Chronic venous insufficiency Management Chronic venous insufficiency Chronic


- Slides: 22
Chronic venous insufficiency Management
Chronic venous insufficiency * Chronic venous insufficiency (C. V. I. ) encompasses disease of the lower limb veins in which venous return is impaired usually over a number of years of reflux, obstruction or calf muscle pump failure. venous hypertension and ultimately clinical complications oedema, eczema, Lipodermatosclerosis and ulceration.
Aetiology: A- Changes in macrocirculation: During exercise in normal individual, effective contraction of the calf muscles combined with vein patency and valvular competence aids venous return and reduces venous pressure around the lower aspect of the leg from about 90 mm. Hg to 30 mm. Hg. Failure of any of these mechanisms may result in postamubulatory venous hypertension which is the underlying haemodynamic abnormality in C. V. I.
Causes of venous hypertension q Superficial venous reflux (long saphenous or short saphenous vein reflux) q Deep vein reflux (Primary or secondary to deep venous thrombosis) It have reported that reflux in the superficial system is present in approximately 90% of limbs with C. V. I. whereas reflux in the deep system is detected in only 30% of limbs and the prevalence of deep venous reflux in limbs with reflux in the superficial system, is approximately 20%. q Deep venous occlusion. q Perforating vein reflux. q Abnormal calf pump (Neurological/musculoskeletal). q Combination of the above.
B- Changes in microcirculation 1 - Fibrin cuff theory: P widening of the pores between endothelial cells allows the passage of larger molecules out of the intravascular compartment into the tissues. PThis allows the accumulation of fibrin around the capillaries of the dermis to form a cuff which acts as a barrier to oxygen and nutrient diffusion to interstitial tissues and cutaneous skin cells resulting in local tissue ischaemia and cell death which produces ulceration.
2 - White cell trapping theory: P It has been proposed that raised venous pressure reduces the capillary perfusion pressure which in turn causes trapping of white cells. P Venous hypertension results in expression of leukocyte adhesion molecules that permit adherence of leukocytes to the capillary endothelial cells. PThe trapped cells become activated releasing proteolytic enzymes and oxygen free radicals which produce endothelial damage and tissue destruction and local ischaemia.
3 - Growth hormone trapping hypothesis PSuggested that the pericapillary cuffs might interfere with the diffusion of growth factors which are essential for skin and tissue repair. This might well explain why ulcerated or damaged tissue fail to heal.
4 - Cutaneous iron overload: PThe rise in hydrostatic pressure within the capillaries combined with increased permeability leads to extravasations of red blood cells. As they degenerate the iron is released from the haemoglobin and deposited within the dermis and when the amount exceeds the ferritin binding capacity, iron becomes available in its bivalent form that can promote the production of oxygen free radicals and lipid peroxides which in turn can lead to tissue destruction.
5 - Other possible changes: óArteriovenous shunting. óDecreased response of dermal fibroblasts to cytokines and growth factors associated with normal wound healing. óCapillary microthrombosis. óDecreased number of collecting lymphatic channels and disruption of lymphatic network. óOveractivation of venoarteriolar reflex resulting in microvascular vasoconstriction in response to venous pressure above 25 mm. Hg. Normally this reflux is abolished by activation of calf muscle pump and reduction in venous pressure.
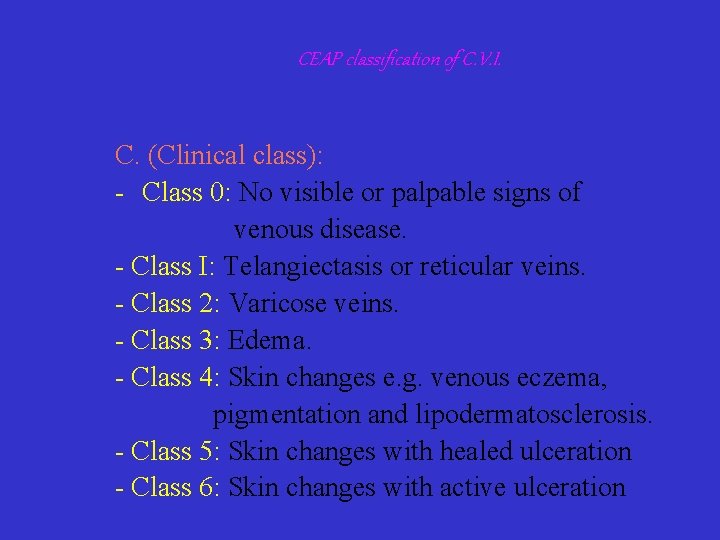
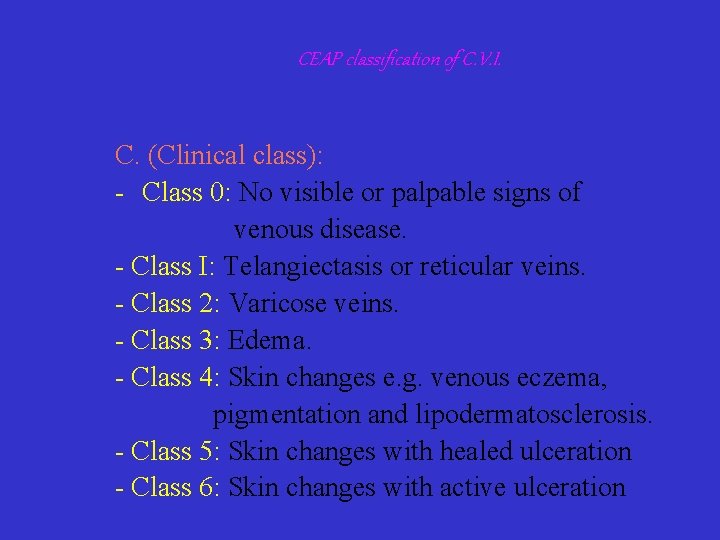
CEAP classification of C. V. I. C. (Clinical class): Class 0: No visible or palpable signs of venous disease. Class I: Telangiectasis or reticular veins. Class 2: Varicose veins. Class 3: Edema. Class 4: Skin changes e. g. venous eczema, pigmentation and lipodermatosclerosis. Class 5: Skin changes with healed ulceration Class 6: Skin changes with active ulceration
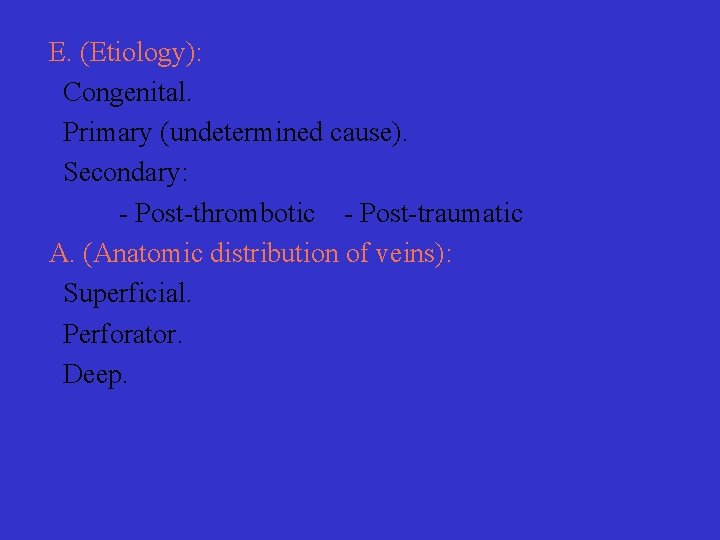
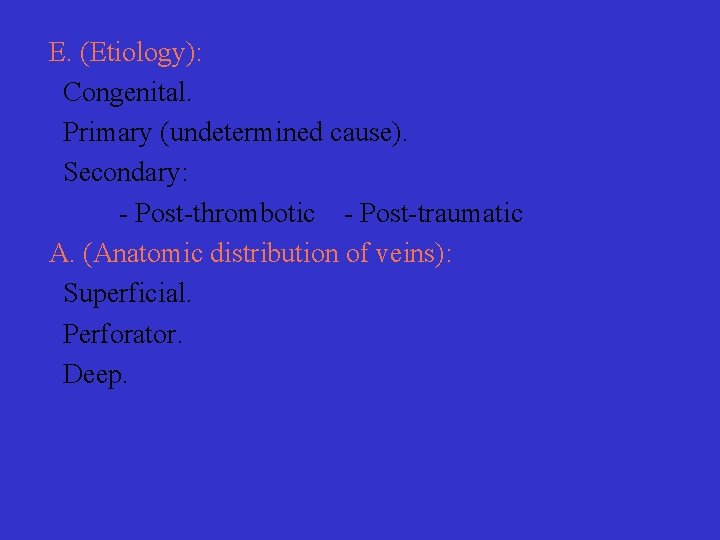
E. (Etiology): Congenital. Primary (undetermined cause). Secondary: Post thrombotic Post traumatic A. (Anatomic distribution of veins): Superficial. Perforator. Deep.
P. (Pathophysiologic mechanism): Reflux. Obstruction. Reflux and obstruction.
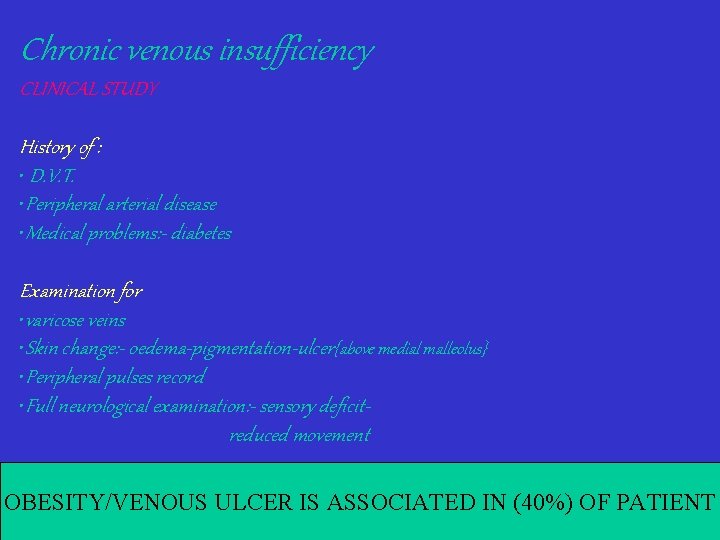
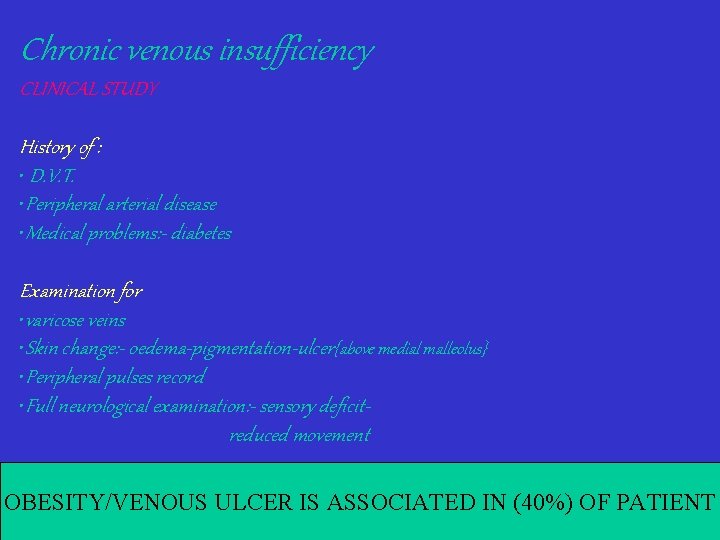
Chronic venous insufficiency CLINICAL STUDY History of : • D. V. T. • Peripheral arterial disease • Medical problems: - diabetes Examination for • varicose veins • Skin change: - oedema-pigmentation-ulcer{above medial malleolus} • Peripheral pulses record • Full neurological examination: - sensory deficitreduced movement OBESITY/VENOUS ULCER IS ASSOCIATED IN (40%) OF PATIENT
Chronic venous insufficiency INVESTIGATION Non-invasive Duplex scanning Phlebography Descending Ascending

Treatment Conservative treatment: 1 - Elevation of the legs at rest helps to reduce oedema, decrease exudates from ulcers and accelerate regression of skin changes. 2 - Graduated elastic compression which is highest at the ankle and decreases proximally
3 - Dressings: The commonest topical ulcer dressings include hydrocolloids (e. g. dermasorb), Hydrogels (e. g. Geliperm), Alginates (e. g. Kaltostat), synthetic foams (e. g. lyofoam), capillary and osmotic absorbants (e. g. debrisan) and polyurethane sheets (e. g. opsite).
4 - Systemic medications to promote healing: Zinc: Improves ulcer healing in patients with low serum zinc level. Stanozolol (Stromba) This fibrinolytic enhancing agent has been used in the treatment of pre ulcerative lipodermatosclerosis Pentoxyfylline (Trental Oxyrutosides (Paroven) It reduces capillary permeability and white blood cell migration and improve tissue oxygenation. Free radical scavengers Using either allopurinol or dimethyl sulfoxide Others: Prostaglandin E l. Diuretics. Aspirin.

Surgical Treatment I) Superficial venous surgery. II) Perforating vein surgery. III) Deep venous reconstruction.
A Venous incompetence 1 Valvuloplasty: * Internal valvuloplasty involving suturing the edge of the valve cusp close to the vein wall in order to tighten it. * External valvuloplasty involving suturing of valve cusps at the line of insertion into the vein wall in order to tighten floppy edges without vein opening. 2 Valve transposition: * Involves dividing the incompetent vein e. g. superficial femoral and reinserting it end to side or end to end into a neighboring vein e. g. profunda femoris or long saphenous vein. 3 Valve transplantation: * Involves removing a segment of brachial or axillary vein containing one or more competent valves and reinserting it into the popliteal or femoral vein.
4 External support of vein wall by a Dacron cuff: * To support an incompetent valve thereby making it competent. 5 Reducing the venous diameter in the region of an incompetent valve: * By removing a triangle of vein wall above the valve.
B Venous outflow obstruction Following deep venous thrombosis there may be failure in recanalization leaving a functional venous outflow obstruction. 1 Femorofemoral cross over graft for iliac obstruction: The long saphenous vein on the unaffected is sutured to a suitable vein in the groin on the affected side which may be the common femoral, the superficial femoral or even the long saphenous vein. 2 Saphenopopliteal bypass: In patients with outflow obstruction due to stenosed or occluded deep thigh veins using the long saphenous vein as a bypass channel. The long saphenous vein is divided below the knee and is sutured end to side to the popliteal vein or one of the tibial veins
IV) Skin grafting: It is done after treatment of underlying venous abnormality and preparation of the ulcer removing all the slough and necrotic tissue. It will reduce the healing time. 1 Split skin mesh grafts. 2 Pinch grafts. 3 Full thickness skin grafts. V) Flaps: When a patient has had repeated ulcers which have irreparably damaged the skin and subcutaneous tissues which are scarred and avascular. * Cross leg fasciocutaneous flaps. * Vascularized free fasciocutaneous flaps.
 Trendelenburg test
Trendelenburg test Convergence insufficiency latham
Convergence insufficiency latham Types of muscle contraction
Types of muscle contraction Passive insufficiency
Passive insufficiency Eye lesions
Eye lesions Pseudo convergence insufficiency
Pseudo convergence insufficiency Esodeviation
Esodeviation Canine exocrine pancreatic insufficiency
Canine exocrine pancreatic insufficiency Flinders model of chronic care self-management
Flinders model of chronic care self-management Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Wagner chronic care model
Wagner chronic care model Stages of cirrhosis of the liver
Stages of cirrhosis of the liver Pancreatitis nursing management
Pancreatitis nursing management Thoracic facet joint pain referral patterns
Thoracic facet joint pain referral patterns Axillary lymph nodes
Axillary lymph nodes Lymph nodes lower body
Lymph nodes lower body Humeral nutrient artery
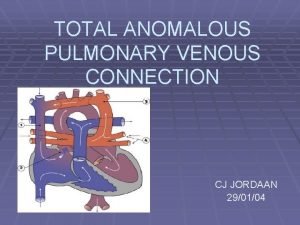
Humeral nutrient artery Tapvc
Tapvc Lateral venous lacunae
Lateral venous lacunae Veins in the chest
Veins in the chest Precapillary resistance
Precapillary resistance Scalp definition
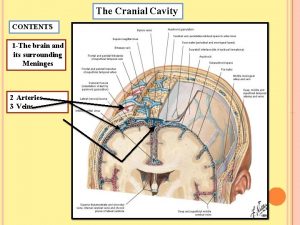
Scalp definition Pituitary gland nerve supply
Pituitary gland nerve supply