Topic Urinary system Functions 1 Removes toxic of
- Slides: 29
Topic: Urinary system.
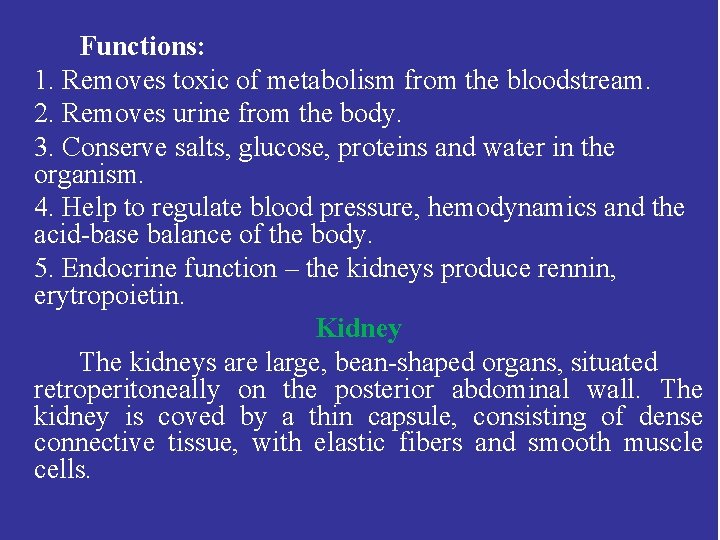
Functions: 1. Removes toxic of metabolism from the bloodstream. 2. Removes urine from the body. 3. Conserve salts, glucose, proteins and water in the organism. 4. Help to regulate blood pressure, hemodynamics and the acid-base balance of the body. 5. Endocrine function – the kidneys produce rennin, erytropoietin. Kidney The kidneys are large, bean-shaped organs, situated retroperitoneally on the posterior abdominal wall. The kidney is coved by a thin capsule, consisting of dense connective tissue, with elastic fibers and smooth muscle cells.
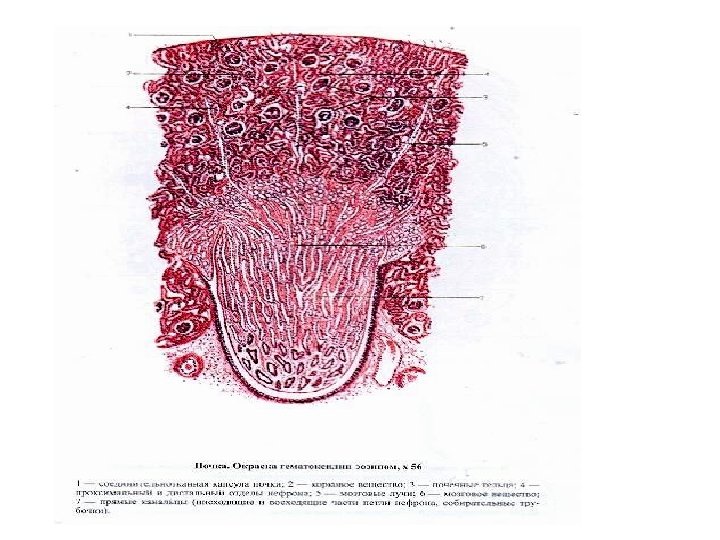
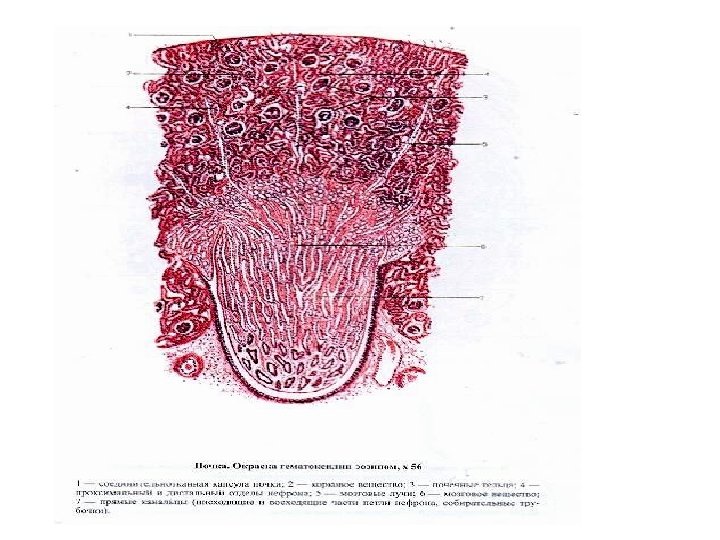
The kidney is separated into a cortex and a medulla. The cortical substance is located under medulla. The medulla contains 6 to 12 the renal pyramids. The base of each pyramid is oriented toward the cortex, its apex called the renal papilla. The apex is surrounded minor calyx, joining two or three neighboring minor calyces, forms a major calyx. The three or four major calyces are opened into the renal pelvis. Neighboring pyramids are separated from each other by the cortical columns. In the cortex of the medullary rays are located. It is continuations of the medulla in the cortical substance.
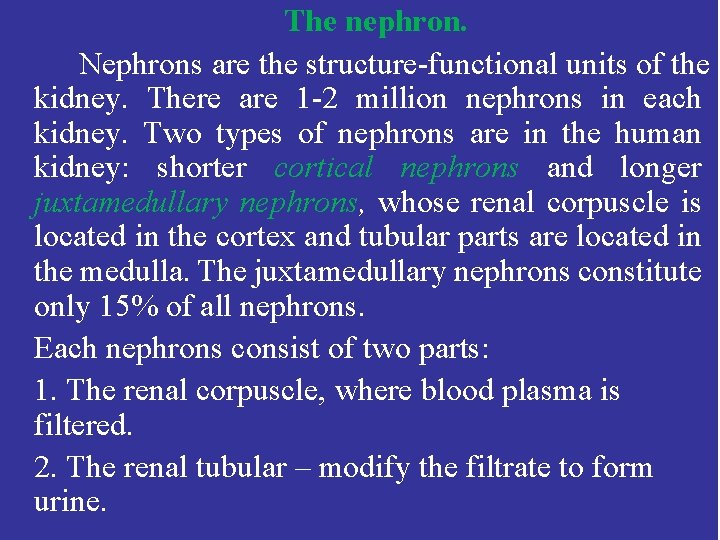
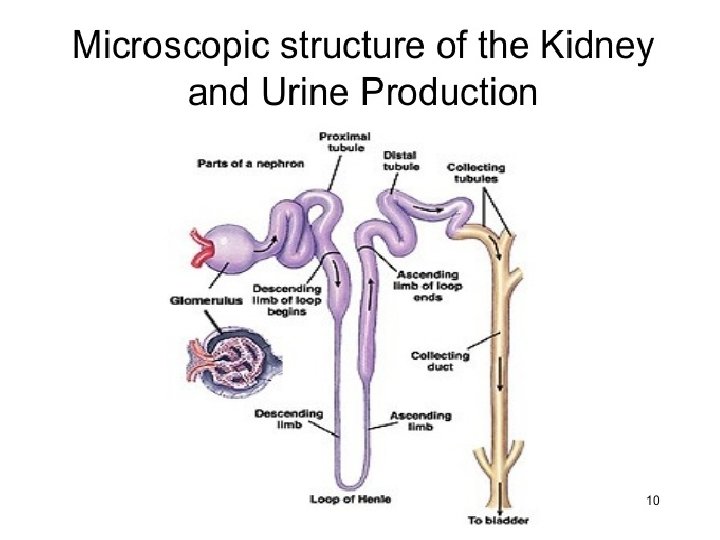
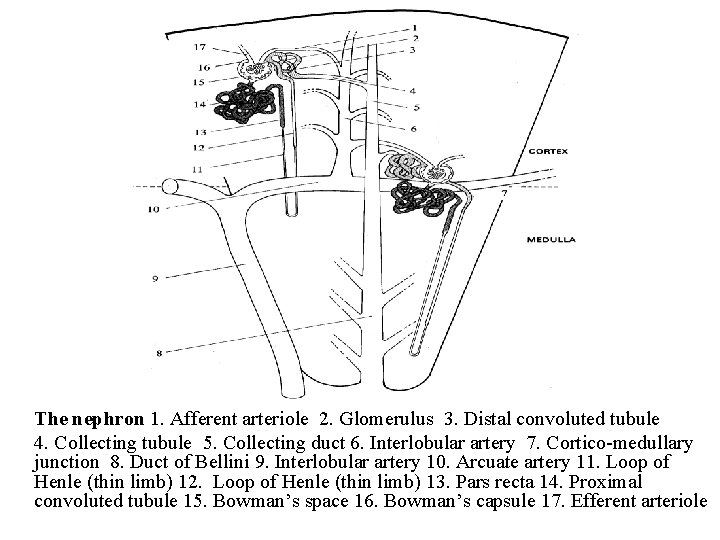
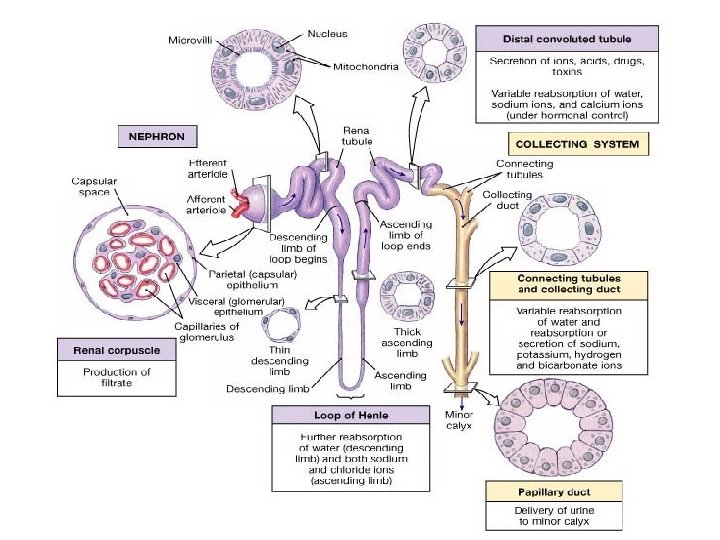
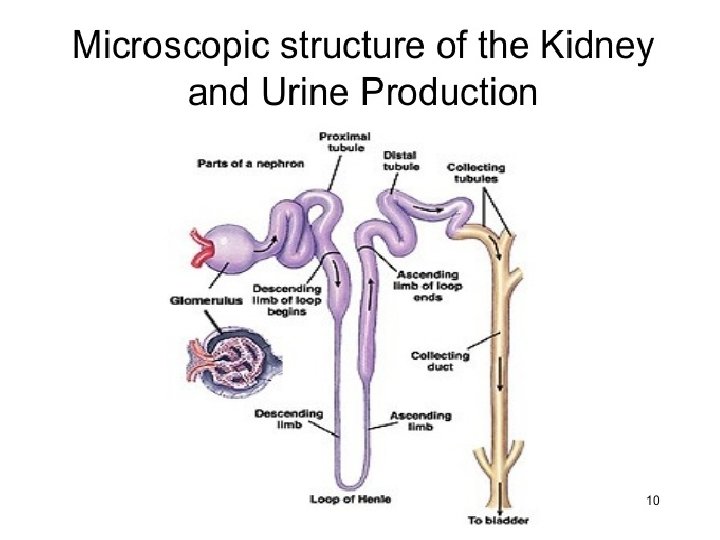
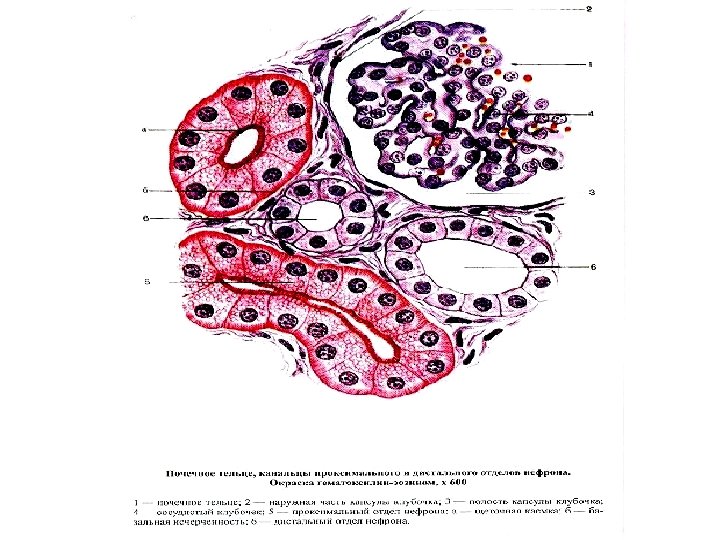
The nephron. Nephrons are the structure-functional units of the kidney. There are 1 -2 million nephrons in each kidney. Two types of nephrons are in the human kidney: shorter cortical nephrons and longer juxtamedullary nephrons, whose renal corpuscle is located in the cortex and tubular parts are located in the medulla. The juxtamedullary nephrons constitute only 15% of all nephrons. Each nephrons consist of two parts: 1. The renal corpuscle, where blood plasma is filtered. 2. The renal tubular – modify the filtrate to form urine.
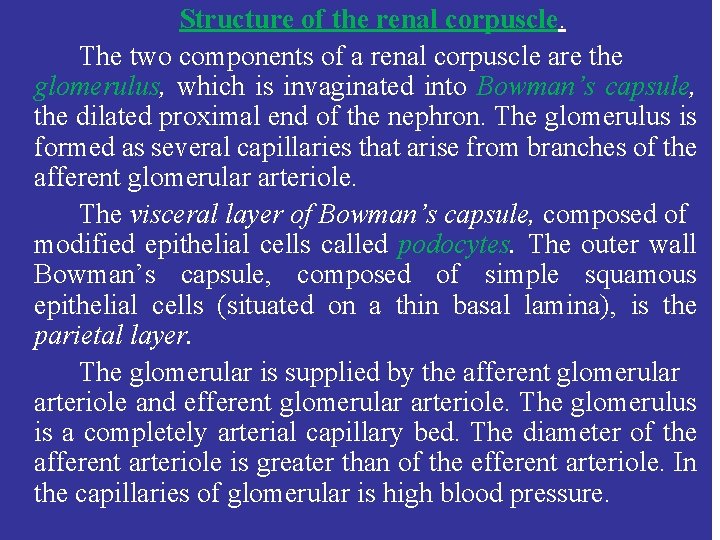
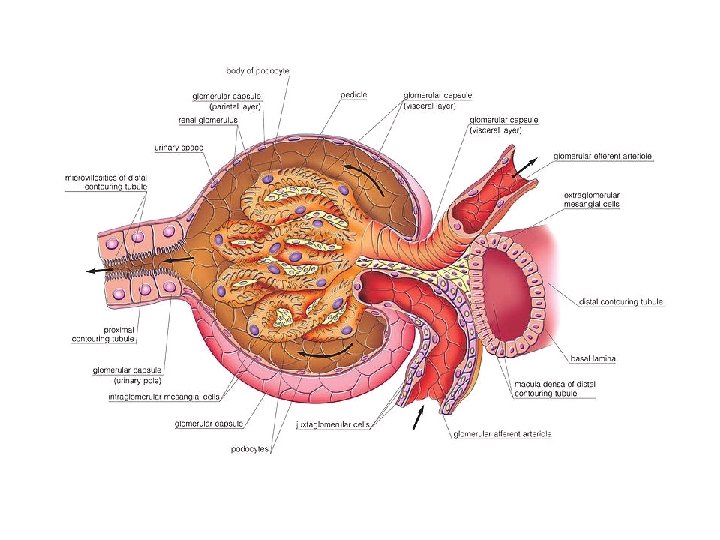
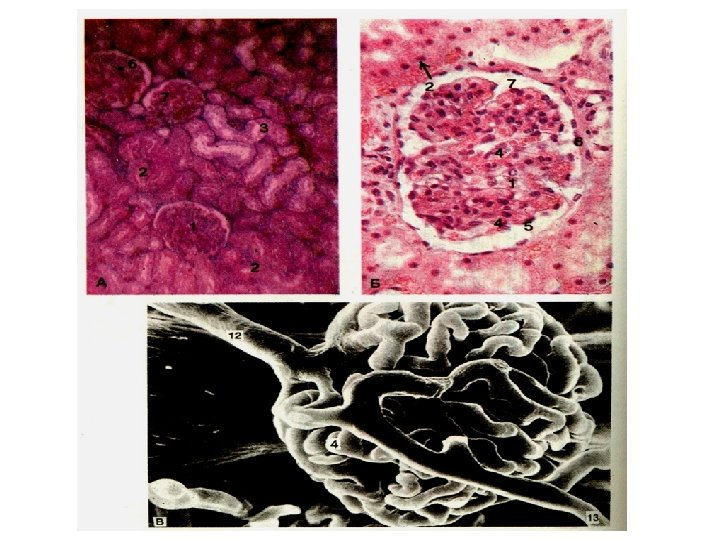
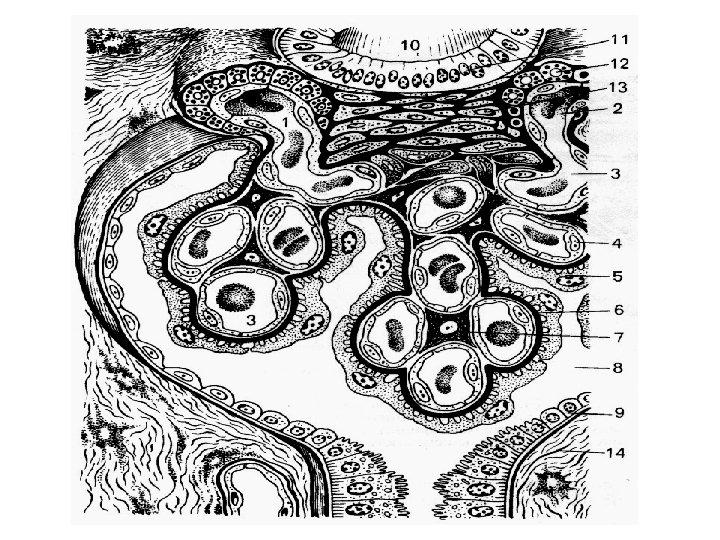
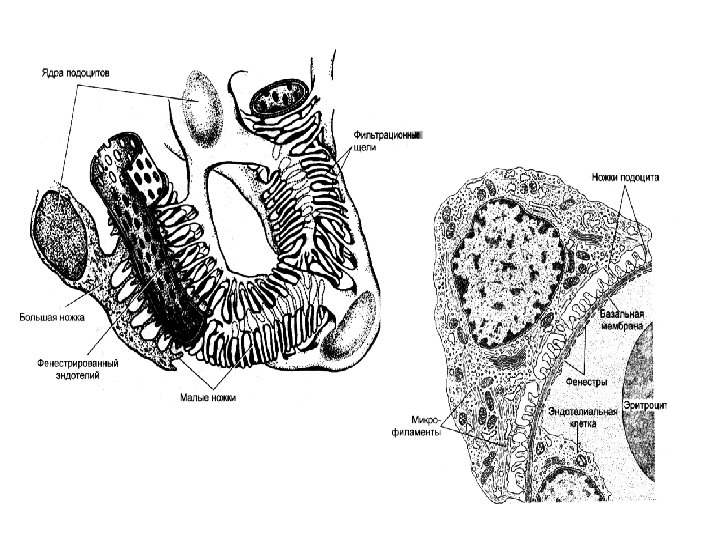
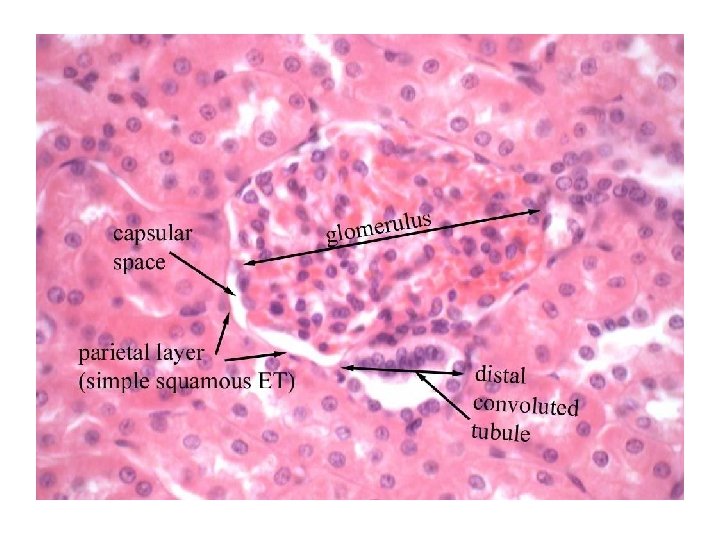
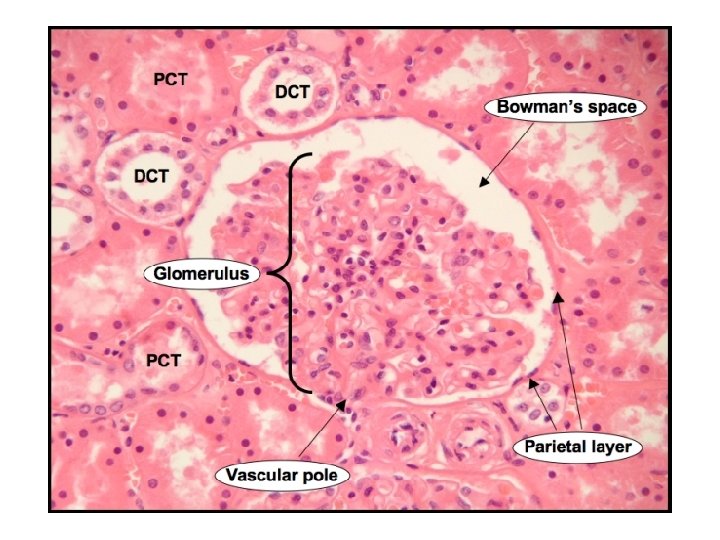
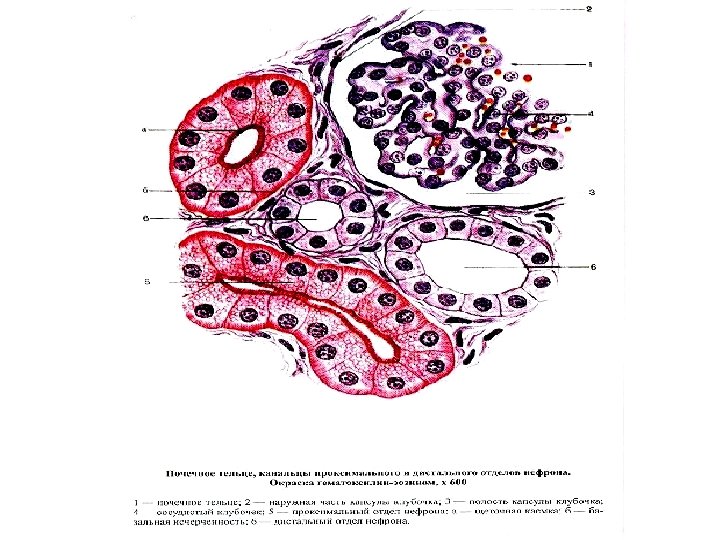
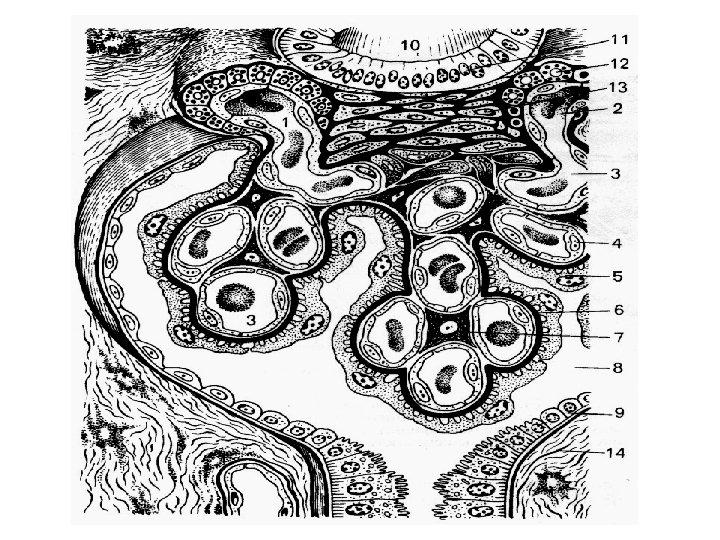
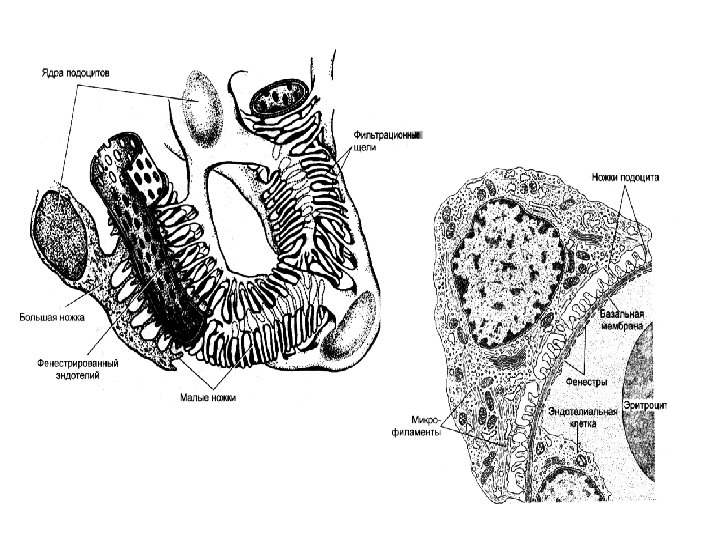
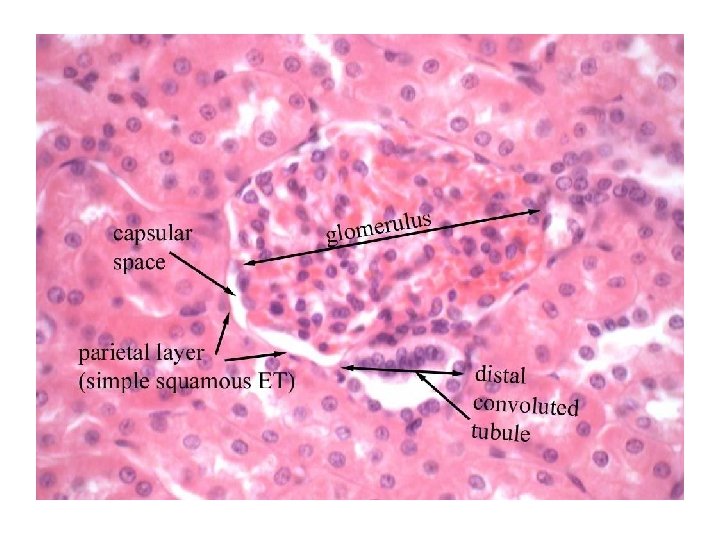
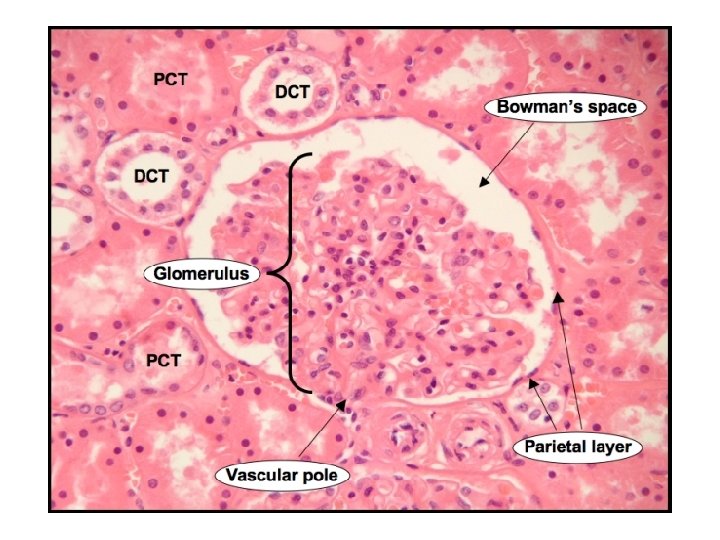
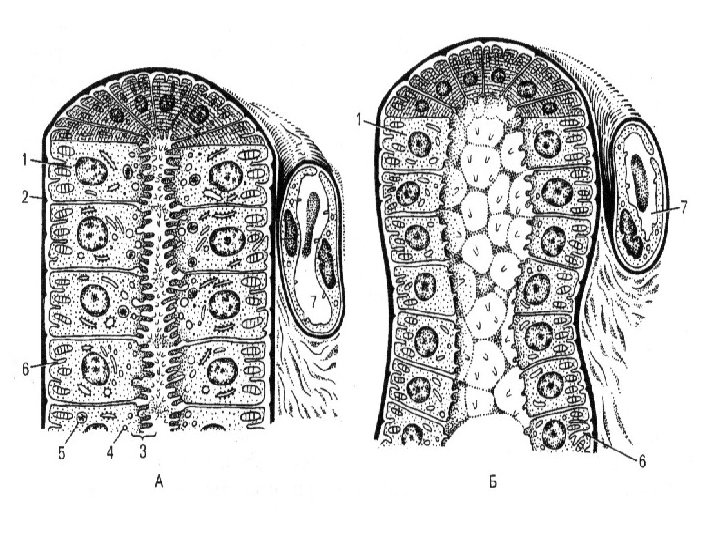
Structure of the renal corpuscle. The two components of a renal corpuscle are the glomerulus, which is invaginated into Bowman’s capsule, the dilated proximal end of the nephron. The glomerulus is formed as several capillaries that arise from branches of the afferent glomerular arteriole. The visceral layer of Bowman’s capsule, composed of modified epithelial cells called podocytes. The outer wall Bowman’s capsule, composed of simple squamous epithelial cells (situated on a thin basal lamina), is the parietal layer. The glomerular is supplied by the afferent glomerular arteriole and efferent glomerular arteriole. The glomerulus is a completely arterial capillary bed. The diameter of the afferent arteriole is greater than of the efferent arteriole. In the capillaries of glomerular is high blood pressure.
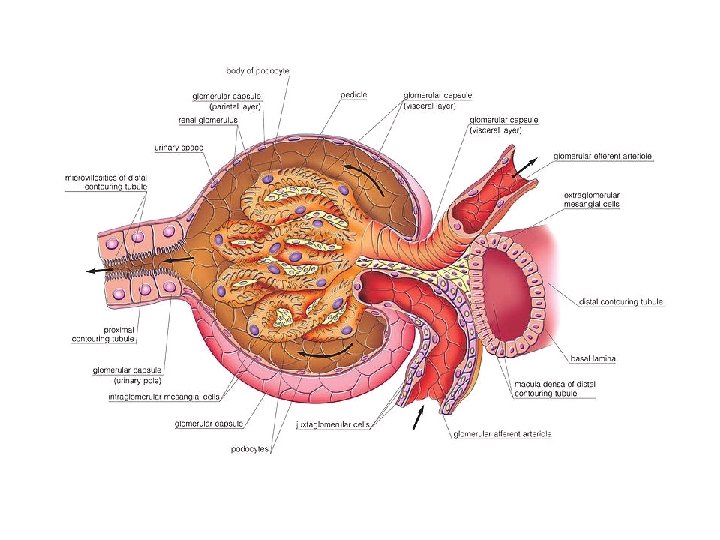
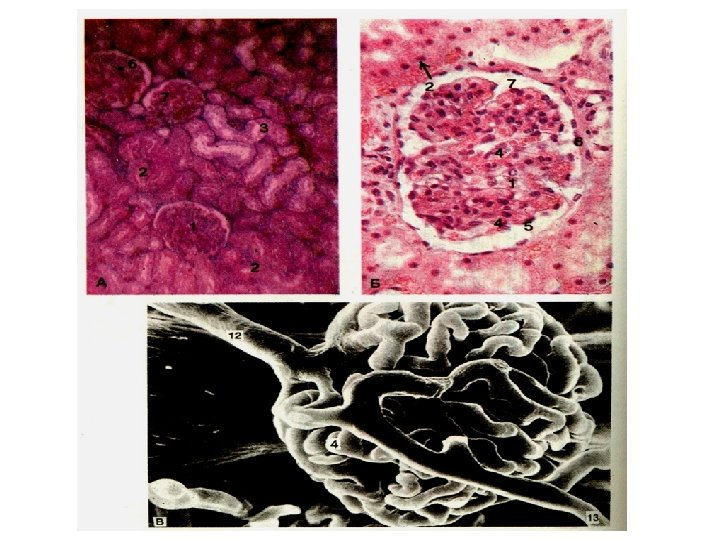
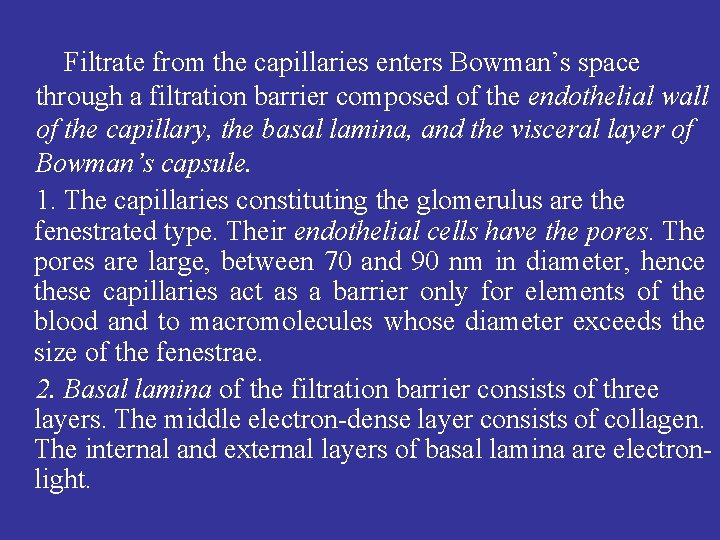
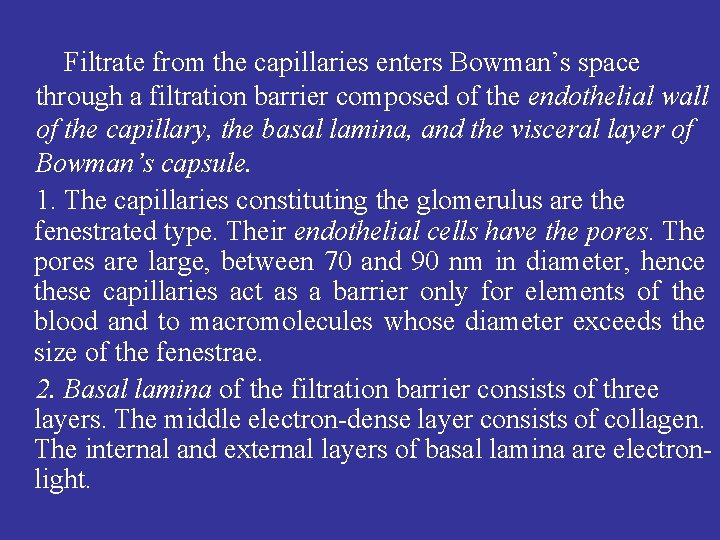
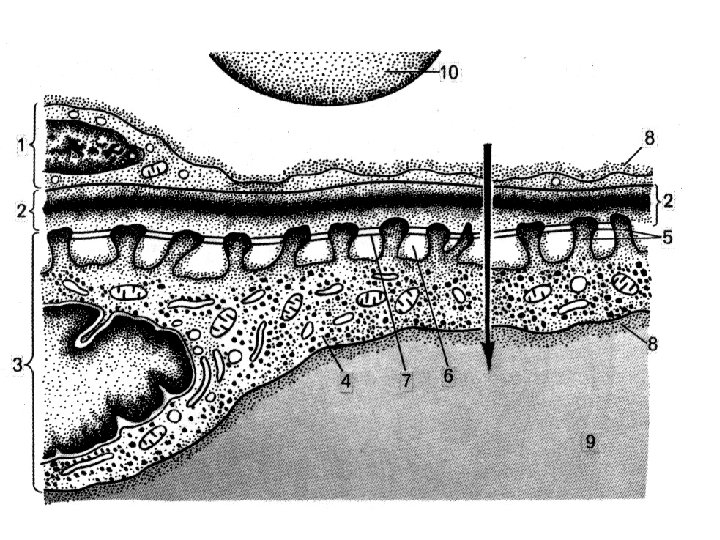
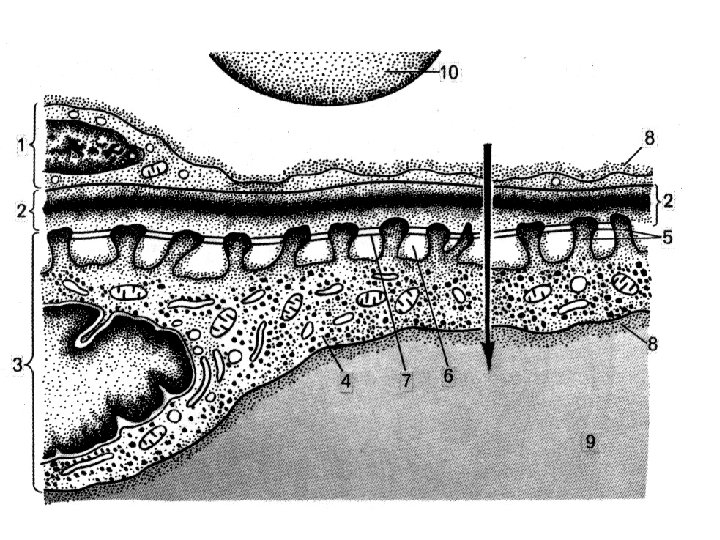
Filtrate from the capillaries enters Bowman’s space through a filtration barrier composed of the endothelial wall of the capillary, the basal lamina, and the visceral layer of Bowman’s capsule. 1. The capillaries constituting the glomerulus are the fenestrated type. Their endothelial cells have the pores. The pores are large, between 70 and 90 nm in diameter, hence these capillaries act as a barrier only for elements of the blood and to macromolecules whose diameter exceeds the size of the fenestrae. 2. Basal lamina of the filtration barrier consists of three layers. The middle electron-dense layer consists of collagen. The internal and external layers of basal lamina are electronlight.
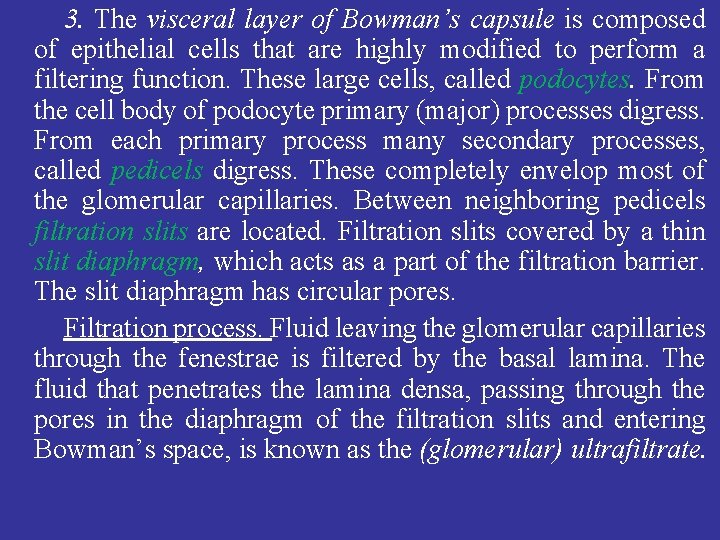
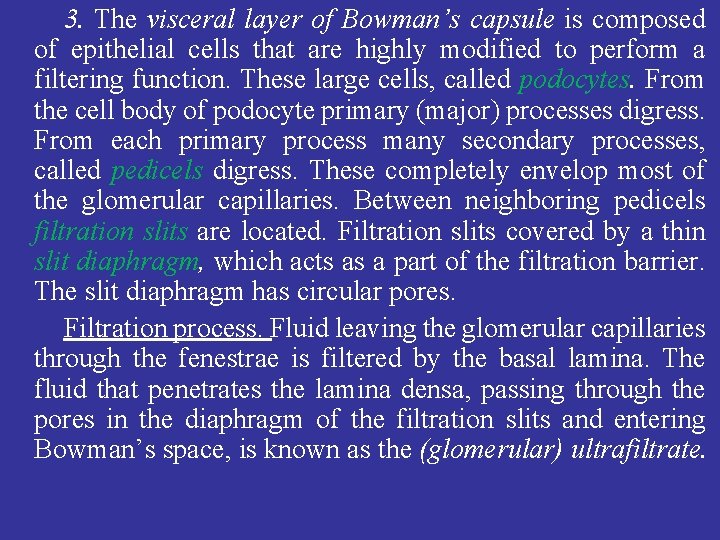
3. The visceral layer of Bowman’s capsule is composed of epithelial cells that are highly modified to perform a filtering function. These large cells, called podocytes. From the cell body of podocyte primary (major) processes digress. From each primary process many secondary processes, called pedicels digress. These completely envelop most of the glomerular capillaries. Between neighboring pedicels filtration slits are located. Filtration slits covered by a thin slit diaphragm, which acts as a part of the filtration barrier. The slit diaphragm has circular pores. Filtration process. Fluid leaving the glomerular capillaries through the fenestrae is filtered by the basal lamina. The fluid that penetrates the lamina densa, passing through the pores in the diaphragm of the filtration slits and entering Bowman’s space, is known as the (glomerular) ultrafiltrate.
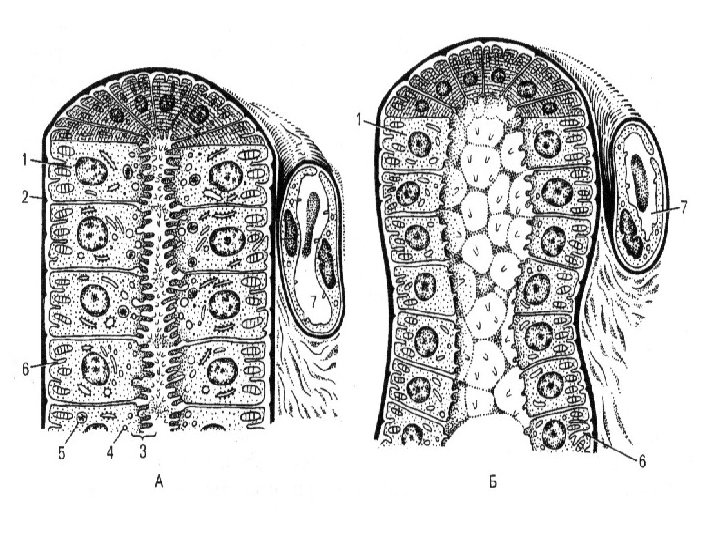
Because of the tripartite filtration barrier, cellular material and large macromolecules cannot leave the glomerulus; thus, the ultrafiltrate is similar to plasma. Structure of the renal tubules. Proximal tubule. Bowman’s space drains into the proximal tubule. In this part, called the neck of the proximal tubule, the simple squamous epithelium of the parietal layer of Bowman’s capsule joins the simple cuboidal epithelium of the tubule. The proximal tubule consists: a) the part convoluta; b) the part recta, which descends in the medulla to become continuous with Henle’s loop. The part recta is also called the descending thick limb of Henle’s loop. The height of the cells varies with functional state from a cuboidal to a high cuboidal epithelium. Cells have microvilli on the apical part. Mitochondria, Golgi apparatus, and other organelles are present in these cells.
Function: In the proximal tubule modification of the ultrafiltrate begins. Materials resorbed from the tubular lumen enter the tubular epithelial cells, from where they are excreted into the interstitial connective tissue. Here, the resorbed substances gain entrance to the rich capillary network and thus are returned to the body via the bloodstream. Most resorption of materials from the ultrafiltrate occurs in the proximal tubule. Normally, of 100% of protein, amino acids, glucose, and creatine, almost of 100% of bicarbonate ions, 80% of water, sodium, and chloride ions are resorbed. Each day, 140 g of glucose, 430 g of Na, 500 g of Cl, 300 g of bicarbonate, 18 g of K ions, and 140 l of water are conserved by the proximal tubules of the kidney.
Thin limbs of Henle’s loop. The part recta of the proximal tubule continues as the thin limb of Henle’s loop. In the juxtamedullary nephrons of the thin tubule form a hairpinlike loop that extends deep into the medulla. The region of the loop continuous with the part recta of the proximal tubule is called the descending thin limb (of Henle’s loop); the hairpin-like bend is Henle’s loop; and the region that connect Henle’s loop to the part recta of the distal tubule is known as the ascending thin limb (of Henle’s loop). The thin tubule is composed of squamous epithelial cells. Functions: - The descending thin limb is highly permeable to water and permeable to sodium, chloride, and other ions. - The ascending thin limb is impermeable to water, permeable to salts; sodium and chloride leave tubule to enter renal interstitium and after that into the blood capillaries.
Distal tubule. The distal tubule is subdivided into the part recta which, as the continuation of the ascending thin limb of Henle’s loop, is also known as the ascending thick limb of Henle’s loop and the part convoluta (distal convoluted tubule). The ascending thick limb of Henle’s loop ascends through the medulla to the cortex. The thick ascending limb is composed of simple cuboidal epithelium. Function. Impermeable to water; sodium and chloride leave tubule to enter renal intestitium. Distal convoluted tubules are short, composed of simple cuboidal epithelium. Function. Impermeable to water; in response to hormone aldosterone, these cells by resorbing sodium and chloride from the lumen of the tubule into the renal intestitium.
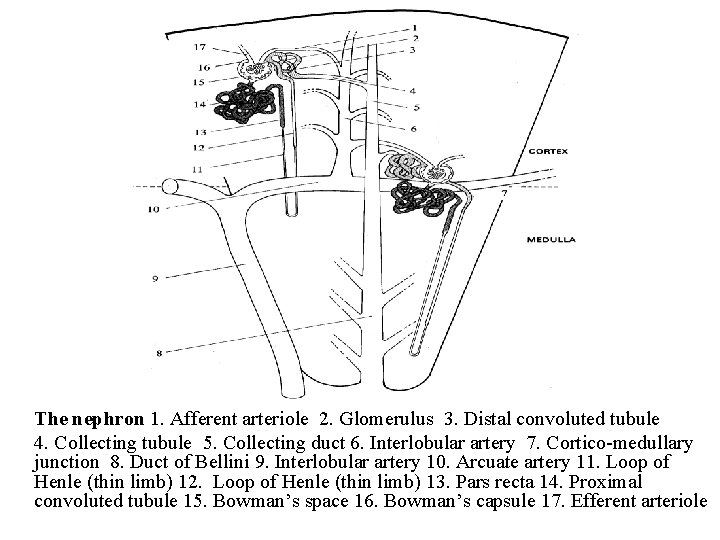
The nephron 1. Afferent arteriole 2. Glomerulus 3. Distal convoluted tubule 4. Collecting tubule 5. Collecting duct 6. Interlobular artery 7. Cortico-medullary junction 8. Duct of Bellini 9. Interlobular artery 10. Arcuate artery 11. Loop of Henle (thin limb) 12. Loop of Henle (thin limb) 13. Pars recta 14. Proximal convoluted tubule 15. Bowman’s space 16. Bowman’s capsule 17. Efferent arteriole
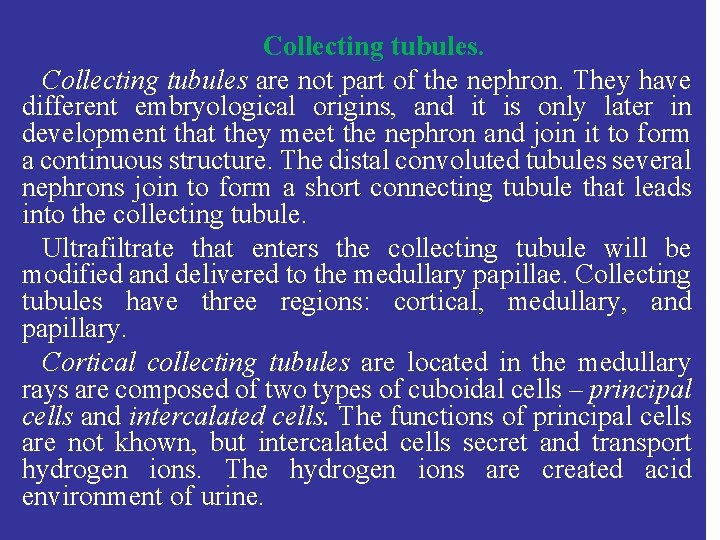
Collecting tubules are not part of the nephron. They have different embryological origins, and it is only later in development that they meet the nephron and join it to form a continuous structure. The distal convoluted tubules several nephrons join to form a short connecting tubule that leads into the collecting tubule. Ultrafiltrate that enters the collecting tubule will be modified and delivered to the medullary papillae. Collecting tubules have three regions: cortical, medullary, and papillary. Cortical collecting tubules are located in the medullary rays are composed of two types of cuboidal cells – principal cells and intercalated cells. The functions of principal cells are not khown, but intercalated cells secret and transport hydrogen ions. The hydrogen ions are created acid environment of urine.
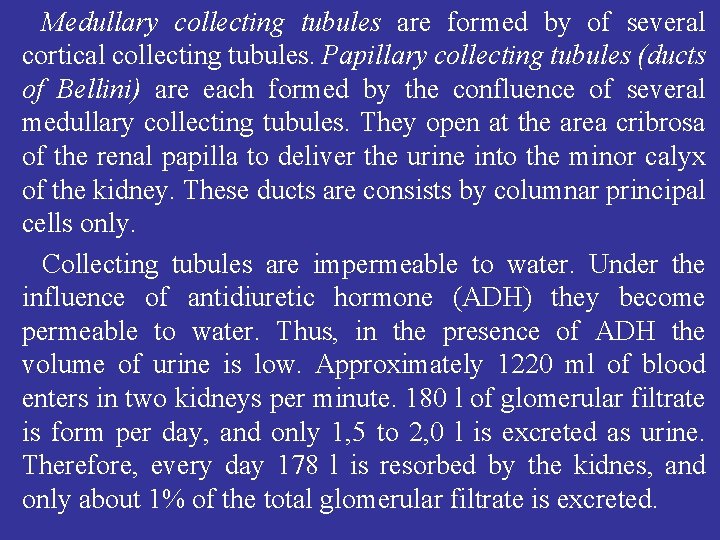
Medullary collecting tubules are formed by of several cortical collecting tubules. Papillary collecting tubules (ducts of Bellini) are each formed by the confluence of several medullary collecting tubules. They open at the area cribrosa of the renal papilla to deliver the urine into the minor calyx of the kidney. These ducts are consists by columnar principal cells only. Collecting tubules are impermeable to water. Under the influence of antidiuretic hormone (ADH) they become permeable to water. Thus, in the presence of ADH the volume of urine is low. Approximately 1220 ml of blood enters in two kidneys per minute. 180 l of glomerular filtrate is form per day, and only 1, 5 to 2, 0 l is excreted as urine. Therefore, every day 178 l is resorbed by the kidnes, and only about 1% of the total glomerular filtrate is excreted.
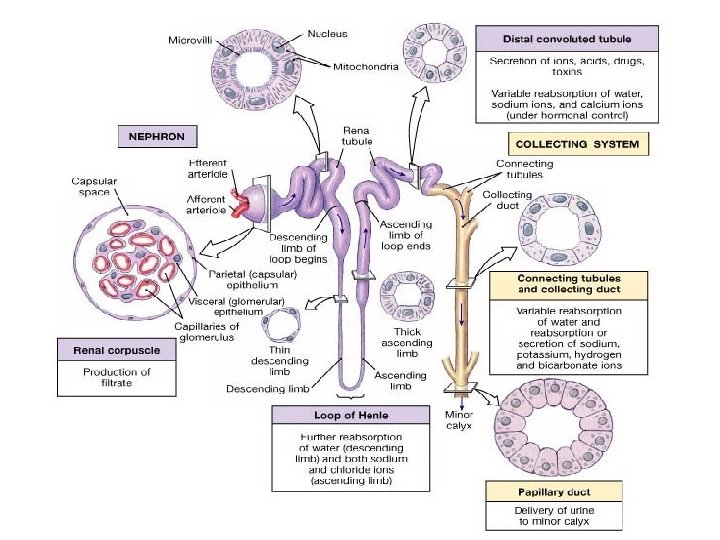
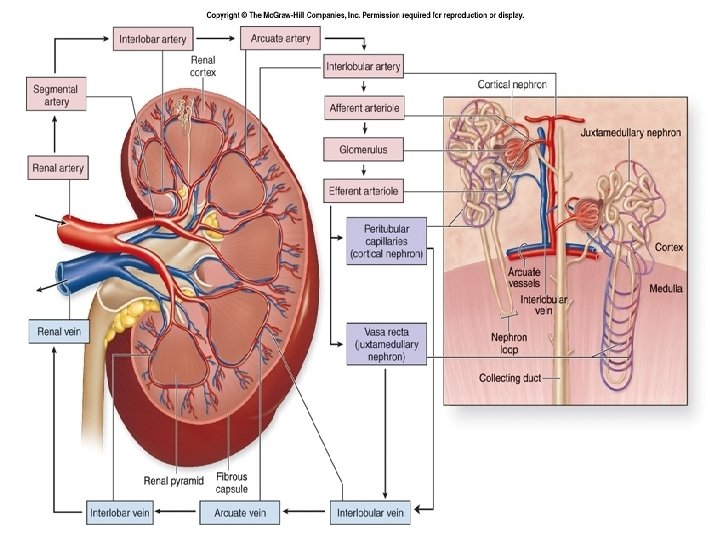
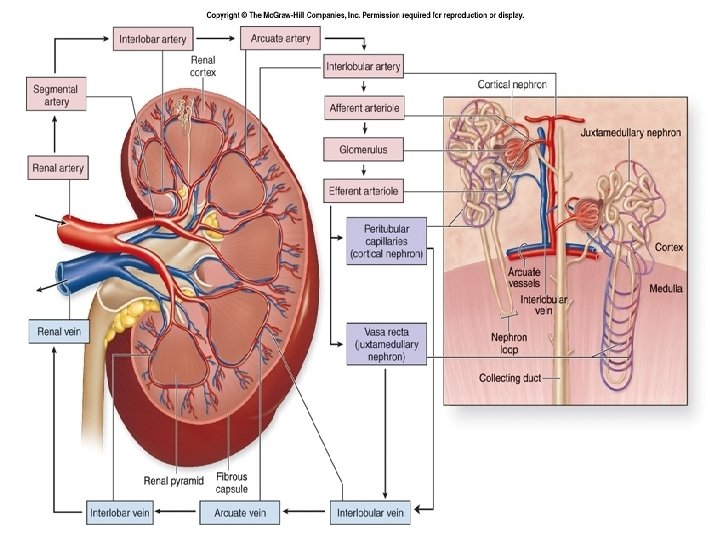
Blood supply of the Kidney. The kidney receives blood supply via the renal artery. The renal artery divides into several segmental arteries. The first branches of the segmental arteries are called lobar arteries. These form inter-lobar arteries, which between the renal pyramids in the renal columns are located. At the bases of the renal pyramids, the inter-lobar arteries forms arches, which between the renalmedulla and cortex are located. They are named arcuate arteries. Divisions of the arcuate arteries produce a series of interlobular arteries, which enter the renal cortex between neighboring medulary rays and give off branches called afferent glomerular arterioles. Each nephron receives one afferent arteriole, which divides into a ball-shaped capillary network called glomerulus. The glomerular capillaries then reunite to form an efferent glomerular arteriole that carries blood out of the glomerulus.
Glomerular capillaries are unique among capillaries in the body because they are positioned between to arterioles and they play an important role in urine formation. The efferent arterioles divide to form the peritubular capillary network, which surround tubular parts of the nephron in the renal cortex. Extending from some efferent arterioles are long loop-shaped capillaries called vasa recta, that supply tubular part of the nephron in the renal medulla. The peritubular capillaries reunite to form peritubular venules and then interlobular veins, which also receive blood from vasa recta. Then the blood drains through the arcuate veins to the interlobar veins are located between the renal pyramids. In the hilum kidney interlobar veins to form the renal vein, which delivers the blood to the inferior vena cava.