys – Expressed in m. L per minute – Not all that is filtered is produced as urine or would urinate constantly. – Reabsorption helps reduce volume of glomerular filtrate. – For every 100 L of fluid filtered from the blood only 1 L is produced as urine. – 99% of original filtrate is reabsorbed back into blood.
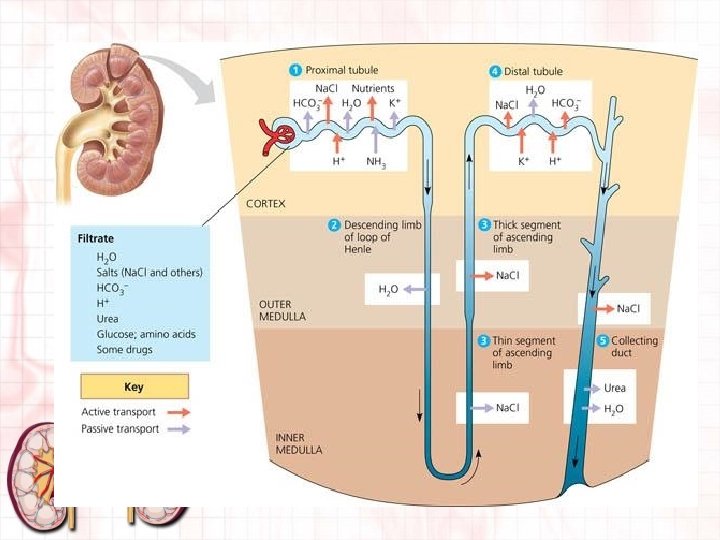
Reabsorption • Reabsorption takes useful substances from the tubules back into the blood. • Most takes place in the PCT but may also take place in Loop of Henle, DCT, and collecting ducts. • Glomerular filtrate is considered outside the body. • Contains waste products that must be cleared from the body as well as substances the body needs back into bloodstream. • Sodium, potassium, calcium, magnesium, glucose, amino acids, chloride, bicarbonate and water.
Reabsorption Continued • Glomerular filtrate enters PCT and becomes tubular filtrate. • In PCT some substances may be passively or actively transported. • Path must travel is: – – Out of tubular lumen Through tubular epithelium Into interstitial fluid Into peritubular capillaries.
Sodium Reabsorption • Attaches to a carrier protein that carries it into the cytoplasm of the PCT epithelial cell. • Requires energy. • Sodium ions are reabsorbed in peritubular capillaries in ascending loop of Henle and DCT. – In DCT, sodium is exchanged for hydrogen, potassium ions and ammonium. – This process is influenced by aldosterone. • Glucose and amino acids “hitch a ride” on this carrier protein so that no extra energy has to be expended. – They follow sodium into epithelial cells by process called sodium cotransport.
Sodium Reabsorption continued • When sodium is pumped out of epithelial cell, electrical imbalance occurs. – Chloride is diffused into cell to correct imbalance. • When some substances leave tubular filtrate, some water moves into peritubular capillaries by osmosis, other substances may be passively reabsorbed at this point. • Urea- a non protein source of nitrogen produced by the liver; is one of the substances that is not completely filtered. – Measured by Blood Urea Nitrogen (BUN) blood enzyme.
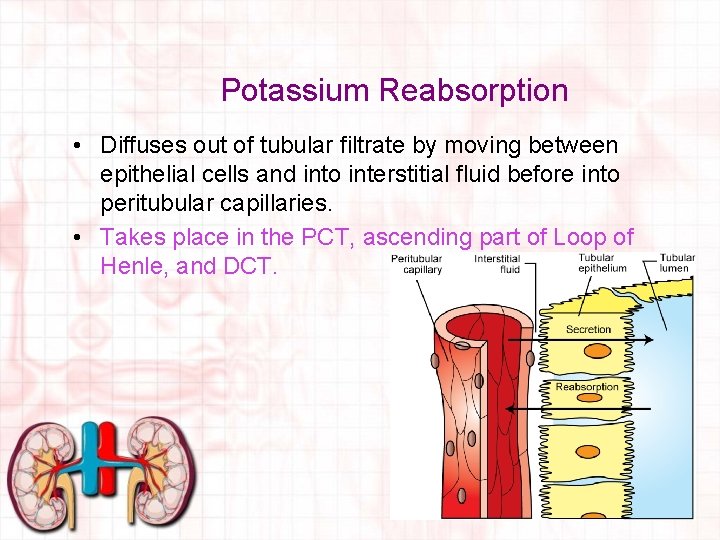
Potassium Reabsorption • Diffuses out of tubular filtrate by moving between epithelial cells and into interstitial fluid before into peritubular capillaries. • Takes place in the PCT, ascending part of Loop of Henle, and DCT.
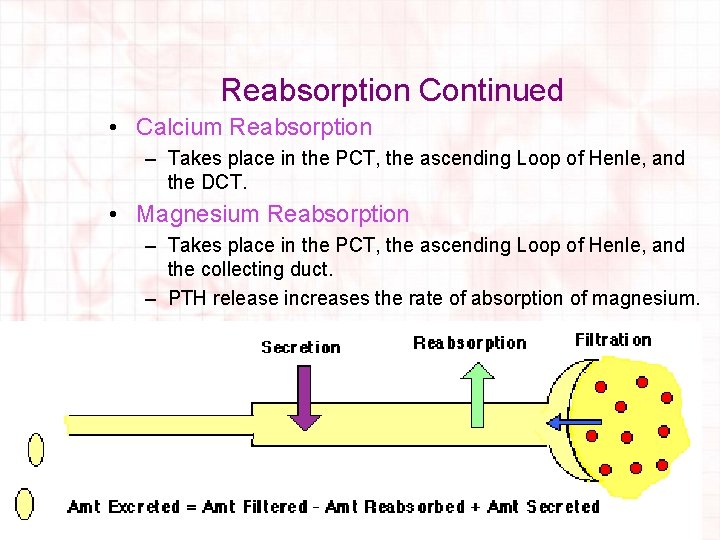
Reabsorption Continued • Calcium Reabsorption – Takes place in the PCT, the ascending Loop of Henle, and the DCT. • Magnesium Reabsorption – Takes place in the PCT, the ascending Loop of Henle, and the collecting duct. – PTH release increases the rate of absorption of magnesium.
Secretion • Whatever is not filtered is a true waste. product and must be eliminated from body. • These substances are transferred through system to tubular filtrate. This process is called tubular secretion. • Takes place in the DCT. • Eliminates Hydrogen, potassium, and ammonia. • Some drugs are eliminated this way as well. – When is this beneficial?
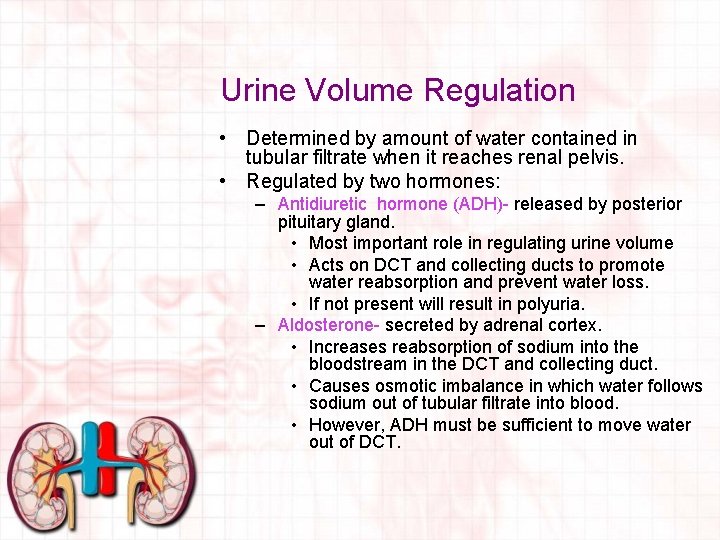
Urine Volume Regulation • Determined by amount of water contained in tubular filtrate when it reaches renal pelvis. • Regulated by two hormones: – Antidiuretic hormone (ADH)- released by posterior pituitary gland. • Most important role in regulating urine volume • Acts on DCT and collecting ducts to promote water reabsorption and prevent water loss. • If not present will result in polyuria. – Aldosterone- secreted by adrenal cortex. • Increases reabsorption of sodium into the bloodstream in the DCT and collecting duct. • Causes osmotic imbalance in which water follows sodium out of tubular filtrate into blood. • However, ADH must be sufficient to move water out of DCT.
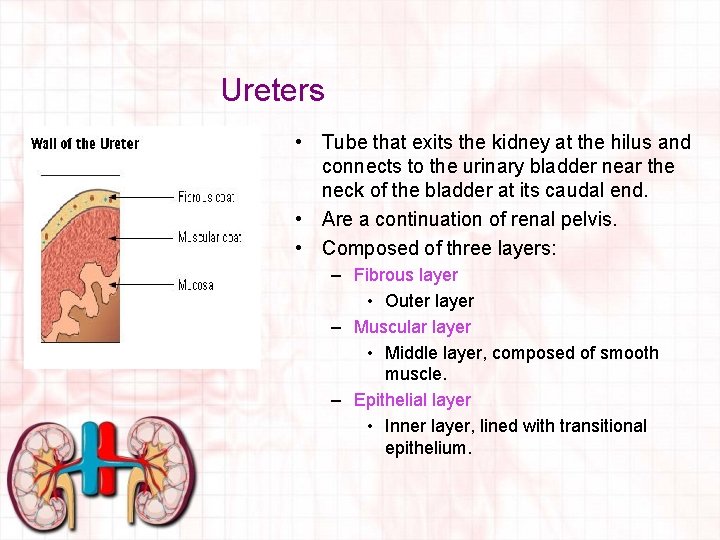
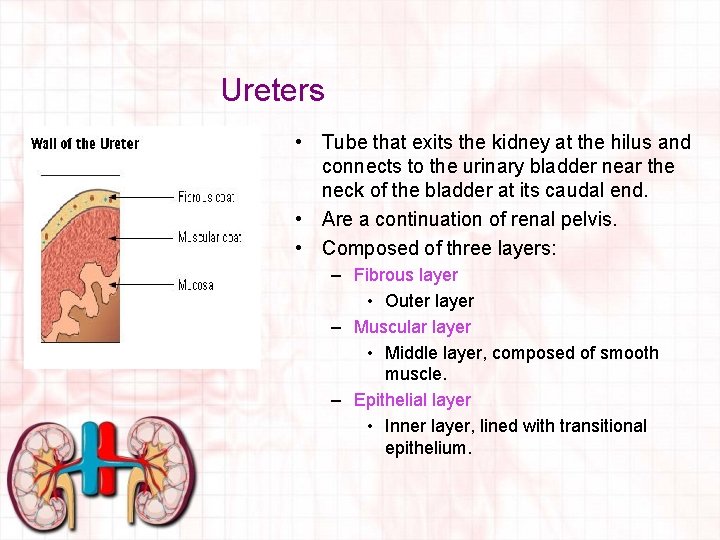
Ureters • Tube that exits the kidney at the hilus and connects to the urinary bladder near the neck of the bladder at its caudal end. • Are a continuation of renal pelvis. • Composed of three layers: – Fibrous layer • Outer layer – Muscular layer • Middle layer, composed of smooth muscle. – Epithelial layer • Inner layer, lined with transitional epithelium.
Function of the Ureters • Continuously move urine from the kidneys to the urinary bladder. • Smooth muscle propels urine through peristaltic contractions. – Enables urine to be moved regardless of position of animal’s body • Ureters enter bladder at oblique angle, so that when bladder is full it will collapse to prevent urine from backing up into ureters. – This will not keep ureters from pushing urine into bladder however.
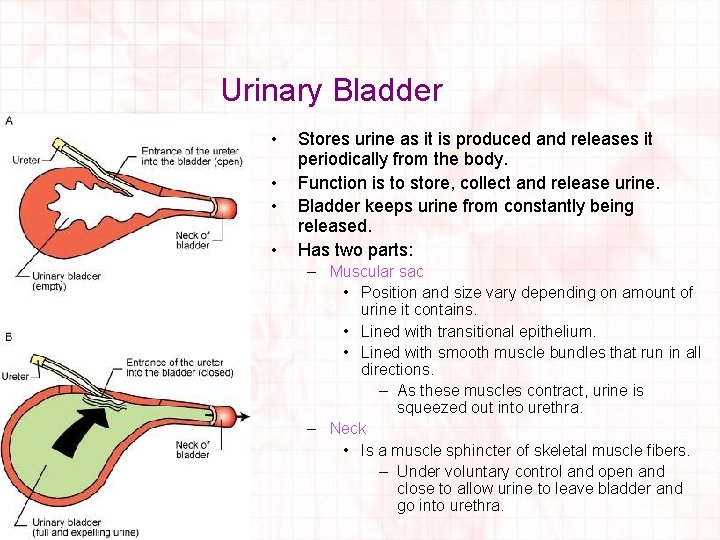
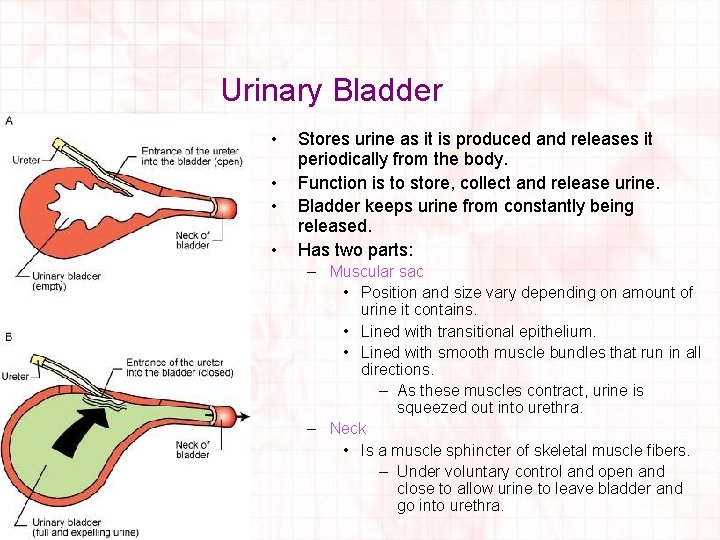
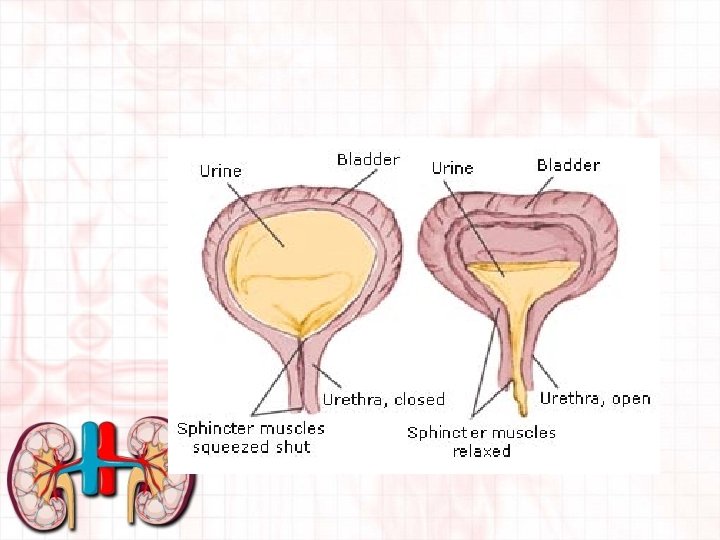
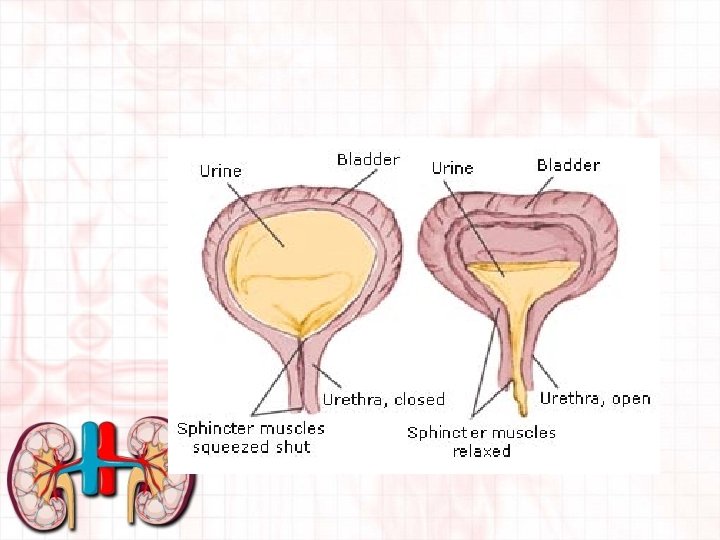
Urinary Bladder • • Stores urine as it is produced and releases it periodically from the body. Function is to store, collect and release urine. Bladder keeps urine from constantly being released. Has two parts: – Muscular sac • Position and size vary depending on amount of urine it contains. • Lined with transitional epithelium. • Lined with smooth muscle bundles that run in all directions. – As these muscles contract, urine is squeezed out into urethra. – Neck • Is a muscle sphincter of skeletal muscle fibers. – Under voluntary control and open and close to allow urine to leave bladder and go into urethra.
Urinary Bladder continued • Rests on pubic bones when empty. • Has thick wall lined with transitional epithelium. • In carnivores, bladder extends to abdominal cavity. • Walls become thinner, the more full the bladder becomes. • Urination (micturition or uresis) is the expulsion of urine from the urinary bladder into the urethra.
Process of Urination • Urine Accumulation – Urine is constantly accumulated in bladder. – When reaches a certain point, triggers stretch receptors. • Where have we seen these before? • Muscle contraction – When trigger point is reached, spinal reflex sends impulse to bladder muscles – Muscles in bladder contract and give sensation of needing to urinate. • Sphincter Muscle Control – Sphincter at neck of bladder provides temporary control of urine. – If enough pressure is exerted on sphincter, will eventually relax and release urine. – Rupture can occur if bladder is not emptied in timely fashion. • Use caution when manually expressing or palpating bladder • https: //youtu. be/US 0 v. Noxs. W-k
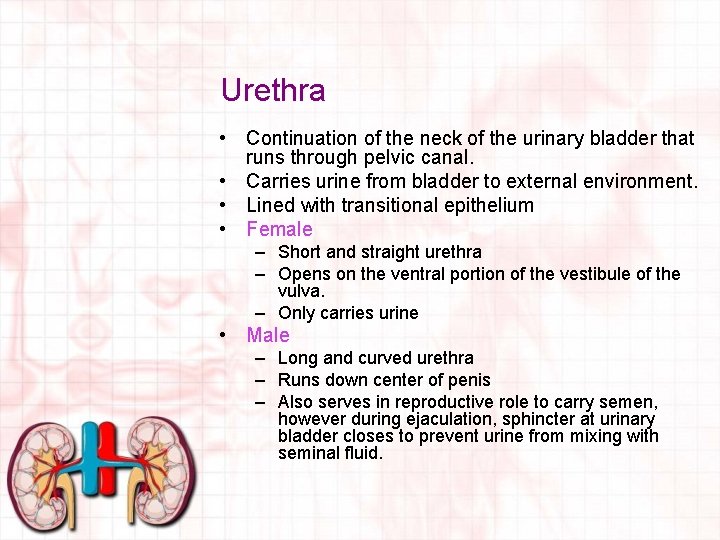
Urethra • Continuation of the neck of the urinary bladder that runs through pelvic canal. • Carries urine from bladder to external environment. • Lined with transitional epithelium • Female – Short and straight urethra – Opens on the ventral portion of the vestibule of the vulva. – Only carries urine • Male – Long and curved urethra – Runs down center of penis – Also serves in reproductive role to carry semen, however during ejaculation, sphincter at urinary bladder closes to prevent urine from mixing with seminal fluid.
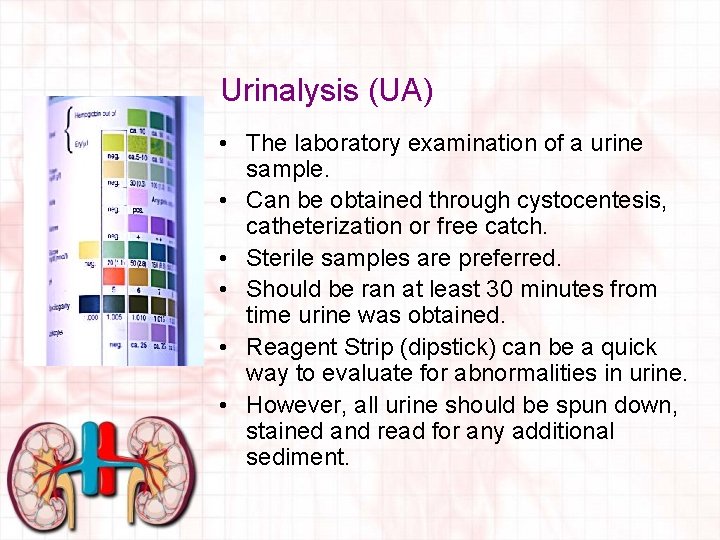
Urinalysis (UA) • The laboratory examination of a urine sample. • Can be obtained through cystocentesis, catheterization or free catch. • Sterile samples are preferred. • Should be ran at least 30 minutes from time urine was obtained. • Reagent Strip (dipstick) can be a quick way to evaluate for abnormalities in urine. • However, all urine should be spun down, stained and read for any additional sediment.
Cystocentesis • The introduction of a sterile needle directly into the bladder to obtain a sterile sample for testing or culture. • Not truly sterile unless you sterile scrub, like prepping for SX. Is the MOST sterile procedure. • Can be palpated, ultrasound guided, or done by landmarks. – Where the alcohol pools
Urinary Cultures • Are used to detect organisms (mainly bacteria) that may be causing a urinary tract infection. • Sterile urine sample is swabbed on an agar plate and grown. • Can see which antibiotics that bacteria is most susceptible to.
Urinary Tract Infections • Most commonly caused by bacteria. • Bacteria may be ingested or travel up urethra to urinary bladder • Can encompass any portion of the urinary system (kidneys, ureters, bladder or urethra). • Symptoms can include blood in urine, painful urination or frequent urination. • If symptoms persist, further imaging may be needed to rule out stones.
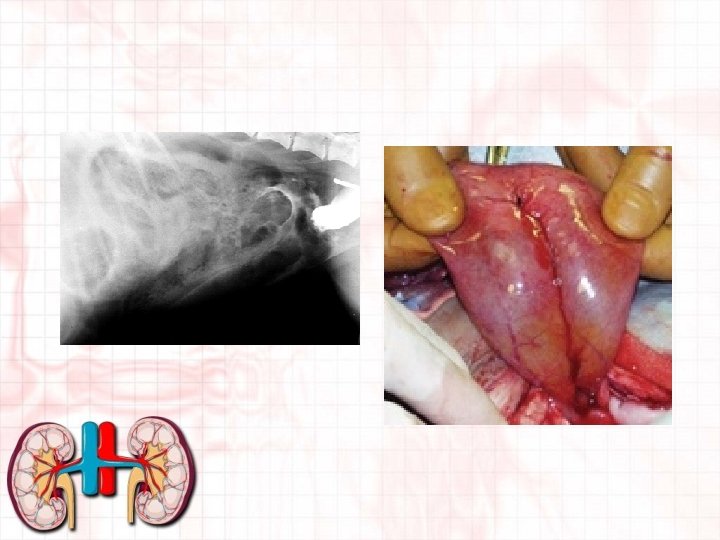
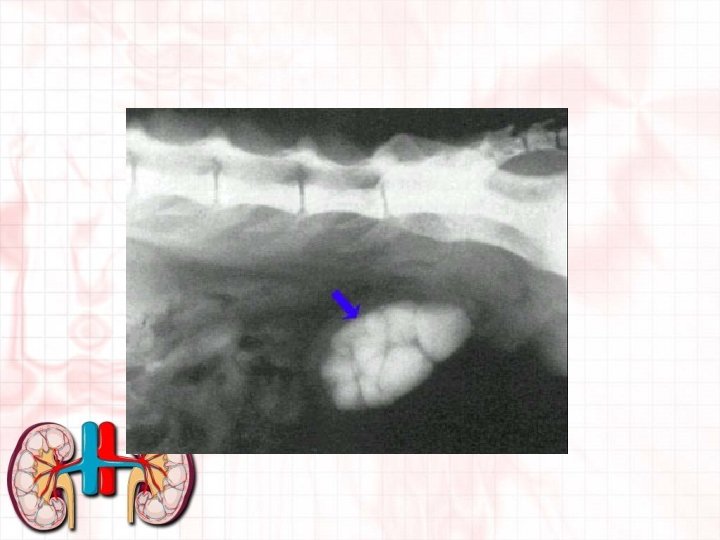
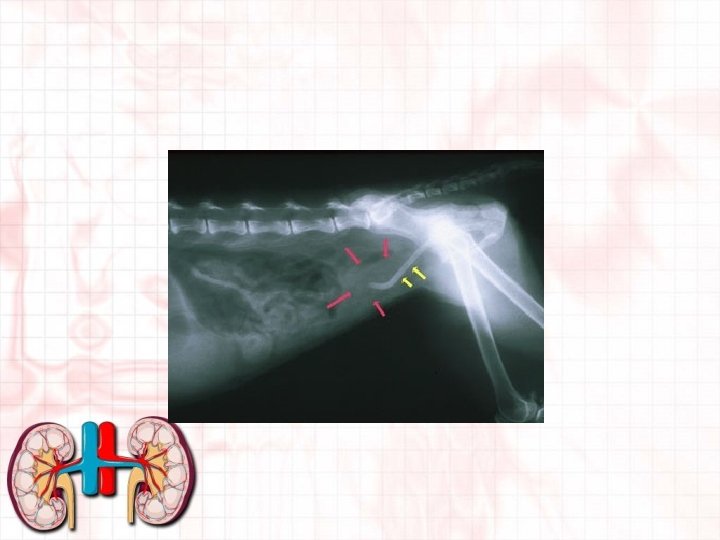
Uroliths and Urolithiasis • Uroliths- aggregates of crystals in the urine that may become urolithiasis. • Urolithiasis- the presence of urinary stones in the bladder. • Usually are formed when the p. H of the urine is too low or too high. • Bacterial infections or diet may influence the p. H levels. • May have a mixed stone.

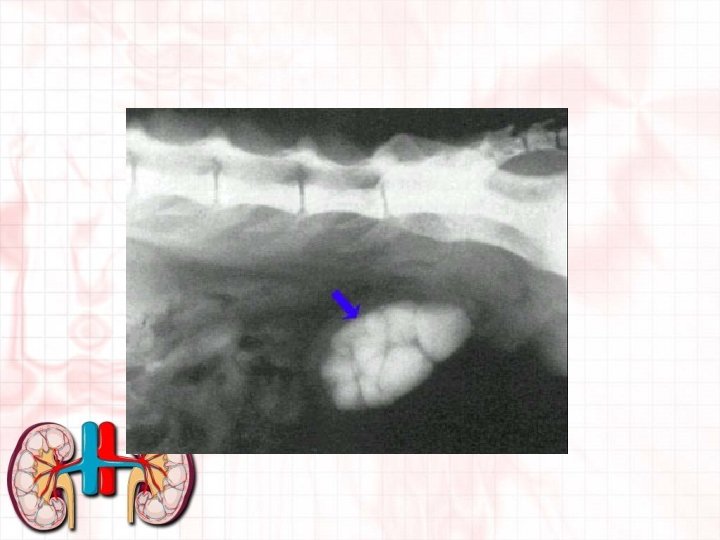
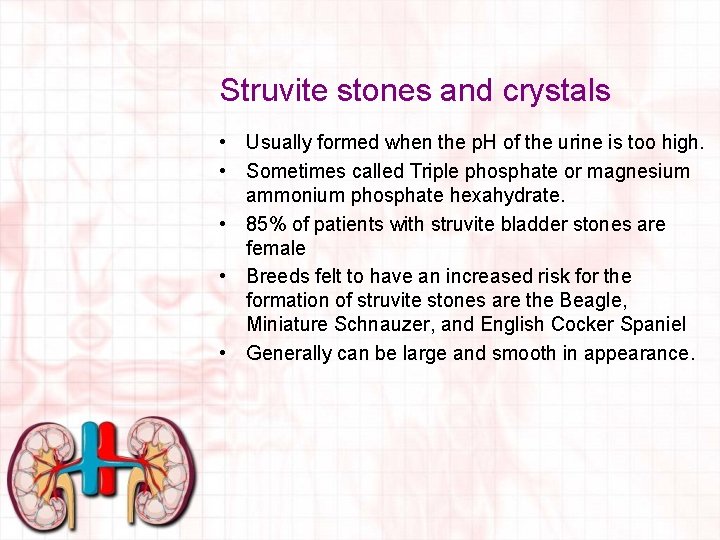
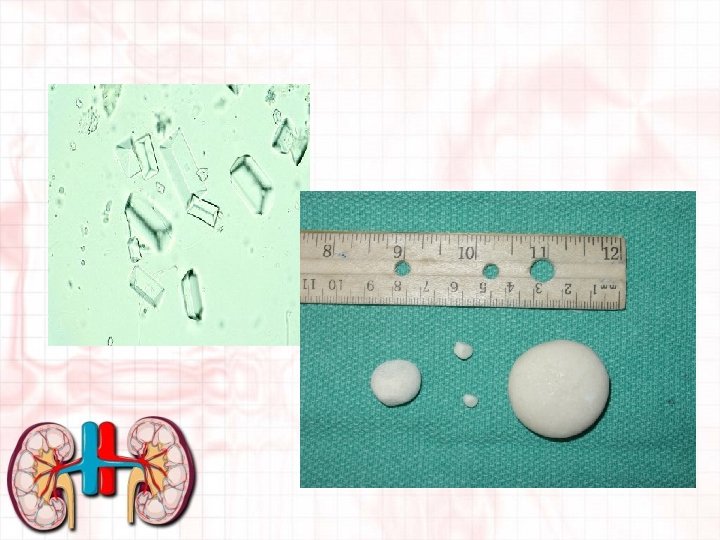
Struvite stones and crystals • Usually formed when the p. H of the urine is too high. • Sometimes called Triple phosphate or magnesium ammonium phosphate hexahydrate. • 85% of patients with struvite bladder stones are female • Breeds felt to have an increased risk for the formation of struvite stones are the Beagle, Miniature Schnauzer, and English Cocker Spaniel • Generally can be large and smooth in appearance.
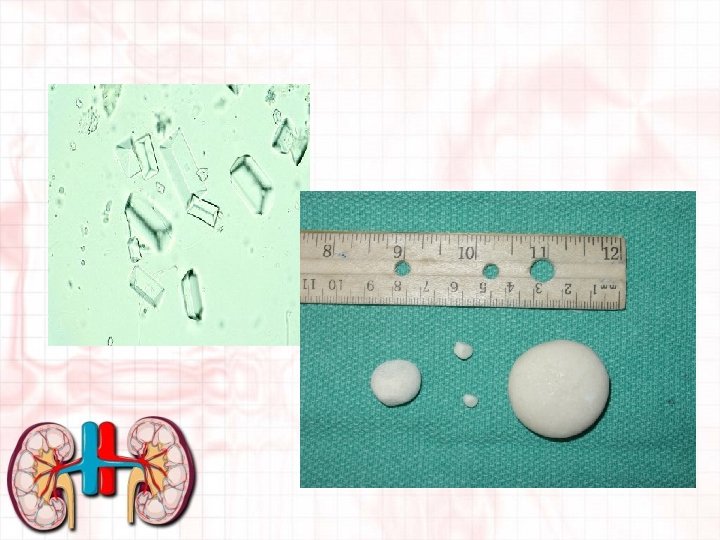
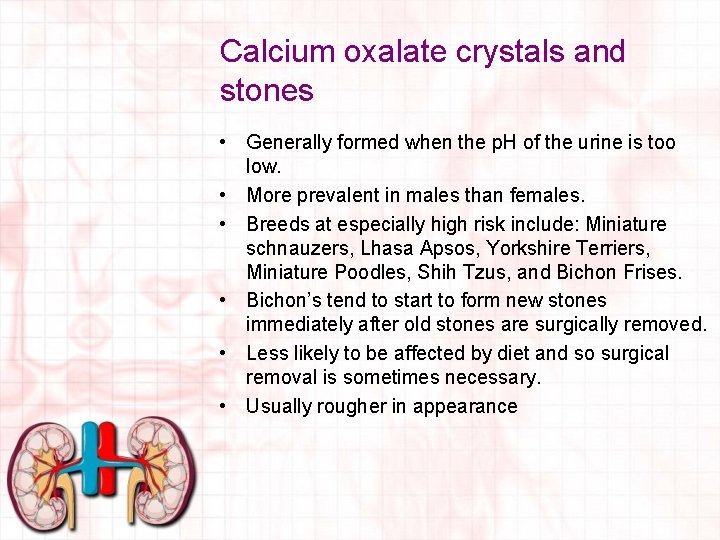
Calcium oxalate crystals and stones • Generally formed when the p. H of the urine is too low. • More prevalent in males than females. • Breeds at especially high risk include: Miniature schnauzers, Lhasa Apsos, Yorkshire Terriers, Miniature Poodles, Shih Tzus, and Bichon Frises. • Bichon’s tend to start to form new stones immediately after old stones are surgically removed. • Less likely to be affected by diet and so surgical removal is sometimes necessary. • Usually rougher in appearance

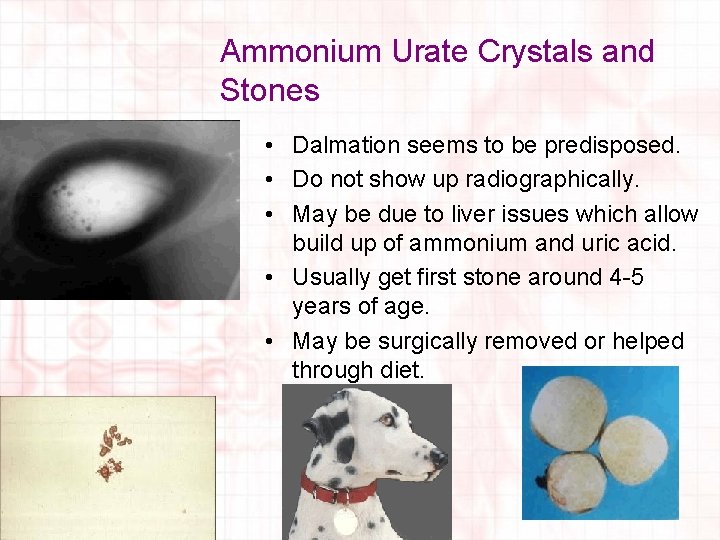
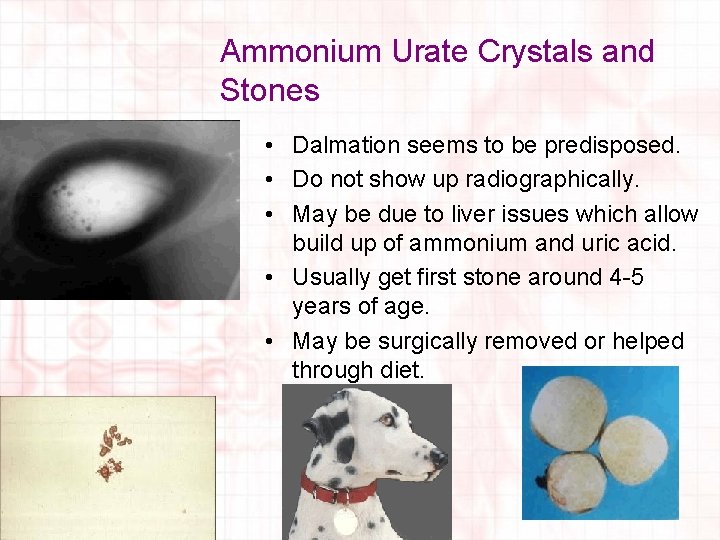
Ammonium Urate Crystals and Stones • Dalmation seems to be predisposed. • Do not show up radiographically. • May be due to liver issues which allow build up of ammonium and uric acid. • Usually get first stone around 4 -5 years of age. • May be surgically removed or helped through diet.

Cystine Stones and Crystals • Very small • May be predisposed in animals that have cystine in the urine. • Newfoundland, English Bulldog and Dachshund are predisposed. • Do not show up radiographically. • Formed in acidic environment • May be dissolved in diet or surgically removed.
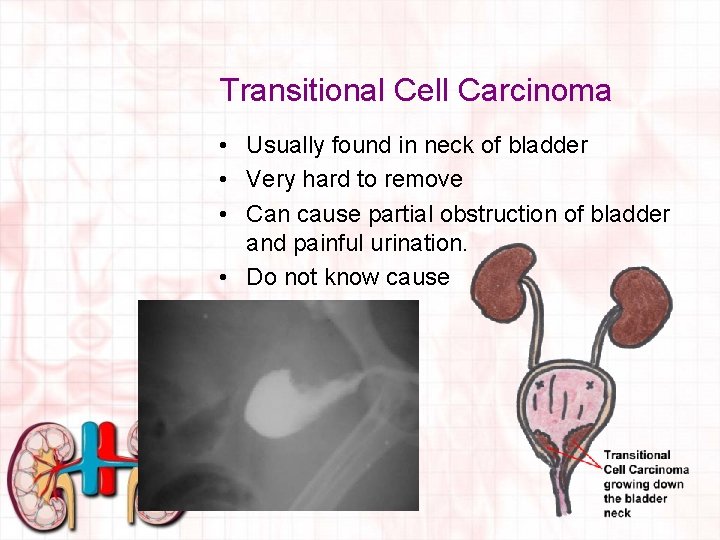
Transitional Cell Carcinoma • Usually found in neck of bladder • Very hard to remove • Can cause partial obstruction of bladder and painful urination. • Do not know cause
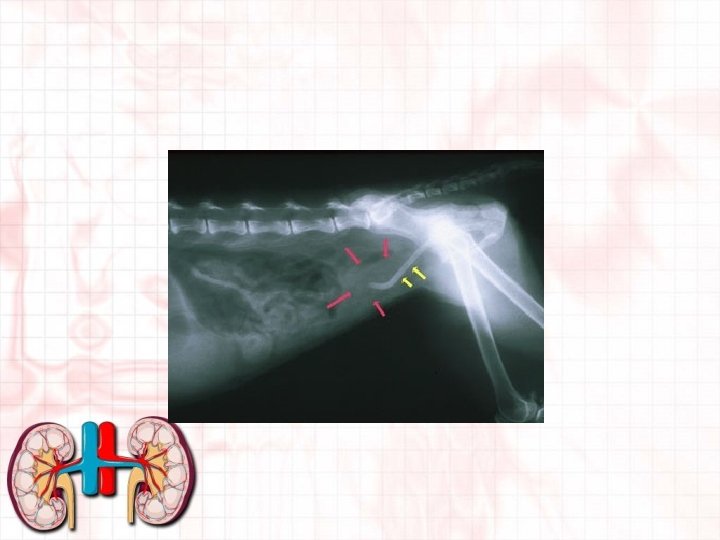
Obstructions • If crystal or stone becomes lodged in urethra can obstruct flow of urine. • May also be caused by tumor. • What we called “blocked” • Feline Lower Urinary Tract Disease. • May need to treat as emergency surgery or place catheter to flush back stone to bladder to dissolve or remove. • If not treated can lead to bladder rupture
Diabetes • Diabetes Insipidus – If ADH not present enough to reabsorb water from collecting ducts. • Diabetes Mellitus – An elevation of glucose due to inadequate amounts of insulin being produced from pancreas. – Signs can be glucose released in urine as well as increased thirst and urination.
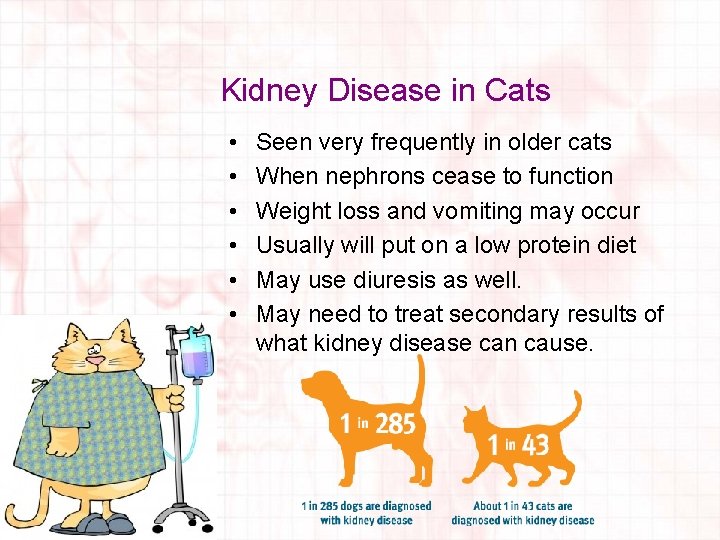
Kidney Disease in Cats • • • Seen very frequently in older cats When nephrons cease to function Weight loss and vomiting may occur Usually will put on a low protein diet May use diuresis as well. May need to treat secondary results of what kidney disease can cause.