Circulatory shock Vasopressors Shock definition Shock is the

- Slides: 21
Circulatory shock Vasopressors
Shock: definition Shock is the physiologic state characterized by significant reduction of systemic tissue perfusion, resulting in decreased tissue oxygen delivery. This creates an imbalance between oxygen delivery and oxygen consumption. Prolonged oxygen deprivation leads to cellular hypoxia and derangement of critical biochemical processes at the cellular level, which can progress to the systemic level
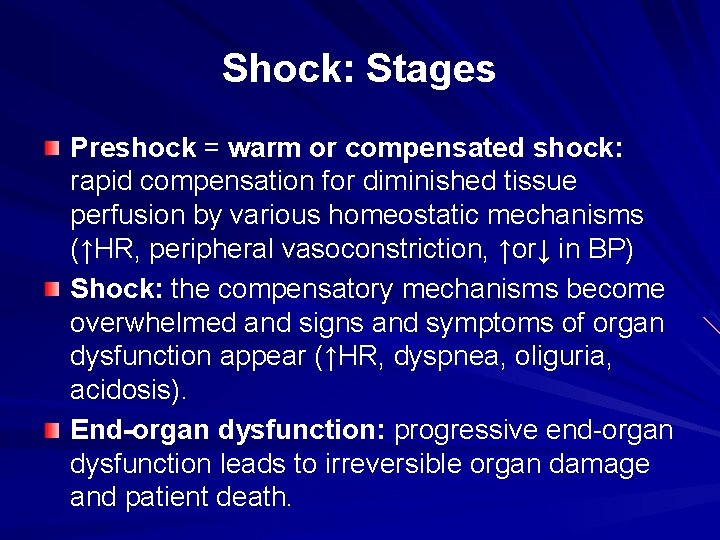
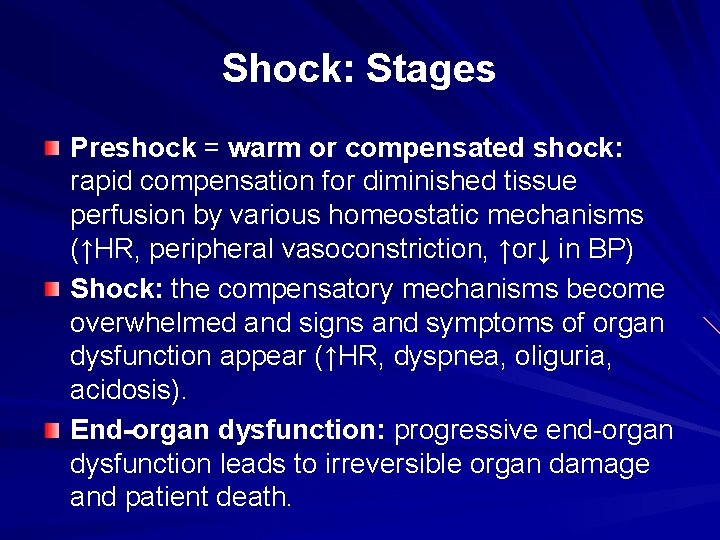
Shock: Stages Preshock = warm or compensated shock: rapid compensation for diminished tissue perfusion by various homeostatic mechanisms (↑HR, peripheral vasoconstriction, ↑or↓ in BP) Shock: the compensatory mechanisms become overwhelmed and signs and symptoms of organ dysfunction appear (↑HR, dyspnea, oliguria, acidosis). End-organ dysfunction: progressive end-organ dysfunction leads to irreversible organ damage and patient death.
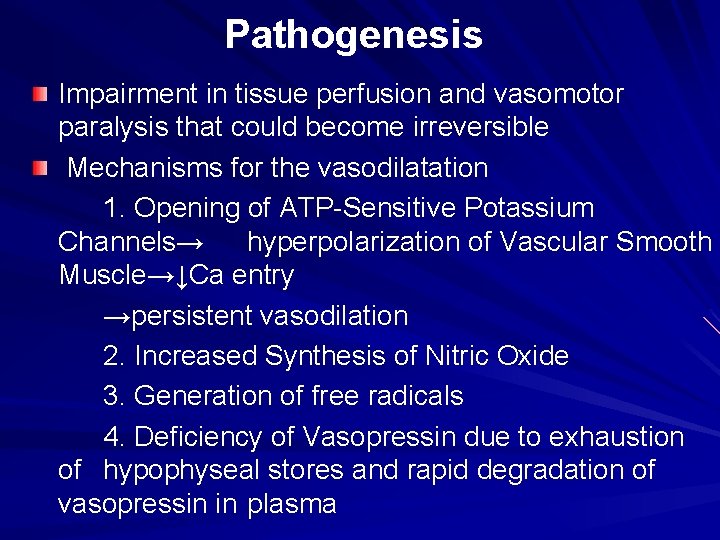
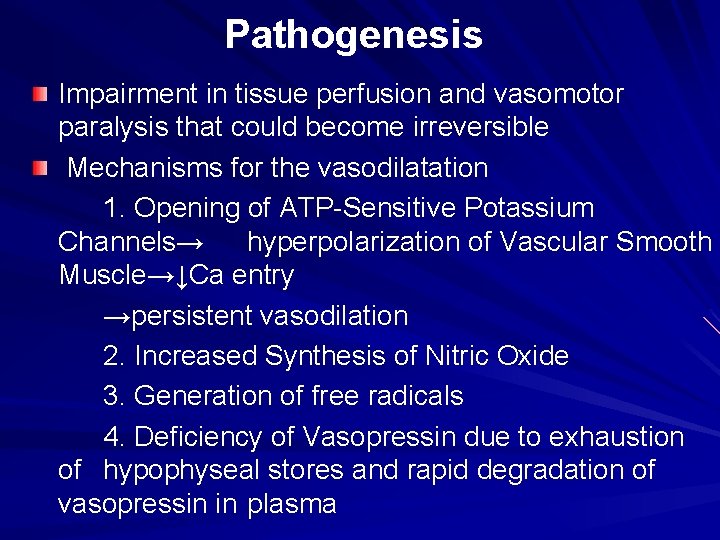
Pathogenesis Impairment in tissue perfusion and vasomotor paralysis that could become irreversible Mechanisms for the vasodilatation 1. Opening of ATP-Sensitive Potassium Channels→ hyperpolarization of Vascular Smooth Muscle→↓Ca entry →persistent vasodilation 2. Increased Synthesis of Nitric Oxide 3. Generation of free radicals 4. Deficiency of Vasopressin due to exhaustion of hypophyseal stores and rapid degradation of vasopressin in plasma
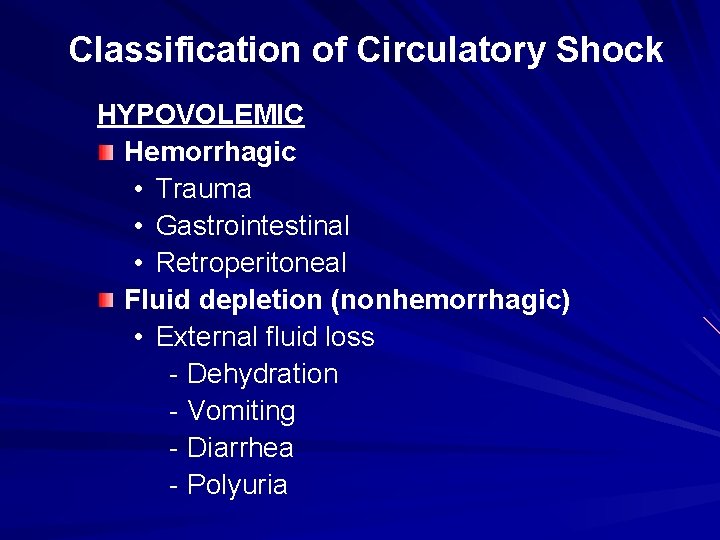
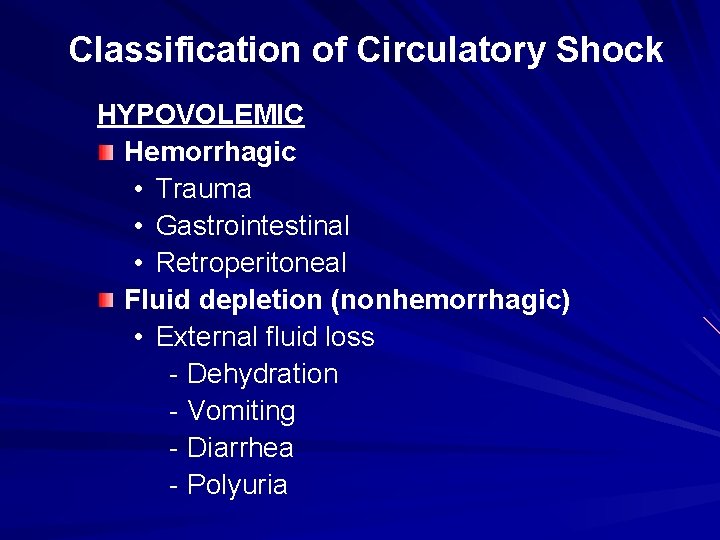
Classification of Circulatory Shock HYPOVOLEMIC Hemorrhagic • Trauma • Gastrointestinal • Retroperitoneal Fluid depletion (nonhemorrhagic) • External fluid loss - Dehydration - Vomiting - Diarrhea - Polyuria
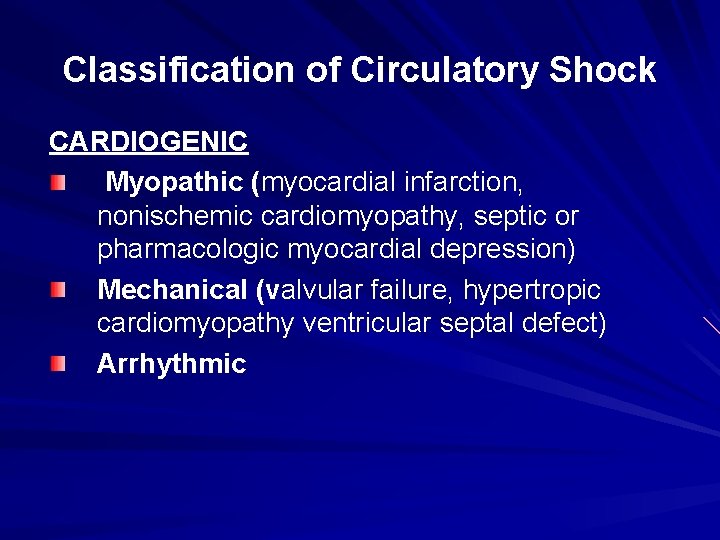
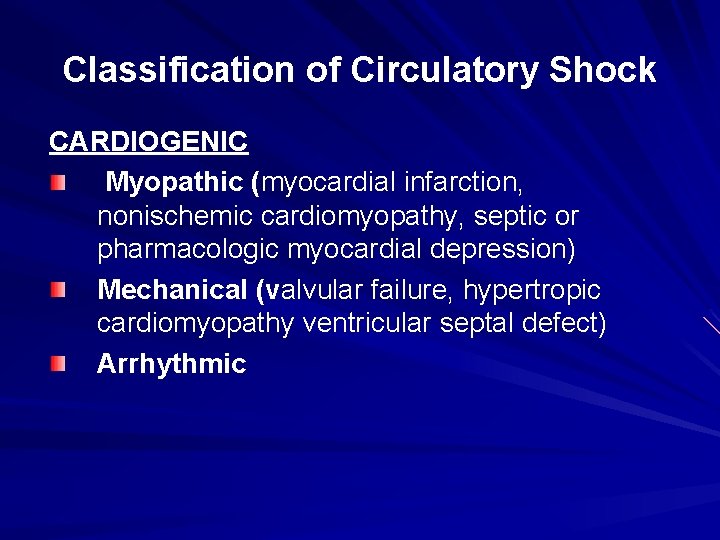
Classification of Circulatory Shock CARDIOGENIC Myopathic (myocardial infarction, nonischemic cardiomyopathy, septic or pharmacologic myocardial depression) Mechanical (valvular failure, hypertropic cardiomyopathy ventricular septal defect) Arrhythmic
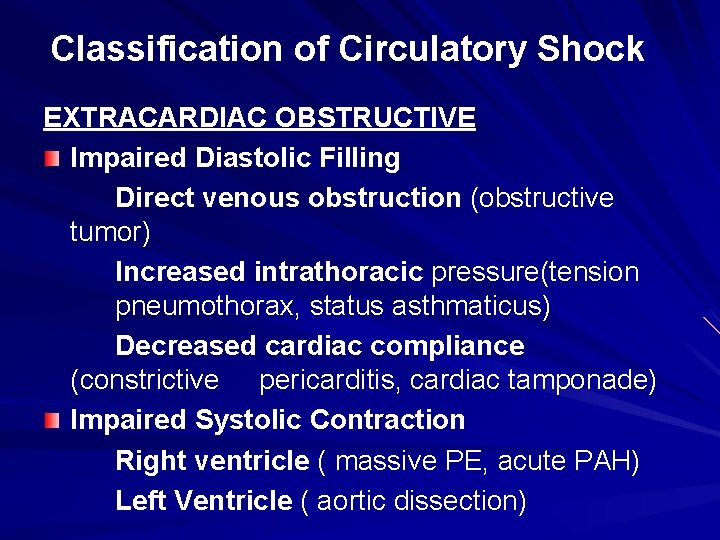
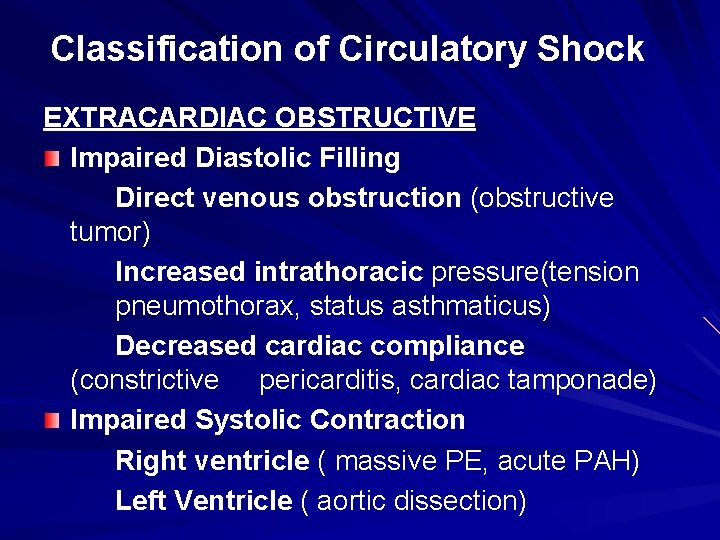
Classification of Circulatory Shock EXTRACARDIAC OBSTRUCTIVE Impaired Diastolic Filling Direct venous obstruction (obstructive tumor) Increased intrathoracic pressure(tension pneumothorax, status asthmaticus) Decreased cardiac compliance (constrictive pericarditis, cardiac tamponade) Impaired Systolic Contraction Right ventricle ( massive PE, acute PAH) Left Ventricle ( aortic dissection)
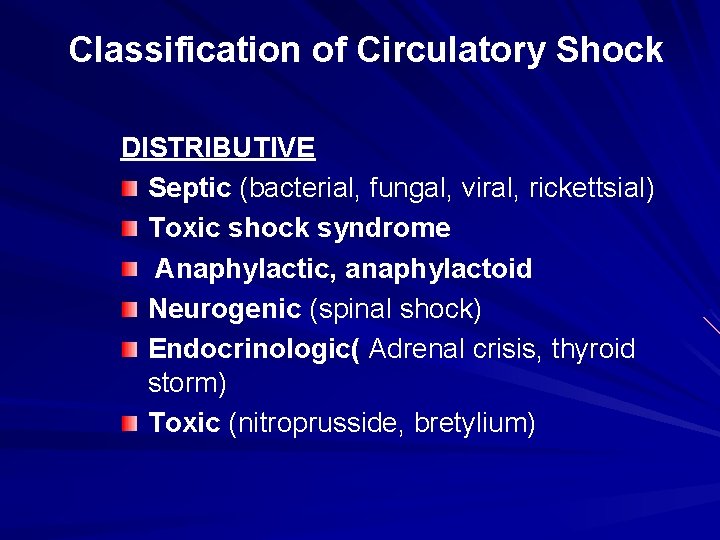
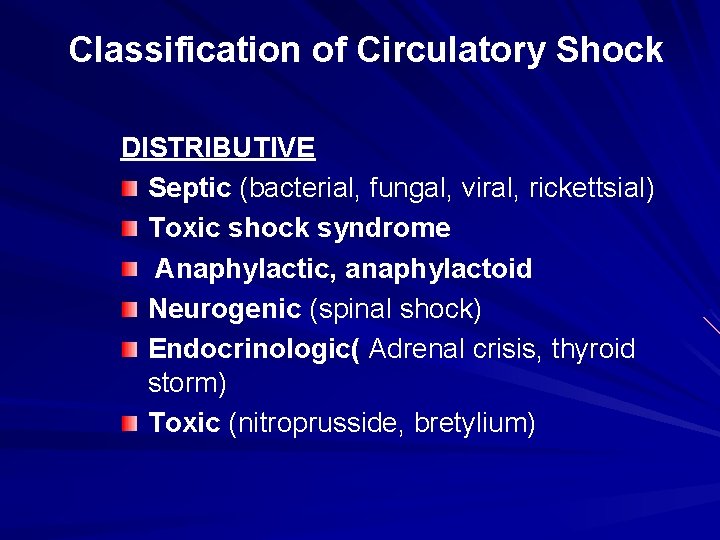
Classification of Circulatory Shock DISTRIBUTIVE Septic (bacterial, fungal, viral, rickettsial) Toxic shock syndrome Anaphylactic, anaphylactoid Neurogenic (spinal shock) Endocrinologic( Adrenal crisis, thyroid storm) Toxic (nitroprusside, bretylium)
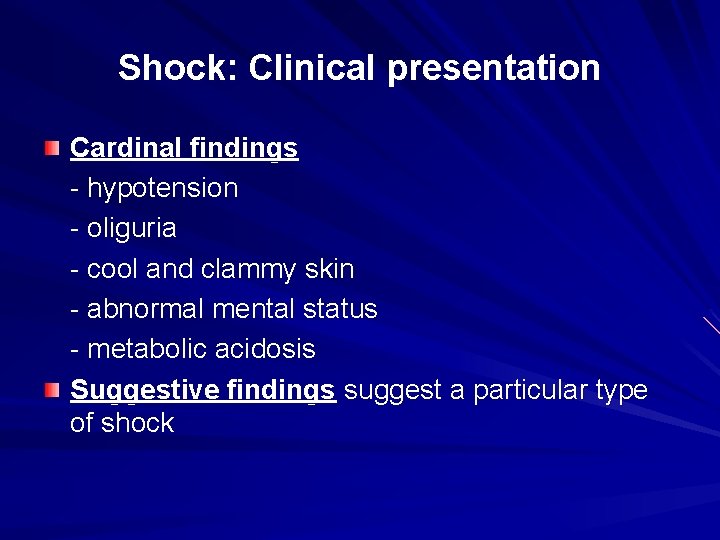
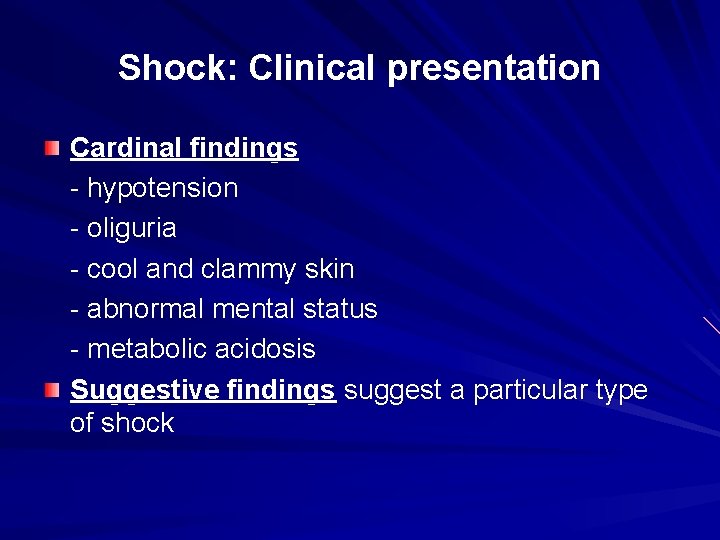
Shock: Clinical presentation Cardinal findings - hypotension - oliguria - cool and clammy skin - abnormal mental status - metabolic acidosis Suggestive findings suggest a particular type of shock
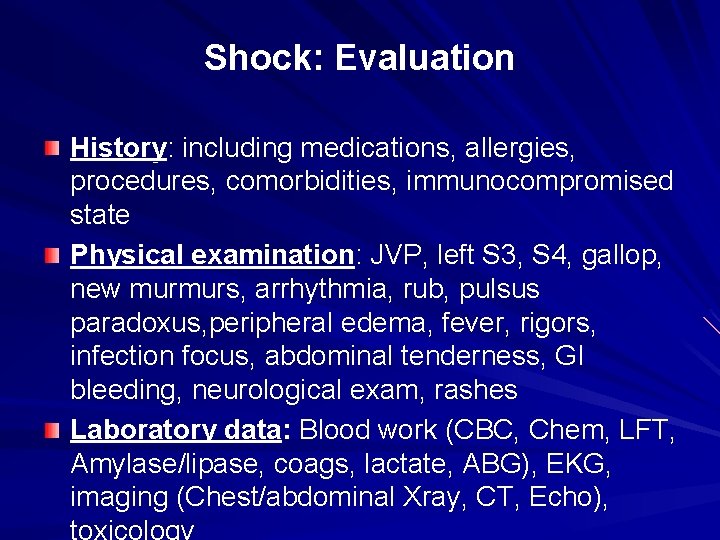
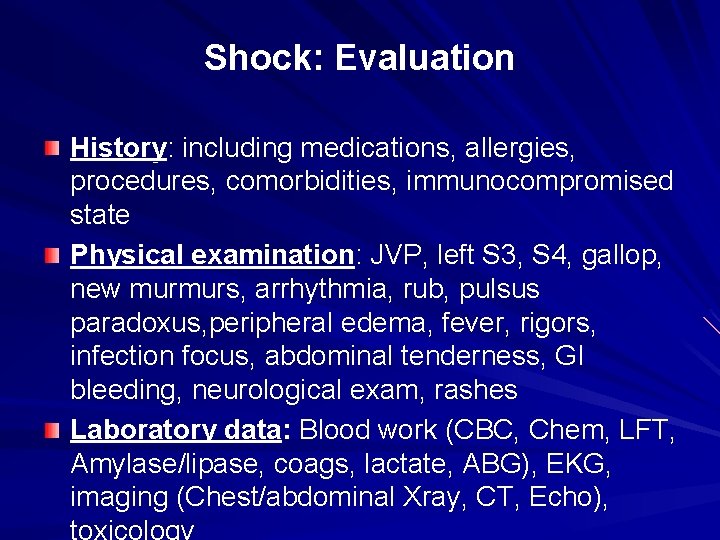
Shock: Evaluation History: including medications, allergies, procedures, comorbidities, immunocompromised state Physical examination: JVP, left S 3, S 4, gallop, new murmurs, arrhythmia, rub, pulsus paradoxus, peripheral edema, fever, rigors, infection focus, abdominal tenderness, GI bleeding, neurological exam, rashes Laboratory data: Blood work (CBC, Chem, LFT, Amylase/lipase, coags, lactate, ABG), EKG, imaging (Chest/abdominal Xray, CT, Echo), toxicology
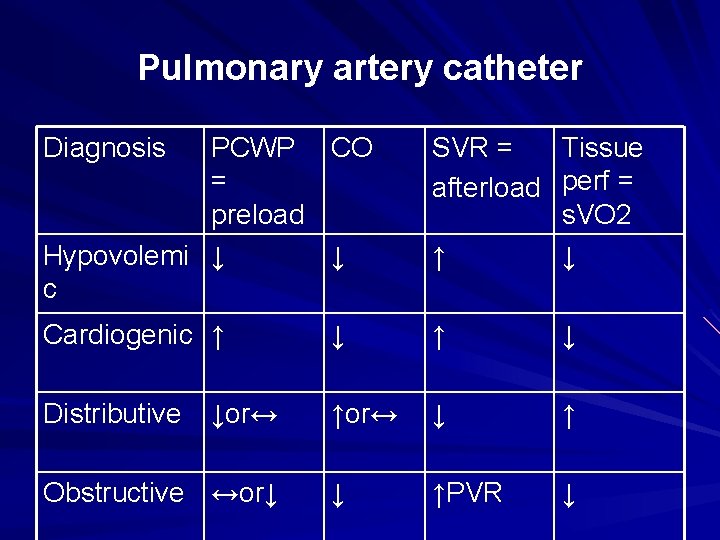
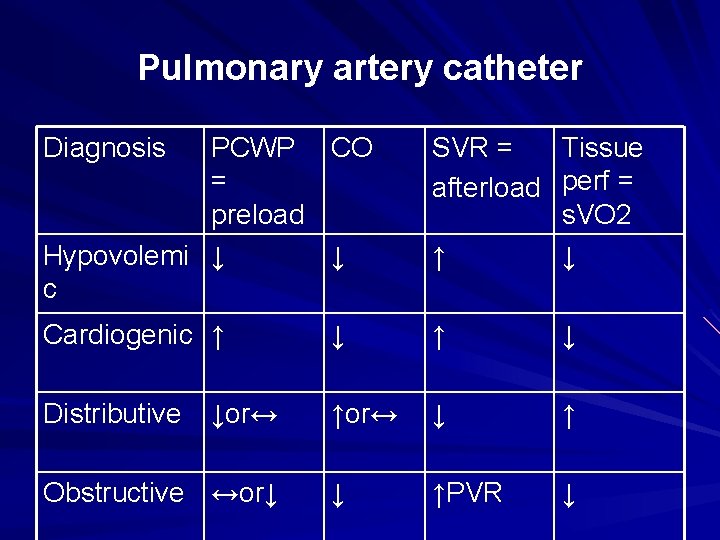
Pulmonary artery catheter Diagnosis PCWP CO = preload Hypovolemi ↓ ↓ c SVR = Tissue afterload perf = s. VO 2 ↑ ↓ Cardiogenic ↑ ↓ Distributive ↑or↔ ↓ ↑PVR ↓ ↓or↔ Obstructive ↔or↓
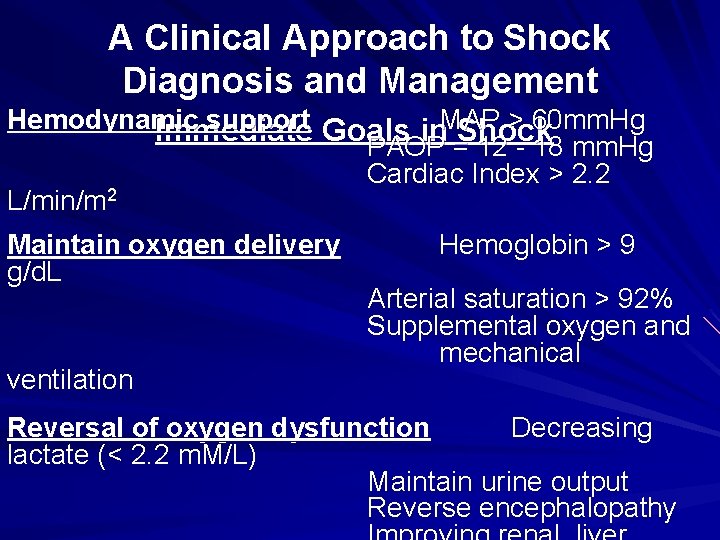
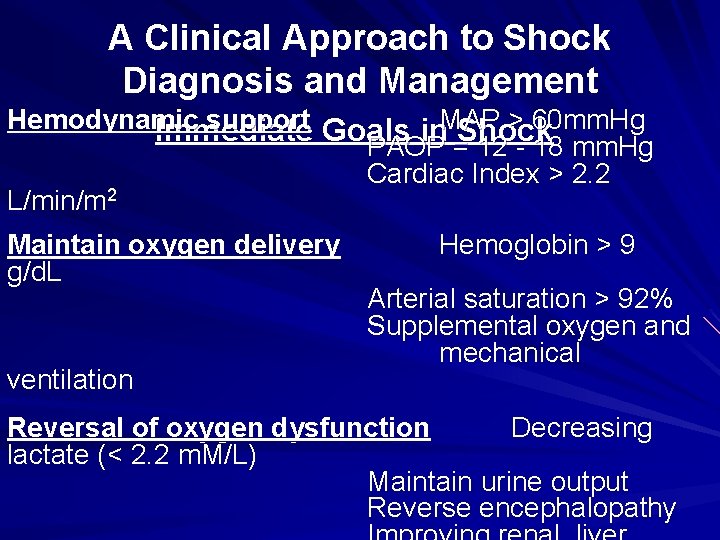
A Clinical Approach to Shock Diagnosis and Management Hemodynamic support Goals MAP > 60 mm. Hg Immediate in Shock PAOP = 12 - 18 mm. Hg Cardiac Index > 2. 2 L/min/m 2 Maintain oxygen delivery Hemoglobin > 9 g/d. L Arterial saturation > 92% Supplemental oxygen and mechanical ventilation Reversal of oxygen dysfunction Decreasing lactate (< 2. 2 m. M/L) Maintain urine output Reverse encephalopathy

Shock: Management Hypovolemi Cardiogenic Distributive Obstructive c l. Rapid l. LV infarct volume -IABP replacement (saline, blood revascularize products) l. RV infarct l. Idenify source of loss fluids/inotrop -Endoscopy es l. Valve Angiography problem -MRI/CTscan -surgery l. Septic l. Pericardial tamponade pericardiocente - Fluids, sis pressors, surgical inotropes drainage - Goals: l. Pulmonary SV 02 > 70% embolism improving Heparin organ VQ scan/CTA function Consider decreasing -Antibiotics
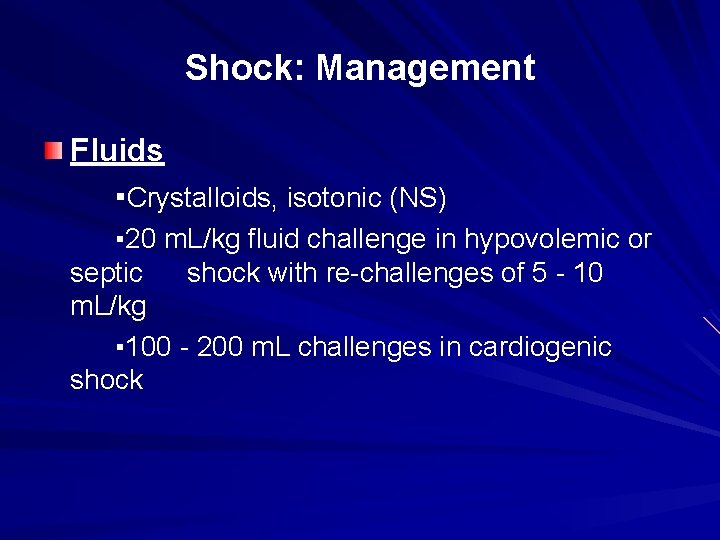
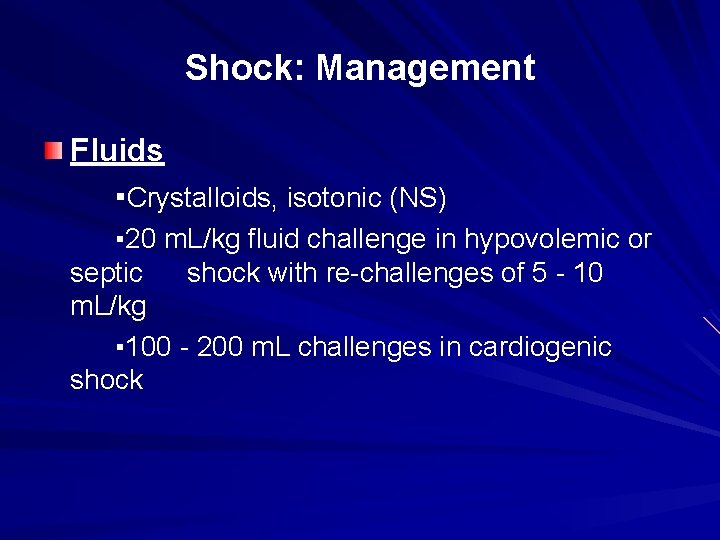
Shock: Management Fluids ▪Crystalloids, isotonic (NS) ▪ 20 m. L/kg fluid challenge in hypovolemic or septic shock with re-challenges of 5 - 10 m. L/kg ▪ 100 - 200 m. L challenges in cardiogenic shock
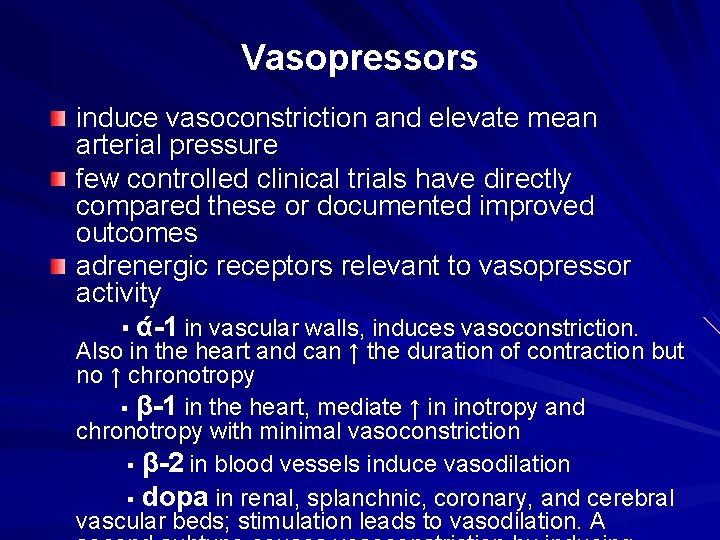
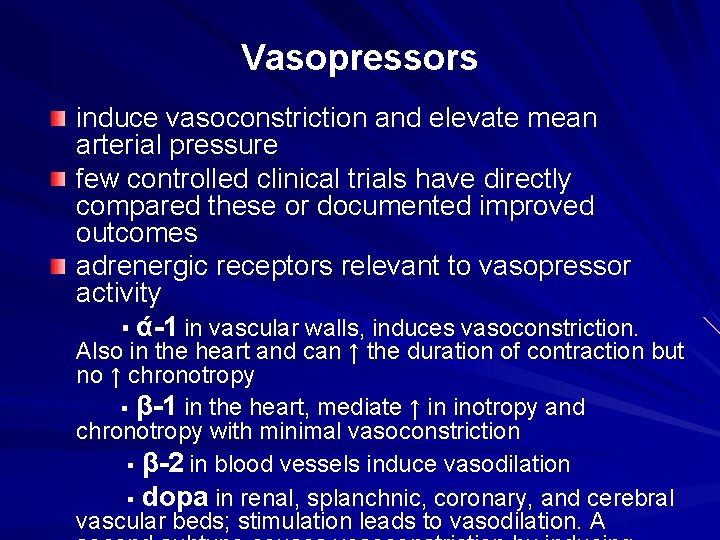
Vasopressors induce vasoconstriction and elevate mean arterial pressure few controlled clinical trials have directly compared these or documented improved outcomes adrenergic receptors relevant to vasopressor activity ▪ ά-1 in vascular walls, induces vasoconstriction. Also in the heart and can ↑ the duration of contraction but no ↑ chronotropy ▪ β-1 in the heart, mediate ↑ in inotropy and chronotropy with minimal vasoconstriction ▪ β-2 in blood vessels induce vasodilation ▪ dopa in renal, splanchnic, coronary, and cerebral vascular beds; stimulation leads to vasodilation. A
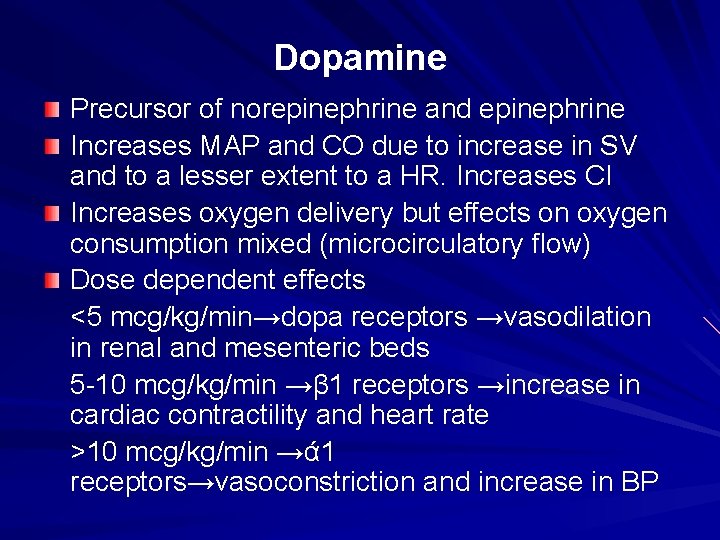
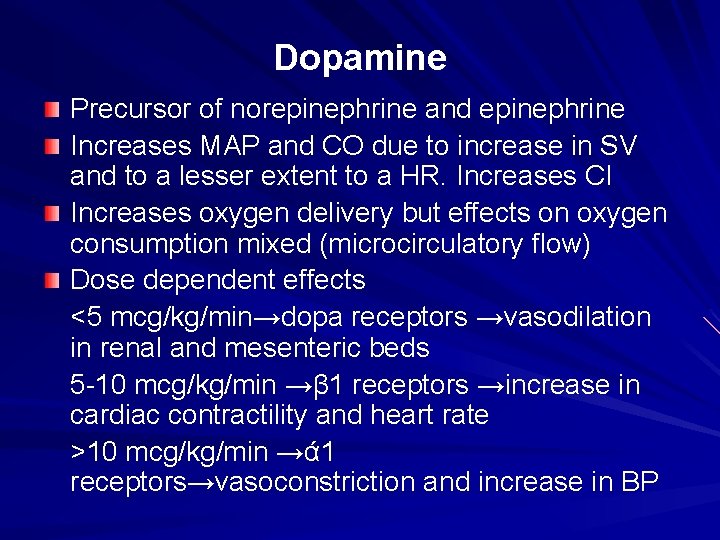
Dopamine Precursor of norepinephrine and epinephrine Increases MAP and CO due to increase in SV and to a lesser extent to a HR. Increases CI Increases oxygen delivery but effects on oxygen consumption mixed (microcirculatory flow) Dose dependent effects <5 mcg/kg/min→dopa receptors →vasodilation in renal and mesenteric beds 5 -10 mcg/kg/min →β 1 receptors →increase in cardiac contractility and heart rate >10 mcg/kg/min →ά 1 receptors→vasoconstriction and increase in BP
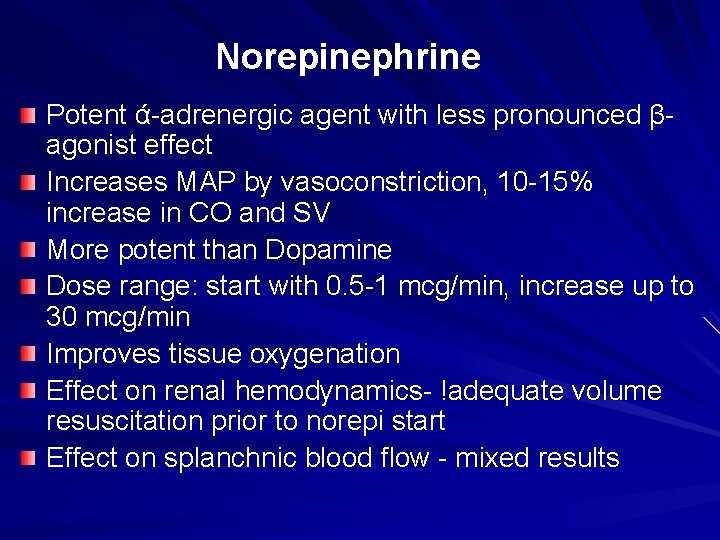
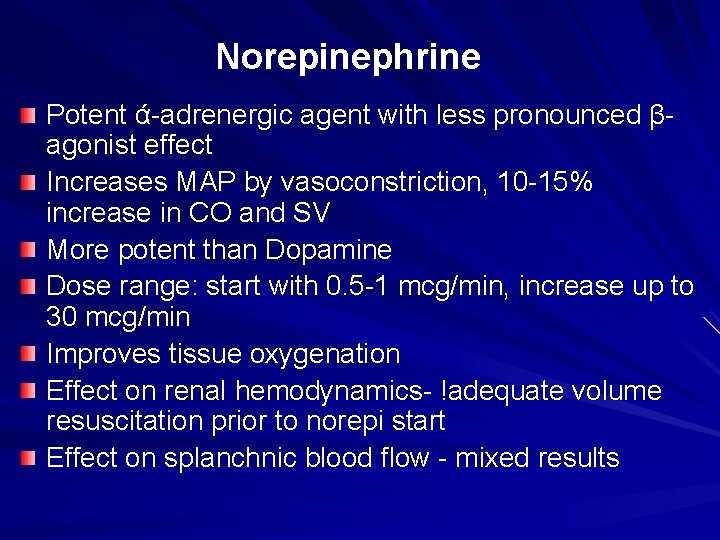
Norepinephrine Potent ά-adrenergic agent with less pronounced βagonist effect Increases MAP by vasoconstriction, 10 -15% increase in CO and SV More potent than Dopamine Dose range: start with 0. 5 -1 mcg/min, increase up to 30 mcg/min Improves tissue oxygenation Effect on renal hemodynamics- !adequate volume resuscitation prior to norepi start Effect on splanchnic blood flow - mixed results
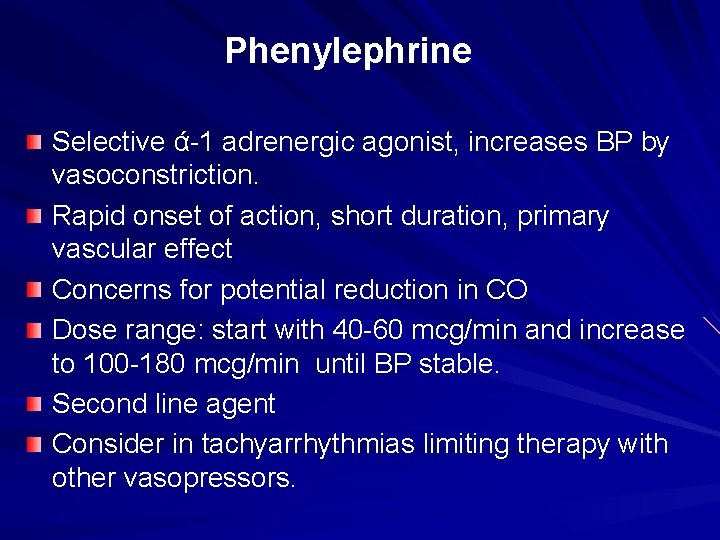
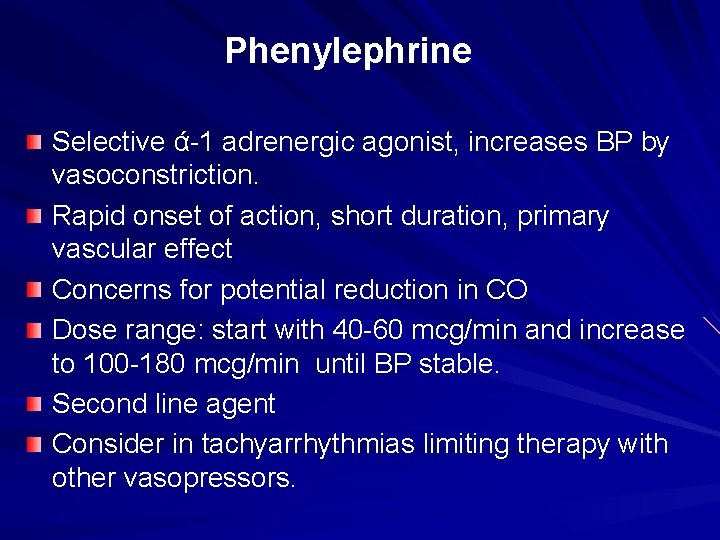
Phenylephrine Selective ά-1 adrenergic agonist, increases BP by vasoconstriction. Rapid onset of action, short duration, primary vascular effect Concerns for potential reduction in CO Dose range: start with 40 -60 mcg/min and increase to 100 -180 mcg/min until BP stable. Second line agent Consider in tachyarrhythmias limiting therapy with other vasopressors.
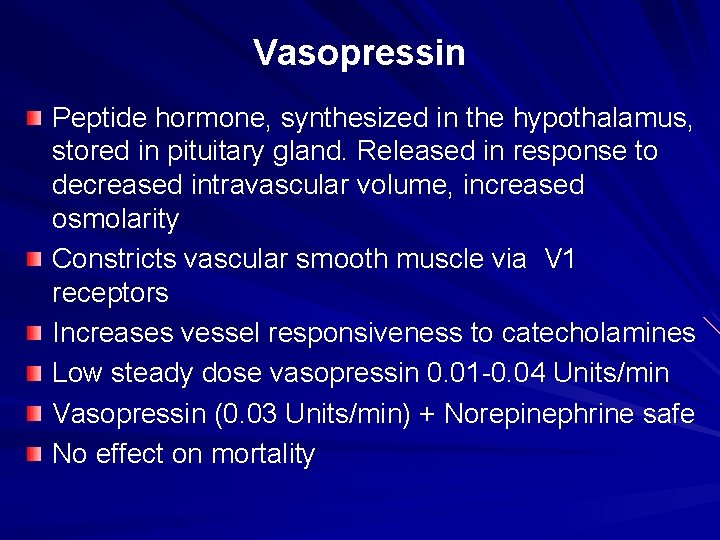
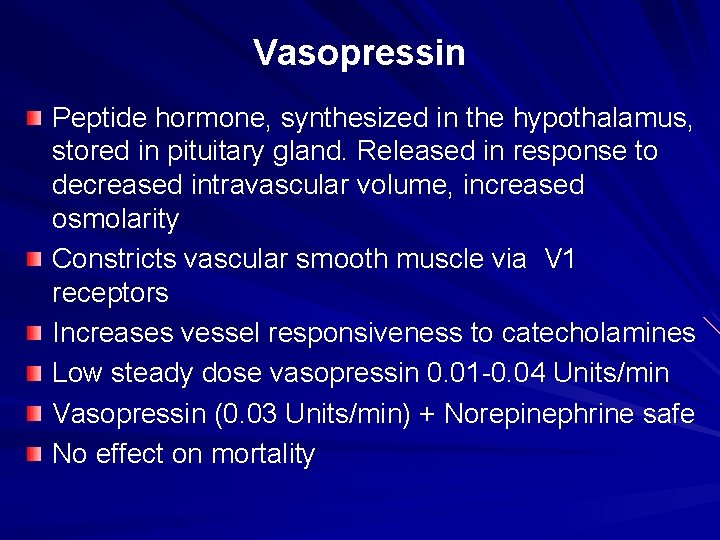
Vasopressin Peptide hormone, synthesized in the hypothalamus, stored in pituitary gland. Released in response to decreased intravascular volume, increased osmolarity Constricts vascular smooth muscle via V 1 receptors Increases vessel responsiveness to catecholamines Low steady dose vasopressin 0. 01 -0. 04 Units/min Vasopressin (0. 03 Units/min) + Norepinephrine safe No effect on mortality
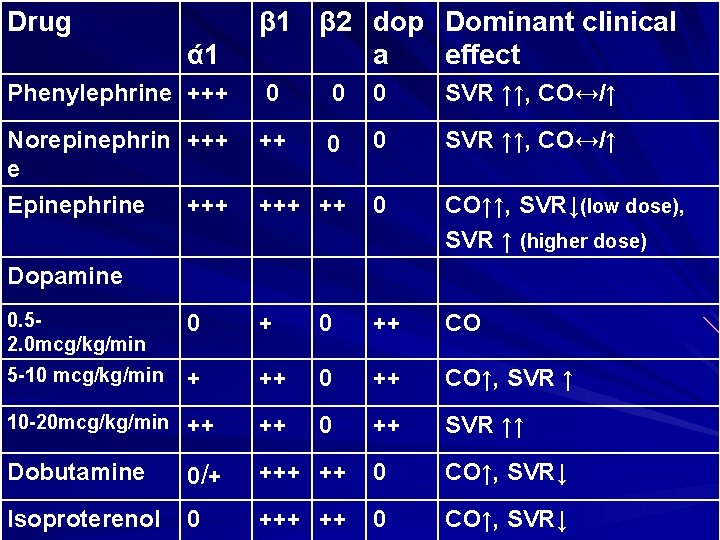
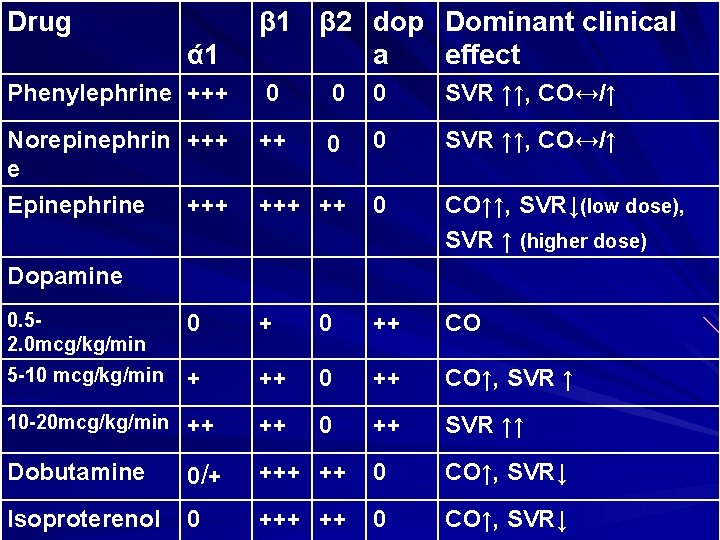
Drug ά 1 β 2 dop Dominant clinical a effect Phenylephrine +++ 0 0 0 SVR ↑↑, CO↔/↑ Norepinephrin +++ e Epinephrine +++ ++ 0 0 SVR ↑↑, CO↔/↑ +++ ++ 0 CO↑↑, SVR↓(low dose), SVR ↑ (higher dose) Dopamine 0. 52. 0 mcg/kg/min 0 ++ CO 5 -10 mcg/kg/min + ++ 0 ++ CO↑, SVR ↑ 10 -20 mcg/kg/min ++ ++ 0 ++ SVR ↑↑ Dobutamine 0/ + ++ 0 CO↑, SVR↓ Isoproterenol 0 +++ ++ 0 CO↑, SVR↓
Vasopressors: complications of use Hypoperfusion Dysrhythmias Myocardial ischemia Local effects Hyperglycemia NO STUDY HAS DEMONSTRATED A SURVIVAL BENEFIT DUE TO ONE VASOPRESSOR COMPARED TO ANOTHER
 Vasopressors
Vasopressors Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Shock normovolemico
Shock normovolemico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock T10 spinal cord
T10 spinal cord Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worm breton
Tư thế worm breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới