MNT for Heart Failure and Transplant Congestive Heart







- Slides: 52

MNT for Heart Failure and Transplant
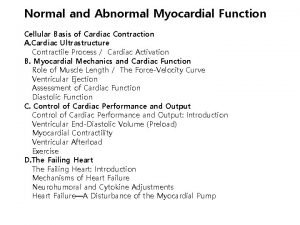
Congestive Heart Failure (CHF) n A clinical syndrome characterized by progressive deterioration of left ventricular function, inadequate tissue perfusion, fatigue, shortness of breath, and congestion

Congestive Heart Failure (CHF) —cont’d Gradual failure of heart 1. Compensated—Lack of O 2 to tissues causes increase in heart rate and enlargement of heart 2. Decompensated—Heart no longer adjusts

Causes of Heart Failure n n Diseases of the heart (valves, muscle, vessels, arteries) and vasculature (hypertension) cause left ventricular systolic dysfunction Once established, myocardial infarction, dietary sodium excess, medication noncompliance, arrhythmias, pulmonary embolism, infection, anemia can precipitate complete CHF
Prevalence and Incidence Unlike other cardiovascular diseases, CHF is on the increase n Number of CHF-related discharges increased 174% from 1979 -2003 n 4. 8 million Americans have CHF; overall prevalence 2 -6% n Krummel DA in Krause, 12 th ed. , 2008
Prevalence and Incidence Prevalence increases with age, especially after age 55 n Black women have the highest rates, followed by black men, Latino men, white women, and Latino women n More Medicare dollars are spent on CHF than on any other diagnosis n
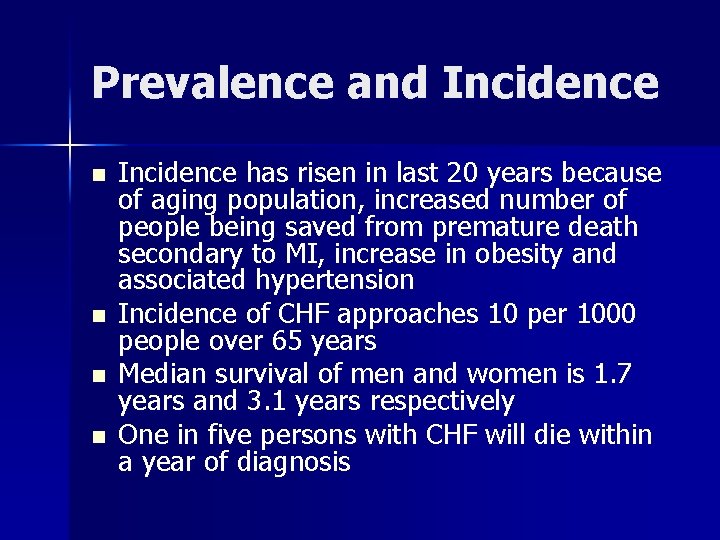
Prevalence and Incidence n n Incidence has risen in last 20 years because of aging population, increased number of people being saved from premature death secondary to MI, increase in obesity and associated hypertension Incidence of CHF approaches 10 per 1000 people over 65 years Median survival of men and women is 1. 7 years and 3. 1 years respectively One in five persons with CHF will die within a year of diagnosis
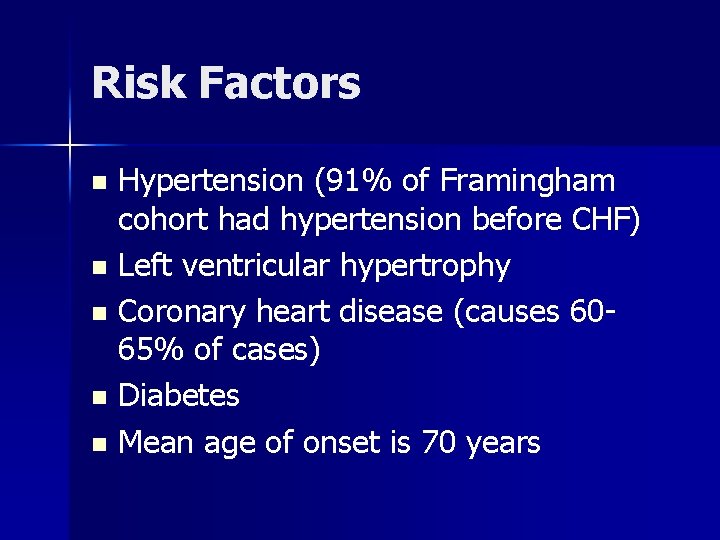
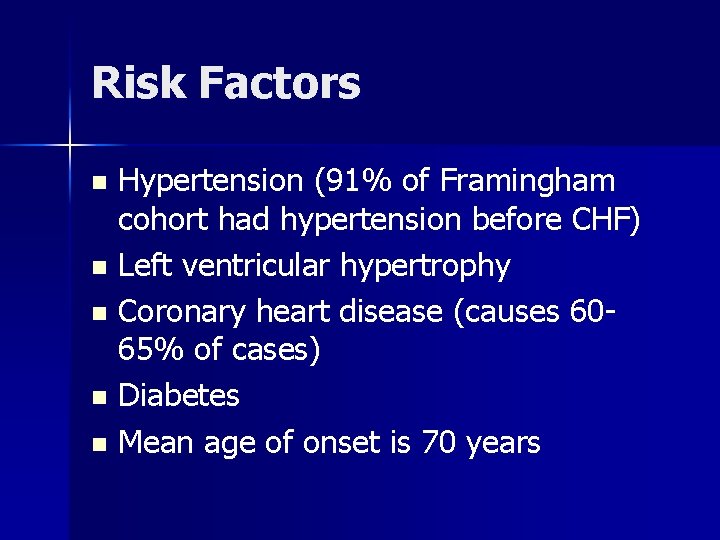
Risk Factors Hypertension (91% of Framingham cohort had hypertension before CHF) n Left ventricular hypertrophy n Coronary heart disease (causes 6065% of cases) n Diabetes n Mean age of onset is 70 years n
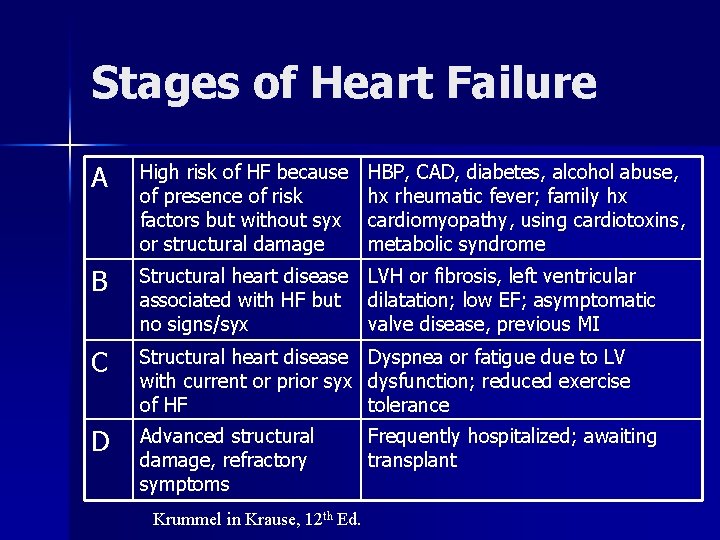
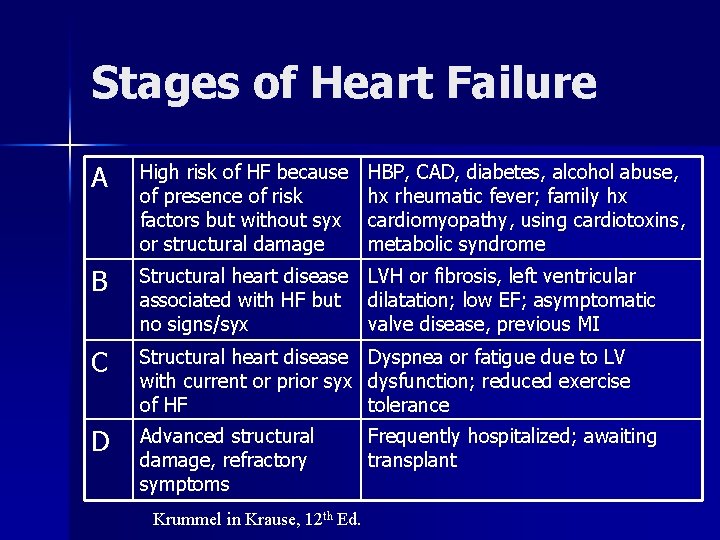
Stages of Heart Failure A High risk of HF because of presence of risk factors but without syx or structural damage B Structural heart disease LVH or fibrosis, left ventricular associated with HF but dilatation; low EF; asymptomatic no signs/syx valve disease, previous MI C Structural heart disease with current or prior syx of HF Dyspnea or fatigue due to LV dysfunction; reduced exercise tolerance D Advanced structural damage, refractory symptoms Frequently hospitalized; awaiting transplant Krummel in Krause, 12 th Ed. HBP, CAD, diabetes, alcohol abuse, hx rheumatic fever; family hx cardiomyopathy, using cardiotoxins, metabolic syndrome
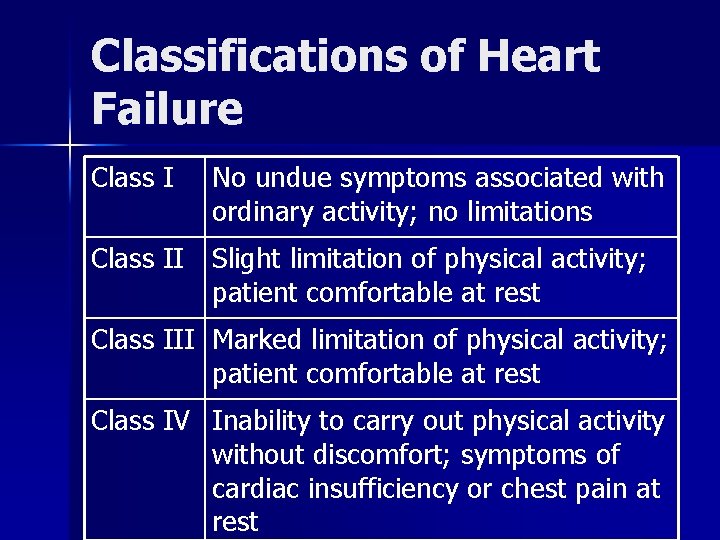
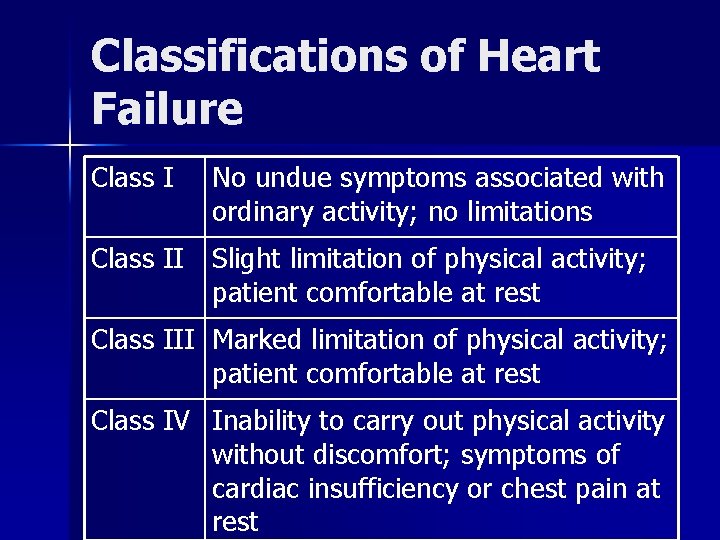
Classifications of Heart Failure Class I No undue symptoms associated with ordinary activity; no limitations Class II Slight limitation of physical activity; patient comfortable at rest Class III Marked limitation of physical activity; patient comfortable at rest Class IV Inability to carry out physical activity without discomfort; symptoms of cardiac insufficiency or chest pain at rest
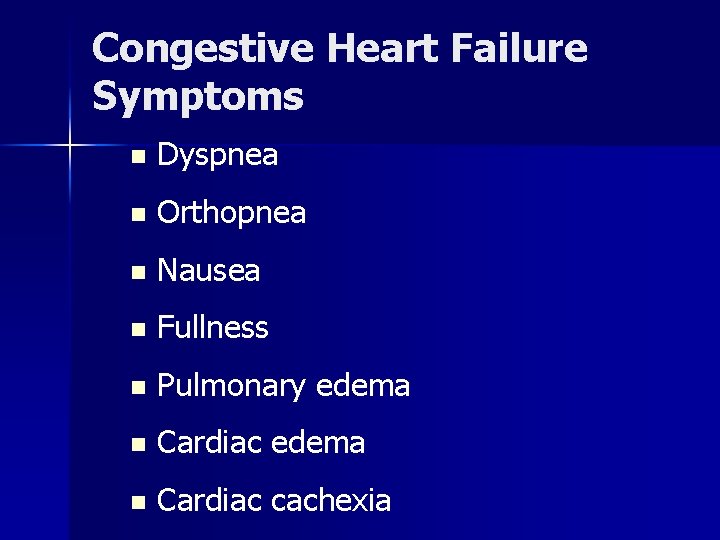
Congestive Heart Failure Symptoms n Dyspnea n Orthopnea n Nausea n Fullness n Pulmonary edema n Cardiac cachexia
CHF DIAGNOSIS n EKG or electrocardiogram – measures the rate and regularity of the heartbeat – May indicate whethere has been heart damage or changes in anatomy n Chest X-ray – Shows whether heart is enlarged, fluid in lungs, pulmonary disease
CHF DIAGNOSIS n Echocardiogram – Most useful test in diagnosis of heart failure – Uses sound waves to create a picture of the heart – Evaluates heart function: cardiac output and areas of the heart that are not contracting normally

Other Cardiac Tests n Holter Monitor: ambulatory electrocardiography – Worn for 24 hours and provides a continuing recording of heart rhythm during normal activity n Cardiac Blood Pool Scan (radionuclide ventriculography or nuclear scan) – Uses radioactive imaging agent injected into a vein to outline chambers of the heart and blood vessels – Shows how well heart is pumping blood to the rest of the body
Other Cardiac Tests n Cardiac Catheterization n Coronary angiography: usually done along with cardiac catheterization – Flexible tube passed through vein in the groin or arm to reach the coronary arteries – Allows physician to visualize the arteries, check pressure and blood flow in coronary arteries, collect blood samples – Dye injected into coronary arteries and/or chambers of the heart – Allows angiographer to visualize flow of blood
Cardiac Tests n Exercise Stress Test – EKG and blood pressure readings are taken before, during, and after exercise to determine how the heart responds to exercise – Patient exercises on a treadmill or stationary bike until reaches a heartrate established by the physician – Echocardiogram often included
BNP and NTpro. BNPBlood Test n n n Measure the concentration of BNP (hormone made by the heart) or NT-pro. BNP (both formed when pro-BNP is cleaved into two fragments) Released as a natural response to heart failure, to hypotension, and to LVH Used to grade the severity of heart failure
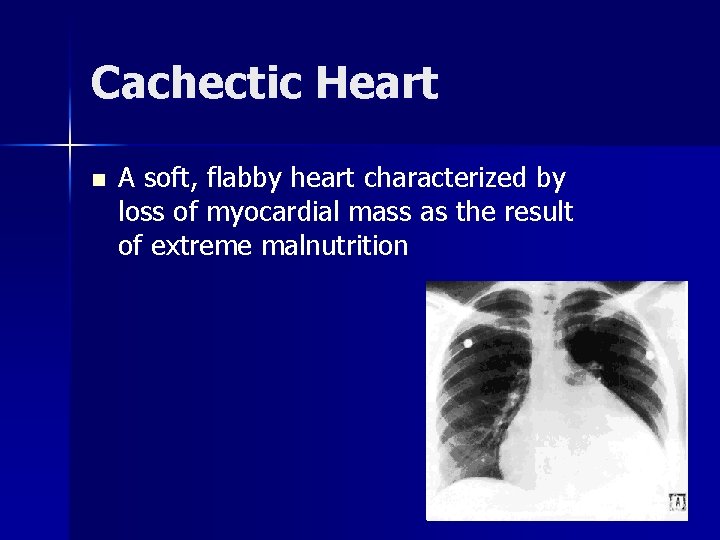
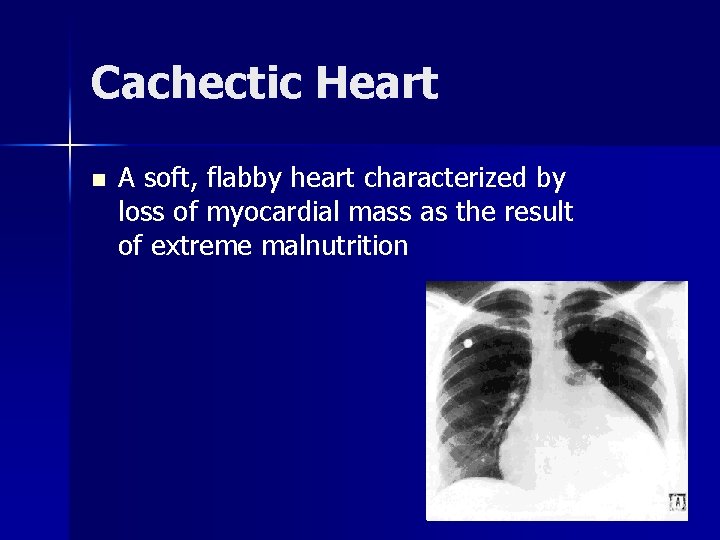
Cachectic Heart n A soft, flabby heart characterized by loss of myocardial mass as the result of extreme malnutrition
Congestive Heart Failure Treatment n Goal: decrease work of heart n Diet 1. Na restriction (500 to 1000 mg) 2. Monitor serum K—hypokalemia possible with diuretics and digoxin) 3. Fluid restriction 4. Alcohol—none to moderate 5. Caffeine—can cause MI or cardiac arrhythmia
Medications Used in Heart Failure n n n Diuretics help reduce fluid buildup in lungs and peripheral edema ACE inhibitors lower blood pressure and reduce the strain on the heart. These medications also may reduce the risk of a future heart attack. Beta blockers slow heart rate and lower blood pressure to decrease the workload on the heart. Digoxin makes the heart beat stronger and pump more blood. Vasodilators: reduce blood pressure and stress on the heart
MNT in HF Fluid restriction n Sodium restriction n Meet energy/protein needs n Prevent cardiac cachexia n Small frequent meals n
Fluid Restriction If hyponatremia occurs (serum sodium <130 m. Eq/L) n Limit total fluids to <2000 ml n In severe decompensation, limit to 1000 -1500 ml n Maintain restricted sodium diet even if serum sodium depleted; sodium has moved from blood to tissues n
Fluid Status and Assessment Patients should record daily weights and advise care providers if weight gain exceeds 2 -3 lb a day or 5 lb in a week n Restricting sodium and fluids (decreasing by 1 to 1. 5 cups) may prevent complete HF n

Fluid Calculations Hospitalized patients may be limited to 500 -2000 ml daily n Foods having a high fluid content may also be limited n Foods that are liquid at room temperature such as ice cream, yogurt, gelatin, popsicles count towards fluid allotment n
Living with Fluid Restrictions Freezing fruit or sucking on sugar free hard candy may help n Fluid status monitored by measuring urine specific gravity and serum electrolyte values and observing for clinical signs of edema n Restrictions often discontinued when patients leave the hospital n
Cardiac. Cachexia n n n Involuntary weight loss of >6% of nonedematous body weight over a 6 -month period Significant loss of lean body mass: exacerbates HF Cachectic heart: soft and flabby Structural, circulatory, metabolic, inflammatory, and neuroendocrine changes in skeletal muscle Serious complication of HF
Cardiac. Cachexia n n n Patients with cardiac cachexia may lose 1015% of their body weight (dry weight) Other markers (serum prealbumin and transferrin) may be disproportionately low because of the dilutional effect of excess fluid Use anthropometrics (measurement of calf and thigh circumference, MUAC) and diet history
Cardiac. Cachexia n n n Proinflammatory state in which cytokines (TNF, IL-1 and I-6) are elevated in the blood and myocardial tissue Reduced blood flow to the gut may reduce gut integrity leading to entry of bacteria and endotoxins High TNF associated with reduced BMI, lower skinfolds, reduced visceral proteins Krummel in Krause, 12 th ed. , 2008
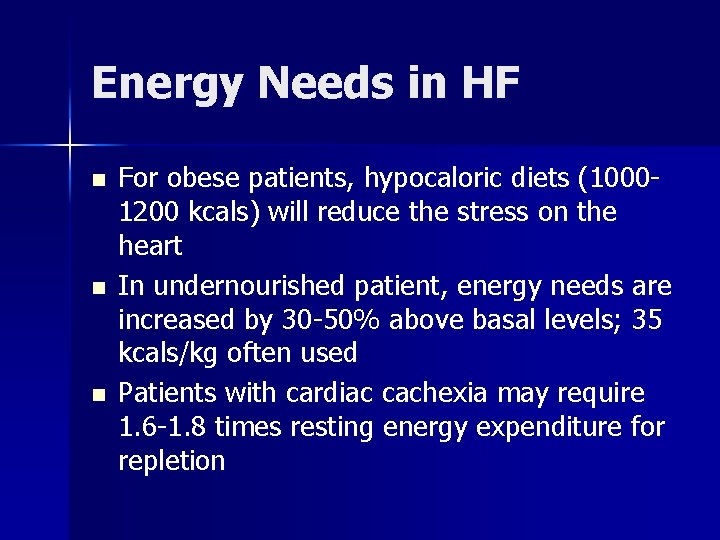
Energy Needs in HF n n n For obese patients, hypocaloric diets (10001200 kcals) will reduce the stress on the heart In undernourished patient, energy needs are increased by 30 -50% above basal levels; 35 kcals/kg often used Patients with cardiac cachexia may require 1. 6 -1. 8 times resting energy expenditure for repletion

Sodium n n n Impaired cardiac function → inadequate blood flow to the kidneys → aldosterone and antidiuretic hormone secretion Aldosterone promotes sodium resorption and ADH promotes water conservation Even patients with mild heart failure can retain sodium and water if consuming a high salt diet (6 g or 250 m. Eq/day)
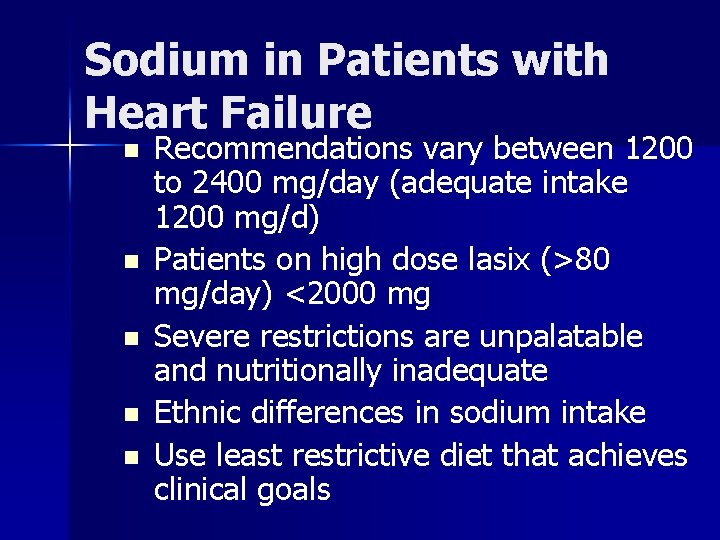
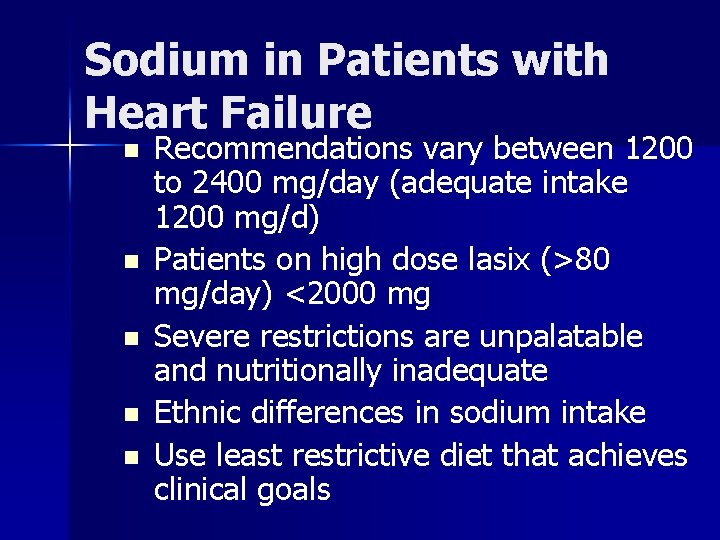
Sodium in Patients with Heart Failure n n n Recommendations vary between 1200 to 2400 mg/day (adequate intake 1200 mg/d) Patients on high dose lasix (>80 mg/day) <2000 mg Severe restrictions are unpalatable and nutritionally inadequate Ethnic differences in sodium intake Use least restrictive diet that achieves clinical goals
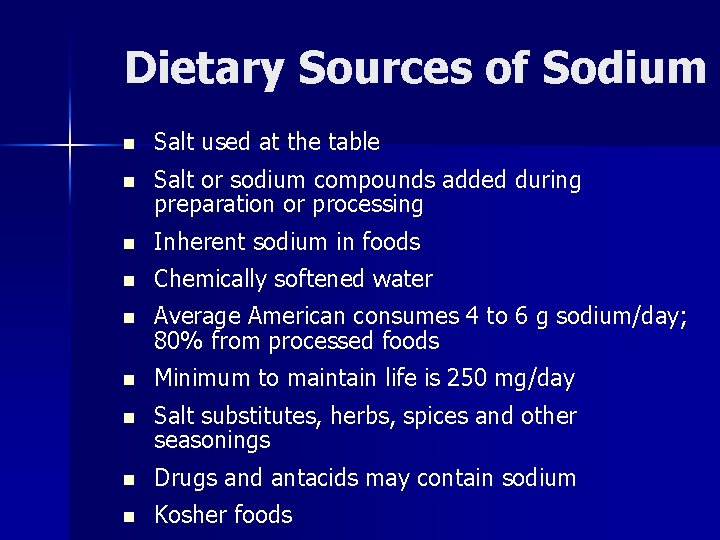
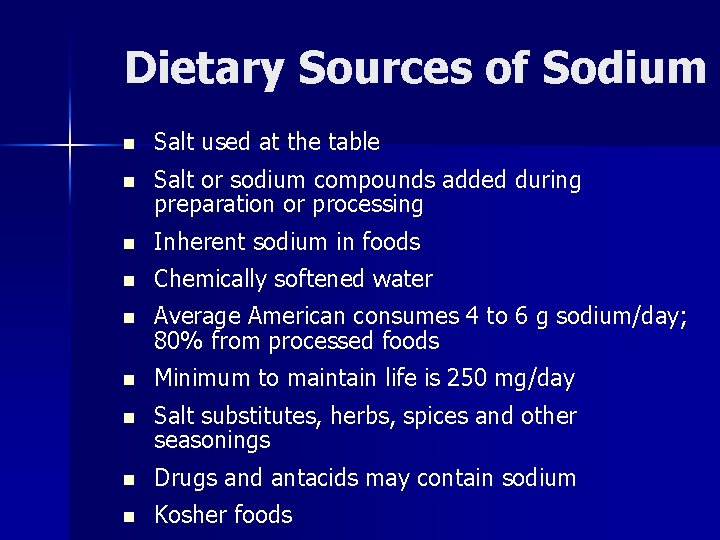
Dietary Sources of Sodium n Salt used at the table n Salt or sodium compounds added during preparation or processing n Inherent sodium in foods n Chemically softened water n Average American consumes 4 to 6 g sodium/day; 80% from processed foods n Minimum to maintain life is 250 mg/day n Salt substitutes, herbs, spices and other seasonings n Drugs and antacids may contain sodium n Kosher foods
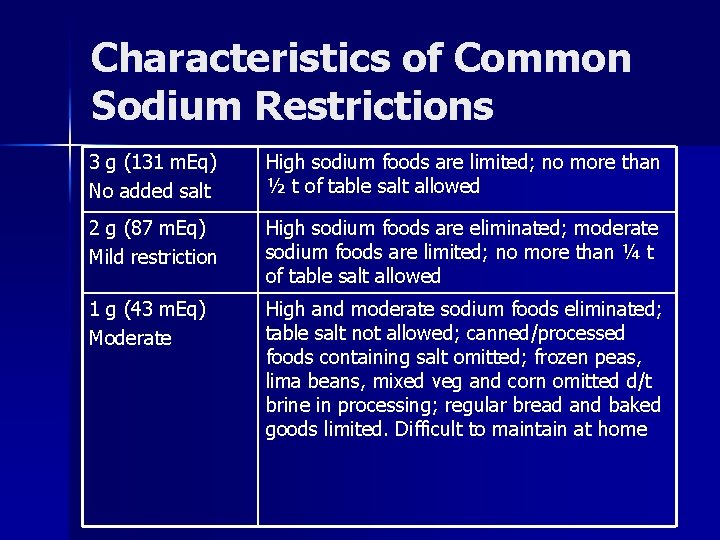
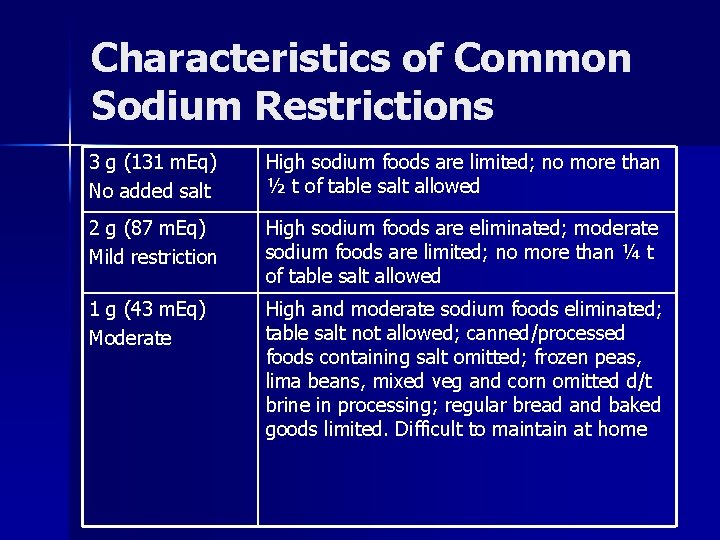
Characteristics of Common Sodium Restrictions 3 g (131 m. Eq) No added salt High sodium foods are limited; no more than ½ t of table salt allowed 2 g (87 m. Eq) Mild restriction High sodium foods are eliminated; moderate sodium foods are limited; no more than ¼ t of table salt allowed 1 g (43 m. Eq) Moderate High and moderate sodium foods eliminated; table salt not allowed; canned/processed foods containing salt omitted; frozen peas, lima beans, mixed veg and corn omitted d/t brine in processing; regular bread and baked goods limited. Difficult to maintain at home
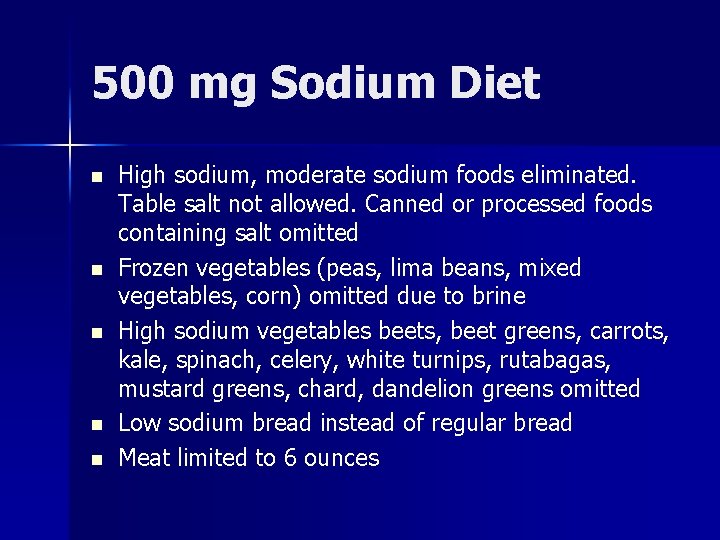
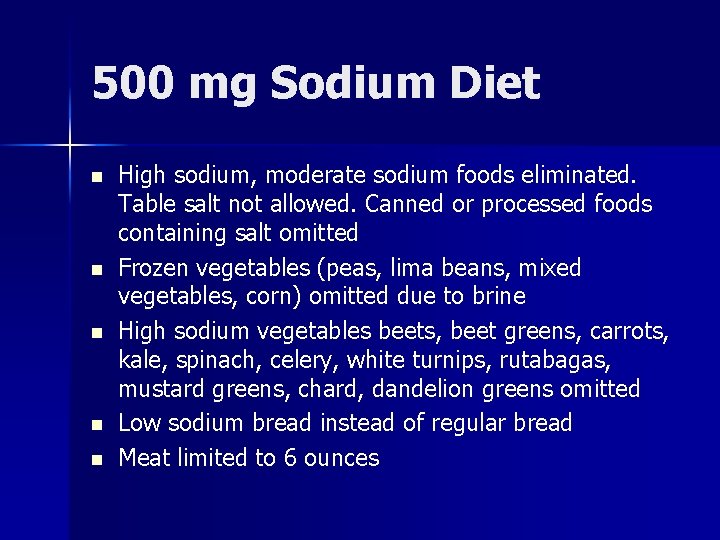
500 mg Sodium Diet n n n High sodium, moderate sodium foods eliminated. Table salt not allowed. Canned or processed foods containing salt omitted Frozen vegetables (peas, lima beans, mixed vegetables, corn) omitted due to brine High sodium vegetables beets, beet greens, carrots, kale, spinach, celery, white turnips, rutabagas, mustard greens, chard, dandelion greens omitted Low sodium bread instead of regular bread Meat limited to 6 ounces
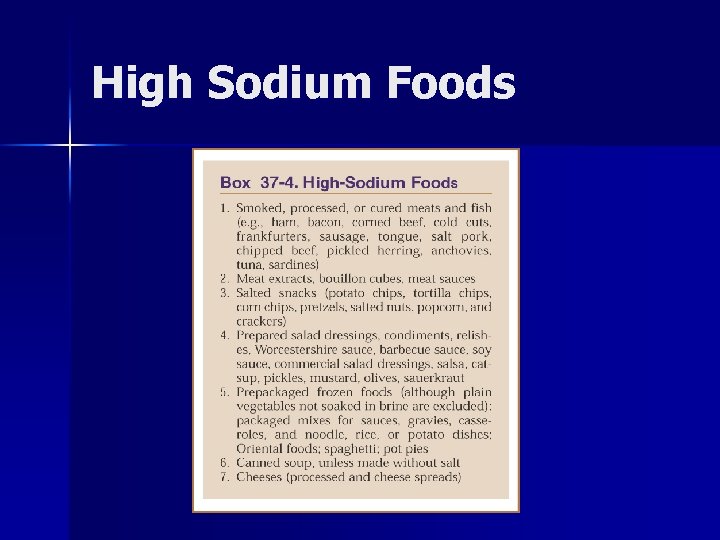
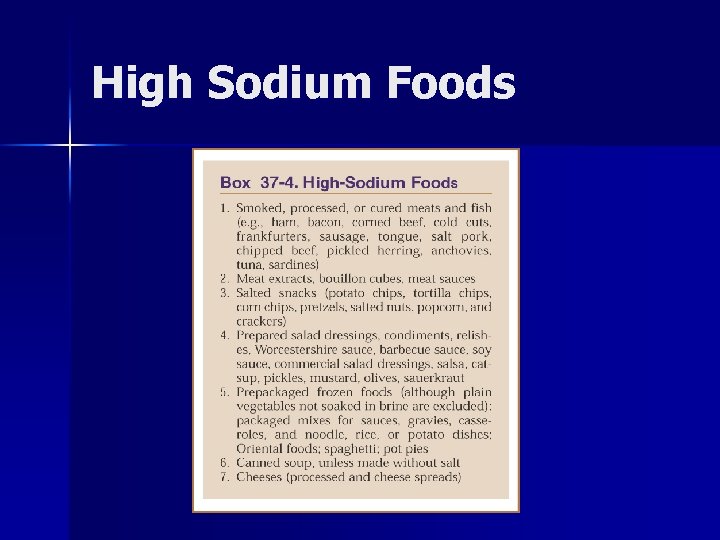
High Sodium Foods
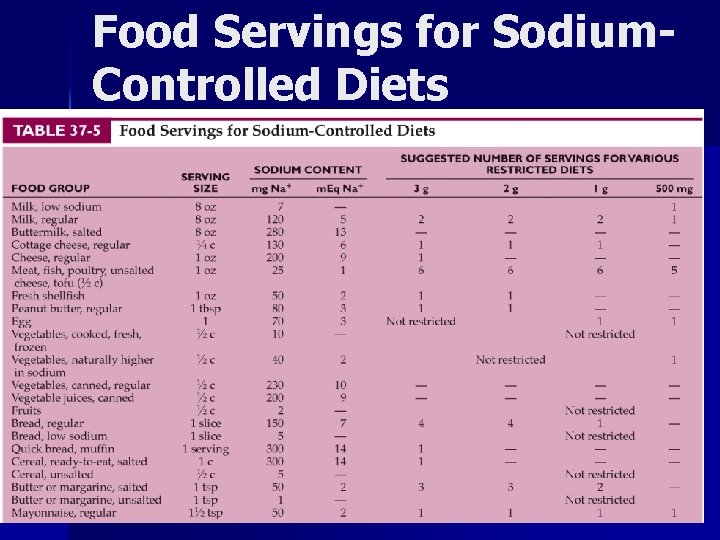
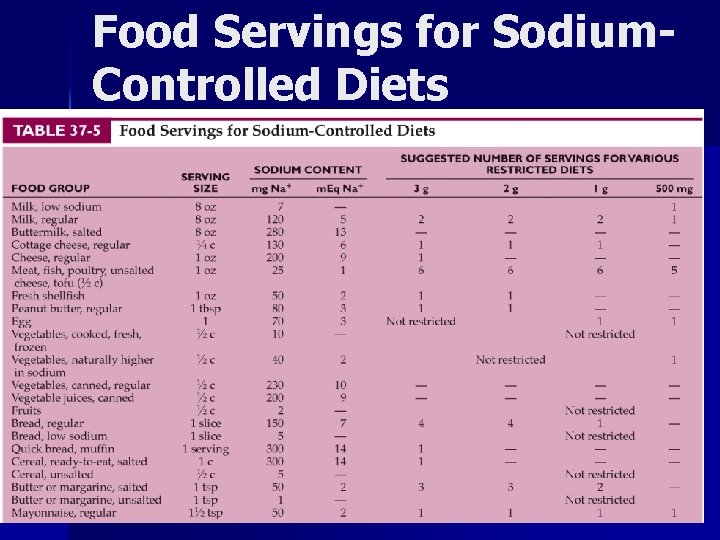
Food Servings for Sodium. Controlled Diets
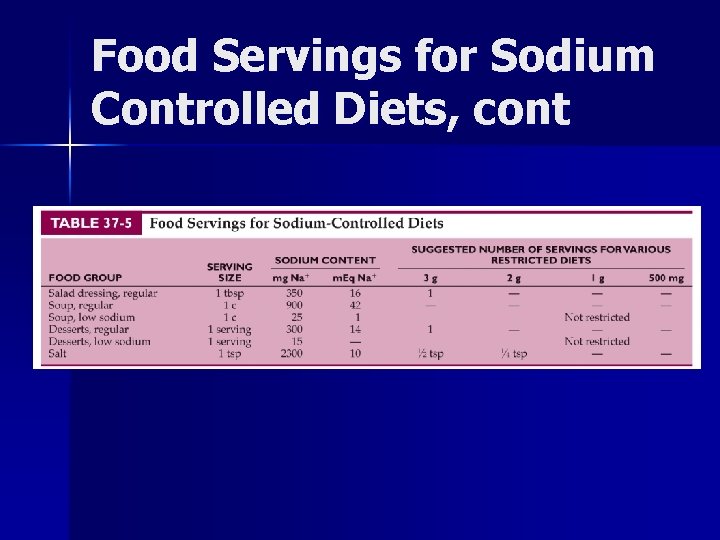
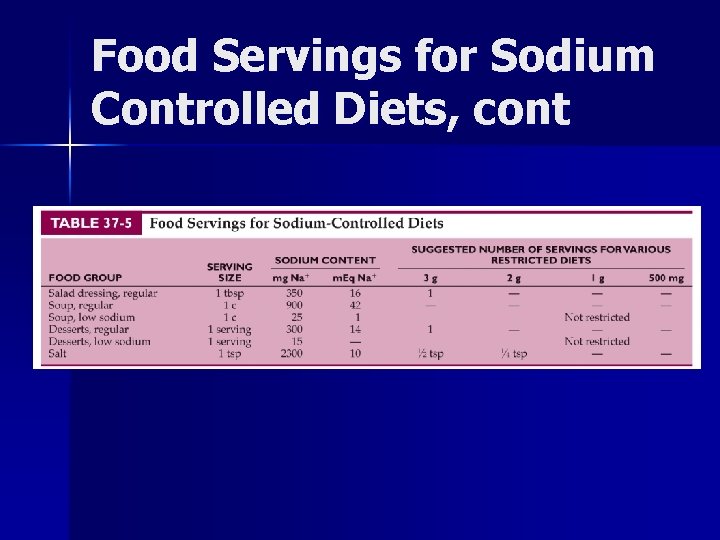
Food Servings for Sodium Controlled Diets, cont

Food Labeling Guide (standard serving) Sodium Free. Less than 5 mg Very Low Sodium 35 mg or less Low Sodium 140 mg or less Reduced Sodium At least 25% less sodium than regular food Light Sodium 50% less sodium Unsalted, No salt added during processing Without Added Salt, No Salt Added Lightly Salted 50% less added sodium than normally added (product must state “not a low-sodium food”)
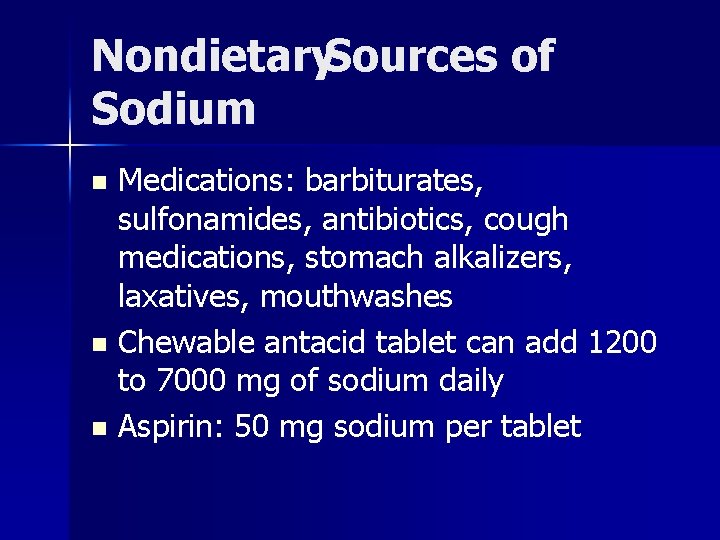
Nondietary. Sources of Sodium Medications: barbiturates, sulfonamides, antibiotics, cough medications, stomach alkalizers, laxatives, mouthwashes n Chewable antacid tablet can add 1200 to 7000 mg of sodium daily n Aspirin: 50 mg sodium per tablet n
Potassium n n n Potassium wasting diuretics (hydrochlorthiazide, furosemide) increase potassium excretion which may lead to digitalis toxicity Some patients will need potassium supplements Salt substitutes can provide 500 -2000 mg of potassium per teaspoon; contraindicated in renal failure and with certain other medications
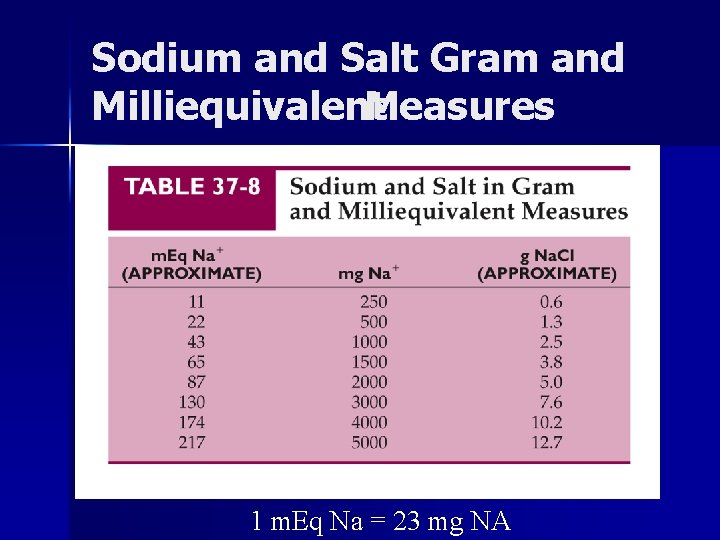
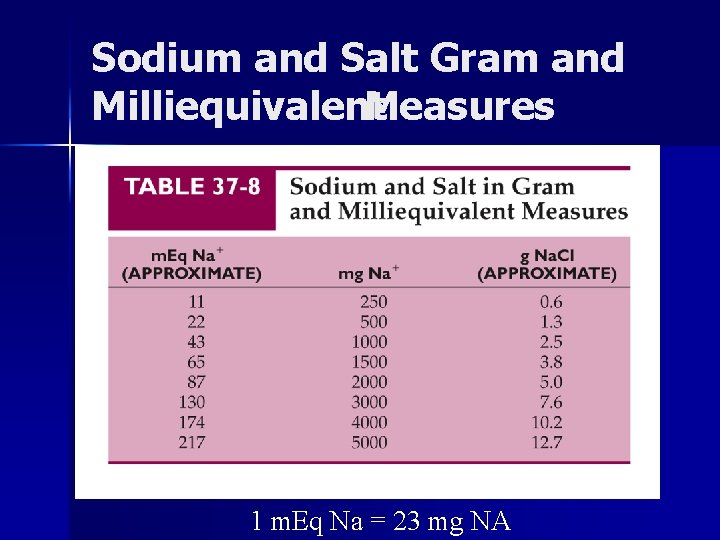
Sodium and Salt Gram and Milliequivalent Measures 1 m. Eq Na = 23 mg NA
Other Dietary Factors in Heart Failure n n n n Alcohol and caffeine Weight maintenance Calcium and vitamin D Magnesium Thiamin supplementation Small frequent feedings Supplements
Other Nutritional Issues n n n Calcium and Vitamin D: half of patients with severe HF have osteopenia or osteoporosis, especially cachectic patients; use calcium supplements with caution w/ cardiac arrhythmias Magnesium: diuretics may increase mg excretion; measure blood mg levels Thiamin status should be evaluated in HF patients on loop diuretics
Cardiac Assist Devices Mechanical heart pumps n May be helpful in pre-transplant HF patients or in those for whom transplant is not an option n
Heart Transplant n n n Only cure for refractory CHF In 2003, 2000 cardiac transplants in the U. S. Highest number in white men 50 -64 years of age
Pretransplant. MNT Goals Body weight 90 -110% of ideal body weight n Extremes of weight (<80% or >140% IBW predict poor outcome n Pretransplant comorbidities (hypertension, hyperlipidemia, diabetes) reduce survival rates n Survival 83% at 1 year, 72% at 5 years, 50% at 9 years n
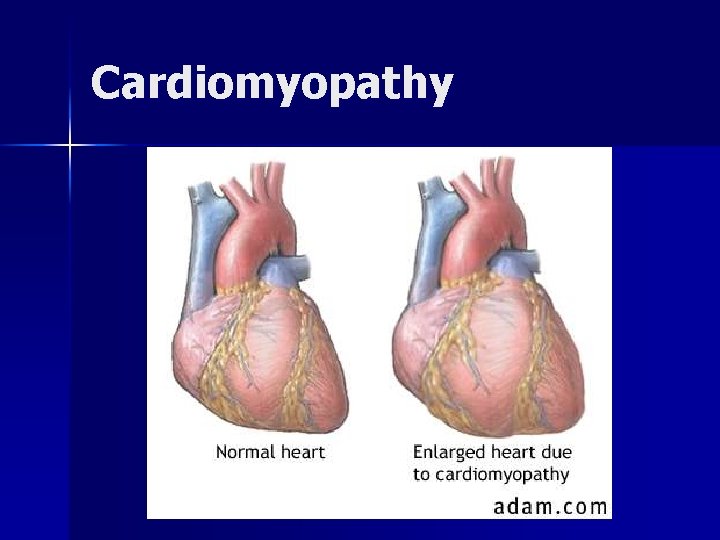
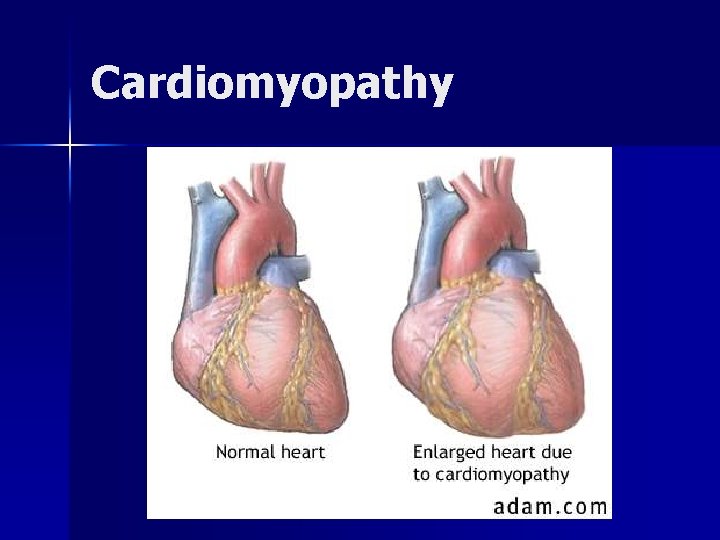
Cardiomyopathy
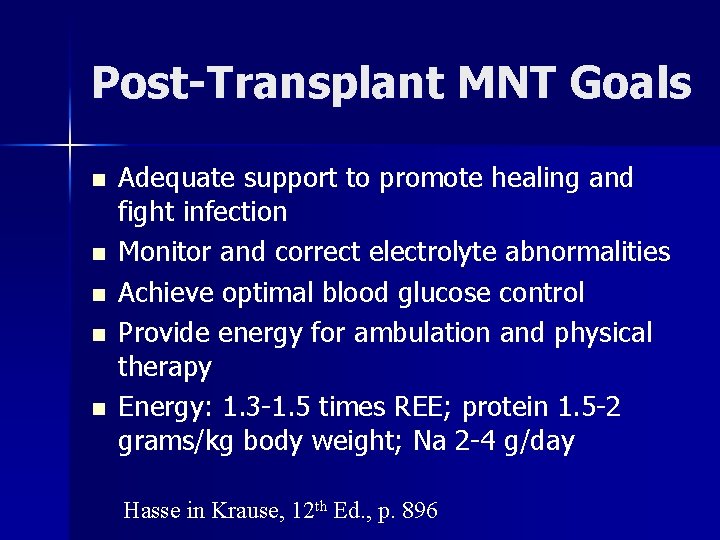
Post-Transplant MNT Goals n n n Adequate support to promote healing and fight infection Monitor and correct electrolyte abnormalities Achieve optimal blood glucose control Provide energy for ambulation and physical therapy Energy: 1. 3 -1. 5 times REE; protein 1. 5 -2 grams/kg body weight; Na 2 -4 g/day Hasse in Krause, 12 th Ed. , p. 896
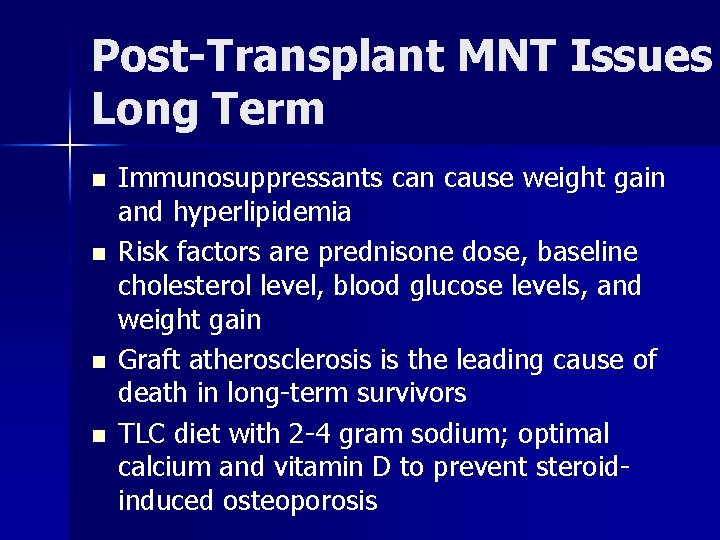
Post-Transplant MNT Issues Long Term n n Immunosuppressants can cause weight gain and hyperlipidemia Risk factors are prednisone dose, baseline cholesterol level, blood glucose levels, and weight gain Graft atherosclerosis is the leading cause of death in long-term survivors TLC diet with 2 -4 gram sodium; optimal calcium and vitamin D to prevent steroidinduced osteoporosis
ADA Nutrition Care Manual Education Resources http: //nutritioncaremanual. org/universi 13 n Heart failure Nutrition Therapy n Hypertension Nutrition Therapy n DASH Diet guidelines n
Summary CHF—most common reason for long lengths of stay in the elderly n Prevention and management is key as prognosis is poor n Aggressive nutritional interventions are important. n
 Edema assessment
Edema assessment Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Congestive heart failure zones for management
Congestive heart failure zones for management Cor pulmonale
Cor pulmonale Non conducted pac ecg
Non conducted pac ecg Failure to fire pacemaker
Failure to fire pacemaker Moderately ductile fracture
Moderately ductile fracture Tartu mnt 13
Tartu mnt 13 Surgical metabolism
Surgical metabolism Mnt programa
Mnt programa How to be anorexic
How to be anorexic Mnt in diabetes
Mnt in diabetes õismäe polikliinik registratuur
õismäe polikliinik registratuur Lvedp normal range
Lvedp normal range Chlorpromide
Chlorpromide Diabetes and heart failure
Diabetes and heart failure Face transplant
Face transplant Disadvantage of kidney transplant
Disadvantage of kidney transplant Slk kidney
Slk kidney Diet after bone marrow transplant
Diet after bone marrow transplant Neograft hair transplant in miami
Neograft hair transplant in miami Heterotopic liver transplant meaning
Heterotopic liver transplant meaning Allogeneic stem cell transplant
Allogeneic stem cell transplant Pichere pasare
Pichere pasare Face transplant
Face transplant National transplant registry malaysia
National transplant registry malaysia Allogeneic stem cell transplant
Allogeneic stem cell transplant How common is leukemia in adults
How common is leukemia in adults Types of transplant
Types of transplant Face transplant
Face transplant Embryo transplant gcse
Embryo transplant gcse Citomegalvirus
Citomegalvirus Kidney donor transplant
Kidney donor transplant Kidney donor transplant
Kidney donor transplant Cardiomegay
Cardiomegay Heart failure defined
Heart failure defined Causes of cardiomegaly in child
Causes of cardiomegaly in child Heart failure complications
Heart failure complications Chapter 24 heart failure drugs
Chapter 24 heart failure drugs Heart failure
Heart failure Lmnop heart failure
Lmnop heart failure Keith rn heart failure case study
Keith rn heart failure case study Donkey analogy heart failure
Donkey analogy heart failure Acute pulmonary congestion histology
Acute pulmonary congestion histology Pvkov
Pvkov Compensatory mechanism of heart failure
Compensatory mechanism of heart failure Apetm
Apetm Acute vs chronic heart failure
Acute vs chronic heart failure Dr nienkemper
Dr nienkemper Kontinuitetshantering
Kontinuitetshantering Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för