Chapter 26 The Urinary System The Urinary System
- Slides: 60
Chapter 26 The Urinary System
The Urinary System § The urinary systems consists of the kidneys, ureters, bladder, and urethra, along with its associated nerves and blood vessels. § The system maintains homeostasis by: l Regulating blood volume, pressure, p. H, and concentration (osmolarity) of electrolytes (Na+, K+, Ca 2+, Cl-, HPO 4 -3, Mg 2+, HCO 3 -) l Reabsorbing glucose and excreting wastes l Releasing certain hormones like renin and EPO Copyright © John Wiley & Sons, Inc. All rights reserved.
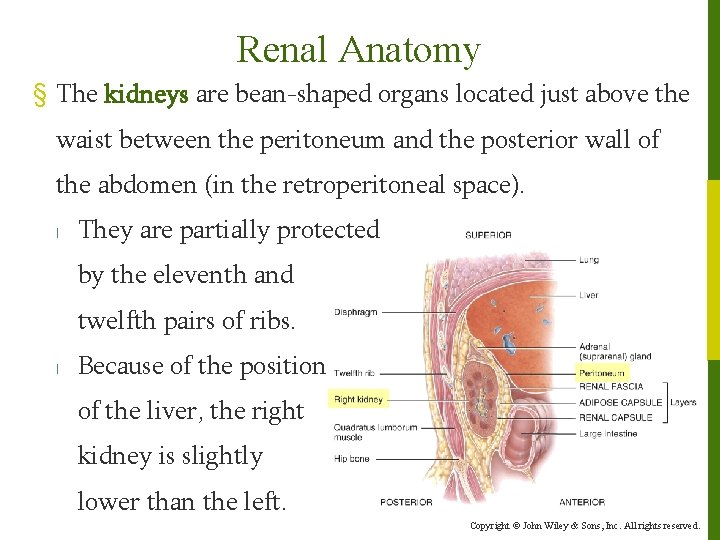
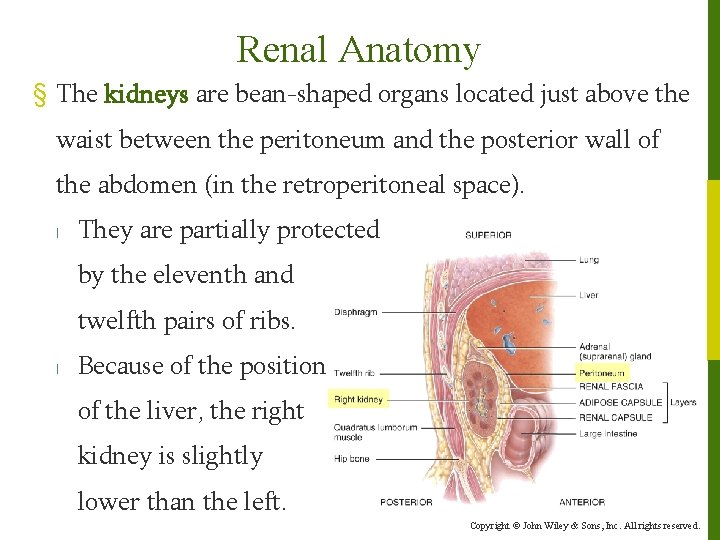
Renal Anatomy § The kidneys are bean-shaped organs located just above the waist between the peritoneum and the posterior wall of the abdomen (in the retroperitoneal space). l They are partially protected by the eleventh and twelfth pairs of ribs. l Because of the position of the liver, the right kidney is slightly lower than the left. Copyright © John Wiley & Sons, Inc. All rights reserved.
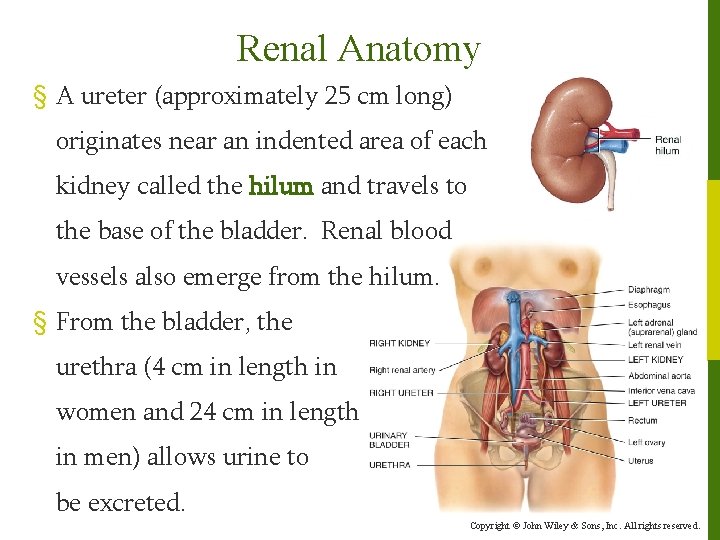
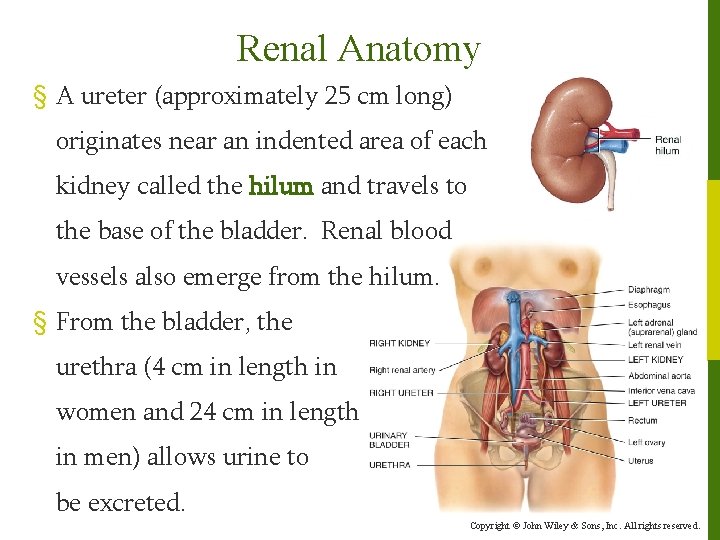
Renal Anatomy § A ureter (approximately 25 cm long) originates near an indented area of each kidney called the hilum and travels to the base of the bladder. Renal blood vessels also emerge from the hilum. § From the bladder, the urethra (4 cm in length in women and 24 cm in length in men) allows urine to be excreted. Copyright © John Wiley & Sons, Inc. All rights reserved.
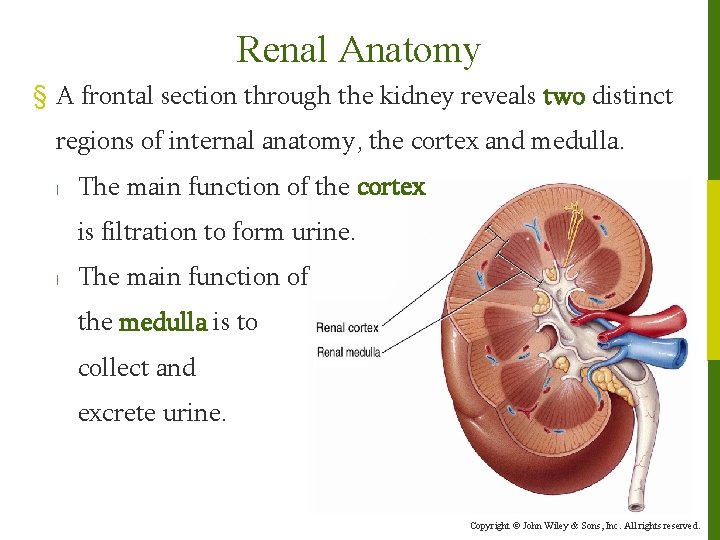
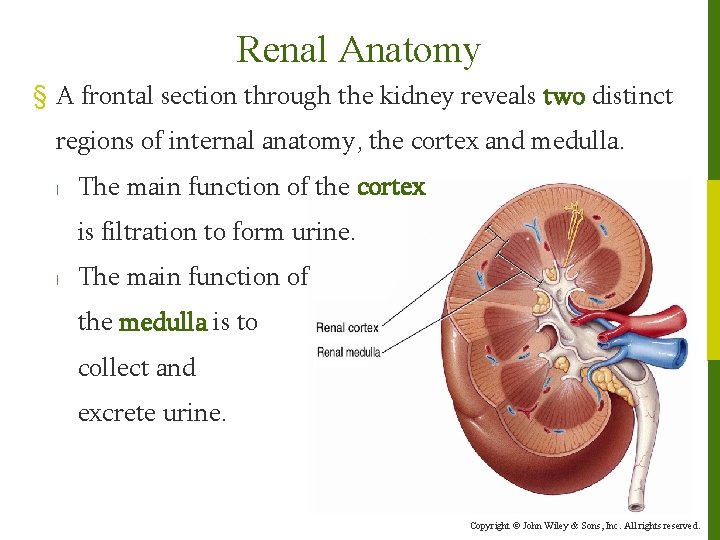
Renal Anatomy § A frontal section through the kidney reveals two distinct regions of internal anatomy, the cortex and medulla. l The main function of the cortex is filtration to form urine. l The main function of the medulla is to collect and excrete urine. Copyright © John Wiley & Sons, Inc. All rights reserved.
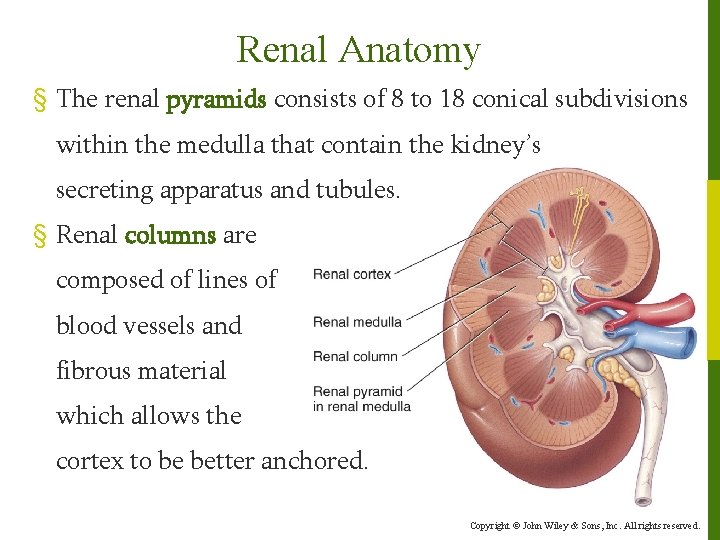
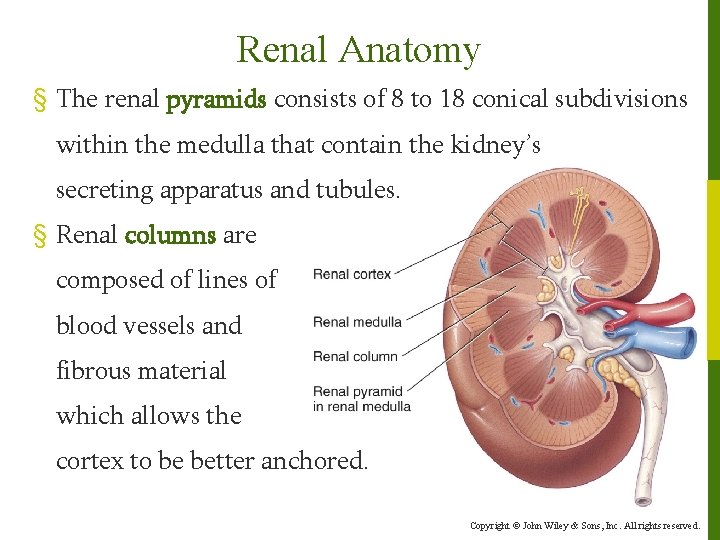
Renal Anatomy § The renal pyramids consists of 8 to 18 conical subdivisions within the medulla that contain the kidney’s secreting apparatus and tubules. § Renal columns are composed of lines of blood vessels and fibrous material which allows the cortex to be better anchored. Copyright © John Wiley & Sons, Inc. All rights reserved.
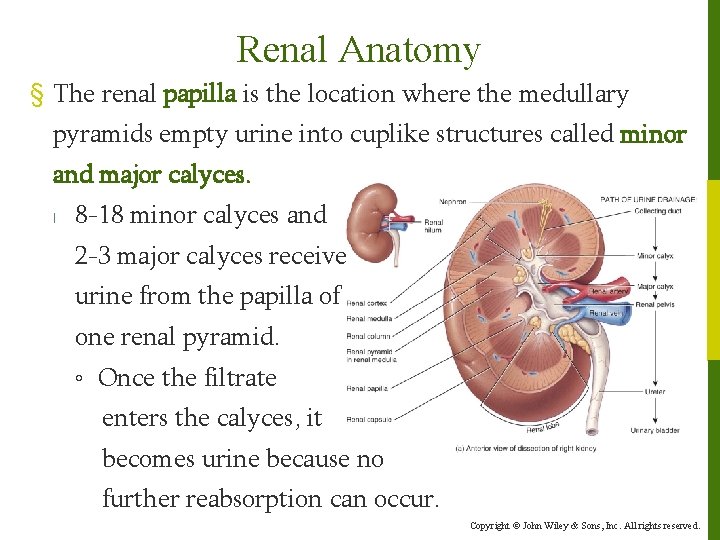
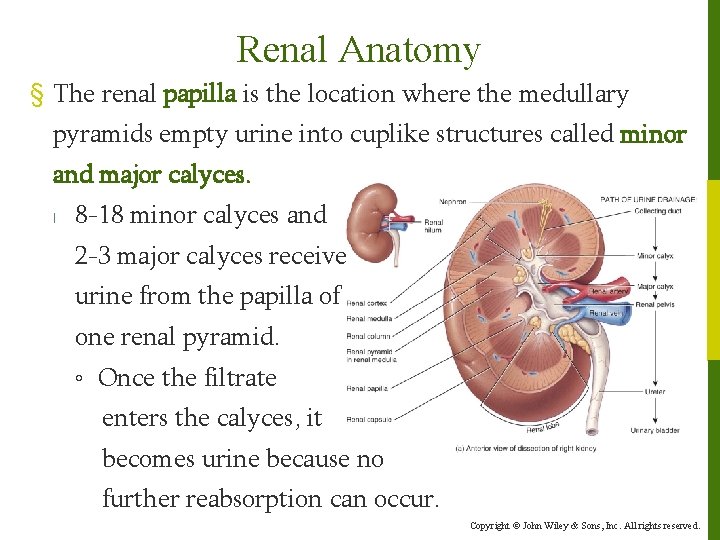
Renal Anatomy § The renal papilla is the location where the medullary pyramids empty urine into cuplike structures called minor and major calyces. l 8 -18 minor calyces and 2 -3 major calyces receive urine from the papilla of one renal pyramid. ◦ Once the filtrate enters the calyces, it becomes urine because no further reabsorption can occur. Copyright © John Wiley & Sons, Inc. All rights reserved.
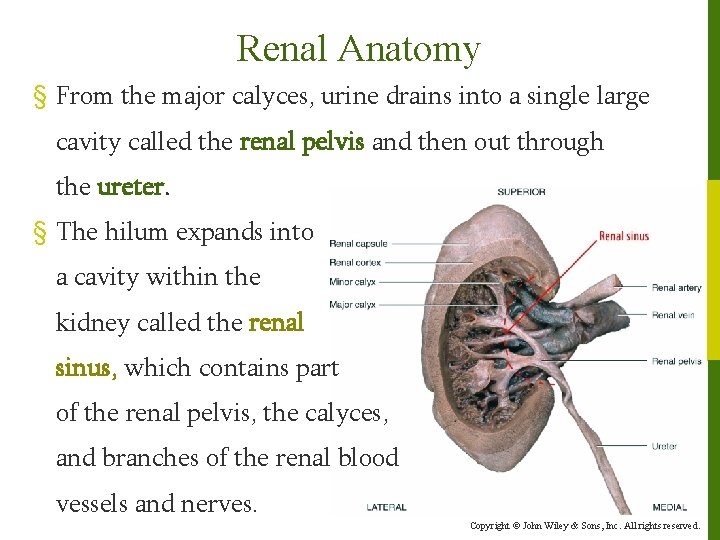
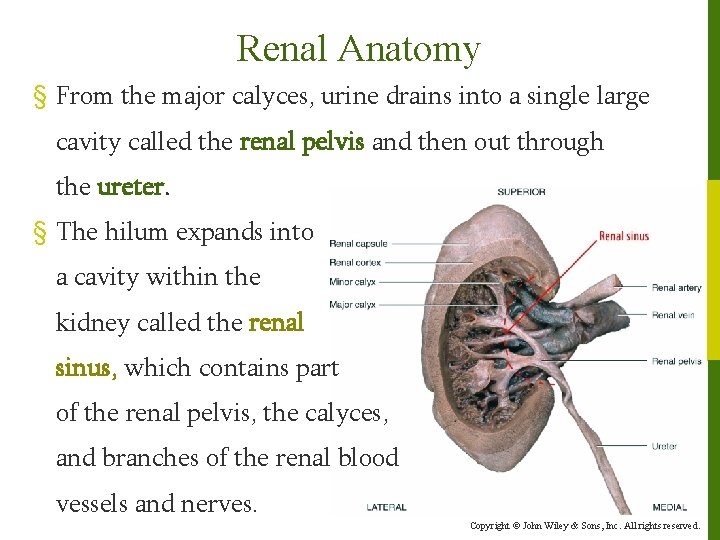
Renal Anatomy § From the major calyces, urine drains into a single large cavity called the renal pelvis and then out through the ureter. § The hilum expands into a cavity within the kidney called the renal sinus, which contains part of the renal pelvis, the calyces, and branches of the renal blood vessels and nerves. Copyright © John Wiley & Sons, Inc. All rights reserved.
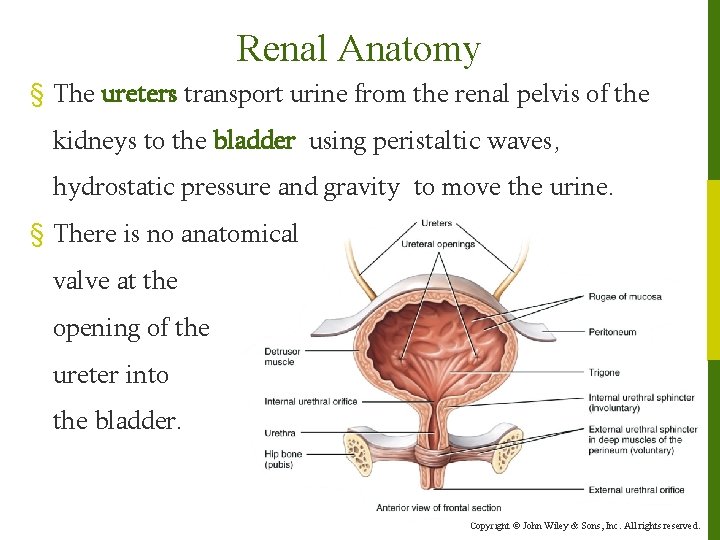
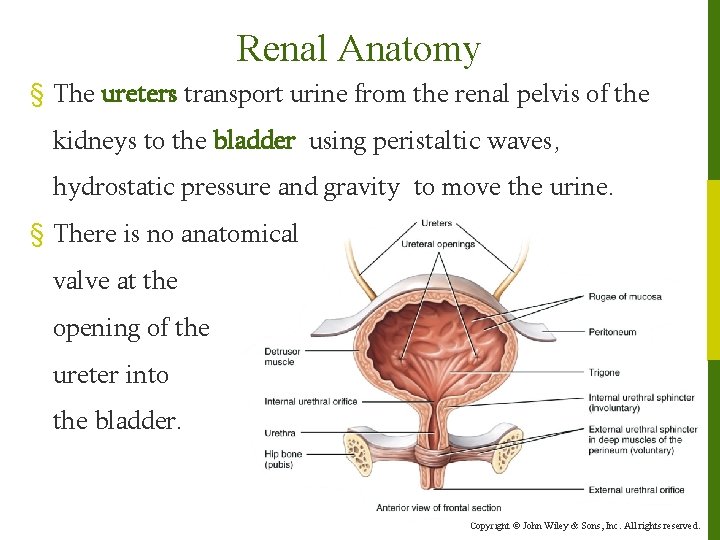
Renal Anatomy § The ureters transport urine from the renal pelvis of the kidneys to the bladder using peristaltic waves, hydrostatic pressure and gravity to move the urine. § There is no anatomical valve at the opening of the ureter into the bladder. Copyright © John Wiley & Sons, Inc. All rights reserved.
Renal Anatomy § The urinary bladder is a hollow, distensible muscular organ with a capacity that averages 700 -800 m. L. l The act of emptying the bladder is called micturition or urination and requires a combination of voluntary and involuntary muscle contractions. ◦ When volume increases, stretch receptors send signals to a micturition center in the spinal cord triggering a spinal reflex – the micturition reflex. ◦ In early childhood, we learn to initiate and stop the reflex voluntarily. Copyright © John Wiley & Sons, Inc. All rights reserved.
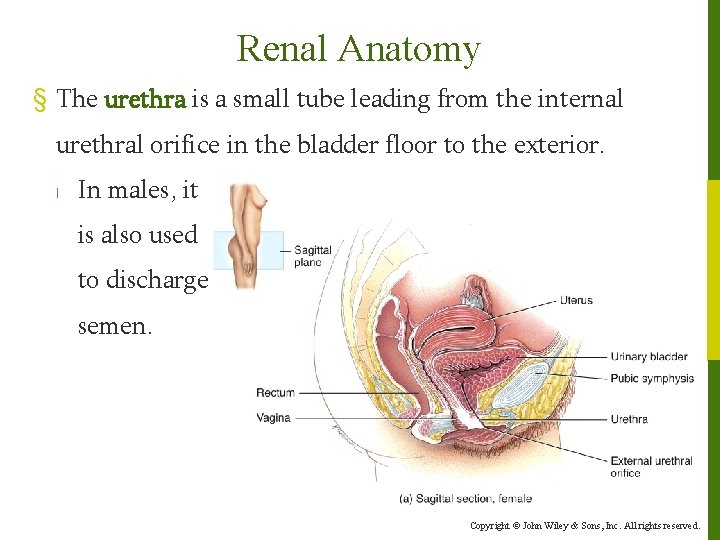
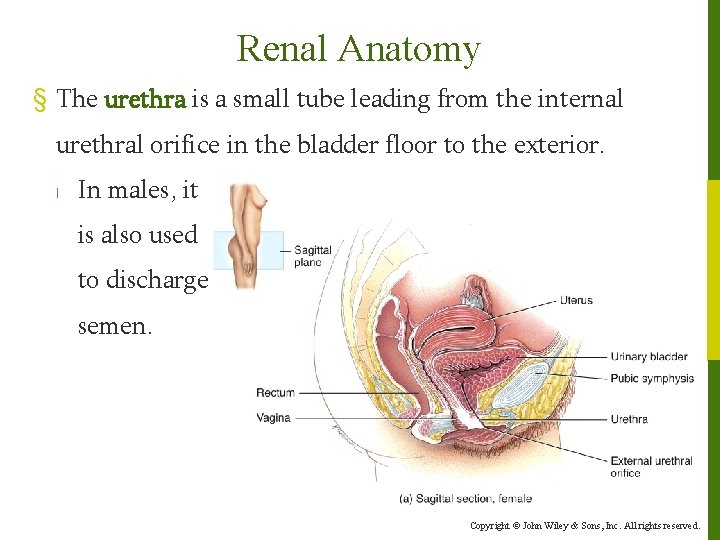
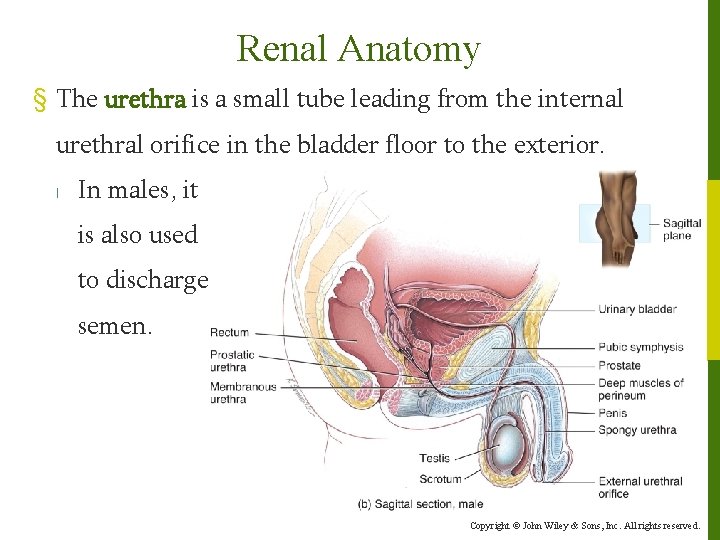
Renal Anatomy § The urethra is a small tube leading from the internal urethral orifice in the bladder floor to the exterior. l In males, it is also used to discharge semen. Copyright © John Wiley & Sons, Inc. All rights reserved.
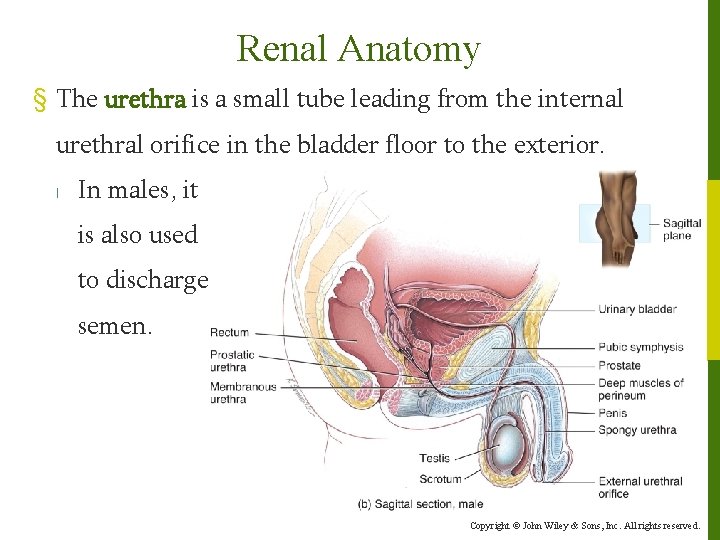
Renal Anatomy § The urethra is a small tube leading from the internal urethral orifice in the bladder floor to the exterior. l In males, it is also used to discharge semen. Copyright © John Wiley & Sons, Inc. All rights reserved.
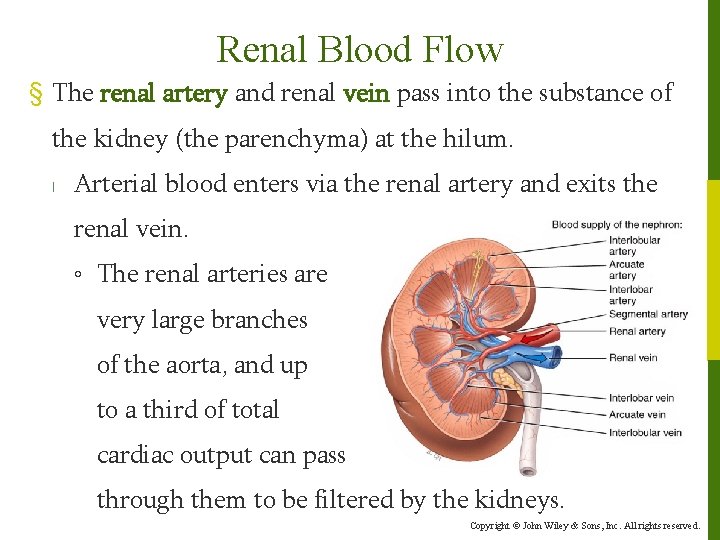
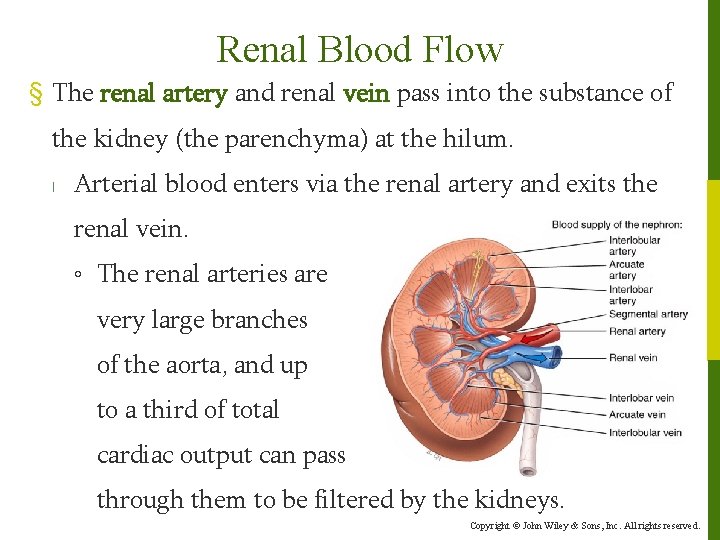
Renal Blood Flow § The renal artery and renal vein pass into the substance of the kidney (the parenchyma) at the hilum. l Arterial blood enters via the renal artery and exits the renal vein. ◦ The renal arteries are very large branches of the aorta, and up to a third of total cardiac output can pass through them to be filtered by the kidneys. Copyright © John Wiley & Sons, Inc. All rights reserved.
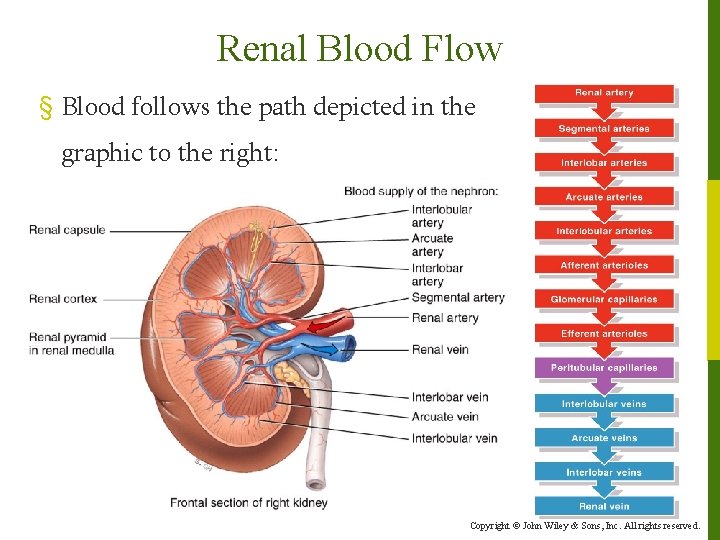
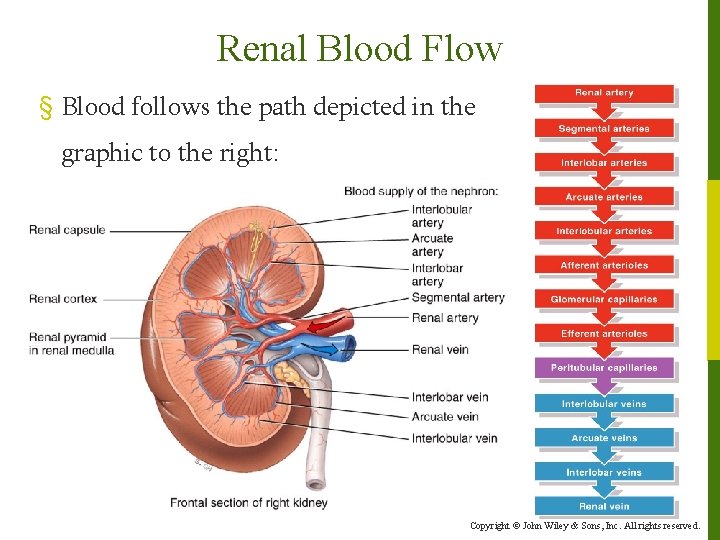
Renal Blood Flow § Blood follows the path depicted in the graphic to the right: Copyright © John Wiley & Sons, Inc. All rights reserved.
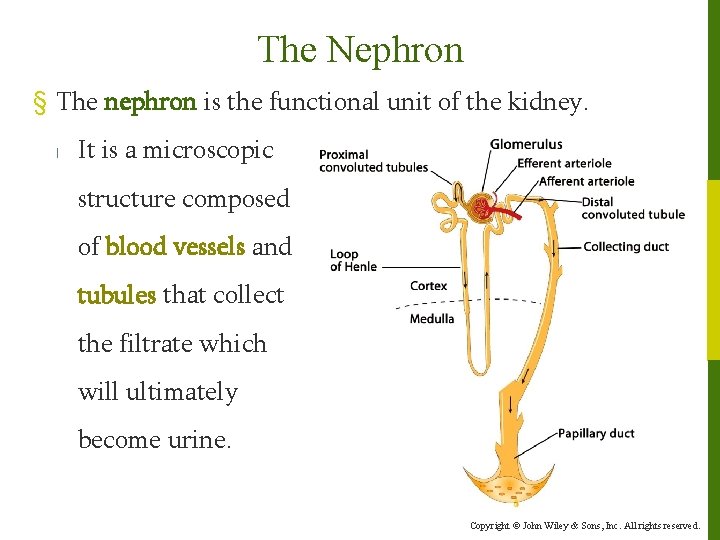
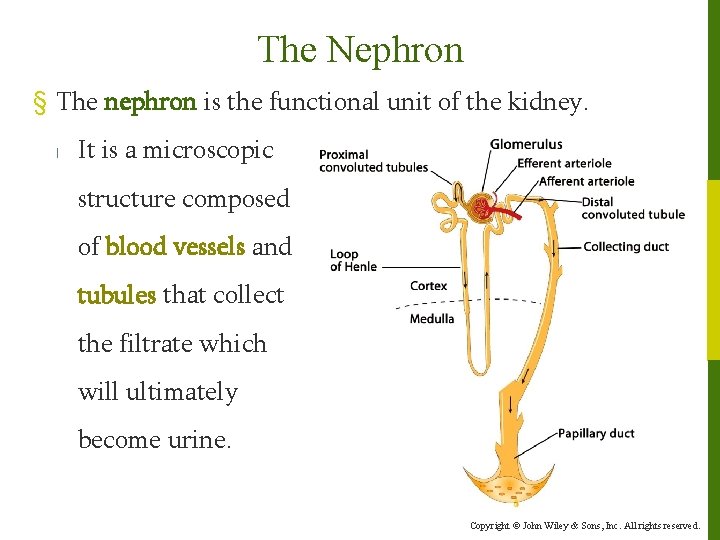
The Nephron § The nephron is the functional unit of the kidney. l It is a microscopic structure composed of blood vessels and tubules that collect the filtrate which will ultimately become urine. Copyright © John Wiley & Sons, Inc. All rights reserved.
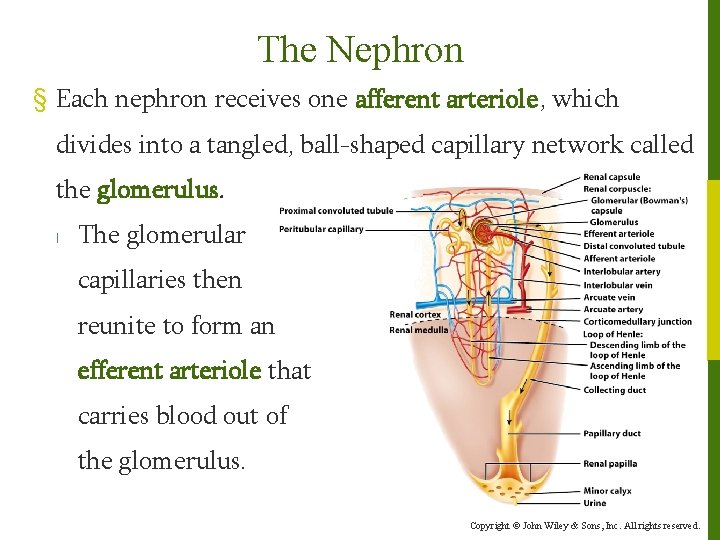
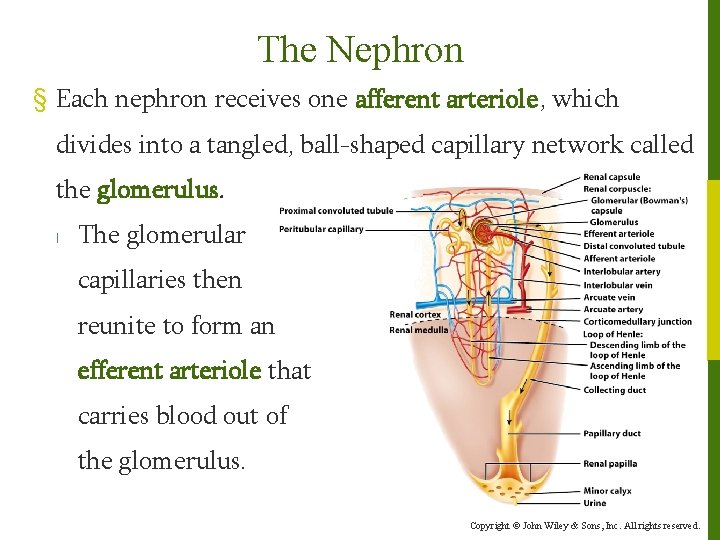
The Nephron § Each nephron receives one afferent arteriole, which divides into a tangled, ball-shaped capillary network called the glomerulus. l The glomerular capillaries then reunite to form an efferent arteriole that carries blood out of the glomerulus. Copyright © John Wiley & Sons, Inc. All rights reserved.
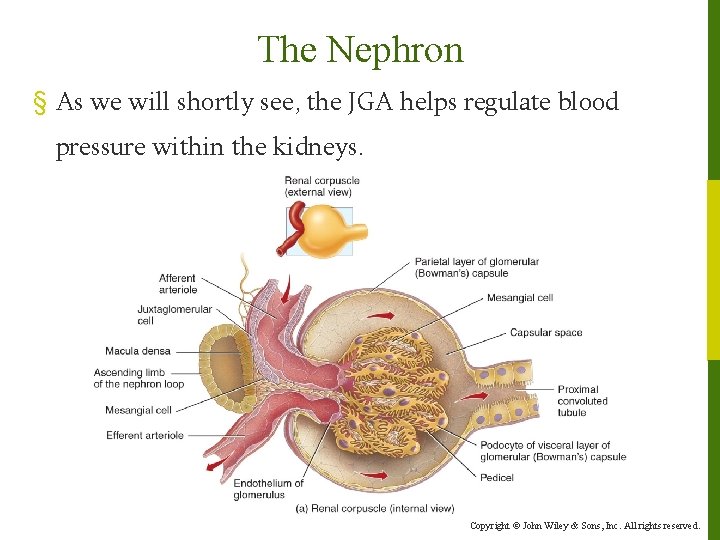
The Nephron § Glomerular capillaries are unique among capillaries in the body because they are positioned between two arterioles, rather than between an arteriole and a venule. l There are venules in the kidney, but they come later. § The Renal Corpuscle consists of two structures: l The glomerular capillaries l The glomerular capsule (Bowman’s capsule) – a doublewalled epithelial cup that surrounds the glomerular capillaries. Copyright © John Wiley & Sons, Inc. All rights reserved.
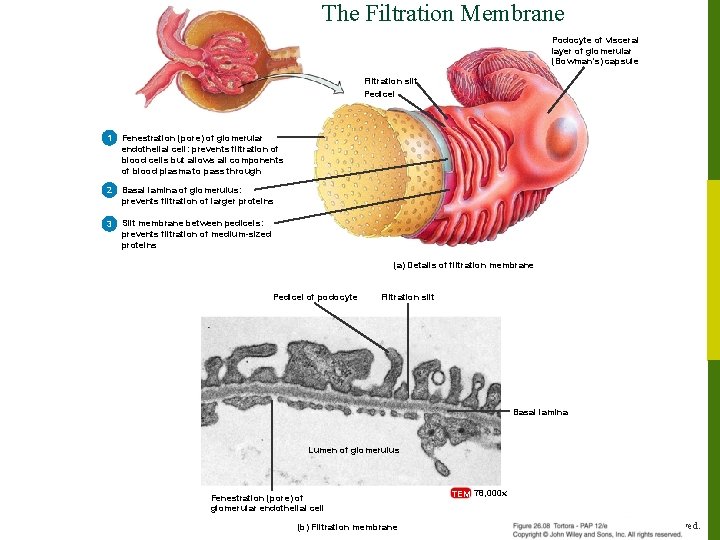
The Nephron § Bowman’s capsule consists of visceral and parietal layers. l The visceral layer is made of modified simple squamous epithelial cells called podocytes. The many foot-like projections of these cells (pedicels) wrap around the single layer of endothelial cells of the glomerular capillaries and form the inner wall of the capsule. l The parietal layer of the glomerular capsule is a simple squamous epithelium and forms the outer wall of the capsule. Copyright © John Wiley & Sons, Inc. All rights reserved.
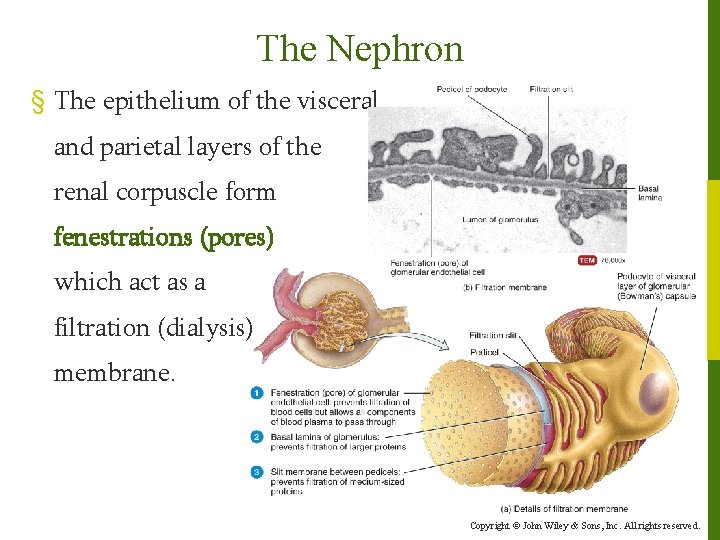
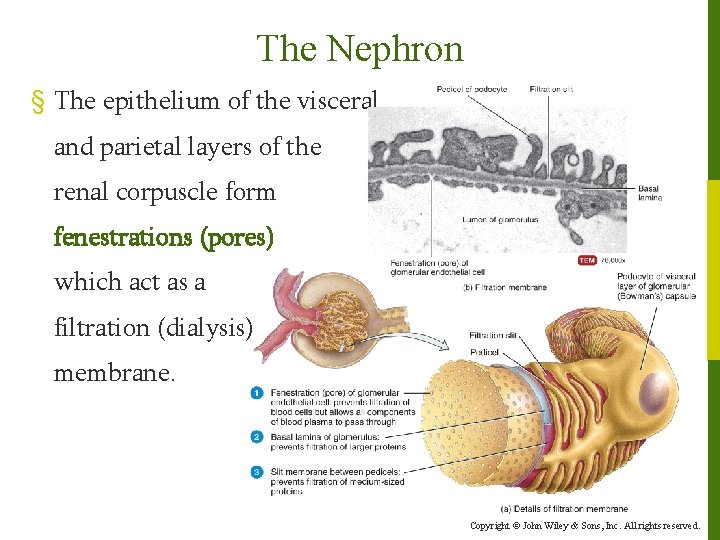
The Nephron § The epithelium of the visceral and parietal layers of the renal corpuscle form fenestrations (pores) which act as a filtration (dialysis) membrane. Copyright © John Wiley & Sons, Inc. All rights reserved.
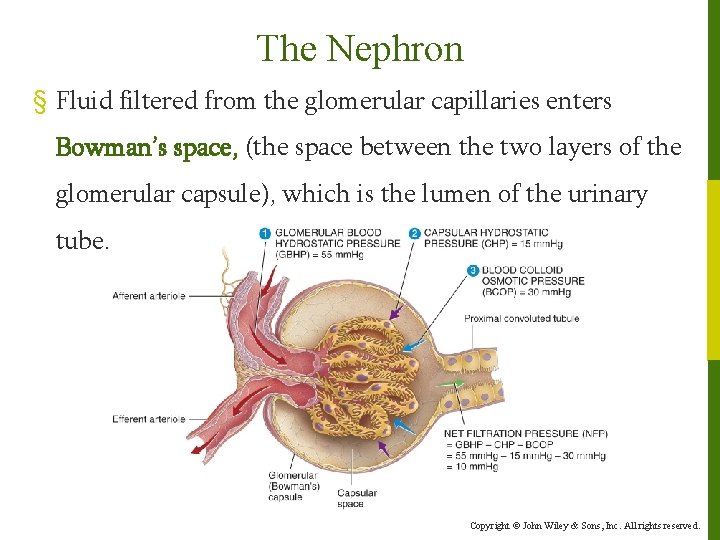
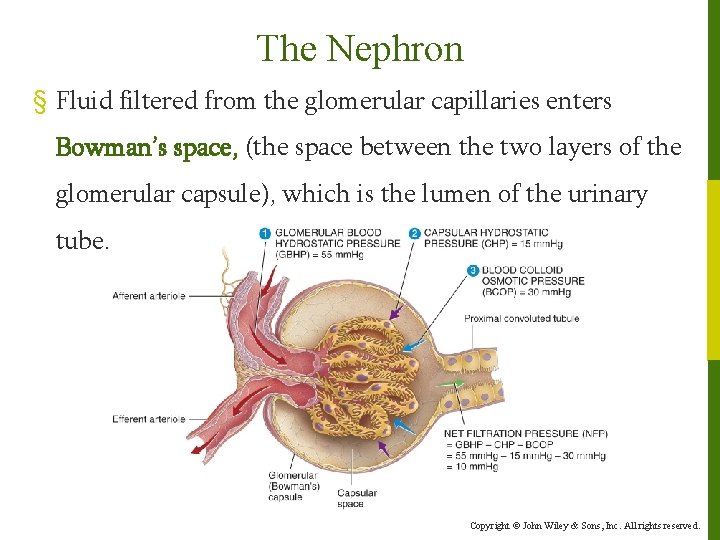
The Nephron § Fluid filtered from the glomerular capillaries enters Bowman’s space, (the space between the two layers of the glomerular capsule), which is the lumen of the urinary tube. Copyright © John Wiley & Sons, Inc. All rights reserved.
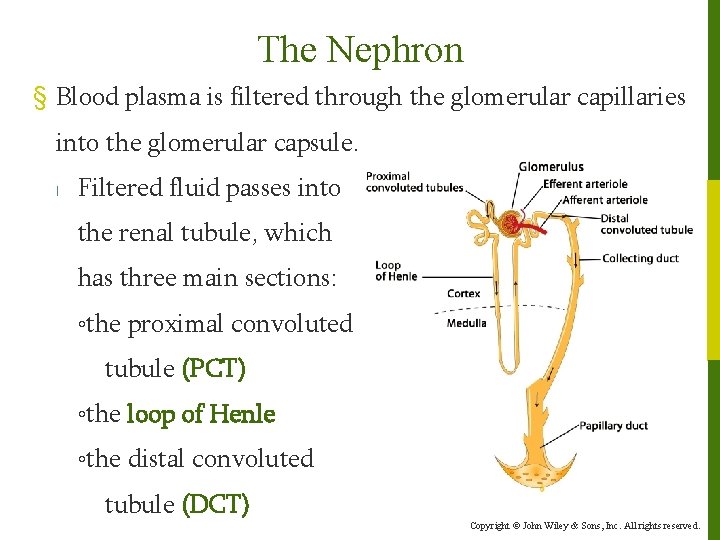
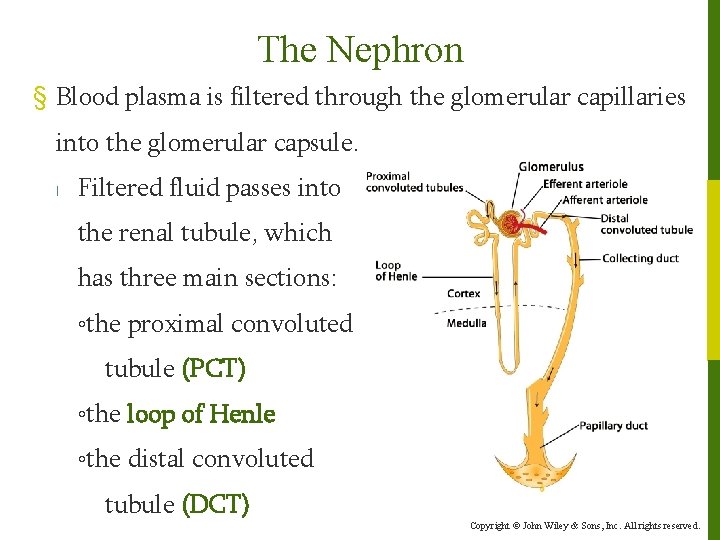
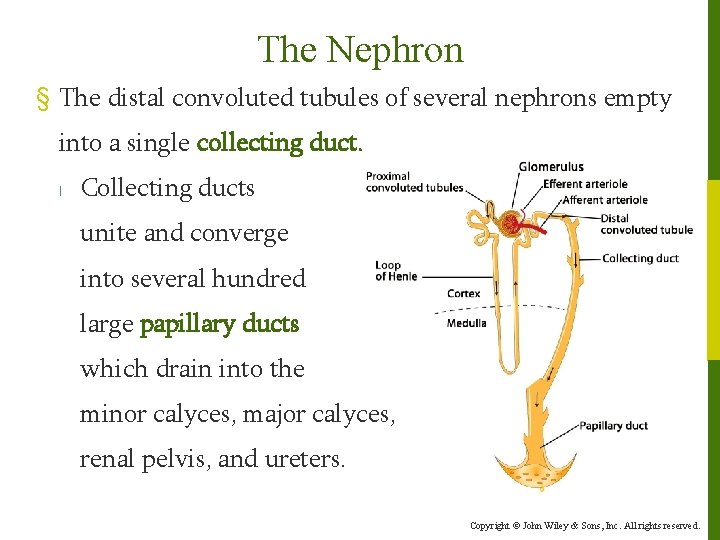
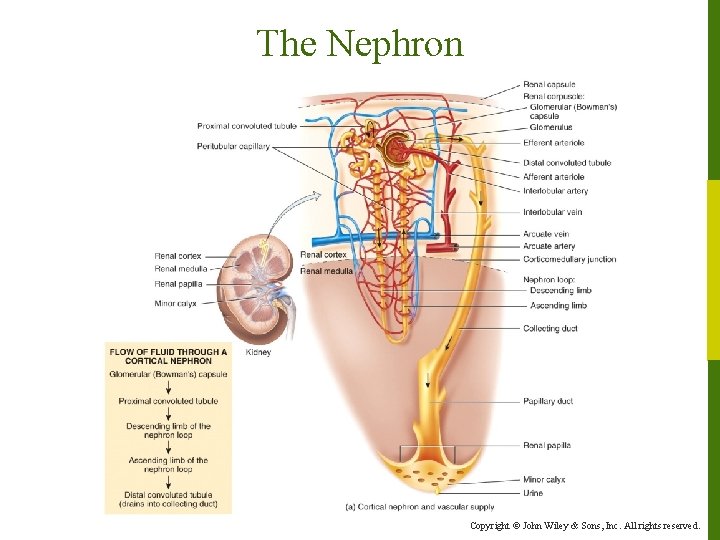
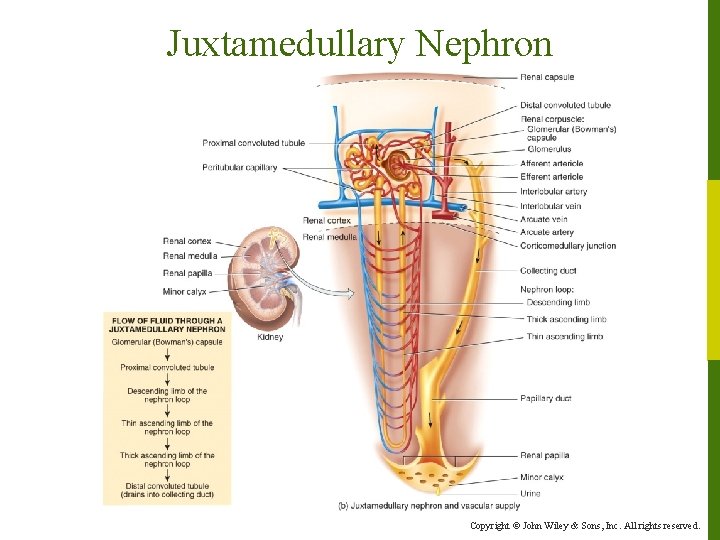
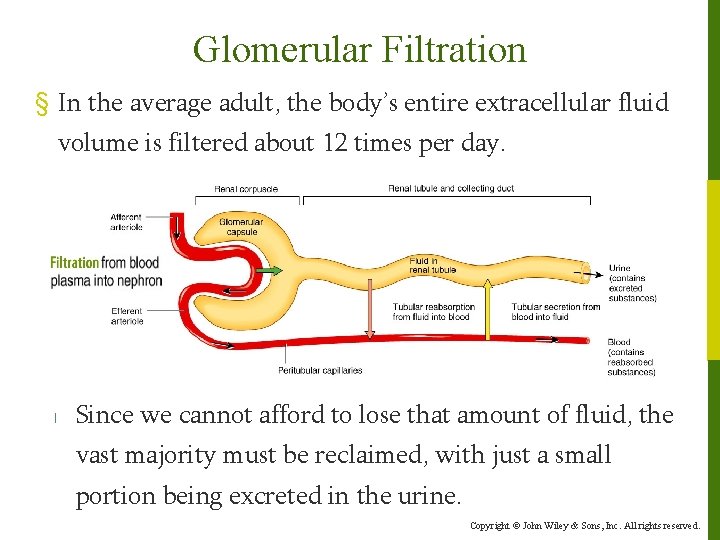
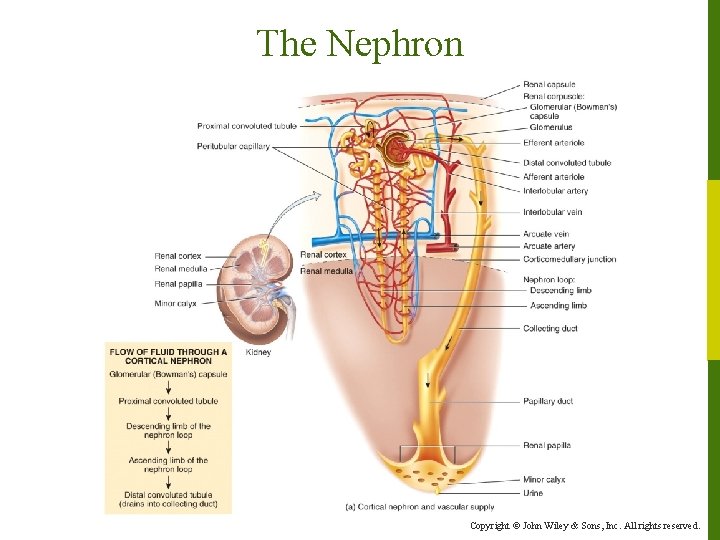
The Nephron § Blood plasma is filtered through the glomerular capillaries into the glomerular capsule. l Filtered fluid passes into the renal tubule, which has three main sections: ◦the proximal convoluted tubule (PCT) ◦the loop of Henle ◦the distal convoluted tubule (DCT) Copyright © John Wiley & Sons, Inc. All rights reserved.
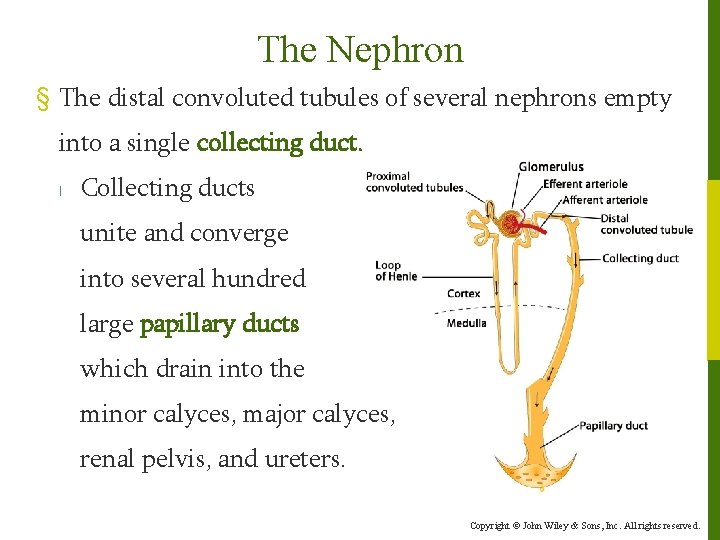
The Nephron § The distal convoluted tubules of several nephrons empty into a single collecting duct. l Collecting ducts unite and converge into several hundred large papillary ducts which drain into the minor calyces, major calyces, renal pelvis, and ureters. Copyright © John Wiley & Sons, Inc. All rights reserved.
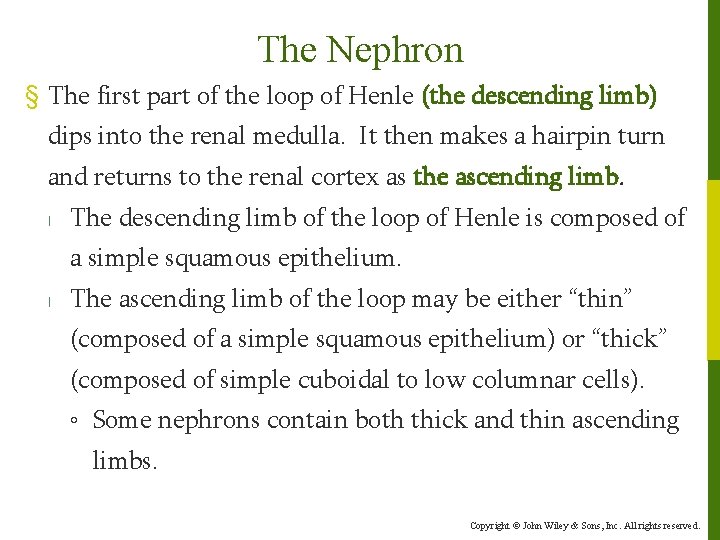
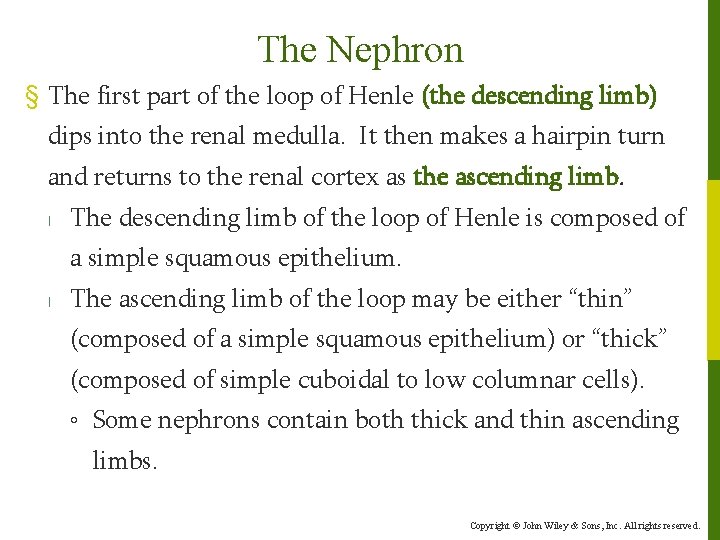
The Nephron § The first part of the loop of Henle (the descending limb) dips into the renal medulla. It then makes a hairpin turn and returns to the renal cortex as the ascending limb. l The descending limb of the loop of Henle is composed of a simple squamous epithelium. l The ascending limb of the loop may be either “thin” (composed of a simple squamous epithelium) or “thick” (composed of simple cuboidal to low columnar cells). ◦ Some nephrons contain both thick and thin ascending limbs. Copyright © John Wiley & Sons, Inc. All rights reserved.
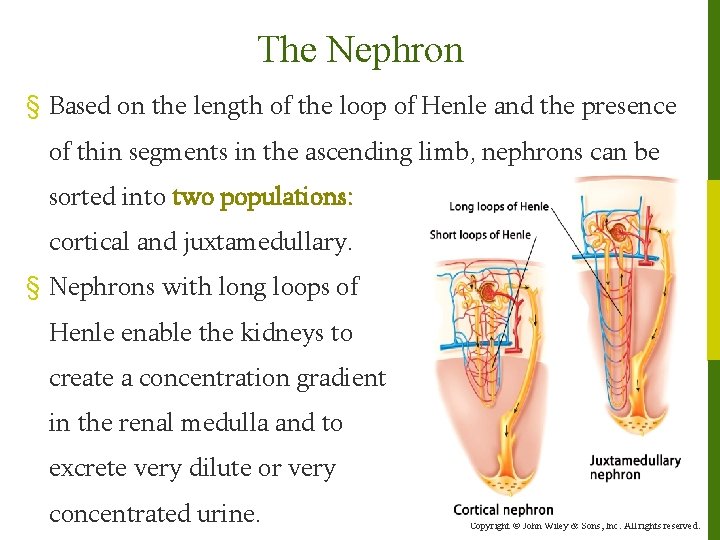
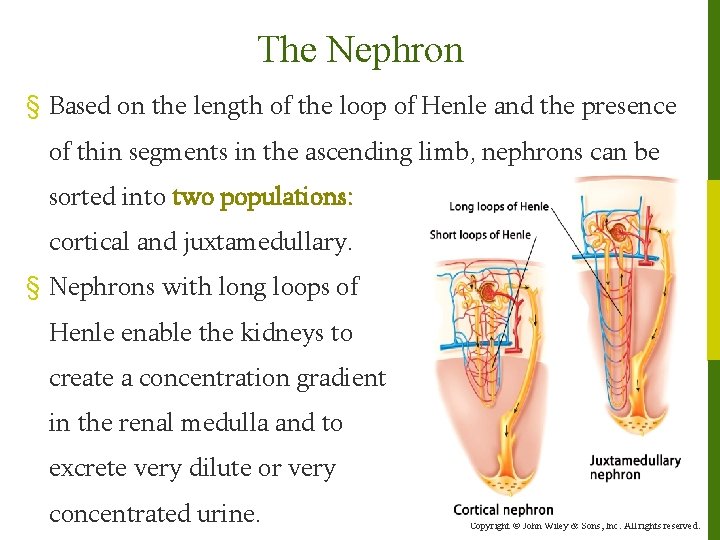
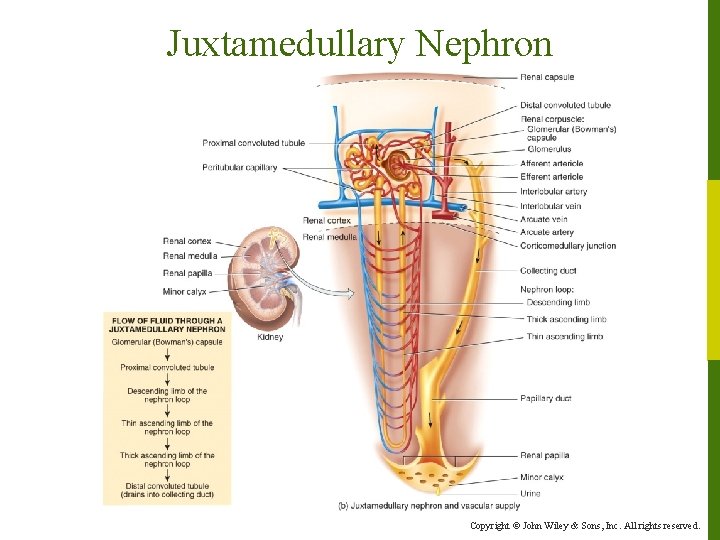
The Nephron § Based on the length of the loop of Henle and the presence of thin segments in the ascending limb, nephrons can be sorted into two populations: cortical and juxtamedullary. § Nephrons with long loops of Henle enable the kidneys to create a concentration gradient in the renal medulla and to excrete very dilute or very concentrated urine. Copyright © John Wiley & Sons, Inc. All rights reserved.
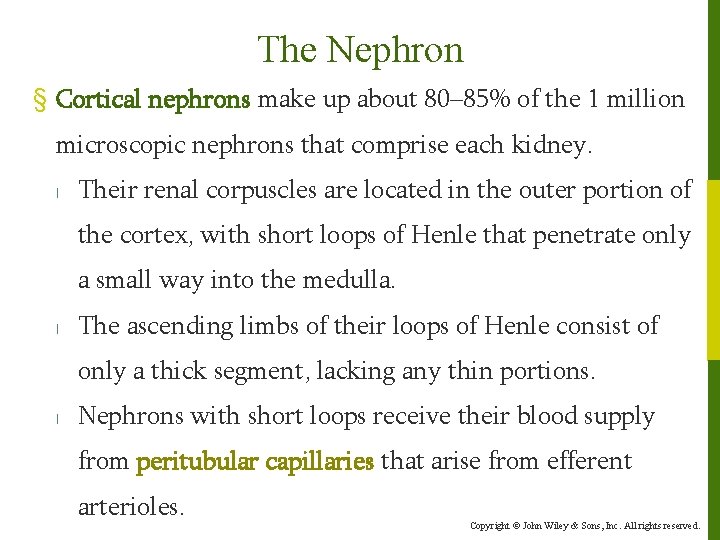
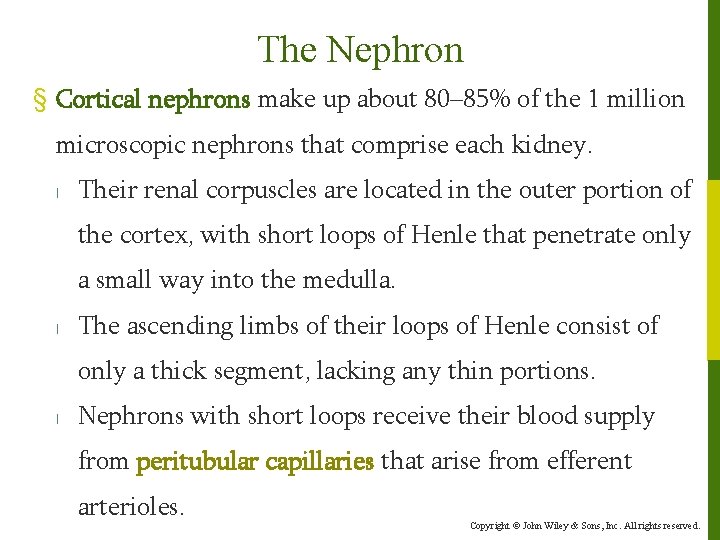
The Nephron § Cortical nephrons make up about 80– 85% of the 1 million microscopic nephrons that comprise each kidney. l Their renal corpuscles are located in the outer portion of the cortex, with short loops of Henle that penetrate only a small way into the medulla. l The ascending limbs of their loops of Henle consist of only a thick segment, lacking any thin portions. l Nephrons with short loops receive their blood supply from peritubular capillaries that arise from efferent arterioles. Copyright © John Wiley & Sons, Inc. All rights reserved.
The Nephron Copyright © John Wiley & Sons, Inc. All rights reserved.
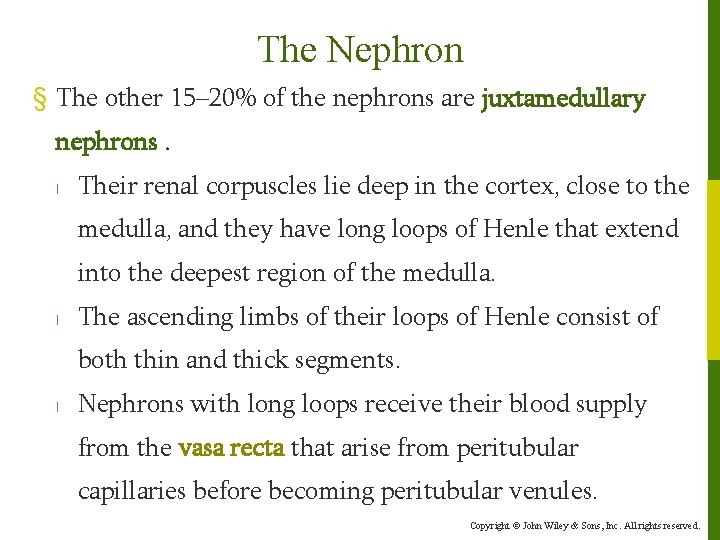
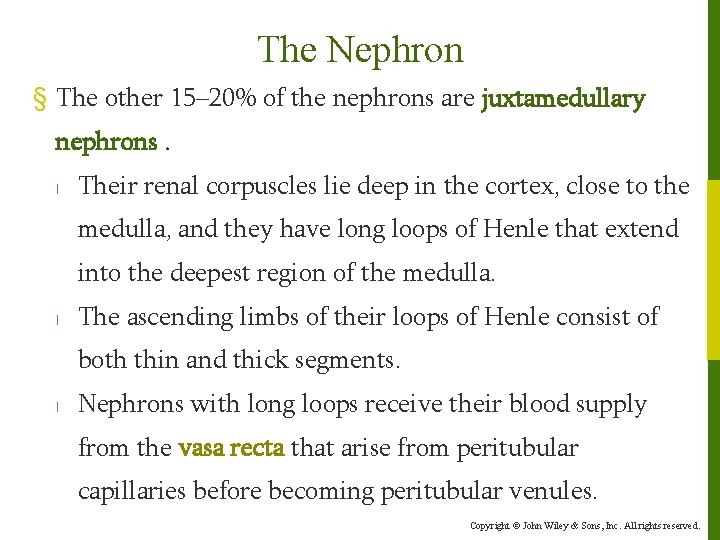
The Nephron § The other 15– 20% of the nephrons are juxtamedullary nephrons. l Their renal corpuscles lie deep in the cortex, close to the medulla, and they have long loops of Henle that extend into the deepest region of the medulla. l The ascending limbs of their loops of Henle consist of both thin and thick segments. l Nephrons with long loops receive their blood supply from the vasa recta that arise from peritubular capillaries before becoming peritubular venules. Copyright © John Wiley & Sons, Inc. All rights reserved.
Juxtamedullary Nephron Copyright © John Wiley & Sons, Inc. All rights reserved.
The Nephron § In each nephron, the final part of the ascending limb of the loop of Henle makes contact with the afferent arteriole serving that renal corpuscle. Because the columnar tubule cells in this region are crowded together, they are known as the macula densa. § Alongside the macula densa, the wall of the afferent arteriole contains modified smooth muscle fibers called juxtaglomerular (JG) cells. ◦ Together with the macula densa, they constitute the juxtaglomerular apparatus (JGA). Copyright © John Wiley & Sons, Inc. All rights reserved.
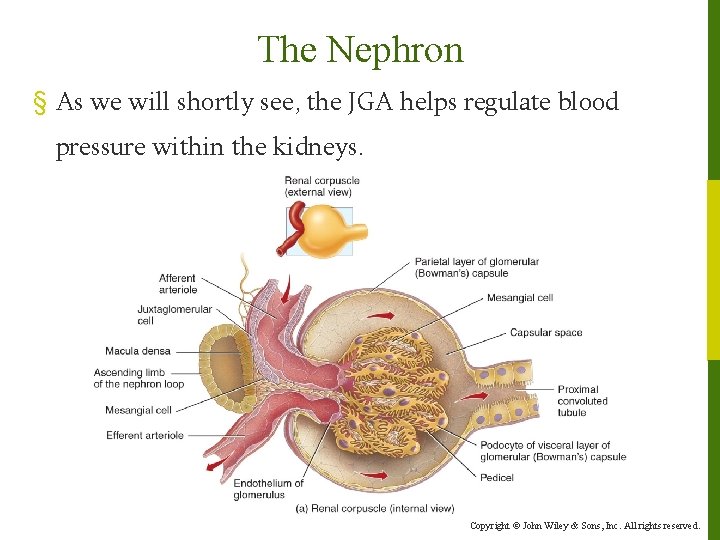
The Nephron § As we will shortly see, the JGA helps regulate blood pressure within the kidneys. Copyright © John Wiley & Sons, Inc. All rights reserved.
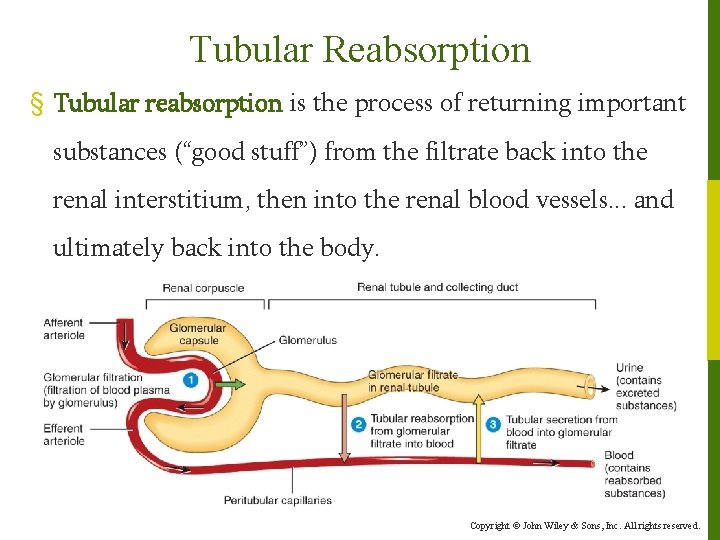
Renal Physiology § The 3 basic functions performed by nephrons and collecting ducts are: l Glomerular filtration - pressure forces filtration of waste -laden blood in the glomerulus. The glomerular filtration rate (GFR) is the amount of filtrate formed in all the renal corpuscles of both kidneys each minute. l Tubular reabsorption – the process of returning important substances from the filtrate back to the body. l Tubular secretion – the movement of waste materials from the body to the filtrate. Copyright © John Wiley & Sons, Inc. All rights reserved.
Glomerular Filtration § Glomerular filtration is the formation of a protein-free filtrate (ultrafiltrate) of plasma across the glomerular membrane. l Only a portion of the blood plasma delivered to the kidney via the renal artery is filtered. l Plasma which escapes filtration, along with its protein and cellular elements, exits the renal corpuscle via the efferent arteriole, perfuses the tubular capillary beds, and is eventually collected in the renal venous system. Copyright © John Wiley & Sons, Inc. All rights reserved.
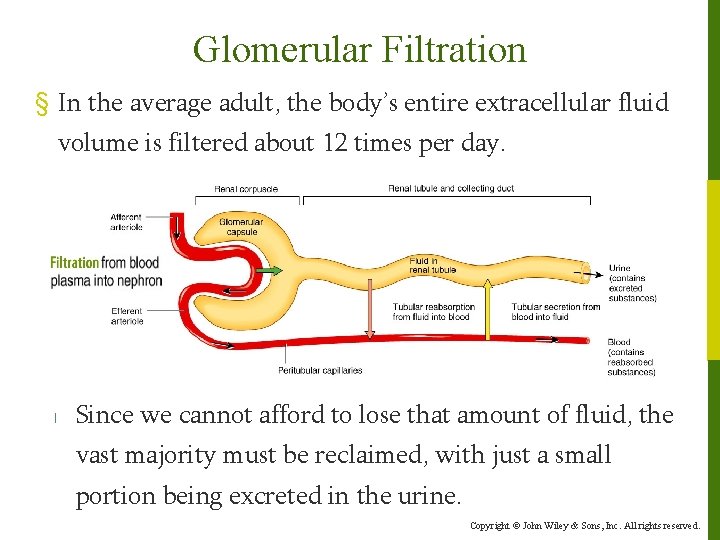
Glomerular Filtration § In the average adult, the body’s entire extracellular fluid volume is filtered about 12 times per day. l Since we cannot afford to lose that amount of fluid, the vast majority must be reclaimed, with just a small portion being excreted in the urine. Copyright © John Wiley & Sons, Inc. All rights reserved.
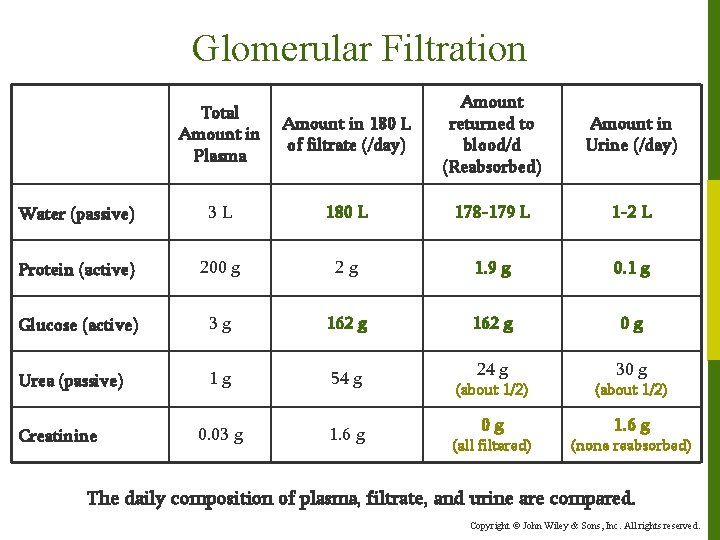
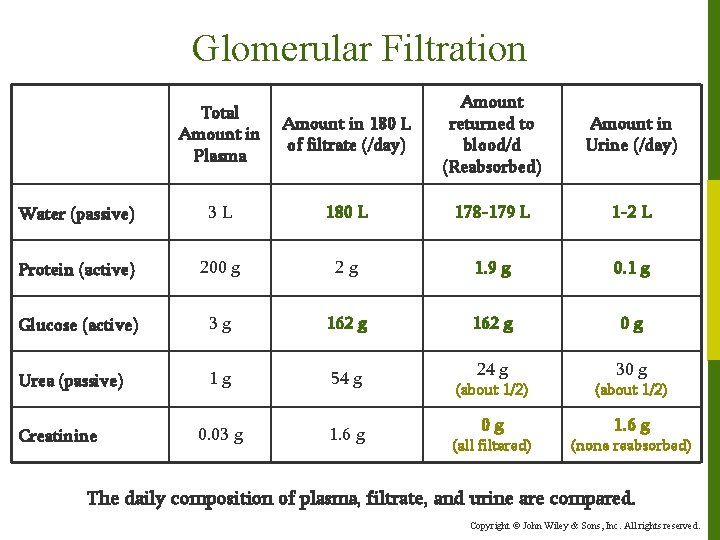
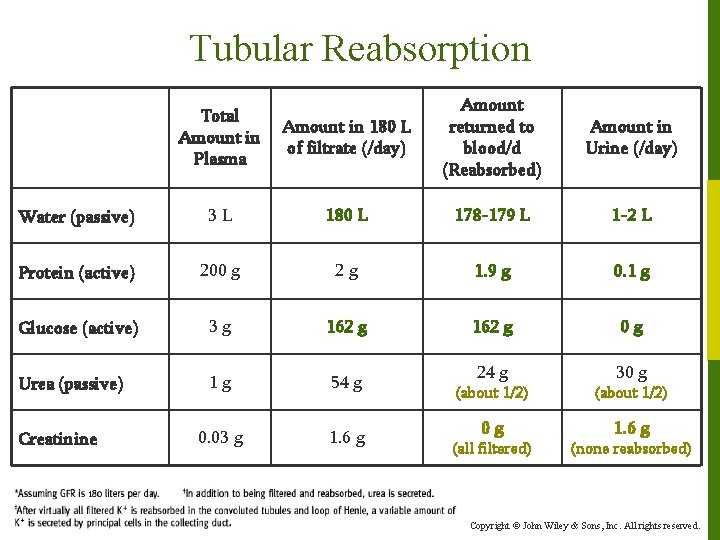
Glomerular Filtration Amount in 180 L of filtrate (/day) Amount returned to blood/d (Reabsorbed) Amount in Urine (/day) 3 L 180 L 178 -179 L 1 -2 L Protein (active) 200 g 2 g 1. 9 g 0. 1 g Glucose (active) 3 g 162 g 0 g Urea (passive) 1 g 54 g 24 g 30 g 0. 03 g 1. 6 g Total Amount in Plasma Water (passive) Creatinine (about 1/2) 0 g 1. 6 g (all filtered) (none reabsorbed) The daily composition of plasma, filtrate, and urine are compared. Copyright © John Wiley & Sons, Inc. All rights reserved.
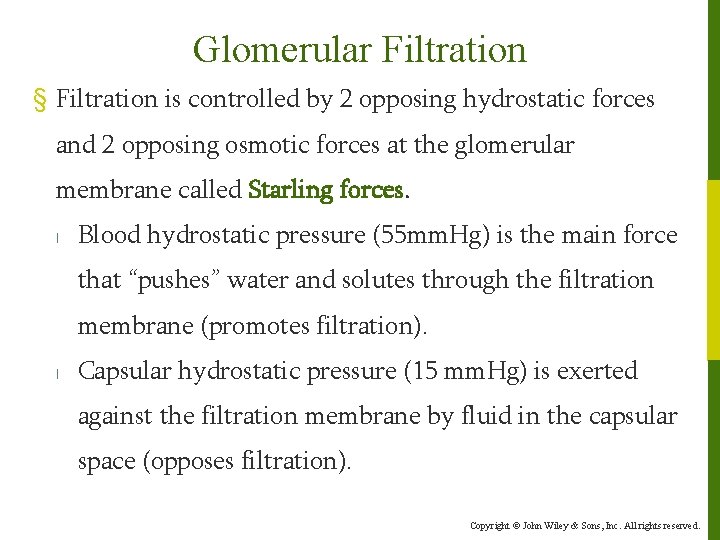
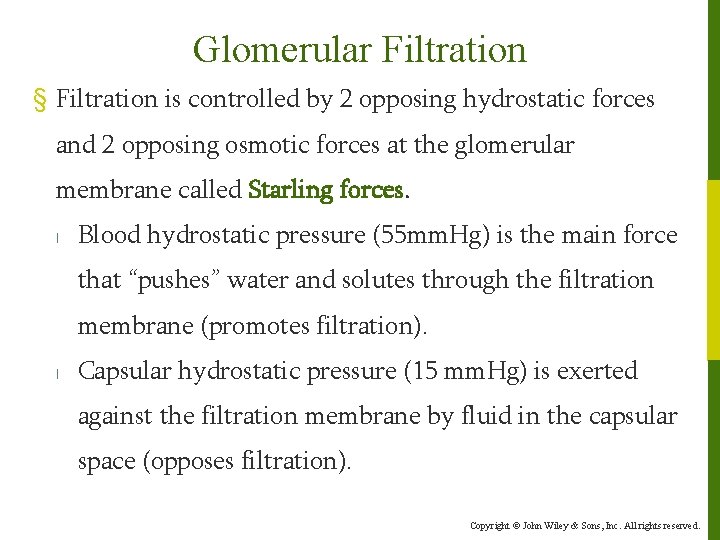
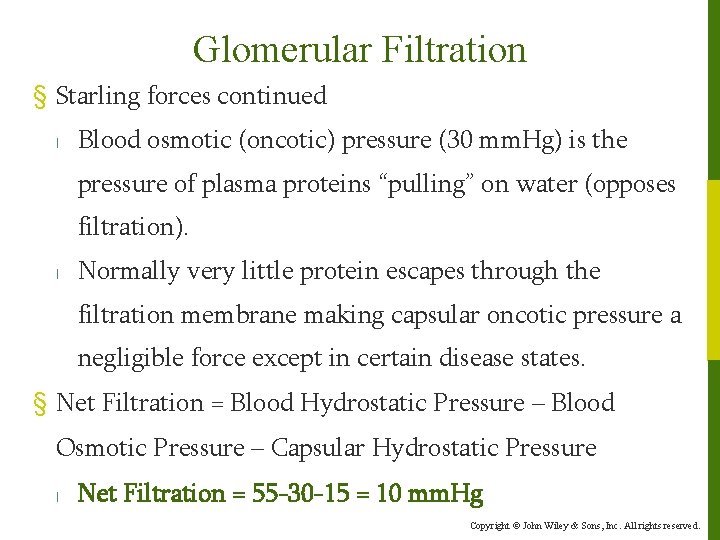
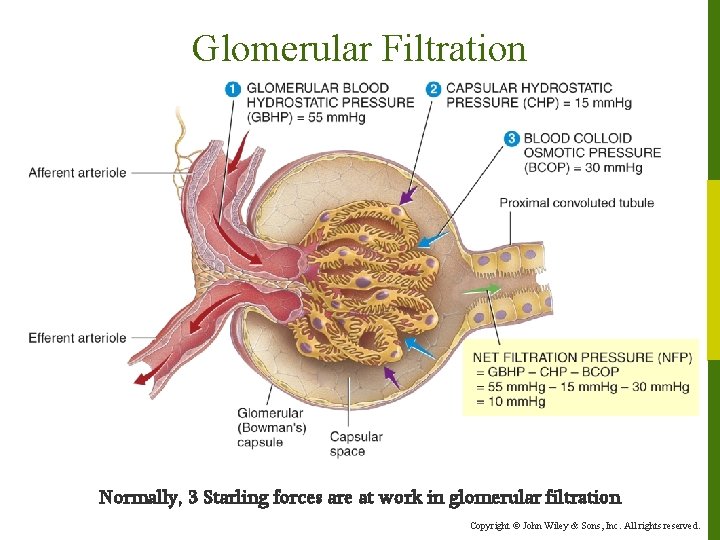
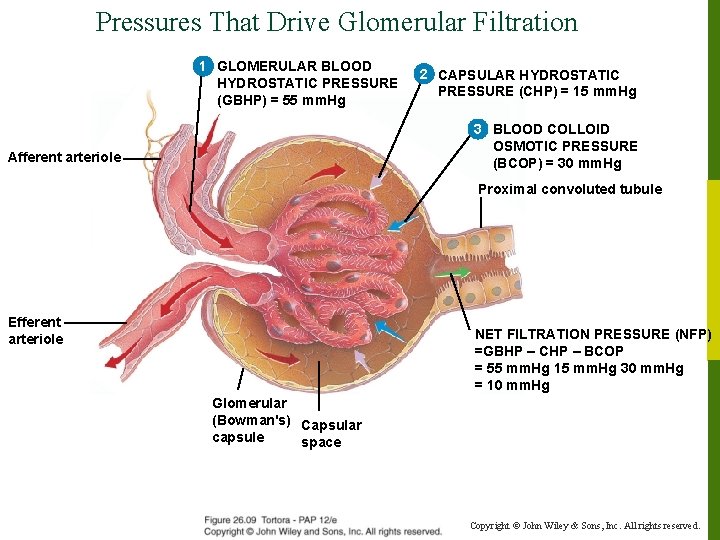
Glomerular Filtration § Filtration is controlled by 2 opposing hydrostatic forces and 2 opposing osmotic forces at the glomerular membrane called Starling forces. l Blood hydrostatic pressure (55 mm. Hg) is the main force that “pushes” water and solutes through the filtration membrane (promotes filtration). l Capsular hydrostatic pressure (15 mm. Hg) is exerted against the filtration membrane by fluid in the capsular space (opposes filtration). Copyright © John Wiley & Sons, Inc. All rights reserved.
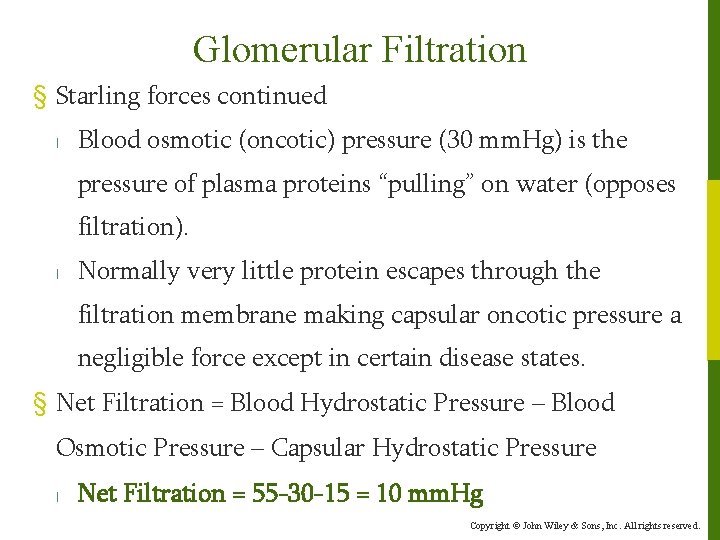
Glomerular Filtration § Starling forces continued l Blood osmotic (oncotic) pressure (30 mm. Hg) is the pressure of plasma proteins “pulling” on water (opposes filtration). l Normally very little protein escapes through the filtration membrane making capsular oncotic pressure a negligible force except in certain disease states. § Net Filtration = Blood Hydrostatic Pressure – Blood Osmotic Pressure – Capsular Hydrostatic Pressure l Net Filtration = 55 -30 -15 = 10 mm. Hg Copyright © John Wiley & Sons, Inc. All rights reserved.
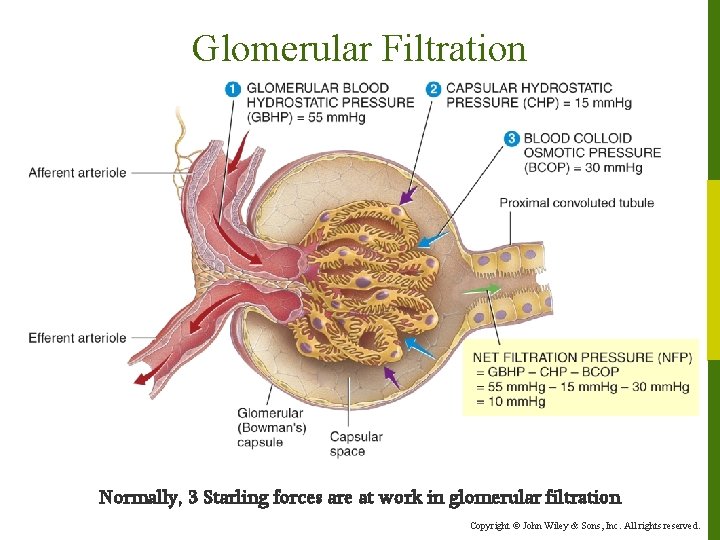
Glomerular Filtration Normally, 3 Starling forces are at work in glomerular filtration Copyright © John Wiley & Sons, Inc. All rights reserved.
Glomerular Filtration § Regulation of the GFR is critical to maintaining homeostasis and is regulated by an assortment of local and systemic mechanisms: l Renal autoregulation occurs when the kidneys themselves regulate GFR. l Neural regulation occurs when the ANS regulates renal blood flow and GFR. l Hormonal regulation involves angiotensin II and atrial natriuretic peptide (ANP). Copyright © John Wiley & Sons, Inc. All rights reserved.
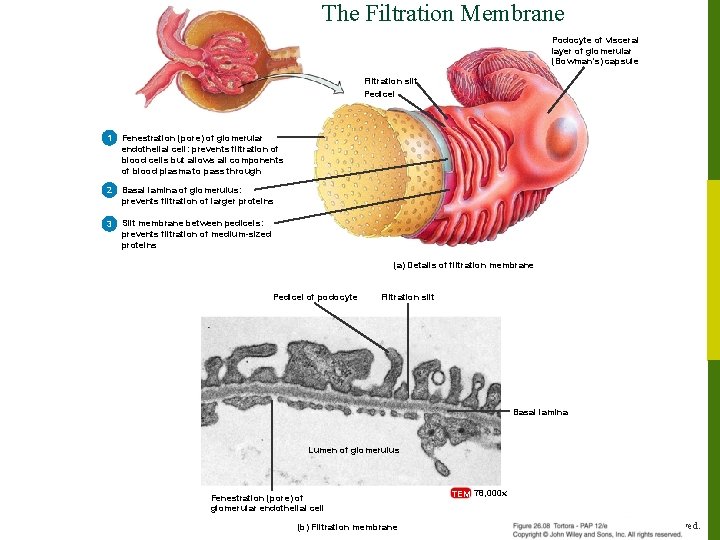
The Filtration Membrane Podocyte of visceral layer of glomerular (Bowman’s) capsule Filtration slit Pedicel 1 Fenestration (pore) of glomerular endothelial cell: prevents filtration of blood cells but allows all components of blood plasma to pass through 2 Basal lamina of glomerulus: prevents filtration of larger proteins 3 Slit membrane between pedicels: prevents filtration of medium-sized proteins (a) Details of filtration membrane Pedicel of podocyte Filtration slit Basal lamina Lumen of glomerulus Fenestration (pore) of glomerular endothelial cell (b) Filtration membrane TEM 78, 000 x Copyright © John Wiley & Sons, Inc. All rights reserved.
Glomerular Filtration (Interactions Animation) Renal Filtration You must be connected to the internet to run this animation Copyright © John Wiley & Sons, Inc. All rights reserved.
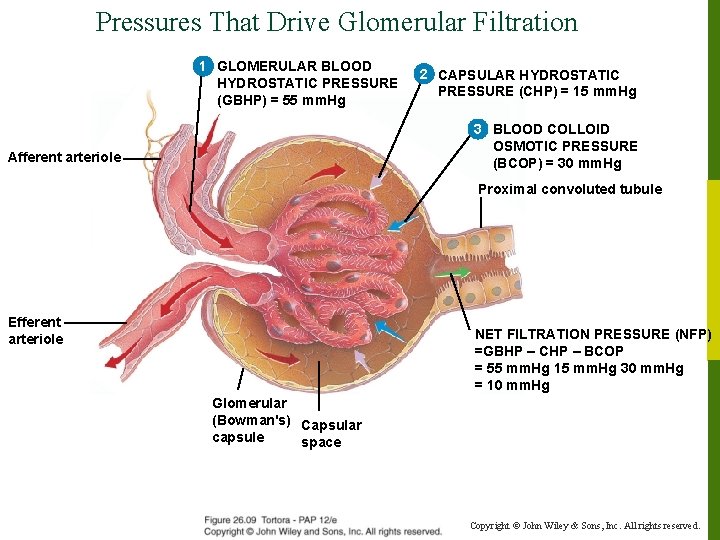
Pressures That Drive Glomerular Filtration 1 GLOMERULAR BLOOD HYDROSTATIC PRESSURE (GBHP) = 55 mm. Hg 2 CAPSULAR HYDROSTATIC PRESSURE (CHP) = 15 mm. Hg 3 BLOOD COLLOID OSMOTIC PRESSURE (BCOP) = 30 mm. Hg Afferent arteriole Proximal convoluted tubule Efferent arteriole NET FILTRATION PRESSURE (NFP) =GBHP – CHP – BCOP = 55 mm. Hg 15 mm. Hg 30 mm. Hg = 10 mm. Hg Glomerular (Bowman's) Capsular capsule space Copyright © John Wiley & Sons, Inc. All rights reserved.
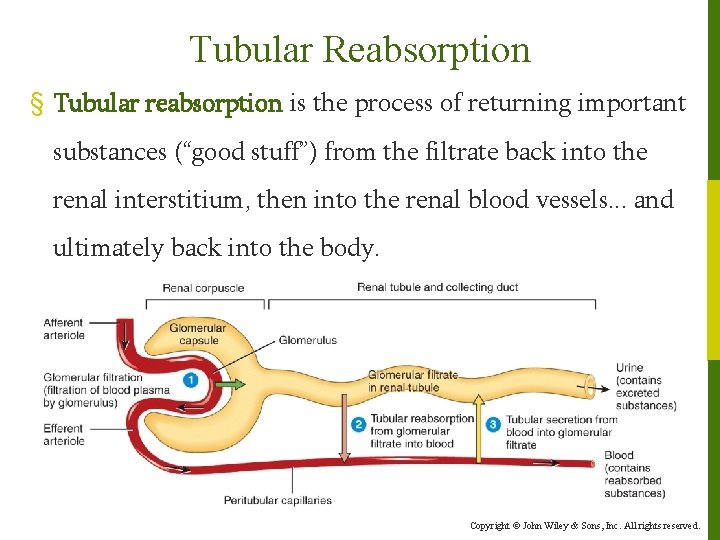
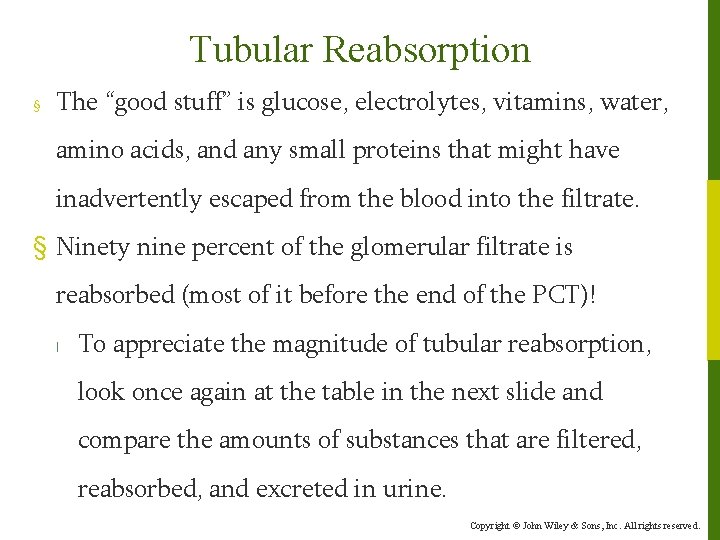
Tubular Reabsorption § Tubular reabsorption is the process of returning important substances (“good stuff”) from the filtrate back into the renal interstitium, then into the renal blood vessels. . . and ultimately back into the body. Copyright © John Wiley & Sons, Inc. All rights reserved.
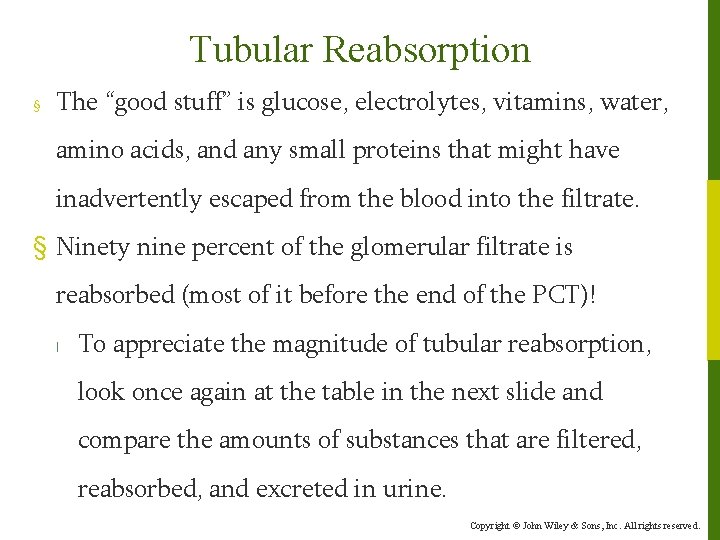
Tubular Reabsorption § The “good stuff” is glucose, electrolytes, vitamins, water, amino acids, and any small proteins that might have inadvertently escaped from the blood into the filtrate. § Ninety nine percent of the glomerular filtrate is reabsorbed (most of it before the end of the PCT)! l To appreciate the magnitude of tubular reabsorption, look once again at the table in the next slide and compare the amounts of substances that are filtered, reabsorbed, and excreted in urine. Copyright © John Wiley & Sons, Inc. All rights reserved.
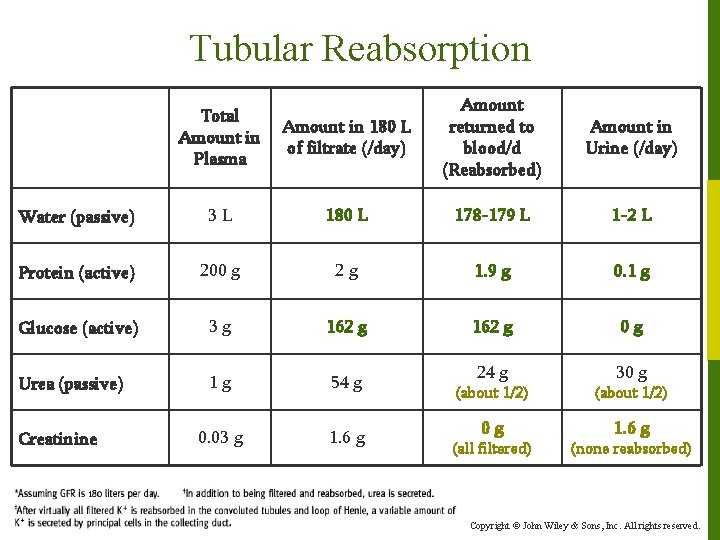
Tubular Reabsorption Amount in 180 L of filtrate (/day) Amount returned to blood/d (Reabsorbed) Amount in Urine (/day) 3 L 180 L 178 -179 L 1 -2 L Protein (active) 200 g 2 g 1. 9 g 0. 1 g Glucose (active) 3 g 162 g 0 g Urea (passive) 1 g 54 g 24 g 30 g 0. 03 g 1. 6 g Total Amount in Plasma Water (passive) Creatinine (about 1/2) 0 g 1. 6 g (all filtered) (none reabsorbed) Copyright © John Wiley & Sons, Inc. All rights reserved.
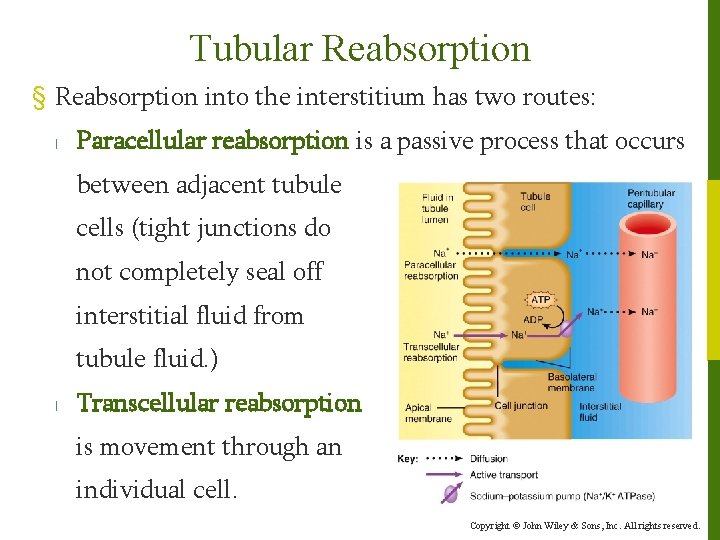
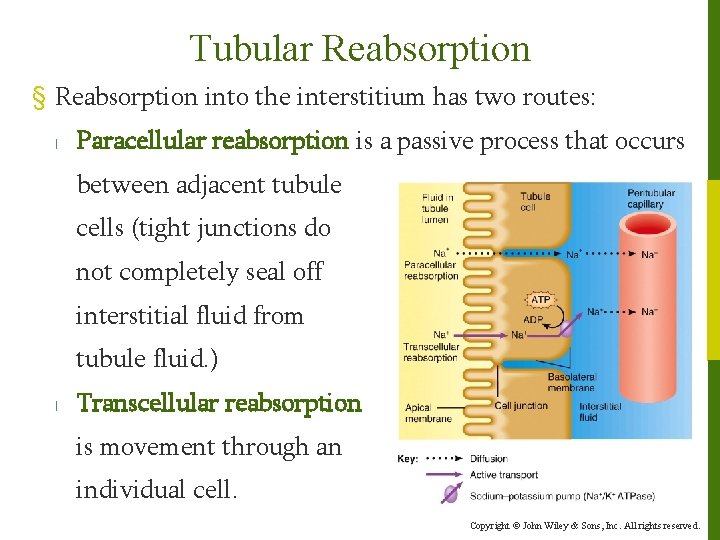
Tubular Reabsorption § Reabsorption into the interstitium has two routes: l Paracellular reabsorption is a passive process that occurs between adjacent tubule cells (tight junctions do not completely seal off interstitial fluid from tubule fluid. ) l Transcellular reabsorption is movement through an individual cell. Copyright © John Wiley & Sons, Inc. All rights reserved.
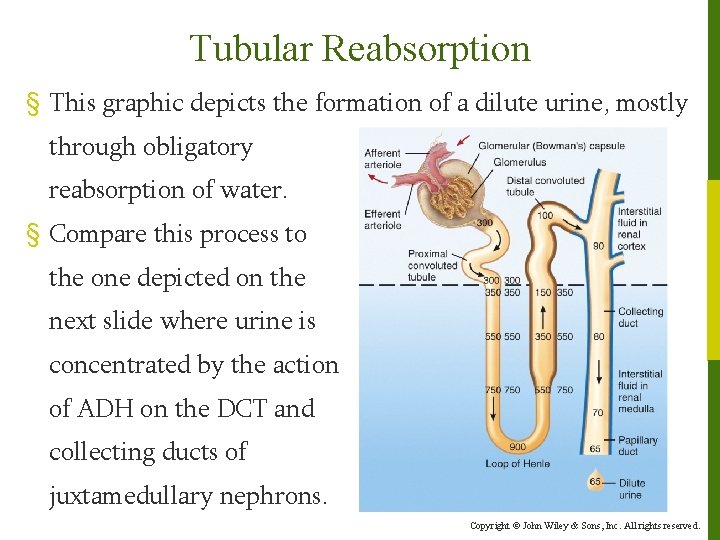
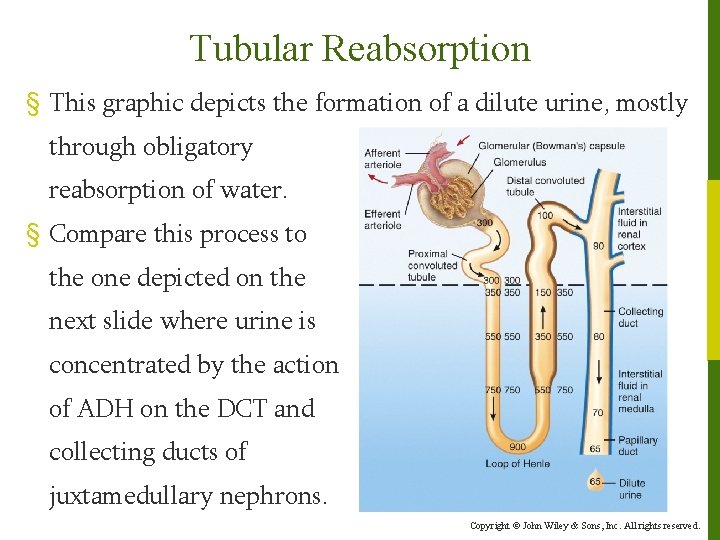
Tubular Reabsorption § This graphic depicts the formation of a dilute urine, mostly through obligatory reabsorption of water. § Compare this process to the one depicted on the next slide where urine is concentrated by the action of ADH on the DCT and collecting ducts of juxtamedullary nephrons. Copyright © John Wiley & Sons, Inc. All rights reserved.
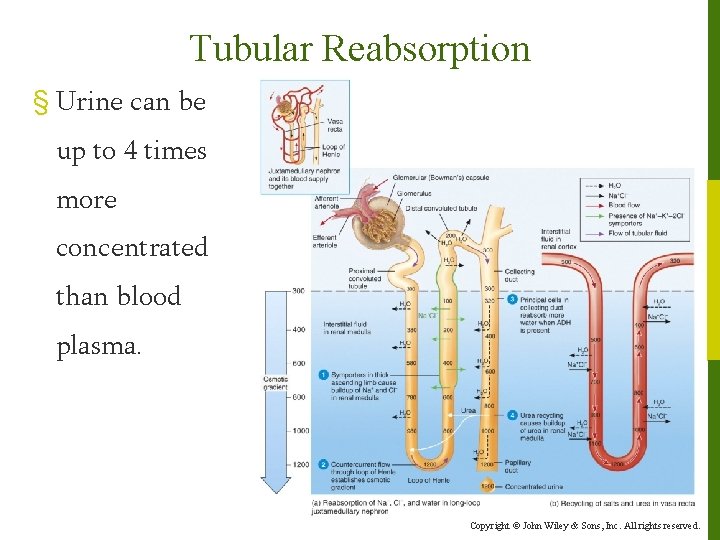
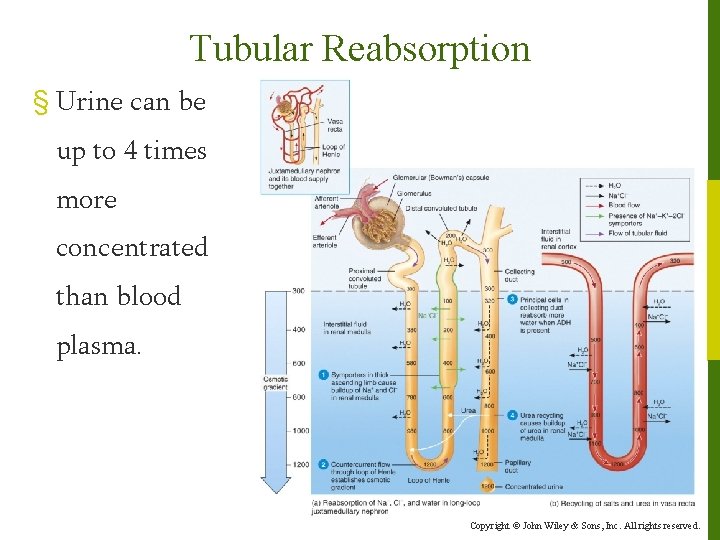
Tubular Reabsorption § Urine can be up to 4 times more concentrated than blood plasma. Copyright © John Wiley & Sons, Inc. All rights reserved.
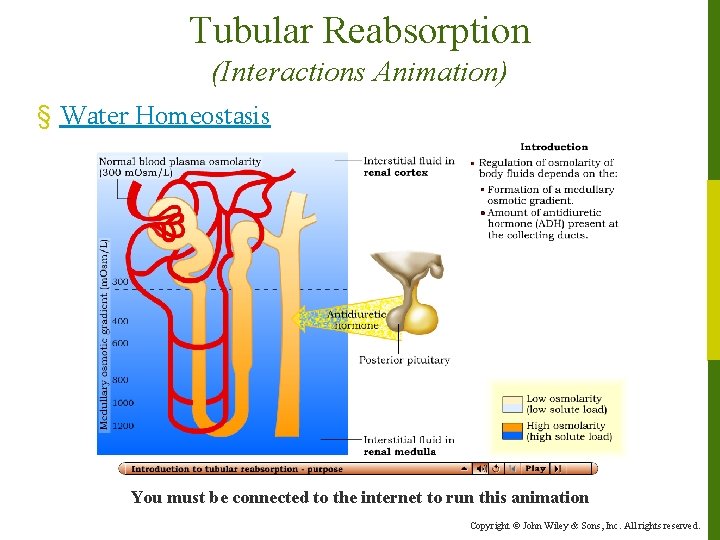
Tubular Reabsorption (Interactions Animation) § Water Homeostasis You must be connected to the internet to run this animation Copyright © John Wiley & Sons, Inc. All rights reserved.
Tubular Reabsorption § If higher than normal amounts of a substance are present in the filtrate, then the renal threshold for reabsorption of that substance may be surpassed. l When that happens, the substance cannot be reabsorbed fast enough, and it will be excreted in the urine. l For example, the renal [reabsorption] threshold of glucose is 180 -200 mg/dl. When this level is exceeded (as in diabetes mellitus), the glucose is said to “spill” into the urine (meaning a substance which is not normally present in urine begins to appear). Copyright © John Wiley & Sons, Inc. All rights reserved.
Tubular Secretion § Tubular secretion is the movement of substances from the capillaries which surround the nephron into the filtrate. l It occurs at a site other than the filtration membrane (in the proximal convoluted tubule, distal convoluted tubule and collecting ducts) by active transport. § The process of tubular secretion controls p. H. l Hydrogen and ammonium ions are secreted to decrease the acidity in the body, and bicarbonate is conserved. ◦ Secreted substances include H+, K+, NH 4+, and some drugs; the amount often depends on body needs. Copyright © John Wiley & Sons, Inc. All rights reserved.
Tubular Secretion § Maintaining the body’s proper p. H requires cooperation mainly between the lungs and the kidneys. l The lungs eliminate CO 2. ◦ Provides a rapid response (minutes) l The kidneys eliminate H+ and NH 4+ ions and conserve bicarbonate. ◦ This is a slower response (hours-days). l The alimentary canal (digestive), and integumentary system (skin) provide minor contributions. Copyright © John Wiley & Sons, Inc. All rights reserved.
Hormones and Homeostasis § Five hormones affect the extent of Na+, Cl–, Ca 2+, and water reabsorption as well as K+ secretion by the renal tubules. These hormones, all of which are key to maintaining homeostasis of not only renal blood flow and B. P. , but systemic blood flow and B. P. , are: l angiotensin II l antidiuretic hormone (ADH) l aldosterone l atrial natriuretic peptide (ANP) l parathyroid hormone (PTH) Copyright © John Wiley & Sons, Inc. All rights reserved.
Hormones and Homeostasis § We have already mentioned the effect of ANP on GFR. § ADH is released by the posterior pituitary in response to low blood flow in this part of the brain. l ADH affects facultative water reabsorption by increasing the water permeability of principal cells in the last part of the distal convoluted tubule and throughout the collecting duct. ◦ In the absence of ADH, the apical membranes of principal cells are almost impermeable to water. Copyright © John Wiley & Sons, Inc. All rights reserved.
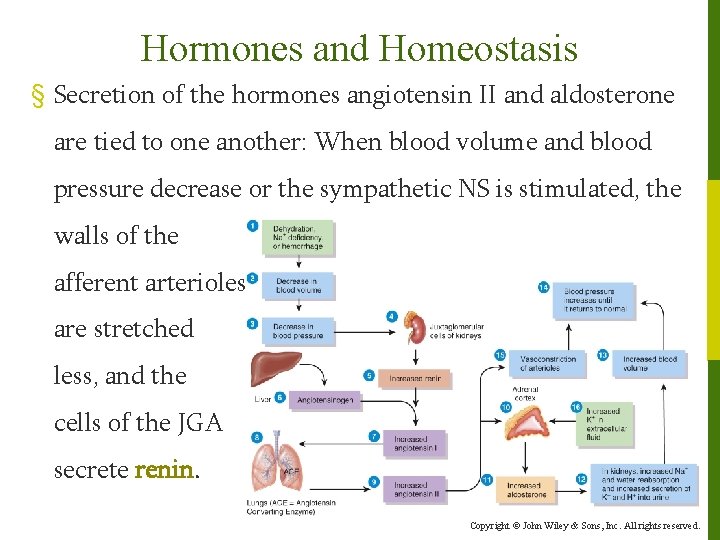
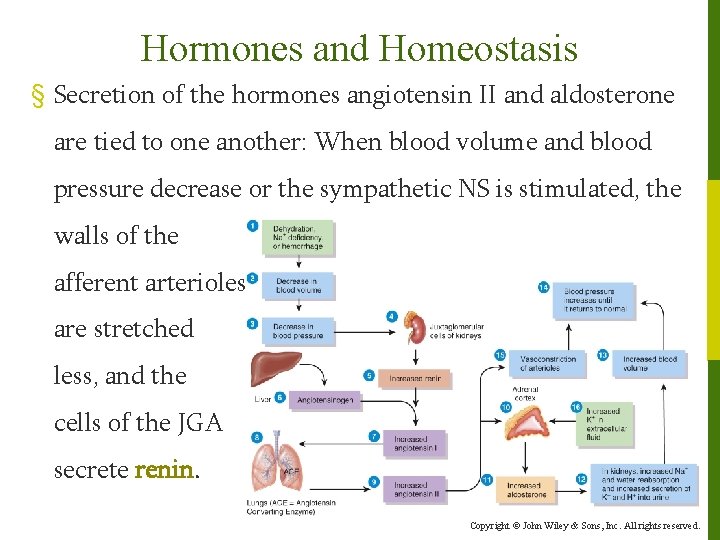
Hormones and Homeostasis § Secretion of the hormones angiotensin II and aldosterone are tied to one another: When blood volume and blood pressure decrease or the sympathetic NS is stimulated, the walls of the afferent arterioles are stretched less, and the cells of the JGA secrete renin. Copyright © John Wiley & Sons, Inc. All rights reserved.
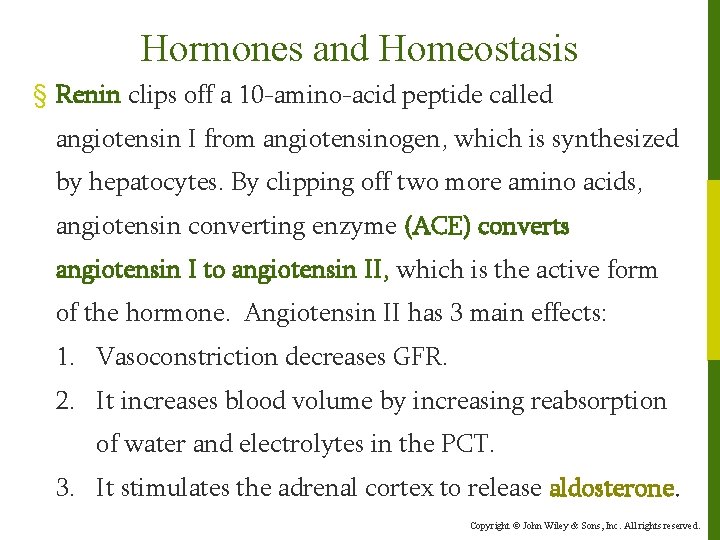
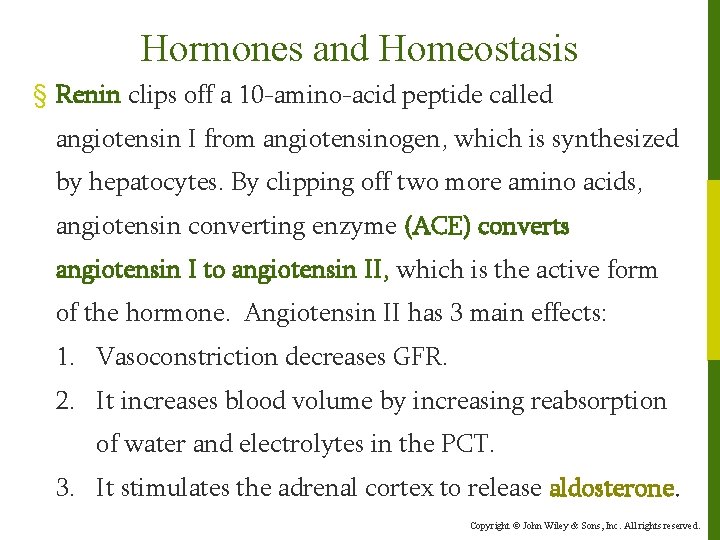
Hormones and Homeostasis § Renin clips off a 10 -amino-acid peptide called angiotensin I from angiotensinogen, which is synthesized by hepatocytes. By clipping off two more amino acids, angiotensin converting enzyme (ACE) converts angiotensin I to angiotensin II, which is the active form of the hormone. Angiotensin II has 3 main effects: 1. Vasoconstriction decreases GFR. 2. It increases blood volume by increasing reabsorption of water and electrolytes in the PCT. 3. It stimulates the adrenal cortex to release aldosterone. Copyright © John Wiley & Sons, Inc. All rights reserved.
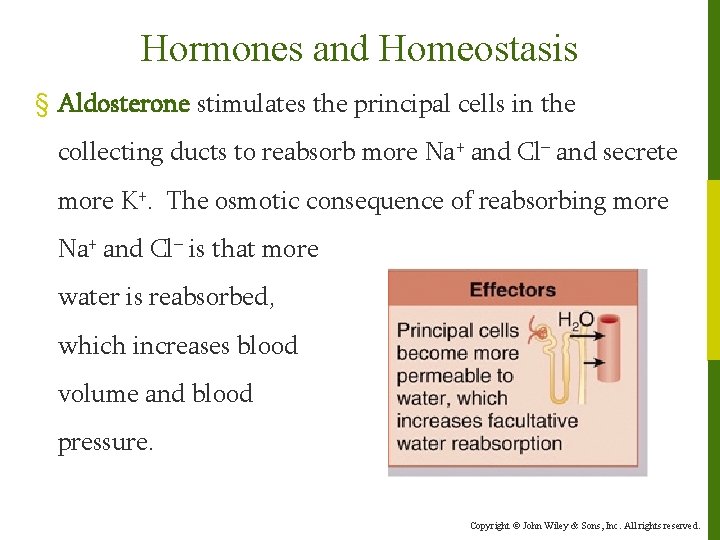
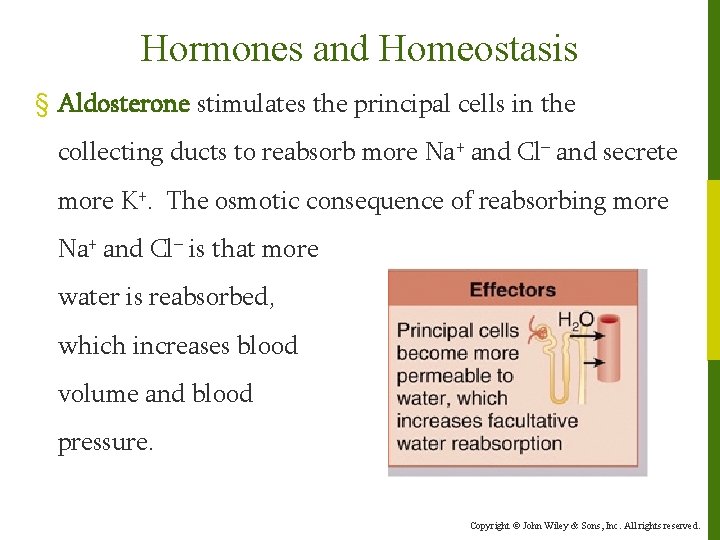
Hormones and Homeostasis § Aldosterone stimulates the principal cells in the collecting ducts to reabsorb more Na+ and Cl– and secrete more K+. The osmotic consequence of reabsorbing more Na+ and Cl– is that more water is reabsorbed, which increases blood volume and blood pressure. Copyright © John Wiley & Sons, Inc. All rights reserved.
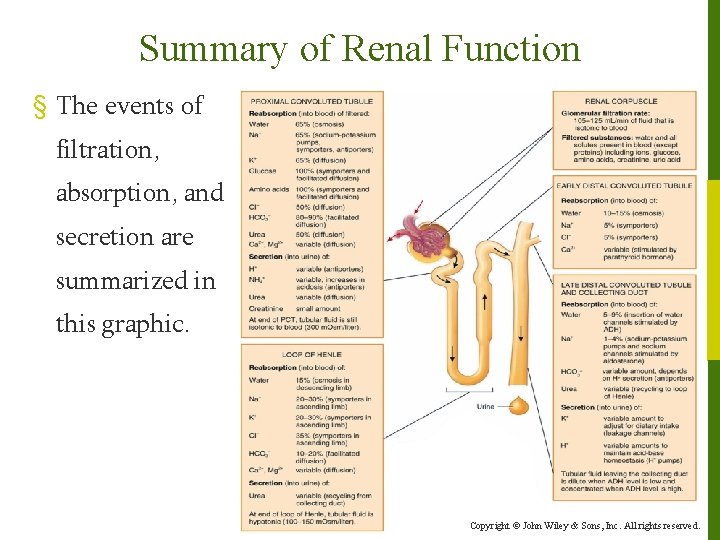
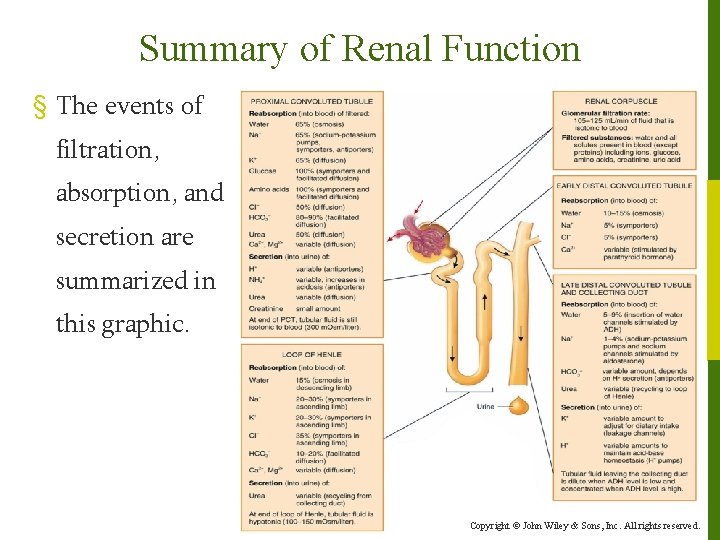
Summary of Renal Function § The events of filtration, absorption, and secretion are summarized in this graphic. Copyright © John Wiley & Sons, Inc. All rights reserved.
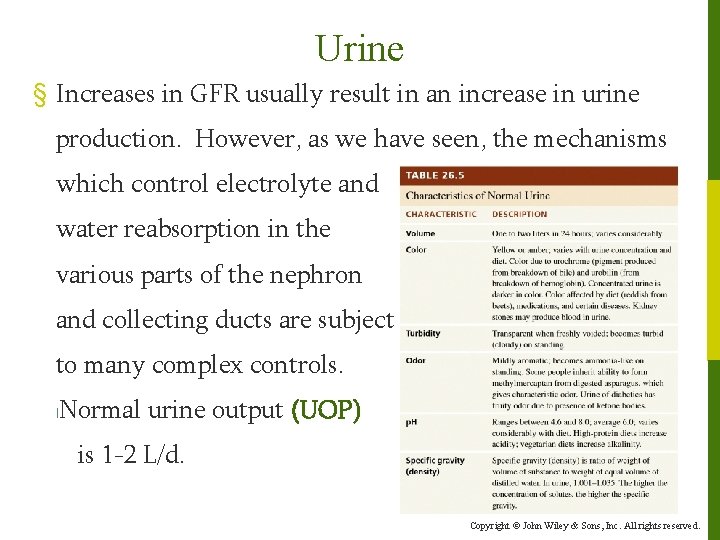
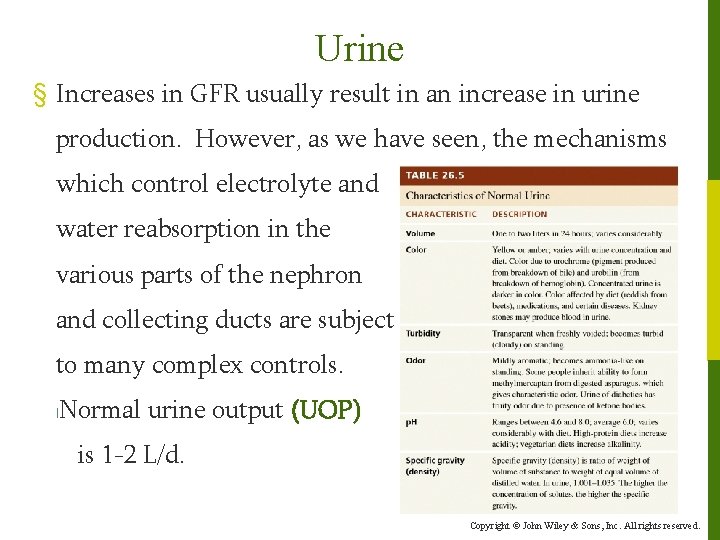
Urine § Increases in GFR usually result in an increase in urine production. However, as we have seen, the mechanisms which control electrolyte and water reabsorption in the various parts of the nephron and collecting ducts are subject to many complex controls. l Normal urine output (UOP) is 1 -2 L/d. Copyright © John Wiley & Sons, Inc. All rights reserved.
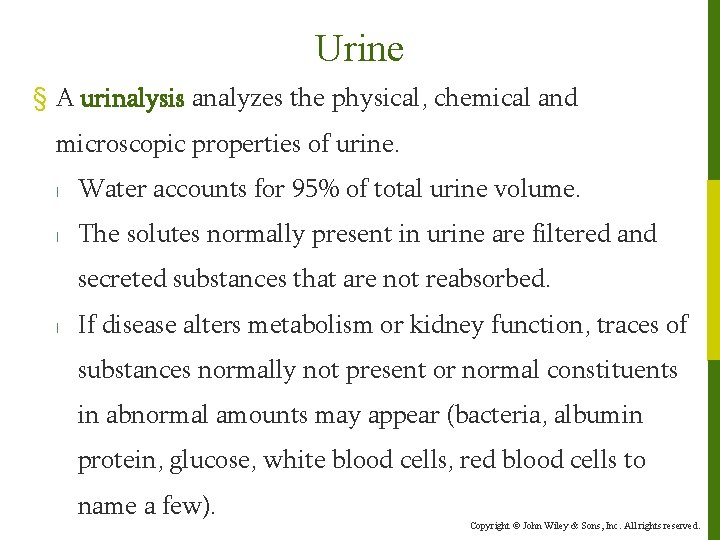
Urine § A urinalysis analyzes the physical, chemical and microscopic properties of urine. l Water accounts for 95% of total urine volume. l The solutes normally present in urine are filtered and secreted substances that are not reabsorbed. l If disease alters metabolism or kidney function, traces of substances normally not present or normal constituents in abnormal amounts may appear (bacteria, albumin protein, glucose, white blood cells, red blood cells to name a few). Copyright © John Wiley & Sons, Inc. All rights reserved.
Urine § In addition to a urinalysis, two blood tests are commonly done clinically to assess the adequacy of renal function. l Blood urea nitrogen (BUN) measures nitrogen wastes in blood from catabolism and deamination of amino acids. l Creatinine levels appear in the blood as a result of catabolism of creatine phosphate in skeletal muscle. ◦ The serum creatinine test measures the amount of creatinine in the blood, which increases in states of renal dysfunction. Copyright © John Wiley & Sons, Inc. All rights reserved.