State of the Integrated Medical Center System Stuart




- Slides: 39
State of the Integrated Medical Center System Stuart F. Seides, MD Physician Executive Director Med. Star Heart & Vascular Institute Washington, DC March 6, 2018
I have no relevant financial relationships.

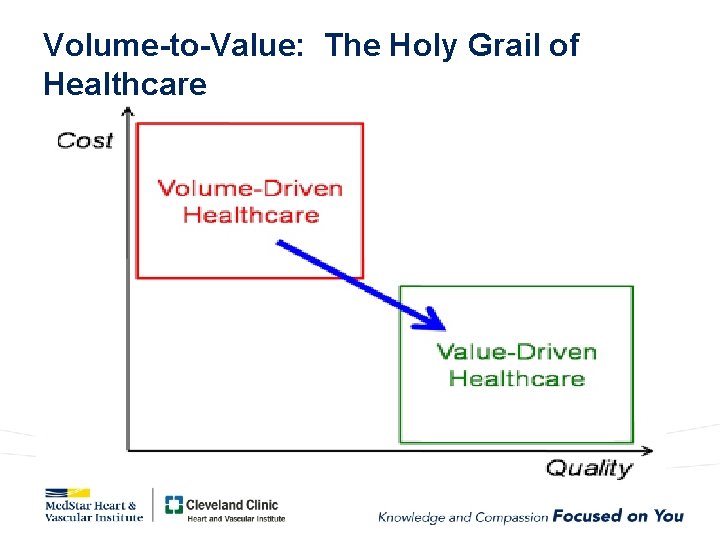
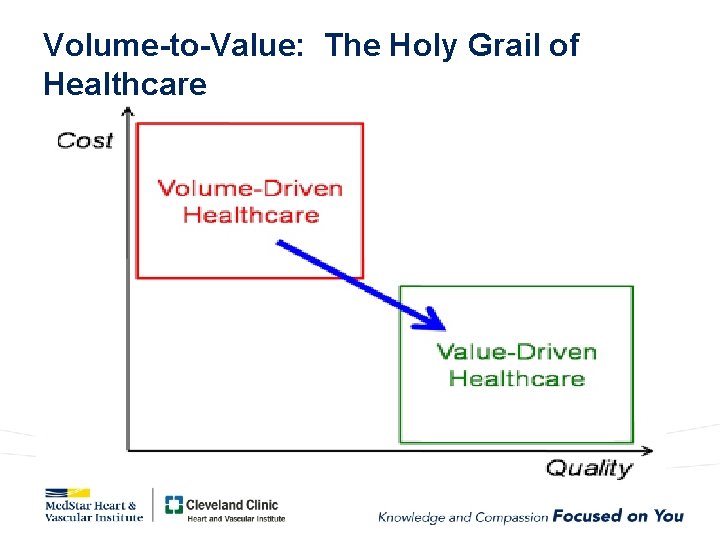
Volume-to-Value: The Holy Grail of Healthcare
Strategies to disrupt the U. S. healthcare paradigm (adapted from Pw. C) Incremental Innovation • • Buy/partner with a third-party administrator. . Offer near-site clinics. Enable direct-to-provider contracting. Enter pharmaceutical/durable medical equipment (DME) distribution and manufacturing. Technology and Analytics • • Offer virtual services. Offer a customized consumer (member/employer) portal. Offer data-driven insights. Offer services for providers/employers. Radical Disruption • • Develop a B 2 B and B 2 C clinical capacity exchange/marketplace. Develop a direct-to-employer (D 2 E) reverse auction platform. Roll out an encounter-based, claimless model. Develop next-generation healthcare connectivity platform.
Insurer mega-merger frenzy: The big 5 wanted to become the big 3 • Start of 2015: Aetna, BC/BS (largest of the 36 is Anthem), Cigna, Humana, and UHC • May 2015: Aetna+Humana, $37. 5 B deal (UHC approached Aetna in June 2015 but failed. ) • July 2015: Anthem+Cigna, $54. 2 B deal (UHC also approached Cigna in June 2015 but failed. ) • Fierce opposition by Am. Hosp. Assn. and AMA • Both deals were expected to close by the end of 2016 BUT BOTH BLOCKED BY FEDERAL COURTS as being anticompetitive.

Notable 2017 U. S. Health Care Deals 1. CVS Health to acquire Aetna • The deal involves Woonsocket, R. I. -based CVS Health and Hartford, Conn. -based Aetna. . 2. United. Health's Optum to buy 300 medical clinics • The deal involves Minnetonka, Minn. -based United Health Group's Optum unit and Da. Vita Medical Group, a subsidiary of Denver-based Da. Vita. . 3. Ascension, Providence St. Joseph in talks to merge • The deal involves St. Louis-based Ascension and Renton, Wash. -based Providence St. Joseph Health. 4. Walgreens pursues deal with Rite Aid • The deal involves Deerfield, Ill. -based Walgreens Boots Alliance and Camp Hill, Pa. -based Rite Aid. 5. CHI, Dignity Health to combine • The deal involves Englewood, Colo. -based Catholic Health Initiatives and San Francisco-based Dignity Health. 6. CHS' hospital divestiture spree • The deal involves Franklin, Tenn. -based Community Health Systems and more 30 hospitals across the nation. 7. Advocate, Aurora Health Care to merge into $11 B health system • The deal involves Downers Grove, Ill. -based Advocate Health Care and Milwaukee-based Aurora Health Care. 8. Advisory Board finalizes $1. 3 B deal with United. Health's Optum • The deal involves The Advisory Board Company and United. Health Group's Optum division. 9. Steward Health Care acquires Iasis • The deal involves Boston-based Steward Health Care and Franklin, Tenn. -based Iasis Healthcare. 10. Blackstone closes $6. 1 B deal to acquire Team. Health • The deal involves Blackstone, a New York City-based private equity, investment banking and asset management corporation, and Team. Health Holdings, a Knoxville, Tenn. -based physician services organization.
Amazon, JPMorgan. Chase, and Berkshire Hathaway launch new healthcare company January 30, 2018 • • • Amazon, Berkshire Hathaway and JPMorgan Chase & Co. are launching a new company aimed at cutting healthcare costs for their U. S. employees (~1 M). In addition to reducing healthcare costs, the companies are aiming to improve employee satisfaction through the new venture. Amazon, Berkshire Hathaway and JPMorgan are hoping the sheer size of each company and their complementary areas of expertise will help them tackle these issues. The companies said the project, which is in the early planning stage, will initially focus on technology solutions. "The ballooning costs of healthcare act as a hungry tapeworm on the American economy, " said Berkshire Hathaway Chairman Warren Buffett. U. S. Healthcare stocks nosedived (losing ~$69 B in aggregate value overnight!) on the news, because of Amazon’s history of being a disruptive force in whatever market they enter. (Amazon has also just announced that they are entering the medical and hospital supply business. )
Hospital-physician consolidation in the marketplace
Hospital Mergers: If you're the only game in town, there may be fewer incentives to improve and/or increase efficiency • A report finding that prices increased 28. 4% to 44. 2% after a merger between Sutter Health and Summit Medical Center (FTC, 2008) • A study of hospital competition finding patients in the least competitive areas experienced 1. 46 percentage points higher mortality rate from acute myocardial infarction than the most competitive markets. (NBER, 1999) • An analysis of the merger between Evanston Northwestern and Highland Park hospitals that found four out of five insurers substantially increased prices that they paid for specified services after the 2000 merger. (FTC, 2011)
Healthcare 2018: “One foot on the dock and one foot on the boat. ” Volume-drivers (F 4 S): Volume-constrainers (population health): revenue generation, skill-set retention , etc. ACA, AUCs, ACOs, RBMs, readmission penalties, GBR, etc.
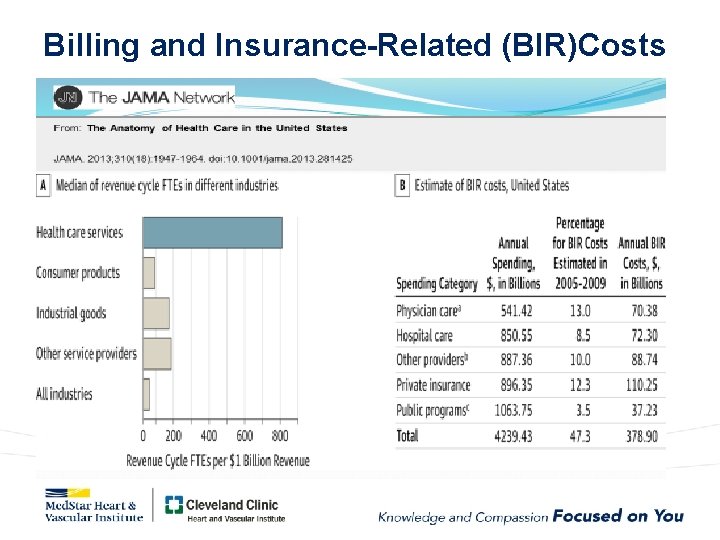
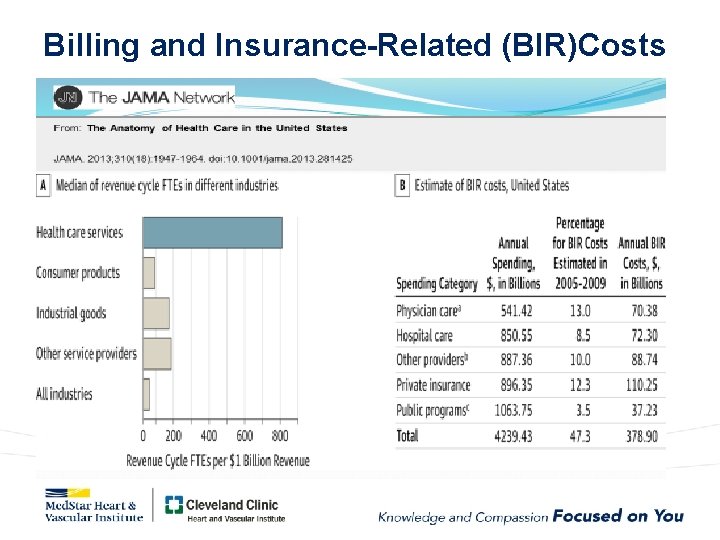
Billing and Insurance-Related (BIR)Costs
The doctor, the patient, and the EMR (and now the integrated health system that is paying for it!)
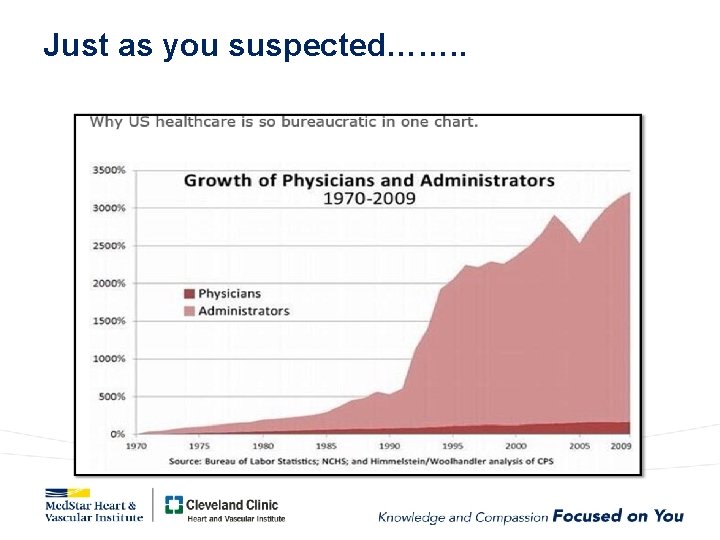
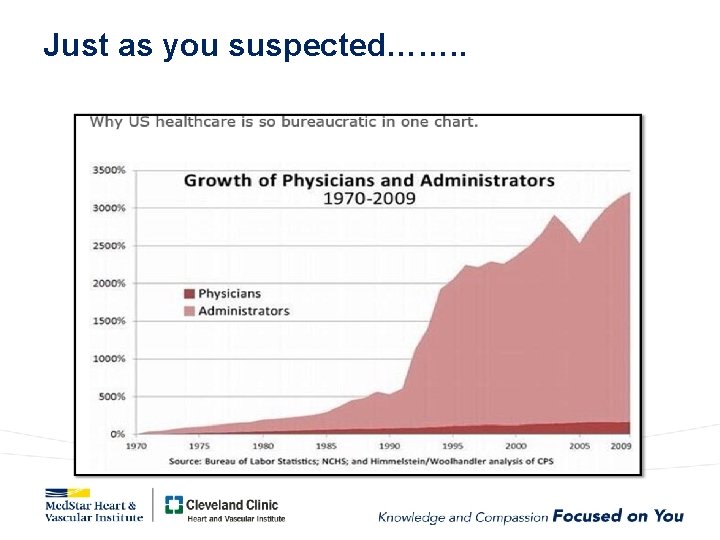
Just as you suspected……. .
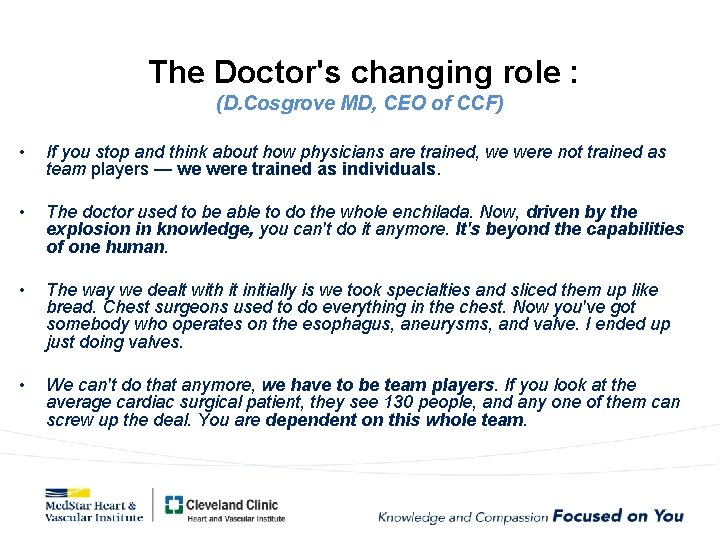
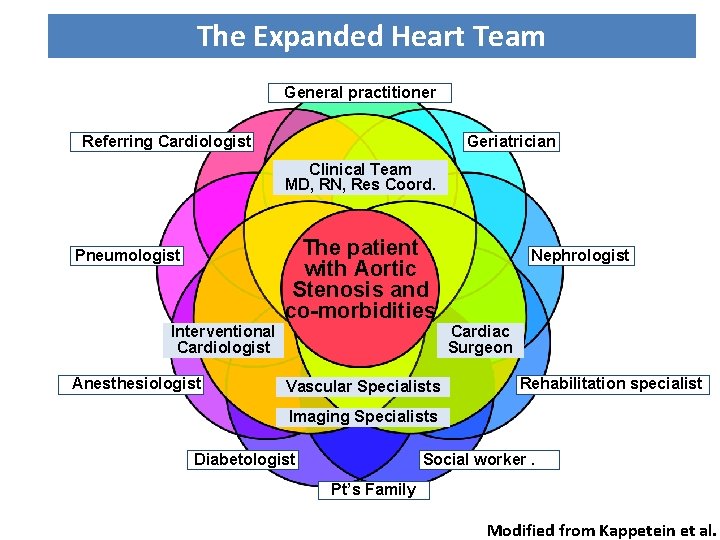
The Doctor's changing role : (D. Cosgrove MD, CEO of CCF) • If you stop and think about how physicians are trained, we were not trained as team players — we were trained as individuals. • The doctor used to be able to do the whole enchilada. Now, driven by the explosion in knowledge, you can't do it anymore. It's beyond the capabilities of one human. • The way we dealt with it initially is we took specialties and sliced them up like bread. Chest surgeons used to do everything in the chest. Now you've got somebody who operates on the esophagus, aneurysms, and valve. I ended up just doing valves. • We can't do that anymore, we have to be team players. If you look at the average cardiac surgical patient, they see 130 people, and any one of them can screw up the deal. You are dependent on this whole team.
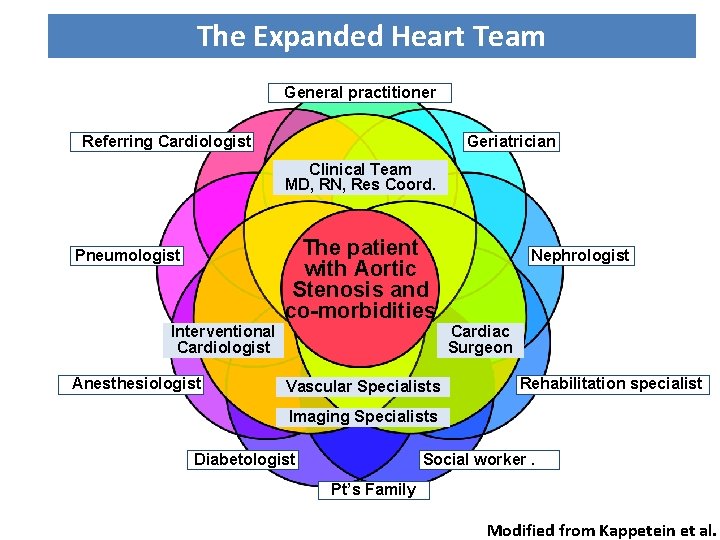
The Expanded Heart Team General practitioner Referring Cardiologist Geriatrician Clinical Team MD, RN, Res Coord. Pneumologist Interventional Cardiologist Anesthesiologist The patient with Aortic Stenosis and co-morbidities Vascular Specialists Nephrologist Cardiac Surgeon Rehabilitation specialist Imaging Specialists Diabetologist Social worker. Pt’s Family Modified from Kappetein et al.
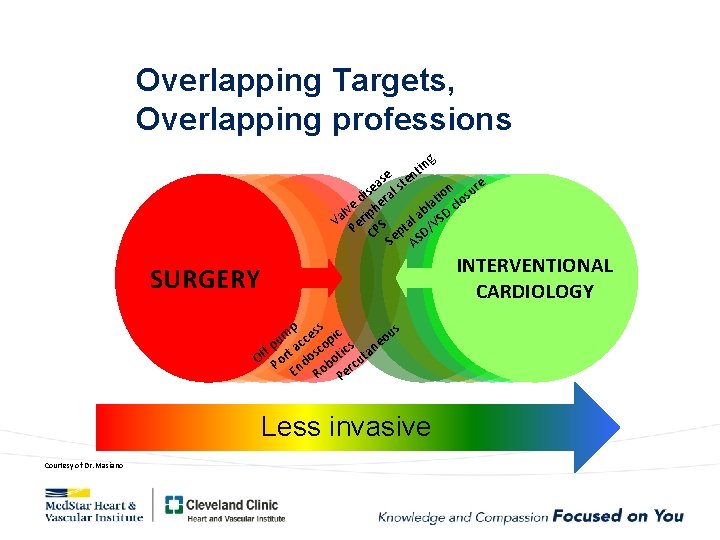
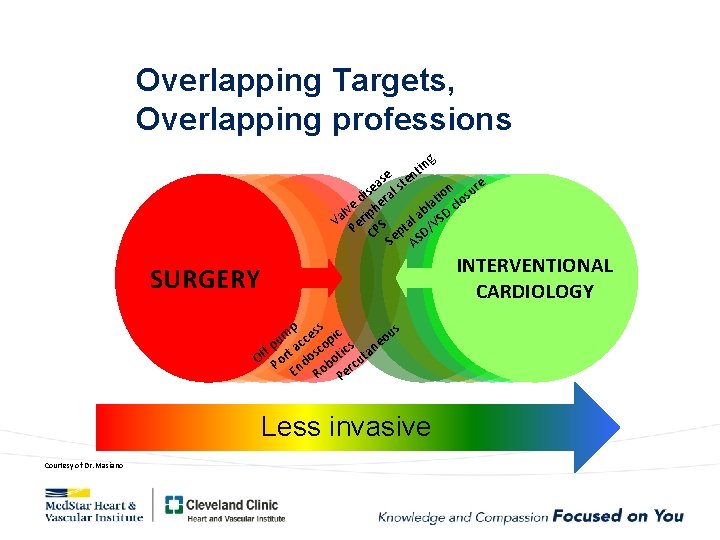
Overlapping Targets, Overlapping professions g tin n e as ste e n sure s ral o i i d e at clo l e h v b l p D Va Peri S tal a /VS CP Sep SD A INTERVENTIONAL CARDIOLOGY SURGERY p ss c us e pi m o c u e c f p a co ics n Of Port dos bot cuta En Ro Per Less invasive Courtesy of Dr. Masiano
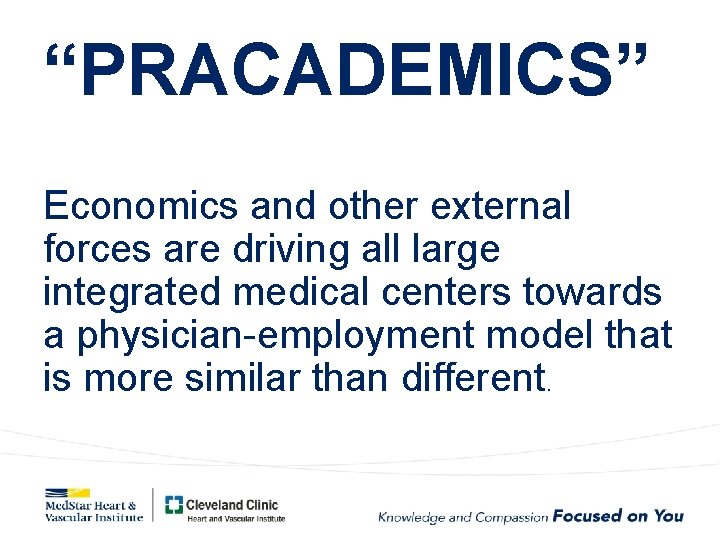
“PRACADEMICS” Economics and other external forces are driving all large integrated medical centers towards a physician-employment model that is more similar than different.
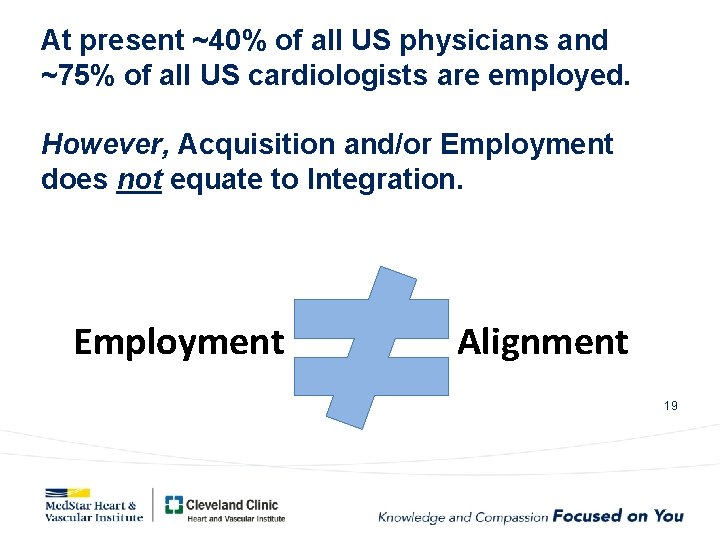
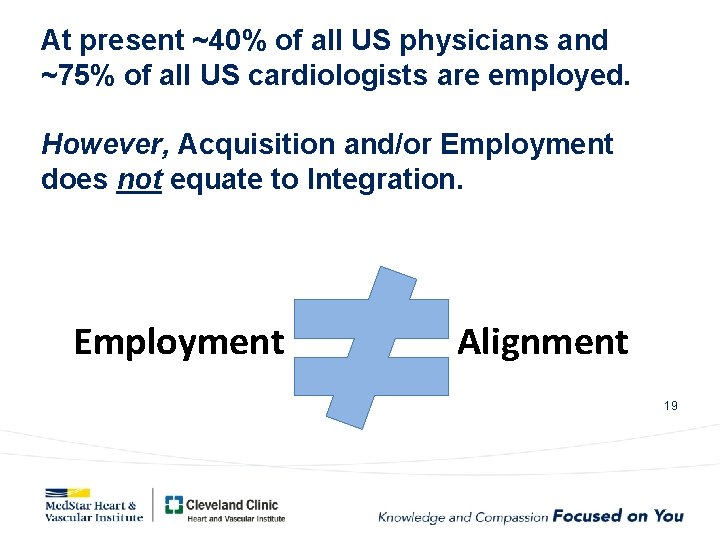
At present ~40% of all US physicians and ~75% of all US cardiologists are employed. However, Acquisition and/or Employment does not equate to Integration. Employment Alignment 19
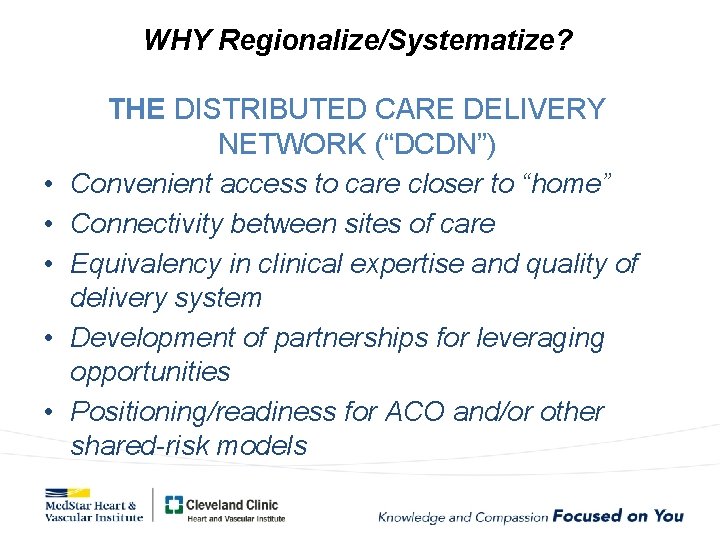
WHY Regionalize/Systematize? • • • THE DISTRIBUTED CARE DELIVERY NETWORK (“DCDN”) Convenient access to care closer to “home” Connectivity between sites of care Equivalency in clinical expertise and quality of delivery system Development of partnerships for leveraging opportunities Positioning/readiness for ACO and/or other shared-risk models
WHY Regionalize/Systematize? Decrease redundancy and enhance efficiency – Common clinical protocols and pathways – Match clinical problem with appropriate resource allocation (community vs. tertiary setting) – Optimize clinical competencies (subspecialty training/expertise, APC utilization) – Inform program purchasing decisions and leverage program infrastructure
WHY Regionalize/Systematize? Develop program cohesiveness – Coordinated strategic and operational leadership – Take advantage of specific areas of expertise of individuals on the team – Multiple sites delivering equivalent expertise and care with the option of leveraging systemwide breadth. – Shift the competitive focus externally.
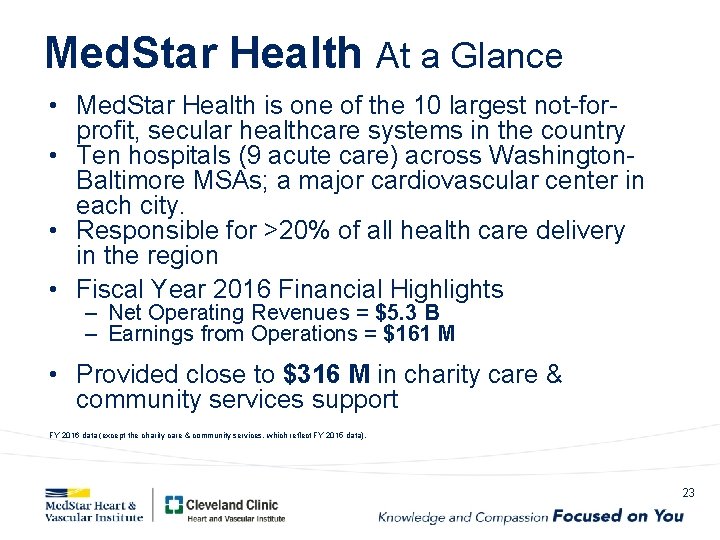
Med. Star Health At a Glance • Med. Star Health is one of the 10 largest not-forprofit, secular healthcare systems in the country • Ten hospitals (9 acute care) across Washington. Baltimore MSAs; a major cardiovascular center in each city. • Responsible for >20% of all health care delivery in the region • Fiscal Year 2016 Financial Highlights – Net Operating Revenues = $5. 3 B – Earnings from Operations = $161 M • Provided close to $316 M in charity care & community services support FY 2016 data (except the charity care & community services, which reflect FY 2015 data). 23
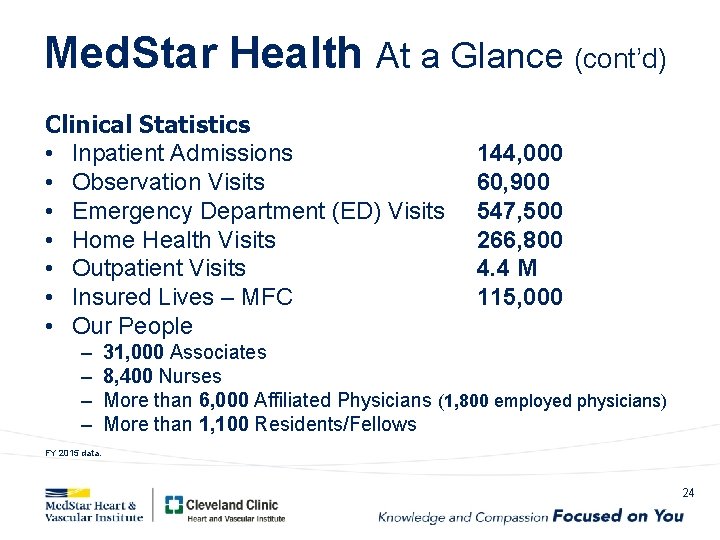
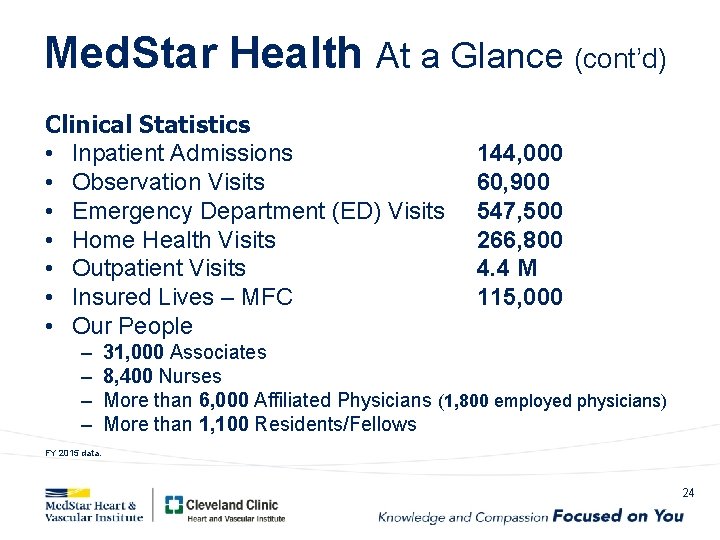
Med. Star Health At a Glance (cont’d) Clinical Statistics • Inpatient Admissions • Observation Visits • Emergency Department (ED) Visits • Home Health Visits • Outpatient Visits • Insured Lives – MFC • Our People – – 144, 000 60, 900 547, 500 266, 800 4. 4 M 115, 000 31, 000 Associates 8, 400 Nurses More than 6, 000 Affiliated Physicians (1, 800 employed physicians) More than 1, 100 Residents/Fellows FY 2015 data. 24
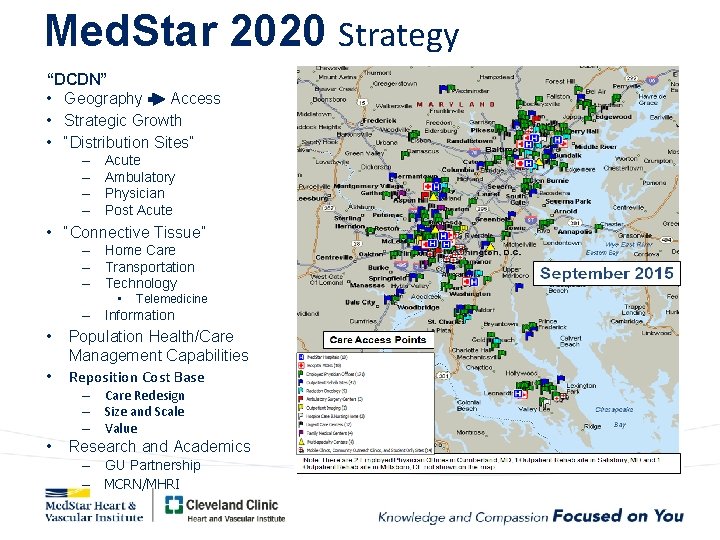
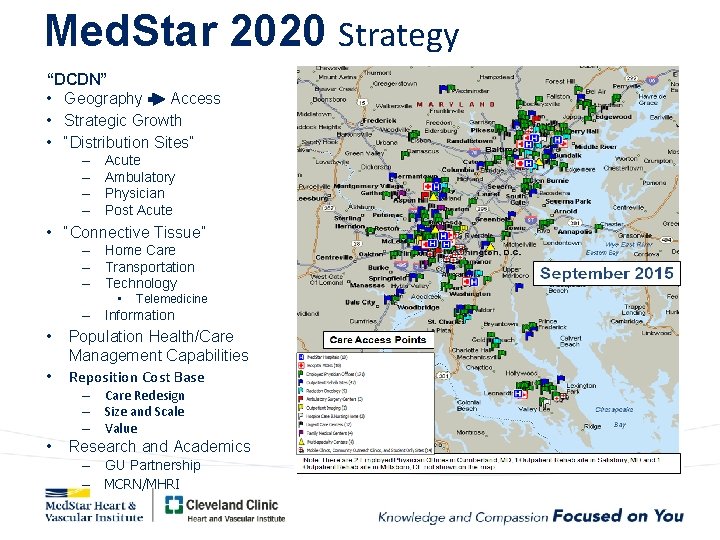
Med. Star 2020 Strategy “DCDN” • Geography Access • Strategic Growth • “Distribution Sites” – – Acute Ambulatory Physician Post Acute • “Connective Tissue” – Home Care – Transportation – Technology • Telemedicine – Information • • Population Health/Care Management Capabilities Reposition Cost Base – Care Redesign – Size and Scale – Value • Research and Academics – GU Partnership – MCRN/MHRI
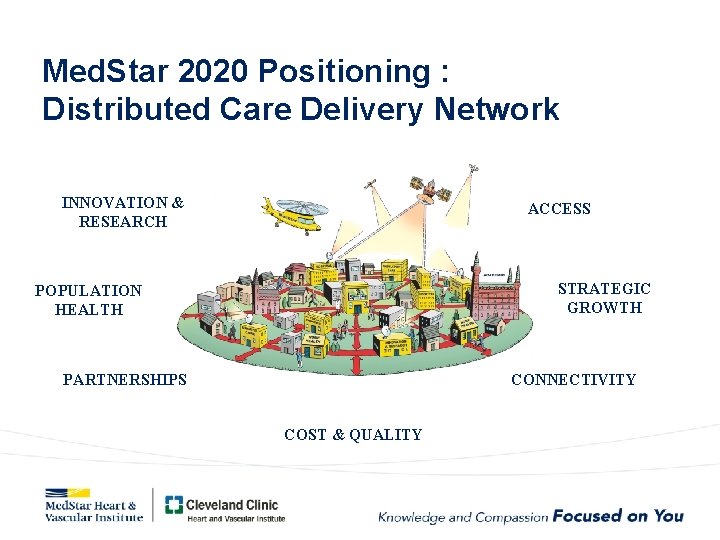
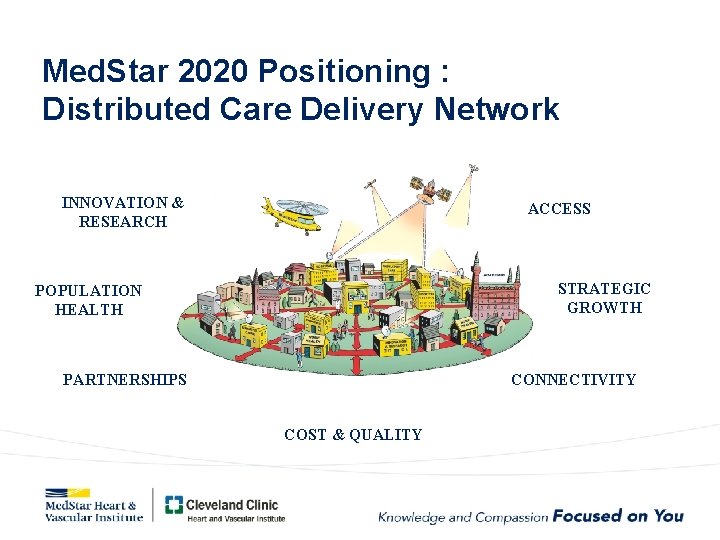
Med. Star 2020 Positioning : Distributed Care Delivery Network INNOVATION & RESEARCH ACCESS STRATEGIC GROWTH POPULATION HEALTH PARTNERSHIPS CONNECTIVITY COST & QUALITY
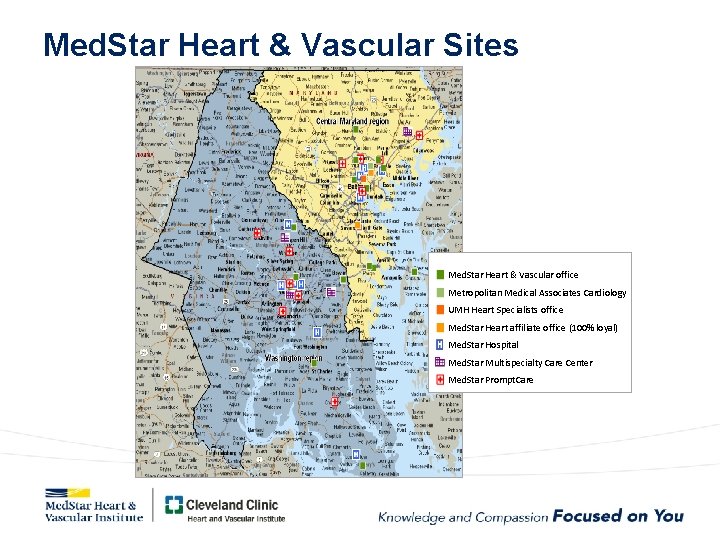
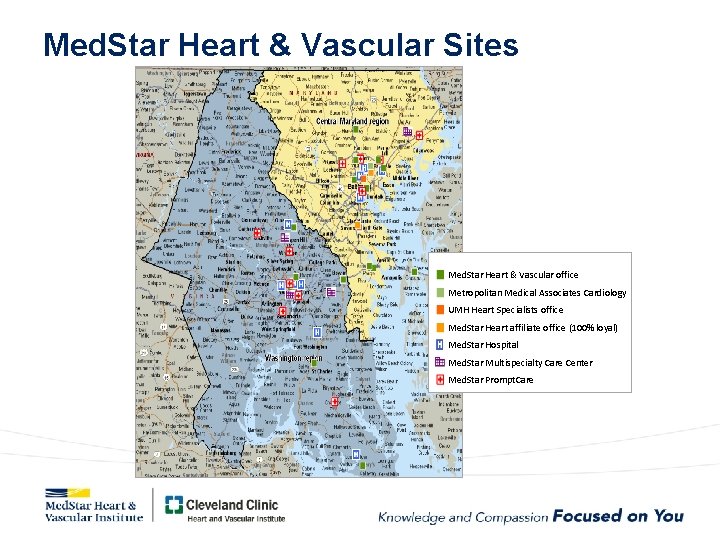
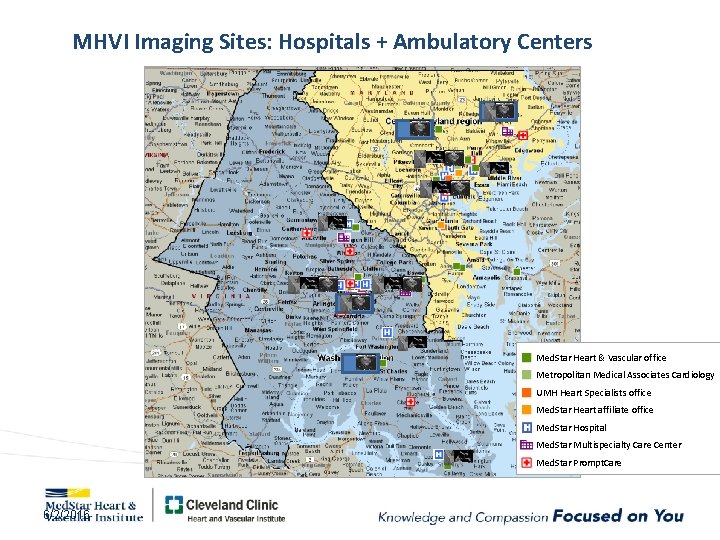
Med. Star Heart & Vascular Sites Med. Star Heart & Vascular office Metropolitan Medical Associates Cardiology UMH Heart Specialists office Med. Star Heart affiliate office (100% loyal) Med. Star Hospital Med. Star Multispecialty Care Center Med. Star Prompt. Care
Med. Star transport, Image. Share, Telemedicine, and Med. Connect ties it all together
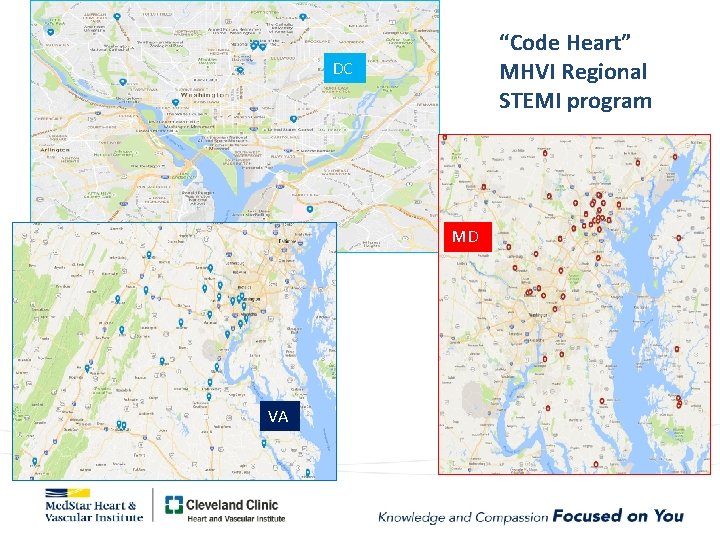
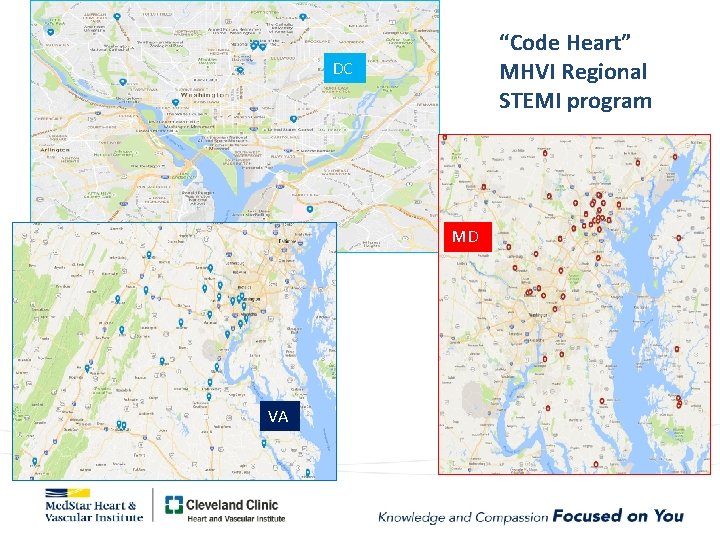
“Code Heart” MHVI Regional STEMI program DC MD VA
Systemwide MHVI service lines • • Cardiac surgery Vascular surgery Advanced heart failure Advanced cardiac imaging Research (MCRN) Cardiac electrophysiology Others in the future
Med. Star Heart and Vascular Institute Regional Collaborative for Noninvasive Imaging
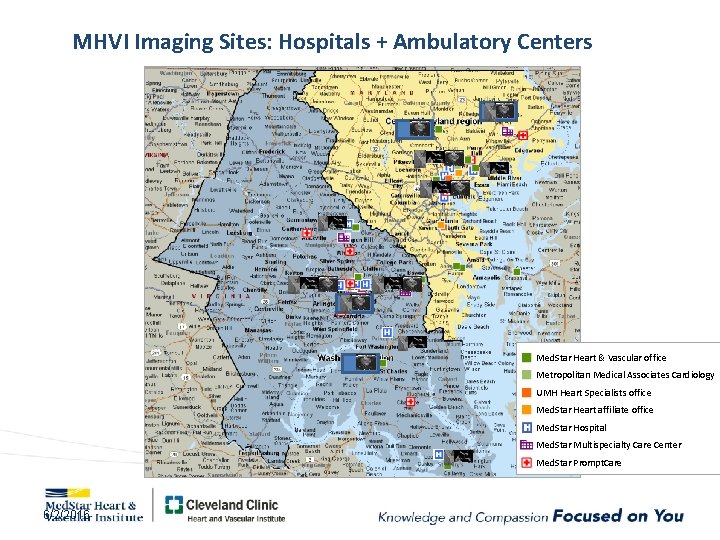
MHVI Imaging Sites: Hospitals + Ambulatory Centers Med. Star Heart & Vascular office Metropolitan Medical Associates Cardiology UMH Heart Specialists office Med. Star Heart affiliate office 32 Med. Star Hospital Med. Star Multispecialty Care Center Med. Star Prompt. Care 6/2/2016
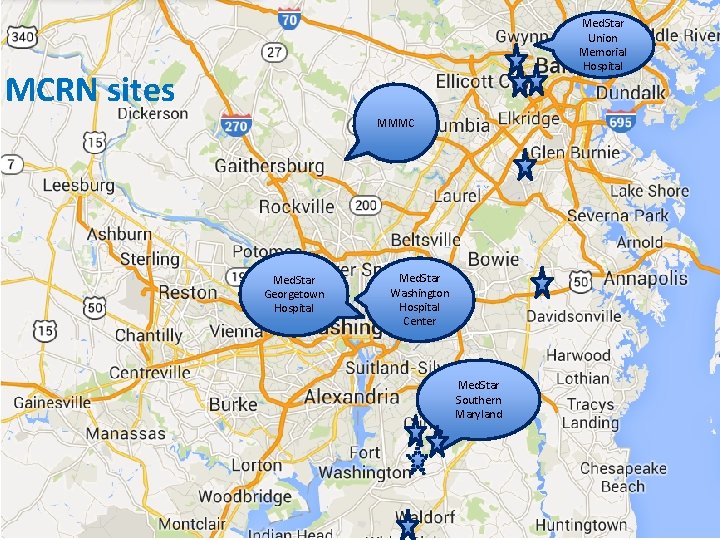
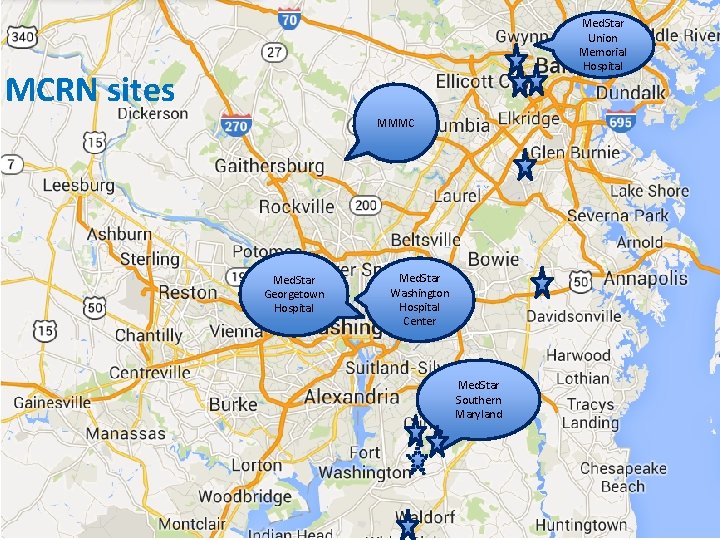
Med. Star Union Memorial Hospital MCRN sites MMMC Med. Star Georgetown Hospital 3/10/2021 Med. Star Washington Hospital Center Med. Star Southern Maryland 33
MHVI “niche” programs: the value of concentrated multidisciplinary expertise • • • Aortic diseases Pulmonary hypertension Cardiomyopathies Adult congenital heart disease Cardiogenetics Cardio-oncology
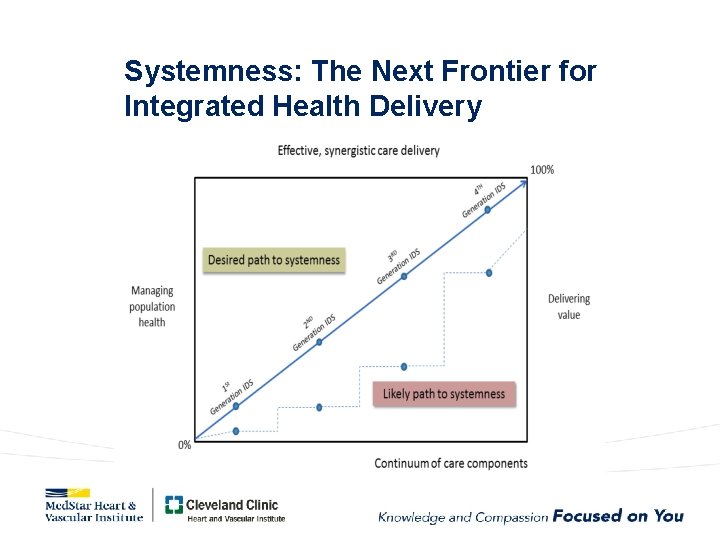
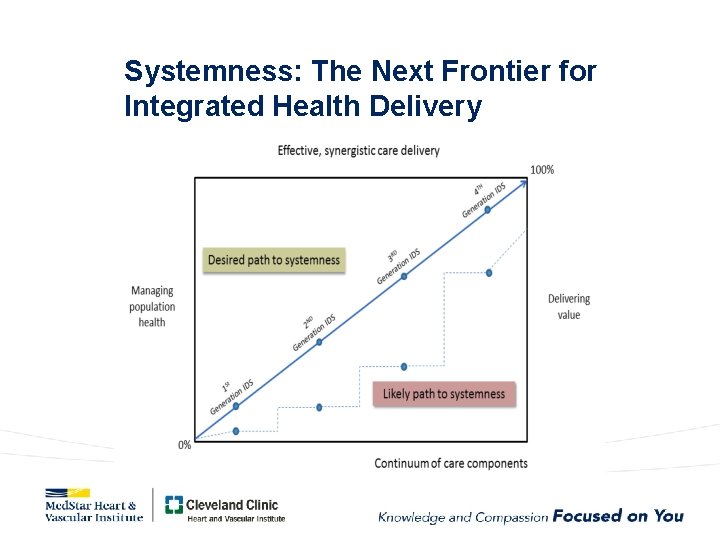
Systemness: The Next Frontier for Integrated Health Delivery
The Leadership Dyad: A clinical and administrative partnership • A philosophy, not a hierarchy, applied to every level of the healthcare organization from bedside to boardroom. • Both partners require analytic skill and emotional intelligence and must carry mutual respect for their differing and complementary expertise. • Both must be invested in optimizing system finance, operations, alignment with other service lines, and the integration of inpt/outpt as well as acute/chronic care.
“It is not the strongest or the most intelligent who will survive but those who can best manage change. ”

Respond to the marketplace. (Habbous District, Casablanca, Morocco, 2016)

Thank you. See you at CRT 2019!
 Gbmc medical records
Gbmc medical records Torrance memorial transitional care unit
Torrance memorial transitional care unit Cartersville medical center medical records
Cartersville medical center medical records Integrated electronic medical record
Integrated electronic medical record Integrated control center
Integrated control center Croydon tramlink extension
Croydon tramlink extension Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Chúa sống lại
Chúa sống lại Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Giọng cùng tên là
Giọng cùng tên là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Các số nguyên tố
Các số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết