Adrenal Insufficiency HALEY MINNEHAN MD Adrenal Insufficiency Definition



- Slides: 38
Adrenal Insufficiency HALEY MINNEHAN, MD
Adrenal Insufficiency Definition A disease state that is caused by lack of glucocorticoids(GC) and/or mineralcorticoids (MC) by interruption at any level of the hypothalamus-pituitary-adrenal axis.
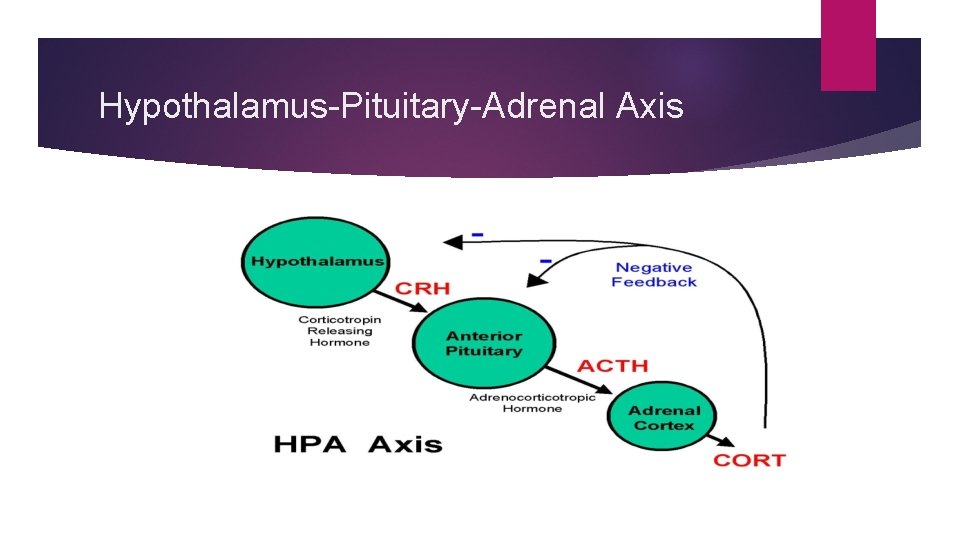
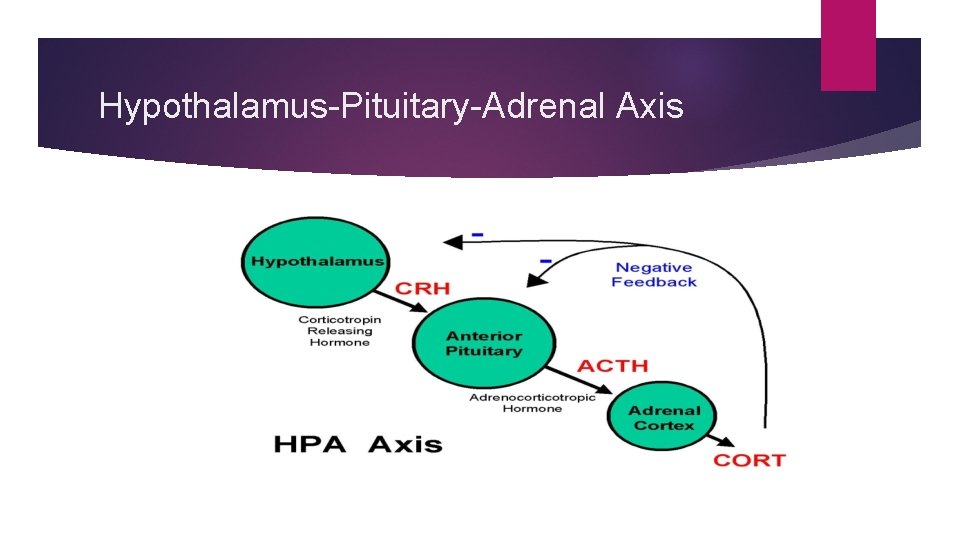
Hypothalamus-Pituitary-Adrenal Axis
Adrenal Insufficiency Primary? Secondary? Tertiary?
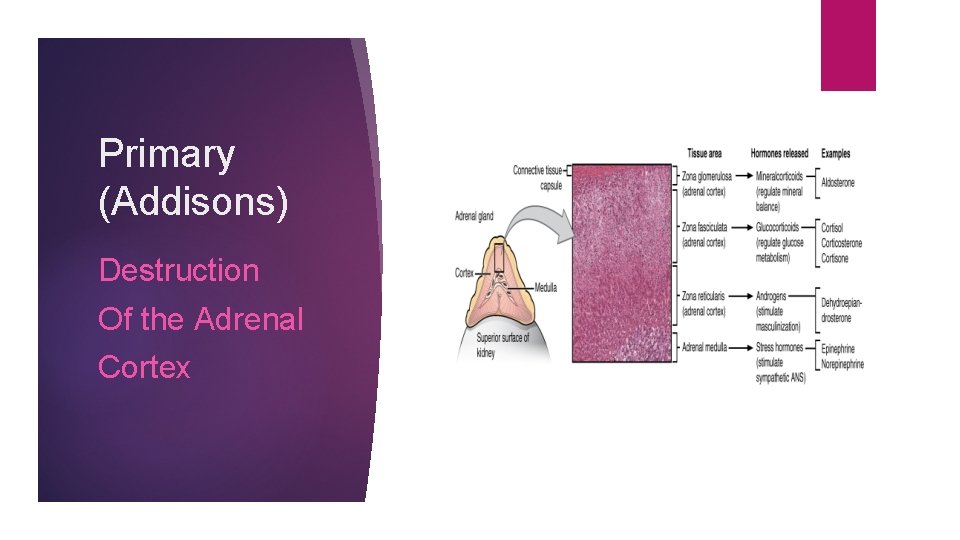
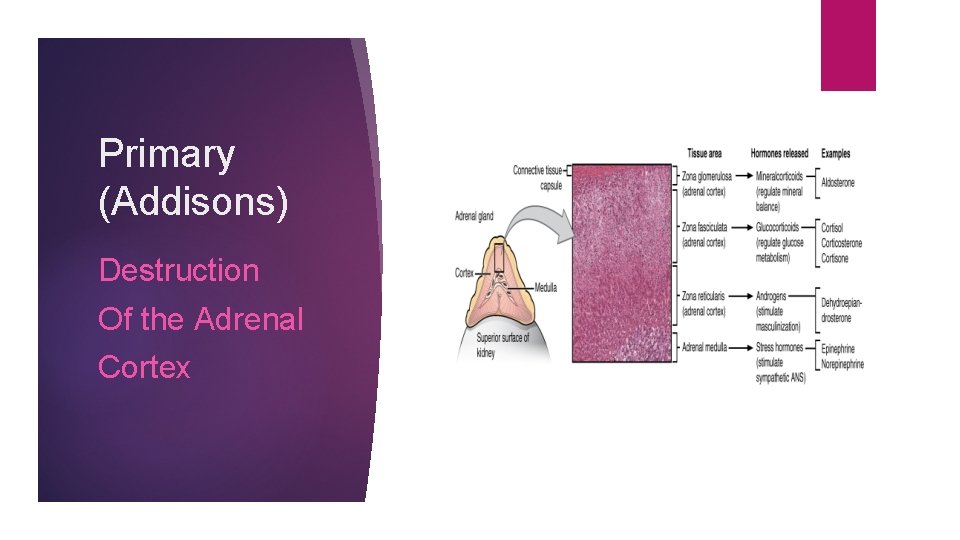
Primary (Addisons) Destruction Of the Adrenal Cortex
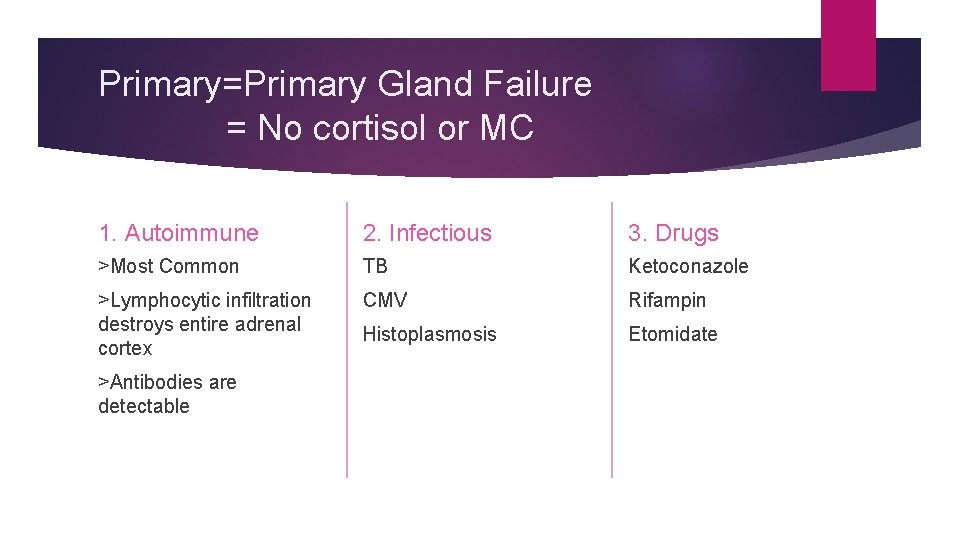
Primary=Primary Gland Failure = No cortisol or MC 1. Autoimmune 2. Infectious 3. Drugs >Most Common TB Ketoconazole >Lymphocytic infiltration destroys entire adrenal cortex CMV Rifampin Histoplasmosis Etomidate >Antibodies are detectable
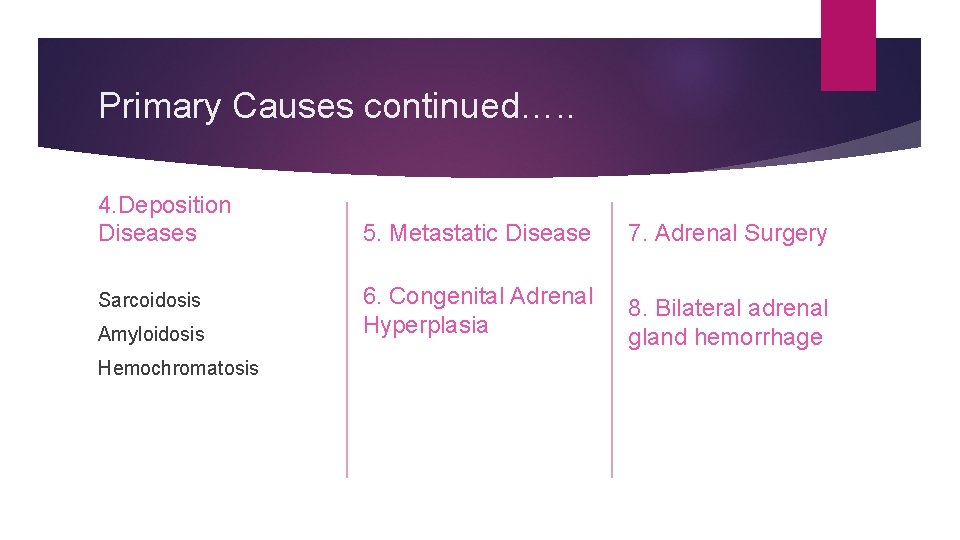
Primary Causes continued…. . 4. Deposition Diseases Sarcoidosis Amyloidosis Hemochromatosis 5. Metastatic Disease 7. Adrenal Surgery 6. Congenital Adrenal Hyperplasia 8. Bilateral adrenal gland hemorrhage
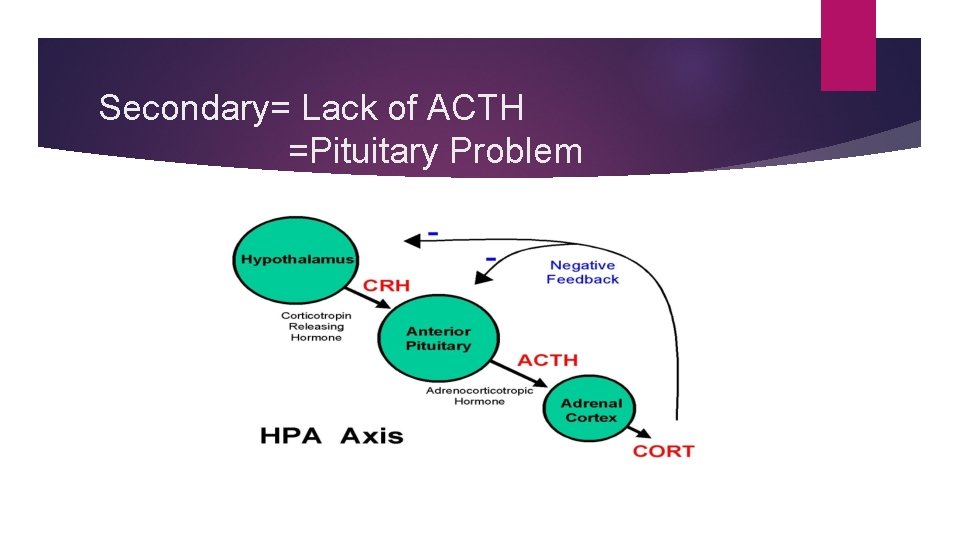
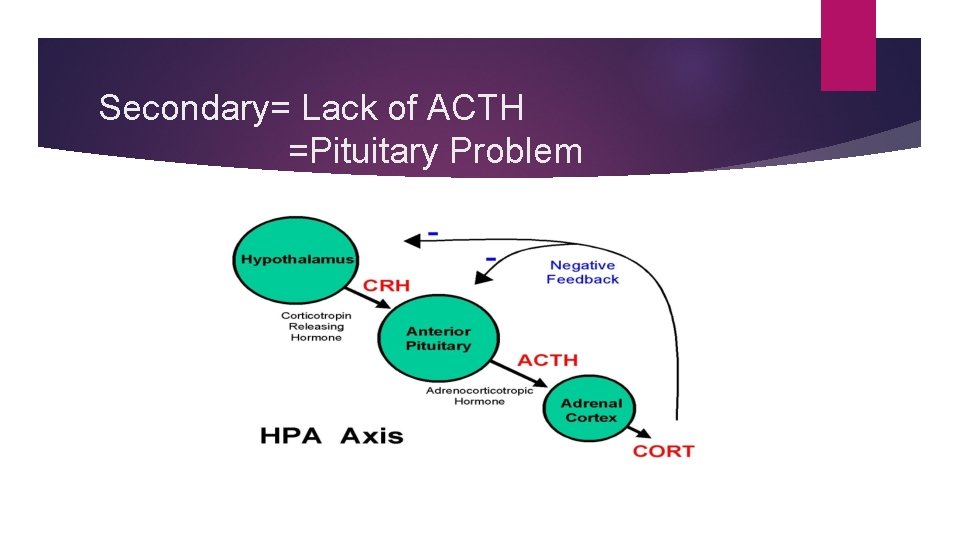
Secondary= Lack of ACTH =Pituitary Problem
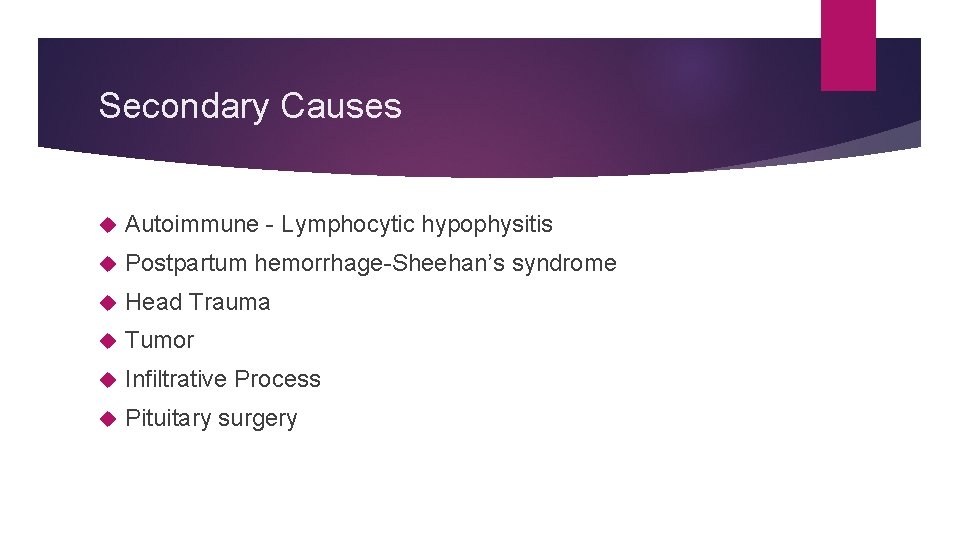
Secondary Causes Autoimmune - Lymphocytic hypophysitis Postpartum hemorrhage-Sheehan’s syndrome Head Trauma Tumor Infiltrative Process Pituitary surgery
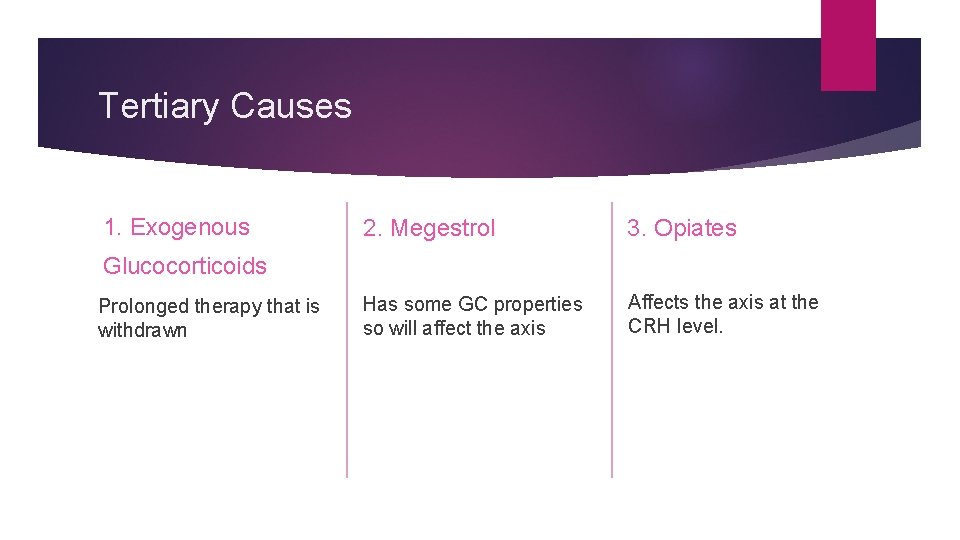
Tertiary Causes 1. Exogenous 2. Megestrol 3. Opiates Has some GC properties so will affect the axis Affects the axis at the CRH level. Glucocorticoids Prolonged therapy that is withdrawn
What does cortisol do? MAINTAINS GLYCOGEN (cause of hypoglycemia) REGULATES IMMUNE FUNCTION (more infections) PART OF HEPATIC NEOGENESIS (gut absorption, nausea, diarrhea, vomiting) VASCULAR TONE (cause of hypotension)
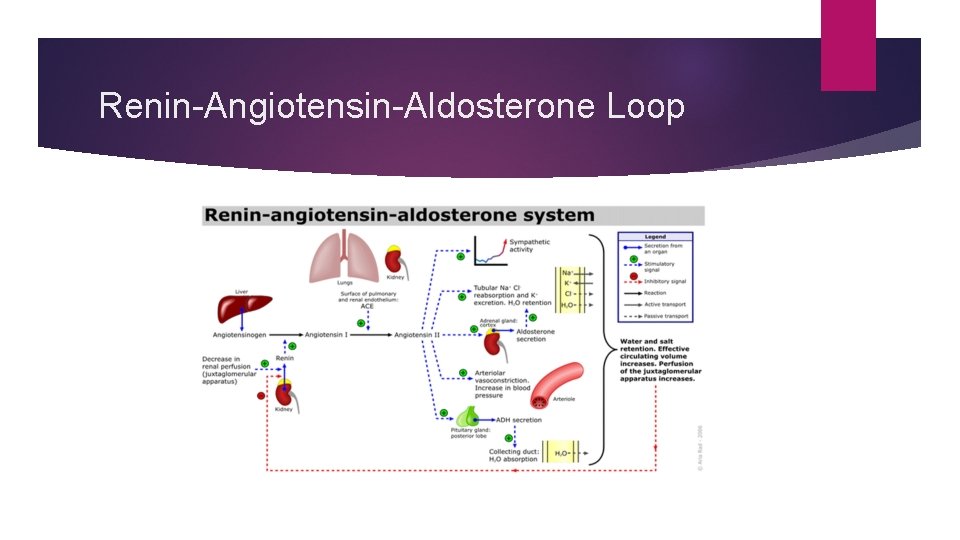
What does MC =Aldosterone do? • Regulates Na and K at the level of the kidney/ renin-angiotensin system (Very little aldosterone secretion comes from ACTH stim) Lack of aldosterone as in Primary AI a) renal wasting of Na b) retention of K c)volume loss >>severe intravascular depletion>>>hyptotension and shock
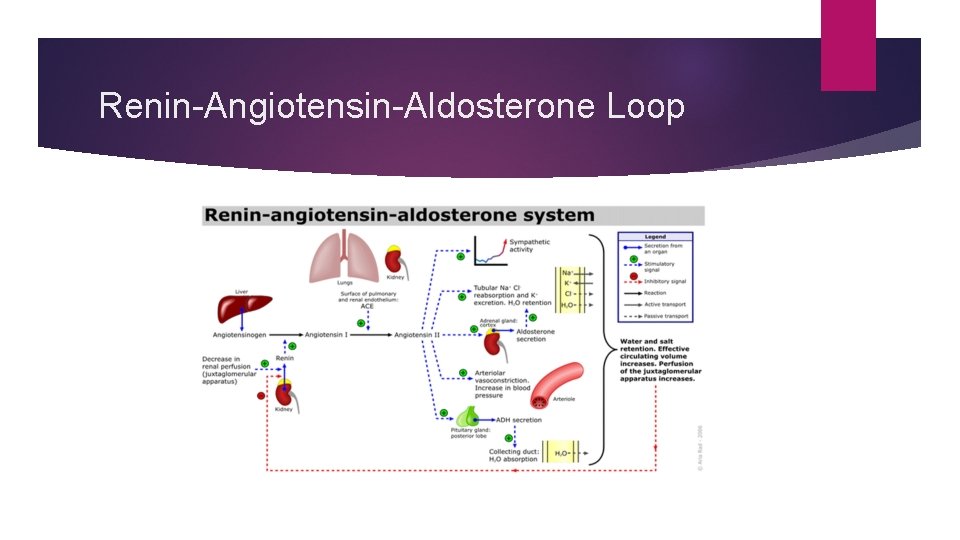
Renin-Angiotensin-Aldosterone Loop
What does AI feel like?
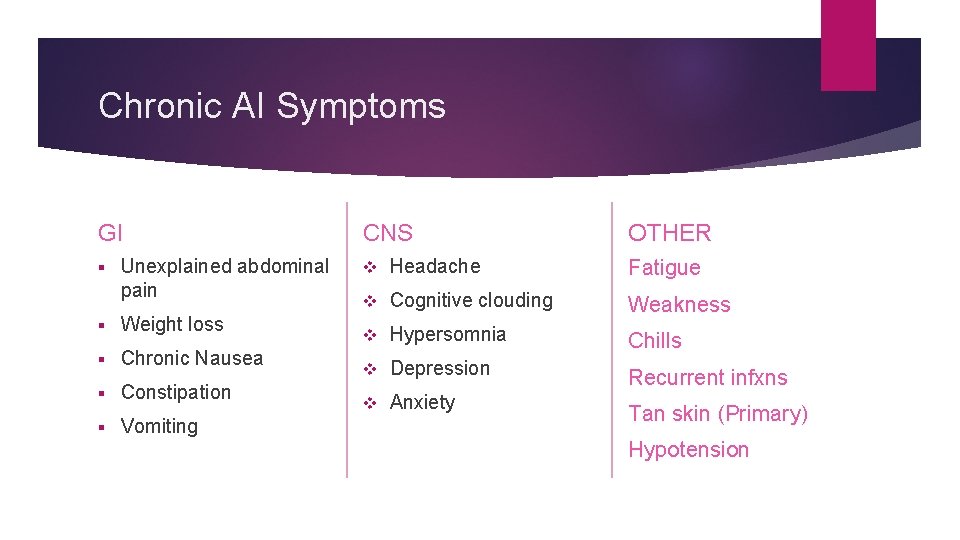
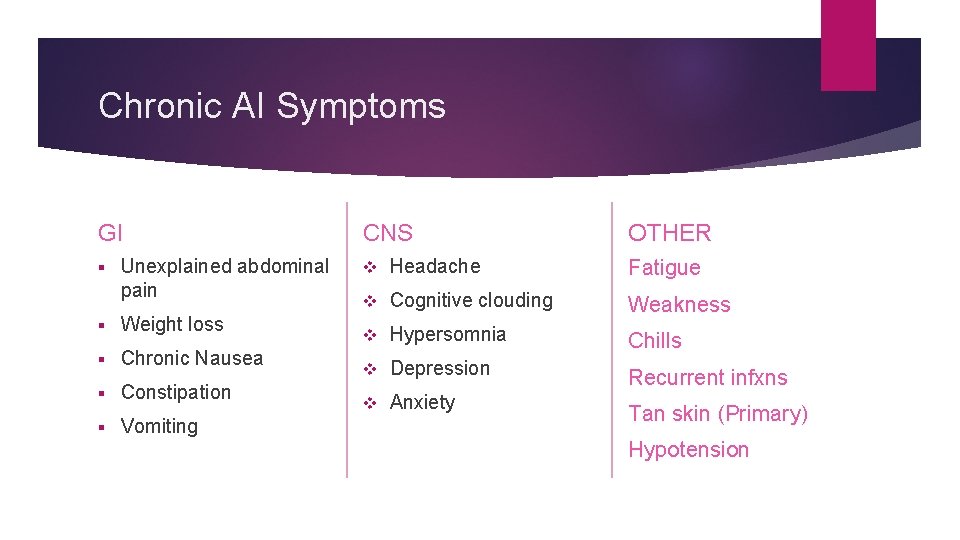
Chronic AI Symptoms GI § Unexplained abdominal pain § Weight loss § Chronic Nausea § Constipation § Vomiting CNS OTHER v Headache Fatigue v Cognitive clouding Weakness v Hypersomnia Chills v Depression Recurrent infxns v Anxiety Tan skin (Primary) Hypotension
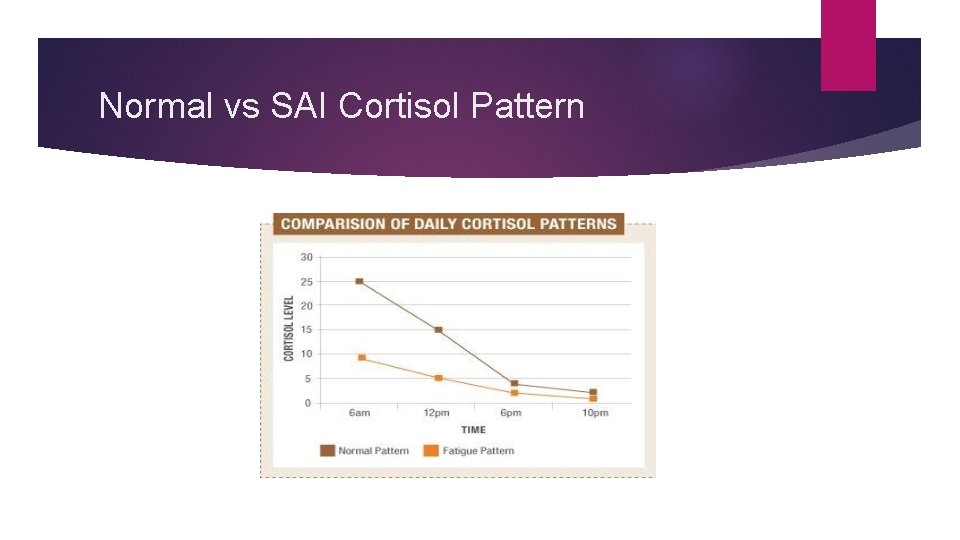
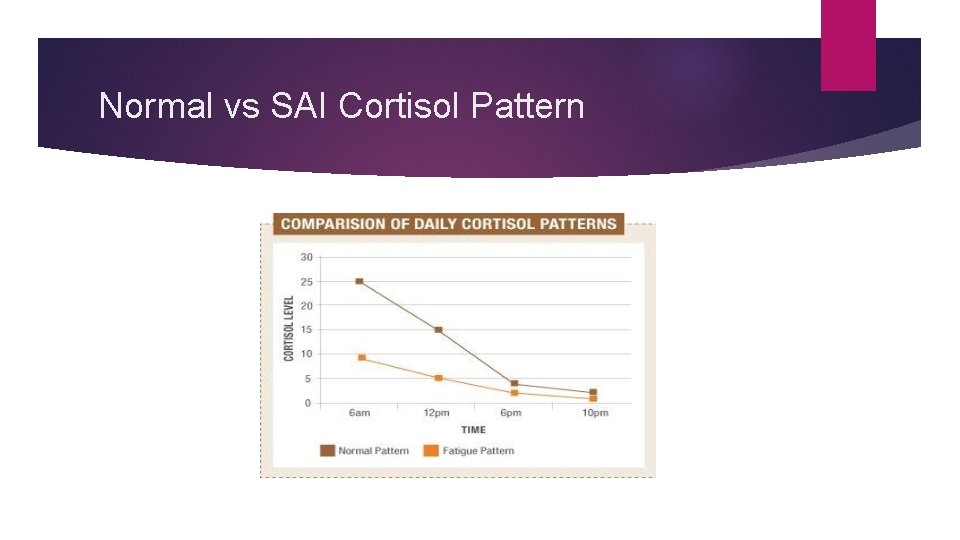
Normal vs SAI Cortisol Pattern
JFK had Addisons Hyperpigmented Chronically ill How sick was JFK?
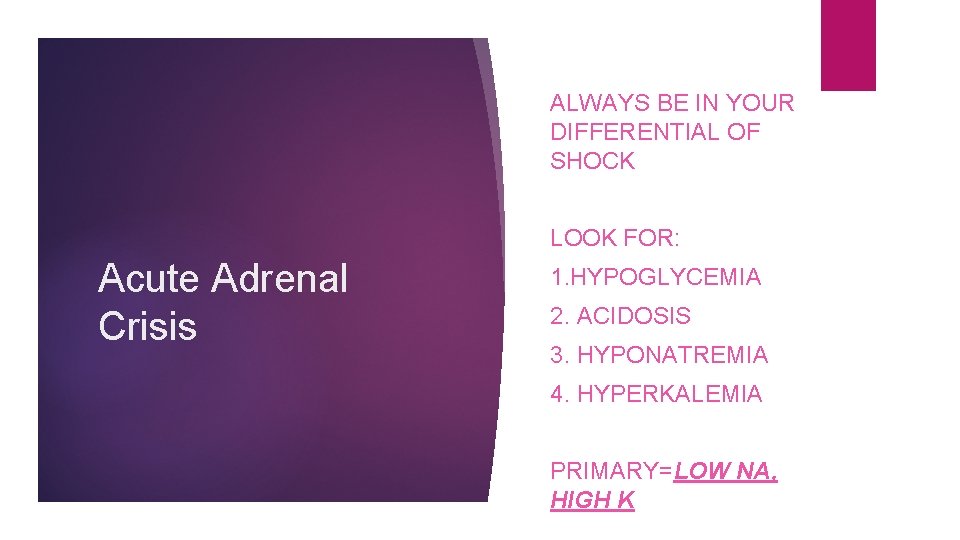
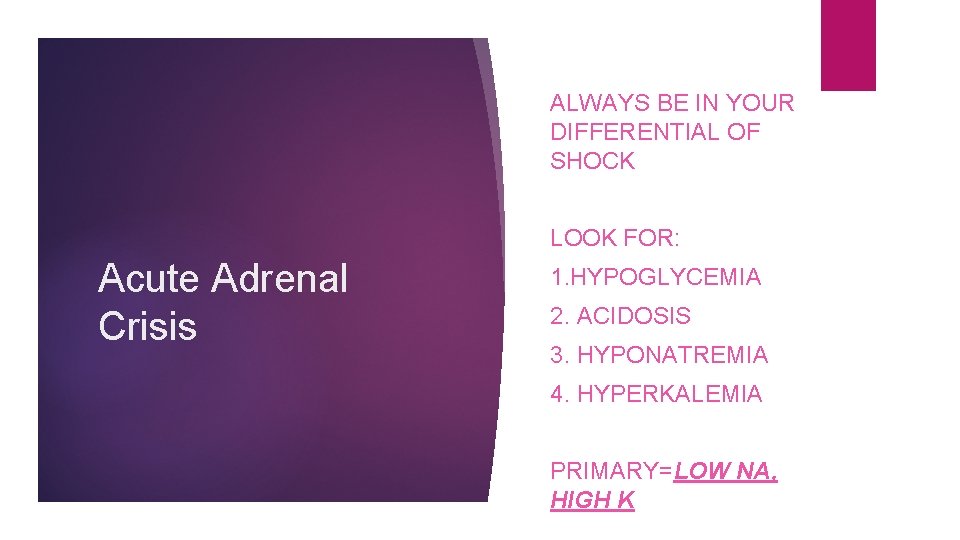
ALWAYS BE IN YOUR DIFFERENTIAL OF SHOCK LOOK FOR: Acute Adrenal Crisis 1. HYPOGLYCEMIA 2. ACIDOSIS 3. HYPONATREMIA 4. HYPERKALEMIA PRIMARY=LOW NA, HIGH K

#1 IS GI FROM VOMITING/DIARRHEA SURGERY ACUTE ADRENAL CRISIS CAUSES HEAT EMOTIONAL DISTRESS TRAUMA PREGNANCY INFECTION
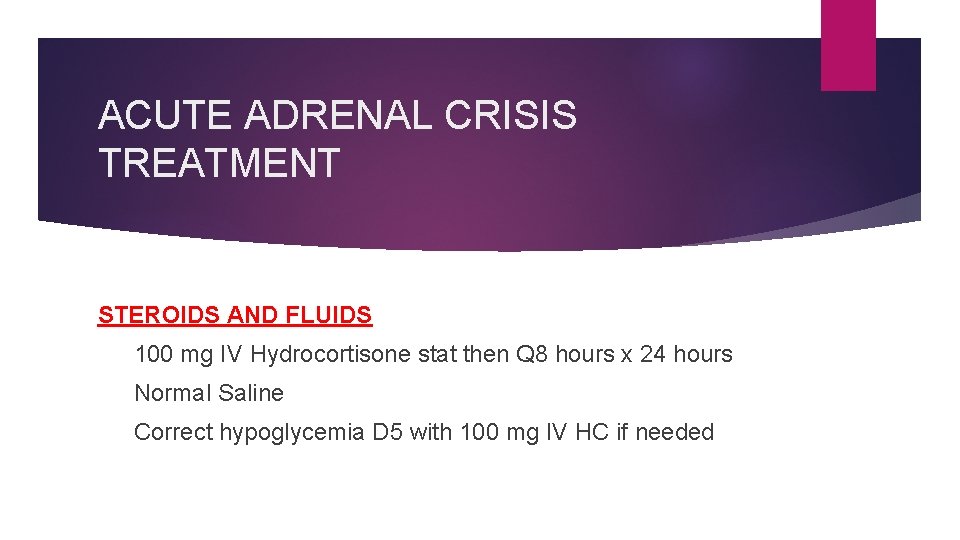
ACUTE ADRENAL CRISIS TREATMENT STEROIDS AND FLUIDS 100 mg IV Hydrocortisone stat then Q 8 hours x 24 hours Normal Saline Correct hypoglycemia D 5 with 100 mg IV HC if needed
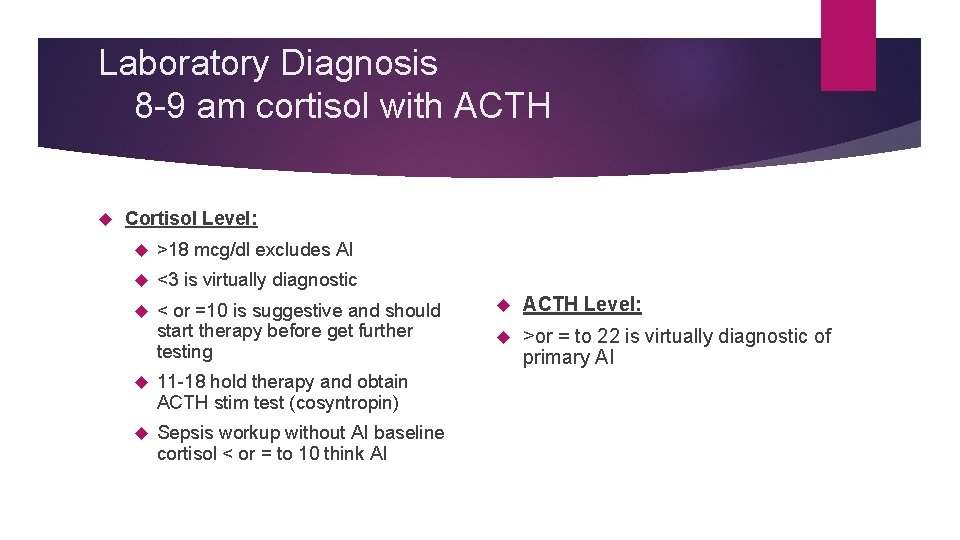
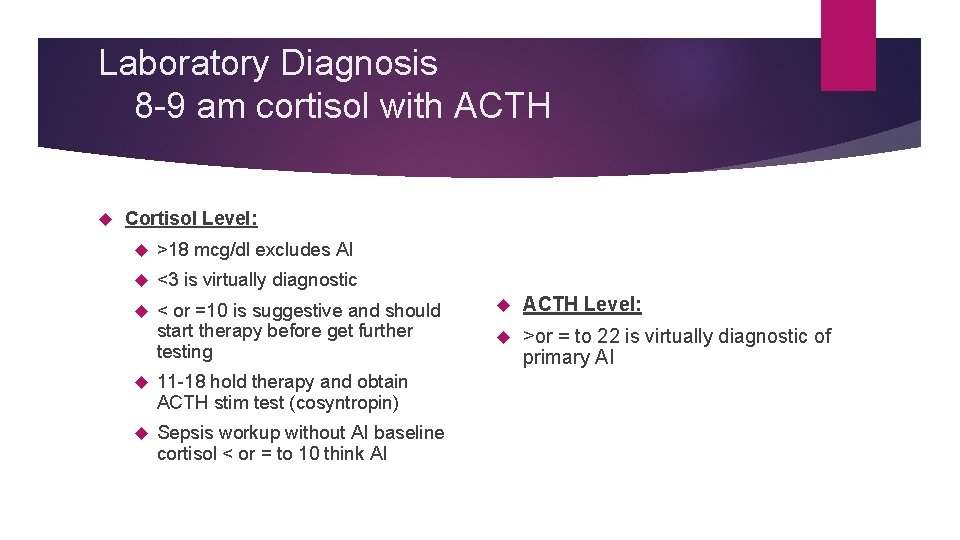
Laboratory Diagnosis 8 -9 am cortisol with ACTH Cortisol Level: >18 mcg/dl excludes AI <3 is virtually diagnostic < or =10 is suggestive and should start therapy before get further testing 11 -18 hold therapy and obtain ACTH stim test (cosyntropin) Sepsis workup without AI baseline cortisol < or = to 10 think AI ACTH Level: >or = to 22 is virtually diagnostic of primary AI
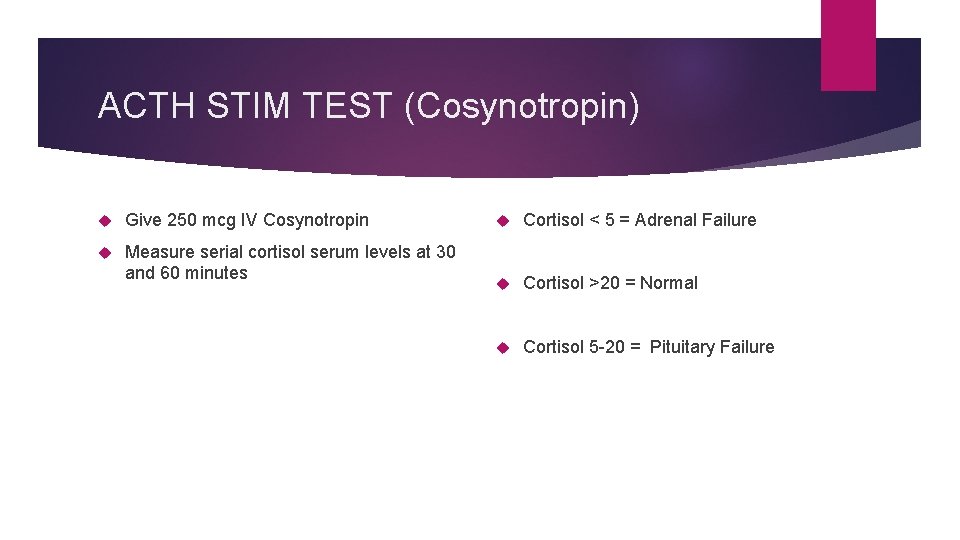
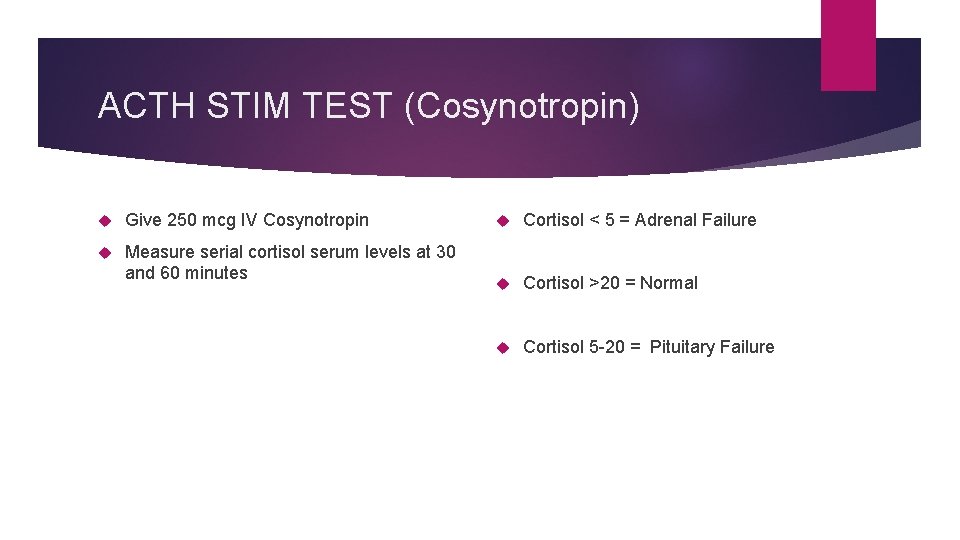
ACTH STIM TEST (Cosynotropin) Give 250 mcg IV Cosynotropin Measure serial cortisol serum levels at 30 and 60 minutes Cortisol < 5 = Adrenal Failure Cortisol >20 = Normal Cortisol 5 -20 = Pituitary Failure

Goals of Treatment #1 #2 #3 Physiological Improve QOL Prevent Adrenal Replacement Of GC/MC Crisis
Glucocorticoid Replacement Options 1) HYDROCORTISONE 2) PREDNISONE 3) DEXAMETHASONE
Glucocorticoids are not all created equal NONE ARE IDEAL IN AVOIDANCE OF RISKS OF OVER OR UNDER REPLACEMENT MOST PHYSIOLOGICAL = HC PREDNISONE POTENCY= 4 XHC DEXAMETHASONE=NO EFFECT ON VASCULAR TONE LAST 24 -36 HRS
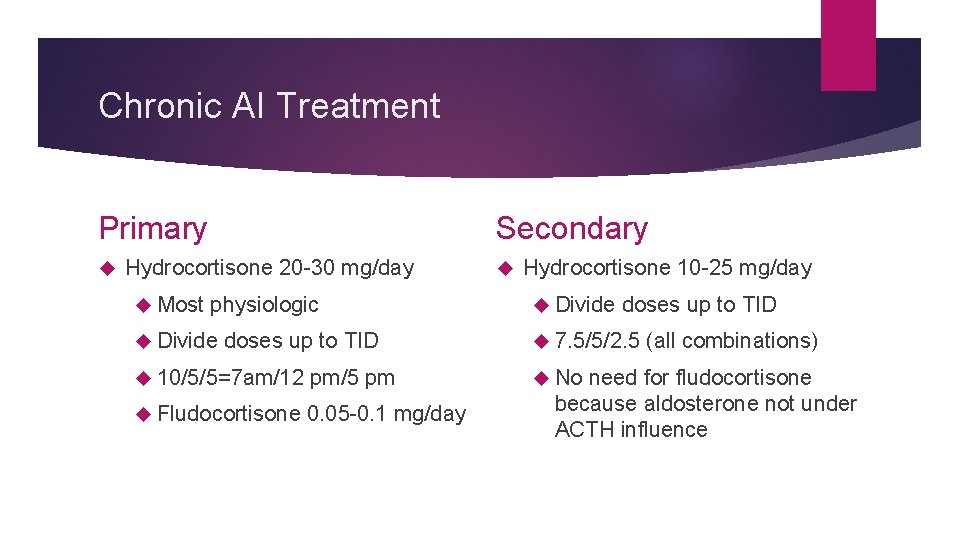
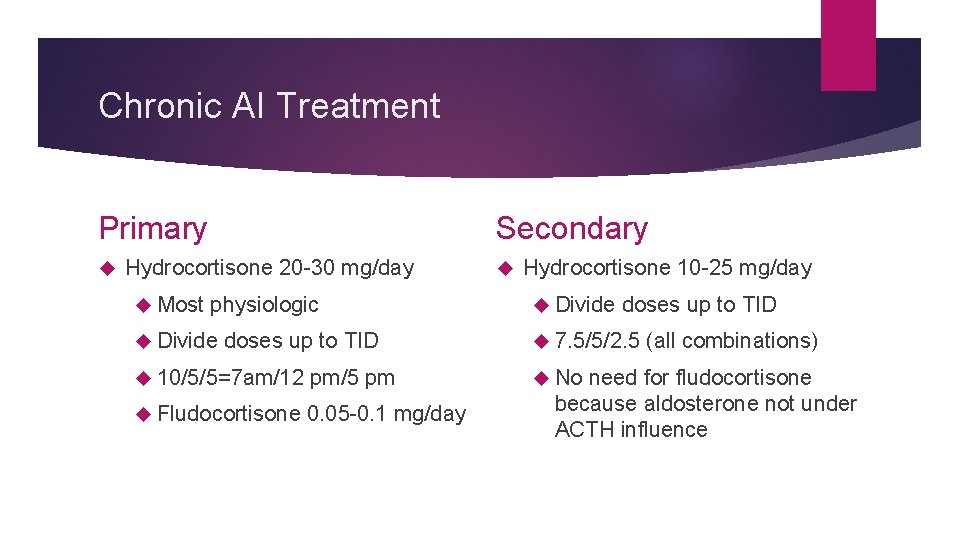
Chronic AI Treatment Primary Secondary Hydrocortisone 20 -30 mg/day Most physiologic Divide doses up to TID 10/5/5=7 am/12 pm/5 pm Fludocortisone 0. 05 -0. 1 mg/day Hydrocortisone 10 -25 mg/day Divide doses up to TID 7. 5/5/2. 5 No (all combinations) need for fludocortisone because aldosterone not under ACTH influence
Chronic AI Treatment cont… Tertiary Removal of the offending drug with a taper if possible (reversible) Treat with maintenance HC if not able to d/c drug As little as 20 mg/day prednisone for 7 days can cause AI Be suspicious in asthmatics, COPD, rheumatology pts
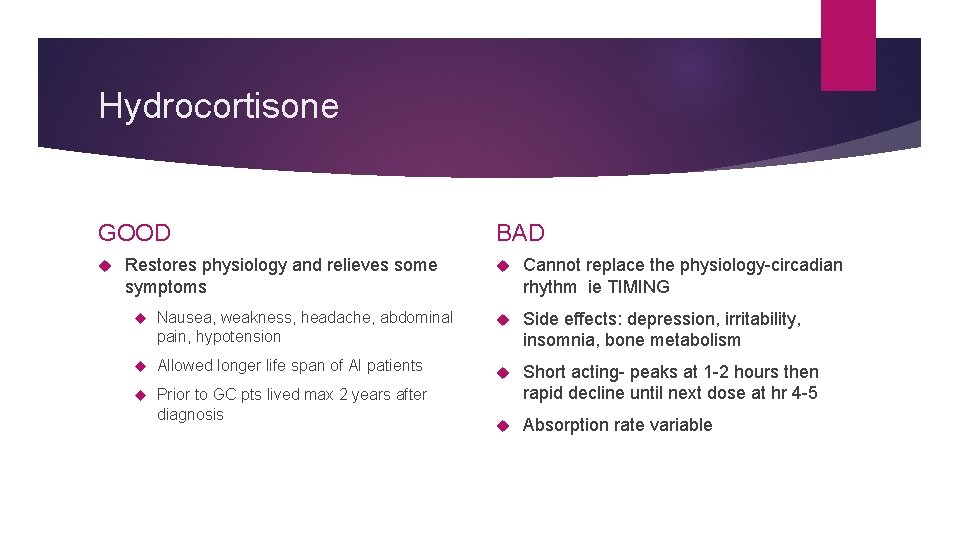
Hydrocortisone GOOD Restores physiology and relieves some symptoms BAD Cannot replace the physiology-circadian rhythm ie TIMING Nausea, weakness, headache, abdominal pain, hypotension Side effects: depression, irritability, insomnia, bone metabolism Allowed longer life span of AI patients Prior to GC pts lived max 2 years after diagnosis Short acting- peaks at 1 -2 hours then rapid decline until next dose at hr 4 -5 Absorption rate variable
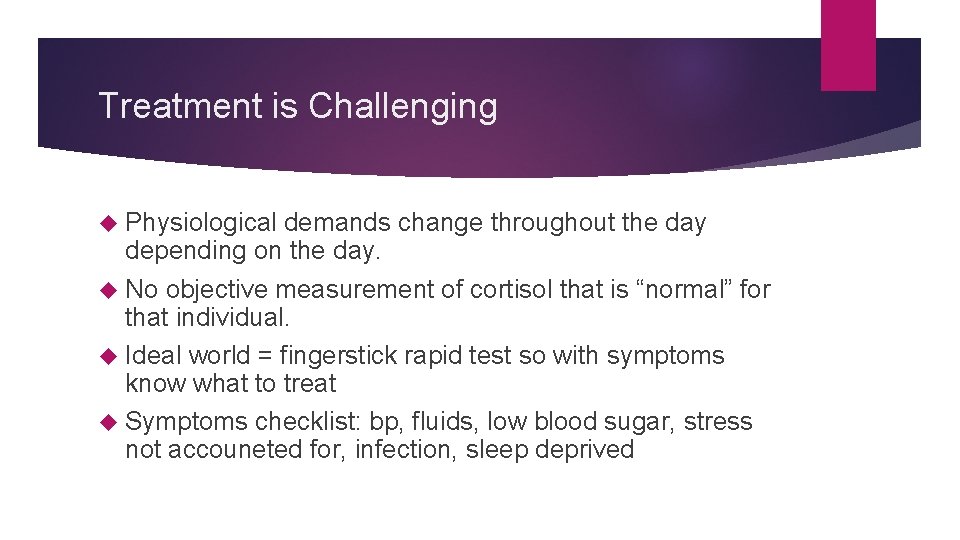
Treatment is Challenging Physiological demands change throughout the day depending on the day. No objective measurement of cortisol that is “normal” for that individual. Ideal world = fingerstick rapid test so with symptoms know what to treat Symptoms checklist: bp, fluids, low blood sugar, stress not accouneted for, infection, sleep deprived
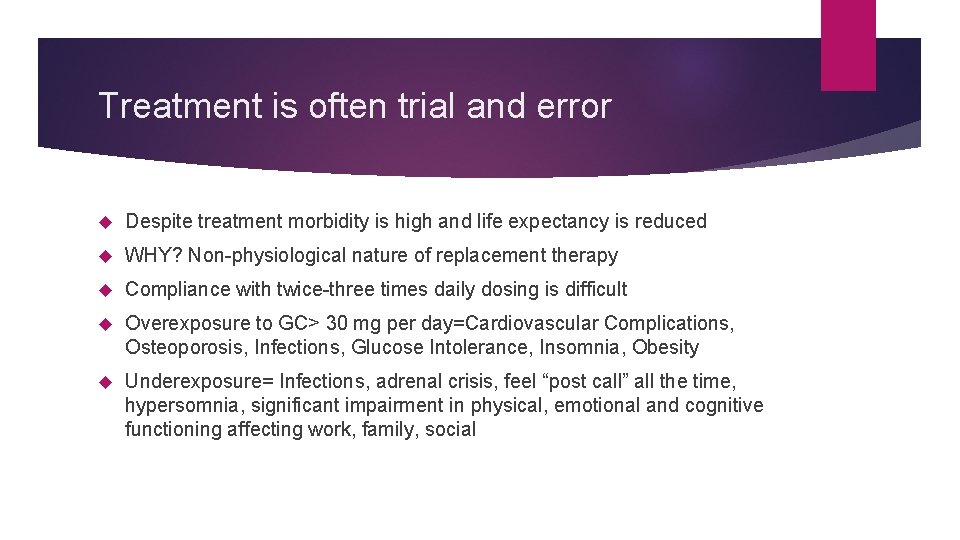
Treatment is often trial and error Despite treatment morbidity is high and life expectancy is reduced WHY? Non-physiological nature of replacement therapy Compliance with twice-three times daily dosing is difficult Overexposure to GC> 30 mg per day=Cardiovascular Complications, Osteoporosis, Infections, Glucose Intolerance, Insomnia, Obesity Underexposure= Infections, adrenal crisis, feel “post call” all the time, hypersomnia, significant impairment in physical, emotional and cognitive functioning affecting work, family, social
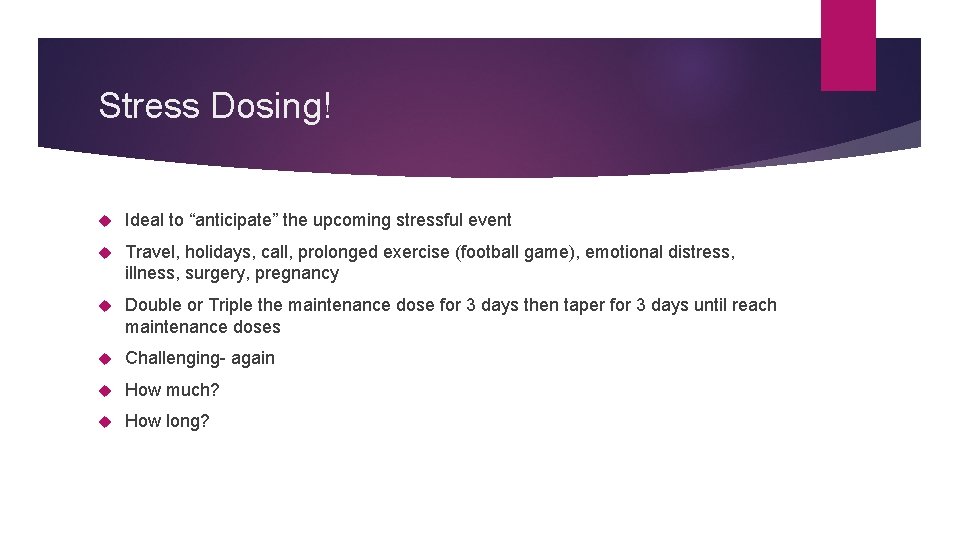
Stress Dosing! Ideal to “anticipate” the upcoming stressful event Travel, holidays, call, prolonged exercise (football game), emotional distress, illness, surgery, pregnancy Double or Triple the maintenance dose for 3 days then taper for 3 days until reach maintenance doses Challenging- again How much? How long?
Stress dose for prolonged exercise
Patient and Family Education on Management Life threatening disease that requires lifelong replacement Educate and Reiterate the importance of stress dosing and how to avoid v adrenal crisis ID Emergency bracelet>>”Adrenal Failure- Need steroids” Emergency kit with 100 mg HC vials, needles, syringes for vomiting/diarrhea or other illness and cannot keep oral down Give Prevnar and Pneumovax to prevent recurrent sinusitis/bronchitis

PATIENTS REPORT POOR QOL WORLDWIDE SURVEY OF 1245 PTS: Despite treatment…. 64% REPORTED COMPROMISED HEALTH STATUS 40% MISSED SCHOOL OR WORK IN LAST 3 MONTHS 38% HOSPITALIZED IN LAST YR 25% DISABILITY
Patients need support Support groups NADF (National adrenal disease foundation) Website: www. nadf. org provides information on emergency kits, patient information, newsletter and online support group- inspire. com Quality of Life Discussions: stress, exercise, routine, dosing compliance, sleep (no dosing after 6 pm), relationships, family life, work Journaling dosing times, bp, hours of sleep, stress
What is in the Pipeline? Cortisol pumps Long acting/IR Cortisol
Adrenal Insufficiency after 4 years of Treatment
Thank you IAFP.