Venous diseases Zsolt Pcsvrady zspecschello hu Pcs V
- Slides: 29
Venous diseases Zsolt Pécsvárady zspecs@chello. hu Pécs
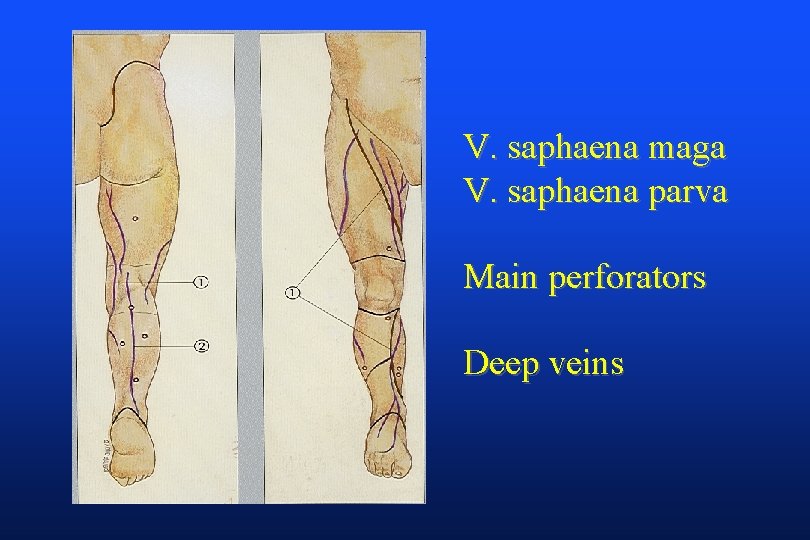
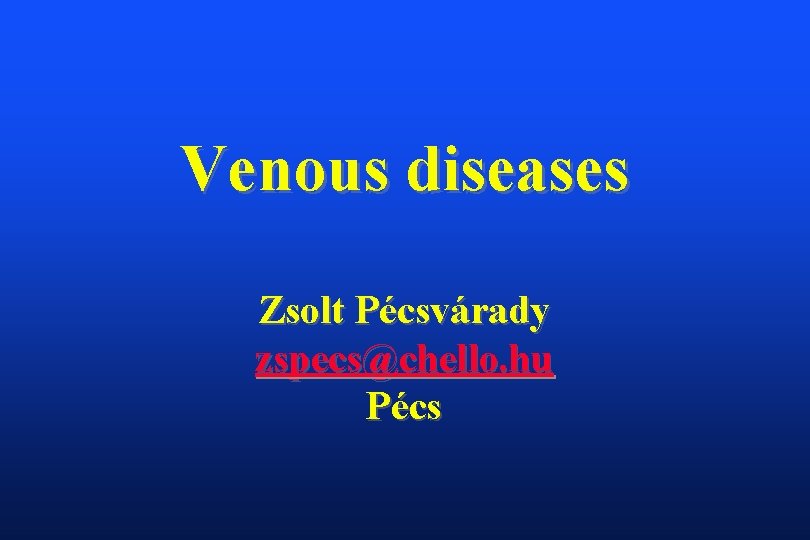
V. saphaena maga V. saphaena parva Main perforators Deep veins
I. Superficial thrombophlebitis II. Deep venous thrombosis and pulmonal embolisation III. Chronic venous insufficiency CVI
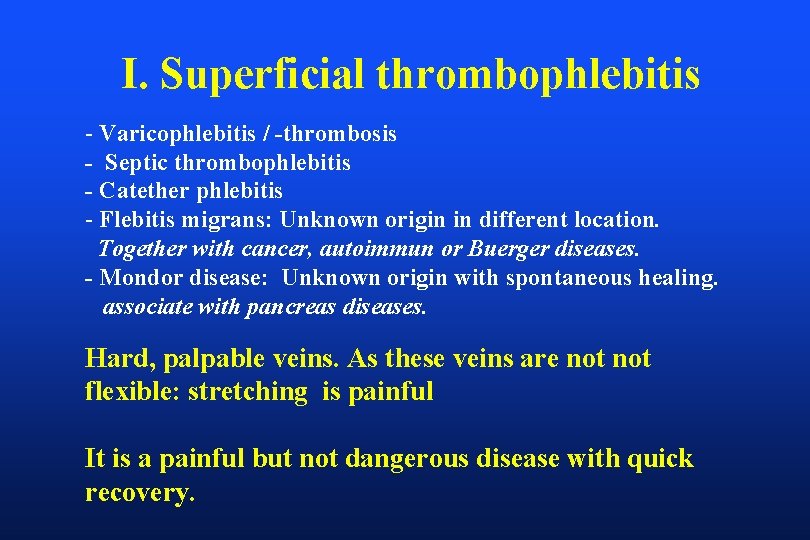
I. Superficial thrombophlebitis - Varicophlebitis / -thrombosis - Septic thrombophlebitis - Catether phlebitis - Flebitis migrans: Unknown origin in different location. Together with cancer, autoimmun or Buerger diseases. - Mondor disease: Unknown origin with spontaneous healing. associate with pancreas diseases. Hard, palpable veins. As these veins are not flexible: stretching is painful It is a painful but not dangerous disease with quick recovery.
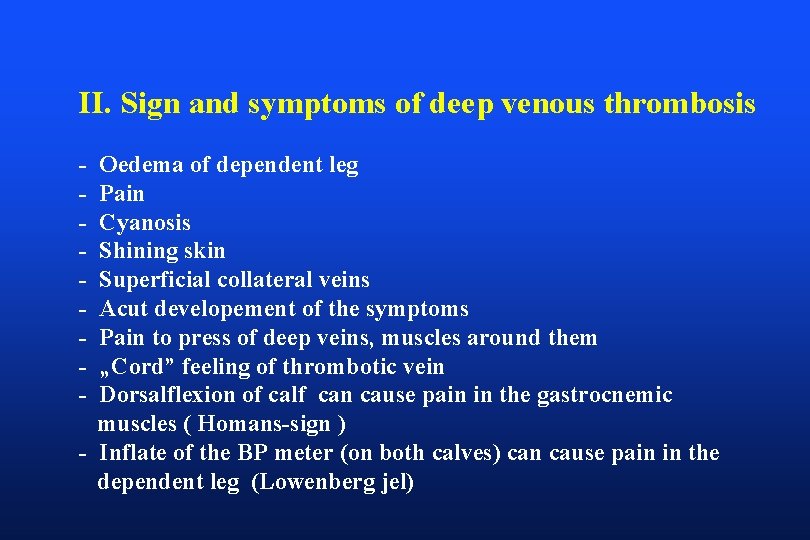
II. Sign and symptoms of deep venous thrombosis - Oedema of dependent leg Pain Cyanosis Shining skin Superficial collateral veins Acut developement of the symptoms Pain to press of deep veins, muscles around them „Cord” feeling of thrombotic vein Dorsalflexion of calf can cause pain in the gastrocnemic muscles ( Homans-sign ) - Inflate of the BP meter (on both calves) can cause pain in the dependent leg (Lowenberg jel)
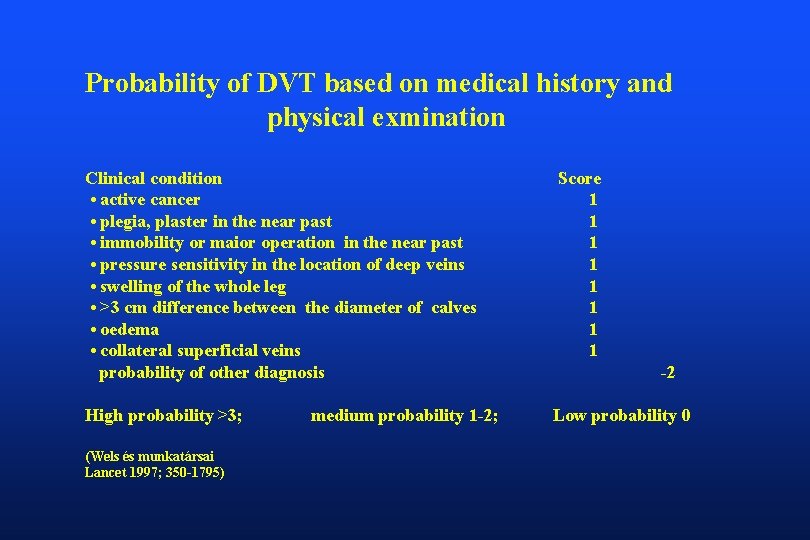
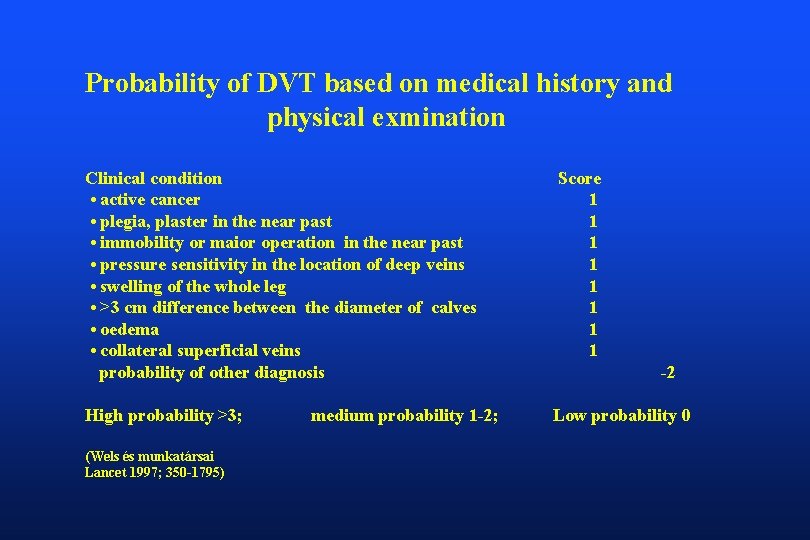
Probability of DVT based on medical history and physical exmination Clinical condition • active cancer • plegia, plaster in the near past • immobility or maior operation in the near past • pressure sensitivity in the location of deep veins • swelling of the whole leg • >3 cm difference between the diameter of calves • oedema • collateral superficial veins probability of other diagnosis Score 1 1 1 1 High probability >3; Low probability 0 (Wels és munkatársai Lancet 1997; 350 -1795) medium probability 1 -2; -2
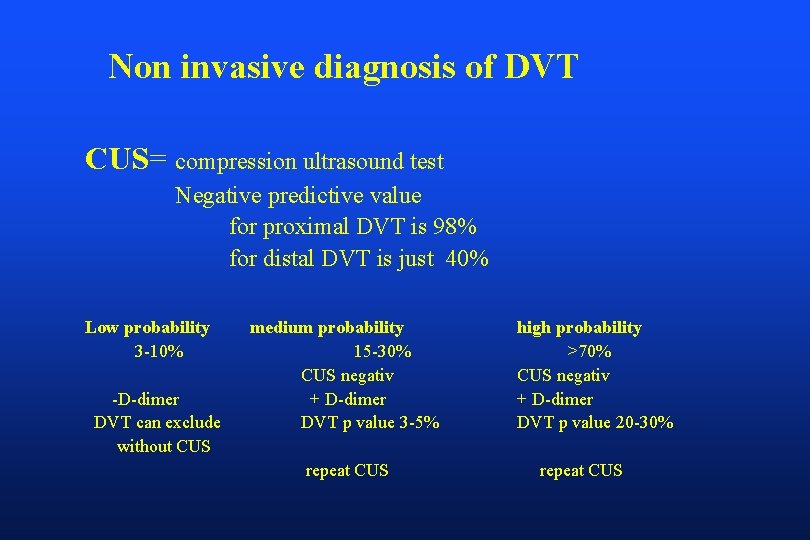
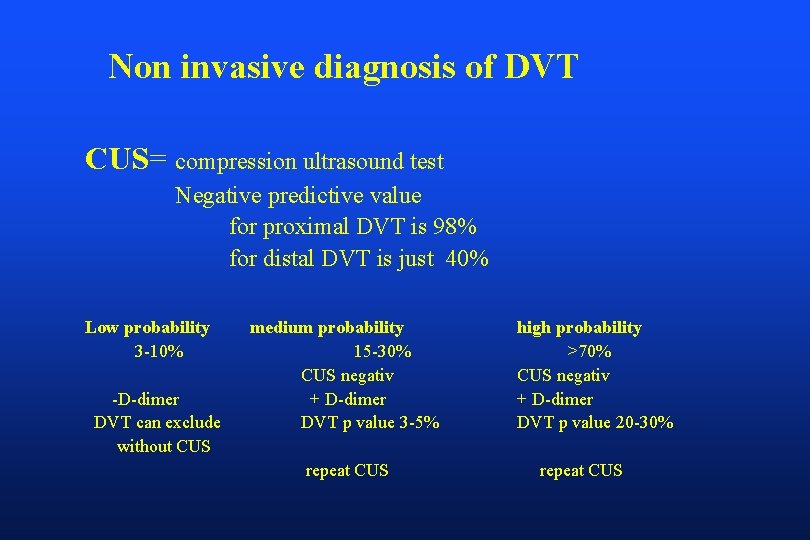
Non invasive diagnosis of DVT CUS= compression ultrasound test Negative predictive value for proximal DVT is 98% for distal DVT is just 40% Low probability 3 -10% -D-dimer DVT can exclude without CUS medium probability 15 -30% CUS negativ + D-dimer DVT p value 3 -5% repeat CUS high probability >70% CUS negativ + D-dimer DVT p value 20 -30% repeat CUS
Risk factors for DVT I. • major orthopedic surgery ( hip, knee ) • malignant disease • trauma, postoperative condition • DVT or PE in medical history • immobilization • heart attack, heart failure • stroke or paralysis • infections, sepsis
Risk factors for DVT II. • Age older than 40 yrs • Obesity • Varicositas • Oral contraceptive, oestrogen treatment, gravidity • Thrombophylia APC resistency, Protein C and S, antithrombin III. insufficiency. fibrin és plasminogen disturbances, myeloproliferatíve diseases • Other serious diseases ( heart, lung, inflammatory bowel disease etc. )
III. Chronic venous insufficiency CVI
Etiology of Primary Insufficiency Heredity: most important risk factor „ Varicose veins are the result of poorly selecting one’s grandparents” Sir William Osler MD
Epidemiology of CVI - Varicositas in Europe: 25, 2% - CVI in Europe: 1, 7 % - Venous ulcer: 1 %
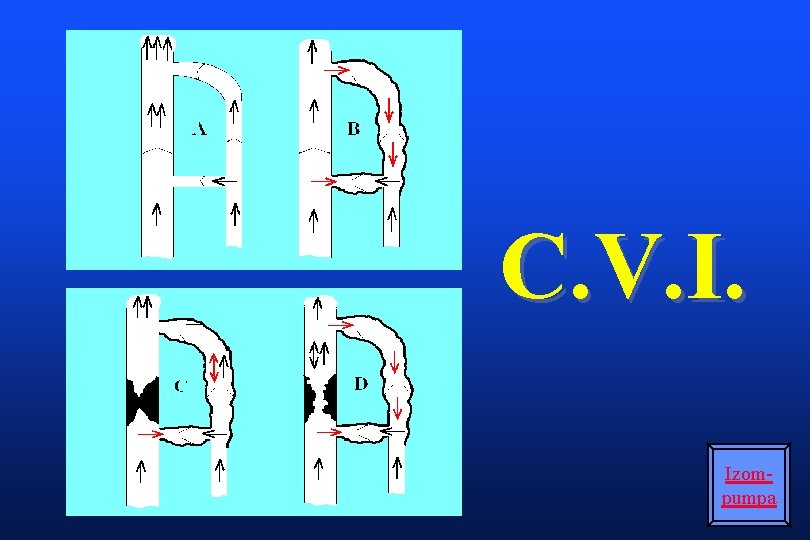
CVI = venous hypertension Causes: - reflux ( insufficiency of valves ) - occlusion ( thrombosis ) - disturbed lymphatic circulation - disturbed muscle pump function
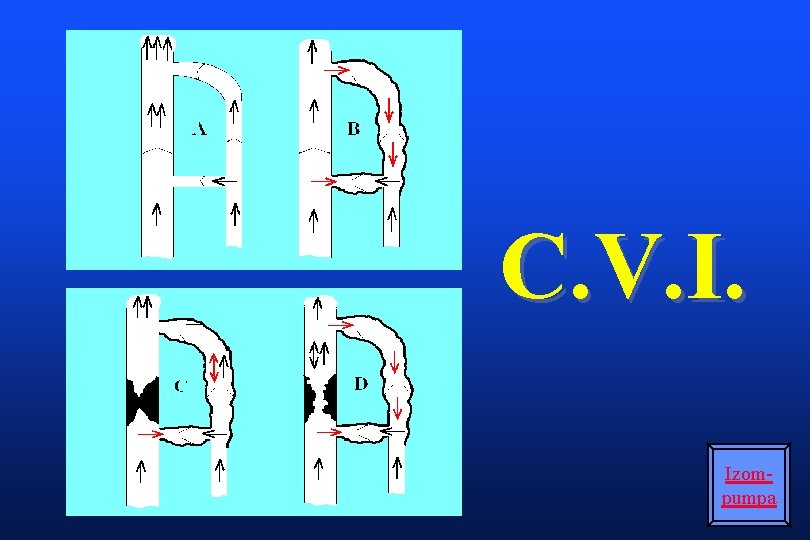
C. V. I. Izompumpa
Physiology of Venous Return Pump Calf muscles provide the force Sinusoidal veins as chambers Valves Maintain unidirectional flow Foot to heart Superficial to deep
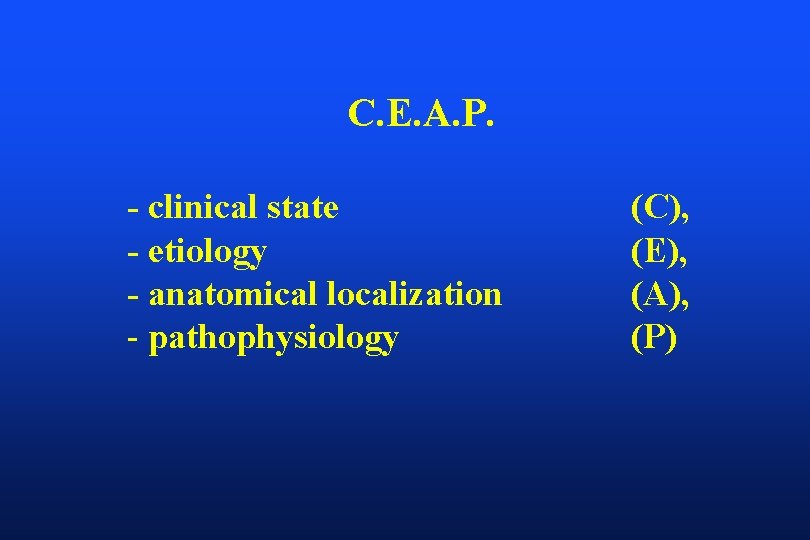
Classification: C. E. A. P.
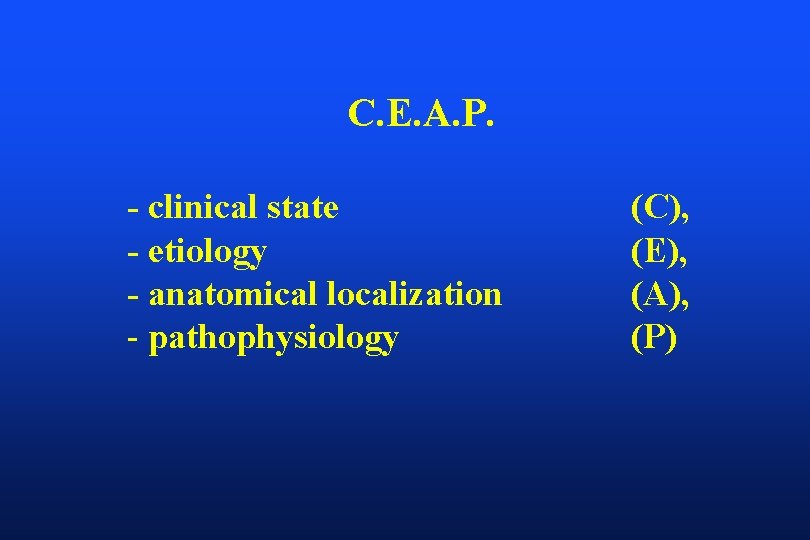
C. E. A. P. - clinical state - etiology - anatomical localization - pathophysiology (C), (E), (A), (P)
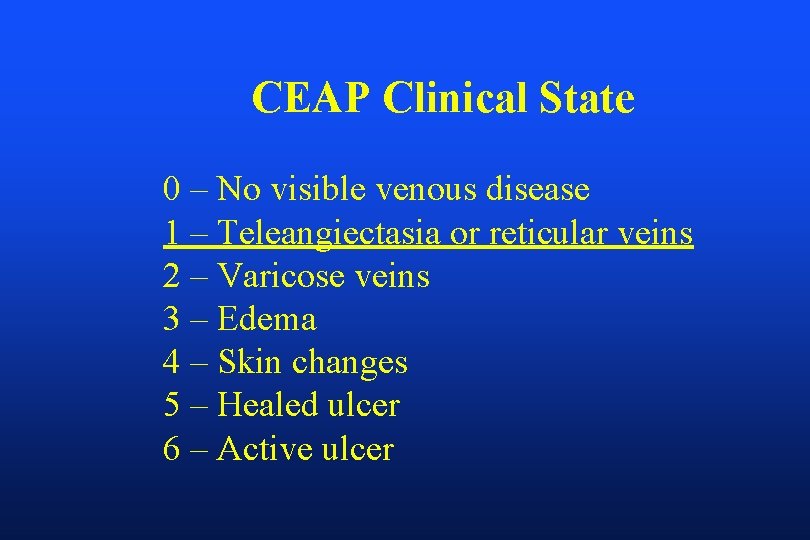
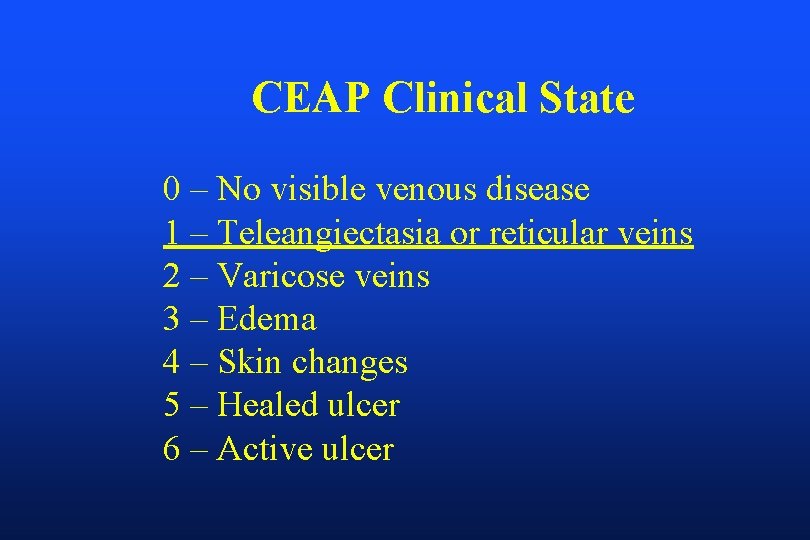
CEAP Clinical State 0 – No visible venous disease 1 – Teleangiectasia or reticular veins 2 – Varicose veins 3 – Edema 4 – Skin changes 5 – Healed ulcer 6 – Active ulcer
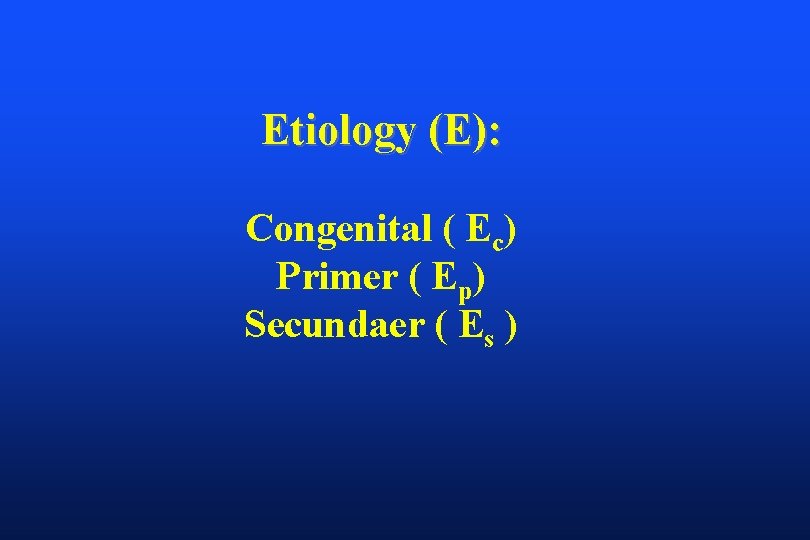
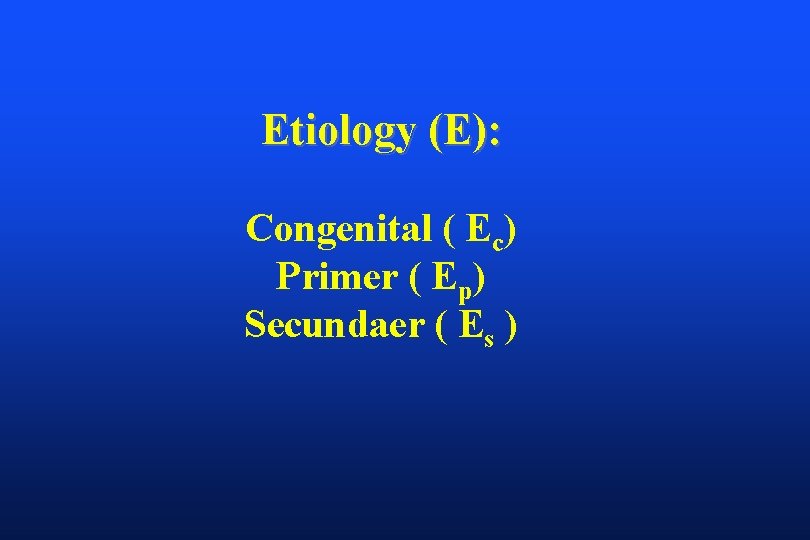
Etiology (E): Congenital ( Ec) Primer ( Ep) Secundaer ( Es )
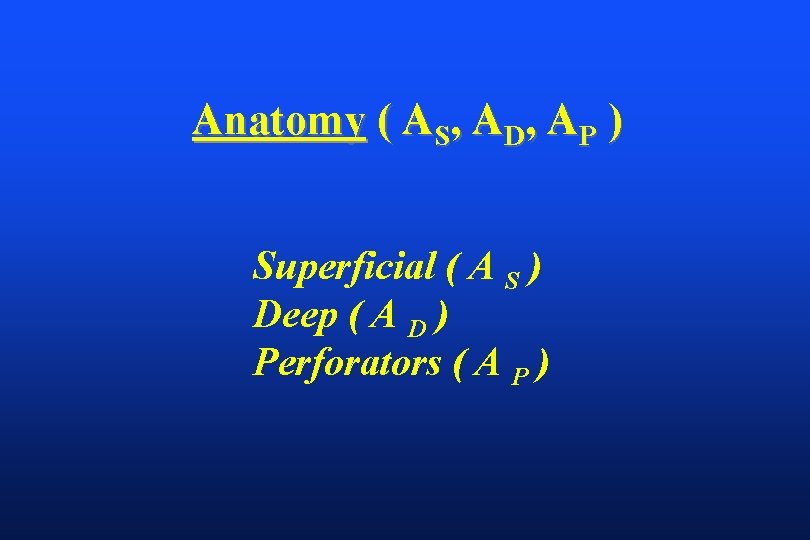
Anatomy ( AS, AD, AP ) Superficial ( A S ) Deep ( A D ) Perforators ( A P )
Pathopysiology ( PR, PO, PRO ) reflux (PR) 81 %, occlusion ( PO) 2 %, combination of these 17 %, ** 3. 5 x risk ** of signs
Patterns of Reflux 1. Truncal reflux saphenous related up to 5/6 of varicose veins 2. Non-truncal Reflux at least 1/6 of varicose veins 3. Deep and perforator reflux Not common alone but increases with severity of disease
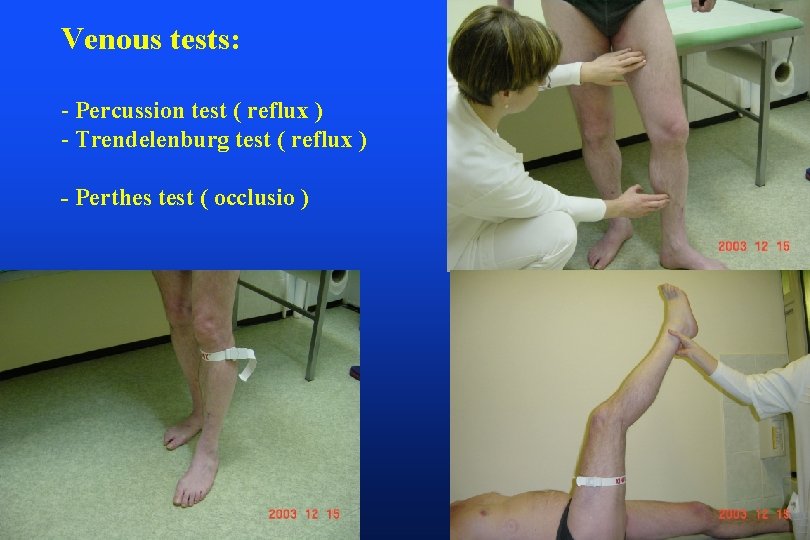
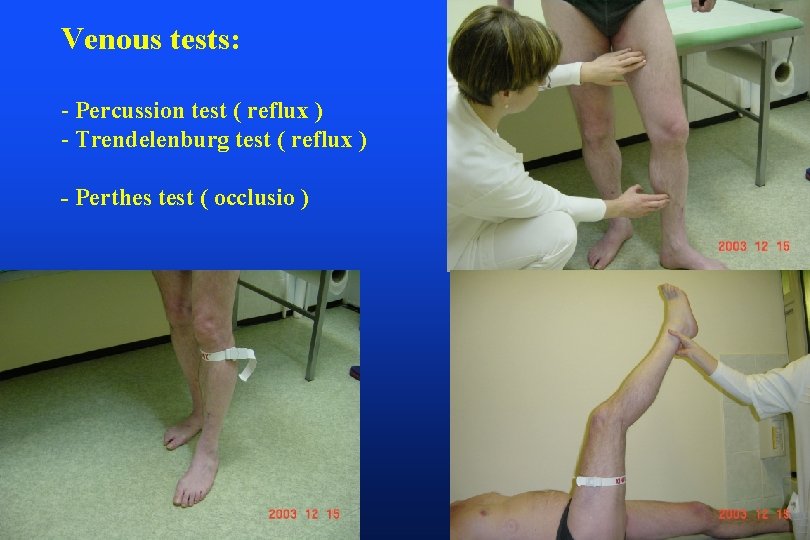
Venous tests: - Percussion test ( reflux ) - Trendelenburg test ( reflux ) - Perthes test ( occlusio )
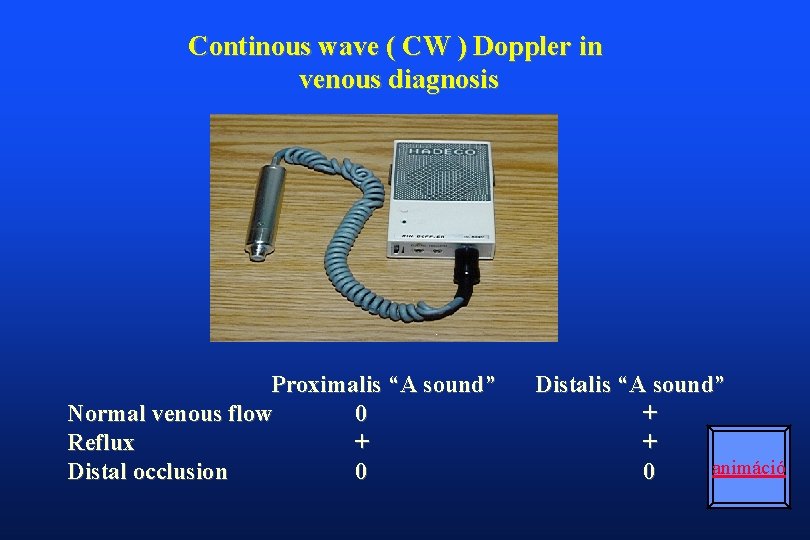
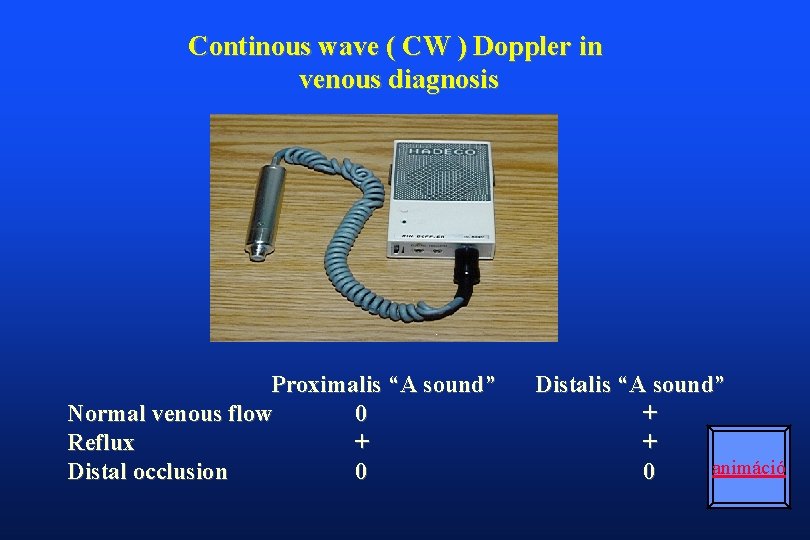
Continous wave ( CW ) Doppler in venous diagnosis Proximalis “A sound” Normal venous flow 0 Reflux + Distal occlusion 0 Distalis “A sound” + + animáció 0
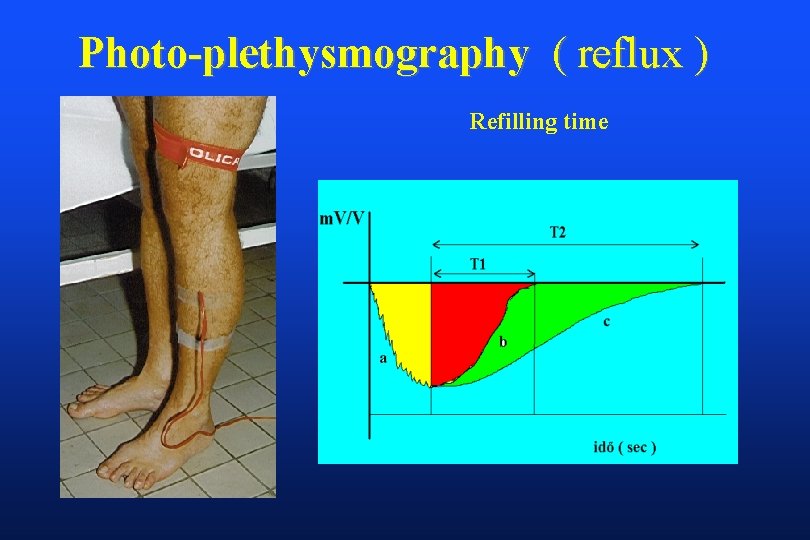
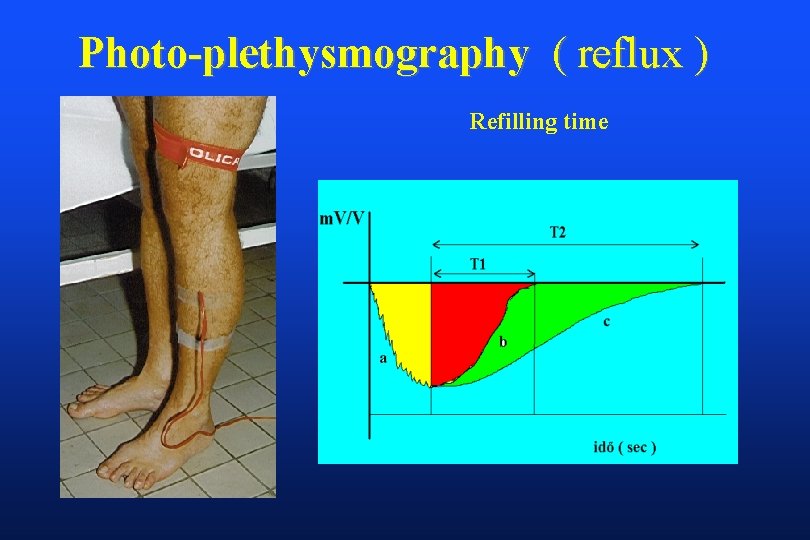
Photo-plethysmography ( reflux ) Refilling time
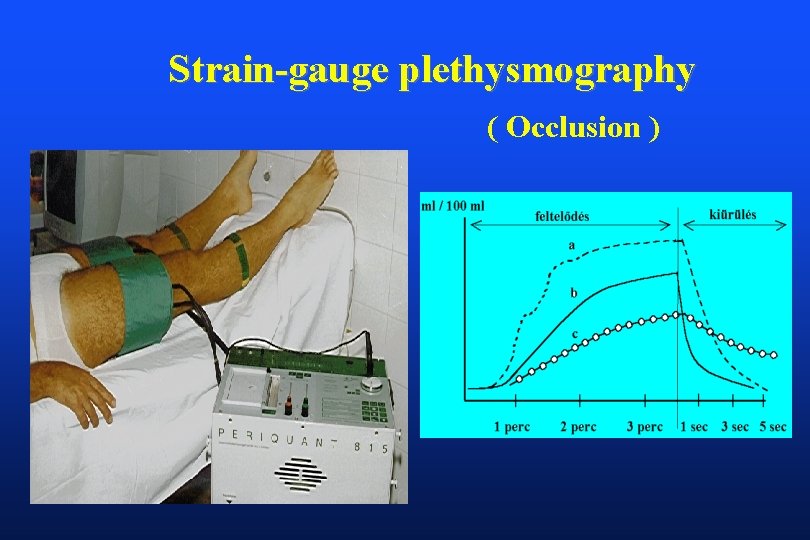
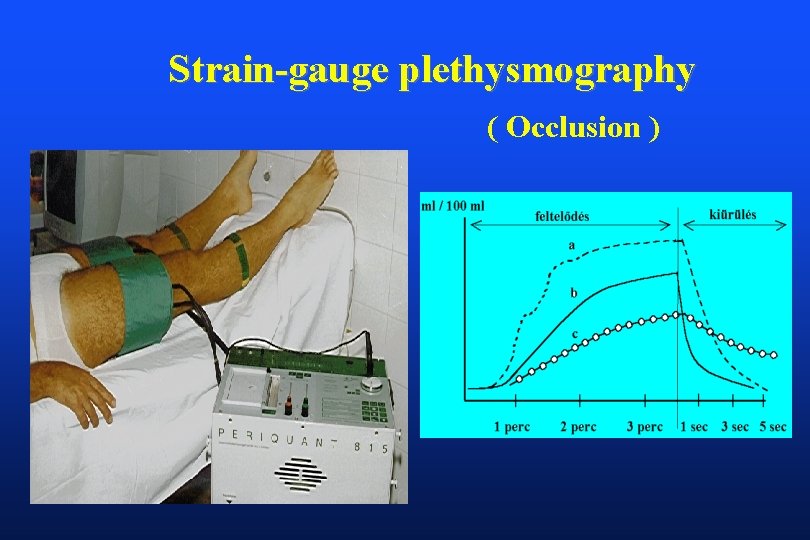
Strain-gauge plethysmography ( Occlusion )
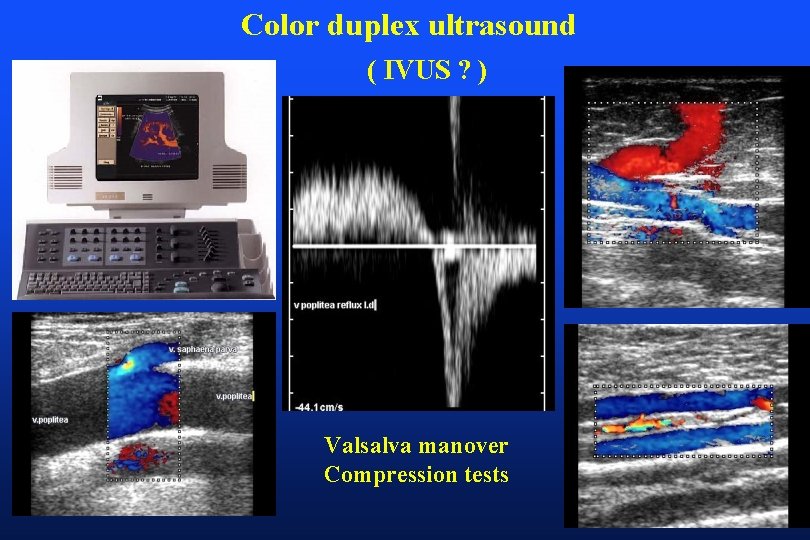
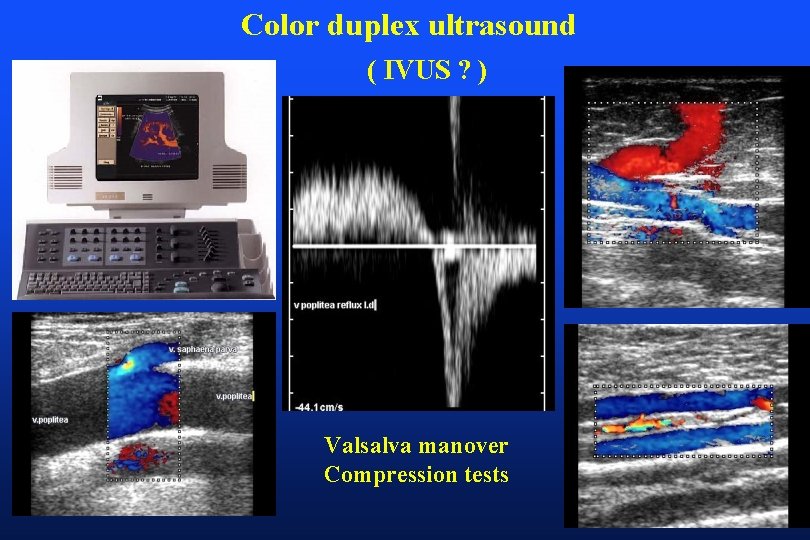
Color duplex ultrasound ( IVUS ? ) Valsalva manover Compression tests
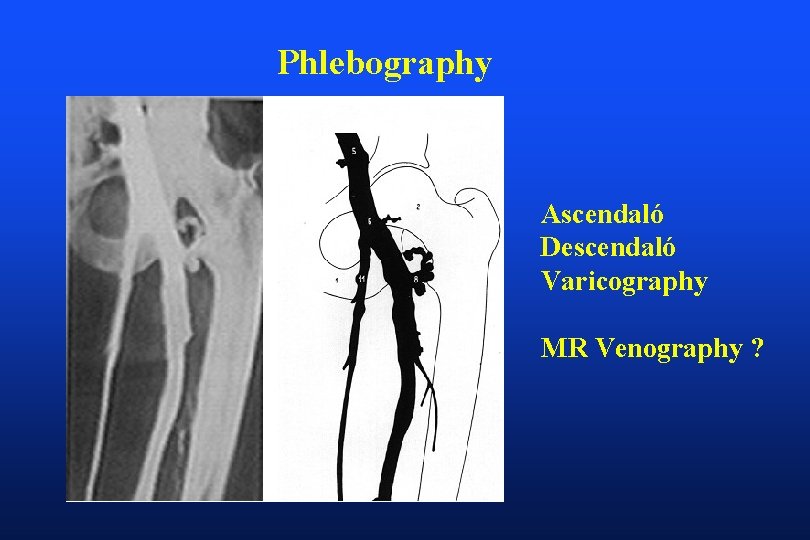
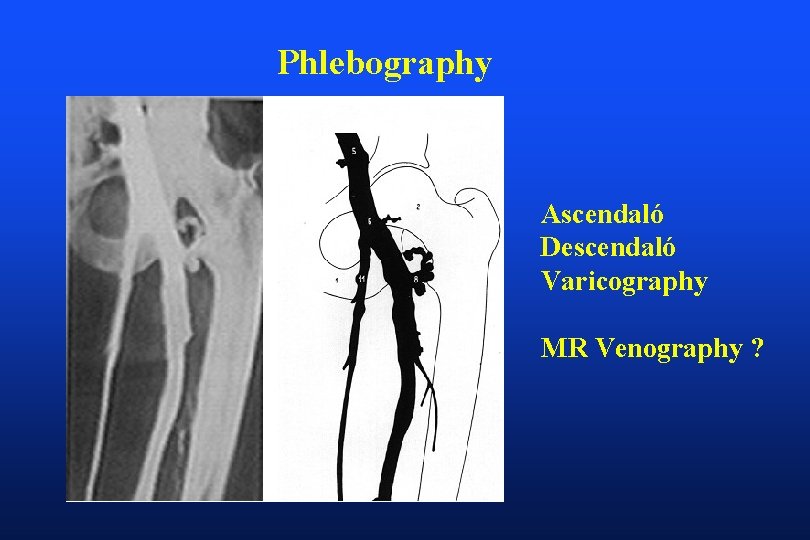
Phlebography Ascendaló Descendaló Varicography MR Venography ?
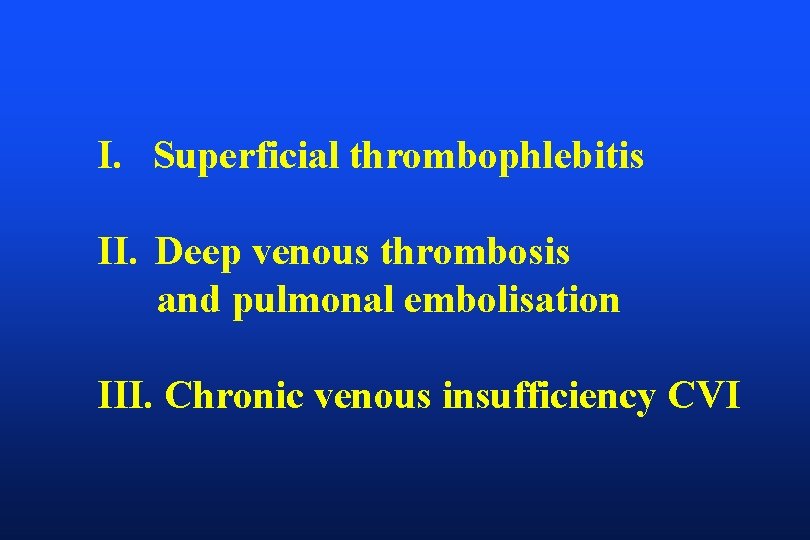
Conclusions - CVI results from venous hypertension usually related to primary reflux in the superficial veins - Heredity is primary risk factor Multiparity increases chance of its expression - Stigmata can vary Depends on veins involved Cosmetic to limb threatening Most patiens have symptoms - Disease occurs in patterns Categorization most important first step