CONGESTIVE HEART FAILURE Cadiotonic drug and Cardiac glycosides

- Slides: 22
CONGESTIVE HEART FAILURE, Cadiotonic drug and Cardiac glycosides DR BUSARI. A. A (MB. BS, M. Sc. , MMCP, FWACP) Consultant Nephrologist & Lecturer Dept. Of Pharmacology, Therapeutics and Toxicology
outline • • Definition Physiology Epidemiology and Clinical feature Classification Causes Therapeutic goal Drug used in heart failure
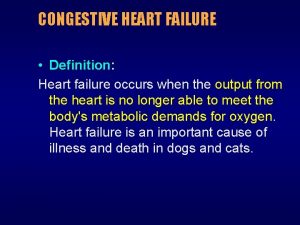
Heart failure • Heart failure is defined as inability of heart to pump blood (CO) at a rate commensurate with the requirements of the metabolizing tissues or is able to do so only with an elevated diastolic filling pressure. • Heart is major contributor of morbidity and mortality worldwide.
Heart failure • HF is due to an impaired ability of the heart to adequately fill with and/or eject blood. • It is often accompanied by abnormal increases in blood volume and interstitial fluid, hence the term congestive. • The terms congestive heart failure (CHF) or congestive cardiac failure (CCF) are often used interchangeably with chronic heart failure.
Heart failure • BVF term is used when both ventricular chambers fail resulting into fluid overload. • There is approximately 5 million people (6 10% of adult population) suffering for CHF in USA. • Mortality of advanced disease exceed 50% • In Africa, it affects 3 -4% of adult population with greater severity.
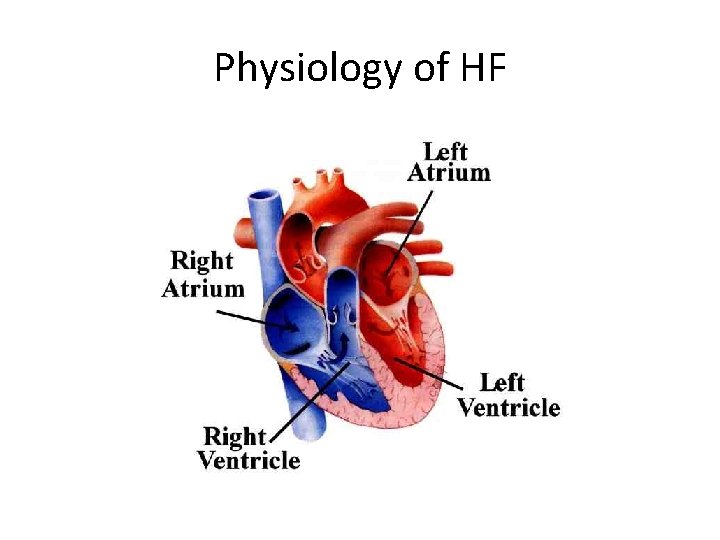
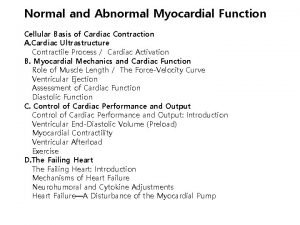
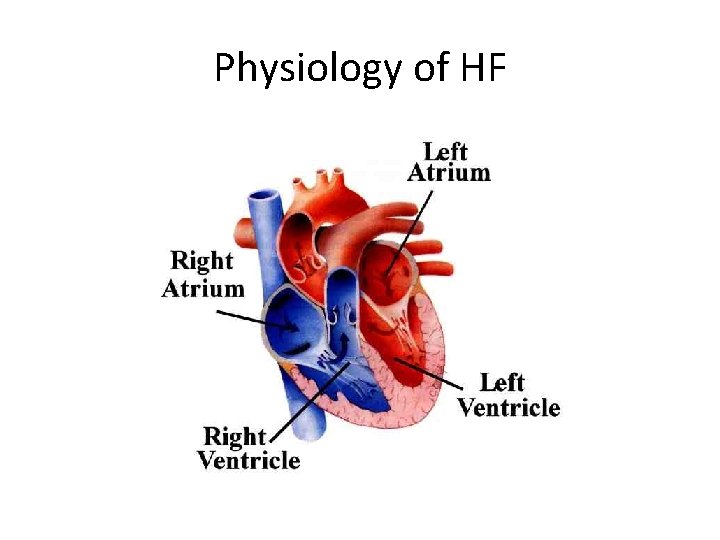
Physiology of HF
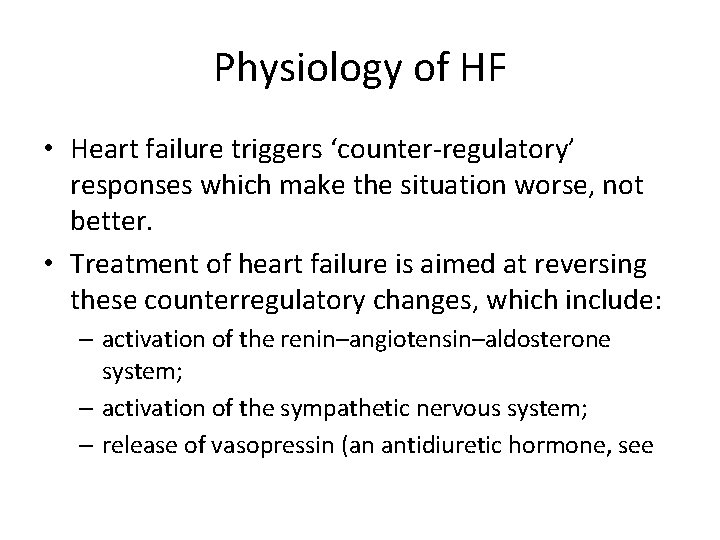
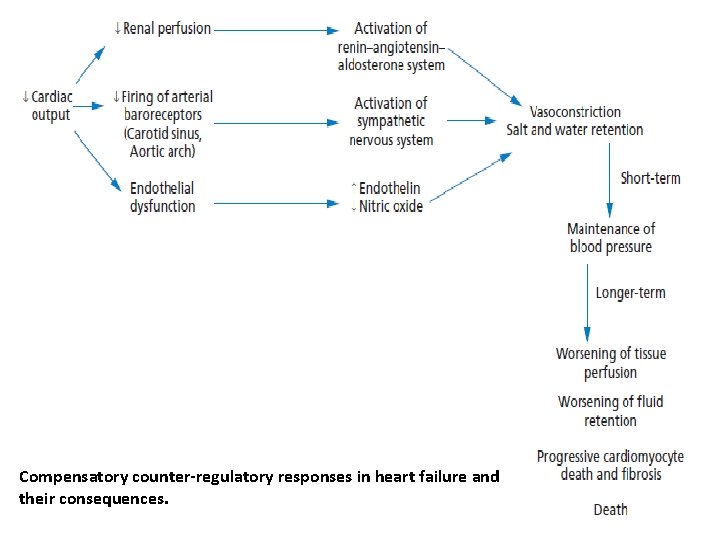
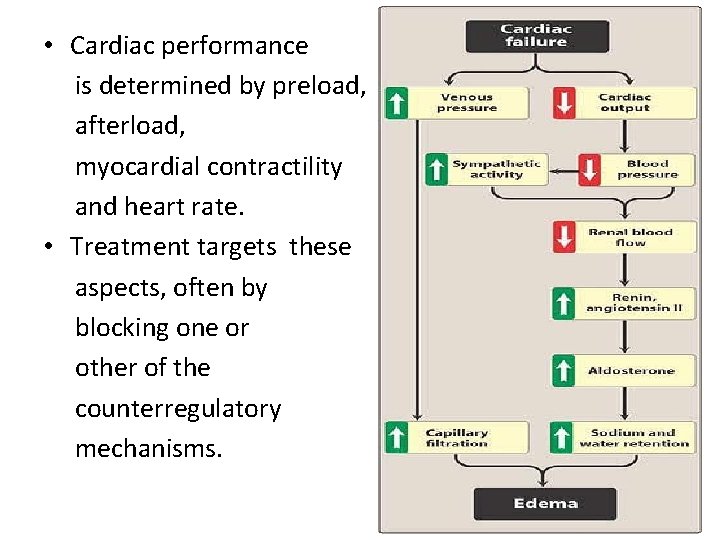
Physiology of HF • Heart failure triggers ‘counter-regulatory’ responses which make the situation worse, not better. • Treatment of heart failure is aimed at reversing these counterregulatory changes, which include: – activation of the renin–angiotensin–aldosterone system; – activation of the sympathetic nervous system; – release of vasopressin (an antidiuretic hormone, see
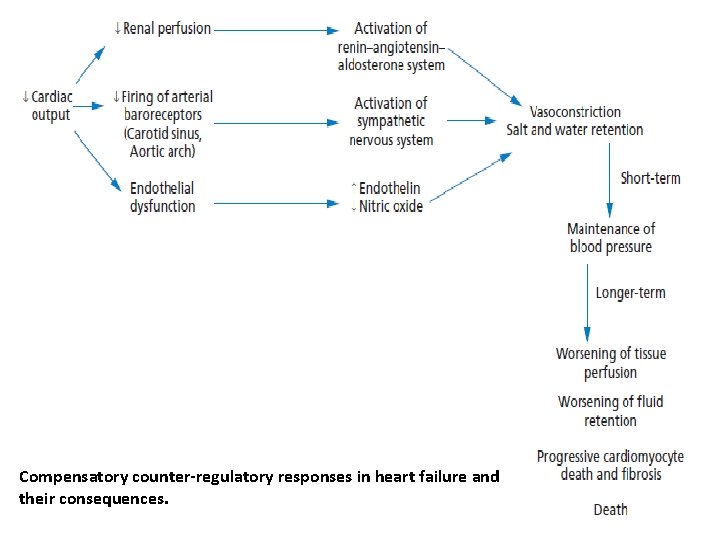
Compensatory counter-regulatory responses in heart failure and their consequences.
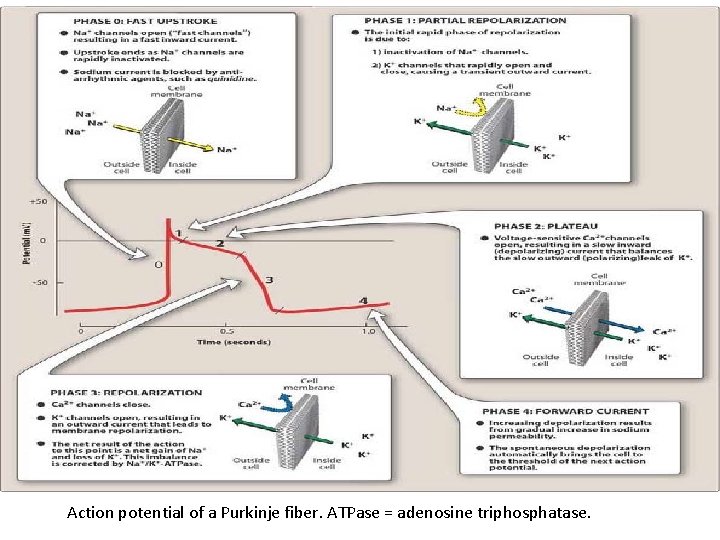
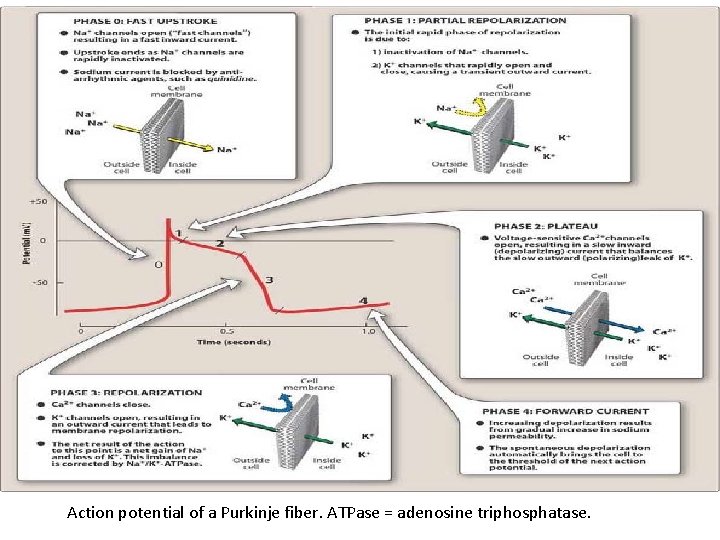
Action potential of a Purkinje fiber. ATPase = adenosine triphosphatase.
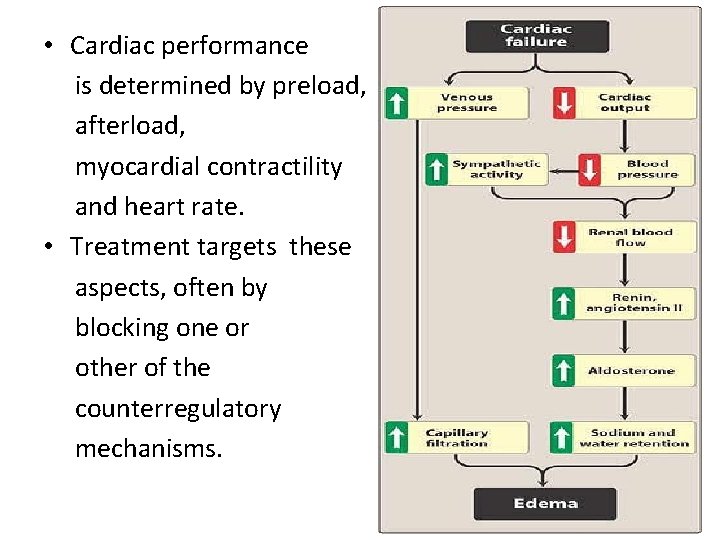
• Cardiac performance is determined by preload, afterload, myocardial contractility and heart rate. • Treatment targets these aspects, often by blocking one or other of the counterregulatory mechanisms.
Circulatory system
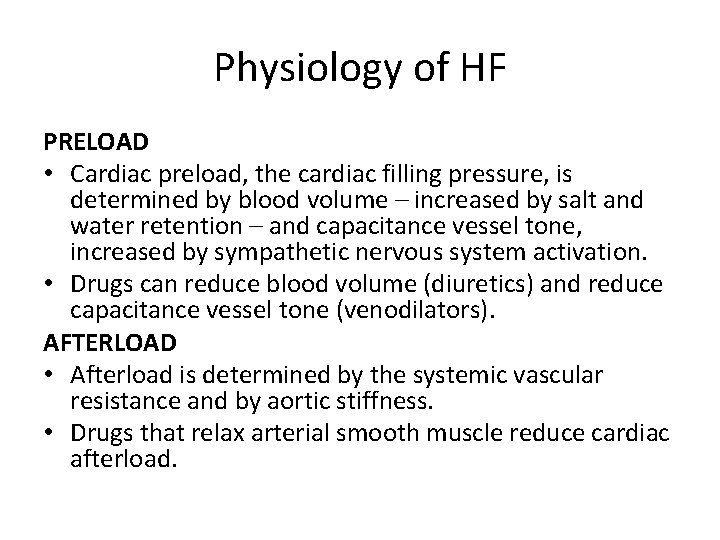
Physiology of HF PRELOAD • Cardiac preload, the cardiac filling pressure, is determined by blood volume – increased by salt and water retention – and capacitance vessel tone, increased by sympathetic nervous system activation. • Drugs can reduce blood volume (diuretics) and reduce capacitance vessel tone (venodilators). AFTERLOAD • Afterload is determined by the systemic vascular resistance and by aortic stiffness. • Drugs that relax arterial smooth muscle reduce cardiac afterload.
Physiology of HF MYOCARDIAL CONTRACTILITY • Positive inotropes (i. e. drugs that increase the force of contraction of the heart) can improve cardiac performance temporarily by increasing contractility, but at the expense of increased oxygen consumption and risk of dysrhythmia. HEART RATE • Cardiac function deteriorates as heart rate increases beyond an optimum, due to insufficient time for filling during diastole. • Heart rate can usefully be slowed by negative chronotropes (i. e. drugs that slow the heart).
Causes of heart failure Myocardial infarction Coronary artery disease Valve disease Idiopathic cardiomyopathy • Viral or bacterial cardiomyopathy • • • Myocarditis Pericarditis Arrhythmias Chronic hypertension Thyroid disease Pregnancy Septic shock
Signs and symptoms of heart failure include the following • Exertional dyspnea and/or dyspnea at rest • Orthopnea • Acute pulmonary edema • Chest pain/pressure and palpitations • Tachycardia • Fatigue and weakness • Nocturia and oliguria • Anorexia, weight loss, nausea • Central or peripheral • Exophthalmos and/or visible pulsation of eyes • Distention of neck veins • Weak, rapid, and thready pulse • Rales, wheezing • S 3 gallop a 4 w 338 nd/or pulsus alternans • Increased intensity of P 2 heart sound • Hepatojugular reflux • Ascites, hepatomegaly, and/or anasarca
The New York Heart Association (NYHA) classification • • Class I: No limitation of physical activity Class II: Slight limitation of physical activity Class III: Marked limitation of physical activity Class IV: Symptoms occur even at rest; discomfort with any physical activity
THERAPEUTIC OBJECTIVES AND GENERAL MEASURES FOR CHRONIC HEART FAILURE • Therapeutic objectives in treating heart failure are – to improve symptoms and – to prolong survival.
Drug used in heart Failure • Accordingly, six classes of drugs have been shown to be effective: • (1) inhibitors of the renin-angiotensin system, • (2) ß-adrenoreceptor blockers, • (3)diuretics, • (4) direct vasodilators, • (5) aldosterone antagonists • (6) inotropic agents e. g Digoxin

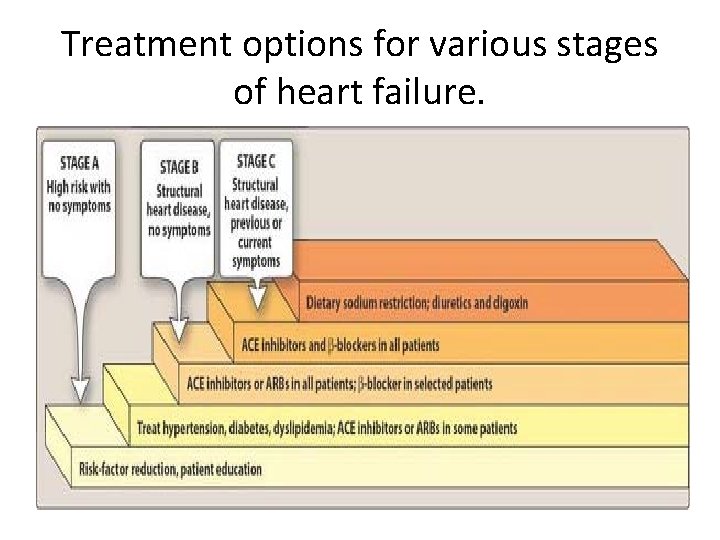
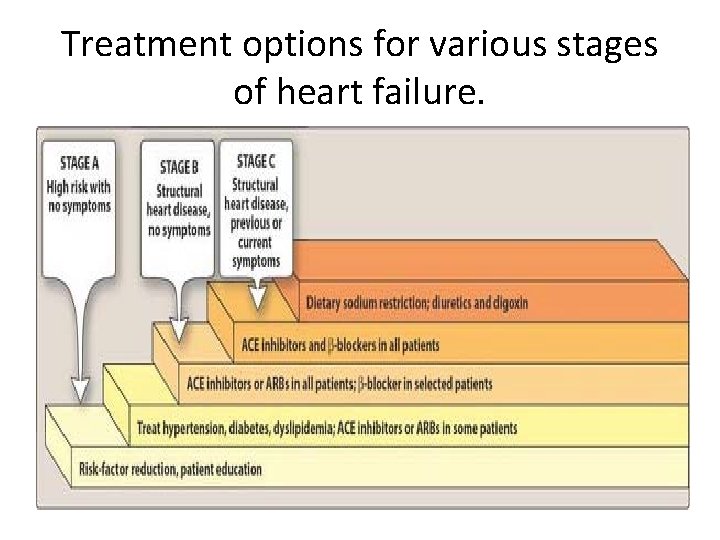
Treatment options for various stages of heart failure.
Nonpharmacologic therapy: • Oxygen and noninvasive positive pressure ventilation, • dietary sodium restriction. • fluid restriction. • physical activity as appropriate. • and attention to weight gain.
Thanks
 Edema assessment
Edema assessment Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Congestive heart failure zones for management
Congestive heart failure zones for management Cor pulmonale
Cor pulmonale Failure to sense
Failure to sense Failure to sense pacemaker
Failure to sense pacemaker Ductile vs brittle fracture surface
Ductile vs brittle fracture surface Relative refractory period
Relative refractory period Cardiac output and heart rate
Cardiac output and heart rate Test for glycosides
Test for glycosides Glycosides in pharmacognosy
Glycosides in pharmacognosy Shatavari is under the chemical class of glycoside *
Shatavari is under the chemical class of glycoside * Anthracene glycoside
Anthracene glycoside Glycosides examples
Glycosides examples Functions of glycosides
Functions of glycosides Glycoside
Glycoside Forrester classification
Forrester classification Diabetes and heart failure
Diabetes and heart failure Diabetes and heart failure
Diabetes and heart failure Accidental adulteration definition
Accidental adulteration definition Heart failure definition
Heart failure definition Heart failure defined
Heart failure defined Causes of cardiomegaly in child
Causes of cardiomegaly in child