MANAGEMENT OF CHRONIC HEART FAILURE Congestive Cardiac Failure
- Slides: 54
MANAGEMENT OF CHRONIC HEART FAILURE (Congestive Cardiac Failure) 1
Heart Failure: Definition • is an inability of the heart to maintain a cardiac output sufficient to meet the requirements of the metabolizing tissues despite a normal filling pressure. • It may affect the left ventricle, right ventricle or both. • It may result from impaired ejection of blood from the heart during systole or from impaired relaxation of the heart during diastole. 2
Heart failure… • It may be caused by disease of the myocardium itself (most commonly ischaemic heart disease), or by circulatory factors such as volume overload (e. g. leaky valves, or arteriovenous shunts caused by congenital defects) or pressure overload (e. g. stenosed-narrowed valves, arterial or pulmonary hypertension). • Some of these underlying causes are surgically correctable, and in some either the underlying disease (e. g. hyperthyroidism; ), or an aggravating factor such as anaemia or atrial fibrillation, is treatable with drugs. 3
Aims of treatment: • Improve quality of life by: Ø improving symptoms Ø avoiding side effects Ø preventing major morbid events such as myocardial infarction or stroke Ø delay death 4
Secondary aims of treatment: • improval cardiac performance • improve exercise capacity • reduce arrhythmiasis (ventricular & supraventricular) • maintain renal function • prevent electrolyte disturbance 5
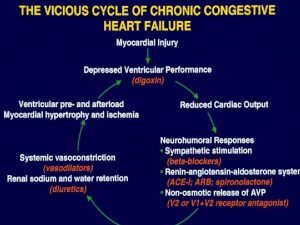
Relevant pathophysiology: • There is a poor relationship between symptoms and cardiac performance in chronic heart failure. • Treatment that improves cardiac function does not necessarily improve symptoms or prognosis and many treatments that have only modest beneficial effects on cardiac function may have clear beneficial effects on symptoms and prognosis. • In contrast, there may be a relationship between haemodynamics, symptoms and prognosis in patients with acute pulmonary oedema or cardiogenic shock. 6
Cardiac performance is influenced by: 1) 2) 3) 4) 5) Preload Force of Cardiac contraction Myocardial compliance After load Neuro endocrine activation 7
1) Preload: • This determines ventricular end-diastolic pressure and volume. • In normal hearts an increased preload leads to increased end-diastolic fibre length, which, in turn, causes increased force of contraction. • In heart failure, this response is reduced or even reversed. 8
2) Force of cardiac contraction: • This is determined largely by the intrinsic strength and integrity of the muscle cells. Force of contraction is decreased by: • ischaemic heart disease (myocardial infarction or chronic severe ischaemia). • Specific disorders affecting heart muscle e. g. hypertension and myocarditis. • Disorders of heart muscle of unknown cause e. g. idiopathic dilated cardiomyopathy. 9
3) Myocardial compliance: • This is an important determinant of ventricular filling and therefore of CO. Compliance is decreased by: • Fibrosis • Hypertrophy • Ischaemia 10
4) Afterload: • This is the ventricular wall tension developed during ejection. Afterload is increased by: • systemic arterial vasoconstriction • increased arterial pressure • obstruction to outflow e. g. aortic stenosis 11
5) Neuro endocrine activation: • • After an acute cardiac insult plasma concentrations of renin, angiotension II, aldosterone, noradrenaline, endothelin, ADH (arginine vasopressin) and the natriuretic peptides are increased. If the patient survives and does not require treatment, then the activity of the reninangiotensin-aldosterone system (RAAS) return to normal, probably a consequence of compensatory salt and water retention, but plasma concentrations of other neuroendocrine systems remain elevated. 12
5) Neuro endocrine activation: . . . • Once diuretics have been administered, RAAS activity increases, as do the concentrations of other neuro-hormones with the exception of the natriuretic peptides, which may decline. • However, as the heart failure progresses, all the above neuroendocrine system becomes markedly activated. 13
5) Neuro endocrine activation: . . . • Increased sympathetic activation via arterial baroreflexes (and possibly a downregulation of inhibitory activity of baroreceptors leads to sympathetically mediated increases in renal renin secretion and further increases in angiotensin II and aldosterone. 14
5) Neuro endocrine activation: . . . • Neuroendocrine activation may be responsible for many of the characteristics features of heart failure. Examples include: • Angiotensin II: Vasoconstriction (esp renal) sodium retention, continuing cardiac myocyte damage causing progressive ventricular dilatation (remodelling); stimulates aldosterone secretion. 15
5) Neuro endocrine activation: . . . • Aldosterone: Sodium retention; potassium loss and myocardial fibrosis (both may lead to arrhythmias). • Sympathetic activation: Ø Vasoconstriction, arrhythmias, hypokalaemia sodium retention. May initially increase cardiac contractility but has adverse effects on long-term cardiac function as for angiotensin II by progressive remodelling following myocardial damage. 16
5) Neuro endocrine activation: . . . • In the mestermined countries heart failure is caused by one of the following: Ø ischaemic heart disease Ø Hypertension Ø heart muscle disorders Ø valvular heart disease 17
Drugs used to treat heart failure: 1) • • 2) • • 3) • • 4) • • • Diuretics: thiazides, loop diuretics decrease peripheral and pulmonary oedema decrease preload by reduction in circulatory volume. Neuroendocrine antagonists: ACE inhibitors β-receptor antagonists ARBs Aldosterone antagonists Drugs with positive inotropic effect; cardiac glycosides (mainly chronic heart failure) β-adrenoceptor agonists (acute heart failure only) Vasodilator agents: Mainly decrease preload: nitrates (glyceryl trinitrate, isorbide dinitrate and isosorbide mononitrate). Mainly decrease afterload: hydralazine Decrease preload and afterload: sodium nitroprusside (acute HF only). 18
STEPS IN THE TREATMENT OF CHRONIC HEART FAILURE Reduce workload of the heart (a) Limit activity level (b) Reduce weight. (c) Control hypertension. 19
• • Restrict sodium. Restrict water (rarely required). Give diuretics. Give ACE inhibitors or angiotensin receptor blocker. 20
• Give digitalis if systolic dysfunction with third heart sound or atrial fibrillation is present. • Give beta blockers to patients with stable class II -IV heart failure. • Give vasodilators. 21
SODIUM REMOVAL • Sodium removal is important step----by dietary salt restriction or diuretic…. especially if oedema is present. • In mild failure, it is reasonable to start with a thiazide diuretic, switching to more powerful agents as required. • Sodium loss causes secondary loss of potassium, which is particularly hazardous if the patient is to be given digitalis. 22
• Hypokalaemia can be treated with potassium supplementation or through the addition of a potassium sparing-diuretic such as spironolactone 23
ACE INHIBITORS AND ANGIOTENSIN RECEPTOR BLOCKERS • In patient with left ventricular dysfunction but no oedema, ACE inhibitors should be used first. • Several large studies have compared ACE inhibitors with other traditional therapies for chronic heart failure. • The results show clearly that ACE inhibitors are superior to both placebo and to vasodilators and must be considered, along with diuretics, as first-line therapy for chronic failure. 24
• However, ACE inhibitors cannot replace digoxin in patients already receiving that drug because patients withdrawn from the cardiac glycoside while on ACE inhibitors therapy deteriorate. 25
• Additional studies suggest that ACE inhibitors are also valuable in asymptomatic patients with ventricular dysfunction. • By reducing pre-load and after-load, these drugs appear to slow the rate of ventricular dilatation and thus delay the onset of clinical heart failure. • Thus, ACE inhibitors are beneficial in all subsets of patients, from those who are asymptomatic to those in severe chronic failure. 26
• It appears that all ACE inhibitors tested to date have beneficial effects in patients with heart failure. • Recent studies have documented beneficial effects with enalapril, captopril, lisinopril, quinapril and ramipril. . • The angiotensin II receptors antagonists (e. g. losartan, valsartan, etc) produce beneficial hemodynamic effects similar to those of the ACE inhibitors. • However, large clinical trials suggest that the angiotensin receptors blockers should be used in patients who are intolerant of ACE inhibitors 27 (usually because of cough).
VASODILATORS • Vasodilators drugs can be divided into selective arteriolar dilators, venous dilators, drugs with non-selective vasodilatory effects. • For this purpose, the ACE inhibitors may be considered non-selective arteriolar and venous dilators. • The choice of agents should be based on the patient’s signs and symptoms and haemodynamic measurements. 28
• Thus, in patients with high filling pressures in whom the principal symptoms is dyspnoea, venous dilators such as longacting nitrates will be most helpful in reducing filing pressure and the symptoms of pulmonary congestion. • In patients whom fatigue due to low ventricular output is primary symptom, an arteriolar dilator such as hydralazine may be helpful in increasing forward cardiac output. 29
• In most patients with severe chronic failure that responds poorly to otherapy, the problem usually involves both elevated filling pressures and reduced cardiac output. • In these circumstances, dilation of both arterioles and veins is required. In one trial, combined therapy with hydralazine (arteriolar dilation) and isosorbide dinitrate (venous dilation) prolonged life more than placebo in patients already receiving digitalis and diuretics. 30
BETA-BLOCKERS AND CALCIUM CHANNEL BLOCKERS • Many trials have evaluated the potential for betablocker therapy in patients with heart failure. The rationale is based on the hypothesis that excessive tachycardia and adverse effects of high catecholamine levels on the heart failure patients contribute to the downward course of heart failure patients. However, such therapy must be initiated very cautiously at low doses, since acutely blocking the supportive effects of catecholamines can worsen heart failure. 31
• Several months of therapy may be required before improvement is noted, this is usually consists of a slight rise in ejection fraction, slower heart rate, and reduction in symptoms. As noted above, bisoprolol, carvedilol, metoprolol have been shown to reduce mortality. • The calcium-blocking drugs appear to have no role in the treatment of patients with heart failure. Their depressant effects on the heart may worsen heart failure. 32
DIGITALIS • Digoxin is indicated in patients with heart failure and atrial fibrillation. It is also most helpful in patients with a dilated heart and third heart sound. • It usually given after ACE inhibitors. • Only about 50% of patients with normal sinus rhythm have documented relief of heart failure from digitalis. 33
• Because it has a moderate but persistent positive inotropic effect, digitalis can, in theory, reverse the signs and symptoms of heart failure. In appropriate patient, digitalis increases the stroke work and cardiac output. • The increased output (and possibly a direct action resetting the sensitivity of baroceptors) eliminates the stimuli evoking increased sympathetic outflow, and both heart rate and vascular tone diminish. 34
• With decreased end-diastolic fiber tension (the result of increased systolic ejection and decreased filling pressure), heart size and oxygen demand decrease. • Finally, increased renal blood flow improves glomerular filtration and reduces aldosteronedriven sodium reabsorption. Thus, oedema fluid can be excreted, further reduction ventricular pre-load and danger of pulmonary oedema. 35
• Digitalis reduces hospitalization and death from progressive heart failure at the expense of an increase in sudden death. • It is important to note that the mortality rate was reduced in patients with serum digoxin concentration of 1 ng/m. L or less but increased in those with digoxin levels greater than 1. 5 ng/m. L. 36
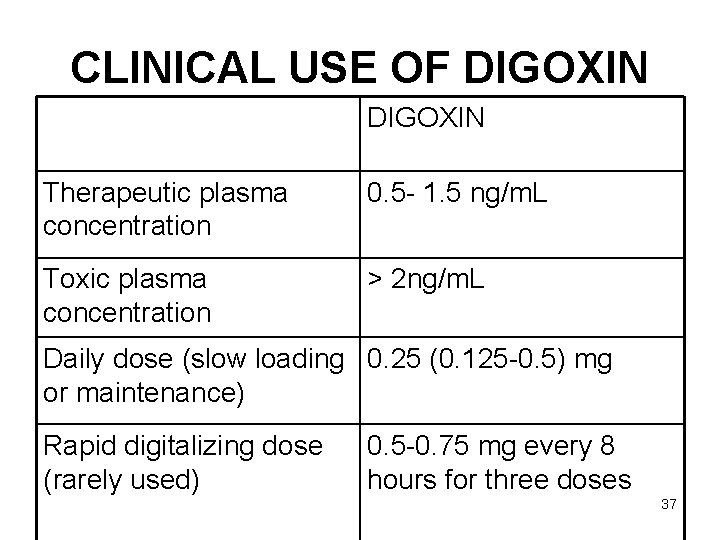
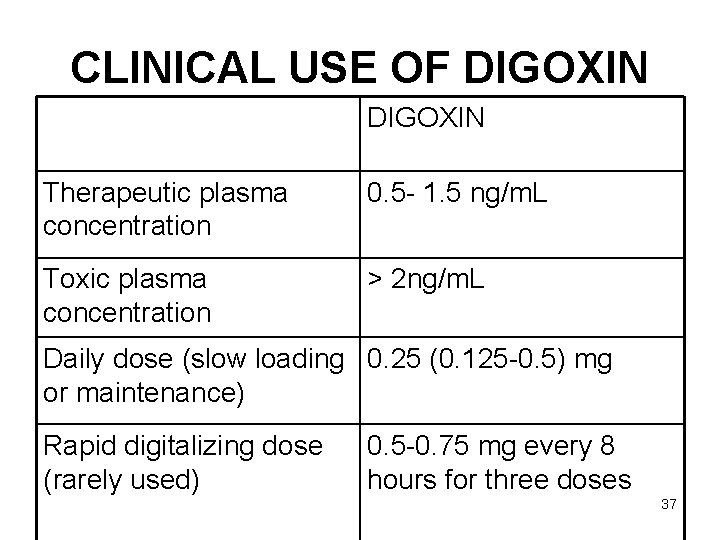
CLINICAL USE OF DIGOXIN Therapeutic plasma concentration 0. 5 - 1. 5 ng/m. L Toxic plasma concentration > 2 ng/m. L Daily dose (slow loading 0. 25 (0. 125 -0. 5) mg or maintenance) Rapid digitalizing dose (rarely used) 0. 5 -0. 75 mg every 8 hours for three doses 37
• These values are appropriate for adults with normal renal and hepatic function. 38
DRUGS WITH POSITIVE INOTROPIC EFFECTS • Drugs that inhibit phosphodiesterases, the family of enzymes that inactivate c. AMP and c. GMP, have long been used in therapy of heart failure. • The bipyridines inamrinone and milrinone are the most successful of these agents found to date. 39
• Levosimendan, an investigational drug that appears to inhibit phosphodiesterase and cause some vasodilatation in addition to its inotropic effects. 40
BIPYRIDINES • Inamrinone (previously called amrinone) and milrinone are bipyridine compounds that inhibit phosphodiesterase. They are active orally as well as parenterally but only available in parenteral forms. • They have elimination half-lives of 3 to 6 hours, with 10 to 40% being excreted in the urine. 41
PHARMACODYNAMICS • The bipyridines increase myocardial contractility by increasing calcium influx in the heart during the action potential. • They also important vasodilating effect. • These drugs are relatively selective for phosphodiesterase isoenzyme 3, a form found in cardiac and smooth muscle. 42
• Inhibition of this enzyme results in an increase in c. AMP and increase in contractility and vasodilatation. • The toxicity of inamrinone includes nausea and vomiting; arrhythmias, thrombocytopenia and liver enzyme changes. 43
• Milrinone appears less likely to cause bone marrow and liver toxicity than inamrinone, but it does cause arrhythmias. • Inamrinone and milrinone are now used only intravenously and only for acute heart failure or exacerbation of chronic heart failure. 44
BETA ADRENOCEPTOR STIMULANTS • The selective β 1 agonist that has been most widely used in patients with heart failure is dobutamine. • This drug produces an increase in cardiac output together with a decrease in ventricular filling pressure • Some tachycardia and increase in myocardial oxygen consumption have been reported. 45
• The potential for producing angina or arrhythmias in patients with coronary artery disease must be considered, as well as the tachyphylaxis that accompanies the use of any β stimulant. • Dopamine has also been used in acute heart failure and be particularly helpful if there is need to raise blood pressure 46
DIURETICS • Their major mechanism of action in heart failure is to reduce venous pressure and ventricular pre-load. • These reductions have two useful effects: reduction of oedema and its symptoms and reduction of cardiac size, which leads to improved pump efficiency. 47
VASODILATORS • The vasodilators are effective in acute heart failure because they provide a reduction in preload (through venodilation), or reduction in after load (through arterial dilatation), or both. • Some evidence suggests that long-term use of hydralazine and isosorbide dinitrate can also reduce damaging remodeling of the heart. 48
• A synthetic form of endogenous peptide brain natriuretic peptide (BNP) has recently been approved for use in acute cardiac failure as nesiritide. • This recombinant product increases c. GMP in smooth muscle cells and effectively reduces venous and arteriolar tone in experimental preparations. It also causes diuresis. 49
• The peptide has a short half-life of about 18 minutes and is administered as a bolus intravenous dose followed by continuous infusion. • Excessive hypotension is the most common adverse effect. 50
• Bosentan, an orally active competitive inhibitor of endothelin, has been shown to have some benefit in experimental animal models heart failure, but results in human trials have not been impressive. • This drug is approved for use in pulmonary hypertension. It has significant teratogenic and hepatotoxic effects. 51
BETA ADRENOCEPTOR BLOCKERS • Most patients with chronic heart failure respond favorably to certain beta-blockers in spite of the fact that these drugs can precipitate acute decompensation of cardiac function. • Studies with bisoprolol, carvedilol, metoprolol showed a reduction in mortality in patients with stable severe heart failure but this effect was not observed with another beta-blocker, bucindolol, 52
• The full understanding of the beneficial action of beta blockade is lacking, but suggested mechanism include attenuation of the adverse effects of high concentration of catecholamines (including apoptosis), up-regulation of betareceptors, decrease heart rate, and reduced remodeling through inhibition of mitogenic activity of catecholamines. 53
• Read on: • The General Principles of Management of Heart Failure 54
 Congestive heart failure zones for management
Congestive heart failure zones for management Edema assessment
Edema assessment Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Cor pulmonale
Cor pulmonale Acute vs chronic heart failure
Acute vs chronic heart failure Earthy look in chronic renal failure
Earthy look in chronic renal failure Chronic rheumatic heart disease
Chronic rheumatic heart disease Cardiac output stroke volume and heart rate
Cardiac output stroke volume and heart rate Heart sounds and murmurs
Heart sounds and murmurs Non conducted pac ecg
Non conducted pac ecg Failure to fire pacemaker
Failure to fire pacemaker Ductile fracture mechanism
Ductile fracture mechanism Forrester classification heart failure
Forrester classification heart failure Cardiomegay
Cardiomegay Heart failure definition
Heart failure definition New york scale heart failure
New york scale heart failure Heart failure complications
Heart failure complications Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Heart failure
Heart failure Lmnop heart failure
Lmnop heart failure Keith rn heart failure case study
Keith rn heart failure case study Donkey analogy heart failure
Donkey analogy heart failure Acute pulmonary congestion histology
Acute pulmonary congestion histology Compensatory mechanism of heart failure
Compensatory mechanism of heart failure Diabetes and heart failure
Diabetes and heart failure Diabetes and heart failure
Diabetes and heart failure Compensatory mechanisms of heart failure
Compensatory mechanisms of heart failure Apetm
Apetm Dr nienkemper
Dr nienkemper Flinders model of chronic care self-management limitations
Flinders model of chronic care self-management limitations Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Wagner model of chronic disease management
Wagner model of chronic disease management Nursing management of liver cirrhosis
Nursing management of liver cirrhosis Pancreatitis nursing
Pancreatitis nursing Thoracic facet joint pain referral patterns
Thoracic facet joint pain referral patterns Dullness of heart
Dullness of heart Goat heart dissection
Goat heart dissection Hrt to hrt merrylands
Hrt to hrt merrylands Angioectasia icd 10
Angioectasia icd 10 Definition of chronic toxicity
Definition of chronic toxicity Chronic granulomatous disease
Chronic granulomatous disease Chronic care model definition
Chronic care model definition Pulp and periapical diseases
Pulp and periapical diseases Types of anaemia
Types of anaemia Cholecystitis
Cholecystitis Fibromyalgia vs chronic fatigue
Fibromyalgia vs chronic fatigue Stigmata of chronic liver disease
Stigmata of chronic liver disease Pulpitis classification
Pulpitis classification 5 cardinal signs of inflammation
5 cardinal signs of inflammation Iceberg phenomenon related to chronic diseases
Iceberg phenomenon related to chronic diseases What causes hemolytic anemia
What causes hemolytic anemia Chronic unease in the workplace
Chronic unease in the workplace Chronic calculous cholecystitis
Chronic calculous cholecystitis Definition of chronic toxicity
Definition of chronic toxicity Chronic blood loss
Chronic blood loss