THE URINARY SYSTEM Waste Products Liver removes amine






- Slides: 28
THE URINARY SYSTEM
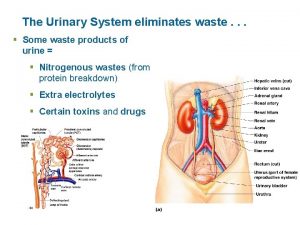
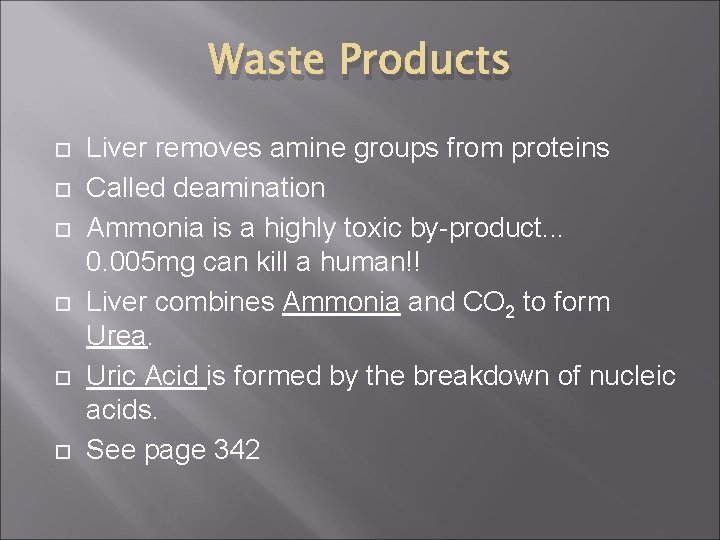
Waste Products Liver removes amine groups from proteins Called deamination Ammonia is a highly toxic by-product. . . 0. 005 mg can kill a human!! Liver combines Ammonia and CO 2 to form Urea. Uric Acid is formed by the breakdown of nucleic acids. See page 342
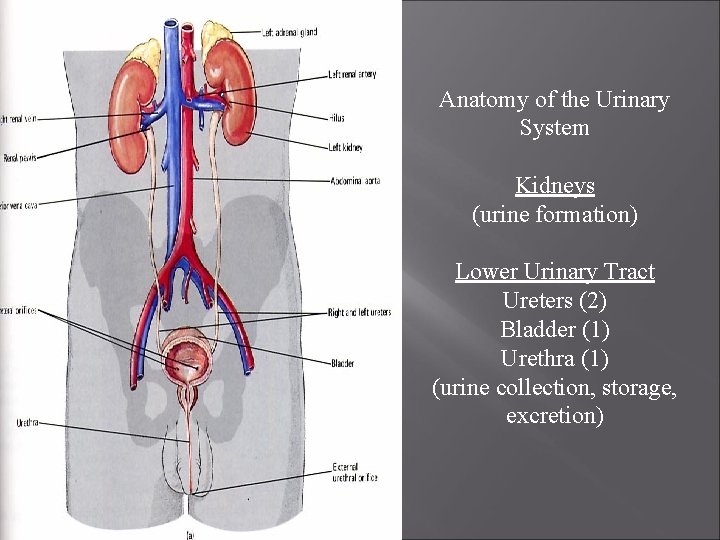
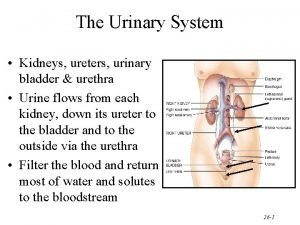
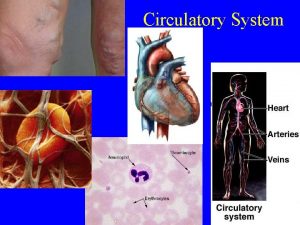
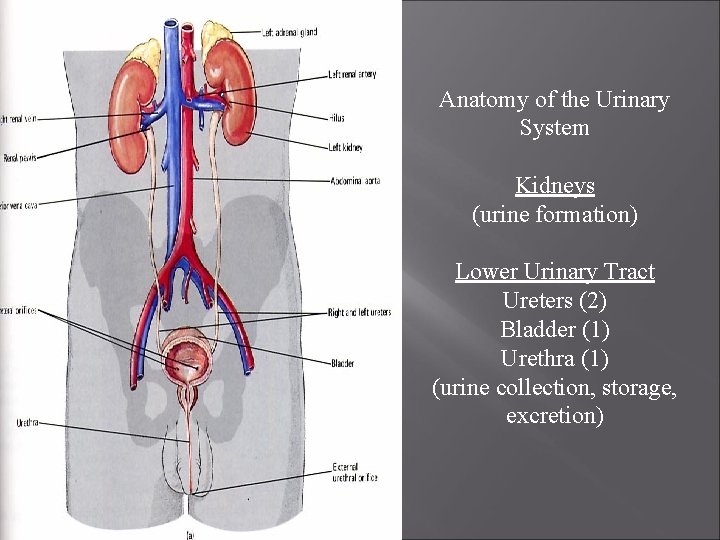
Anatomy of the Urinary System Kidneys (urine formation) Lower Urinary Tract Ureters (2) Bladder (1) Urethra (1) (urine collection, storage, excretion)
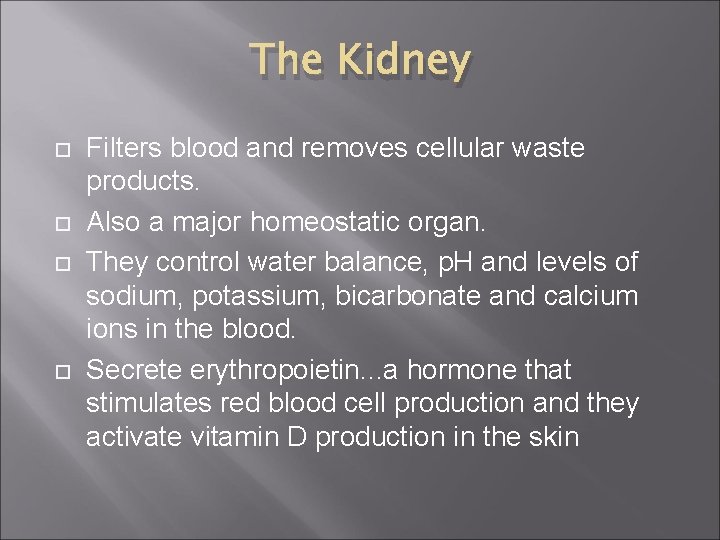
The Kidney Filters blood and removes cellular waste products. Also a major homeostatic organ. They control water balance, p. H and levels of sodium, potassium, bicarbonate and calcium ions in the blood. Secrete erythropoietin. . . a hormone that stimulates red blood cell production and they activate vitamin D production in the skin
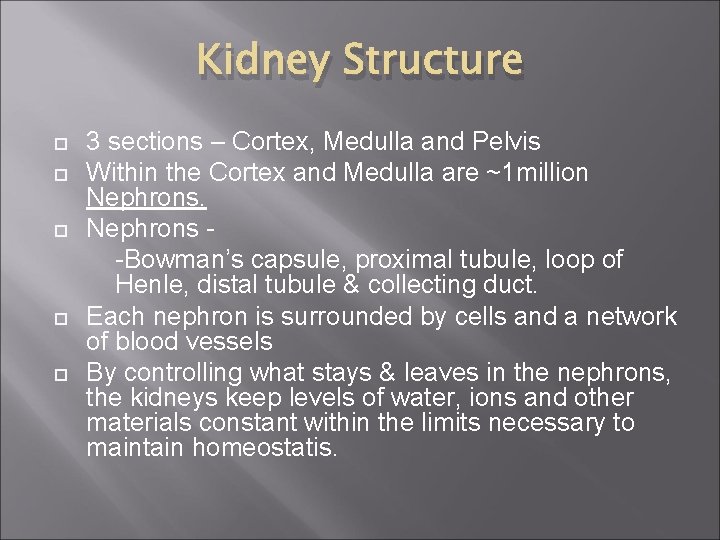
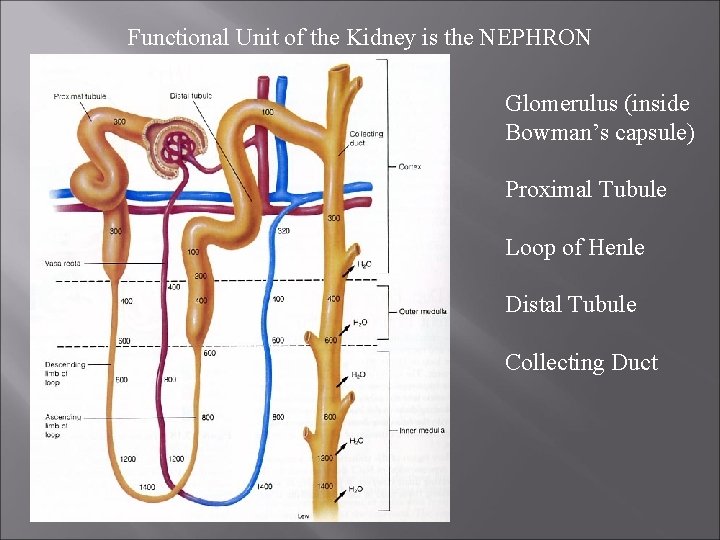
Kidney Structure 3 sections – Cortex, Medulla and Pelvis Within the Cortex and Medulla are ~1 million Nephrons -Bowman’s capsule, proximal tubule, loop of Henle, distal tubule & collecting duct. Each nephron is surrounded by cells and a network of blood vessels By controlling what stays & leaves in the nephrons, the kidneys keep levels of water, ions and other materials constant within the limits necessary to maintain homeostatis.
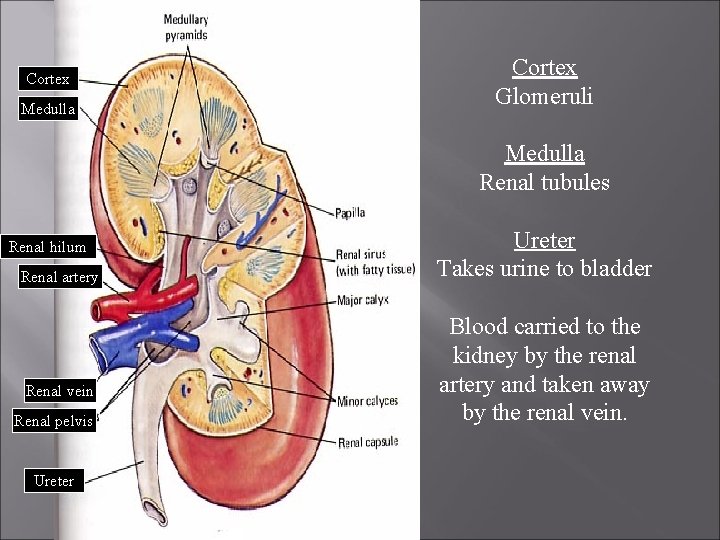
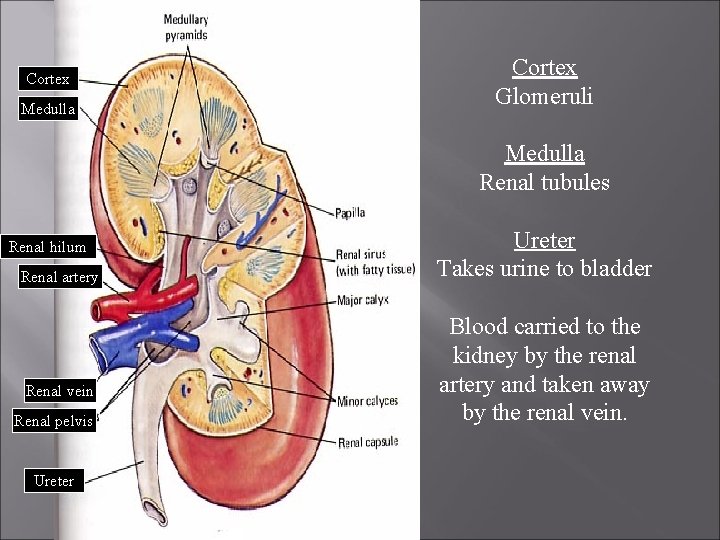
Cortex Medulla Cortex Glomeruli Medulla Renal tubules Renal hilum Renal artery Renal vein Renal pelvis Ureter Takes urine to bladder Blood carried to the kidney by the renal artery and taken away by the renal vein.
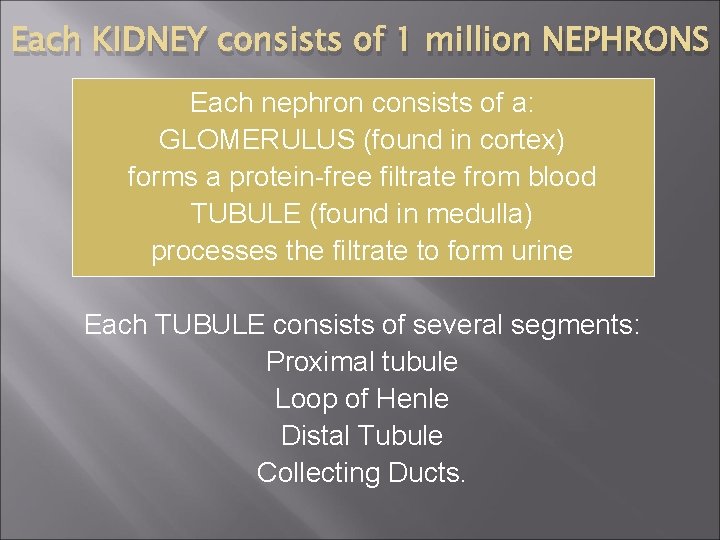
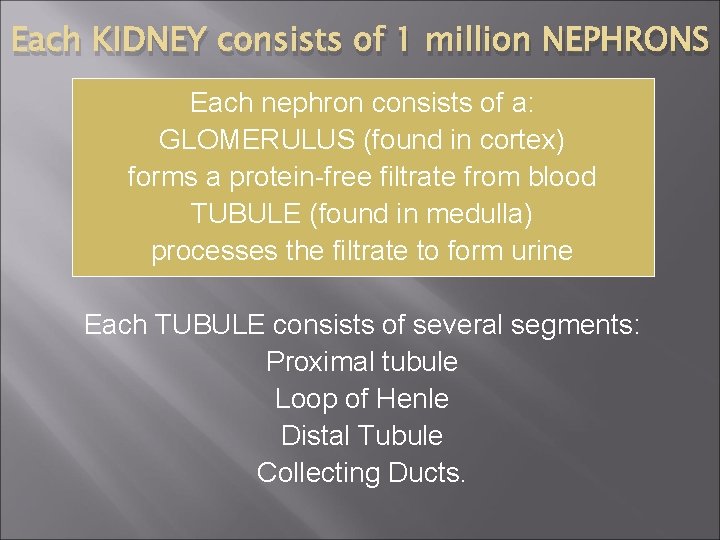
Each KIDNEY consists of 1 million NEPHRONS Each nephron consists of a: GLOMERULUS (found in cortex) forms a protein-free filtrate from blood TUBULE (found in medulla) processes the filtrate to form urine Each TUBULE consists of several segments: Proximal tubule Loop of Henle Distal Tubule Collecting Ducts.
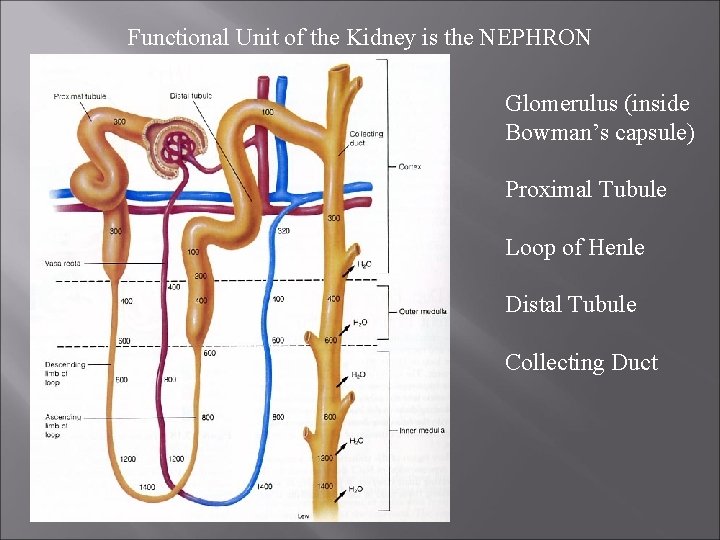
Functional Unit of the Kidney is the NEPHRON Glomerulus (inside Bowman’s capsule) Proximal Tubule Loop of Henle Distal Tubule Collecting Duct
http: //www. youtube. com/watch? v=a. QZa. NXNro VY&feature=related P 345 #1 -3 P 348 #1 -4
Urine Formation - Filtration Is accomplished by movement of fluids from blood into Bowman’s capsule. Each nephron of kidney has its own blood supply Materials move from high [ ] to low [ ] generally
Reabsorption Involves the transfer of essential solutes and water from the nephron back to the blood About 600 m. L fluid flows through kidneys every minute About 20% filtered into nephrons 1 m. L of urine formed for every 120 m. L of fluid filtered into nephron (remainder reabsorbed) selective Reabsorption both active and passive carrier molecules move Na+ ions over across cell membranes of cells which line the nephron Negative ions (Cl-, HCO 3 -) follow Na+ by charge attraction Excess Na. Cl remains in nephron and excreted in urine when reabsorption reaches the threshold level (max amount of material that can be moved across the nephron. Proteins in the bloodstream draw water from the interstitial fluid (fluid that surrounds the body cells) into the blood
Secretion Involves movement of materials from blood back to nephron N-containing wastes, excess H+ ions, and minerals such as K+ are examples of substances secreted Even drugs (e. g. penicillin) can be secreted Molecules are shuttled (active tran) from blood to nephron


Page 352 # 1 -6
Water Balance Involves the interaction of the body’s two communication systems Nervous system Endocrine system
Regulating ADH Antidiuretic hormone (ADH) helps regulate osmotic pressure of body fluids by causing kidneys to increase water reabsorption when ADH released, more concentrated urine is produced (therefore conserving water) ADH produced by hypothalamus and moves to pituitary gland (via specialized fibres) which stores and releases ADH into blood
Osmoreceptors located in hypothalamus detect changes in osmotic pressure Decrease of water [ ] causes blood solutes to increase in [ ], thereby increasing blood’s osmotic pressure Water then moves into bloodstream causing hypothalamus cells to shrink and sensation of thirst Causes signalling the release of ADH from pituitary, carried by bloodstream to kidneys Kidneys reabsorb more water, thereby creating more concentrated urine, preventing increase of osmotic pressure of body fluids.

If sensation of thirst causes intake of water, if more water is taken in, it is absorbed by blood and [ ] of solutes in blood decreases. Greater amount of H 2 O taken in, lower osmotic pressure of blood. Blood becomes more dilute, fluids move to hypothalamus cells and they swell. Nerve messages to pituitary stop. Less ADH released, less H 2 O reabsorbed from nephrons.
Kidneys and Blood Pressure Dec. Blood pressure or blood volume (from dehydration, blood loss) can cause a reduction in the delivery of oxygen nutrients to tissues. Blood pressure receptors in the Juxtaglomerular Apparatus (found near the glomerulus) detect this low BP Specialized cells in the J. A. then release Renin is an enyme that converts Angiotensinogen (a plasma Protein produced by the liver) into Angiotensin (active form)
Kidneys and Blood Pressure Angiotensin causes constriction of blood vessels; this increases Blood Pressure. It also stimulates the release of Aldosterone (from the Adrenal Glands above each kidney) It acts on the Nephrons to increase Na+ reabsorption This increases the osmotic gradient, so water moves out of the Nephron by osmosis back into the bloodstream. This increase Blood Volume

p. H Balance Kidneys maintain p. H balance p. H of human body remains relatively constant (7. 3 -7. 5) p. H may lower during Cell Resp – Acids produced Acid-base balance maintained by buffer systems that absorb excess H+ ions. Buffer systems maintain Acid-Base balance

p. H Balance Bicarbonate ions buffer excess H+ ions, producing carbonic acid Carbonic acid is a weak acid that breaks down into CO 2 and goes to the lungs and is exhaled. This rxn is reversed in the kidneys CO 2 is actively transported from capillaries into the cells that line the nephron. Here CO 2 combines with water to initiate the reverse rxn generating HCO 3 - H+ ions The ions diffuse back into the blood, restoring the buffer The H+ ions left recombine with the phosphate ions or ammonia and are excreted with the nephric filtrate

Kidney Diseases Make short note on. . . 1. Diabetes Mellitus 2. Diabetes Insipitus 3. Bright’s Disease 4. Kidney Stones 5. Dialysis Technology 6. Kidney Transplants and Xenotransplants (p 360) HW Page 356 1 -8
Urine Analysis Lab
 Tertiary amine structure
Tertiary amine structure Lymphatic system and urinary system
Lymphatic system and urinary system Face shapes milady
Face shapes milady Word basic
Word basic The most common form of hair removal in salons and spas is
The most common form of hair removal in salons and spas is West african cotton farmers are very upset
West african cotton farmers are very upset Mustard gas removes guanine from dna
Mustard gas removes guanine from dna Assimilation is indicated by the letter(s) _____.
Assimilation is indicated by the letter(s) _____. Physiology of urine formation
Physiology of urine formation The urinary system chapter 15
The urinary system chapter 15 Combining form for urinary bladder
Combining form for urinary bladder Intugementary
Intugementary Urogenital papilla fetal pig
Urogenital papilla fetal pig Chapter 30 the urinary system
Chapter 30 the urinary system Chapter 15 the urinary system figure 15-3
Chapter 15 the urinary system figure 15-3 Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system model
Urinary system model Osteichthyes
Osteichthyes Urinary system powerpoint
Urinary system powerpoint Urinary system also known as
Urinary system also known as Adh hormone function
Adh hormone function Renal corpuscle
Renal corpuscle Figure 15-3 is a diagram of the nephron
Figure 15-3 is a diagram of the nephron L
L Defination of urine
Defination of urine Homework
Homework Rat appendix
Rat appendix Rat urinary system
Rat urinary system