LIU Chuan Yong Institute of Physiology Medical School







- Slides: 107
LIU Chuan Yong 刘传勇 Institute of Physiology Medical School of SDU Tel 88381175 (lab) 88382098 (office) Email: liucy@sdu. edu. cn Website: www. physiology. sdu. edu. cn 1
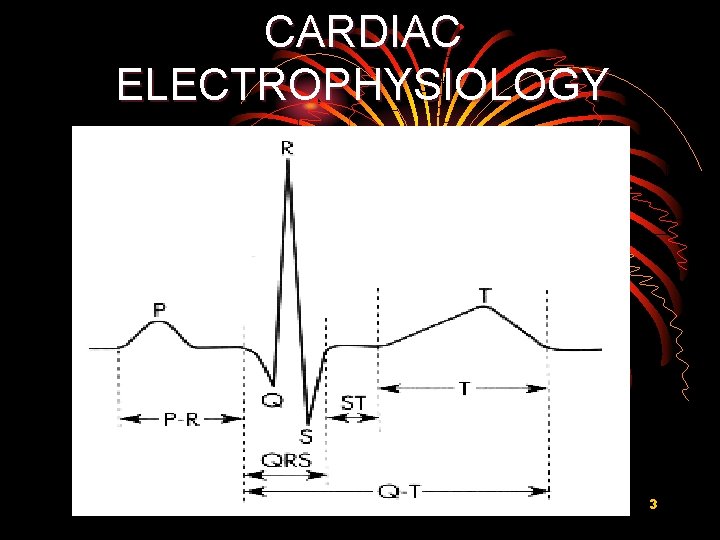
Section 2 Electrophysiology of the Heart 2
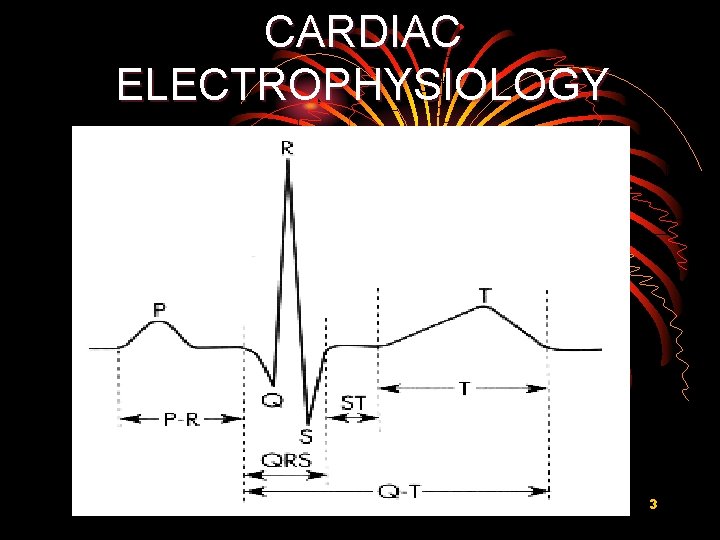
CARDIAC ELECTROPHYSIOLOGY 3
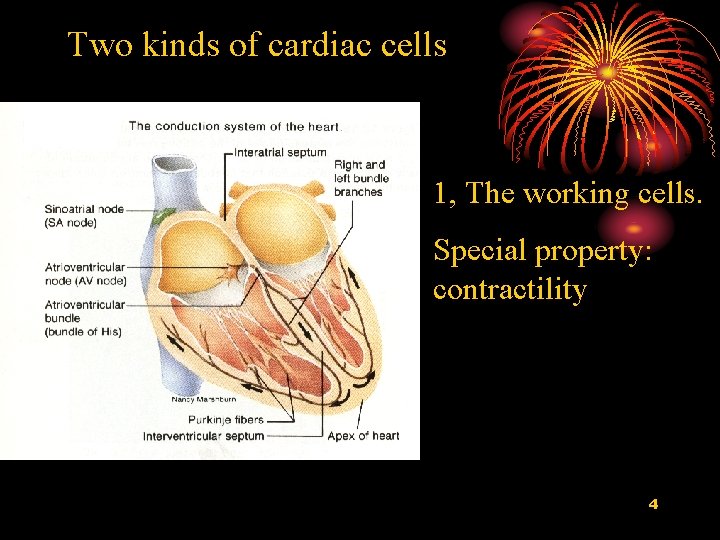
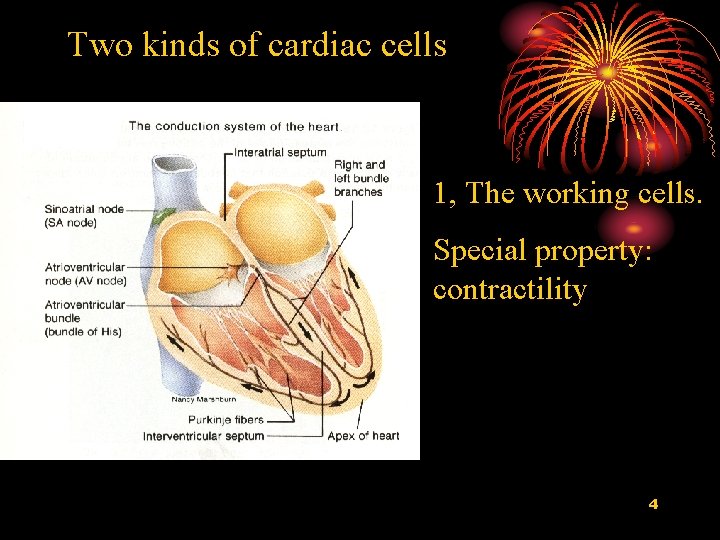
Two kinds of cardiac cells 1, The working cells. Special property: contractility 4
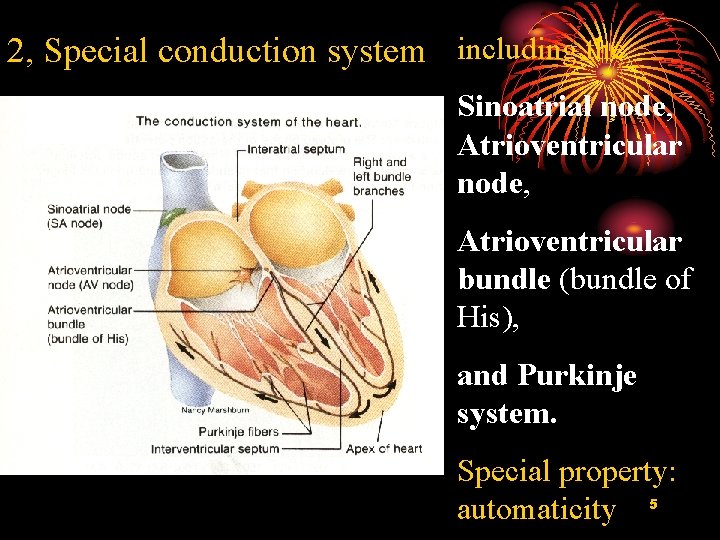
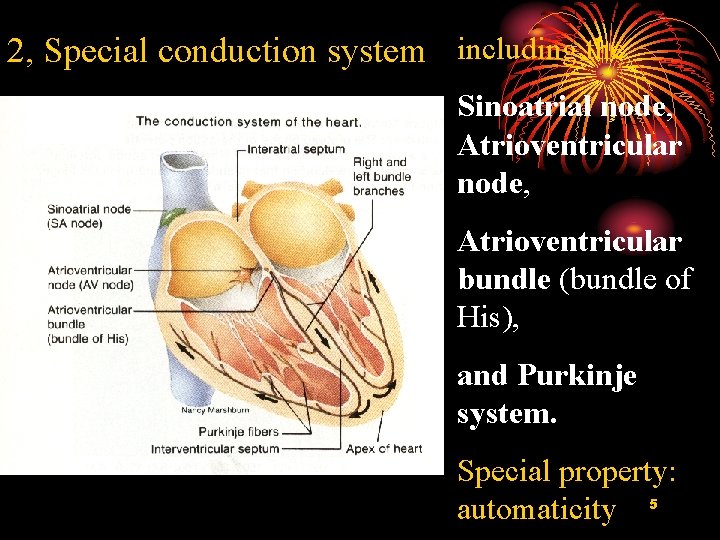
2, Special conduction system including the Sinoatrial node, Atrioventricular bundle (bundle of His), and Purkinje system. Special property: automaticity 5
I. Transmembrane Potentials of II. Myocardial Cells 6
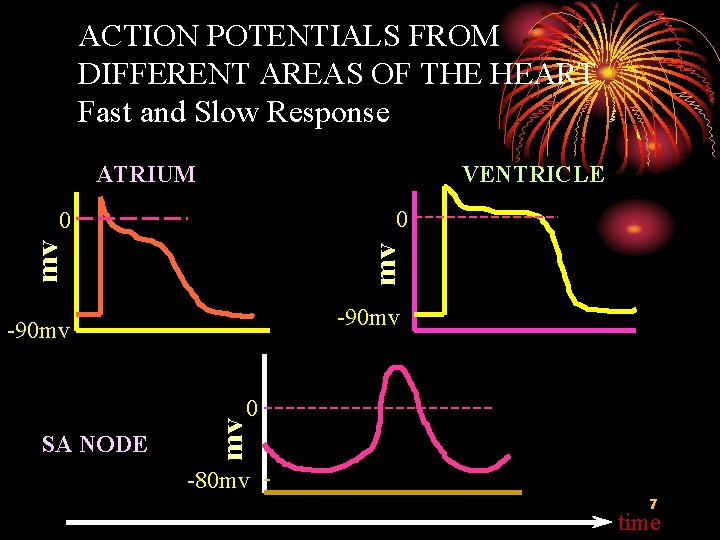
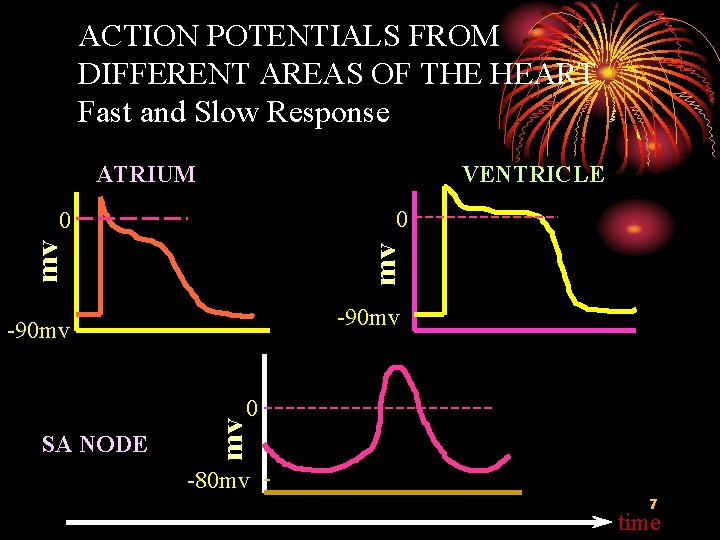
ACTION POTENTIALS FROM DIFFERENT AREAS OF THE HEART Fast and Slow Response ATRIUM VENTRICLE 0 mv mv 0 -90 mv SA NODE mv 0 -80 mv 7 time
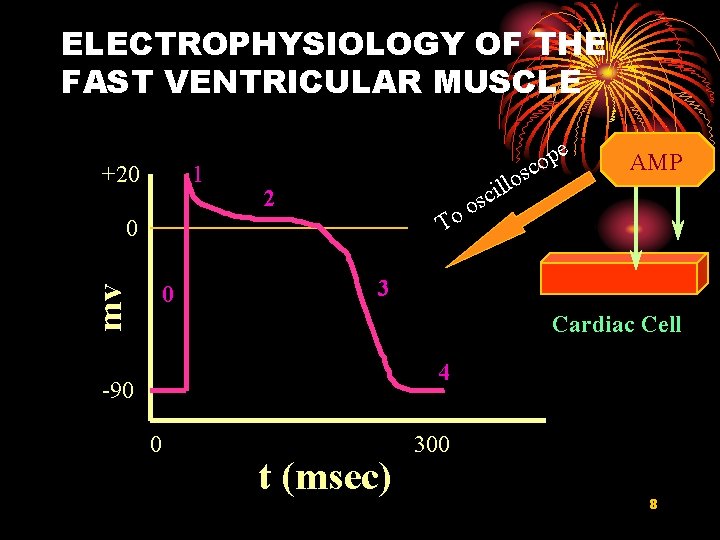
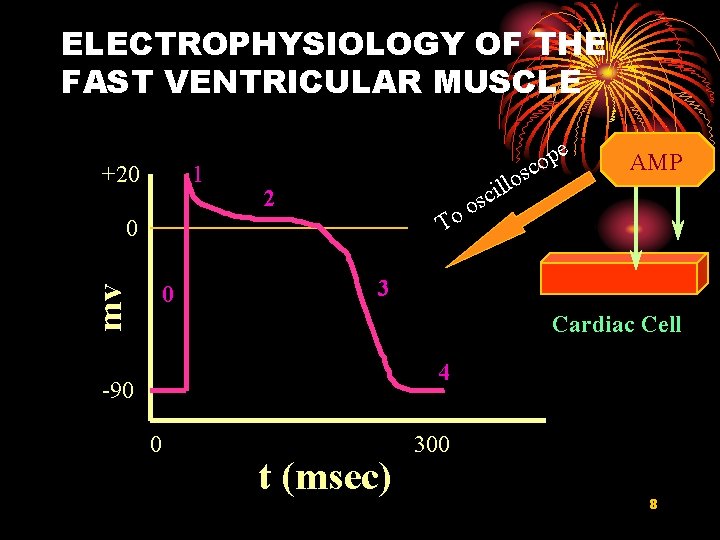
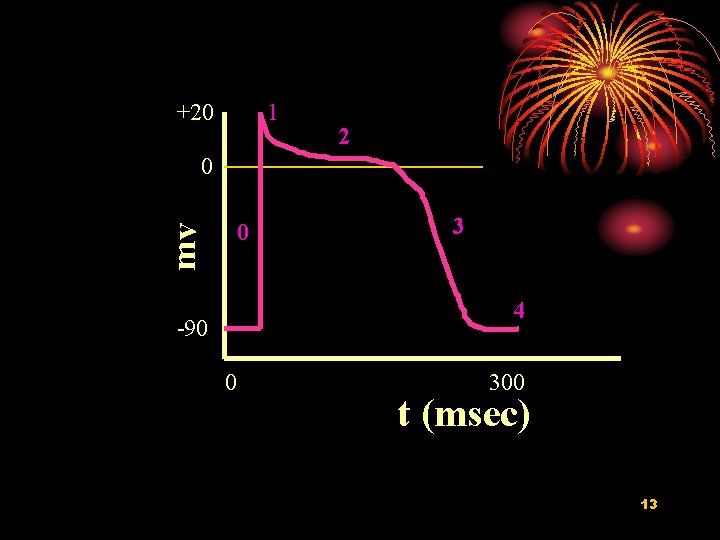
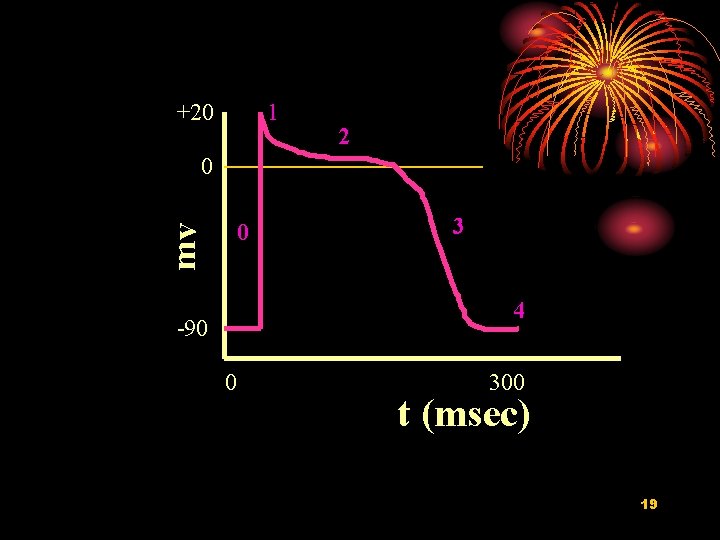
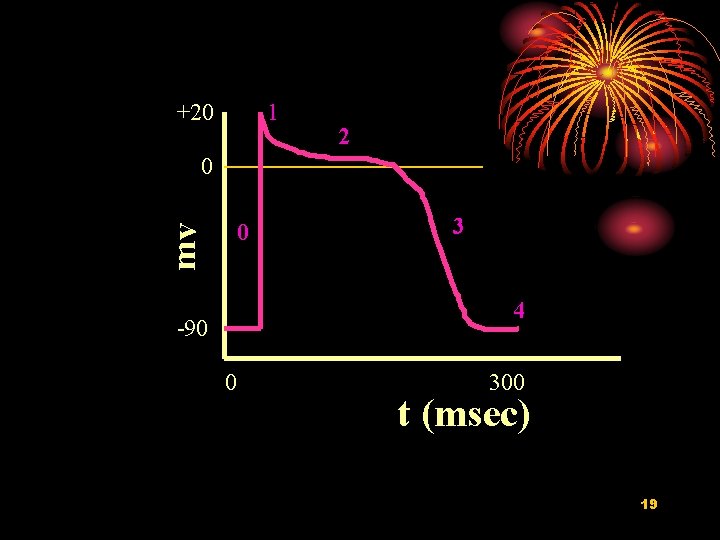
ELECTROPHYSIOLOGY OF THE FAST VENTRICULAR MUSCLE +20 1 e p o c s lo l i sc 2 o o T 0 mv 0 AMP 3 Cardiac Cell 4 -90 0 t (msec) 300 8
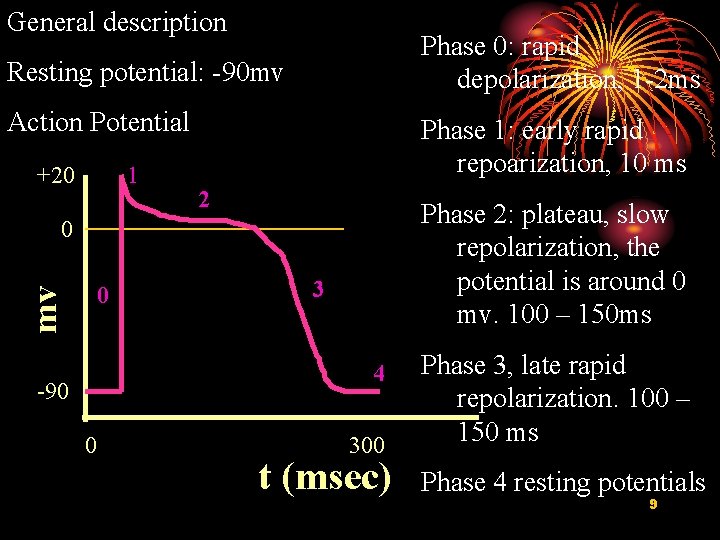
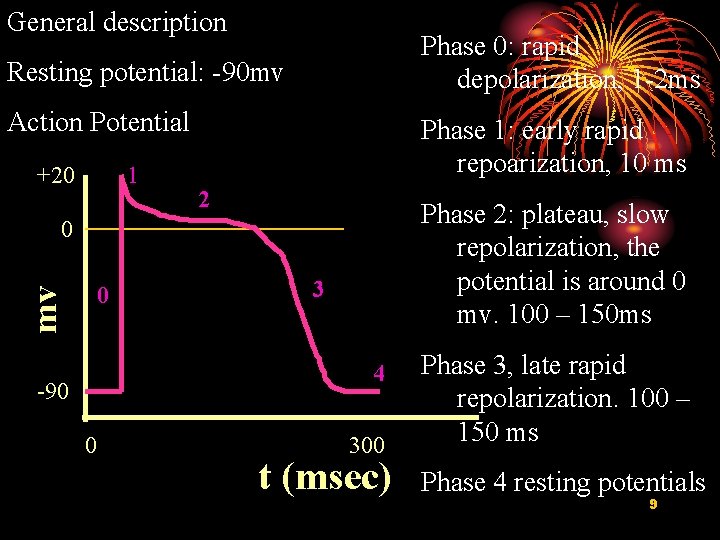
General description Phase 0: rapid depolarization, 1 -2 ms Resting potential: -90 mv Action Potential +20 1 Phase 1: early rapid repoarization, 10 ms 2 Phase 2: plateau, slow repolarization, the potential is around 0 mv. 100 – 150 ms 0 mv 0 3 4 -90 0 300 t (msec) Phase 3, late rapid repolarization. 100 – 150 ms Phase 4 resting potentials 9
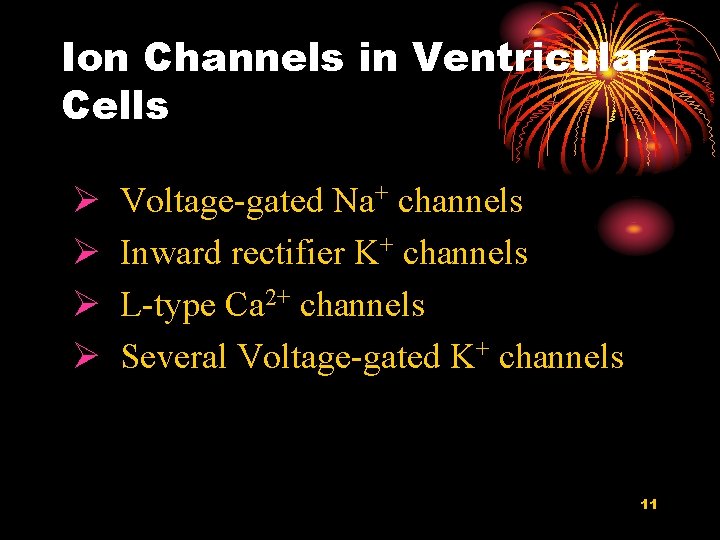
Ion Channels in Working Muscle Ø Essentially same in atrial and ventricular muscle Ø Best understood in ventricular cells 10
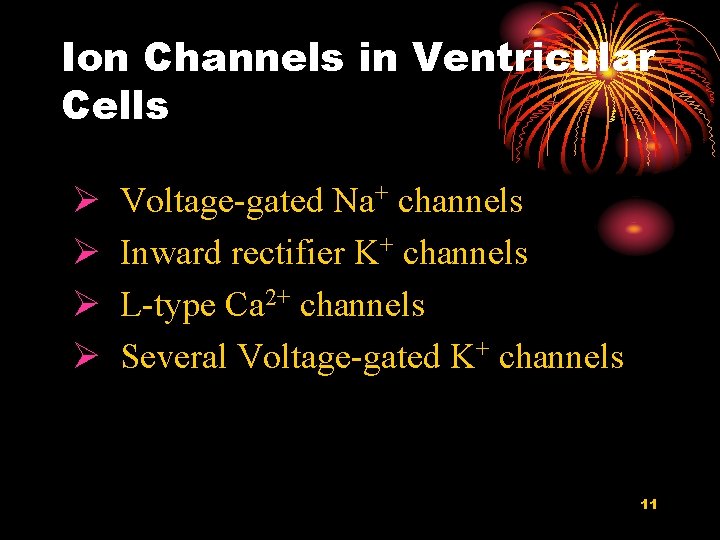
Ion Channels in Ventricular Cells Ø Ø Voltage-gated Na+ channels Inward rectifier K+ channels L-type Ca 2+ channels Several Voltage-gated K+ channels 11
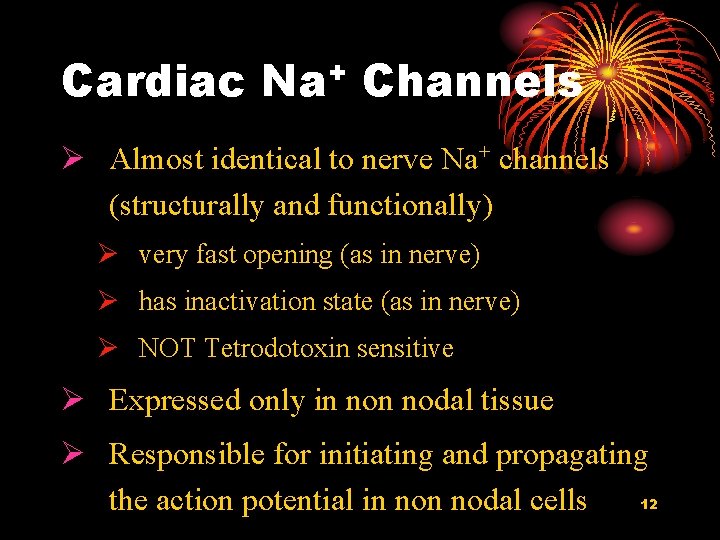
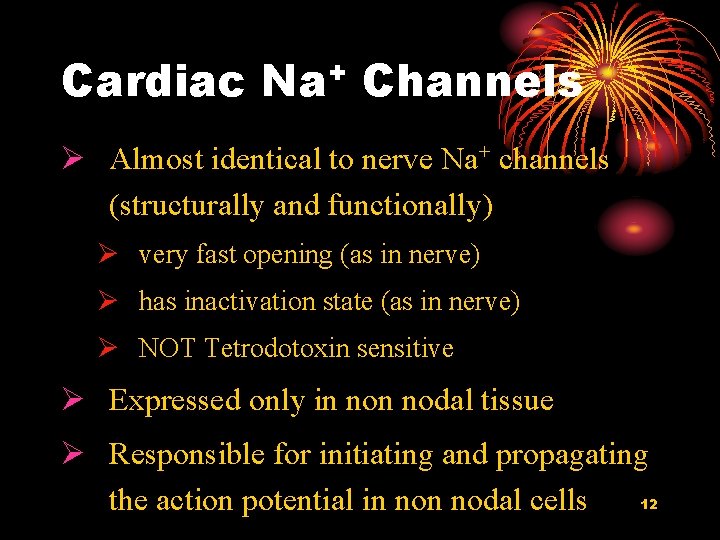
Cardiac + Na Channels Ø Almost identical to nerve Na+ channels (structurally and functionally) Ø very fast opening (as in nerve) Ø has inactivation state (as in nerve) Ø NOT Tetrodotoxin sensitive Ø Expressed only in nodal tissue Ø Responsible for initiating and propagating 12 the action potential in nodal cells
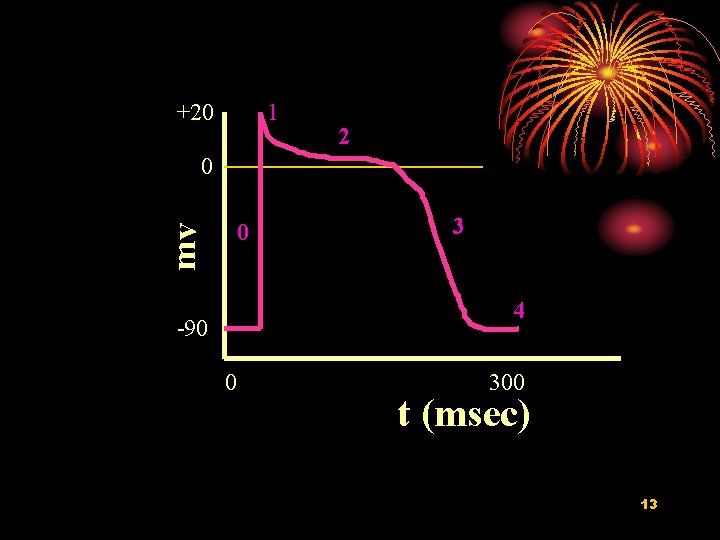
+20 1 2 0 mv 0 3 4 -90 0 300 t (msec) 13
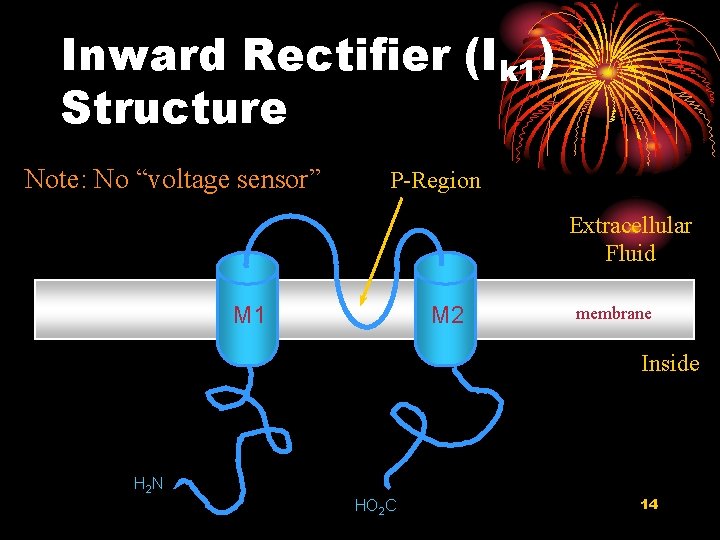
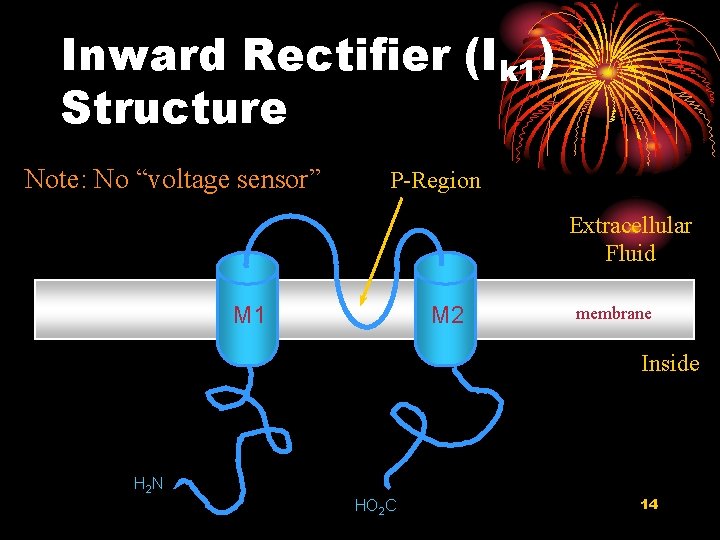
Inward Rectifier (Ik 1) Structure Note: No “voltage sensor” P-Region Extracellular Fluid M 1 M 2 membrane Inside H 2 N HO 2 C 14
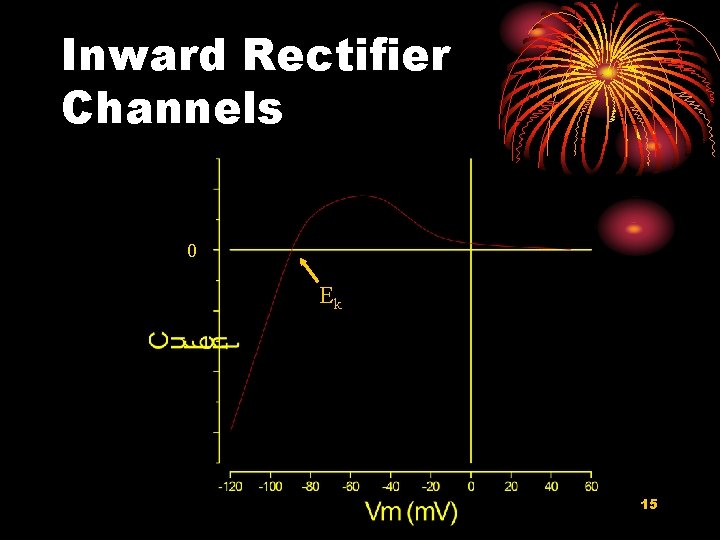
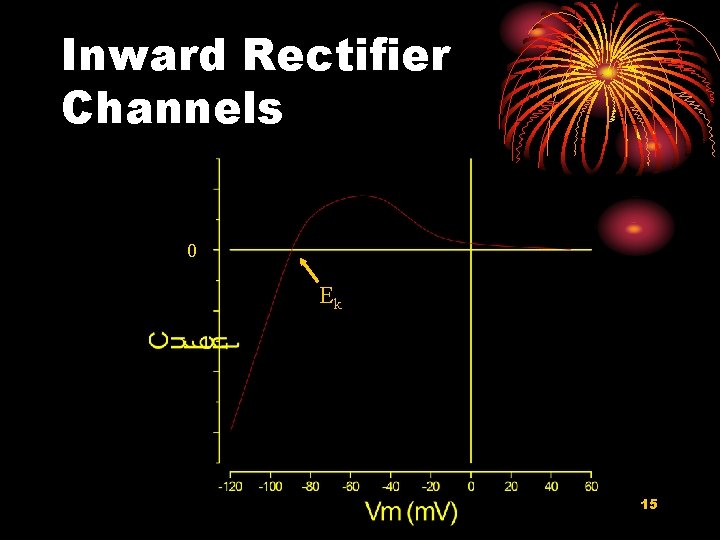
Inward Rectifier Channels 0 Ek 15
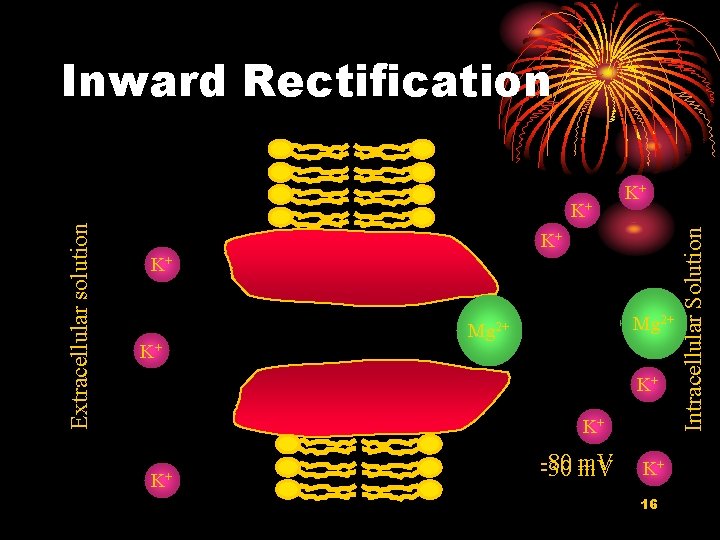
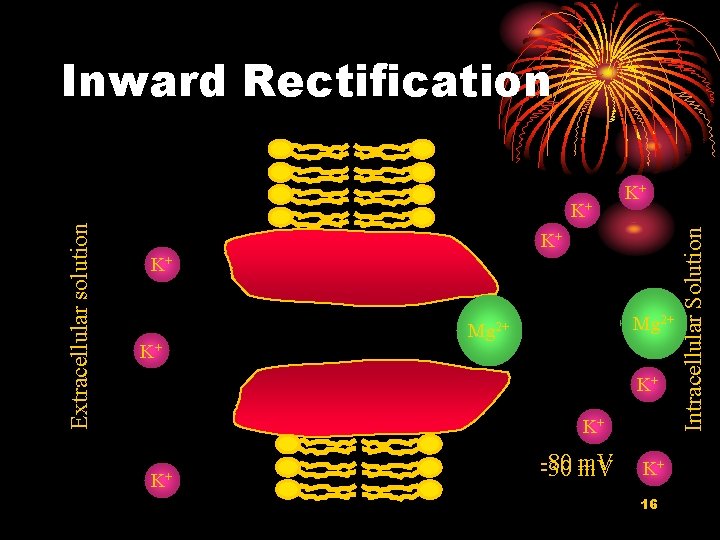
Inward Rectification K+ K+ K+ Mg 2+ K+ K+ K+ -80 -30 m. V K+ 16 Intracellular Solution Extracellular solution K+ K+
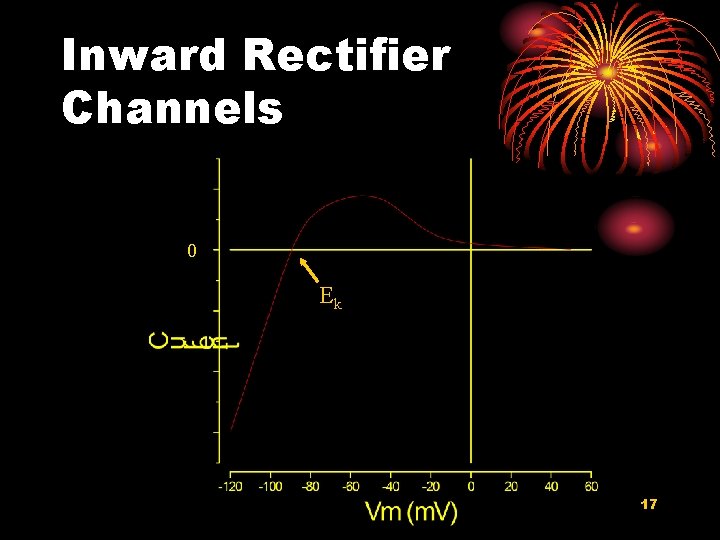
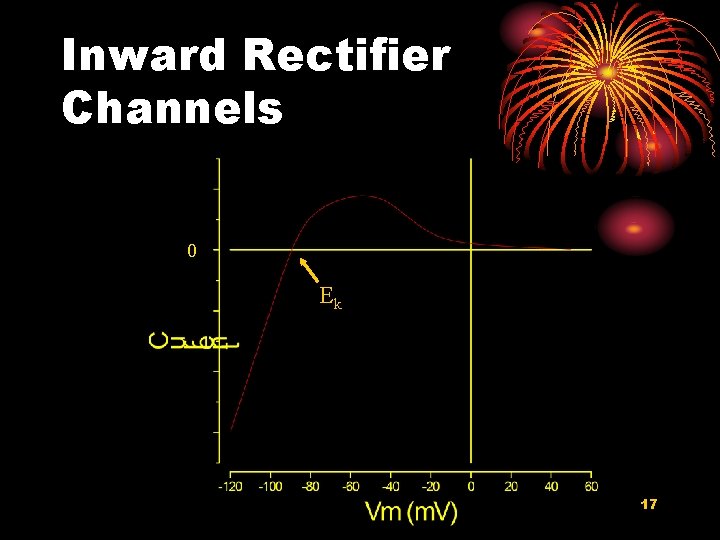
Inward Rectifier Channels 0 Ek 17
Role for Inward Rectifier Ø Expressed primarily in nodal tissues Ø Sets resting potential in atrial and ventricular muscle Ø Contributes to the late phase of action potential repolarization in nodal cells 18
+20 1 2 0 mv 0 3 4 -90 0 300 t (msec) 19
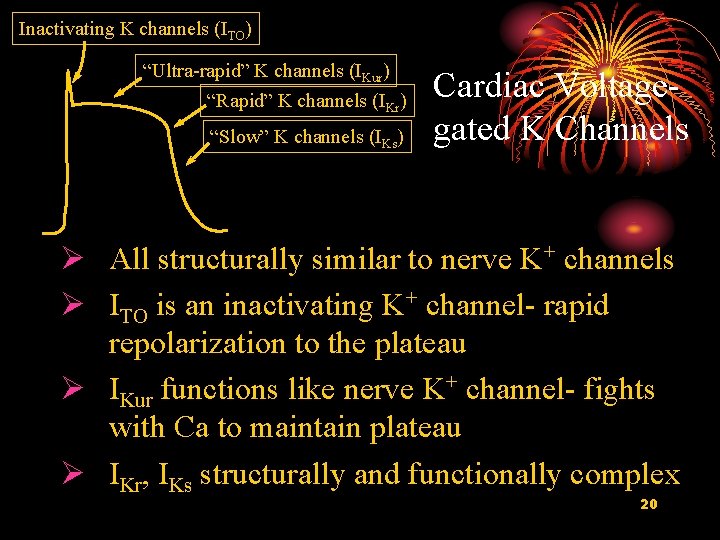
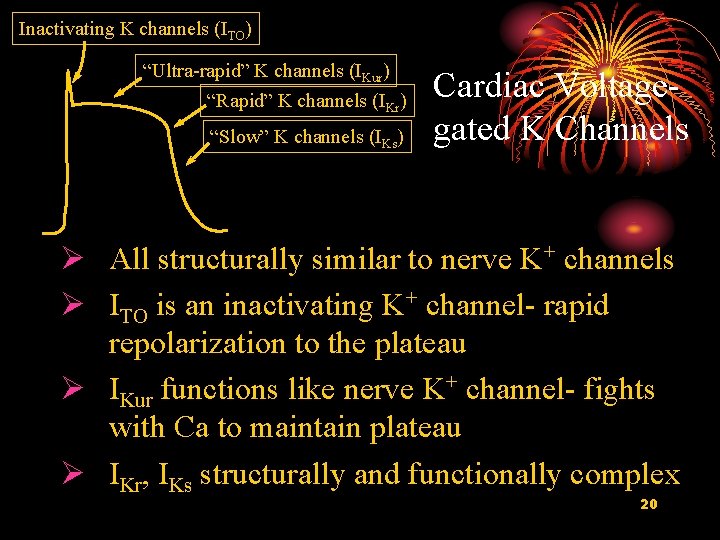
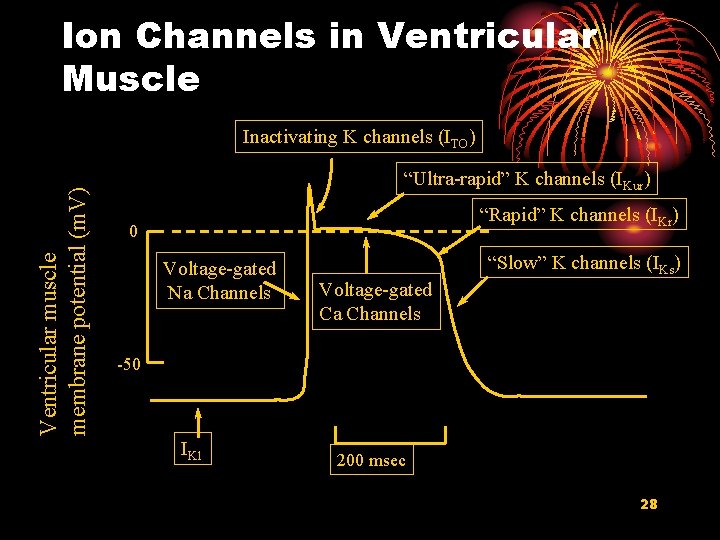
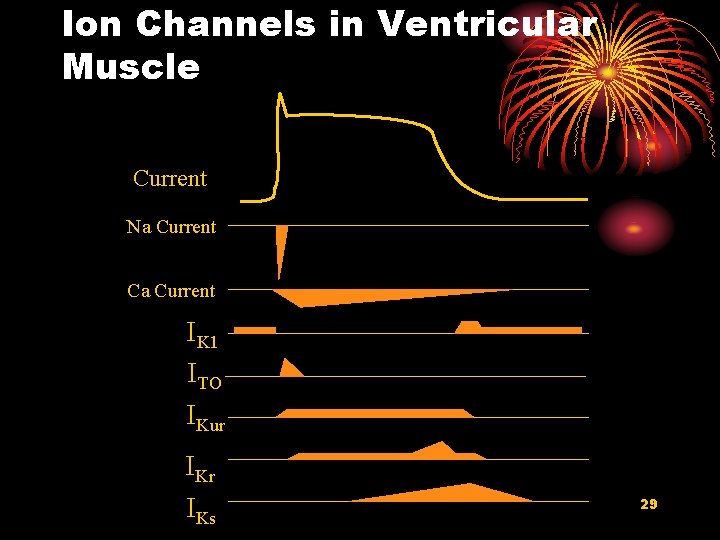
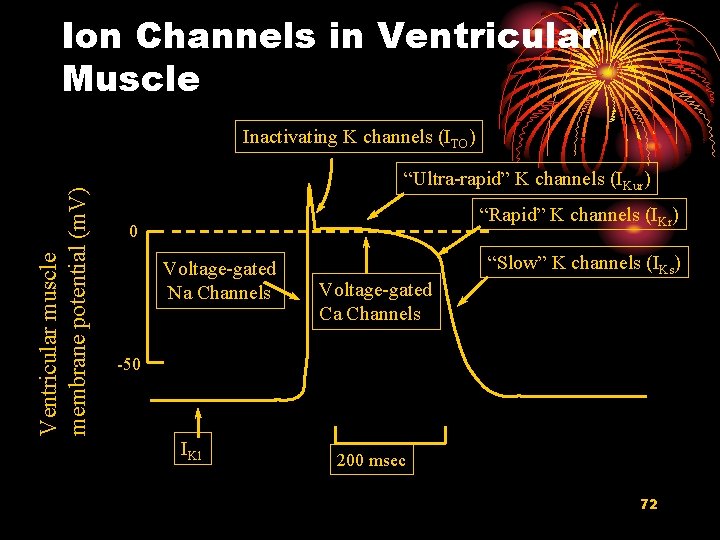
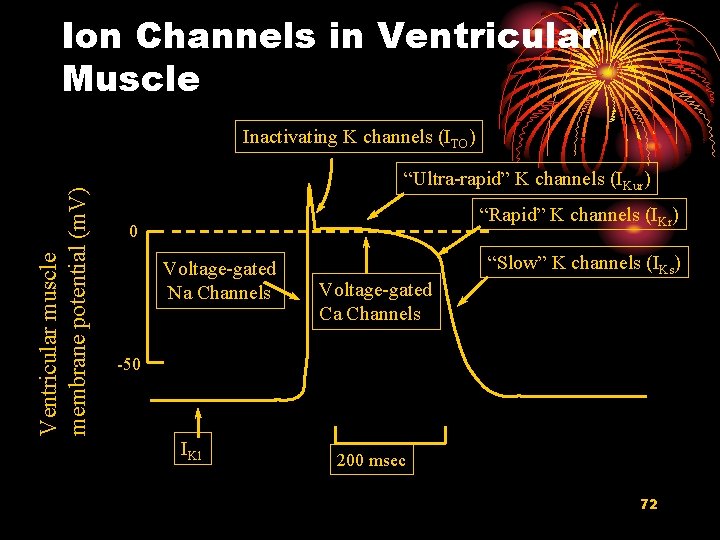
Inactivating K channels (ITO) “Ultra-rapid” K channels (IKur) “Rapid” K channels (IKr) “Slow” K channels (IKs) Cardiac Voltagegated K Channels Ø All structurally similar to nerve K+ channels Ø ITO is an inactivating K+ channel- rapid repolarization to the plateau Ø IKur functions like nerve K+ channel- fights with Ca to maintain plateau Ø IKr, IKs structurally and functionally complex 20
Cardiac 2+ Ca Channels Ø L-type Ø Structurally rather similar to Na+ channels Ø Some functional similarity to Na+ channels Ø depolarization opens Ca 2+ channels Ø Functionally different than Na+ channels Ø slower to open Ø very slow, rather incomplete inactivation Ø generates much less current flow 21
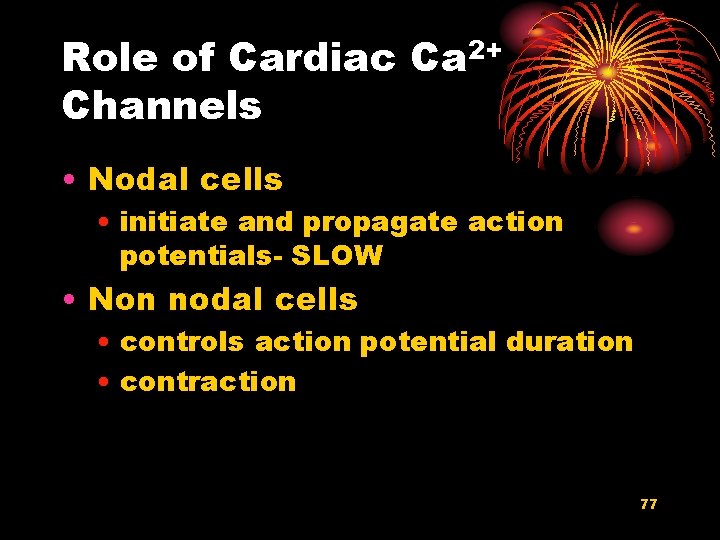
Role of Cardiac Ca 2+ Channels Ø Nodal cells Ø initiate and propagate action potentials- SLOW Ø Non nodal cells Ø controls action potential duration Ø contraction 22
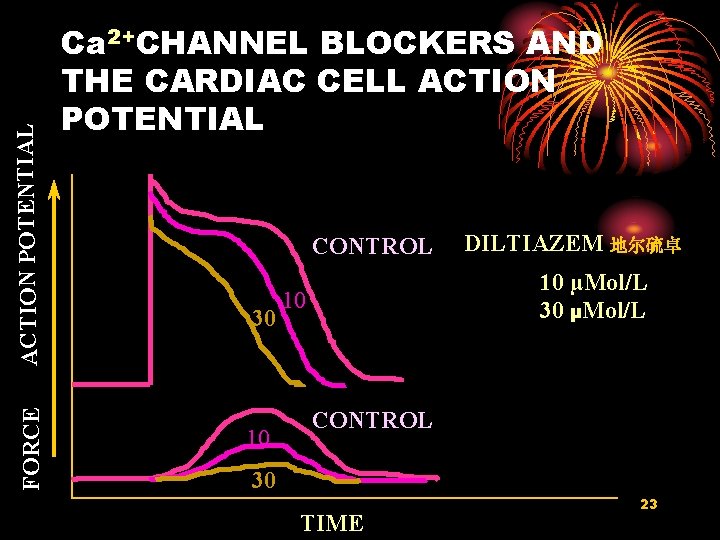
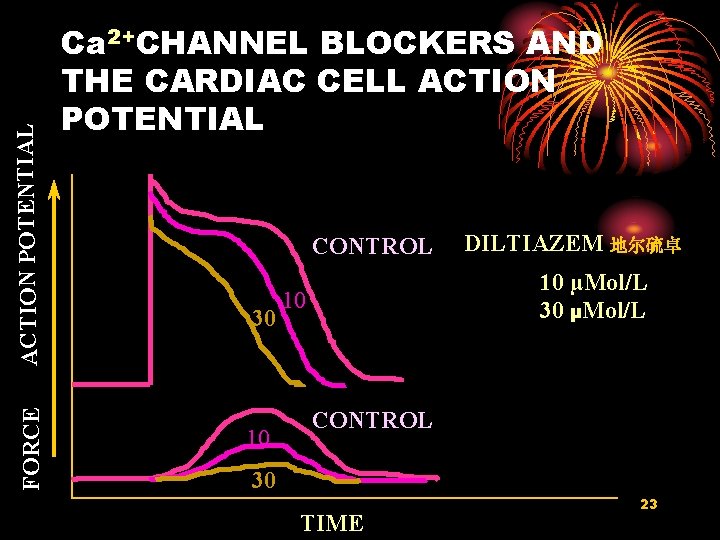
ACTION POTENTIAL FORCE Ca 2+CHANNEL BLOCKERS AND THE CARDIAC CELL ACTION POTENTIAL CONTROL 30 10 DILTIAZEM 地尔硫卓 10 µMol/L 30 µMol/L 10 CONTROL 30 TIME 23
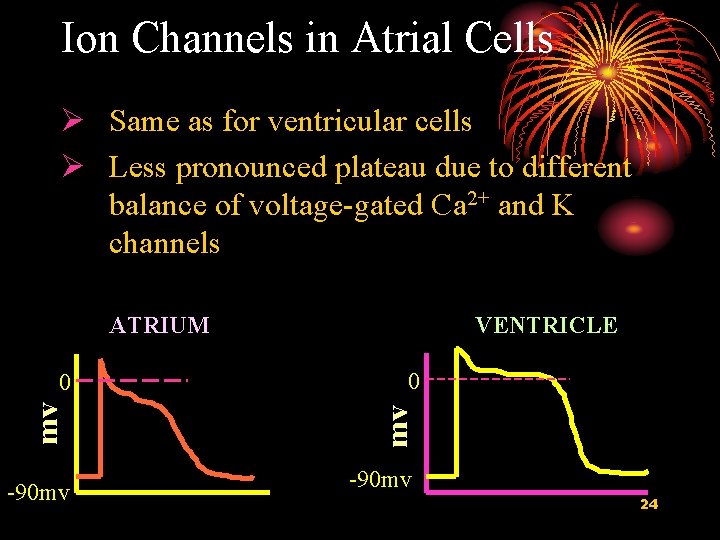
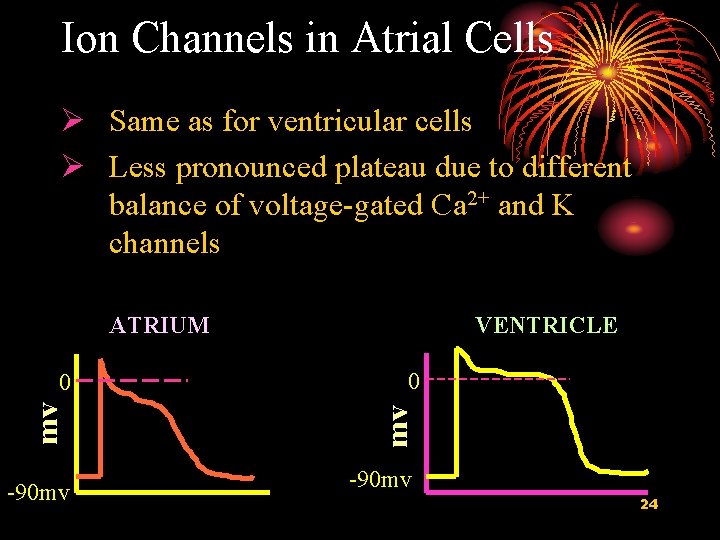
Ion Channels in Atrial Cells Ø Same as for ventricular cells Ø Less pronounced plateau due to different balance of voltage-gated Ca 2+ and K channels ATRIUM -90 mv 0 mv mv 0 VENTRICLE -90 mv 24
OVERVIEW OF SPECIFIC EVENTS IN THE VENTRICULAR ACTION POTENTIAL 25
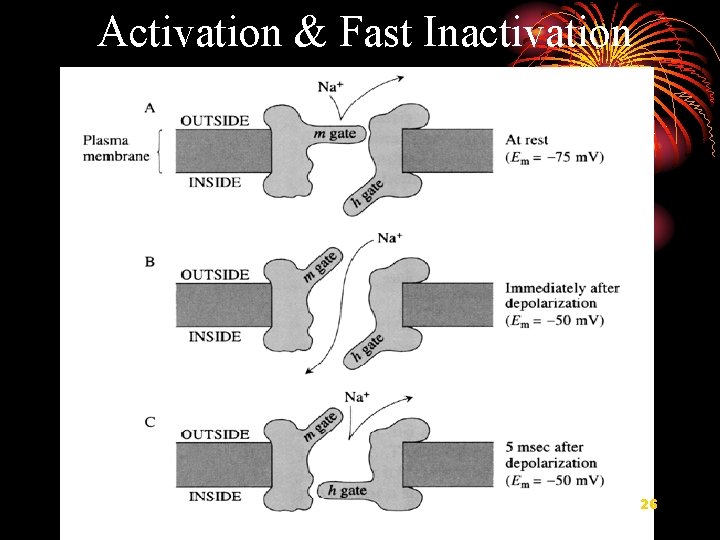
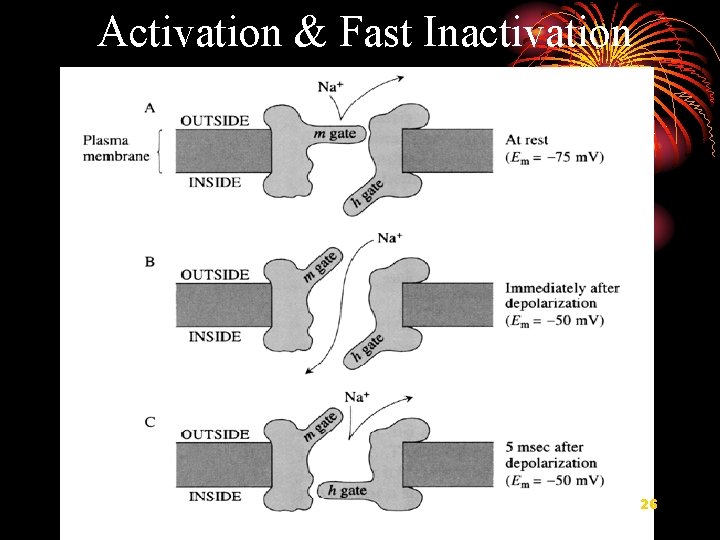
Activation & Fast Inactivation 26
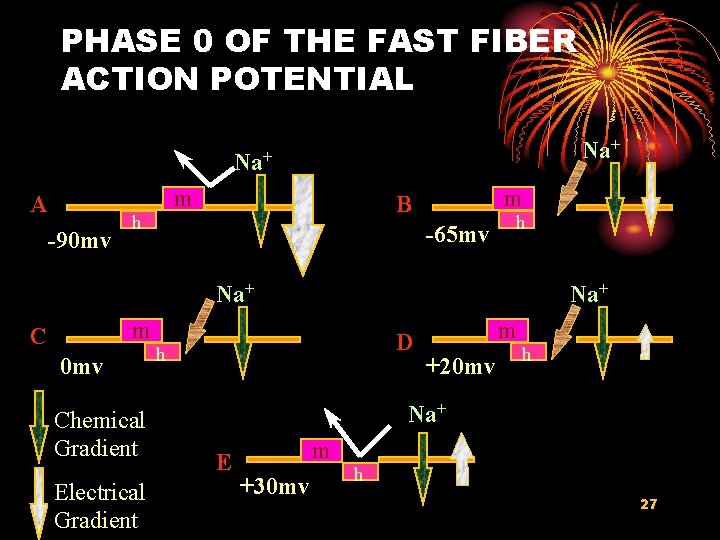
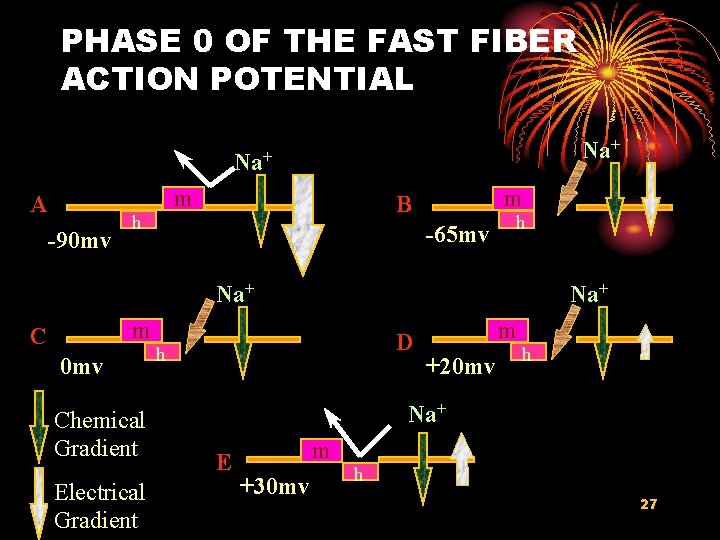
PHASE 0 OF THE FAST FIBER ACTION POTENTIAL Na+ m A -90 mv m m B h -65 mv h Na+ m C 0 mv Chemical Gradient Electrical Gradient D h m +20 mv h Na+ E m +30 mv h 27
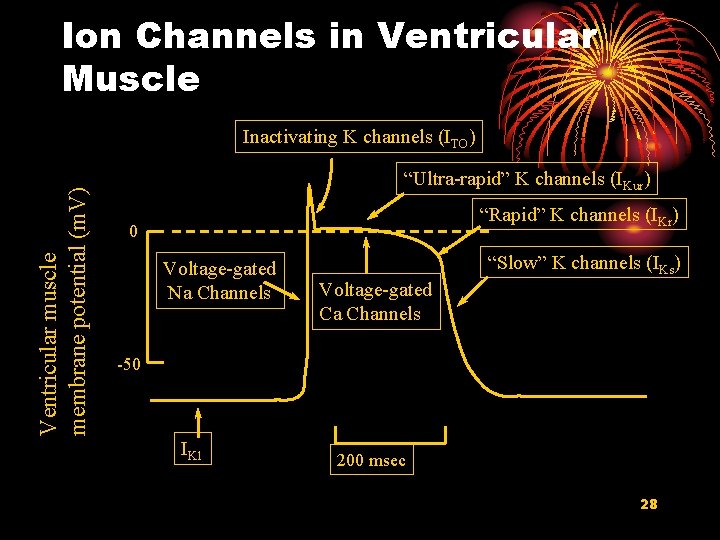
Ion Channels in Ventricular Muscle Ventricular muscle membrane potential (m. V) Inactivating K channels (ITO) “Ultra-rapid” K channels (IKur) “Rapid” K channels (IKr) 0 Voltage-gated Na Channels “Slow” K channels (IKs) Voltage-gated Ca Channels -50 IK 1 200 msec 28
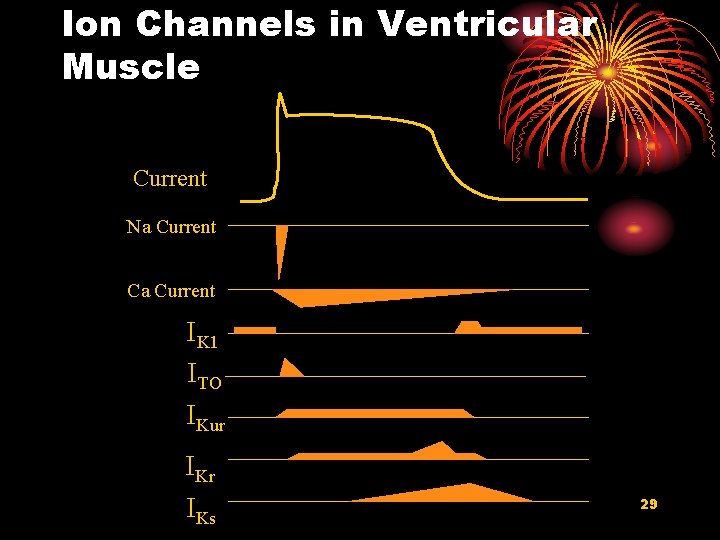
Ion Channels in Ventricular Muscle Current Na Current Ca Current IK 1 ITO IKur IKs 29
2. Transmembrane Potential of Rhythmic Cells 30
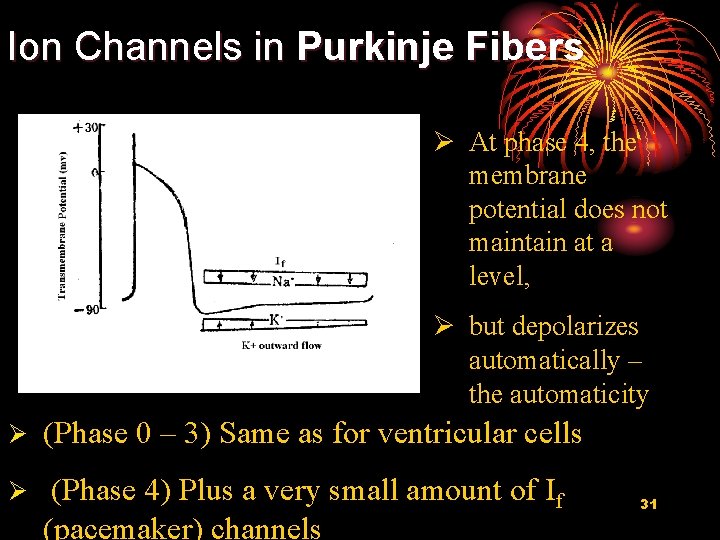
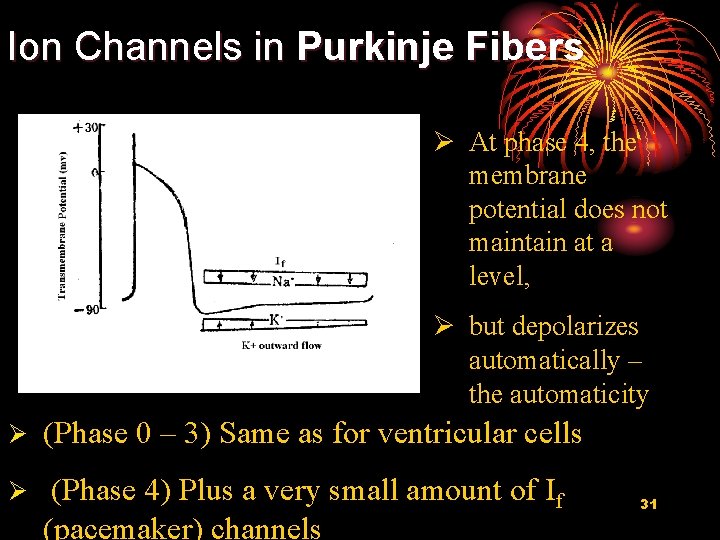
Ion Channels in Purkinje Fibers Ø At phase 4, the membrane potential does not maintain at a level, Ø but depolarizes automatically – the automaticity Ø (Phase 0 – 3) Same as for ventricular cells Ø (Phase 4) Plus a very small amount of If (pacemaker) channels 31
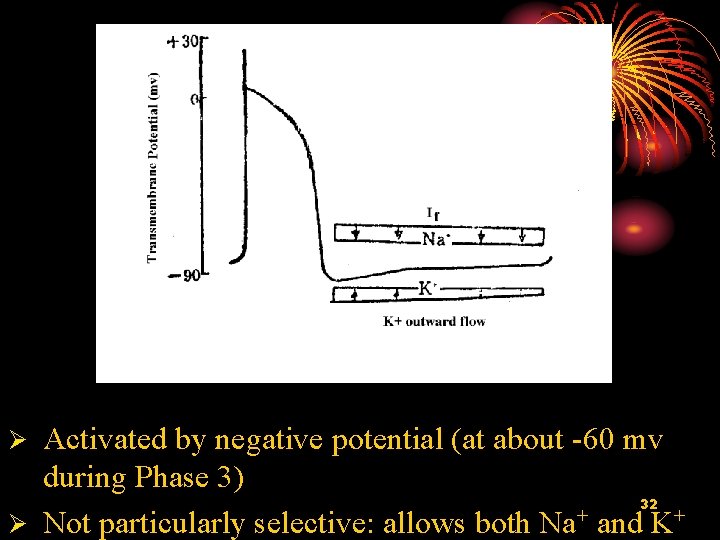
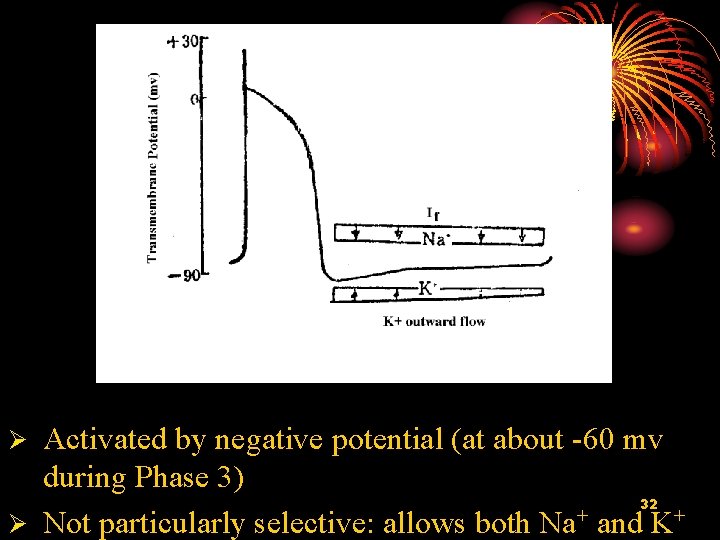
Activated by negative potential (at about -60 mv during Phase 3) 32 + Ø Not particularly selective: allows both Na and K+ Ø
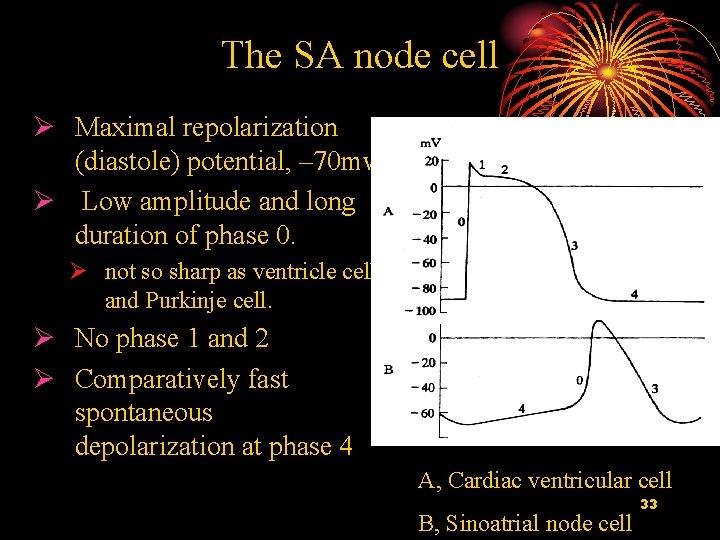
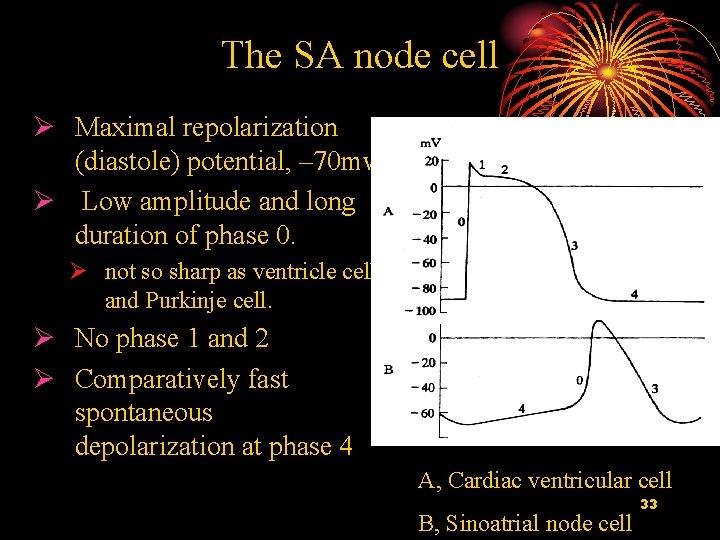
The SA node cell Ø Maximal repolarization (diastole) potential, – 70 mv Ø Low amplitude and long duration of phase 0. Ø not so sharp as ventricle cell and Purkinje cell. Ø No phase 1 and 2 Ø Comparatively fast spontaneous depolarization at phase 4 A, Cardiac ventricular cell B, Sinoatrial node cell 33
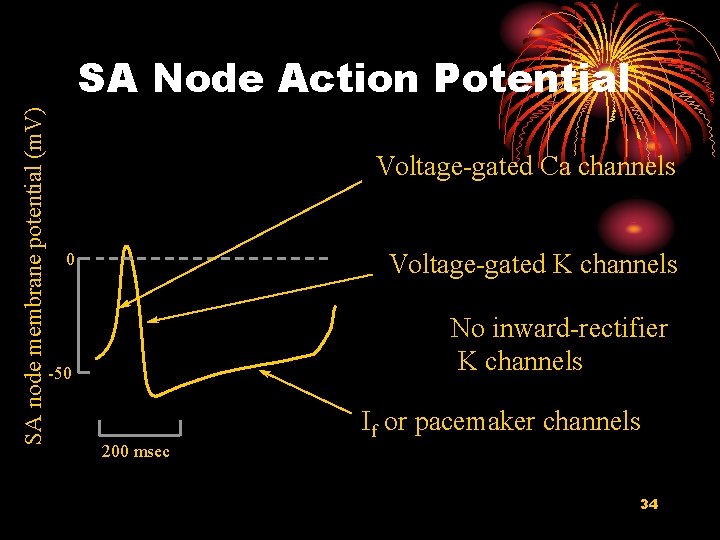
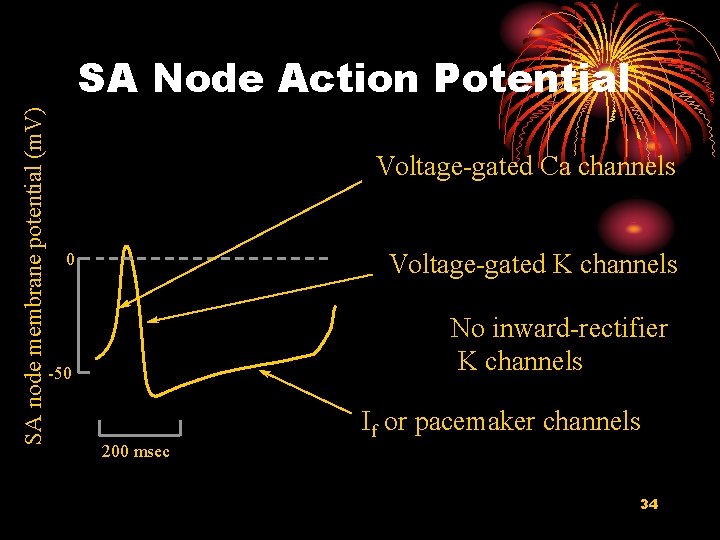
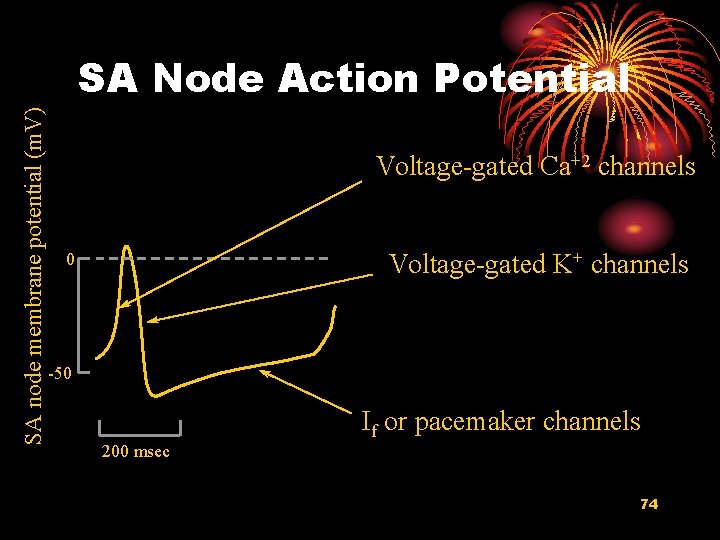
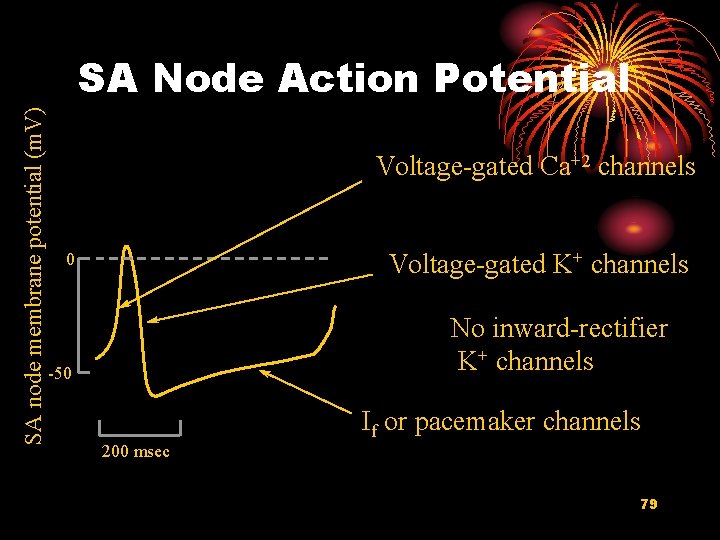
SA node membrane potential (m. V) SA Node Action Potential Voltage-gated Ca channels Voltage-gated K channels 0 No inward-rectifier K channels -50 If or pacemaker channels 200 msec 34
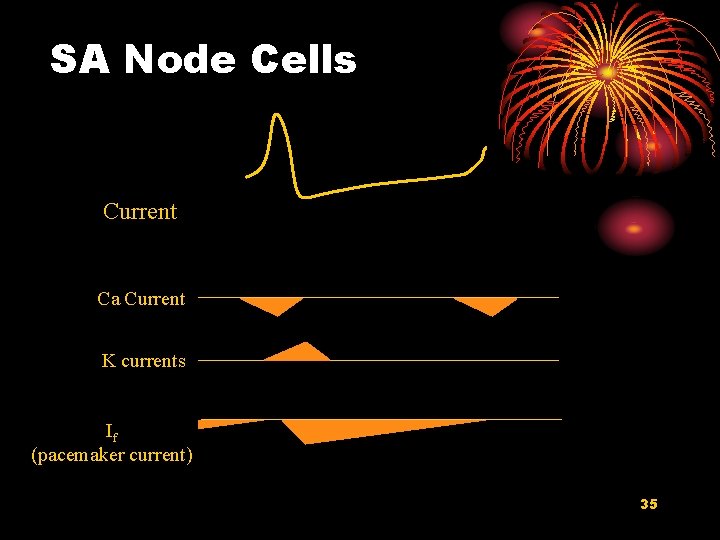
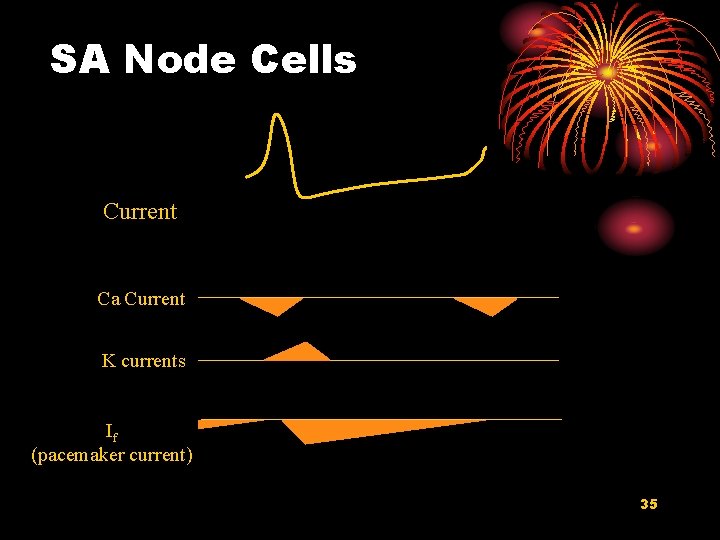
SA Node Cells Current Ca Current K currents If (pacemaker current) 35
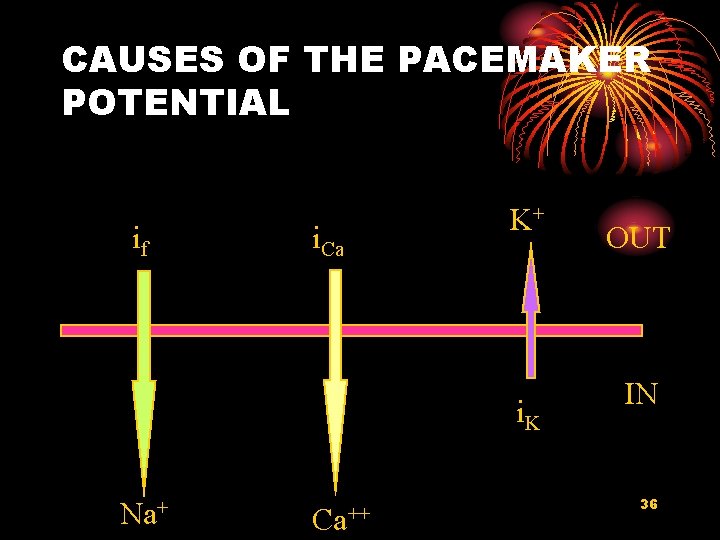
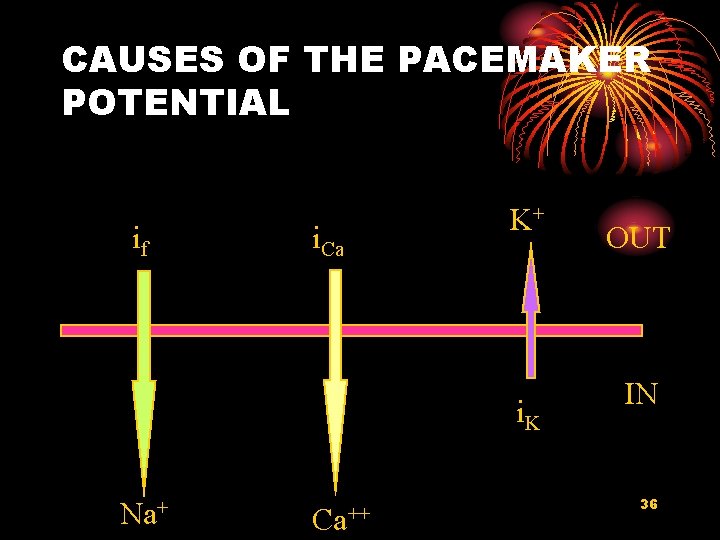
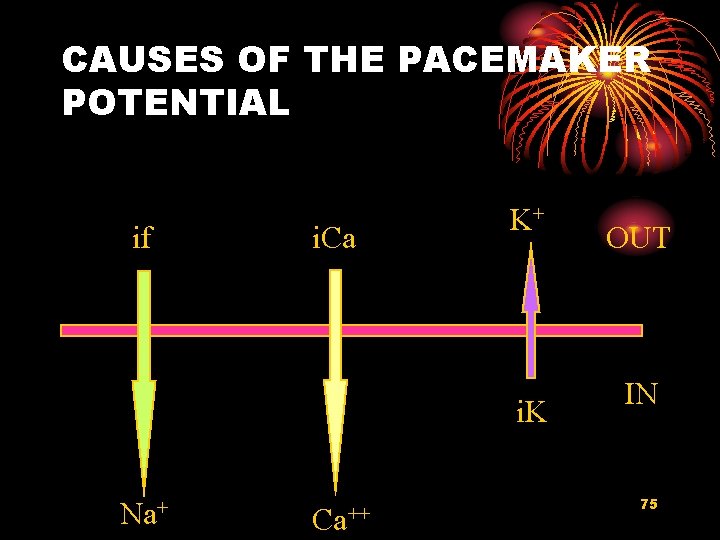
CAUSES OF THE PACEMAKER POTENTIAL if i. Ca K+ i. K Na+ Ca++ OUT IN 36
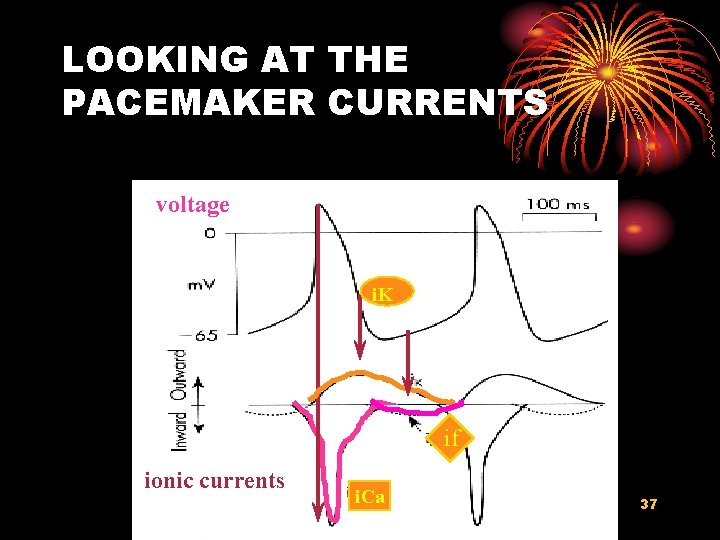
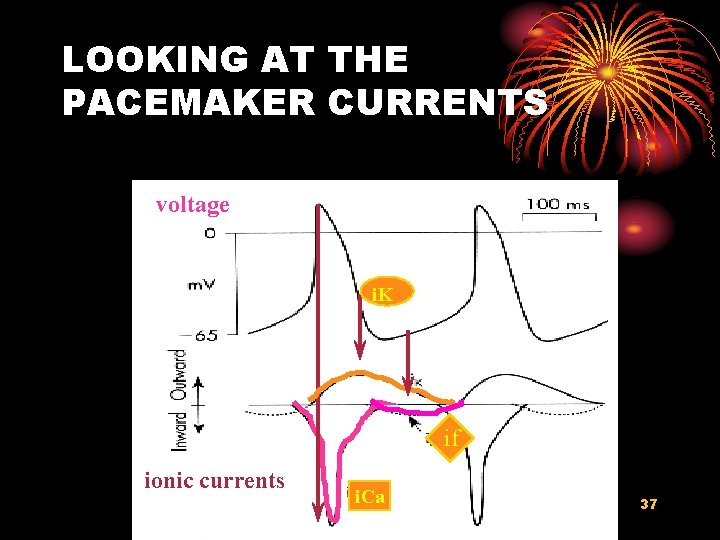
LOOKING AT THE PACEMAKER CURRENTS voltage i. K if ionic currents i. Ca 37
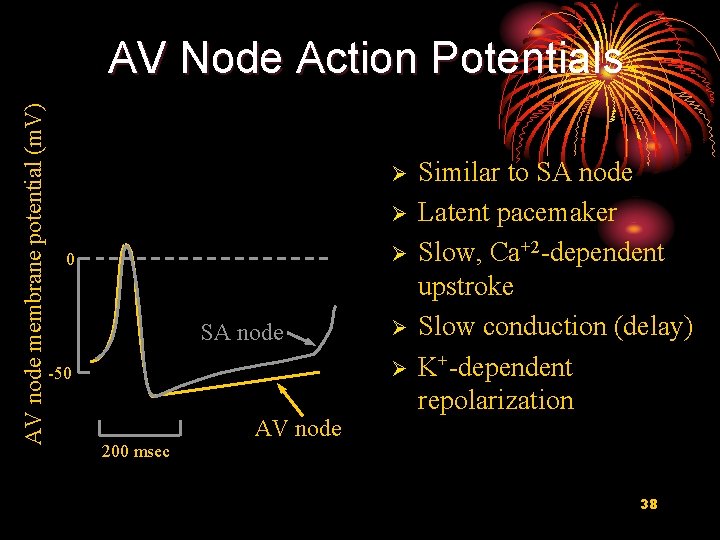
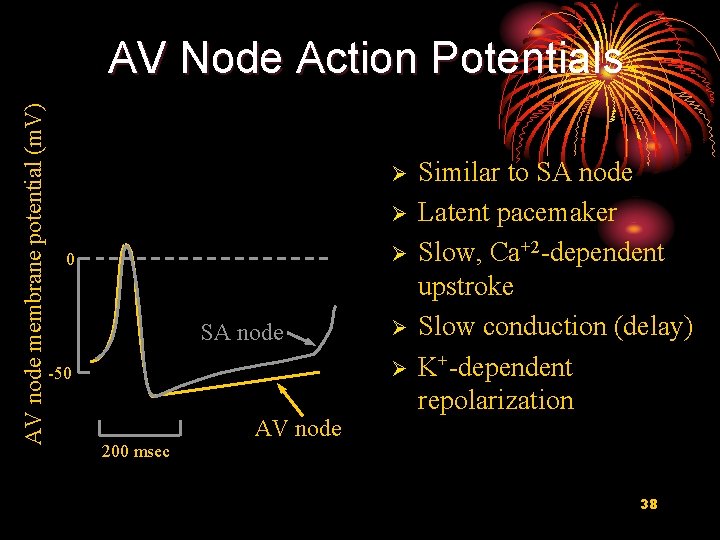
AV node membrane potential (m. V) AV Node Action Potentials Ø Ø Ø 0 SA node Ø Ø -50 AV node Similar to SA node Latent pacemaker Slow, Ca+2 -dependent upstroke Slow conduction (delay) K+-dependent repolarization 200 msec 38
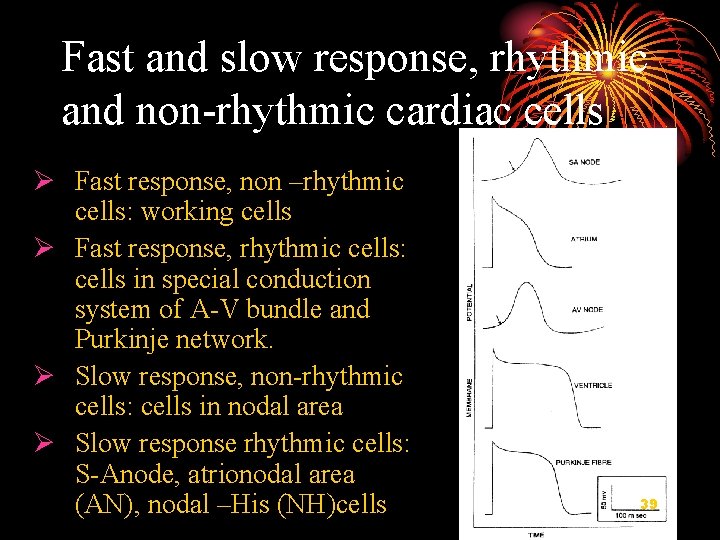
Fast and slow response, rhythmic and non-rhythmic cardiac cells Ø Fast response, non –rhythmic cells: working cells Ø Fast response, rhythmic cells: cells in special conduction system of A-V bundle and Purkinje network. Ø Slow response, non-rhythmic cells: cells in nodal area Ø Slow response rhythmic cells: S-Anode, atrionodal area (AN), nodal –His (NH)cells 39
II Electrical Properties of Cardiac Cells Excitability, Conductivity and Automaticity 40

1. Excitability of Cardiac Muscle 41
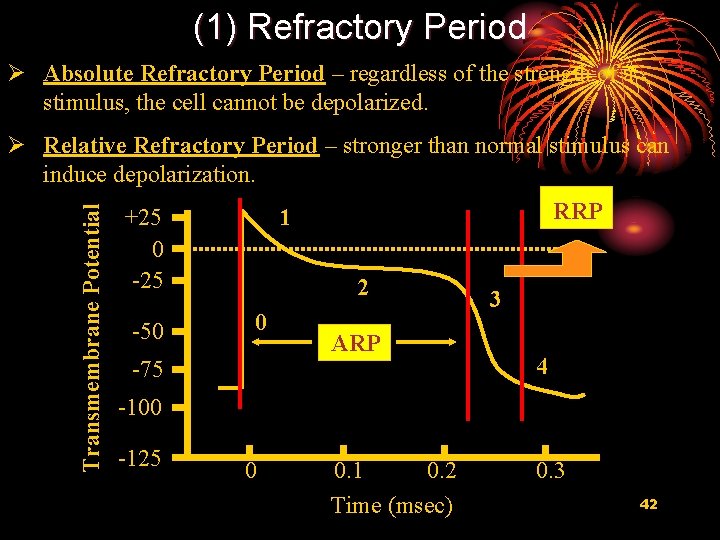
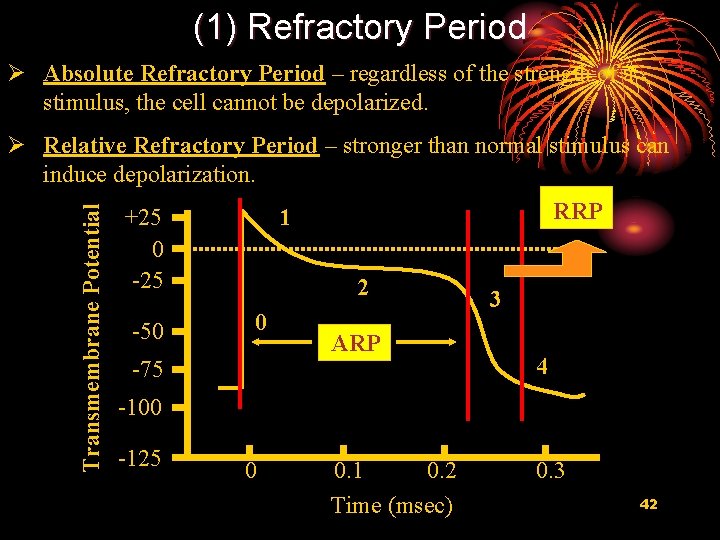
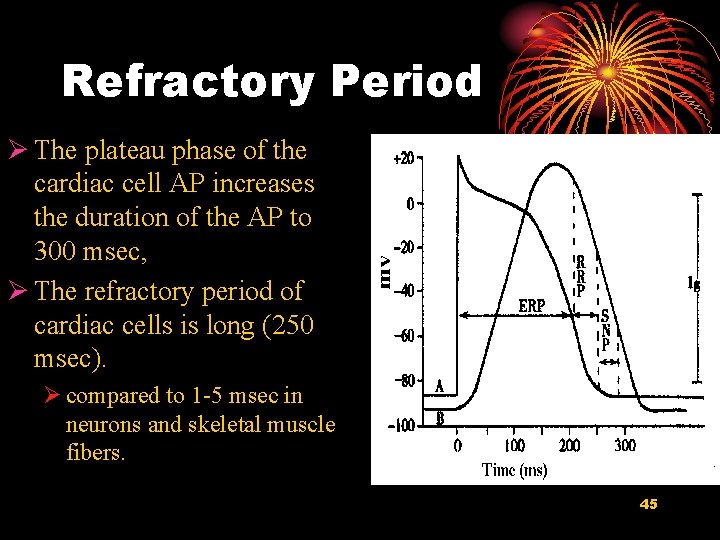
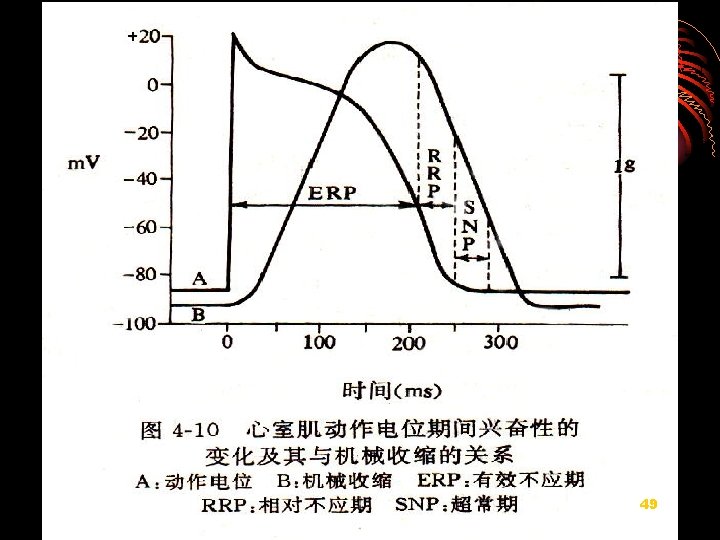
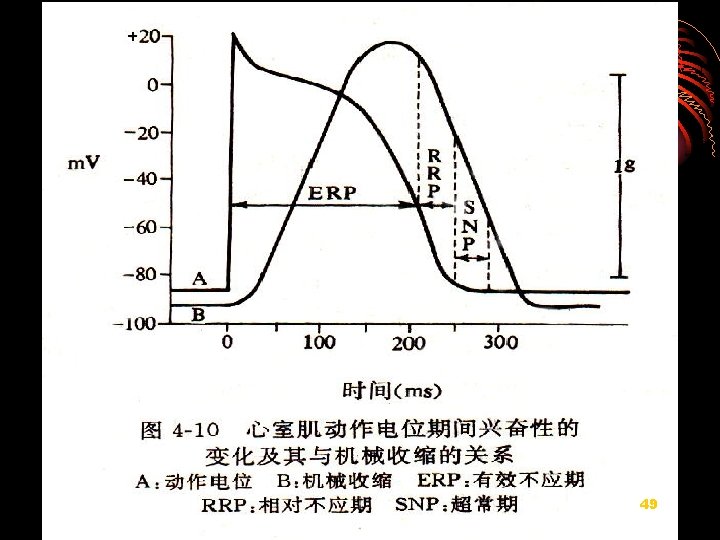
(1) Refractory Period Ø Absolute Refractory Period – regardless of the strength of a stimulus, the cell cannot be depolarized. Transmembrane Potential Ø Relative Refractory Period – stronger than normal stimulus can induce depolarization. +25 0 -25 -50 RRP 1 2 0 -75 ARP 3 4 -100 -125 0 0. 1 0. 2 Time (msec) 0. 3 42
Refractory Period Ø Absolute Refractory Period (ARC): Cardiac muscle cell completely insensitive to further stimulation Ø Relative Refractory Period (RRC): Cell exhibits reduced sensitivity to additional stimulation 43
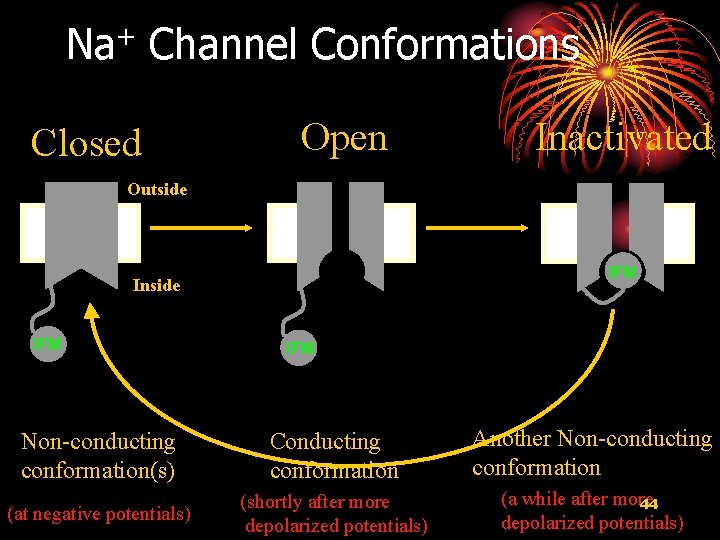
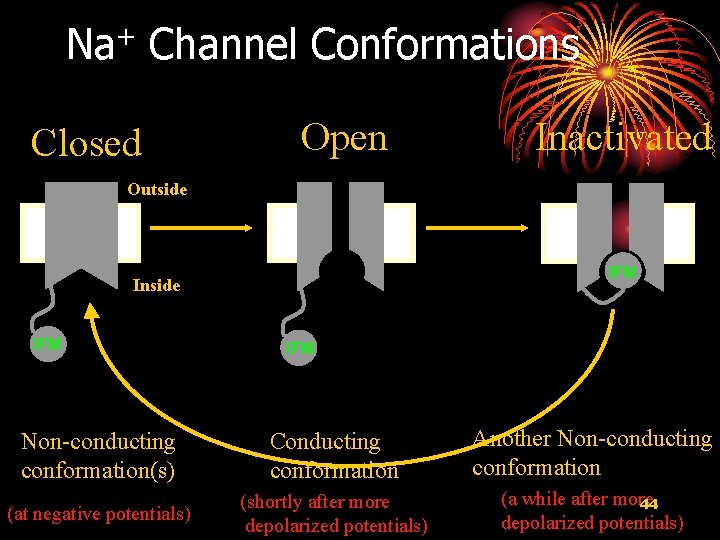
Na+ Channel Conformations Closed Open Inactivated Outside IFM Inside IFM Non-conducting conformation(s) Conducting conformation Another Non-conducting conformation (at negative potentials) (shortly after more depolarized potentials) (a while after more 44 depolarized potentials)
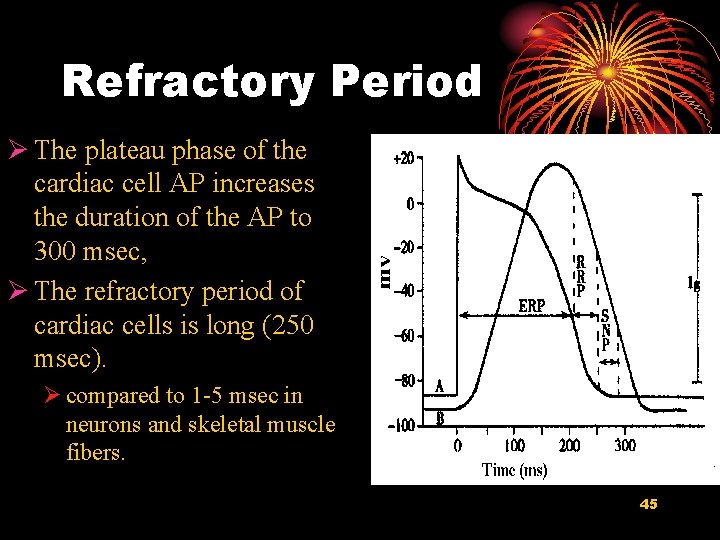
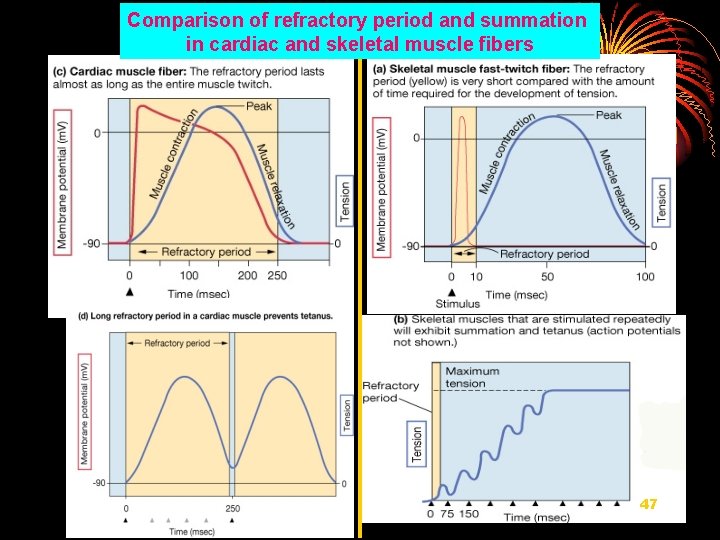
Refractory Period Ø The plateau phase of the cardiac cell AP increases the duration of the AP to 300 msec, Ø The refractory period of cardiac cells is long (250 msec). Ø compared to 1 -5 msec in neurons and skeletal muscle fibers. 45
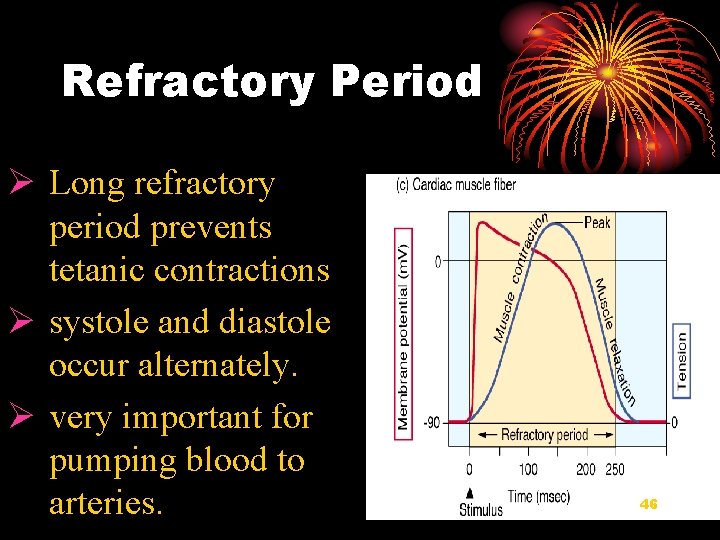
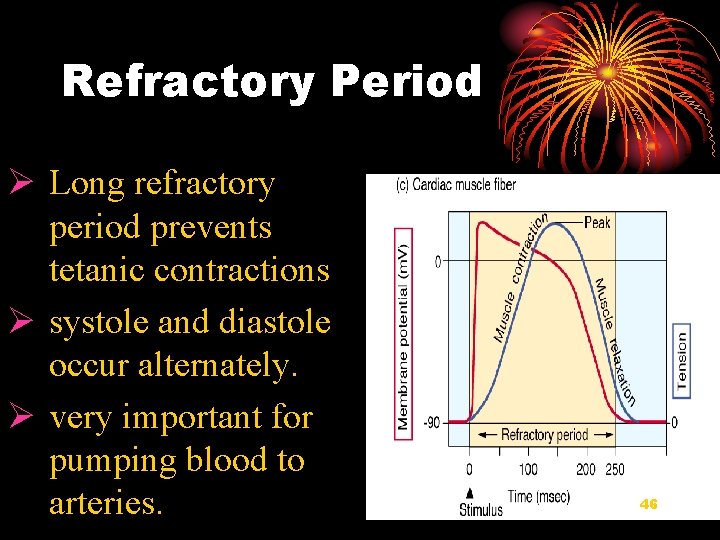
Refractory Period Ø Long refractory period prevents tetanic contractions Ø systole and diastole occur alternately. Ø very important for pumping blood to arteries. 46
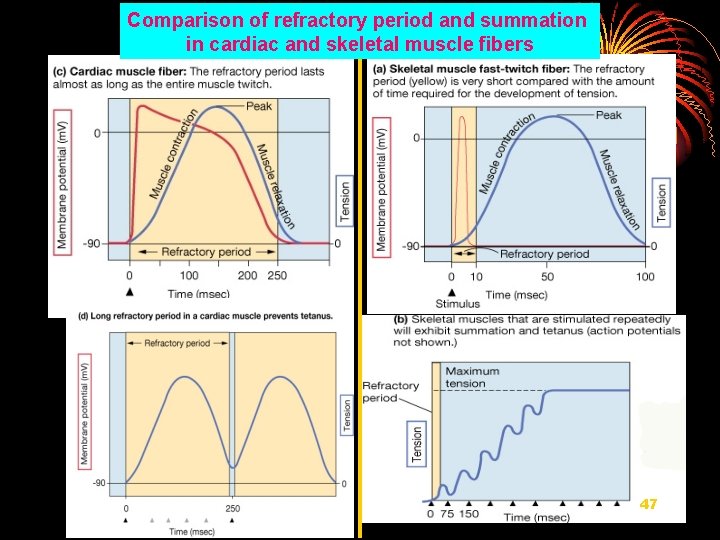
Comparison of refractory period and summation in cardiac and skeletal muscle fibers 47
Supranormal period: Ø Occurs early in phase 4 and is usually accompanied by negative after-potentials as some potassium channels close. Ø The membrane potential is about 80 mv - -90 mv, near threshold potential Absolute S. N. Rel 48
49
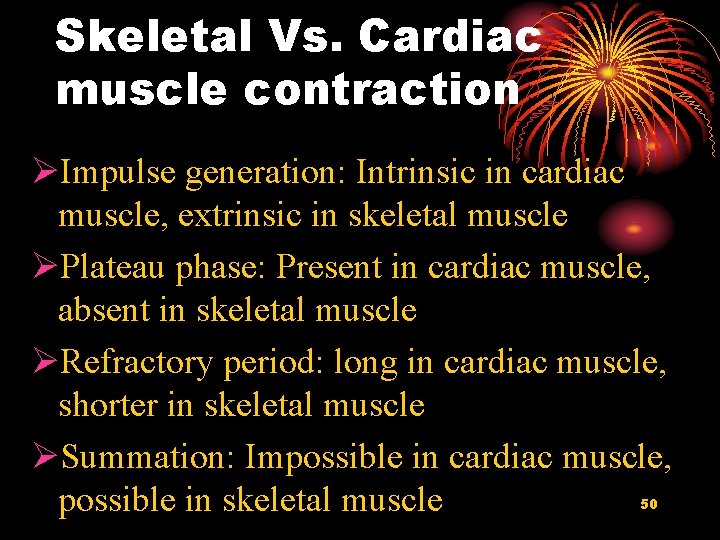
Skeletal Vs. Cardiac muscle contraction ØImpulse generation: Intrinsic in cardiac muscle, extrinsic in skeletal muscle ØPlateau phase: Present in cardiac muscle, absent in skeletal muscle ØRefractory period: long in cardiac muscle, shorter in skeletal muscle ØSummation: Impossible in cardiac muscle, possible in skeletal muscle 50
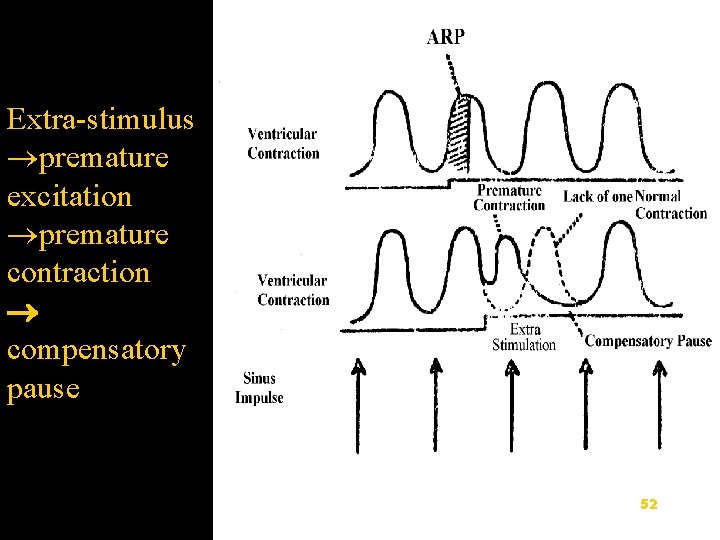
2) Premature excitation, premature contraction and compensatory pause 51
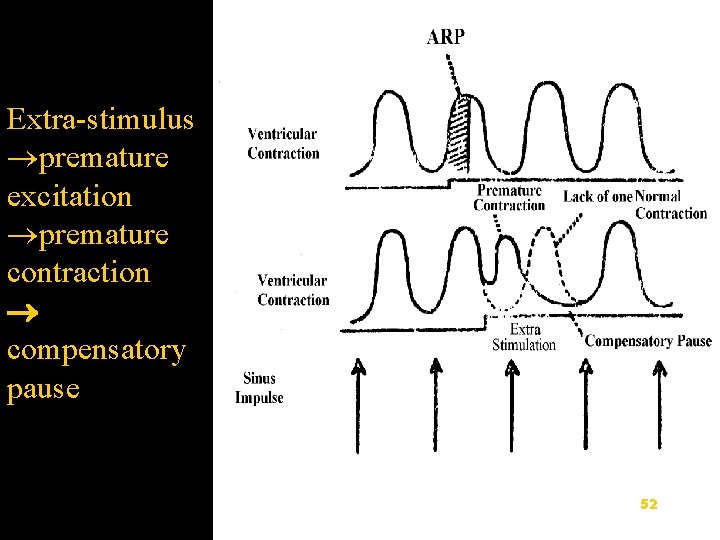
Extra-stimulus premature excitation premature contraction compensatory pause 52

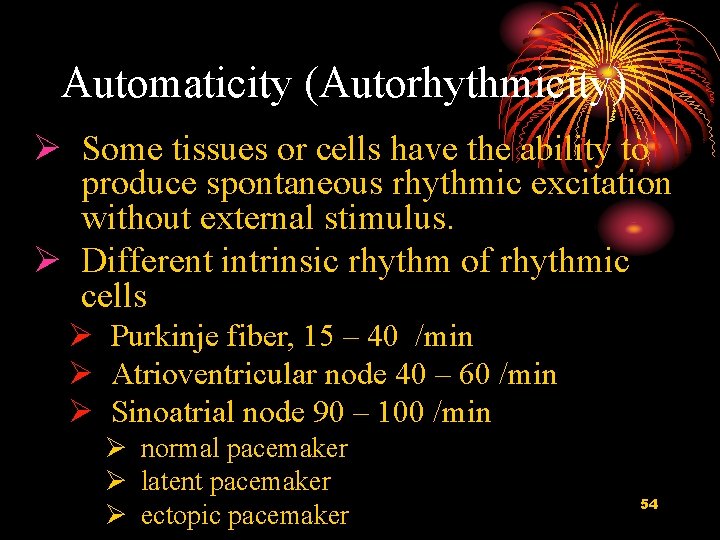
2. Automaticity (Autorhythmicity) 53
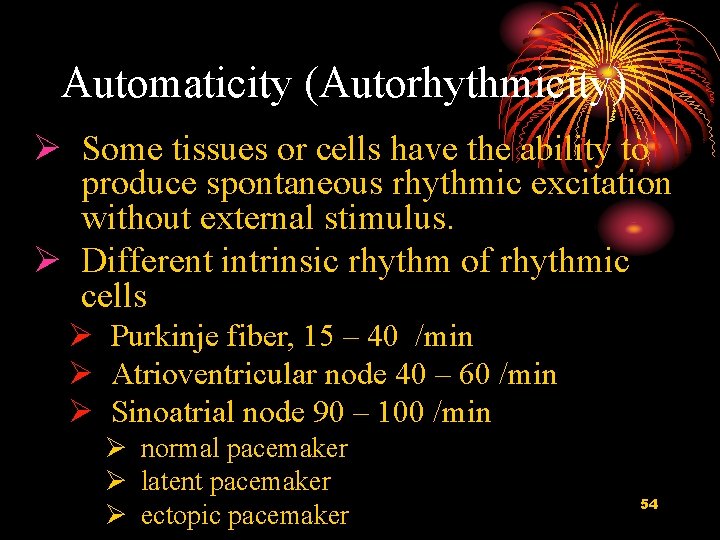
Automaticity (Autorhythmicity) Ø Some tissues or cells have the ability to produce spontaneous rhythmic excitation without external stimulus. Ø Different intrinsic rhythm of rhythmic cells Ø Purkinje fiber, 15 – 40 /min Ø Atrioventricular node 40 – 60 /min Ø Sinoatrial node 90 – 100 /min Ø normal pacemaker Ø latent pacemaker Ø ectopic pacemaker 54
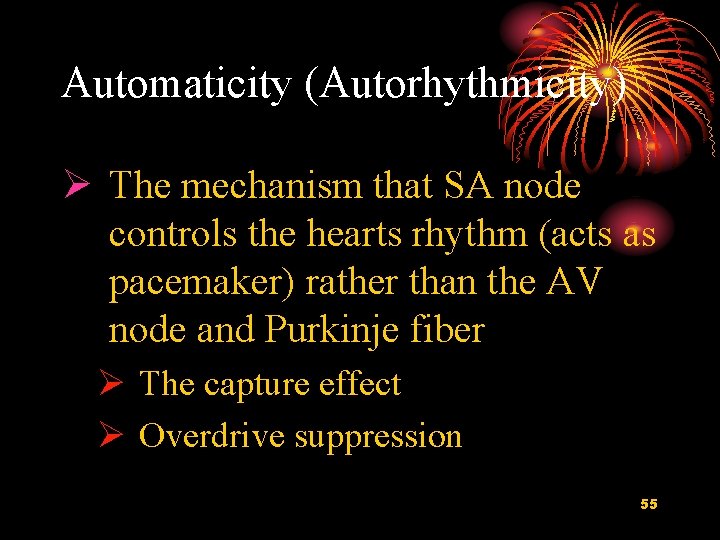
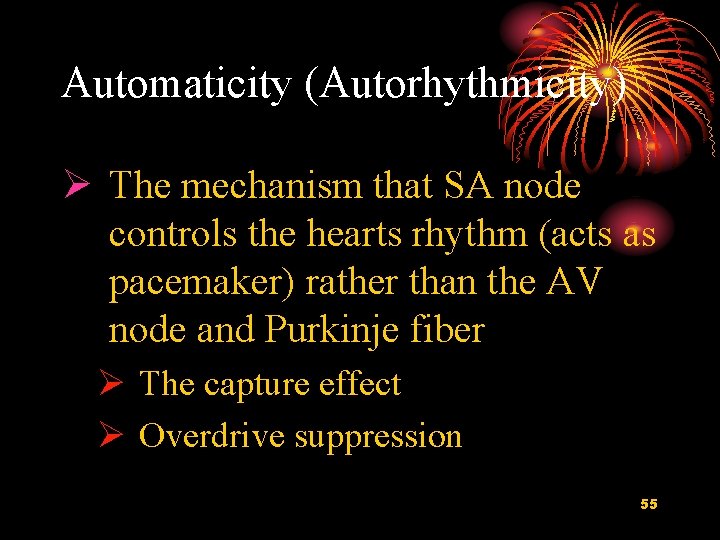
Automaticity (Autorhythmicity) Ø The mechanism that SA node controls the hearts rhythm (acts as pacemaker) rather than the AV node and Purkinje fiber Ø The capture effect Ø Overdrive suppression 55
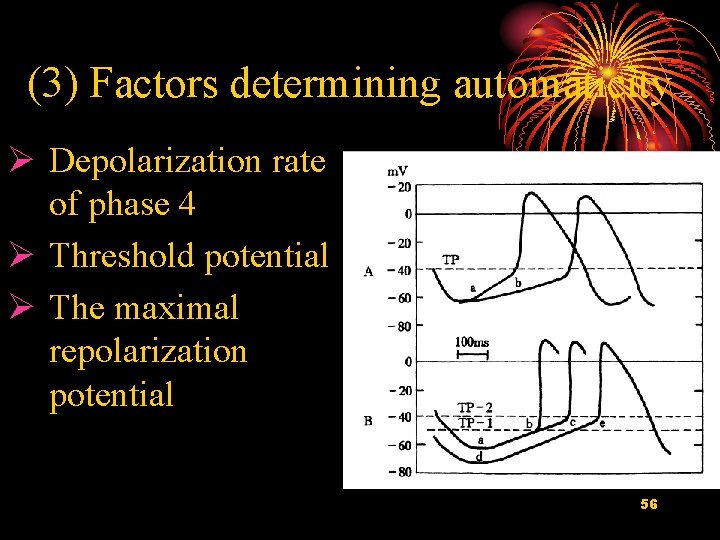
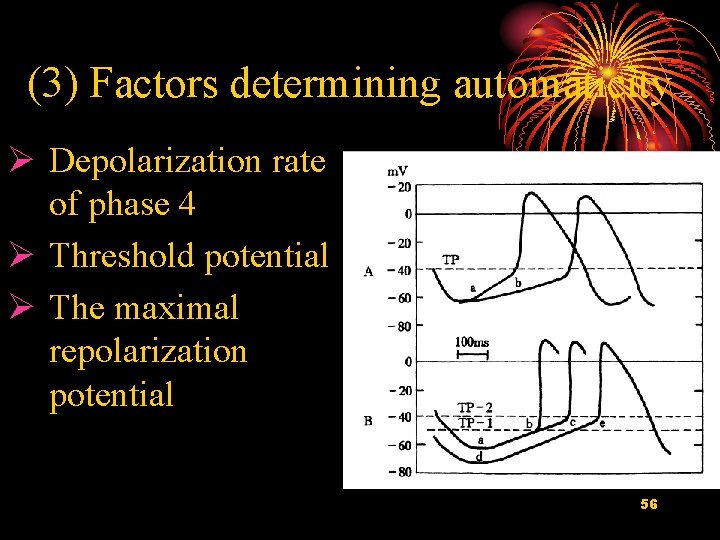
(3) Factors determining automaticity Ø Depolarization rate of phase 4 Ø Threshold potential Ø The maximal repolarization potential 56

3. Conductivity 57

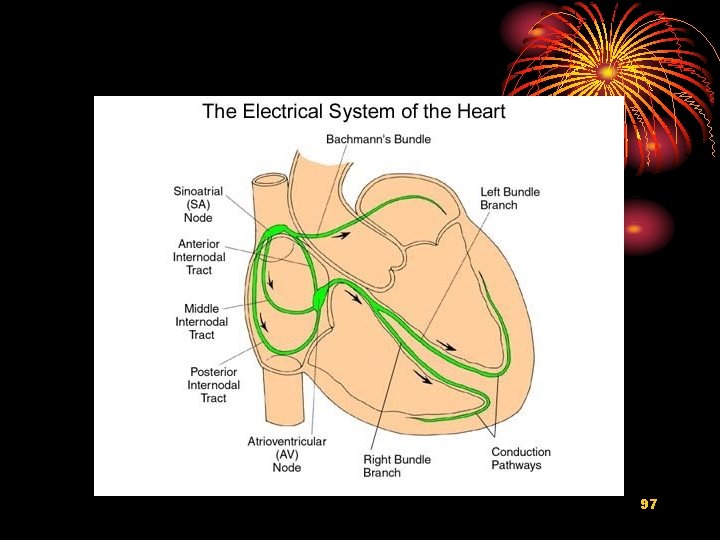
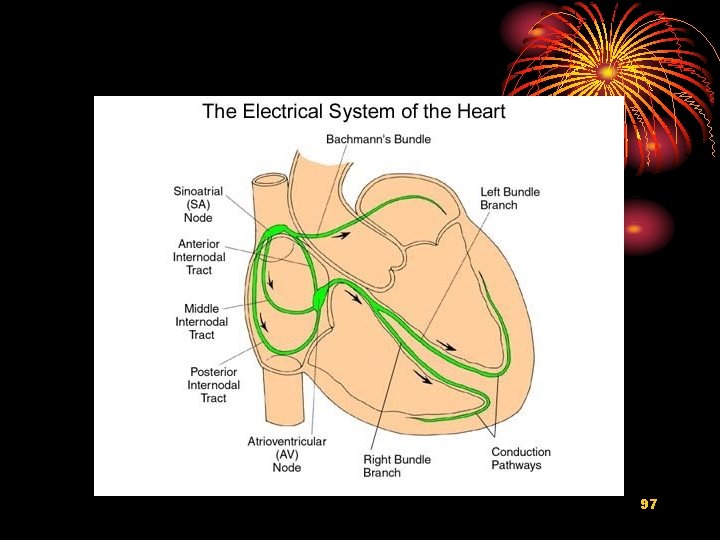
(1) Pathways and characteristics of conduction in heart 58
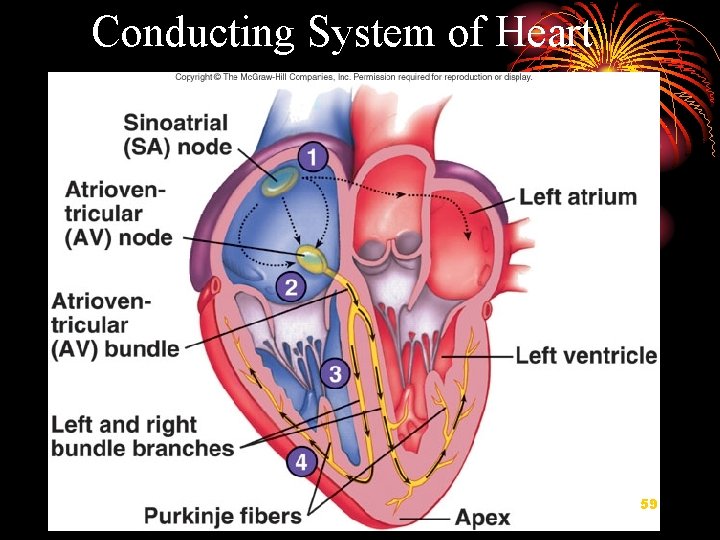
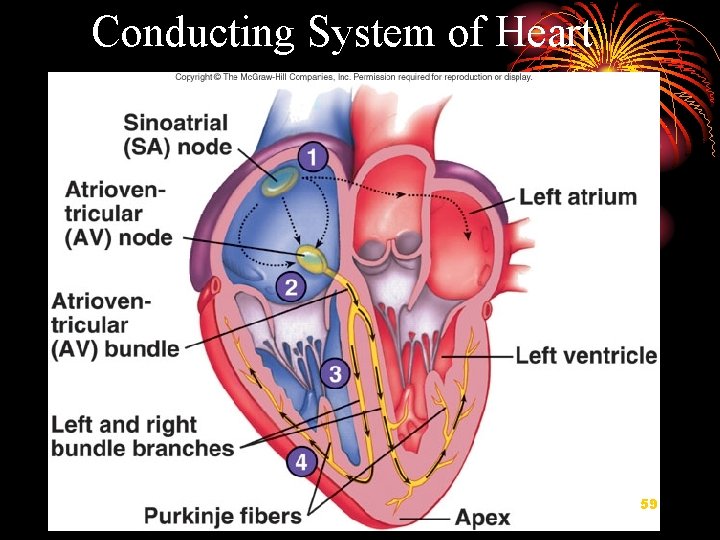
Conducting System of Heart 59
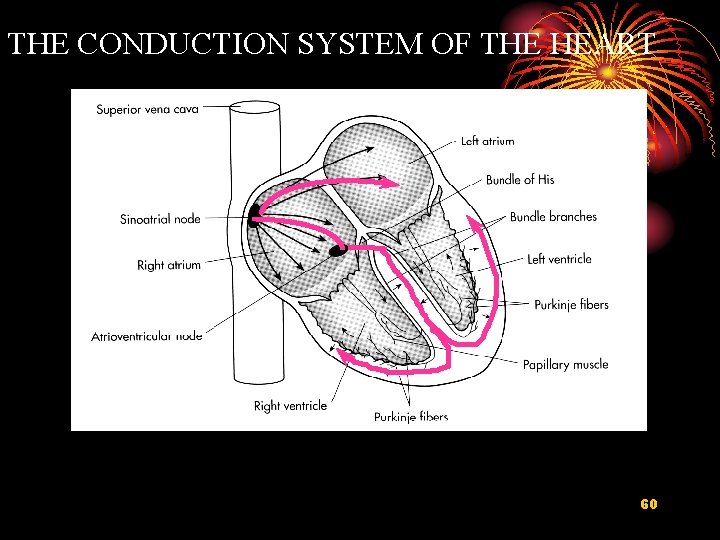
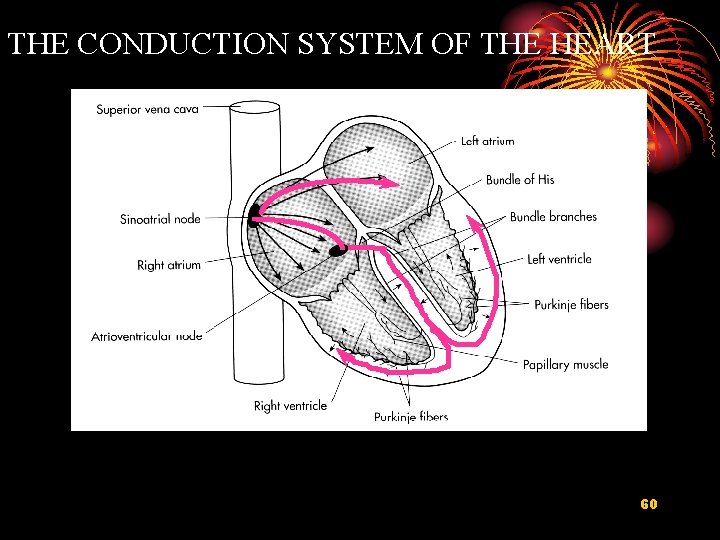
THE CONDUCTION SYSTEM OF THE HEART 60
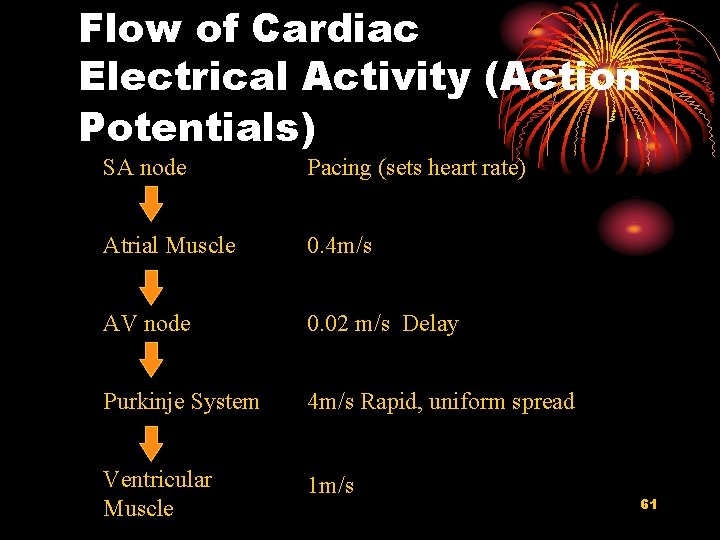
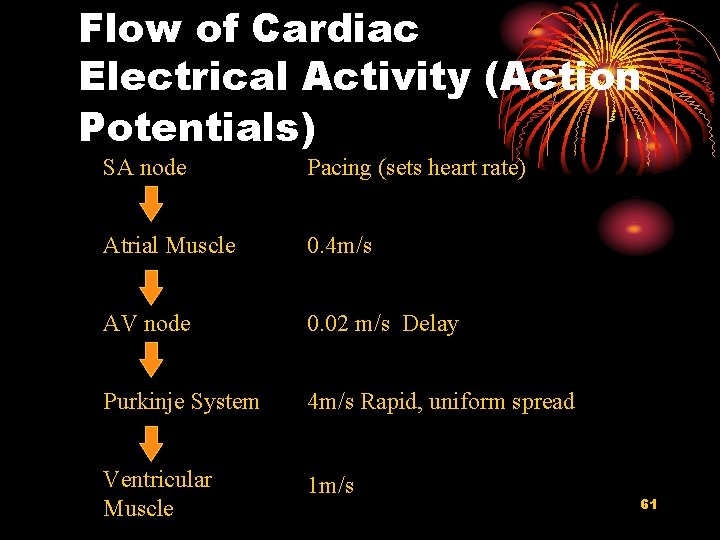
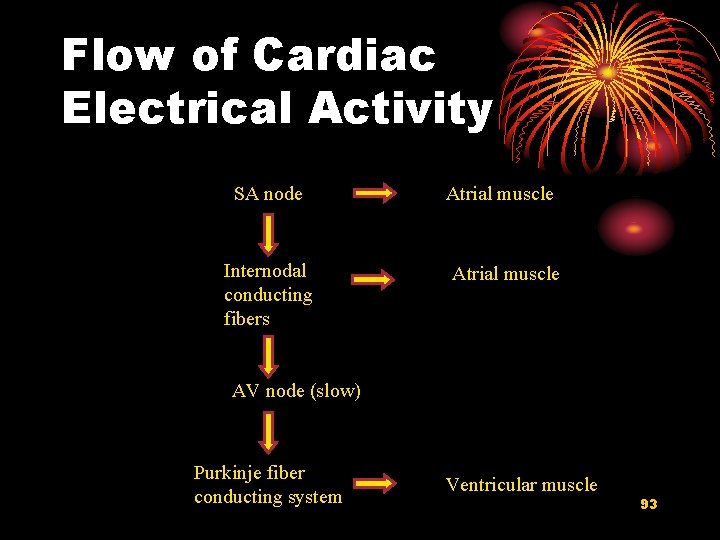
Flow of Cardiac Electrical Activity (Action Potentials) SA node Pacing (sets heart rate) Atrial Muscle 0. 4 m/s AV node 0. 02 m/s Delay Purkinje System 4 m/s Rapid, uniform spread Ventricular Muscle 1 m/s 61
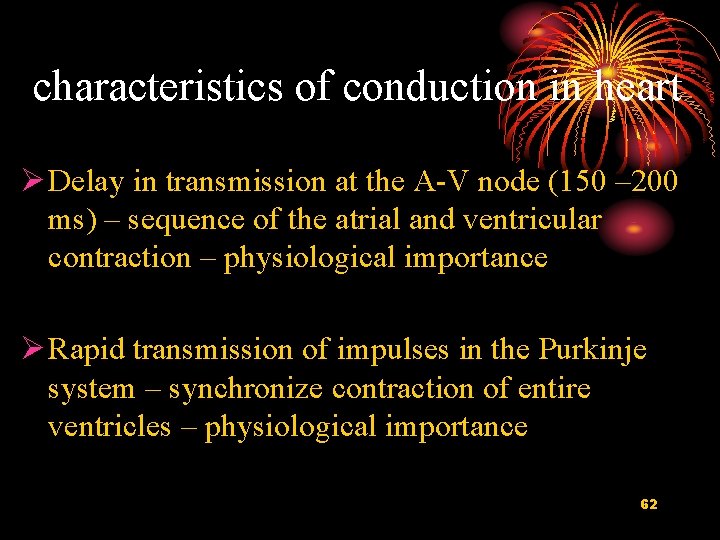
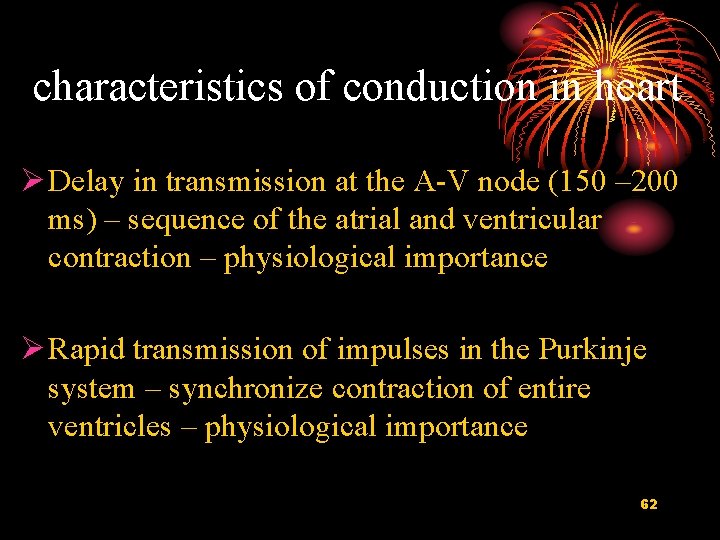
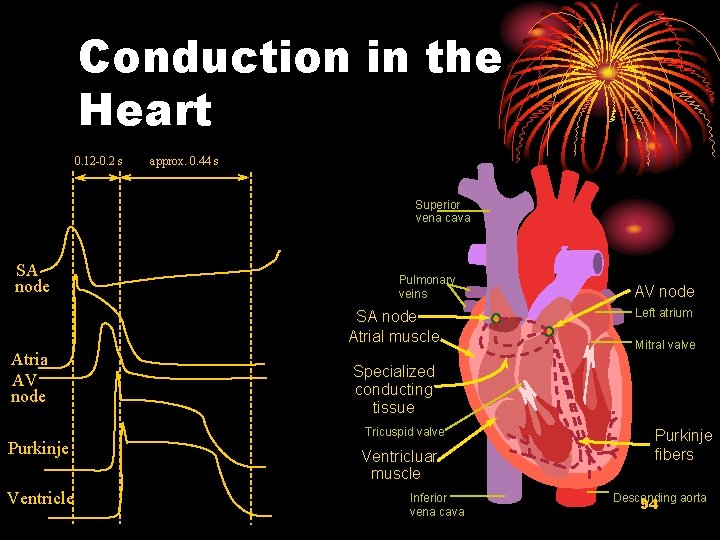
characteristics of conduction in heart Ø Delay in transmission at the A-V node (150 – 200 ms) – sequence of the atrial and ventricular contraction – physiological importance Ø Rapid transmission of impulses in the Purkinje system – synchronize contraction of entire ventricles – physiological importance 62
(2) Factors determining conductivity Ø Anatomical factors Ø Physiological factors 63
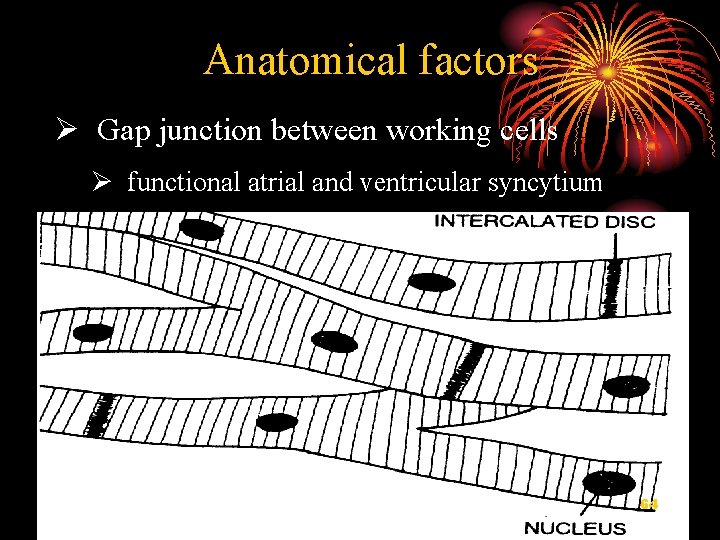
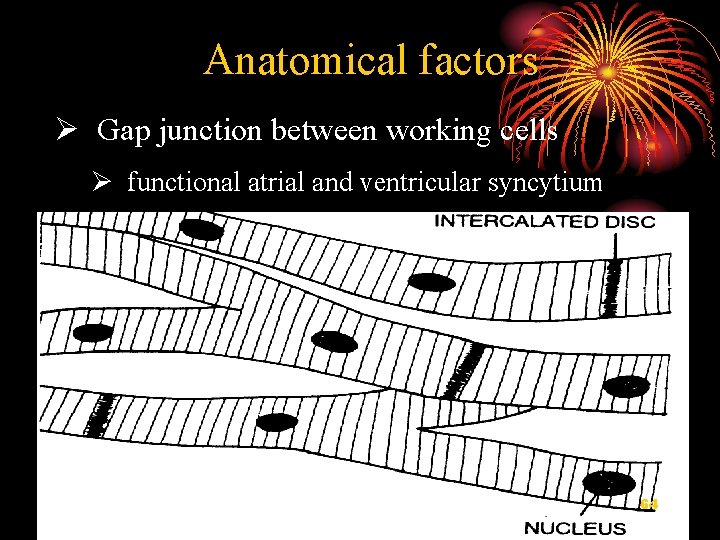
Anatomical factors Ø Gap junction between working cells Ø functional atrial and ventricular syncytium 64

65
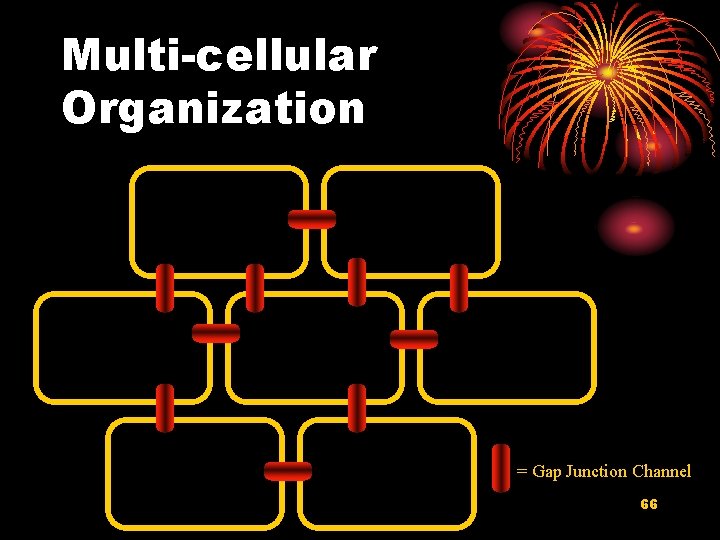
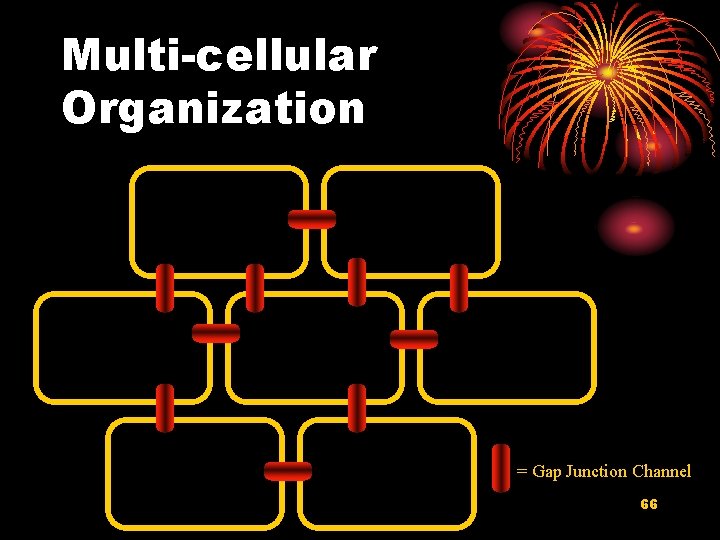
Multi-cellular Organization = Gap Junction Channel 66
Anatomical factors Ø Gap junction between working cells and functional atrial and ventricular syncytium Ø Diameter of the cardiac cell – conductive resistance – conductivity 67
Physiological factors Ø A. Slope of depolarization and amplitude of phase 0 Ø Fast and slow response cells Ø B. Excitability of the adjacent unexcited membrane 68
III. Neural and humoral control of the cardiac function 1. Vagus nerve and acetylcholine (Ach) 2. Vagus nerve : release Ach from postganglionic fiber M receptor on cardiac cells K+ channel permeability increase but Ca 2+ channel permeability decrease 69
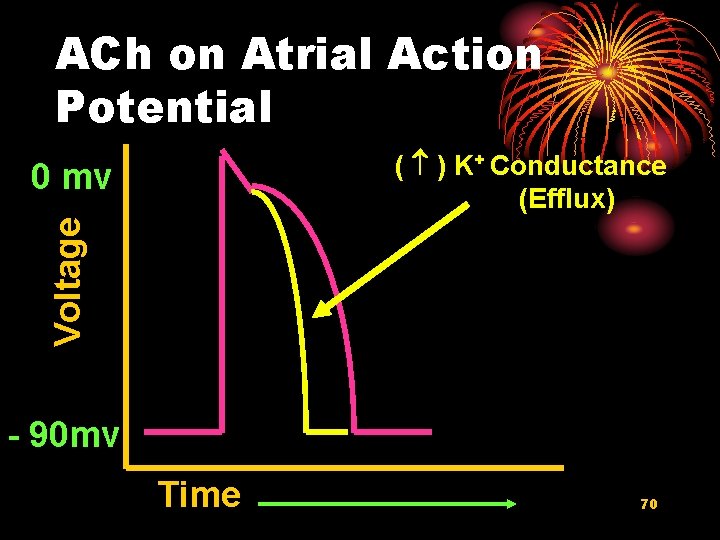
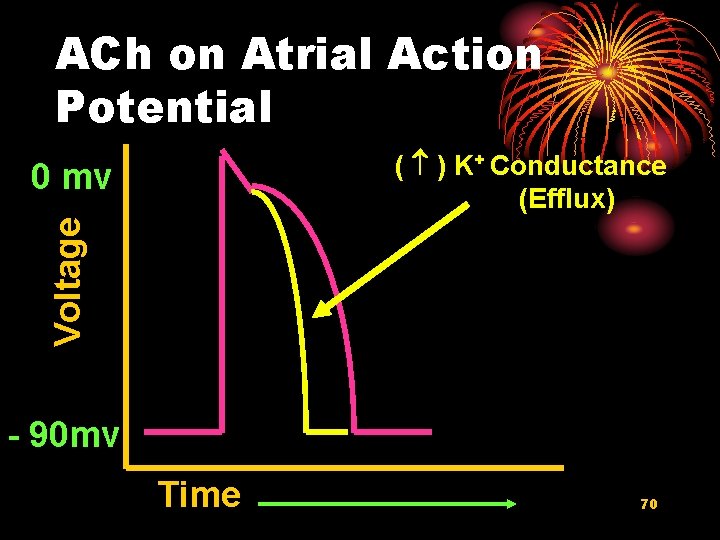
ACh on Atrial Action Potential ( ) K+ Conductance (Efflux) Voltage 0 mv - 90 mv Time 70
1) K+ channel permeability increase resting potential (maximal diastole potential) more negative excitability decrease 71
Ion Channels in Ventricular Muscle Ventricular muscle membrane potential (m. V) Inactivating K channels (ITO) “Ultra-rapid” K channels (IKur) “Rapid” K channels (IKr) 0 Voltage-gated Na Channels “Slow” K channels (IKs) Voltage-gated Ca Channels -50 IK 1 200 msec 72
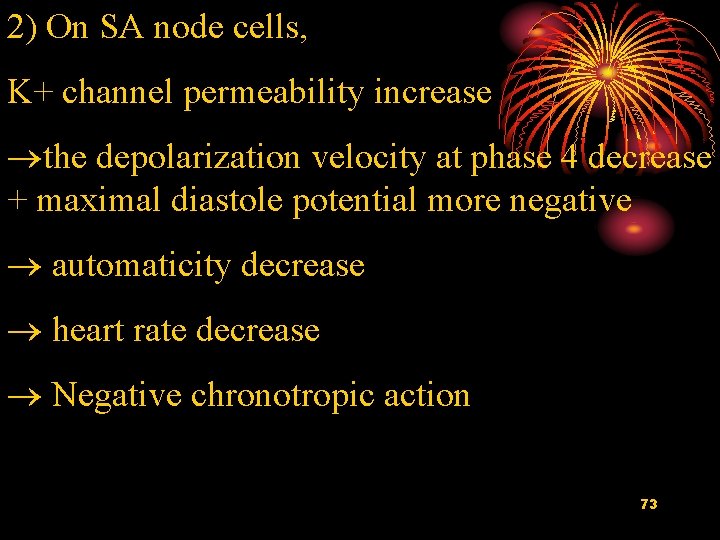
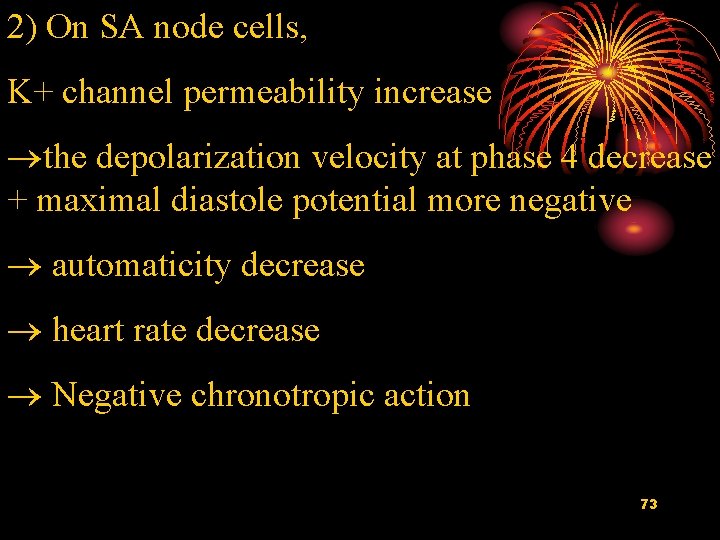
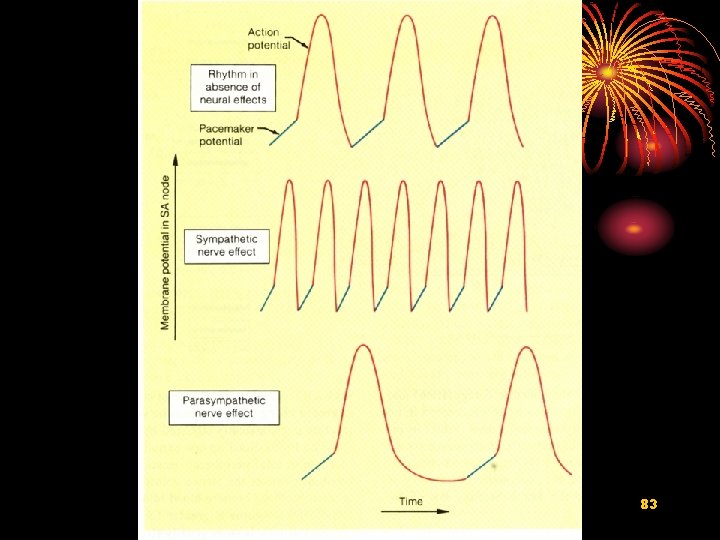
2) On SA node cells, K+ channel permeability increase the depolarization velocity at phase 4 decrease + maximal diastole potential more negative automaticity decrease heart rate decrease Negative chronotropic action 73
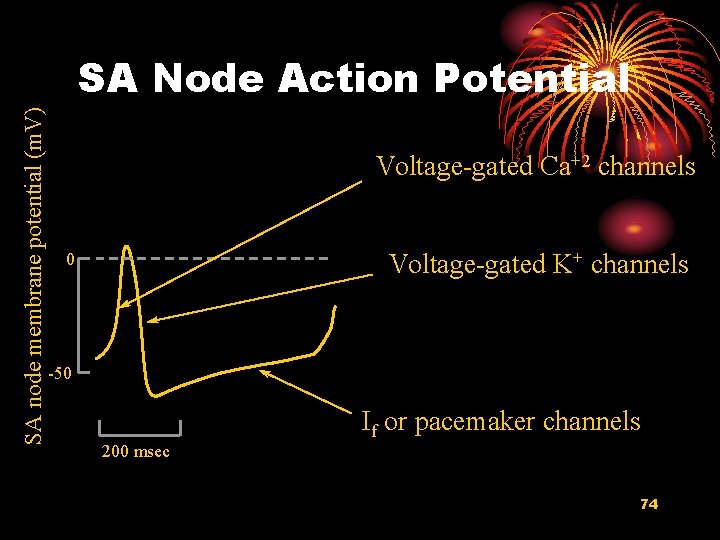
SA node membrane potential (m. V) SA Node Action Potential Voltage-gated Ca+2 channels Voltage-gated K+ channels 0 -50 If or pacemaker channels 200 msec 74
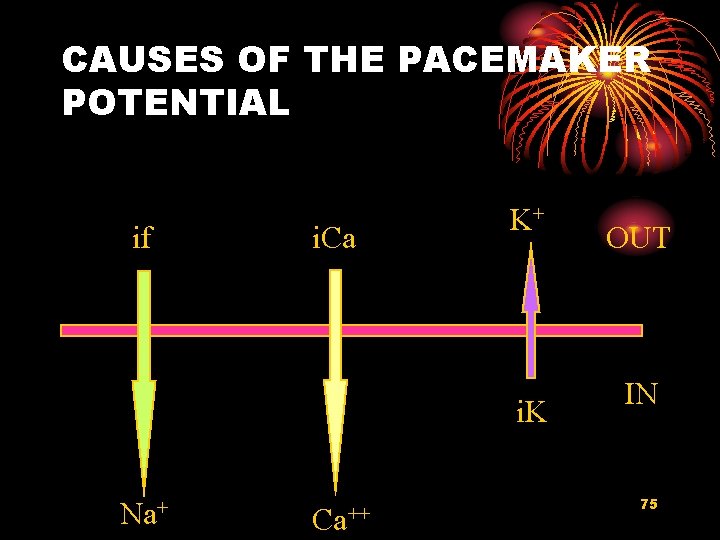
CAUSES OF THE PACEMAKER POTENTIAL if i. Ca K+ i. K Na+ Ca++ OUT IN 75
3) Ca 2+ channel permeability decrease myocardial contractility decrease negative inotropic action 76
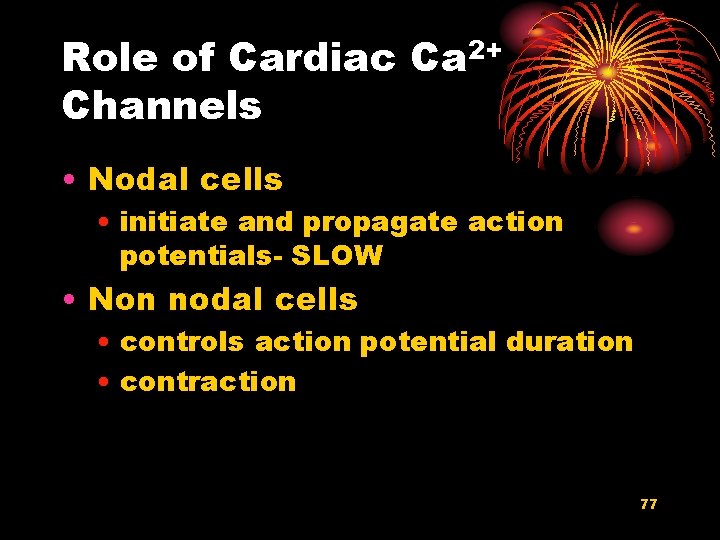
Role of Cardiac Ca 2+ Channels • Nodal cells • initiate and propagate action potentials- SLOW • Non nodal cells • controls action potential duration • contraction 77
4) Ca 2+ channel permeability decrease depolarization rate of slow response cells decrease conductivity of these cell decrease negative dromotropic action 78
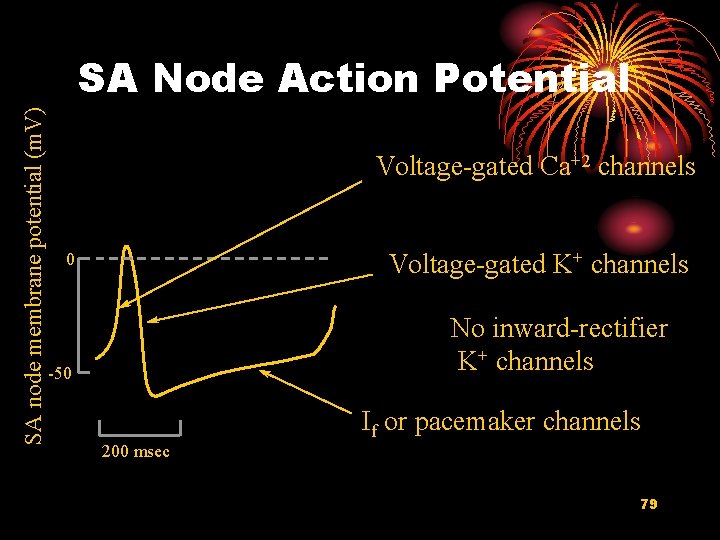
SA node membrane potential (m. V) SA Node Action Potential Voltage-gated Ca+2 channels Voltage-gated K+ channels 0 No inward-rectifier K+ channels -50 If or pacemaker channels 200 msec 79
2. Effects of Sympathetic Nerve and catecholamine on the Properties of Cardiac Muscle Sympathetic nerve release norepinephrine from the postganglionic endings; epinephrine and norepinephrine released from the adrenal glands binding with β 1 receptor on cardiac cells increase the Ca 2+ channel permeability 80
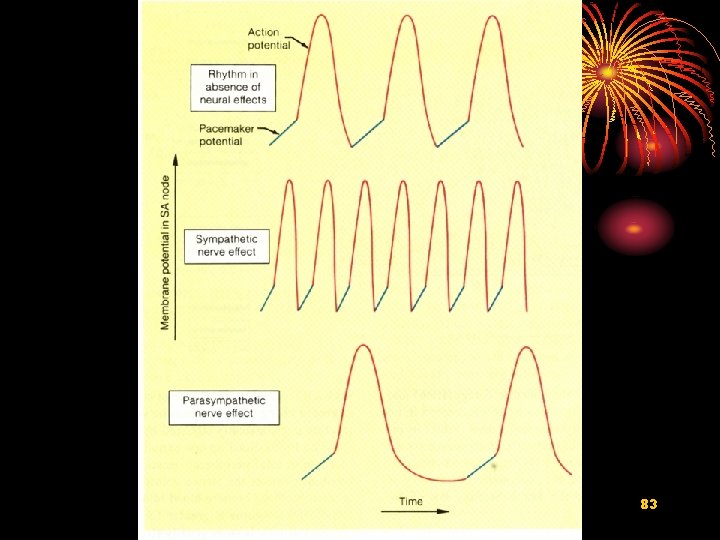
Ca 2+ channel permeability increase: Increase the spontaneous depolarization rate at phase 4 automaticity of SA node cell rise heart rate increase Positive chronotropic action 81
Ca 2+ channel permeability increase: Increase the depolarization rate (slope) and amplitude at phase 0 increase the conductivity of slow response cells Positive dromotropic action Increase the Ca 2+ concentration in plasma during excitation myocardial contractility increase positive inotropic action 82
83
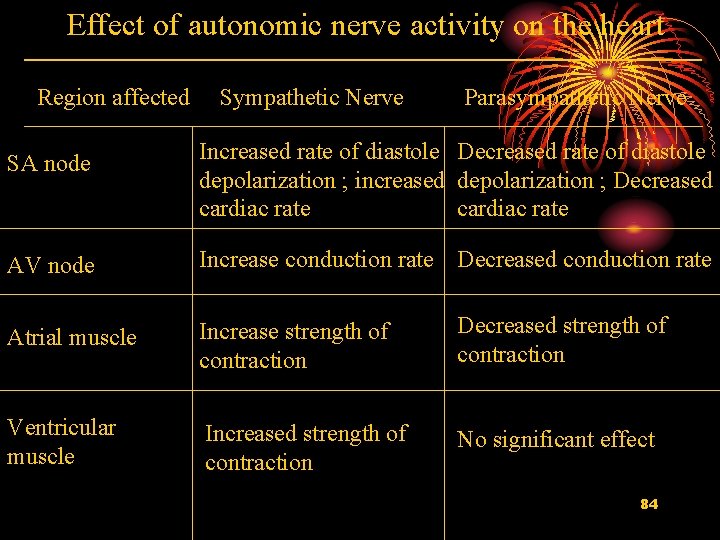
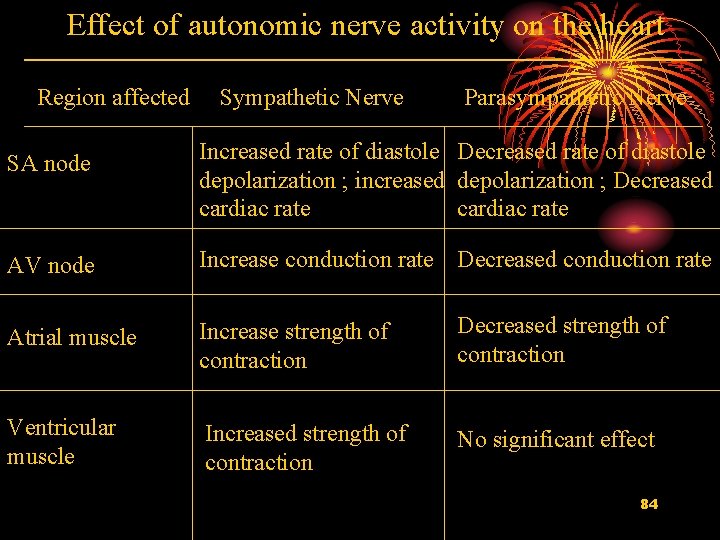
Effect of autonomic nerve activity on the heart Region affected Sympathetic Nerve Parasympathetic Nerve SA node Increased rate of diastole Decreased rate of diastole depolarization ; increased depolarization ; Decreased cardiac rate AV node Increase conduction rate Decreased conduction rate Atrial muscle Increase strength of contraction Decreased strength of contraction Ventricular muscle Increased strength of contraction No significant effect 84
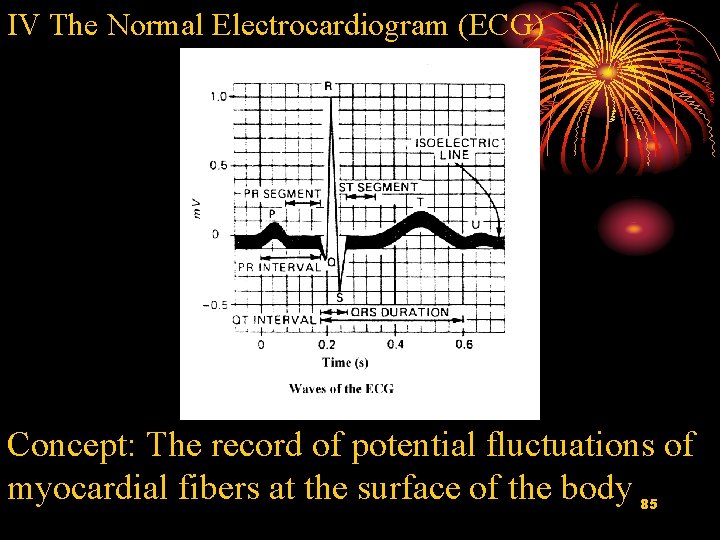
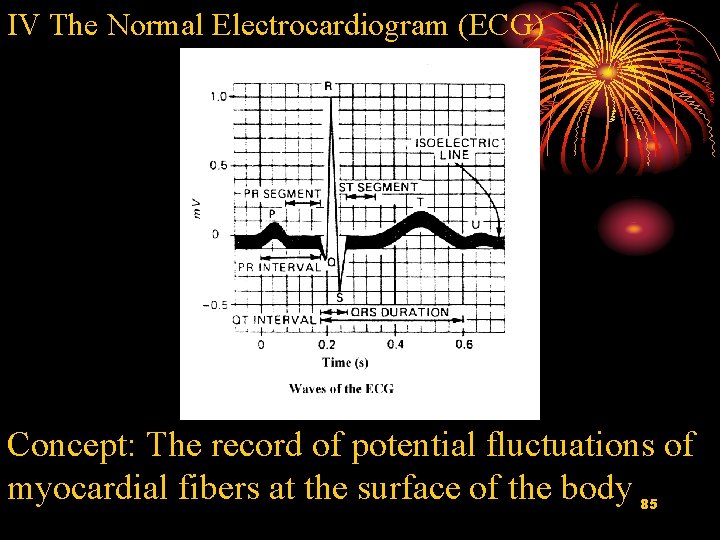
IV The Normal Electrocardiogram (ECG) Concept: The record of potential fluctuations of myocardial fibers at the surface of the body 85

1 The Basic Mechanism 86
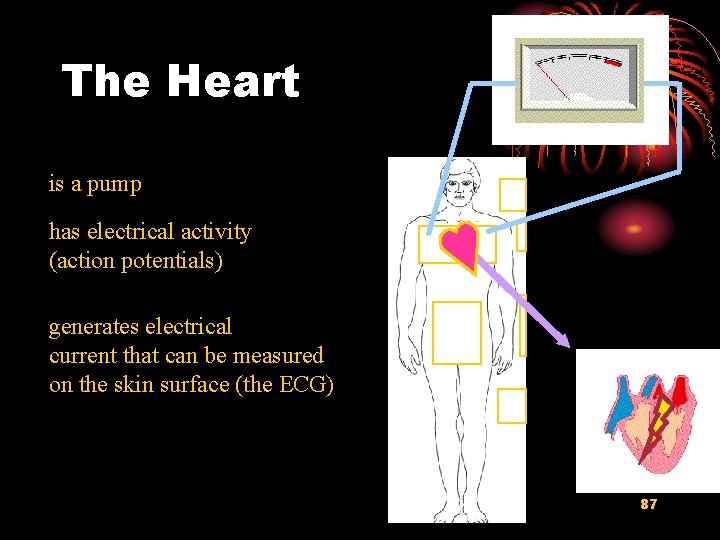
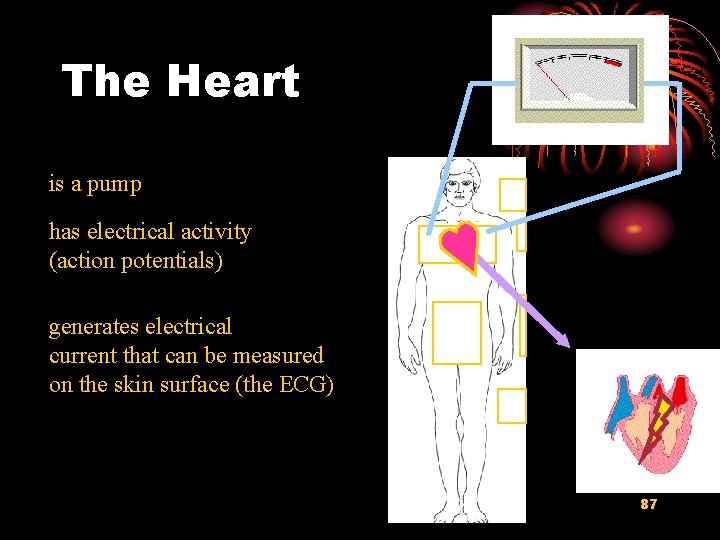
The Heart is a pump has electrical activity (action potentials) generates electrical current that can be measured on the skin surface (the ECG) 87
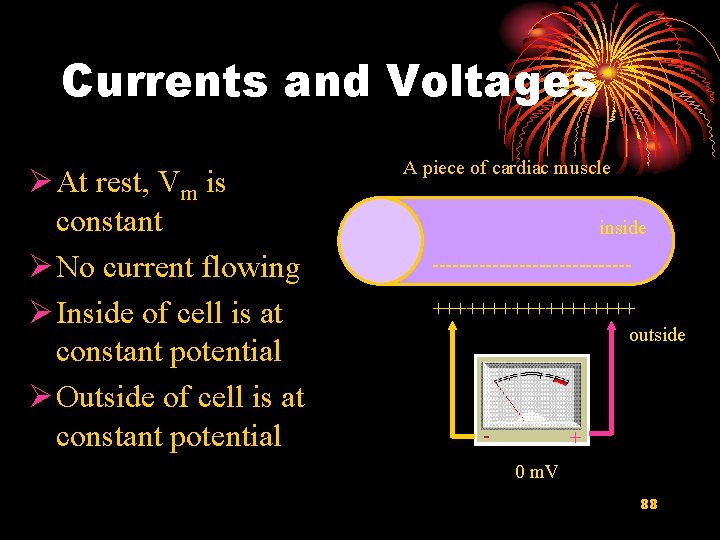
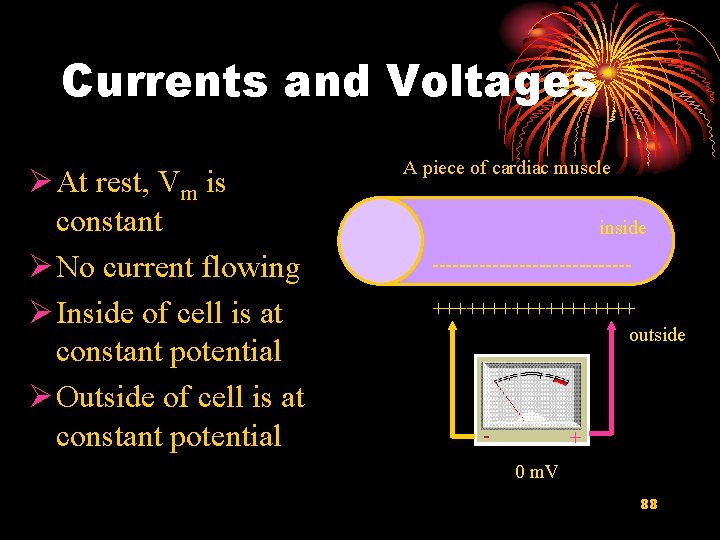
Currents and Voltages Ø At rest, Vm is constant Ø No current flowing Ø Inside of cell is at constant potential Ø Outside of cell is at constant potential A piece of cardiac muscle inside ---------------+++++++++ outside - + 0 m. V 88
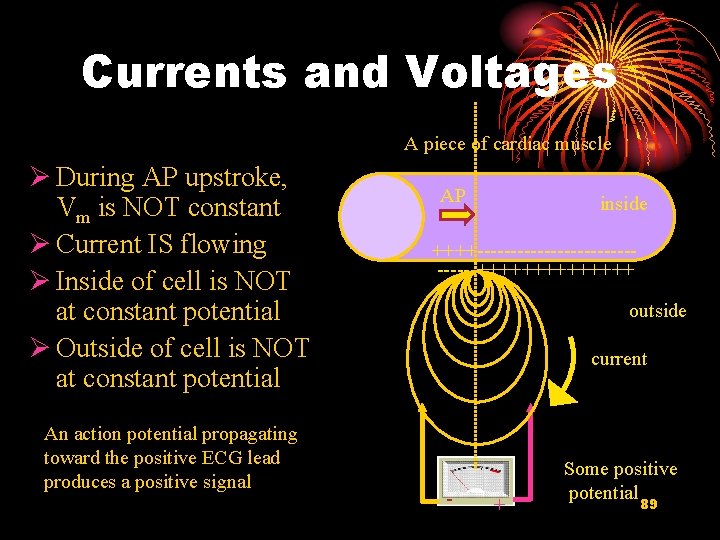
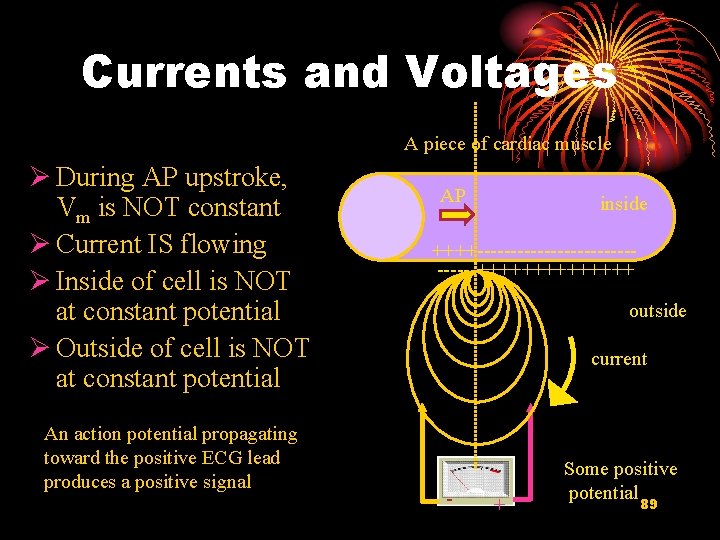
Currents and Voltages A piece of cardiac muscle Ø During AP upstroke, Vm is NOT constant Ø Current IS flowing Ø Inside of cell is NOT at constant potential Ø Outside of cell is NOT at constant potential An action potential propagating toward the positive ECG lead produces a positive signal AP inside ++++---------------+++++++ outside current - + Some positive potential 89
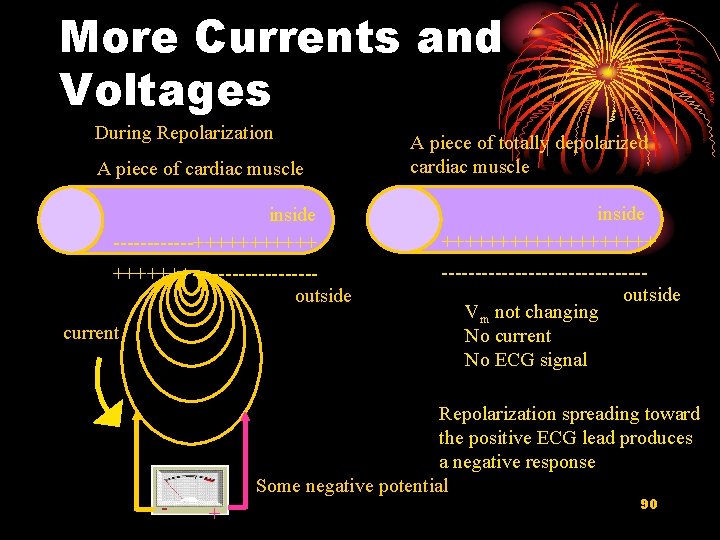
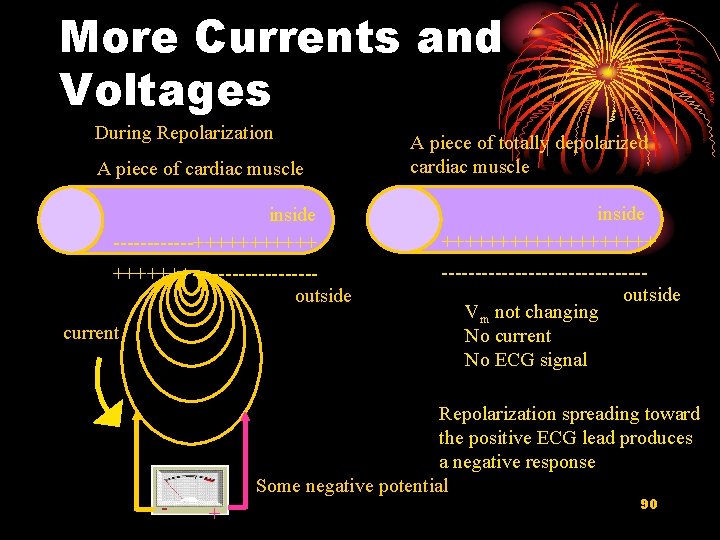
More Currents and Voltages During Repolarization A piece of cardiac muscle A piece of totally depolarized cardiac muscle inside ------++++++ inside ++++++++++---------outside ---------------outside Vm not changing No current No ECG signal current - Repolarization spreading toward the positive ECG lead produces a negative response Some negative potential + 90
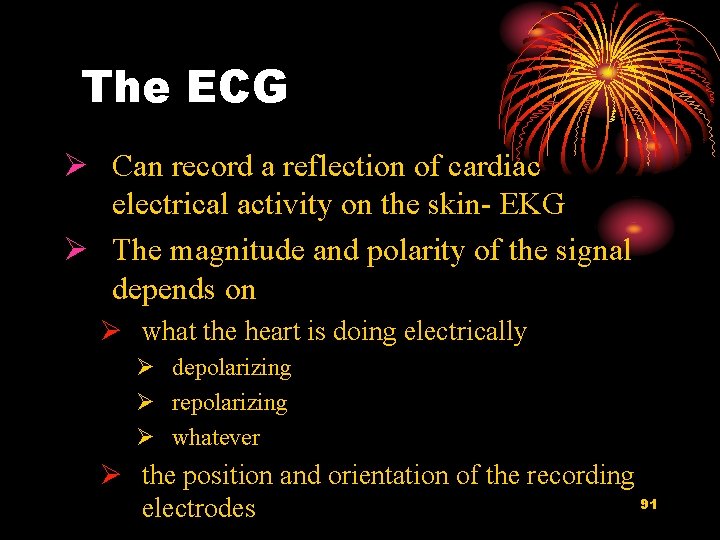
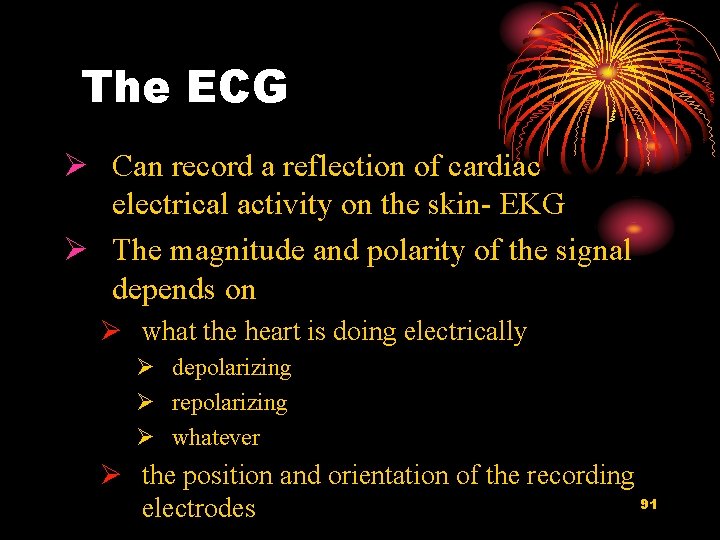
The ECG Ø Can record a reflection of cardiac electrical activity on the skin- EKG Ø The magnitude and polarity of the signal depends on Ø what the heart is doing electrically Ø depolarizing Ø repolarizing Ø whatever Ø the position and orientation of the recording 91 electrodes
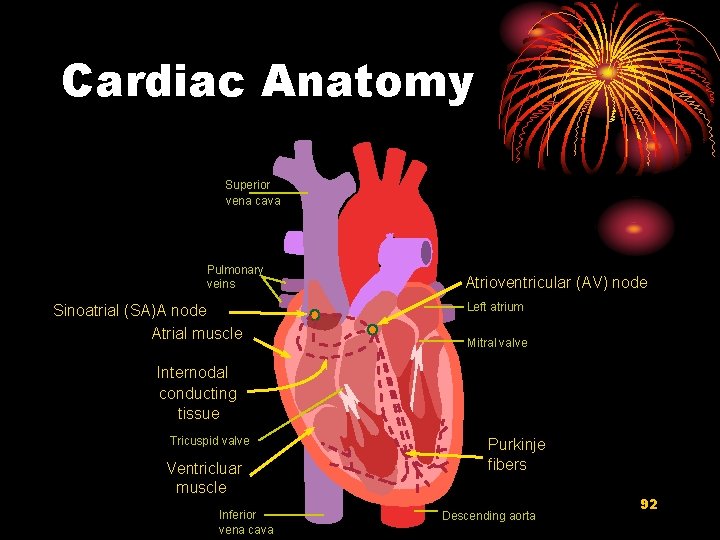
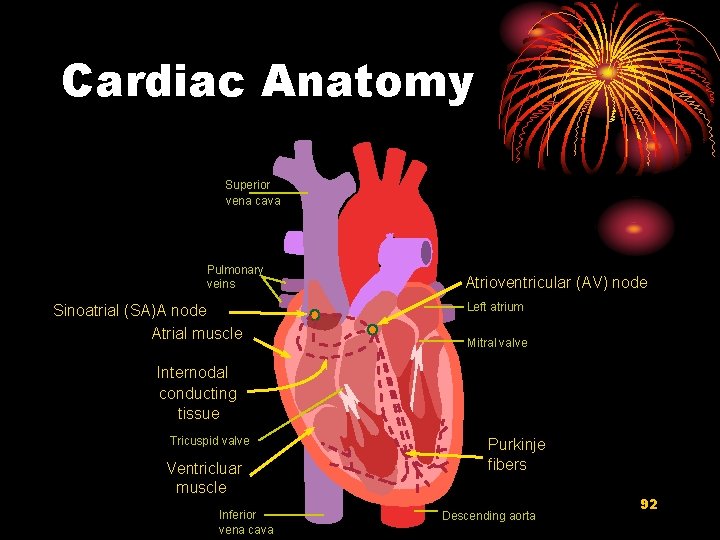
Cardiac Anatomy Superior vena cava Pulmonary veins Sinoatrial (SA)A node Atrial muscle Atrioventricular (AV) node Left atrium Mitral valve Internodal conducting tissue Tricuspid valve Ventricluar muscle Inferior vena cava Purkinje fibers Descending aorta 92
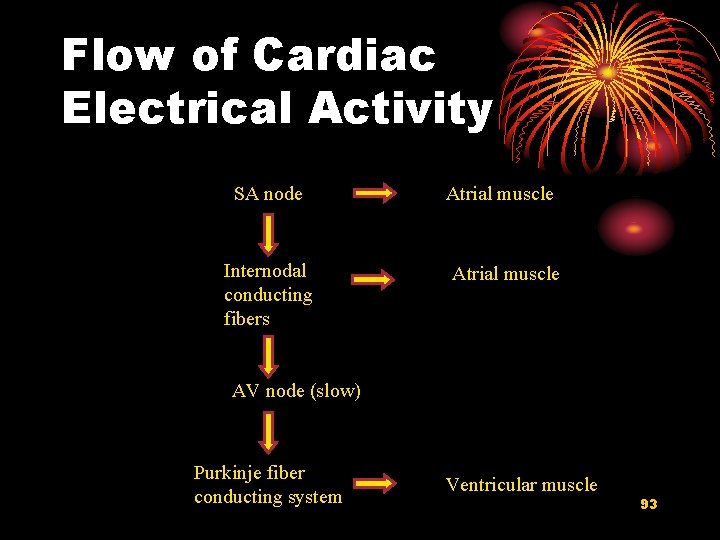
Flow of Cardiac Electrical Activity SA node Internodal conducting fibers Atrial muscle AV node (slow) Purkinje fiber conducting system Ventricular muscle 93
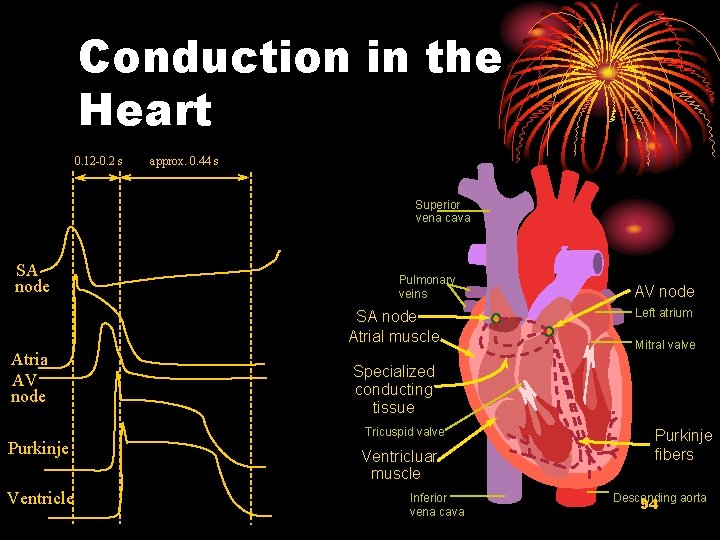
Conduction in the Heart 0. 12 -0. 2 s approx. 0. 44 s Superior vena cava SA node Pulmonary veins SA node Atrial muscle Atria AV node Purkinje Ventricle AV node Left atrium Mitral valve Specialized conducting tissue Tricuspid valve Ventricluar muscle Inferior vena cava Purkinje fibers Descending aorta 94
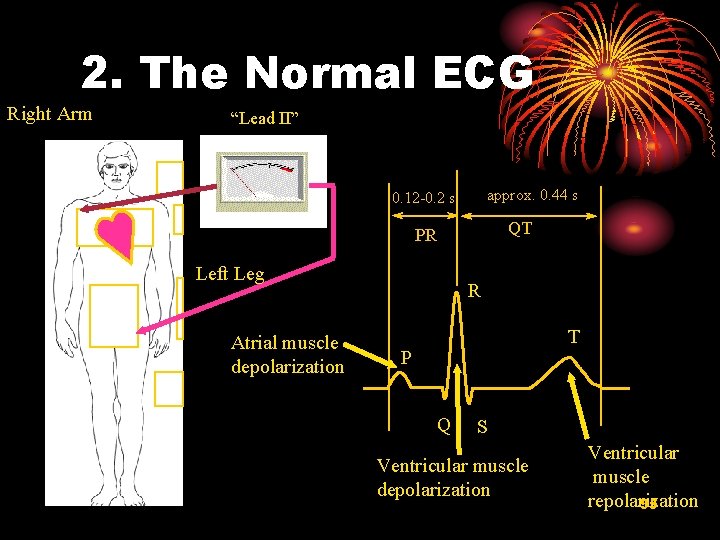
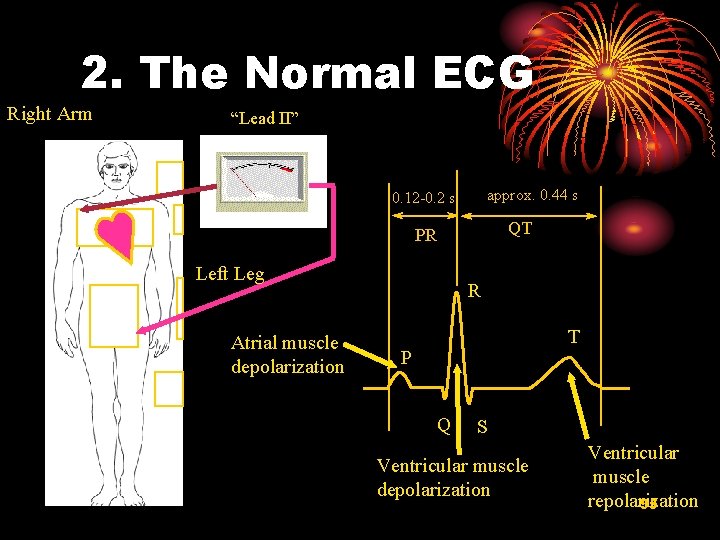
2. The Normal ECG Right Arm “Lead II” approx. 0. 44 s 0. 12 -0. 2 s QT PR Left Leg Atrial muscle depolarization R T P Q S Ventricular muscle depolarization Ventricular muscle repolarization 95
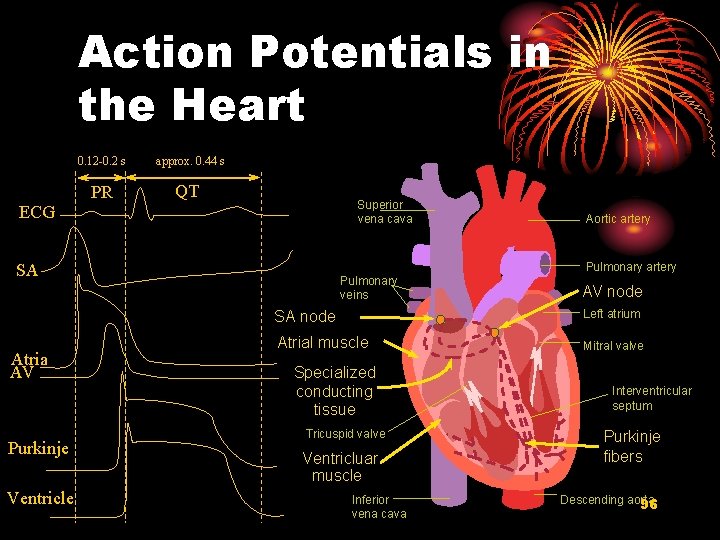
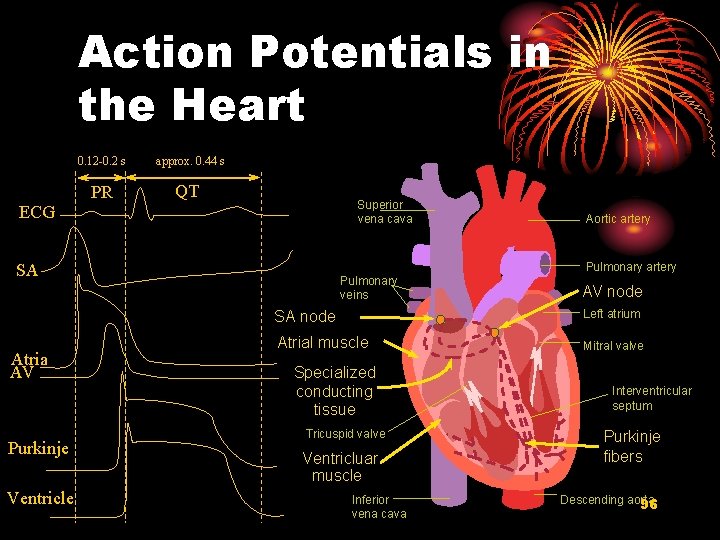
Action Potentials in the Heart 0. 12 -0. 2 s approx. 0. 44 s PR QT Superior vena cava ECG SA Atria AV Purkinje Ventricle Aortic artery Pulmonary veins AV node SA node Left atrium Atrial muscle Mitral valve Specialized conducting tissue Tricuspid valve Ventricluar muscle Inferior vena cava Interventricular septum Purkinje fibers Descending aorta 96
97
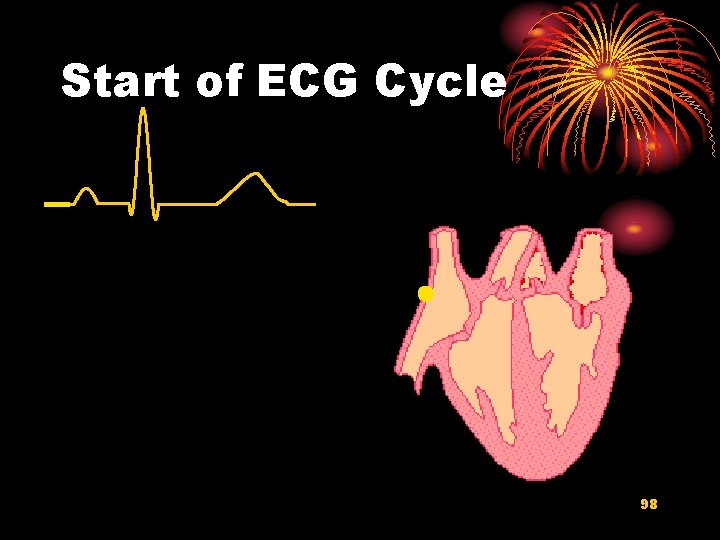
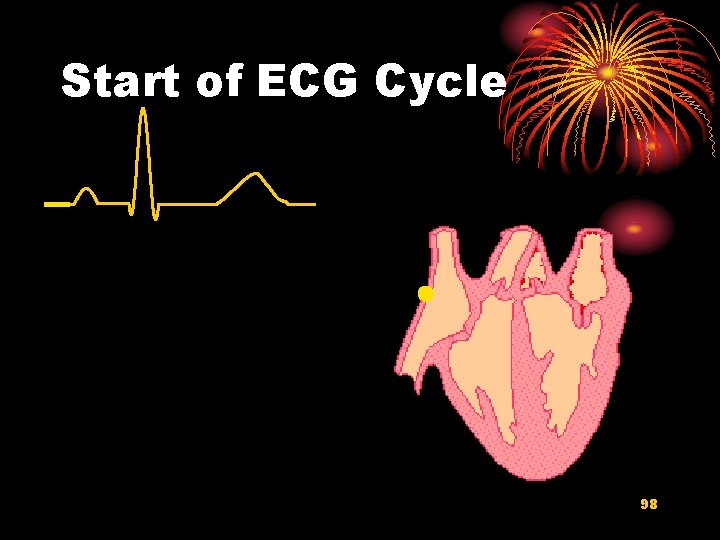
Start of ECG Cycle 98
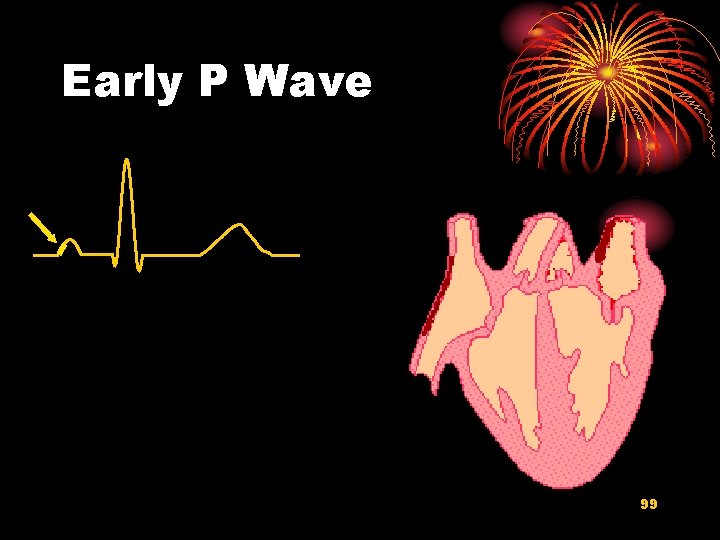
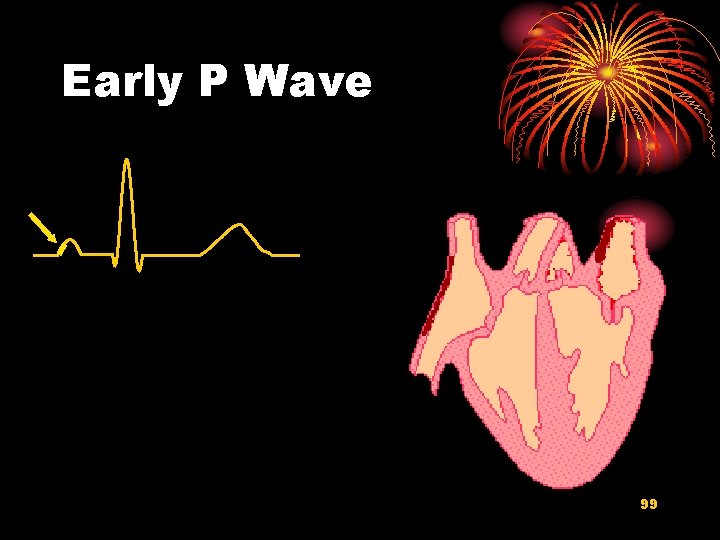
Early P Wave 99
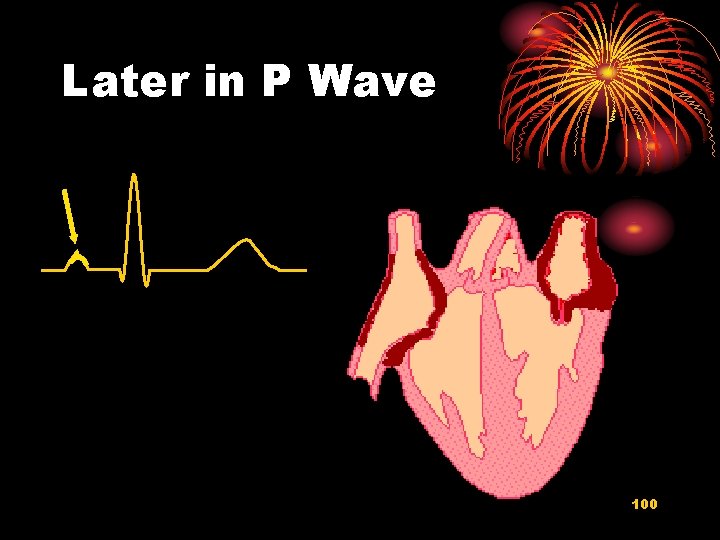
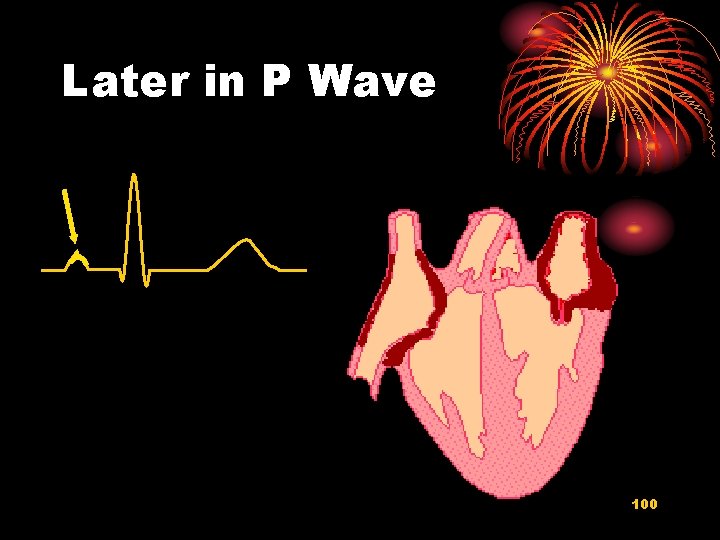
Later in P Wave 100
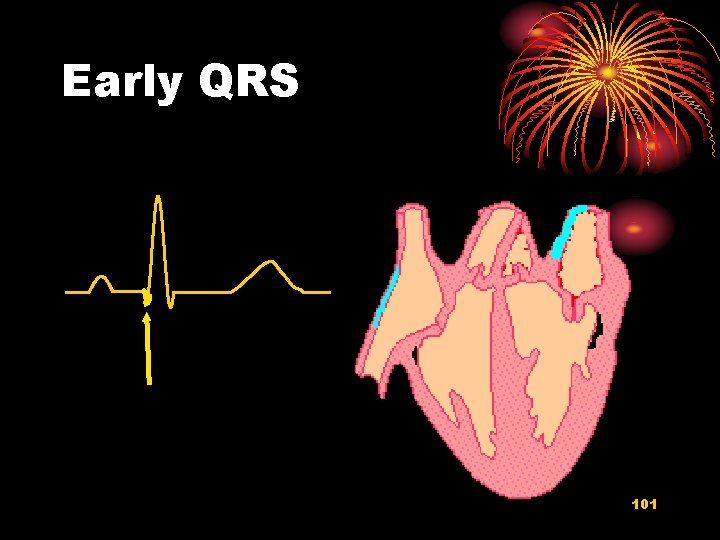
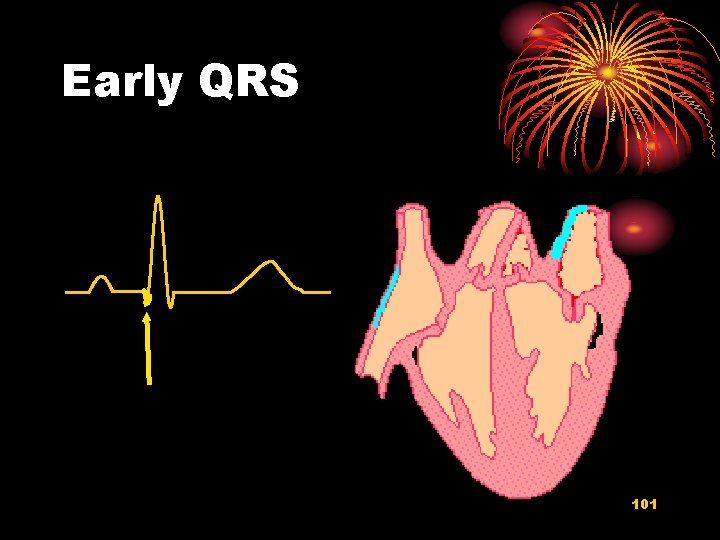
Early QRS 101
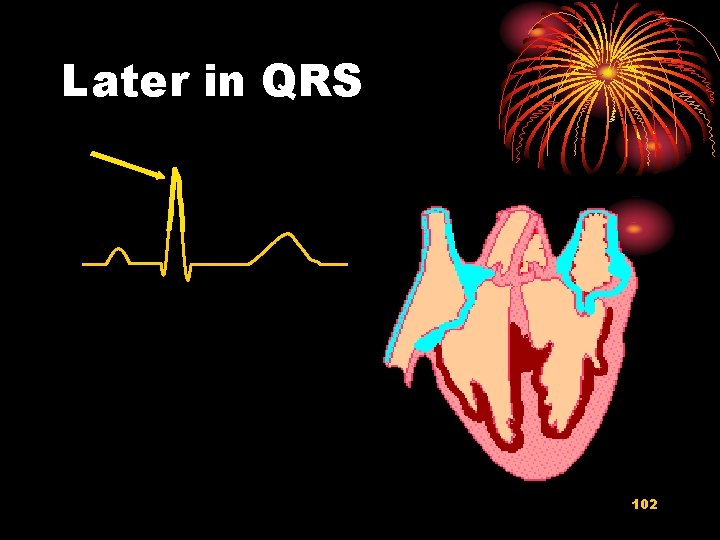
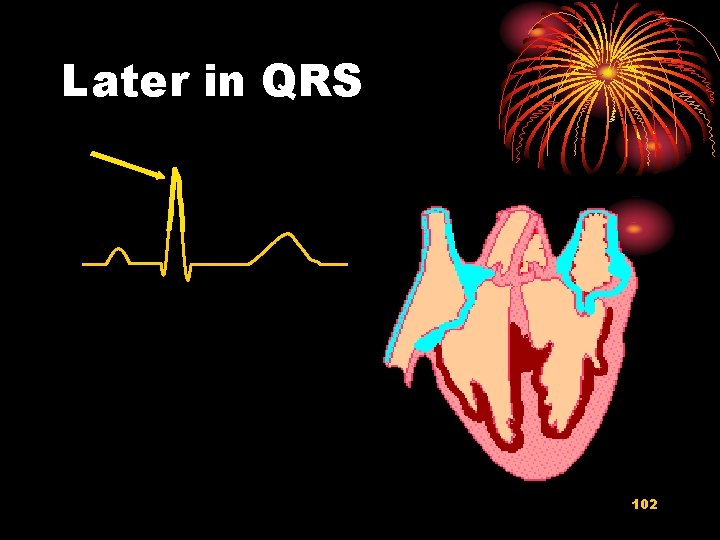
Later in QRS 102
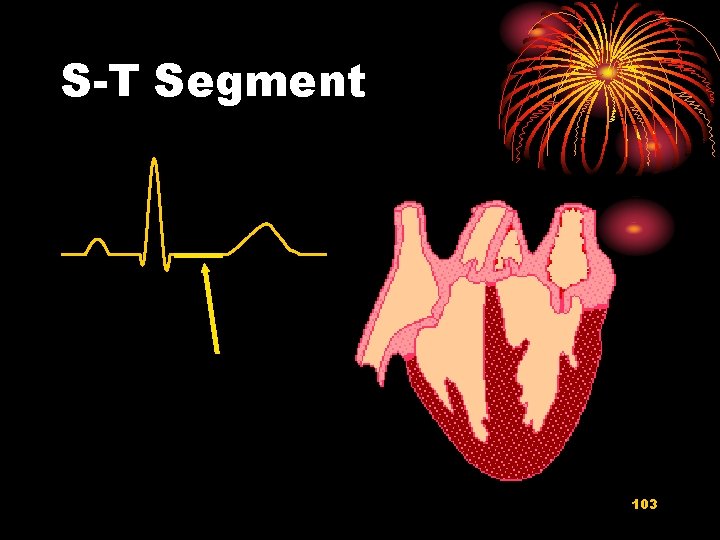
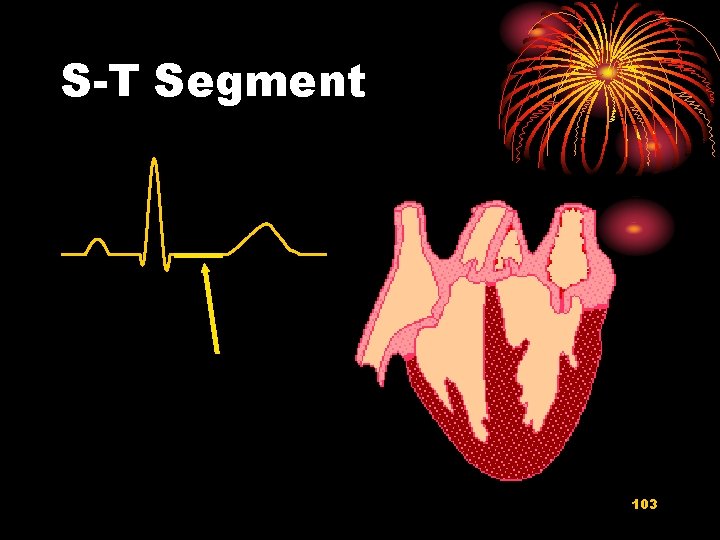
S-T Segment 103
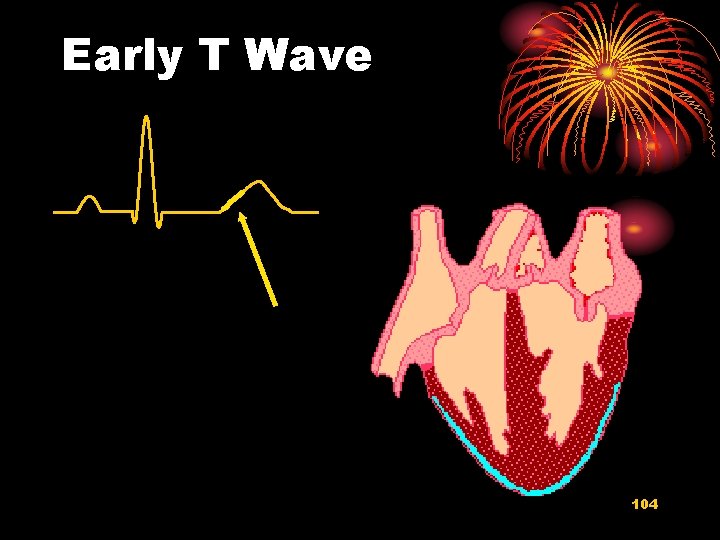
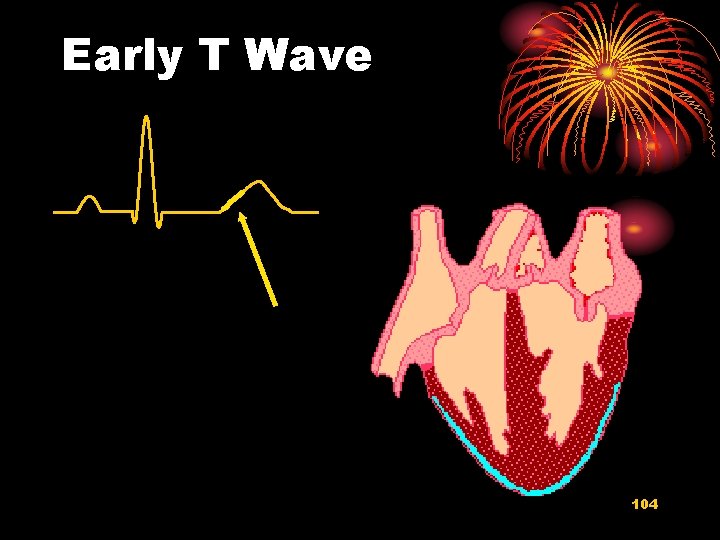
Early T Wave 104
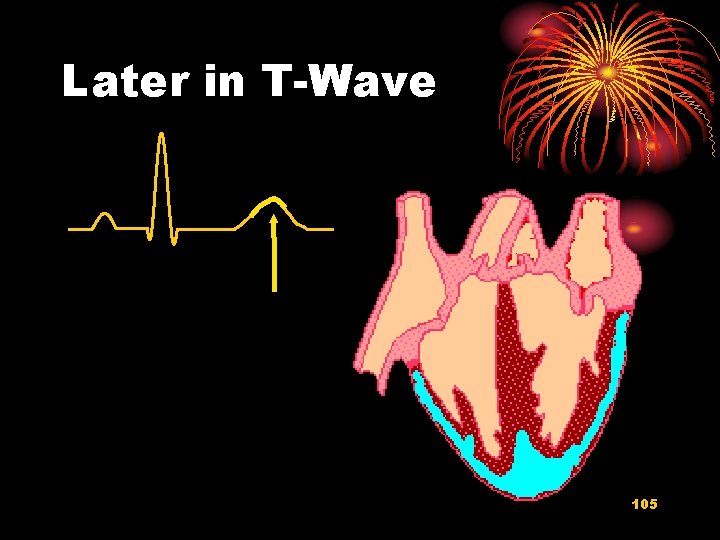
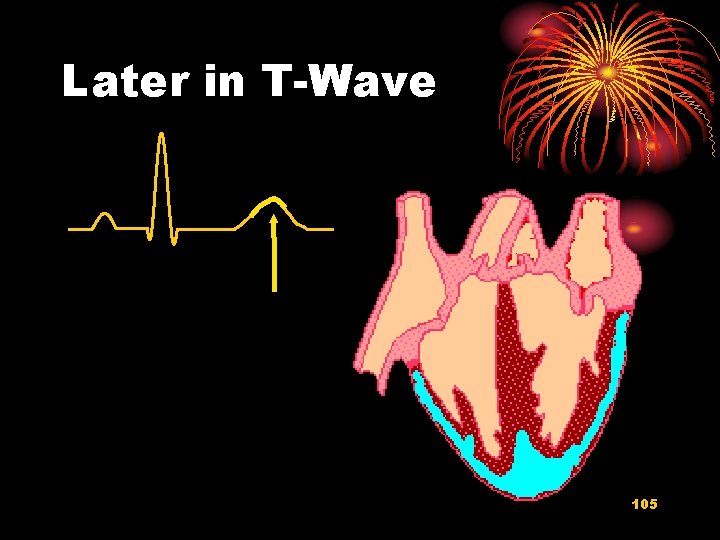
Later in T-Wave 105

Back to where we started 106
3. Uses of the ECG ©Heart Rate ©Conduction in the heart ©Cardiac arrhythmia ©Direction of the cardiac vector ©Damage to the heart muscle ©Provides NO information about pumping or mechanical events in the heart. 107
 Download sequel pro for windows
Download sequel pro for windows Alex liu cecilia liu
Alex liu cecilia liu Líu líu lo lo ta ca hát say sưa
Líu líu lo lo ta ca hát say sưa Yong loo lin school of medicine
Yong loo lin school of medicine Kim ung yong
Kim ung yong Spring, summer, fall, winter... and spring (2003)
Spring, summer, fall, winter... and spring (2003) Yong mok hin
Yong mok hin Kwon ji yong age
Kwon ji yong age Yong lei
Yong lei Berney v tronoh mines
Berney v tronoh mines Nus cs1010
Nus cs1010 Yong lei
Yong lei Yong soon min
Yong soon min Pakaian mak yong
Pakaian mak yong Csub bpa
Csub bpa Ban yong
Ban yong Yong hoon kim
Yong hoon kim Sql yong
Sql yong Sql yong
Sql yong Textbook
Textbook Logic vị từ là gì
Logic vị từ là gì Biểu diễn số thực
Biểu diễn số thực Shan gen acupuncture point
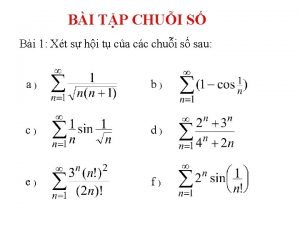
Shan gen acupuncture point Tính tổng chuỗi số
Tính tổng chuỗi số Giáo dục chuẩn mực ngữ âm tiếng việt
Giáo dục chuẩn mực ngữ âm tiếng việt Tiêu chuẩn d'alembert
Tiêu chuẩn d'alembert 5 tiêu chuẩn finer
5 tiêu chuẩn finer Biểu diễn số thực 32 bit
Biểu diễn số thực 32 bit Tam chứng anthonisen
Tam chứng anthonisen Chuẩn đoán
Chuẩn đoán Tiêu chuẩn atlanta 2012
Tiêu chuẩn atlanta 2012 Chuẩn mực nhóm
Chuẩn mực nhóm độ lệch chuẩn
độ lệch chuẩn đánh giá theo chuẩn nghề nghiệp giáo viên csgdpt
đánh giá theo chuẩn nghề nghiệp giáo viên csgdpt Cho lược đồ quan hệ q(abcdegh)
Cho lược đồ quan hệ q(abcdegh) Target institute of medical education and research
Target institute of medical education and research Pima medical institute dress code
Pima medical institute dress code Beijing medical equipment institute
Beijing medical equipment institute California medical license for foreign medical graduates
California medical license for foreign medical graduates Gbmc medical records
Gbmc medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial medical center medical records
Torrance memorial medical center medical records Cartersville medical center medical records
Cartersville medical center medical records Charter school institute
Charter school institute Santa fe institute summer school
Santa fe institute summer school Diane liu md
Diane liu md Melissa liu math
Melissa liu math Lucy lui with my girl drew
Lucy lui with my girl drew Chee wee liu
Chee wee liu Yang liu stanford
Yang liu stanford Tongping liu
Tongping liu Jingchen liu
Jingchen liu Karin björsten liu
Karin björsten liu Sissi liu
Sissi liu Chim đậu trên cành chim hót líu lo
Chim đậu trên cành chim hót líu lo J liu
J liu Bing images
Bing images Jun s. liu
Jun s. liu 732a64
732a64 Ni jia you ji ge ren in english
Ni jia you ji ge ren in english Jasmine pai
Jasmine pai Andrea j liu
Andrea j liu Hypergene liu
Hypergene liu Kevin liu toto
Kevin liu toto Liu xiang weightlifter
Liu xiang weightlifter Yang liu stanford
Yang liu stanford Ict seneca
Ict seneca Zaijia liu
Zaijia liu Changbin liu
Changbin liu Anli liu md ma
Anli liu md ma Dong liu ustc
Dong liu ustc Chu liu edmonds algorithm
Chu liu edmonds algorithm Qingxia liu
Qingxia liu Yale math placement
Yale math placement Liu shen & associates
Liu shen & associates Bài hát vườn trường mùa thu mp3
Bài hát vườn trường mùa thu mp3 Cafe java liu
Cafe java liu Liu hui mathematician
Liu hui mathematician Fengjing liu
Fengjing liu Junda liu
Junda liu Liu pengpeng
Liu pengpeng Liu bolin
Liu bolin Yang liu stanford
Yang liu stanford Jintan liu
Jintan liu Weibin liu
Weibin liu Vena cana
Vena cana Yunhuai liu
Yunhuai liu Jj liu microsoft
Jj liu microsoft Tongping liu
Tongping liu Dr perry liu
Dr perry liu Ba jin
Ba jin Xiang yu liu bang
Xiang yu liu bang Liu xiang
Liu xiang Tony sucks vinnie
Tony sucks vinnie Chee wee liu
Chee wee liu W. vincent liu
W. vincent liu Steve z liu
Steve z liu Liu po-shan
Liu po-shan Bing liu uic
Bing liu uic Mis liu
Mis liu Xiang yang liu
Xiang yang liu Quy trình khai phá dữ liệu
Quy trình khai phá dữ liệu Liu web
Liu web Liu thiu
Liu thiu Dong liu ustc
Dong liu ustc Xiulong liu
Xiulong liu Xueqin liu
Xueqin liu Network ls
Network ls