Intrapartum Nursing Care On Admission InductionCesarean Section Care


- Slides: 77
Intrapartum Nursing Care On Admission Induction/Cesarean Section Care in 1 st, 2 nd, 3 rd, and 4 th Stages of Labor Precipitous/Out-of-Hospital Delivery
When to go to Hospital n n Regular Contractions with intensity SROM Vaginal Bleeding Changes in Fetal Movement—especially a in fetal movement as described in the Daily Fetal Movement Count
On Admission to Hospital n Evaluate Is this True Labor? n IMMINENCE OF DELIVERY n Condition of mother n Condition of fetus n Previous experience with labor n Childbirth education—Lamaze, Childbirth preparation, breastfeeding, cesarean section class n Is there a BIRTH PLAN? Any plans for anesthesia?
Identify Patient n n n Note time of arrival/reason for admission Pt’s name, MD-both Obstetrician and pediatrician Plans to breast or bottle feed Assess when she last ate or drank Assess support person and what they perceive as their role in the labor process. Remember to introduce yourself as the RN and explain all assessment parameters and interventions in simple terms
Review Prenatal History n n n n EDC/EDD Is baby term? OB History: GTPAL status, previous labors Medications taken during pregnancy including Prenatal vitamins and Iron Use of alcohol, illicit drugs, tobacco during pg Labs (Blood Type & Rh, Rubella, Beta Strep, MSAFP, VDRL/RPR, GC culture) Diagnostic Tests (Amniocentesis, Ultrasound) Allergies Complications (Medical/OB)—chronic illnesses, BP, dysuria, edema of hands and face, etc.
Physical Assessment on Admission n n Maternal Vital Signs—between contractions Fetal Status—baseline FHR, accels/decels, fetal movement and FHR response n Labor Status n Contractions—frequency, duration, intensity n Vaginal Discharge (? ? SROM = NO GEL)— bloody show? , color and odor of amniotic fluid if SROM, use Nitrazine paper to assess SROM n Vaginal Changes—dilatation, effacement n Descent of Fetus– Presentation, Station, Position
Physical Assessment, cont’d n Abdominal Exam n n Chest n n Assess bowel sounds laterally Assess fundal height Perform Leopold’s Maneuvers Assess heart and lung sounds DTR’s n n Assess patellar reflexes bilaterally Note hyperreflexia, if +3 -+4, check for clonus
Psychosocial Assessment on Admission n Mother’s Status—in early labor, pt is often excited, teachable, and talkative. As labor progresses, anxiety increases as pain increases & the ability of the pt to focus decreases. Noting these variables helps the nurse determine the progress of labor n Support Persons—assess who they are & how they expect to participate in the labor process e. g. active labor coach vs. observer n Nurse’s Role—support pt and significant others and encourage to verbalize fears & concerns. Evaluate how best to provide Family-Centered Care for this family system
Admission/Diagnostics n n CBC (Hgb, Hct), Type/Rh (if unknown) U/A n Dipstick—often done in the lab Glucose n Albumin n U/A if ordered Blood Type and Cross-match for C/S only
Nursing Care On Admission n Place EFM ASAP—Assess fetal status Do Vag Exam—Assess Labor Status Complete OB Paperwork n n Check Orders n n n Assessment, Hx, Database, PG Hx, Vitals Start IV, especially if pt wants epidural soon Lab Work Orient to Room
ALWAYS assess FHR n AFTER AROM or SROM n n BEFORE starting Pitocin for Induction n n (risk of prolapsed cord) Throughout induction BEFORE & AFTER analgesia/anesthesia
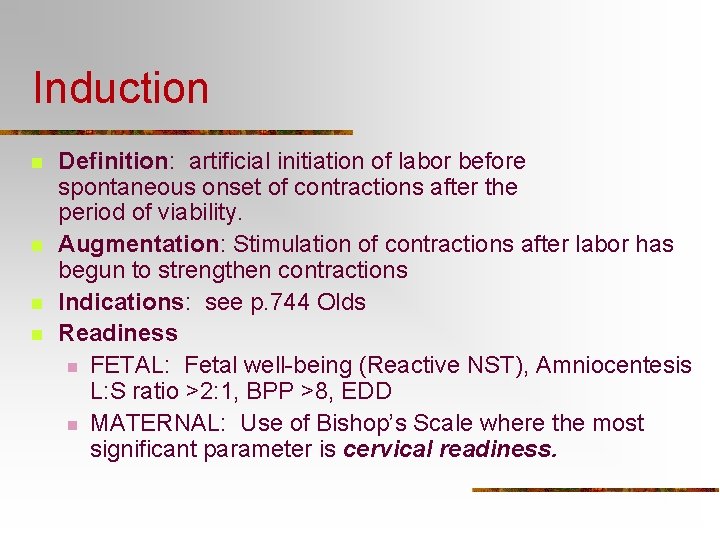
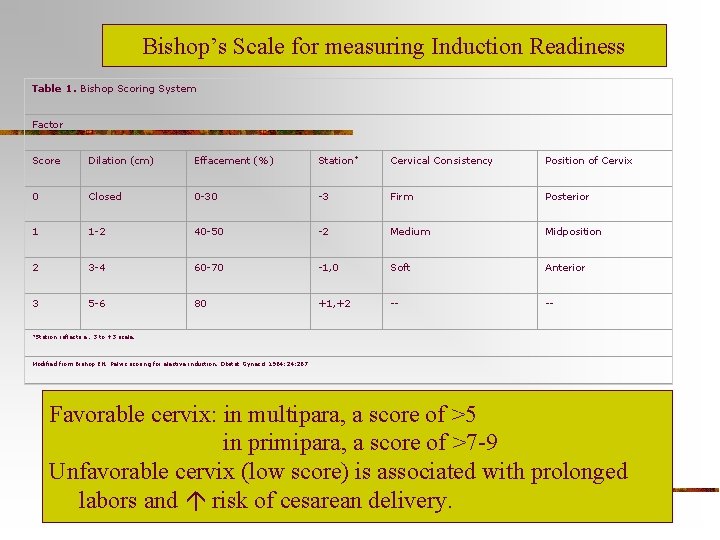
Induction n n Definition: artificial initiation of labor before spontaneous onset of contractions after the period of viability. Augmentation: Stimulation of contractions after labor has begun to strengthen contractions Indications: see p. 744 Olds Readiness n FETAL: Fetal well-being (Reactive NST), Amniocentesis L: S ratio >2: 1, BPP >8, EDD n MATERNAL: Use of Bishop’s Scale where the most significant parameter is cervical readiness.
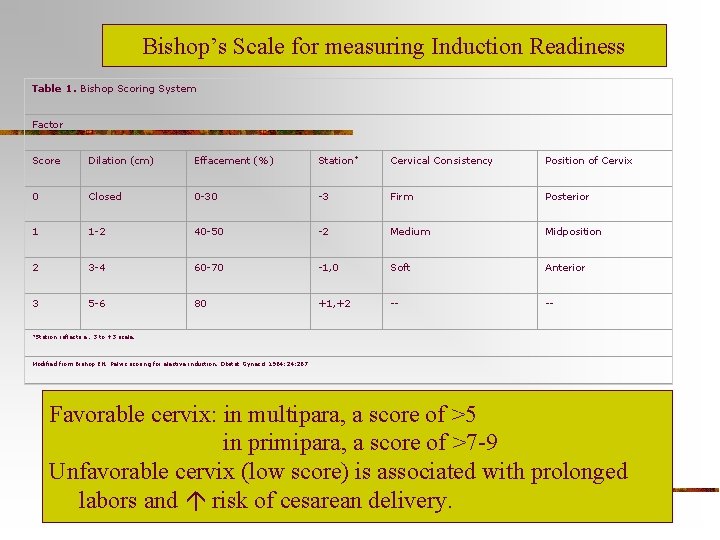
Bishop’s Scale for measuring Induction Readiness Table 1. Bishop Scoring System Factor Score Dilation (cm) Effacement (%) Station* Cervical Consistency Position of Cervix 0 Closed 0 -30 -3 Firm Posterior 1 1 -2 40 -50 -2 Medium Midposition 2 3 -4 60 -70 -1, 0 Soft Anterior 3 5 -6 80 +1, +2 -- -- *Station reflects a. 3 to +3 scale. Modified from Bishop EH. Pelvic scoring for elective induction. Obstet Gynecol 1964; 24: 267 Favorable cervix: in multipara, a score of >5 in primipara, a score of >7 -9 Unfavorable cervix (low score) is associated with prolonged labors and risk of cesarean delivery.
Methods of Staged Induction– especially used if cervix is not ripe n n Laminaria– seaweed is hydrophilic and absorbs water thus swelling in the cx and causing it to dilate. MD places these in the external os of the cx and allows the “tent” to swell overnight. Prostaglandin– a variety of forms from gels inserted transvaginally, to suppositories, or vaginal inserts
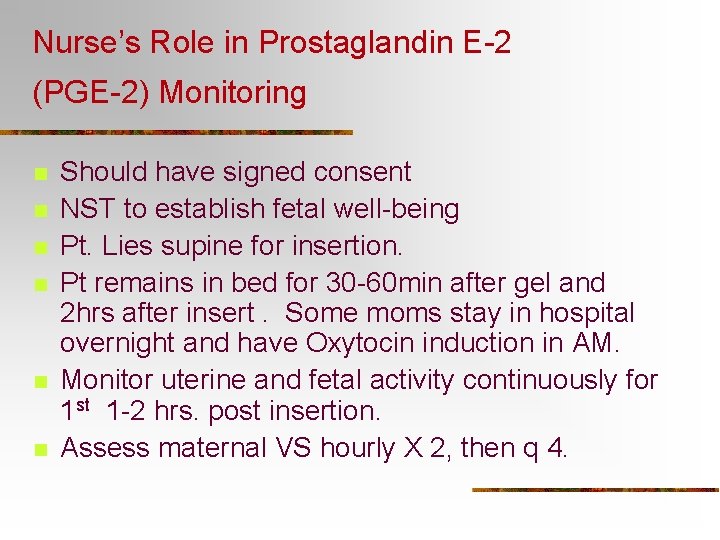
Nurse’s Role in Prostaglandin E-2 (PGE-2) Monitoring n n n Should have signed consent NST to establish fetal well-being Pt. Lies supine for insertion. Pt remains in bed for 30 -60 min after gel and 2 hrs after insert. Some moms stay in hospital overnight and have Oxytocin induction in AM. Monitor uterine and fetal activity continuously for 1 st 1 -2 hrs. post insertion. Assess maternal VS hourly X 2, then q 4.
Nurse’s Role in Prostaglandin E-2 (PGE-2) Monitoring Cervidil n n After 2 hours, pt is encouraged to walk. She may be advised to go home if no active labor evident, & instructed to return if BOW breaks, contractions become more regular, or fetal movements decrease. RISKS: uterine hyperstimulation, but uncommon if properly inserted. Be prepared to remove excess gel with gauze squares or remove Cervidil insert in cases of hyperstimulation.
Methods of Induction-when Cervix is ripe and ready n AROM/Amniotomy n n Potential complication: a. Infection b. Prolapsed cord c. Fetal head or cord compression Contraindications: a. When presenting part is floating high b. If fetus is in a breech or transverse lie
Methods of Induction-when Cervix is ripe and ready n Nursing Care after AROM: a. Assessment– FHT of baby immediately -VS of mom a & p, Temp q 2 h -Assess color & odor of fluid immediately after AROM b. Intervention/Plan– -Explain procedure to pt -Prepare room: supine position, sterile gloves, for MD, KY lubricant, Amniotome or Fetal Scalp Electrode -Change waterproof pads under pt prn. c. Evaluation— -FHR remains stable, pt is comfortable
Methods of Induction-when Cervix is ripe and ready n Oxytocin (Pitocin) n Uses: *induce rhythmic uterine contractions *augment weak or ineffective contr. *promote uterine contraction in 4 th stage of labor
Oxytocin (Pitocin) n Contraindications: *any obstruction that interferes with fetal descent *any risk of uterine rupture(e. g. . VBAC) *hypertonic uterus *existing fetal distress (e. g. positive CST) *placenta previa *genital herpes (active lesions)
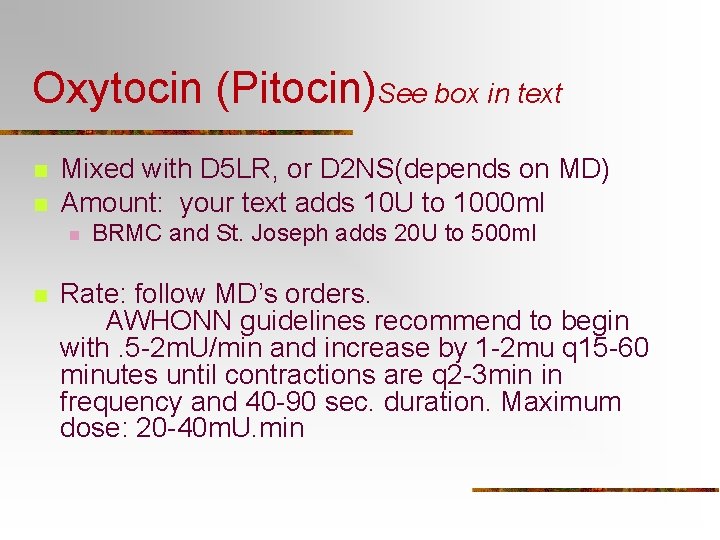
Oxytocin (Pitocin)See box in text n n Mixed with D 5 LR, or D 2 NS(depends on MD) Amount: your text adds 10 U to 1000 ml n n BRMC and St. Joseph adds 20 U to 500 ml Rate: follow MD’s orders. AWHONN guidelines recommend to begin with. 5 -2 m. U/min and increase by 1 -2 mu q 15 -60 minutes until contractions are q 2 -3 min in frequency and 40 -90 sec. duration. Maximum dose: 20 -40 m. U. min
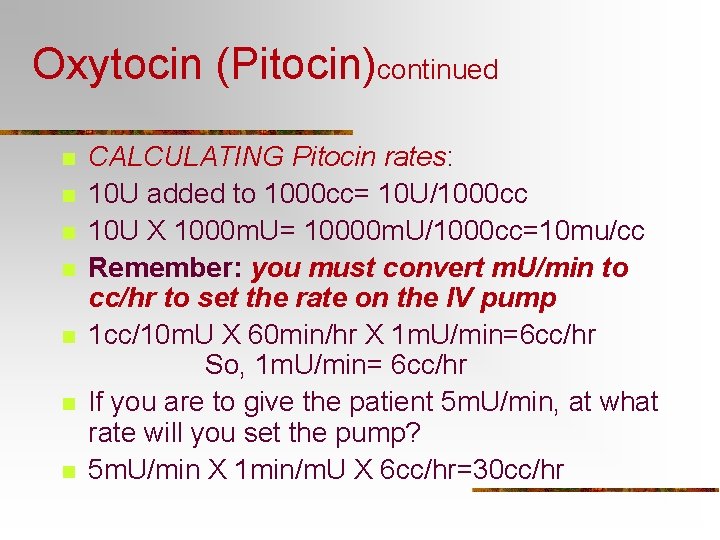
Oxytocin (Pitocin)continued n n n n CALCULATING Pitocin rates: 10 U added to 1000 cc= 10 U/1000 cc 10 U X 1000 m. U= 10000 m. U/1000 cc=10 mu/cc Remember: you must convert m. U/min to cc/hr to set the rate on the IV pump 1 cc/10 m. U X 60 min/hr X 1 m. U/min=6 cc/hr So, 1 m. U/min= 6 cc/hr If you are to give the patient 5 m. U/min, at what rate will you set the pump? 5 m. U/min X 1 min/m. U X 6 cc/hr=30 cc/hr
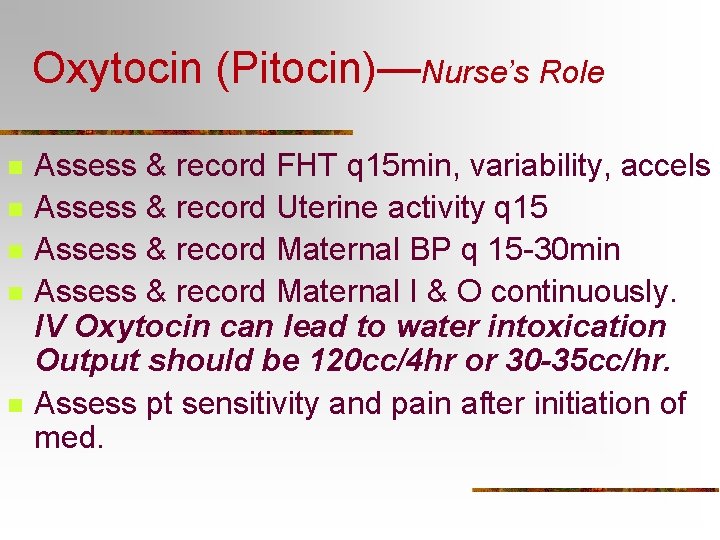
Oxytocin (Pitocin)—Nurse’s Role n n n Assess & record FHT q 15 min, variability, accels Assess & record Uterine activity q 15 Assess & record Maternal BP q 15 -30 min Assess & record Maternal I & O continuously. IV Oxytocin can lead to water intoxication Output should be 120 cc/4 hr or 30 -35 cc/hr. Assess pt sensitivity and pain after initiation of med.
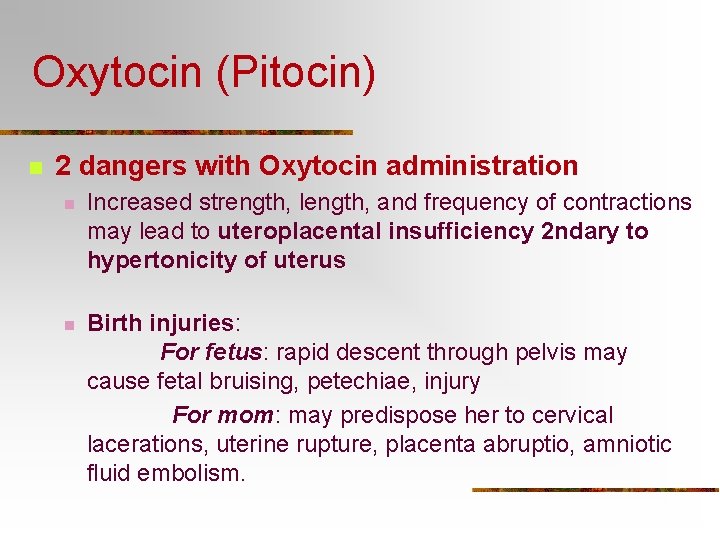
Oxytocin (Pitocin) n 2 dangers with Oxytocin administration n Increased strength, length, and frequency of contractions may lead to uteroplacental insufficiency 2 ndary to hypertonicity of uterus n Birth injuries: For fetus: rapid descent through pelvis may cause fetal bruising, petechiae, injury For mom: may predispose her to cervical lacerations, uterine rupture, placenta abruptio, amniotic fluid embolism.
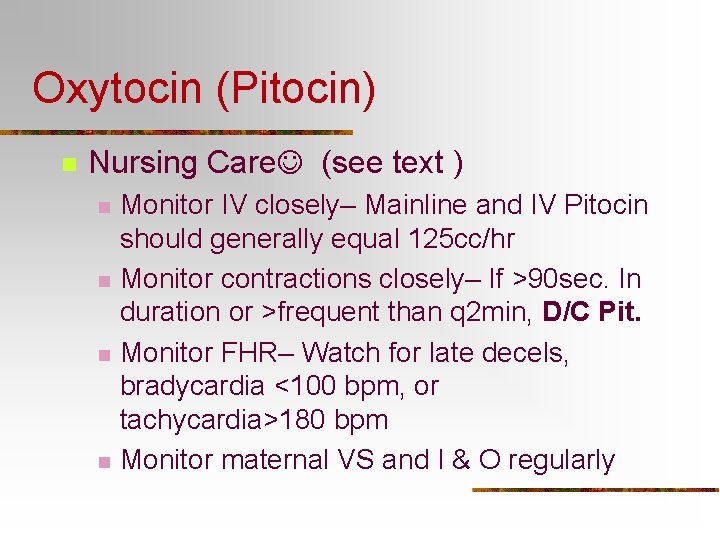
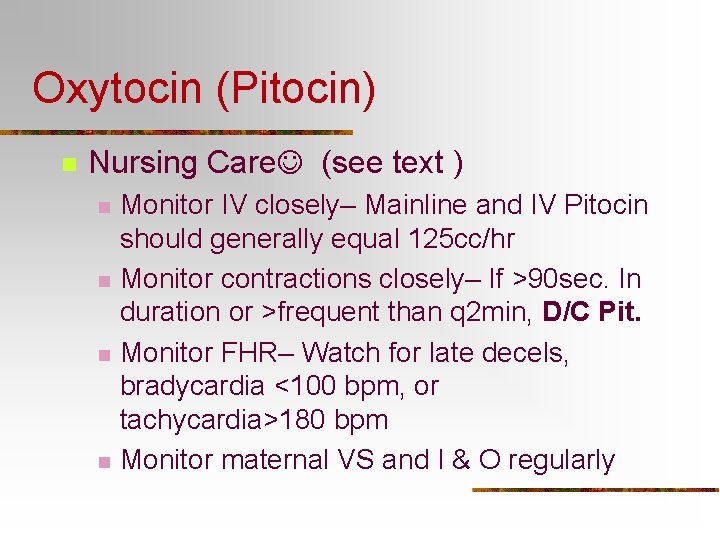
Oxytocin (Pitocin) n Nursing Care (see text ) n n Monitor IV closely– Mainline and IV Pitocin should generally equal 125 cc/hr Monitor contractions closely– If >90 sec. In duration or >frequent than q 2 min, D/C Pit. Monitor FHR– Watch for late decels, bradycardia <100 bpm, or tachycardia>180 bpm Monitor maternal VS and I & O regularly
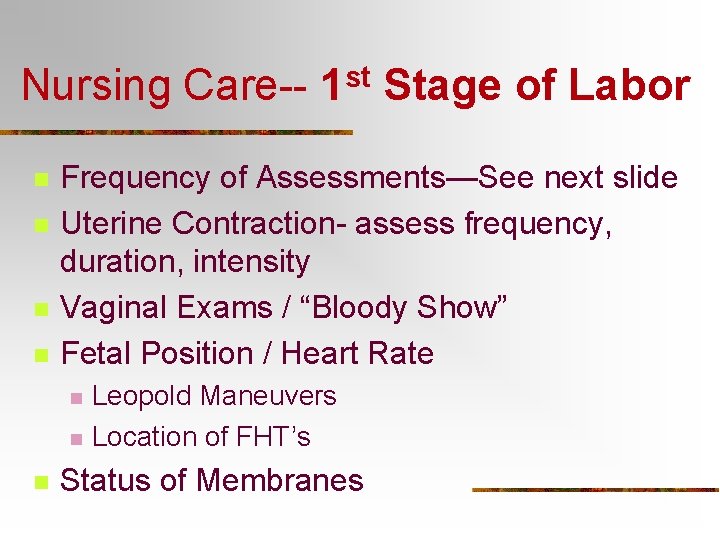
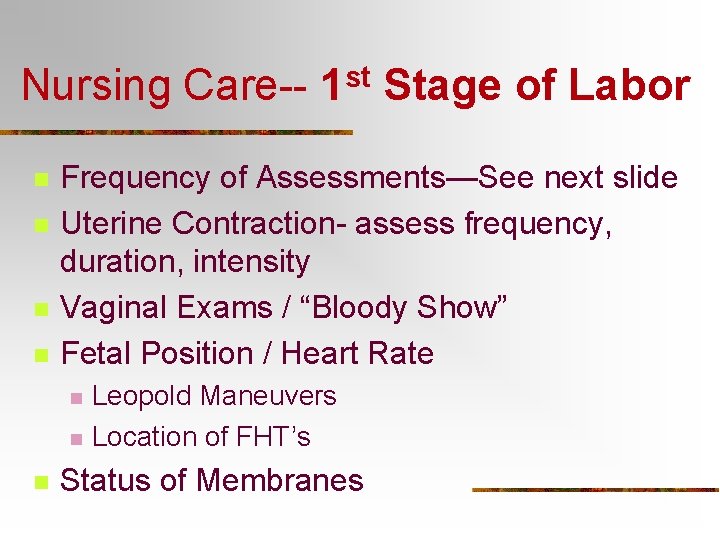
Nursing Care-n n Stage of Labor Frequency of Assessments—See next slide Uterine Contraction- assess frequency, duration, intensity Vaginal Exams / “Bloody Show” Fetal Position / Heart Rate n n n st 1 Leopold Maneuvers Location of FHT’s Status of Membranes
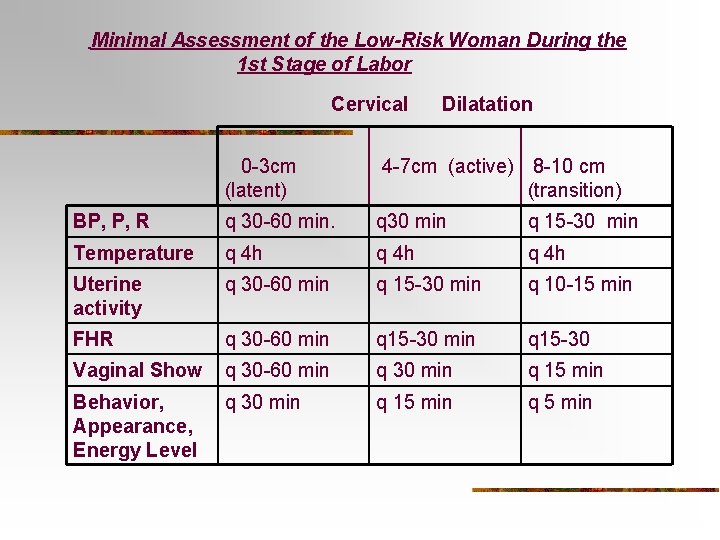
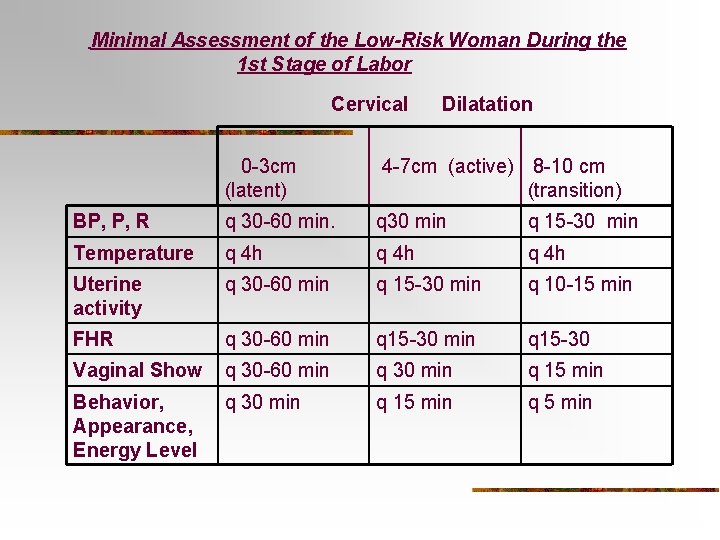
Minimal Assessment of the Low-Risk Woman During the 1 st Stage of Labor Cervical Dilatation 0 -3 cm (latent) 4 -7 cm (active) 8 -10 cm (transition) BP, P, R q 30 -60 min. q 30 min q 15 -30 min Temperature q 4 h Uterine activity q 30 -60 min q 15 -30 min q 10 -15 min FHR q 30 -60 min q 15 -30 Vaginal Show q 30 -60 min q 30 min q 15 min Behavior, Appearance, Energy Level q 30 min q 15 min q 5 min
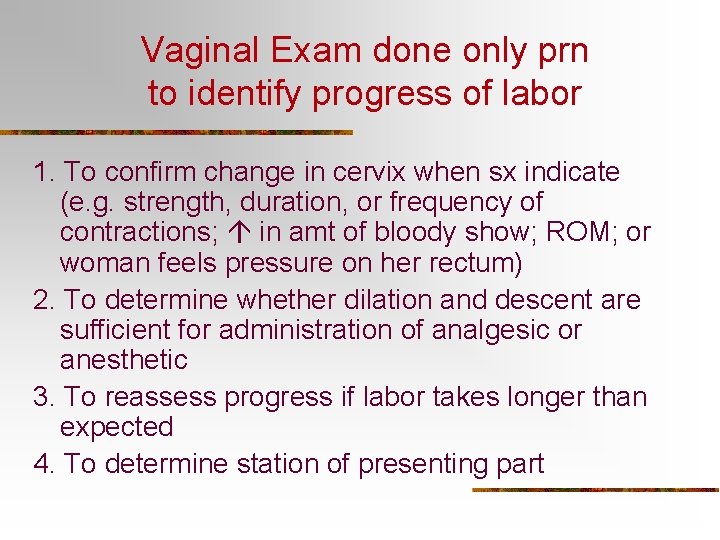
Vaginal Exam done only prn to identify progress of labor 1. To confirm change in cervix when sx indicate (e. g. strength, duration, or frequency of contractions; in amt of bloody show; ROM; or woman feels pressure on her rectum) 2. To determine whether dilation and descent are sufficient for administration of analgesic or anesthetic 3. To reassess progress if labor takes longer than expected 4. To determine station of presenting part
Signs of Transition n n in bloody show Nausea and vomiting Increased rectal pressure Desire to push ability to focus due to intensity and frequency of contractions
Nursing Care / Psychosocial n n n Confidentiality Be Respectful Supportive Care / Include Support Persons Use of Touch Reassurance / Gentle Coaching Modesty
Nursing Care / Physical n Positioning n Hydration n Bladder n Dealing with Contractions
Signs of Potential Complications n n n n Rising Intrauterine Pressures Cntx > 90 sec. Or < 2 minutes apart Fetal bradycardia, tachycardia, decreased variability Meconium-stained, bloody or foul-smelling fluid from vagina Arrested progress of labor Maternal temperature > 38 o C Persistent bright or dark-red vaginal bleeding
Amnioinfusion n Warmed, sterile NS or Ringer’s Lactate infused INTO uterus via Intrauterine Pressure Catheter (IUPC; 250 – 500 cc) Increase Intrauterine Fluid Volume Intrauterine Used to treat Problems related to fetus n n Thick Meconium Decelerations r/t Cord Compression
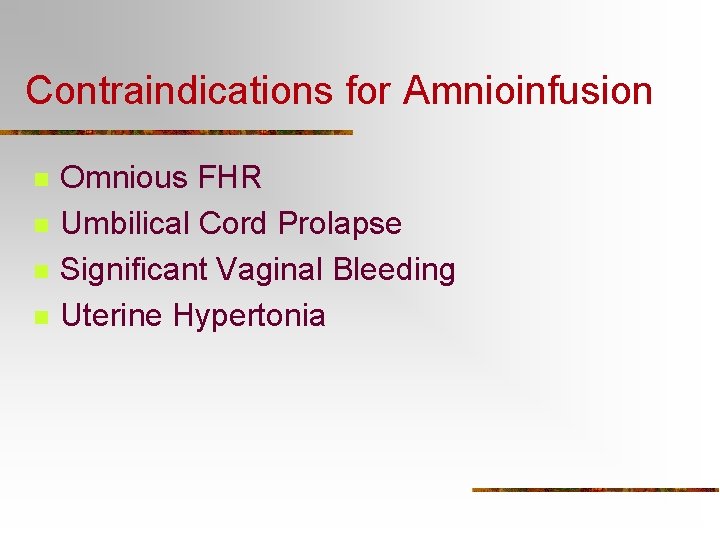
Contraindications for Amnioinfusion n n Omnious FHR Umbilical Cord Prolapse Significant Vaginal Bleeding Uterine Hypertonia
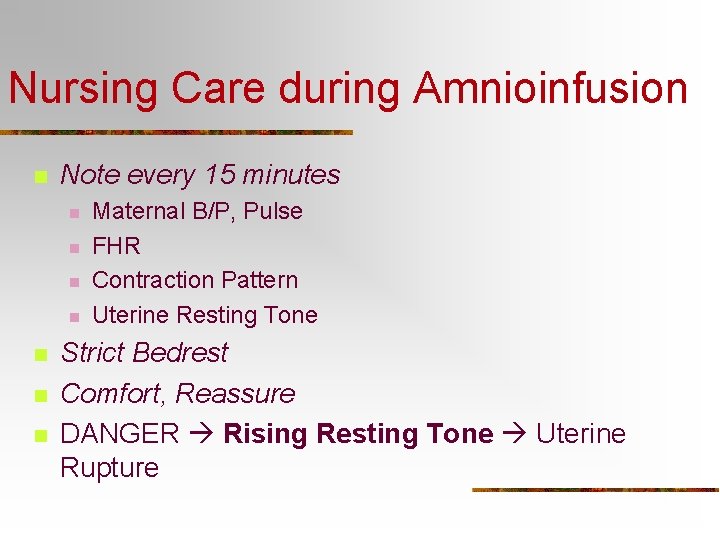
Nursing Care during Amnioinfusion n Note every 15 minutes n n n n Maternal B/P, Pulse FHR Contraction Pattern Uterine Resting Tone Strict Bedrest Comfort, Reassure DANGER Rising Resting Tone Uterine Rupture
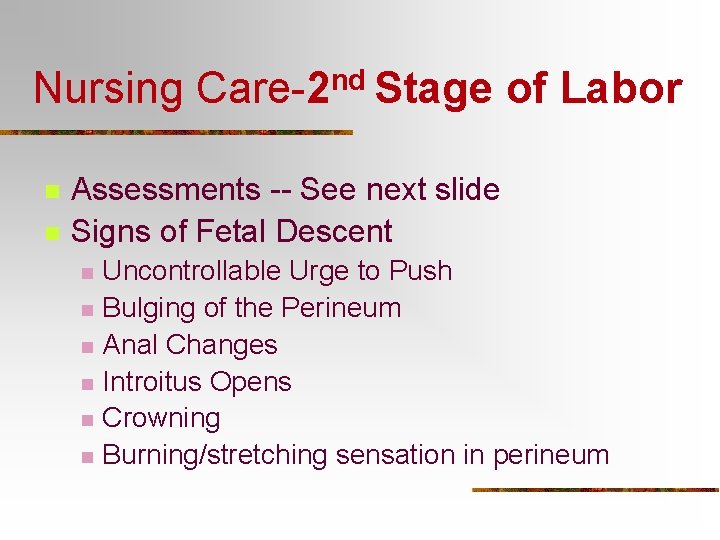
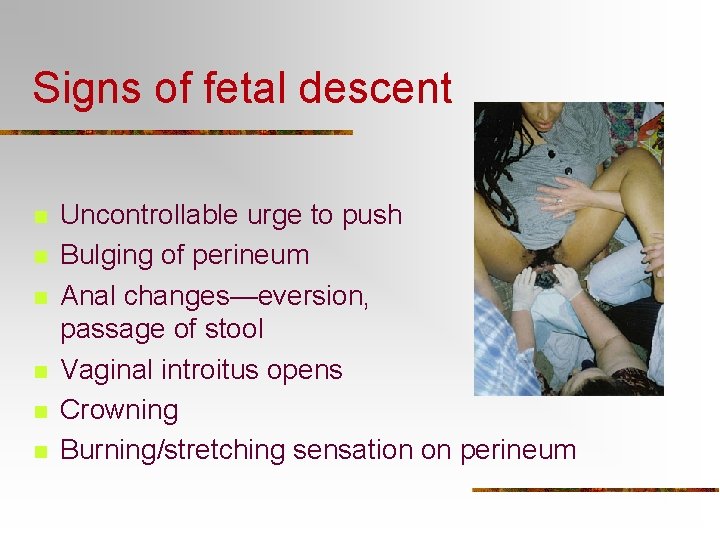
Nursing Care-2 nd Stage of Labor n n Assessments -- See next slide Signs of Fetal Descent n n n Uncontrollable Urge to Push Bulging of the Perineum Anal Changes Introitus Opens Crowning Burning/stretching sensation in perineum
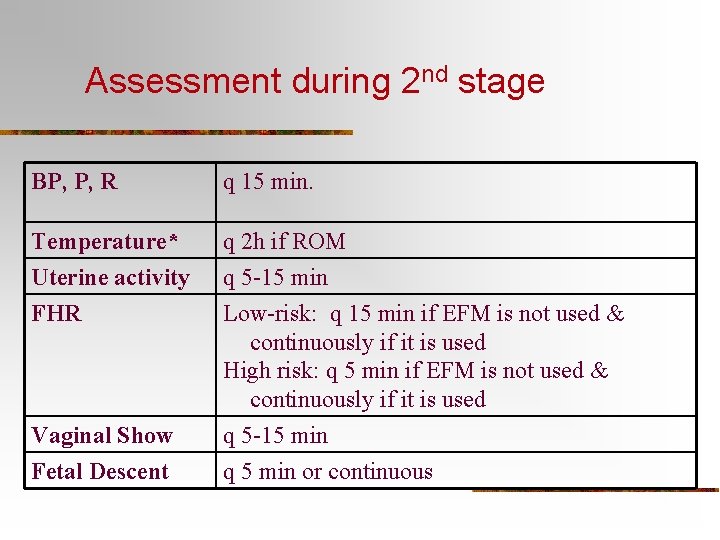
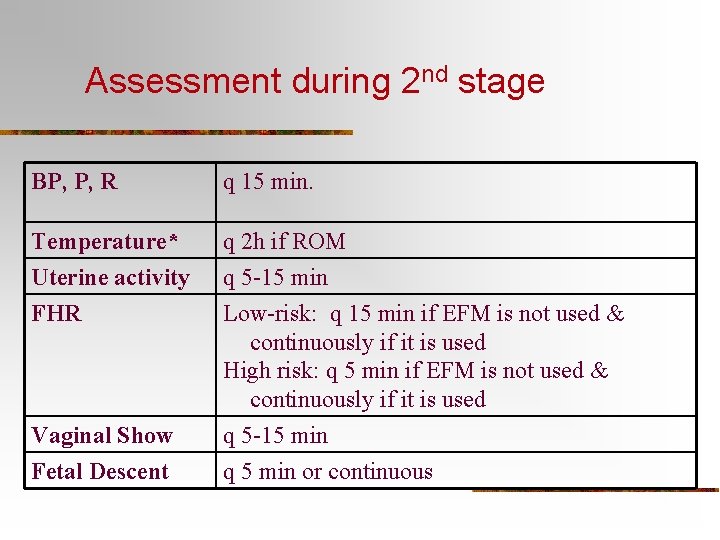
Assessment during 2 nd stage BP, P, R q 15 min. Temperature* Uterine activity FHR q 2 h if ROM q 5 -15 min Low-risk: q 15 min if EFM is not used & continuously if it is used High risk: q 5 min if EFM is not used & continuously if it is used q 5 -15 min q 5 min or continuous Vaginal Show Fetal Descent

Assessment in 2 nd stage (cont’d) Status of bladder especially in women who have an epidural block Behavior, Appearance Energy Level Include assessment of emotional response of woman and partner to 2 nd stage. Continuously
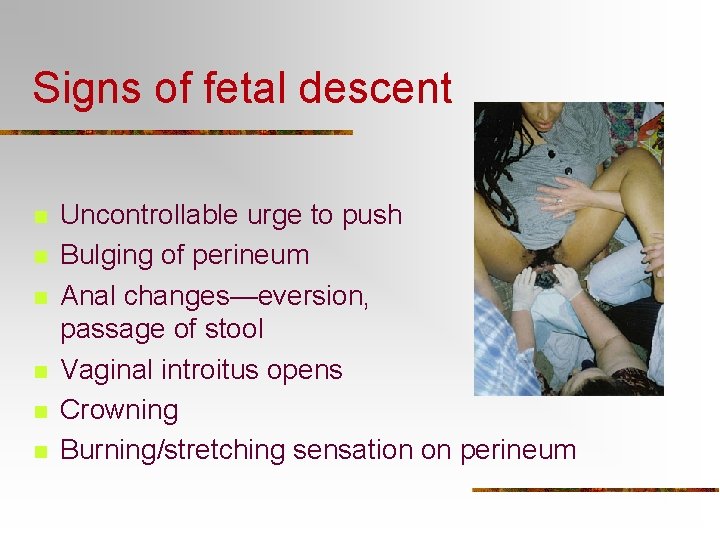
Signs of fetal descent n n n Uncontrollable urge to push Bulging of perineum Anal changes—eversion, passage of stool Vaginal introitus opens Crowning Burning/stretching sensation on perineum
Nursing Care. Psychosocial Assessments n n n Less Irritated VERY focused on work of Birth More Cooperative Doze off between Contractions May be exhausted Little modesty at this point
Nursing Care— Physical/Psychological Support n Positions for Pushing n n n Lithotomy/semi-fowler’s Sim’s/Side-lying Squatting Kneeling Breathing n n n Open glottis~groaning/grunting Prolonged pushing~ O 2 to baby Cleansing breath & deep breath between pushes
Physical/Psychological Support n Environment n n n Quiet between contractions to allow for rest Massage legs if pt c/o of leg cramping Psychological Support n n ENCOURAGE mom through each push 1 person give short, explicit instructions Offer LOTS of praise for effort Keep thinking with the end in mind!
Prepare for Delivery n n n Continue Emotional Support of Mom & S. O. Instrument Table (Tech usually does) Infant Warmer, Resuscitation, ID n n Medical Support for Mom n n O 2, De. Lee & Suction, Meds, Laryngoscope Light, Bulb Syringe, O 2, , Suction, Pitocin “Break Bed” when Doctor is on the way or present
Other Responsibilities n n n Prep/wash perineum Keep a watch on fetal status through each contraction Provide scalp stimulation prn Pour mineral oil in and around perineum to help stretch perineum and need for epis Note type of episiotomy/laceration Note time of delivery
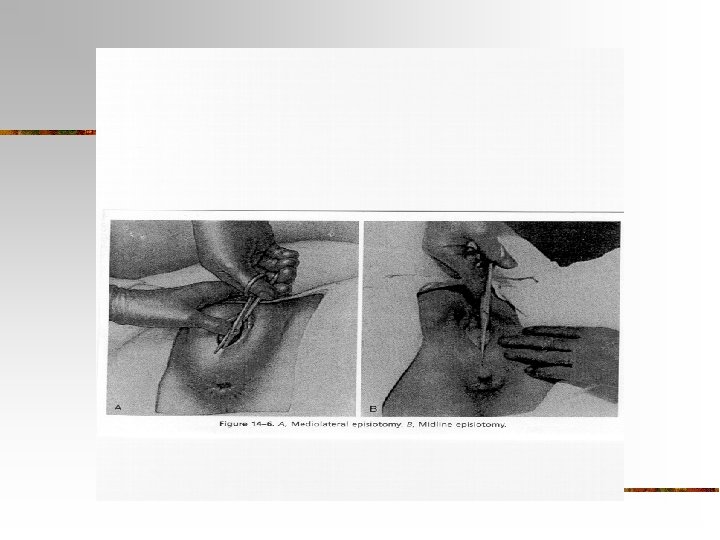
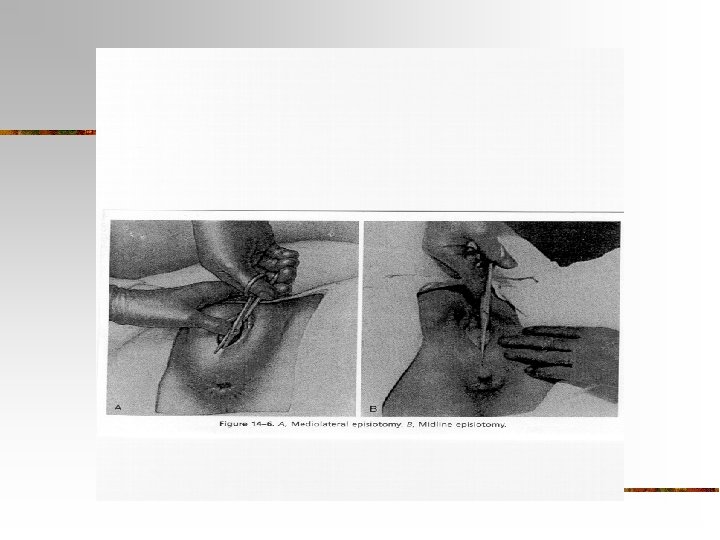
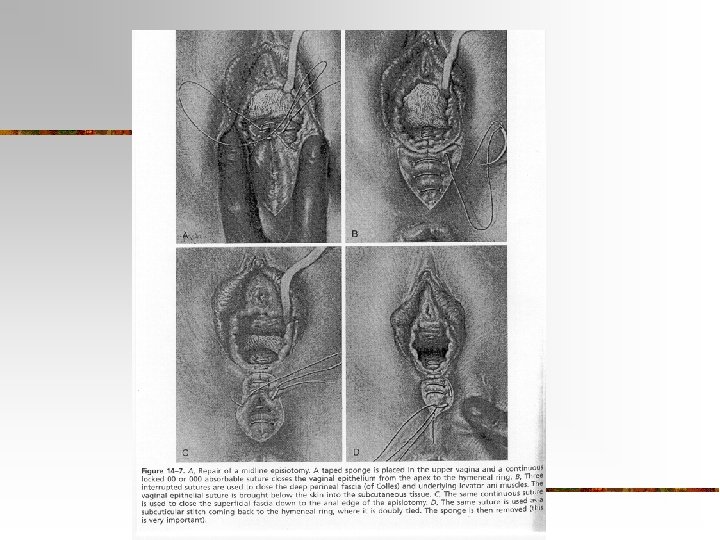
Other Elective Procedures Episiotomies n Definition: surgical incision of the perineum performed more with primiparas than multiparas. A controversial procedure done more by MD’s than CNM’s. Performed just prior to delivery when the presenting part is crowning, usually performed under regional or local anesthesia.
Episiotomies n Mediolateral: start at midline and extend @ a 45 degree angle to the R or L. n Advantage: avoids trauma to rectum, may provide more room n Disadvantage: increased blood loss, longer time to heal, > discomfort during early pp period.
Episiotomies n Midline/median– begins at midline and may extend down the midline through the perineal body. n Advantages: easy to repair, heals with less discomfort for mom n Disadvantage: if episiotomy extends, it may tear through the rectum
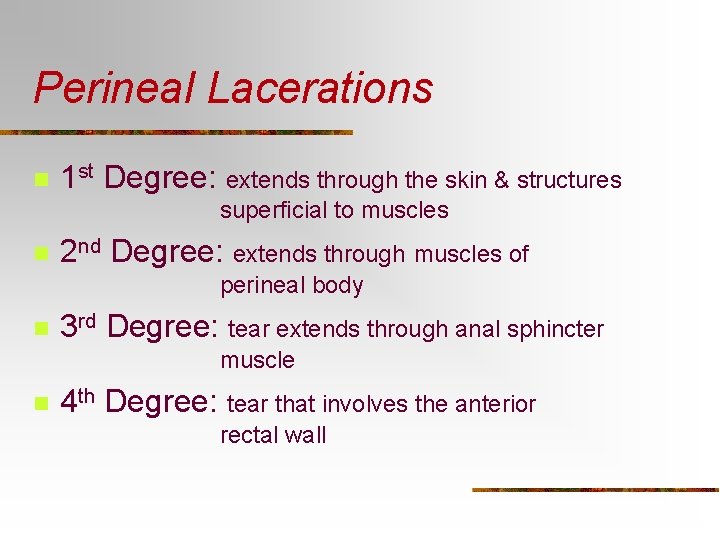
Perineal Lacerations n 1 st Degree: extends through the skin & structures superficial to muscles n 2 nd Degree: extends through muscles of perineal body n 3 rd Degree: tear extends through anal sphincter muscle n 4 th Degree: tear that involves the anterior rectal wall
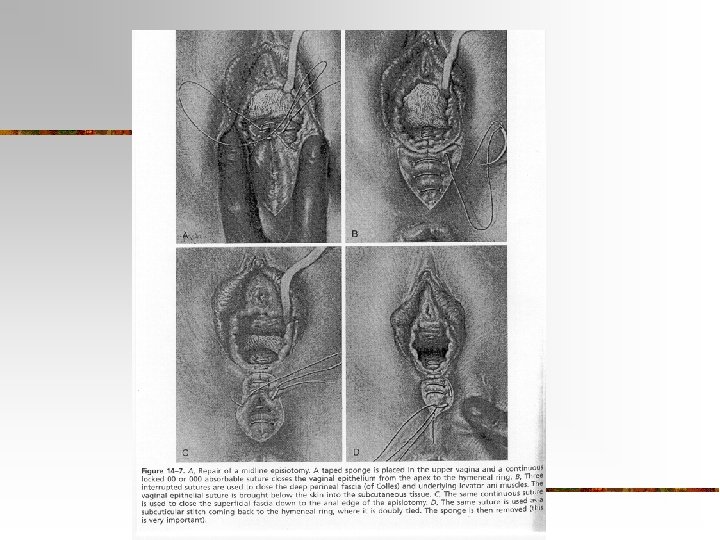
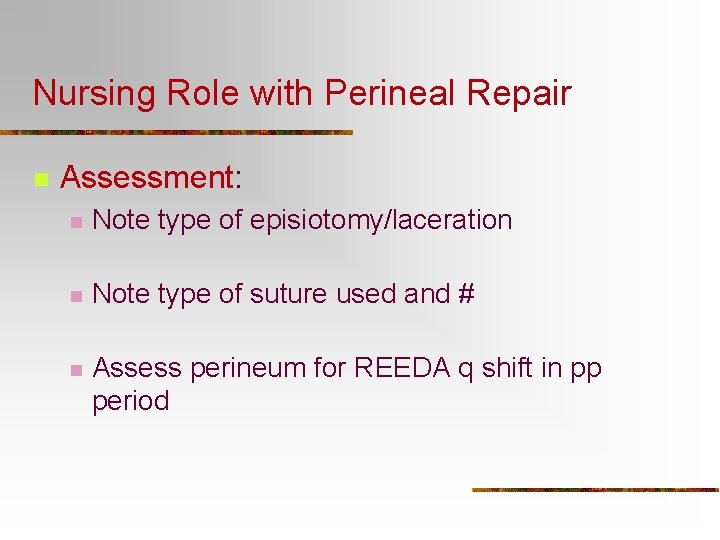
Nursing Role with Perineal Repair n Assessment: n Note type of episiotomy/laceration n Note type of suture used and # n Assess perineum for REEDA q shift in pp period
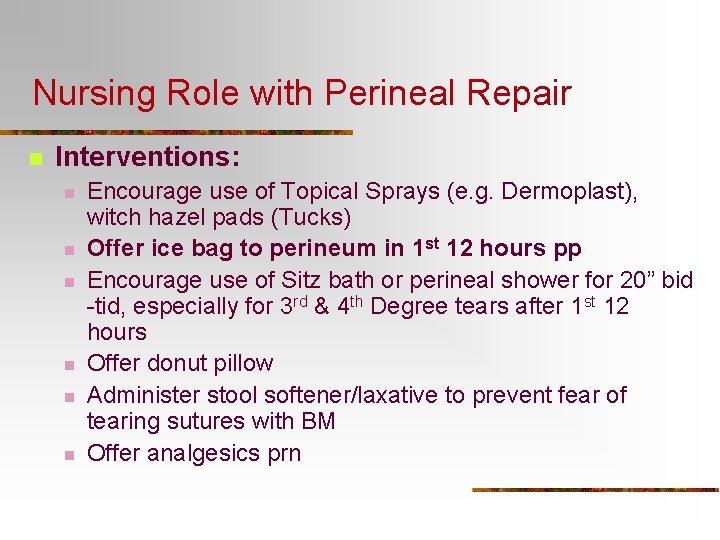
Nursing Role with Perineal Repair n Interventions: n n n Encourage use of Topical Sprays (e. g. Dermoplast), witch hazel pads (Tucks) Offer ice bag to perineum in 1 st 12 hours pp Encourage use of Sitz bath or perineal shower for 20” bid -tid, especially for 3 rd & 4 th Degree tears after 1 st 12 hours Offer donut pillow Administer stool softener/laxative to prevent fear of tearing sutures with BM Offer analgesics prn
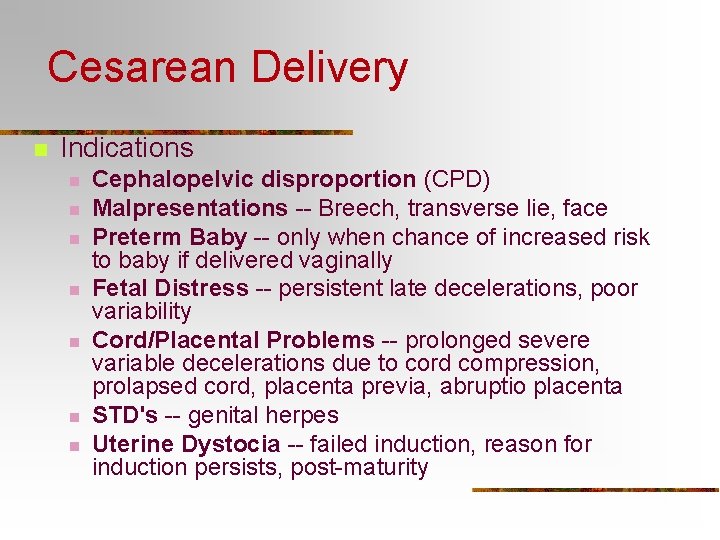
Cesarean Delivery n Indications n n n n Cephalopelvic disproportion (CPD) Malpresentations -- Breech, transverse lie, face Preterm Baby -- only when chance of increased risk to baby if delivered vaginally Fetal Distress -- persistent late decelerations, poor variability Cord/Placental Problems -- prolonged severe variable decelerations due to cord compression, prolapsed cord, placenta previa, abruptio placenta STD's -- genital herpes Uterine Dystocia -- failed induction, reason for induction persists, post-maturity
Pre-op Nursing Care n n n n IV fluids-- Usually warm Lactated Ringer’s (LR) if spinal or epidural anesthesia Labs--UA, CBC, type & crossmatch, Blood Chemistry Consent forms signed Abdominal shave/clip (per dr. order) Foley catheter Keep dad present and involved/allow privacy between couple when time allows Explain all procedures--teach about return of sensation to lower extremities, T, C, & DB & pain management post-op
Pre-op Nursing Care (cont’d) Remove all rings, jewelry, nail polish n Monitor labor status - FHR & contractions, till OR n Always maintain calm attitude n Administer an antacid e. g. Bicitra 30 cc. po approx. 30 min before surgery n Complete all admission hx and physical assessment documentation n
Cesarean Section n Skin Incisions Uterine Incisions Nursing Care During C/Section n Reassure Mom during anesthesia induction. Assess S. O. Coping Care for Baby Immediately after Birth
Forceps n n web link on forceps and suction Function: to provide traction, to rotate, or both in the second stage of labor Midforceps: when fetal head is at the level of the ischial spines but above the +2 station (Rarely used) Outlet forceps: when the fetal head is visible on the perineum without spreading the labia apart. They shorten the length of 2 nd stage. Requirements forceps: Cx dilated 10 cm, bladder empty, presenting part 0 station, vertex presentation, membranes ruptured.
Vacuum Extractor n n A suction cap applied to fetal head traction is applied to facilitate fetal descent in 2 nd stage of labor Risks to fetus: cephalhematoma, scalp lacerations, subdural hematoma Risks to mom: perineal, vaginal, or cervical lacerations Requirements for vacuum: Cx dilated 10 cm, bladder empty, presenting part 0 station, vertex presentation, membranes ruptured.
Indications for Forceps or Vacuum n n Prolonged second stage Maternal condition precludes pushing: n n Fetal Distress– n n Heart disease, Pulmonary Edema Exhaustion Spinal, Epidural, Caudal Anesthesia– no sensation to effectively push late decels, poor variability. Bradycardia <100 for more that 2 -3 minutes Threat to mother’s life
Immediate nursing actions n n Unwrap sterile packages and place onto sterile field or in sterile basin with betadine Assess maternal/fetal status Teach mom that she may feel increased pressure internally in vagina. Coach mom through contractions to effectively push with traction by forceps of vacuum extractor
Nursing Actions after Delivery with Forceps or Vacuum n n Check for sx of trauma to face, head, neck of baby, lacerations or forceps face marks in eye area Check for increased ICP, lethargy, seizures, paralysis (facial nerve palsy) Answer parents’ questions about possible trauma to their infant Check mother for pp hemorrhage, vaginal or labial hematoma
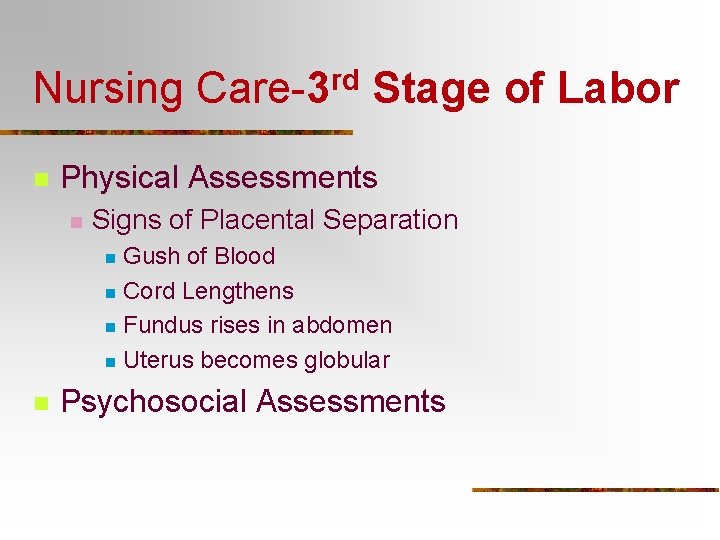
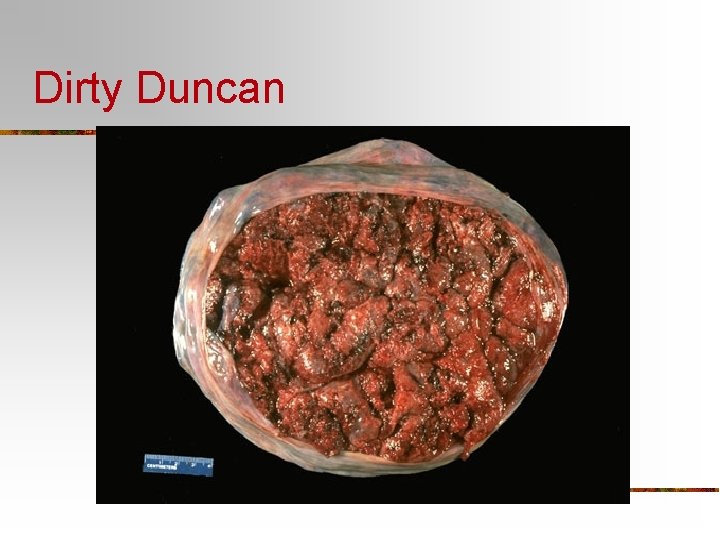
Nursing Care-3 rd Stage of Labor n Physical Assessments n Signs of Placental Separation Gush of Blood n Cord Lengthens n Fundus rises in abdomen n Uterus becomes globular n n Psychosocial Assessments
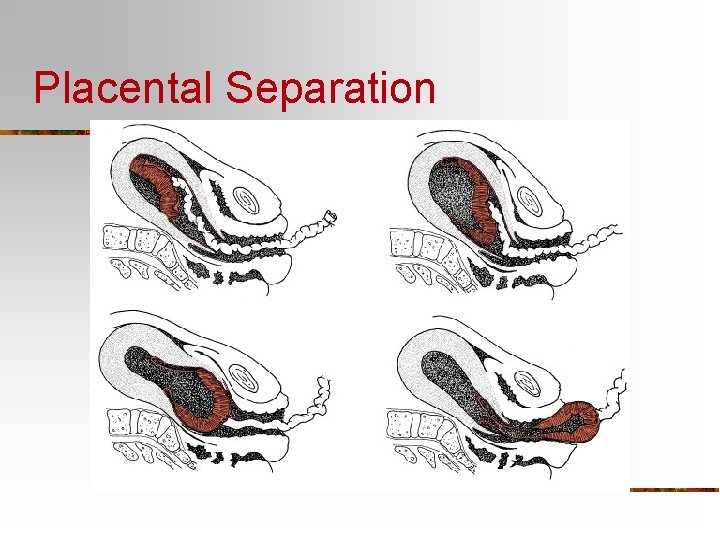
Placental Separation
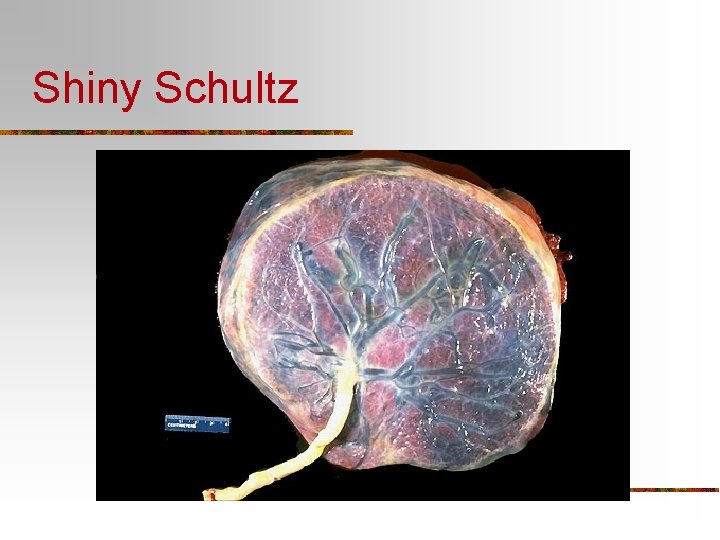
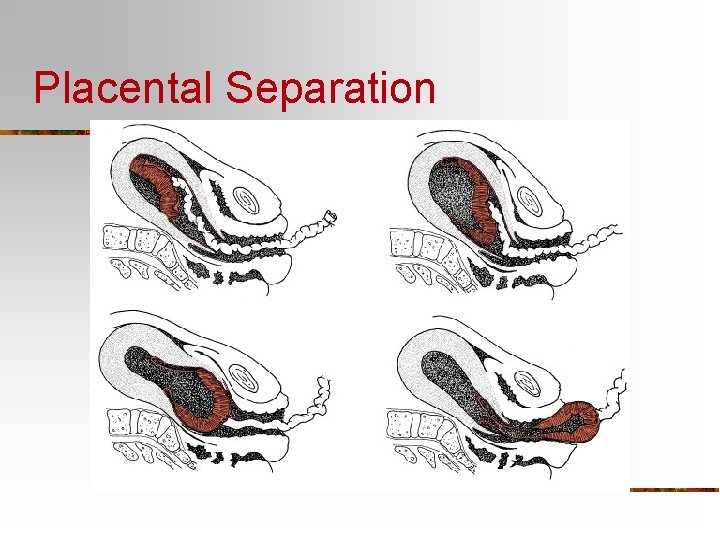
Shiny Schultz
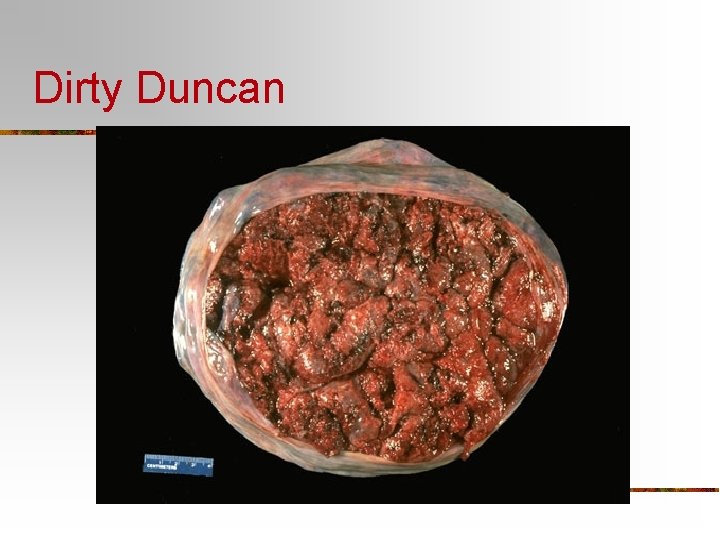
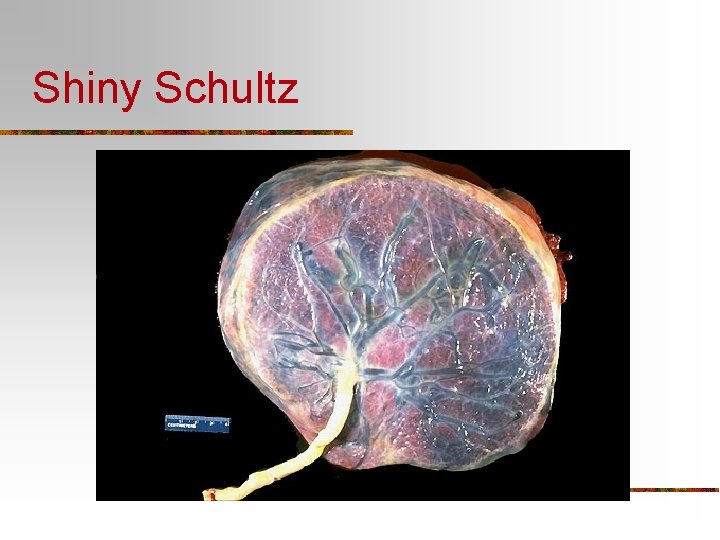
Dirty Duncan
Nursing Care— 3 rd Stage of Labor n Care of Mother – Physical n n n Encourage her to push AFTER placenta separates Note time of Placental Expulsion Add Pitocin to IV or Open Pitocin Drip CHECK FUNDUS Note how epis. Repair is going Care of Mother – Emotional
Nursing Care – 3 rd Stage of Labor n n n Care of Newborn Care after Episiotomy Repair During C/Section n Note time of Placental Separation Emotional Support to Mom and S. O. ESTIMATE BLOOD LOSS
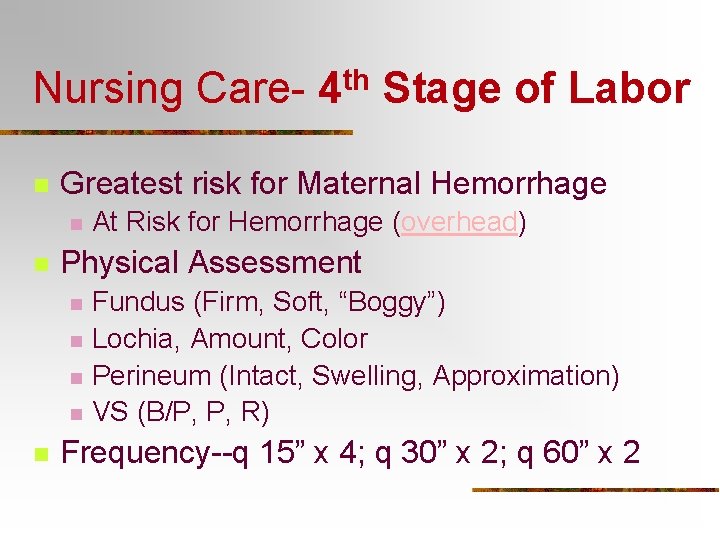
Nursing Care- 4 th Stage of Labor n Greatest risk for Maternal Hemorrhage n n Physical Assessment n n n At Risk for Hemorrhage (overhead) Fundus (Firm, Soft, “Boggy”) Lochia, Amount, Color Perineum (Intact, Swelling, Approximation) VS (B/P, P, R) Frequency--q 15” x 4; q 30” x 2; q 60” x 2
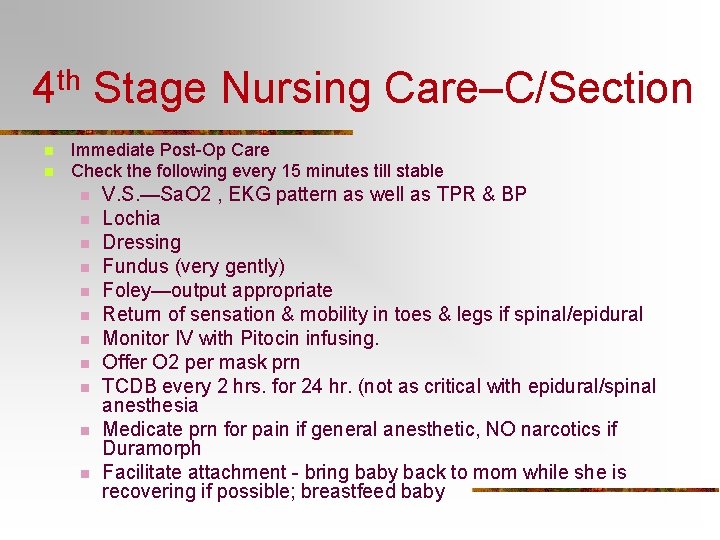
4 th Stage Nursing Care–C/Section n n Immediate Post-Op Care Check the following every 15 minutes till stable n n n V. S. —Sa. O 2 , EKG pattern as well as TPR & BP Lochia Dressing Fundus (very gently) Foley—output appropriate Return of sensation & mobility in toes & legs if spinal/epidural Monitor IV with Pitocin infusing. Offer O 2 per mask prn TCDB every 2 hrs. for 24 hr. (not as critical with epidural/spinal anesthesia Medicate prn for pain if general anesthetic, NO narcotics if Duramorph Facilitate attachment - bring baby back to mom while she is recovering if possible; breastfeed baby
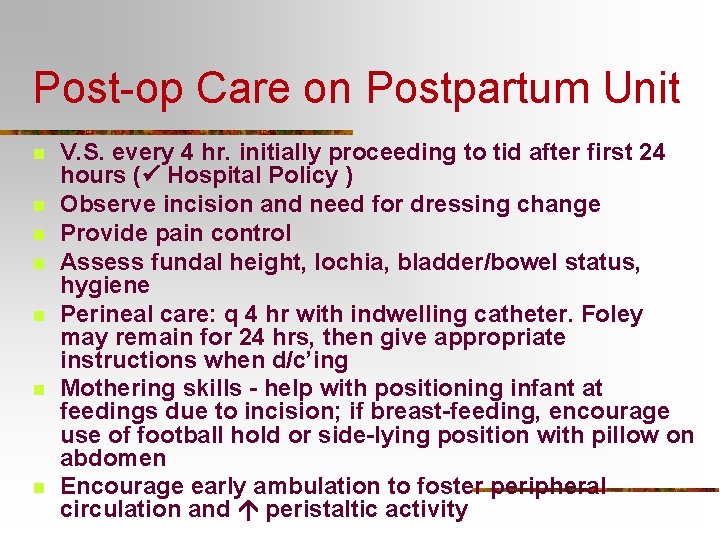
Post-op Care on Postpartum Unit n n n n V. S. every 4 hr. initially proceeding to tid after first 24 hours ( Hospital Policy ) Observe incision and need for dressing change Provide pain control Assess fundal height, lochia, bladder/bowel status, hygiene Perineal care: q 4 hr with indwelling catheter. Foley may remain for 24 hrs, then give appropriate instructions when d/c’ing Mothering skills - help with positioning infant at feedings due to incision; if breast-feeding, encourage use of football hold or side-lying position with pillow on abdomen Encourage early ambulation to foster peripheral circulation and peristaltic activity
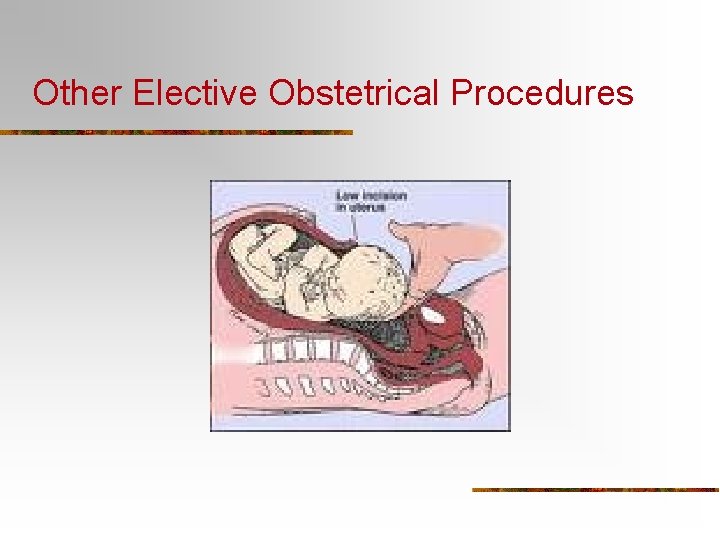
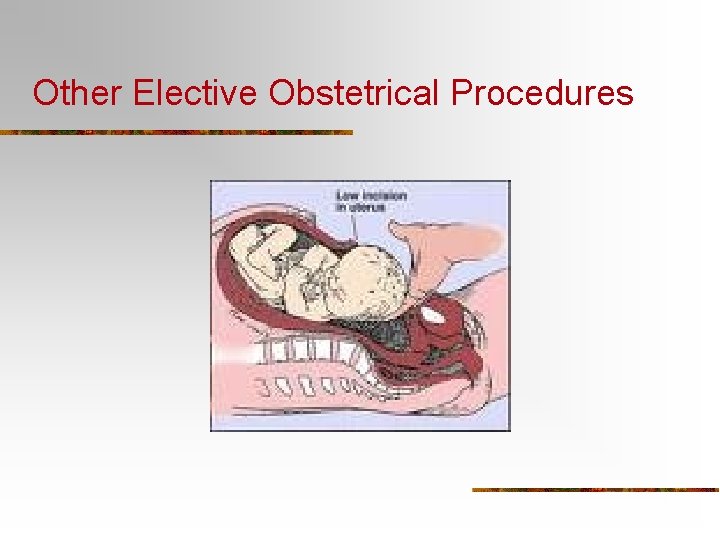
Other Elective Obstetrical Procedures
External Cephalic Version n n Definition: The alteration of fetal position by abdominal or intrauterine manipulation to accomplish a more favorable fetal position for vaginal delivery. Indications: n n n Presenting part NOT engaged Maternal abdominal wall thin enough to permit good palpation NO uterine irritability or contractions Adequate amniotic fluid, intact membranes NO known history of CPD
Version– Nursing Interventions n n n Get consent for procedure and inform of possible emergency C/S Prepare for ultrasound to confirm fetal position Close monitoring of fetus via fetal monitoring, NST Follow MD orders if tocolytic ordered to relax uterus Nurse may need to assist to head down position by applying pressure over fetal head (pubic area) to encourage fetus to stay in cephalic presentation. Monitor maternal status for possible hemorrhage & discomfort after procedure
Precipitous Delivery n n Definition = Labor < 3 hours Assessment n Vaginal Exam/Visualization
Precipitous Delivery-Nursing Care n n n n Don’t Break the Bed Support Perineum, Deliver Fetal Head Check for Nuchal Cord Delivery Actions Suction Baby’s mouth & nose Clamp Cord, Wait for Placenta to come out Dry Baby, Place on Mother’s Abdomen
Care -- Out-of Hospital Delivery n n Follow Precipitous Labor Actions Try to be as clean as possible Essential to protect infant from HEAT LOSS (blankets, coats, newspaper) BE CALM & CONFIDENT

THAT’S ALL FOLKS! n Be sure to review Handout “A” “Cultural Influences During Intrapartum Period” as well!