Differentiating Shock Syndromes Hemodynamics and Vasopressors in the
- Slides: 42
Differentiating Shock Syndromes: Hemodynamics and Vasopressors in the ICU Michael D Schmidt, Pharm. D Critical Care Clinical Pharmacist Belleville Memorial Hospital Belleville, IL
Disclosures • I have no conflicts of interest to disclose
Learning Objectives 1. Understand hemodynamic variables used to classify shock syndromes 2. Classify 4 different types of shock based on etiology 3. Compare vasoactive drugs commonly used to treat shock 4. Develop a treatment plan for a patient presenting with shock
Introduction • What is shock? – Inadequate perfusion – Leading to inadequate oxygen delivery • Is it hypotension? – Commonly – Be aware of patient specific variables
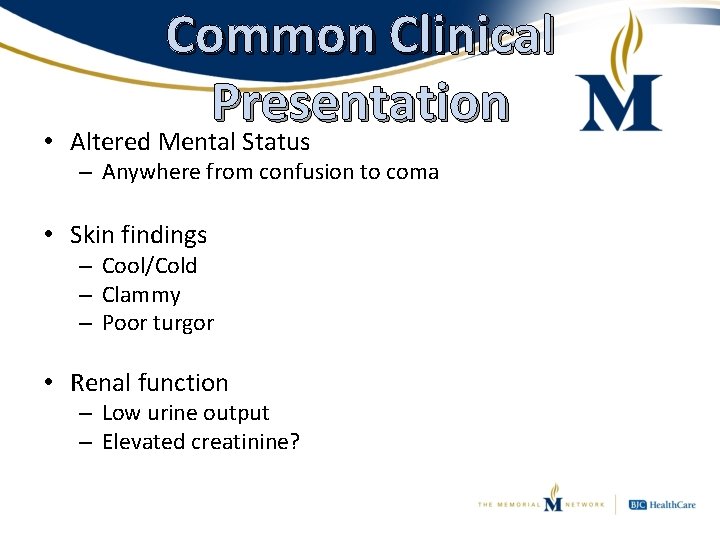
Common Clinical Presentation • Altered Mental Status – Anywhere from confusion to coma • Skin findings – Cool/Cold – Clammy – Poor turgor • Renal function – Low urine output – Elevated creatinine?
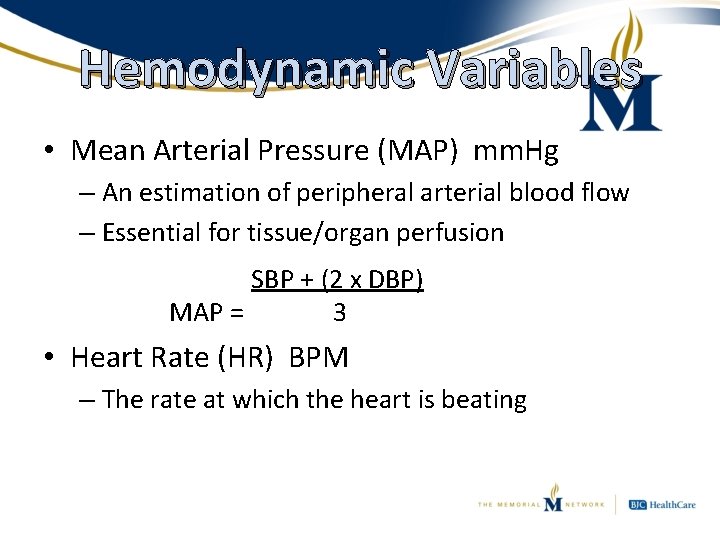
Hemodynamic Variables • Mean Arterial Pressure (MAP) mm. Hg – An estimation of peripheral arterial blood flow – Essential for tissue/organ perfusion SBP + (2 x DBP) MAP = 3 • Heart Rate (HR) BPM – The rate at which the heart is beating
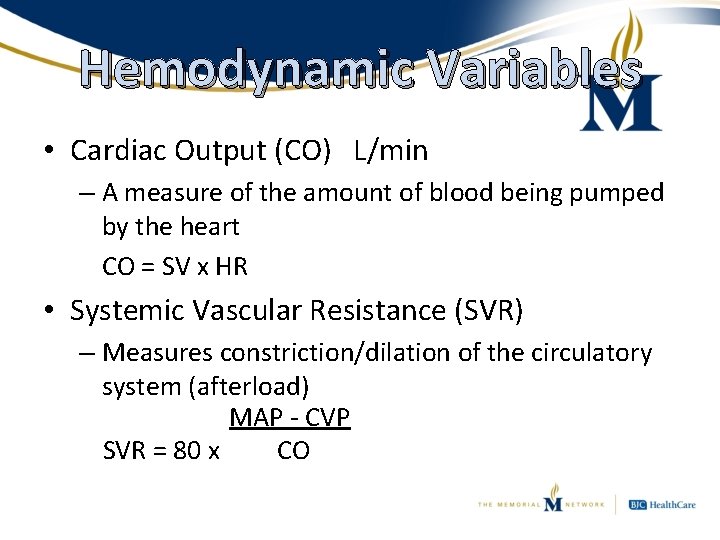
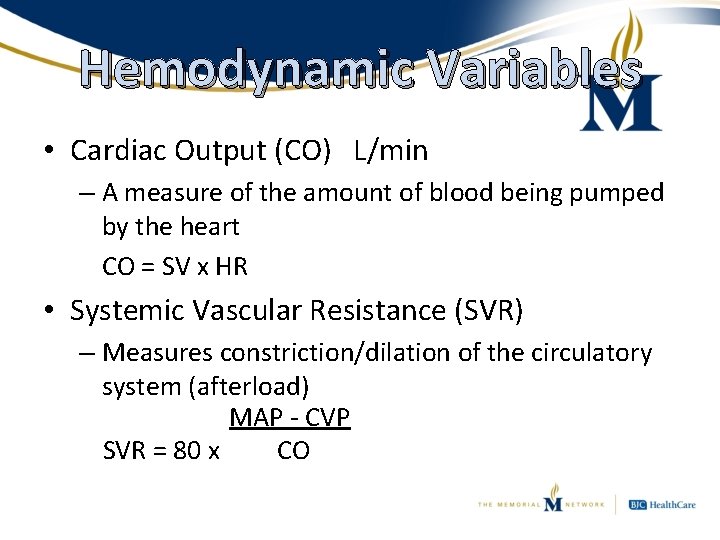
Hemodynamic Variables • Cardiac Output (CO) L/min – A measure of the amount of blood being pumped by the heart CO = SV x HR • Systemic Vascular Resistance (SVR) – Measures constriction/dilation of the circulatory system (afterload) MAP - CVP SVR = 80 x CO
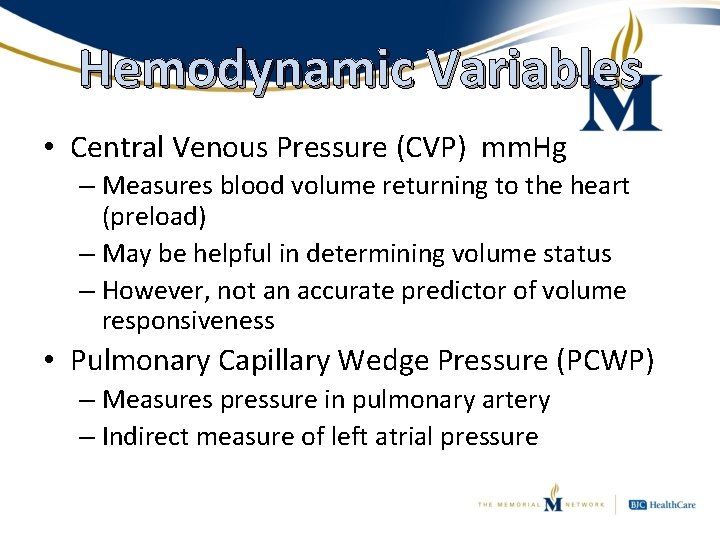
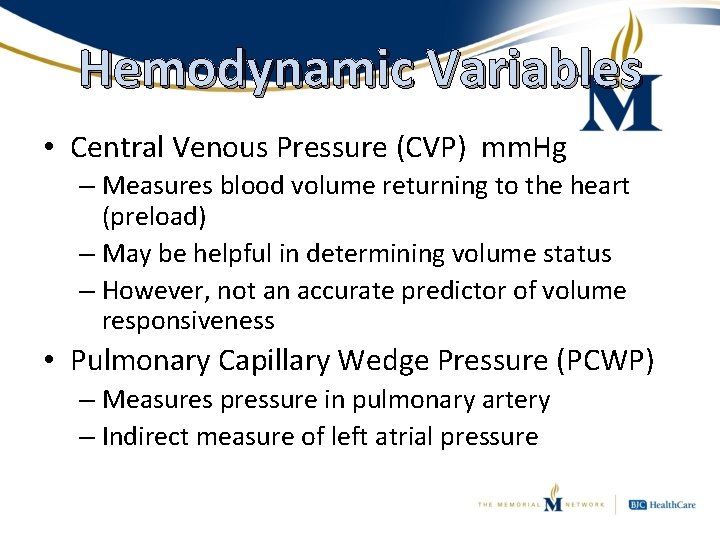
Hemodynamic Variables • Central Venous Pressure (CVP) mm. Hg – Measures blood volume returning to the heart (preload) – May be helpful in determining volume status – However, not an accurate predictor of volume responsiveness • Pulmonary Capillary Wedge Pressure (PCWP) – Measures pressure in pulmonary artery – Indirect measure of left atrial pressure
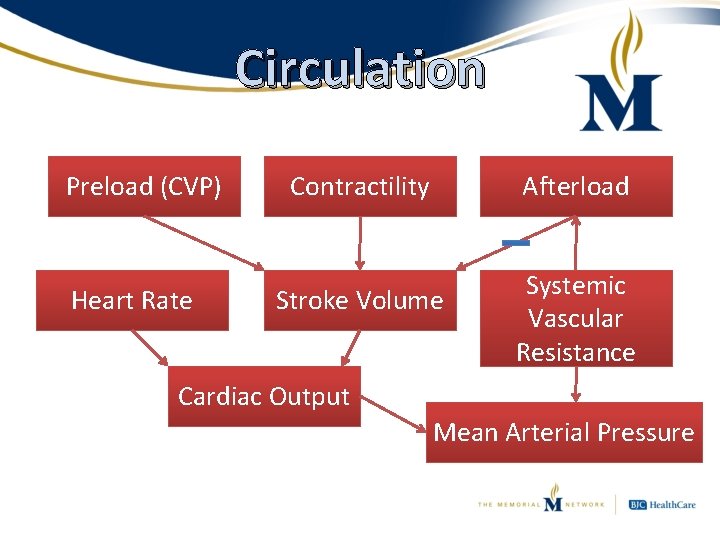
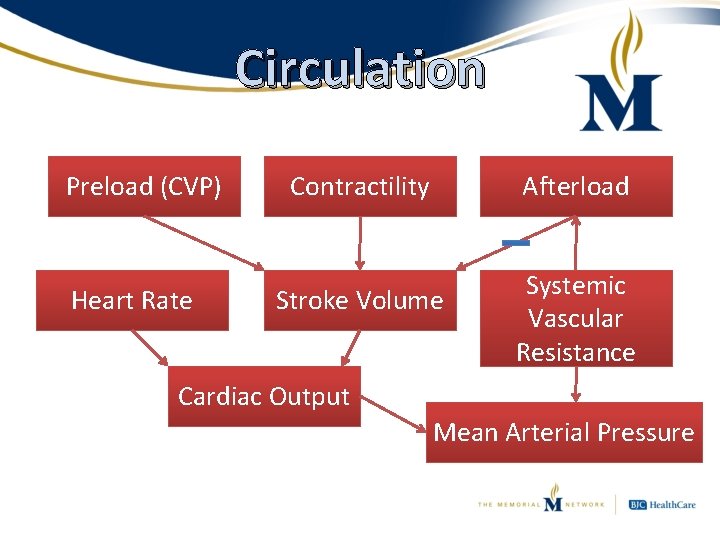
Circulation Preload (CVP) Heart Rate Contractility Afterload Stroke Volume Systemic Vascular Resistance Cardiac Output Mean Arterial Pressure
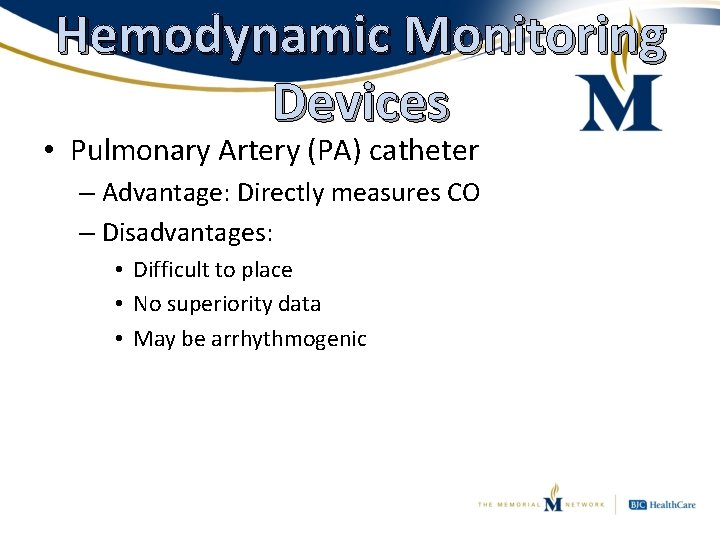
Hemodynamic Monitoring Devices • Pulmonary Artery (PA) catheter – Advantage: Directly measures CO – Disadvantages: • Difficult to place • No superiority data • May be arrhythmogenic
Hemodynamic Monitoring Devices • Central Venous Catheter (CVC) – Advantages: • Easier and safer than PA catheter • Can measure CVP • Can measure Scv. O 2 – Unless femoral CVC * * Chest 2010; 138(1): 76 -83
Hemodynamic Monitoring Devices • Arterial pulse pressure waveform analysis – Many different brand names – Advantages: • Continuous CO measurement • Assessment of stroke volume and pulse pressure – As well as variation in these parameters – Disadvantages: • Valve dysfunction and arrhythmias decrease accuracy • SVV is only validated in intubated patients
Laboratory Markers • Lactate – Product of anaerobic metabolism • Elevation is a good marker of tissue hypoperfusion – Trending may be useful to grade, or possibly guide, resuscitation in septic shock – Can cause anion-gap metabolic acidosis
Laboratory Markers • Central Venous Oxygen Saturation (Scv. O 2) – Accurate measure of peripheral oxygen delivery • Assuming patient is not profoundly anemic – When oxygen delivery is appropriate: • Sa. O 2 – Scv. O 2 = 25% (100% - 75% = 25%) • 25% is the normal extraction ratio (ERO 2) – When oxygen delivery is inadequate: • ERO 2 increases • Scv. O 2 decreases – Continuous monitoring is more appropriate than occasional
Differentiating Shock States • 4 main types of shock: – Hypovolemic • “Not enough blood” – Cardiogenic • “Heart not working” – Obstructive • “Something’s in the way” – Vasodilatory/Distributive • “No pressure”
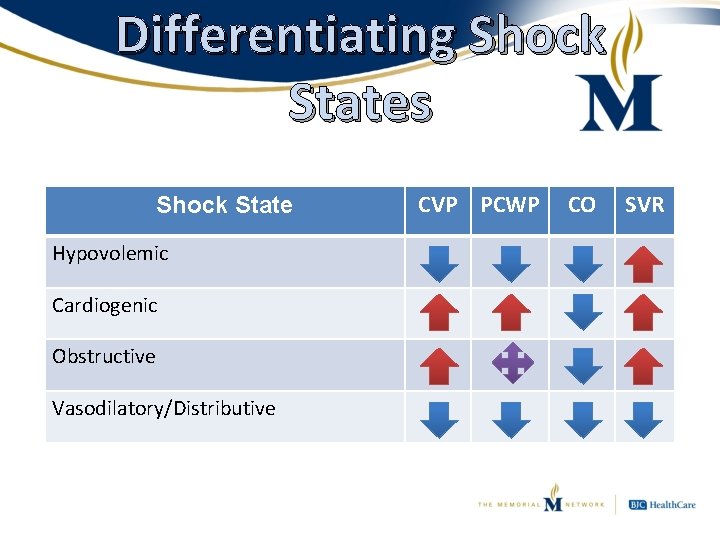
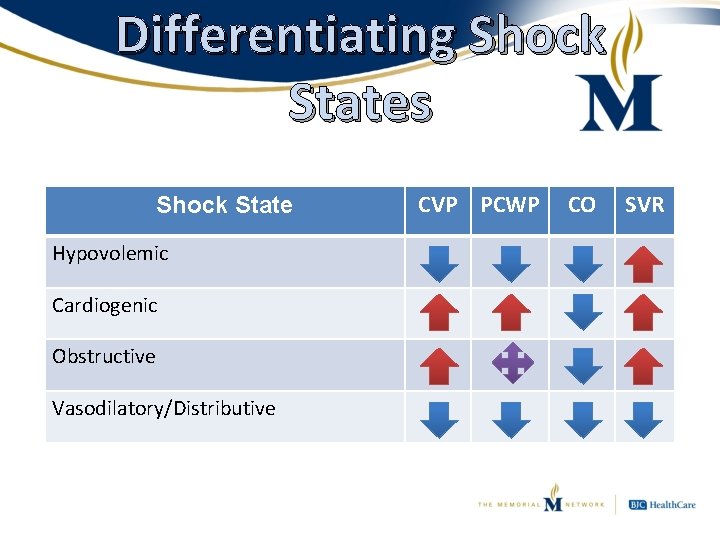
Differentiating Shock States Shock State Hypovolemic Cardiogenic Obstructive Vasodilatory/Distributive CVP PCWP CO SVR
Differentiating Shock States • Hypovolemic shock – Characterized by inadequate blood volume – Causes: • • Hemorrhage (trauma, GI, post-partum, etc. ) Burns Diarrhea/Vomiting Excessive perspiration – Treatment: • Fix the underlying cause • Replace volume lost • Support BP if necessary
Differentiating Shock States • Cardiogenic shock – Inability of the heart muscle to adequately pump blood – Causes: • Damage to the heart – Myocardial infarction, decompensated heart failure, mycordial/septal/valve rupture, arrhythmia (tachy or brady) – Treatment: • Fix the underlying cause • Stimulate the heart muscle • Optimize fluid and BP
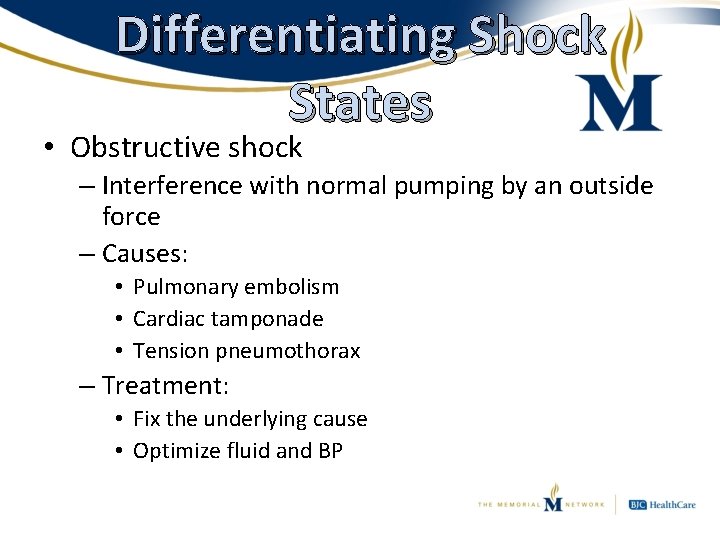
Differentiating Shock States • Obstructive shock – Interference with normal pumping by an outside force – Causes: • Pulmonary embolism • Cardiac tamponade • Tension pneumothorax – Treatment: • Fix the underlying cause • Optimize fluid and BP
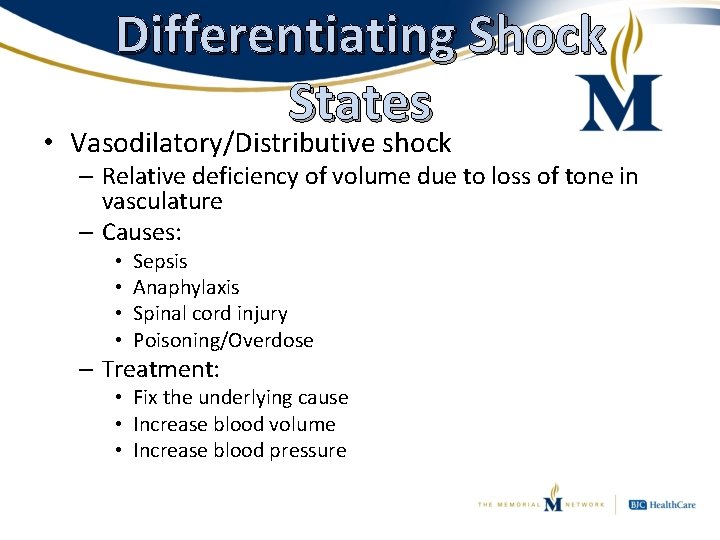
Differentiating Shock States • Vasodilatory/Distributive shock – Relative deficiency of volume due to loss of tone in vasculature – Causes: • • Sepsis Anaphylaxis Spinal cord injury Poisoning/Overdose – Treatment: • Fix the underlying cause • Increase blood volume • Increase blood pressure
Vasoactive Agents • Definition: Drugs that cause either constriction or dilation of blood vessels – Inotropic drugs often lumped in as well • Mostly analogues of naturally occurring chemicals within the body – Specifically chemicals that impact the adrenergic system – “Fight or Flight” response • All should be run through a central line
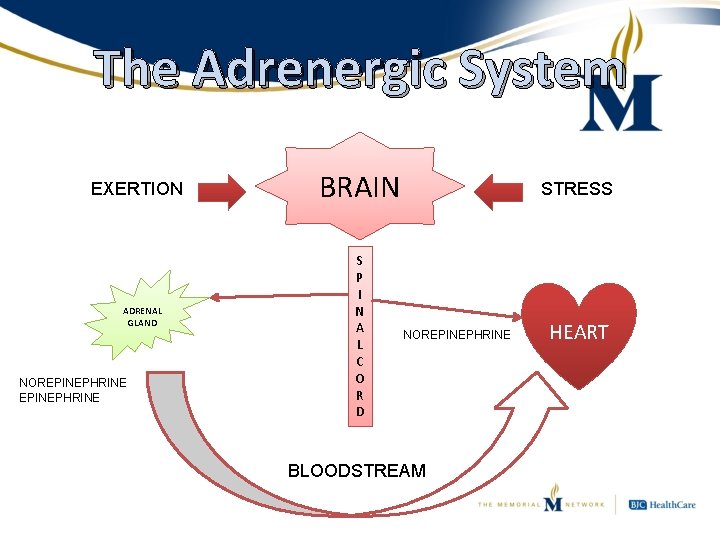
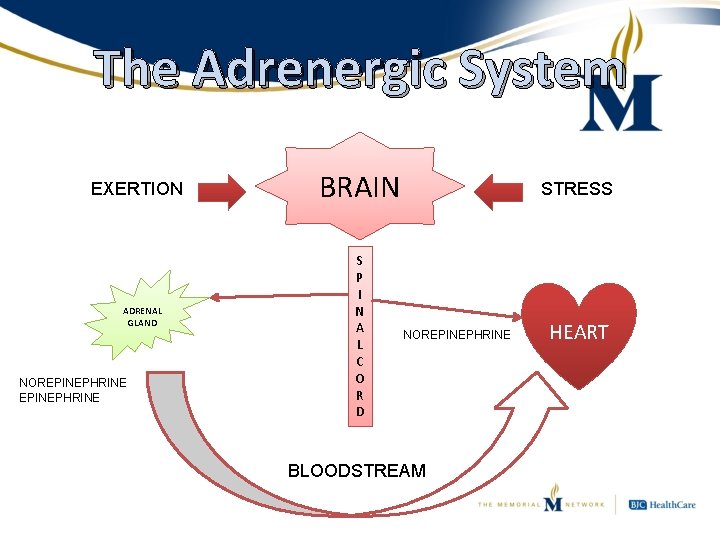
The Adrenergic System EXERTION ADRENAL GLAND NOREPINEPHRINE BRAIN S P I N A L C O R D STRESS NOREPINEPHRINE BLOODSTREAM HEART
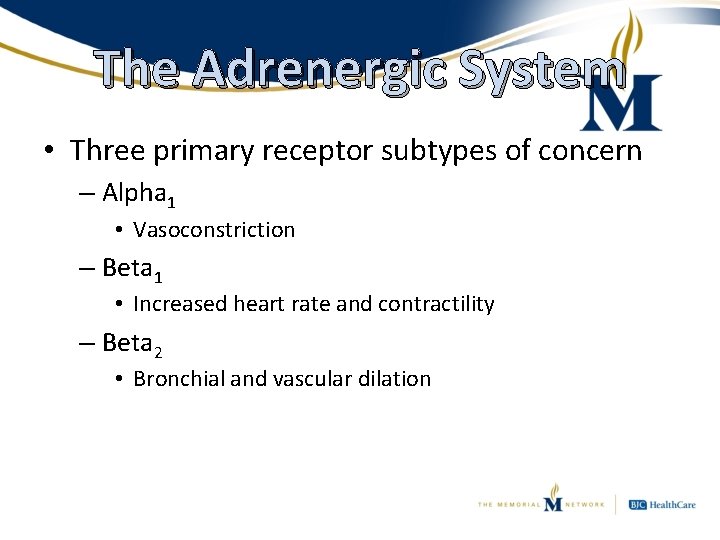
The Adrenergic System • Three primary receptor subtypes of concern – Alpha 1 • Vasoconstriction – Beta 1 • Increased heart rate and contractility – Beta 2 • Bronchial and vascular dilation
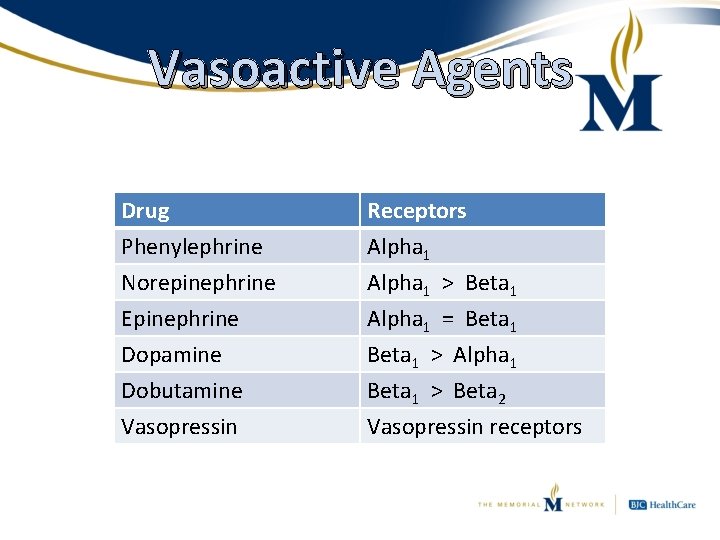
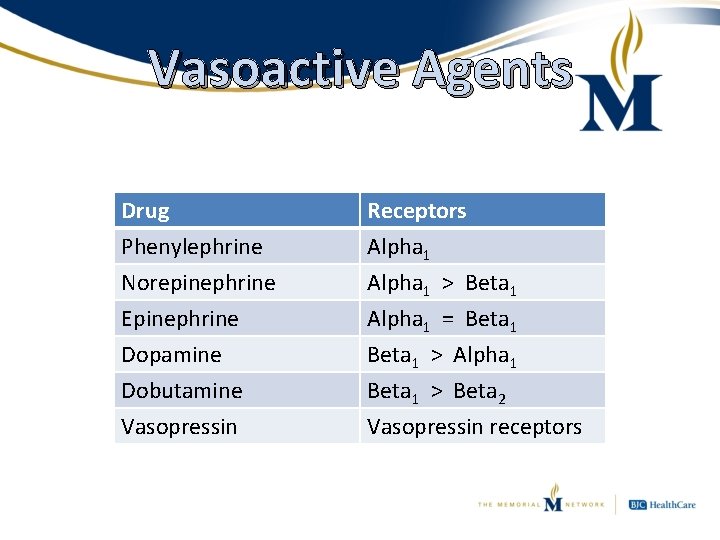
Vasoactive Agents Drug Phenylephrine Norepinephrine Epinephrine Receptors Alpha 1 > Beta 1 Alpha 1 = Beta 1 Dopamine Dobutamine Vasopressin Beta 1 > Alpha 1 Beta 1 > Beta 2 Vasopressin receptors
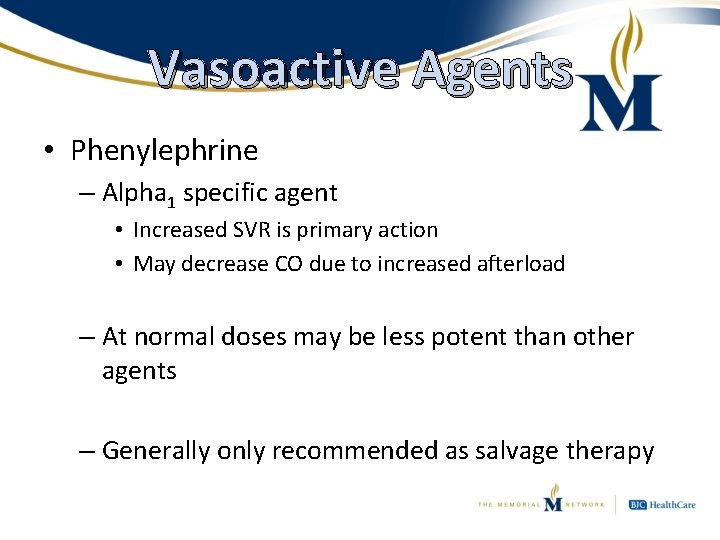
Vasoactive Agents • Phenylephrine – Alpha 1 specific agent • Increased SVR is primary action • May decrease CO due to increased afterload – At normal doses may be less potent than other agents – Generally only recommended as salvage therapy
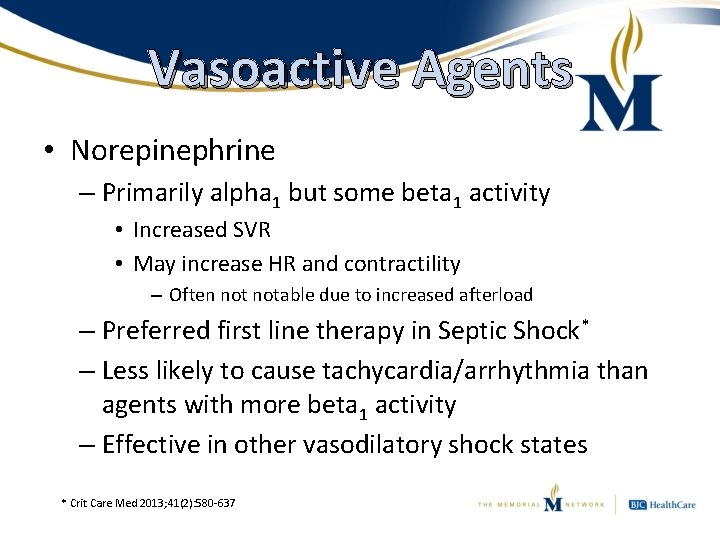
Vasoactive Agents • Norepinephrine – Primarily alpha 1 but some beta 1 activity • Increased SVR • May increase HR and contractility – Often notable due to increased afterload – Preferred first line therapy in Septic Shock* – Less likely to cause tachycardia/arrhythmia than agents with more beta 1 activity – Effective in other vasodilatory shock states * Crit Care Med 2013; 41(2): 580 -637
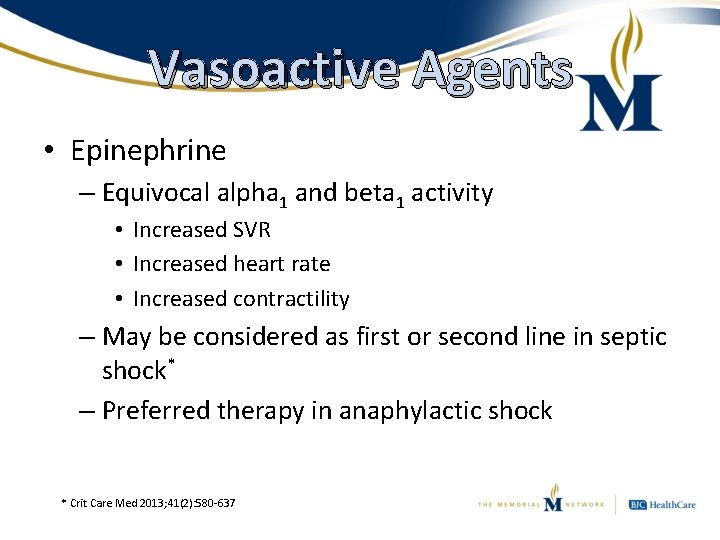
Vasoactive Agents • Epinephrine – Equivocal alpha 1 and beta 1 activity • Increased SVR • Increased heart rate • Increased contractility – May be considered as first or second line in septic shock* – Preferred therapy in anaphylactic shock * Crit Care Med 2013; 41(2): 580 -637
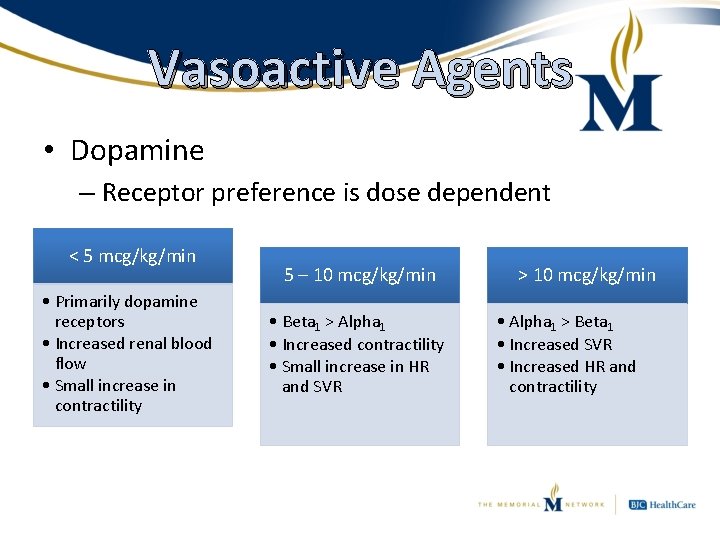
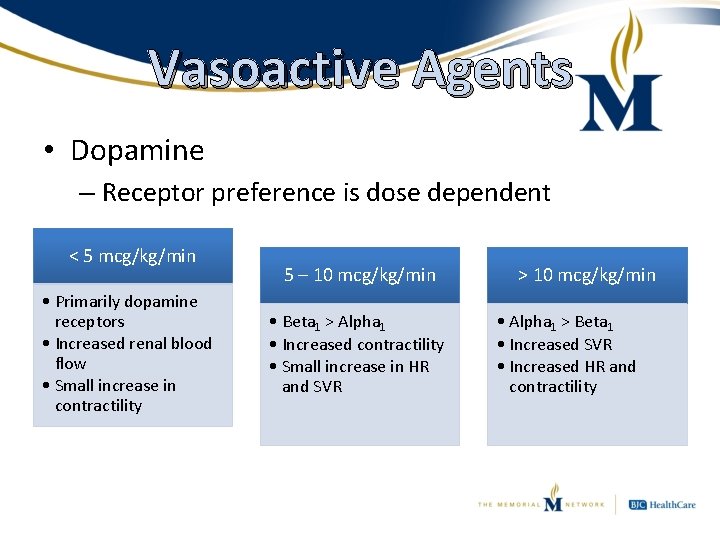
Vasoactive Agents • Dopamine – Receptor preference is dose dependent < 5 mcg/kg/min • Primarily dopamine receptors • Increased renal blood flow • Small increase in contractility 5 – 10 mcg/kg/min • Beta 1 > Alpha 1 • Increased contractility • Small increase in HR and SVR > 10 mcg/kg/min • Alpha 1 > Beta 1 • Increased SVR • Increased HR and contractility
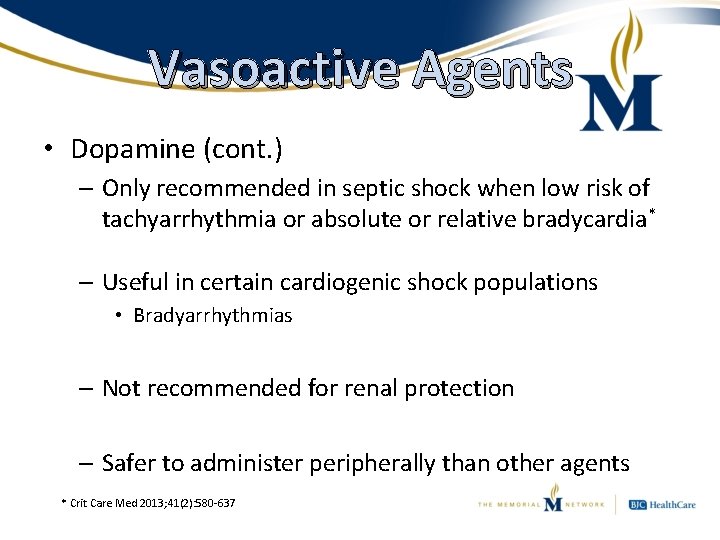
Vasoactive Agents • Dopamine (cont. ) – Only recommended in septic shock when low risk of tachyarrhythmia or absolute or relative bradycardia* – Useful in certain cardiogenic shock populations • Bradyarrhythmias – Not recommended for renal protection – Safer to administer peripherally than other agents * Crit Care Med 2013; 41(2): 580 -637
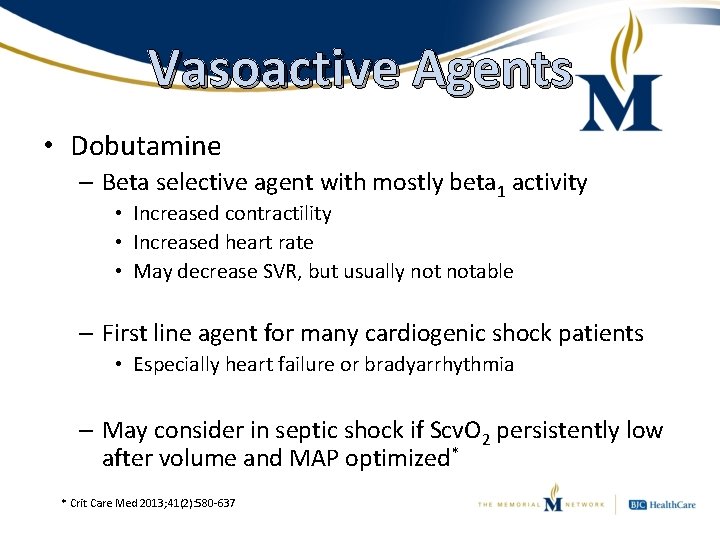
Vasoactive Agents • Dobutamine – Beta selective agent with mostly beta 1 activity • Increased contractility • Increased heart rate • May decrease SVR, but usually notable – First line agent for many cardiogenic shock patients • Especially heart failure or bradyarrhythmia – May consider in septic shock if Scv. O 2 persistently low after volume and MAP optimized* * Crit Care Med 2013; 41(2): 580 -637
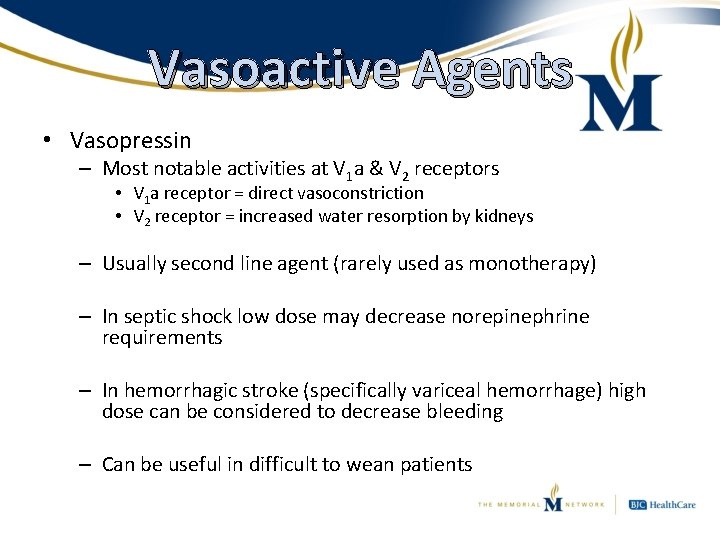
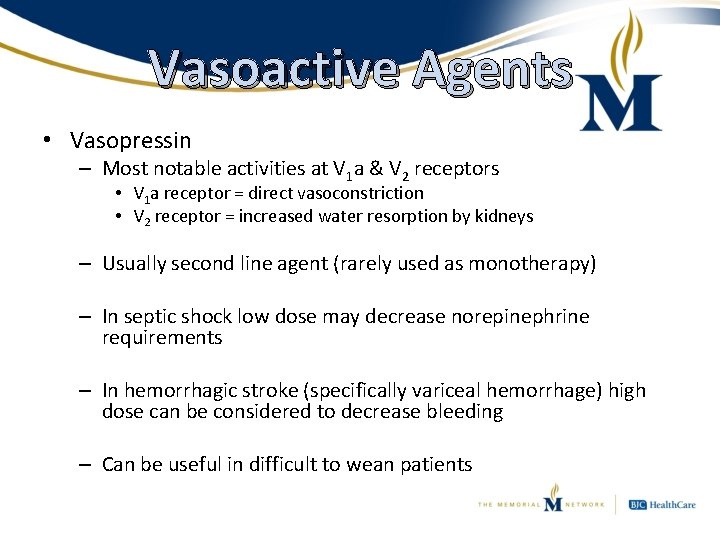
Vasoactive Agents • Vasopressin – Most notable activities at V 1 a & V 2 receptors • V 1 a receptor = direct vasoconstriction • V 2 receptor = increased water resorption by kidneys – Usually second line agent (rarely used as monotherapy) – In septic shock low dose may decrease norepinephrine requirements – In hemorrhagic stroke (specifically variceal hemorrhage) high dose can be considered to decrease bleeding – Can be useful in difficult to wean patients
Putting It All Together 1. Identify the etiology of the shock 2. Treat the underlying cause 3. Target drugs to treat the dysfunctional circulation
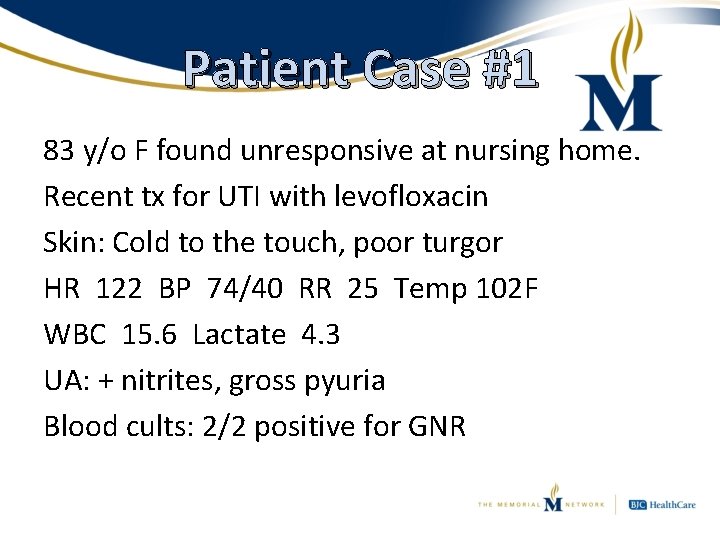
Patient Case #1 83 y/o F found unresponsive at nursing home. Recent tx for UTI with levofloxacin Skin: Cold to the touch, poor turgor HR 122 BP 74/40 RR 25 Temp 102 F WBC 15. 6 Lactate 4. 3 UA: + nitrites, gross pyuria Blood cults: 2/2 positive for GNR
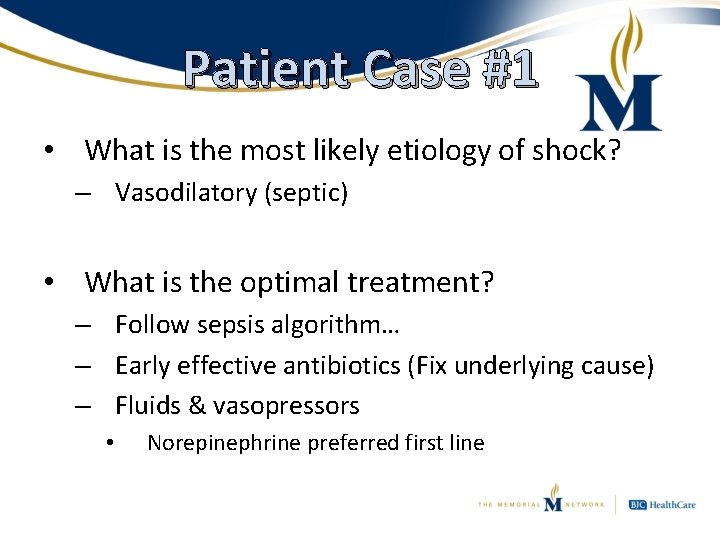
Patient Case #1 • What is the most likely etiology of shock? – Vasodilatory (septic) • What is the optimal treatment? – Follow sepsis algorithm… – Early effective antibiotics (Fix underlying cause) – Fluids & vasopressors • Norepinephrine preferred first line
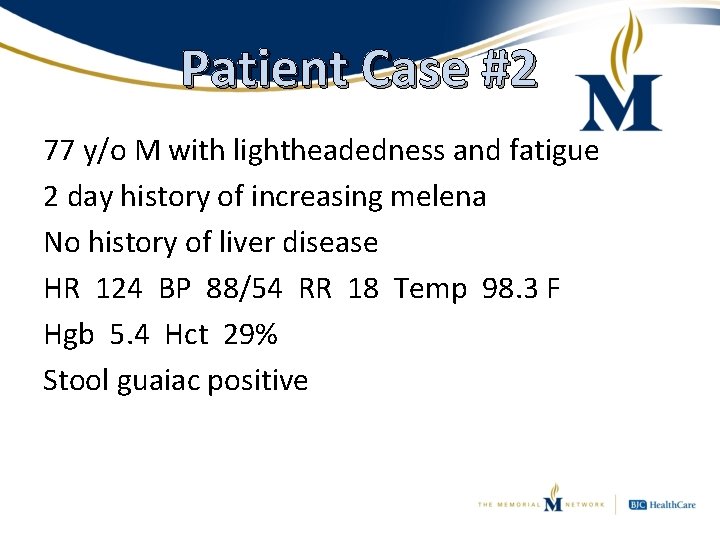
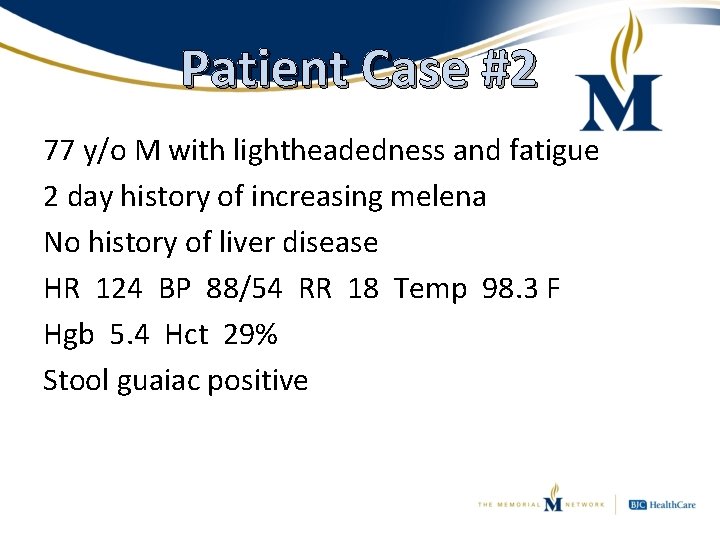
Patient Case #2 77 y/o M with lightheadedness and fatigue 2 day history of increasing melena No history of liver disease HR 124 BP 88/54 RR 18 Temp 98. 3 F Hgb 5. 4 Hct 29% Stool guaiac positive
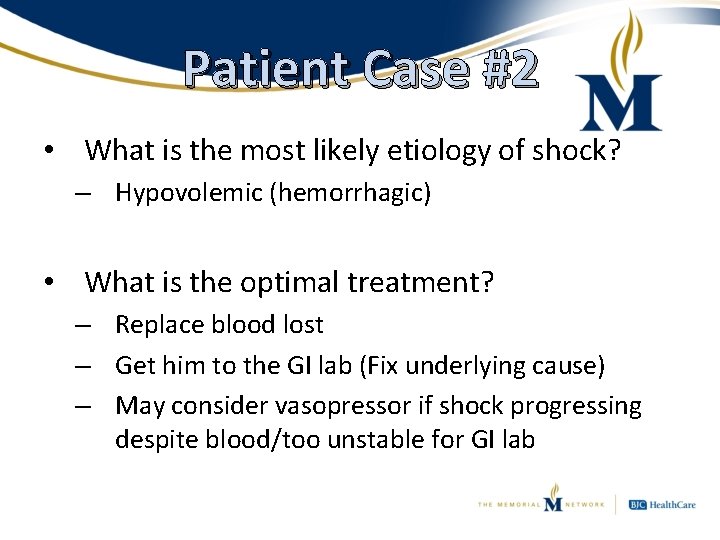
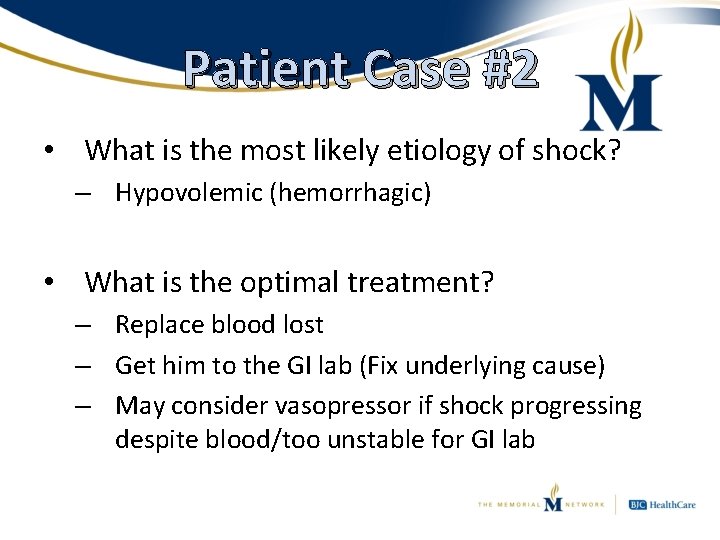
Patient Case #2 • What is the most likely etiology of shock? – Hypovolemic (hemorrhagic) • What is the optimal treatment? – Replace blood lost – Get him to the GI lab (Fix underlying cause) – May consider vasopressor if shock progressing despite blood/too unstable for GI lab
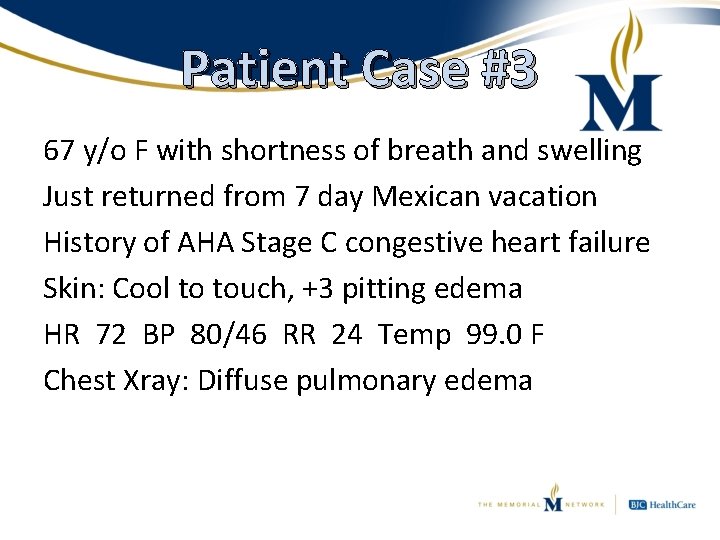
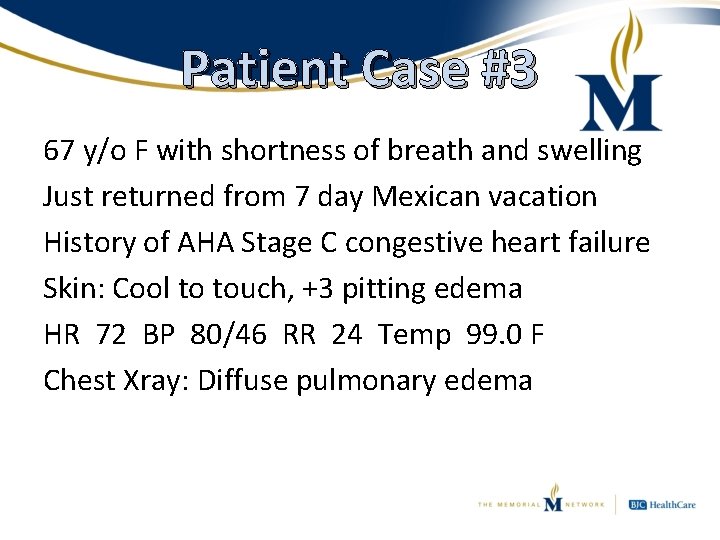
Patient Case #3 67 y/o F with shortness of breath and swelling Just returned from 7 day Mexican vacation History of AHA Stage C congestive heart failure Skin: Cool to touch, +3 pitting edema HR 72 BP 80/46 RR 24 Temp 99. 0 F Chest Xray: Diffuse pulmonary edema
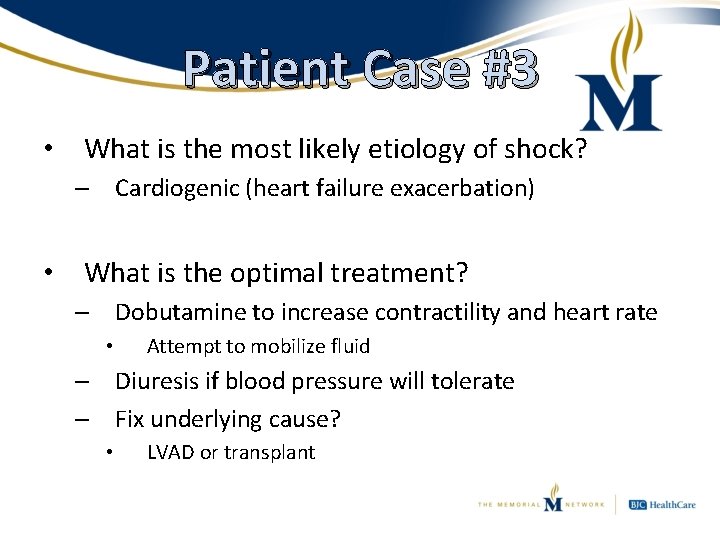
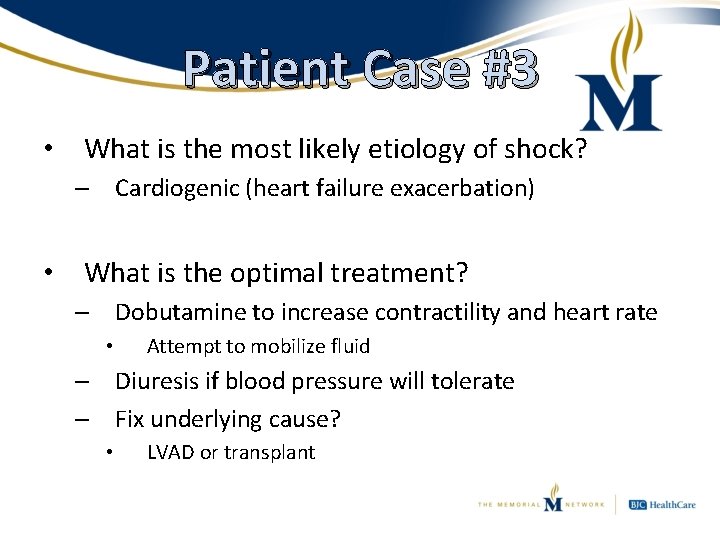
Patient Case #3 • What is the most likely etiology of shock? – Cardiogenic (heart failure exacerbation) • What is the optimal treatment? – Dobutamine to increase contractility and heart rate • Attempt to mobilize fluid – Diuresis if blood pressure will tolerate – Fix underlying cause? • LVAD or transplant
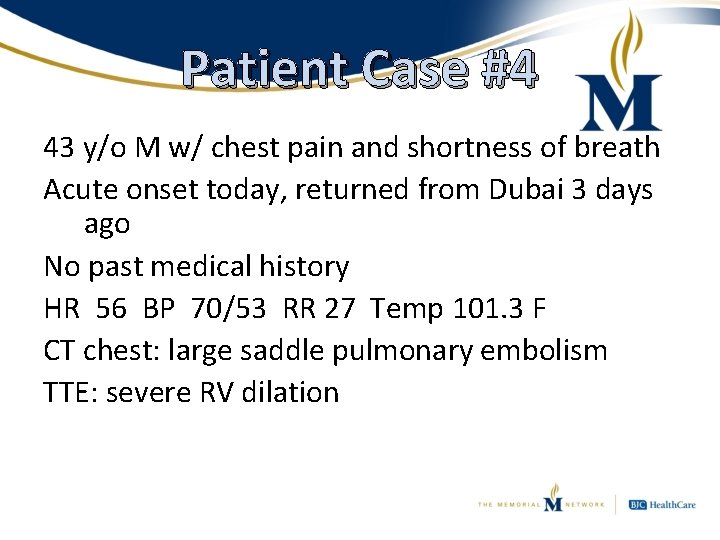
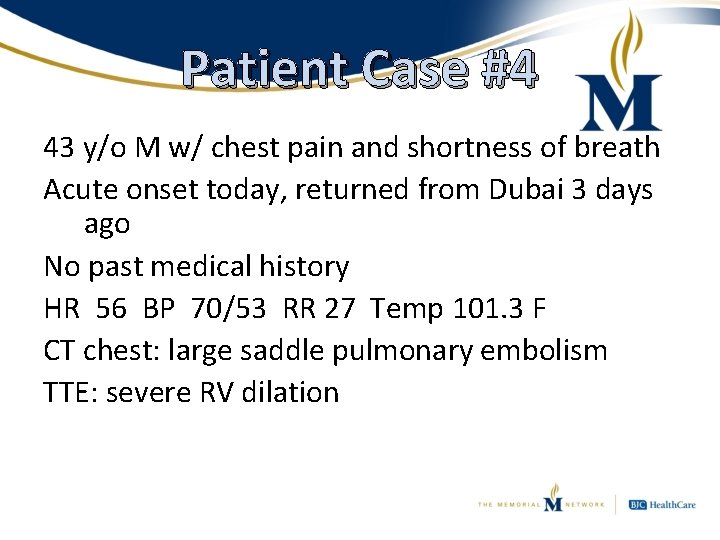
Patient Case #4 43 y/o M w/ chest pain and shortness of breath Acute onset today, returned from Dubai 3 days ago No past medical history HR 56 BP 70/53 RR 27 Temp 101. 3 F CT chest: large saddle pulmonary embolism TTE: severe RV dilation
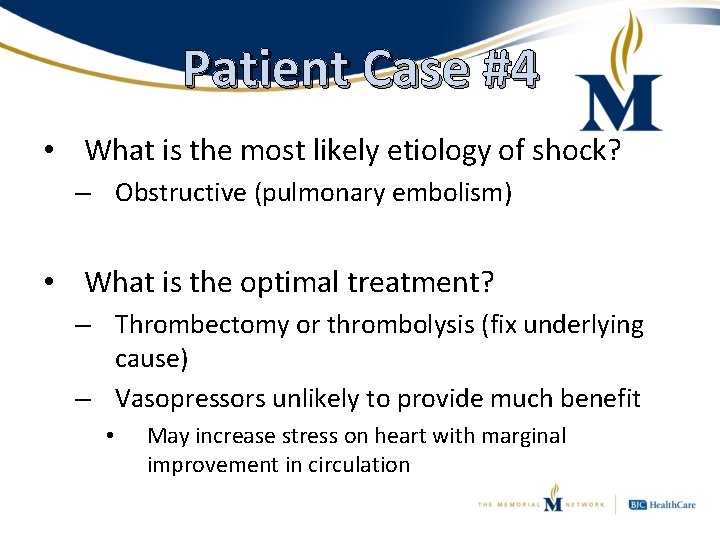
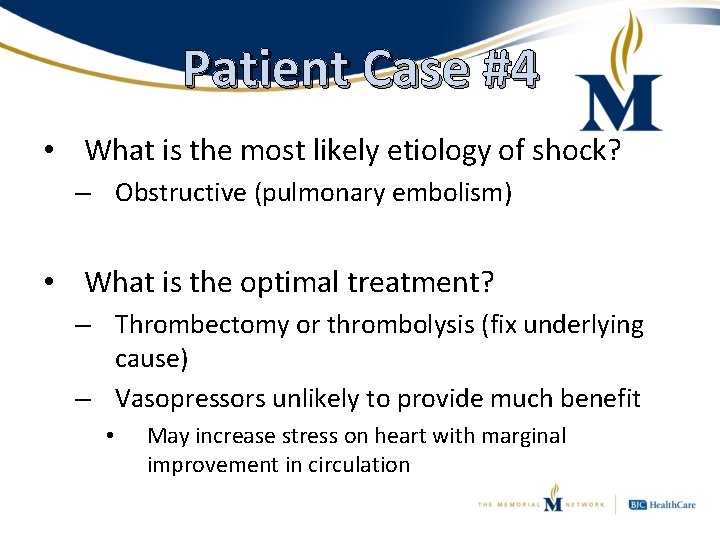
Patient Case #4 • What is the most likely etiology of shock? – Obstructive (pulmonary embolism) • What is the optimal treatment? – Thrombectomy or thrombolysis (fix underlying cause) – Vasopressors unlikely to provide much benefit • May increase stress on heart with marginal improvement in circulation
Summary • Early recognition and classification of shock syndrome can help to guide therapy • Determining the underlying cause and rapidly fixing it (if possible) is the most effective therapy • Commonly used vasopressors have different hemodynamic effects and should be selected based on goals of therapy
Questions? Michael D Schmidt, Pharm. D Critical Care Clinical Pharmacist Belleville Memorial Hospital Belleville, IL mschmidt 2@memhosp. com
 Shock prof
Shock prof Anaphylactic shock risk factors
Anaphylactic shock risk factors Vasopressors
Vasopressors Site:slidetodoc.com
Site:slidetodoc.com Shock normovolemico
Shock normovolemico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Subacute combined degeneration
Subacute combined degeneration Hemodynamics
Hemodynamics Chapter 21 hemodynamics
Chapter 21 hemodynamics Chapter 21 hemodynamics
Chapter 21 hemodynamics Sepsis hour 1 bundle
Sepsis hour 1 bundle Neuroendocrine disorders in gynecology
Neuroendocrine disorders in gynecology What is geriatric syndromes
What is geriatric syndromes Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology Brainstem stroke syndromes
Brainstem stroke syndromes Cerebellar syndromes
Cerebellar syndromes Cerebellar syndromes
Cerebellar syndromes Circumscribing phase
Circumscribing phase Differentiating process examples
Differentiating process examples School environment examples
School environment examples Scaffolding vs differentiation
Scaffolding vs differentiation Differentiating acceleration
Differentiating acceleration Trigonometric functions
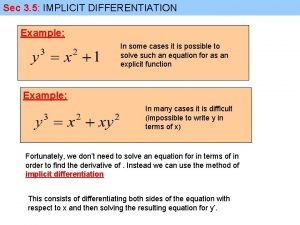
Trigonometric functions Implicit differentation
Implicit differentation Contoh differentiating competencies
Contoh differentiating competencies Contoh threshold competencies
Contoh threshold competencies Differentiating factors in constructing market indexes
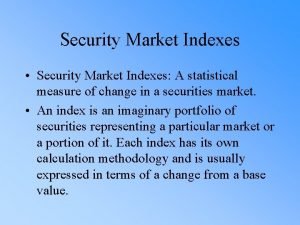
Differentiating factors in constructing market indexes Differentiating ex
Differentiating ex Differentiating factors in constructing market indexes
Differentiating factors in constructing market indexes Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Môn thể thao bắt đầu bằng từ đua
Môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ