LIU Chuan Yong Institute of Physiology Medical School



- Slides: 83
LIU Chuan Yong 刘传勇 Institute of Physiology Medical School of SDU Tel 88381175 (lab) 88382098 (office) Email: liucy@sdu. edu. cn Website: www. physiology. sdu. edu. cn 1
Section 3 Muscle Contraction
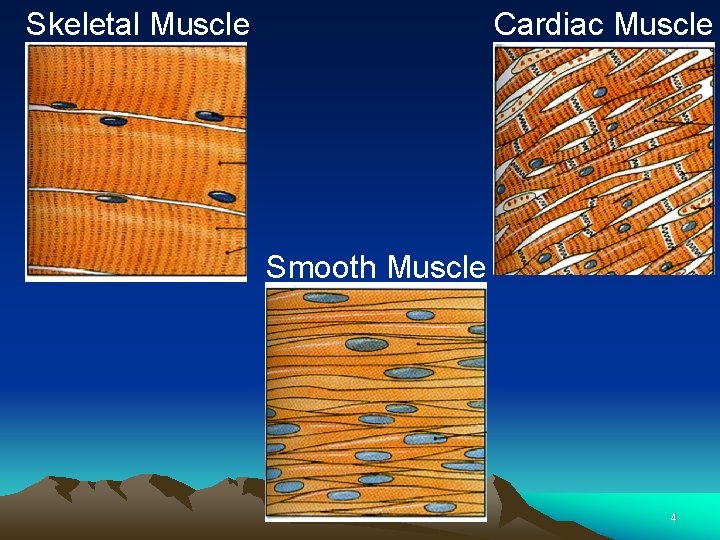
Classification of the Muscle Ø According to the structure: Striated Muscle, Smooth Muscle Ø According to the nerve innervation: Voluntary Muscle, Involuntary Muscle Ø According to the Function: Skeletal Muscle, Cardiac Contraction, Smooth Muscle 3
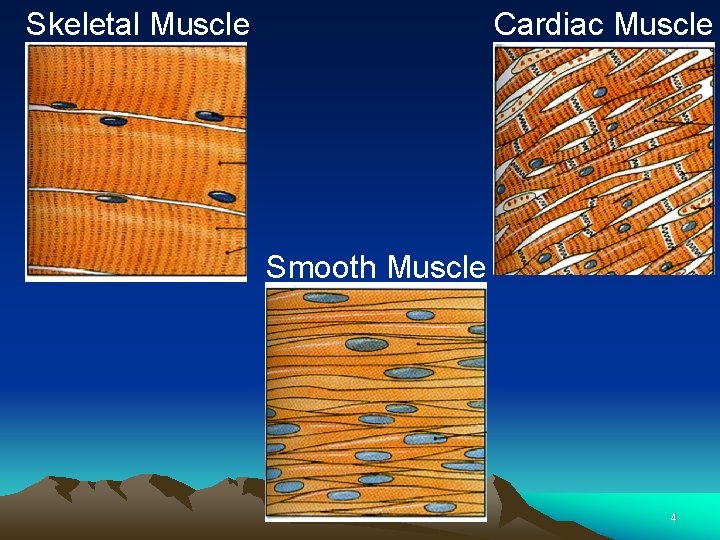
Skeletal Muscle Cardiac Muscle Smooth Muscle 4
I Signal Transmission Through the Neuromuscular Junction
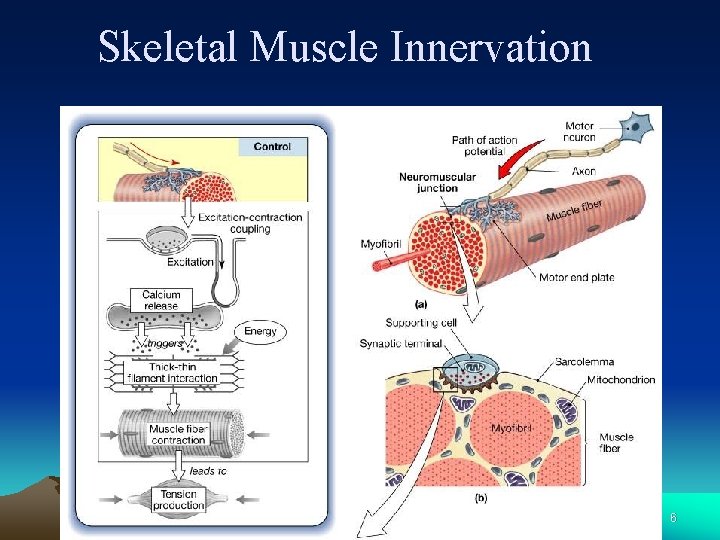
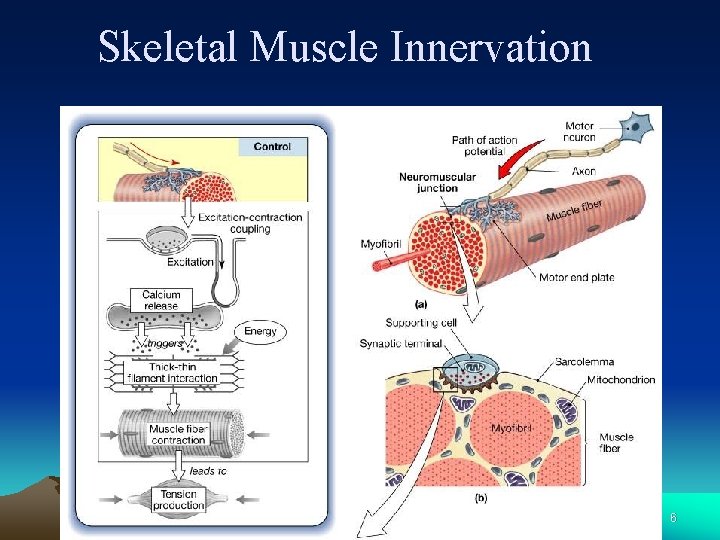
Skeletal Muscle Innervation 6
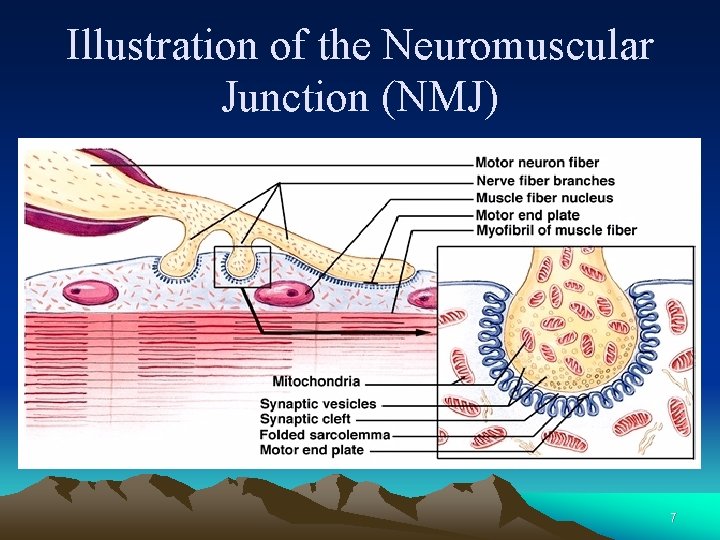
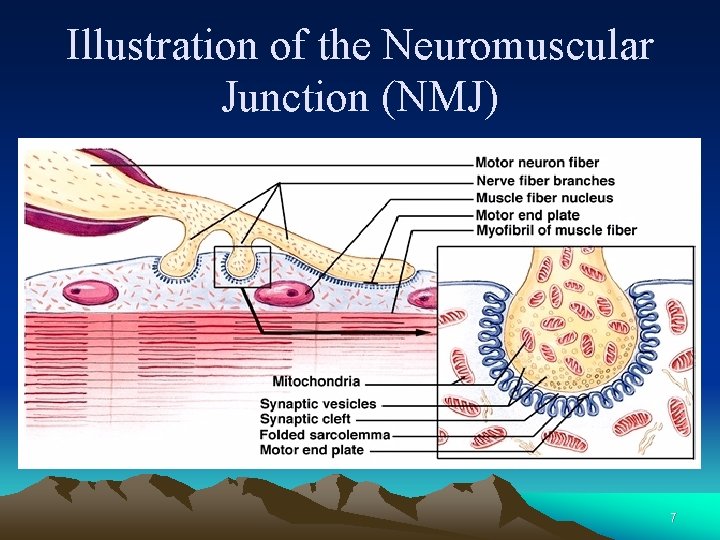
Illustration of the Neuromuscular Junction (NMJ) 7
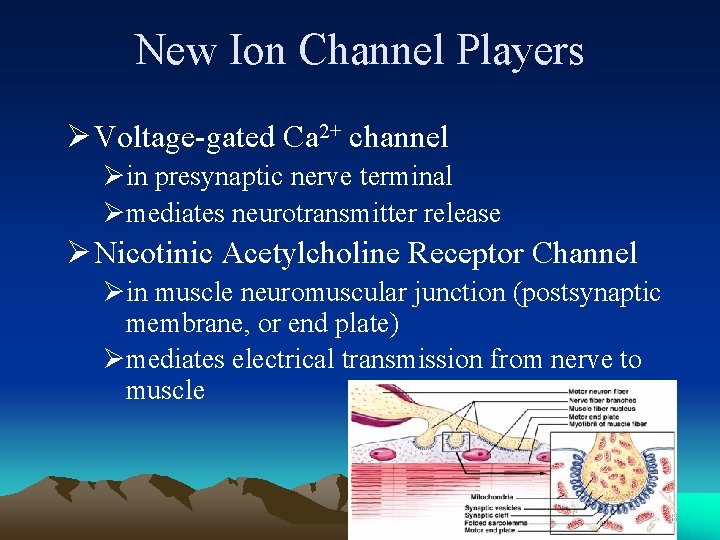
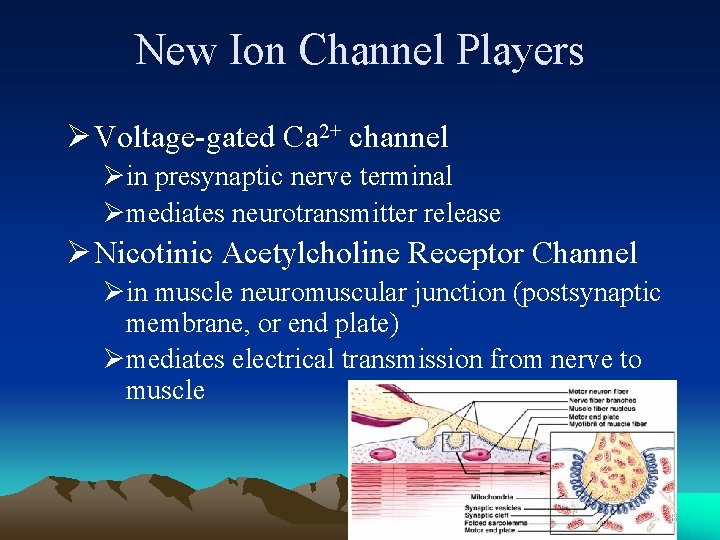
New Ion Channel Players Ø Voltage-gated Ca 2+ channel Øin presynaptic nerve terminal Ømediates neurotransmitter release Ø Nicotinic Acetylcholine Receptor Channel Øin muscle neuromuscular junction (postsynaptic membrane, or end plate) Ømediates electrical transmission from nerve to muscle 8
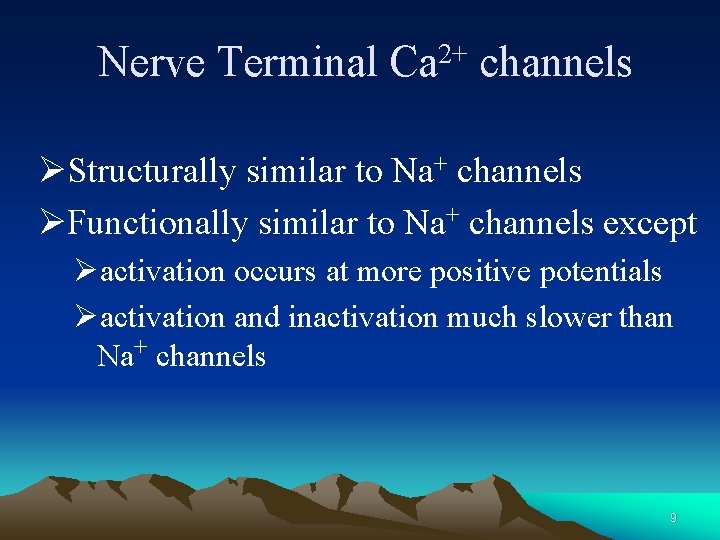
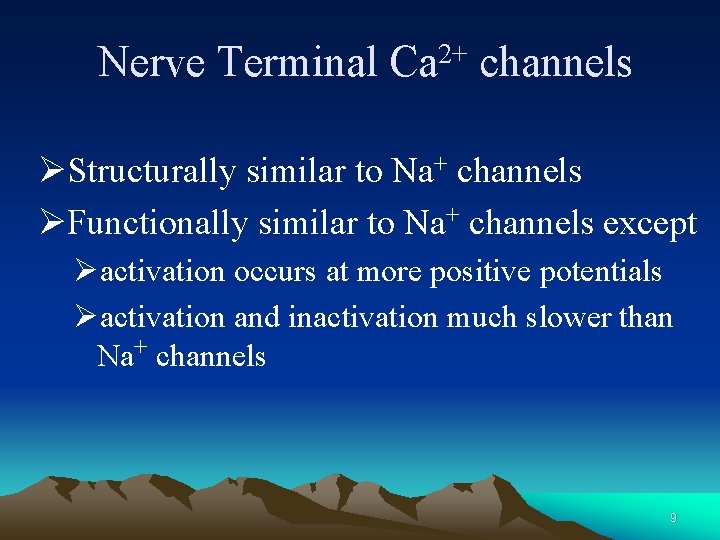
Nerve Terminal 2+ Ca channels ØStructurally similar to Na+ channels ØFunctionally similar to Na+ channels except Øactivation occurs at more positive potentials Øactivation and inactivation much slower than Na+ channels 9
Neuromuscular Transmission M ye lin Axon Terminal Skeletal Muscle 10
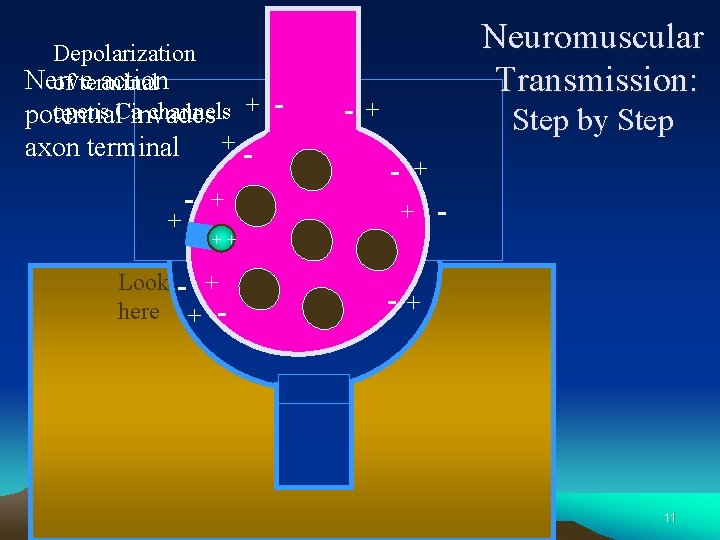
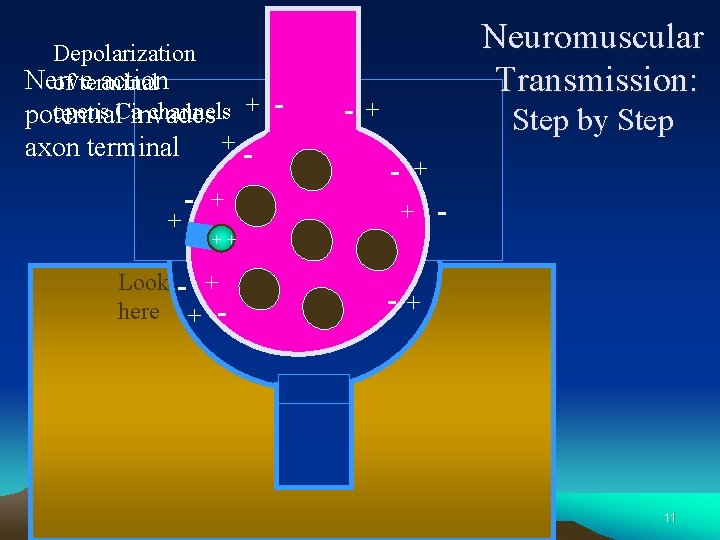
Depolarization Nerve action of terminal opens Cainvades channels + potential axon terminal + - + -++ Look - + here + - - - Neuromuscular Transmission: + Step by Step - + + - -+ 11
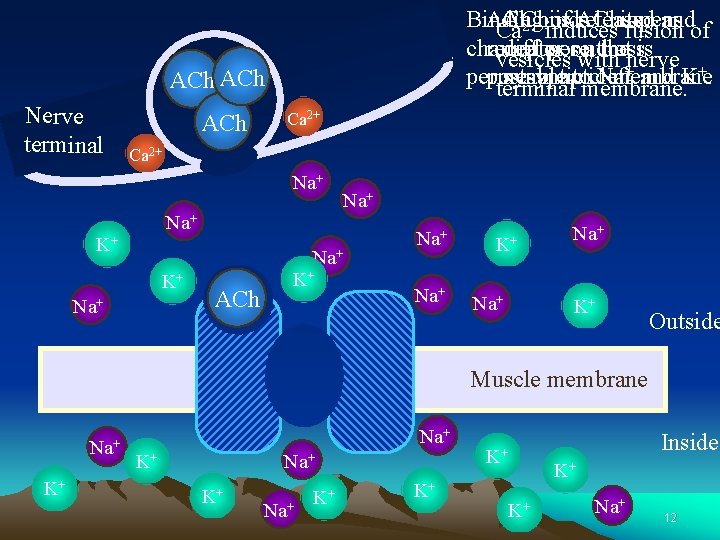
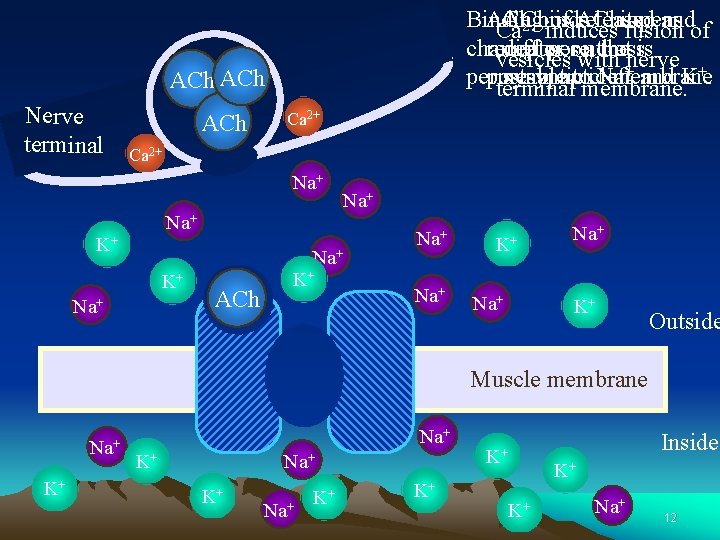
Binding ACh of is ACh released to its opens andof 2+binds Ca induces fusion channel receptor diffuses pore on across that thenerve is vesicles with + and K+. permeable postsynaptic to cleft. Na membrane terminal membrane. ACh Nerve terminal ACh Ca 2+ Na+ Na+ K+ Na+ ACh K+ Na+ Na+ K+ Outside Muscle membrane Na+ K+ K+ Na+ K+ K+ Inside K+ K+ K+ Na+ 12
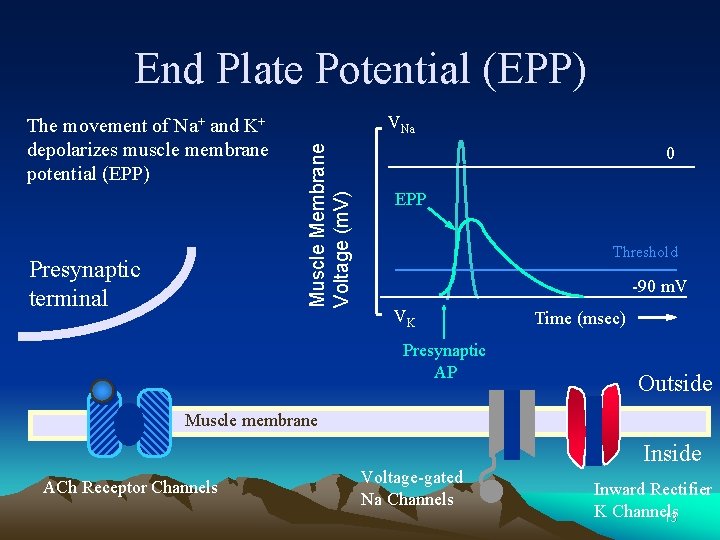
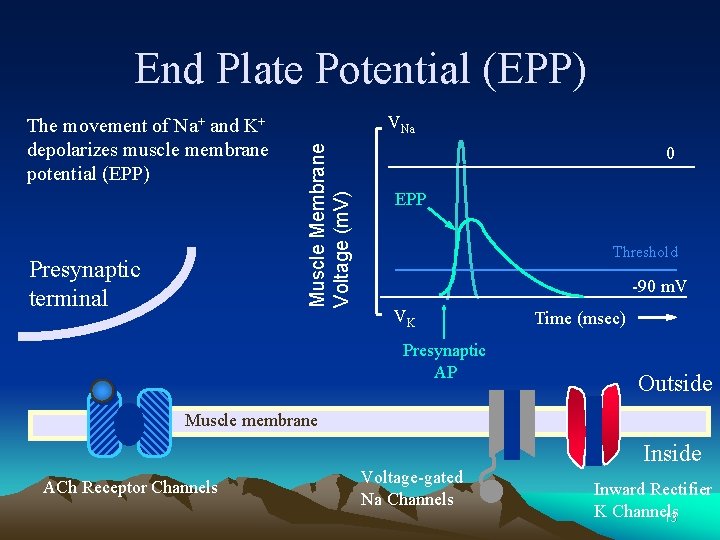
End Plate Potential (EPP) Presynaptic terminal VNa Muscle Membrane Voltage (m. V) The movement of Na+ and K+ depolarizes muscle membrane potential (EPP) 0 EPP Threshold -90 m. V VK Presynaptic AP Time (msec) Outside Muscle membrane Inside ACh Receptor Channels Voltage-gated Na Channels Inward Rectifier K Channels 13
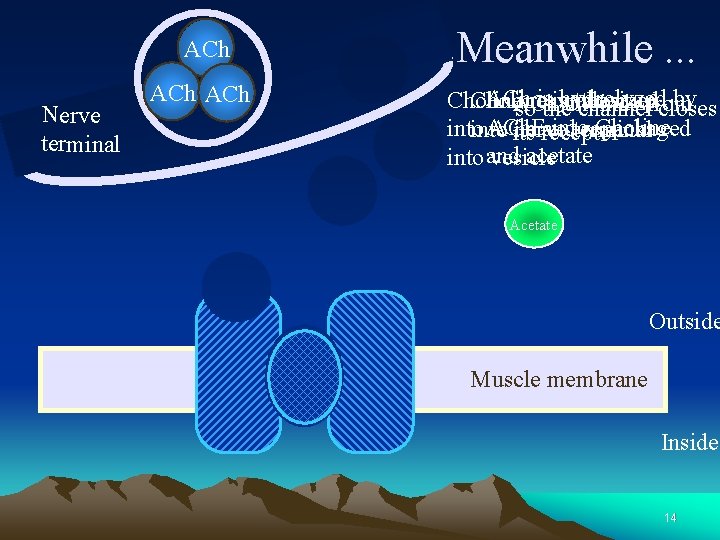
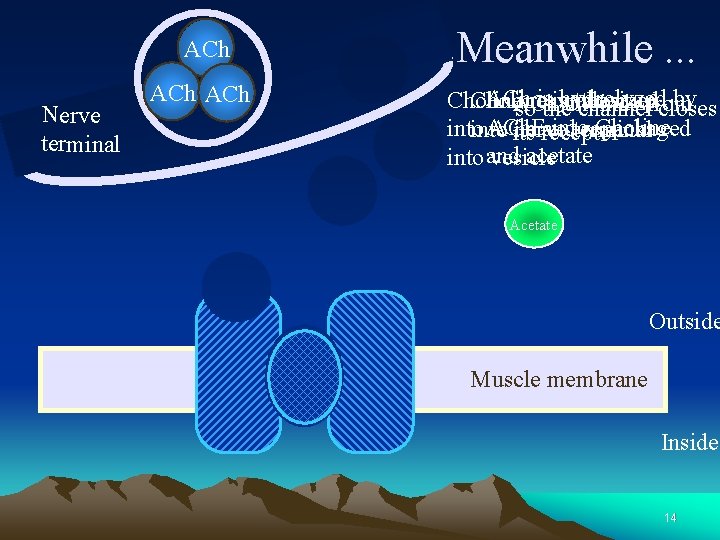
ACh Nerve terminal Choline ACh Choline Meanwhile. . . ACh isthe by Choline ishydrolyzed taken upfrom ACh unbinds soresynthesized channel closes ACh. E into Choline into ACh and repackaged into nerve terminal its receptor acetate into and vesicle ACh Acetate ACh Outside Muscle membrane Inside 14
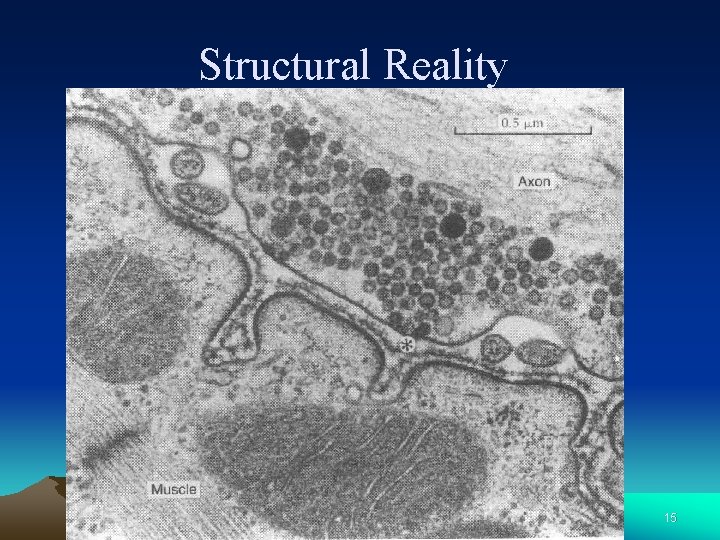
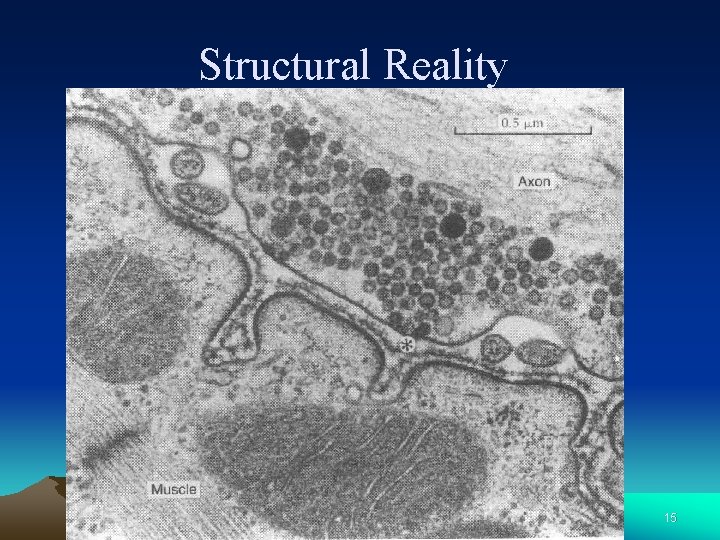
Structural Reality 15
Neuromuscular Transmission Ø Properties of neuromuscular junction Ø 1: 1 transmission Ø An unidirectional process Ø Time delay. 20 nm/0. 5 -1 ms Ø Easily affect by drugs and some factors Ø The NMJ is a site of considerable clinical importance 16
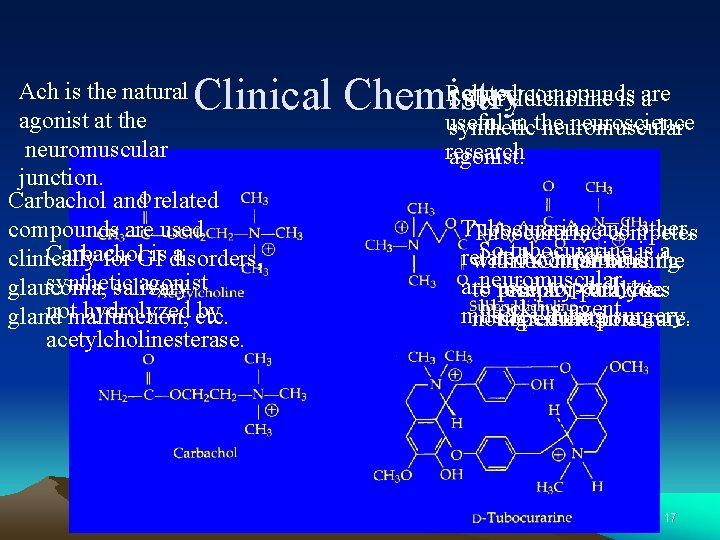
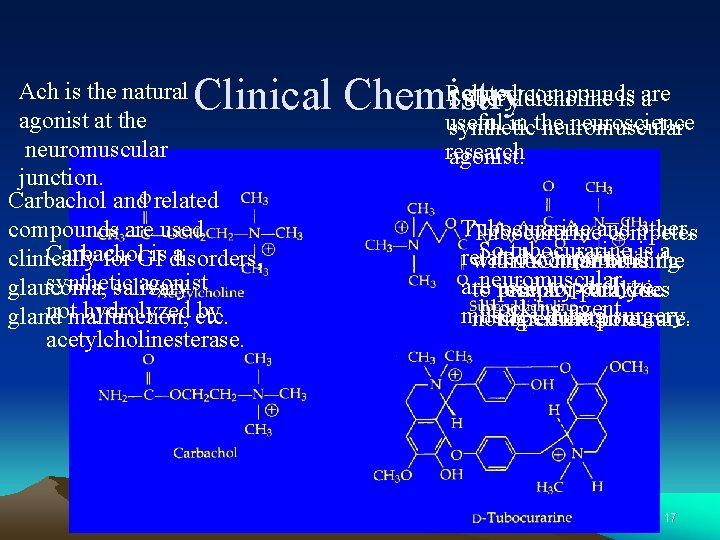
Related compounds Suberyldicholine is are a Clinical Chemistry useful in the neuroscience Ach is the natural agonist at the neuromuscular junction. Carbachol and related compounds are used Carbachol a clinically for GIis disorders, synthetic agonist glaucoma, salivary notmalfunction, hydrolyzed etc. by gland acetylcholinesterase. synthetic neuromuscular research agonist. Tubocurarine other, Tubocurarineand competes So. Tubocurarine tubocurarine a related compounds isis the with ACh for binding are used to paralyze primary paralytic toneuromuscular receptorbut does blocking agent. muscles ingredient insurgery. curare. not openduring the pore. 17
Anticholinesterase Agents Ø Anticholinesterase (anti-Ch. E) agents inhibit acetylcholinesterase (乙酰胆碱酯 酶) Øprolong excitation at the NMJ 18
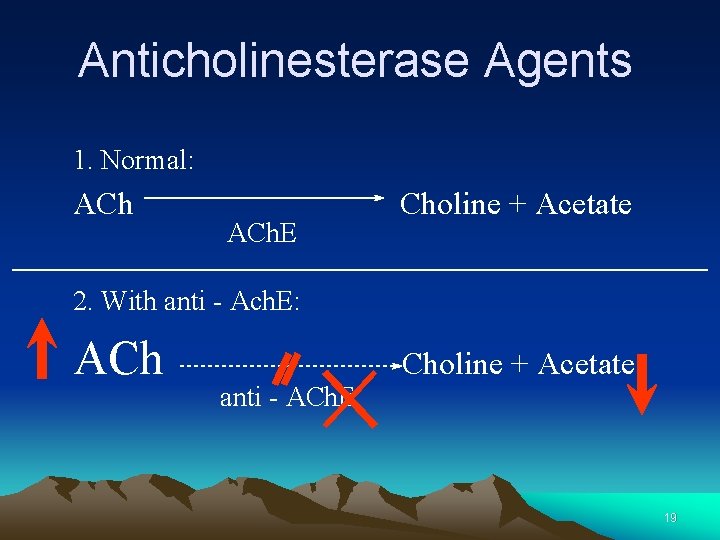
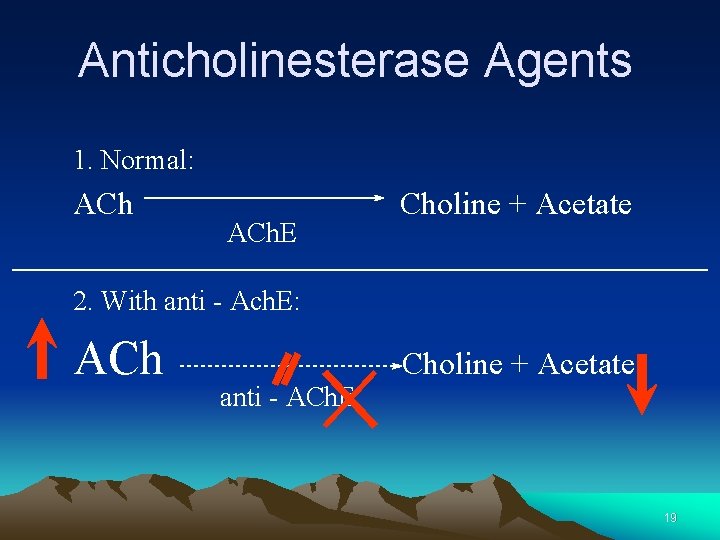
Anticholinesterase Agents 1. Normal: ACh. E Choline + Acetate 2. With anti - Ach. E: ACh anti - ACh. E Choline + Acetate 19
Uses of anti-Ch. E agents ØClinical applications (Neostigmine, 新斯的明, Physostigmine毒扁豆碱) ØInsecticides (organophosphate 有机磷酸酯) ØNerve gas (e. g. Sarin 沙林,甲氟膦酸异丙酯。 一种用作神经性毒气的化学剂)) 20
Sarin Ø comes in both liquid and gas forms, Ø a highly toxic and volatile nerve agent developed by Nazi scientists in Germany in the 1930 s. Ø 500 times more toxic than cyanide (氢 化物) gas. 21
NMJ Diseases ØMyasthenia Gravis (重症肌无力) Autoimmunity to ACh receptor Ø Fewer functional ACh receptors Ø Low “safety factor” for NM transmission ØLambert-Eaton syndrome(兰伯特-伊 顿综合征 ,癌性肌无力综合征 ) 2+ Ø Autoimmunity directed against Ca channels Ø Reduced ACh release Ø Low “safety factor” for NM transmission Ø 22

II Microstructure of Skeletal Muscle
Skeletal Muscle ØHuman body contains over 400 skeletal muscles Ø 40 -50% of total body weight ØFunctions of skeletal muscle ØForce production for locomotion and breathing ØForce production for postural support ØHeat production during cold stress 24
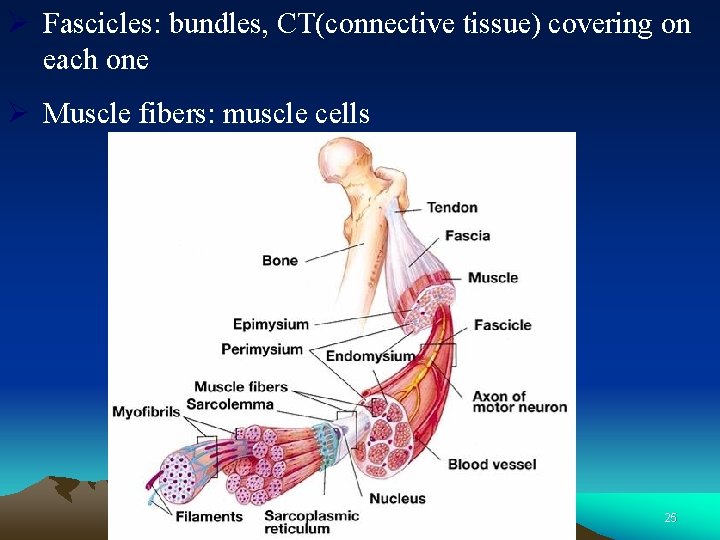
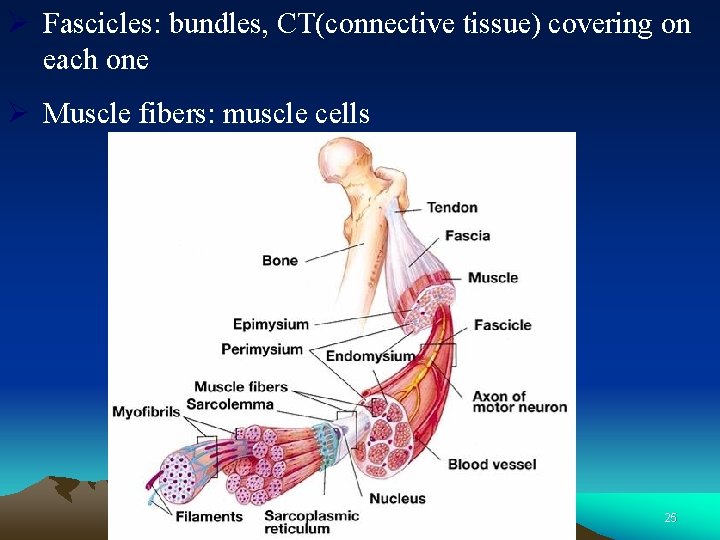
Ø Fascicles: bundles, CT(connective tissue) covering on each one Ø Muscle fibers: muscle cells 25
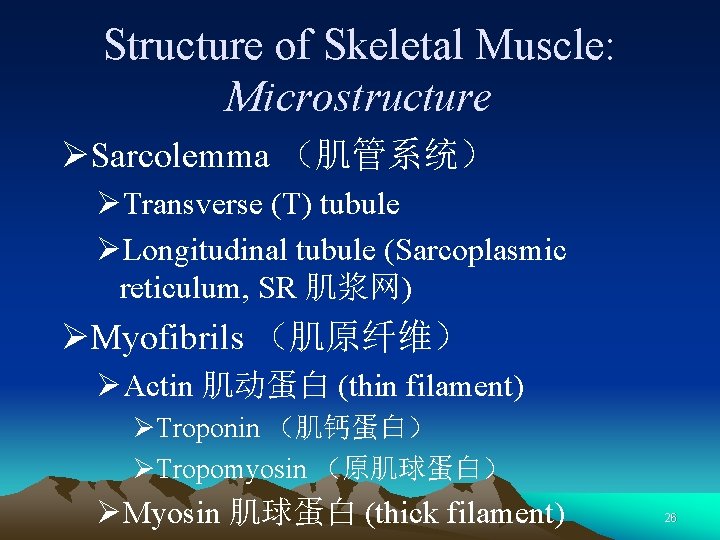
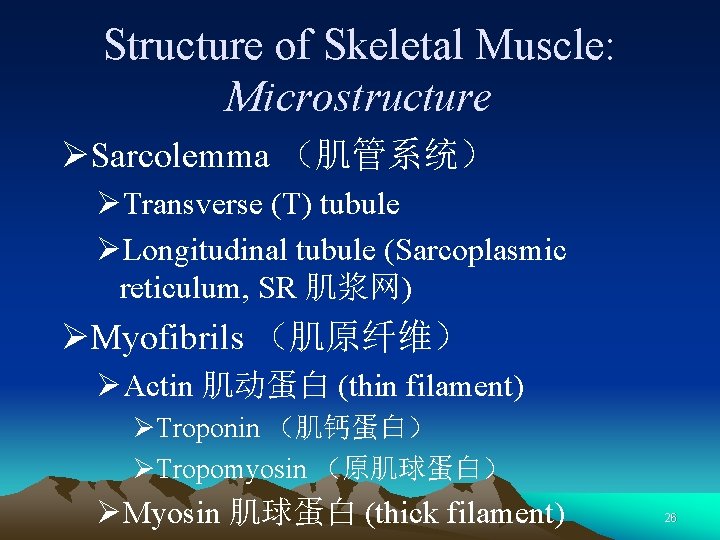
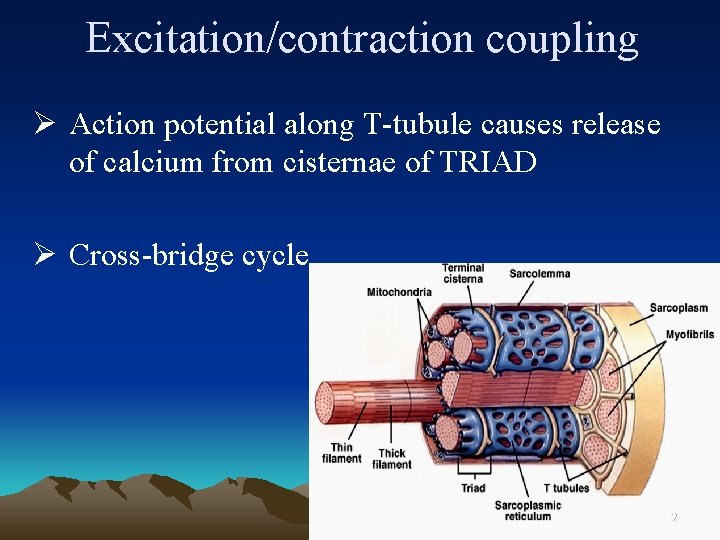
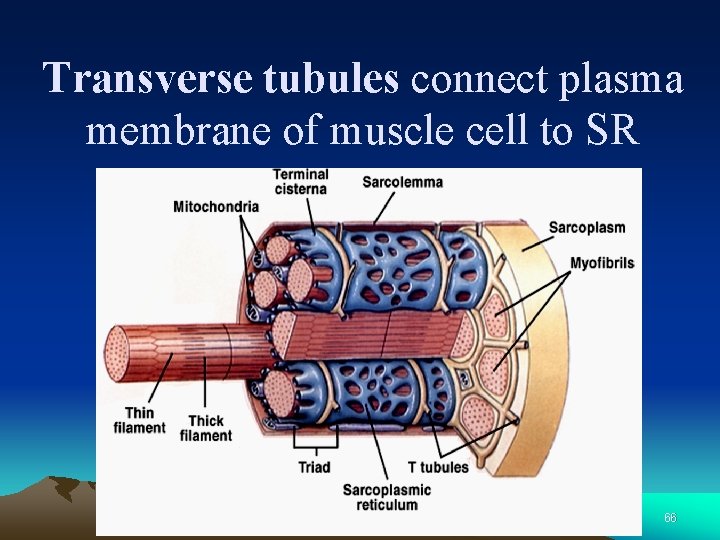
Structure of Skeletal Muscle: Microstructure ØSarcolemma (肌管系统) ØTransverse (T) tubule ØLongitudinal tubule (Sarcoplasmic reticulum, SR 肌浆网) ØMyofibrils (肌原纤维) ØActin 肌动蛋白 (thin filament) ØTroponin (肌钙蛋白) ØTropomyosin (原肌球蛋白) ØMyosin 肌球蛋白 (thick filament) 26
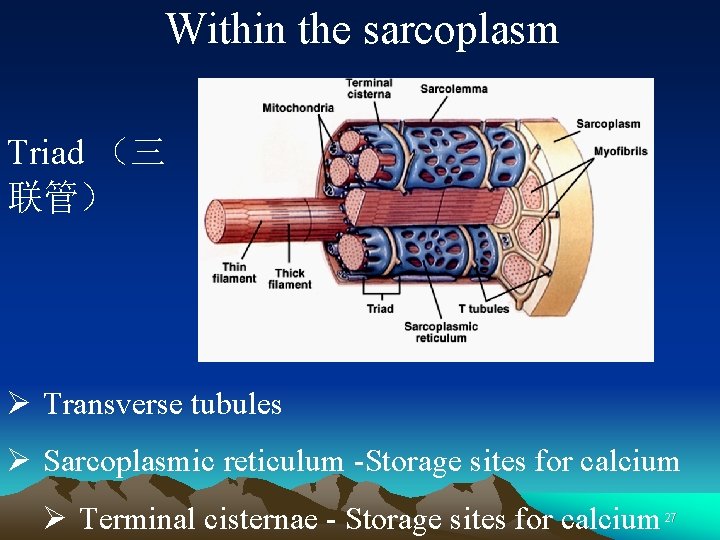
Within the sarcoplasm Triad (三 联管) Ø Transverse tubules Ø Sarcoplasmic reticulum -Storage sites for calcium Ø Terminal cisternae - Storage sites for calcium 27
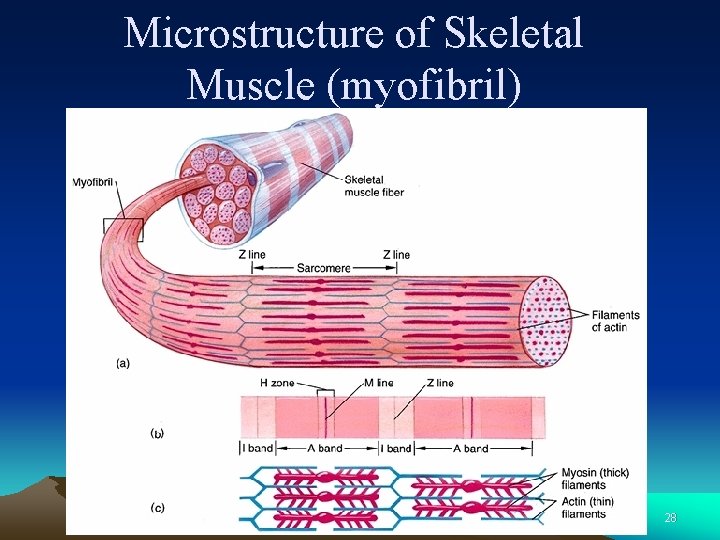
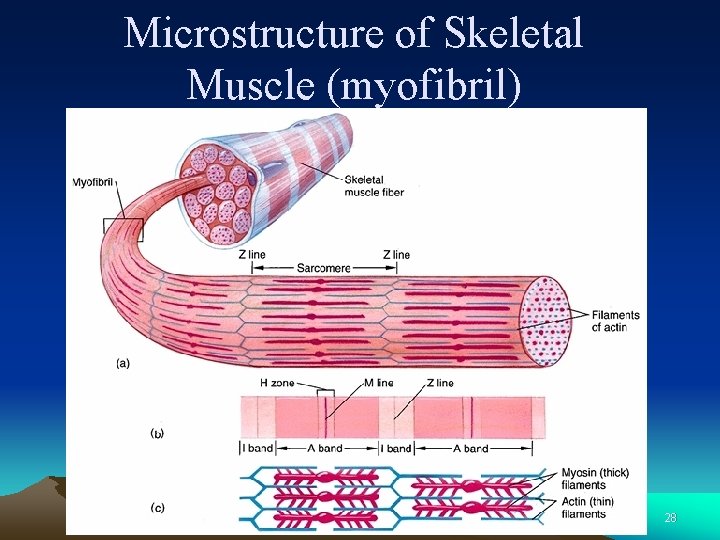
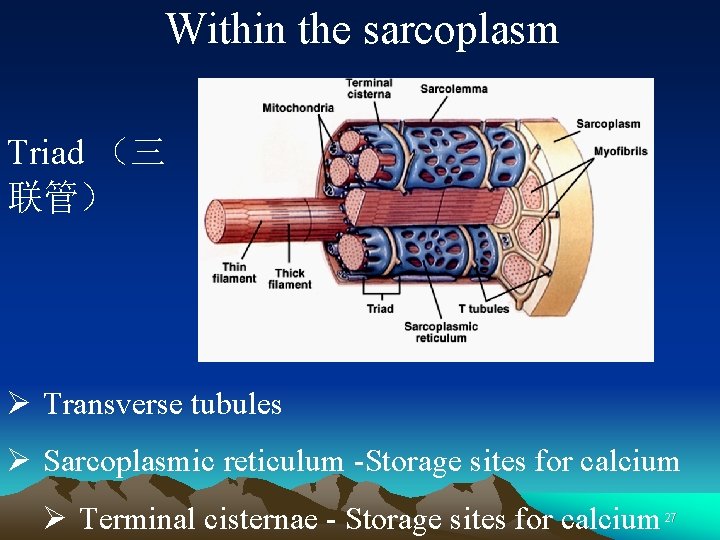
Microstructure of Skeletal Muscle (myofibril) 28
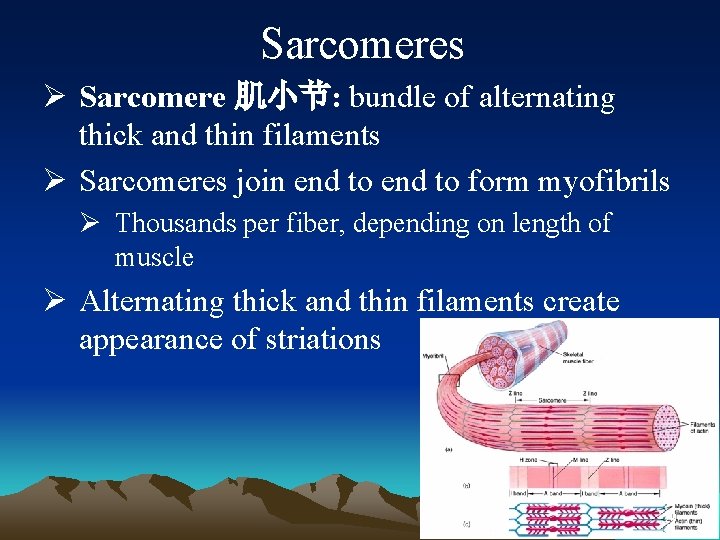
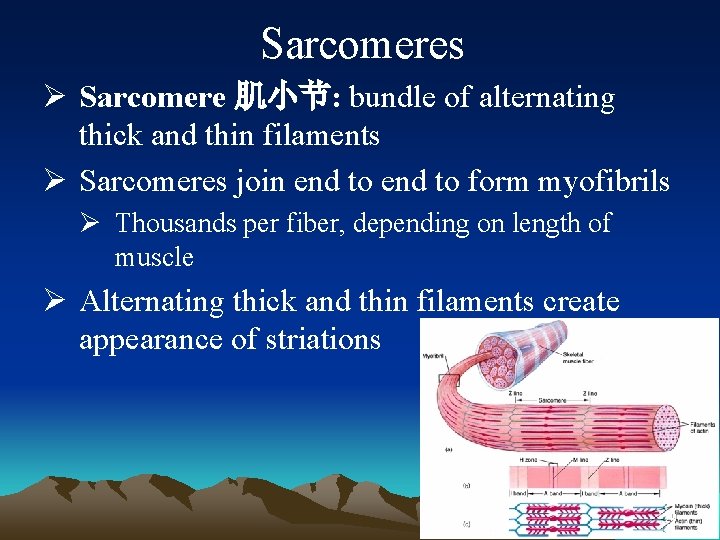
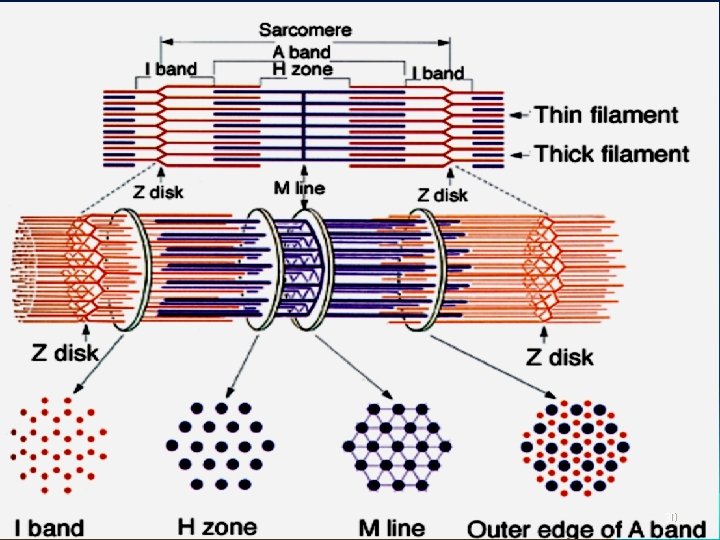
Sarcomeres Ø Sarcomere 肌小节: bundle of alternating thick and thin filaments Ø Sarcomeres join end to form myofibrils Ø Thousands per fiber, depending on length of muscle Ø Alternating thick and thin filaments create appearance of striations 29
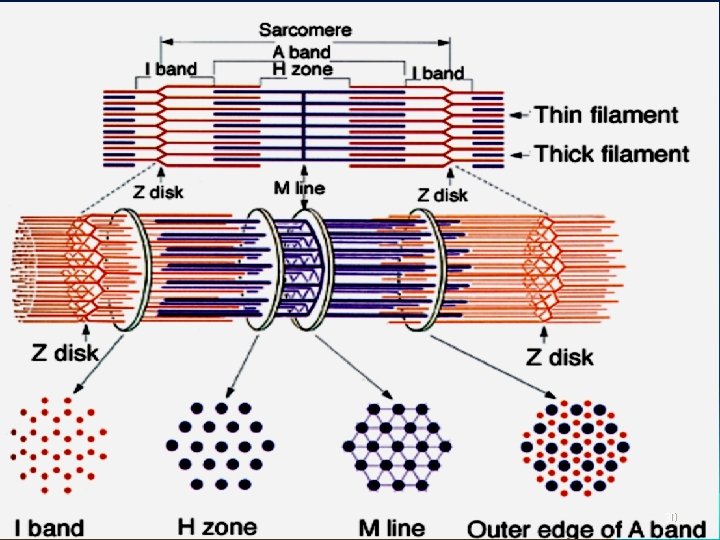
30
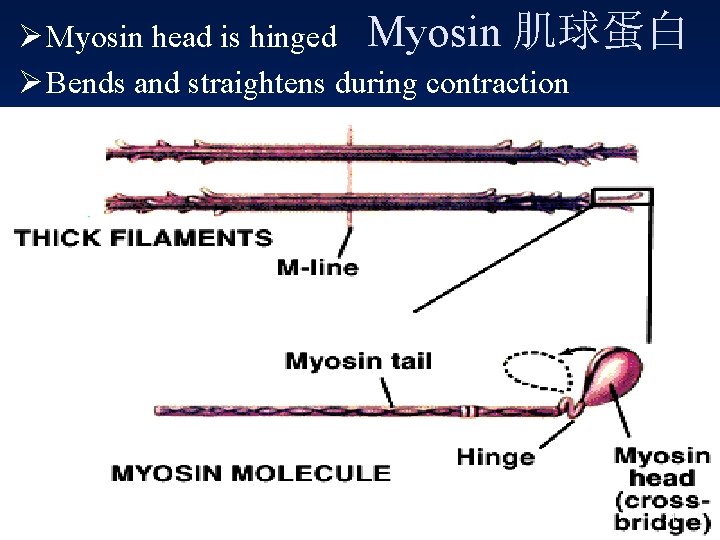
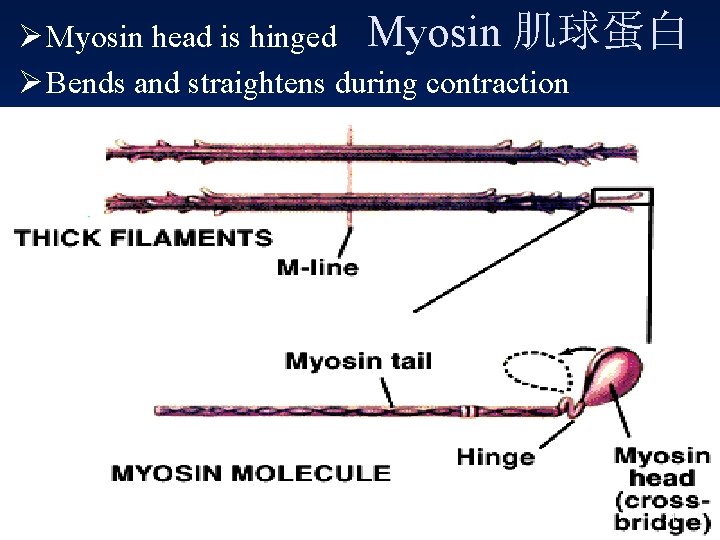
Ø Myosin head is hinged Myosin 肌球蛋白 Ø Bends and straightens during contraction 31
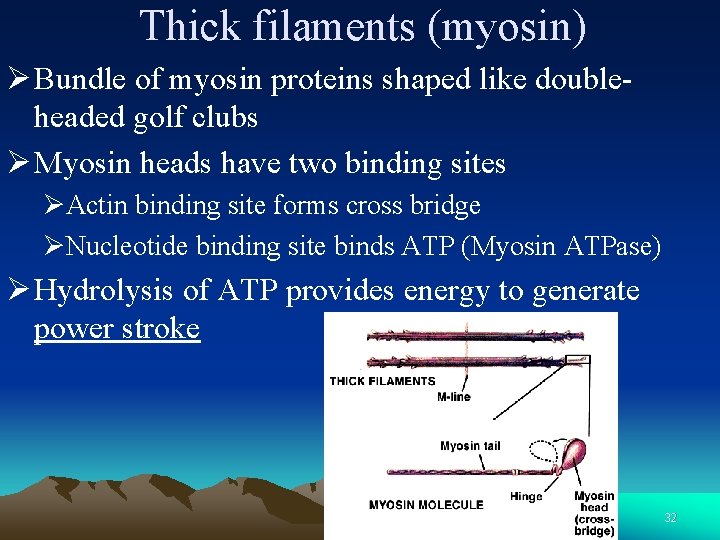
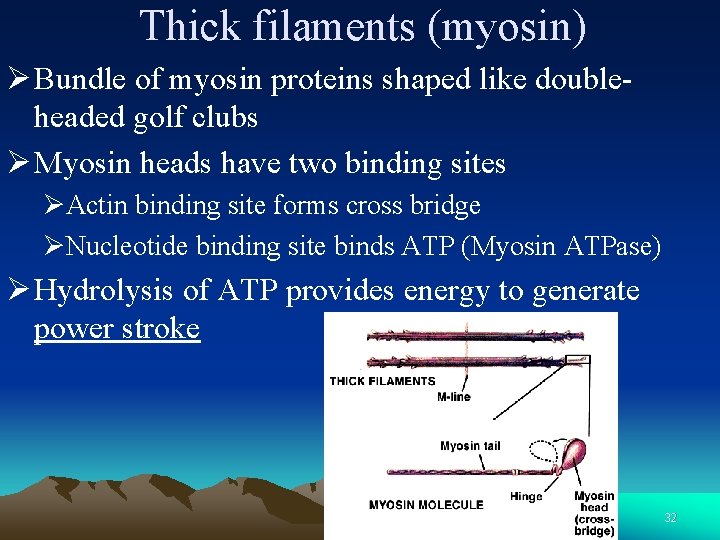
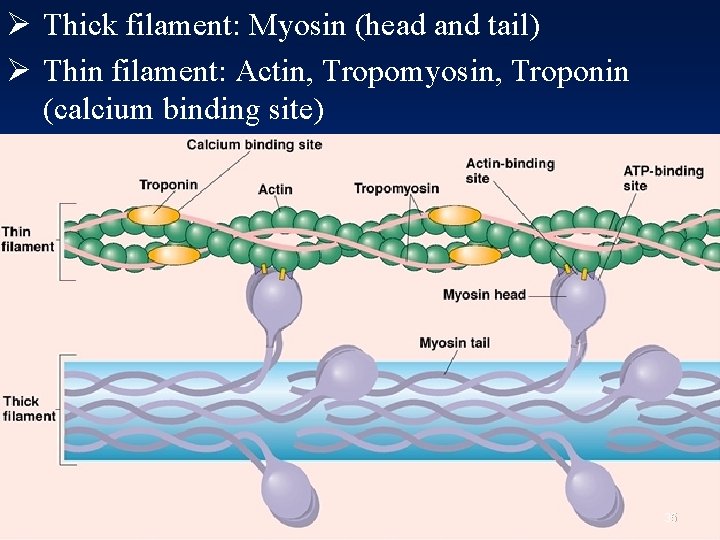
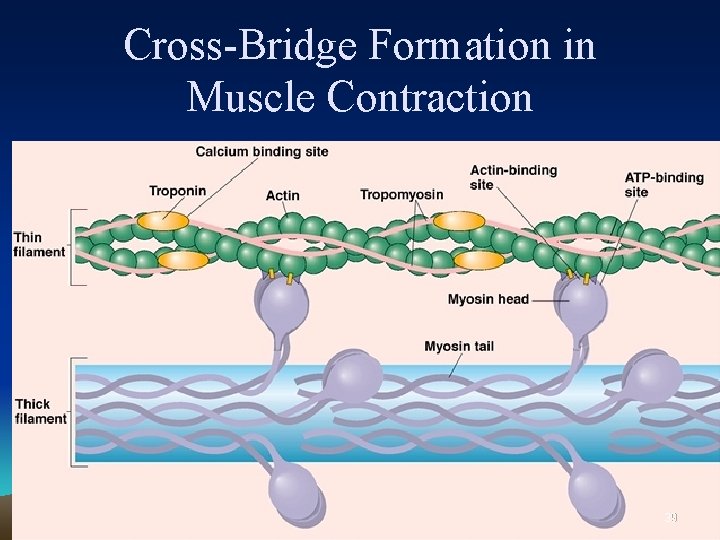
Thick filaments (myosin) Ø Bundle of myosin proteins shaped like doubleheaded golf clubs Ø Myosin heads have two binding sites ØActin binding site forms cross bridge ØNucleotide binding site binds ATP (Myosin ATPase) Ø Hydrolysis of ATP provides energy to generate power stroke 32

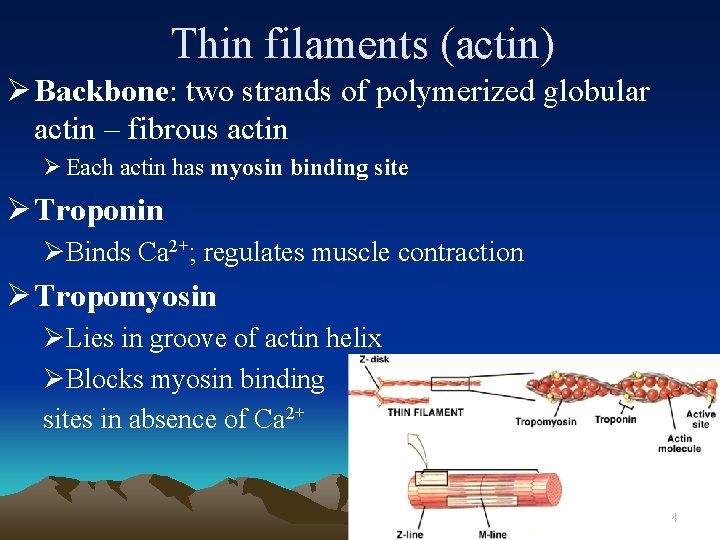
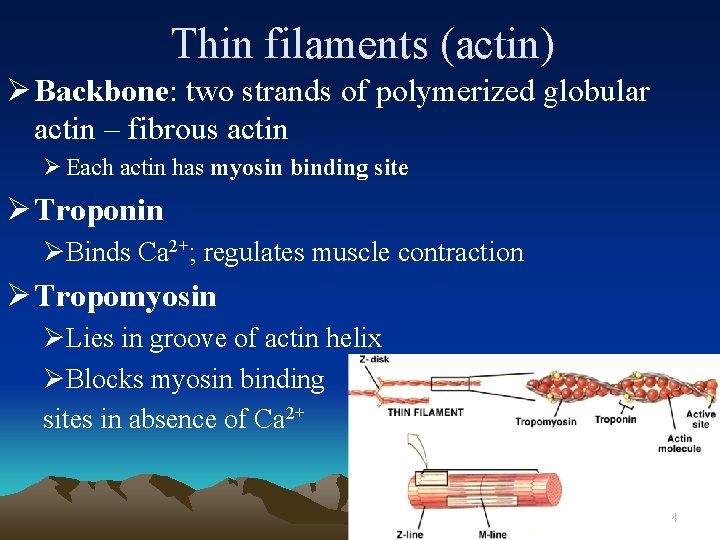
Thin filaments (actin) Ø Backbone: two strands of polymerized globular actin – fibrous actin Ø Each actin has myosin binding site Ø Troponin ØBinds Ca 2+; regulates muscle contraction Ø Tropomyosin ØLies in groove of actin helix ØBlocks myosin binding sites in absence of Ca 2+ 34
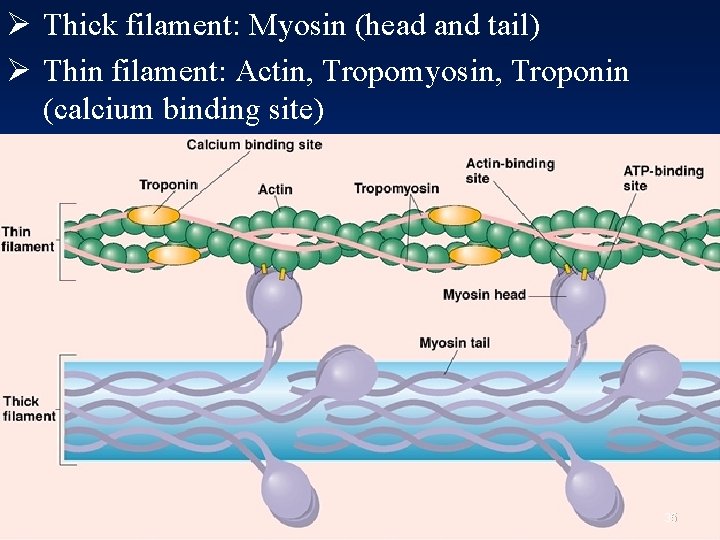
Ø Thick filament: Myosin (head and tail) Ø Thin filament: Actin, Tropomyosin, Troponin (calcium binding site) 35
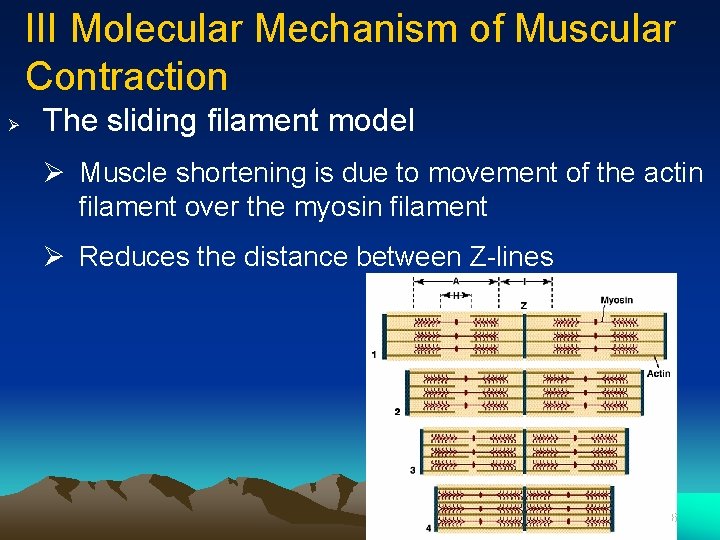
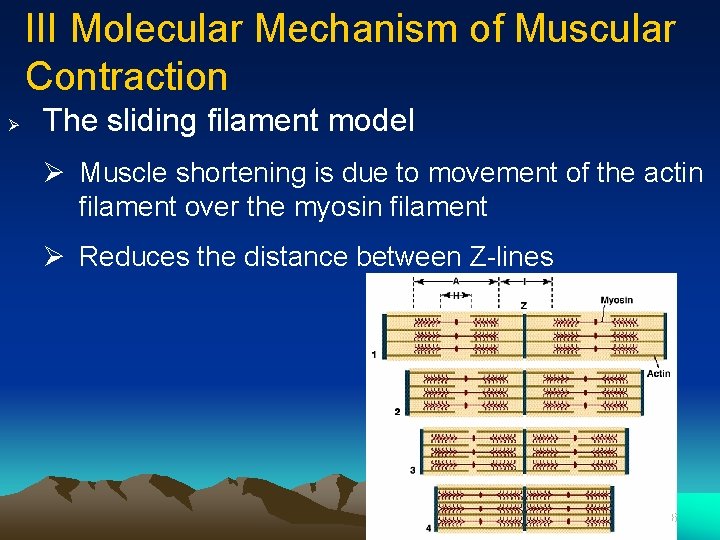
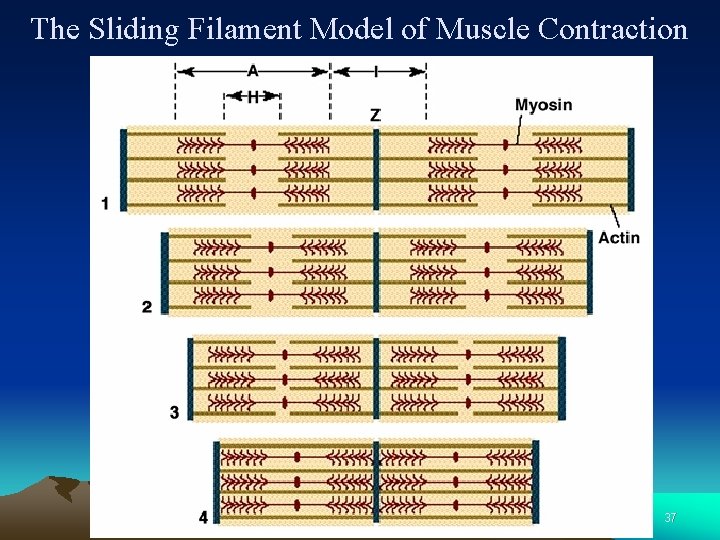
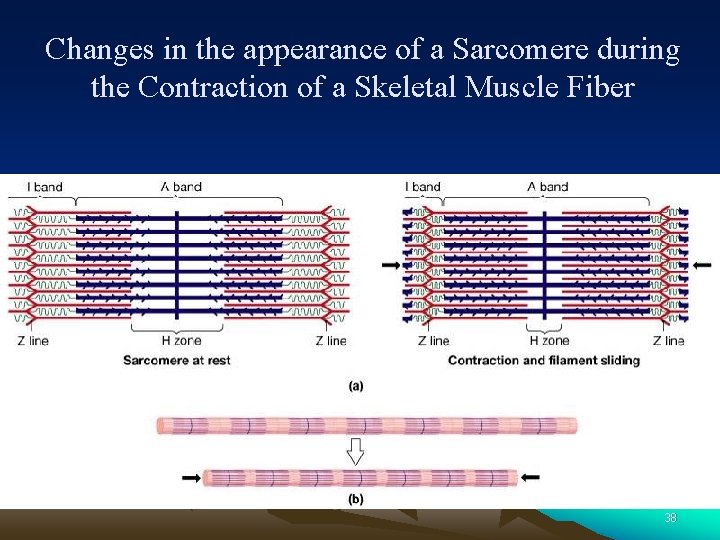
III Molecular Mechanism of Muscular Contraction Ø The sliding filament model Ø Muscle shortening is due to movement of the actin filament over the myosin filament Ø Reduces the distance between Z-lines 36
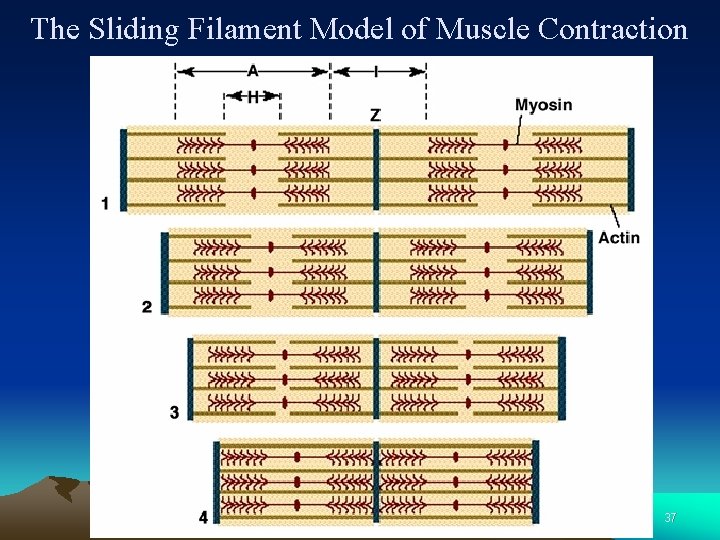
The Sliding Filament Model of Muscle Contraction 37
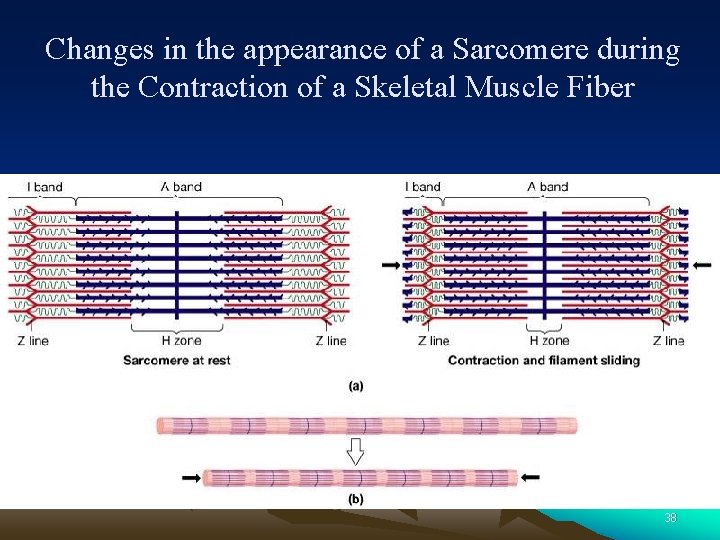
Changes in the appearance of a Sarcomere during the Contraction of a Skeletal Muscle Fiber 38
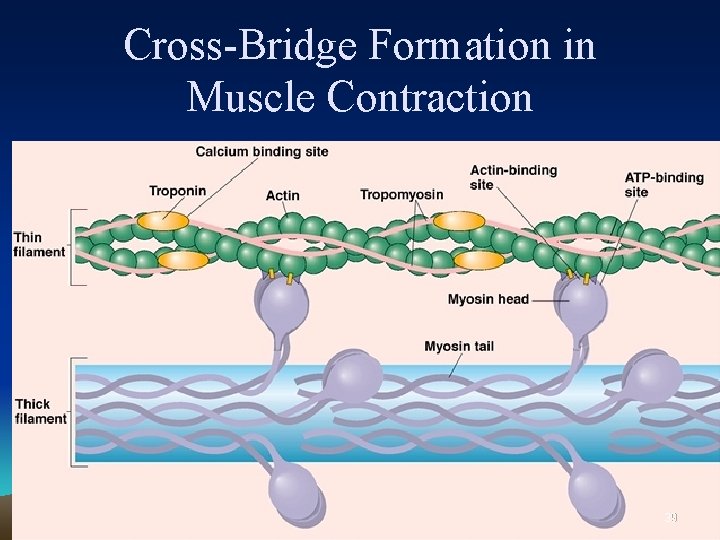
Cross-Bridge Formation in Muscle Contraction 39
Energy for Muscle Contraction Ø ATP is required for muscle contraction ØMyosin ATPase breaks down ATP as fiber contracts 40
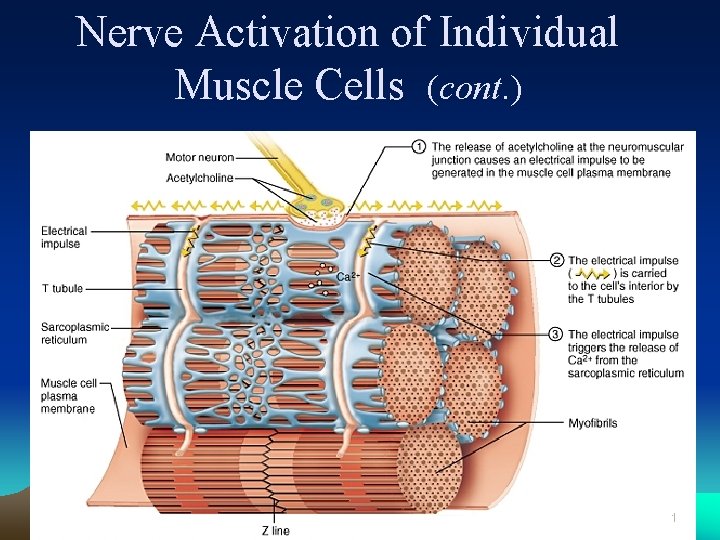
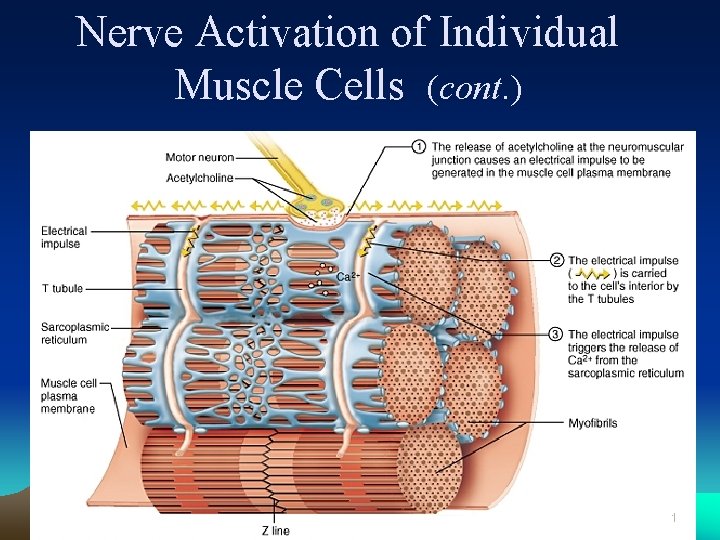
Nerve Activation of Individual Muscle Cells (cont. ) 41
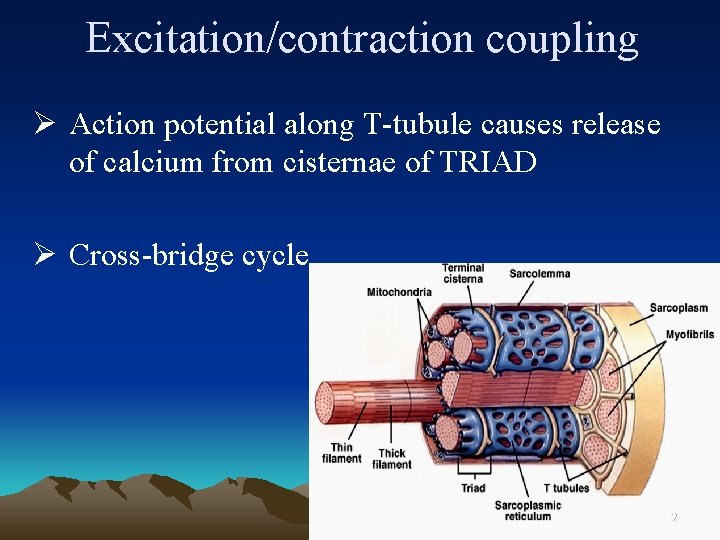
Excitation/contraction coupling Ø Action potential along T-tubule causes release of calcium from cisternae of TRIAD Ø Cross-bridge cycle 42
Begin cycle with myosin already bound to actin
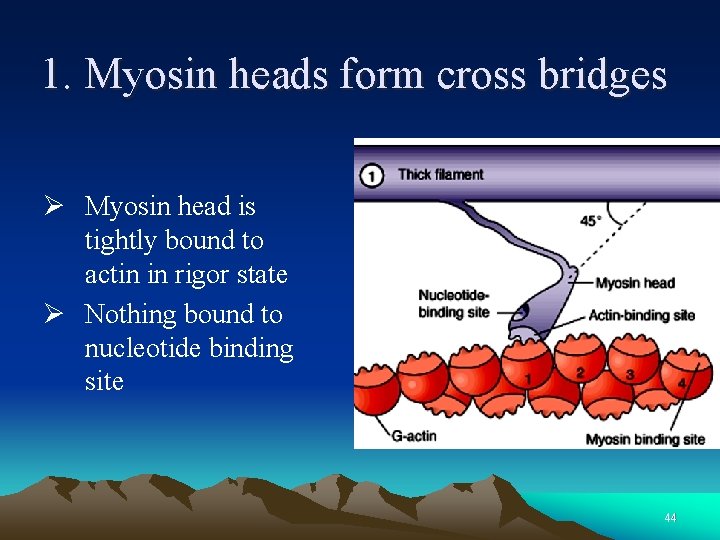
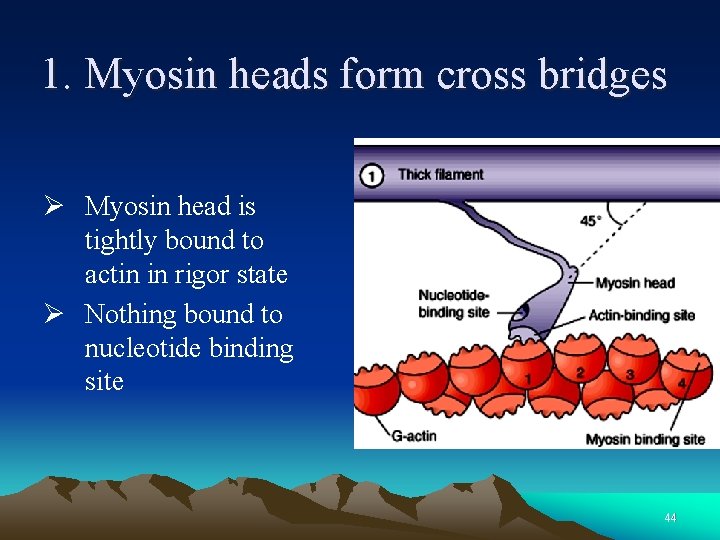
1. Myosin heads form cross bridges Ø Myosin head is tightly bound to actin in rigor state Ø Nothing bound to nucleotide binding site 44
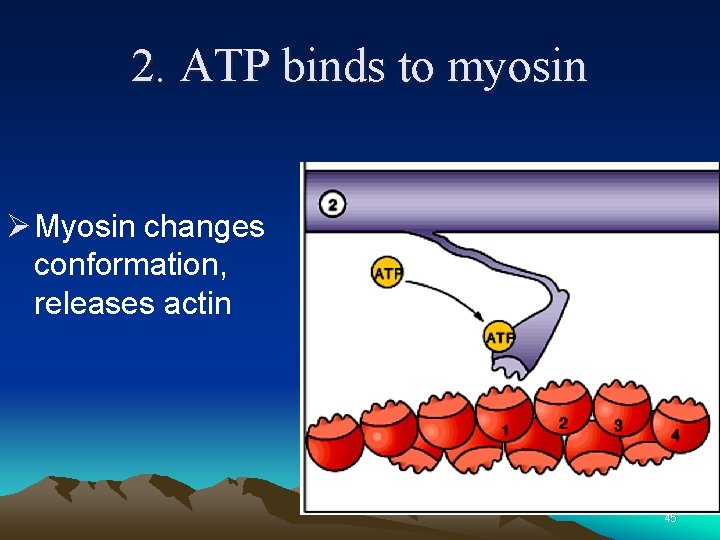
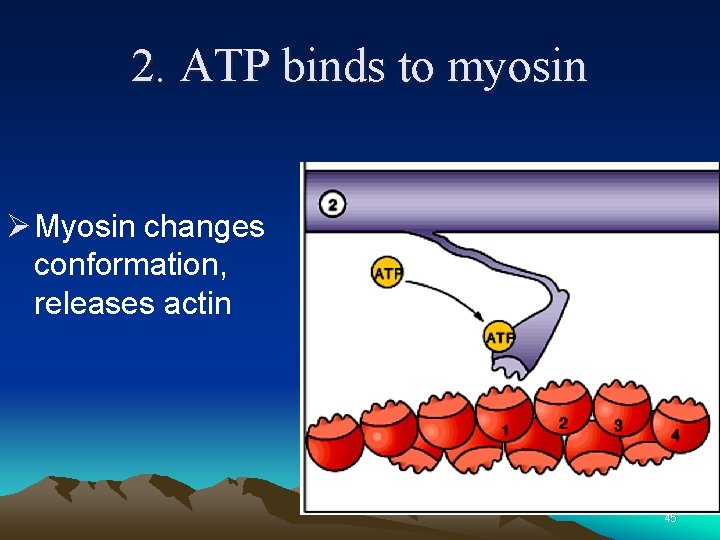
2. ATP binds to myosin Ø Myosin changes conformation, releases actin 45

3. ATP hydrolysis Ø ATP is broken down into: ØADP + Pi (inorganic phosphate) Ø Both ADP and Pi remain bound to myosin 46
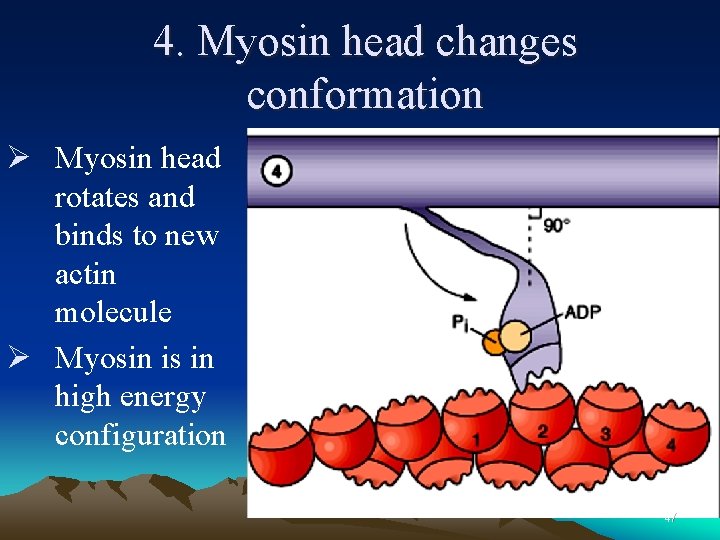
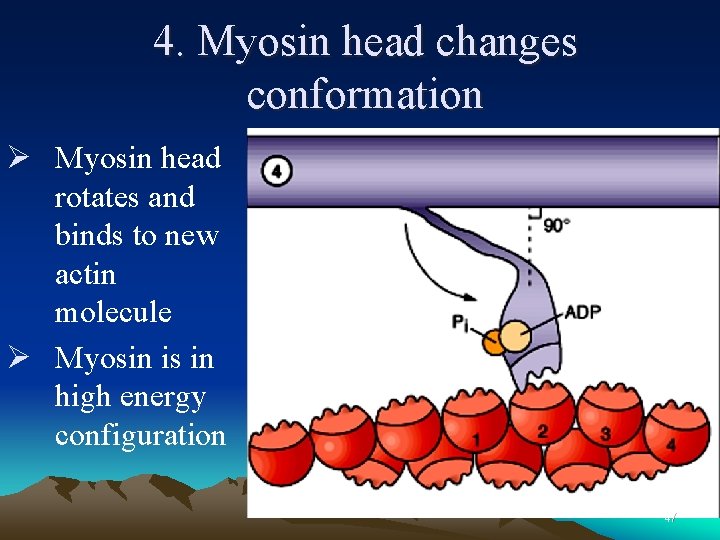
4. Myosin head changes conformation Ø Myosin head rotates and binds to new actin molecule Ø Myosin is in high energy configuration 47
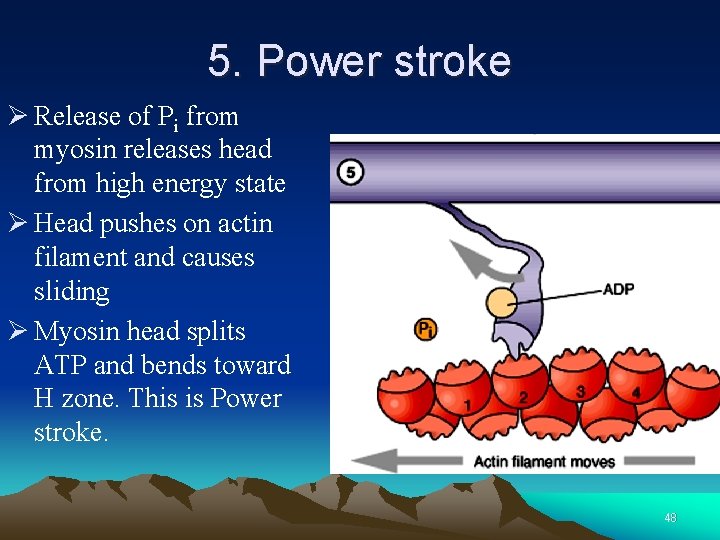
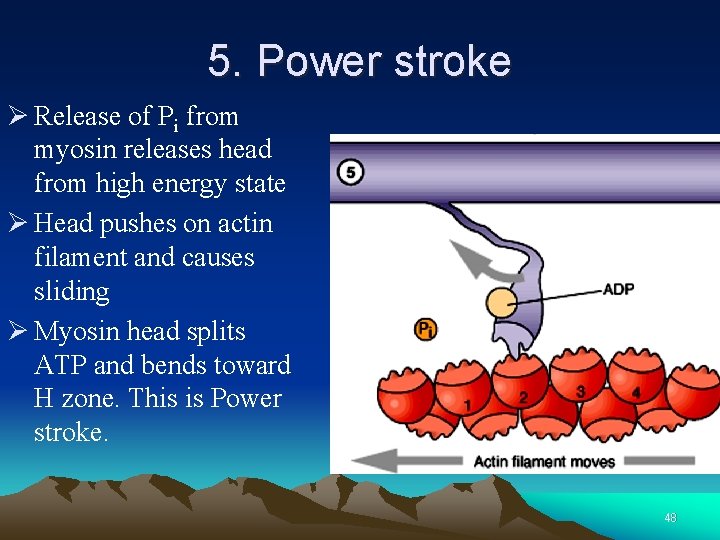
5. Power stroke Ø Release of Pi from myosin releases head from high energy state Ø Head pushes on actin filament and causes sliding Ø Myosin head splits ATP and bends toward H zone. This is Power stroke. 48
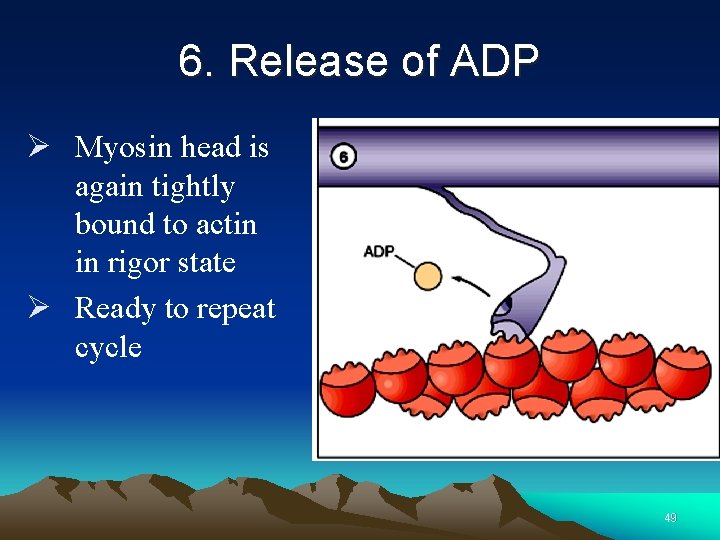
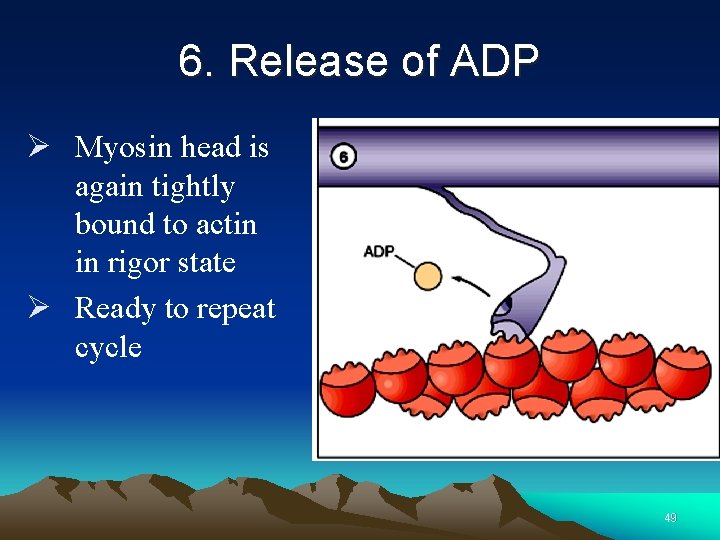
6. Release of ADP Ø Myosin head is again tightly bound to actin in rigor state Ø Ready to repeat cycle 49
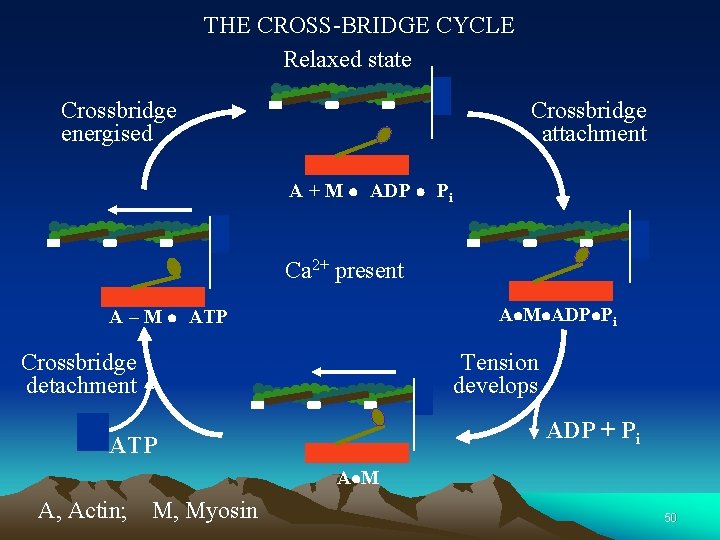
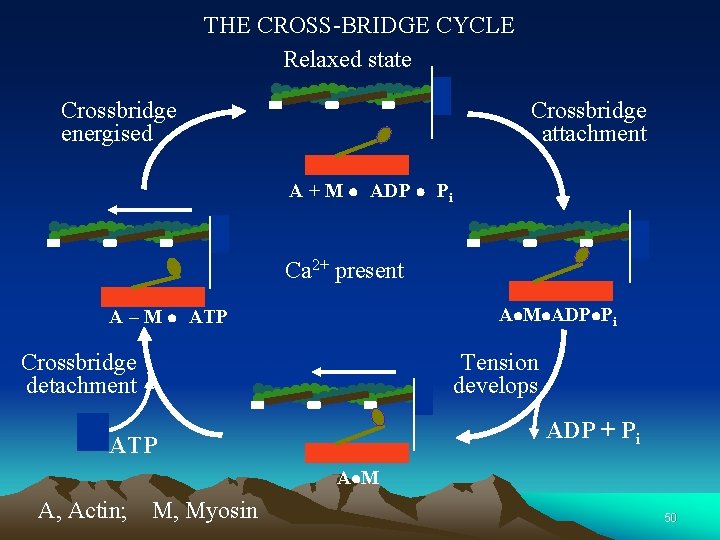
THE CROSS-BRIDGE CYCLE Relaxed state Crossbridge energised Crossbridge attachment A + M l ADP l Pi Ca 2+ present Al. Ml. ADPl. Pi A – M l ATP Crossbridge detachment Tension develops ADP + Pi ATP Al M A, Actin; M, Myosin 50
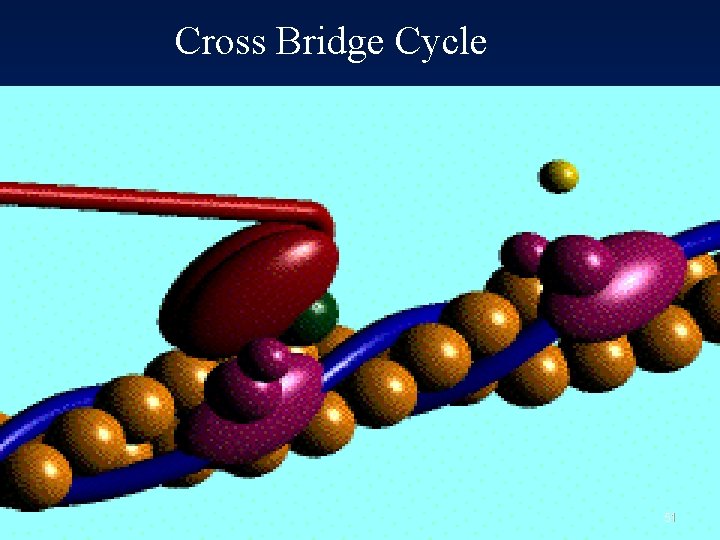
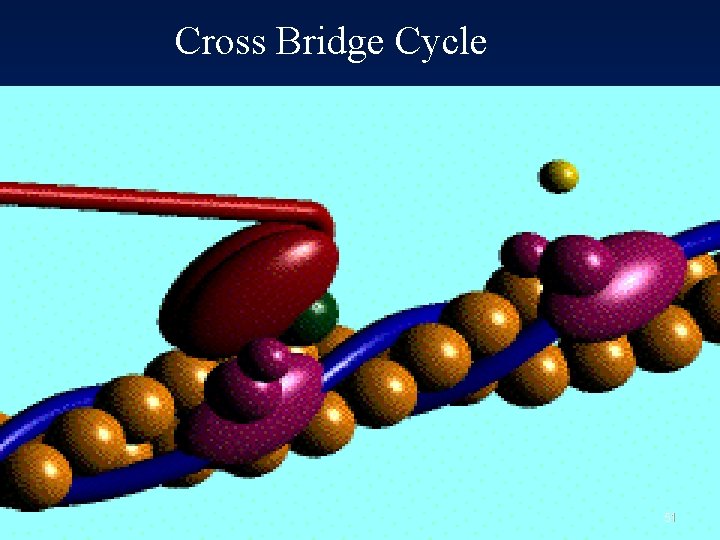
Cross Bridge Cycle 51
Rigor mortis Ø Myosin cannot release actin until a new ATP molecule binds Ø Run out of ATP at death, cross-bridges never release 52
Many contractile cycles occur asynchronously during a single muscle contraction • Need steady supply of ATP! 53
The action potential triggers contraction ØHow does the AP trigger contraction? Ø We should ask: Øhow does the AP cause release of Ca 2+ from the SR, so leading to an increase in [Ca 2+]i? Øhow does an increase in [Ca 2+]i cause contraction?
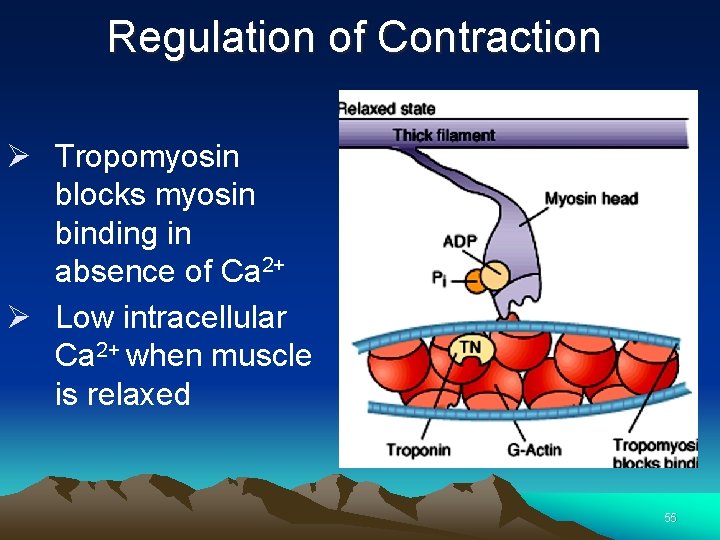
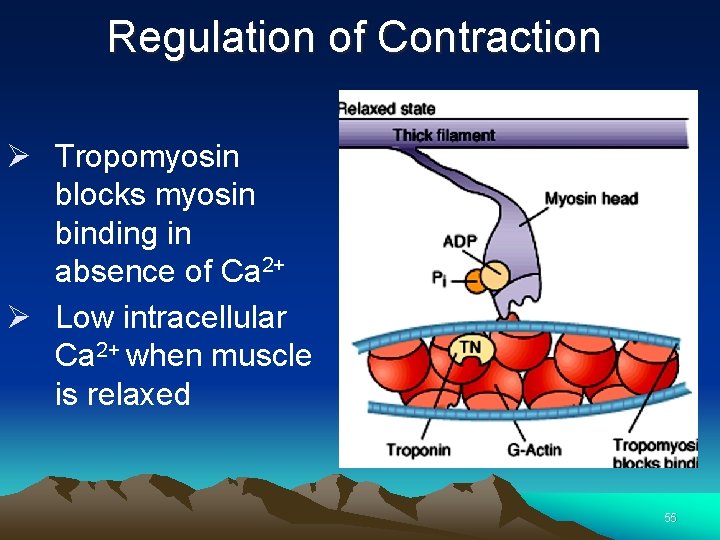
Regulation of Contraction Ø Tropomyosin blocks myosin binding in absence of Ca 2+ Ø Low intracellular Ca 2+ when muscle is relaxed 55
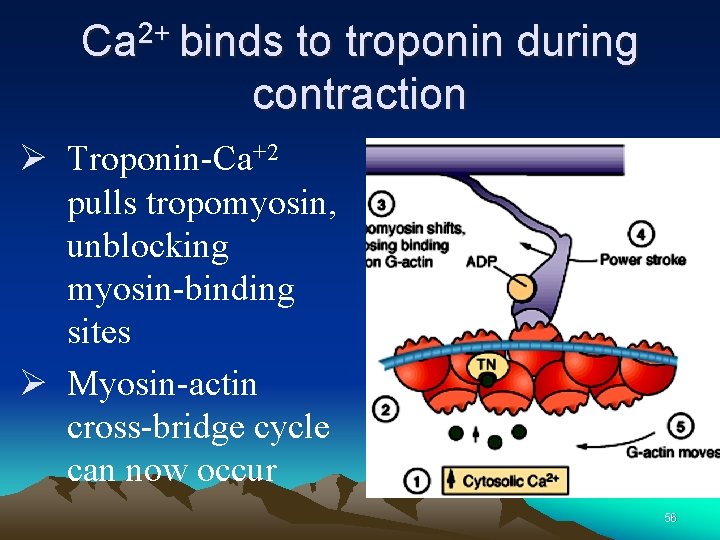
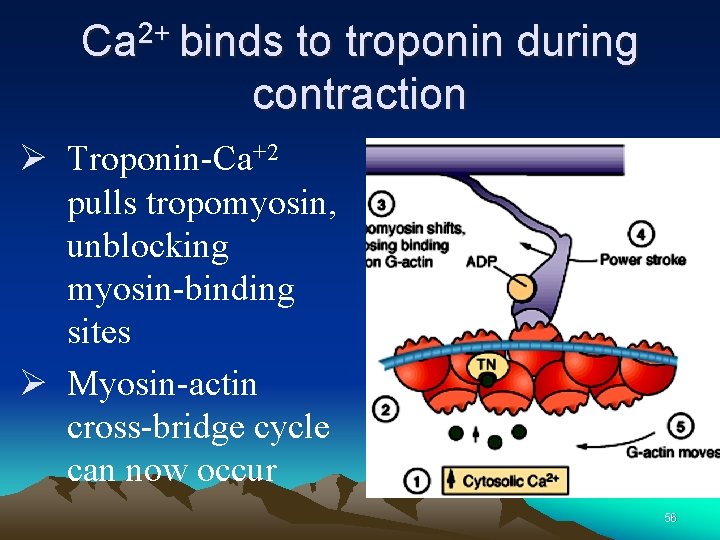
Ca 2+ binds to troponin during contraction Ø Troponin-Ca+2 pulls tropomyosin, unblocking myosin-binding sites Ø Myosin-actin cross-bridge cycle can now occur 56
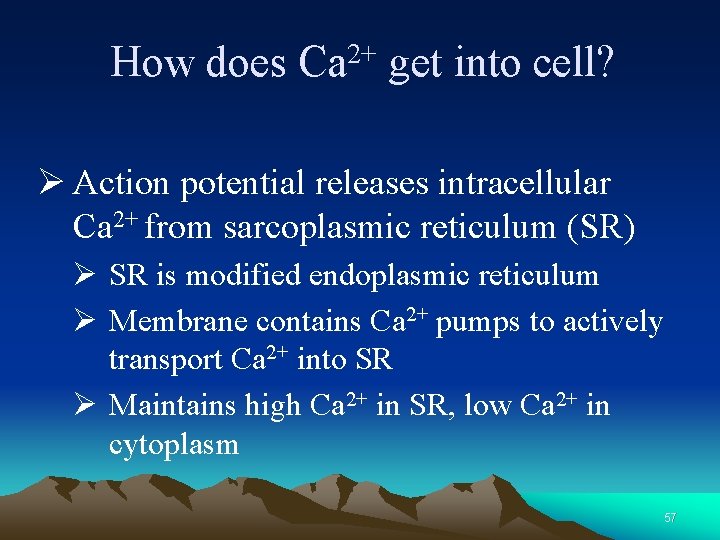
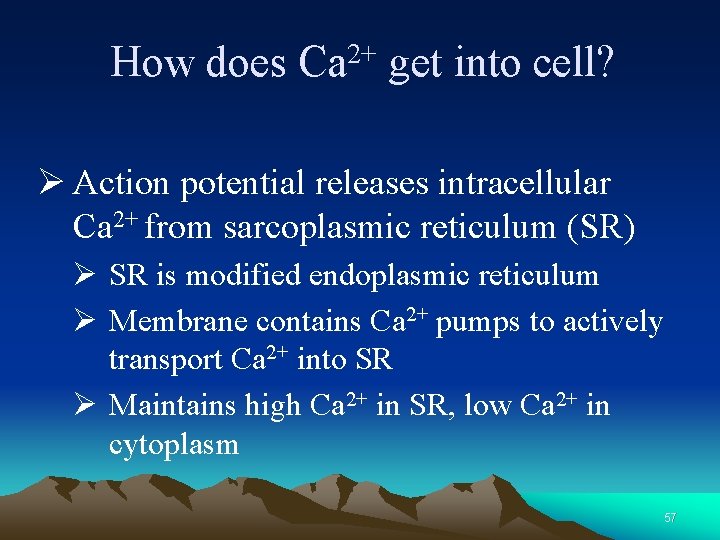
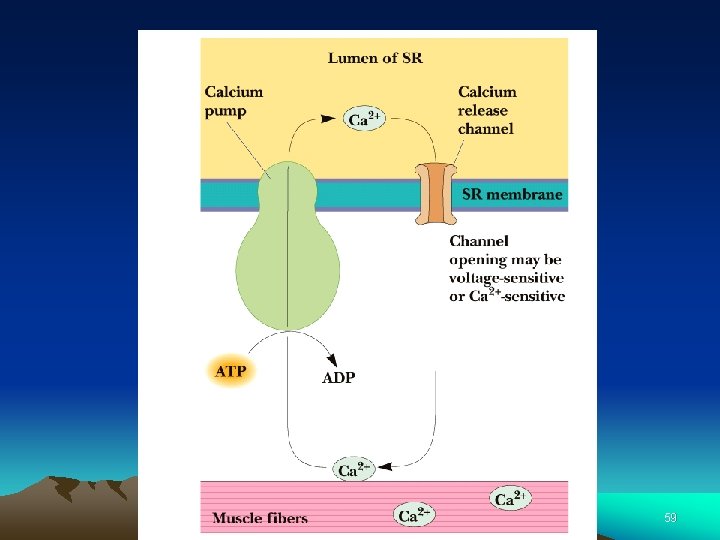
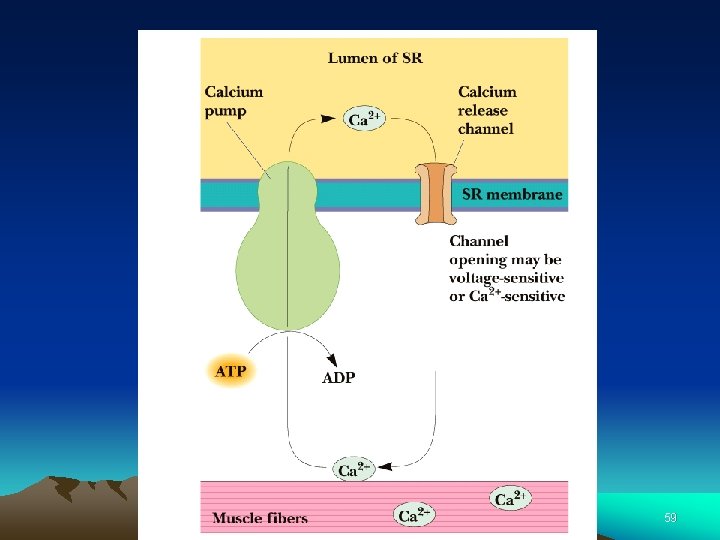
How does 2+ Ca get into cell? Ø Action potential releases intracellular Ca 2+ from sarcoplasmic reticulum (SR) Ø SR is modified endoplasmic reticulum Ø Membrane contains Ca 2+ pumps to actively transport Ca 2+ into SR Ø Maintains high Ca 2+ in SR, low Ca 2+ in cytoplasm 57
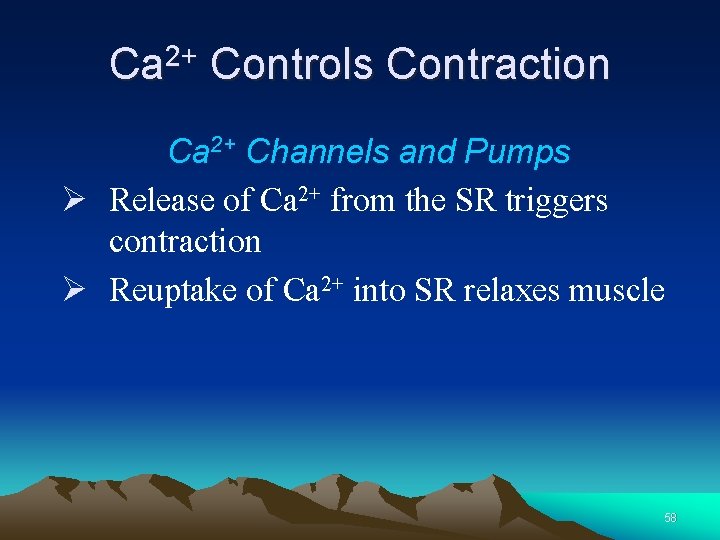
Ca 2+ Controls Contraction Ca 2+ Channels and Pumps Ø Release of Ca 2+ from the SR triggers contraction Ø Reuptake of Ca 2+ into SR relaxes muscle 58
59
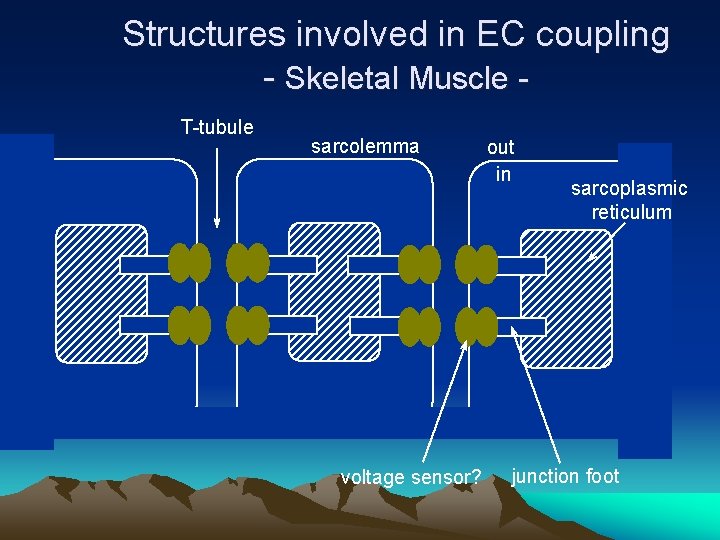
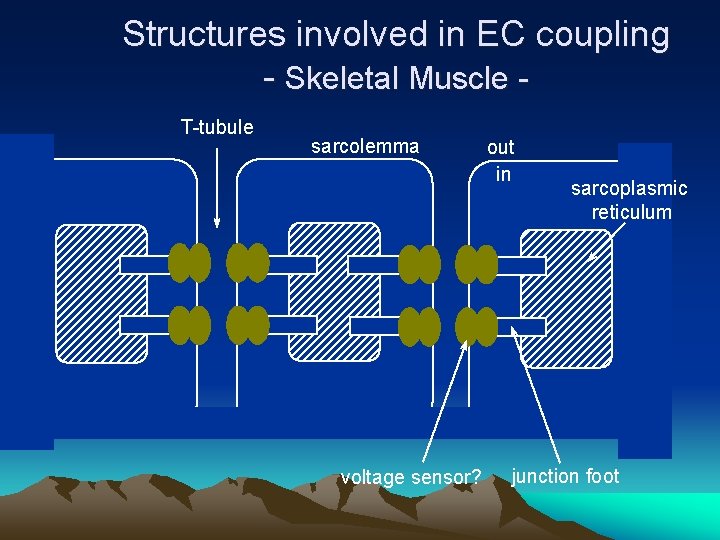
Structures involved in EC coupling - Skeletal Muscle T-tubule sarcolemma voltage sensor? out in sarcoplasmic reticulum junction foot
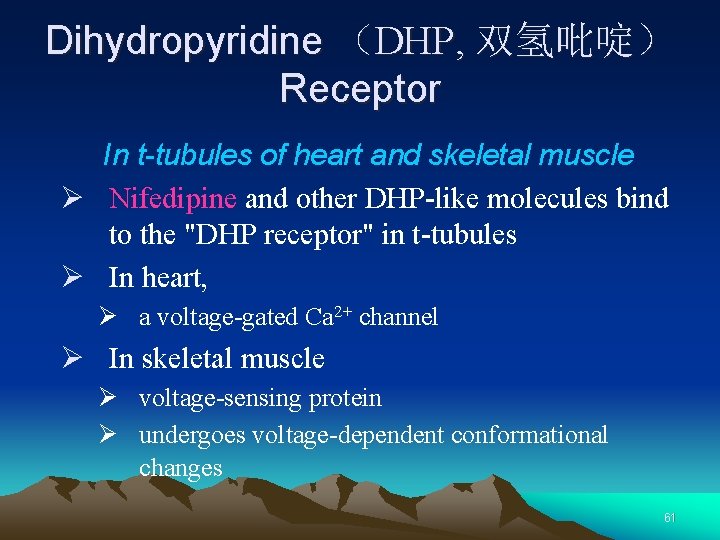
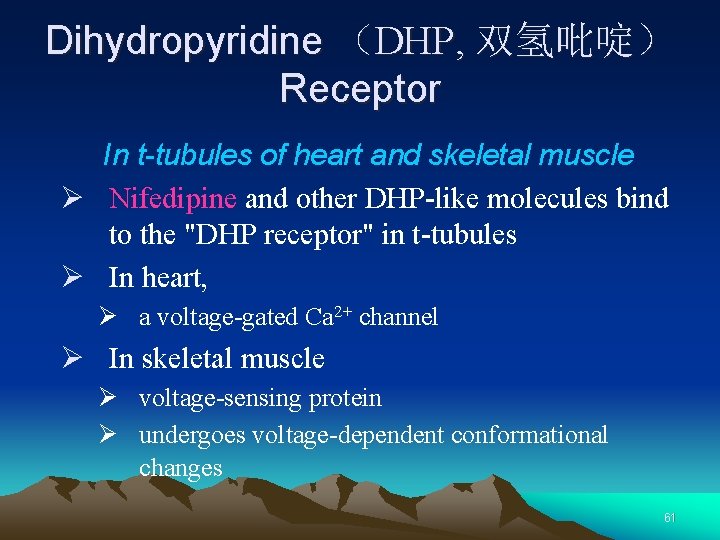
Dihydropyridine (DHP, 双氢吡啶) Receptor In t-tubules of heart and skeletal muscle Ø Nifedipine and other DHP-like molecules bind to the "DHP receptor" in t-tubules Ø In heart, Ø a voltage-gated Ca 2+ channel Ø In skeletal muscle Ø voltage-sensing protein Ø undergoes voltage-dependent conformational changes 61
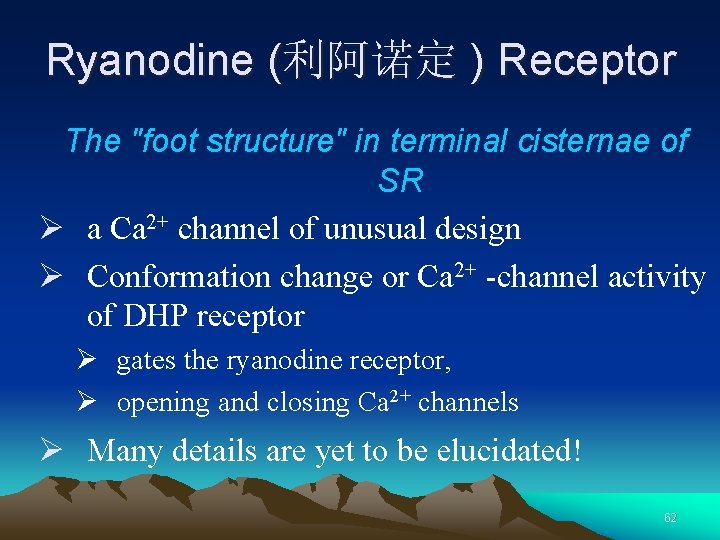
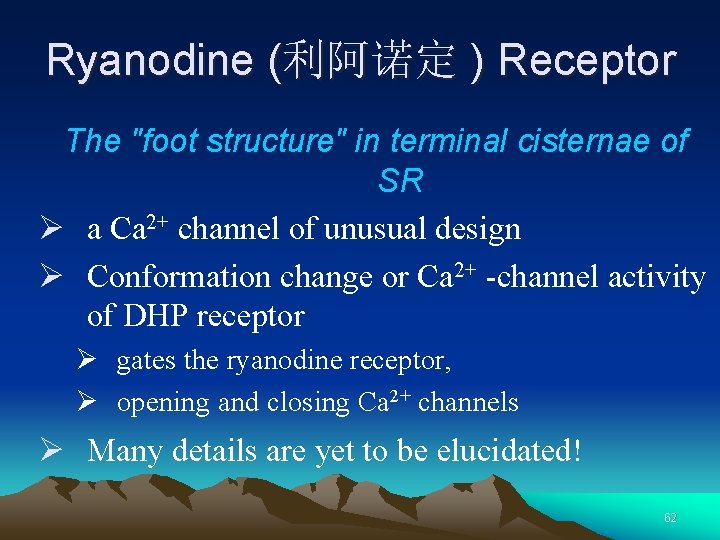
Ryanodine (利阿诺定 ) Receptor The "foot structure" in terminal cisternae of SR Ø a Ca 2+ channel of unusual design Ø Conformation change or Ca 2+ -channel activity of DHP receptor Ø gates the ryanodine receptor, Ø opening and closing Ca 2+ channels Ø Many details are yet to be elucidated! 62
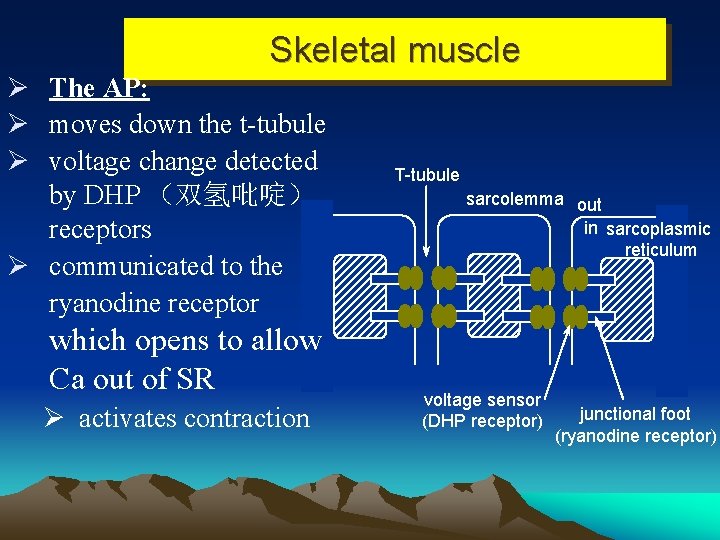
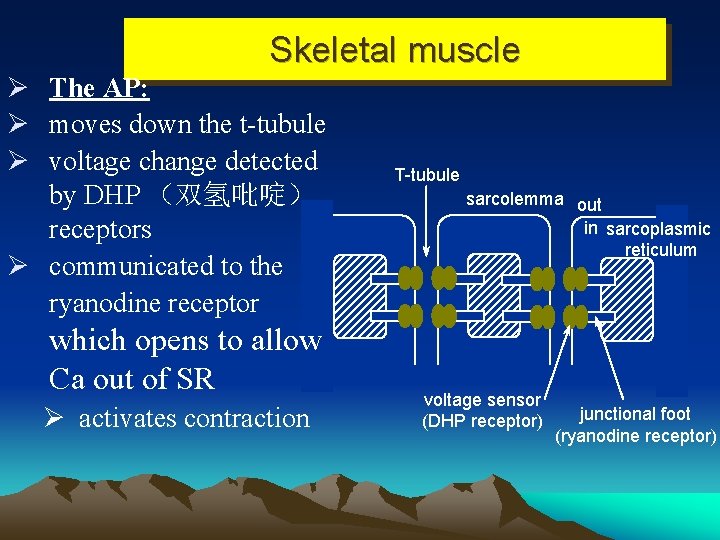
Skeletal muscle Ø The AP: Ø moves down the t-tubule Ø voltage change detected by DHP (双氢吡啶) receptors Ø communicated to the ryanodine receptor which opens to allow Ca out of SR Ø activates contraction T-tubule sarcolemma out in sarcoplasmic reticulum voltage sensor (DHP receptor) junctional foot (ryanodine receptor)
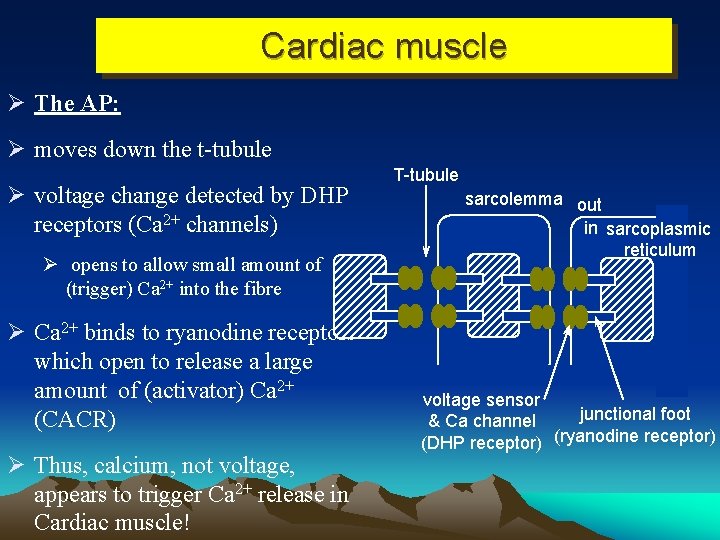
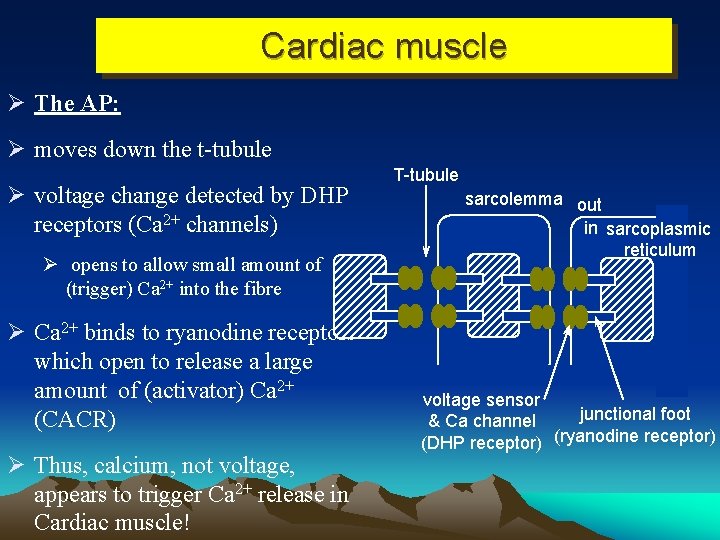
Cardiac muscle Ø The AP: Ø moves down the t-tubule Ø voltage change detected by DHP receptors (Ca 2+ channels) Ø opens to allow small amount of (trigger) Ca 2+ into the fibre Ø Ca 2+ binds to ryanodine receptors which open to release a large amount of (activator) Ca 2+ (CACR) Ø Thus, calcium, not voltage, appears to trigger Ca 2+ release in Cardiac muscle! T-tubule sarcolemma out in sarcoplasmic reticulum voltage sensor junctional foot & Ca channel (DHP receptor) (ryanodine receptor)
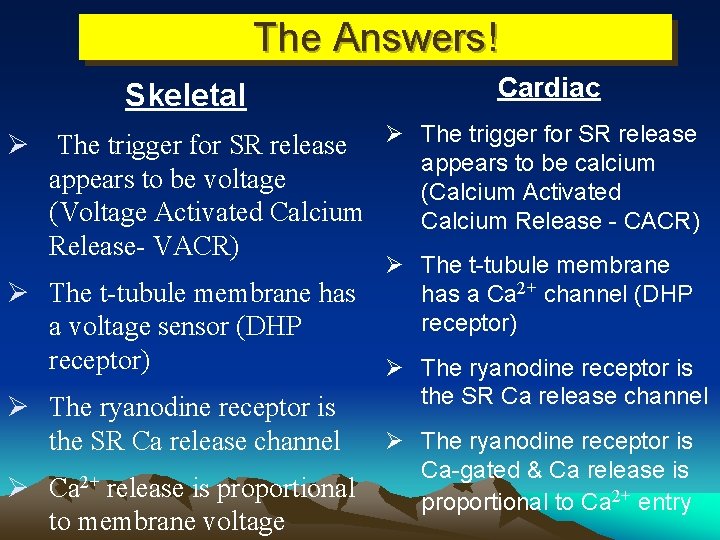
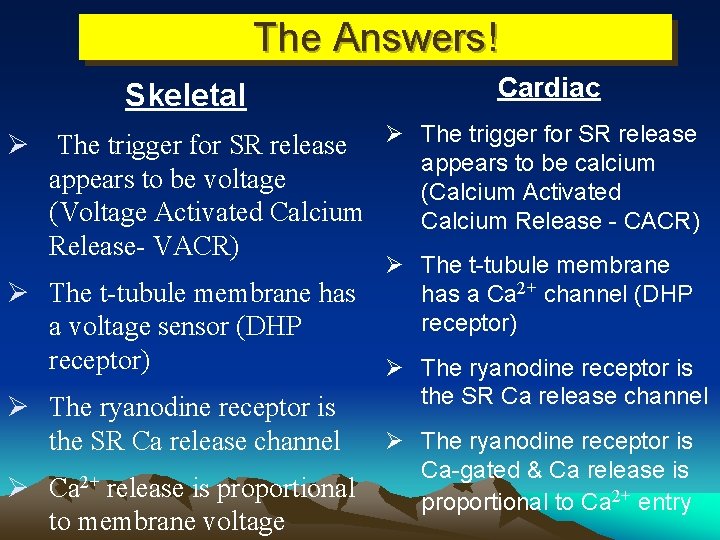
The Answers! Skeletal Cardiac Ø The trigger for SR release appears to be calcium appears to be voltage (Calcium Activated (Voltage Activated Calcium Release - CACR) Release- VACR) Ø The t-tubule membrane has a voltage sensor (DHP receptor) Ø The ryanodine receptor is the SR Ca release channel Ø Ca 2+ release is proportional to membrane voltage Ø The t-tubule membrane has a Ca 2+ channel (DHP receptor) Ø The ryanodine receptor is the SR Ca release channel Ø The ryanodine receptor is Ca-gated & Ca release is proportional to Ca 2+ entry
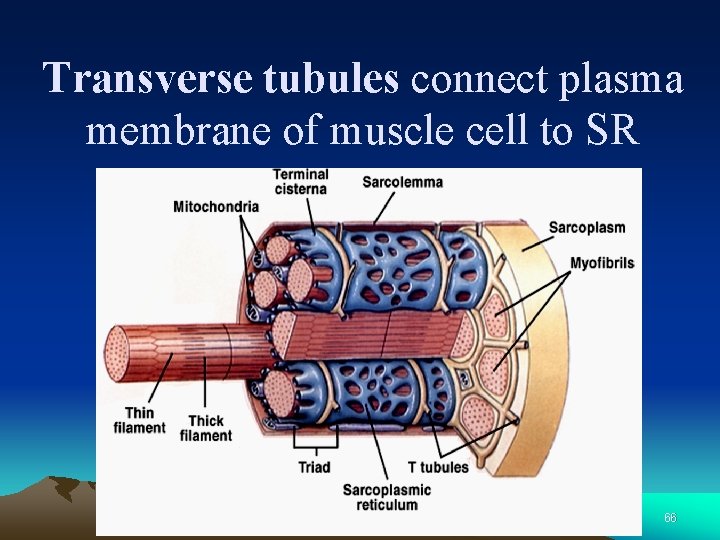
Transverse tubules connect plasma membrane of muscle cell to SR 66
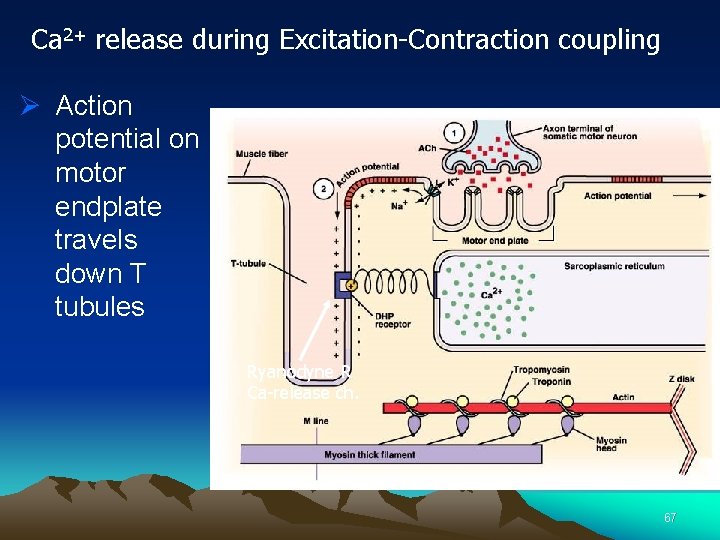
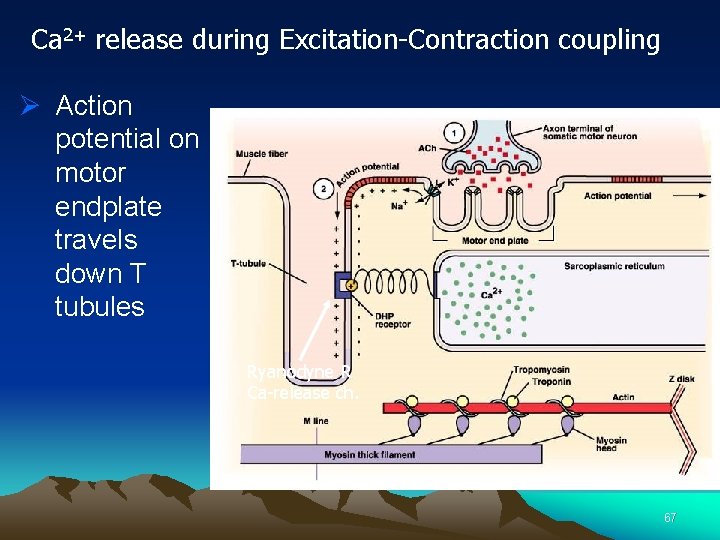
Ca 2+ release during Excitation-Contraction coupling Ø Action potential on motor endplate travels down T tubules Ryanodyne R Ca-release ch. 67
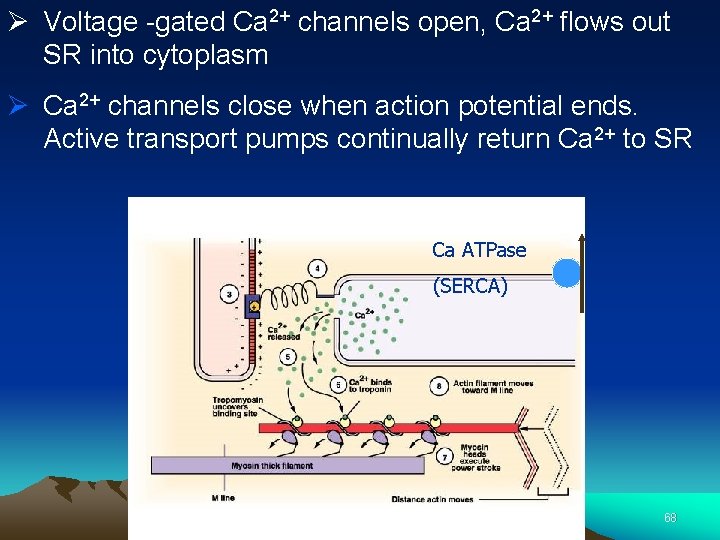
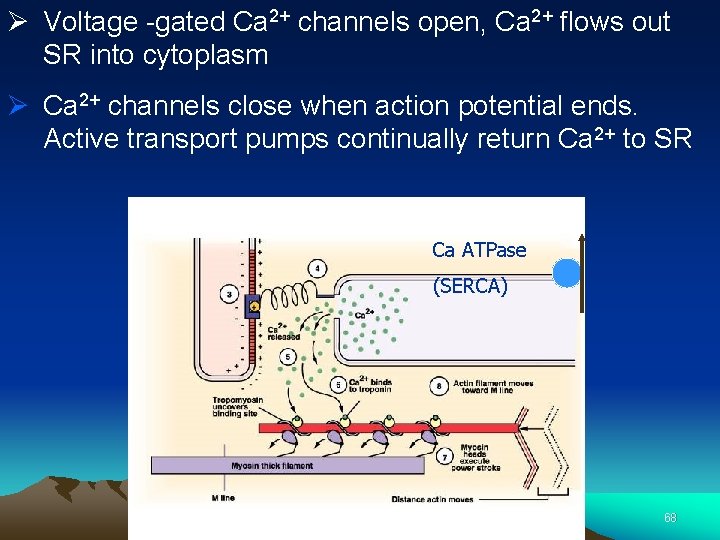
Ø Voltage -gated Ca 2+ channels open, Ca 2+ flows out SR into cytoplasm Ø Ca 2+ channels close when action potential ends. Active transport pumps continually return Ca 2+ to SR Ca ATPase (SERCA) 68
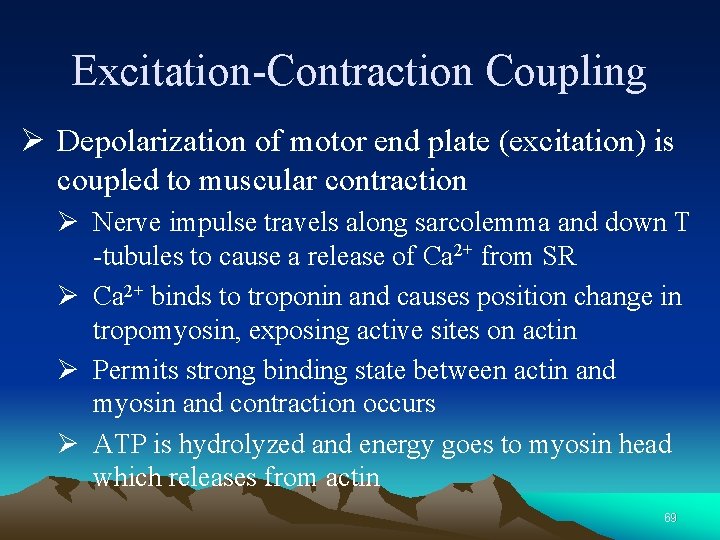
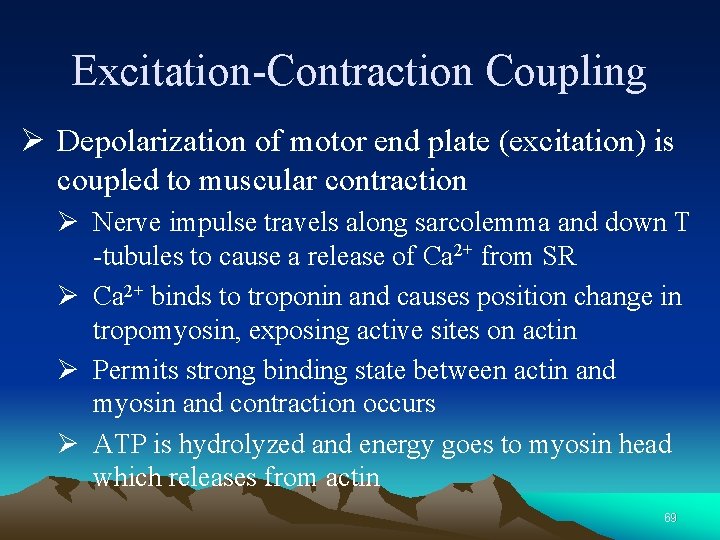
Excitation-Contraction Coupling Ø Depolarization of motor end plate (excitation) is coupled to muscular contraction Ø Nerve impulse travels along sarcolemma and down T -tubules to cause a release of Ca 2+ from SR Ø Ca 2+ binds to troponin and causes position change in tropomyosin, exposing active sites on actin Ø Permits strong binding state between actin and myosin and contraction occurs Ø ATP is hydrolyzed and energy goes to myosin head which releases from actin 69
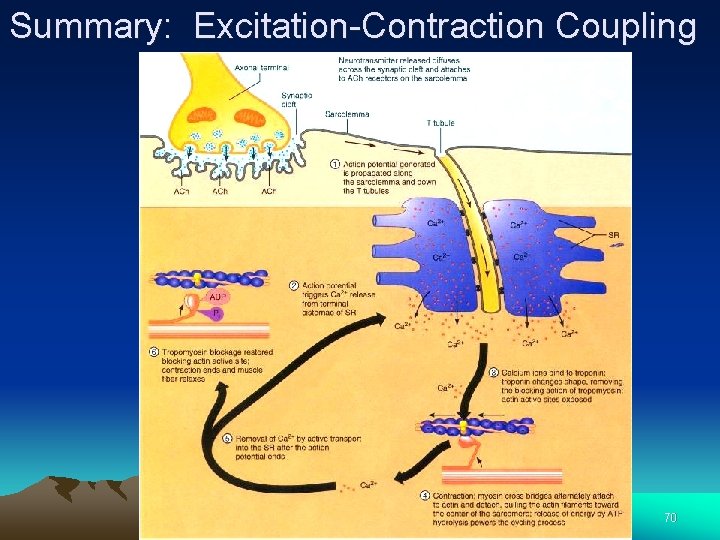
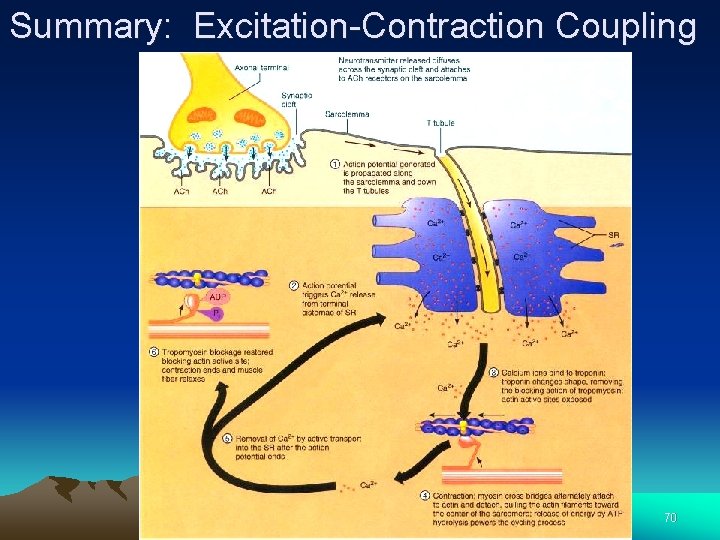
Summary: Excitation-Contraction Coupling 70
IV Factors that Affect the Efficiency of Muscle Contraction
Tension and Load Ø The force exerted on an object by a contracting muscle is known as tension. Ø The force exerted on the muscle by an object (usually its weight) is termed load. Ø According to the time of effect exerted by the loads on the muscle contraction the load was divided into two forms, preload and afterload. 72
Preload ØPreload is a load on the muscle before muscle contraction. ØDetermines the initial length of the muscle before contraction. ØInitial length is the length of the muscle fiber before its contraction. ØIt is positively proportional to the preload. 73
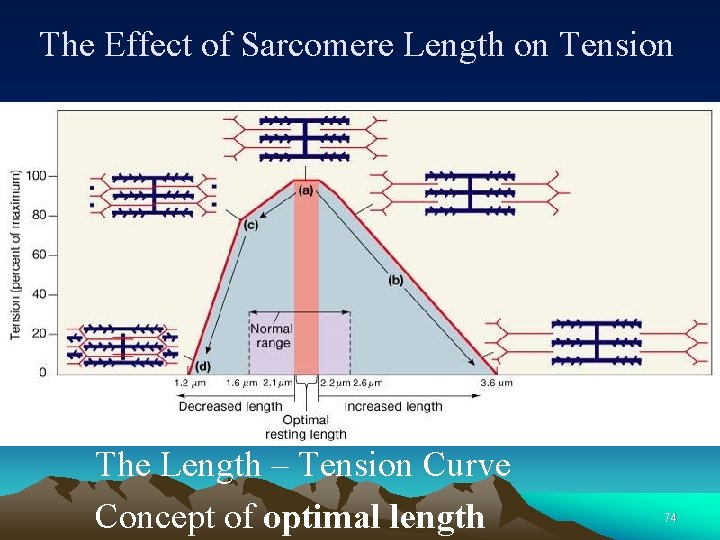
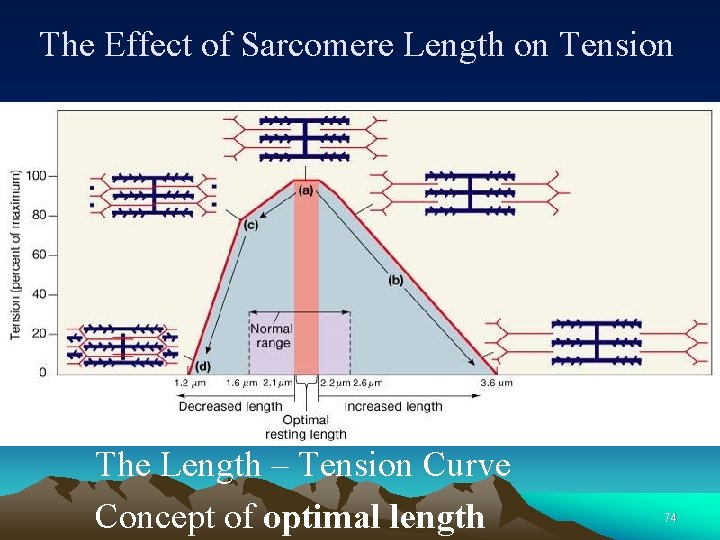
The Effect of Sarcomere Length on Tension The Length – Tension Curve Concept of optimal length 74
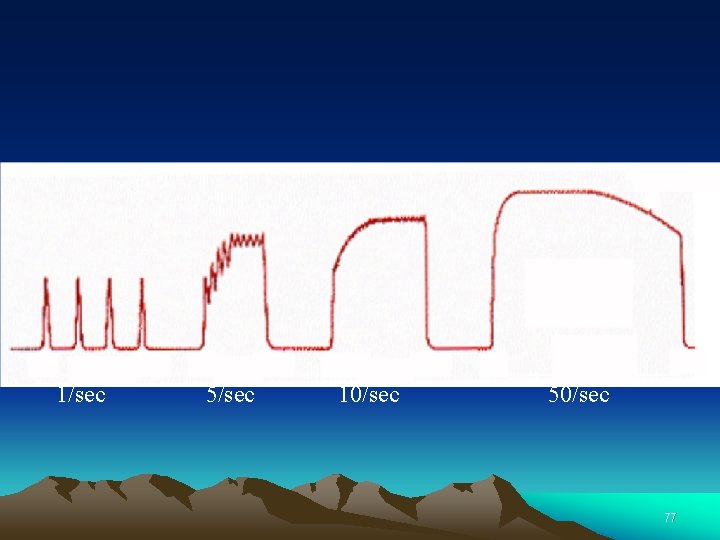
Types of Contractions I Ø Twitch: a brief mechanical contraction of a single fiber produced by a single action potential at low frequency stimulation is known as single twitch. Ø Tetanus: It means a summation of twitches that occurs at high frequency stimulation 75
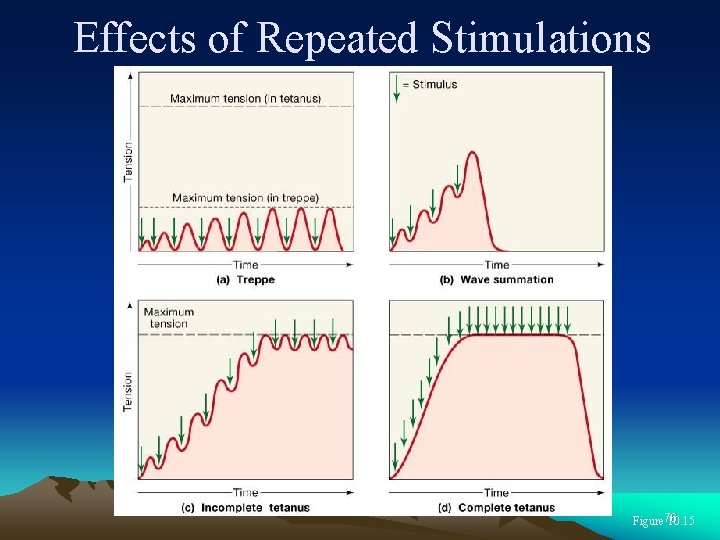
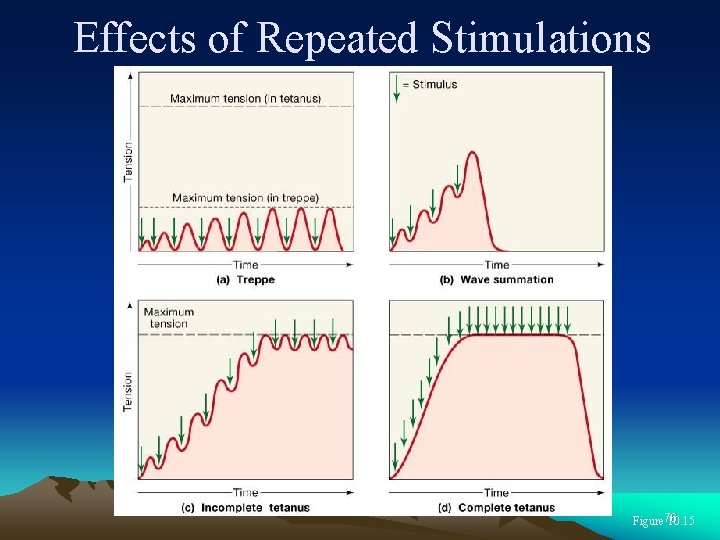
Effects of Repeated Stimulations Figure 76 10. 15
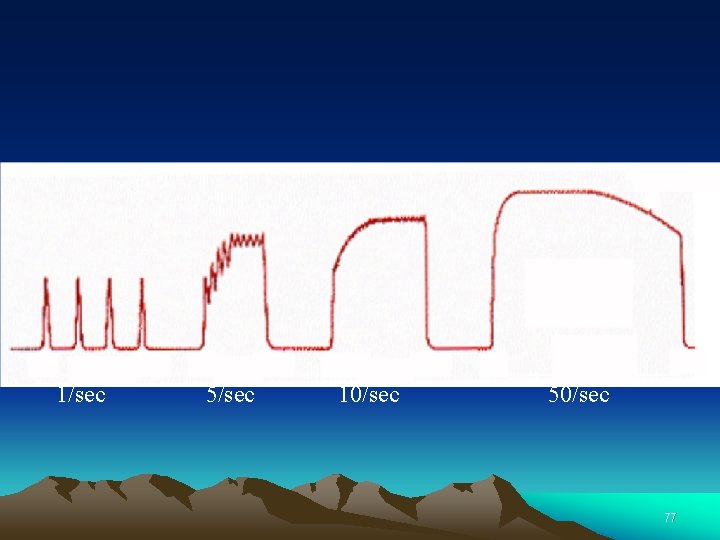
1/sec 5/sec 10/sec 50/sec 77
Afterload Ø a load on the muscle after the beginning of muscle contraction. Ø The reverse force that oppose the contractile force caused by muscle contraction. Ø does not change the initial length of the muscle Ø prevent muscle from shortening because a part of force developed by contraction is used to overcome the afterload 78
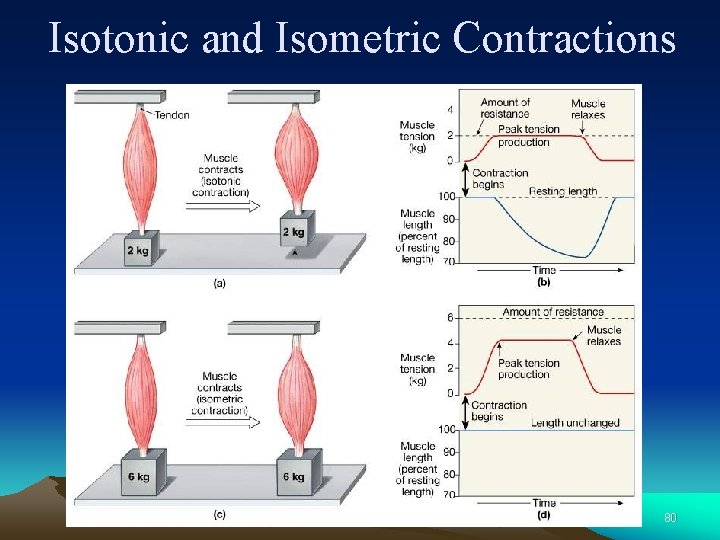
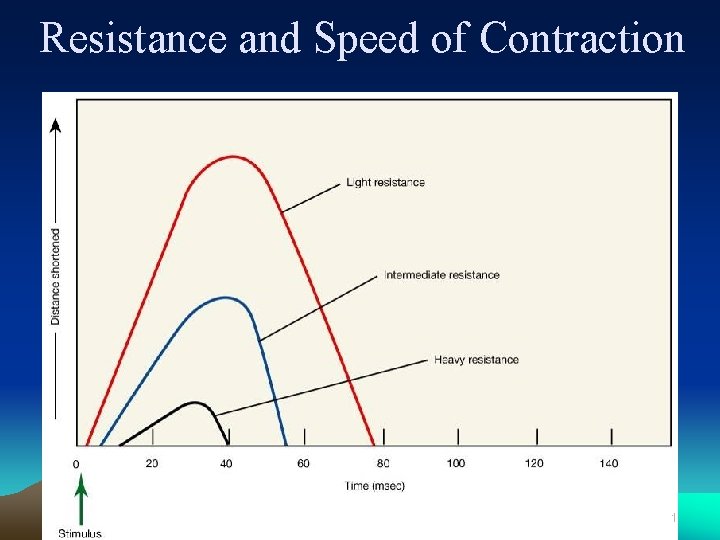
Types of Contractions (II) Ø Afterload on muscle is resistance Ø Isometric Ø Length of muscle remains constant. Peak tension produced. Does not involve movement Ø Isotonic Ø Length of muscle changes. Tension fairly constant. Involves movement at joints Ø Resistance and speed of contraction inversely related 79
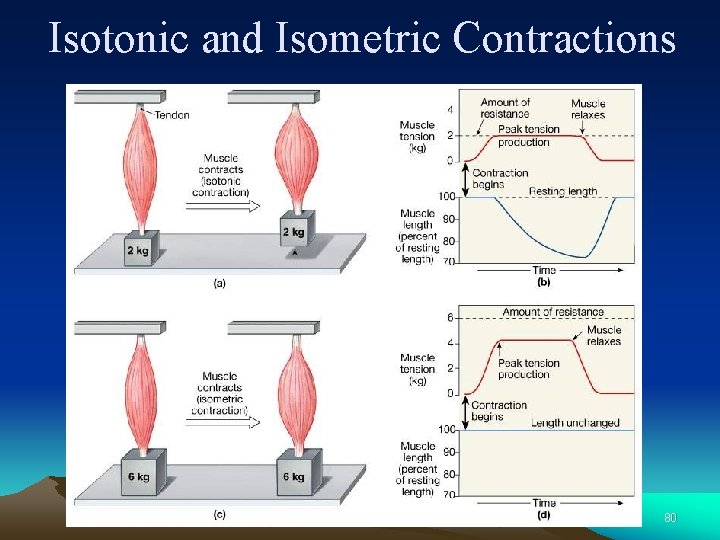
Isotonic and Isometric Contractions 80
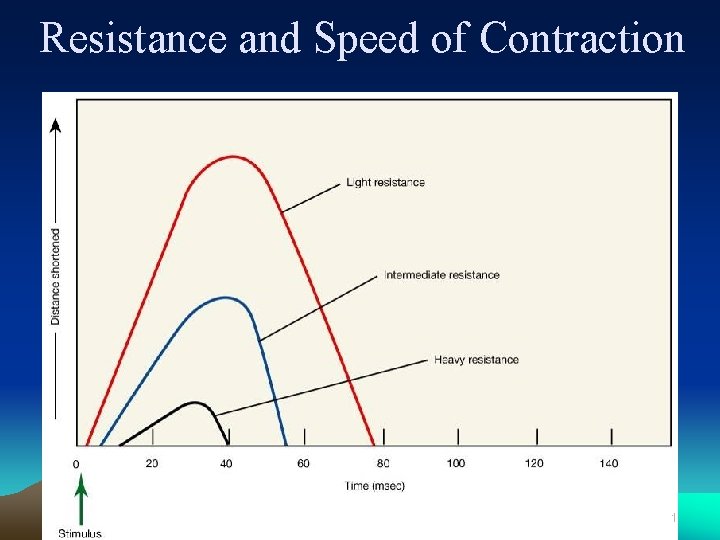
Resistance and Speed of Contraction 81
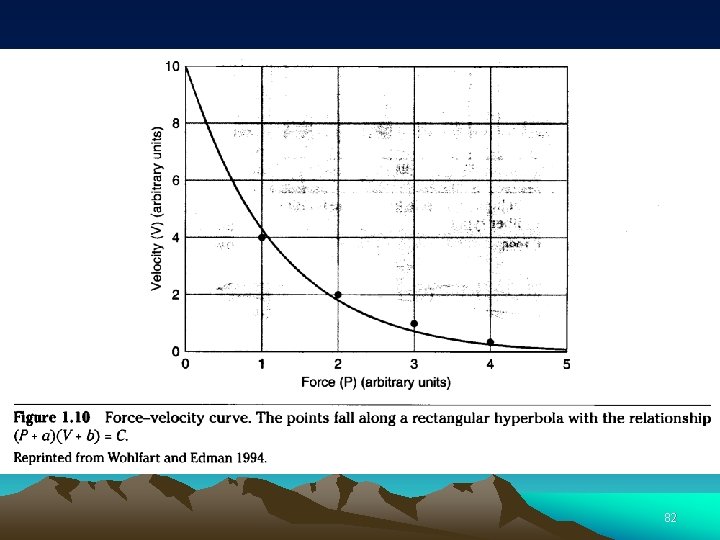
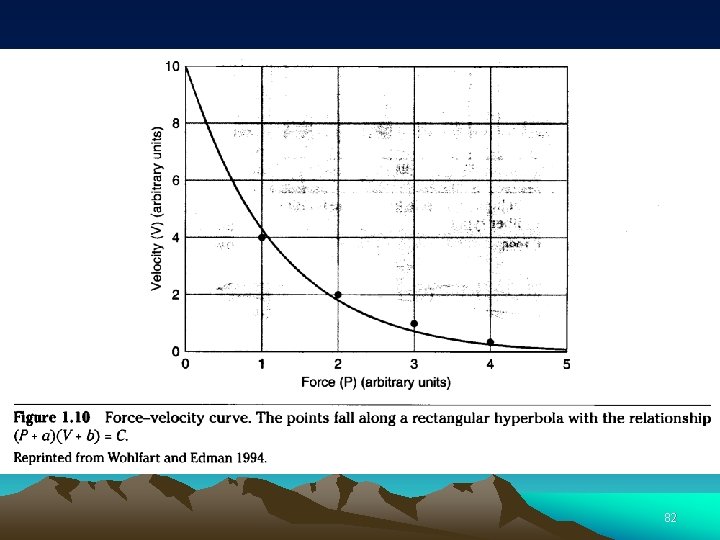
82
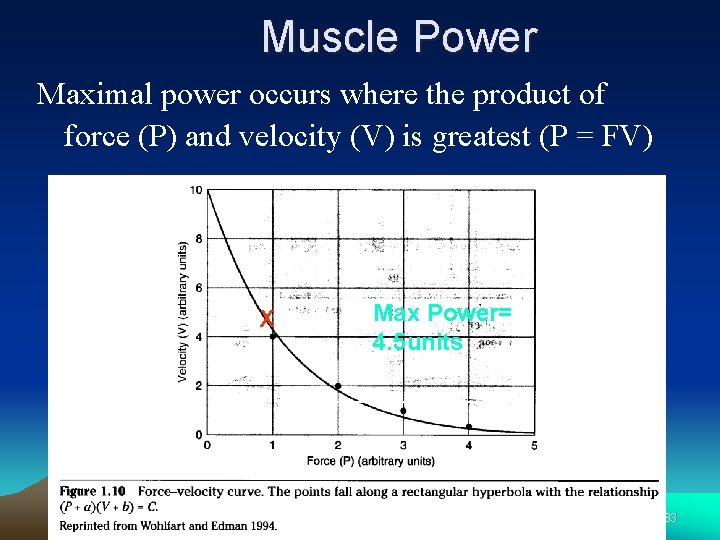
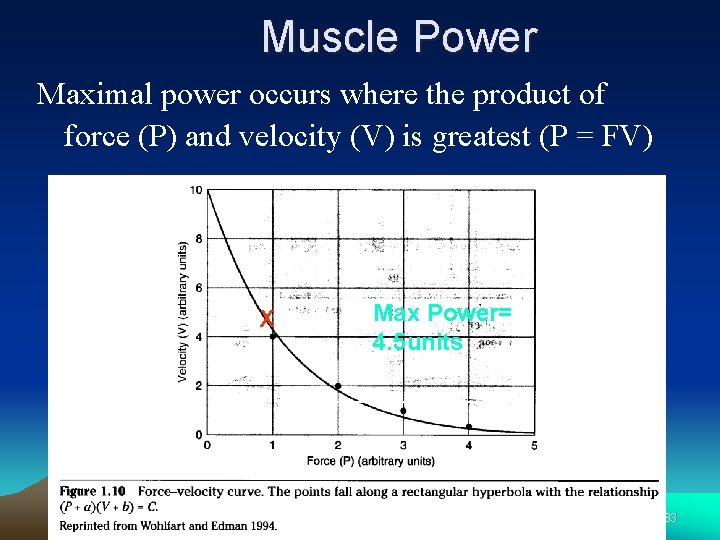
Muscle Power Maximal power occurs where the product of force (P) and velocity (V) is greatest (P = FV) X Max Power= 4. 5 units 83
 Download sequel pro for windows
Download sequel pro for windows Alex liu cecilia liu
Alex liu cecilia liu Líu líu lo lo ta ca hát say sưa
Líu líu lo lo ta ca hát say sưa Yong loo lin school of medicine
Yong loo lin school of medicine Kim ung yong
Kim ung yong Spring, summer, fall, winter... and spring cast
Spring, summer, fall, winter... and spring cast Tong aik v eastern minerals
Tong aik v eastern minerals Kwon ji yong age
Kwon ji yong age Lei yong
Lei yong What is frustration in psychology
What is frustration in psychology Yong aaron tan
Yong aaron tan Yong lei
Yong lei Yong soon min
Yong soon min Cerita salmiah 11
Cerita salmiah 11 Csub bpa
Csub bpa Ban yong
Ban yong Dissected heart
Dissected heart Sql yong
Sql yong Sql query
Sql query Medical physiology
Medical physiology Xbongda
Xbongda Chuẩn ieee 754/85
Chuẩn ieee 754/85 Ding chuan acupuncture point
Ding chuan acupuncture point Công thức bán kính hội tụ
Công thức bán kính hội tụ Giáo dục chuẩn mực ngữ âm tiếng việt
Giáo dục chuẩn mực ngữ âm tiếng việt Tiêu chuẩn d'alembert
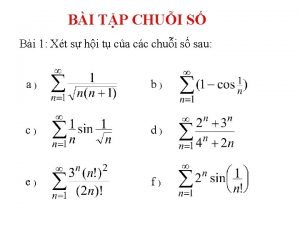
Tiêu chuẩn d'alembert 5 tiêu chuẩn finer
5 tiêu chuẩn finer Biểu diễn số thực theo chuẩn ieee 754
Biểu diễn số thực theo chuẩn ieee 754 Tiêu chuẩn anthonisen
Tiêu chuẩn anthonisen Chuẩn đoán
Chuẩn đoán Tiêu chuẩn atlanta 2012
Tiêu chuẩn atlanta 2012 Chuẩn mực nhóm
Chuẩn mực nhóm độ lệch chuẩn
độ lệch chuẩn đánh giá theo chuẩn nghề nghiệp giáo viên csgdpt
đánh giá theo chuẩn nghề nghiệp giáo viên csgdpt Cho lược đồ quan hệ q(abcdegh)
Cho lược đồ quan hệ q(abcdegh) Target institute of medical education and research
Target institute of medical education and research Pima medical institute dress code
Pima medical institute dress code Beijing medical equipment institute
Beijing medical equipment institute California medical license application
California medical license application Gbmc infoweb
Gbmc infoweb Hepburn osteometric board
Hepburn osteometric board Torrance memorial outpatient lab
Torrance memorial outpatient lab Cartersville medical center medical records
Cartersville medical center medical records Charter school institute
Charter school institute Santa fe institute summer school
Santa fe institute summer school Diane liu md
Diane liu md Chiu-chu liu
Chiu-chu liu Lucy liu what my girl do
Lucy liu what my girl do Chee wee liu
Chee wee liu Yang liu stanford
Yang liu stanford Dthreads
Dthreads Jingchen liu
Jingchen liu Karin björsten liu
Karin björsten liu Sissi liu
Sissi liu Chim đậu trên cành chim hót líu lo
Chim đậu trên cành chim hót líu lo J liu
J liu Bing images
Bing images Jun s. liu
Jun s. liu 732a64
732a64 Zi=
Zi= Candace liu
Candace liu Andrea j liu
Andrea j liu Hypergene liu
Hypergene liu Kevin liu toto
Kevin liu toto Liu xiang weightlifter
Liu xiang weightlifter Yang liu stanford
Yang liu stanford Peter liu seneca
Peter liu seneca Zaijia liu
Zaijia liu Changbin liu
Changbin liu Anli liu md ma
Anli liu md ma Dong liu ustc
Dong liu ustc Chu liu edmonds algorithm
Chu liu edmonds algorithm Qingxia liu
Qingxia liu Liu math entrance exam samples
Liu math entrance exam samples Liu shen & associates
Liu shen & associates Bài hát vườn trường mùa thu mp3
Bài hát vườn trường mùa thu mp3 Cafe java liu
Cafe java liu Liu hui mathematician
Liu hui mathematician Fengjing liu
Fengjing liu Junda liu
Junda liu Liu pengpeng
Liu pengpeng Liu bolin
Liu bolin Soliscism
Soliscism Jintan liu
Jintan liu