PLACENTA Placenta plahsentah is a Latin word It






![• Human Placental Lactogen (h. PL [Human Chorionic Somatomammotropin]): This hormone is lactogenic • Human Placental Lactogen (h. PL [Human Chorionic Somatomammotropin]): This hormone is lactogenic](https://slidetodoc.com/presentation_image/3df3a766183083369ab0106450b62385/image-77.jpg)
- Slides: 103

PLACENTA
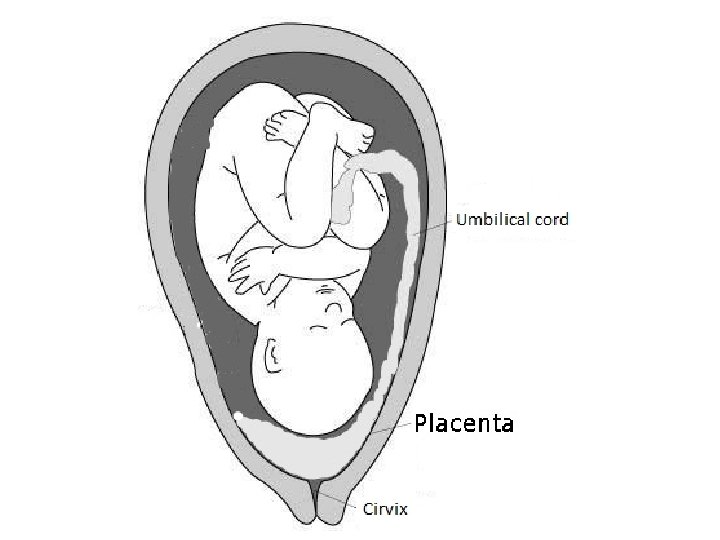
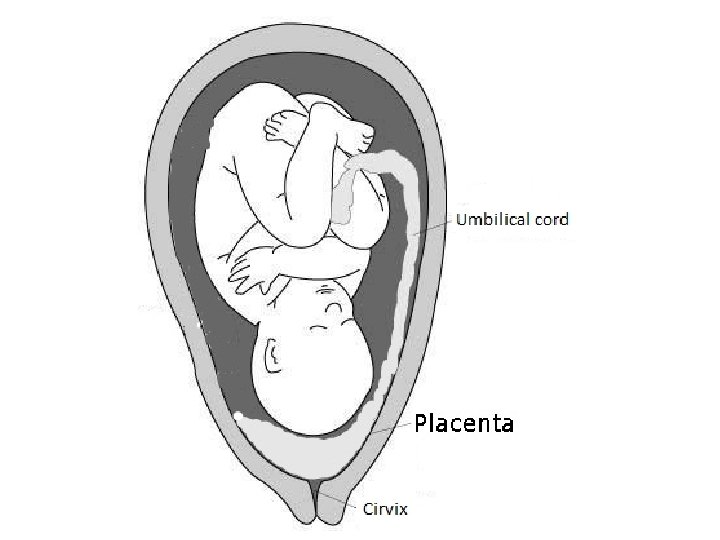
Placenta (plah-sen’tah) is a Latin word. It means “a flat cake”. • Placenta is an organ characteristic of mammals, developing during pregnancy, joining mother and offspring, providing necessary provisions for the sustenance of developing human in intrauterine life.
• The placenta is an organ that connects the developing fetus to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. • "True" placentas are a defining characteristic of eutherian or "placental" mammals,
• Eutheria (/juːˈθɪəriə/; from Ancient Greek ευθήριον, euthērion, meaning "true/good beasts") is the clade consisting of primates and all other mammals—in many orders—that are more closely related to them than they are to marsupials.
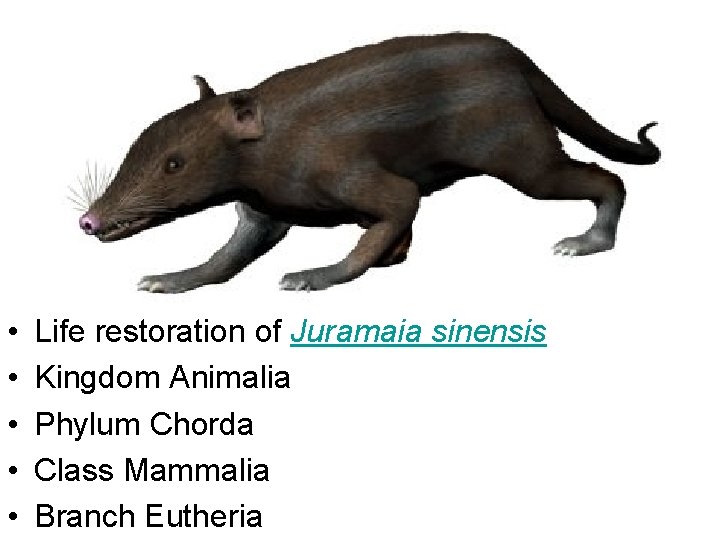
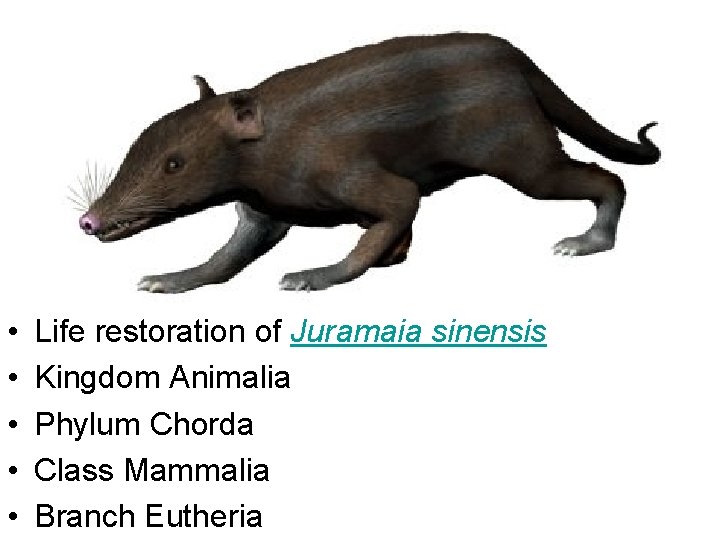
• • • Life restoration of Juramaia sinensis Kingdom Animalia Phylum Chorda Class Mammalia Branch Eutheria
• Marsupials are an infraclass of mammals living primarily in the Southern Hemisphere; a distinctive characteristic, common to most species, is that the young are carried in a pouch.
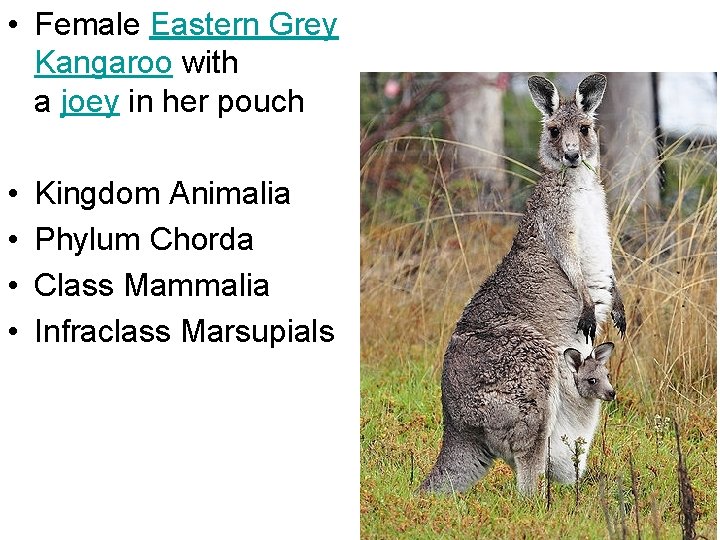
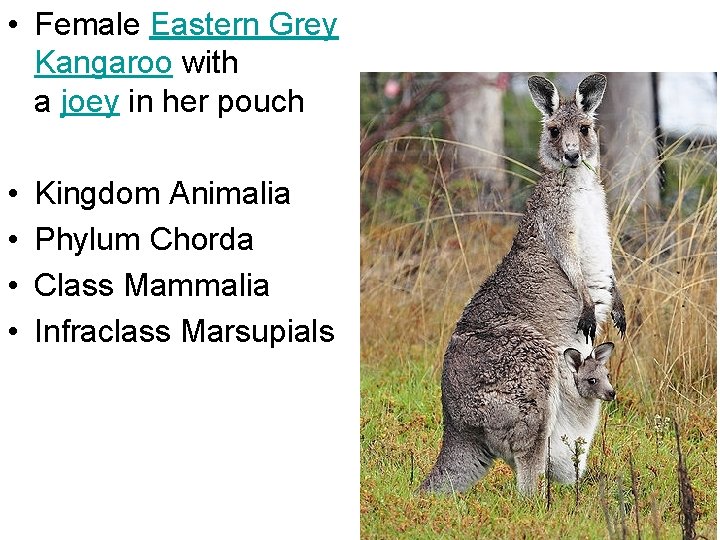
• Female Eastern Grey Kangaroo with a joey in her pouch • • Kingdom Animalia Phylum Chorda Class Mammalia Infraclass Marsupials
• A clade (from Ancient Greek κλάδος, klados, "branch") or monophylum (see monophyletic) is a group consisting of an ancestor and all its descendants, a single "branch" on the "tree of life"
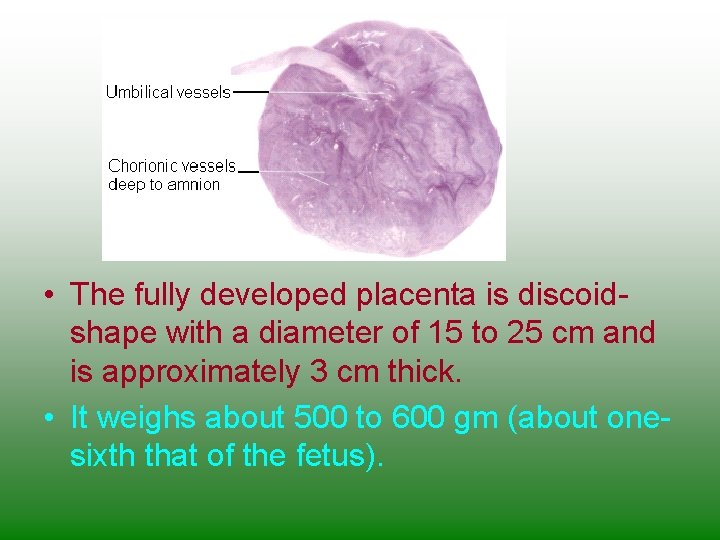
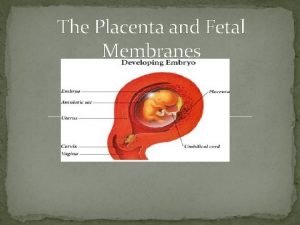
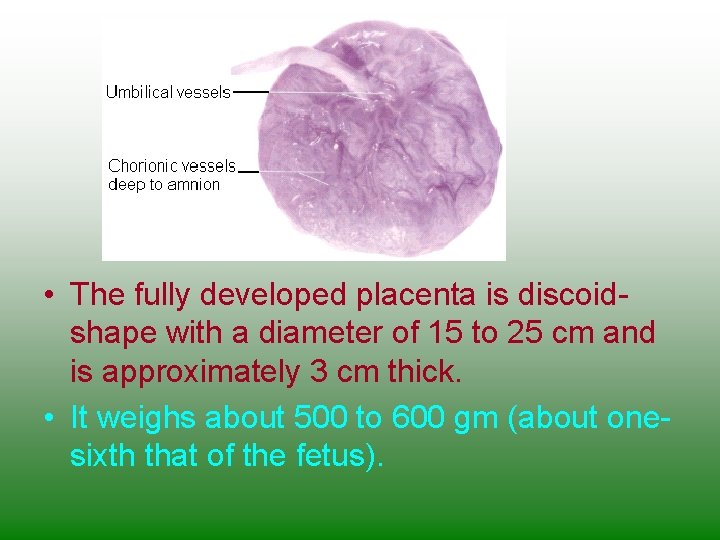
• The fully developed placenta is discoidshape with a diameter of 15 to 25 cm and is approximately 3 cm thick. • It weighs about 500 to 600 gm (about onesixth that of the fetus).
• In humans, the placenta averages 22 cm (9 inch) in length and 2– 2. 5 cm (0. 8– 1 inch) in thickness, with the center being the thickest, and the edges being the thinnest. • It typically weighs approximately 500 grams (1 lb).
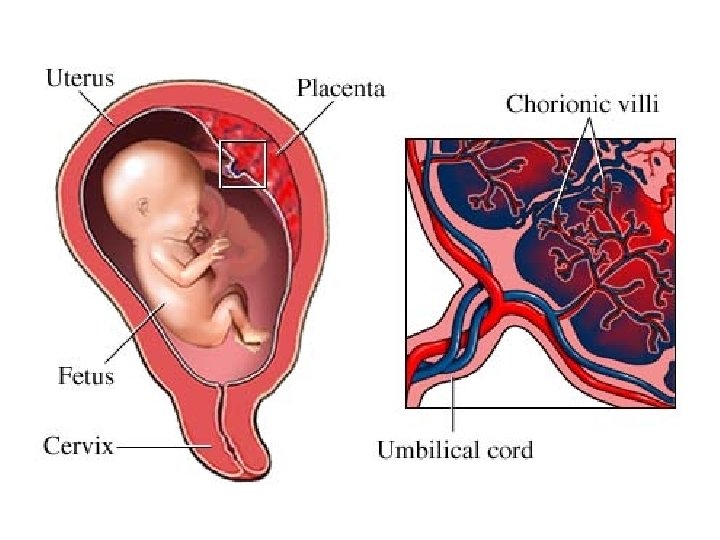
• It has a dark reddish-blue or crimson color. • It connects to the fetus by an umbilical cord of approximately 55– 60 cm (22– 24 inch) in length, which contains two umbilical arteries and one umbilical vein
• The umbilical cord inserts into the chorionic plate (has an eccentric attachment). • Vessels branch out over the surface of the placenta and further divide to form a network covered by a thin layer of cells. This results in the formation of villous tree structures.
• On the maternal side, these villous tree structures are grouped into lobules called cotyledons. • In humans, the placenta usually has a disc shape, but size varies vastly between different mammalian species


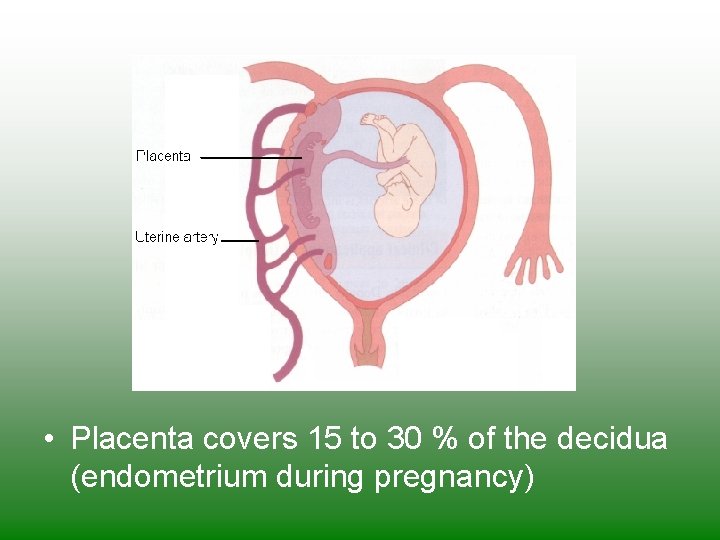
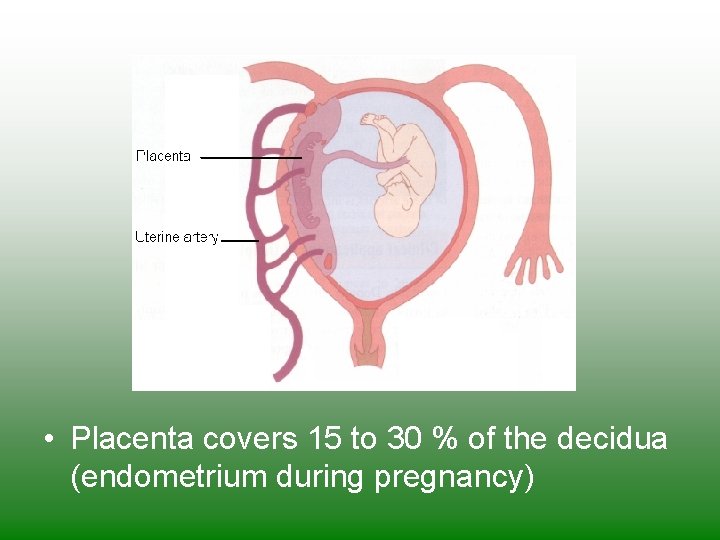
• Placenta covers 15 to 30 % of the decidua (endometrium during pregnancy)
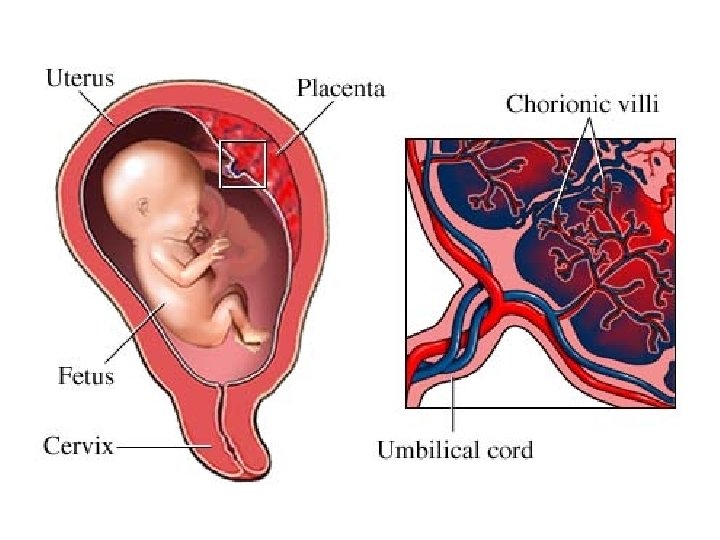
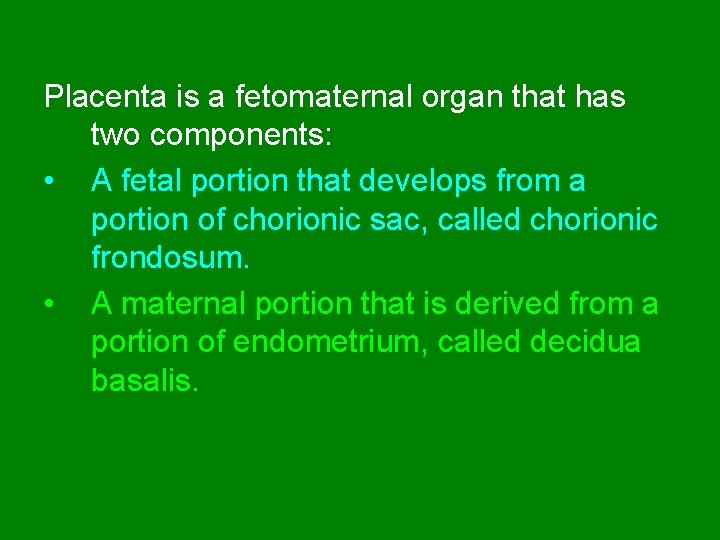
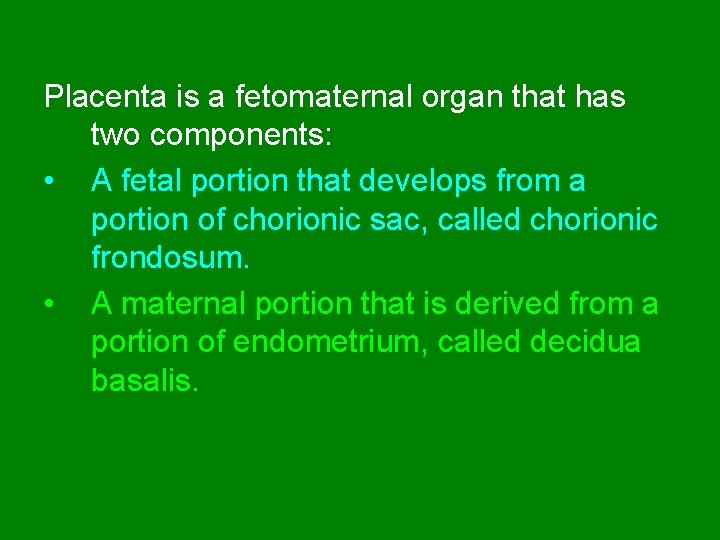
Placenta is a fetomaternal organ that has two components: • A fetal portion that develops from a portion of chorionic sac, called chorionic frondosum. • A maternal portion that is derived from a portion of endometrium, called decidua basalis.

DEVELOPMENT OF PLACENTA
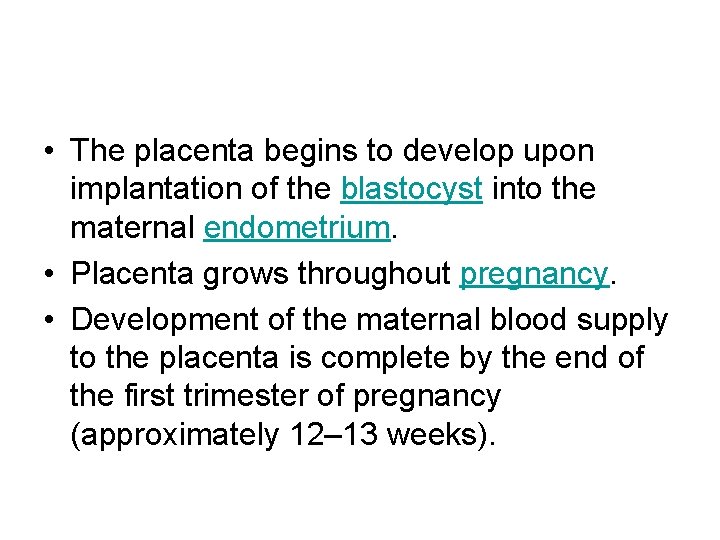
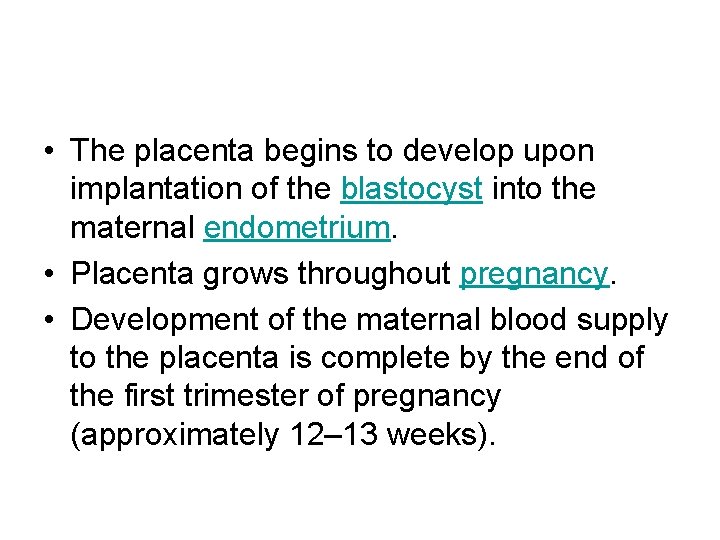
• The placenta begins to develop upon implantation of the blastocyst into the maternal endometrium. • Placenta grows throughout pregnancy. • Development of the maternal blood supply to the placenta is complete by the end of the first trimester of pregnancy (approximately 12– 13 weeks).
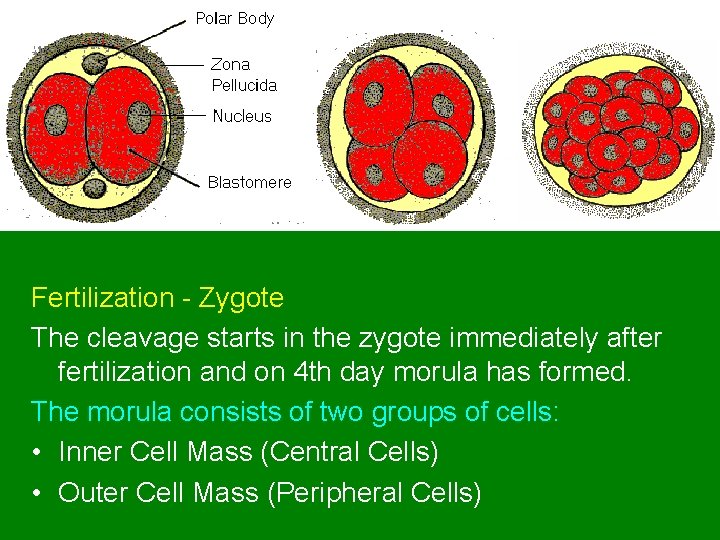
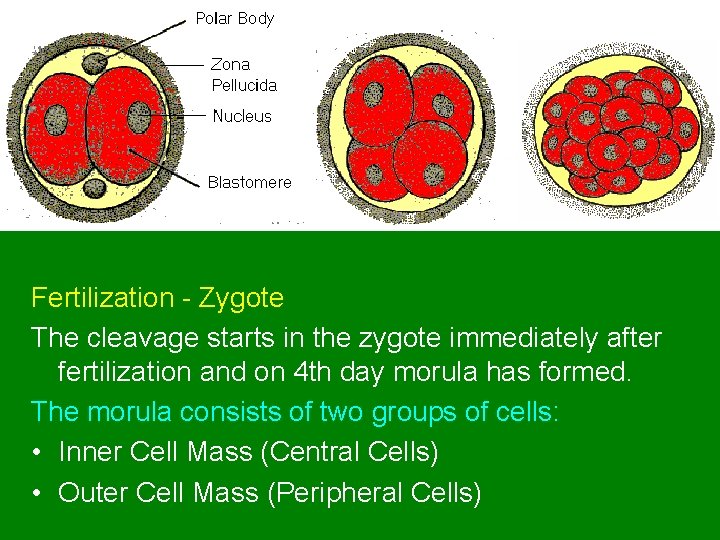
Fertilization - Zygote The cleavage starts in the zygote immediately after fertilization and on 4 th day morula has formed. The morula consists of two groups of cells: • Inner Cell Mass (Central Cells) • Outer Cell Mass (Peripheral Cells)
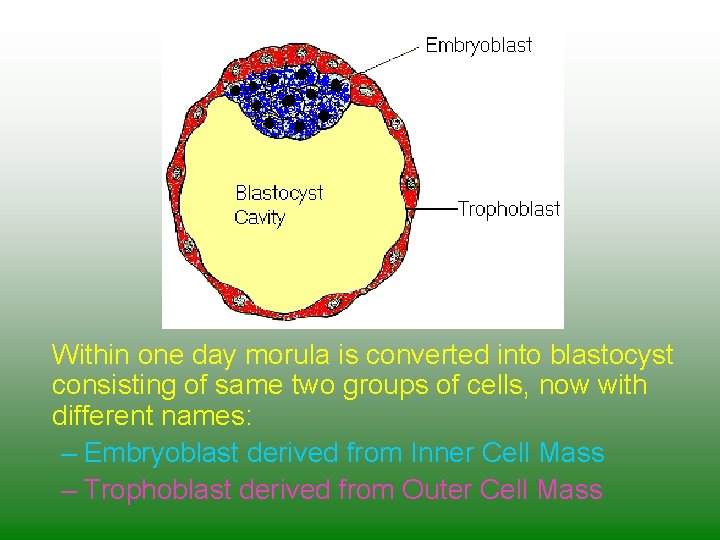
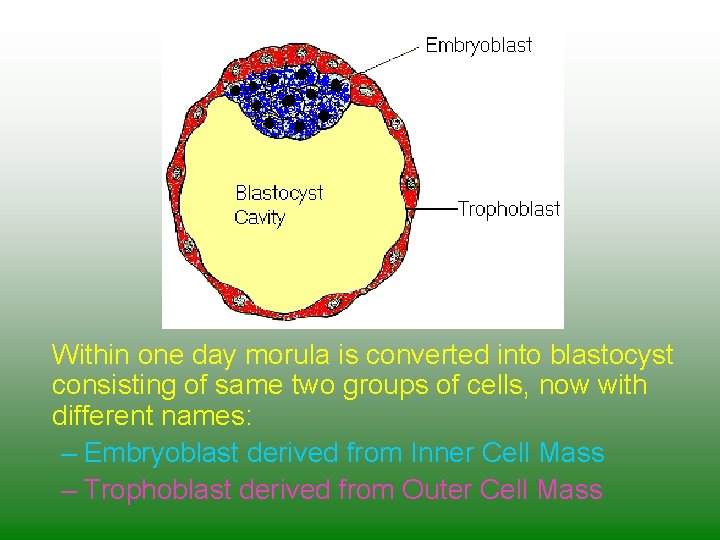
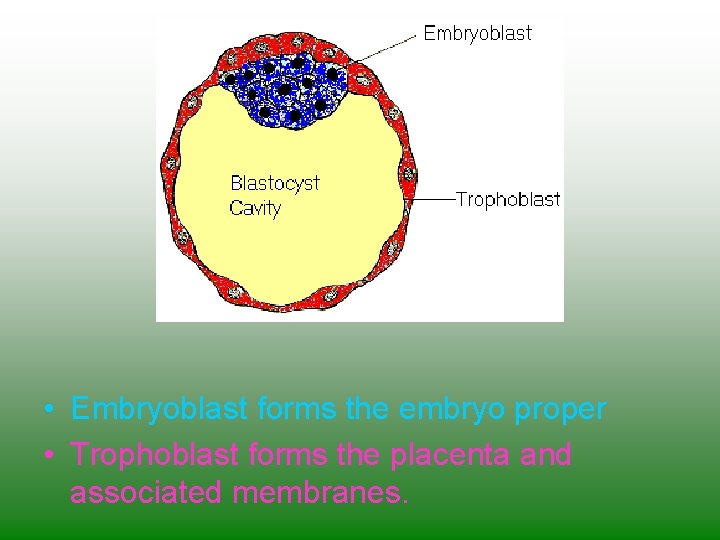
Within one day morula is converted into blastocyst consisting of same two groups of cells, now with different names: – Embryoblast derived from Inner Cell Mass – Trophoblast derived from Outer Cell Mass
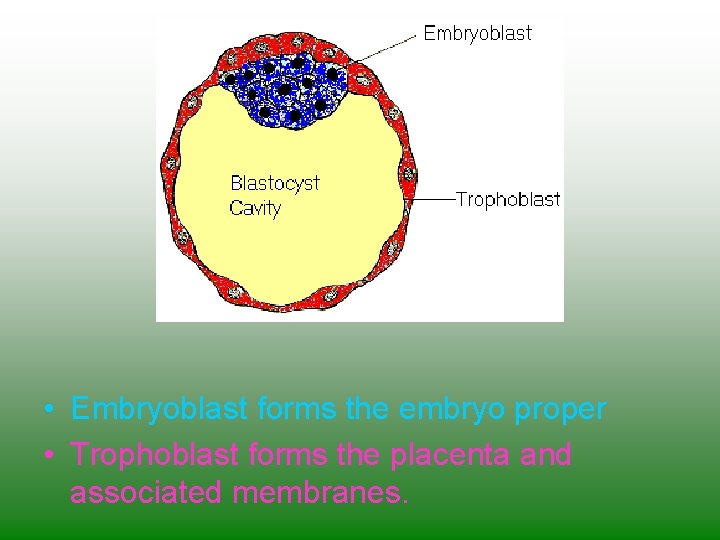
• Embryoblast forms the embryo proper • Trophoblast forms the placenta and associated membranes.
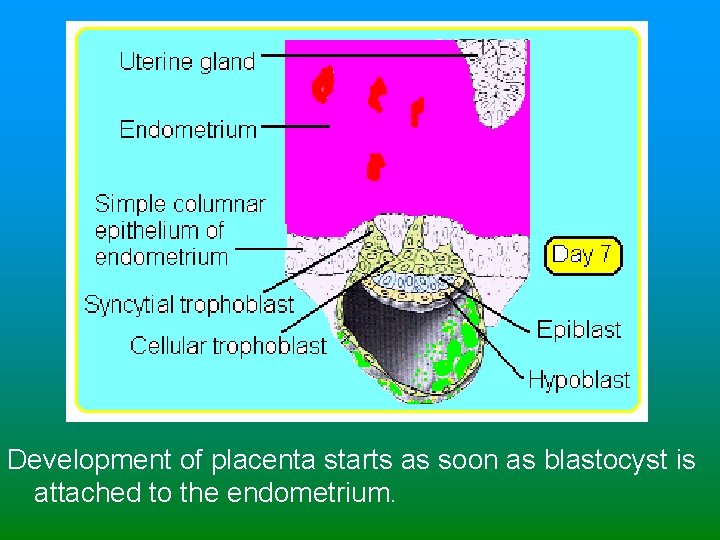
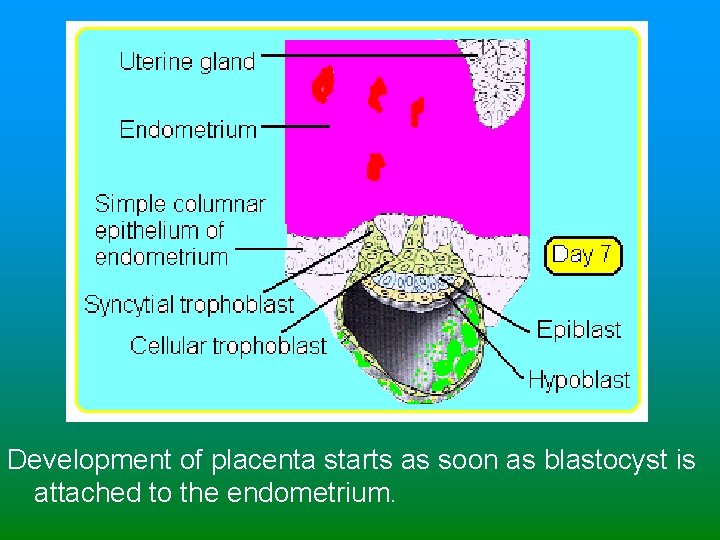
Development of placenta starts as soon as blastocyst is attached to the endometrium.
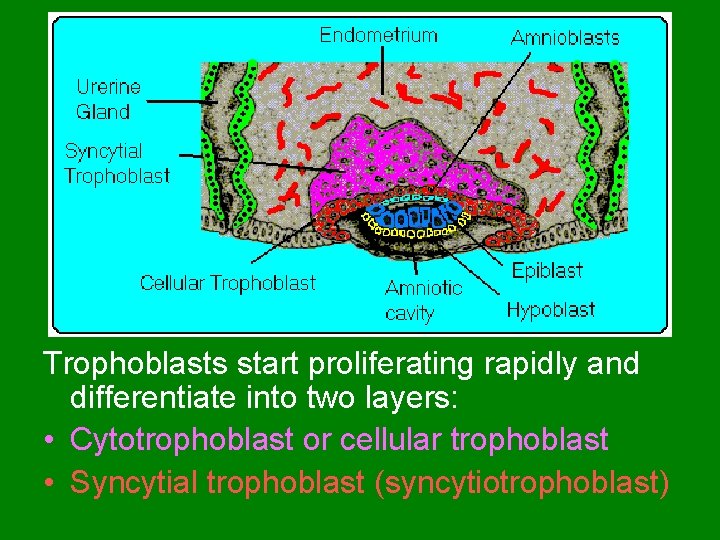
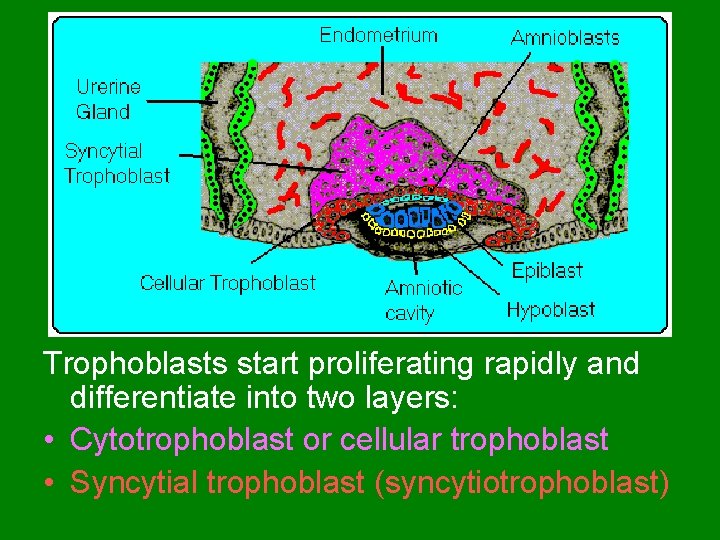
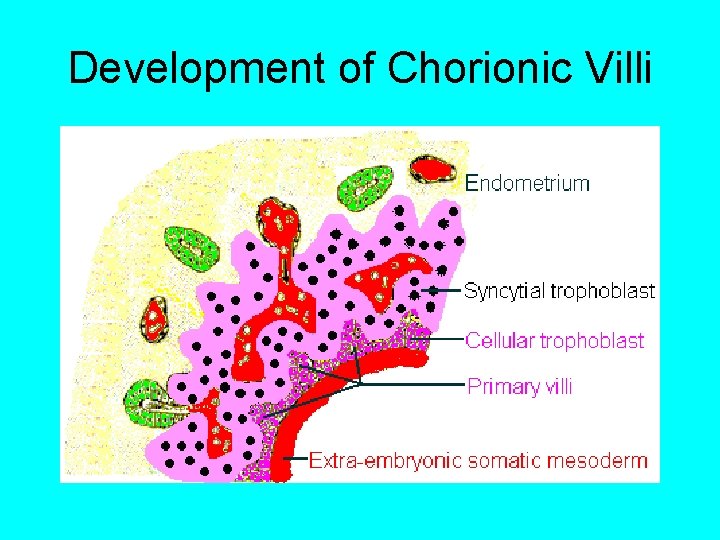
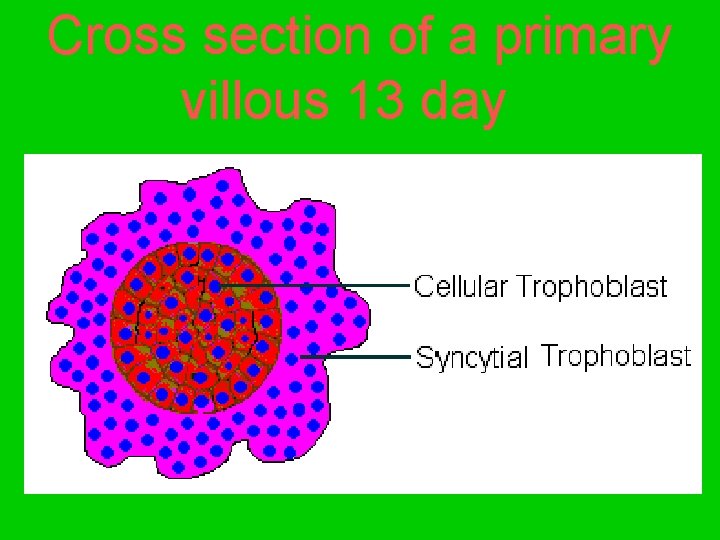
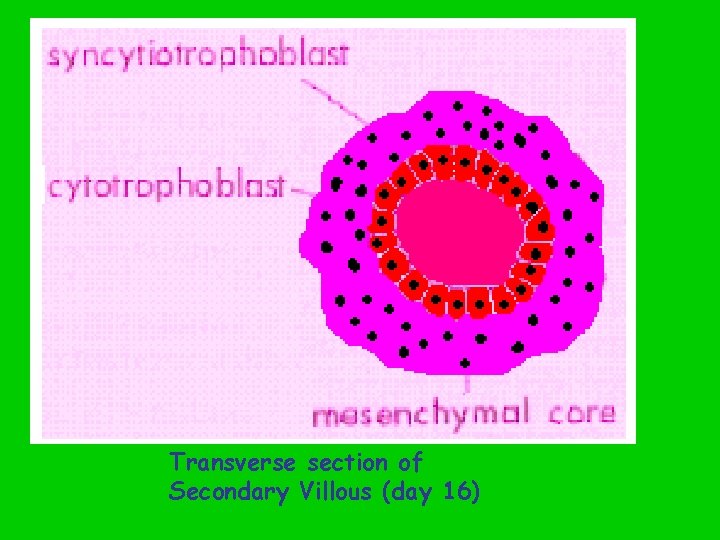
Trophoblasts start proliferating rapidly and differentiate into two layers: • Cytotrophoblast or cellular trophoblast • Syncytial trophoblast (syncytiotrophoblast)
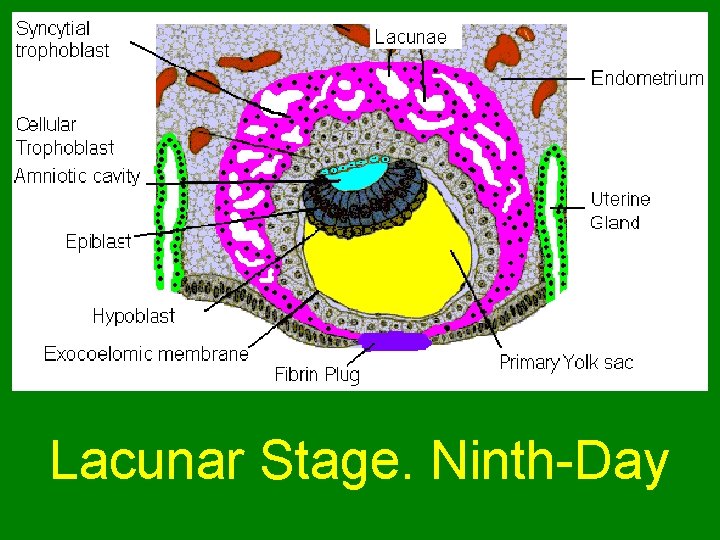
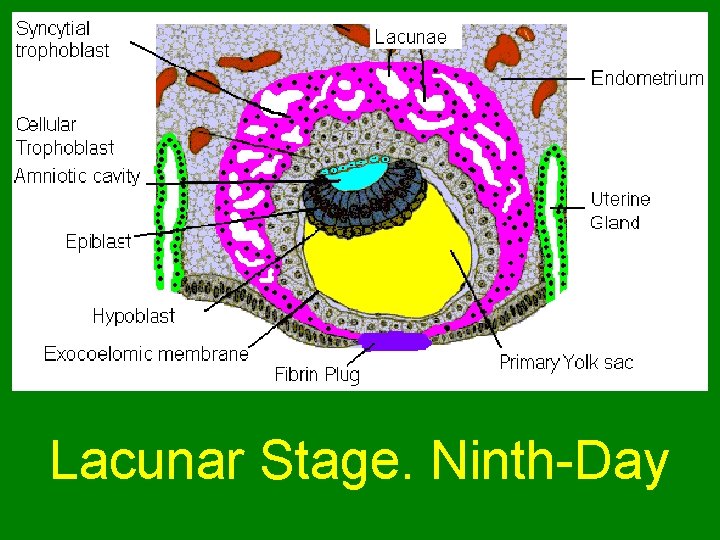
Lacunar Stage. Ninth-Day
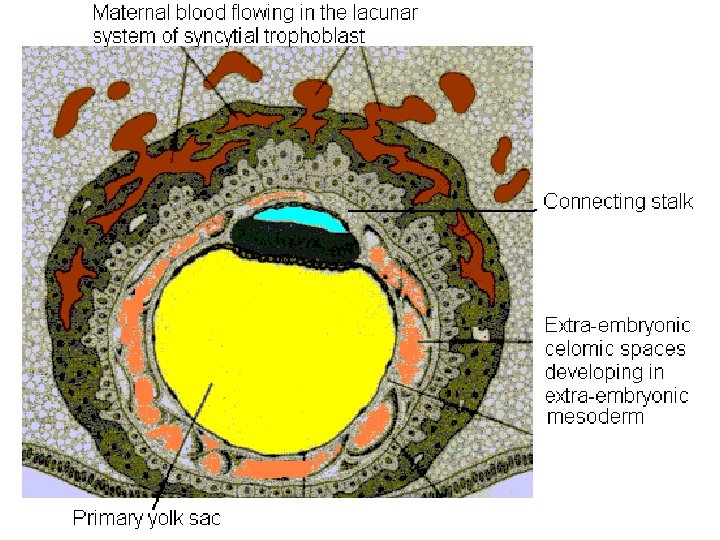
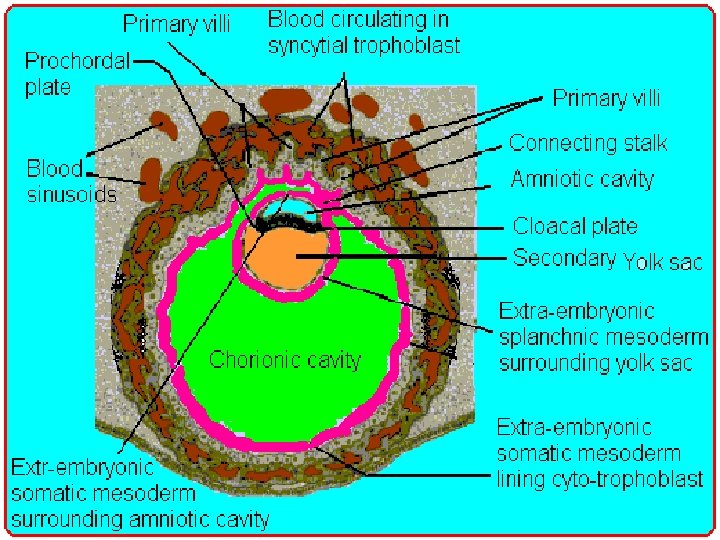
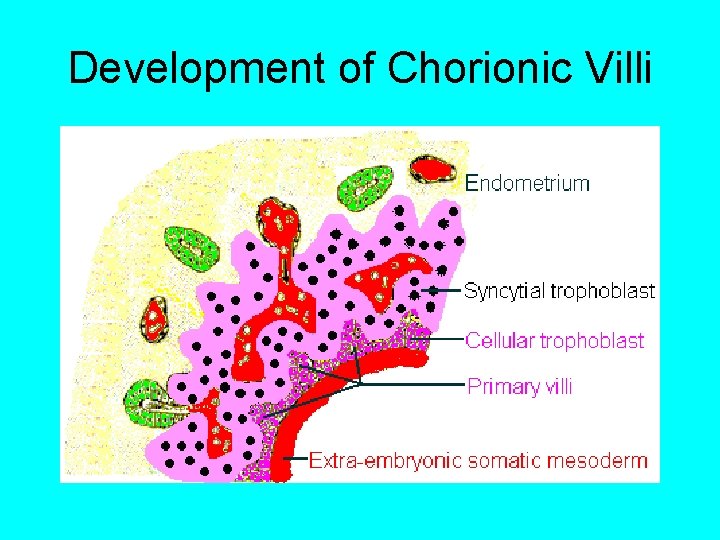
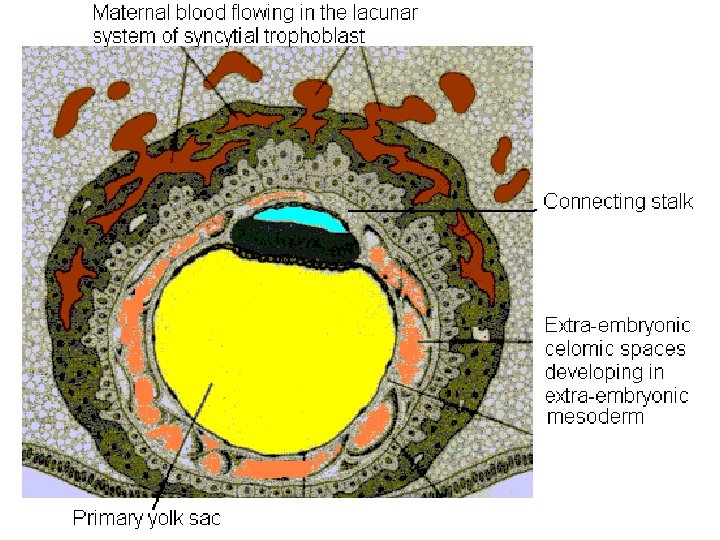
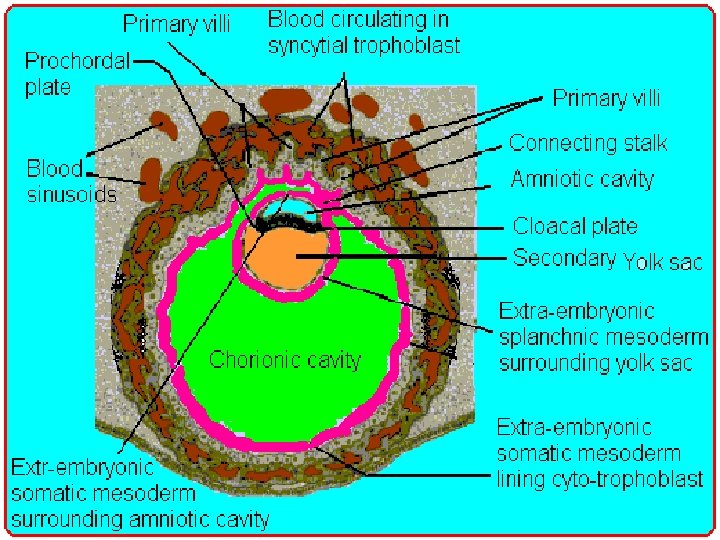
Development of Chorionic Villi
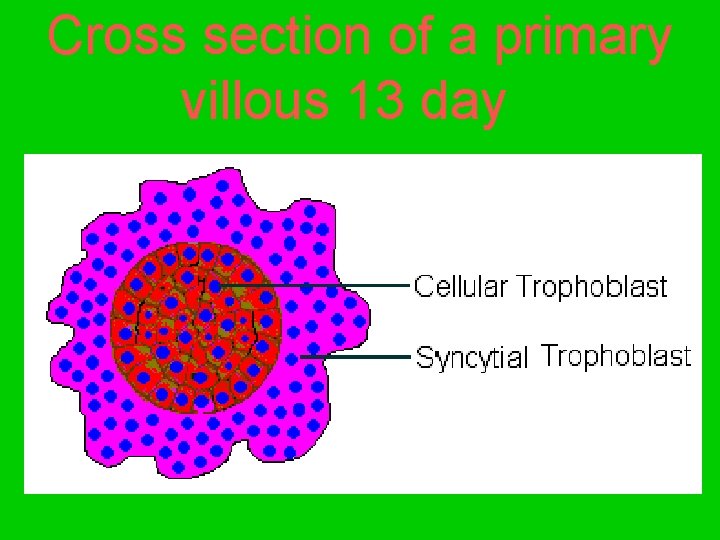
Cross section of a primary villous 13 day
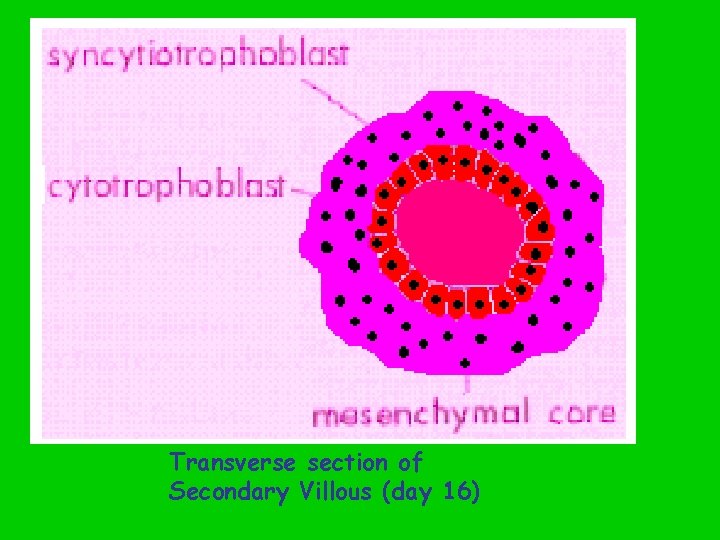
Transverse section of Secondary Villous (day 16)
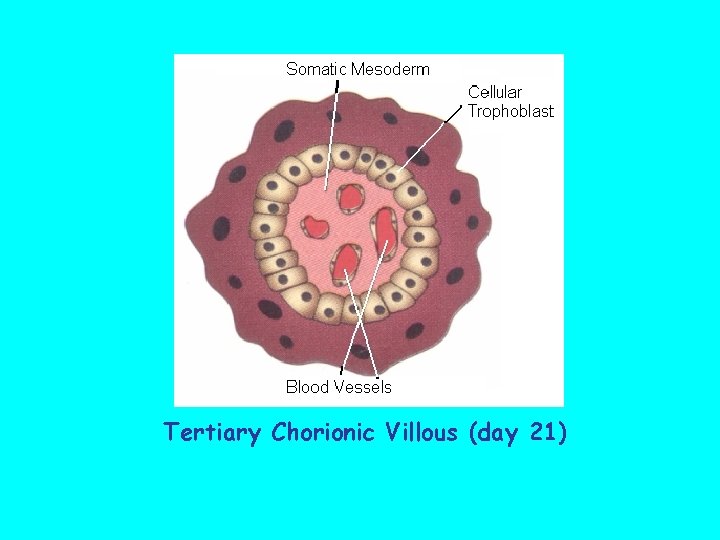
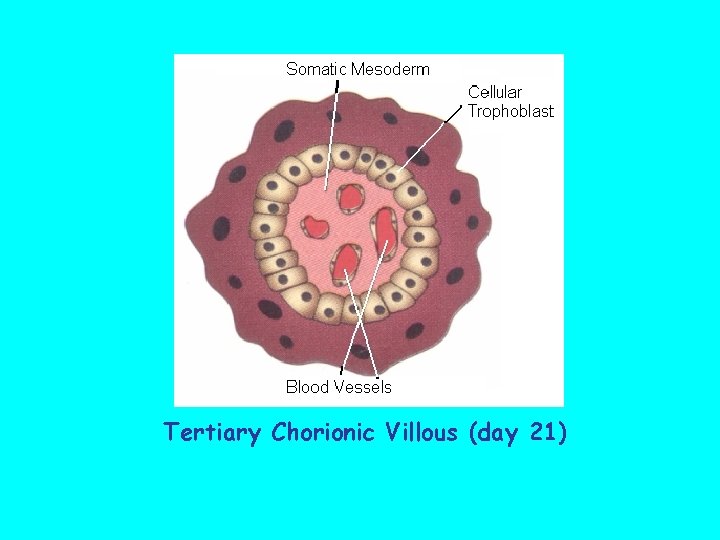
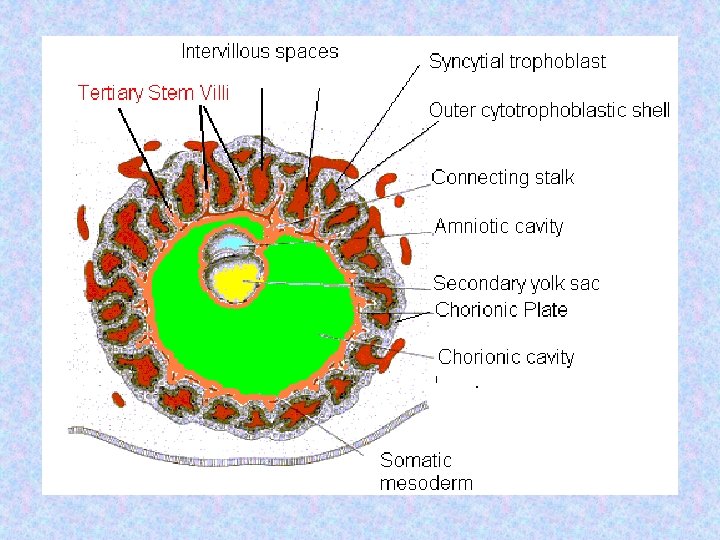
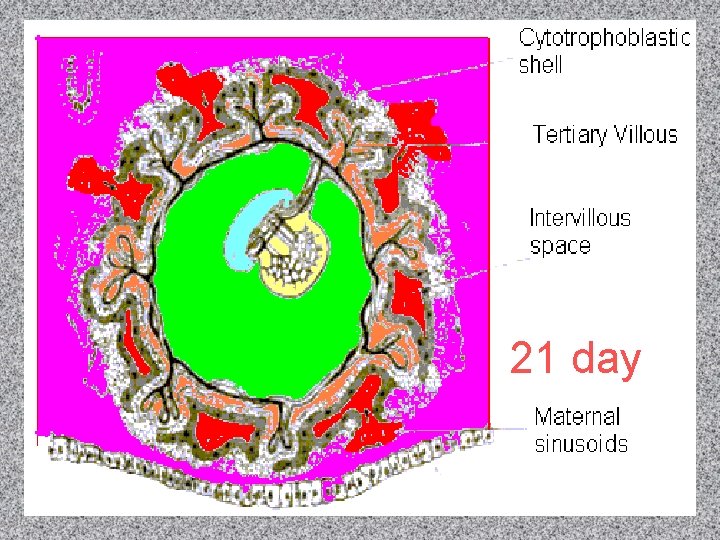
Tertiary Chorionic Villous (day 21)
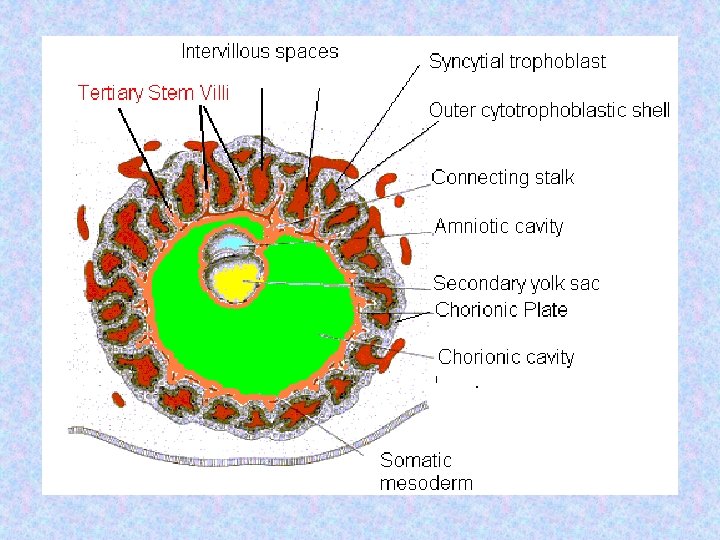
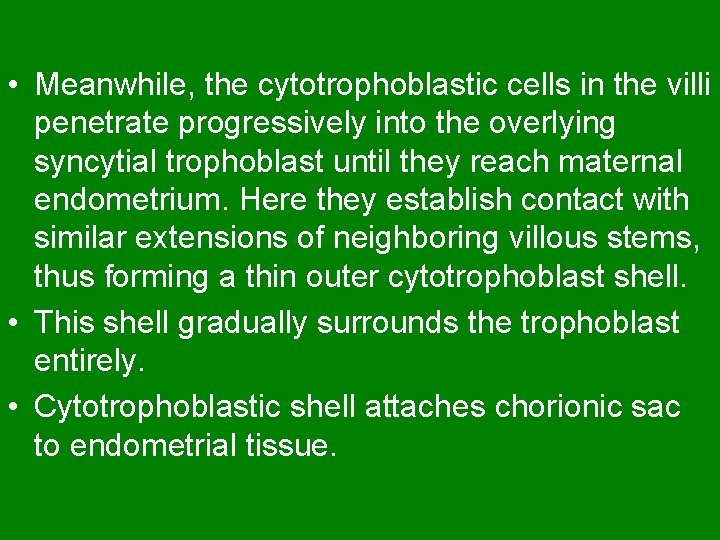
• Meanwhile, the cytotrophoblastic cells in the villi penetrate progressively into the overlying syncytial trophoblast until they reach maternal endometrium. Here they establish contact with similar extensions of neighboring villous stems, thus forming a thin outer cytotrophoblast shell. • This shell gradually surrounds the trophoblast entirely. • Cytotrophoblastic shell attaches chorionic sac to endometrial tissue.
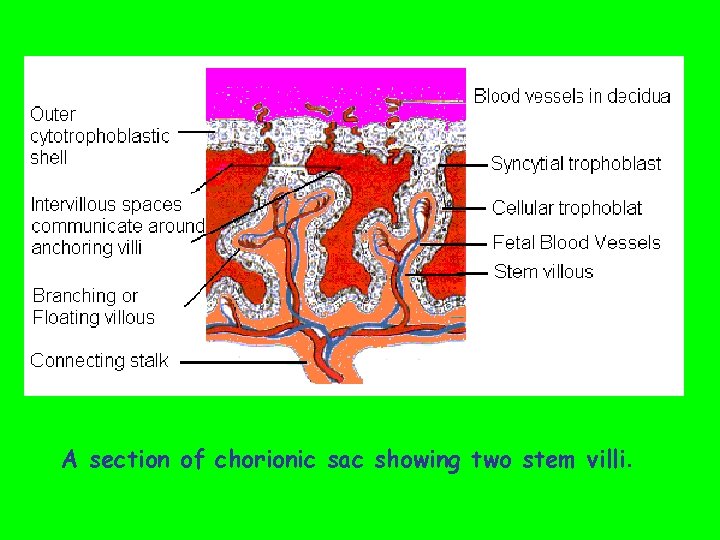
• Stem Villi that are attached to the maternal tissues via cytotrophoblastic shell are called stem villi or anchoring villi. • Floating Villi The villi that branch from stem villi and float free in intervillous space are called branching villi or floating villi. These villi are not attached to maternal tissue.
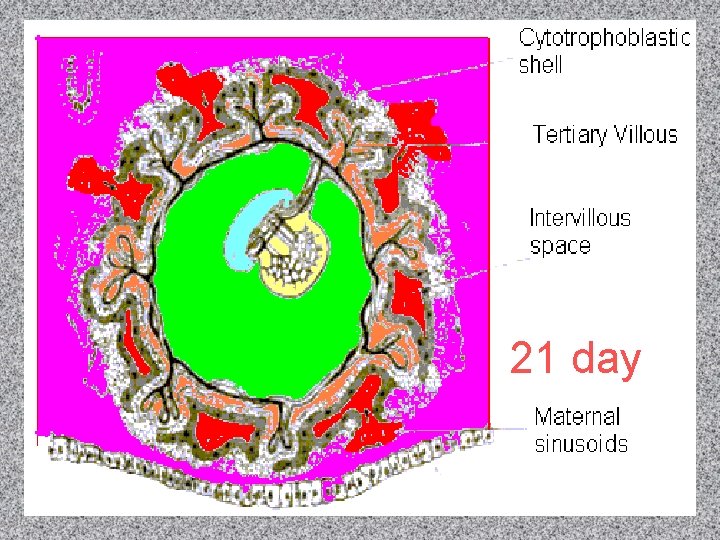
21 day
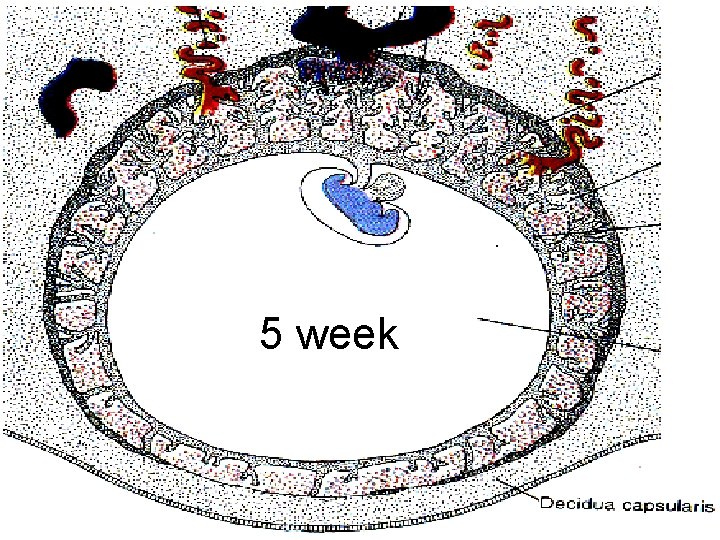
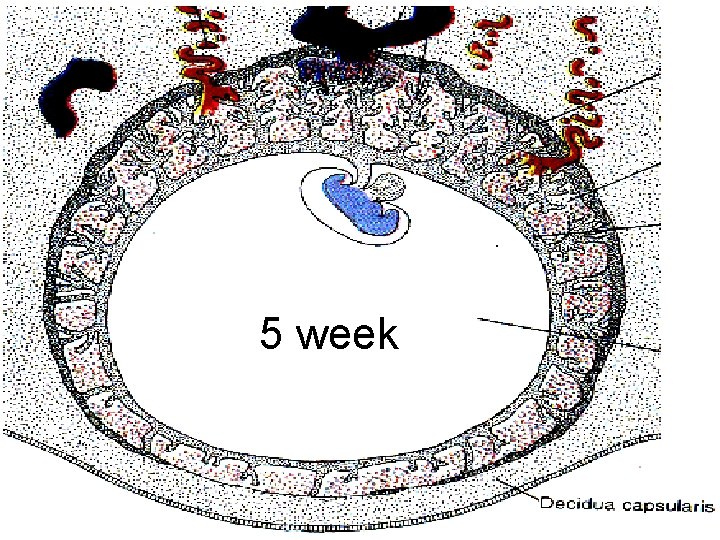
5 week
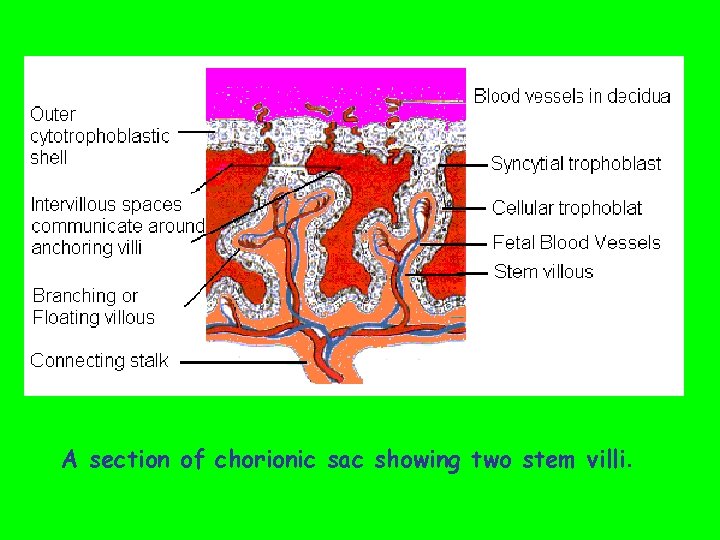
A section of chorionic sac showing two stem villi.
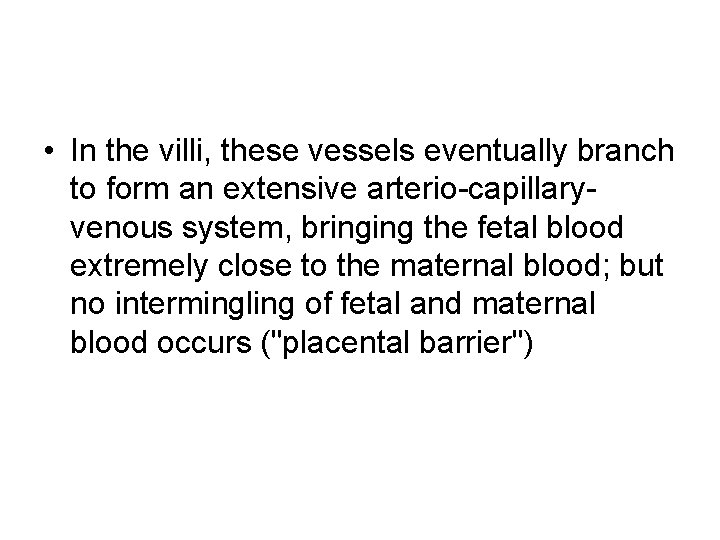
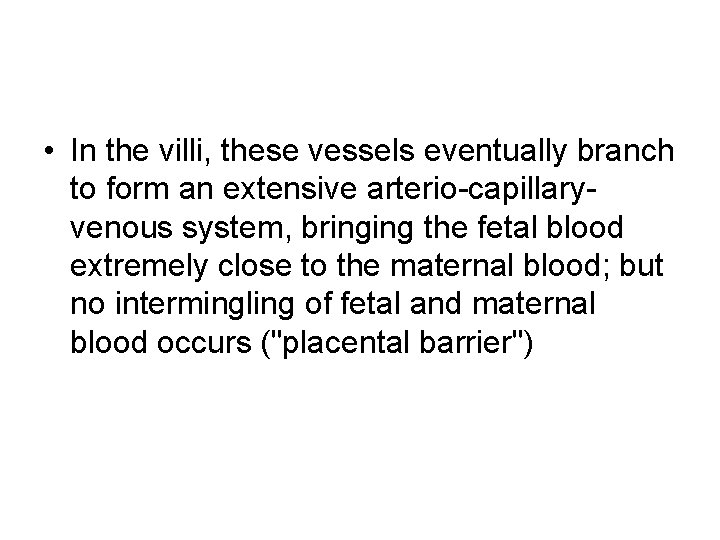
• In the villi, these vessels eventually branch to form an extensive arterio-capillaryvenous system, bringing the fetal blood extremely close to the maternal blood; but no intermingling of fetal and maternal blood occurs ("placental barrier")
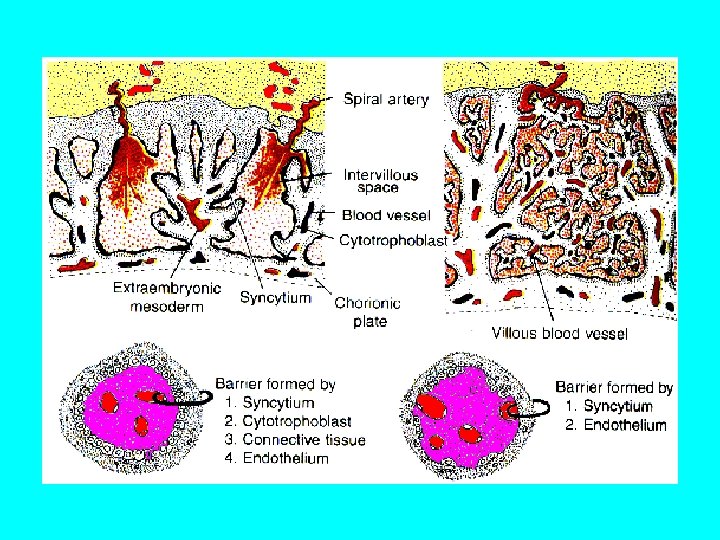
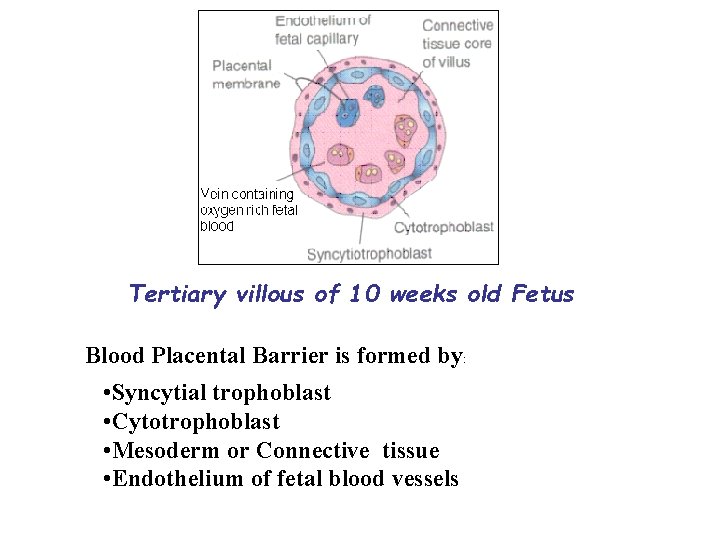
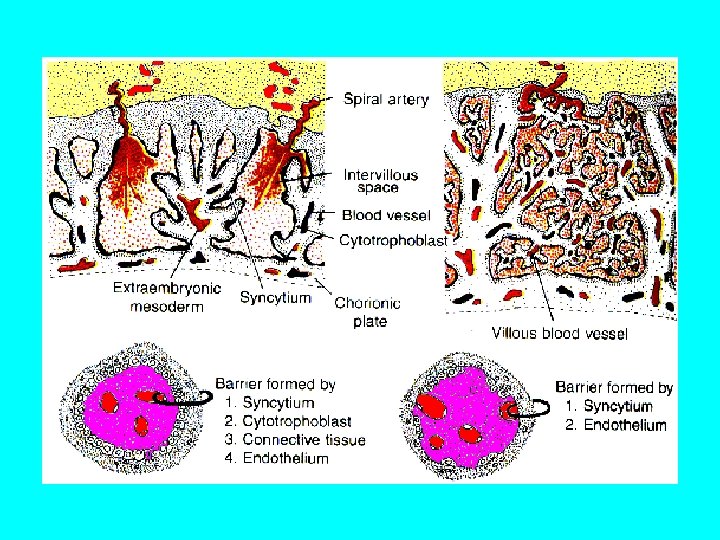
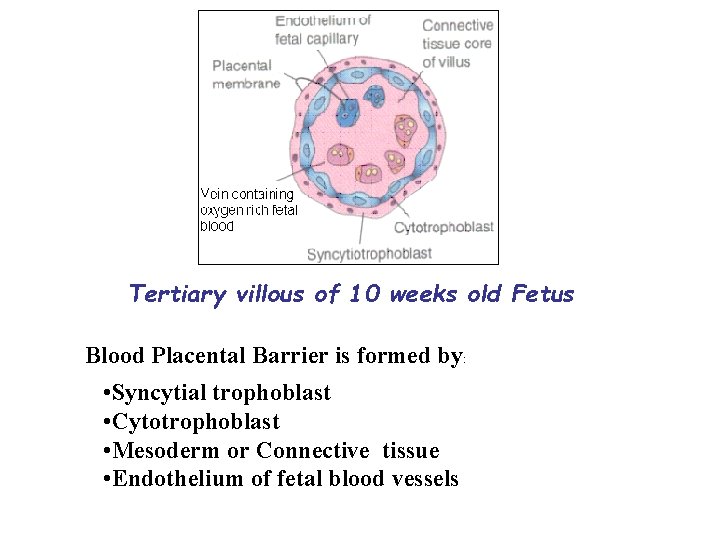
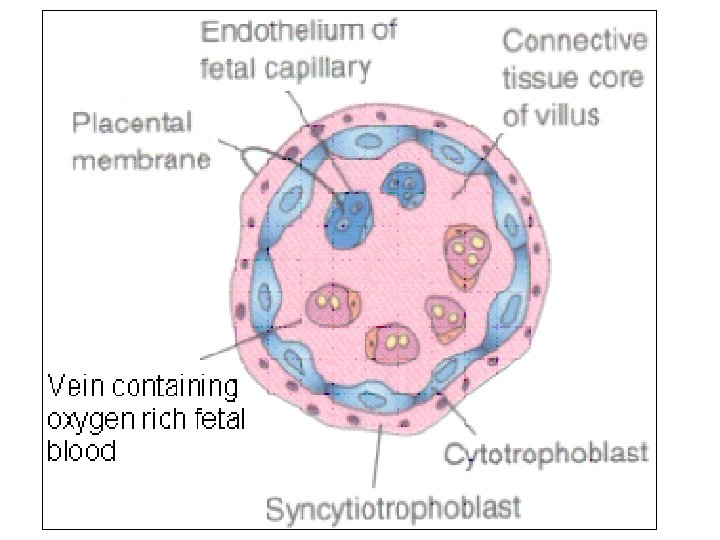
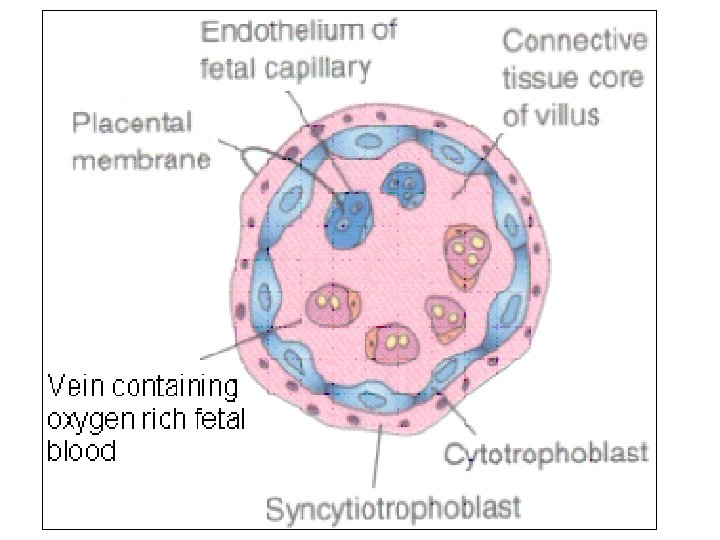
Tertiary villous of 10 weeks old Fetus Blood Placental Barrier is formed by: • Syncytial trophoblast • Cytotrophoblast • Mesoderm or Connective tissue • Endothelium of fetal blood vessels
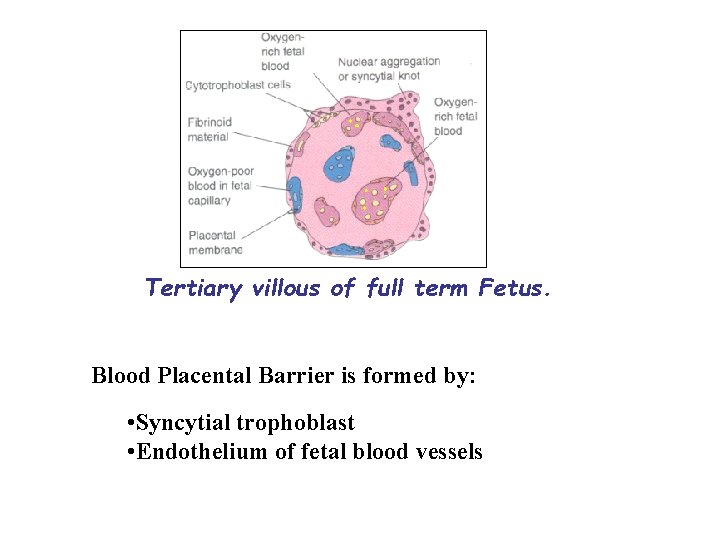
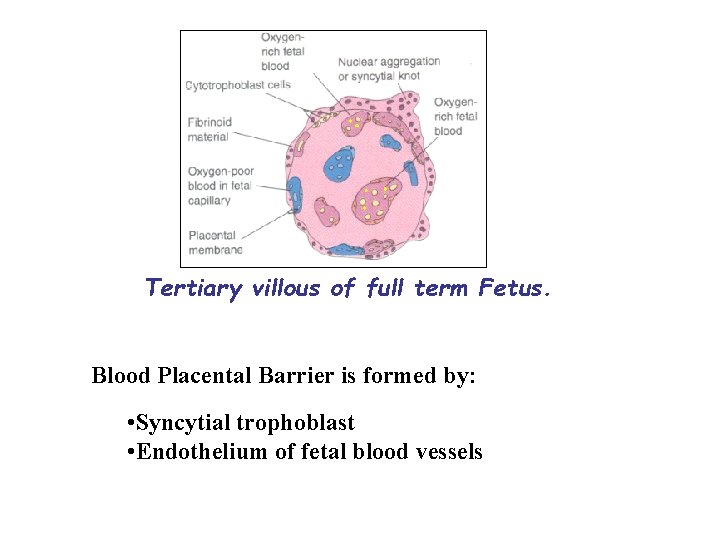
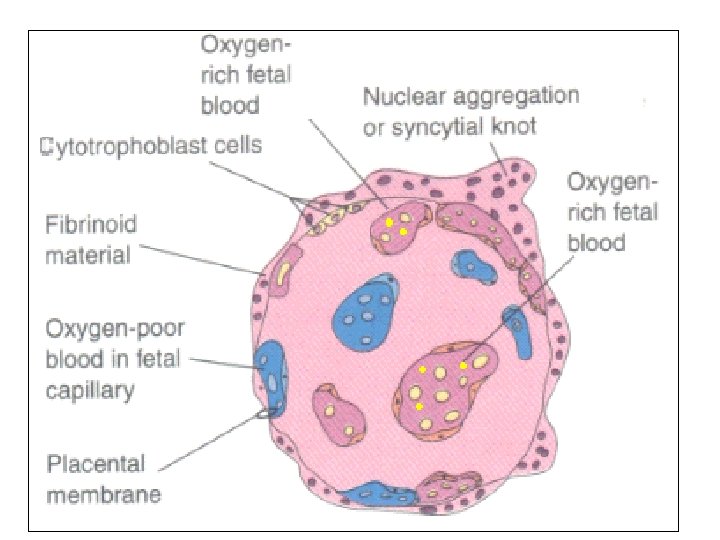
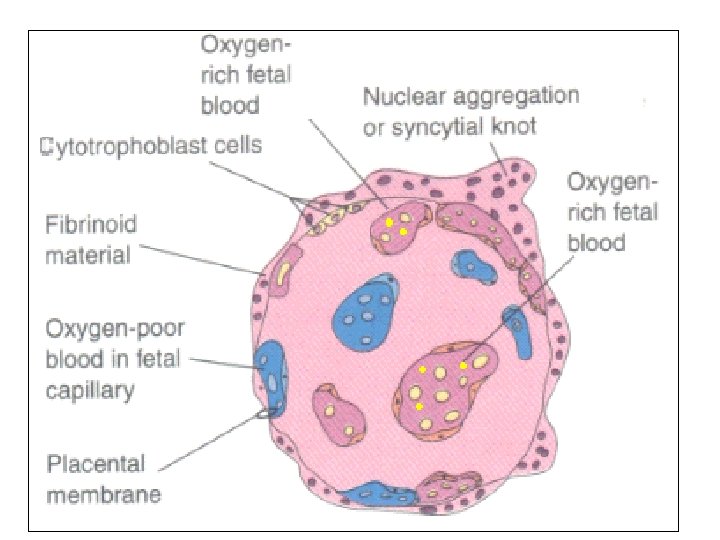
Tertiary villous of full term Fetus. Blood Placental Barrier is formed by: • Syncytial trophoblast • Endothelium of fetal blood vessels
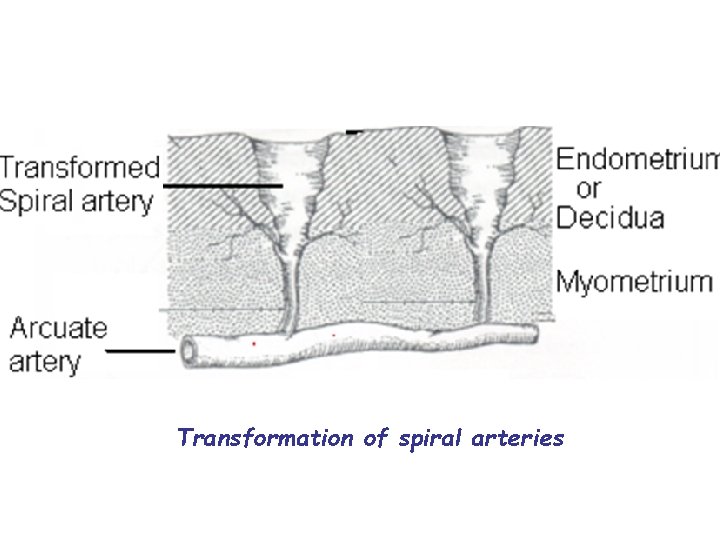
• In preparation for implantation, the uterine endometrium undergoes "decidualisation". • Spiral arteries in decidua are remodeled so that they become less convoluted and their diameter is increased.
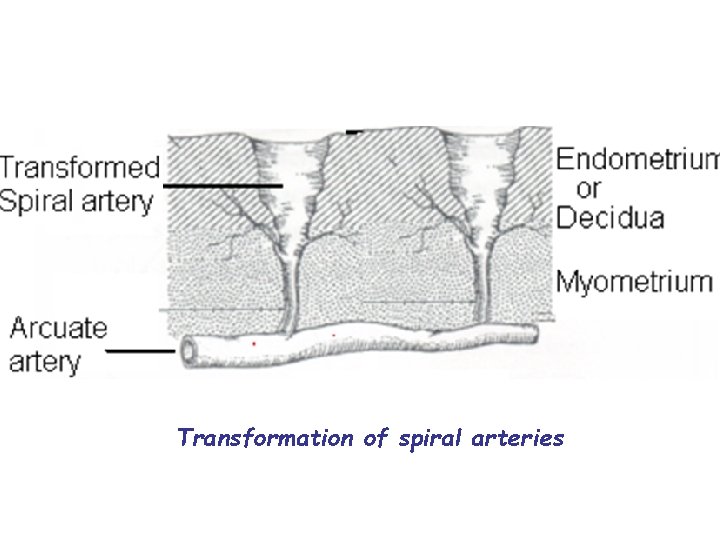
Transformation of spiral arteries
• The increased diameter and straighter flow path both act to increase maternal blood flow to the placenta. • The relatively high pressure as the maternal blood fills intervillous space through these spiral arteries bathes the fetal villi in blood, allowing an exchange of gases to take place.

• In humans and other hemochorial placentals, the maternal blood comes into direct contact with the fetal chorion, though no fluid is exchanged. • As the pressure decreases between pulses, the deoxygenated blood flows back through the endometrial veins. • Maternal blood flow is approximately 600– 700 ml/min at term.
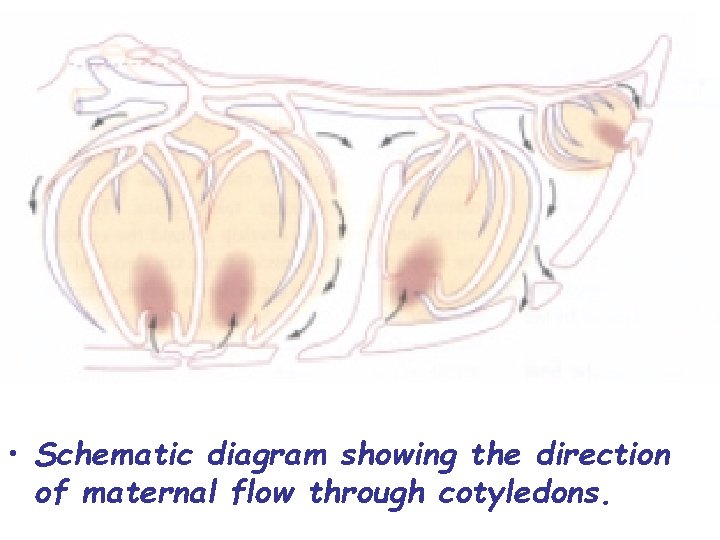
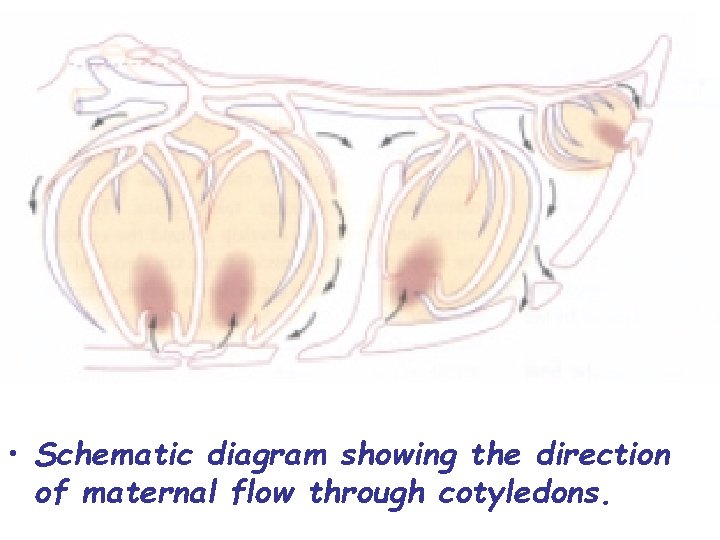
• Schematic diagram showing the direction of maternal flow through cotyledons.
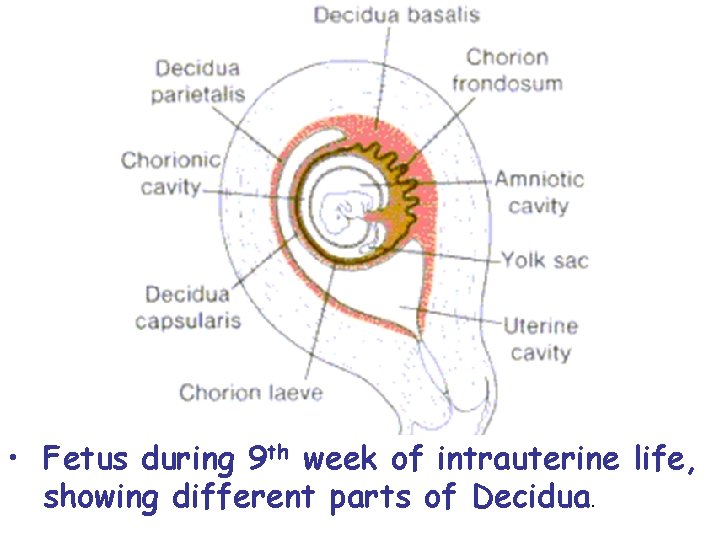
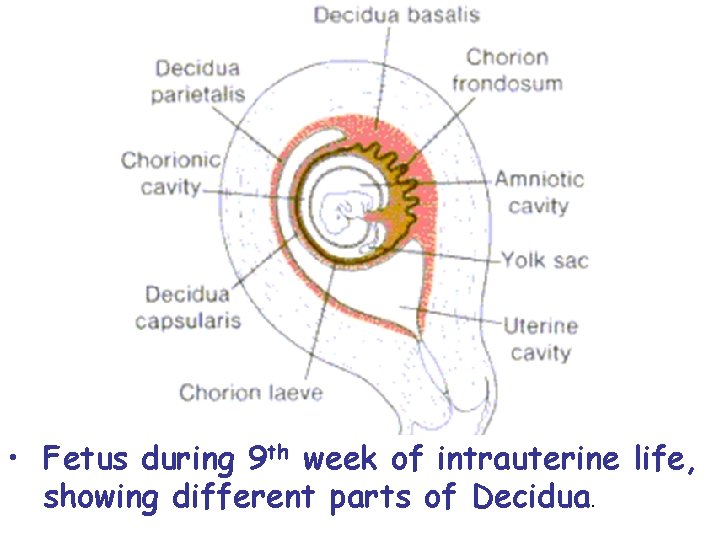
• Fetus during 9 th week of intrauterine life, showing different parts of Decidua.
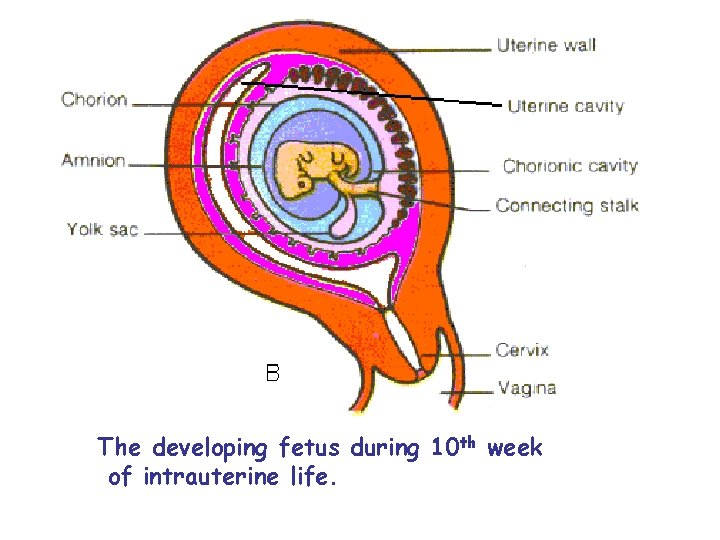
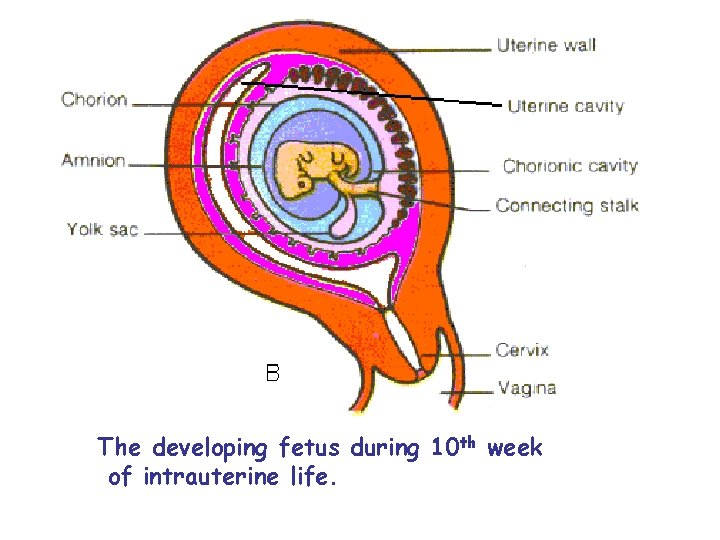
The developing fetus during 10 th week of intrauterine life.
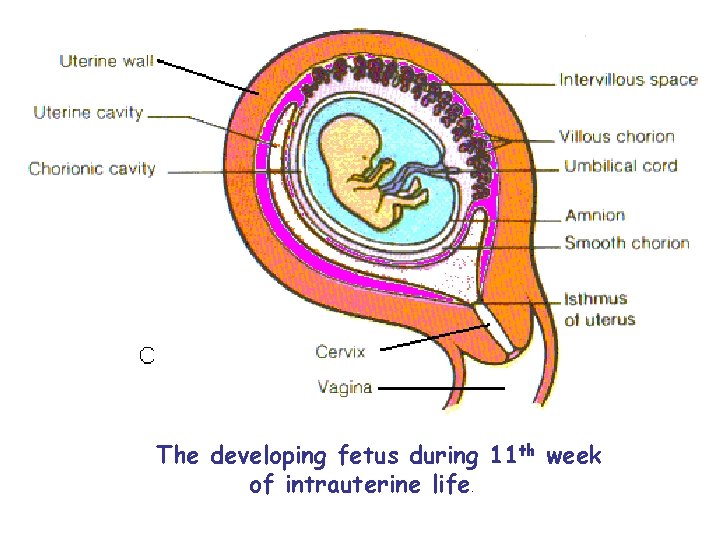
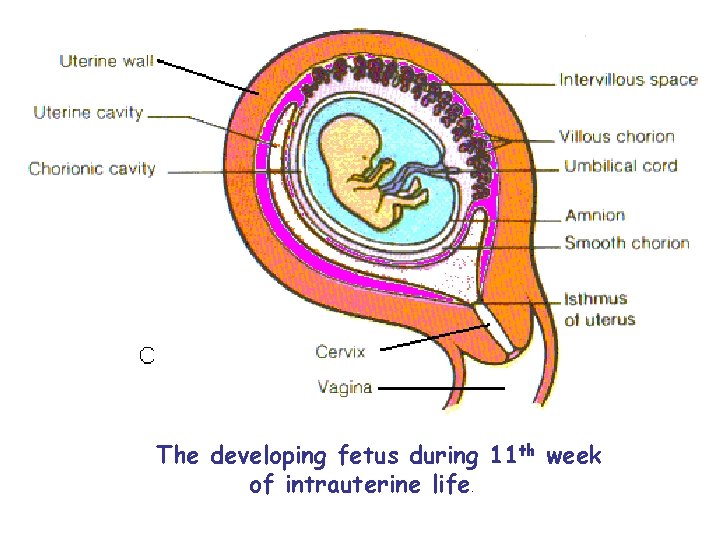
The developing fetus during 11 th week of intrauterine life.
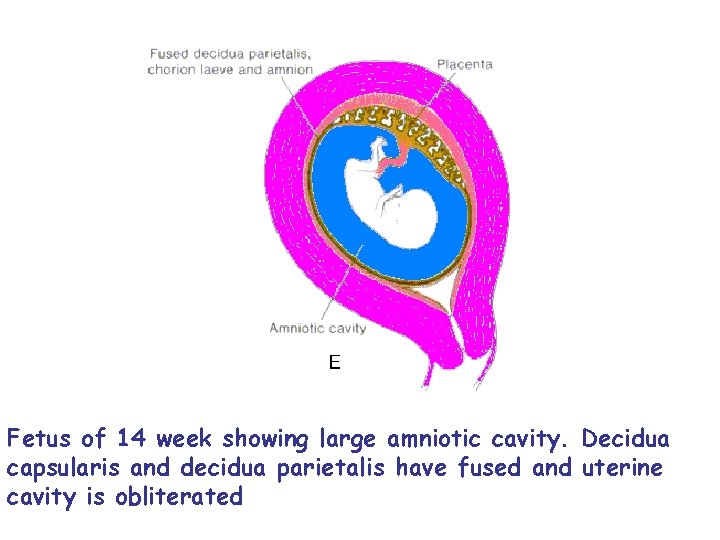
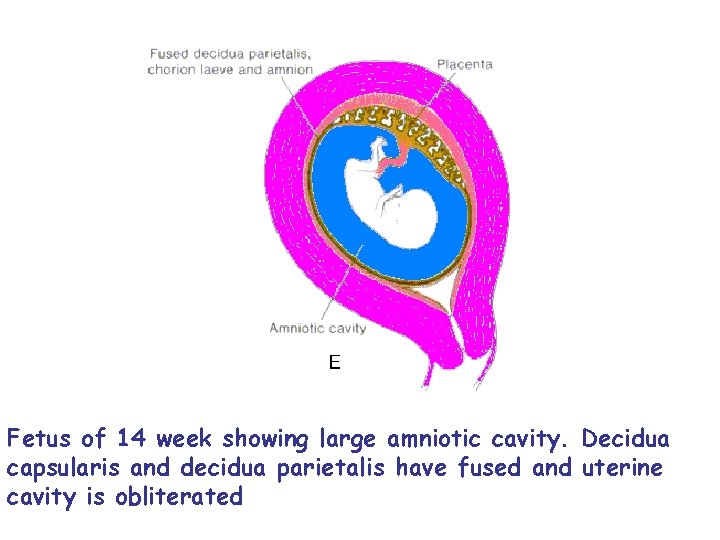
Fetus of 14 week showing large amniotic cavity. Decidua capsularis and decidua parietalis have fused and uterine cavity is obliterated
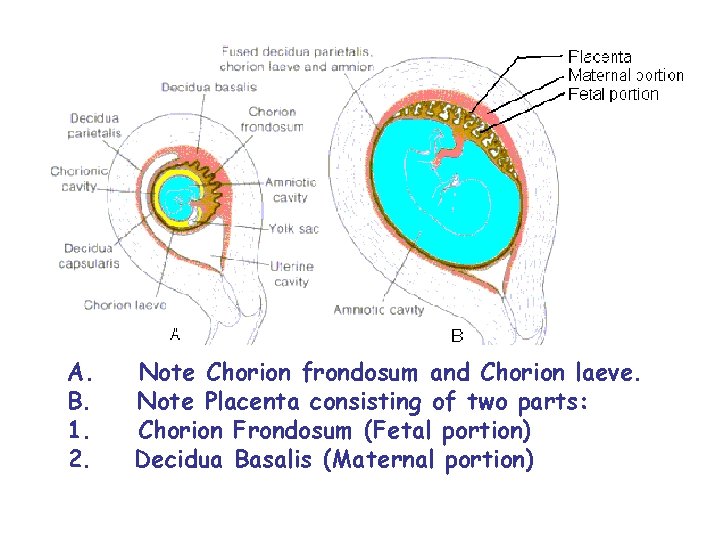
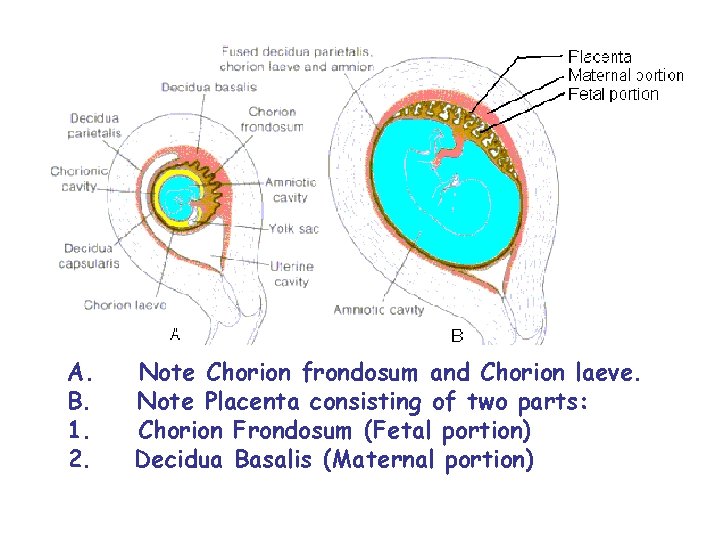
A. Note Chorion frondosum and Chorion laeve. B. Note Placenta consisting of two parts: 1. Chorion Frondosum (Fetal portion) 2. Decidua Basalis (Maternal portion)
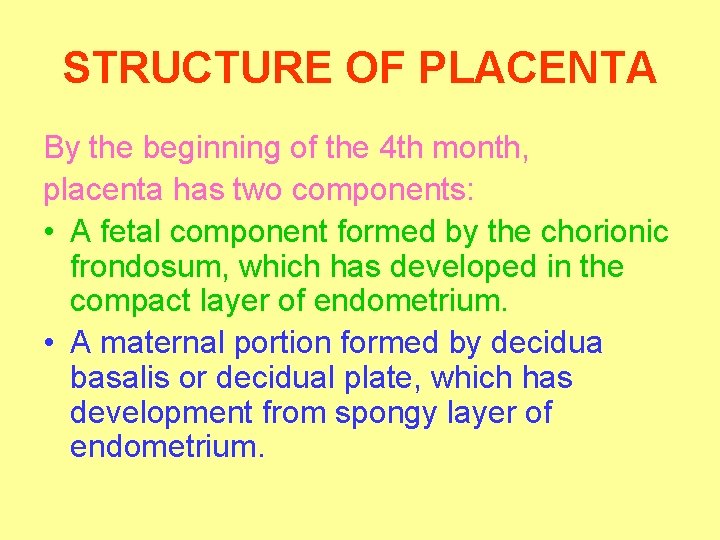
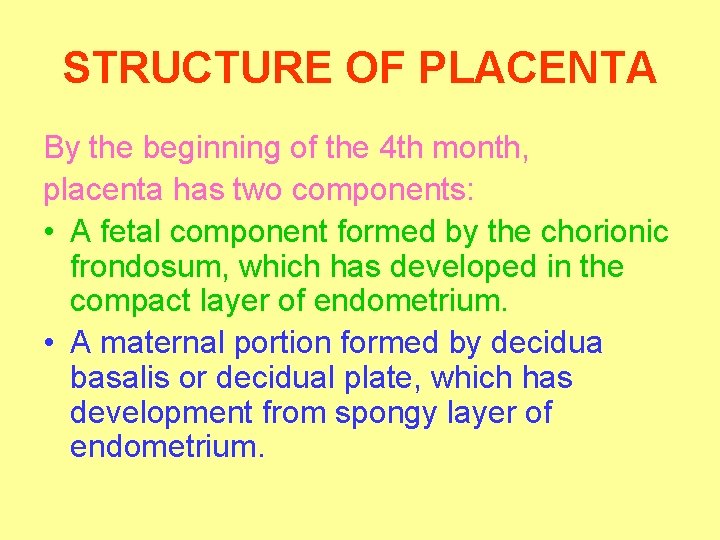
STRUCTURE OF PLACENTA By the beginning of the 4 th month, placenta has two components: • A fetal component formed by the chorionic frondosum, which has developed in the compact layer of endometrium. • A maternal portion formed by decidua basalis or decidual plate, which has development from spongy layer of endometrium.

Fetal component Consists of chorionic plate, anchoring and floating villi, and outer cytotrophoblastic shell. The chorionic plate and outer cytotrophoblastic shell is separated by lake of maternal blood. The anchoring villi connect chorionic plate and outer cytotrophoblastic shell and pass through the blood lake, thus converting this maternal blood lake into so-called intervillous spaces seen in two dimension pictures. The floating villi branch from anchoring villi and float freely in the maternal blood lake.
Maternal portion Decidual plate is intimately incorporated into the outer cytotrophoblastic shell. Here the trophoblast cells and decidua cells intermingle. During the 4 th and 5 th months, a number of septa project into the maternal blood lake, from the decidual plate. They never reach the chorionic plate. As a result of this septum formation, the maternal blood lake is divided into incomplete compartments.
• Growth in the size and thickness of the placenta continues rapidly until the fetus is about 18 weeks old (20 weeks’ gestation). • The placenta at this stage is fully developed. • Later on it enlarges only due to arborization of existing villus tree.
• Deoxygenated fetal blood passes through umbilical arteries to the placenta. • At the junction of umbilical cord and placenta, the umbilical arteries branch radially to form chorionic arteries. • Chorionic arteries, in turn, branch into cotyledon arteries.
• Placental expulsion begins as a physiological separation from the wall of the uterus. • The period from just after the fetus is expelled until just after the placenta is expelled is called the "third stage of labor". • The placenta is usually expelled within 15– 30 minutes of birth.
• After the delivery of fetus, rapid reduction in the size of the uterus leads to detachment of placenta from the uterine wall. • The uterus than undergoes a second series of contraction due to which placenta and its associated membranes (amnion and chorion leave) are forced out.
• Normally, the placenta grows onto the upper part of the uterus and stays there until your baby is born. • During the last stage of labor, the placenta separates from the uterus, and your contractions help push it into the vagina (birth canal). • This is also called the afterbirth.
• Placental expulsion can be managed actively, for example by giving oxytocin via intramuscular injection followed by cord traction to assist in delivering the placenta. • Alternatively, it can be managed expectantly, allowing the placenta to be expelled without medical assistance.
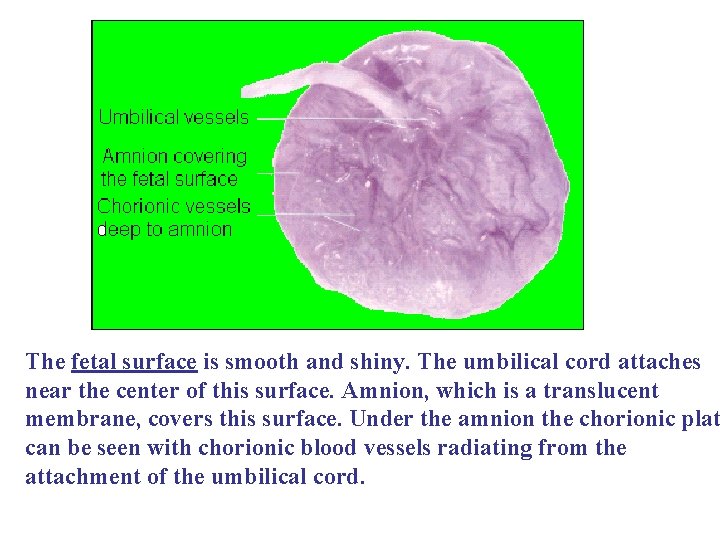
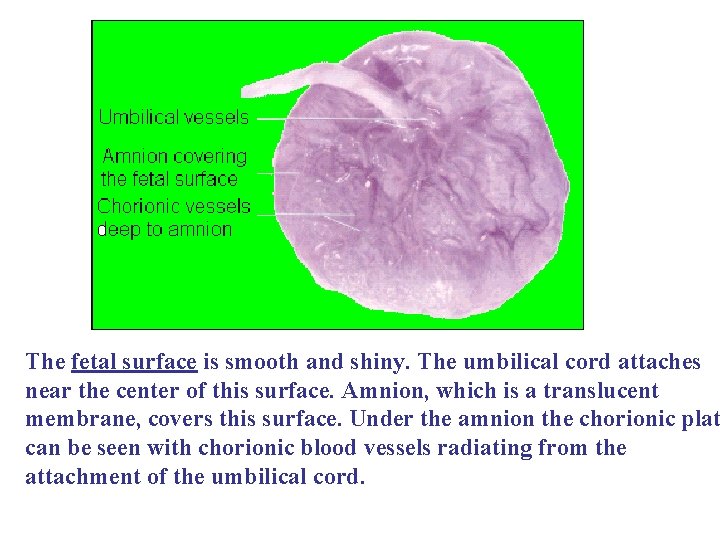
The fetal surface is smooth and shiny. The umbilical cord attaches near the center of this surface. Amnion, which is a translucent membrane, covers this surface. Under the amnion the chorionic plat can be seen with chorionic blood vessels radiating from the attachment of the umbilical cord.
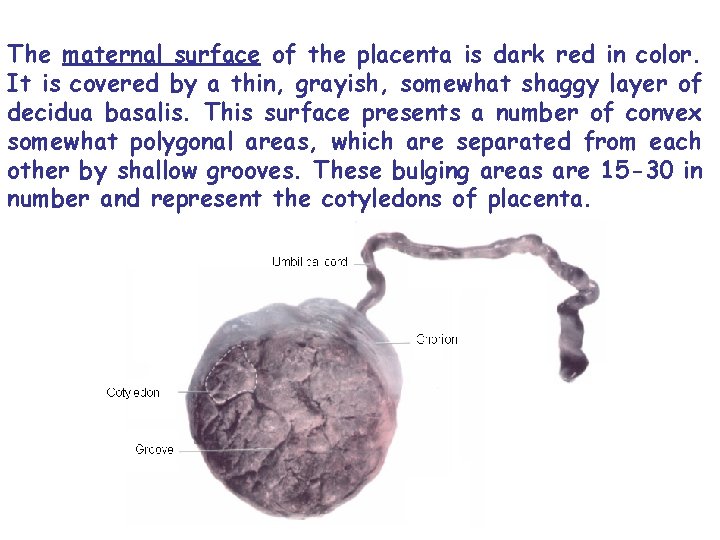
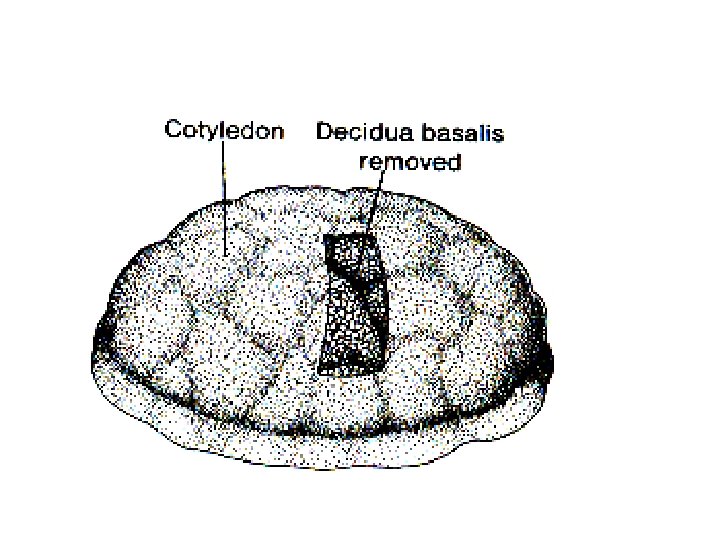
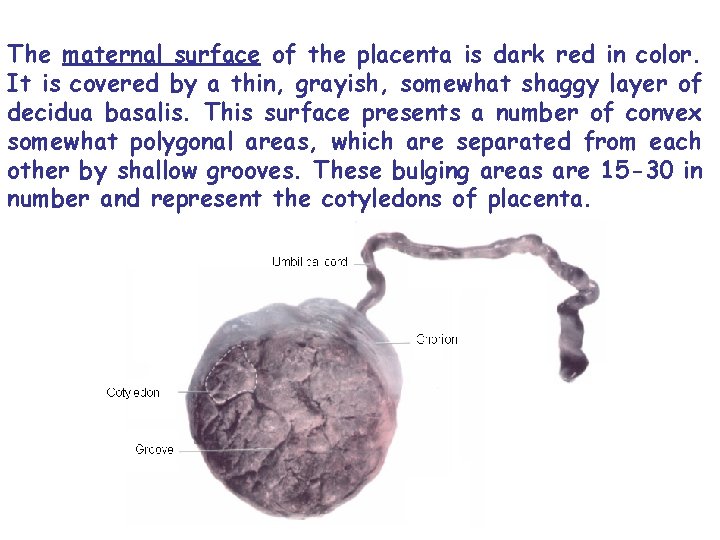
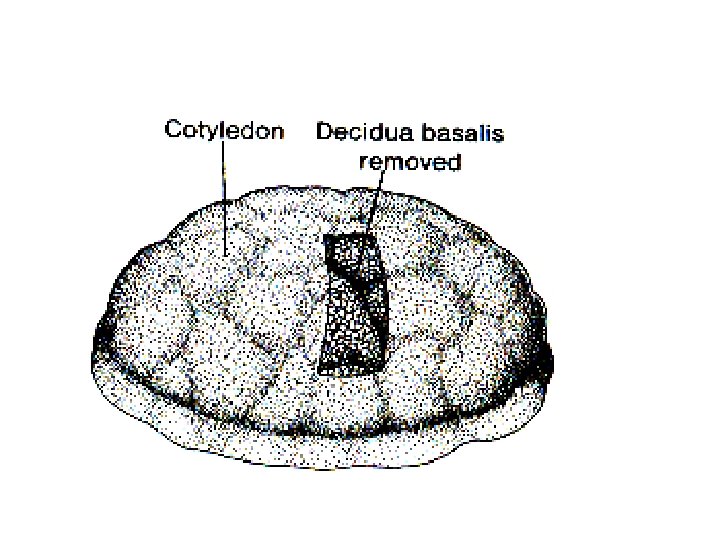
The maternal surface of the placenta is dark red in color. It is covered by a thin, grayish, somewhat shaggy layer of decidua basalis. This surface presents a number of convex somewhat polygonal areas, which are separated from each other by shallow grooves. These bulging areas are 15 -30 in number and represent the cotyledons of placenta.
FUNCTIONS OF PLACENTA
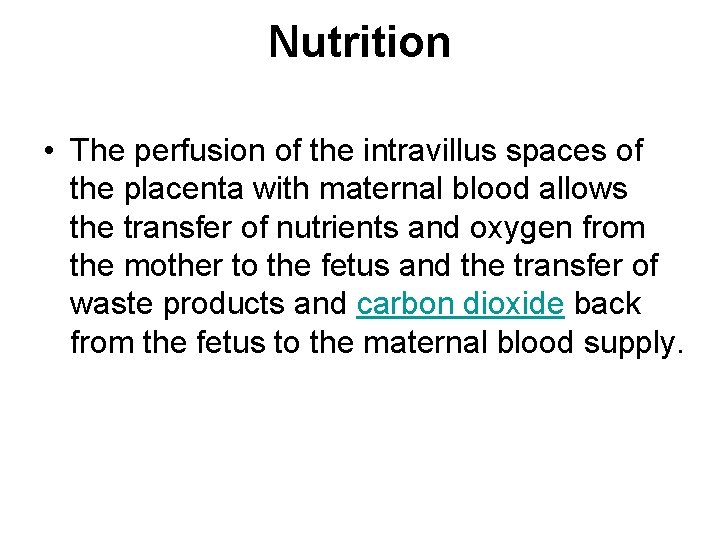
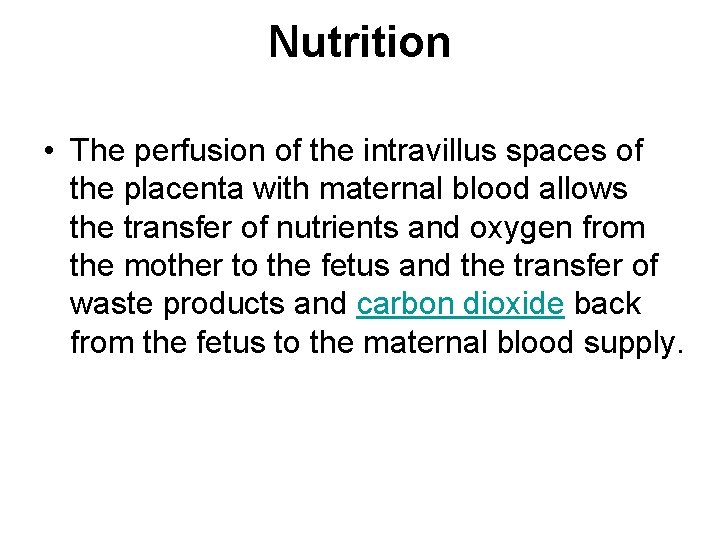
Nutrition • The perfusion of the intravillus spaces of the placenta with maternal blood allows the transfer of nutrients and oxygen from the mother to the fetus and the transfer of waste products and carbon dioxide back from the fetus to the maternal blood supply.
Excretion • Waste products excreted from the fetus such as urea, uric acid, and creatinine are transferred to the maternal blood by diffusion across the placenta.
Immunity • Ig. G antibodies can pass through the human placenta, thereby providing protection to the fetus in utero • Immunoglobulin G (Ig. G) is an antibody isotype. • It is a protein complex composed of four peptide chains — two identical heavy chainsand two identical light chains arranged in a Y-shape typical of antibody monomers.
• Each Ig. G has two antigen binding sites. Representing approximately 75% of serum immunoglobulins in humans, Ig. G is the most abundant antibody isotype found in the circulation. • Ig. G molecules are synthesized and secreted by plasma B cells.
Endocrine function • The placenta secretes hormones that are secreted by syncytial layer of chorionic villi) that are important during pregnancy.
• Human Chorionic Gonadotropin (h. CG): The first placental hormone produced is h. CG, which can be found in maternal blood and urine as early as the first missed menstrual period (shortly after implantation has occurred) • This is the hormone analyzed by pregnancy test
• Women's blood serum will be completely negative for h. CG by one to two weeks after birth. • h. CG testing is proof that all placental tissue is delivered. • h. CG is present only during pregnancy because it is secreted by the placenta.
• h. CG also ensures that the corpus luteum continues to secrete progesterone and estrogen. • Progesterone is very important during pregnancy because, when its secretion decreases, the endometrial lining will slough off and pregnancy will be lost.
![Human Placental Lactogen h PL Human Chorionic Somatomammotropin This hormone is lactogenic • Human Placental Lactogen (h. PL [Human Chorionic Somatomammotropin]): This hormone is lactogenic](https://slidetodoc.com/presentation_image/3df3a766183083369ab0106450b62385/image-77.jpg)
• Human Placental Lactogen (h. PL [Human Chorionic Somatomammotropin]): This hormone is lactogenic and growthpromoting properties. • It promotes mammary gland growth in preparation for lactation in the mother. • It also regulates maternal glucose, protein, and fat levels so that this is always available to the fetus.
• Estrogen: referred to as the "hormone of women" because it stimulates the development of secondary female sex characteristics. • It contributes to the woman's mammary gland development in preparation for lactation and stimulates uterine growth to accommodate growing fetus.
• Progesterone: necessary to maintain endometrial lining of the uterus during pregnancy. • This hormone prevents preterm labor by reducing myometrial contraction. • Levels of progesterone are high during pregnancy.
Cloaking from immune system of mother • The placenta and fetus may be regarded as a foreign allograft inside the mother, and thus must evade from attack by the mother's immune system.
• Allotransplantation (allo- from the Greek meaning "other") is the transplantation of cells, tissues, or organs, to a recipient from a genetically non-identical donor of the same species. • The transplant is called an allograft, allogeneic transplant, or homograft.
• For this purpose, the placenta uses several mechanisms: • It secretes Neurokinin Bcontaining phosphocholine molecules. This is the same mechanism used by parasitic nematodes to avoid detection by the immune system of their host
• There is presence of small lymphocytic suppressor cells in the fetus that inhibit maternal cytotoxic T cells by inhibiting the response to interleukin 2
• However, the Placental barrier is not the sole means to evade the immune system, as foreign foetal cells also persist in the maternal circulation, on the other side of the placental barrier
• The placenta also provides a reservoir of blood for the fetus, delivering blood to it in case of hypotension and vice versa, comparable to a capacitor
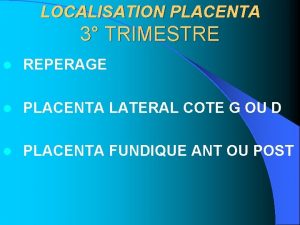
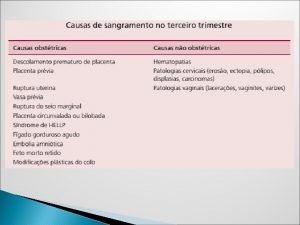
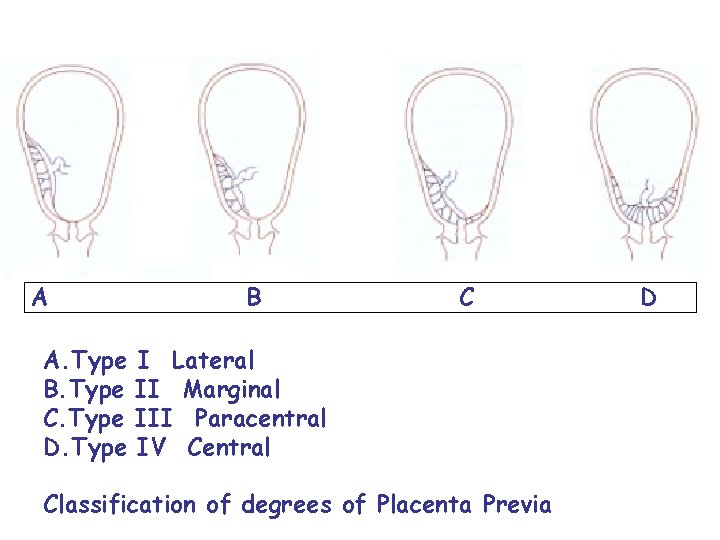
• Placenta praevia (placenta previa) is an obstetric complication in which the placenta is inserted partially or wholly in lower uterine segment
• It can sometimes occur in the later part of the first trimester, but usually during the second or third. • It is a leading cause of antepartum haemorrhage (vaginal bleeding). • It affects approximately 0. 4 -0. 5% of all labours
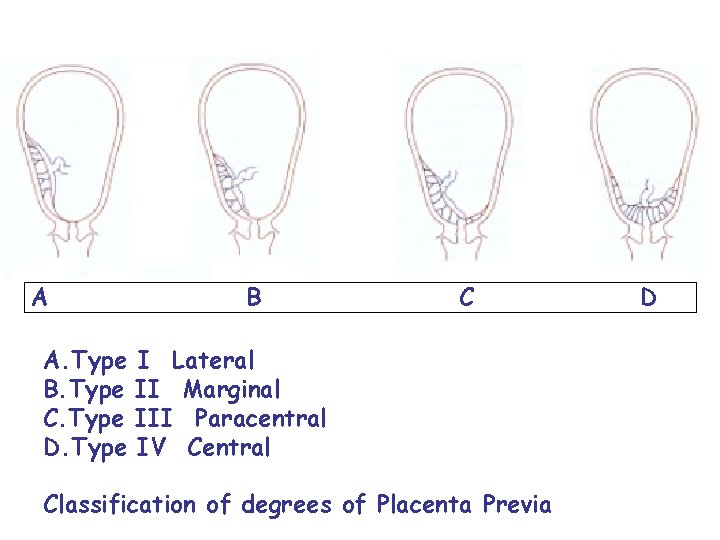
A B C A. Type I Lateral B. Type II Marginal C. Type III Paracentral D. Type IV Central Classification of degrees of Placenta Previa D
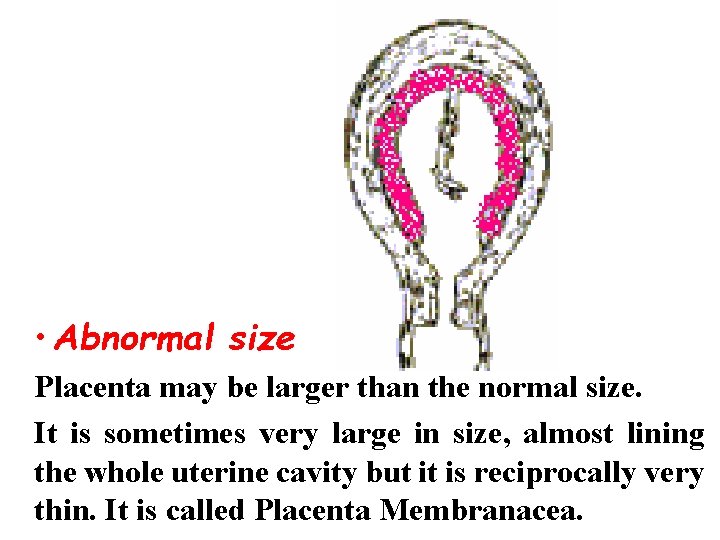
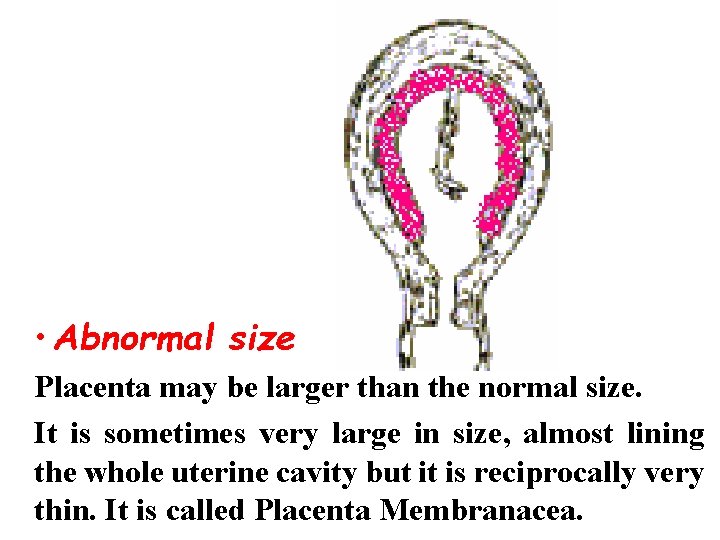
• Abnormal size Placenta may be larger than the normal size. It is sometimes very large in size, almost lining the whole uterine cavity but it is reciprocally very thin. It is called Placenta Membranacea.
Abnormal weight The normal weight of placenta is about 500 to 600 gm (about one-sixth that of the fetus). Very small placentas are found in women suffering from chronic hypertension. Excessively large placentae occur with fetal hydrops.
• Hydrops fetalis is a condition in the fetus characterized by an accumulation of fluid, or edema, in at least two fetal compartments. • By comparison, hydrops allantois or hydrops amnion are an accumulation of excessive fluid in the allantoic or amniotic space respectively
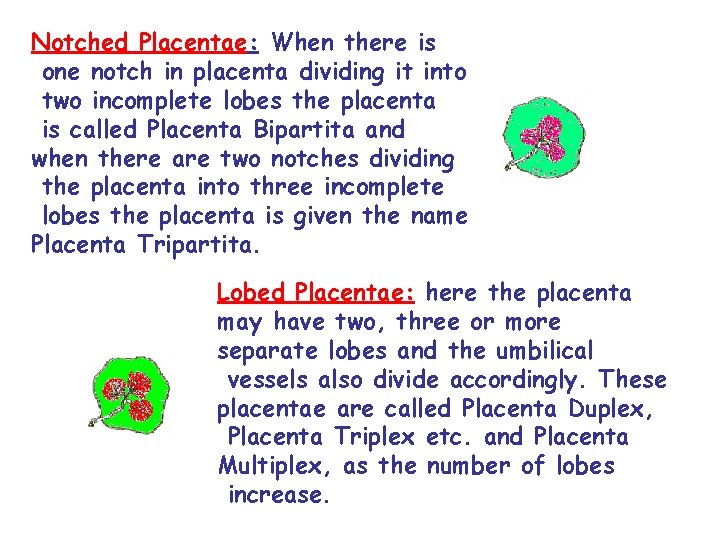
Abnormalities of Shape Normally the placenta has a circular shape. But sometimes it may have oval, fusiform, crescentic or other shapes. The placenta may be notched or lobed.
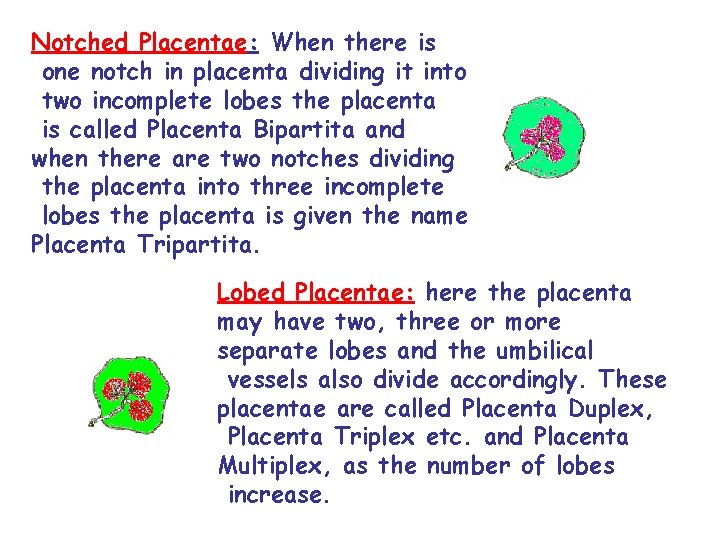
Notched Placentae: When there is one notch in placenta dividing it into two incomplete lobes the placenta is called Placenta Bipartita and when there are two notches dividing the placenta into three incomplete lobes the placenta is given the name Placenta Tripartita. Lobed Placentae: here the placenta may have two, three or more separate lobes and the umbilical vessels also divide accordingly. These placentae are called Placenta Duplex, Placenta Triplex etc. and Placenta Multiplex, as the number of lobes increase.
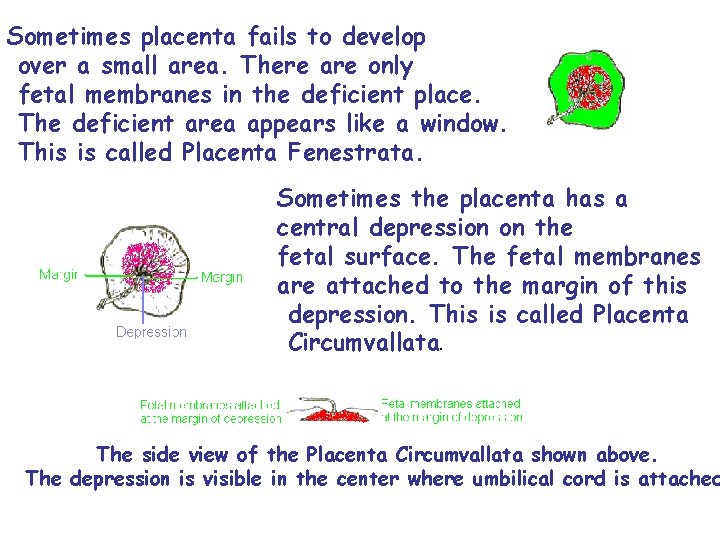
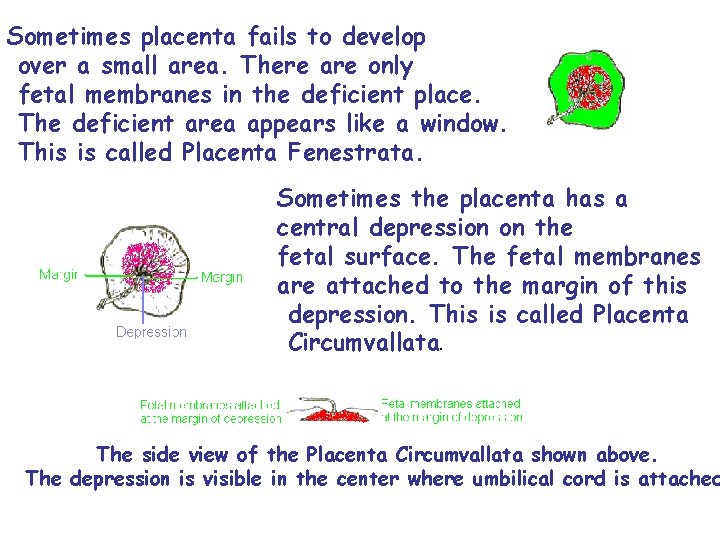
Sometimes placenta fails to develop over a small area. There are only fetal membranes in the deficient place. The deficient area appears like a window. This is called Placenta Fenestrata. Sometimes the placenta has a central depression on the fetal surface. The fetal membranes are attached to the margin of this depression. This is called Placenta Circumvallata. The side view of the Placenta Circumvallata shown above. The depression is visible in the center where umbilical cord is attached
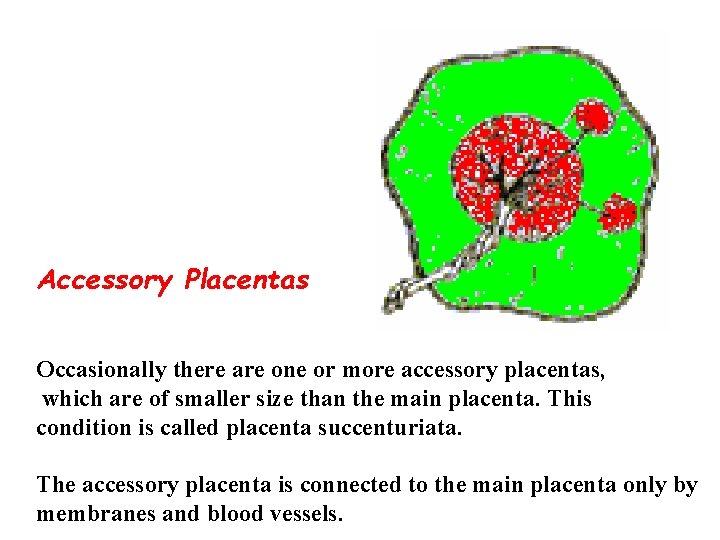
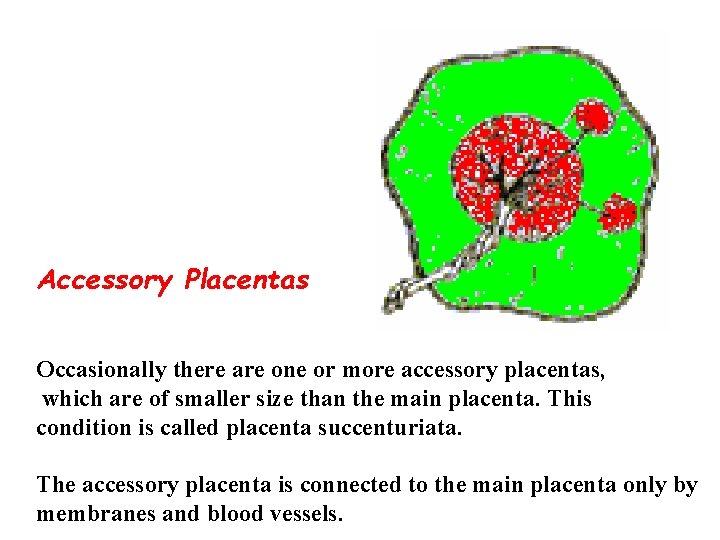
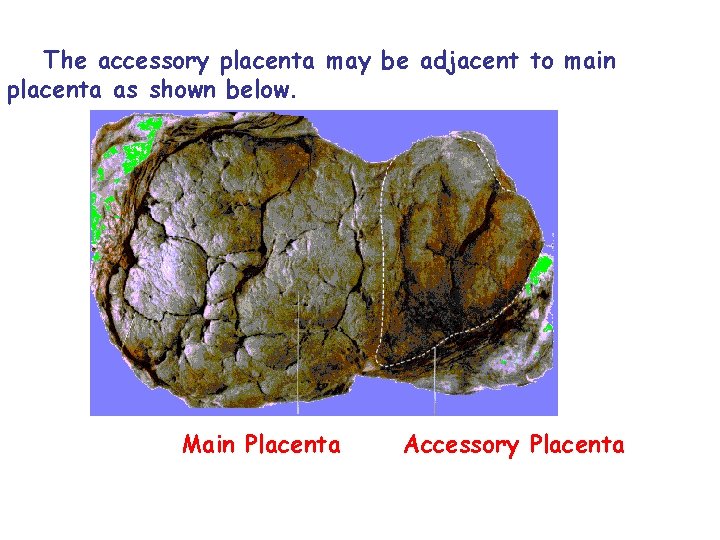
Accessory Placentas Occasionally there are one or more accessory placentas, which are of smaller size than the main placenta. This condition is called placenta succenturiata. The accessory placenta is connected to the main placenta only by membranes and blood vessels.
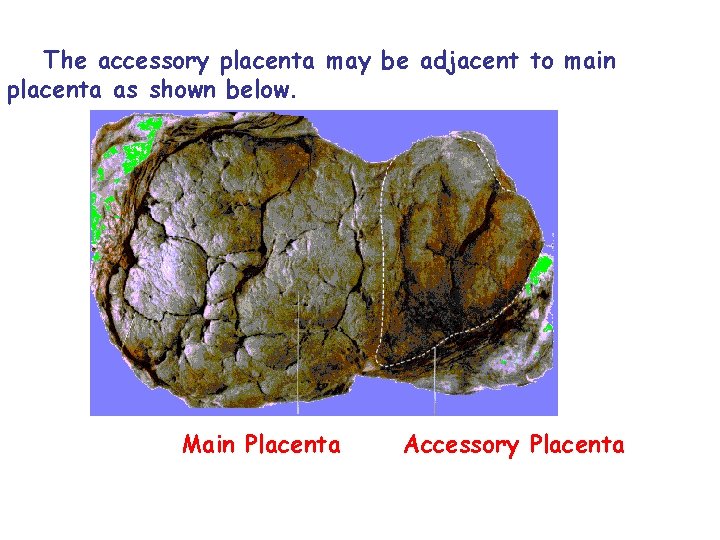
The accessory placenta may be adjacent to main placenta as shown below. Main Placenta Accessory Placenta
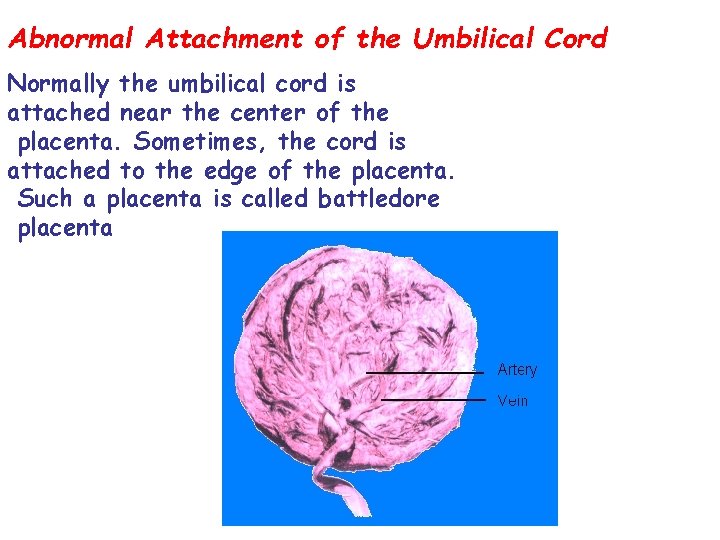
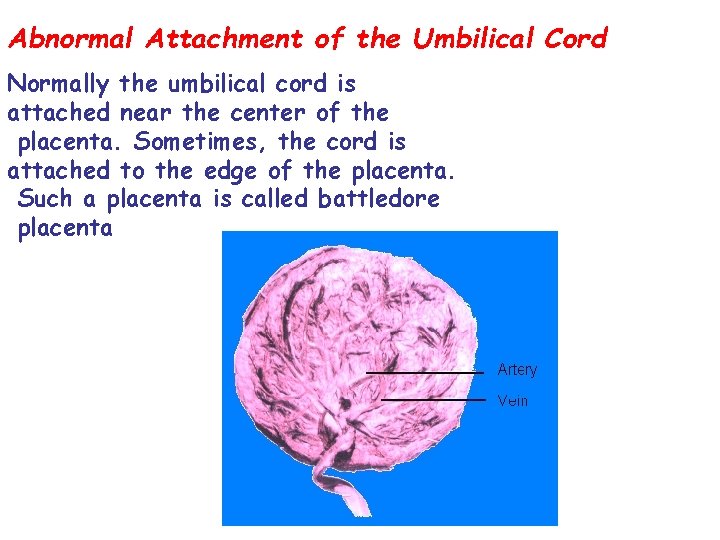
Abnormal Attachment of the Umbilical Cord Normally the umbilical cord is attached near the center of the placenta. Sometimes, the cord is attached to the edge of the placenta. Such a placenta is called battledore placenta
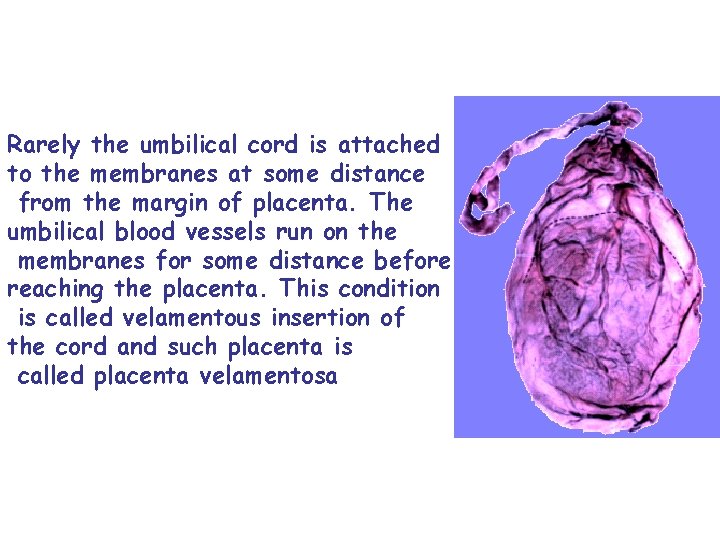
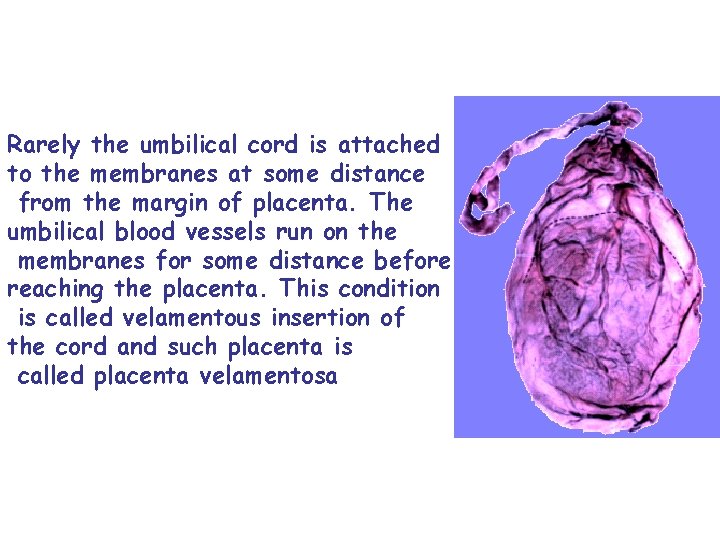
Rarely the umbilical cord is attached to the membranes at some distance from the margin of placenta. The umbilical blood vessels run on the membranes for some distance before reaching the placenta. This condition is called velamentous insertion of the cord and such placenta is called placenta velamentosa
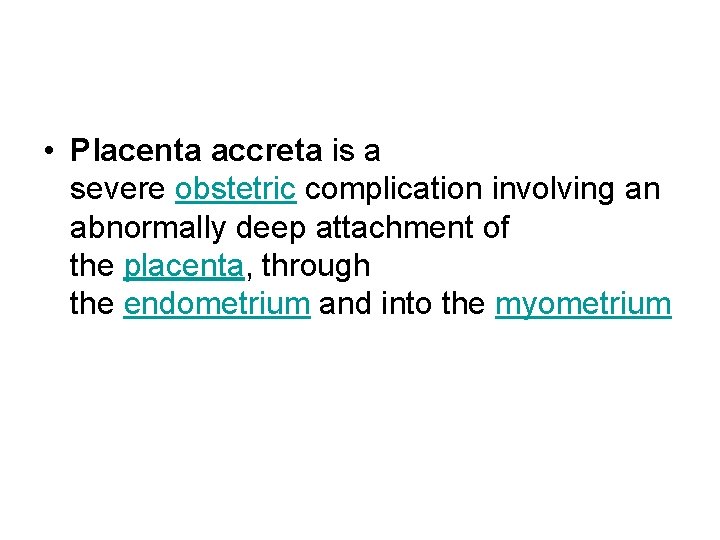
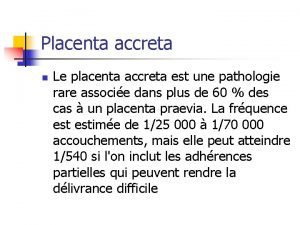
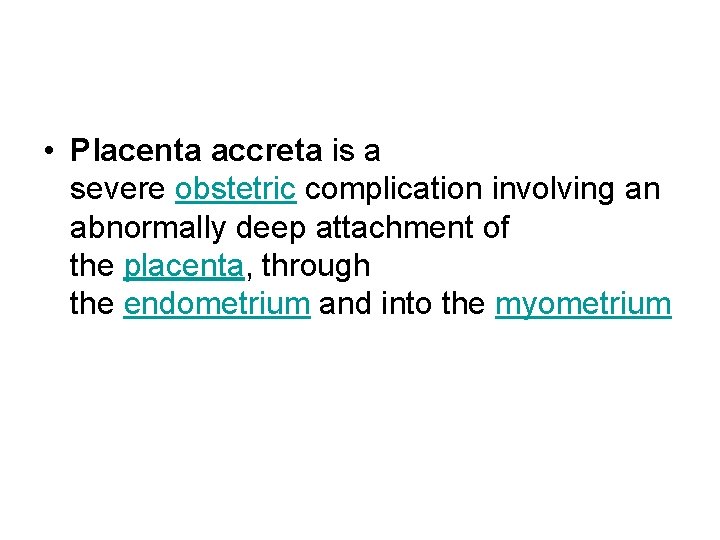
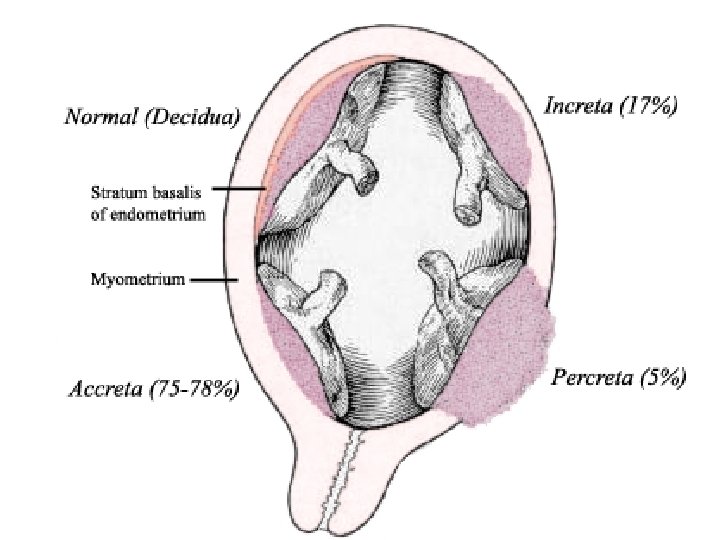
• Placenta accreta is a severe obstetric complication involving an abnormally deep attachment of the placenta, through the endometrium and into the myometrium
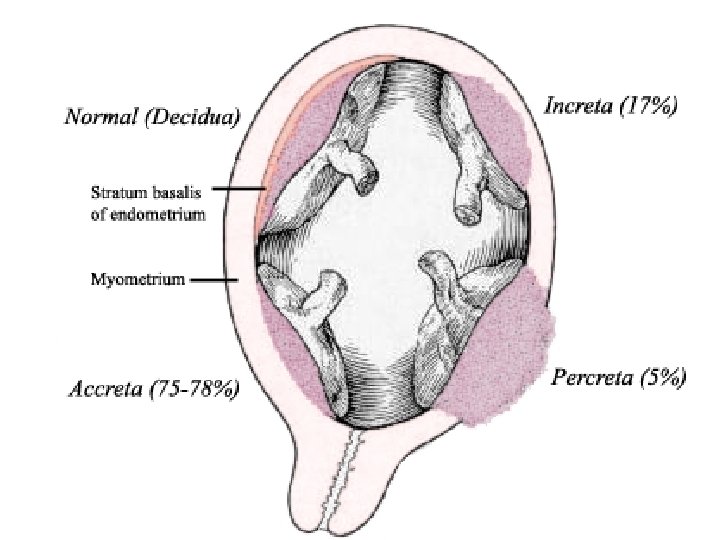
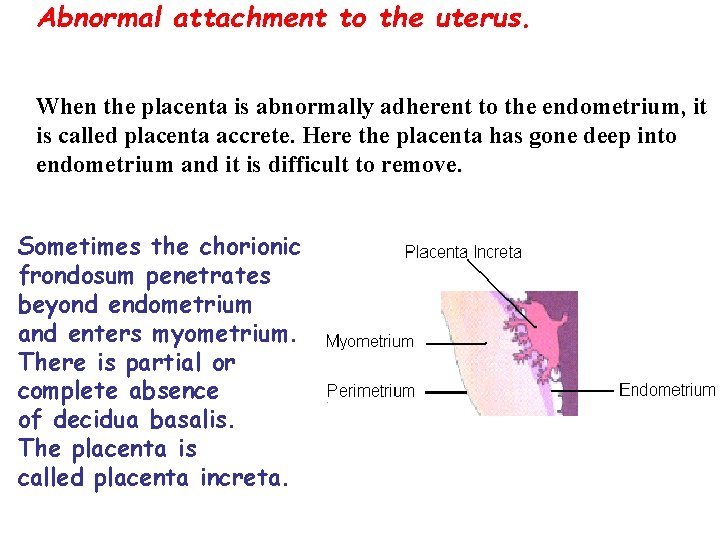
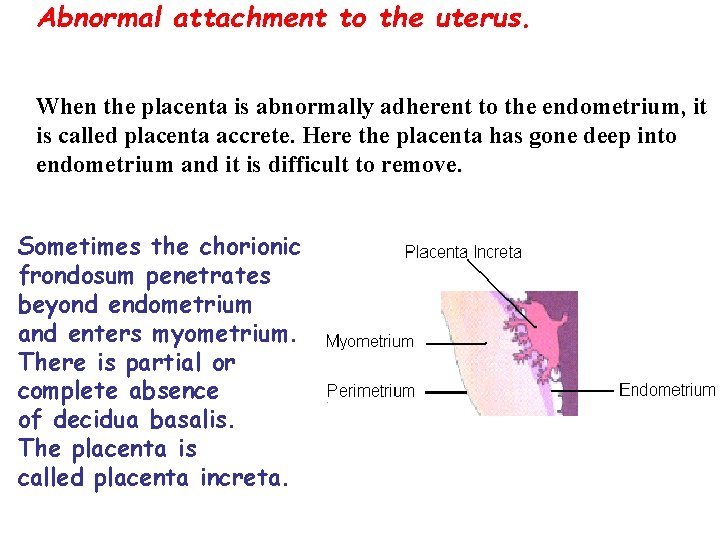
Abnormal attachment to the uterus. When the placenta is abnormally adherent to the endometrium, it is called placenta accrete. Here the placenta has gone deep into endometrium and it is difficult to remove. Sometimes the chorionic frondosum penetrates beyond endometrium and enters myometrium. There is partial or complete absence of decidua basalis. The placenta is called placenta increta.
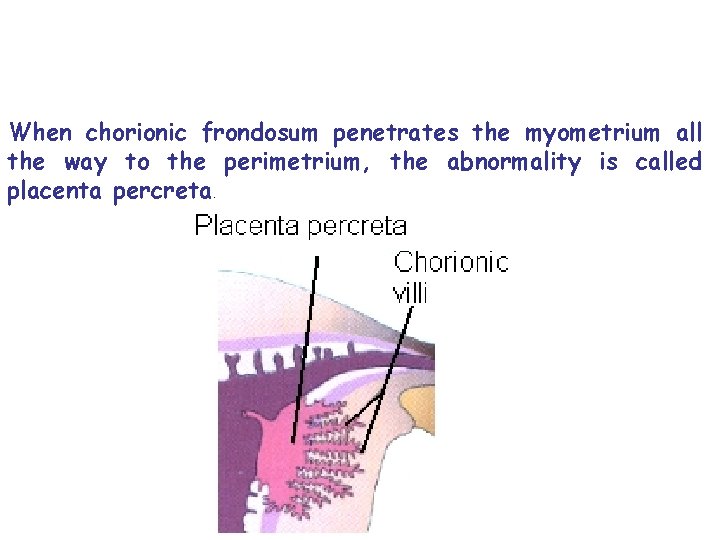
When chorionic frondosum penetrates the myometrium all the way to the perimetrium, the abnormality is called placenta percreta.
 Placenta previa classification
Placenta previa classification Latin word means knowledge
Latin word means knowledge Root word of auditor
Root word of auditor Advent comes from the latin word “adventus” which means
Advent comes from the latin word “adventus” which means The word report is derived from the latin word
The word report is derived from the latin word Concave lens
Concave lens Revelation comes from the latin word
Revelation comes from the latin word Word bank derived from
Word bank derived from When was the word computer first used
When was the word computer first used Why called latin america
Why called latin america It literally means rebirth
It literally means rebirth Latin noun declensions
Latin noun declensions Latin word of literature
Latin word of literature Fort root words
Fort root words Fossilis latin
Fossilis latin What does forensic mean in latin
What does forensic mean in latin Trophic root word
Trophic root word Far side spider slide
Far side spider slide Dataisplural
Dataisplural Latin words
Latin words Latin word of cell
Latin word of cell Coda meaning
Coda meaning What is pisces favorite animal
What is pisces favorite animal Characteristics of hospitality
Characteristics of hospitality Cut with the kitchen knife dada through of germany
Cut with the kitchen knife dada through of germany Latin word for war
Latin word for war Brevis latin meaning
Brevis latin meaning Words with the stem cor
Words with the stem cor Latin word for poison
Latin word for poison Science comes from the latin word
Science comes from the latin word Difference between rampant and nursing bottle caries
Difference between rampant and nursing bottle caries The word authority is derived from
The word authority is derived from Art appreciation subject in college philippines
Art appreciation subject in college philippines Oto root word
Oto root word Civilization comes from the latin word
Civilization comes from the latin word Latin word for sea creature in photography
Latin word for sea creature in photography Latin legalese
Latin legalese Ultimus definition
Ultimus definition Punic is the latin word for
Punic is the latin word for Ped root word
Ped root word Latin word for renaissance
Latin word for renaissance Latin word for net
Latin word for net Tunica albuginea
Tunica albuginea Vasa previa
Vasa previa Placental cotyledons
Placental cotyledons Vas deferens
Vas deferens Seno marginal de la placenta
Seno marginal de la placenta Anexos embrionarios
Anexos embrionarios Placenta previa grades
Placenta previa grades Site:slidetodoc.com
Site:slidetodoc.com Dog placenta
Dog placenta Placenta bas inséré
Placenta bas inséré Chorion
Chorion Types of placenta
Types of placenta Sips vs nipt
Sips vs nipt Placenta circumvallata
Placenta circumvallata Placenta granum
Placenta granum Gastrula
Gastrula Seno marginal de la placenta
Seno marginal de la placenta Dirty duncan placenta
Dirty duncan placenta Kode icd 10 letkep
Kode icd 10 letkep Dirty duncan and shiny schultz
Dirty duncan and shiny schultz Glandula mamaria activa
Glandula mamaria activa Hémorragie de benkiser
Hémorragie de benkiser Family feud questions philippines
Family feud questions philippines Fetal warfarin syndrome mnemonic
Fetal warfarin syndrome mnemonic Anabolisme gravidique
Anabolisme gravidique Seno marginal de la placenta
Seno marginal de la placenta Puntos toconomicos
Puntos toconomicos Placenta centralis
Placenta centralis Placenta praevia bessis
Placenta praevia bessis Cotilédones placenta
Cotilédones placenta Choriová dutina
Choriová dutina Classification de bessis placenta praevia
Classification de bessis placenta praevia Structure of placenta ppt
Structure of placenta ppt Parte fetal da placenta
Parte fetal da placenta Placenta tipo schultze
Placenta tipo schultze Placenta image
Placenta image Chorionic cavity
Chorionic cavity Placenta circumvalata
Placenta circumvalata Placenta
Placenta Placenta previa
Placenta previa Placenta centralis
Placenta centralis Placenta previa lateralis
Placenta previa lateralis Placenta previa
Placenta previa Placenta abruption
Placenta abruption Carissa santos
Carissa santos Placenta pancreta
Placenta pancreta Mac robert manoeuvre
Mac robert manoeuvre Placenta prvia
Placenta prvia Placenta previa
Placenta previa Fetomaternal organ
Fetomaternal organ Placenta prvia
Placenta prvia Placenta circumvalata
Placenta circumvalata Anulus tendineus communis zinni
Anulus tendineus communis zinni Placenta previa
Placenta previa Gestacy
Gestacy Cotiledón placentario
Cotiledón placentario Gametes
Gametes Placenta previa
Placenta previa Twin placenta
Twin placenta Placenta circumvallata
Placenta circumvallata Placenta praevia marginalis
Placenta praevia marginalis Battledore cord insertion
Battledore cord insertion