Evaluation and Management of Chronic Diarrhea Joe Harkins




- Slides: 74
Evaluation and Management of Chronic Diarrhea Joe Harkins, PA-C Gastroenterology Center of Maine EMMC Bangor, ME
OBJECTIVES 1. Understand definition of Chronic Diarrhea and recognize difference between osmotic and secretory types. 2. Identify various causes of Chronic diarrhea. 3. Evaluate cases of Chronic Diarrhea including history, exam, and testing. 4. Understand endoscopy guidelines including EGD, Colonoscopy, and Capsule endoscopy. 5. Determine appropriate work-up on basis of whether feces is watery, fatty, or bloody. 6. Choose effective treatments for respective cases of chronic diarrhea.
1 st - RULE OUT CONSTIPATION • Sometimes patient thinks it is diarrhea when actually it is overflow from constipation. • Pelvic Floor Dysfunction can happen if trouble with IAS, HX abdominal/pelvic surgery, Connective tissue disorder, DM, adverse drug effects, dehydration. • Check upright KUB for fecal loading.
RED FLAGS • • • Fever Blood Loss Unexplained weight loss Abdominal Pain Nocturnal episodes • REFER TO ER OR call GI.
DEFINITION of diarrhea 1. Loose stools 2. More than 3 BM per day 3. Stool output weight>200 gram/day
Definition • CHRONIC diarrhea: duration > 4 weeks. • Functional Diarrhea , ROME III criteria: daytime painless diarrhea > 3 months.
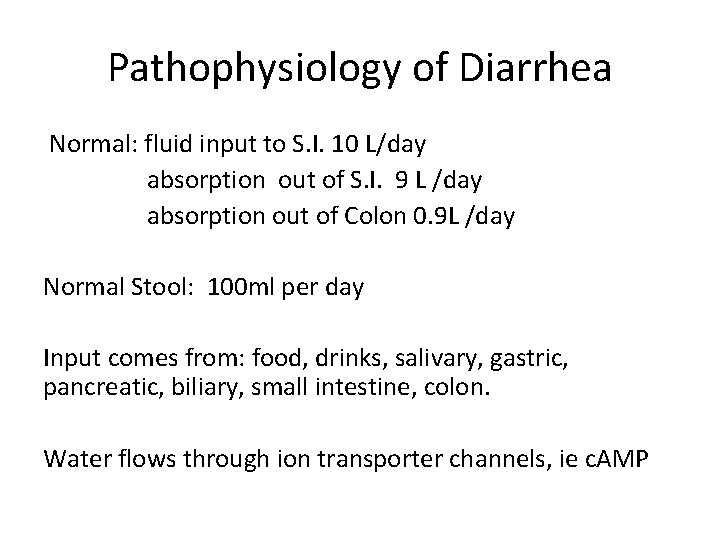
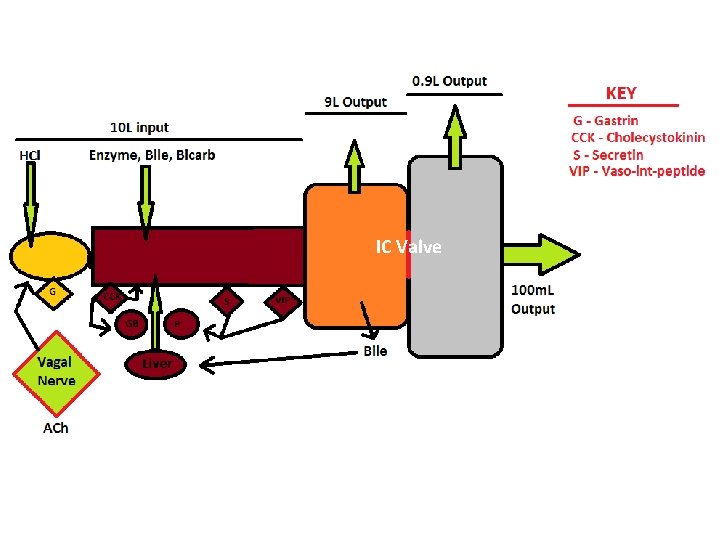
Pathophysiology of Diarrhea Normal: fluid input to S. I. 10 L/day absorption out of S. I. 9 L /day absorption out of Colon 0. 9 L /day Normal Stool: 100 ml per day Input comes from: food, drinks, salivary, gastric, pancreatic, biliary, small intestine, colon. Water flows through ion transporter channels, ie c. AMP
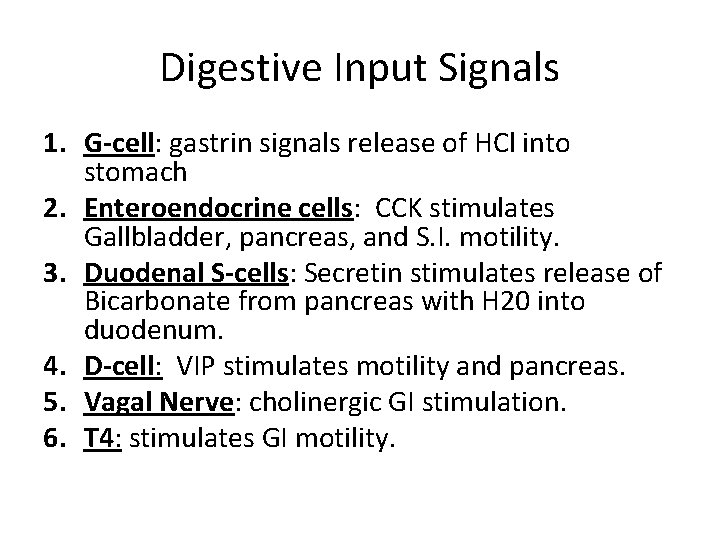
Digestive Input Signals 1. G-cell: gastrin signals release of HCl into stomach 2. Enteroendocrine cells: CCK stimulates Gallbladder, pancreas, and S. I. motility. 3. Duodenal S-cells: Secretin stimulates release of Bicarbonate from pancreas with H 20 into duodenum. 4. D-cell: VIP stimulates motility and pancreas. 5. Vagal Nerve: cholinergic GI stimulation. 6. T 4: stimulates GI motility.
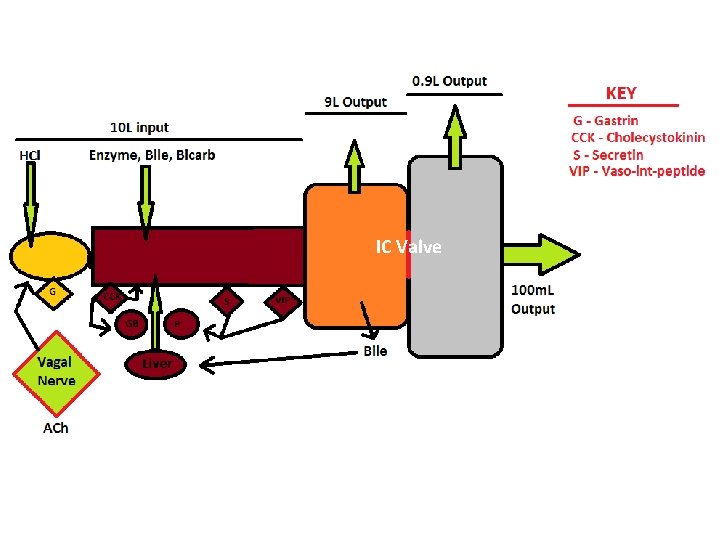
IC Valve

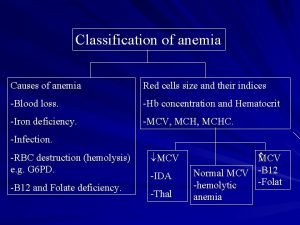
Types of Diarrhea • Osmotic • Secretory • In Practice: Watery Fatty Bloody
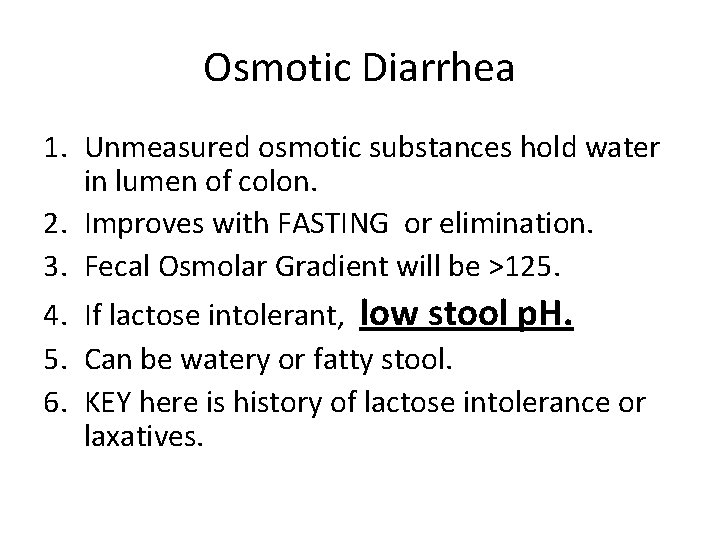
Osmotic Diarrhea 1. Unmeasured osmotic substances hold water in lumen of colon. 2. Improves with FASTING or elimination. 3. Fecal Osmolar Gradient will be >125. 4. If lactose intolerant, low stool p. H. 5. Can be watery or fatty stool. 6. KEY here is history of lactose intolerance or laxatives.
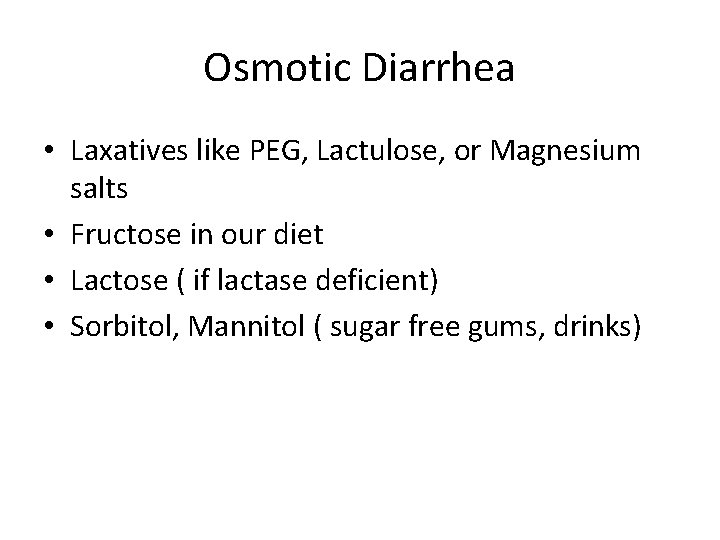
Osmotic Diarrhea • Laxatives like PEG, Lactulose, or Magnesium salts • Fructose in our diet • Lactose ( if lactase deficient) • Sorbitol, Mannitol ( sugar free gums, drinks)
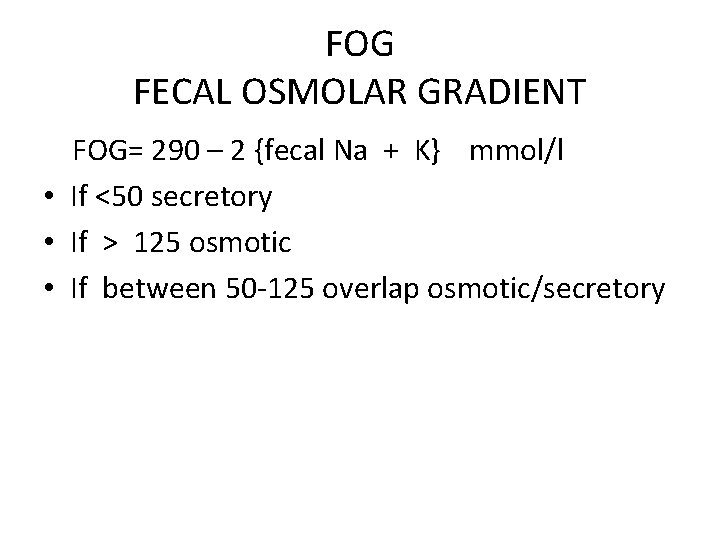
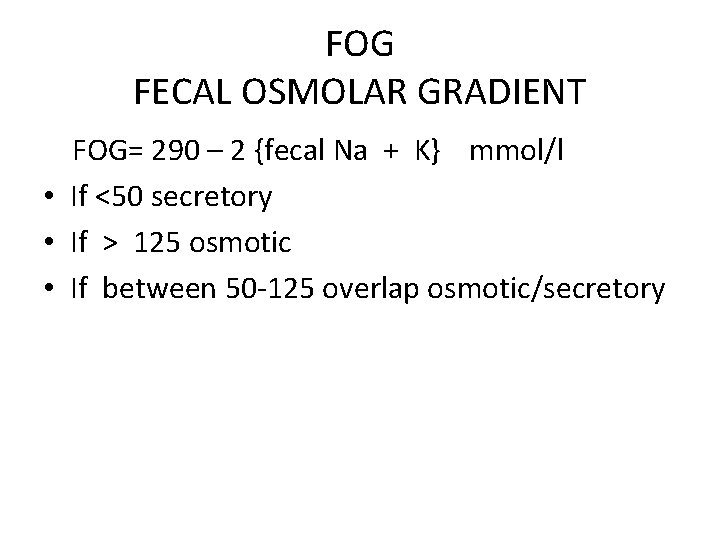
FOG FECAL OSMOLAR GRADIENT FOG= 290 – 2 {fecal Na + K} mmol/l • If <50 secretory • If > 125 osmotic • If between 50 -125 overlap osmotic/secretory
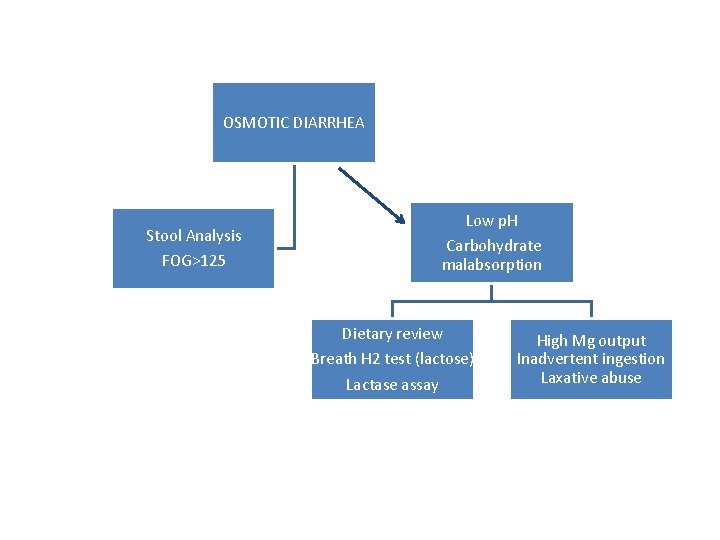
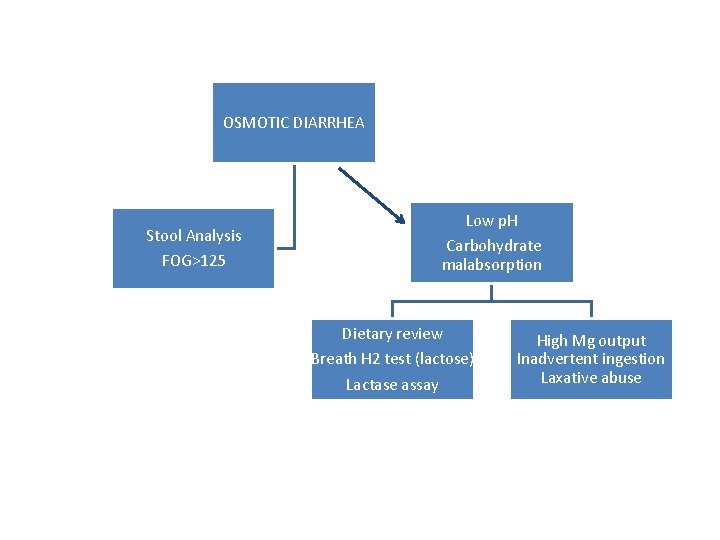
OSMOTIC DIARRHEA Stool Analysis FOG>125 Low p. H Carbohydrate malabsorption Dietary review Breath H 2 test (lactose) Lactase assay High Mg output Inadvertent ingestion Laxative abuse
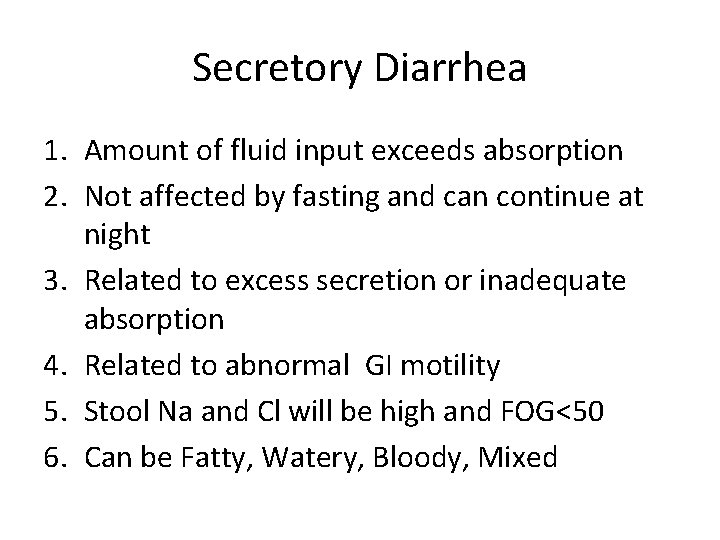
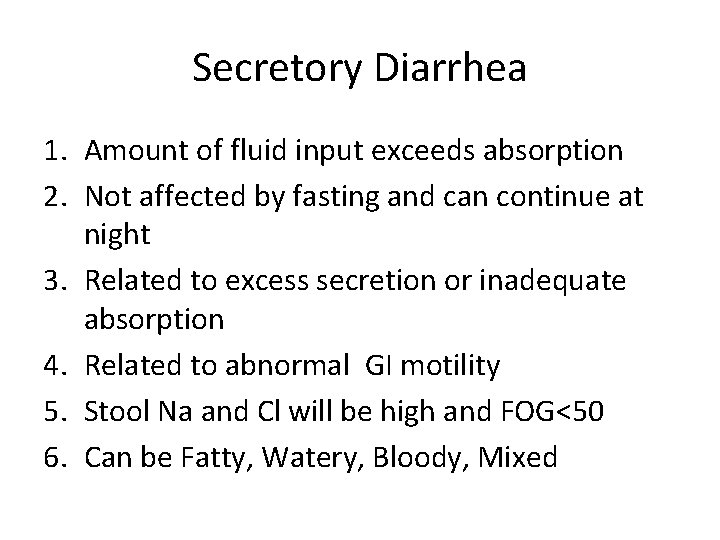
Secretory Diarrhea 1. Amount of fluid input exceeds absorption 2. Not affected by fasting and can continue at night 3. Related to excess secretion or inadequate absorption 4. Related to abnormal GI motility 5. Stool Na and Cl will be high and FOG<50 6. Can be Fatty, Watery, Bloody, Mixed
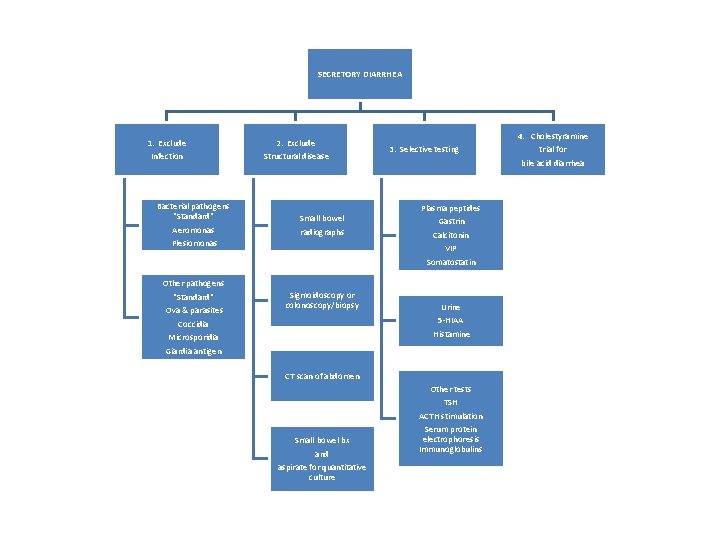
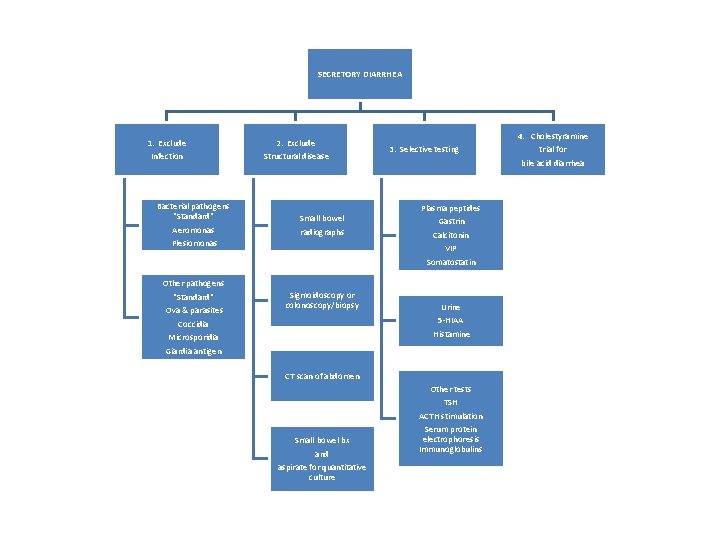
SECRETORY DIARRHEA 1. Exclude Infection 2. Exclude Structural disease Bacterial pathogens "Standard" Aeromonas Plesiomonas Small bowel radiographs Other pathogens "Standard" Ova & parasites Coccidia Sigmoidoscopy or colonoscopy/biopsy Microsporidia Giardia antigen 3. Selective testing Plasma peptides Gastrin Calcitonin VIP Somatostatin Urine 5 -HIAA Histamine CT scan of abdomen Small bowel bx and aspirate for quantitative culture Other tests TSH ACTH stimulation Serum protein electrophoresis Immunoglobulins 4. Cholestyramine trial for bile acid diarrhea
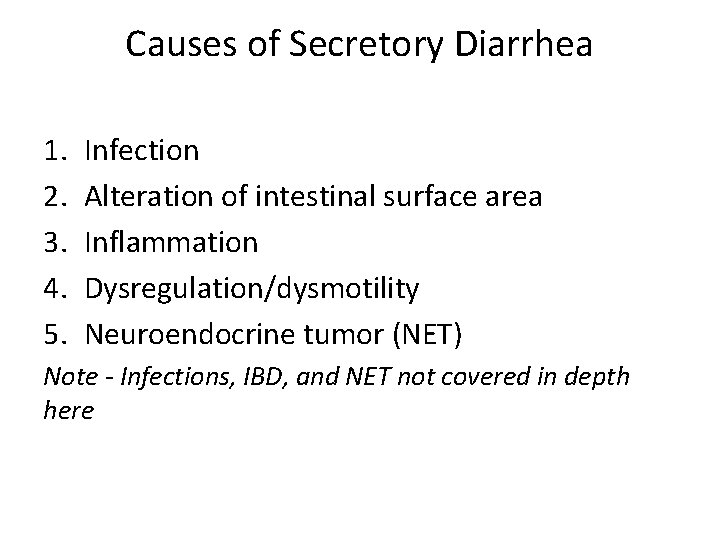
Causes of Secretory Diarrhea 1. 2. 3. 4. 5. Infection Alteration of intestinal surface area Inflammation Dysregulation/dysmotility Neuroendocrine tumor (NET) Note - Infections, IBD, and NET not covered in depth here
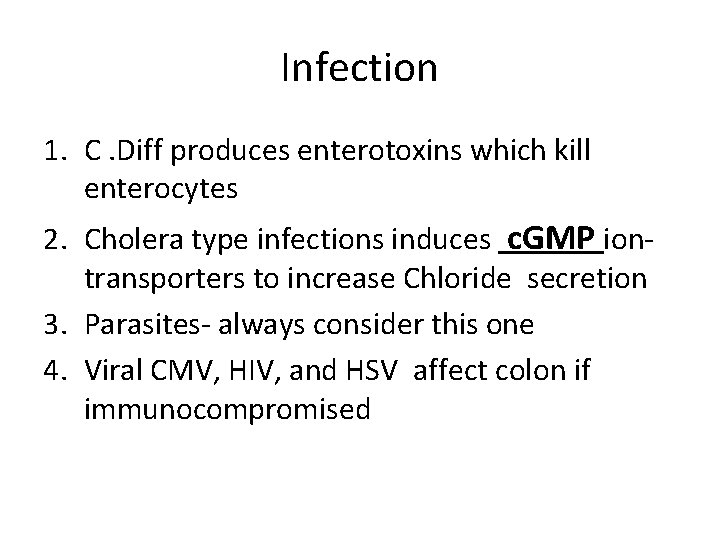
Infection 1. C. Diff produces enterotoxins which kill enterocytes 2. Cholera type infections induces c. GMP iontransporters to increase Chloride secretion 3. Parasites- always consider this one 4. Viral CMV, HIV, and HSV affect colon if immunocompromised
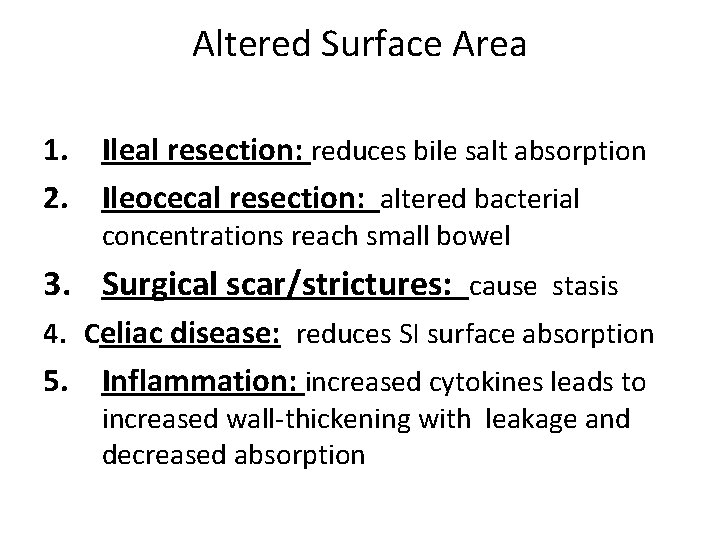
Altered Surface Area 1. Ileal resection: reduces bile salt absorption 2. Ileocecal resection: altered bacterial concentrations reach small bowel 3. Surgical scar/strictures: cause stasis 4. Celiac disease: reduces SI surface absorption 5. Inflammation: increased cytokines leads to increased wall-thickening with leakage and decreased absorption
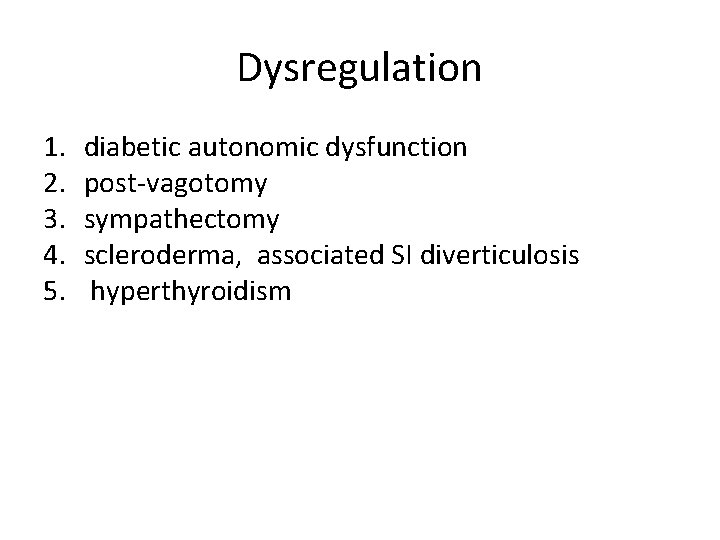
Dysregulation 1. 2. 3. 4. 5. diabetic autonomic dysfunction post-vagotomy sympathectomy scleroderma, associated SI diverticulosis hyperthyroidism
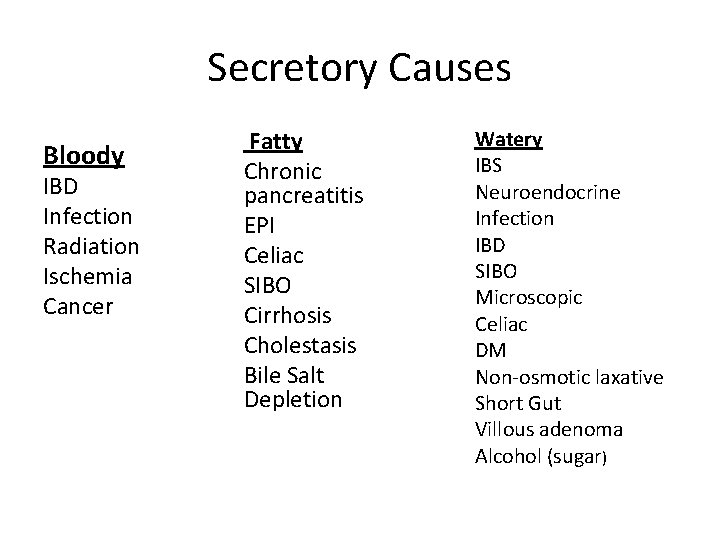
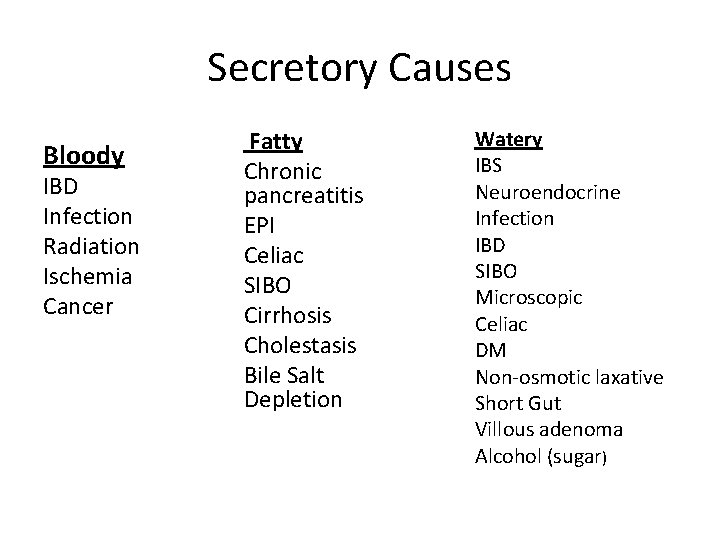
Secretory Causes Bloody IBD Infection Radiation Ischemia Cancer Fatty Chronic pancreatitis EPI Celiac SIBO Cirrhosis Cholestasis Bile Salt Depletion Watery IBS Neuroendocrine Infection IBD SIBO Microscopic Celiac DM Non-osmotic laxative Short Gut Villous adenoma Alcohol (sugar)
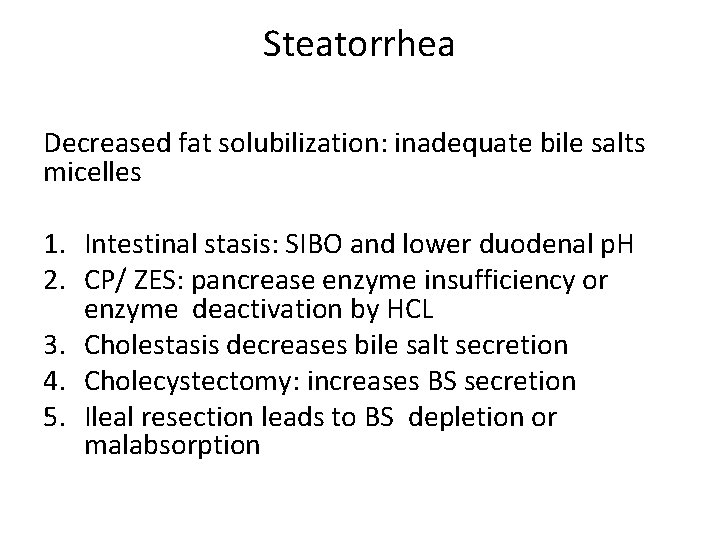
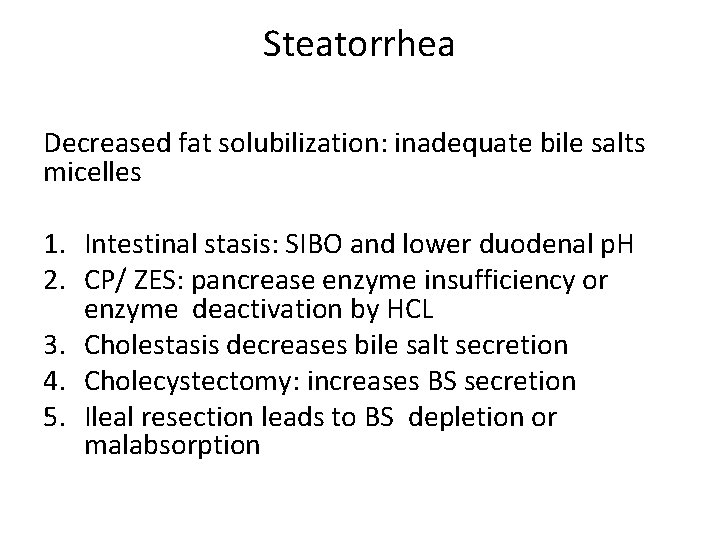
Steatorrhea Decreased fat solubilization: inadequate bile salts micelles 1. Intestinal stasis: SIBO and lower duodenal p. H 2. CP/ ZES: pancrease enzyme insufficiency or enzyme deactivation by HCL 3. Cholestasis decreases bile salt secretion 4. Cholecystectomy: increases BS secretion 5. Ileal resection leads to BS depletion or malabsorption
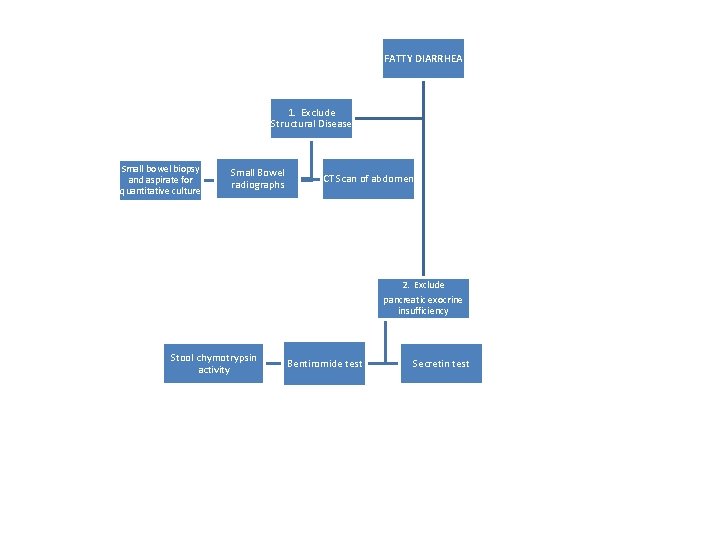
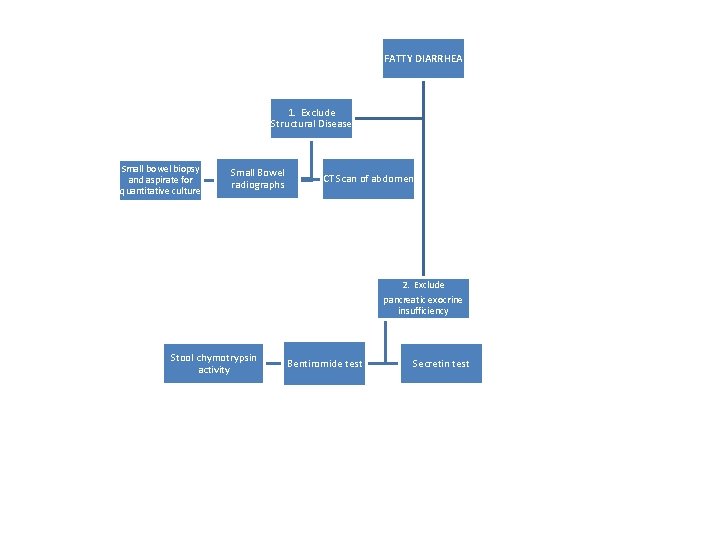
FATTY DIARRHEA 1. Exclude Structural Disease Small bowel biopsy and aspirate for quantitative culture Small Bowel radiographs CT Scan of abdomen 2. Exclude pancreatic exocrine insufficiency Stool chymotrypsin activity Bentiromide test Secretin test
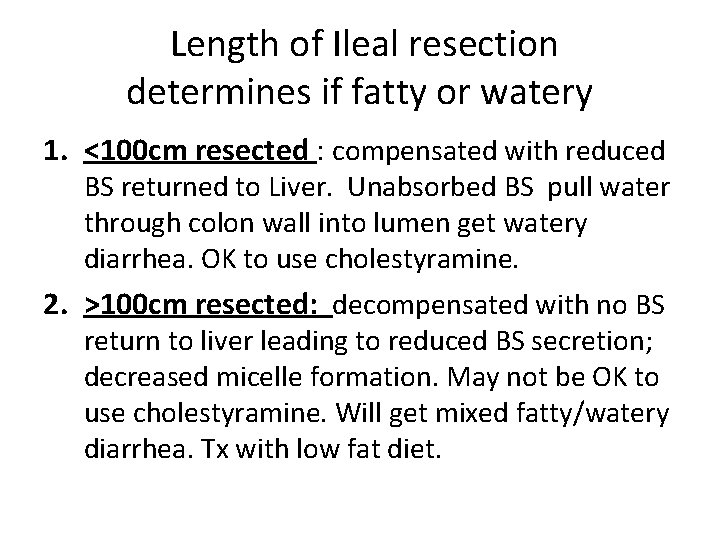
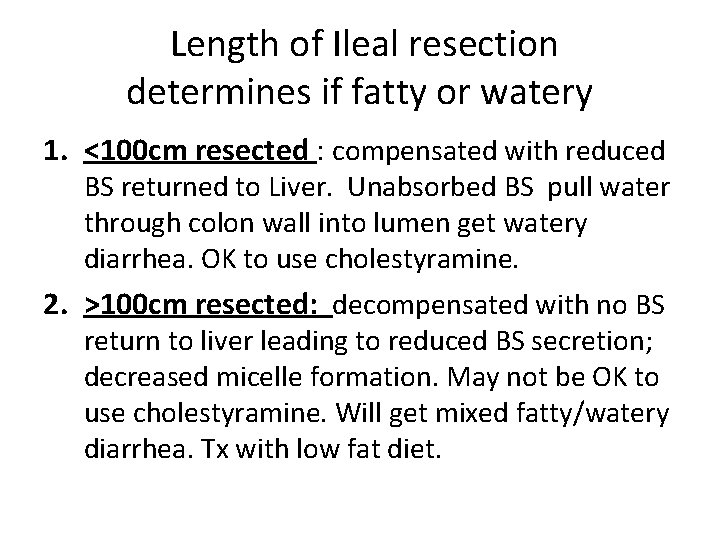
Length of Ileal resection determines if fatty or watery 1. <100 cm resected : compensated with reduced BS returned to Liver. Unabsorbed BS pull water through colon wall into lumen get watery diarrhea. OK to use cholestyramine. 2. >100 cm resected: decompensated with no BS return to liver leading to reduced BS secretion; decreased micelle formation. May not be OK to use cholestyramine. Will get mixed fatty/watery diarrhea. Tx with low fat diet.
Inflammation • Wall-thickening • Leaky wall • Impaired absorptive transporters
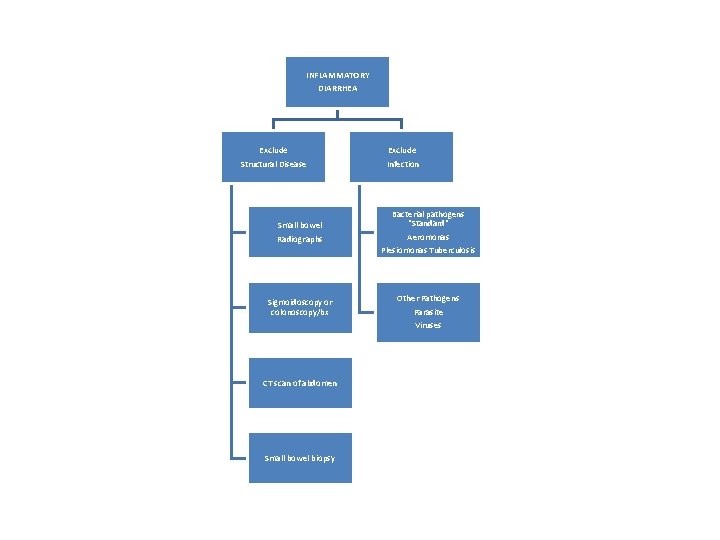
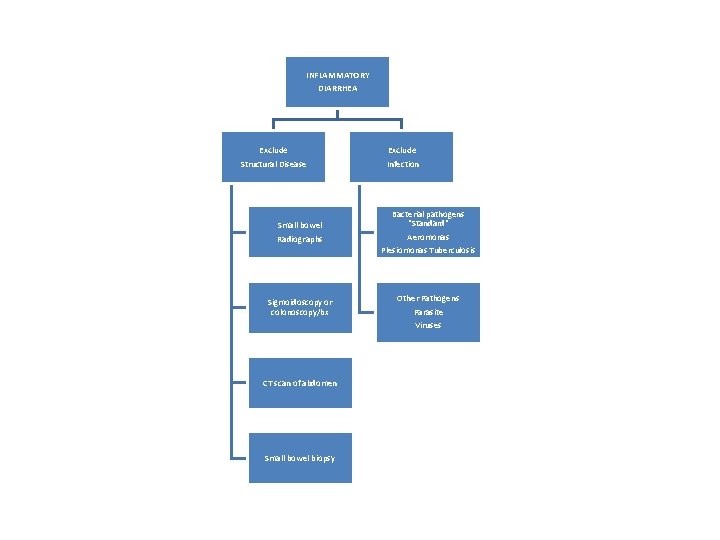
INFLAMMATORY DIARRHEA Exclude Structural Disease Small bowel Radiographs Sigmoidoscopy or colonoscopy/bx CT scan of abdomen Small bowel biopsy Exclude Infection Bacterial pathogens "Standard" Aeromonas Plesiomonas Tuberculosis Other Pathogens Parasite Viruses
Evaluation of Diarrhea 1. 2. 3. 4. 5. 6. History Medication Physical Exam Labs/tests Imaging Endoscopy
History 1. Stool: Duration, Frequency, Intermittent vs. continuous, affected by fasting, blood, greasy, watery, mucus, Nocturnal, incontinence. 2. Physical Symptoms reveal Clues and Severity 3. Weight loss
History • Hx Surgery, radiation therapy. • PMHx: Chronic pancreatitis, Peptic Ulcers, Thyroid disease, Diabetes, HIV. • Check Diet: caffeine, FODMAPs, lactose, alcohol, diet sweeteners. • Travel History. • Well water ( giardia). • Sick contacts.
Medications 1. 2. 3. 4. OTC and Prescription Vitamin C (it is an acid) Cholinergics Laxatives: osmotic and non-osmotic
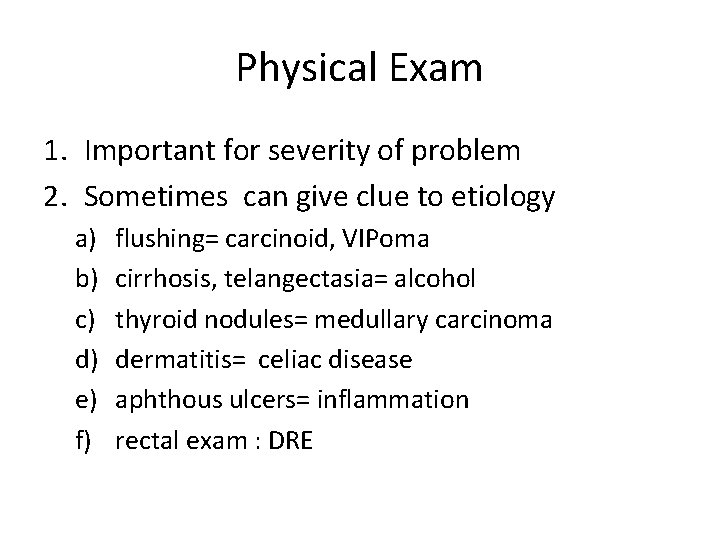
Physical Exam 1. Important for severity of problem 2. Sometimes can give clue to etiology a) b) c) d) e) f) flushing= carcinoid, VIPoma cirrhosis, telangectasia= alcohol thyroid nodules= medullary carcinoma dermatitis= celiac disease aphthous ulcers= inflammation rectal exam : DRE
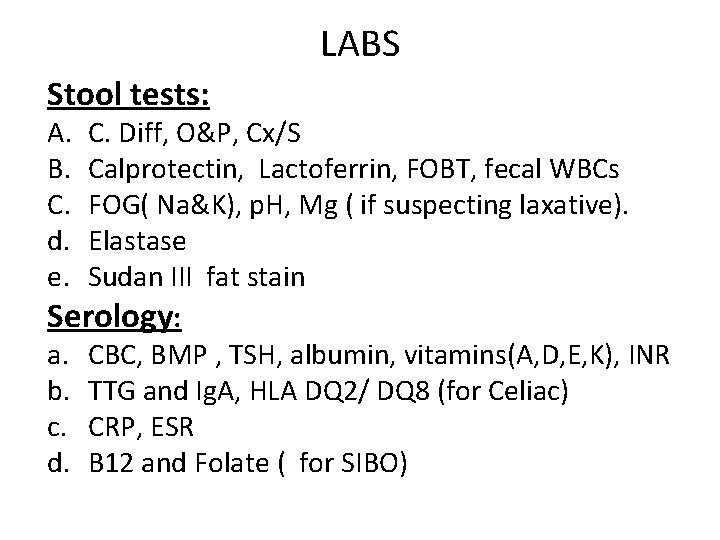
LABS Stool tests: A. B. C. d. e. C. Diff, O&P, Cx/S Calprotectin, Lactoferrin, FOBT, fecal WBCs FOG( Na&K), p. H, Mg ( if suspecting laxative). Elastase Sudan III fat stain Serology: a. CBC, BMP , TSH, albumin, vitamins(A, D, E, K), INR b. TTG and Ig. A, HLA DQ 2/ DQ 8 (for Celiac) c. CRP, ESR d. B 12 and Folate ( for SIBO)
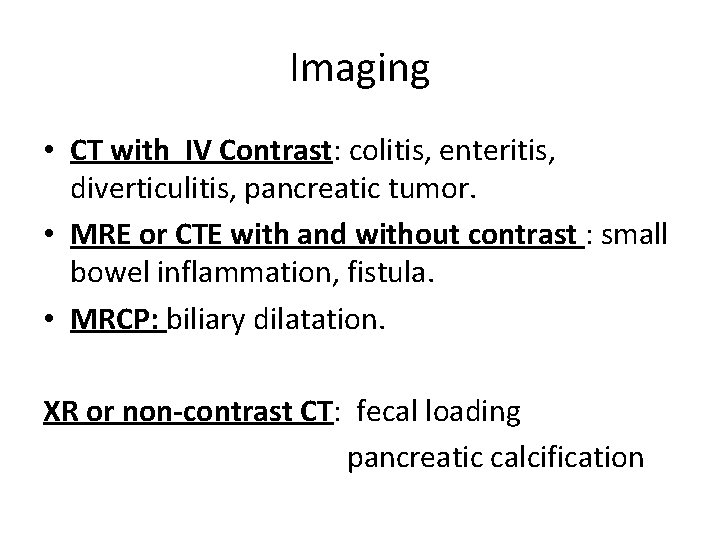
Imaging • CT with IV Contrast: colitis, enteritis, diverticulitis, pancreatic tumor. • MRE or CTE with and without contrast : small bowel inflammation, fistula. • MRCP: biliary dilatation. XR or non-contrast CT: fecal loading pancreatic calcification
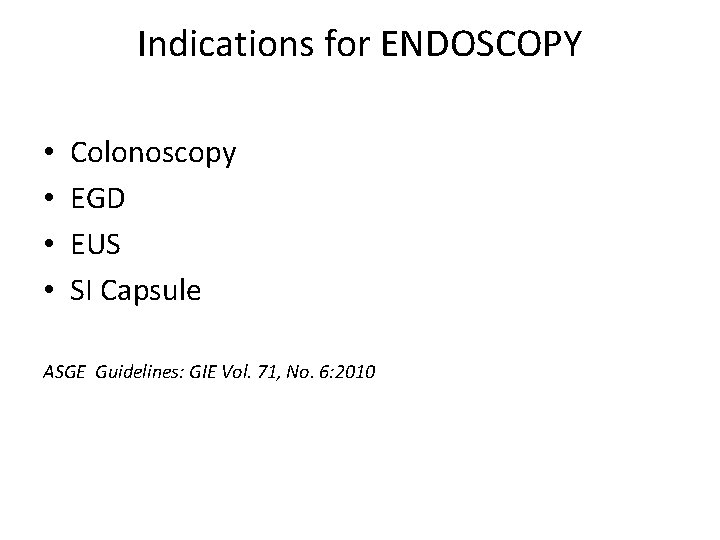
Indications for ENDOSCOPY • • Colonoscopy EGD EUS SI Capsule ASGE Guidelines: GIE Vol. 71, No. 6: 2010
Colonoscopy • If mucus, blood, copious watery • If suspect: IBD, microscopic, serrated villous adenoma, cancer, NSAID ileitis/colitis, eosinophilic colitis. • Flexible Sigmoidoscopy : suspect distal viral or ischemia when full colon is high-risk ASGE Guidelines: GIE Vol. 71, No. 6: 2010
EGD/EUS • • Giardia Gastric ulcers ZES Celiac SI Crohns Lymphangectasia Lymphoma ASGE Guidelines: GIE Vol. 71, No. 6: 2010
Small Bowel Capsule • If colonoscopy and EGD normal and suspect small bowel source for inflammation • CT and MRI may not show mucosal lesion or bleeding ASGE Guidelines: GIE Vol. 71, No. 6: 2010
CASE #1: MICROSCOPIC COLITIS • 11/2015: 30 yo female presents with chronic alcohol abuse, severe neuropathy, large ascites. • She reports history of Crohns diagnosed at 26 yo. Had diarrhea and colonoscopy in 2012. Tried Lialda but stopped medication. Now reports 2 BM per day. • Treated for cirrhosis and discharged to Acute Rehab for severe neuropathy.
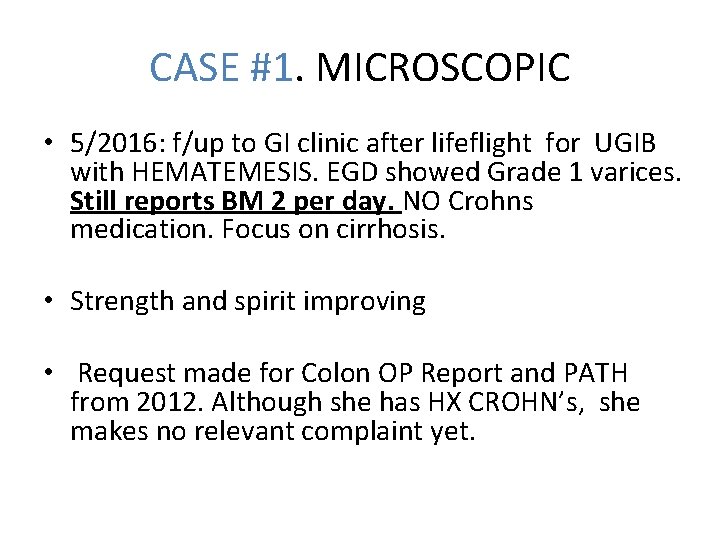
CASE #1. MICROSCOPIC • 5/2016: f/up to GI clinic after lifeflight for UGIB with HEMATEMESIS. EGD showed Grade 1 varices. Still reports BM 2 per day. NO Crohns medication. Focus on cirrhosis. • Strength and spirit improving • Request made for Colon OP Report and PATH from 2012. Although she has HX CROHN’s, she makes no relevant complaint yet.
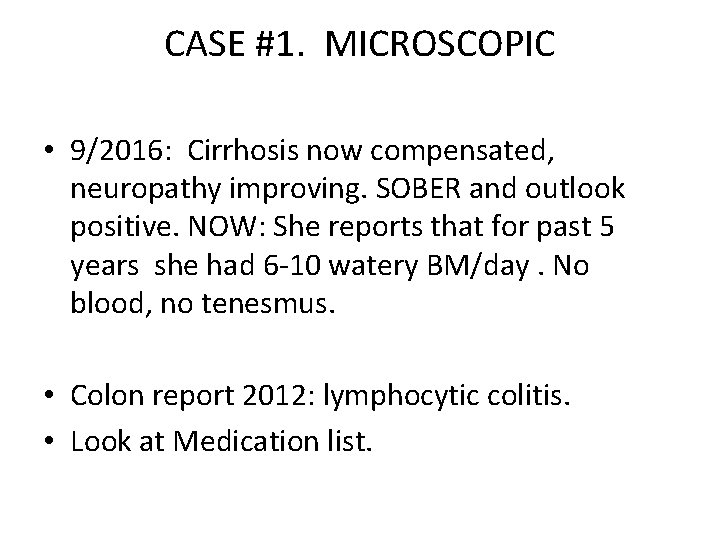
CASE #1. MICROSCOPIC • 9/2016: Cirrhosis now compensated, neuropathy improving. SOBER and outlook positive. NOW: She reports that for past 5 years she had 6 -10 watery BM/day. No blood, no tenesmus. • Colon report 2012: lymphocytic colitis. • Look at Medication list.
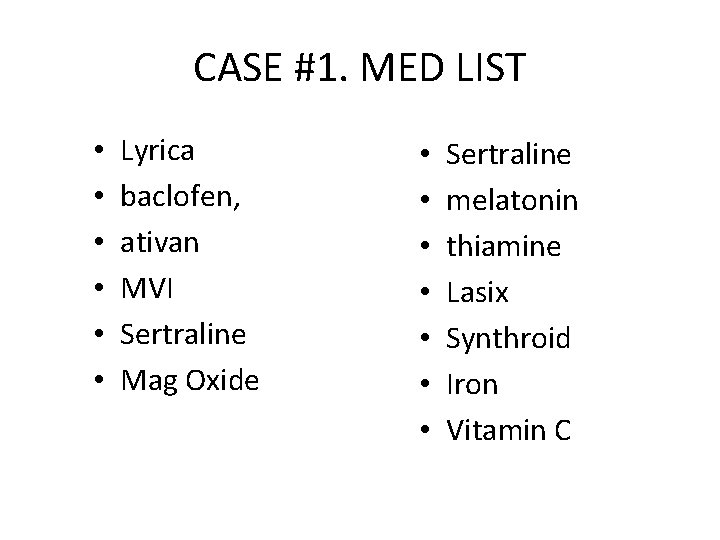
CASE #1. MED LIST • • • Lyrica baclofen, ativan MVI Sertraline Mag Oxide • • Sertraline melatonin thiamine Lasix Synthroid Iron Vitamin C
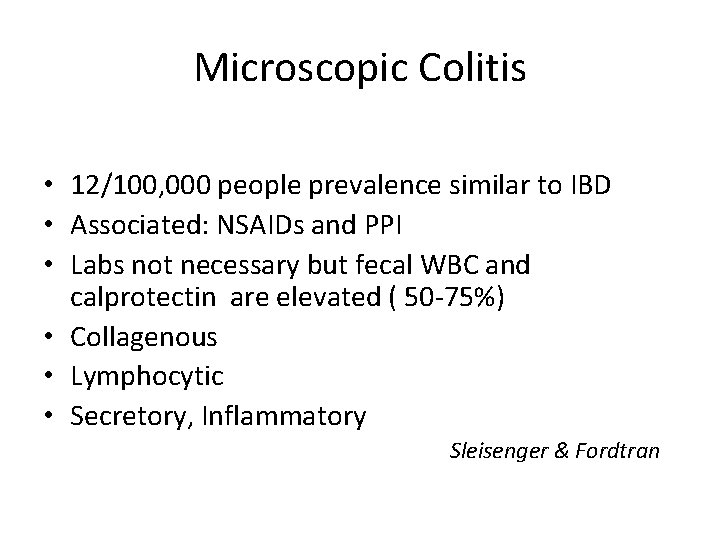
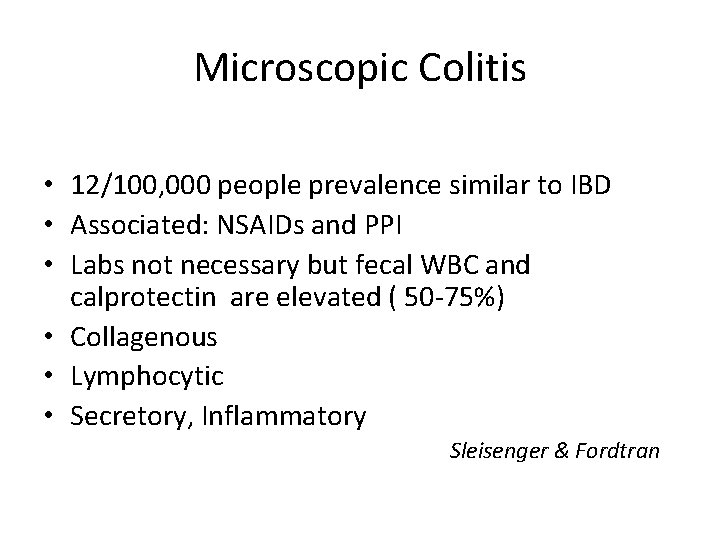
Microscopic Colitis • 12/100, 000 people prevalence similar to IBD • Associated: NSAIDs and PPI • Labs not necessary but fecal WBC and calprotectin are elevated ( 50 -75%) • Collagenous • Lymphocytic • Secretory, Inflammatory Sleisenger & Fordtran
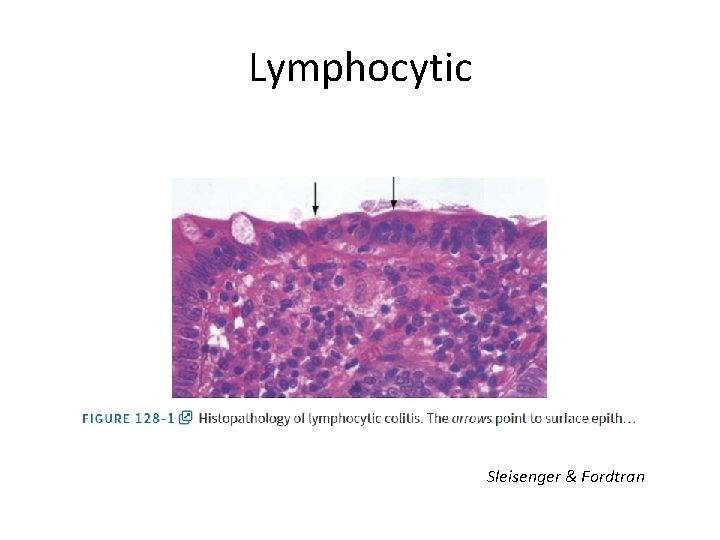
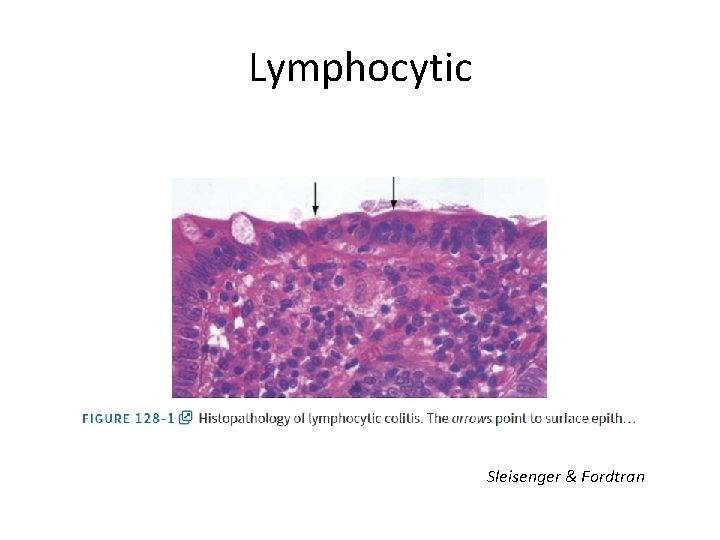
Lymphocytic Sleisenger & Fordtran
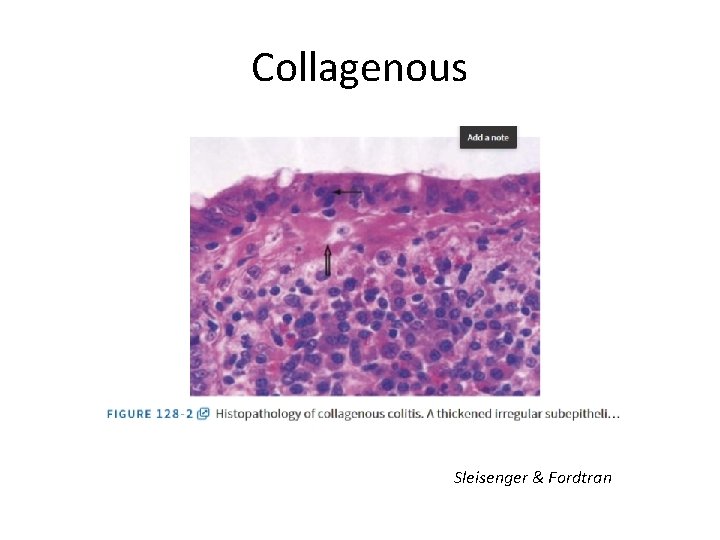
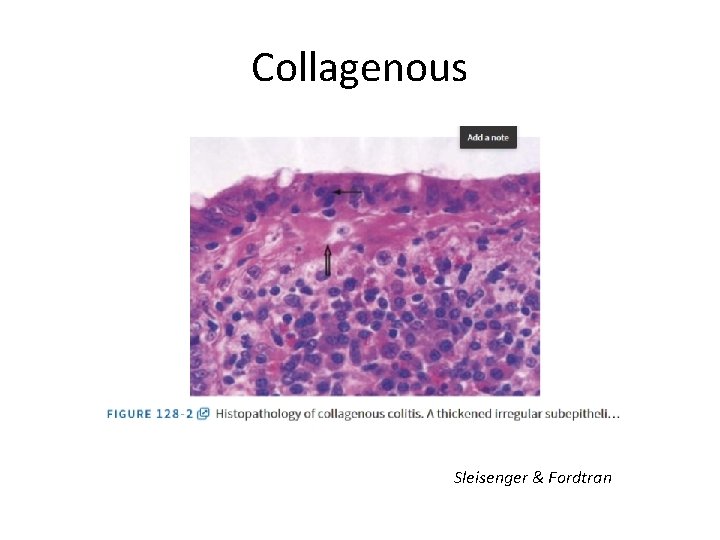
Collagenous Sleisenger & Fordtran
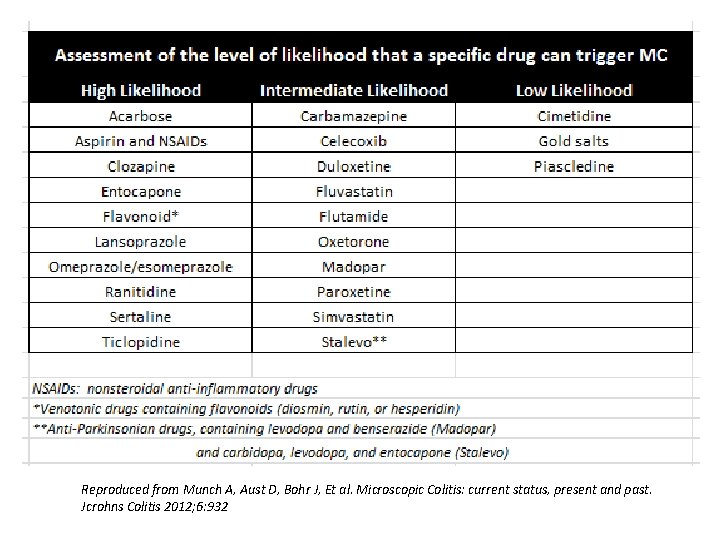
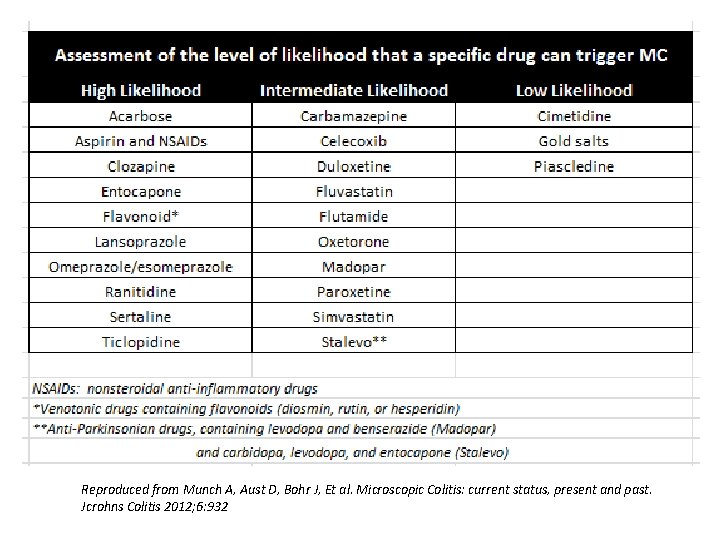
Reproduced from Munch A, Aust D, Bohr J, Et al. Microscopic Colitis: current status, present and past. Jcrohns Colitis 2012; 6: 932
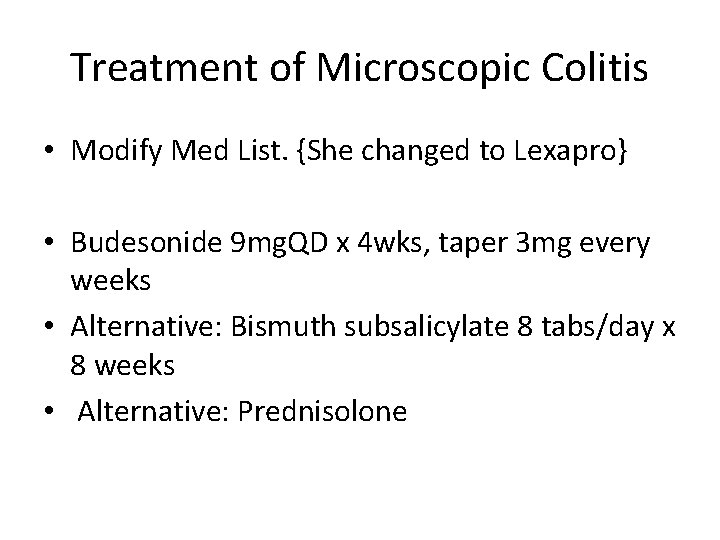
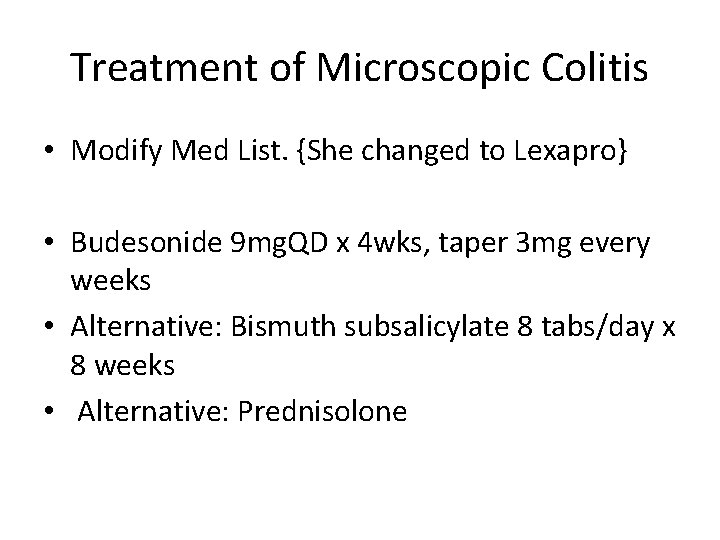
Treatment of Microscopic Colitis • Modify Med List. {She changed to Lexapro} • Budesonide 9 mg. QD x 4 wks, taper 3 mg every weeks • Alternative: Bismuth subsalicylate 8 tabs/day x 8 weeks • Alternative: Prednisolone
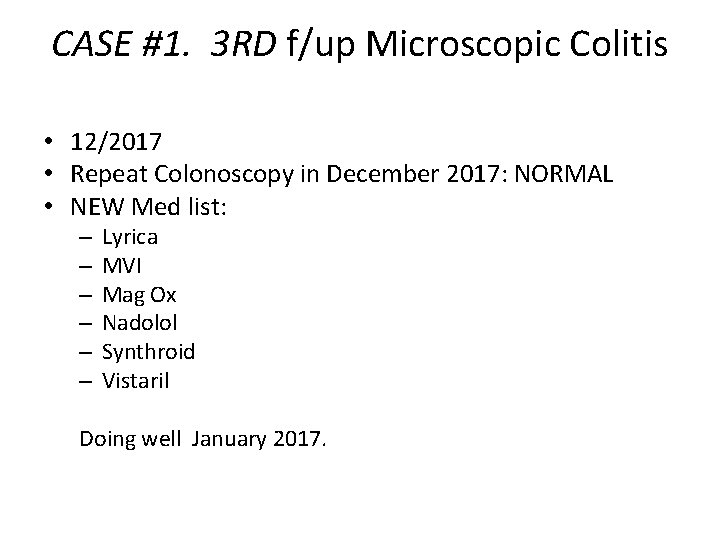
CASE #1. 3 RD f/up Microscopic Colitis • 12/2017 • Repeat Colonoscopy in December 2017: NORMAL • NEW Med list: – – – Lyrica MVI Mag Ox Nadolol Synthroid Vistaril Doing well January 2017.
CASE #1. Microscopic Colitis can recur. OK to retreat empirically without scope but 1 st check Stool tests for infection, and blood for ESR/CRP.
CASE# 2: SIBO • 19 yo female from NH going to college in ME, active as rock climber and backcountry pursuits presents with HX diarrhea past 2 years. 4 -6 per day but some days>10 per day. • Brown, watery or mushy, not greasy, No blood. Weight stable. • Frequent bloating, nausea, and occasional bilious vomit. • MED: lexapro • FM HX: Mom has IBS-C.
CASE #2: SIBO • PCP at NH did CRP, ESR, TTG/Ig. A, Stool Cx, O&P, RUQ SONO, XRAY. • Patient tried Lactose-Gluten Free, Elavil, Bentyl. • Vitamin D level normal 28, Albumin 4. 9, Calprotectin<50. • We did a COLON and EGD: normal. • HBT : both CH 4 and H 2 both increase>20 ppm
CASE # 2: SIBO • DX: SIBO with mixed CH 4 and H 2 production • Treat: Flagyl / Keflex each 500 mg PO TID 7 -10 days. Per Upto. Date • Use low SIBO diet • Refer to Dietician
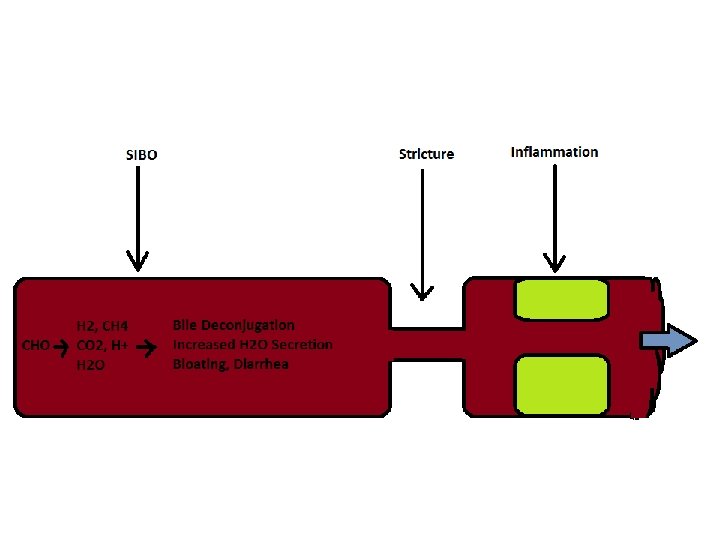
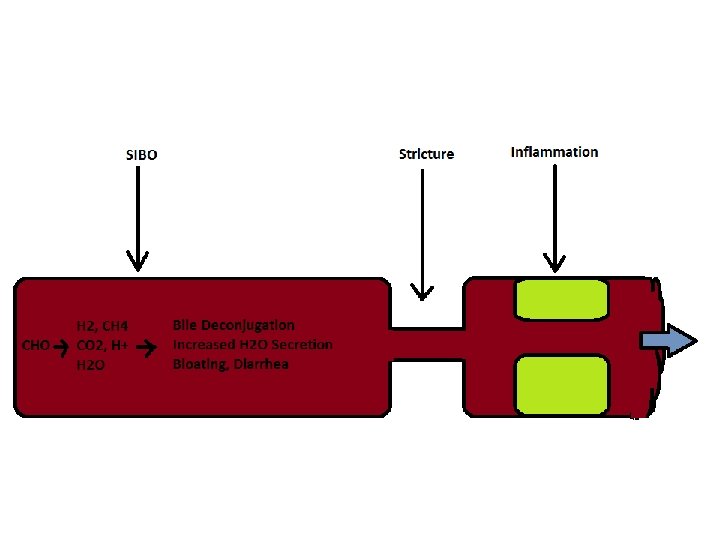
SIBO 1. Intestinal Stasis, scleroderma, gastroparesis, DM, Ileocecal Valve resection, Enteroenteric Fistula, Stricture from radiation, IBD, Stenosis from ischemia or inflammation. 2. Bacteria consume nutrients>> low B 12, high Folate>> increase H 2/CH 4>> bloating and diarrhea Dr. Ali Rezaie, Curr. GI Reports, SIBO , (2016)18. 8.
Hydrogen Breath Testing: ingest tracer-food, bacteria convert to H 2 and CH 4 which are absorbed into blood, go to lungs, exhaled. If more than 20 ppm increase, it shows SIBO. Dr. Ali Rezaie, Curr. GI Reports, SIBO , (2016)18. 8.
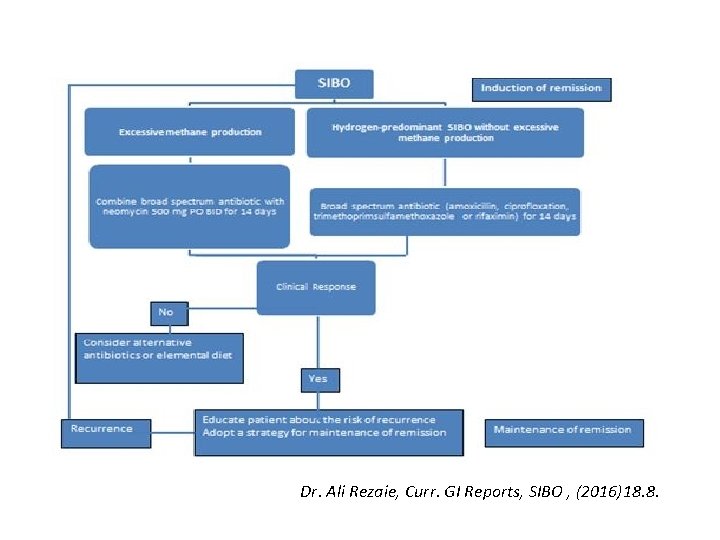
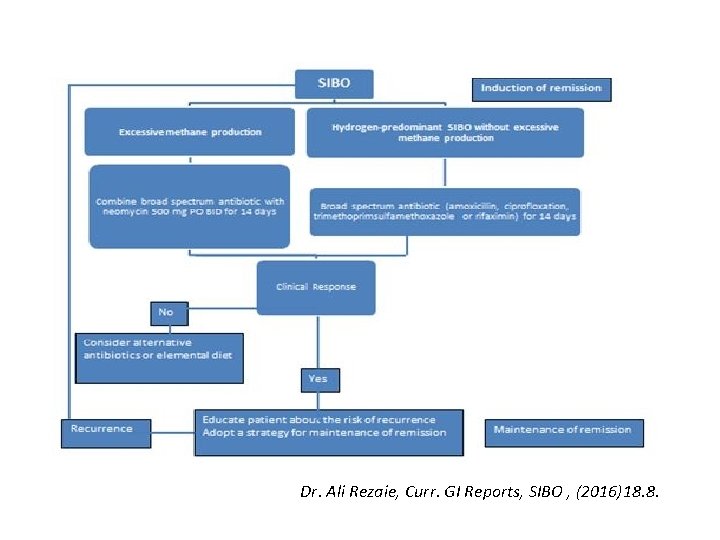
Dr. Ali Rezaie, Curr. GI Reports, SIBO , (2016)18. 8.
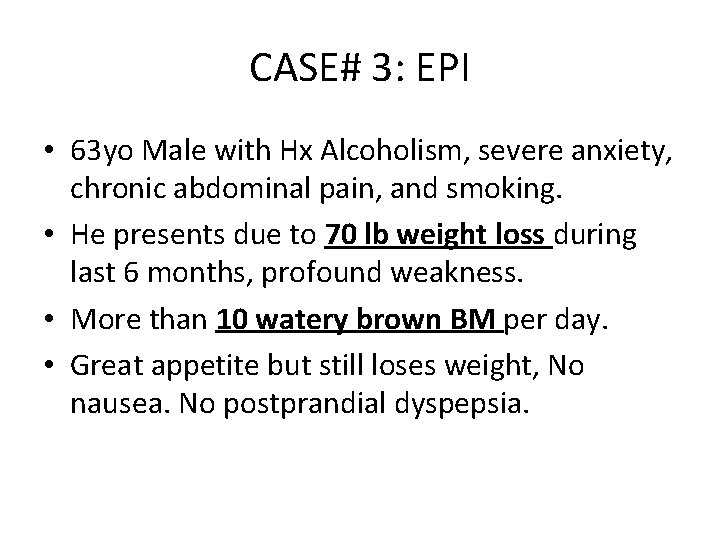
CASE# 3: EPI • 63 yo Male with Hx Alcoholism, severe anxiety, chronic abdominal pain, and smoking. • He presents due to 70 lb weight loss during last 6 months, profound weakness. • More than 10 watery brown BM per day. • Great appetite but still loses weight, No nausea. No postprandial dyspepsia.
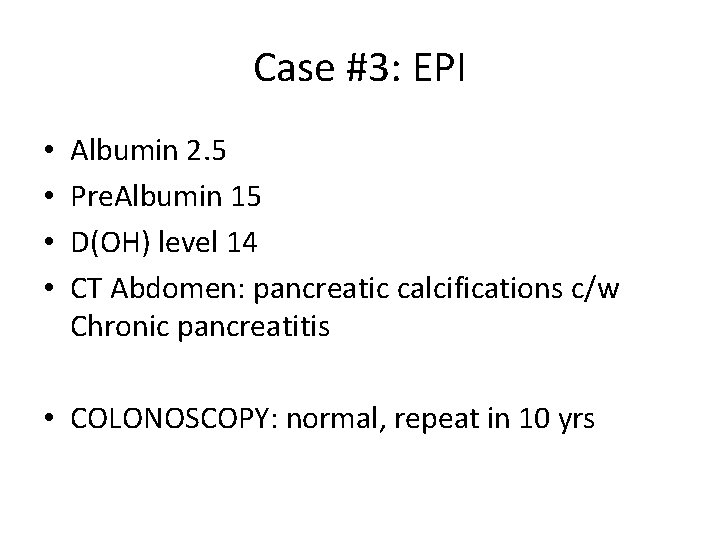
Case #3: EPI • • Albumin 2. 5 Pre. Albumin 15 D(OH) level 14 CT Abdomen: pancreatic calcifications c/w Chronic pancreatitis • COLONOSCOPY: normal, repeat in 10 yrs
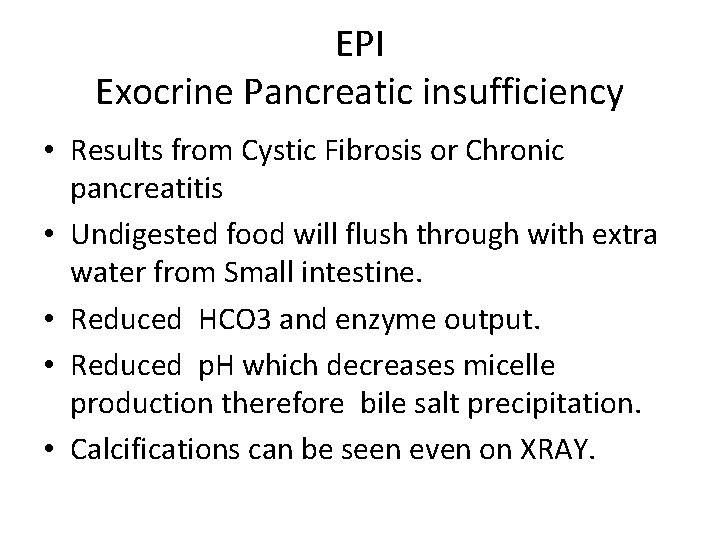
EPI Exocrine Pancreatic insufficiency • Results from Cystic Fibrosis or Chronic pancreatitis • Undigested food will flush through with extra water from Small intestine. • Reduced HCO 3 and enzyme output. • Reduced p. H which decreases micelle production therefore bile salt precipitation. • Calcifications can be seen even on XRAY.

CASE # 3: EPI • Weight-based pancrease enzymes started • No testing for Fecal elastase done • Vitamin D ordered 50, 000 IU PO weekly 10 weeks • F/up 8 weeks after hospital: 20 lb. weight gain, BM now 2 -3 per day and formed. Less fatigue. • Working on Anxiety • REMEMBER to adjust ENZYME DOSE to weights
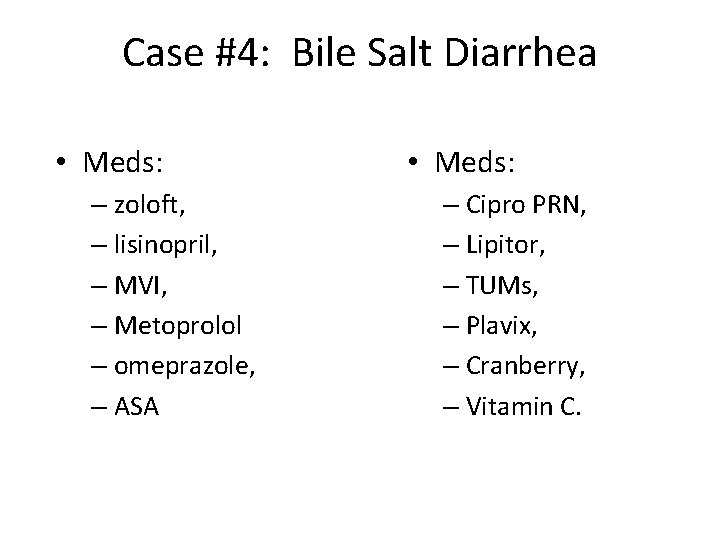
Case #4: Bile Salt Diarrhea • 76 yo female yellow explosive liquid 6 -10 BM/day for years. • Frequent UTI and tinea cruris • Hx CCy, Nissen, GERD, CAD
Case #4: Bile Salt Diarrhea • Meds: – zoloft, – lisinopril, – MVI, – Metoprolol – omeprazole, – ASA • Meds: – Cipro PRN, – Lipitor, – TUMs, – Plavix, – Cranberry, – Vitamin C.

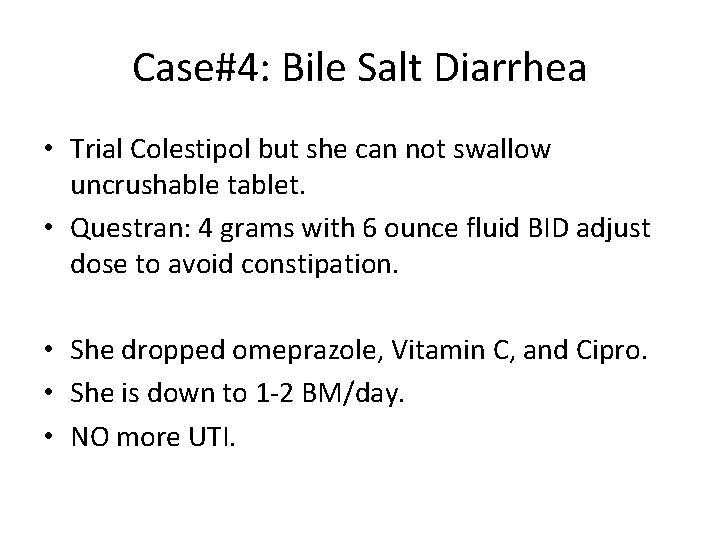
Case#4: Bile Salt Diarrhea • Trial Colestipol but she can not swallow uncrushable tablet. • Questran: 4 grams with 6 ounce fluid BID adjust dose to avoid constipation. • She dropped omeprazole, Vitamin C, and Cipro. • She is down to 1 -2 BM/day. • NO more UTI.
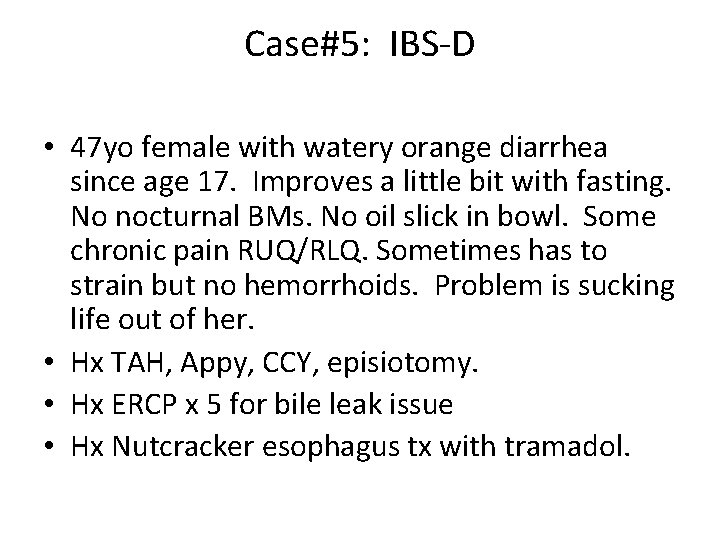
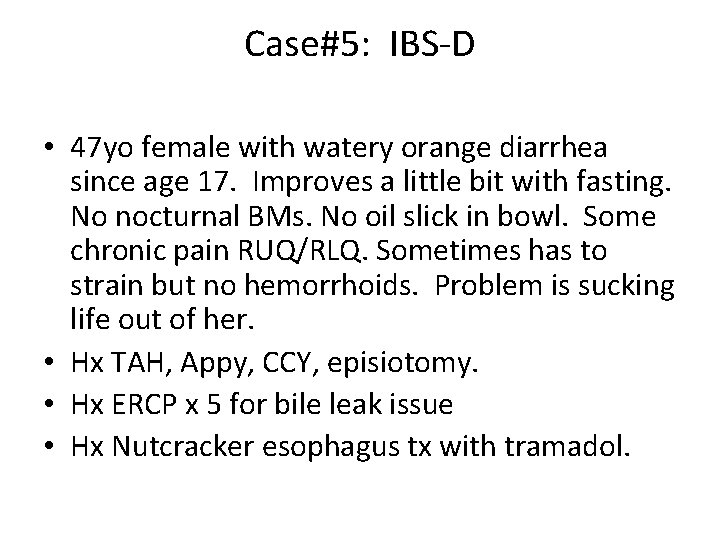
Case#5: IBS-D • 47 yo female with watery orange diarrhea since age 17. Improves a little bit with fasting. No nocturnal BMs. No oil slick in bowl. Some chronic pain RUQ/RLQ. Sometimes has to strain but no hemorrhoids. Problem is sucking life out of her. • Hx TAH, Appy, CCY, episiotomy. • Hx ERCP x 5 for bile leak issue • Hx Nutcracker esophagus tx with tramadol.
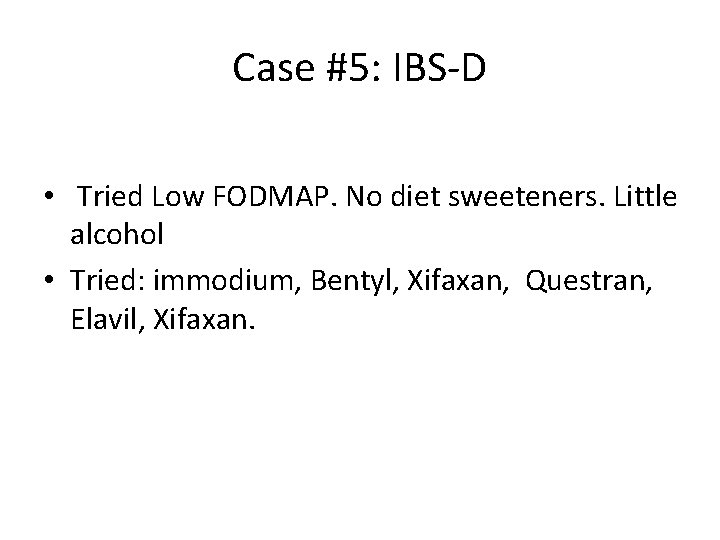
Case #5: IBS-D • Tried Low FODMAP. No diet sweeteners. Little alcohol • Tried: immodium, Bentyl, Xifaxan, Questran, Elavil, Xifaxan.
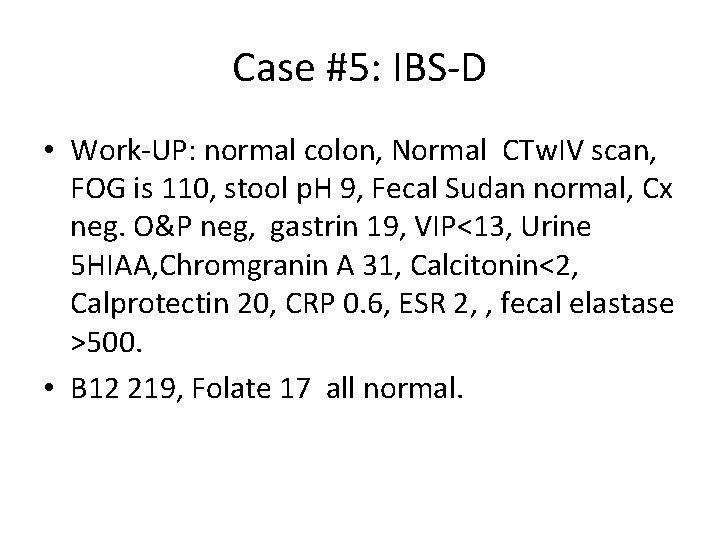
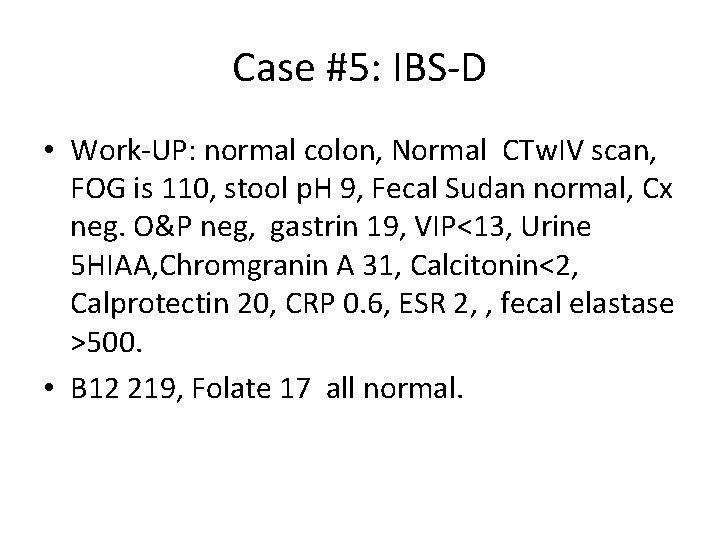
Case #5: IBS-D • Work-UP: normal colon, Normal CTw. IV scan, FOG is 110, stool p. H 9, Fecal Sudan normal, Cx neg. O&P neg, gastrin 19, VIP<13, Urine 5 HIAA, Chromgranin A 31, Calcitonin<2, Calprotectin 20, CRP 0. 6, ESR 2, , fecal elastase >500. • B 12 219, Folate 17 all normal.
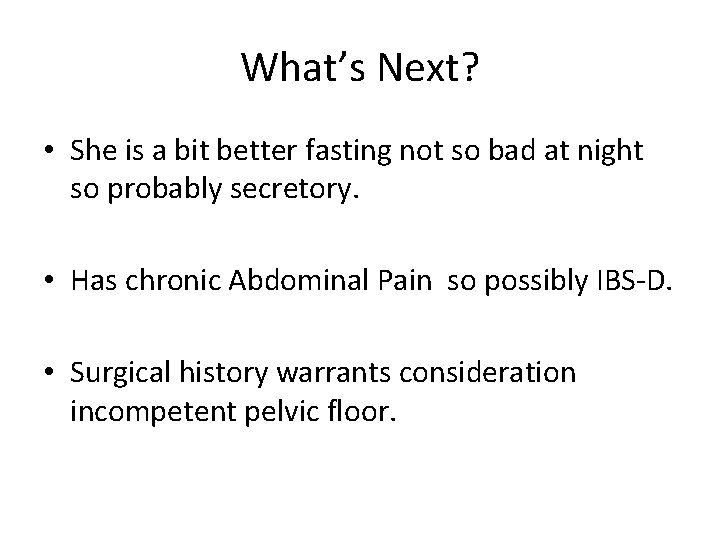
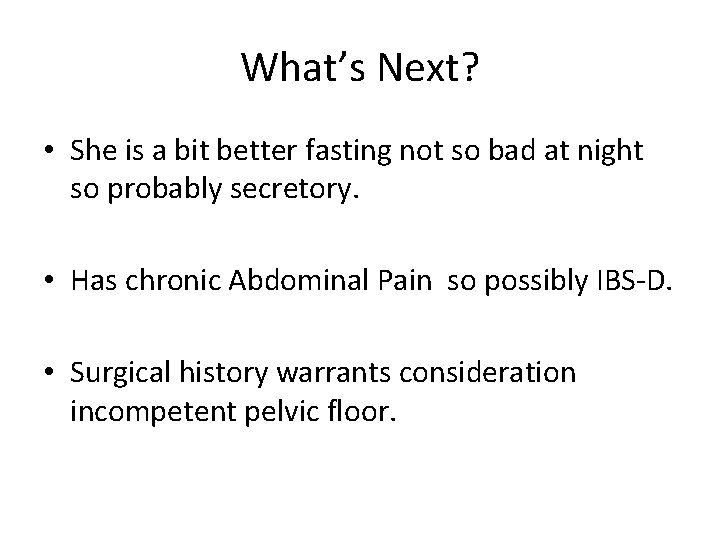
What’s Next? • She is a bit better fasting not so bad at night so probably secretory. • Has chronic Abdominal Pain so possibly IBS-D. • Surgical history warrants consideration incompetent pelvic floor.

Case #5: IBS-D • Eluxodoline 75 mg q HS, normal dose 75 mg BID. Hold dose on days you have alcohol. This can titrate to 100 mg BID, see contraindications. Updated 3/2017, do not use if no gallbladder. • RESULT: problem resolved. 2 BM/day. • Explanation: IBS-D with abdominal pain.
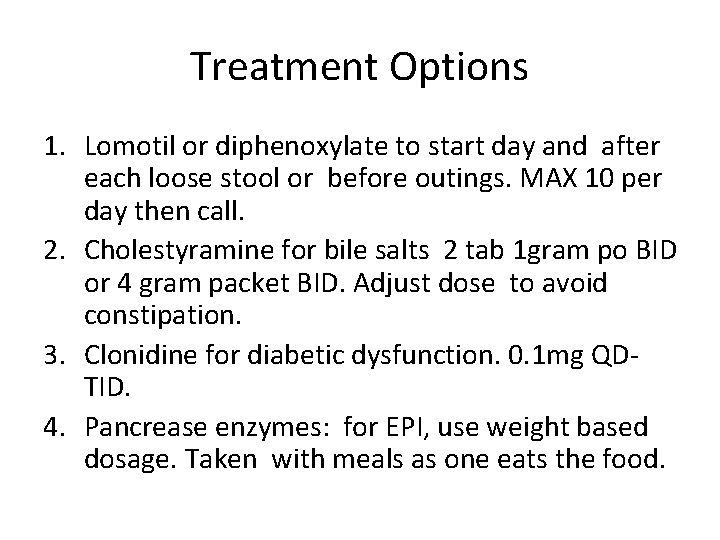
Treatment Options 1. Lomotil or diphenoxylate to start day and after each loose stool or before outings. MAX 10 per day then call. 2. Cholestyramine for bile salts 2 tab 1 gram po BID or 4 gram packet BID. Adjust dose to avoid constipation. 3. Clonidine for diabetic dysfunction. 0. 1 mg QDTID. 4. Pancrease enzymes: for EPI, use weight based dosage. Taken with meals as one eats the food.
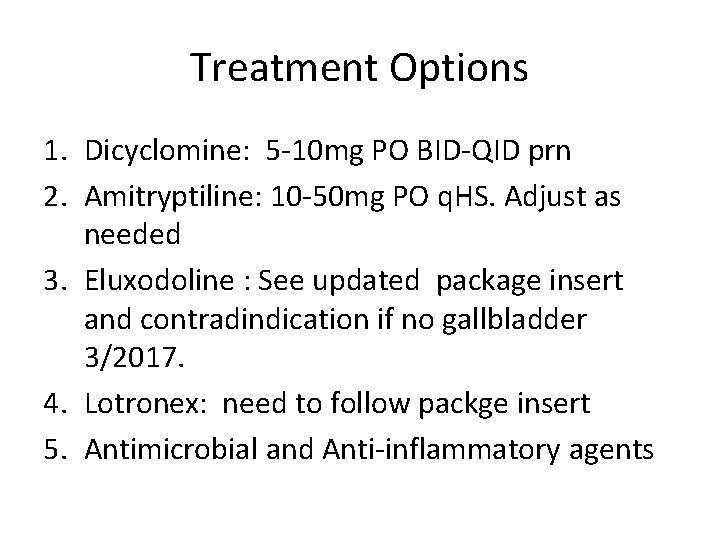
Treatment Options 1. Dicyclomine: 5 -10 mg PO BID-QID prn 2. Amitryptiline: 10 -50 mg PO q. HS. Adjust as needed 3. Eluxodoline : See updated package insert and contradindication if no gallbladder 3/2017. 4. Lotronex: need to follow packge insert 5. Antimicrobial and Anti-inflammatory agents
References 1. Dr. L. Schiller, MD. AGA DDSEP 8 Chapter 9, Diarrhea. 2. Dr. Schiller, MD. , Dr. JH Sellin, MD. Chapter 16: Sleisenger & Fordtran’s Gastrointestinal and Liver Diseases, Pathology, Diagnosis, Treatment. 10 th edition. 3. ASGE guidelines. Journal GIE 2010 vol 71, No. 6: 2010. 4. Dr. Ali Rezaie, Curr. GI Reports, SIBO , (2016)18. 8.
TAKE HOME • Diarrhea is really a symptom. We need find diagnosis for the chronic diarrhea.
 Zoloft and microscopic colitis
Zoloft and microscopic colitis Chronic diarrhea
Chronic diarrhea Dr ali azzam
Dr ali azzam Angela harkins dentist
Angela harkins dentist Michelle harkins
Michelle harkins Michelle harkins
Michelle harkins Imnci colour coding
Imnci colour coding Nicholas seeliger
Nicholas seeliger Secretory diarrhea pathophysiology
Secretory diarrhea pathophysiology Cervical spine reflexology
Cervical spine reflexology Radwan
Radwan What is bile acid diarrhea
What is bile acid diarrhea Types of diarrhoea
Types of diarrhoea Plan b of dehydration management
Plan b of dehydration management Zinc for diarrhea
Zinc for diarrhea Osmotic diarrhea meaning
Osmotic diarrhea meaning Pig diarrhea chart
Pig diarrhea chart Overflow diarrhea
Overflow diarrhea Diarrhea
Diarrhea Liemyosarcoma
Liemyosarcoma Hiv stool color
Hiv stool color Diarrhea chief complaint
Diarrhea chief complaint Diarrhea
Diarrhea Diarrhea
Diarrhea Travelers diarrhea
Travelers diarrhea Git normal flora
Git normal flora Diarrhea introduction
Diarrhea introduction Optimental formula
Optimental formula Metformin and constipation
Metformin and constipation Factitial diarrhea
Factitial diarrhea Overflow diarrhea
Overflow diarrhea Dan laufenberg
Dan laufenberg Flinders model of chronic care self-management
Flinders model of chronic care self-management Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Who developed the chronic care model
Who developed the chronic care model Nursing management of liver cirrhosis
Nursing management of liver cirrhosis Acute pancreatitis pathophysiology nursing
Acute pancreatitis pathophysiology nursing Chronic pain management irwin
Chronic pain management irwin Differences between acute and chronic inflammation
Differences between acute and chronic inflammation Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Inflammation
Inflammation Leukemia survival rate
Leukemia survival rate Define periradicular disease
Define periradicular disease Knowledge management monitoring and evaluation
Knowledge management monitoring and evaluation Angioectasia icd 10
Angioectasia icd 10 Definition of chronic toxicity
Definition of chronic toxicity Earthy look in chronic renal failure
Earthy look in chronic renal failure Chronic granulomatous disease
Chronic granulomatous disease Chronic care model definition
Chronic care model definition Periapical granuloma vs abscess
Periapical granuloma vs abscess Chronic blood loss
Chronic blood loss Pathogenesis of cholecystitis
Pathogenesis of cholecystitis Fibromyalgia vs chronic fatigue
Fibromyalgia vs chronic fatigue Stigmata of chronic liver disease
Stigmata of chronic liver disease Irreversible pulpitis vs reversible pulpitis
Irreversible pulpitis vs reversible pulpitis Iceberg phenomenon
Iceberg phenomenon Hemolytic anemia symptoms
Hemolytic anemia symptoms Chronic unease safety
Chronic unease safety Pathophysiology of cholelithiasis ppt
Pathophysiology of cholelithiasis ppt Definition of chronic toxicity
Definition of chronic toxicity Chronic blood loss
Chronic blood loss Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Acute subacute chronic
Acute subacute chronic Jewish chronic disease study
Jewish chronic disease study Ersd
Ersd Pigment gallstones causes
Pigment gallstones causes Basic & clinical pharmacology
Basic & clinical pharmacology Chronic blood loss
Chronic blood loss Cld vs dcld
Cld vs dcld Nih score
Nih score Mouse nibbled vocal cord
Mouse nibbled vocal cord Types of gastritis
Types of gastritis Chronic care solutions
Chronic care solutions Peripheral stigmata of cld
Peripheral stigmata of cld Stigmata of chronic liver disease
Stigmata of chronic liver disease