Hemodynamics in the OR Definition Hemodynamics The movement

- Slides: 64
Hemodynamics in the OR
Definition Hemodynamics ◦ The movement of blood and the measurement of the pressure involved in that movement. ◦ Pressure = Volume X Resistance With hemodynamic monitoring, we are able to evaluate a patient’s cardiac function, circulating blood volume and response to therapeutic interventions.
Key Concepts Determinants of Cardiac Performance ◦ Heart rate ◦ Contractility ◦ Preload ◦ Afterload
Heart Rate Number of contractions per minute. Quickest way to change cardiac output. Most effective method of changing cardiac output. Versant Advantage, Inc. , 2007
Contractility Inherent property of the myocardium to contract. Regulated by ion concentration, particularly K+. Na+, Ca++. Cannot be directly measured. Reflected in EF, CO, CI and appearance of the patient.
Preload Volume in ventricles at end diastole. Determined by venous return. Measured by CVP or PAOP.
Afterload Impedance (or resistance) that the ventricles must overcome to eject blood. Determined by SVR/PVR, obstructions. Measured by SVR/PVR. SVR = systemic vascular resistance PVR = pulmonary vascular resistance
Technical Considerations Components Leveling of the system Zero balancing Accuracy of system
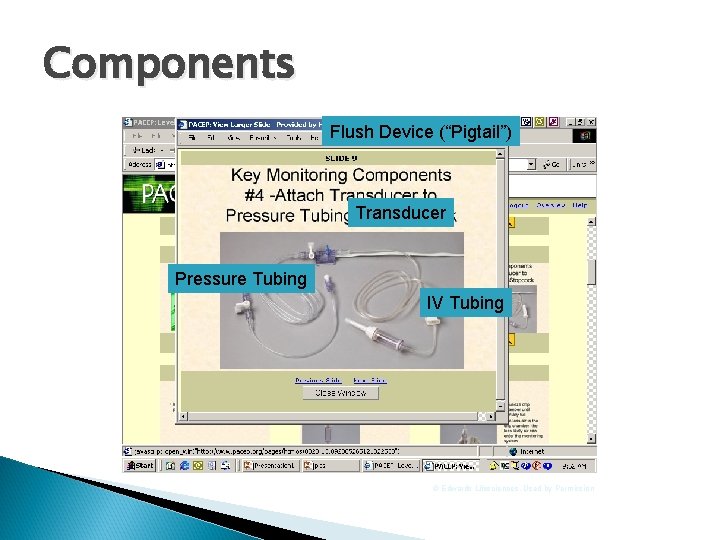
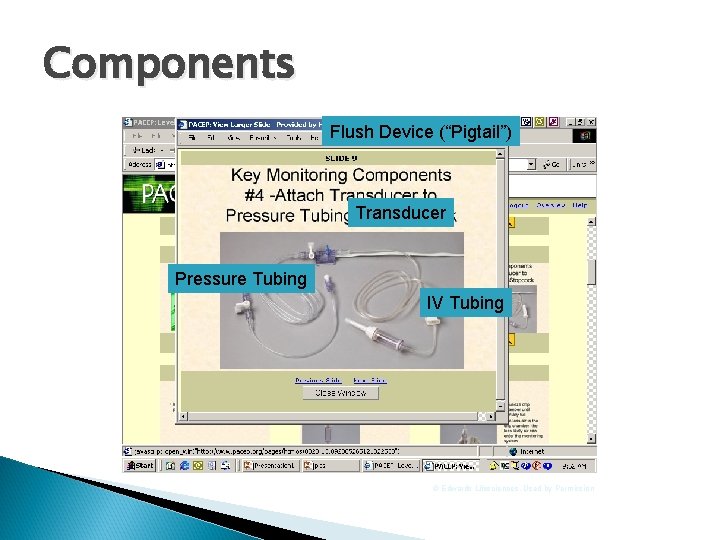
Components Flush Device (“Pigtail”) Transducer Pressure Tubing IV Tubing © Edwards Lifesciences, Used by Permission
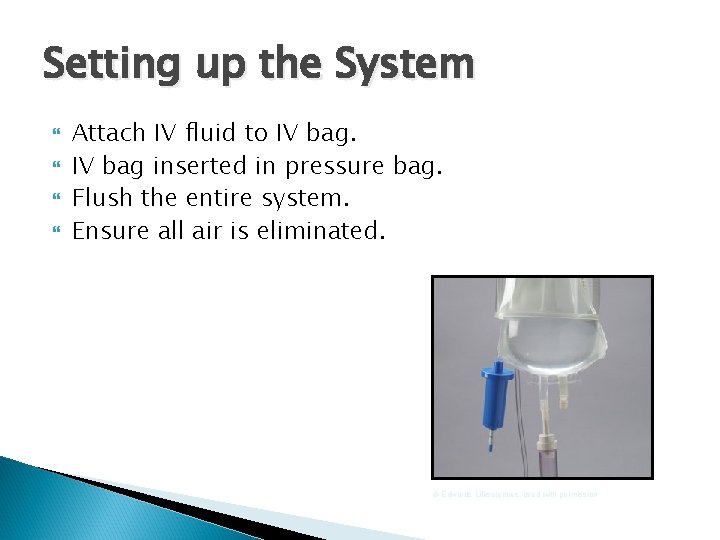
Setting up the System Attach IV fluid to IV bag inserted in pressure bag. Flush the entire system. Ensure all air is eliminated. © Edwards Lifesciences, used with permission
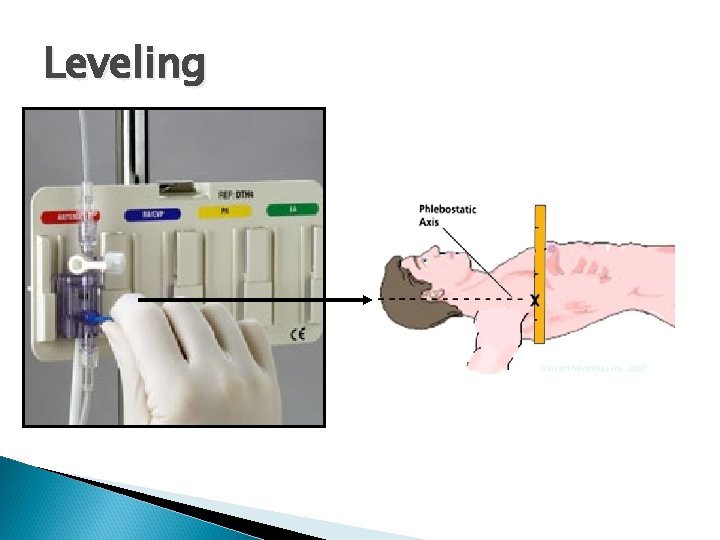
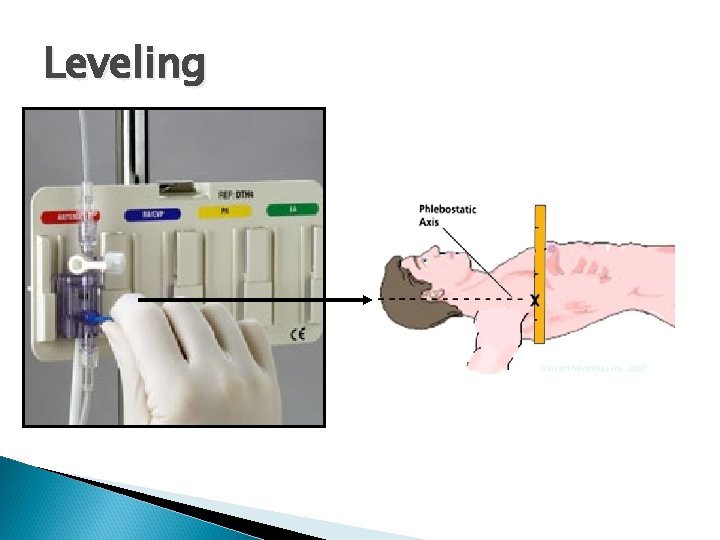
Leveling Versant Advantage Inc. , 2007
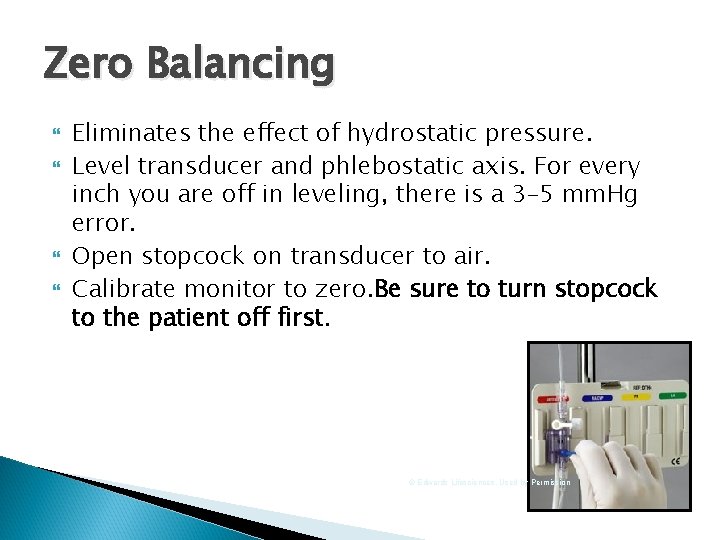
Zero Balancing Eliminates the effect of hydrostatic pressure. Level transducer and phlebostatic axis. For every inch you are off in leveling, there is a 3– 5 mm. Hg error. Open stopcock on transducer to air. Calibrate monitor to zero. Be sure to turn stopcock to the patient off first. © Edwards Lifesciences, Used by Permission
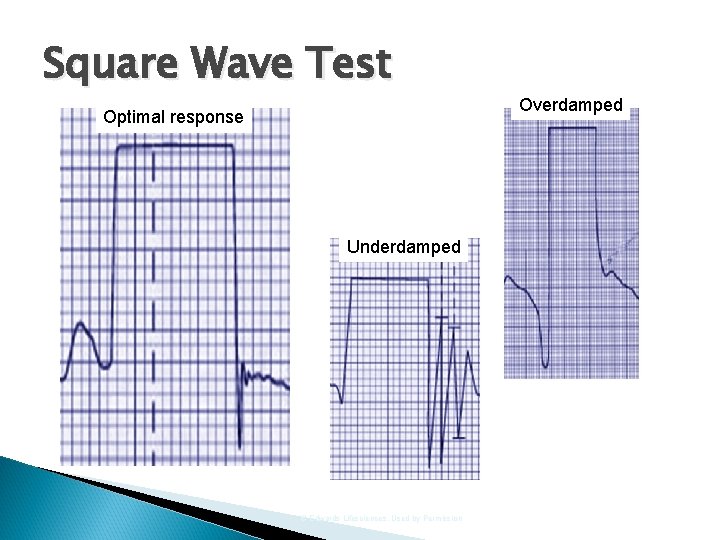
Accuracy Natural Frequency: Damping Coefficient Ratio Measures the system’s overall capability of accurately reproducing signals. Test for accuracy (Frequency Response) with the square wave test.
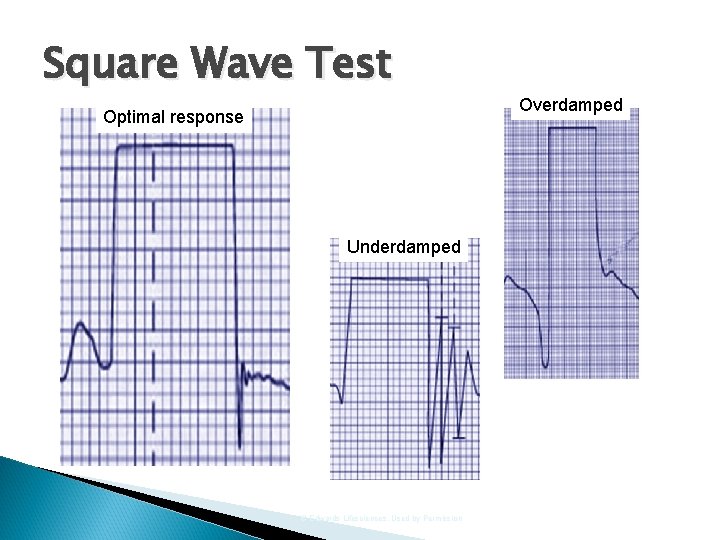
Square Wave Test Optimal response Underdamped © Edwards Lifesciences, Used by Permission Overdamped
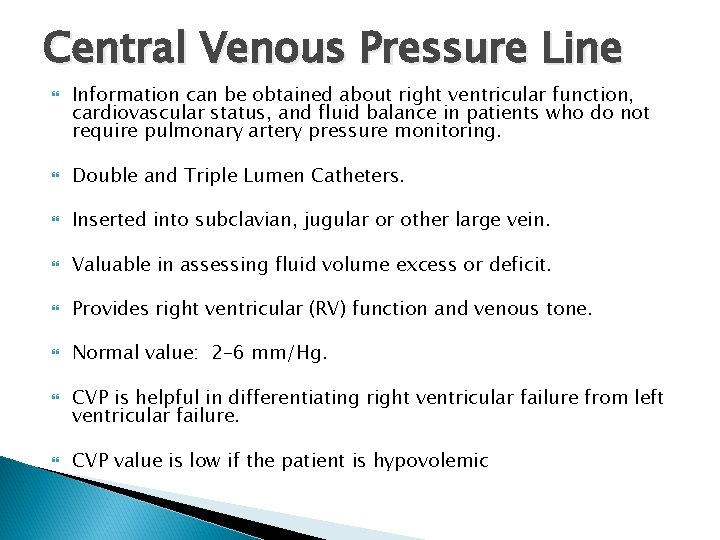
Central Venous Pressure Line Information can be obtained about right ventricular function, cardiovascular status, and fluid balance in patients who do not require pulmonary artery pressure monitoring. Double and Triple Lumen Catheters. Inserted into subclavian, jugular or other large vein. Valuable in assessing fluid volume excess or deficit. Provides right ventricular (RV) function and venous tone. Normal value: 2– 6 mm/Hg. CVP is helpful in differentiating right ventricular failure from left ventricular failure. CVP value is low if the patient is hypovolemic
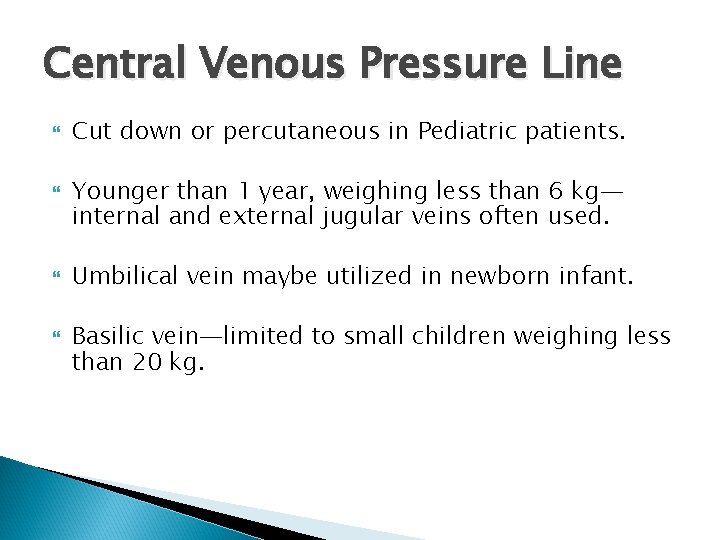
Central Venous Pressure Line Cut down or percutaneous in Pediatric patients. Younger than 1 year, weighing less than 6 kg— internal and external jugular veins often used. Umbilical vein maybe utilized in newborn infant. Basilic vein—limited to small children weighing less than 20 kg.
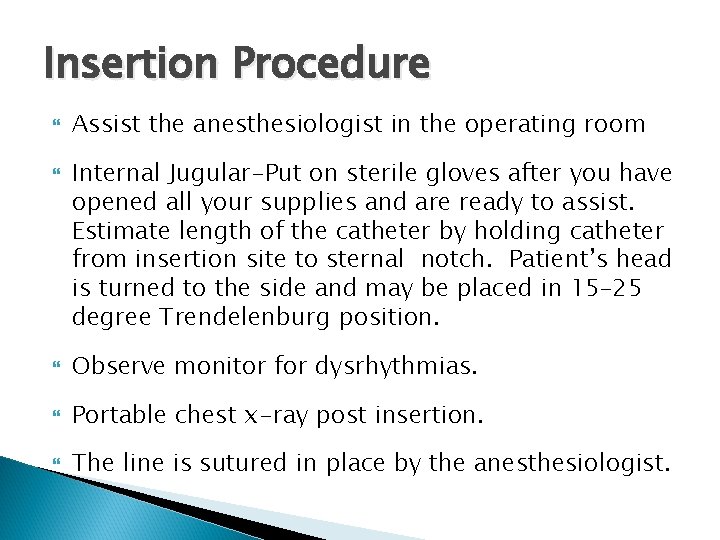
Insertion Procedure Assist the anesthesiologist in the operating room Internal Jugular-Put on sterile gloves after you have opened all your supplies and are ready to assist. Estimate length of the catheter by holding catheter from insertion site to sternal notch. Patient’s head is turned to the side and may be placed in 15– 25 degree Trendelenburg position. Observe monitor for dysrhythmias. Portable chest x-ray post insertion. The line is sutured in place by the anesthesiologist.
Indications for Central Lines Administration of Fluids or Blood Products Medication Access Parenteral Nutrition CVP Monitoring Transvenous Pacemaker Access Lack of Peripheral Access
Contraindications of Central Lines Coagulopathy Fibrinolytic Therapy Infection at Site High risk of pneumothorax ◦ PEEP, CPAP, COPD #1 Complication–Infection
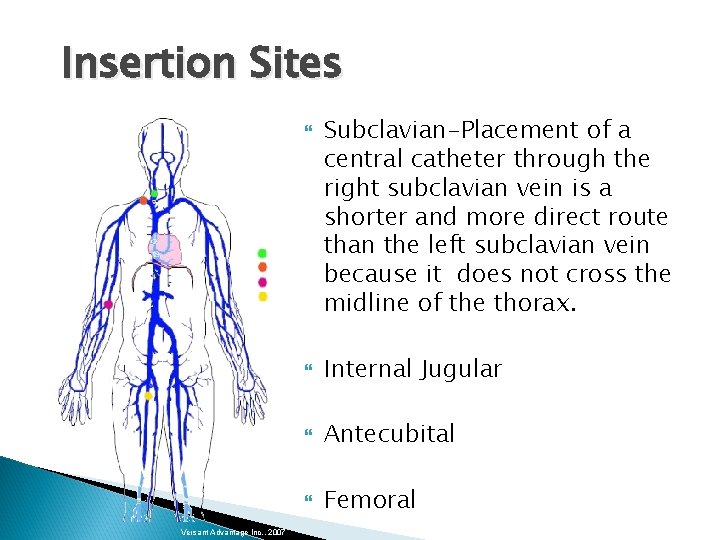
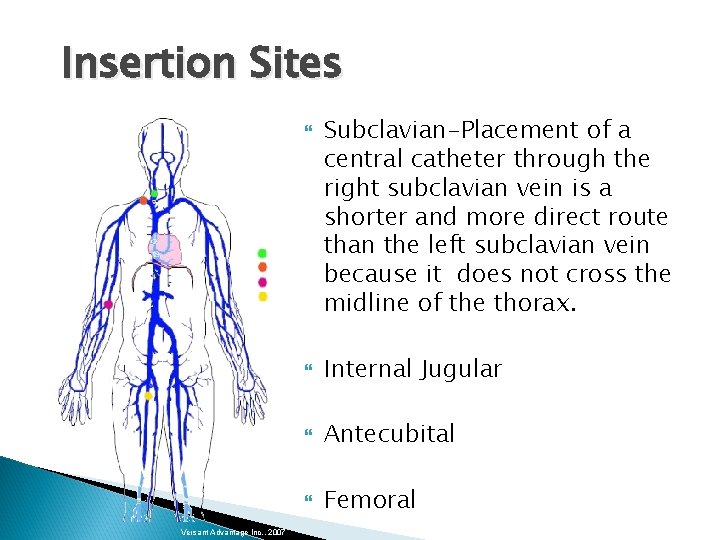
Insertion Sites Versant Advantage Inc. , 2007 Subclavian-Placement of a central catheter through the right subclavian vein is a shorter and more direct route than the left subclavian vein because it does not cross the midline of the thorax. Internal Jugular Antecubital Femoral
Subclavian Vein Advantages: ◦ Easily accessible ◦ Ease in maintaining sterile dressing ◦ Low incidence of thrombosis
Subclavian Vein Disadvantages: ◦ Risk of air embolism ◦ Possible puncture of subclavian artery ◦ Risk of pneumothorax ◦ Nerve injury ◦ Tracheal perforation ◦ ET cuff perforation

Internal Jugular Vein Advantages: ◦ Direct path to SVC ◦ Low rate of thrombosis ◦ Low incidence of pneumothorax
Internal Jugular Vein Disadvantages: ◦ Air embolism ◦ Puncture of carotid artery ◦ Puncture of trachea or ET
Femoral Vein Advantages: ◦ Easy access ◦ Familiarity with site
Femoral Vein Disadvantages: ◦ Infection ◦ Difficulty in maintaining dressing ◦ Difficult to locate in obese patients ◦ Thrombosis risk ◦ Difficulty in immobilization
Antecubital Sites Advantages: ◦ No risk of pneumothorax ◦ Bleeding easily controlled
Antecubital Sites Disadvantages: ◦ Difficult in obese ◦ Cutdown required ◦ Thrombosis risk ◦ Advancement difficult ◦ Vein small ◦ Must immobilize arm ◦ Dislodgement
Documentation Type of catheter Site of insertion Dysrhythmias noted Difficulty during insertion Pressure values Microsoft Office Clipart
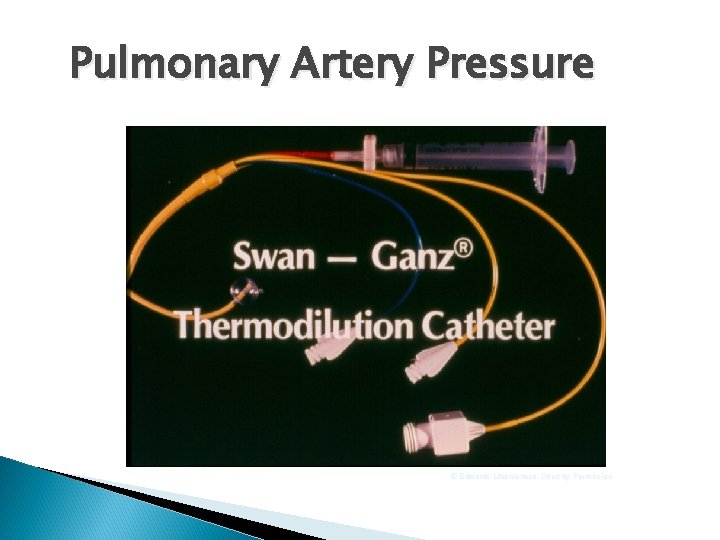
Pulmonary Artery Pressure © Edwards Lifesciences, Used by Permission
Pulmonary Artery Monitoring With the catheter in place, we can monitor pressures in: 1. Right atrium- RA pressure and CVP pressure are synonymous in clinical practice. 2. Pulmonary artery 3. Left atrium 4. Left ventricle-this is an indirect measurement
PA Catheter Sizes In adults— 7. 5 F Two general sizes for pediatrics: ◦ 5. 0 or 5. 5 F for 10 -25 kg patients More easily occluded ◦ 7. 0— 7. 5 F catheter for over 25 kg
Indications for PA Monitoring Assessment of cardiovascular function ◦ MI, CHF Shock Assessment of pulmonary status ◦ ARDS, PE, Pulmonary HTN, CHF Assessment of fluid requirements ◦ Burns These measurements are usually taken to locate the source of the patient’s circulatory problem, determine circulating blood volume, get the earliest possible warning signs of compromised circulation and monitor the effects of treatment.
Indications for PA Monitoring Perioperative monitoring Therapeutic ◦ Aspiration of Air Emboli ◦ Ventricular pacing Diagnostic ◦ Mixed venous blood, SVO 2 monitoring ◦ Heart catheterization
Indications for PA Monitoring in Children Shock. For precise tracking of parameters. Postoperative monitoring of unstable patient. Tracking of oxygen transport parameters. Severe pulmonary hypertension.
Contraindications for PA Monitoring in Children Presence of large intracardiac shunts. Serious dysrhythmias. Low cardiac output. Any time potential risks outweigh potential benefits.
Insertion Have line set up and zeroed. Explain procedure to patient. Have supplies ready. Flush ports PRIOR to insertion. Inserted by physician. Record procedures. Apply dressing.
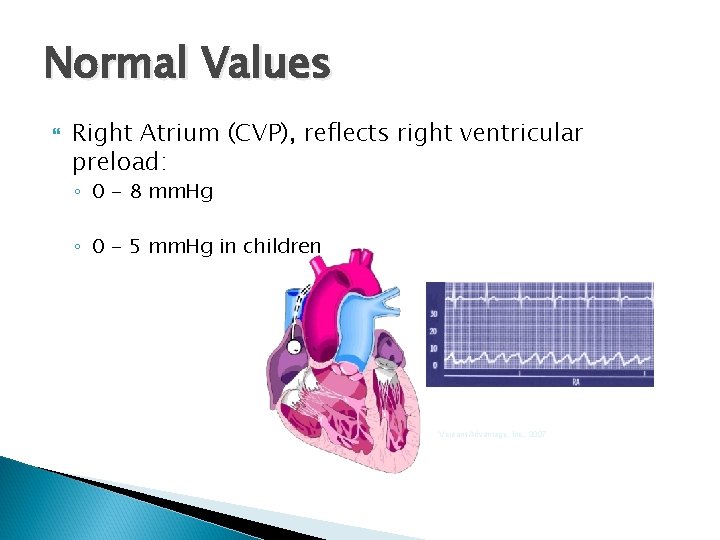
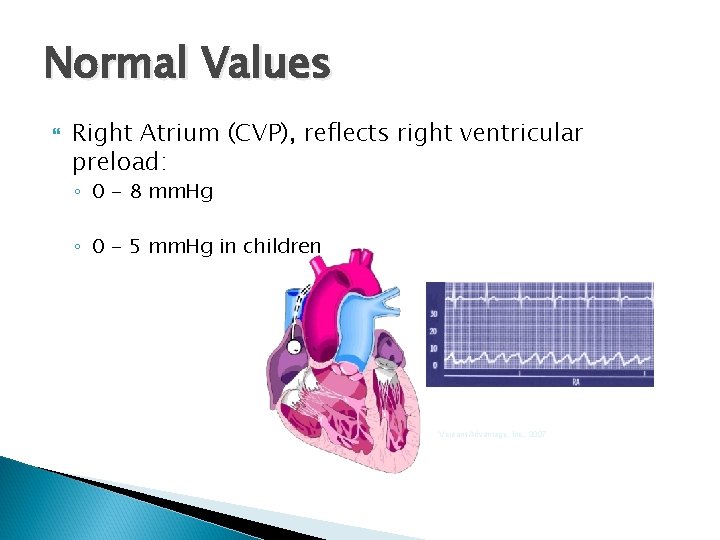
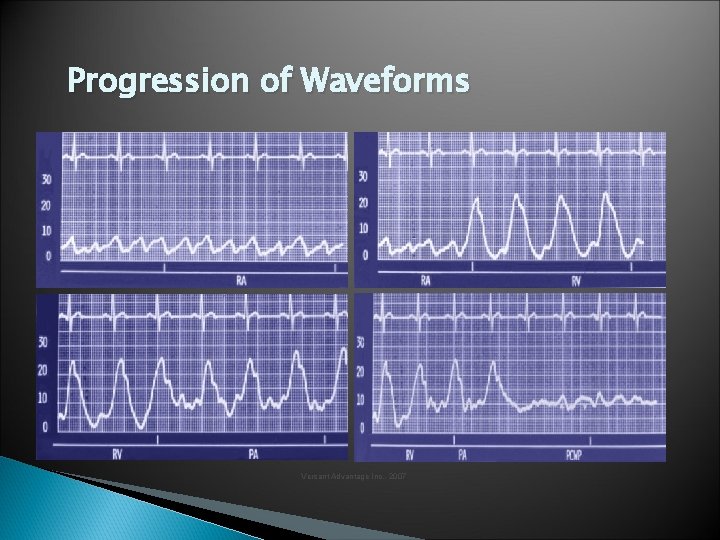
Normal Values Right Atrium (CVP), reflects right ventricular preload: ◦ 0 - 8 mm. Hg ◦ 0 - 5 mm. Hg in children Versant Advantage, Inc. , 2007
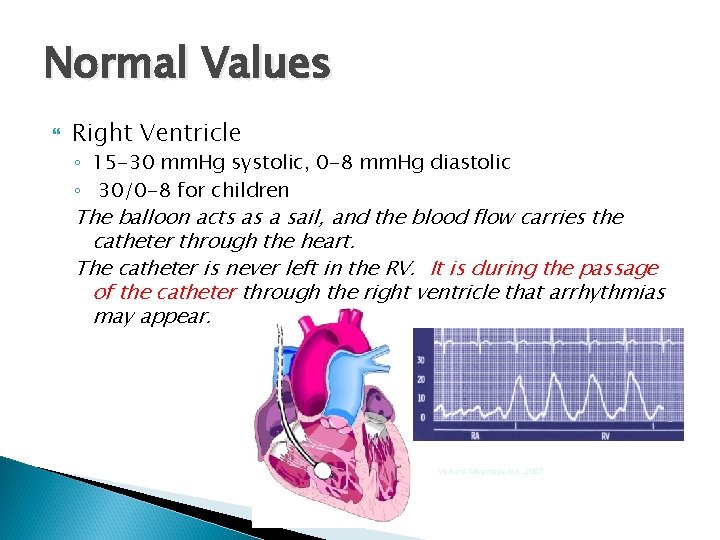
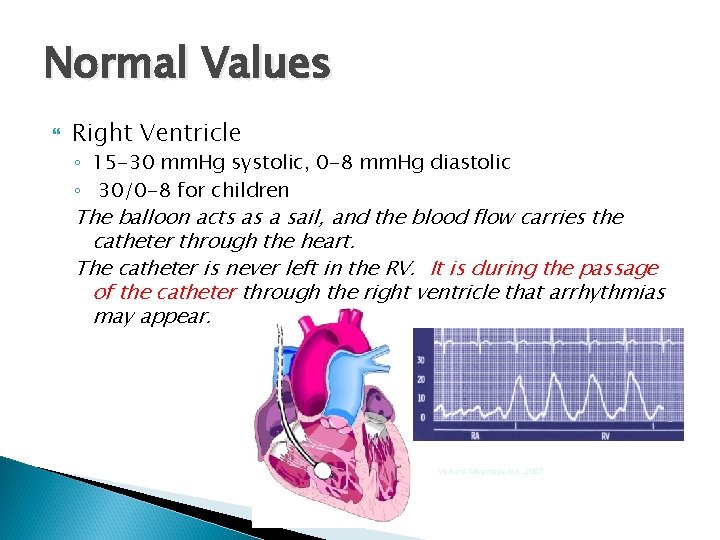
Normal Values Right Ventricle ◦ 15 -30 mm. Hg systolic, 0 -8 mm. Hg diastolic ◦ 30/0 -8 for children The balloon acts as a sail, and the blood flow carries the catheter through the heart. The catheter is never left in the RV. It is during the passage of the catheter through the right ventricle that arrhythmias may appear. Versant Advantage Inc. , 2007
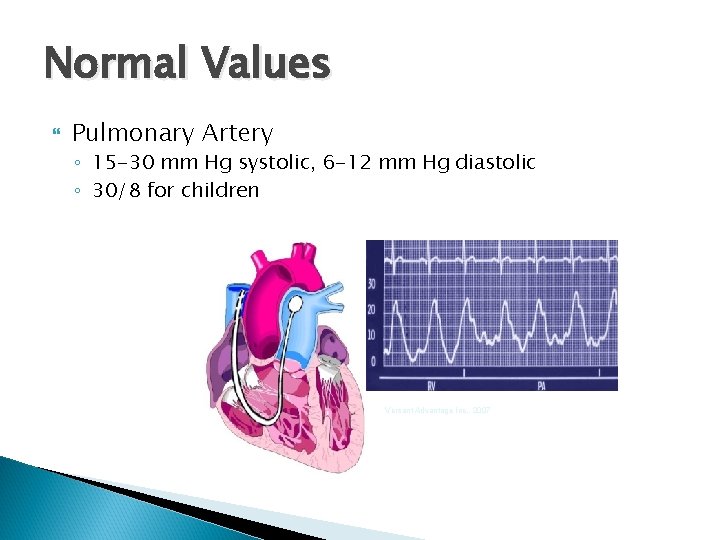
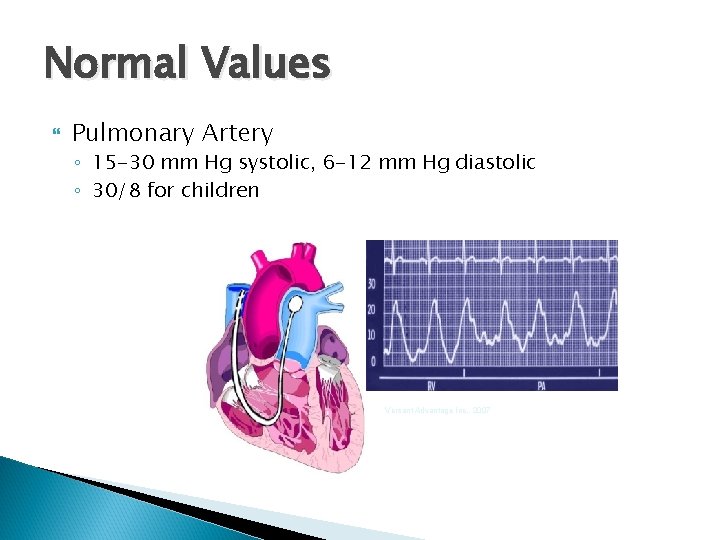
Normal Values Pulmonary Artery ◦ 15 -30 mm Hg systolic, 6 -12 mm Hg diastolic ◦ 30/8 for children Versant Advantage Inc. , 2007
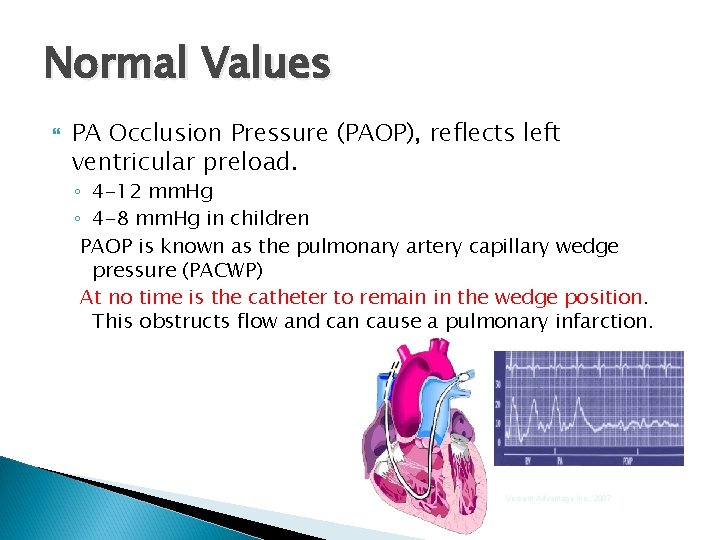
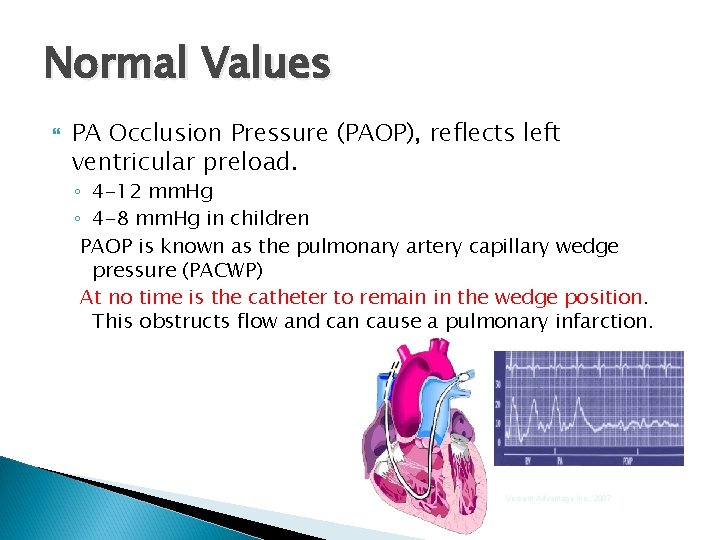
Normal Values PA Occlusion Pressure (PAOP), reflects left ventricular preload. ◦ 4 -12 mm. Hg ◦ 4 -8 mm. Hg in children PAOP is known as the pulmonary artery capillary wedge pressure (PACWP) At no time is the catheter to remain in the wedge position. This obstructs flow and can cause a pulmonary infarction. Versant Advantage Inc. , 2007
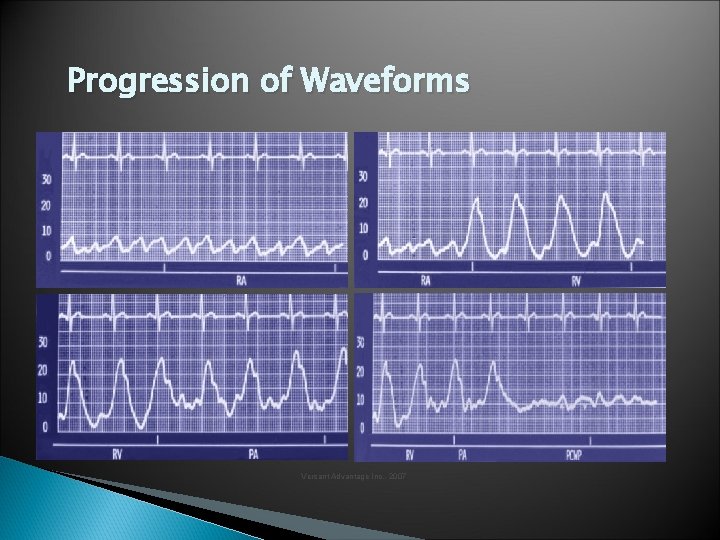
Progression of Waveforms Versant Advantage Inc. , 2007
Abnormal Values Increased ◦ Hypervolemia / Fluid overload ◦ Pulmonary Hypertension ◦ Valvular Stenosis / Regurgitation ◦ PE ◦ Cardiac Tamponade
Abnormal Values Decreased: ◦ Hypovolemia/Dehydration ◦ Hemorrhage ◦ Vasodilation
Considerations Treat the patient, not the monitor. Allow air to escape from balloon passively. Balloon capacity 1. 5 cc max (less in smaller catheters). Do not overfill the balloon. If the balloon does not inflate with 1. 5 cc of air, it will not inflate with more. To force more air into the balloon Do not allow the balloon to be inflated for greater than 8 -15 seconds. Prolonged and excessive inflation of the balloon and overinflation cause pulmonary infarction Fast flush often helps in the prevention of clot formation. .
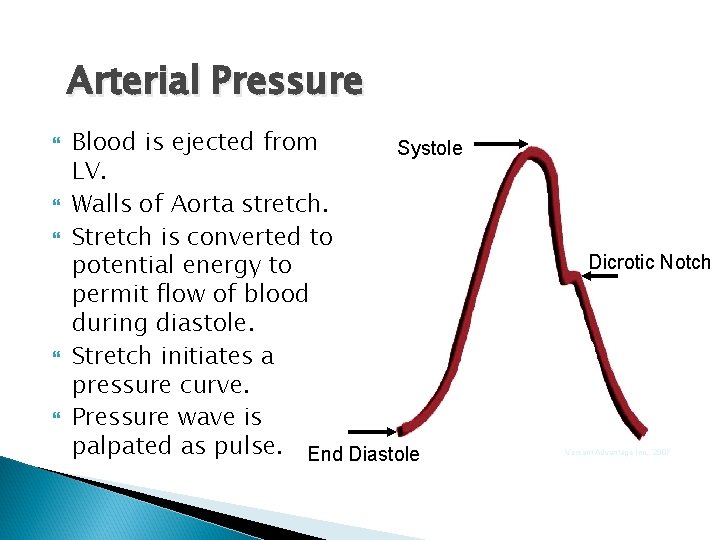
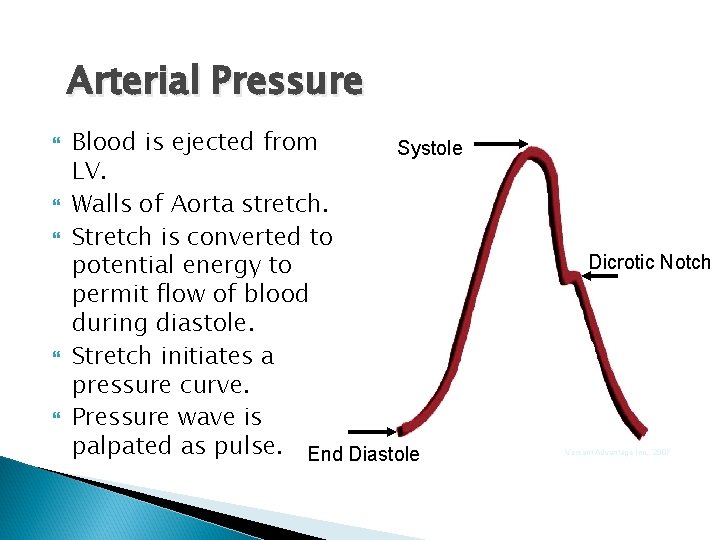
Arterial Pressure Blood is ejected from Systole LV. Walls of Aorta stretch. Stretch is converted to potential energy to permit flow of blood during diastole. Stretch initiates a pressure curve. Pressure wave is palpated as pulse. End Diastole Dicrotic Notch Versant Advantage Inc. , 2007
Indications for Arterial Cannulation Perioperative monitoring Major procedures Hemodynamically unstable patients Monitor vasopressor or vasodilator therapy IABP Intracranial pressure monitoring Hypertensive crisis ABG monitoring
Sites for Arterial Cannulation Radial artery ◦ Easily accessible Brachial artery ◦ Difficult to immobilize Femoral artery ◦ Useful in shock patients ◦ Possible hematoma & embolus
Sites for Arterial Cannulation Pediatric In all but the smallest neonates, radial artery is preferred. Dorsalis pedis and posterior tibial arteries may also be used. Umbilical arteries—can be cannulated for the first several days of life before obliterated. ◦ Used in neonates ◦ Safe ◦ Reliable
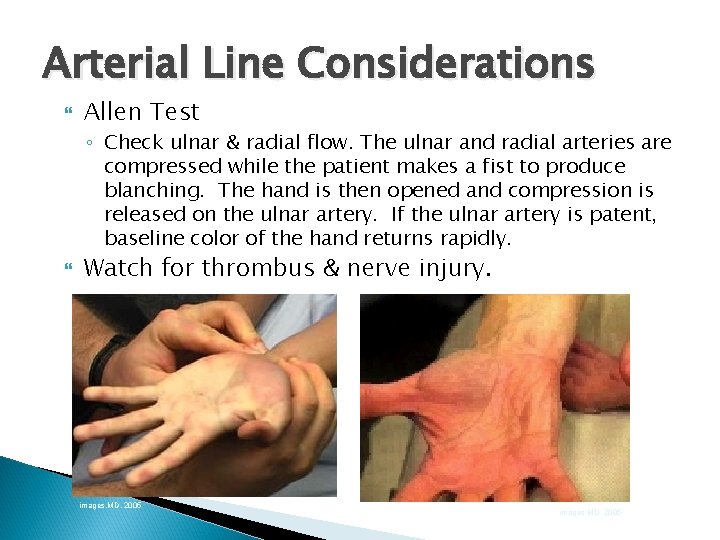
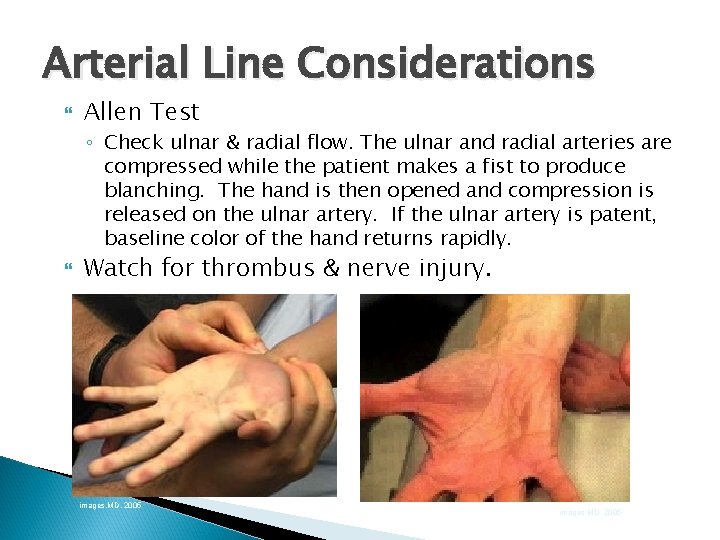
Arterial Line Considerations Allen Test ◦ Check ulnar & radial flow. The ulnar and radial arteries are compressed while the patient makes a fist to produce blanching. The hand is then opened and compression is released on the ulnar artery. If the ulnar artery is patent, baseline color of the hand returns rapidly. Watch for thrombus & nerve injury. images. MD, 2005
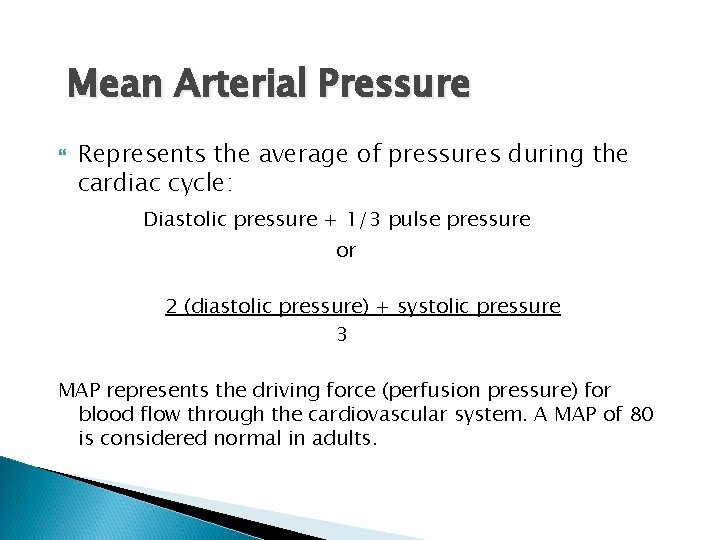
Mean Arterial Pressure Represents the average of pressures during the cardiac cycle: Diastolic pressure + 1/3 pulse pressure or 2 (diastolic pressure) + systolic pressure 3 MAP represents the driving force (perfusion pressure) for blood flow through the cardiovascular system. A MAP of 80 is considered normal in adults.
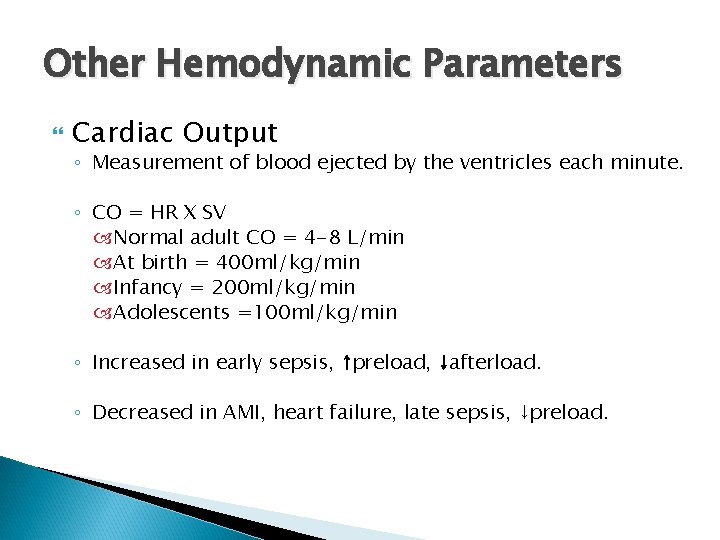
Other Hemodynamic Parameters Cardiac Output ◦ Measurement of blood ejected by the ventricles each minute. ◦ CO = HR X SV Normal adult CO = 4 -8 L/min At birth = 400 ml/kg/min Infancy = 200 ml/kg/min Adolescents =100 ml/kg/min ◦ Increased in early sepsis, ↑preload, ↓afterload. ◦ Decreased in AMI, heart failure, late sepsis, ↓preload.
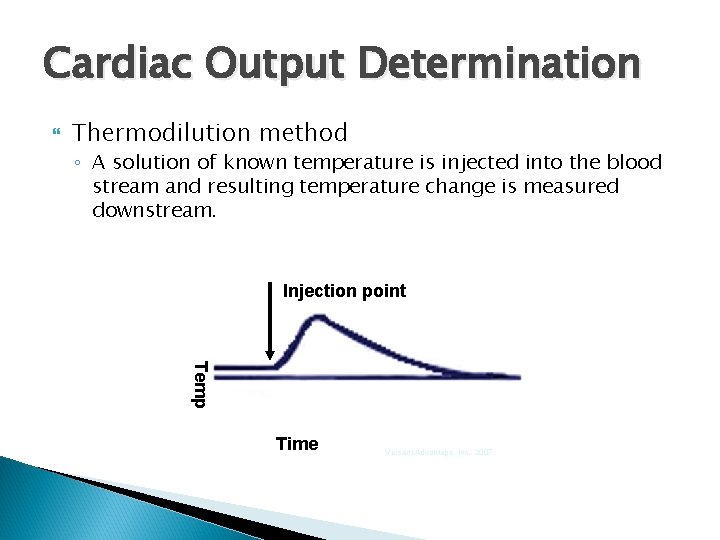
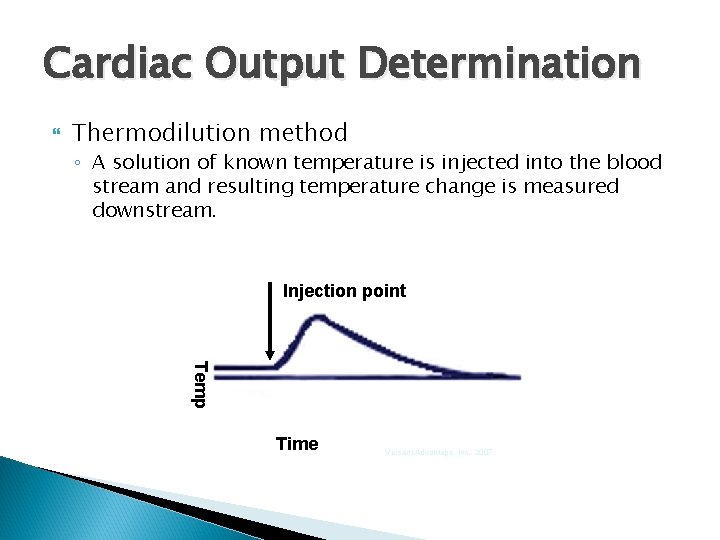
Cardiac Output Determination Thermodilution method ◦ A solution of known temperature is injected into the blood stream and resulting temperature change is measured downstream. Injection point Temp Time Versant Advantage, Inc. , 2007
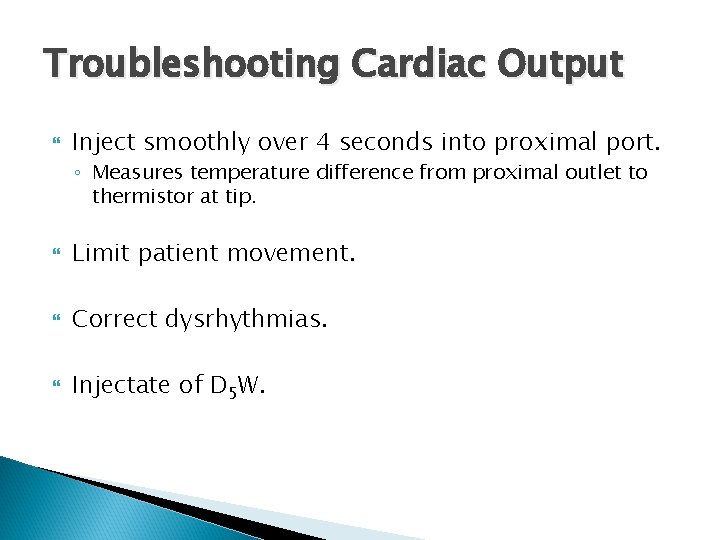
Troubleshooting Cardiac Output Inject smoothly over 4 seconds into proximal port. ◦ Measures temperature difference from proximal outlet to thermistor at tip. Limit patient movement. Correct dysrhythmias. Injectate of D 5 W.
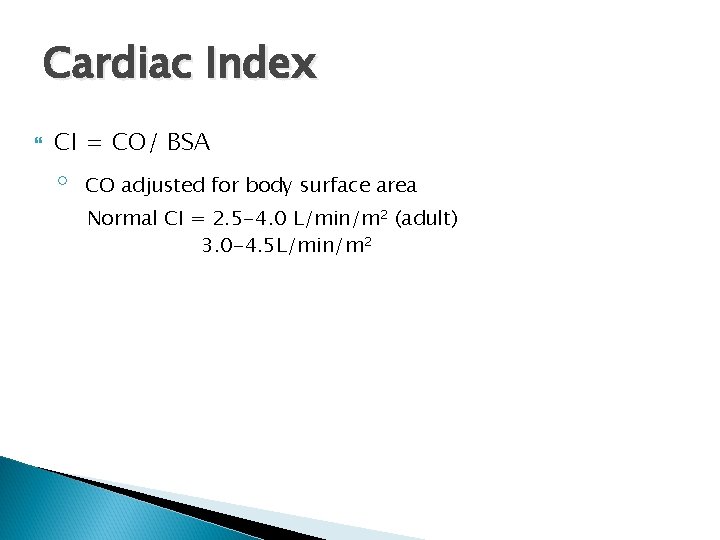
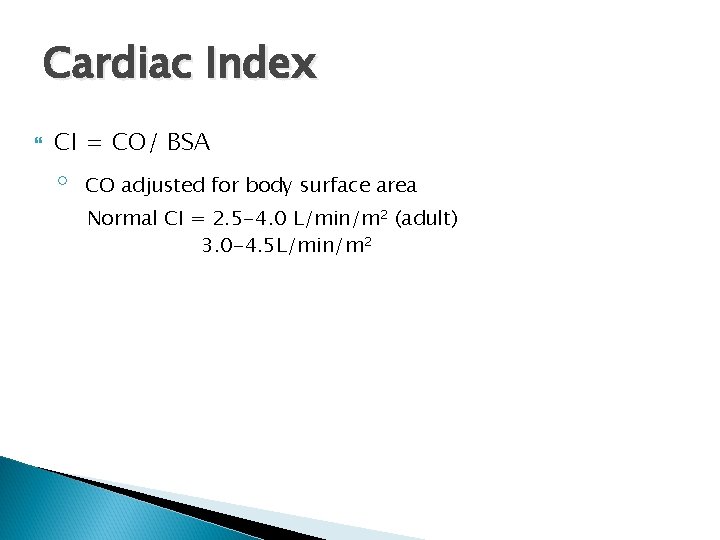
Cardiac Index CI = CO/ BSA ◦ CO adjusted for body surface area Normal CI = 2. 5 -4. 0 L/min/m 2 (adult) 3. 0 -4. 5 L/min/m 2
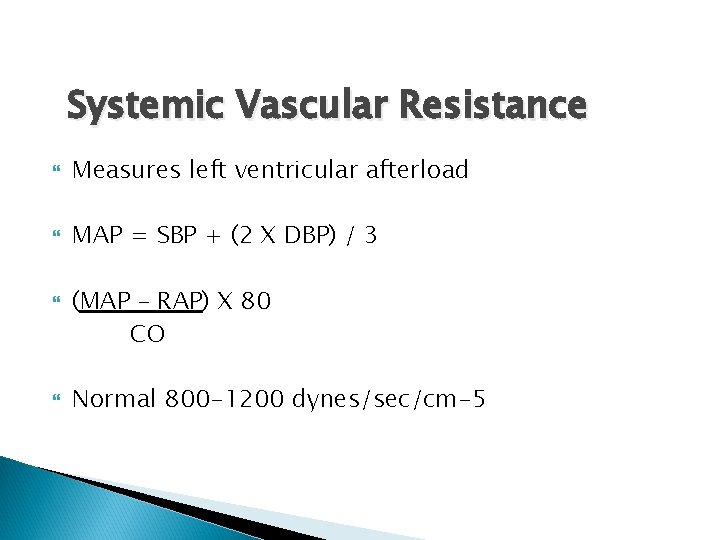
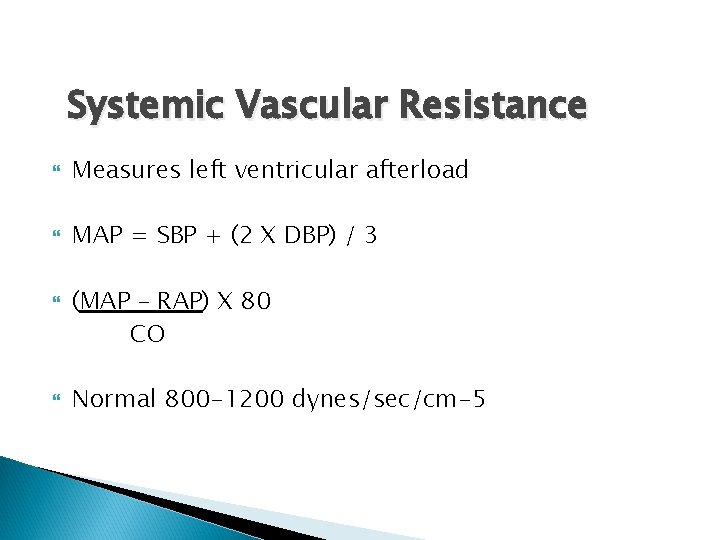
Systemic Vascular Resistance Measures left ventricular afterload MAP = SBP + (2 X DBP) / 3 (MAP – RAP) X 80 CO Normal 800 -1200 dynes/sec/cm-5
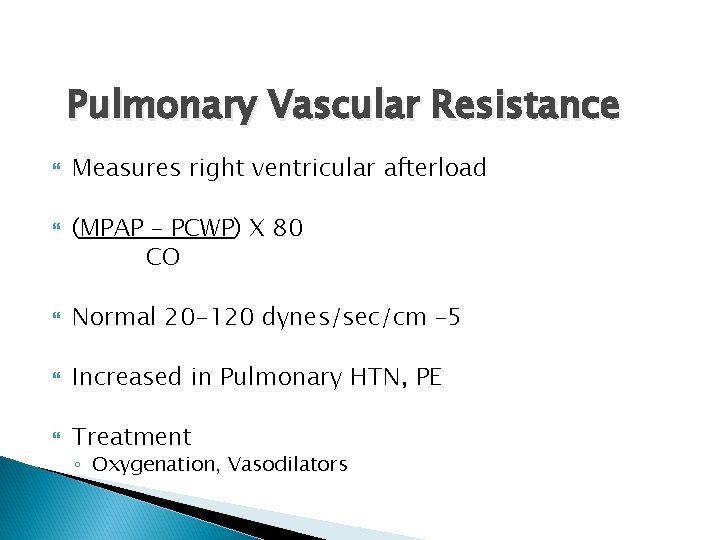
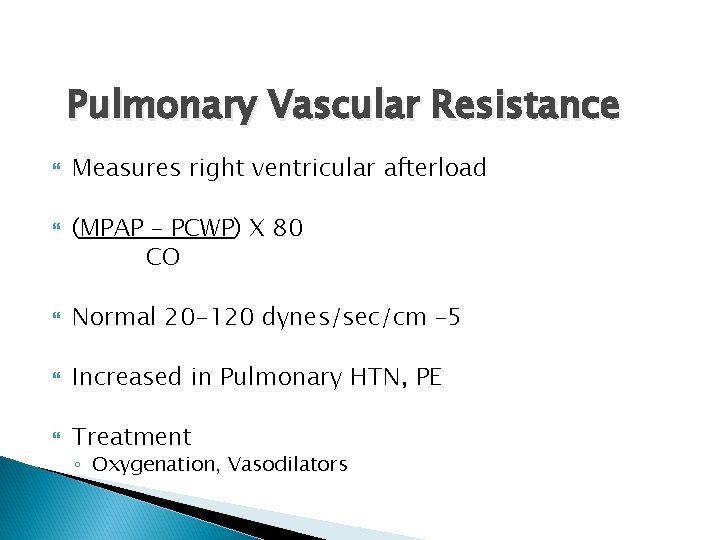
Pulmonary Vascular Resistance Measures right ventricular afterload (MPAP – PCWP) X 80 CO Normal 20 -120 dynes/sec/cm – 5 Increased in Pulmonary HTN, PE Treatment ◦ Oxygenation, Vasodilators
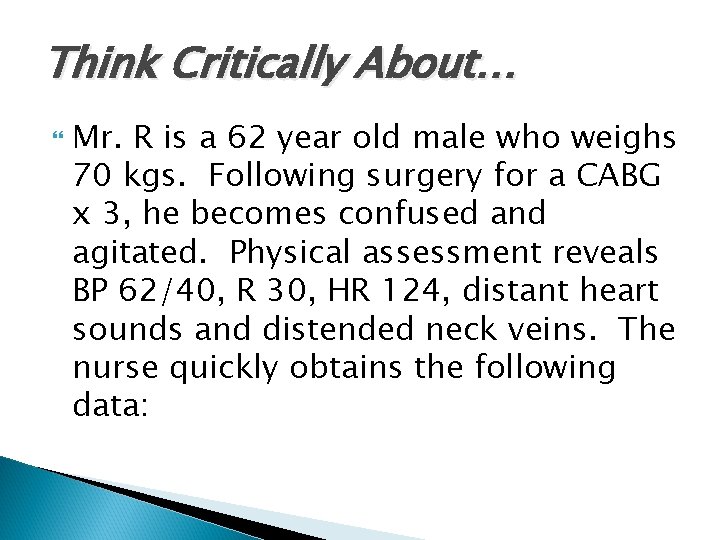
Think Critically About… Mr. R is a 62 year old male who weighs 70 kgs. Following surgery for a CABG x 3, he becomes confused and agitated. Physical assessment reveals BP 62/40, R 30, HR 124, distant heart sounds and distended neck veins. The nurse quickly obtains the following data:
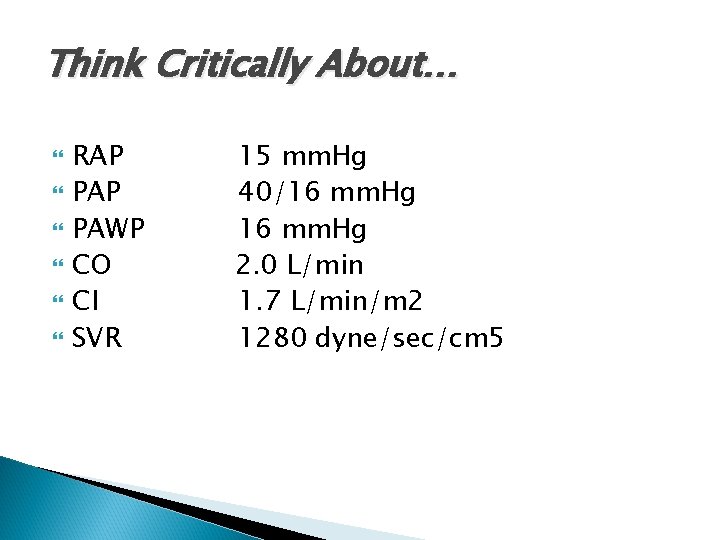
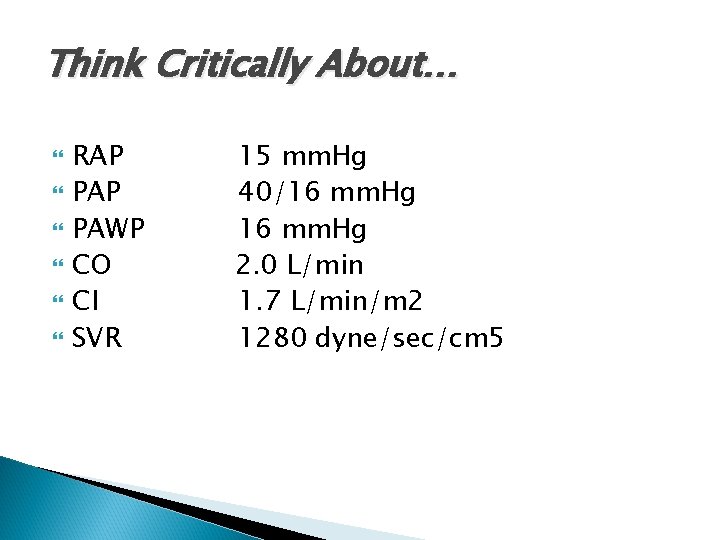
Think Critically About… RAP PAWP CO CI SVR 15 mm. Hg 40/16 mm. Hg 2. 0 L/min 1. 7 L/min/m 2 1280 dyne/sec/cm 5
Think Critically About… Are his hemodynamic parameters within normal limits? High or low? What is your assessment of the situation? What are appropriate nursing actions with this condition?
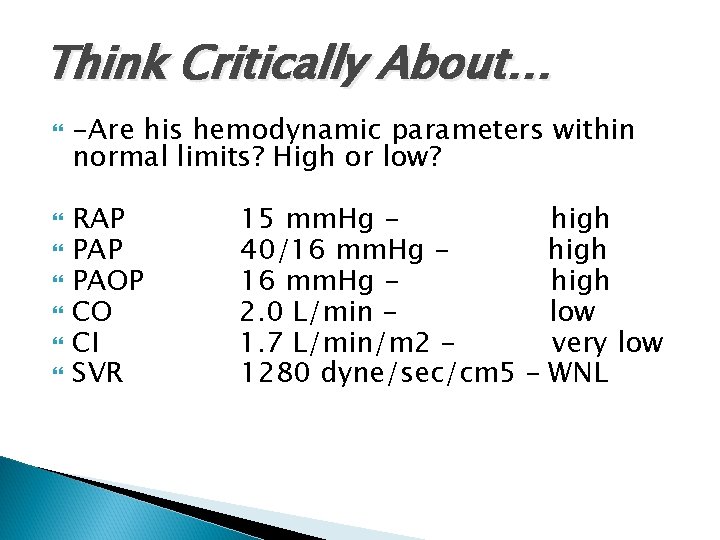
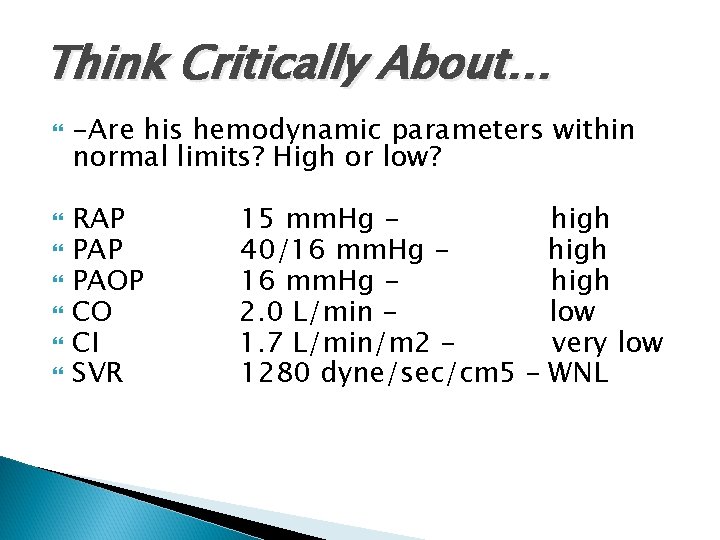
Think Critically About… -Are his hemodynamic parameters within normal limits? High or low? RAP PAOP CO CI SVR 15 mm. Hg high 40/16 mm. Hg high 2. 0 L/min low 1. 7 L/min/m 2 – very low 1280 dyne/sec/cm 5 – WNL
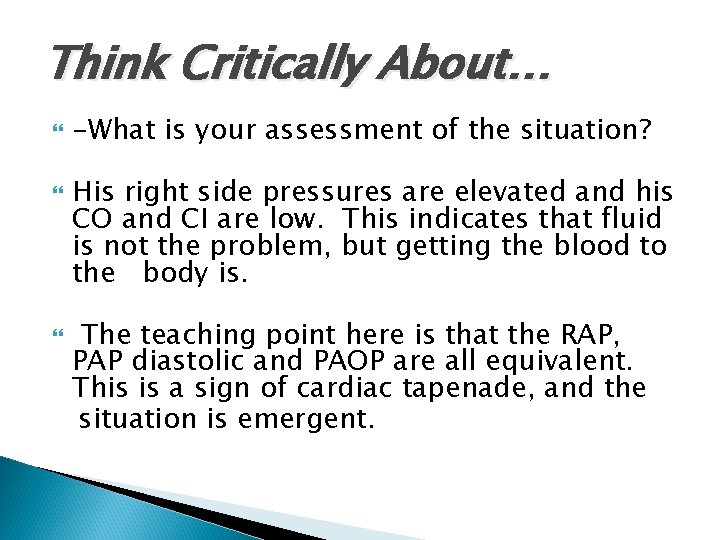
Think Critically About… -What is your assessment of the situation? His right side pressures are elevated and his CO and CI are low. This indicates that fluid is not the problem, but getting the blood to the body is. The teaching point here is that the RAP, PAP diastolic and PAOP are all equivalent. This is a sign of cardiac tapenade, and the situation is emergent.
Think Critically About… Assessment of the situation continued Cardiac tamponade is the accumulation of fluid (in this case, blood) in the pericardial sac. The blood increases the intracardiac pressures and compresses the atria and ventricles (thus the rise in pressures). This leads to decreased venous return and decreased filling pressures which leads to decreased cardiac output.
Think Critically About… Assessment of the situation continued In addition, the classical presentation of tamponade is called Beck’s triad— presence of elevated CVP, distended neck veins and muffled heart sounds are present in this patient. Even without invasive hemodynamic monitoring this condition should be noted.