SHOCK Pretest A patient was in a motorcycle




- Slides: 92
SHOCK
Pretest A patient was in a motorcycle accident. He is confused and hypotensive. What type of shock could he have? a) Hypovolemic b) Cardiogenic c) Distributive d) Obstructive
Pretest What statements about early hypovolemic shock are true? a) The patient may be alert and oriented. b) A patient may have a normal blood pressure. c) The patient may have a widened pulse pressure. d) The patient may not have a palpable femoral pulse. e) The patient may be tachycardic.
Pretest Which of the following signs might you find on examination in a patient with obstructive shock? a) High JVP b) Crepitations on chest auscultation c) Decreased breath sounds d) Tachycardia e) Subcutaneous emphysema
Pretest Which of the following can cause distributive shock? a) Myocardial infarction b) Burn c) Spinal cord injury d) Severe allergy / Anaphylaxis e) Sepsis
Pretest A 70 year old man has a history of chest pain with exertion. On examination he has a high JVP, an S 3 heart sound, and bilateral pulmonary crepitations. His RR = 30, PR = 115, BP = 90/60. Appropriate treatment includes: a) Give 1 L bolus of NS b) Give oxygen c) Give diuretic (I. e. Lasix) d) Insert chest tubes e) Give drug to reduce systemic vascular resistance
Pre-test 30 year old female has postpartum bleeding. She is restless. Vital signs: RR=30, BP=90/60, PR=130. Her weight appears to be 50 kg. Appropriate management includes: a) b) c) d) e) f) 1 - 2 litres of NS immediately 1 - 2 litres of D 5 W immediately At least 4 litres of NS immediately Close monitoring of vital signs and urine output Cross-match for blood transfusion as soon as possible Find and treat cause of bleeding
What Is Shock?
Shock • Body tissues are not properly perfused (not enough oxygen delivery) • Either the body cannot supply enough oxygen, or the cells cannot take up the oxygen • Cells become hypoxic and cannot function
Pathophysiology of Shock • Cardiac Output (CO) is the volume of blood pumped by heart in 1 minute CO = HR X SV HR = Heart rate (beats per minute) SV = Stroke volume (volume of blood ejected through heart per beat)
Pathophysiology of Shock • Mean Arterial Pressure (MAP) is the average blood pressure in a person MAP (approx) = CO X SVR CO = Cardiac output SVR = Systemic vascular resistance – If either decrease, the BP will decrease
Pathophysiology of Shock • Not enough blood flow cells starved for oxygen Production of lactic acid • Lactic acidosis Na+ floods into cells swell • Swelling of mitochondria in cells stops metabolism cells die
Physiological Response • How does the body respond to insufficient perfusion (not enough O 2 being delivered to major organs)?
Physiological Response • Body tries to increase CO and increase SVR to improve BP MAP (BP) = CO X SVR
What is the Cardiovascular Response? • • Heart rate increase Peripheral vasoconstriction Adrenalin release Central vasodilation to improve blood flow to heart, kidneys, brain
What is the Renal Response? • Increased release of renin-angiotensin • Increased Na+ reabsorption by kidneys to improve blood volume • Vasoconstriction to increase systemic SVR
What is the Neuroendocrine Response? • ADH release with increased water absorption by kidneys to improve blood volume
What do we need for perfusion?
Requirements for Perfusion • • Functioning pump Intact vascular system Adequate volume Adequate air exchange ** Failure of any one or more causes SHOCK
What are the Types of Shock?
What are the Types of Shock? • • Hypovolemic Cardiogenic Distributive Obstructive
What is Hypovolemic Shock?
What is Hypovolemic Shock? • Loss of blood or plasma – Decreased circulating blood volume within the total vascular capacity – Results in decreased diastolic filling pressures into heart
What are causes of Hypovolemic Shock?
What are causes of Hypovolemic Shock? • Hemorrhagic / Bleeding – Trauma • Intraabdominal / Retroperitoneal / Intrathoracic / Thighs – GI bleeding – Pregnancy related • Non Hemorrhagic – Plasma Loss • Dehydration – Vomiting / Diarrhea / Gastroenteritis – Interstitial Fluid Redistribution • • Peritonitis Severe Pancreatitis Burns Diabetic Ketoacidosis
What is Cardiogenic Shock?
What is Cardiogenic Shock? • Poor ventricular function because of loss of myocardial contractility (The heart pump is NOT working well) • Results in increased diastolic filling pressures and volumes in the heart
What are causes of Cardiogenic Shock?
What are causes of Cardiogenic Shock? • • Myocardial Infarction Cardiomyopathy Valvular disease Myocardial contusion – Patient may present with: • Congestive Heart Failure • Arrhythmias
What is Distributive Shock?
What is Distributive Shock? • Loss of vasomotor control resulting in arterial / venous dilatation • Characterized (after fluid resuscitation) by increased cardiac output and decreased SVR
What are causes of Distributive Shock?
What are causes of Distributive Shock? • Septic Shock – Vasodilation and increased vascular permeability (plasma volume loss) • Anaphylactic Shock – Vasodilation • Neurogenic Shock / Spinal Cord Injury – Loss of vasomotor control (no vasoconstriction)
What is Obstructive Shock?
What is Obstructive Shock? • Obstruction to flow in the cardiovascular system – Not due to poor cardiac ventricles – Blood cannot get into heart • impairment in diastolic filling – Blood cannot get out of heart • Excessive afterload
What are causes of Obstructive Shock?
What are causes of Obstructive Shock? • Impaired Diastolic Filling (Decreased ventricle preload) – Tension pneumothorax – Cardiac tamponade – Constrictive pericarditis • Impaired Systolic Contraction (Increased ventricle afterload) – Pulmonary embolism (large) – Acute pulmonary hypertension
Common Effects of Shock on Organs • Systemic – Capillary leak, cytokine release • CV – Depression of cardiac function, arrhythmia • Hematology – DIC, coagulopathy, bone marrow suppression, platelet dysfunction
Common Effects of Shock on Organs • Hepatic – Elevation of liver enzymes, coagulopathy, hepatic failure • Neuroendocrine – Adrenal suppression, insulin resistance • Renal – Acute kidney injury, increased creatinine and BUN
General Approach • Primary Survey – A: Airway – B: Breathing – C: Circulation – D: Disability – E: Exposure Assess Resuscitate Monitor • History and Secondary Survey • Continue to monitor / Arrange transport
Monitoring • Regular and ongoing monitoring is very important – Respiratory rate – Pulse rate – Blood pressure – Temperature – Urine output • Minimum urine output in adult is 0. 5 ml/kg/hr – Level of consciousness (i. e. Glasgow coma scale)
Common Mistakes in Managing Shock • Patient assessment is not thorough • Symptoms and signs of a serious illness are not recognized • Appropriate and urgent care is not provided • Patient is not regularly monitored
PATIENT HISTORY will usually indicate the cause of the shock
Circulation • Assess – Inspect: • Colour (pale / cyanosis) • Temperature of skin • Dilated neck veins • Dry mucous membranes – Palpate: • Pulse rate and character (compare peripheral and central pulse) • Capillary refill / Skin turgor • Character and location of cardiac apex beat – Auscultate: • BP • Heart sounds / Extra heart sounds / Murmurs
Circulation • Remember the signs of heart failure – – – Tachycardia Raised JVP (often not seen in infants with heart failure) Lung crepitations on auscultation Enlarged liver … and listen for a heart murmur
What are the signs of Early Shock?

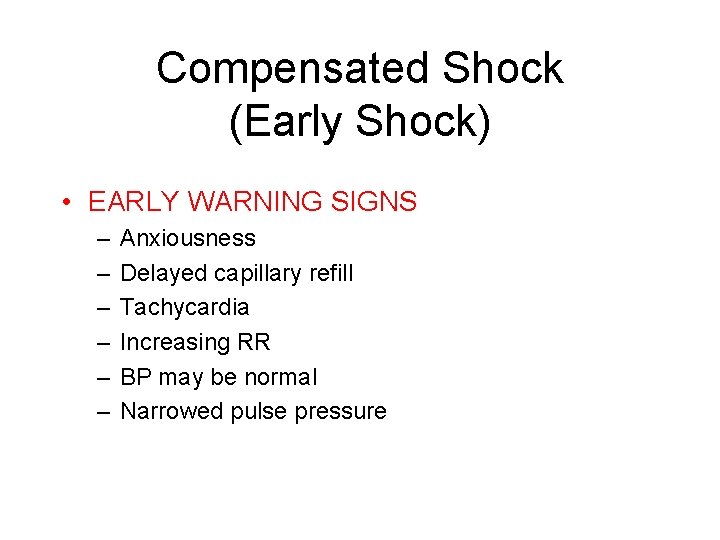
Early Shock • Early shock may have few symptoms or signs in young healthy patients – Healthy cardiovascular system compensates • Older patients may show signs and symptoms earlier – Cardiovascular system is less capable to compensate
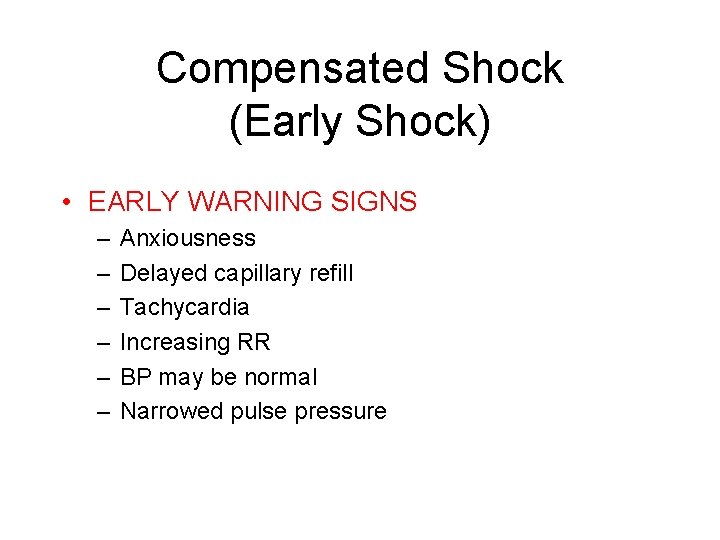
Compensated Shock (Early Shock) • EARLY WARNING SIGNS – – – Anxiousness Delayed capillary refill Tachycardia Increasing RR BP may be normal Narrowed pulse pressure
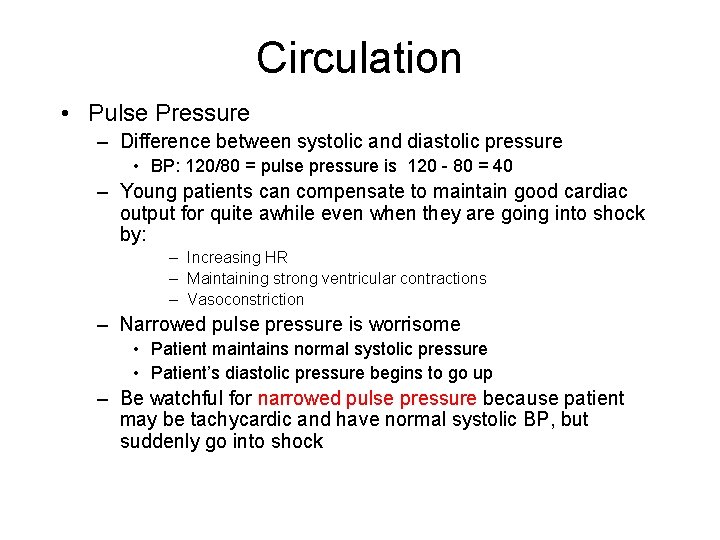
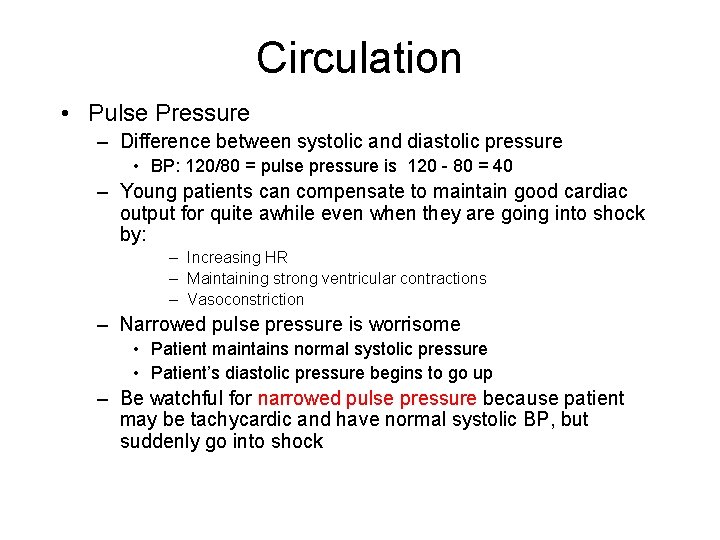
Circulation • Pulse Pressure – Difference between systolic and diastolic pressure • BP: 120/80 = pulse pressure is 120 - 80 = 40 – Young patients can compensate to maintain good cardiac output for quite awhile even when they are going into shock by: – Increasing HR – Maintaining strong ventricular contractions – Vasoconstriction – Narrowed pulse pressure is worrisome • Patient maintains normal systolic pressure • Patient’s diastolic pressure begins to go up – Be watchful for narrowed pulse pressure because patient may be tachycardic and have normal systolic BP, but suddenly go into shock
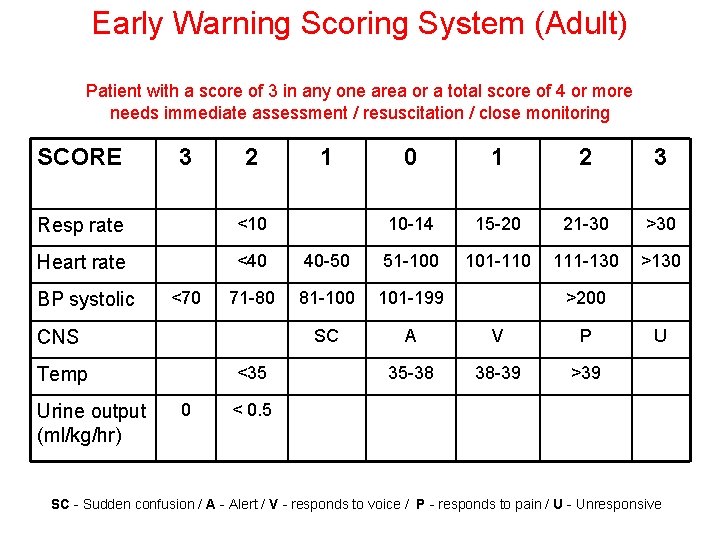
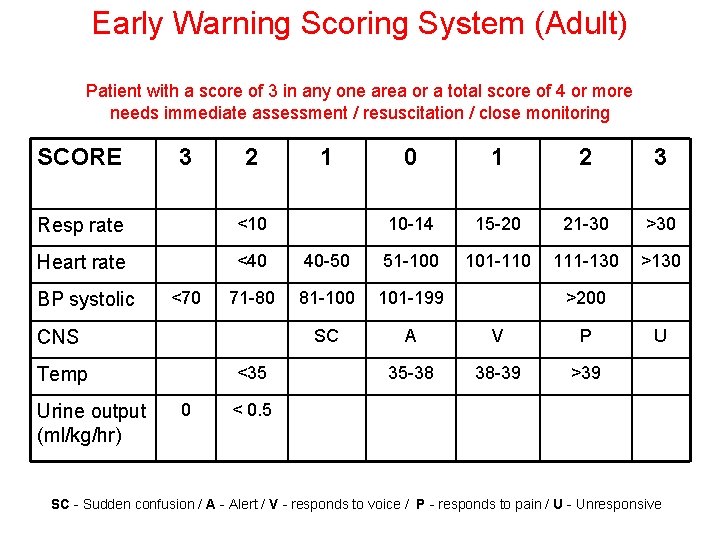
Early Warning Scoring System (Adult) Patient with a score of 3 in any one area or a total score of 4 or more needs immediate assessment / resuscitation / close monitoring SCORE 3 2 1 0 1 2 3 10 -14 15 -20 21 -30 >30 101 -110 111 -130 >130 Resp rate <10 Heart rate <40 40 -50 51 -100 71 -80 81 -100 101 -199 SC A V P 35 -38 38 -39 >39 BP systolic <70 CNS <35 Temp Urine output (ml/kg/hr) 0 >200 U < 0. 5 SC - Sudden confusion / A - Alert / V - responds to voice / P - responds to pain / U - Unresponsive
REMEMBER • Closely Monitor – Pulse rate / BP – Urine output – O 2 saturation (if available)
What are the signs of Late Shock?
Decompensated Shock (Late Shock) • • • Decreased consciousness BP drops Weak, thready pulse (may slow) Weak, ineffective respirations (may slow( Irreversible shock – occurs when the body can no longer deliver sufficient oxygen to organs
Management of Hypovolemic Shock
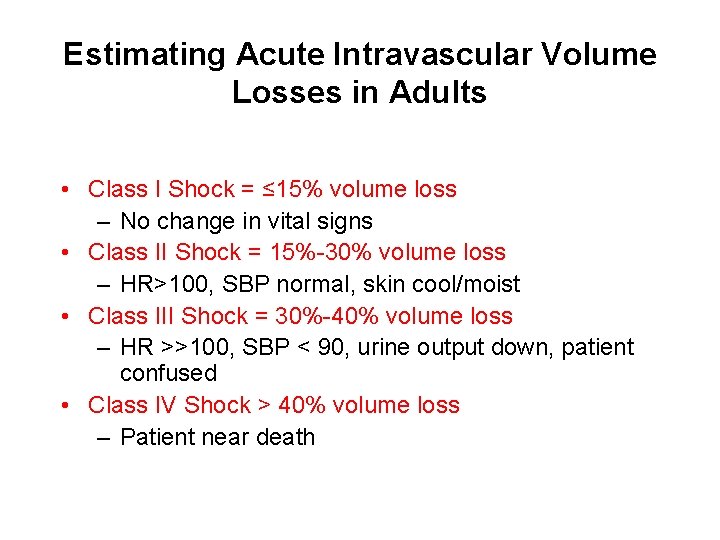
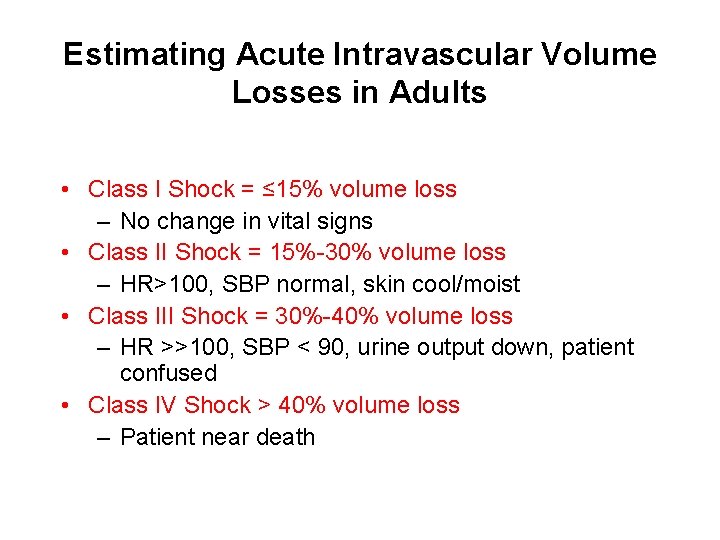
Estimating Acute Intravascular Volume Losses in Adults • Class I Shock = ≤ 15% volume loss – No change in vital signs • Class II Shock = 15%-30% volume loss – HR>100, SBP normal, skin cool/moist • Class III Shock = 30%-40% volume loss – HR >>100, SBP < 90, urine output down, patient confused • Class IV Shock > 40% volume loss – Patient near death
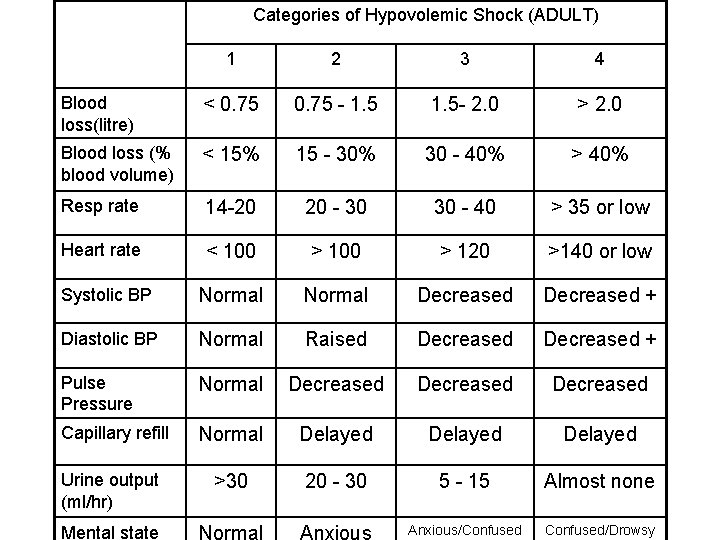
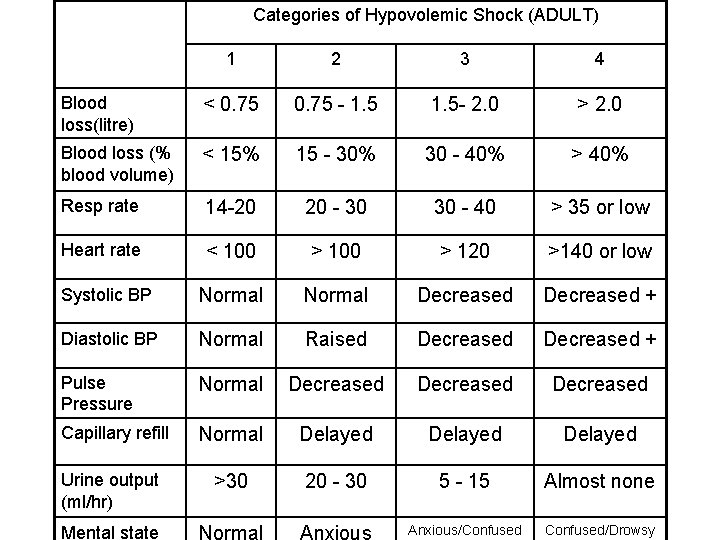
Categories of Hypovolemic Shock (ADULT) 1 2 3 4 Blood loss(litre) < 0. 75 - 1. 5 - 2. 0 > 2. 0 Blood loss (% blood volume) < 15% 15 - 30% 30 - 40% > 40% Resp rate 14 -20 20 - 30 30 - 40 > 35 or low Heart rate < 100 > 120 >140 or low Systolic BP Normal Decreased + Diastolic BP Normal Raised Decreased + Pulse Pressure Normal Decreased Capillary refill Normal Delayed Urine output (ml/hr) >30 20 - 30 5 - 15 Almost none Anxious/Confused/Drowsy Mental state
Estimating Blood Loss • Patients with Class I or II shock who stabilize with NS or RL often do not need transfusions • Patients with Class III or IV shock usually require transfusions
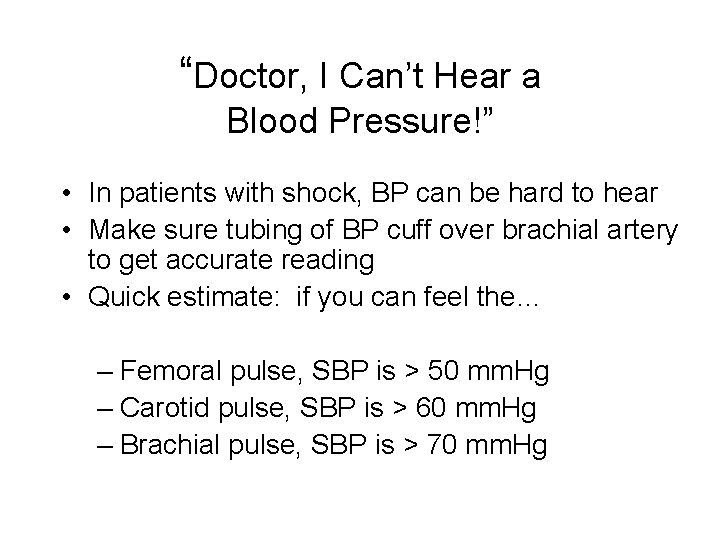
“Doctor, I Can’t Hear a Blood Pressure!” • In patients with shock, BP can be hard to hear • Make sure tubing of BP cuff over brachial artery to get accurate reading • Quick estimate: if you can feel the… – Femoral pulse, SBP is > 50 mm. Hg – Carotid pulse, SBP is > 60 mm. Hg – Brachial pulse, SBP is > 70 mm. Hg
Hypovolemic Shock • Estimate Fluid Resuscitation – Circulating blood volume: • 70 cc/kg in adult male – Interstitial fluid volume: • 2 X circulating blood volume • Significant amount of IV fluid goes interstitial

Estimate Volume Resuscitation (Adult) • Estimate volume deficit using vital signs and patient’s weight • Replace the estimated volume loss with 3 times that amount of normal saline… to replace intravascular and interstitial loss • 60 kg male with HR>100, BP = 110/70 – Normal total circulating volume = 70 cc/kg x 60 kg = 4200 cc – 20% fluid deficit based on vital signs –. 20 X 4200 cc = 840 cc deficit – 840 cc X 3 = 2520 cc NS needed – Patient needs > 2 litres of NS or RL
Why Multiply Normal Saline 3 Times? • NS or RL are the best fluids to replace lost volume because they are isotonic • 2/3 of the NS or RL given goes out of the blood vessels into the interstitial space • Must give 3 cc for every 1 cc of fluid deficit
Target Vital Signs • Goals of fluid resuscitation – Good peripheral perfusion (warm and dry skin, capillary refill < 2 seconds) – Awake and oriented – SBP = 90 or better – Heart rate < 100 – Urine output for adults: 0. 5 cc/kg/hr
Hypovolemic Shock in Children
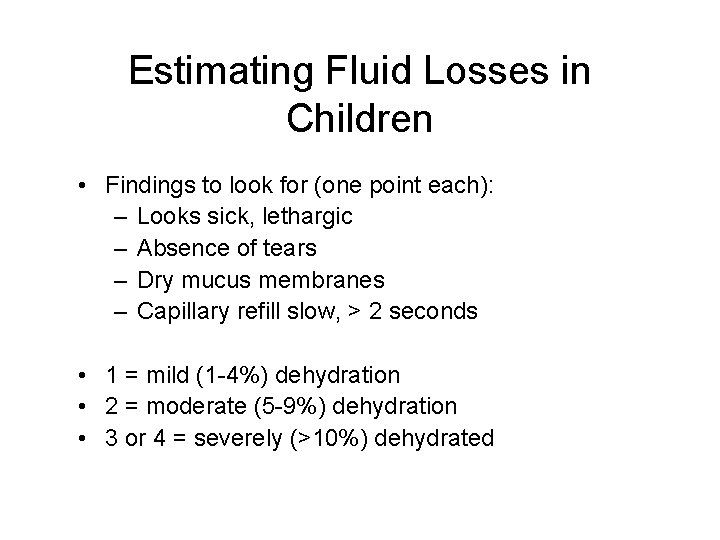
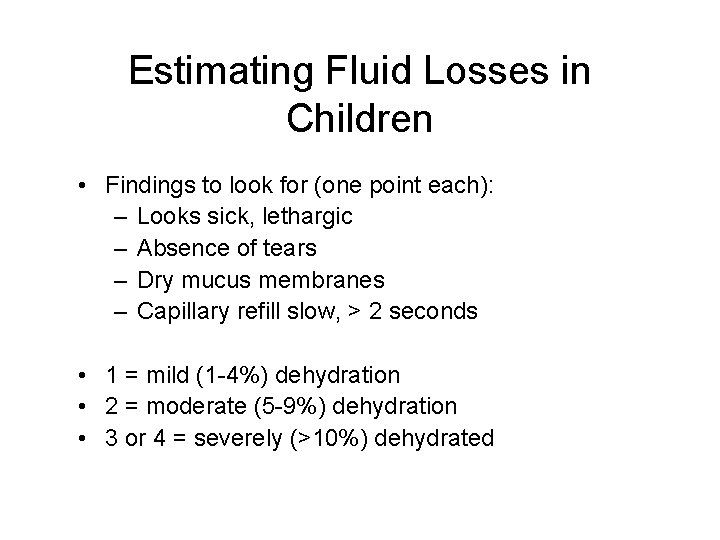
Estimating Fluid Losses in Children • Findings to look for (one point each): – Looks sick, lethargic – Absence of tears – Dry mucus membranes – Capillary refill slow, > 2 seconds • 1 = mild (1 -4%) dehydration • 2 = moderate (5 -9%) dehydration • 3 or 4 = severely (>10%) dehydrated
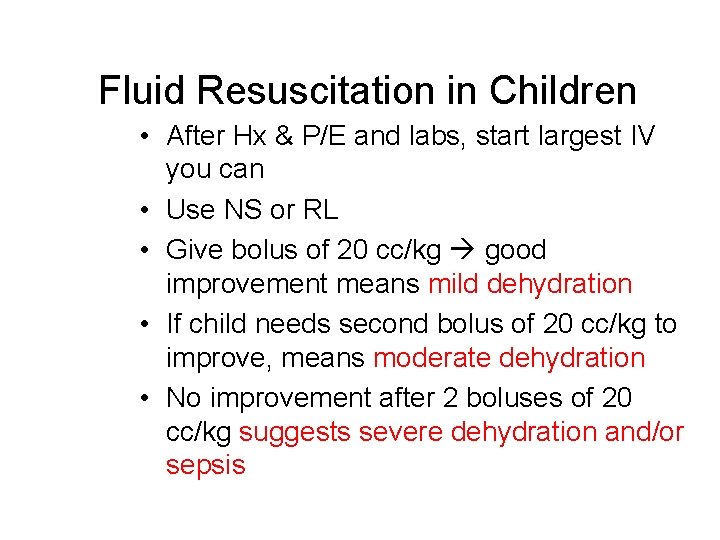
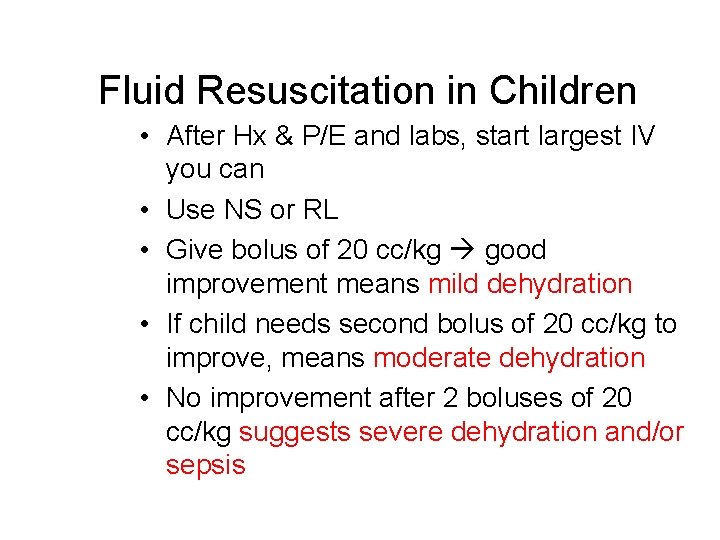
Fluid Resuscitation in Children • After Hx & P/E and labs, start largest IV you can • Use NS or RL • Give bolus of 20 cc/kg good improvement means mild dehydration • If child needs second bolus of 20 cc/kg to improve, means moderate dehydration • No improvement after 2 boluses of 20 cc/kg suggests severe dehydration and/or sepsis
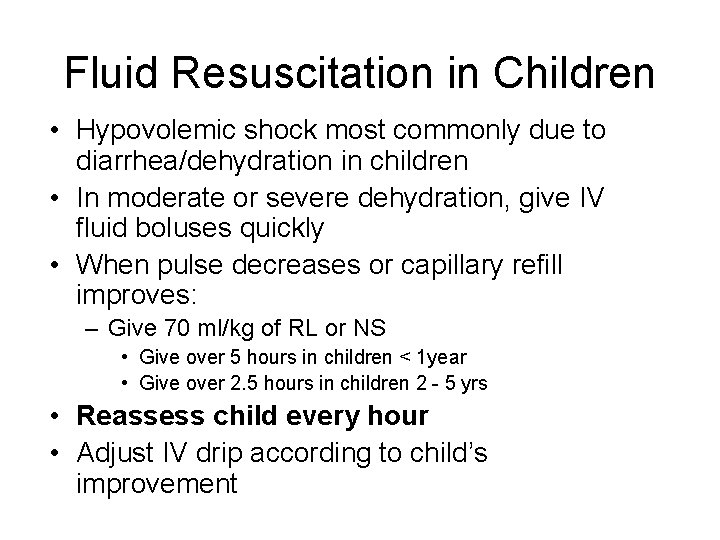
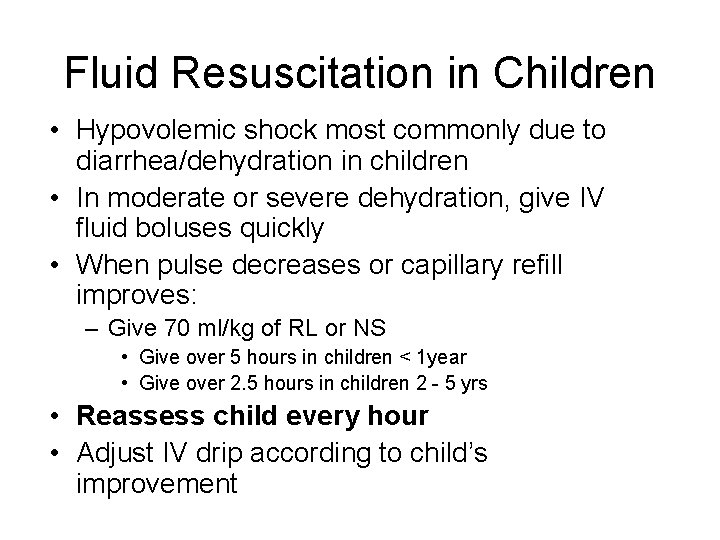
Fluid Resuscitation in Children • Hypovolemic shock most commonly due to diarrhea/dehydration in children • In moderate or severe dehydration, give IV fluid boluses quickly • When pulse decreases or capillary refill improves: – Give 70 ml/kg of RL or NS • Give over 5 hours in children < 1 year • Give over 2. 5 hours in children 2 - 5 yrs • Reassess child every hour • Adjust IV drip according to child’s improvement

Normal Vital Signs in Children Age HR RR Systolic BP < 6 months 90 - 180 25 -60 65 -110 6 months - 2 yrs 90 - 170 25 - 40 90 - 110 2 - 5 yrs 90 - 140 20 - 30 90 - 110 5 - 7 yrs 65 - 130 18 - 25 100 - 120 Children should make > 1 ml/ kg/ hr of urine
Venous Access Problems • Often hard to start IVs in dehydrated children • Consider: – External jugular vein – Femoral vein – Intraosseous infusion into proximal medial tibia
Management of Cardiogenic Shock
Cardiogenic Shock Signs and Symptoms • Patients may present with chest pain due to myocardial infarction or have history of cardiovascular disease • SBP, cardiac output (CO), oxygen saturation and urine output LOW • Heart rate, respiratory rate fast • Patient may have cool, skin, crepitations, S 3 heart sound, high JVP
Cardiogenic Shock Management • Oxygen: if O 2 sat does not improve on oxygen, consider intubation • Give fluid cautiously / May need diuretic if congestive heart failure • Diagnosis: EKG, CXR, Echo (if possible) • High mortality / ? Patient transfer / ? Patient may need pressors
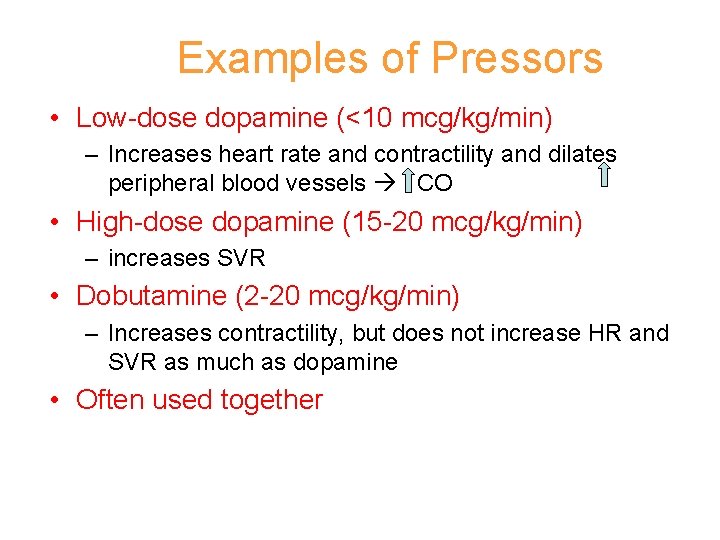
Examples of Pressors • Low-dose dopamine (<10 mcg/kg/min) – Increases heart rate and contractility and dilates peripheral blood vessels CO • High-dose dopamine (15 -20 mcg/kg/min) – increases SVR • Dobutamine (2 -20 mcg/kg/min) – Increases contractility, but does not increase HR and SVR as much as dopamine • Often used together
Distributive Shock • Problem: severe arterial and venous dilation SVR • Sepsis is most common cause • 30 -50% mortality, especially children and elderly pts
Management of Septic Shock • Goals • • – Improve BP – Correct dehydration – Treat source of infection Give 20 ml/kg rapid bolus of NS or RL (1 -2 L in adult) Try to identify source of infection Give broad spectrum antibiotics (i. e. ceftriaxone, gentamicin) Transfer early if no improvement to treatment (may need pressors if severe)
Management of Anaphylactic Shock • Give oxygen • Give epineprhine / adrenalin 0. 5 mg IM – Repeat every 5 minutes until BP improves • Give NS or RL 20 mg/kg IV bolus • Give antihistamine – Give IV initially – Continue po for 48 hours • May need to administeroids
Obstructive Shock • Need to treat the etiology • Tension pneumothorax – CXR will confirm – Treatment: Needle decompression / chest tube • Cardiac tamponade – Echo will confirm – Treatment: Pericardial tap • Pulmonary embolus – CT will confirm – Treatment: Anticoagulation
Summary • HISTORY will almost always help you to know the type of shock the patient has • Be thorough in patient assessment • Start resuscitation immediately • Continue to monitor • Arrange transfer early if no improvement
Summary • Resuscitate – Hypovolemic shock • • Large bore IV (16 or 18 gauge) / Start two IV’s Give 2 litres of isotonic fluid quickly Consider giving blood Control hemorrhage / Call surgery – Cardiogenic shock • Careful with fluid / Drugs to improve cardiac function / Drugs for pulmonary edema – Distributive shock • Septic shock – IV isotonic fluid bolus & IV antibiotics (broad spectrum) • Anaphylactic shock – IV isotonic fluid bolus & epinephrine – Obstructive shock • Treat cause
Summary • Hypovolemic shock most common – In young adults and children, SBP is a late indicator of volume statu – Normal Saline or Ringer’s Lactate are acceptable volume resuscitation fluids (isotonic) – Do not use D 5 W for resuscitation – Look for cause of volume loss while administering fluids – Order blood early
Summary • Signs of success in hypovolemic shock: – – – – Warm extremities Good mentation SBP>90, HR <100 Urine output 0. 5 cc/kg/hour for adults Urine output 1. 0 cc/kg/hr for children Cause of bleeding / fluid loss found Therapeutic intervention to treat the cause of bleeding
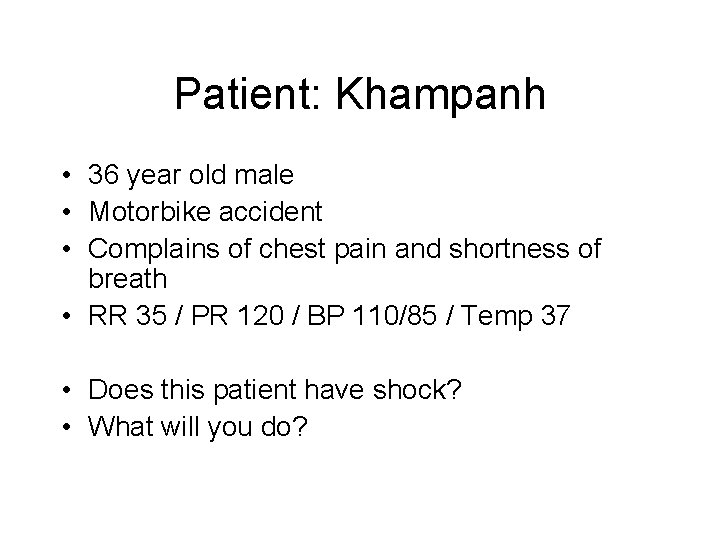
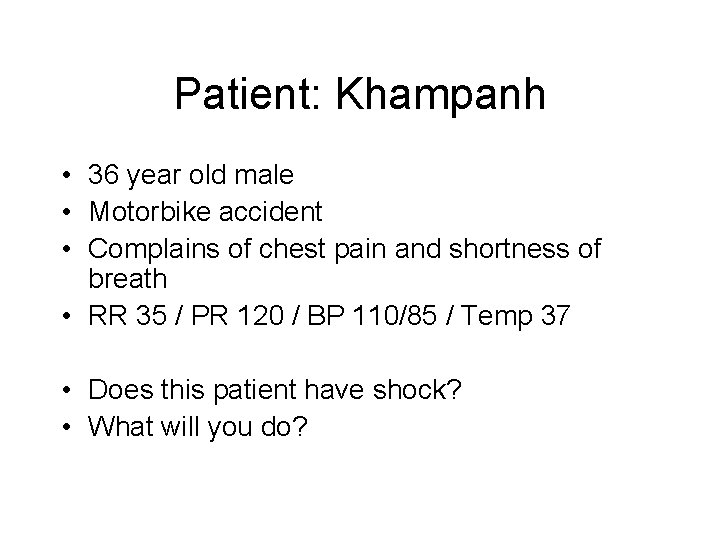
Patient: Khampanh • 36 year old male • Motorbike accident • Complains of chest pain and shortness of breath • RR 35 / PR 120 / BP 110/85 / Temp 37 • Does this patient have shock? • What will you do?
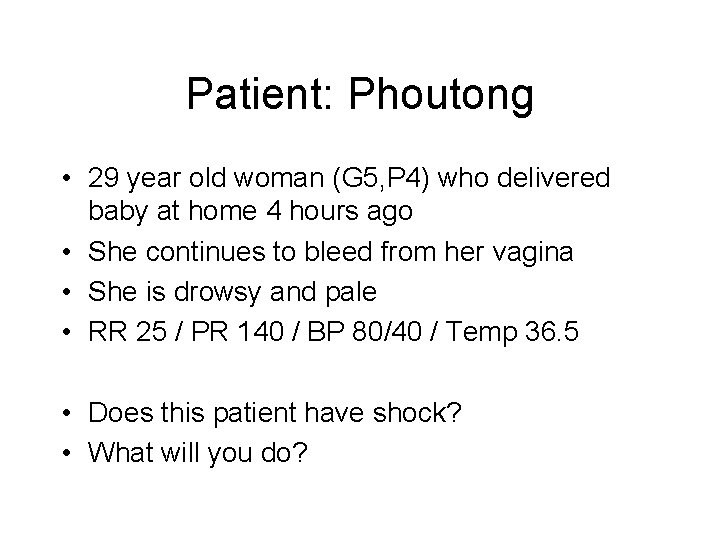
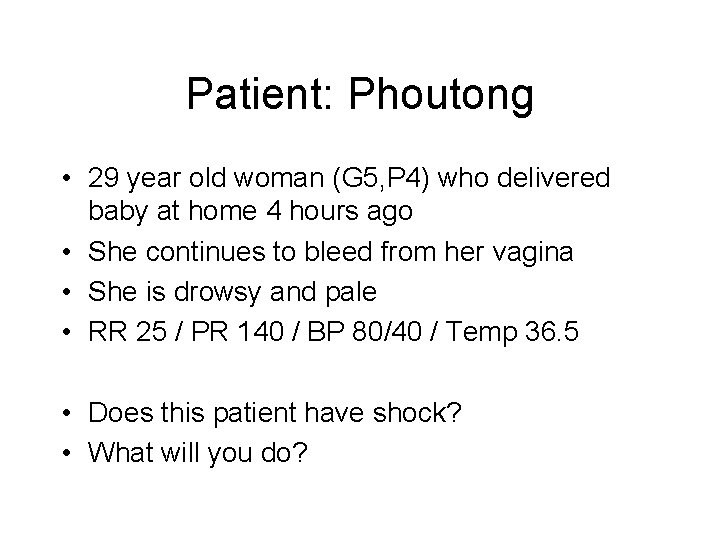
Patient: Phoutong • 29 year old woman (G 5, P 4) who delivered baby at home 4 hours ago • She continues to bleed from her vagina • She is drowsy and pale • RR 25 / PR 140 / BP 80/40 / Temp 36. 5 • Does this patient have shock? • What will you do?
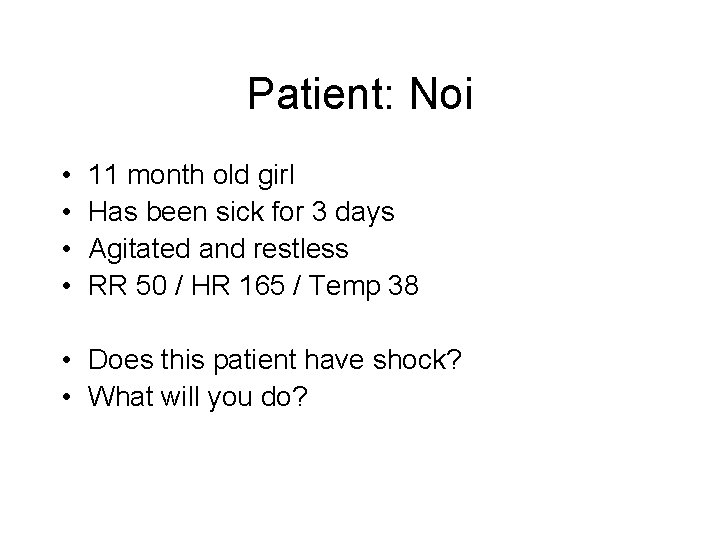
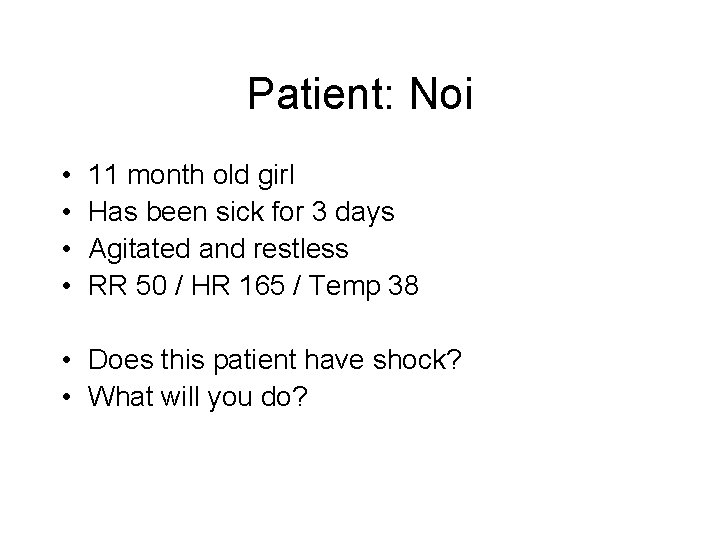
Patient: Noi • • 11 month old girl Has been sick for 3 days Agitated and restless RR 50 / HR 165 / Temp 38 • Does this patient have shock? • What will you do?
Give me examples of patients who had shock that you treated • Is there anything you could have done differently that may have improved patient care or outcome?
Ideas • How could you improve management of patients presenting with shock at your health care setting?
Post-test A patient was in a motorcycle accident. He is confused and hypotensive. What type of shock could he have? a) Hypovolemic b) Cardiogenic c) Distributive d) Obstructive
Post-test What statements about early hypovolemic shock are true? a) The patient may be alert and oriented. b) A patient may have a normal blood pressure. c) The patient may have a widened pulse pressure. d) The patient may not have a palpable femoral pulse. e) The patient may be tachycardic.
Post-test Which of the following signs might you find on examination in a patient with obstructive shock? a) High JVP b) Crepitations on chest auscultation c) Decreased breath sounds d) Tachycardia e) Subcutaneous emphysema
Post-test Which of the following can cause distributive shock? a) Myocardial infarction b) Burn c) Spinal cord injury d) Severe allergy / Anaphylaxis e) Sepsis

Post-test A 70 year old man has a history of chest pain with exertion. On examination he has a high JVP, an S 3 heart sound, and bilateral pulmonary crepitations. His RR = 30, PR = 115, BP = 90/60. Appropriate treatment includes: a) Give 1 L bolus of NS b) Give oxygen c) Give diuretic (I. e. Lasix) d) Insert chest tubes e) Give drug to reduce systemic vascular resistance
Post-test 30 year old female has postpartum bleeding. She is restless. Vital signs: RR=30, BP=90/60, PR=130. Her weight appears to be 50 kg. Appropriate management includes: a) b) c) d) e) f) 1 - 2 litres of NS immediately 1 - 2 litres of D 5 W immediately At least 4 litres of NS immediately Close monitoring of vital signs and urine output Cross-match for blood transfusion as soon as possible Find and treat cause of bleeding
Questions
 Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Site:slidetodoc.com
Site:slidetodoc.com Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Shock normovolemico
Shock normovolemico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Patient 2 patient
Patient 2 patient Pretest: growth, development, and sexuality
Pretest: growth, development, and sexuality Wound care pretest
Wound care pretest Proxy pretest
Proxy pretest Pepp pretest
Pepp pretest Which two sentences contain a restrictive clause?
Which two sentences contain a restrictive clause? Whats a pretest
Whats a pretest Pretest publicitario ejemplo
Pretest publicitario ejemplo Slipes
Slipes Repetition structure in c++
Repetition structure in c++ Medication administration test answers
Medication administration test answers Identify the part of speech
Identify the part of speech Pretest communism and the cold war
Pretest communism and the cold war Hdmaster map
Hdmaster map Pretest: art in the 20th century and today
Pretest: art in the 20th century and today Injectable medication administration pretest
Injectable medication administration pretest Isquemia miocardica
Isquemia miocardica Proxy pretest design
Proxy pretest design Pretest: developing an academic and career plan
Pretest: developing an academic and career plan Pretest: the universe
Pretest: the universe Starcom motorcycle intercom
Starcom motorcycle intercom A motion map for a motorcycle is shown
A motion map for a motorcycle is shown Velocity=distance/time
Velocity=distance/time Basic rider course michigan
Basic rider course michigan Drag racing sponsorship packages
Drag racing sponsorship packages Maryland motorcycle safety program
Maryland motorcycle safety program Jose has just played a long bruising football game
Jose has just played a long bruising football game An nguyen motorcycle
An nguyen motorcycle Wmtc test cycle
Wmtc test cycle Ardie motorcycle
Ardie motorcycle Automobile car motorcycle venn diagram
Automobile car motorcycle venn diagram Erider team oregon
Erider team oregon Sonder motorcycle
Sonder motorcycle Cesar scheme
Cesar scheme Vertical motion examples
Vertical motion examples National bikers roundup
National bikers roundup The mouse and the motorcycle chapter 1
The mouse and the motorcycle chapter 1 Flip flops on motorcycle
Flip flops on motorcycle I go to school by motorcycle
I go to school by motorcycle Icd 10 kll
Icd 10 kll A 250 kg motorcycle is driven around a 12 meter tall
A 250 kg motorcycle is driven around a 12 meter tall The motorcycle project
The motorcycle project Explanation
Explanation A motorcycle undergoes acceleration when
A motorcycle undergoes acceleration when Oregon motorcycle training
Oregon motorcycle training Motorcycle riders foundation
Motorcycle riders foundation Car engine size chart
Car engine size chart Giacomo balla speed of a motorcycle
Giacomo balla speed of a motorcycle Che guevara quotes motorcycle diaries
Che guevara quotes motorcycle diaries Bondservants motorcycle
Bondservants motorcycle Kf memory case study
Kf memory case study Iso motorcycle
Iso motorcycle Earth shock in physiotherapy
Earth shock in physiotherapy Class of shock
Class of shock Wave shock marine biology
Wave shock marine biology Comfort devices bibliography
Comfort devices bibliography Criteria of shock
Criteria of shock Golden hour politrauma
Golden hour politrauma Compensated shock
Compensated shock Simile for shock
Simile for shock Unit 1 post test
Unit 1 post test William schnettler
William schnettler Shawn dowling
Shawn dowling Shock and vibration symposium
Shock and vibration symposium Pulmonary toilet
Pulmonary toilet Anaphylactic shock
Anaphylactic shock Aggregate supply equation
Aggregate supply equation Shock caldo e freddo
Shock caldo e freddo Brass v drape
Brass v drape Inotropes drugs
Inotropes drugs Momentary shock
Momentary shock Types of haemorrhage
Types of haemorrhage Shock prof
Shock prof Emergency drugs
Emergency drugs Neurogenic shock
Neurogenic shock Shock hipovolemico clasificacion
Shock hipovolemico clasificacion Damper dynamometer
Damper dynamometer Secondo shock petrolifero
Secondo shock petrolifero Ync shock
Ync shock Progressive stage of shock
Progressive stage of shock Md facs definition
Md facs definition Shock stall
Shock stall Distributive shock
Distributive shock Tipos de shock
Tipos de shock Osmotic shock
Osmotic shock Anaphylactic shock hemodynamics
Anaphylactic shock hemodynamics Decompensated shock
Decompensated shock Hoeveel bloedverlies shock
Hoeveel bloedverlies shock