LIU Chuan Yong Institute of Physiology Medical School






- Slides: 56
LIU Chuan Yong 刘传勇 Institute of Physiology Medical School of SDU Tel 88381175 (lab) 88382098 (office) Email: liucy@sdu. edu. cn Website: www. physiology. sdu. edu. cn
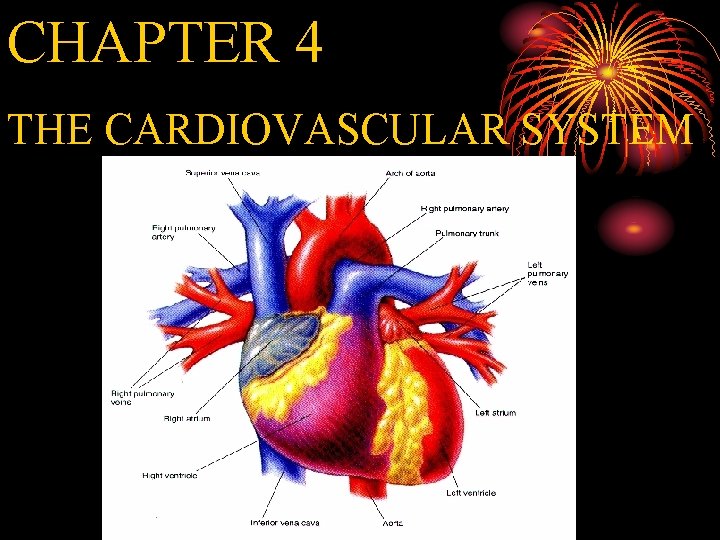
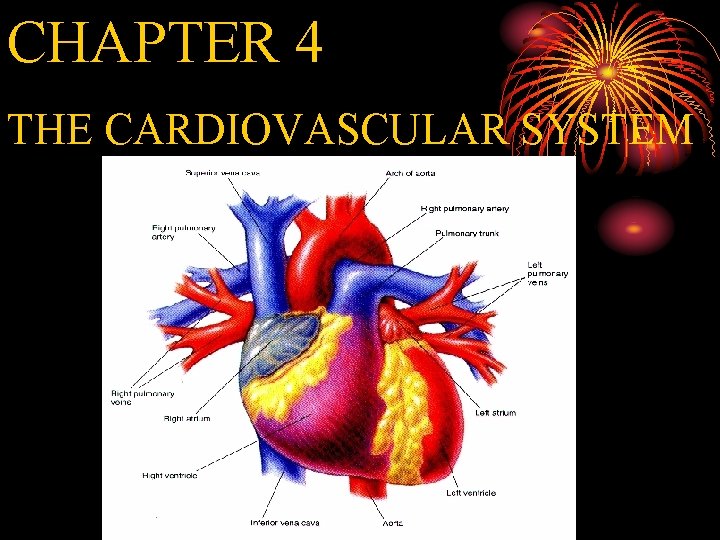
CHAPTER 4 THE CARDIOVASCULAR SYSTEM
Ø Weight of the heart 300 g Ø Work: 75/min, 10000 beats /day Ø 35 million beats /year, 2. 5 billion beats/life Ø 70 ml/beat, 7200 l/day The work of the heart in one life is equivalent to lifting 30 tons to the Mount Everest The busy and hard working heart!
MAIN FUNCTIONS OF THE CIRCULATORY SYSTEM Ø Transport and distribute essential substances to the tissues. Ø Remove metabolic byproducts. Ø Adjustment of oxygen and nutrient supply in different physiologic states. Ø Regulation of body temperature. Ø Humoral communication.
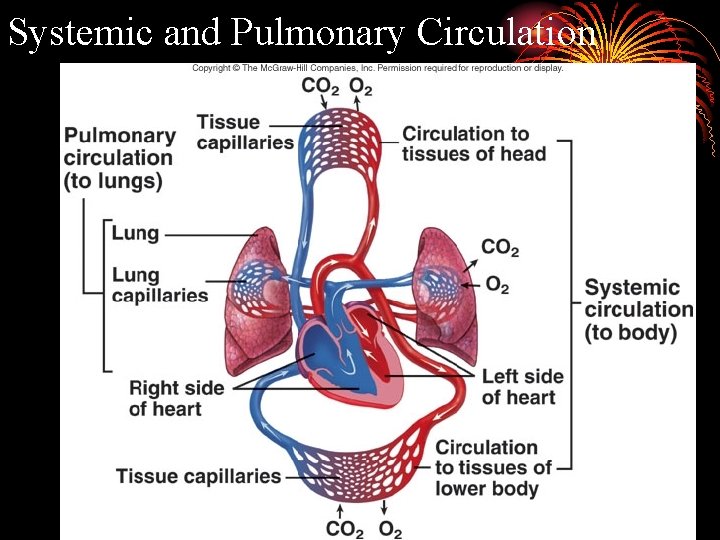
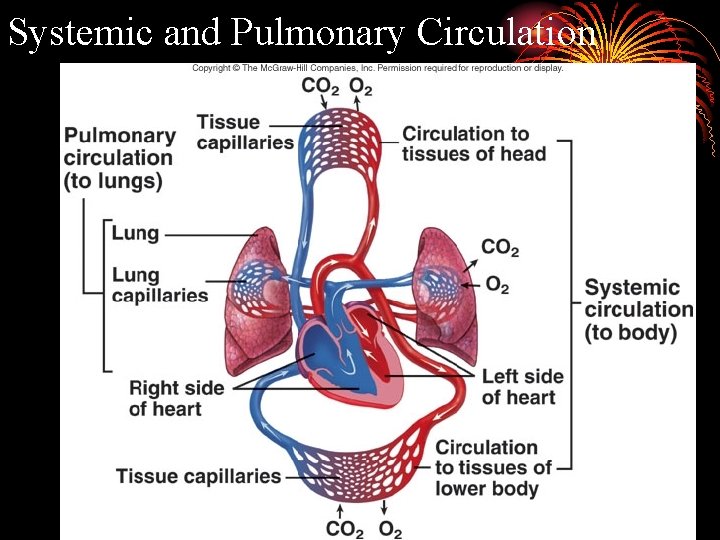
Systemic and Pulmonary Circulation
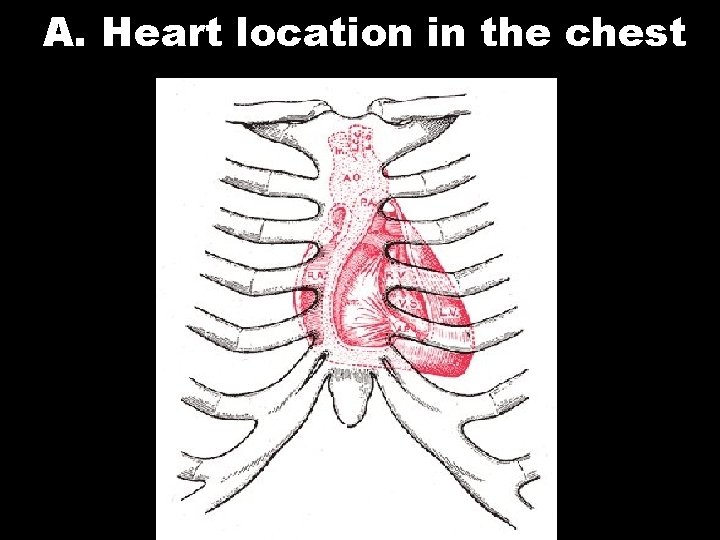
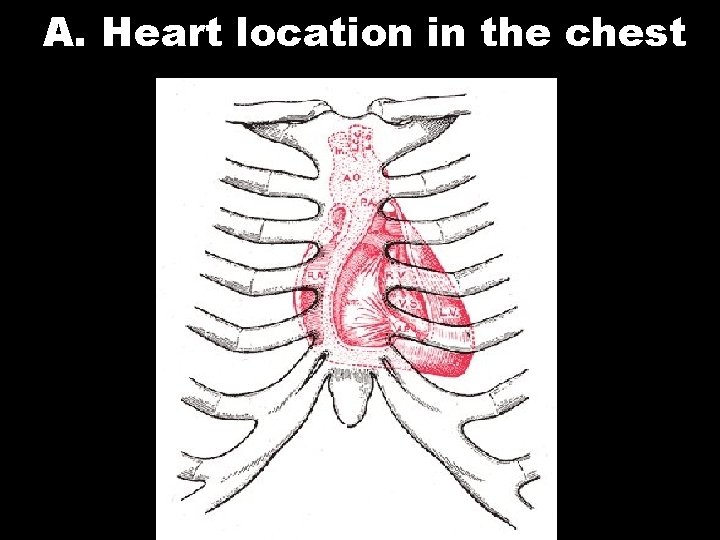
A. Heart location in the chest
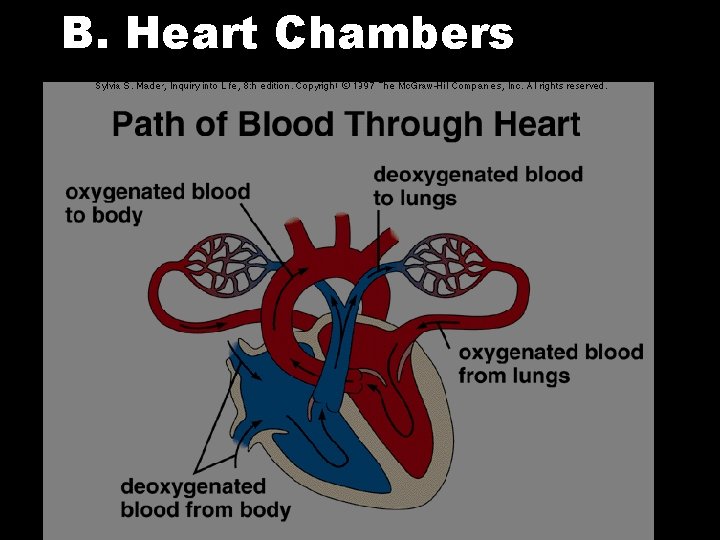
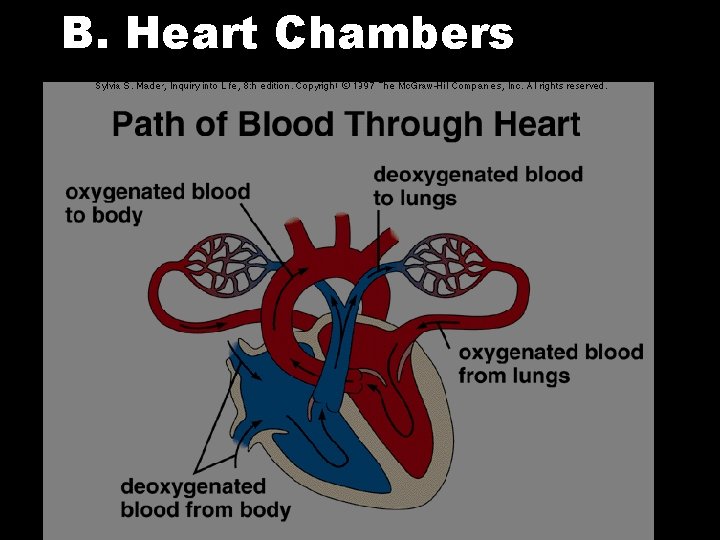
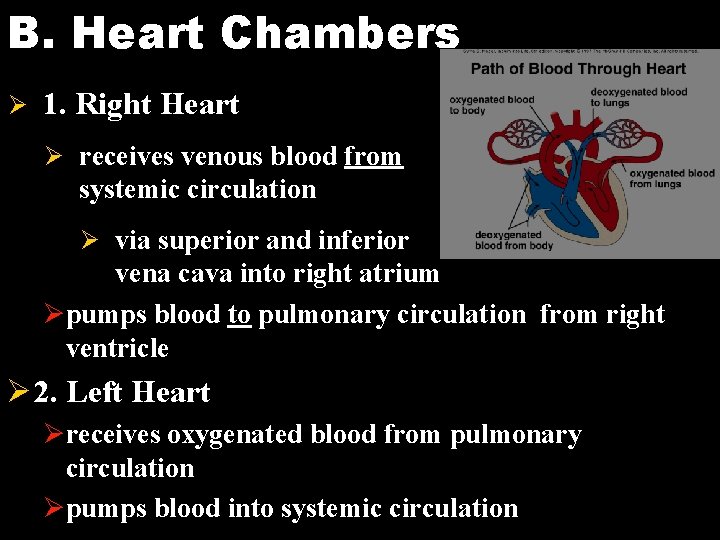
B. Heart Chambers
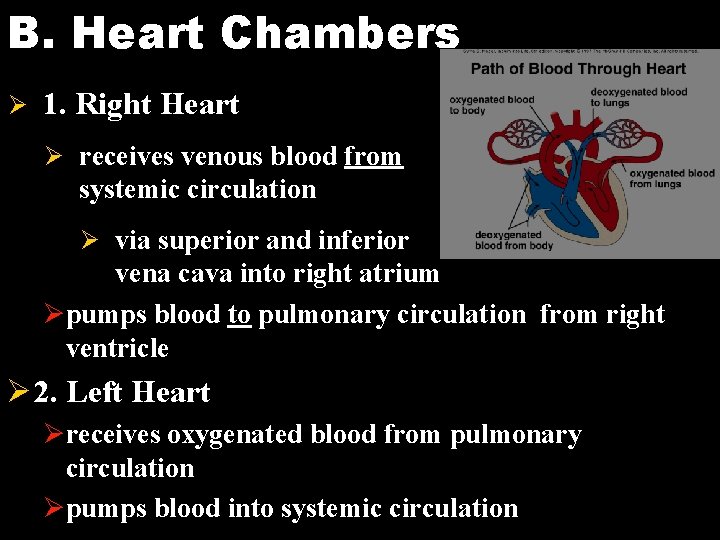
B. Heart Chambers Ø 1. Right Heart Ø receives venous blood from systemic circulation Ø via superior and inferior vena cava into right atrium Øpumps blood to pulmonary circulation from right ventricle Ø 2. Left Heart Øreceives oxygenated blood from pulmonary circulation Øpumps blood into systemic circulation
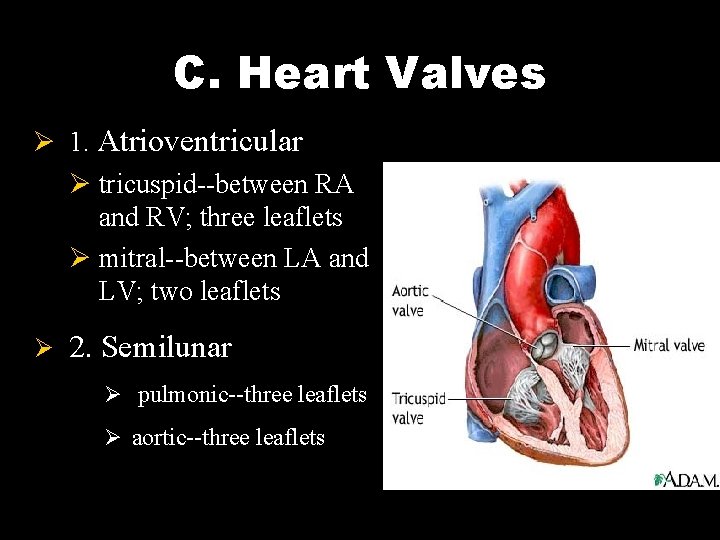
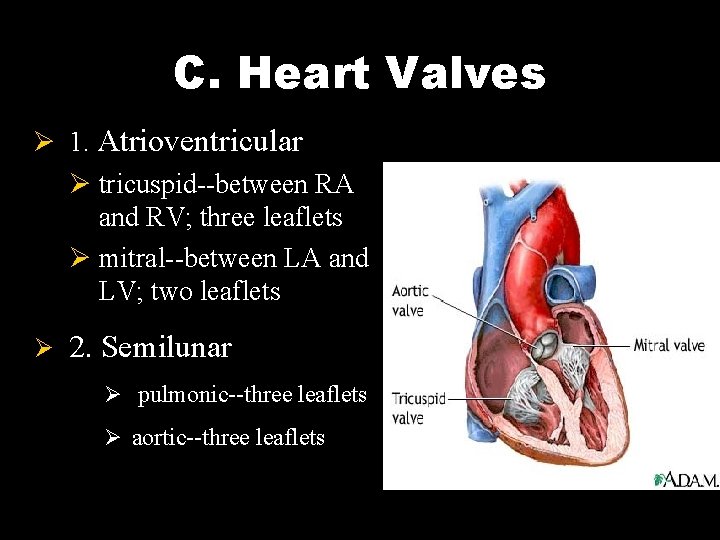
C. Heart Valves Ø 1. Atrioventricular Ø tricuspid--between RA and RV; three leaflets Ø mitral--between LA and LV; two leaflets Ø 2. Semilunar Ø pulmonic--three leaflets Ø aortic--three leaflets


Heart Valves Ø Prevent backward regurgitation Ø Provide low resistance to forward flow
Section 1 The Heart as a Pump Ø I Cardiac Cycle Ø The period from the end of one heart contraction to the end of the next
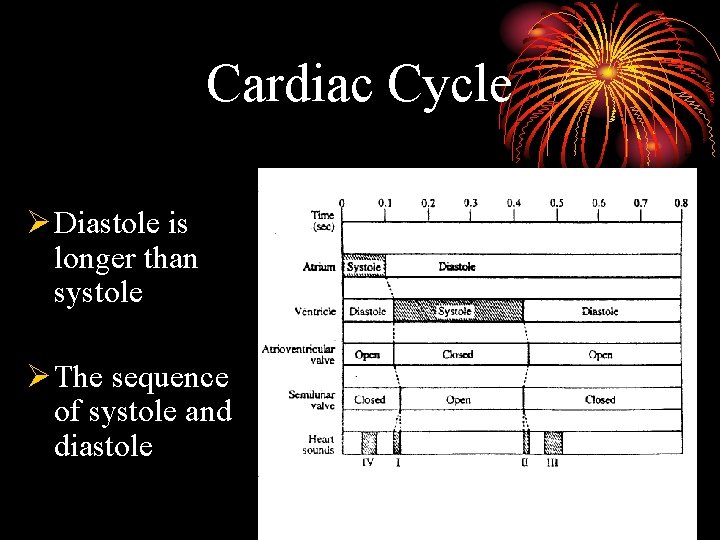
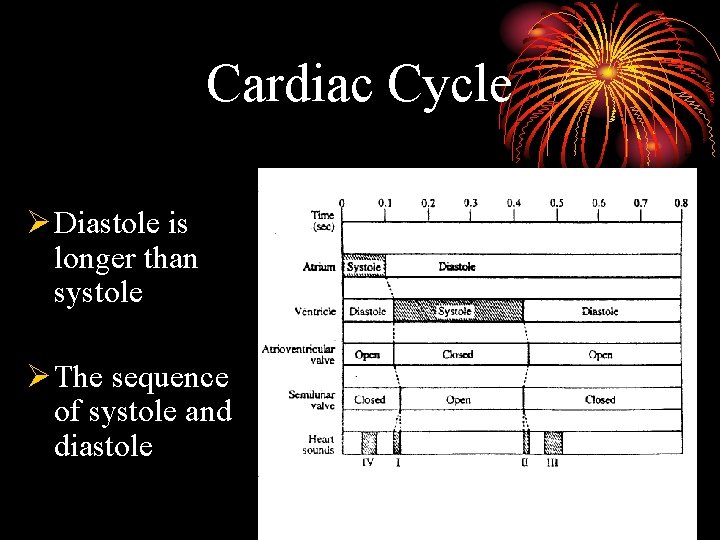
Cardiac Cycle Ø Diastole is longer than systole Ø The sequence of systole and diastole
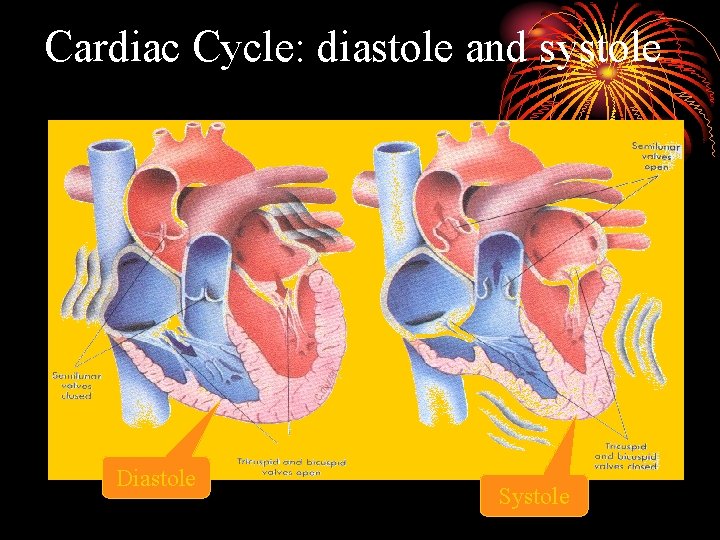
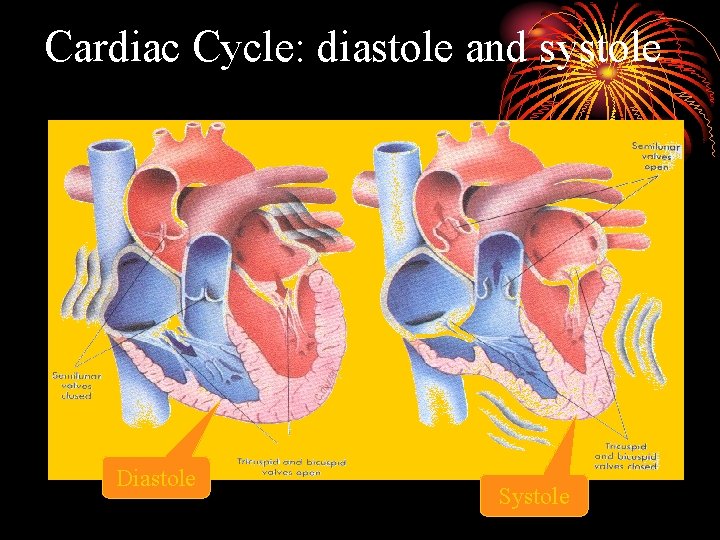
Cardiac Cycle: diastole and systole Diastole Systole
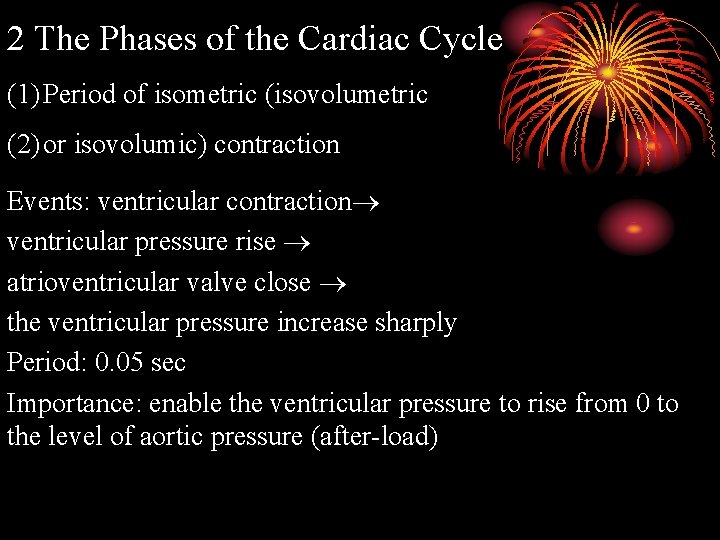
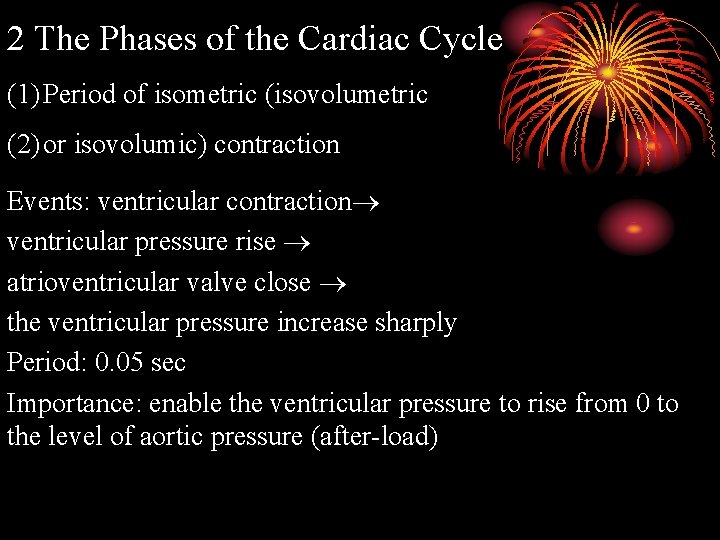
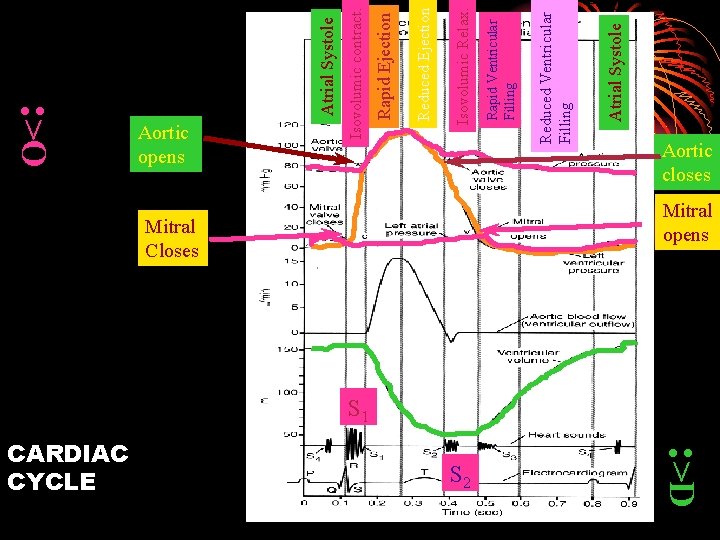
2 The Phases of the Cardiac Cycle (1) Period of isometric (isovolumetric (2) or isovolumic) contraction Events: ventricular contraction ventricular pressure rise atrioventricular valve close the ventricular pressure increase sharply Period: 0. 05 sec Importance: enable the ventricular pressure to rise from 0 to the level of aortic pressure (after-load)
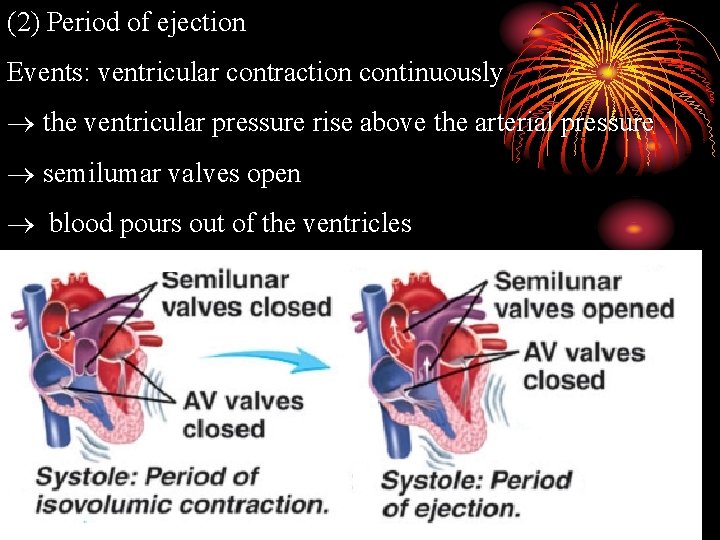
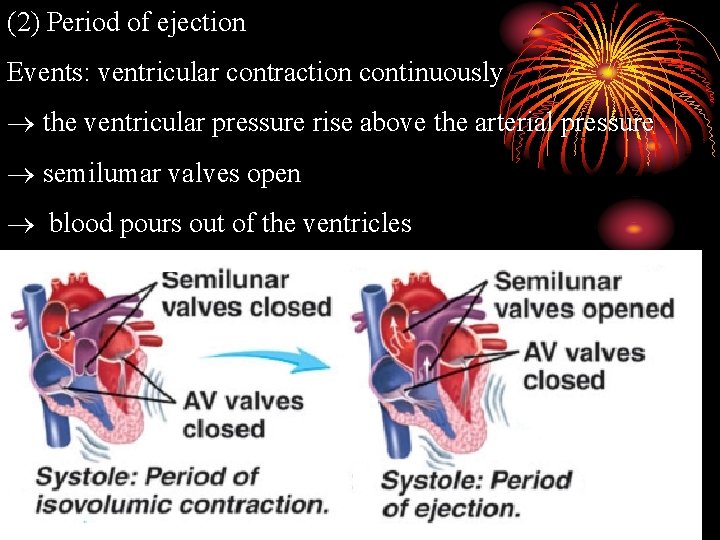
(2) Period of ejection Events: ventricular contraction continuously the ventricular pressure rise above the arterial pressure semilumar valves open blood pours out of the ventricles
Ø Rapid ejection period (0. 10 s, 60% of the stroke volume) Ø Reduced ejection period (0. 15 s, 40% of the stroke volume)
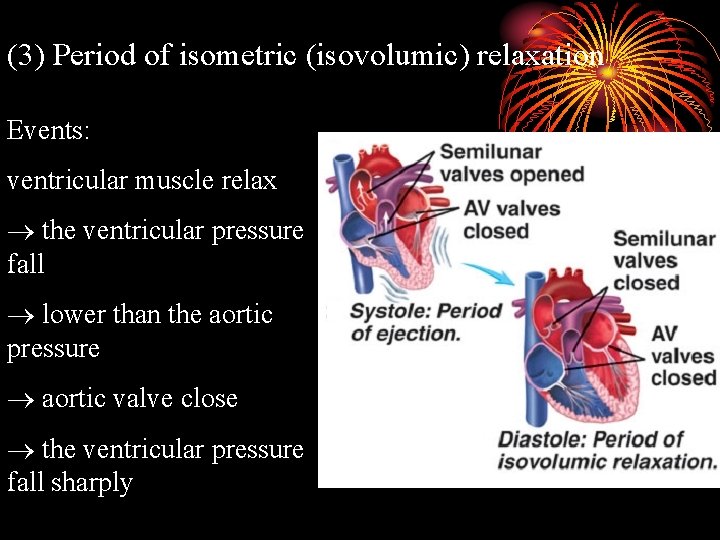
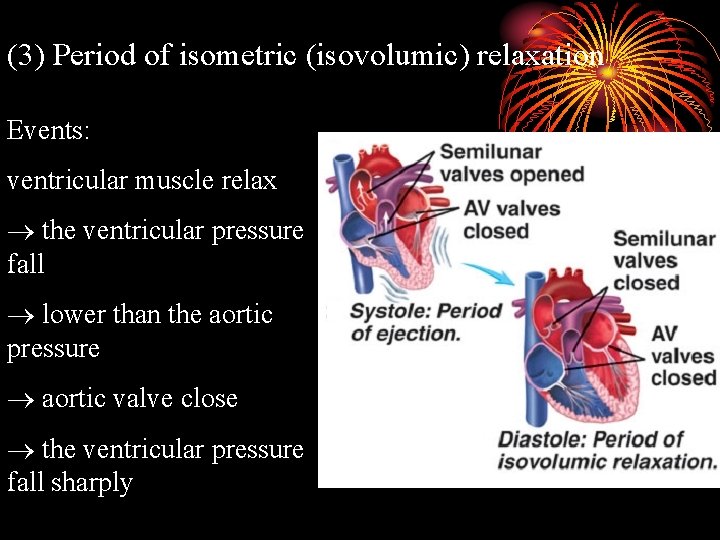
(3) Period of isometric (isovolumic) relaxation Events: ventricular muscle relax the ventricular pressure fall lower than the aortic pressure aortic valve close the ventricular pressure fall sharply
Period: 0. 06 -0. 08 s Importance: Enable the ventricular pressure fall to the level near the atrial pressure
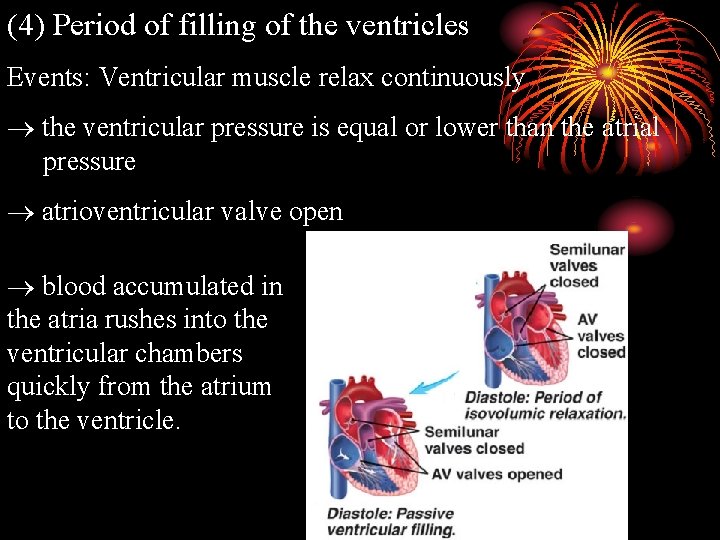
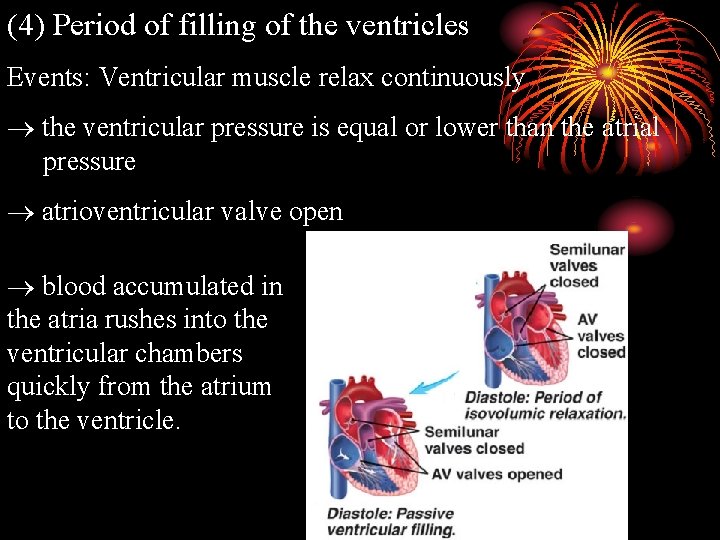
(4) Period of filling of the ventricles Events: Ventricular muscle relax continuously the ventricular pressure is equal or lower than the atrial pressure atrioventricular valve open blood accumulated in the atria rushes into the ventricular chambers quickly from the atrium to the ventricle.
Ø Period of rapid filling. (0. 11 s, amount of filling, 2/3) Ø Period of reduced filling (0. 22 s, little blood fills into the ventricle)
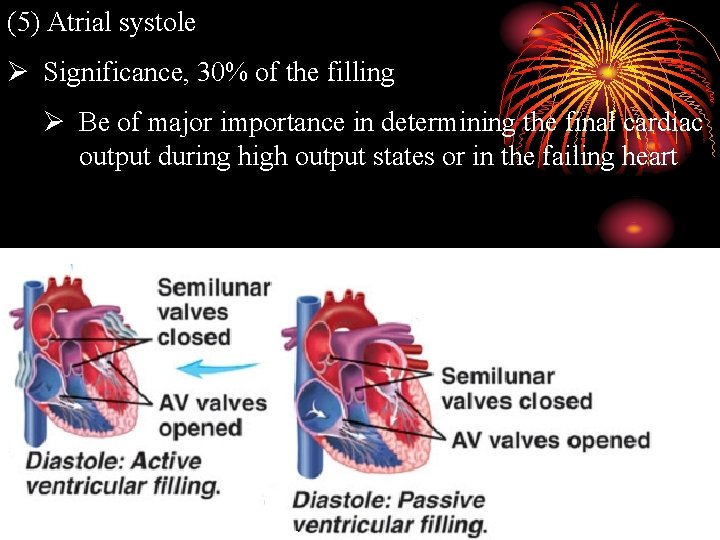
(5) Atrial systole Ø Significance, 30% of the filling Ø Be of major importance in determining the final cardiac output during high output states or in the failing heart

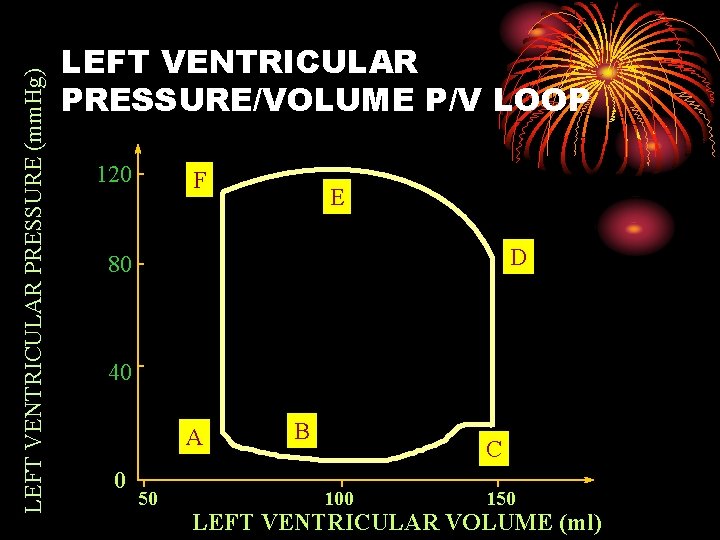
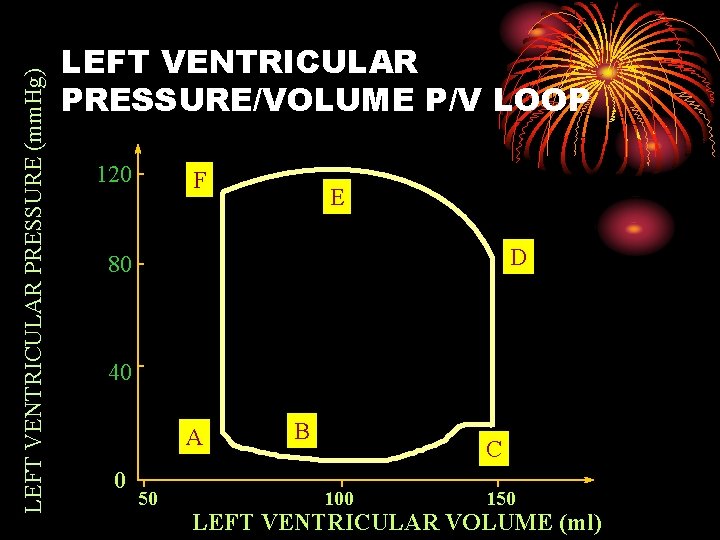
LEFT VENTRICULAR PRESSURE (mm. Hg) LEFT VENTRICULAR PRESSURE/VOLUME P/V LOOP 120 F E D 80 40 A 0 50 B C 100 150 LEFT VENTRICULAR VOLUME (ml)

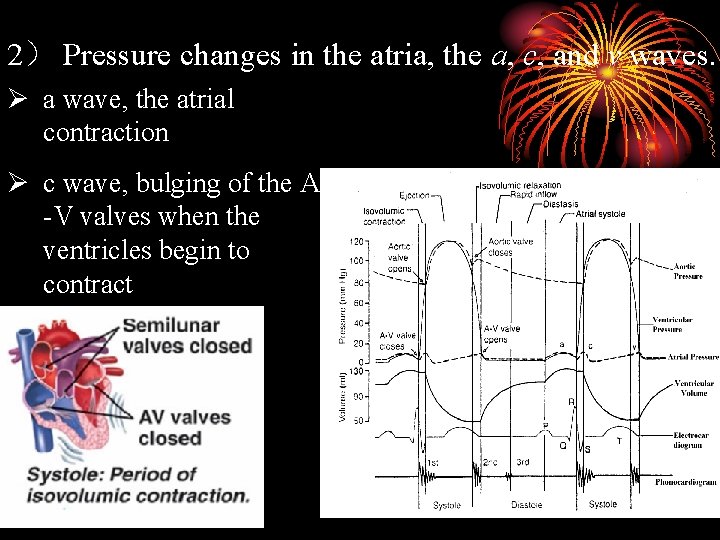
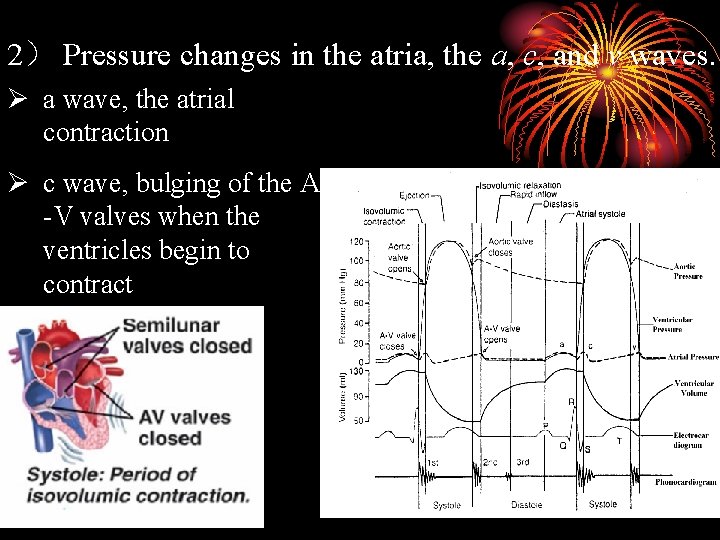
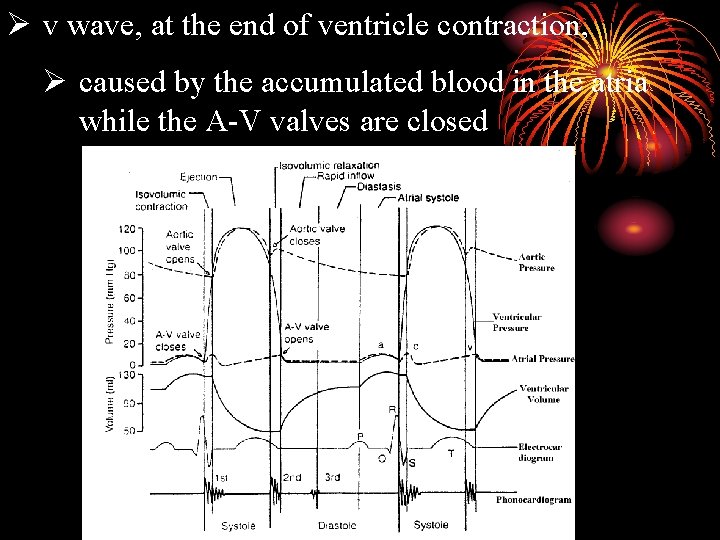
2) Pressure changes in the atria, the a, c, and v waves. Ø a wave, the atrial contraction Ø c wave, bulging of the A -V valves when the ventricles begin to contract
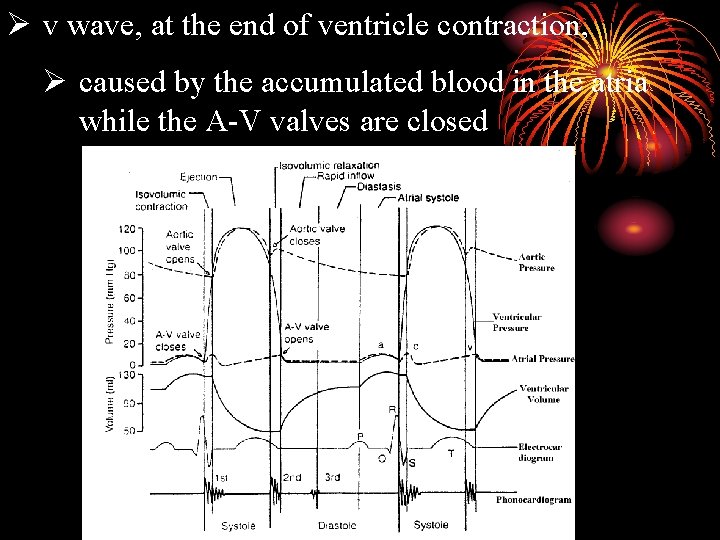
Ø v wave, at the end of ventricle contraction, Ø caused by the accumulated blood in the atria while the A-V valves are closed
Heart Sounds The sounds heard over the cardiac region produced by the functioning of the heart.
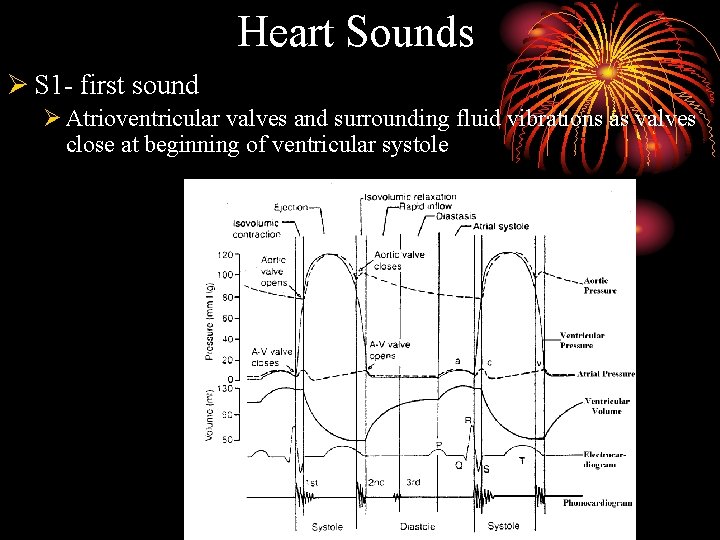
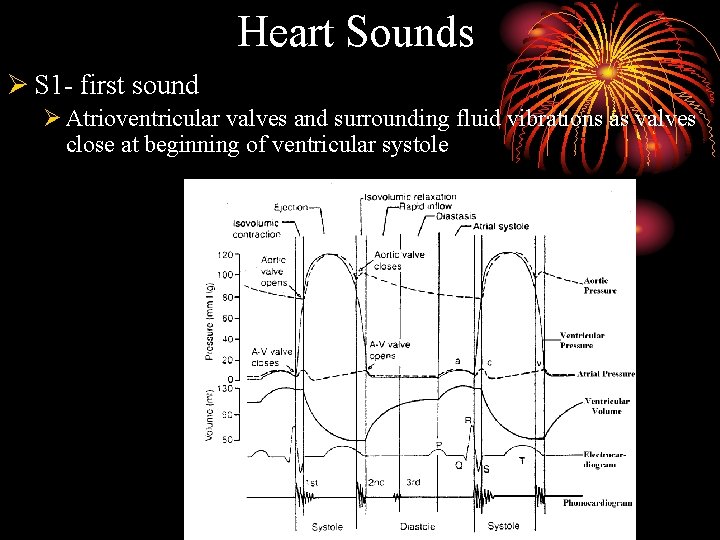
Heart Sounds Ø S 1 - first sound Ø Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole
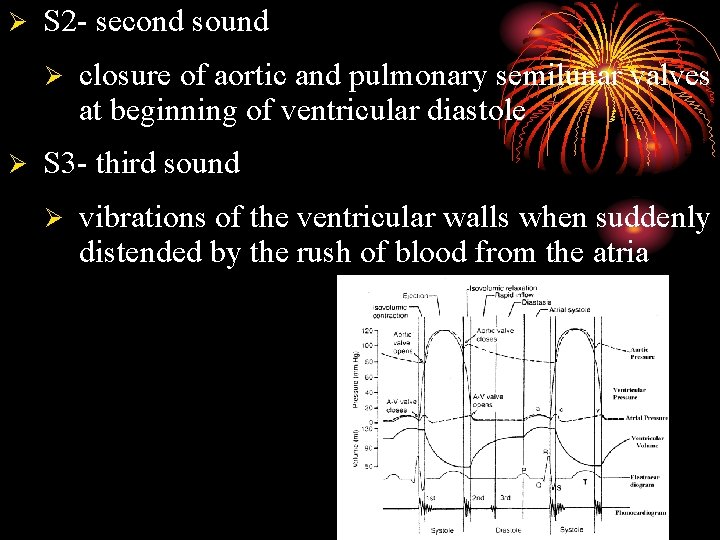
Ø S 2 - second sound Ø Ø closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole S 3 - third sound Ø vibrations of the ventricular walls when suddenly distended by the rush of blood from the atria
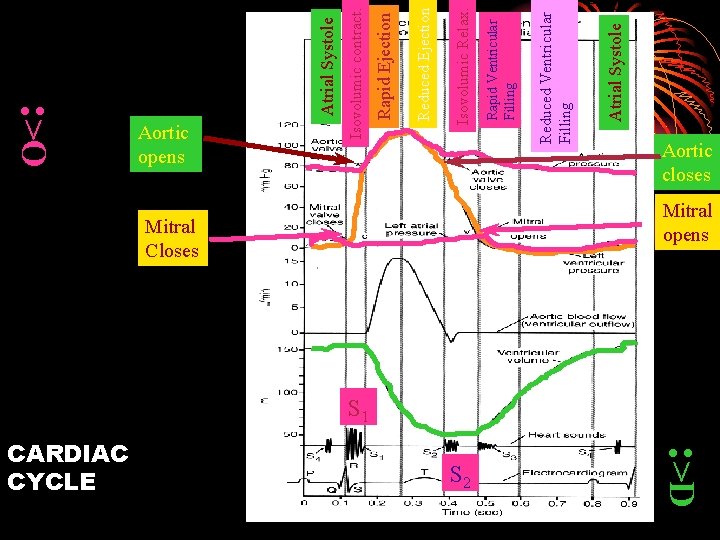
Mitral Closes : >D S 2 Atrial Systole Reduced Ventricular Filling Rapid Ventricular Filling Isovolumic Relax. Reduced Ejection Rapid Ejection Isovolumic contract. Atrial Systole : >O CARDIAC CYCLE Aortic opens Aortic closes Mitral opens S 1

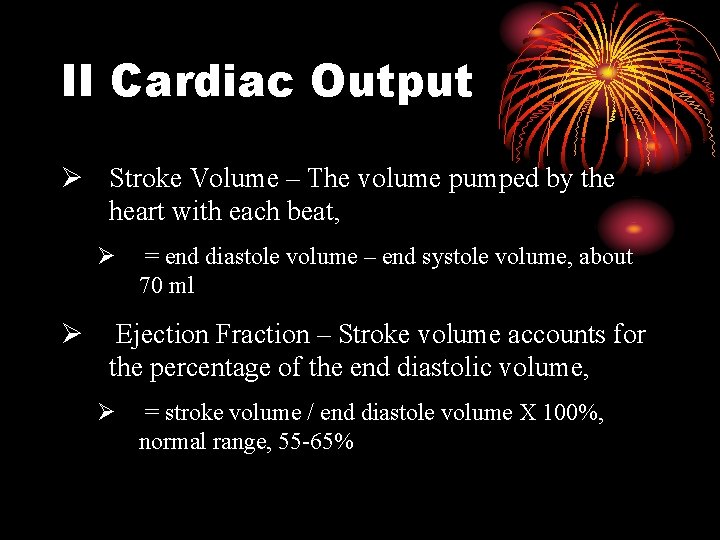
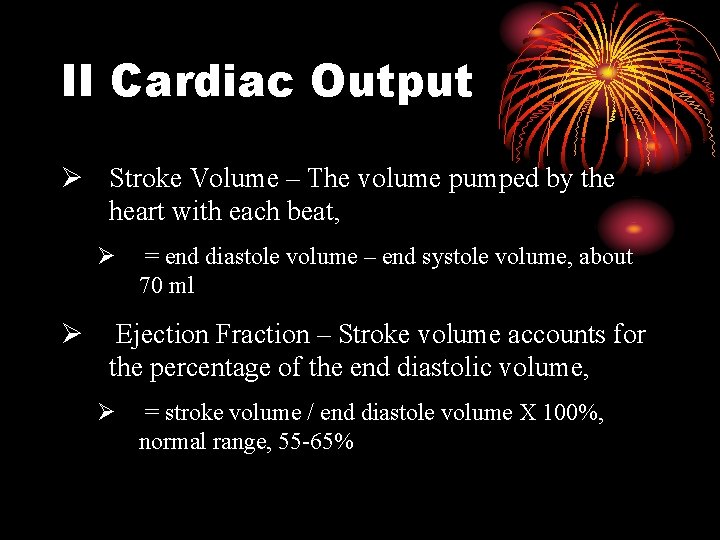
II Cardiac Output Ø Stroke Volume – The volume pumped by the heart with each beat, Ø Ø = end diastole volume – end systole volume, about 70 ml Ejection Fraction – Stroke volume accounts for the percentage of the end diastolic volume, Ø = stroke volume / end diastole volume X 100%, normal range, 55 -65%
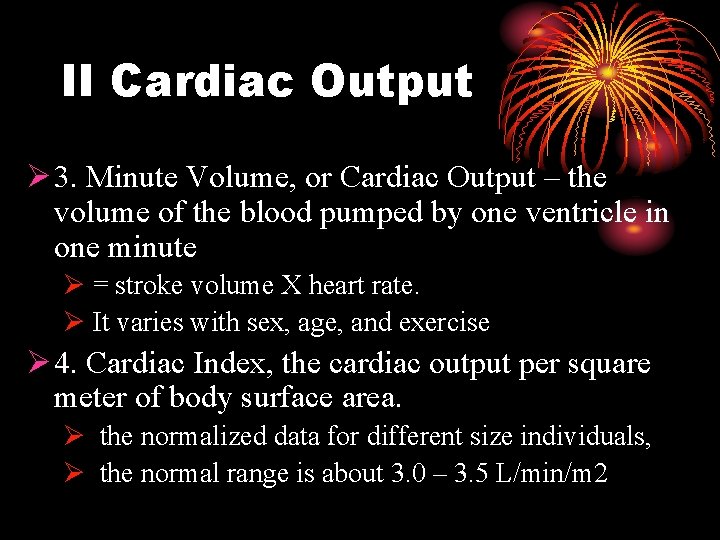
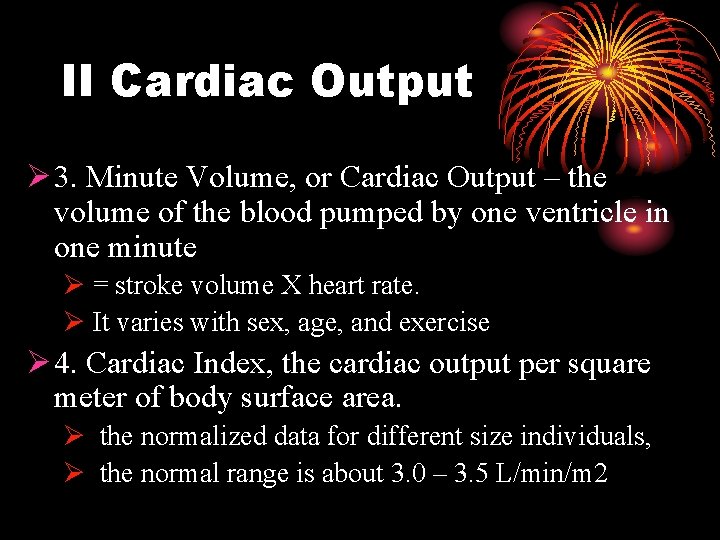
II Cardiac Output Ø 3. Minute Volume, or Cardiac Output – the volume of the blood pumped by one ventricle in one minute Ø = stroke volume X heart rate. Ø It varies with sex, age, and exercise Ø 4. Cardiac Index, the cardiac output per square meter of body surface area. Ø the normalized data for different size individuals, Ø the normal range is about 3. 0 – 3. 5 L/min/m 2
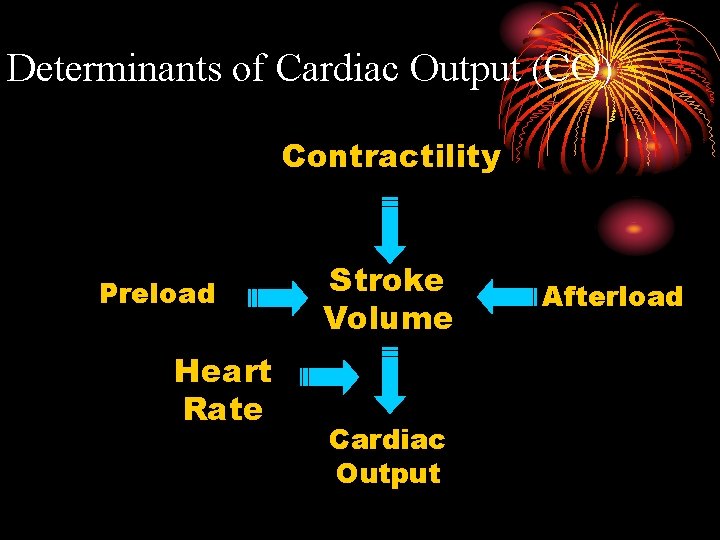
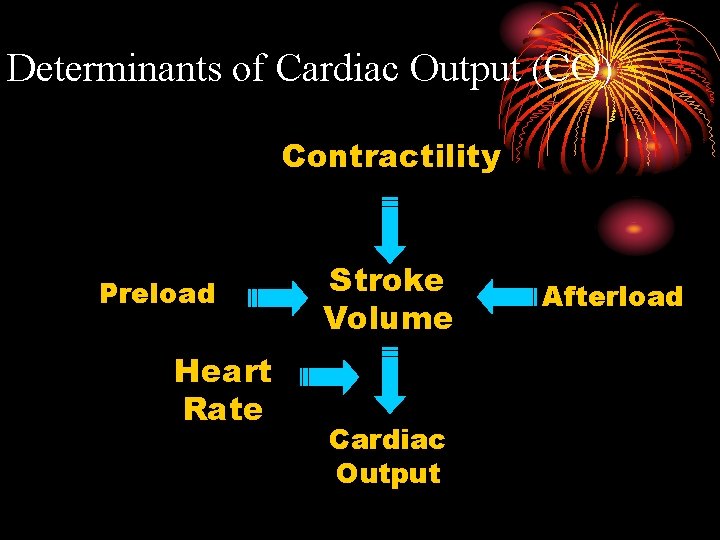
Determinants of Cardiac Output (CO) Contractility Preload Heart Rate Stroke Volume Cardiac Output Afterload
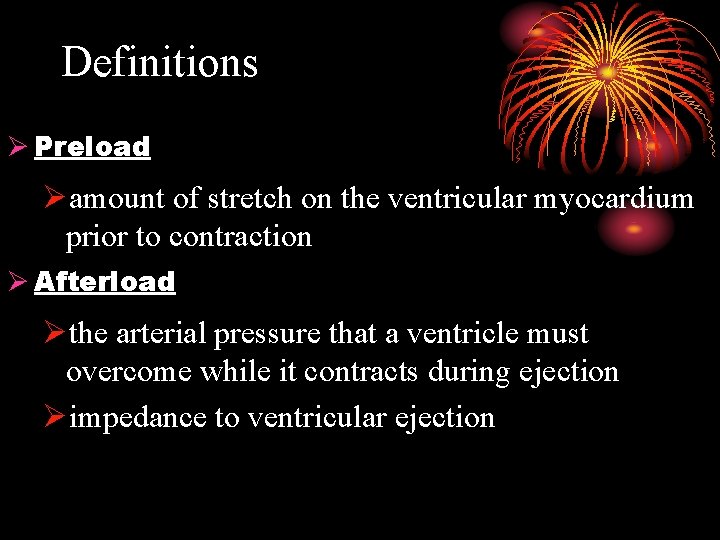
Definitions Ø Preload Øamount of stretch on the ventricular myocardium prior to contraction Ø Afterload Øthe arterial pressure that a ventricle must overcome while it contracts during ejection Øimpedance to ventricular ejection
Definitions Ø Contractility Ø myocardium’s intrinsic ability to efficiently contract and empty the ventricle Ø (independent of preload & afterload)
Determinants of Cardiac Output 1. Preload
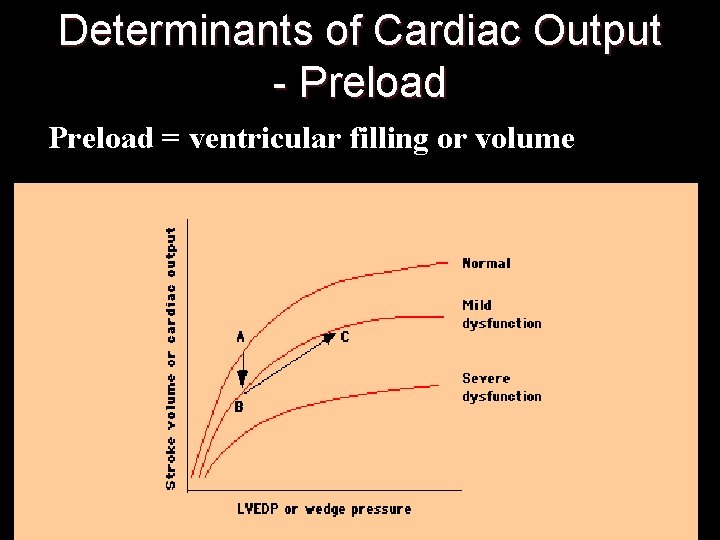
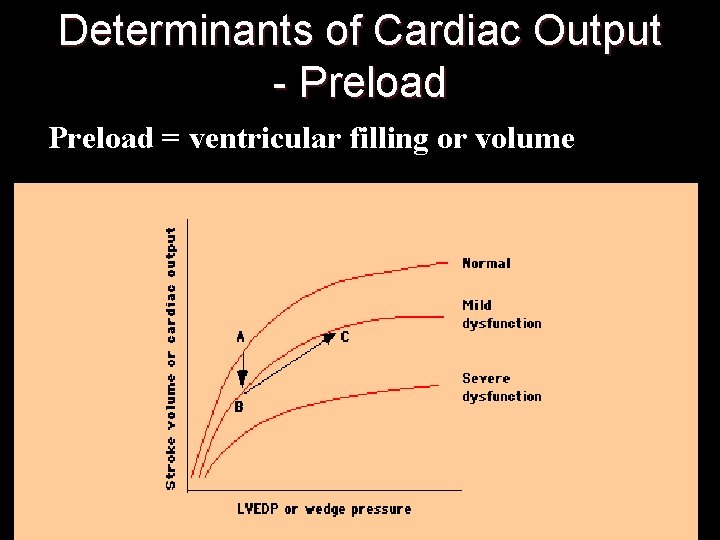
Determinants of Cardiac Output - Preload = ventricular filling or volume
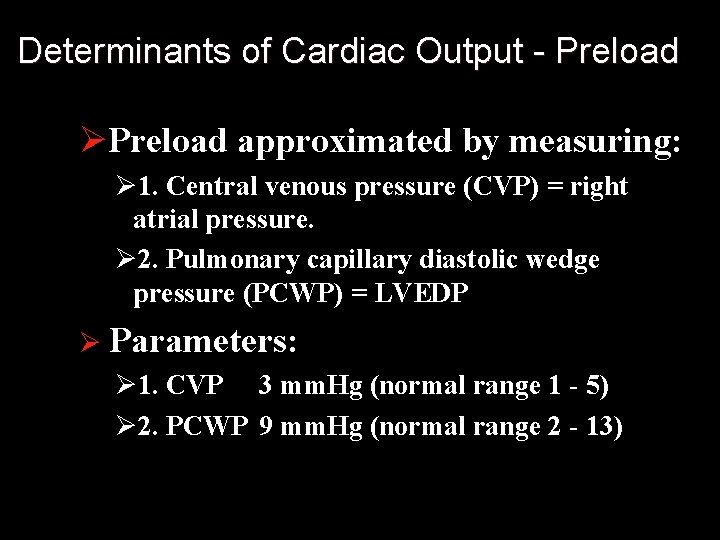
Determinants of Cardiac Output - Preload ØPreload approximated by measuring: Ø 1. Central venous pressure (CVP) = right atrial pressure. Ø 2. Pulmonary capillary diastolic wedge pressure (PCWP) = LVEDP Ø Parameters: Ø 1. CVP 3 mm. Hg (normal range 1 - 5) Ø 2. PCWP 9 mm. Hg (normal range 2 - 13)
Frank-Starling Mechanism of the Heart The intrinsic ability of the heart to adapt to changing volumes of inflowing blood
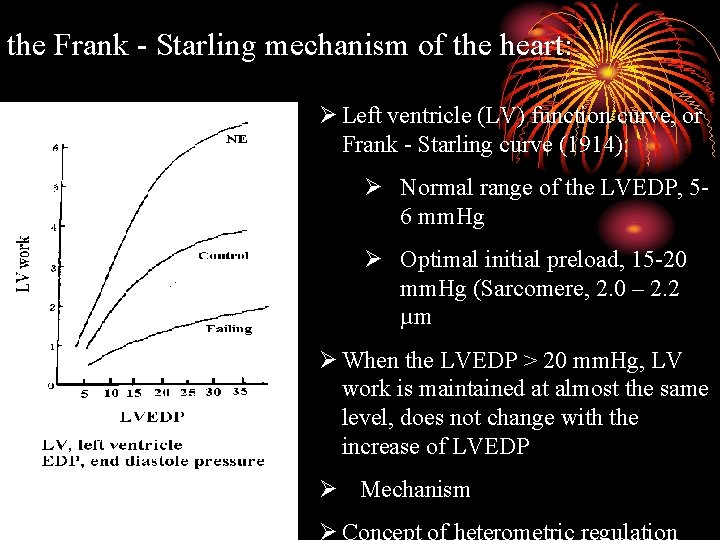
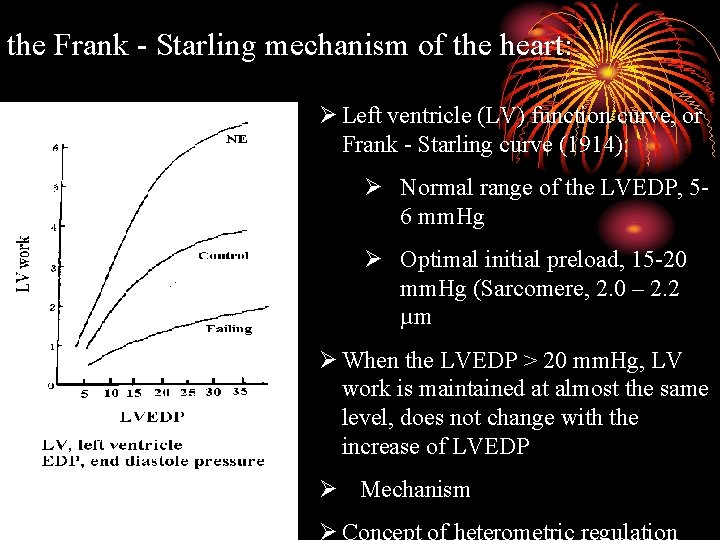
the Frank - Starling mechanism of the heart: Ø Left ventricle (LV) function curve, or Frank - Starling curve (1914): Ø Normal range of the LVEDP, 56 mm. Hg Ø Optimal initial preload, 15 -20 mm. Hg (Sarcomere, 2. 0 – 2. 2 µm Ø When the LVEDP > 20 mm. Hg, LV work is maintained at almost the same level, does not change with the increase of LVEDP Ø Mechanism
Factors determining the preload (LVEDP) Ø Period of the ventricle diastole (filling) – heart rate Ø Speed of the venous return Ø (difference between the venous pressure and atrial pressure)
Importance of the heterometeric regulation Ø In general, heterometric regulation plays only a short-time role, such as during Øthe body posture change Øartery pressure increase Øunbalance of ventricular outputs Ø In other conditions, such as exercise, cardiac output is mainly regulated by homometric regulation.
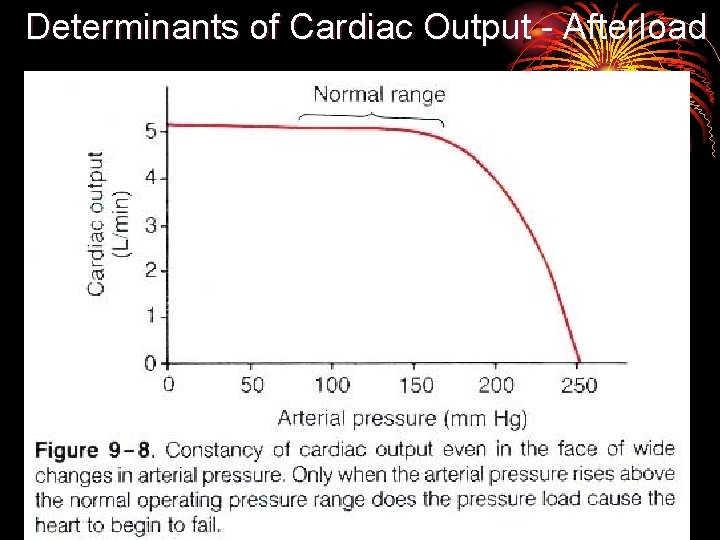
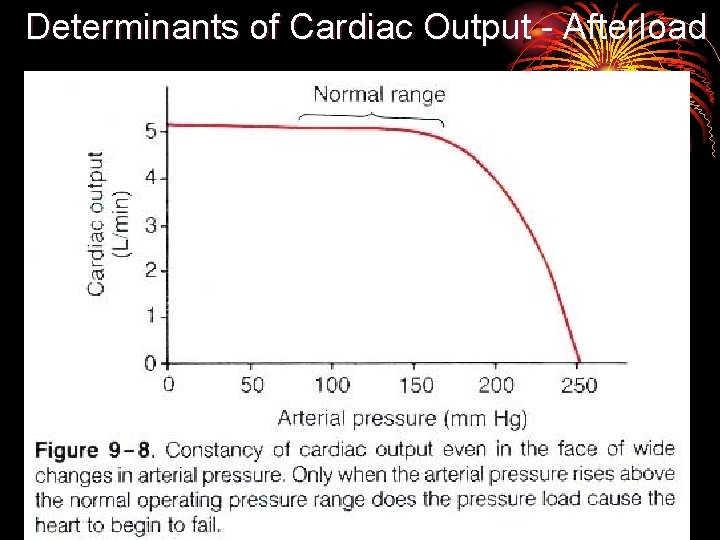
Determinants of Cardiac Output - Afterload
Short time change of the arterial pressure Transit arterial pressure rise Øisovolumetric contraction phase become longer Ø period of ejection shorter Ø stroke volume less Ø more blood left in the ventricle left ØLVEDP increase Ø through heterometeric regulation Ø stroke volume return to normal in next beat.
Long time high arterial pressure Øthrough neural and humoral regulation Ø the stroke volume is maintained at normal level Øpathogenesis of the cardiovascular system
Determinants of Cardiac Output - Contractility (neural and humoral regulation) Sympathetic nerve (norepinephrine) or the epinephrine and norepinephrine (adrenal gland) enhance the strength and the velocity of the cardiac contraction. The change of myocardial property is independent of the preload. We call it the contractility. Importance: exert a long – time influence on the cardiac output.

Definitions Ø Contractility Ømyocardium’s intrinsic ability to efficiently contract and empty the ventricle Ø(independent of preload & afterload)
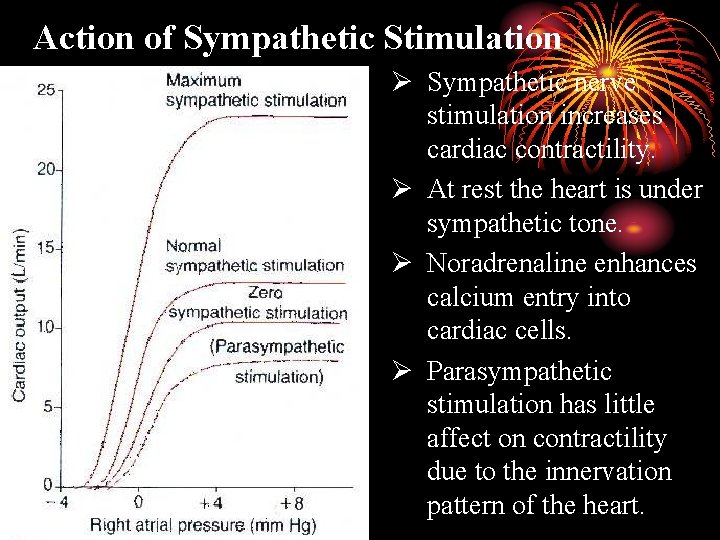
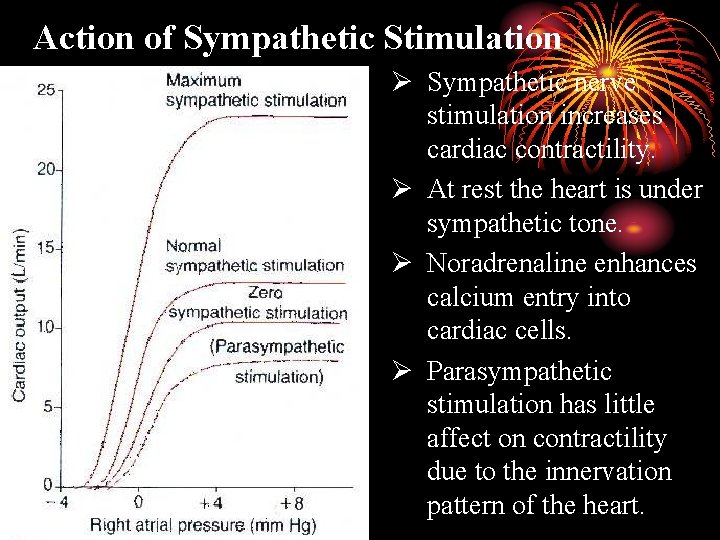
Action of Sympathetic Stimulation Ø Sympathetic nerve stimulation increases cardiac contractility. Ø At rest the heart is under sympathetic tone. Ø Noradrenaline enhances calcium entry into cardiac cells. Ø Parasympathetic stimulation has little affect on contractility due to the innervation pattern of the heart.
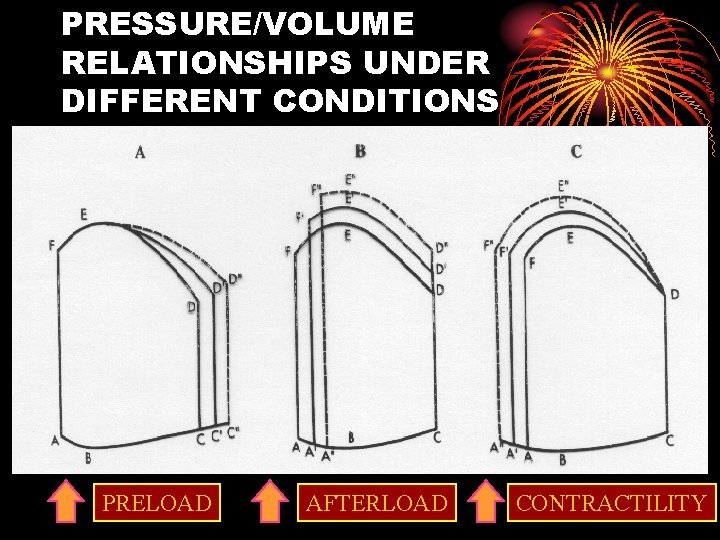
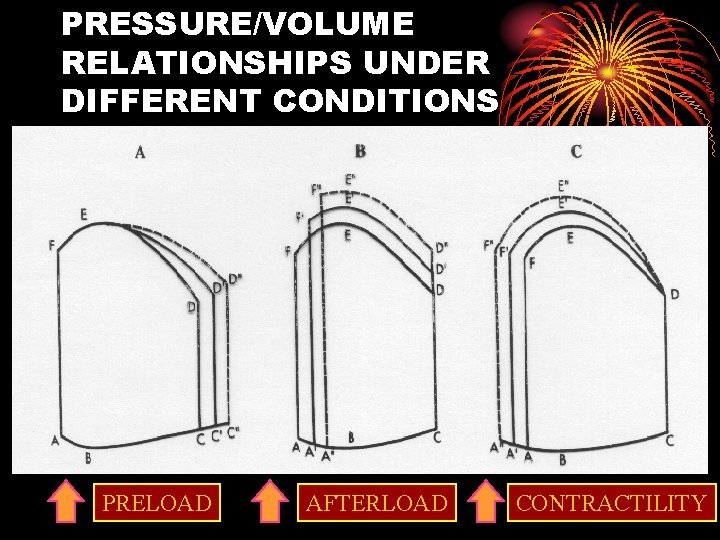
PRESSURE/VOLUME RELATIONSHIPS UNDER DIFFERENT CONDITIONS PRELOAD AFTERLOAD CONTRACTILITY
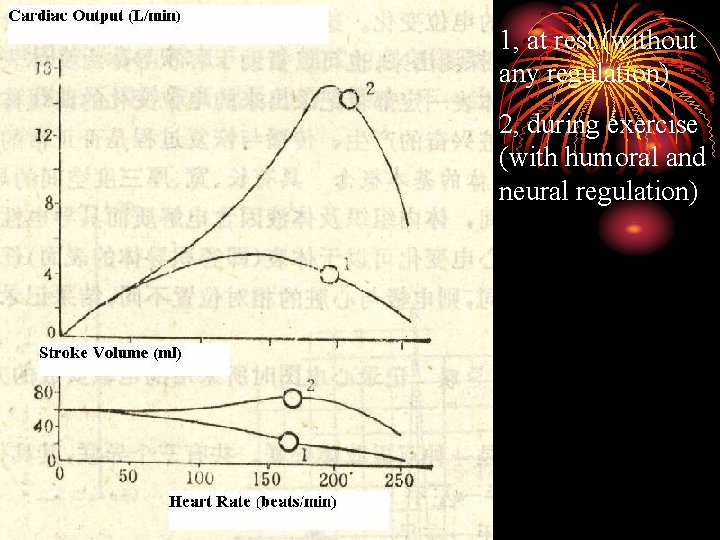
Determinants of Cardiac Output - The heart rate ØNormal range of the heart rate 60 – 100 beats/min ØWithin physiological limit? , the higher the heart rate, the more blood that the heart pump.
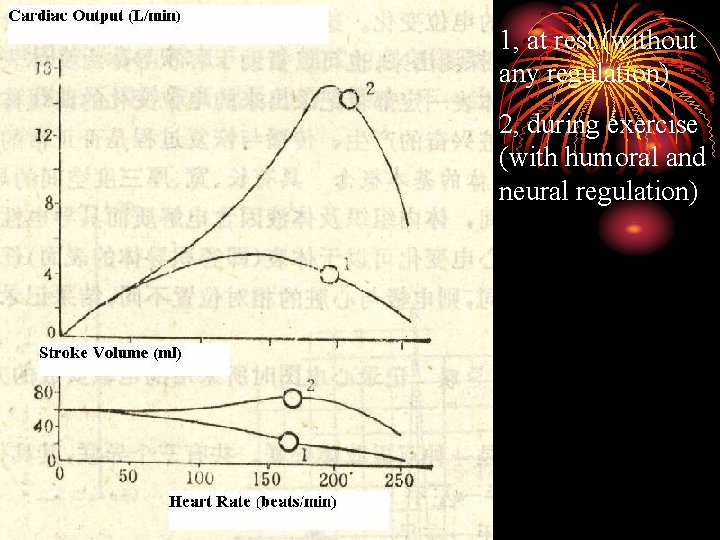
1, at rest (without any regulation) 2, during exercise (with humoral and neural regulation)
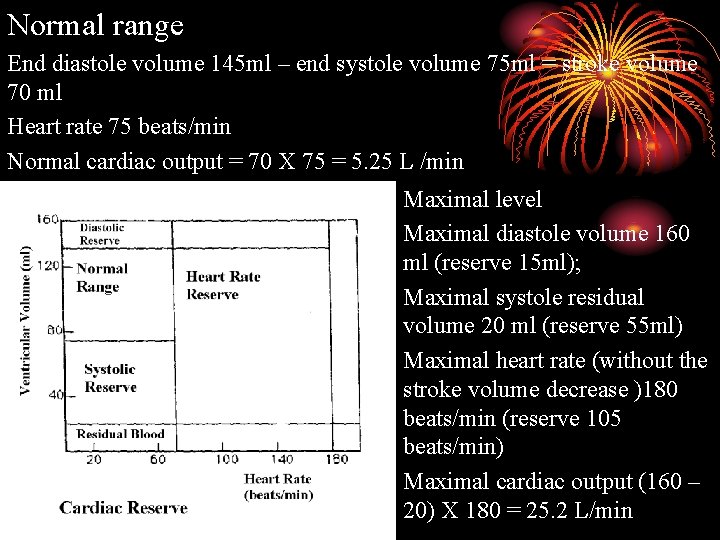
IV Cardiac Output Reserve ØThe maximal cardiac output subtracts the normal value. ØIt reflects the ability of the heart to adapt the change of environment (internal or external)
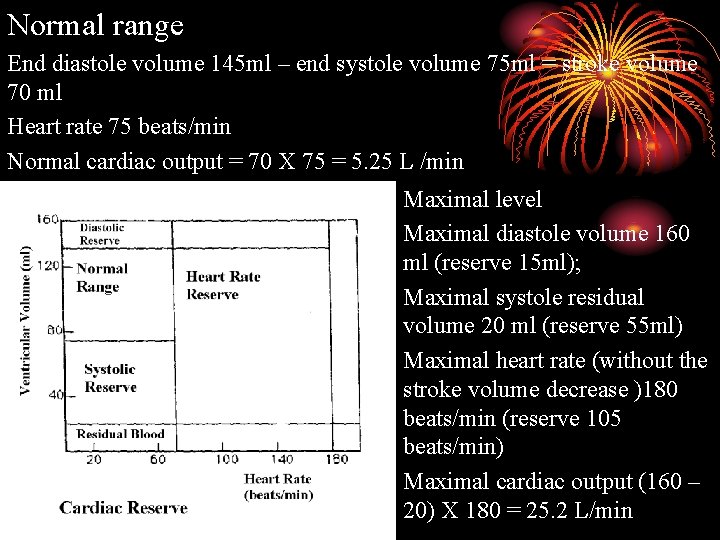
Normal range End diastole volume 145 ml – end systole volume 75 ml = stroke volume 70 ml Heart rate 75 beats/min Normal cardiac output = 70 X 75 = 5. 25 L /min Maximal level Maximal diastole volume 160 ml (reserve 15 ml); Maximal systole residual volume 20 ml (reserve 55 ml) Maximal heart rate (without the stroke volume decrease )180 beats/min (reserve 105 beats/min) Maximal cardiac output (160 – 20) X 180 = 25. 2 L/min
 Sequel
Sequel Alex liu cecilia liu
Alex liu cecilia liu Líu líu lo lo ta ca hát say sưa
Líu líu lo lo ta ca hát say sưa Yong loo lin school of medicine
Yong loo lin school of medicine What is the next letter? a z b y c x d
What is the next letter? a z b y c x d Four seasons korean movie
Four seasons korean movie Yong mok hin
Yong mok hin Kwon ji yong age
Kwon ji yong age Lei yong
Lei yong Berney v tronoh mines
Berney v tronoh mines Aaron tan tuck choy
Aaron tan tuck choy Yong lei
Yong lei Yong soon min
Yong soon min Mak yong
Mak yong Mis yong
Mis yong Ban yong
Ban yong Causes of cardiac arrest
Causes of cardiac arrest Sql yong
Sql yong Sql query
Sql query Membrane potential
Membrane potential Xbongda
Xbongda Chuẩn ieee 754/85
Chuẩn ieee 754/85 Ding chuan acupuncture point
Ding chuan acupuncture point Tìm miền hội tụ của chuỗi lũy thừa
Tìm miền hội tụ của chuỗi lũy thừa Giáo dục chuẩn mực ngữ âm tiếng việt
Giáo dục chuẩn mực ngữ âm tiếng việt Tiêu chuẩn leibnitz
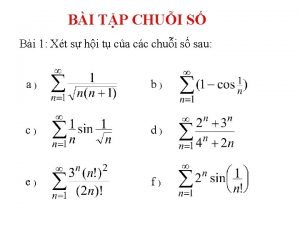
Tiêu chuẩn leibnitz 5 tiêu chuẩn finer
5 tiêu chuẩn finer Biểu diễn số thực 32 bit
Biểu diễn số thực 32 bit Tam chứng anthonisen
Tam chứng anthonisen Chuẩn đoán
Chuẩn đoán Xét nghiệm amylase
Xét nghiệm amylase Chuẩn mực nhóm
Chuẩn mực nhóm độ lệch chuẩn
độ lệch chuẩn đánh giá theo chuẩn nghề nghiệp giáo viên csgdpt
đánh giá theo chuẩn nghề nghiệp giáo viên csgdpt Gv tu jie
Gv tu jie Target institute of medical education and research
Target institute of medical education and research Pima medical institute dress code
Pima medical institute dress code Beijing medical equipment institute
Beijing medical equipment institute Ptal california medical board
Ptal california medical board Gbmc infoweb
Gbmc infoweb Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial lab manhattan beach
Torrance memorial lab manhattan beach Cartersville medical center medical records
Cartersville medical center medical records Charter school institute
Charter school institute Santa fe institute summer school
Santa fe institute summer school Diane liu md
Diane liu md Chiu-chu melissa liu
Chiu-chu melissa liu Lucy loo with my girl drew
Lucy loo with my girl drew Chee ming liu
Chee ming liu Yang liu stanford
Yang liu stanford Tongping liu
Tongping liu Jingchen liu
Jingchen liu Karin björsten liu
Karin björsten liu Seismoscope
Seismoscope Chim đậu trên cành chim hót líu lo
Chim đậu trên cành chim hót líu lo J liu
J liu Bing liu sentiment analysis
Bing liu sentiment analysis