PLACENTAL DISORDERS Kristine Glory MendilloEstanislao RN Kristine Glory
![Risk Factors ◦ Smoking during pregnancy; [1] cocaine use during pregnancy[9][10] ◦ Women who Risk Factors ◦ Smoking during pregnancy; [1] cocaine use during pregnancy[9][10] ◦ Women who](https://slidetodoc.com/presentation_image_h2/53a174a9e3d78155abede5ec38b73df0/image-8.jpg)
![Fetal Complications ◦ IUGR (15% incidence)[5] ◦ Premature delivery ◦ Death Fetal Complications ◦ IUGR (15% incidence)[5] ◦ Premature delivery ◦ Death](https://slidetodoc.com/presentation_image_h2/53a174a9e3d78155abede5ec38b73df0/image-13.jpg)
- Slides: 25
PLACENTAL DISORDERS Kristine Glory Mendillo-Estanislao, RN Kristine Glory DR. Mendillo, RN
How to make a healthy baby?
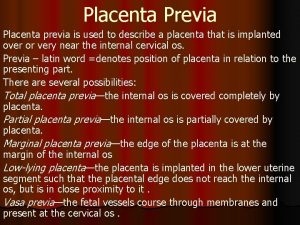
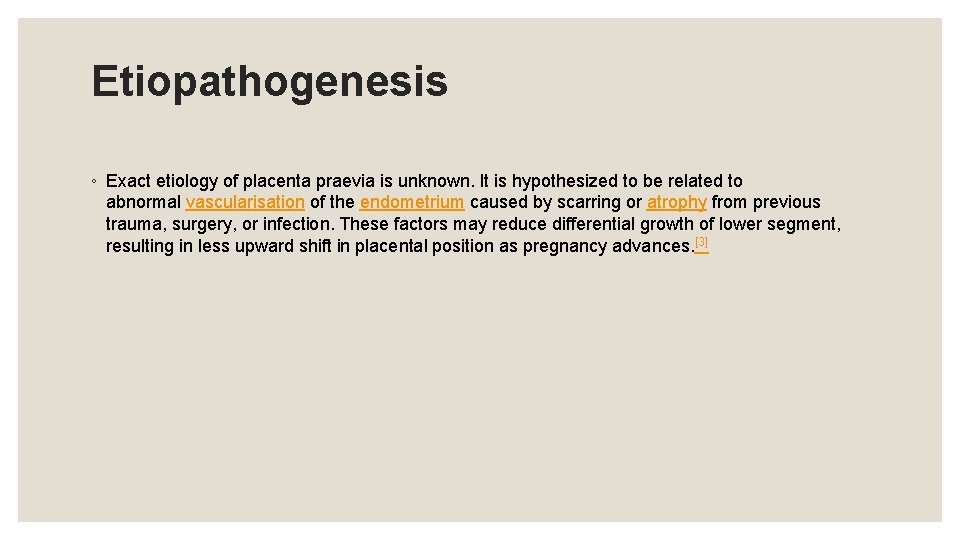
What is placenta previa? ◦ Placenta praevia (placenta previa AE) is an obstetric complication in which the placenta is inserted partially or wholly in lower uterine segment. [1]It can sometimes occur in the later part of the first trimester, but usually during the second or third. It is a leading cause of antepartum haemorrhage(vaginal bleeding). It affects approximately 0. 4 -0. 5% of all labours. [2]
What is placenta previa? ◦ In the last trimester of pregnancy the isthmus of the uterus unfolds and forms the lower segment. In a normal pregnancy the placenta does not overlie. If the placenta does overlie the lower segment, as is the case with placenta praevia, it may shear off and a small section may bleed.
Etiopathogenesis ◦ Exact etiology of placenta praevia is unknown. It is hypothesized to be related to abnormal vascularisation of the endometrium caused by scarring or atrophy from previous trauma, surgery, or infection. These factors may reduce differential growth of lower segment, resulting in less upward shift in placental position as pregnancy advances. [3]
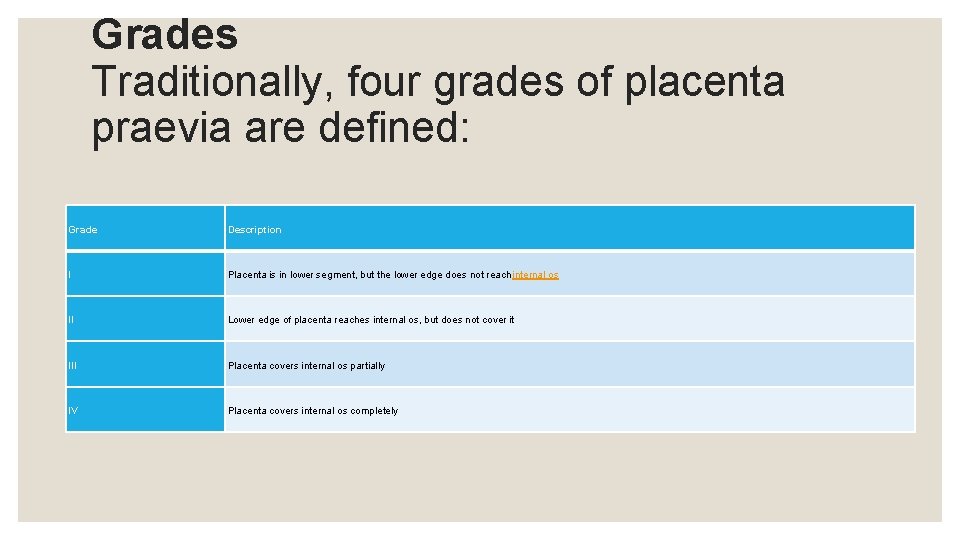
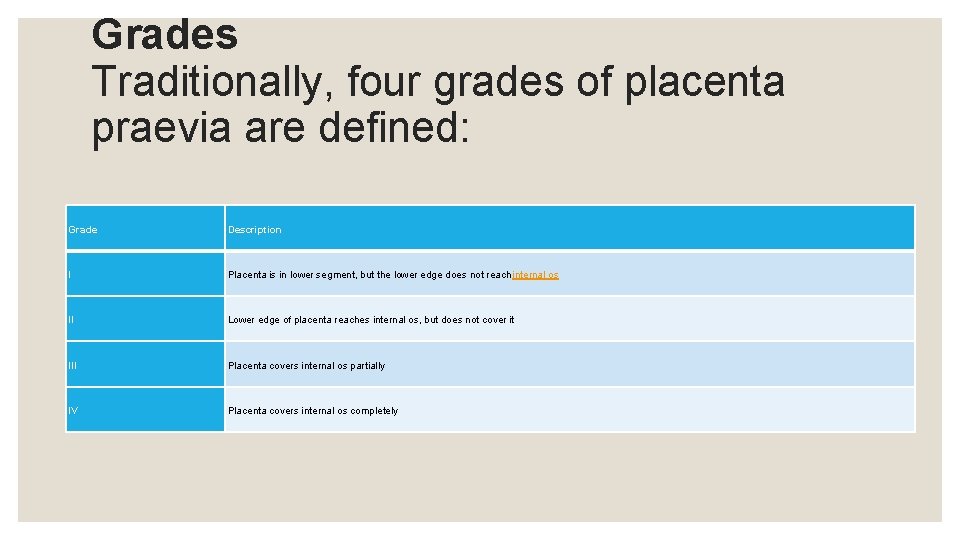
Grades Traditionally, four grades of placenta praevia are defined: Grade Description I Placenta is in lower segment, but the lower edge does not reach internal os II Lower edge of placenta reaches internal os, but does not cover it III Placenta covers internal os partially IV Placenta covers internal os completely
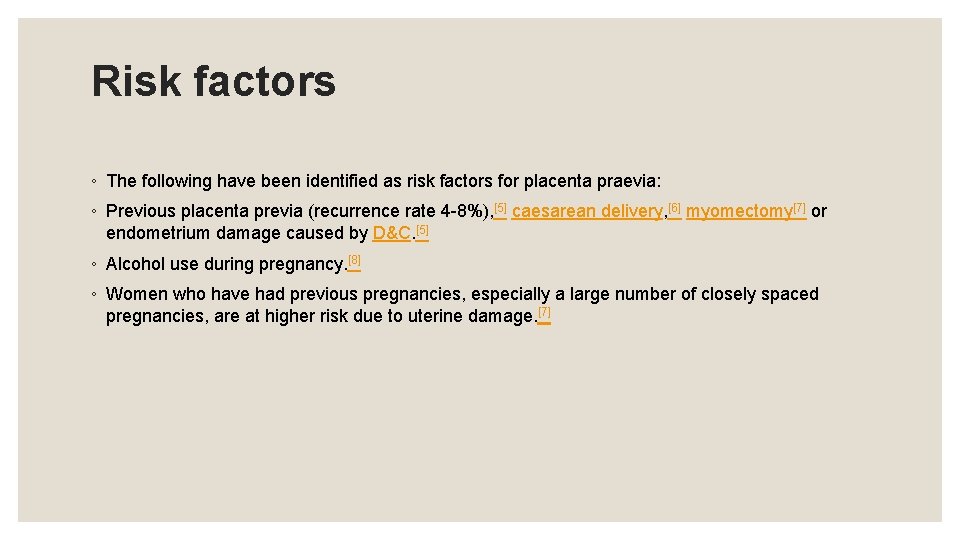
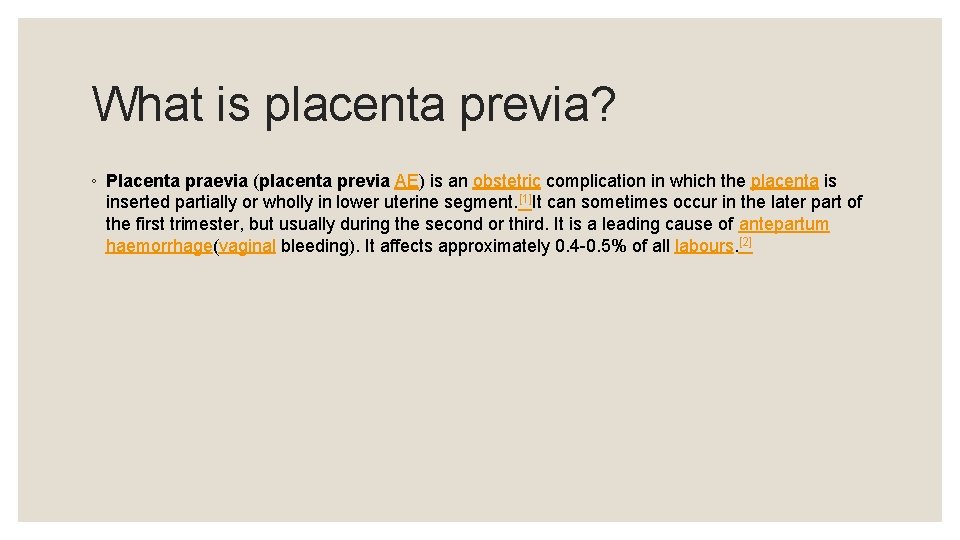
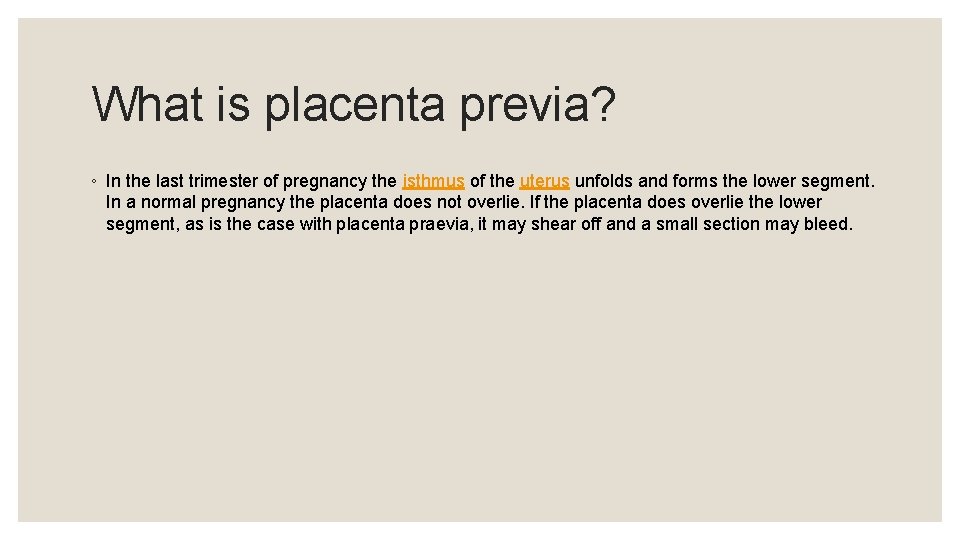
Risk factors ◦ The following have been identified as risk factors for placenta praevia: ◦ Previous placenta previa (recurrence rate 4 -8%), [5] caesarean delivery, [6] myomectomy[7] or endometrium damage caused by D&C. [5] ◦ Alcohol use during pregnancy. [8] ◦ Women who have had previous pregnancies, especially a large number of closely spaced pregnancies, are at higher risk due to uterine damage. [7]
![Risk Factors Smoking during pregnancy 1 cocaine use during pregnancy910 Women who Risk Factors ◦ Smoking during pregnancy; [1] cocaine use during pregnancy[9][10] ◦ Women who](https://slidetodoc.com/presentation_image_h2/53a174a9e3d78155abede5ec38b73df0/image-8.jpg)
Risk Factors ◦ Smoking during pregnancy; [1] cocaine use during pregnancy[9][10] ◦ Women who are younger than 20 are at higher risk and women older than 35 are at increasing risk as they get older. ◦ Women with a large placentae from twins or erythroblastosis are at higher risk. ◦ Race is a controversial risk factor, with some studies finding that people from Asia and Africa are at higher risk and others finding no difference. ◦ Placental pathology (Vellamentous insertion, succinturiate lobes, bipartite i. e. bilobed placenta etc. )[5]
Management ◦ An initial assessment to determine the status of the mother and fetus is required. Although mothers used to be treated in the hospital from the first bleeding episode until birth, it is now considered safe to treat placenta praevia on an outpatient basis if the fetus is at less than 30 weeks of gestation, and neither the mother nor the fetus are in distress. Immediate delivery of the fetus may be indicated if the fetus is mature or if the fetus or mother are in distress. ◦ Blood volume replacement (to maintain blood pressure) and blood plasma replacement (to maintain fibrinogen levels) may be necessary
Mode of delivery ◦ The mode of delivery is determined by clinical state of the mother, fetus and ultrasound findings. In minor degrees (traditional grade I and II), vaginal delivery is possible. RCOG recommends that placenta should be at least 2 cm away from internal os for an attempted vaginal delivery. [19] ◦ When a vaginal delivery is attempted, consultant obstetrician and anesthetists are present in delivery suite. In cases of fetal distress and major degrees (traditional grade III and IV) a caesarean section is indicated. 20]
Mode of delivery ◦ Caesarian section is contraindicated in cases of disseminated intravascular coagulation. Obstetrician may need to divide the anterior lying placenta. In such cases, blood loss is expected to be high and thus blood and blood products are always kept ready. In rare cases, hysterectomy may be required. [
Complications ◦ Antepartum hemorrhage ◦ Malpresentation ◦ Abnormal placentation ◦ Postpartum hemorrhage ◦ Placenta praevia increases the risk of puerperal sepsis and postpartum haemorrhage because the lower segment to which the placenta was attached contracts less well post-delivery.
![Fetal Complications IUGR 15 incidence5 Premature delivery Death Fetal Complications ◦ IUGR (15% incidence)[5] ◦ Premature delivery ◦ Death](https://slidetodoc.com/presentation_image_h2/53a174a9e3d78155abede5ec38b73df0/image-13.jpg)
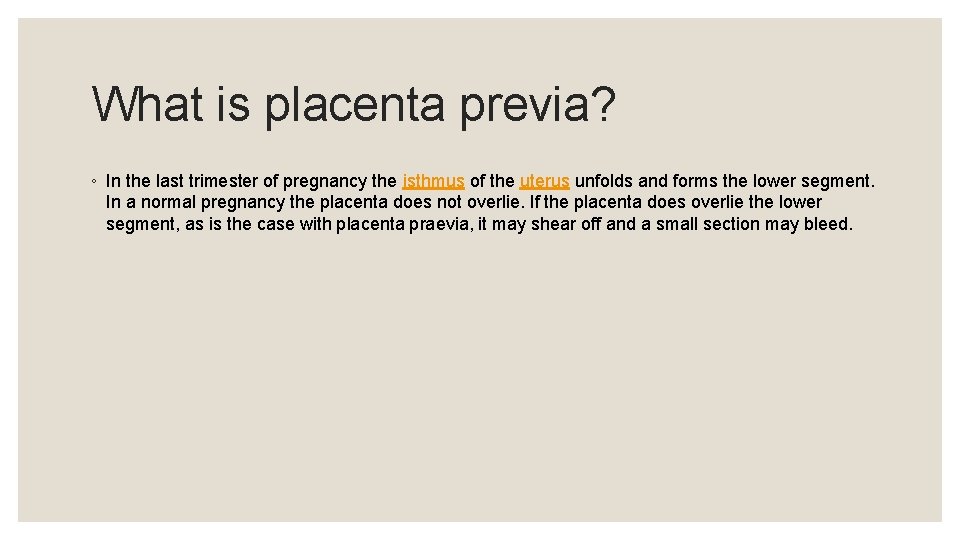
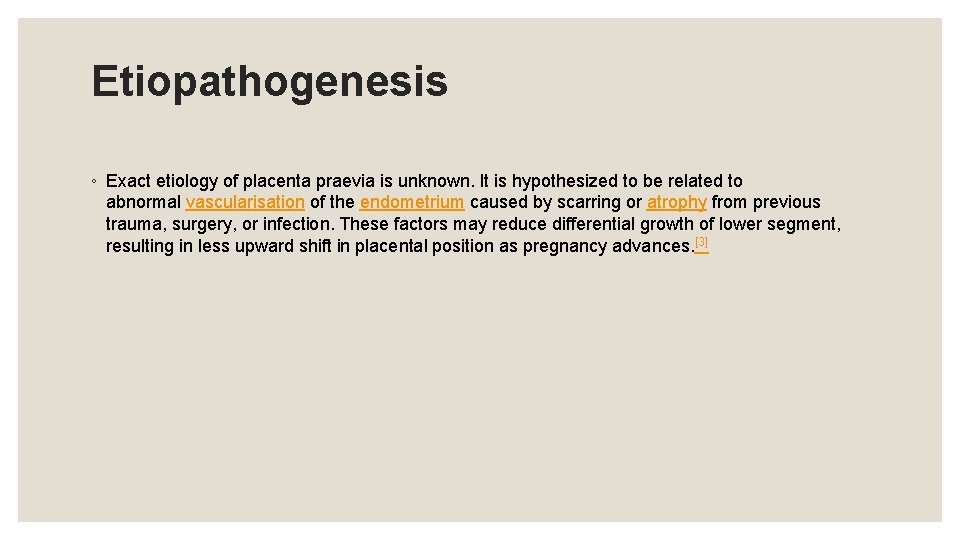
Fetal Complications ◦ IUGR (15% incidence)[5] ◦ Premature delivery ◦ Death
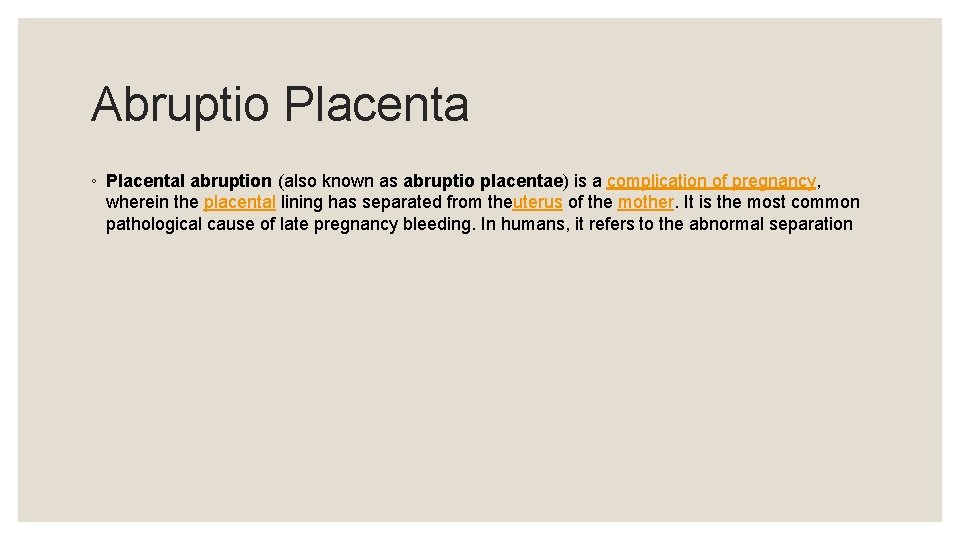
Abruptio Placenta
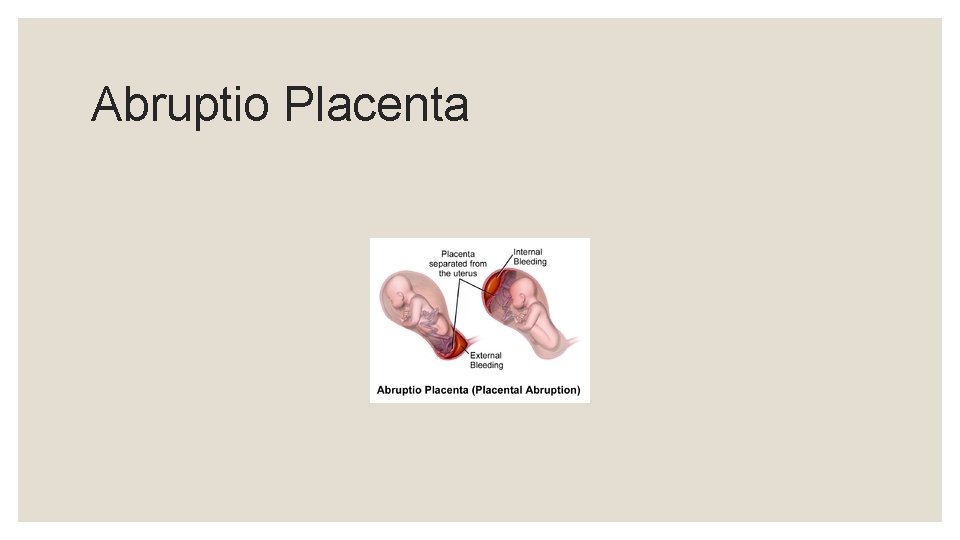
Abruptio Placenta ◦ Placental abruption (also known as abruptio placentae) is a complication of pregnancy, wherein the placental lining has separated from theuterus of the mother. It is the most common pathological cause of late pregnancy bleeding. In humans, it refers to the abnormal separation
Abruptio Placenta ◦ after 20 weeks of gestation and prior to birth. It occurs in 1% of pregnancies worldwide. Placental abruption is a significant contributor to maternal mortality worldwide; early and skilled medical intervention is needed to ensure a good outcome, and this is not available in many parts of the world. Treatment depends on how serious the abruption is and how far along the woman is in her pregnancy. [1]
Lasting effects on the mother ◦ A large loss of blood or hemorrhage may require blood transfusions and intensive care after delivery. 'APH weakens for PPH to kill'. ◦ The uterus may not contract properly after delivery so the mother may need medication to help her uterus contract. ◦ The mother may have problems with blood clotting for a few days. ◦ If the mother's blood does not clot (particularly during a caesarean section) and too many transfusions could put the mother into disseminated intravascular coagulation (DIC) due to increased thromboplastin, the doctor may consider a hysterectomy
Lasting effects on the mother ◦ A severe case of shock may affect other organs, such as the liver, kidney, and pituitary gland. Diffuse cortical necrosis in the kidney is a serious and often fatal complication. ◦ In some cases where the abruption is high up in the uterus, or is slight, there is no bleeding, though extreme pain is felt and reported.
Lasting effects on the fetus ◦ If a large amount of the placenta separates from the uterus, the baby will probably be in distress until delivery and may die in utero, thus resulting in a stillbirth. ◦ The baby may be premature and need to be placed in the newborn intensive care unit. He or she might have problems with breathing and feeding. ◦ If the baby is in distress in the uterus, he or she may have a low level of oxygen in the blood after birth. ◦ The newborn may have low blood pressure or a low blood count.
Lasting effects on the fetus ◦ If the separation is severe enough, the baby could suffer brain damage or die before or shortly after birth. ◦ The newborn may have learning issues at later development stages, often requiring professional pedagogical aid.
Symptoms ◦ contractions that don't stop (and may follow one another so rapidly as to seem continuous) ◦ pain in the uterus ◦ tenderness in the abdomen ◦ vaginal bleeding (sometimes) ◦ uterus may be disproportionately enlarged ◦ pallor
Clinical Manifestation ◦ Class 0: asymptomatic. Diagnosis is made retrospectively by finding an organized blood clot or a depressed area on a delivered placenta.
Clinical Manifestation ◦ Class 1: mild and represents approximately 48% of all cases. Characteristics include the following: ◦ ◦ ◦ No vaginal bleeding to mild vaginal bleeding Slightly tender uterus Normal maternal BP and heart rate No coagulopathy No fetal distress
Clinical Manifestation ◦ Class 2: moderate and represents approximately 27% of all cases. Characteristics include the following: ◦ ◦ ◦ No vaginal bleeding to moderate vaginal bleeding Moderate-to-severe uterine tenderness with possible tetanic contractions Maternal tachycardia with orthostatic changes in BP and heart rate Fetal distress Hypofibrinogenemia (i. e. , 50– 250 mg/d. L)
Clinical Manifestation ◦ Class 3: severe and represents approximately 24% of all cases. Characteristics include the following: ◦ ◦ ◦ No vaginal bleeding to heavy vaginal bleeding Very painful tetanic uterus Maternal shock Hypofibrinogenemia (i. e. , <150 mg/d. L) Coagulopathy Fetal death
 榮耀神羔羊
榮耀神羔羊 Glory glory how the angels sing
Glory glory how the angels sing All god's children singing glory glory
All god's children singing glory glory 493 sda hymnal
493 sda hymnal Holy holy holy lord god almighty
Holy holy holy lord god almighty Placental examination
Placental examination Mathew duncan method of placental separation
Mathew duncan method of placental separation Amnion
Amnion Fetal circulation flow chart
Fetal circulation flow chart Placental cotyledons
Placental cotyledons Placental
Placental Parturition
Parturition Kleihauer-betke test
Kleihauer-betke test Placental circulation flow chart
Placental circulation flow chart Dr june carroll
Dr june carroll Upper uterine segment
Upper uterine segment Placenta mosaicism
Placenta mosaicism Lower uterine segment
Lower uterine segment Stages of labor
Stages of labor Placenta prvia
Placenta prvia Placental bulge
Placental bulge Characteristics of placental mammals
Characteristics of placental mammals Kristīne madelāne
Kristīne madelāne Kristine kopperud timberlid
Kristine kopperud timberlid Apocalypse herbal incense
Apocalypse herbal incense Aplastic anemia
Aplastic anemia