INTEGRATED MANAGEMENT OF NEONATAL AND CHILDHOOD ILLNESSES IMNCI
































- Slides: 150

INTEGRATED MANAGEMENT OF NEONATAL AND CHILDHOOD ILLNESSES (IMNCI) 2/25/2021 Mrs. Sharin Neetal D'souza 1
INTEGRATED MANAGEMENT OF NEONATAL AND CHILDHOOD ILLNESSES (IMNCI) Prepared by: Mrs. Sharin Neetal D’souza Lecturer Dept. Child health nursing Yenepoya nursing college 2/25/2021 Reviewed by: Prof. Umarani J Dr. Priya Reshma Aranha Mrs. Sharin Neetal D'souza 2
Learning objectives At the end of the class students will be able to • define IMNCI • list the objectives • find the beneficiaries of IMNCI • enumerate the components • explain the principles • explain the colour codes of IMNCI 2/25/2021 Mrs. Sharin Neetal D'souza 3
2/25/2021 Mrs. Sharin Neetal D'souza 4
2/25/2021 Mrs. Sharin Neetal D'souza 5
2/25/2021 Mrs. Sharin Neetal D'souza 6

2/25/2021 Mrs. Sharin Neetal D'souza 7
2/25/2021 Mrs. Sharin Neetal D'souza 8

2/25/2021 Mrs. Sharin Neetal D'souza 9
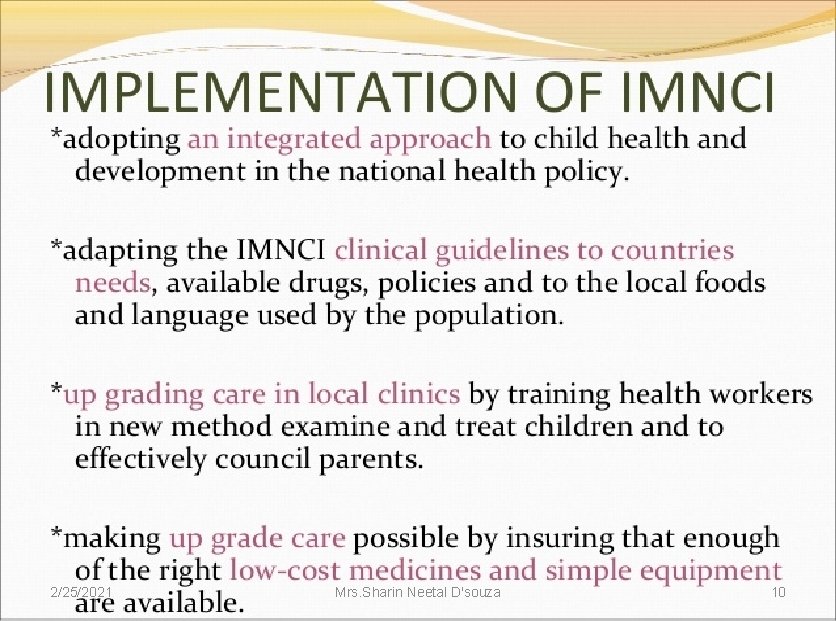
2/25/2021 Mrs. Sharin Neetal D'souza 10
2/25/2021 Mrs. Sharin Neetal D'souza 11

2/25/2021 Mrs. Sharin Neetal D'souza 12
2/25/2021 Mrs. Sharin Neetal D'souza 13
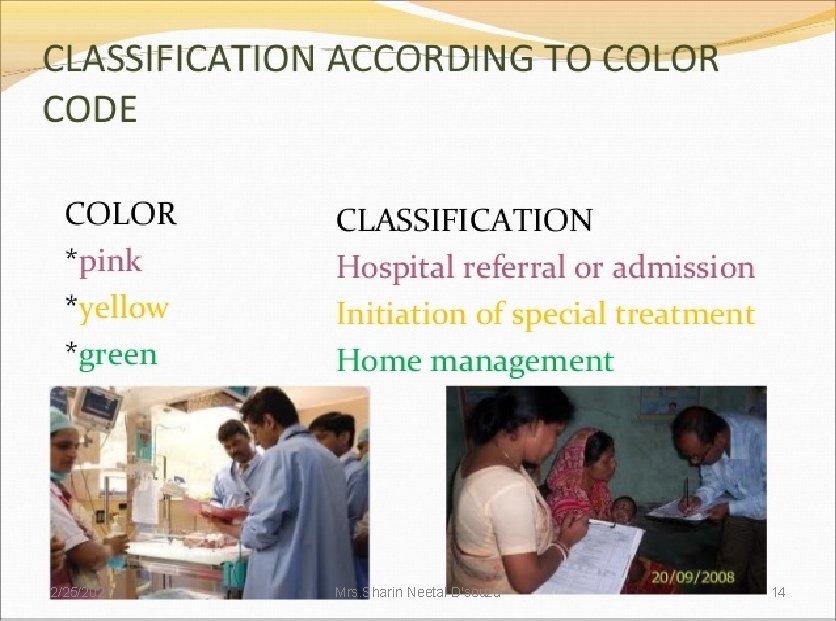
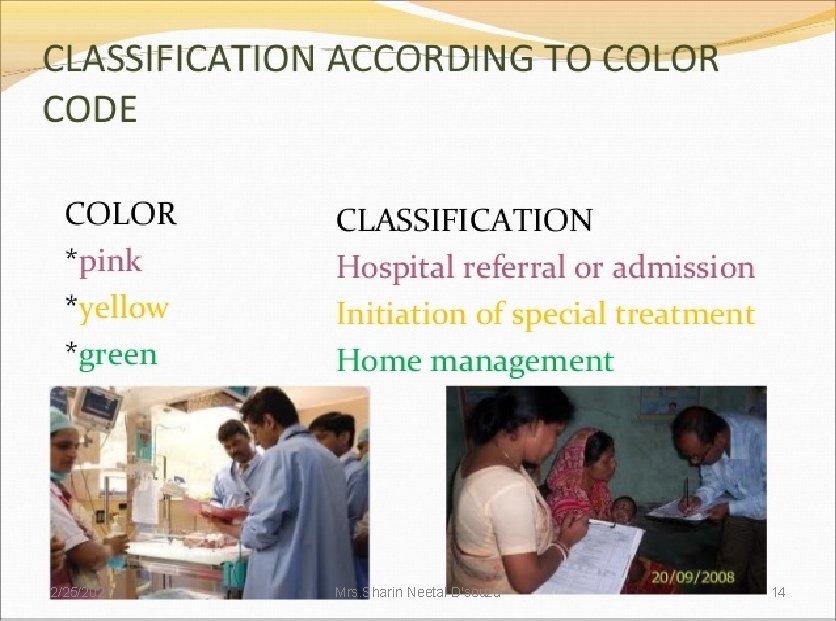
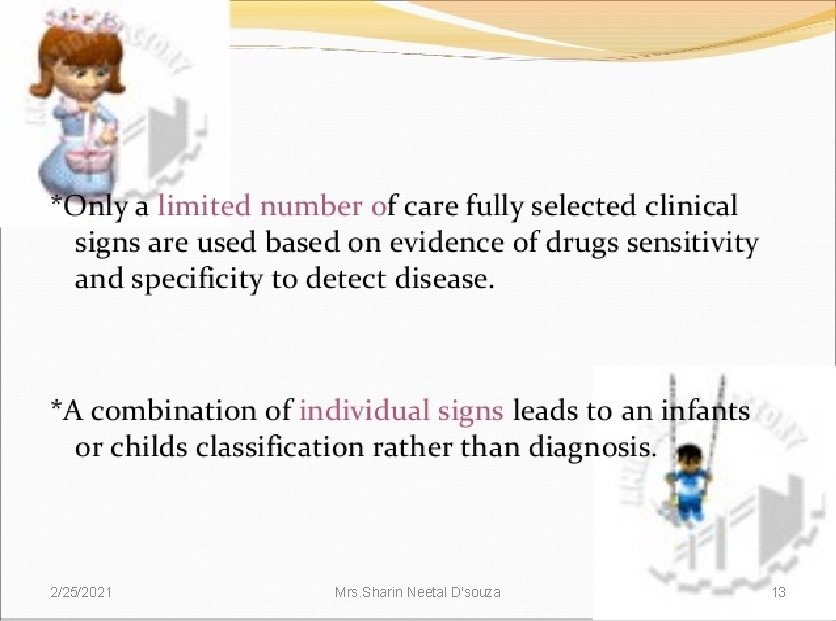
2/25/2021 Mrs. Sharin Neetal D'souza 14
2/25/2021 Mrs. Sharin Neetal D'souza 15
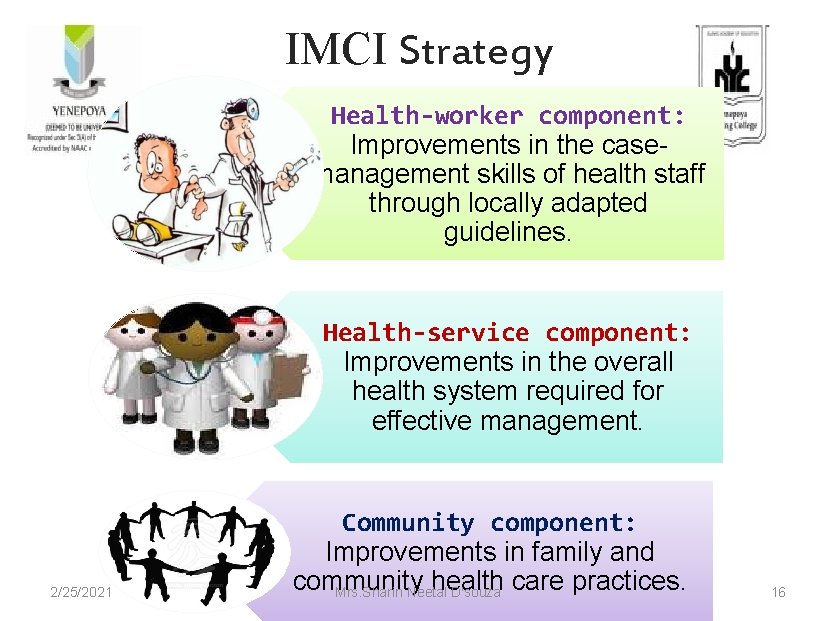
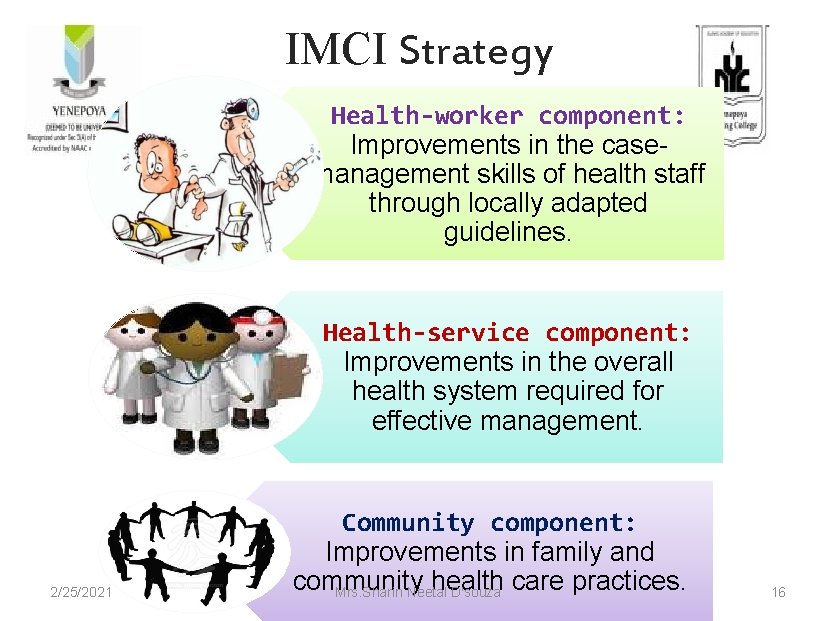
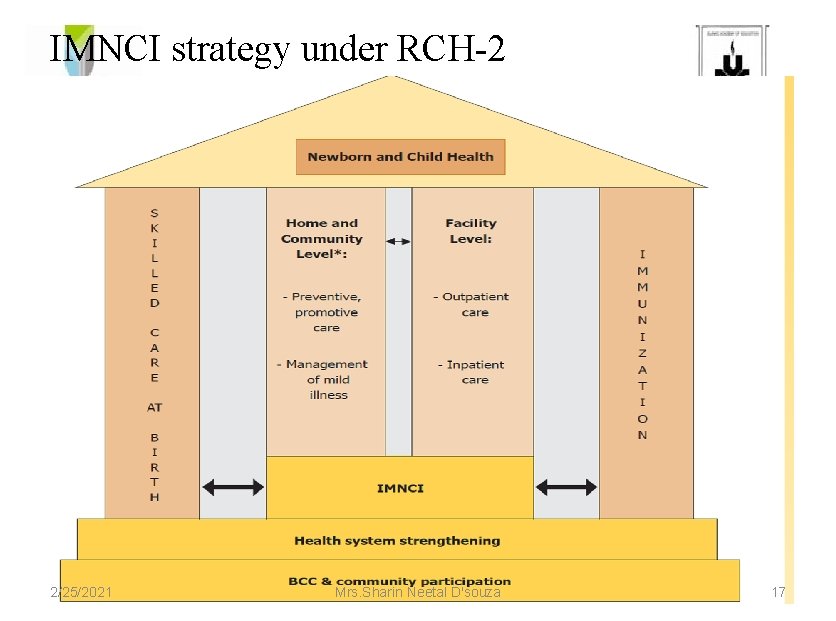
IMCI Strategy Health-worker component: Improvements in the casemanagement skills of health staff through locally adapted guidelines. Health-service component: Improvements in the overall health system required for effective management. 2/25/2021 Community component: Improvements in family and community health care practices. Mrs. Sharin Neetal D'souza 16
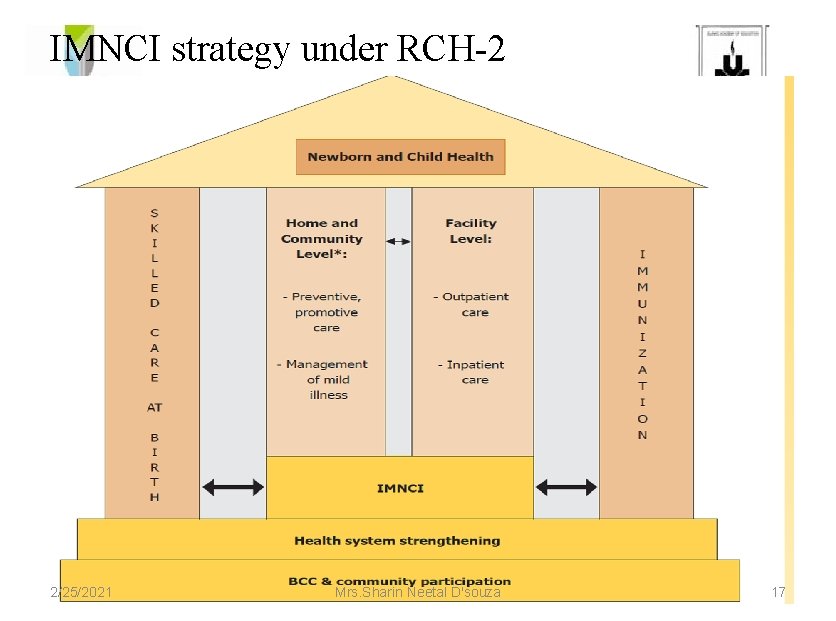
IMNCI strategy under RCH-2 2/25/2021 Mrs. Sharin Neetal D'souza 17
Learning objectives At the end of the class students will be able to • list the elements of IMNCI • explain the management of child with various disease conditions under IMNCI process with the age group of below 2 months and 2 months – 5 years 2/25/2021 Mrs. Sharin Neetal D'souza 18
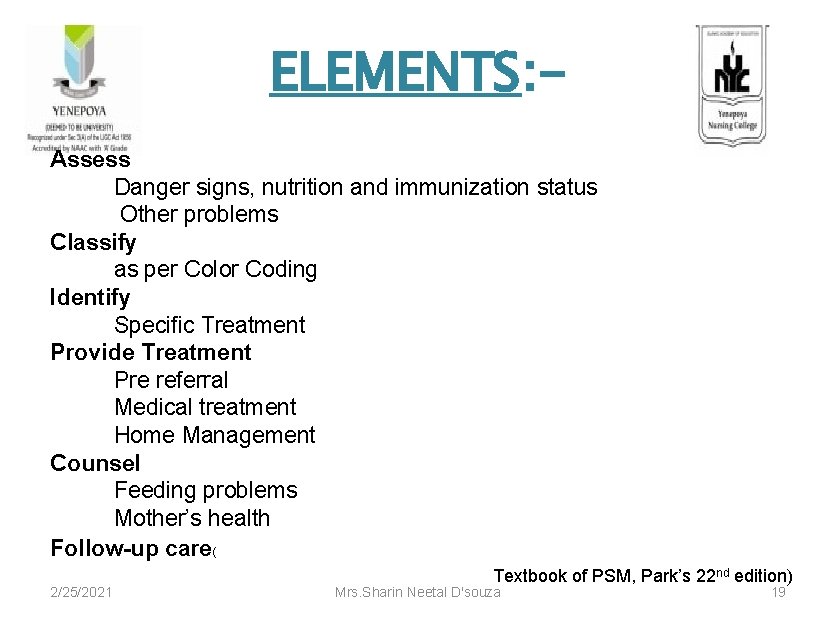
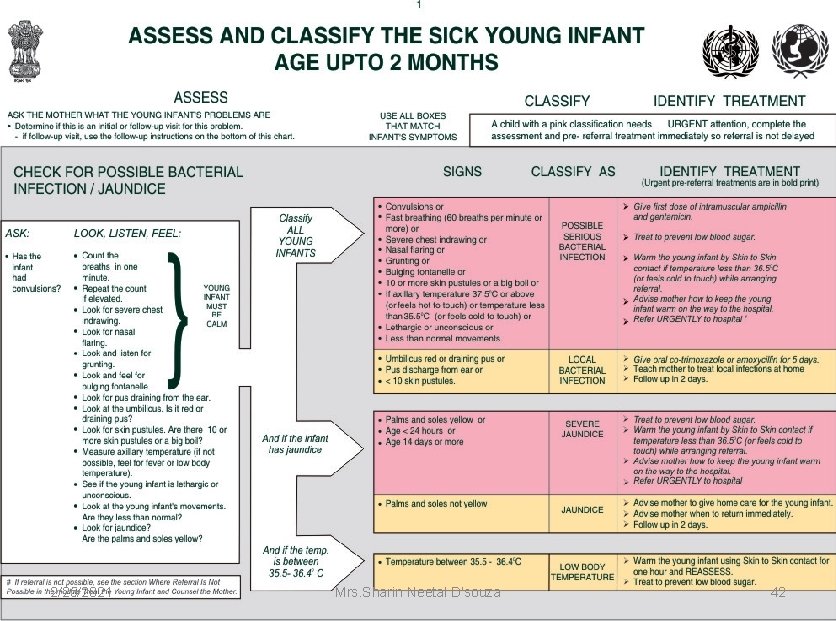
ELEMENTS: Assess Danger signs, nutrition and immunization status Other problems Classify as per Color Coding Identify Specific Treatment Provide Treatment Pre referral Medical treatment Home Management Counsel Feeding problems Mother’s health Follow-up care( 2/25/2021 Textbook of PSM, Park’s 22 nd edition) Mrs. Sharin Neetal D'souza 19

2/25/2021 Mrs. Sharin Neetal D'souza 20
2/25/2021 Mrs. Sharin Neetal D'souza 21
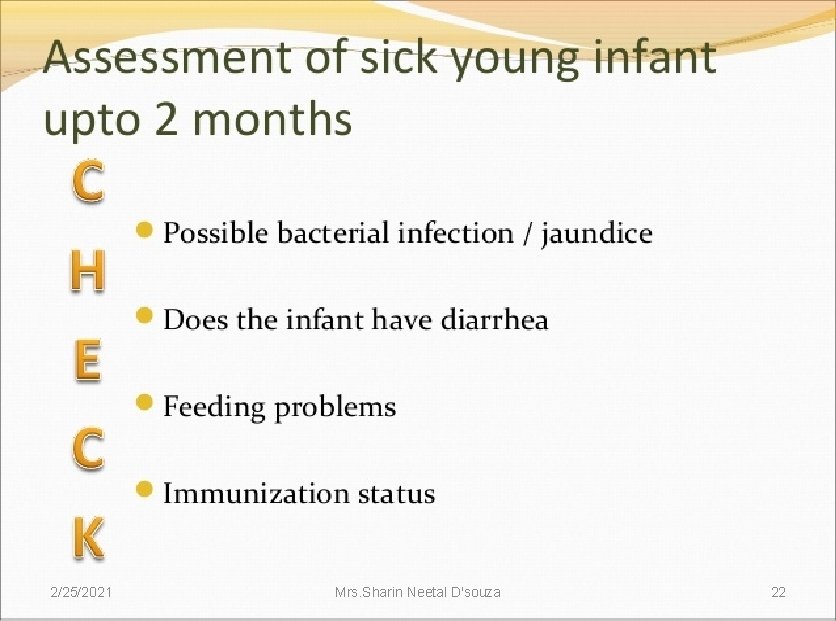
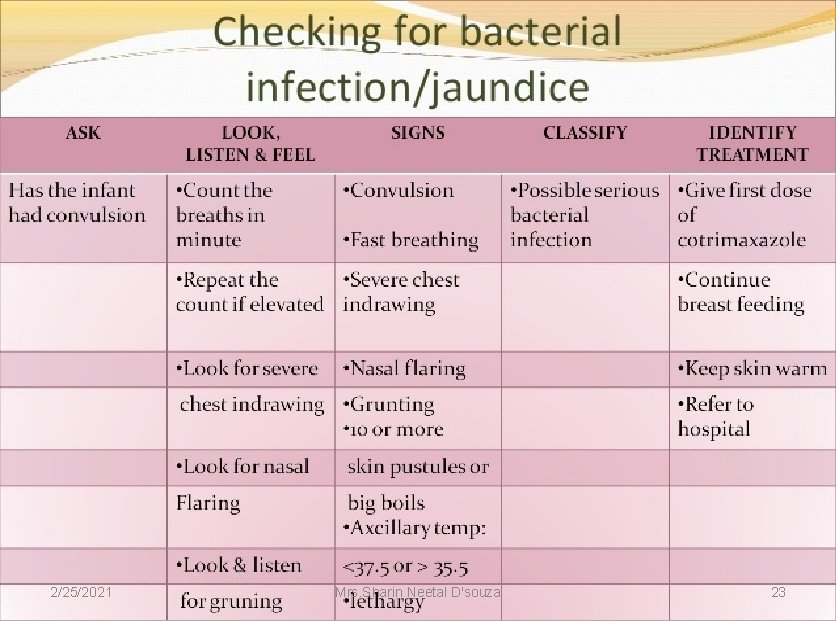
2/25/2021 Mrs. Sharin Neetal D'souza 22
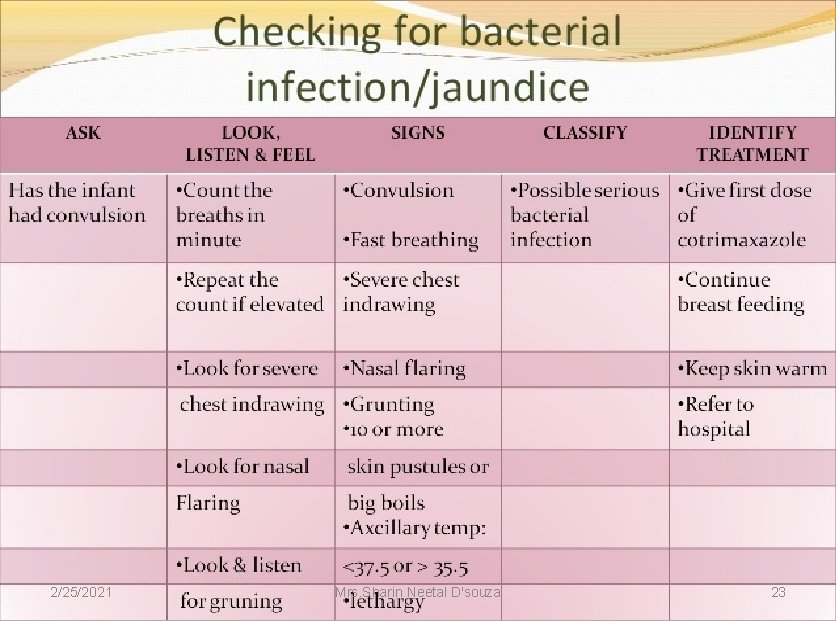
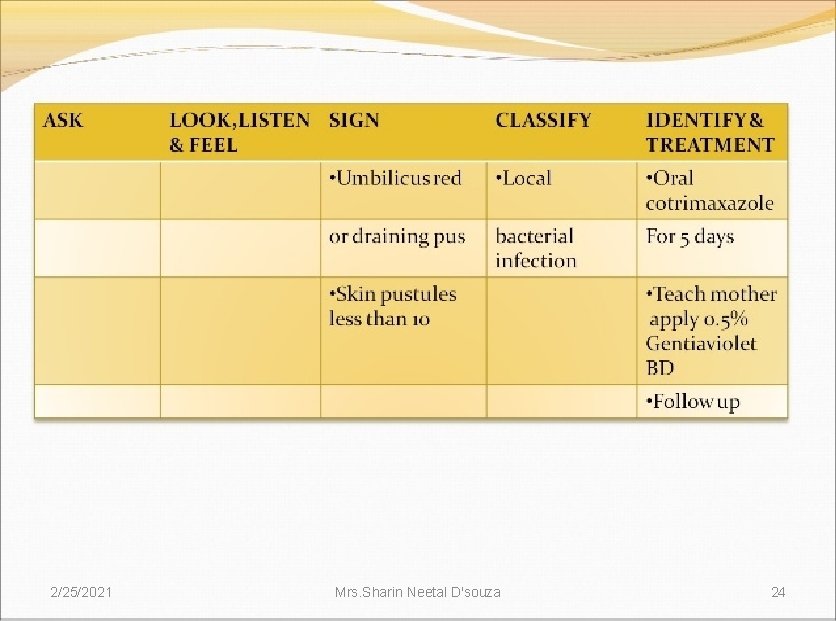
2/25/2021 Mrs. Sharin Neetal D'souza 23
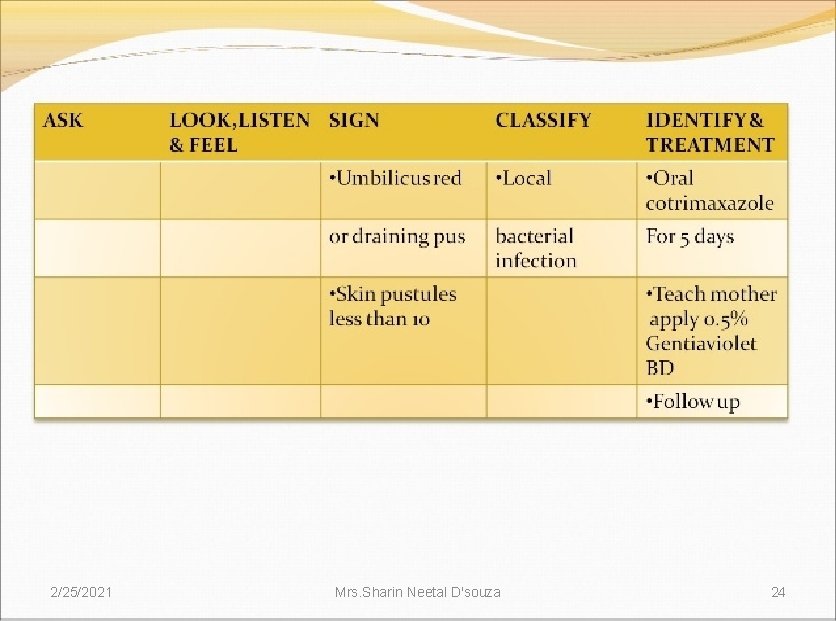
2/25/2021 Mrs. Sharin Neetal D'souza 24
Fast breathing 2/25/2021 Mrs. Sharin Neetal D'souza 25

Look for severe chest in drawing 2/25/2021 Mrs. Sharin Neetal D'souza 26
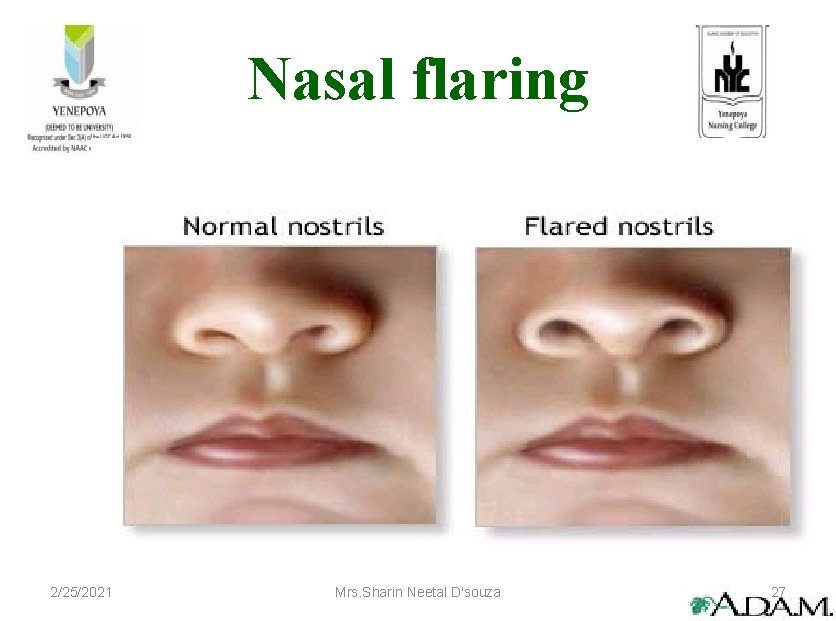
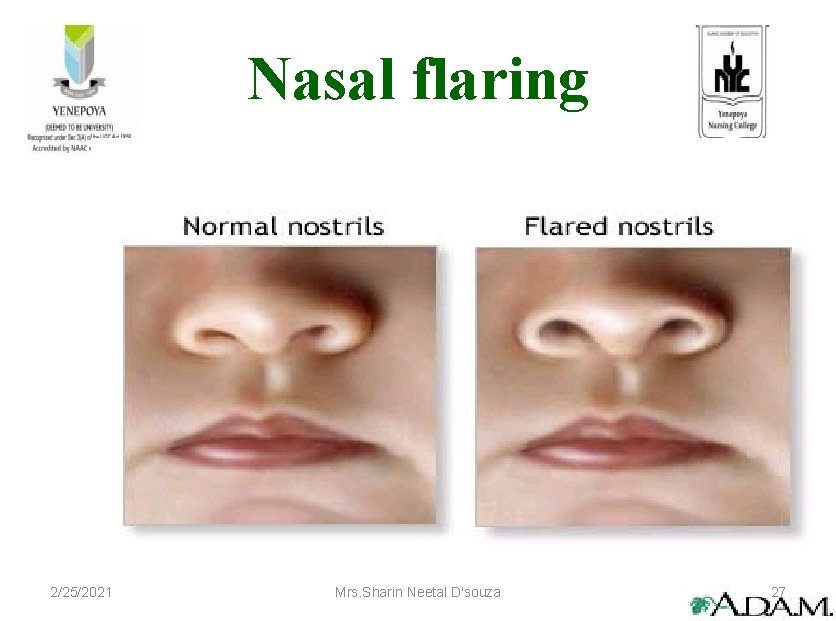
Nasal flaring 2/25/2021 Mrs. Sharin Neetal D'souza 27
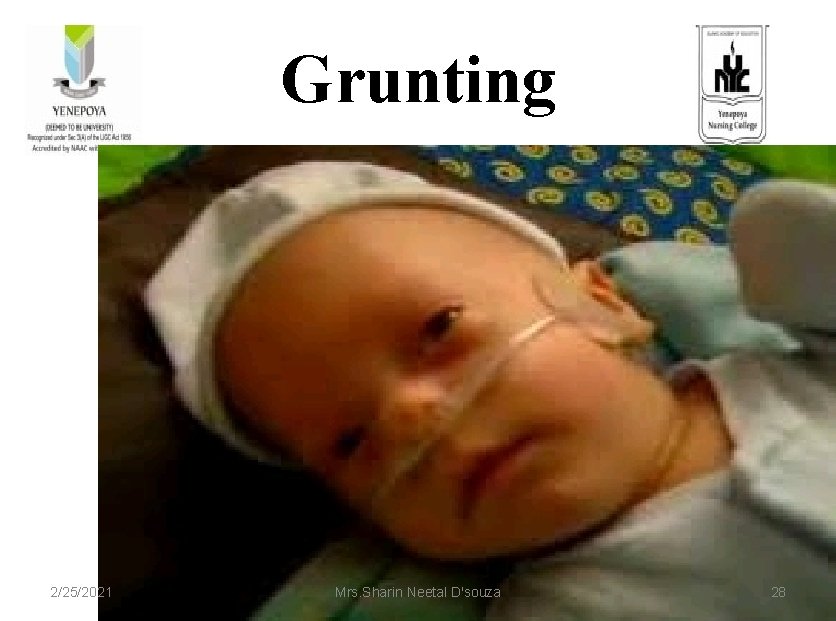
Grunting 2/25/2021 Mrs. Sharin Neetal D'souza 28
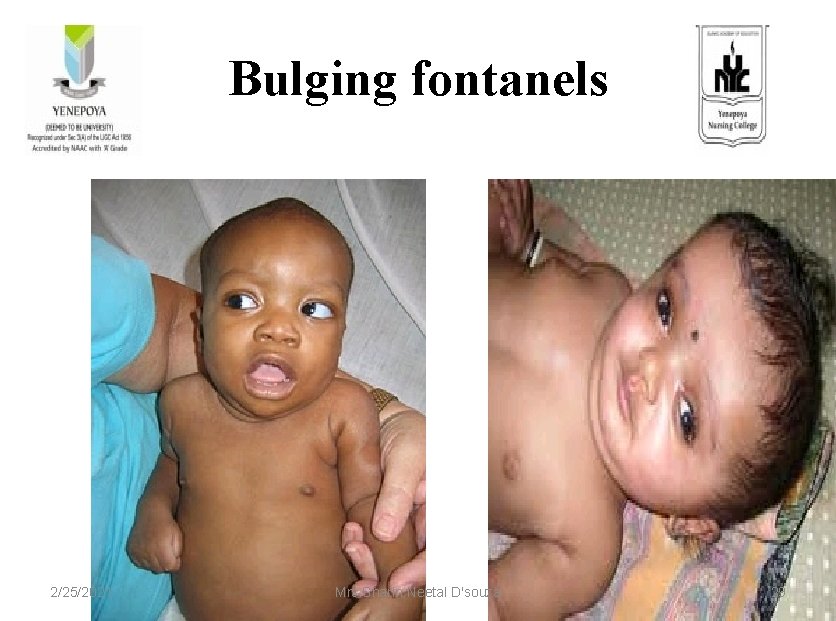
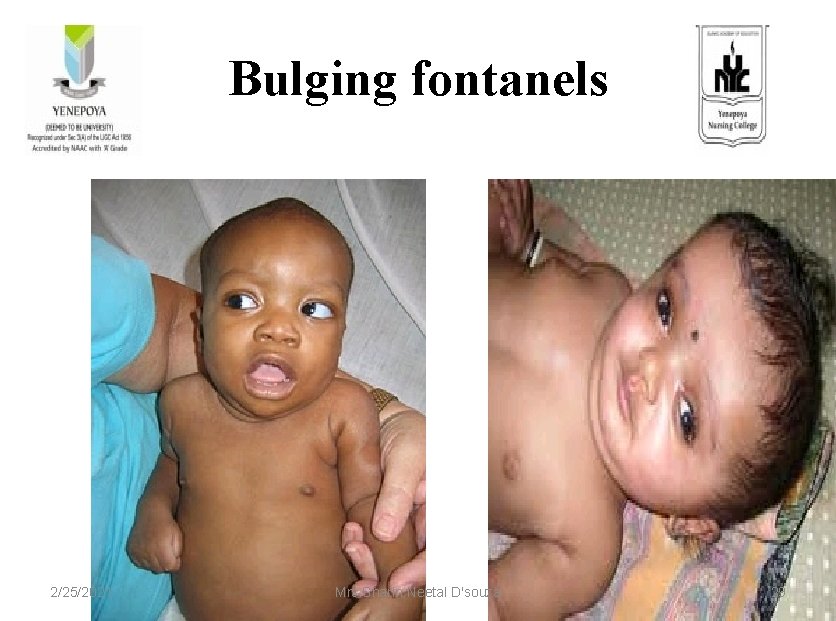
Bulging fontanels 2/25/2021 Mrs. Sharin Neetal D'souza 29
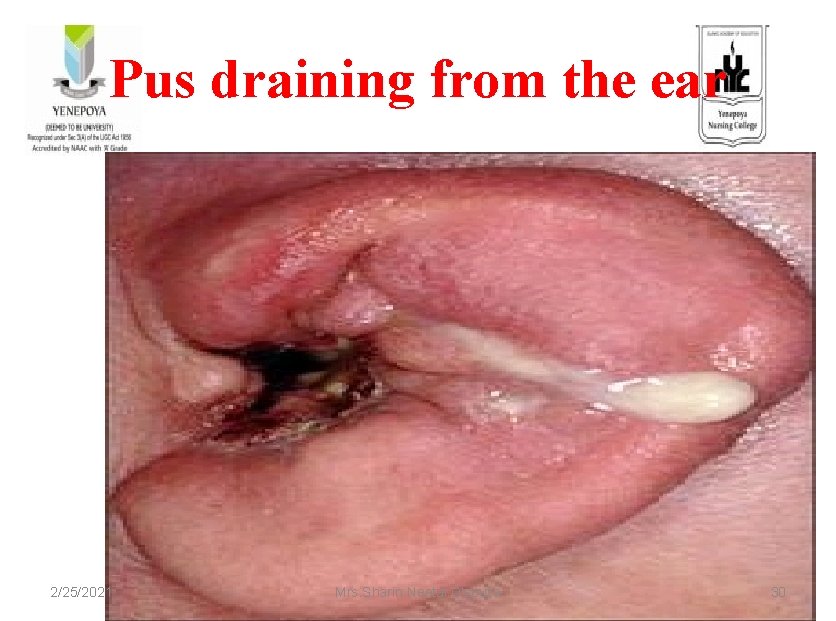
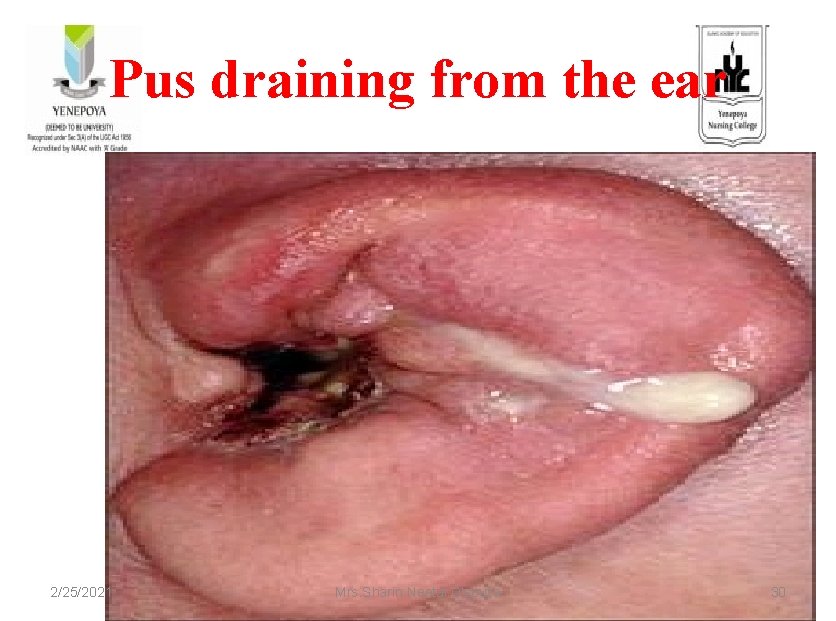
Pus draining from the ear 2/25/2021 Mrs. Sharin Neetal D'souza 30

Skin pustules 2/25/2021 Mrs. Sharin Neetal D'souza 31
Temperature 2/25/2021 Mrs. Sharin Neetal D'souza 32
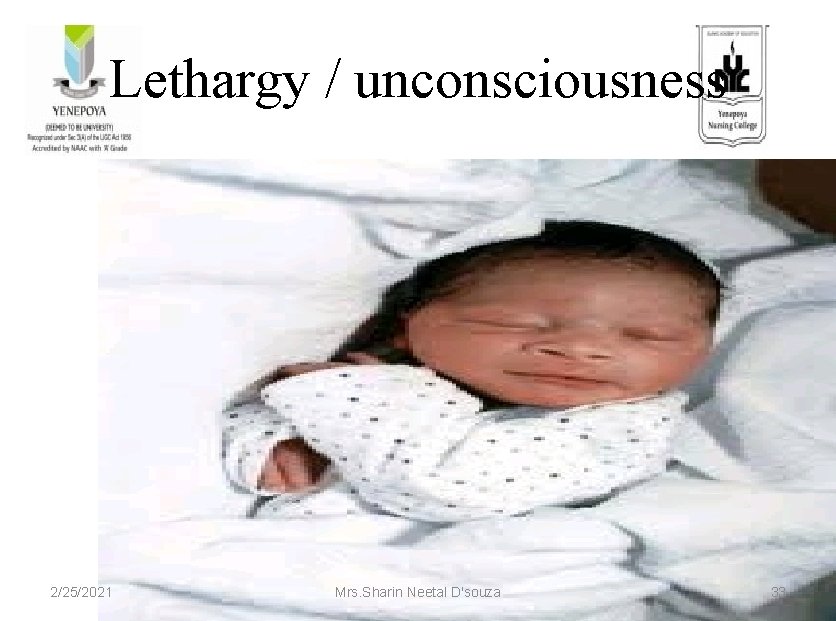
Lethargy / unconsciousness 2/25/2021 Mrs. Sharin Neetal D'souza 33

Jaundice 2/25/2021 Mrs. Sharin Neetal D'souza 34
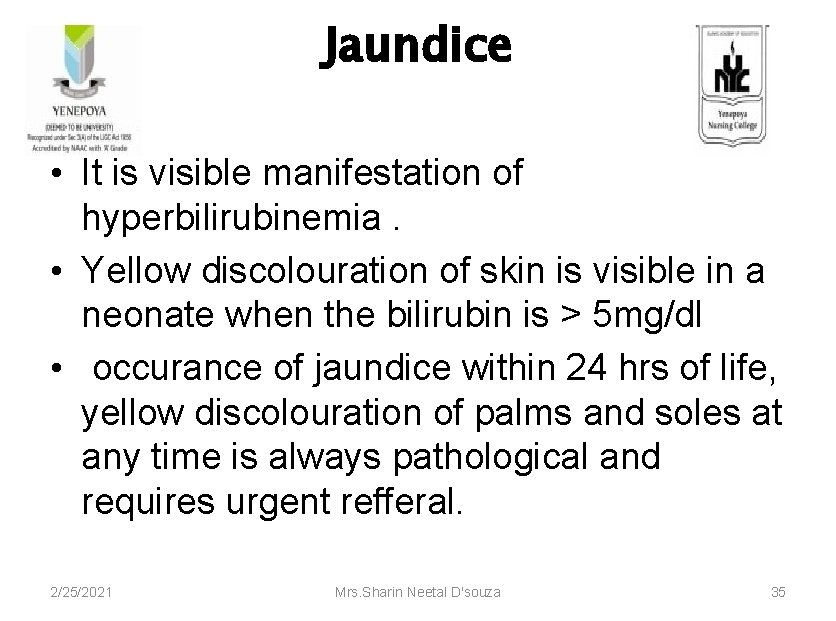
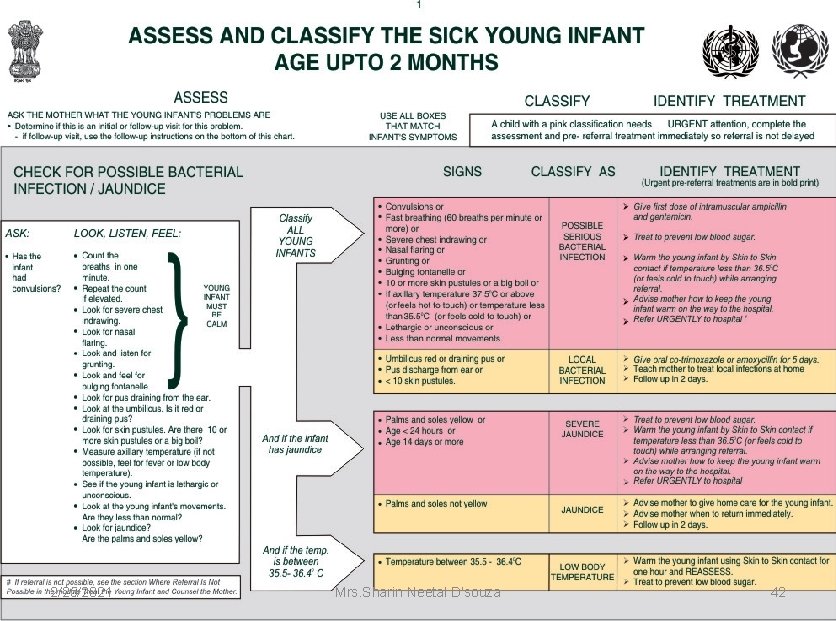
Jaundice • It is visible manifestation of hyperbilirubinemia. • Yellow discolouration of skin is visible in a neonate when the bilirubin is > 5 mg/dl • occurance of jaundice within 24 hrs of life, yellow discolouration of palms and soles at any time is always pathological and requires urgent refferal. 2/25/2021 Mrs. Sharin Neetal D'souza 35
CLASSIFICATION OF JAUNDICE Severe jaundice 2/25/2021 Mrs. Sharin Neetal D'souza jaundice 36
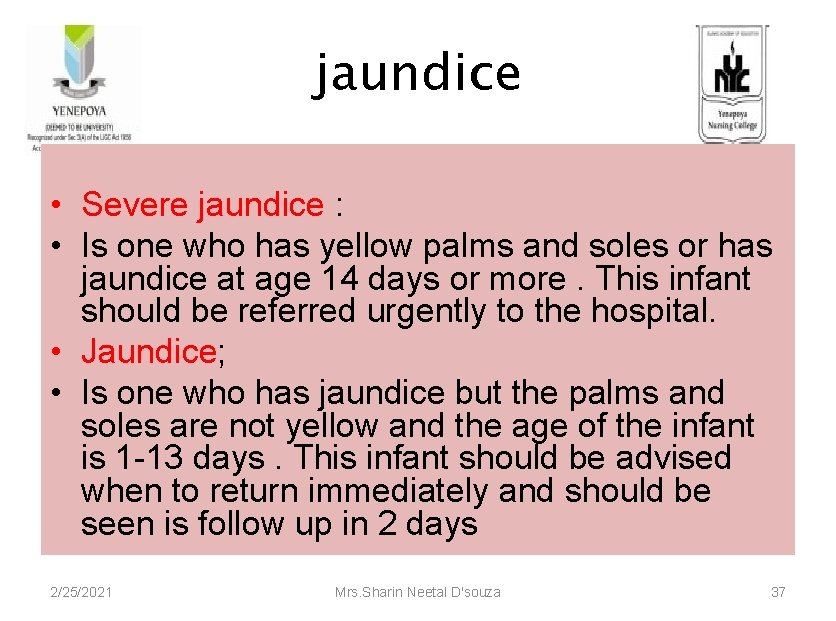
jaundice • Severe jaundice : • Is one who has yellow palms and soles or has jaundice at age 14 days or more. This infant should be referred urgently to the hospital. • Jaundice; • Is one who has jaundice but the palms and soles are not yellow and the age of the infant is 1 -13 days. This infant should be advised when to return immediately and should be seen is follow up in 2 days 2/25/2021 Mrs. Sharin Neetal D'souza 37
SEVERE JAUNDICE • Yellow palms and soles • Age < 24 hours • Age 14 days or more 2/25/2021 Mrs. Sharin Neetal D'souza 38
TREATMENT • Refer urgently to the hospital after being given treatment to prevent hypoglycemia • Advice to keep the baby warm 2/25/2021 Mrs. Sharin Neetal D'souza 39

JAUNDICE • Palms and soles not yellow • Age 1 to 13 days 2/25/2021 Mrs. Sharin Neetal D'souza 40
TREATMENT • Home care • Follow up in 2 days 2/25/2021 Mrs. Sharin Neetal D'souza 41
2/25/2021 Mrs. Sharin Neetal D'souza 42
2/25/2021 Mrs. Sharin Neetal D'souza 43
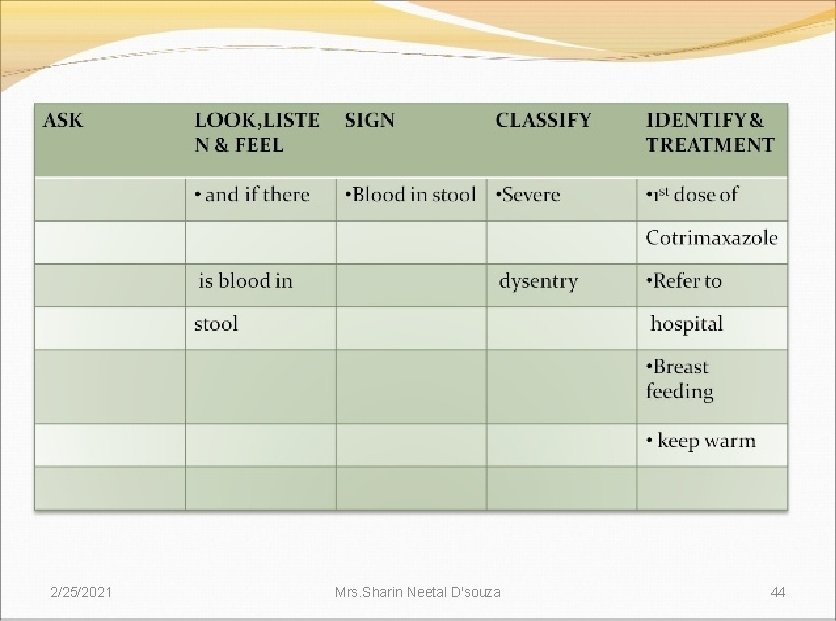
2/25/2021 Mrs. Sharin Neetal D'souza 44
2/25/2021 Mrs. Sharin Neetal D'souza 45

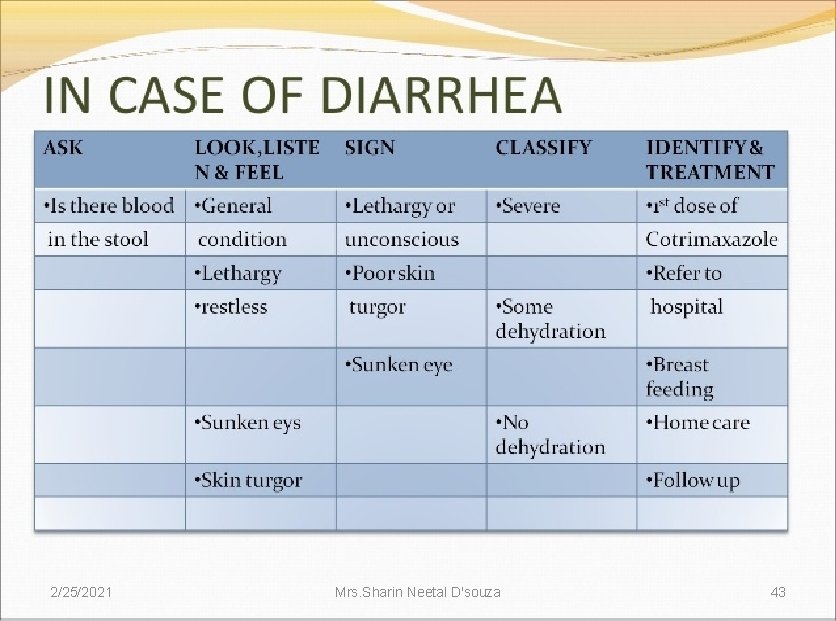
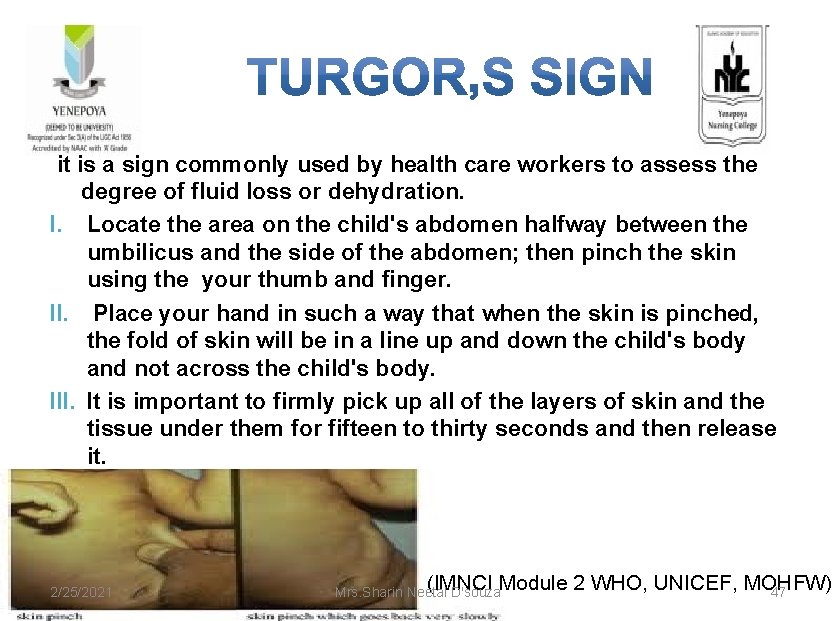
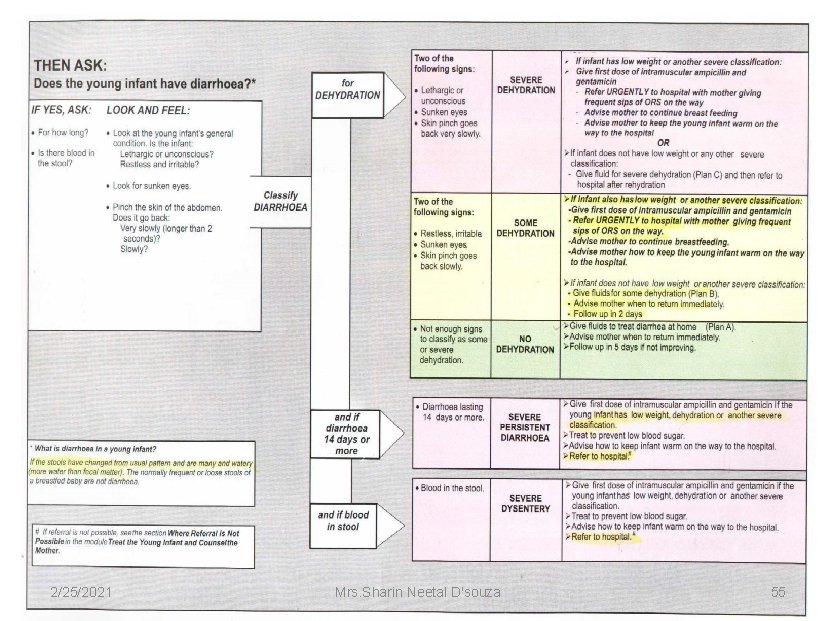
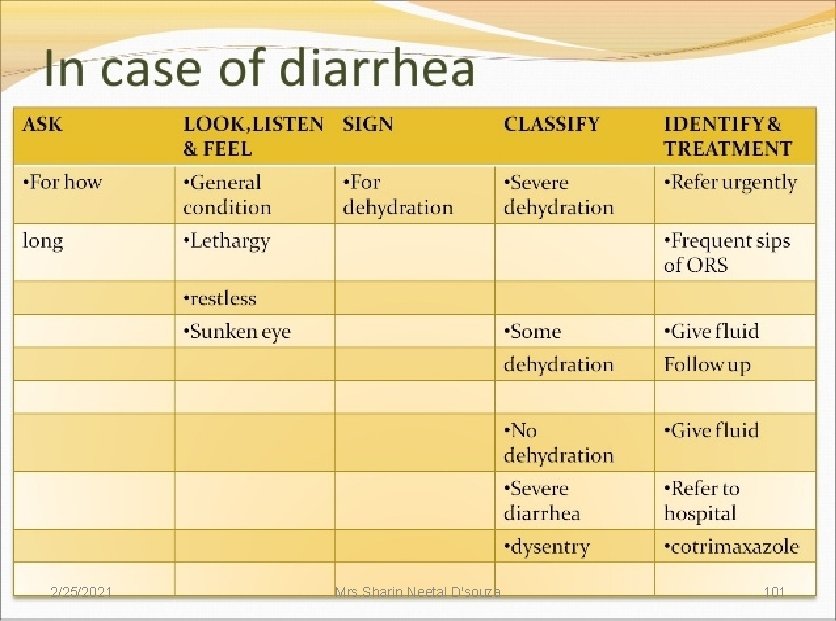
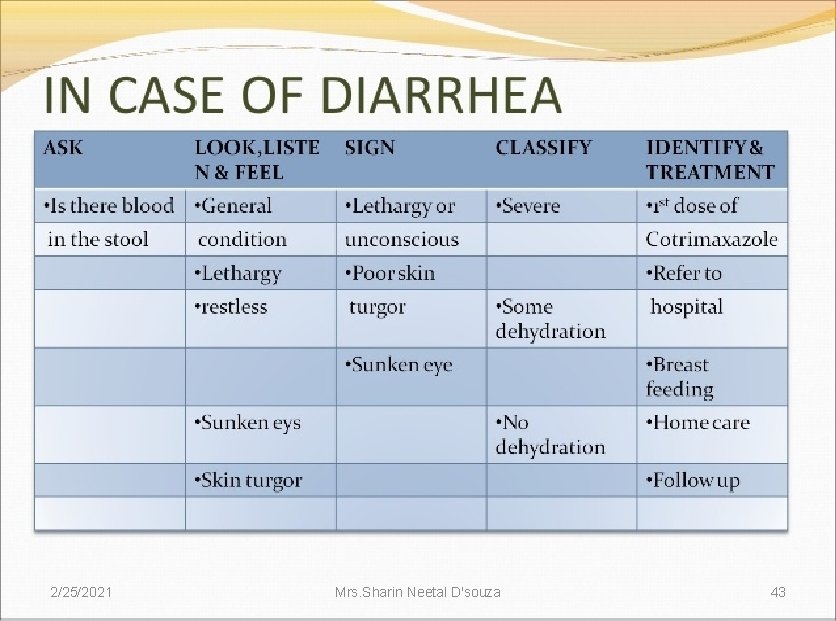
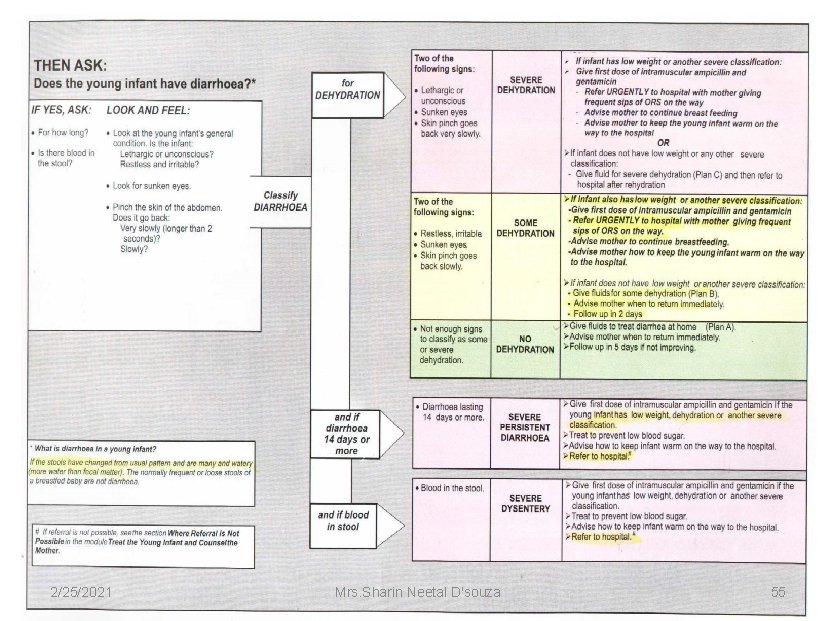
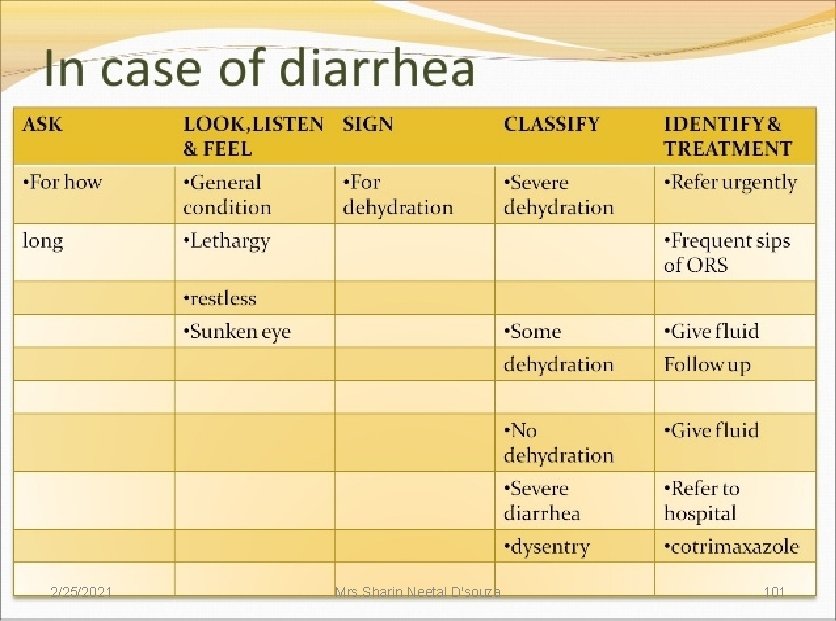
ASK: • Does the child have diarrhea? • IF YES THEN , FOR HOW LONG? LOOK AND FEEL: • Look at the general conditions. Is he/she -lethargic or unconscious? -restless and irritable? • Look for sunken eyes • Pinch the skin of abdomen , and notice how it goes back: -very slowly( longer than two seconds)? -slowly? -immediately? 2/25/2021 Mrs. Sharin Neetal D'souza 46 (IMNCI Module 2 WHO, UNICEF, MOHFW)
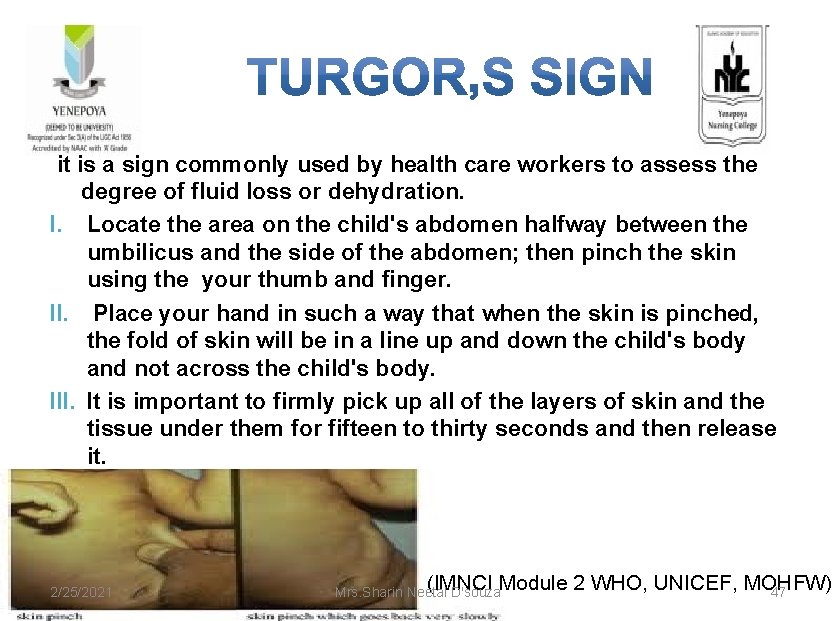
it is a sign commonly used by health care workers to assess the degree of fluid loss or dehydration. I. Locate the area on the child's abdomen halfway between the umbilicus and the side of the abdomen; then pinch the skin using the your thumb and finger. II. Place your hand in such a way that when the skin is pinched, the fold of skin will be in a line up and down the child's body and not across the child's body. III. It is important to firmly pick up all of the layers of skin and the tissue under them for fifteen to thirty seconds and then release it. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 47
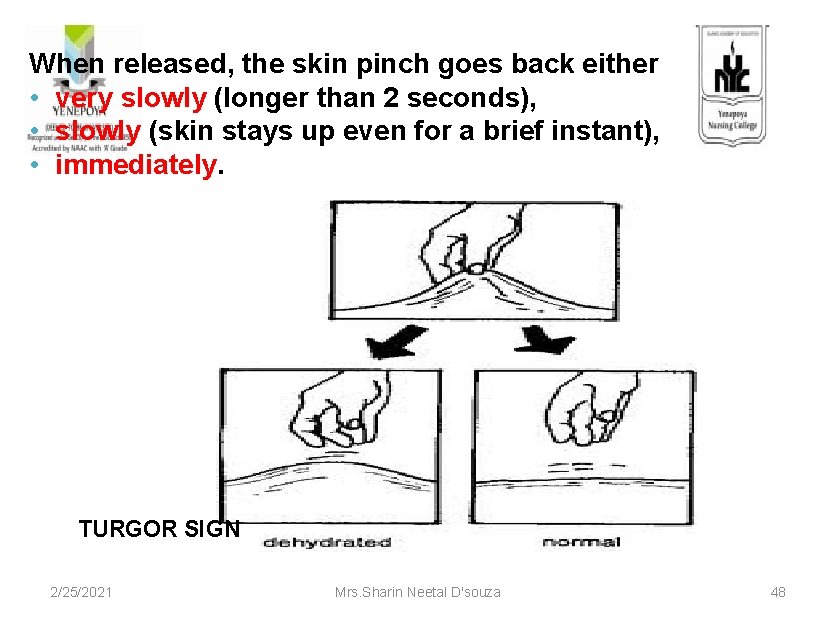
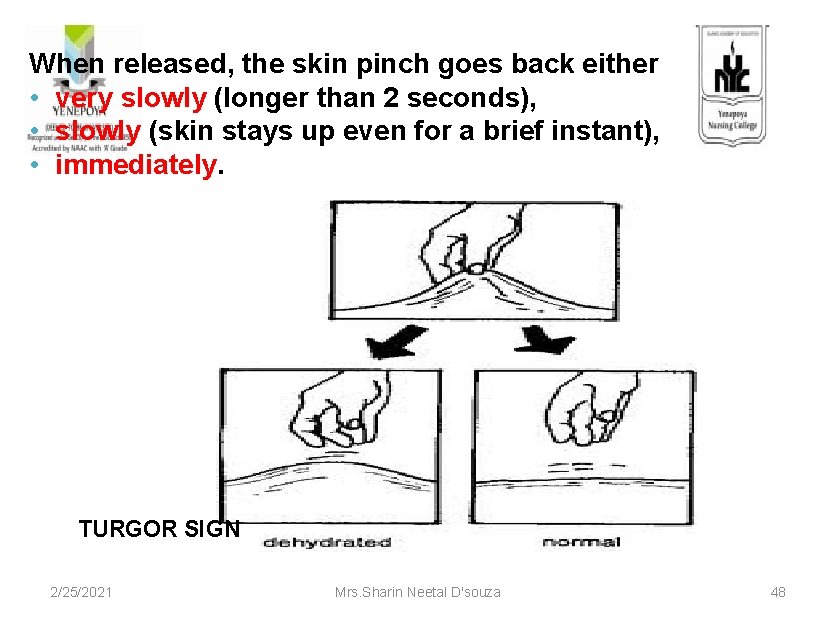
When released, the skin pinch goes back either • very slowly (longer than 2 seconds), • slowly (skin stays up even for a brief instant), • immediately. TURGOR SIGN 2/25/2021 Mrs. Sharin Neetal D'souza 48
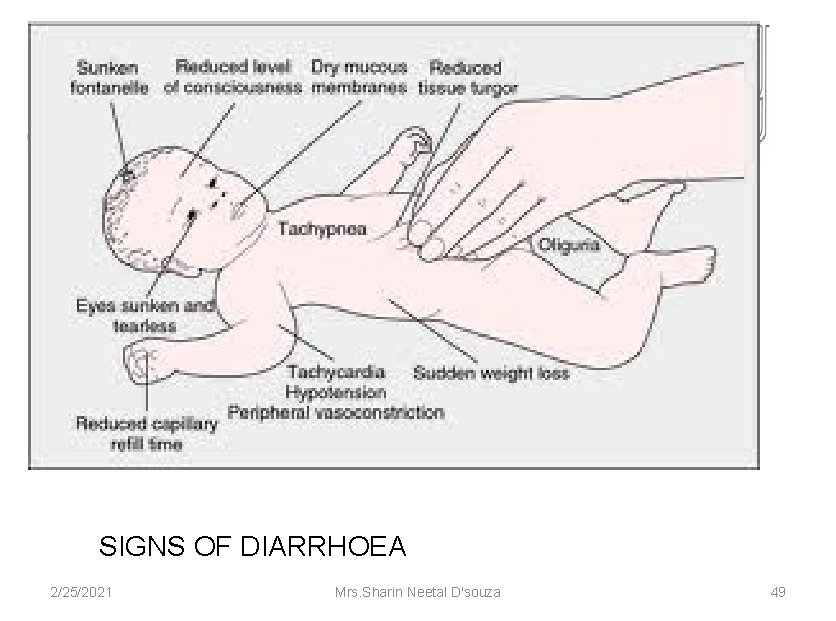
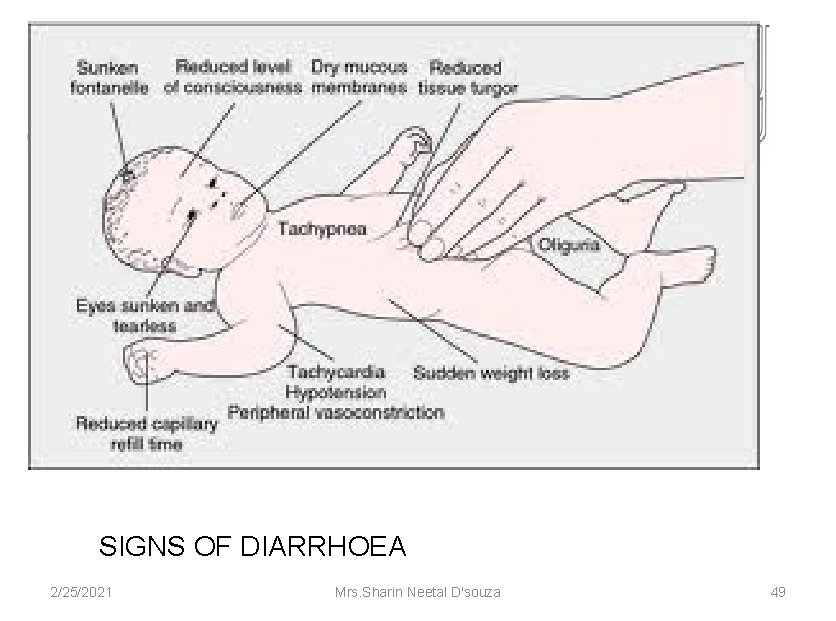
SIGNS OF DIARRHOEA 2/25/2021 Mrs. Sharin Neetal D'souza 49

Classification: Signs Classify treatment Two of the SEVERE following DEHYDRATION signs: Lethargic or unconscious Sunken eyes Skin goes back very slowly 2/25/2021 If infant has low weight or another severe classification: Give first dose of intramuscular ampicillin and gentamicin - Refer URGENTLY to hospital with mother giving frequent sips of ORS on the way - Advise mother to continue breast feeding - Advise mother to keep the young infant warm on the way to the hospital OR If infant does not have low weight or any other severe classification: - Give fluid for severe dehydration (Plan C) and then refer to hospital after rehydration Mrs. Sharin Neetal D'souza 50 (IMNCI Module 2 WHO, UNICEF, MOHFW)
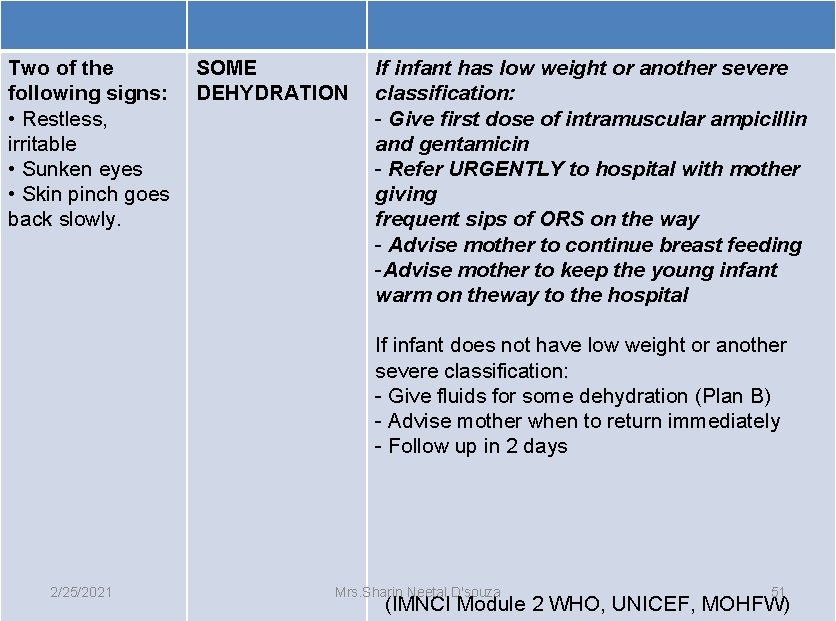
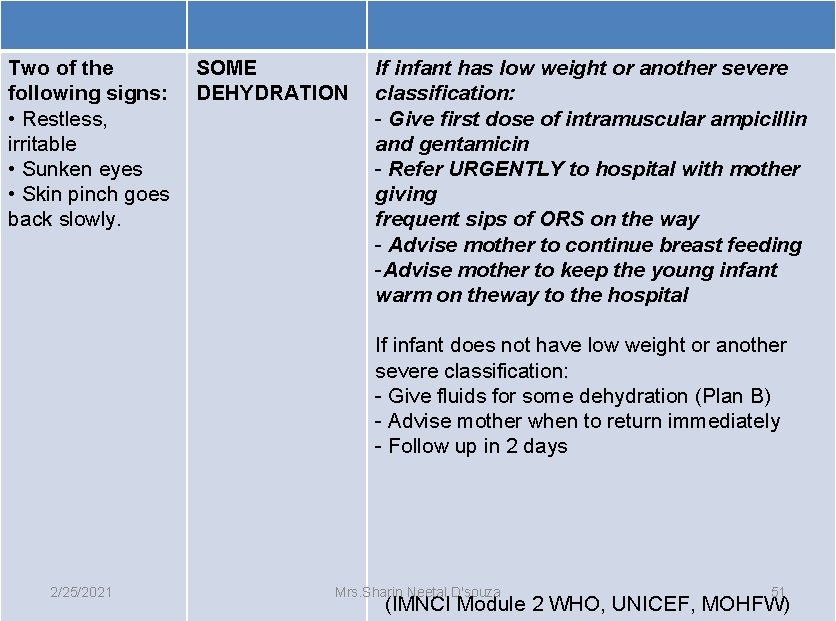
Two of the following signs: • Restless, irritable • Sunken eyes • Skin pinch goes back slowly. SOME DEHYDRATION If infant has low weight or another severe classification: - Give first dose of intramuscular ampicillin and gentamicin - Refer URGENTLY to hospital with mother giving frequent sips of ORS on the way - Advise mother to continue breast feeding -Advise mother to keep the young infant warm on theway to the hospital If infant does not have low weight or another severe classification: - Give fluids for some dehydration (Plan B) - Advise mother when to return immediately - Follow up in 2 days 2/25/2021 Mrs. Sharin Neetal D'souza 51 (IMNCI Module 2 WHO, UNICEF, MOHFW)
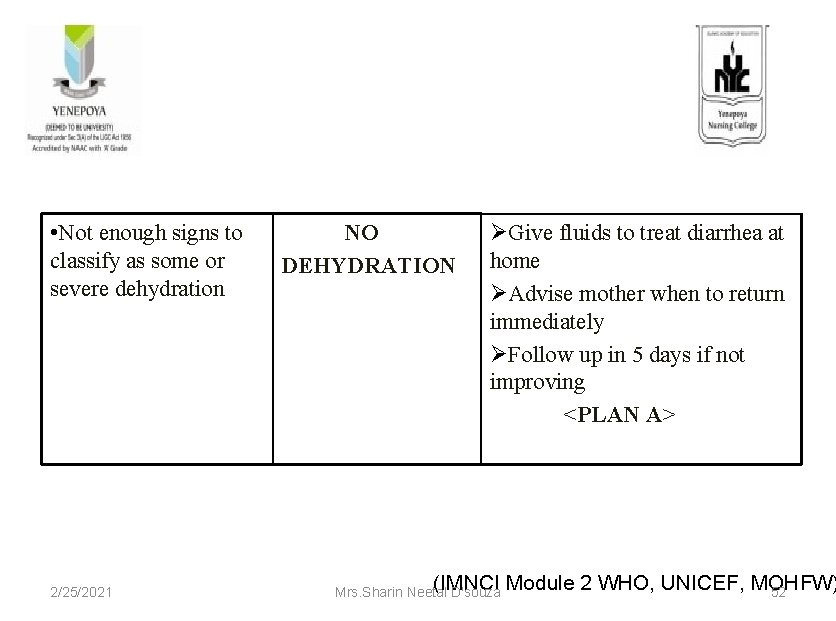
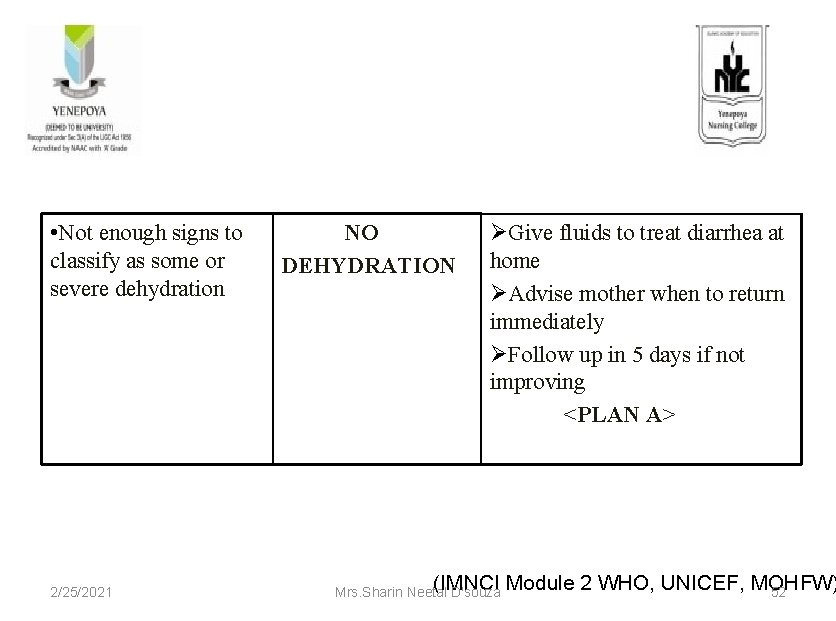
• Not enough signs to classify as some or severe dehydration 2/25/2021 NO DEHYDRATION ØGive fluids to treat diarrhea at home ØAdvise mother when to return immediately ØFollow up in 5 days if not improving <PLAN A> (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 52
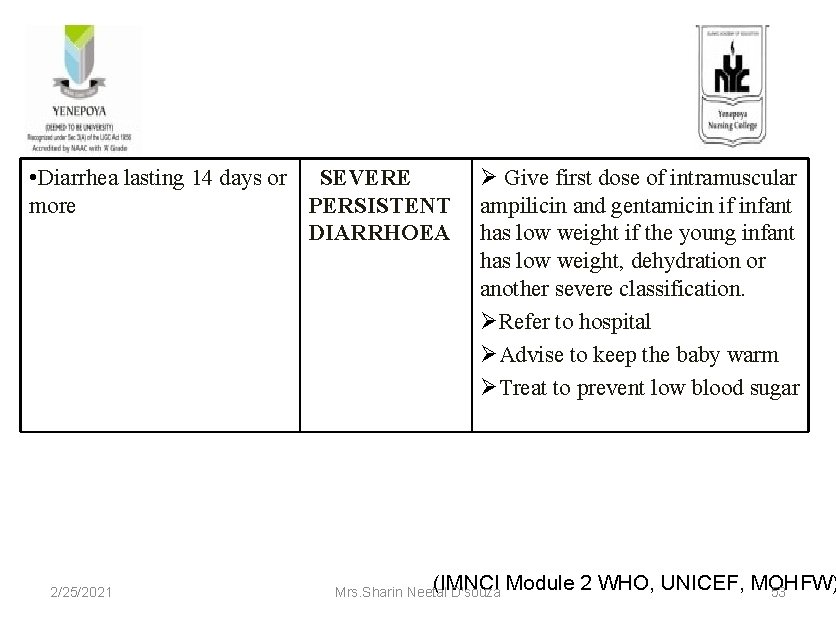
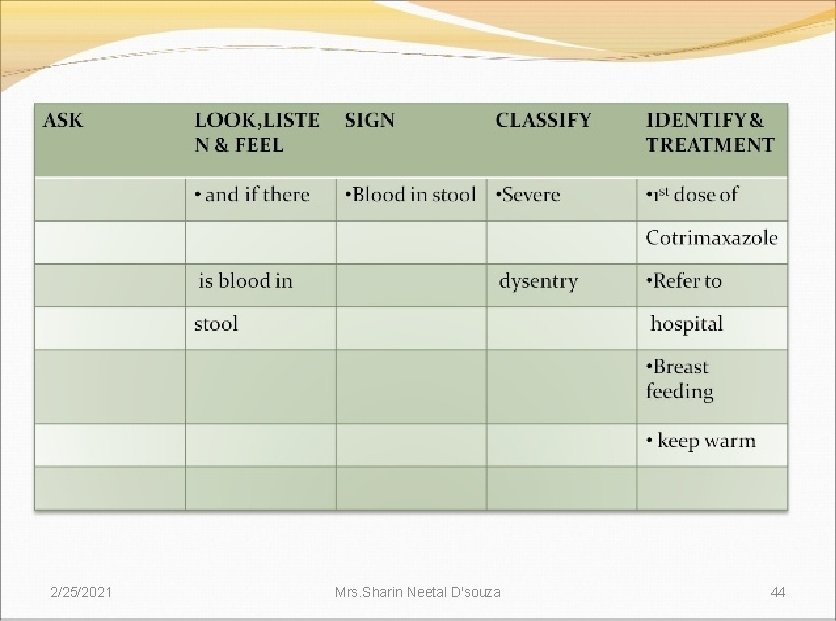
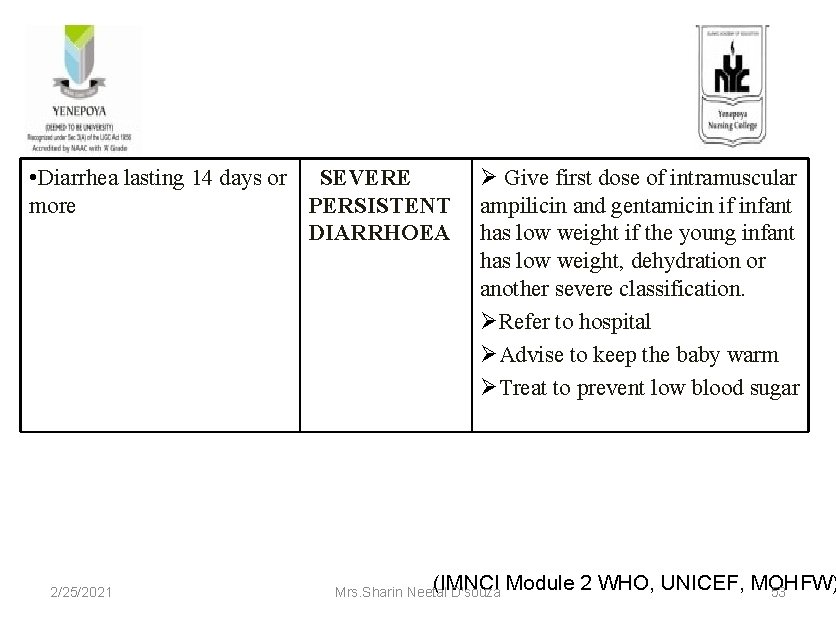
• Diarrhea lasting 14 days or SEVERE more PERSISTENT DIARRHOEA 2/25/2021 Ø Give first dose of intramuscular ampilicin and gentamicin if infant has low weight if the young infant has low weight, dehydration or another severe classification. ØRefer to hospital ØAdvise to keep the baby warm ØTreat to prevent low blood sugar (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 53
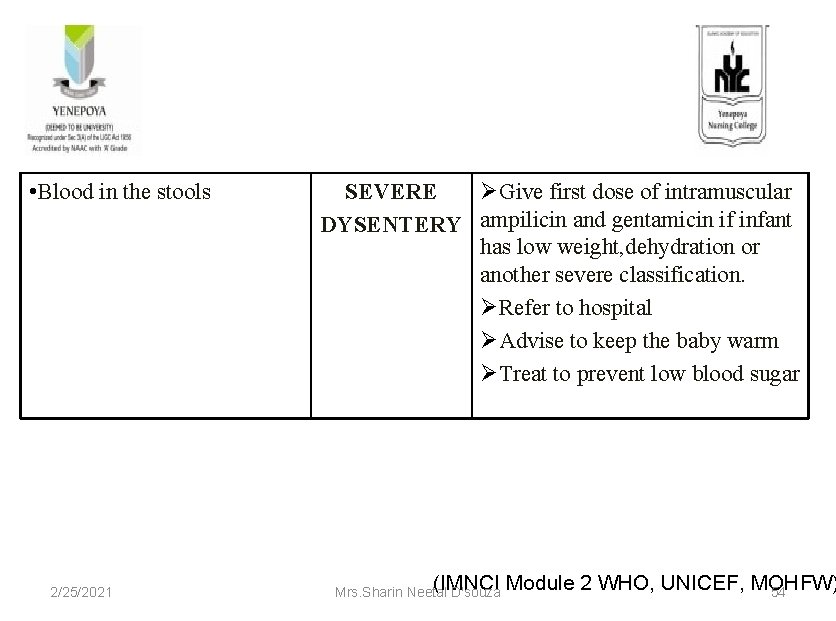
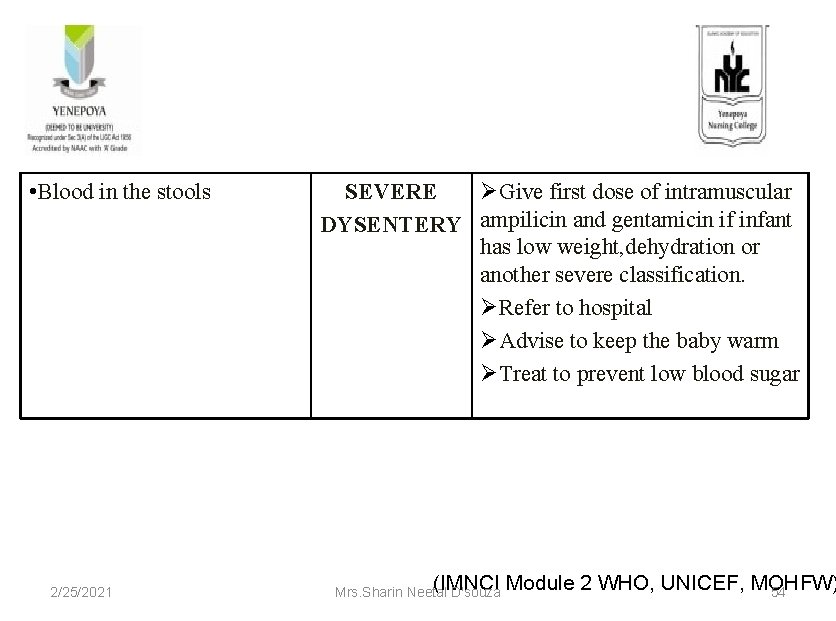
• Blood in the stools 2/25/2021 SEVERE ØGive first dose of intramuscular DYSENTERY ampilicin and gentamicin if infant has low weight, dehydration or another severe classification. ØRefer to hospital ØAdvise to keep the baby warm ØTreat to prevent low blood sugar (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 54
2/25/2021 Mrs. Sharin Neetal D'souza 55

2/25/2021 Mrs. Sharin Neetal D'souza 56
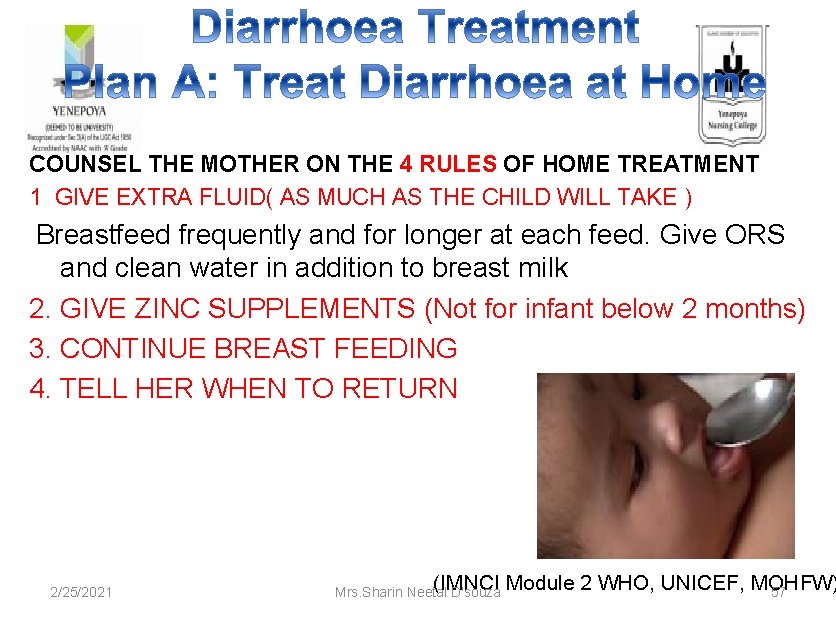
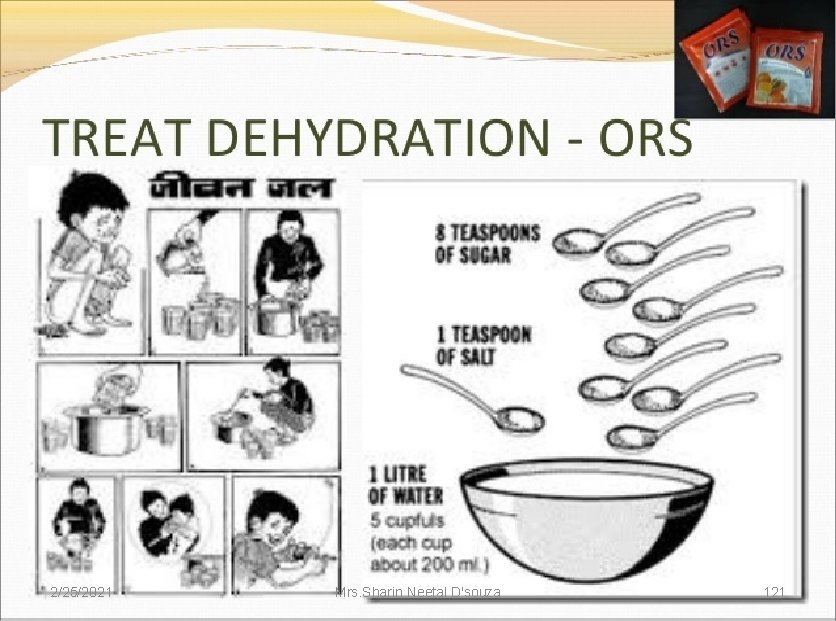
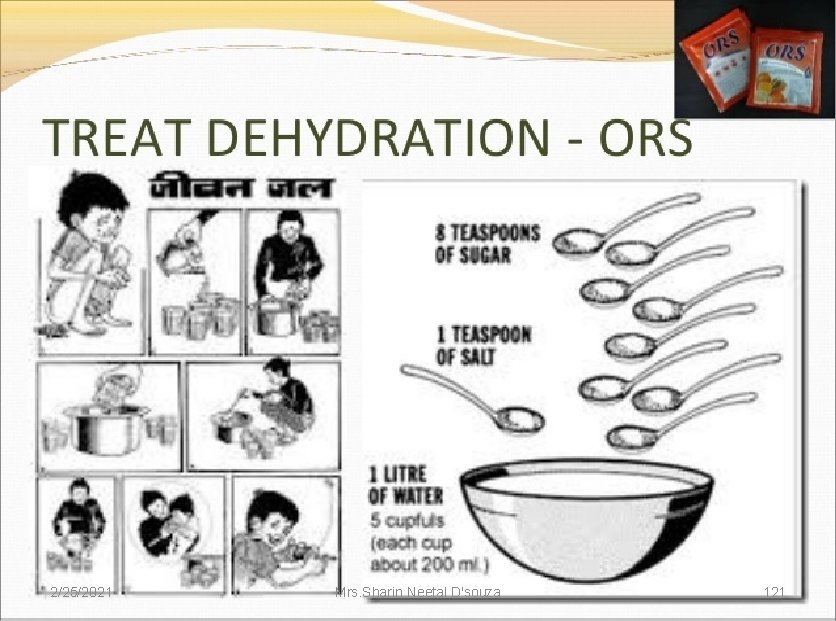
COUNSEL THE MOTHER ON THE 4 RULES OF HOME TREATMENT 1 GIVE EXTRA FLUID( AS MUCH AS THE CHILD WILL TAKE ) Breastfeed frequently and for longer at each feed. Give ORS and clean water in addition to breast milk 2. GIVE ZINC SUPPLEMENTS (Not for infant below 2 months) 3. CONTINUE BREAST FEEDING 4. TELL HER WHEN TO RETURN 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 57
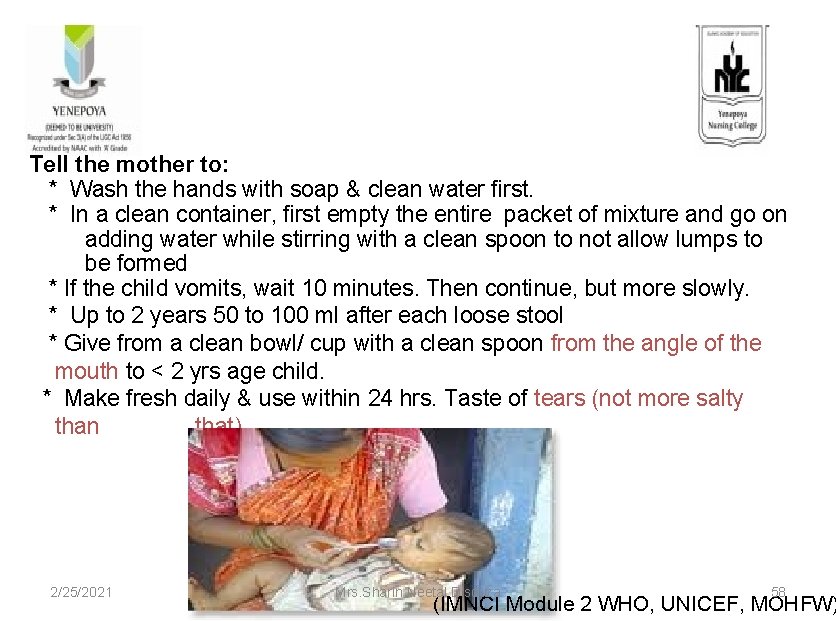
Tell the mother to: * Wash the hands with soap & clean water first. * In a clean container, first empty the entire packet of mixture and go on adding water while stirring with a clean spoon to not allow lumps to be formed * If the child vomits, wait 10 minutes. Then continue, but more slowly. * Up to 2 years 50 to 100 ml after each loose stool * Give from a clean bowl/ cup with a clean spoon from the angle of the mouth to < 2 yrs age child. * Make fresh daily & use within 24 hrs. Taste of tears (not more salty than that). 2/25/2021 Mrs. Sharin Neetal D'souza 58 (IMNCI Module 2 WHO, UNICEF, MOHFW)
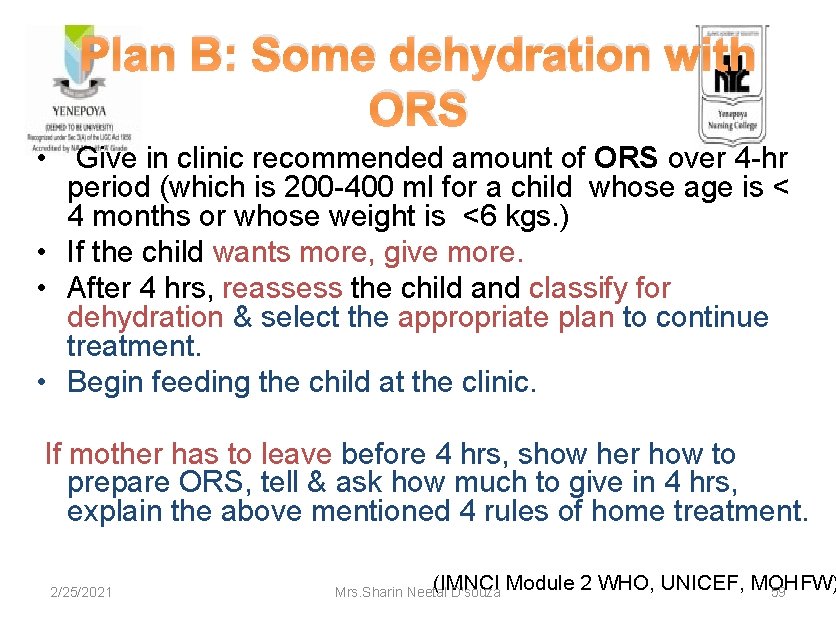
Plan B: Some dehydration with ORS • Give in clinic recommended amount of ORS over 4 -hr period (which is 200 -400 ml for a child whose age is < 4 months or whose weight is <6 kgs. ) • If the child wants more, give more. • After 4 hrs, reassess the child and classify for dehydration & select the appropriate plan to continue treatment. • Begin feeding the child at the clinic. If mother has to leave before 4 hrs, show her how to prepare ORS, tell & ask how much to give in 4 hrs, explain the above mentioned 4 rules of home treatment. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 59
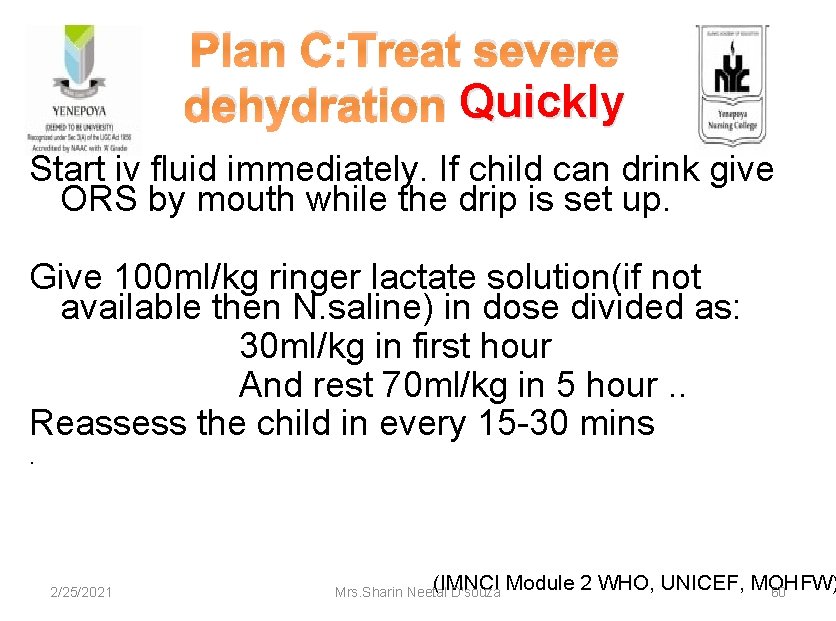
Plan C: Treat severe dehydration Quickly Start iv fluid immediately. If child can drink give ORS by mouth while the drip is set up. Give 100 ml/kg ringer lactate solution(if not available then N. saline) in dose divided as: 30 ml/kg in first hour And rest 70 ml/kg in 5 hour. . Reassess the child in every 15 -30 mins . 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 60
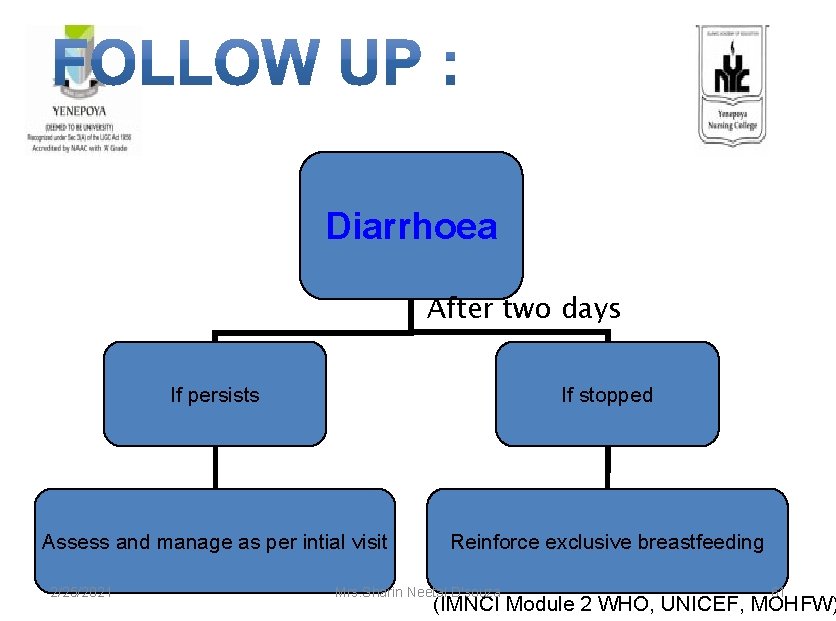
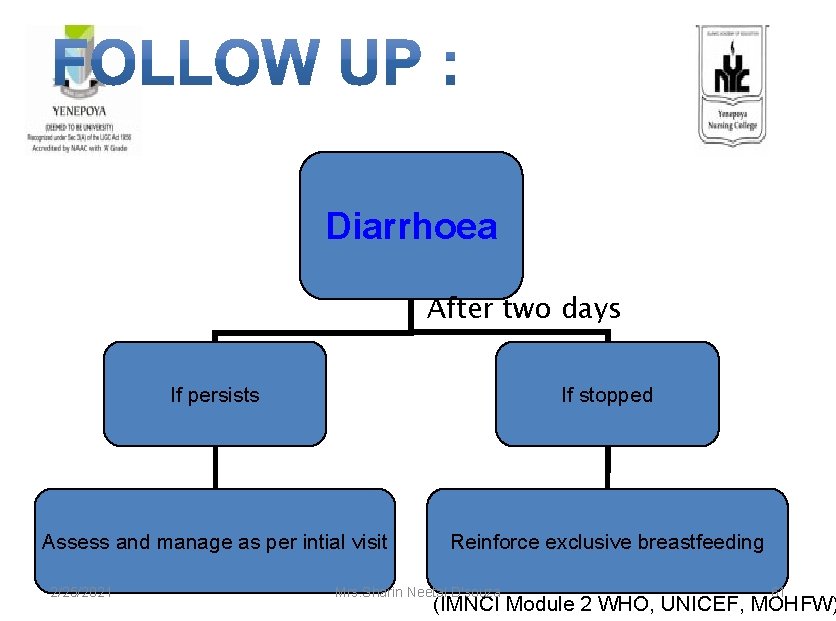
Diarrhoea After two days If persists If stopped Assess and manage as per intial visit Reinforce exclusive breastfeeding 2/25/2021 Mrs. Sharin Neetal D'souza 61 (IMNCI Module 2 WHO, UNICEF, MOHFW)
2/25/2021 Mrs. Sharin Neetal D'souza 62

2/25/2021 Mrs. Sharin Neetal D'souza 63
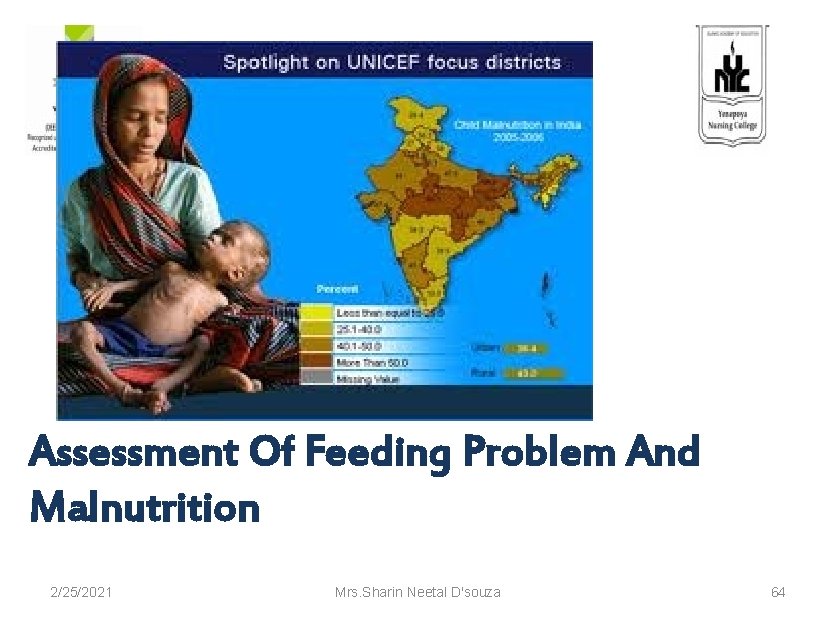
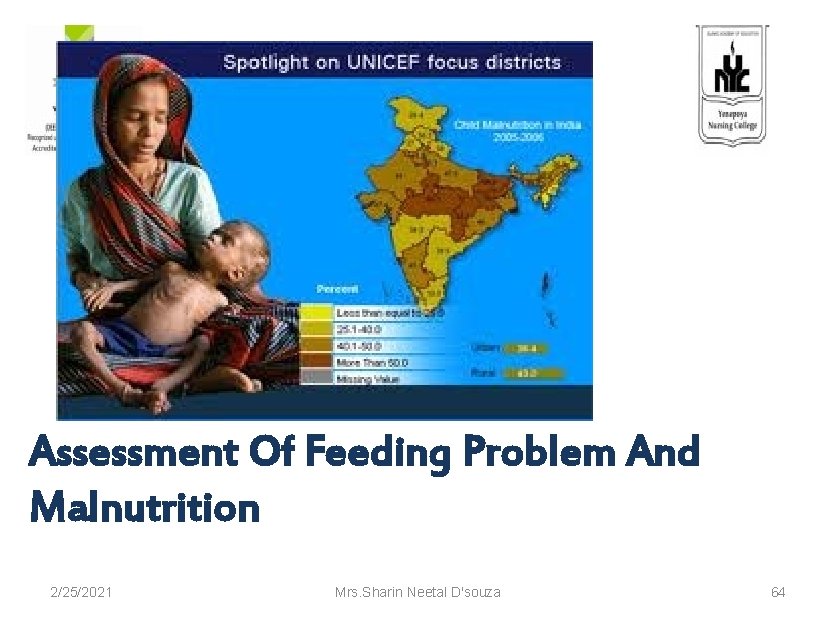
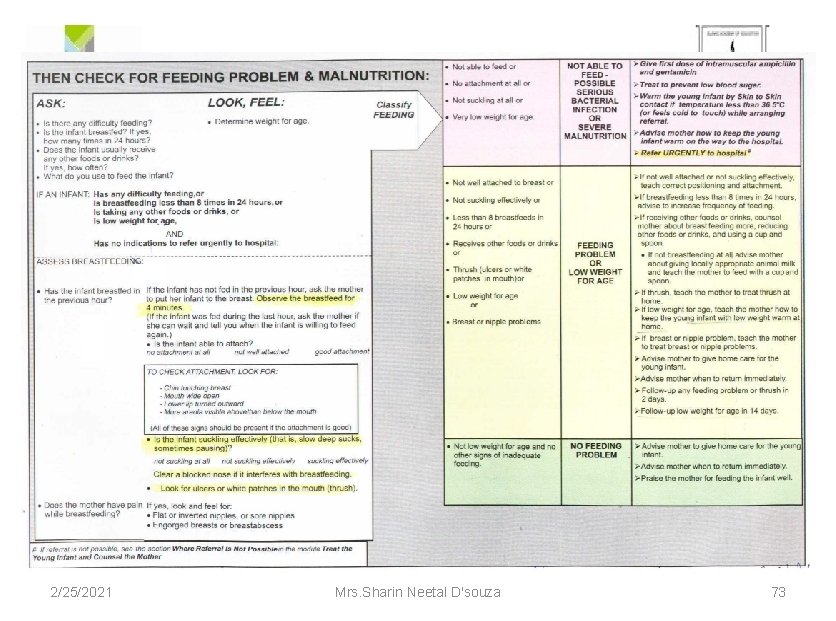
Assessment Of Feeding Problem And Malnutrition 2/25/2021 Mrs. Sharin Neetal D'souza 64
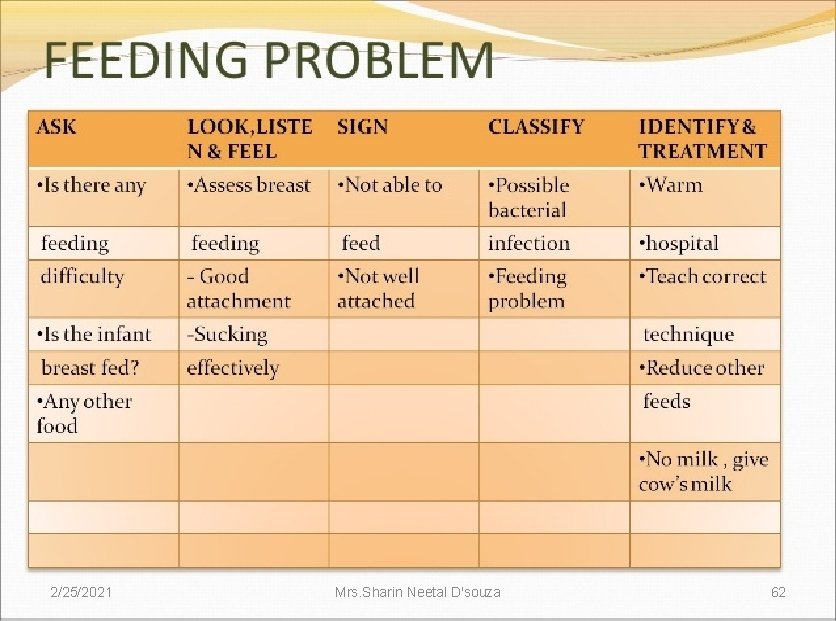
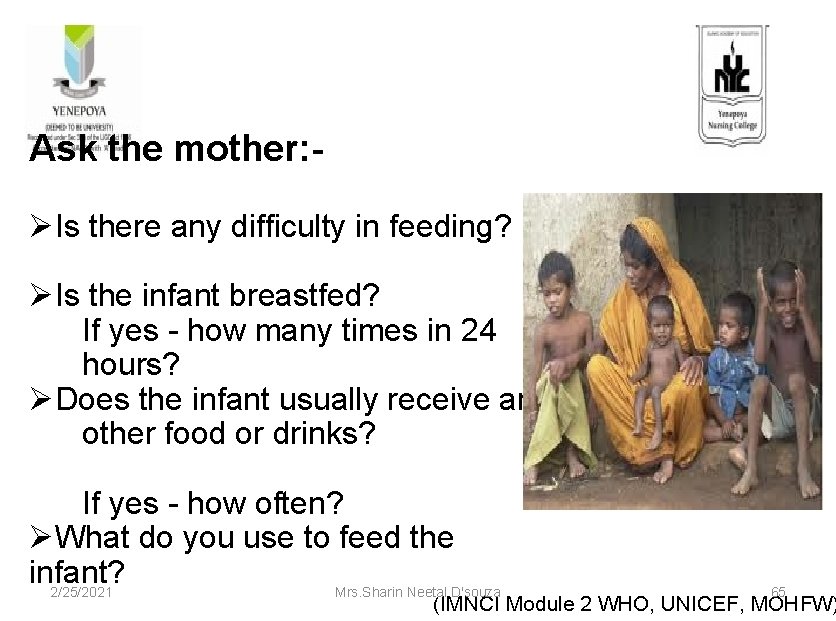
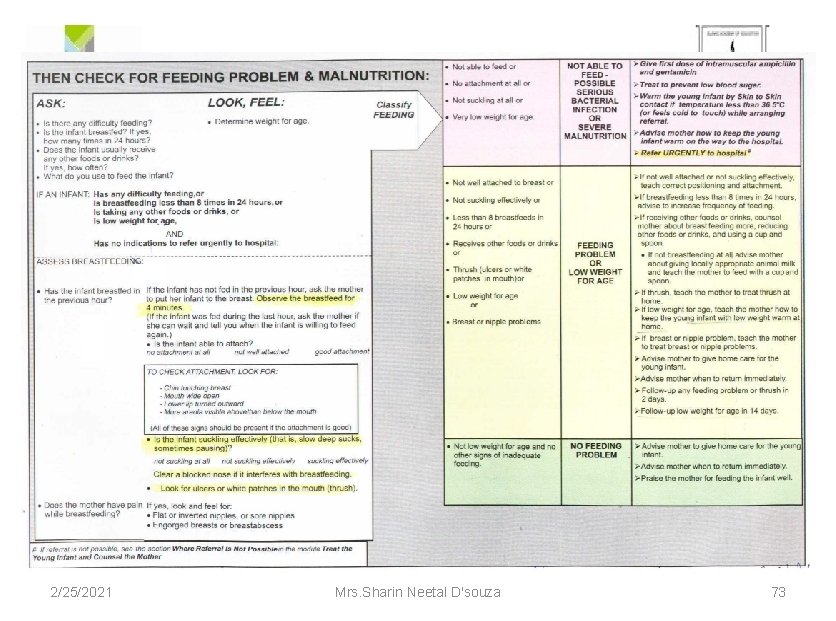
Ask the mother: ØIs there any difficulty in feeding? ØIs the infant breastfed? If yes - how many times in 24 hours? ØDoes the infant usually receive any other food or drinks? If yes - how often? ØWhat do you use to feed the infant? 2/25/2021 Mrs. Sharin Neetal D'souza 65 (IMNCI Module 2 WHO, UNICEF, MOHFW)

Look , Feel: ØDetermine weight for age -Mid Upper Arm Circumference(MUAC) MUAC TAPE 2/25/2021 Mrs. Sharin Neetal D'souza 66 (IMNCI Module 2 WHO, UNICEF, MOHFW)
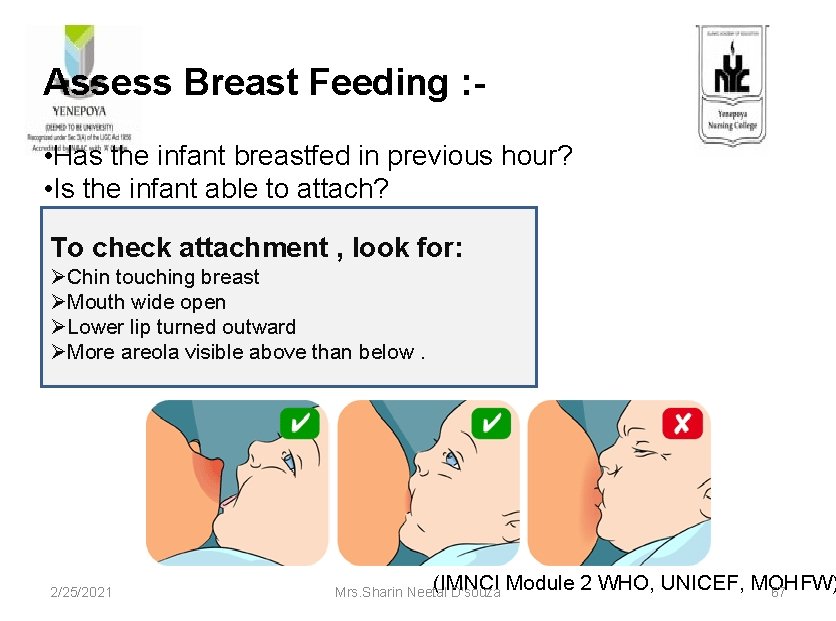
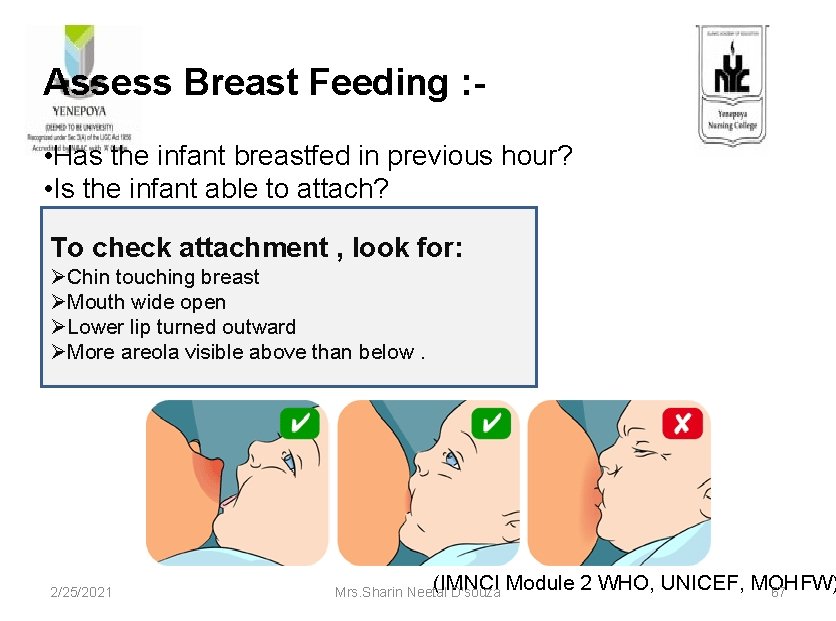
Assess Breast Feeding : • Has the infant breastfed in previous hour? • Is the infant able to attach? To check attachment , look for: ØChin touching breast ØMouth wide open ØLower lip turned outward ØMore areola visible above than below. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 67
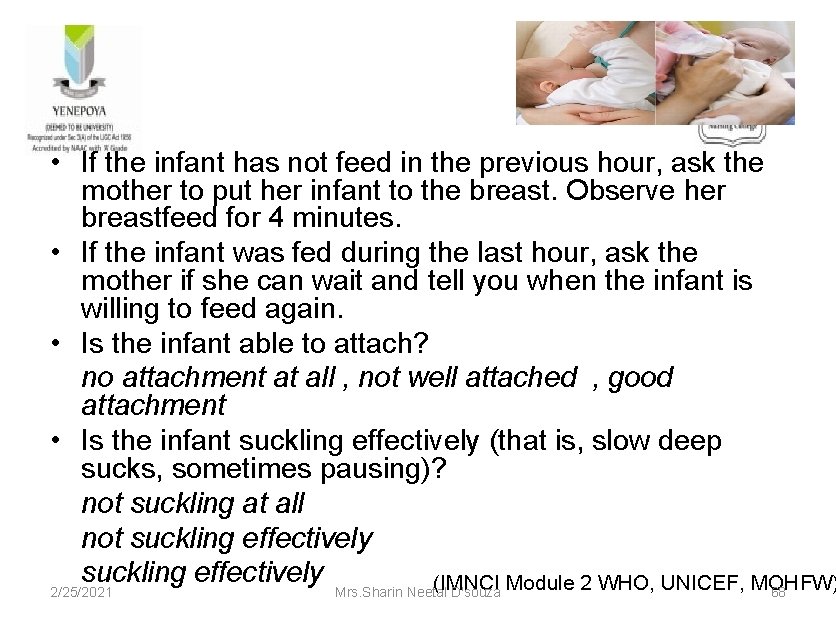
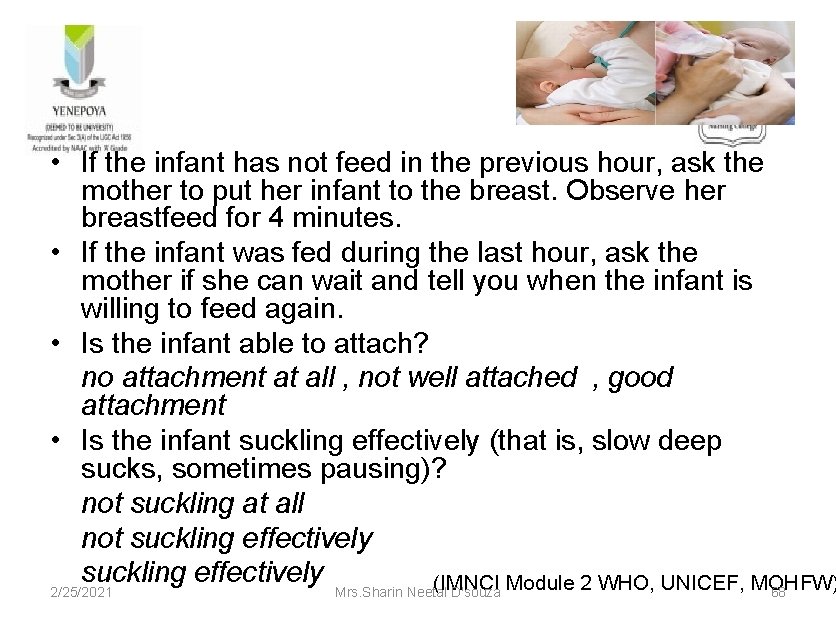
• If the infant has not feed in the previous hour, ask the mother to put her infant to the breast. Observe her breastfeed for 4 minutes. • If the infant was fed during the last hour, ask the mother if she can wait and tell you when the infant is willing to feed again. • Is the infant able to attach? no attachment at all , not well attached , good attachment • Is the infant suckling effectively (that is, slow deep sucks, sometimes pausing)? not suckling at all not suckling effectively (IMNCI Module 2 WHO, UNICEF, MOHFW) 2/25/2021 Mrs. Sharin Neetal D'souza 68
• Clear a blocked nose if it interferes with breastfeeding • Look for ulcers or white patches in the mouth(thrush) If yes, look and feel for: Flat or inverted nipples, or sore nipples Engorged breasts or breast abscess • Does the mother have pain while breastfeeding? 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 69

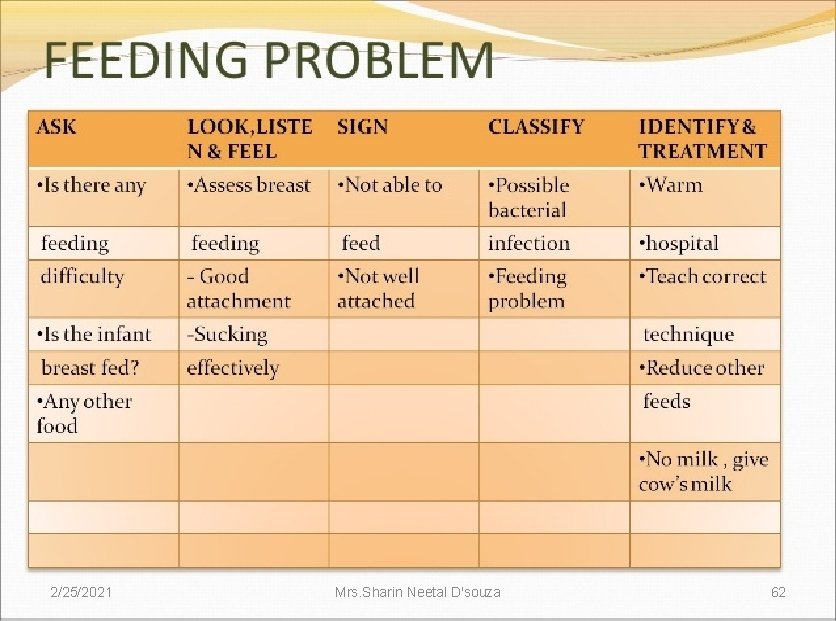
(IMNCI Module 2 WHO, UNICEF, MOHFW) SIG CLASSIFY AS TREATMENT NS • Not able to feed or • No attachment or • Not suckling at all or • Very low wt for age 2/25/2021 Not able to feed –Possible serious bact. infection or Severe malnutrition Mrs. Sharin Neetal D'souza Give first dose of intramuscular ampicillin and gentamicin � Treat to prevent low blood sugar � Warm the young infant by skin to skin contact if temperature less than 36. 5 o. C (or feels cold to touch) while arranging referral � Advise mother how to keep the young infant warm on the way to the hospital � Refer URGENTLY to hospital 70
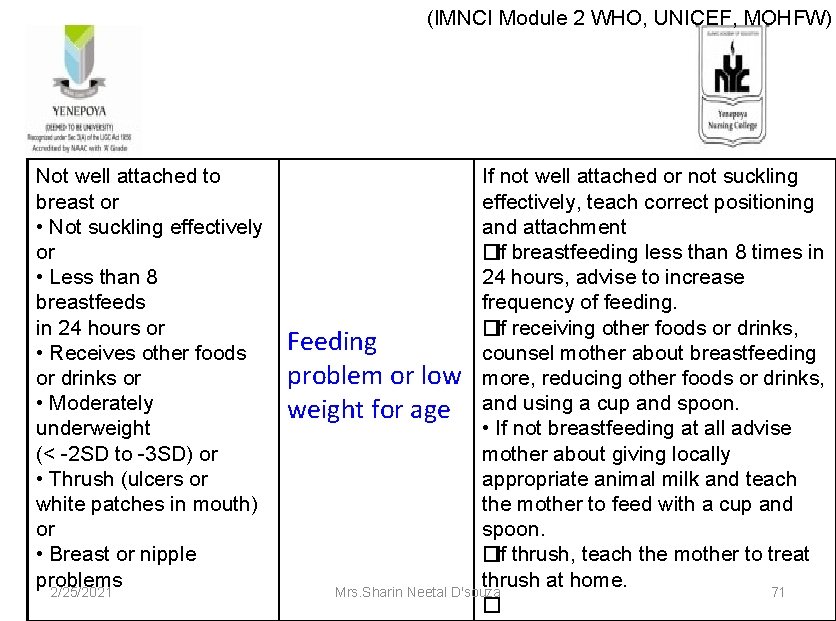
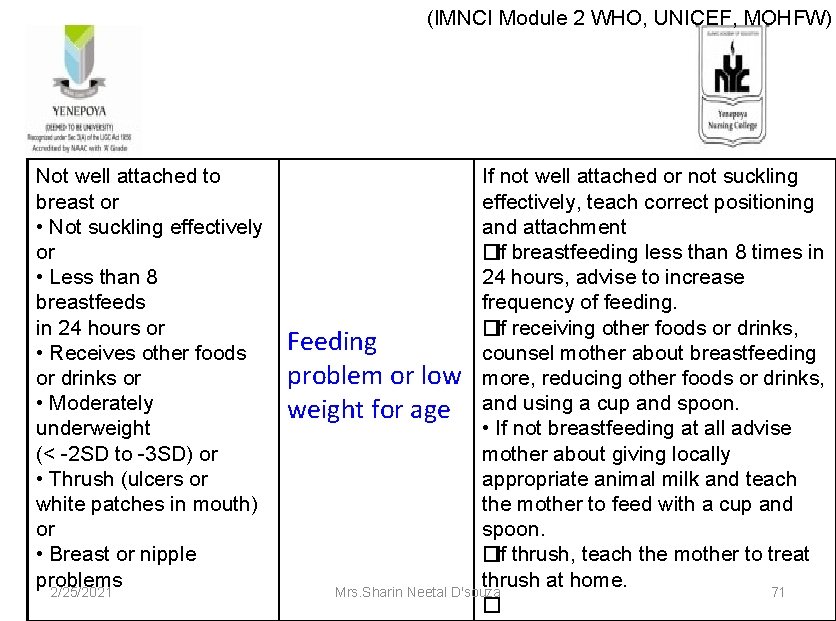
(IMNCI Module 2 WHO, UNICEF, MOHFW) Not well attached to breast or • Not suckling effectively or • Less than 8 breastfeeds in 24 hours or • Receives other foods or drinks or • Moderately underweight (< -2 SD to -3 SD) or • Thrush (ulcers or white patches in mouth) or • Breast or nipple problems 2/25/2021 If not well attached or not suckling effectively, teach correct positioning and attachment � If breastfeeding less than 8 times in 24 hours, advise to increase frequency of feeding. � If receiving other foods or drinks, Feeding counsel mother about breastfeeding problem or low more, reducing other foods or drinks, weight for age and using a cup and spoon. • If not breastfeeding at all advise mother about giving locally appropriate animal milk and teach the mother to feed with a cup and spoon. � If thrush, teach the mother to treat thrush at home. Mrs. Sharin Neetal D'souza 71 �
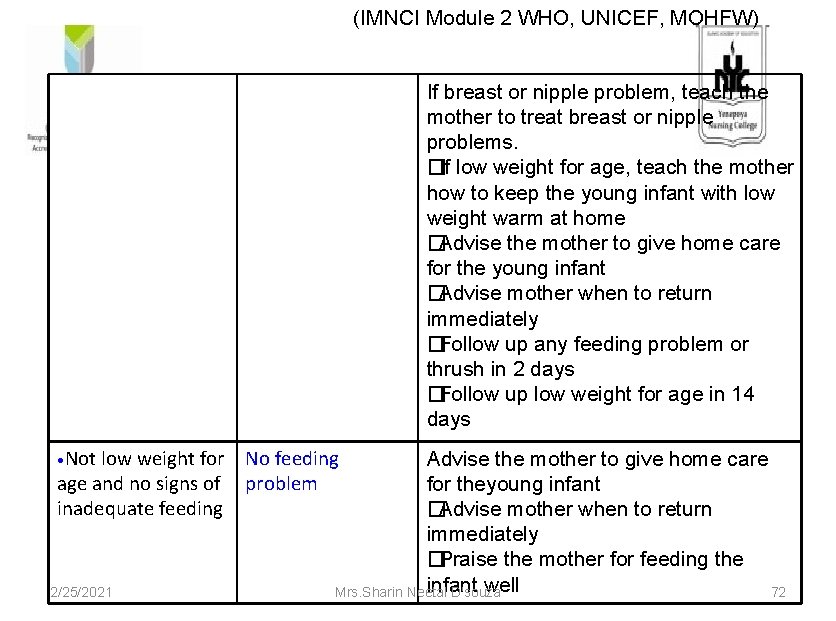
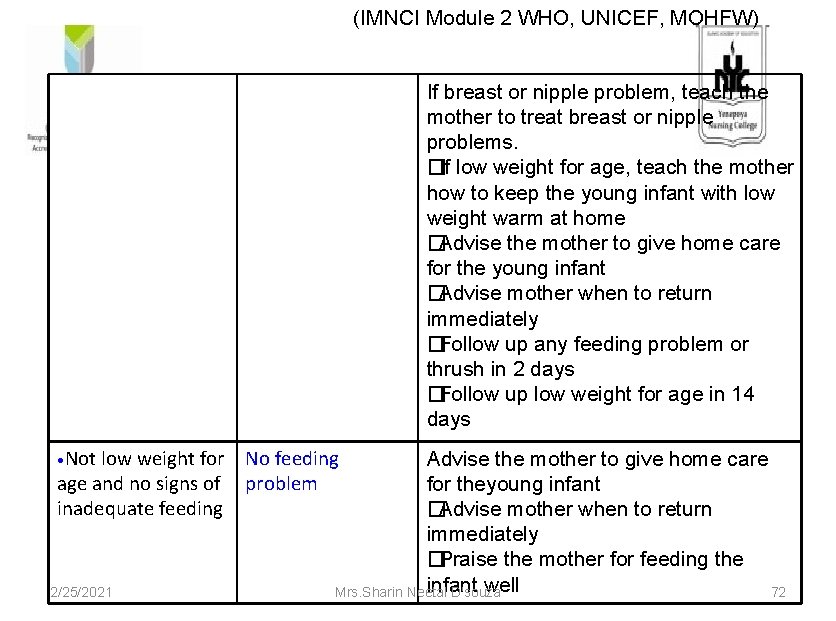
(IMNCI Module 2 WHO, UNICEF, MOHFW) If breast or nipple problem, teach the mother to treat breast or nipple problems. � If low weight for age, teach the mother how to keep the young infant with low weight warm at home � Advise the mother to give home care for the young infant � Advise mother when to return immediately � Follow up any feeding problem or thrush in 2 days � Follow up low weight for age in 14 days • Not low weight for No feeding age and no signs of problem inadequate feeding 2/25/2021 Advise the mother to give home care for theyoung infant � Advise mother when to return immediately � Praise the mother for feeding the infant well Mrs. Sharin Neetal D'souza 72
2/25/2021 Mrs. Sharin Neetal D'souza 73
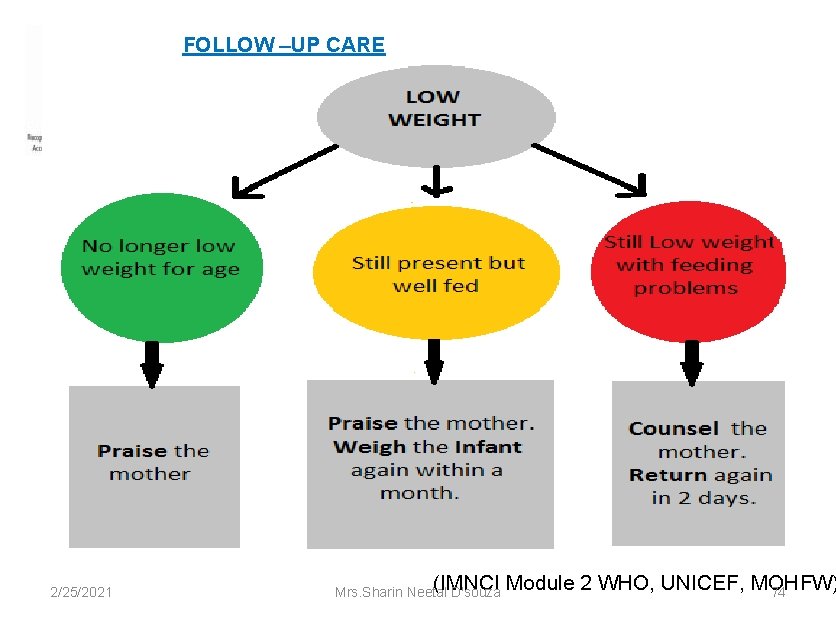
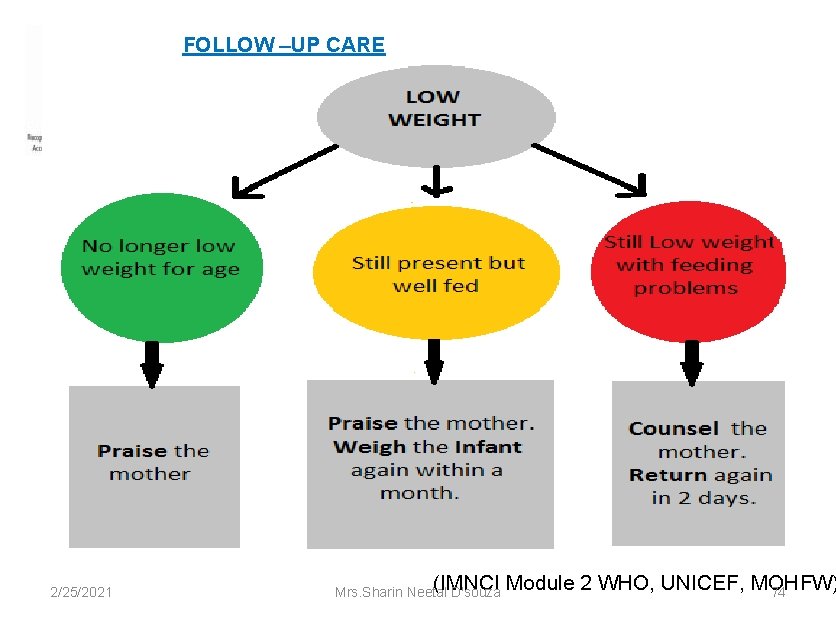
FOLLOW –UP CARE 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 74
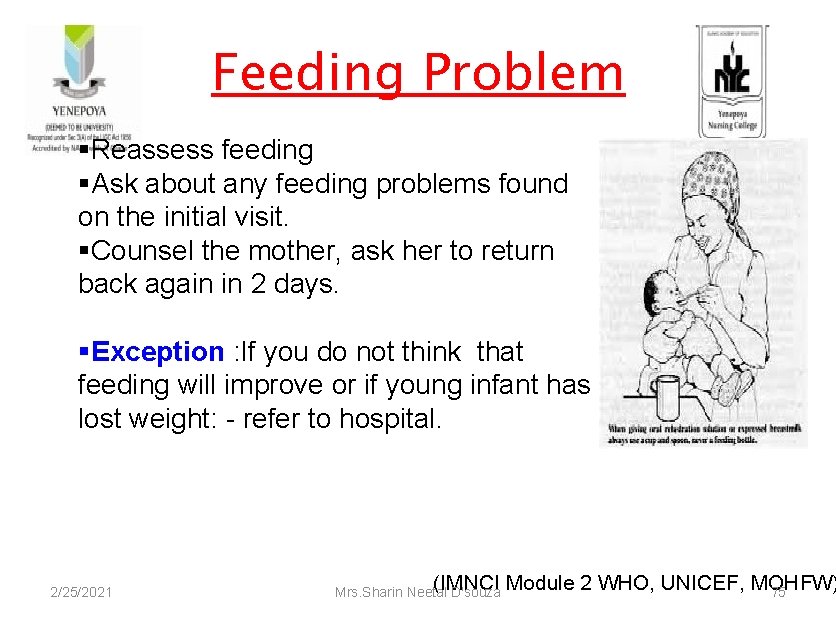
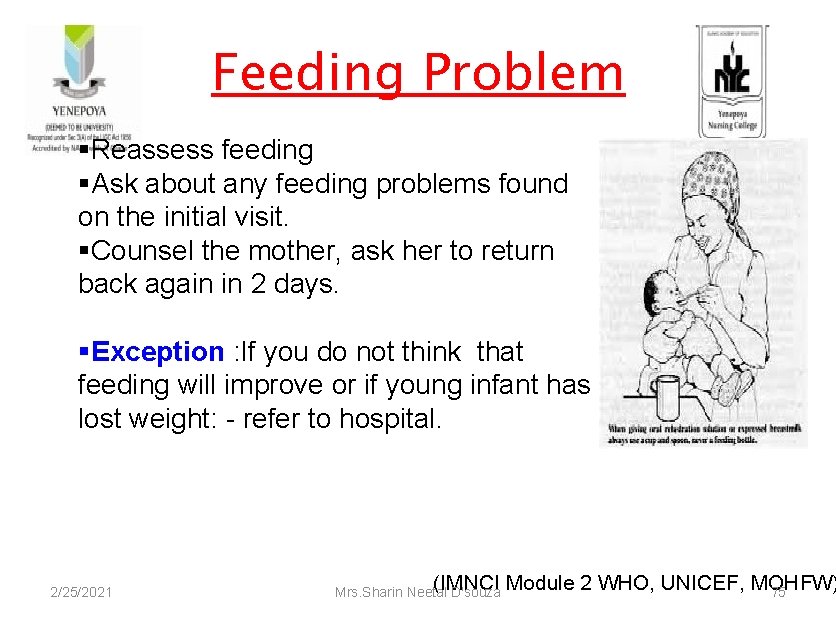
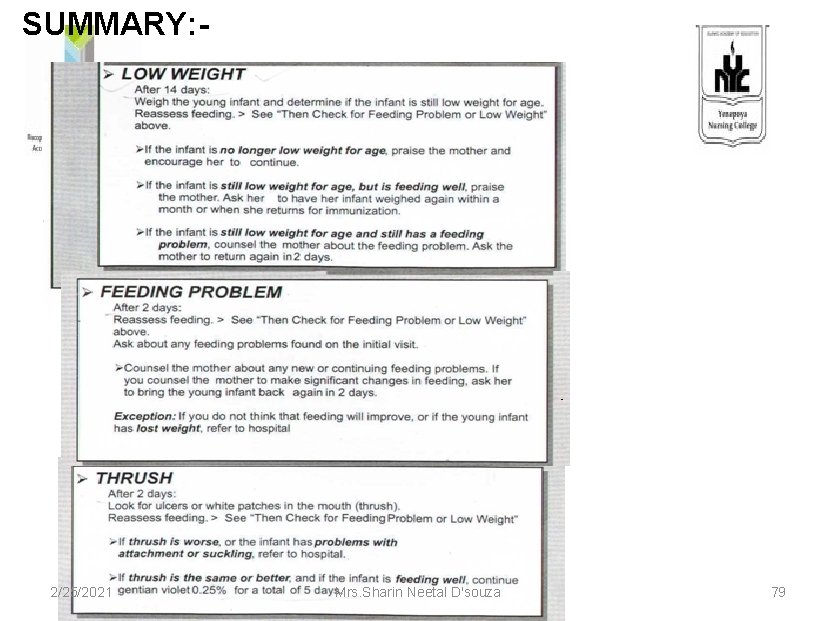
Feeding Problem §Reassess feeding §Ask about any feeding problems found on the initial visit. §Counsel the mother, ask her to return back again in 2 days. §Exception : If you do not think that feeding will improve or if young infant has lost weight: - refer to hospital. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 75
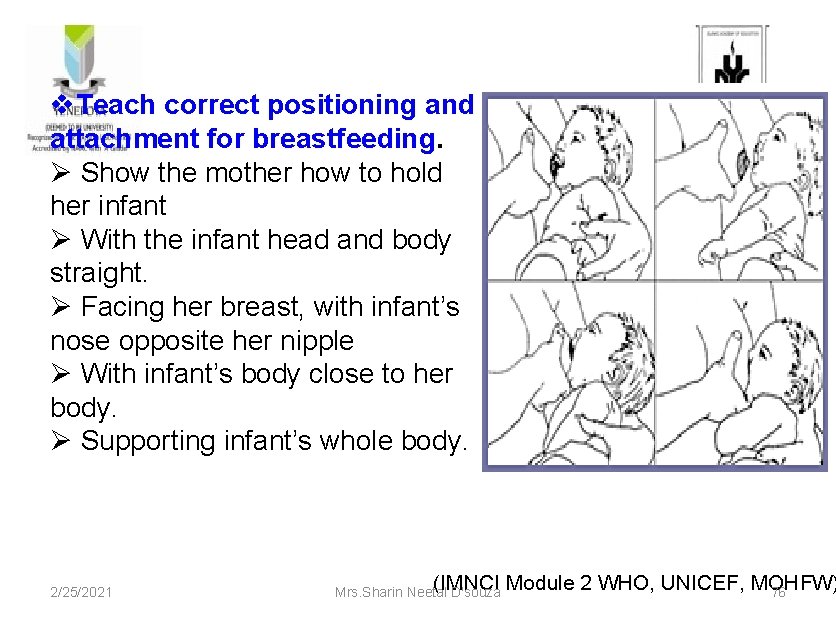
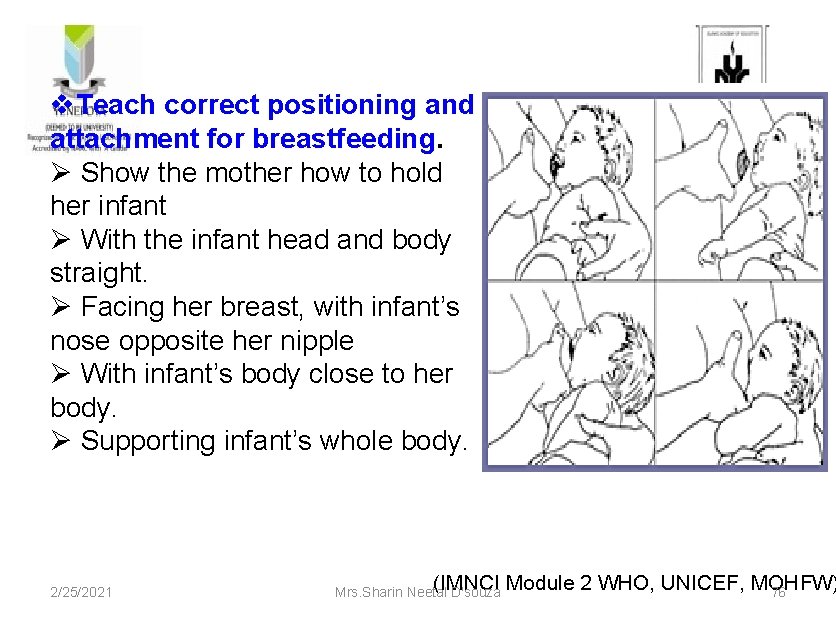
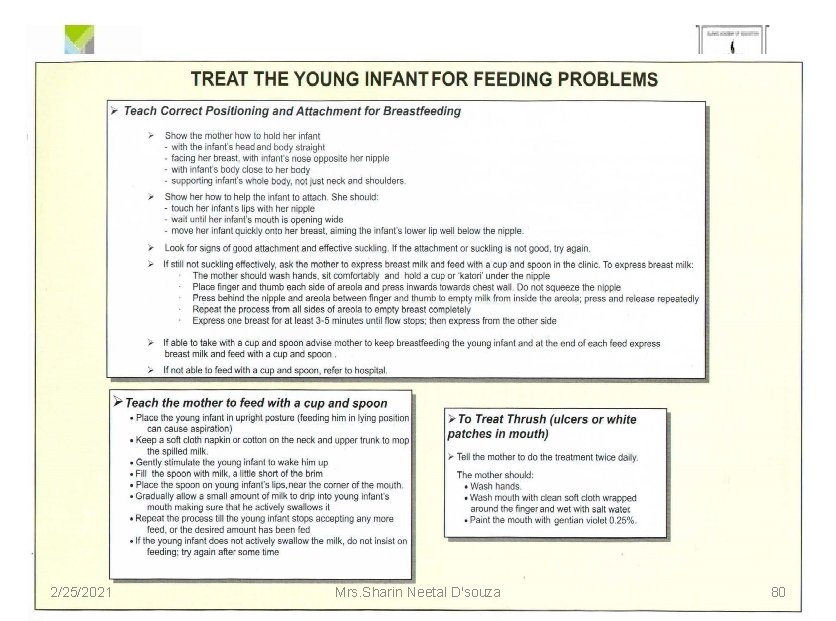
v. Teach correct positioning and attachment for breastfeeding. Ø Show the mother how to hold her infant Ø With the infant head and body straight. Ø Facing her breast, with infant’s nose opposite her nipple Ø With infant’s body close to her body. Ø Supporting infant’s whole body. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 76
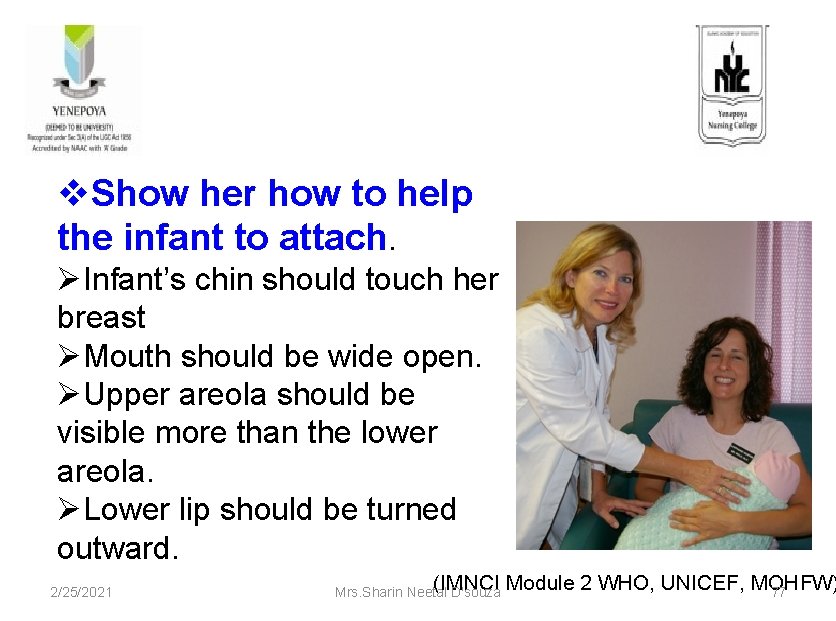
v. Show her how to help the infant to attach. ØInfant’s chin should touch her breast ØMouth should be wide open. ØUpper areola should be visible more than the lower areola. ØLower lip should be turned outward. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 77
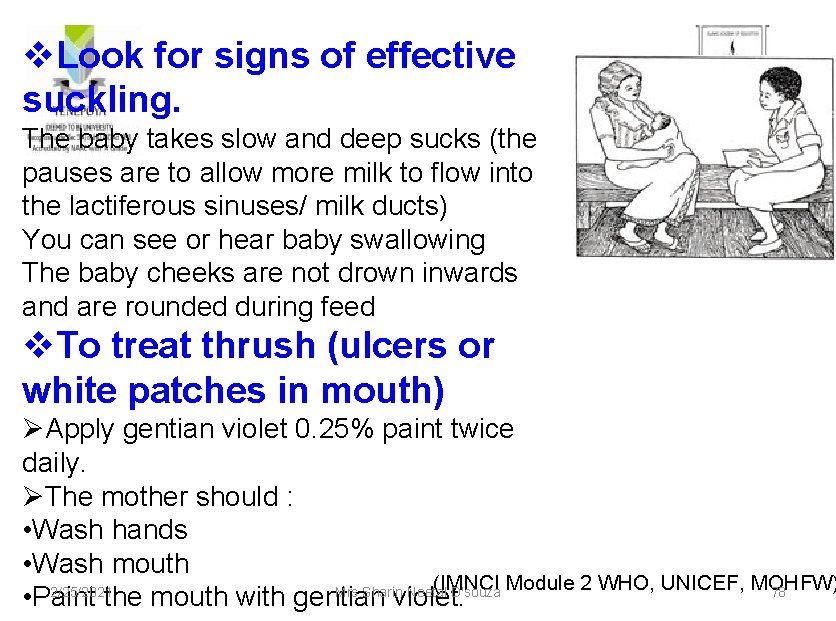
v. Look for signs of effective suckling. The baby takes slow and deep sucks (the pauses are to allow more milk to flow into the lactiferous sinuses/ milk ducts) You can see or hear baby swallowing The baby cheeks are not drown inwards and are rounded during feed v. To treat thrush (ulcers or white patches in mouth) ØApply gentian violet 0. 25% paint twice daily. ØThe mother should : • Wash hands • Wash mouth (IMNCI Module 2 WHO, UNICEF, MOHFW) 2/25/2021 Mrs. Sharin Neetal D'souza 78 • Paint the mouth with gentian violet.
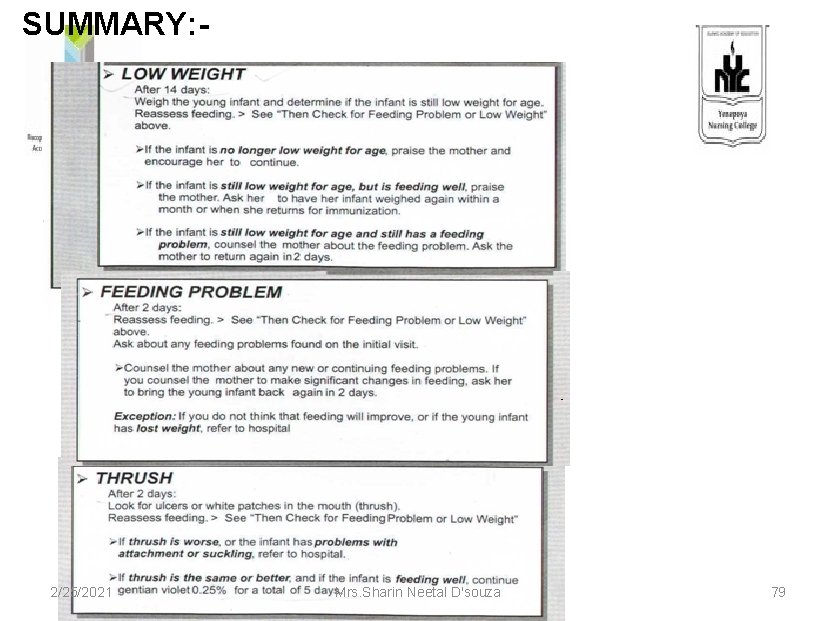
SUMMARY: - 2/25/2021 Mrs. Sharin Neetal D'souza 79
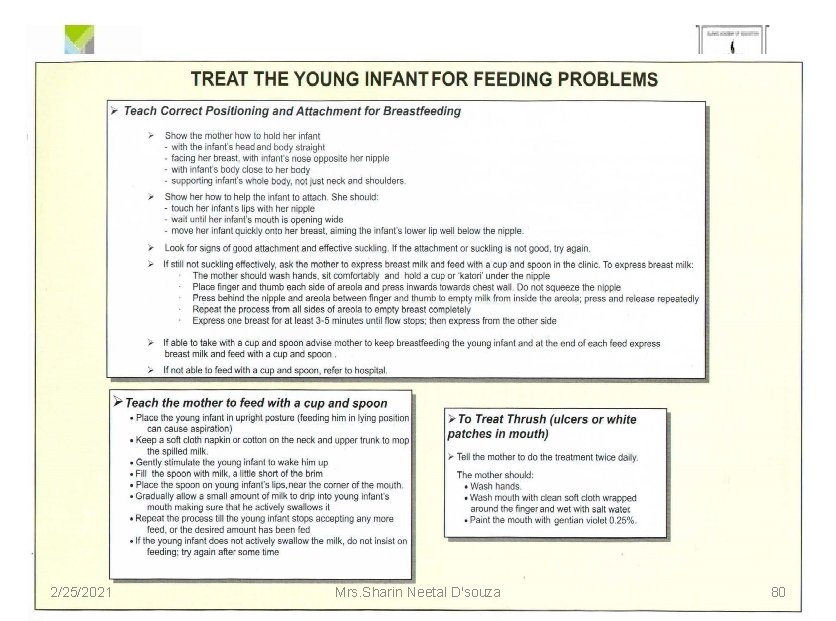
2/25/2021 Mrs. Sharin Neetal D'souza 80
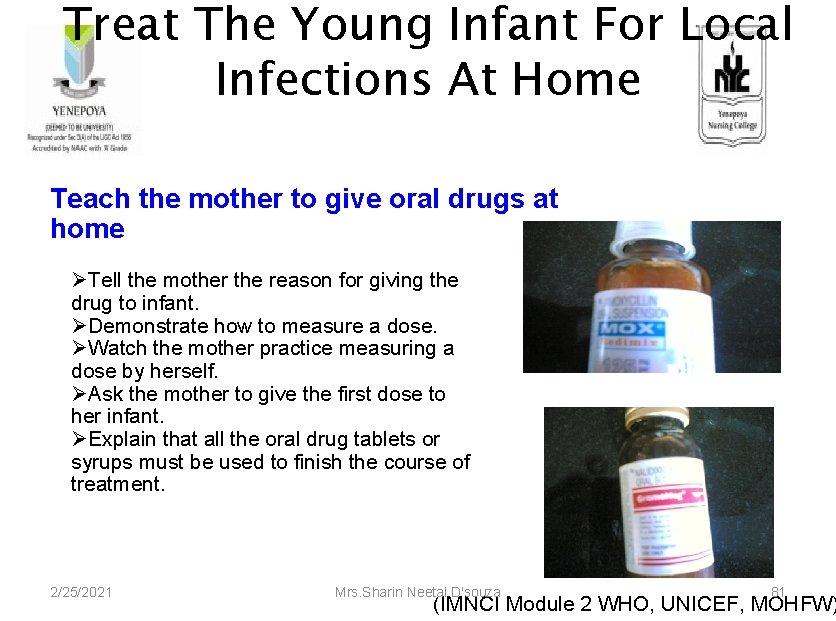
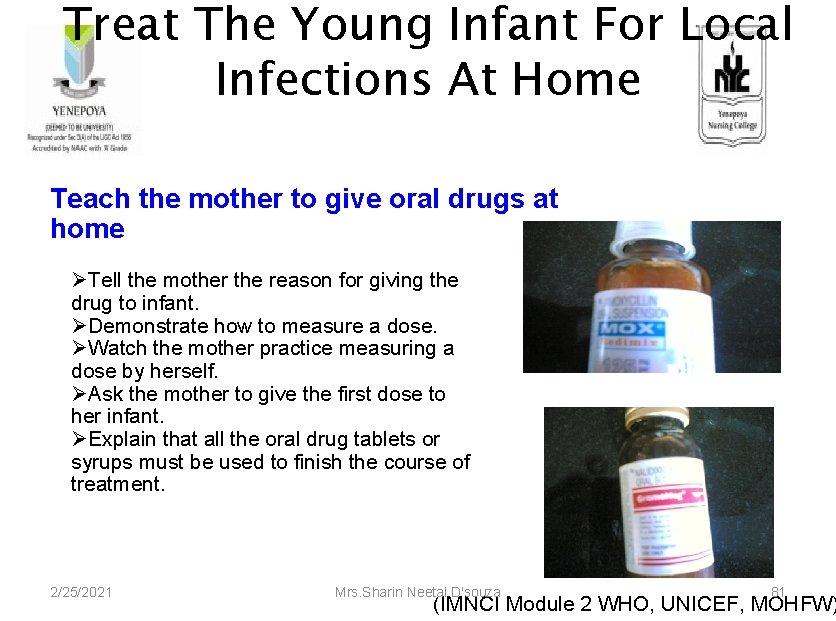
Treat The Young Infant For Local Infections At Home Teach the mother to give oral drugs at home ØTell the mother the reason for giving the drug to infant. ØDemonstrate how to measure a dose. ØWatch the mother practice measuring a dose by herself. ØAsk the mother to give the first dose to her infant. ØExplain that all the oral drug tablets or syrups must be used to finish the course of treatment. 2/25/2021 Mrs. Sharin Neetal D'souza 81 (IMNCI Module 2 WHO, UNICEF, MOHFW)

Follow-Up Care Local bacterial infections Umbilicus red or draining pus Skin pustules Ear Discharge Improved, continue treatment Continue wicking >10 or big boil Remains or worse <10 and no big boil dry the ear refer to hospital Refer to hospital 2/25/2021 Continue treatment Mrs. Sharin Neetal D'souza 82 (IMNCI Module 2 WHO, UNICEF, MOHFW)
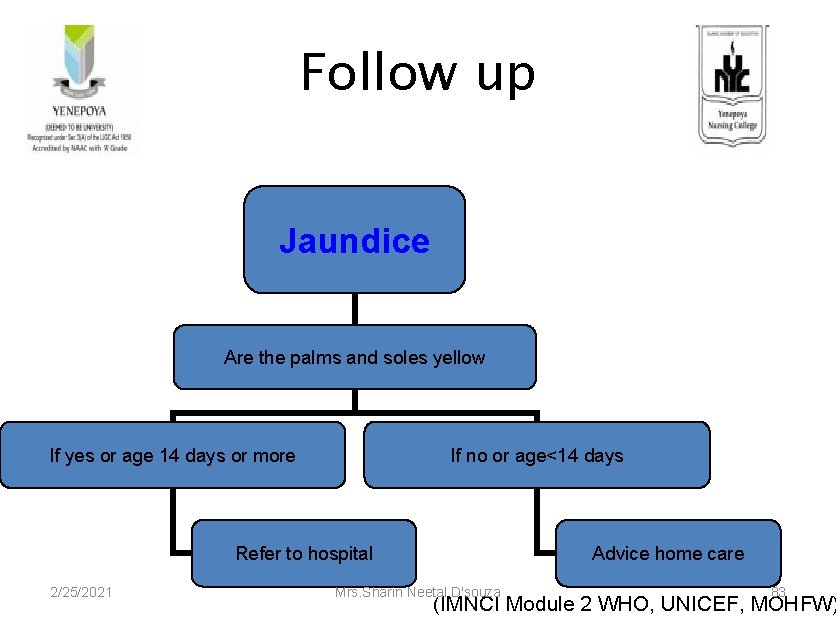
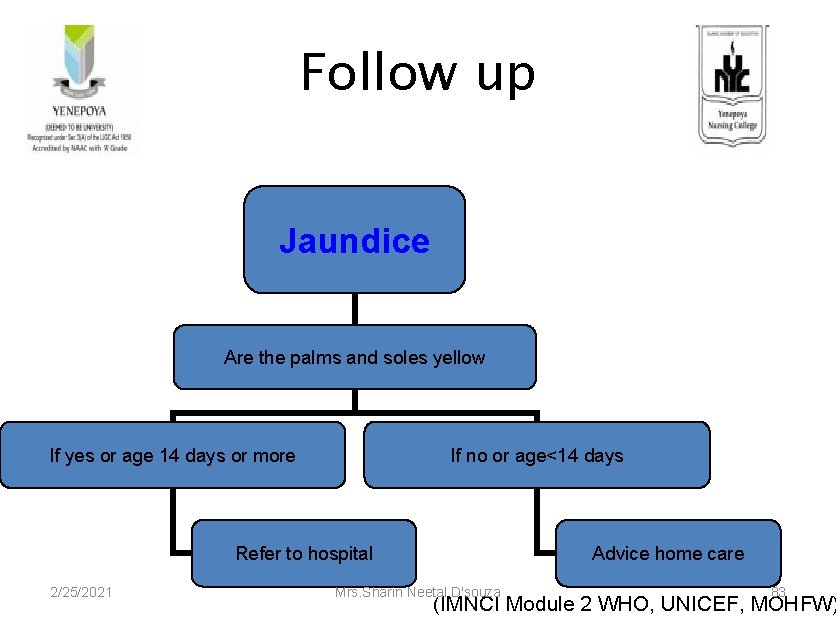
Follow up Jaundice Are the palms and soles yellow If yes or age 14 days or more If no or age<14 days Refer to hospital 2/25/2021 Advice home care Mrs. Sharin Neetal D'souza 83 (IMNCI Module 2 WHO, UNICEF, MOHFW)
CHECK FOR POSSIBLE HYPOTHERMIA 2/25/2021 Mrs. Sharin Neetal D'souza 84
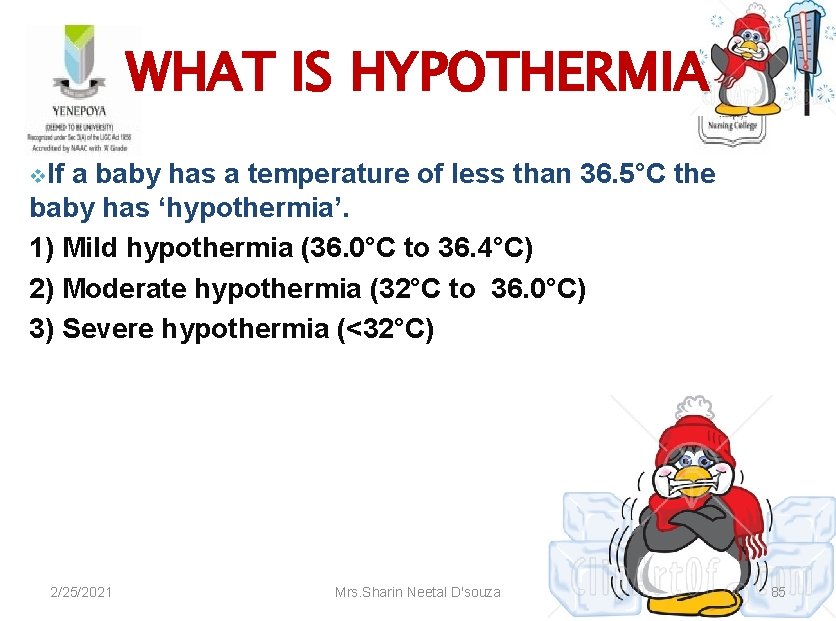
WHAT IS HYPOTHERMIA v. If a baby has a temperature of less than 36. 5°C the baby has ‘hypothermia’. 1) Mild hypothermia (36. 0°C to 36. 4°C) 2) Moderate hypothermia (32°C to 36. 0°C) 3) Severe hypothermia (<32°C) 2/25/2021 Mrs. Sharin Neetal D'souza 85

CAUSES OF HYPOTHERMIA Large surface area of babies compared to their weight. • Limited heat generation mechanism. • Vulnerability to getting exposed. • Decreased subcutaneous fat and brown fat. • Poorer homeostatic response to hypothermia and early exhaustion of metabolic store like glucose. 2/25/2021 Mrs. Sharin Neetal D'souza 86

METHODS OF TEMPERATURE MEASUREMENT Axillary (standard method) • Rectal • Skin • Human touch • abdomen, feet and hands are warm- Normal • abdomen is warm but feet and hands are cold- Cold stress • abdomen, feet and hands are cold- Hypothermia 2/25/2021 Mrs. Sharin Neetal D'souza 87
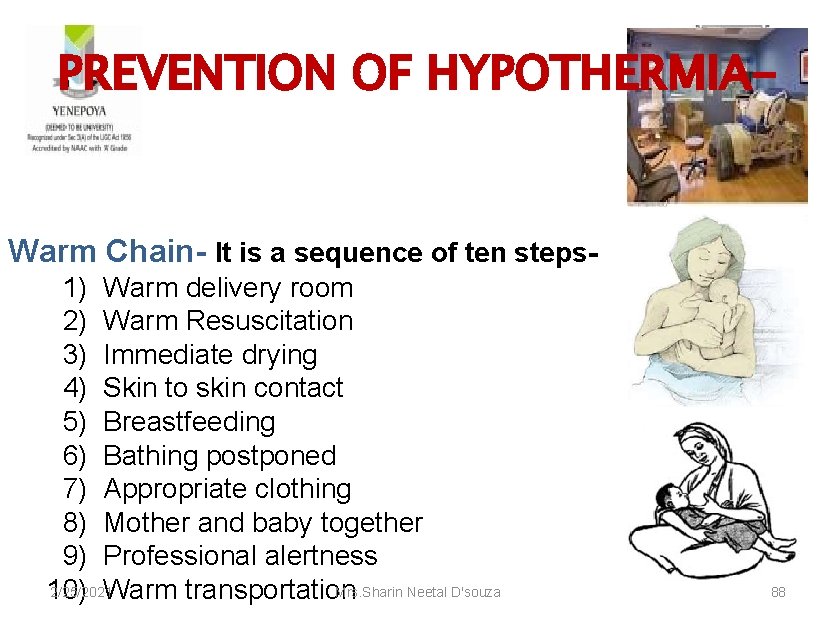
PREVENTION OF HYPOTHERMIA- Warm Chain- It is a sequence of ten steps 1) Warm delivery room 2) Warm Resuscitation 3) Immediate drying 4) Skin to skin contact 5) Breastfeeding 6) Bathing postponed 7) Appropriate clothing 8) Mother and baby together 9) Professional alertness 2/25/2021 Mrs. Sharin Neetal D'souza 10) Warm transportation 88

KANGAROO MOTHER CARE Kangaroo mother care for low birth weight babies, was introduced in COLUMBIA in 1979, by Dr’s Hector Martinez and Edzar Rey. 2/25/2021 Mrs. Sharin Neetal D'souza 89
• Skin-to-skin contact between mother and baby is called Kangaroo Mother Care. • It is the most practical, preferred method of warming a hypothermic infant in a primary health care facility. 2/25/2021 Mrs. Sharin Neetal D'souza 90
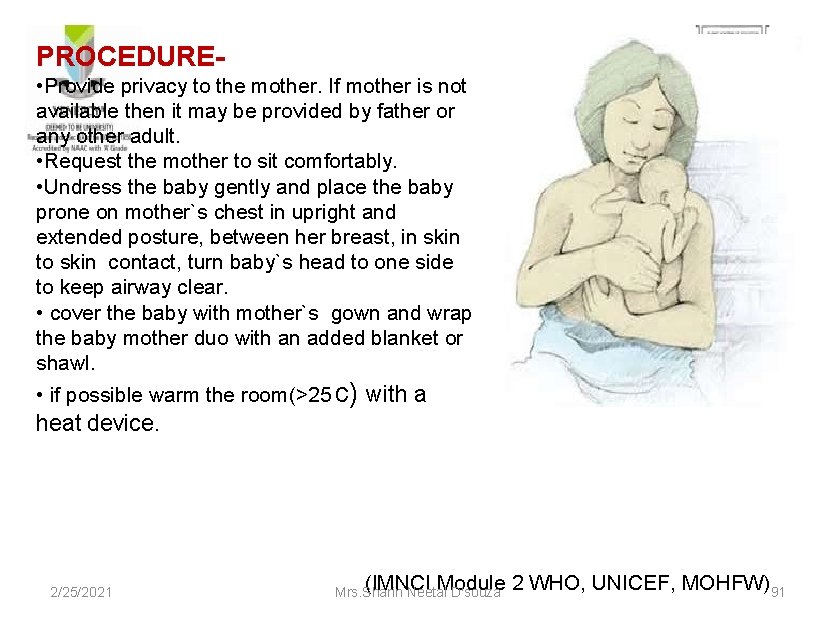
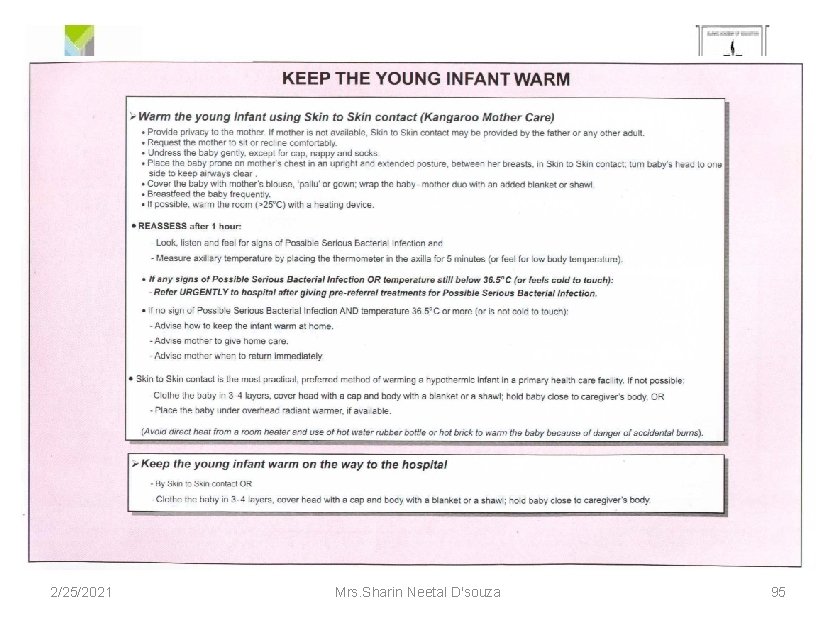
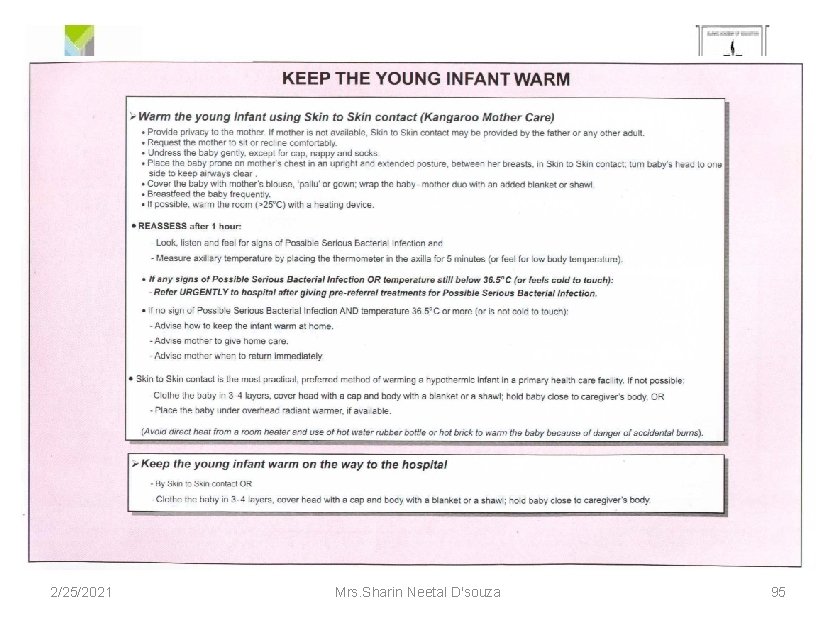
PROCEDURE • Provide privacy to the mother. If mother is not available then it may be provided by father or any other adult. • Request the mother to sit comfortably. • Undress the baby gently and place the baby prone on mother`s chest in upright and extended posture, between her breast, in skin to skin contact, turn baby`s head to one side to keep airway clear. • cover the baby with mother`s gown and wrap the baby mother duo with an added blanket or shawl. • if possible warm the room(>25 c) with a heat device. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) 91 Mrs. Sharin Neetal D'souza
• Reassess after 1 hour. Ø Look for signs of possible serious bacterial infection. Ø Measure axillary temperature (or feel for low body temperature) • If signs present or temperature still below 36. 50 c refer urgently after giving pre-referral treatment. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 92

MANAGEMENT OF HYPOTHERMIA 1) Mild hypothermia (36. 0°C to 36. 4°C) Skin-to-Skin contact is the best way to keep a baby warm and the best way to ‘rewarm’ a baby who is cold to touch. Ø 2) Moderate hypothermia (32°C to 36. 0°C) ØWarm the young infant using Skin to Skin contact. ØIf Skin to Skin contact is not possible, radiant warmer may be used if available. ØEncourage mother to breastfeed more frequently. ØIf the baby’s temperature is not up to 36. 50 C or more after 2 hours of ‘rewarming’, reassess the baby for other 2/25/2021 Mrs. Sharin Neetal D'souza problems. 93
3) Severe hypothermia (<32°C) Remove cold or wet clothing. Dress in warm clothes and a cap, and cover with a warm blanket. Warm immediately using a pre warmed radiant warmer. Check and treat for hypoglycemia. Treat for sepsis. Start IV fluids. Provide oxygen if indicated. Monitor temperature of the baby every ½ hourly. 2/25/2021 Mrs. Sharin Neetal D'souza 94
2/25/2021 Mrs. Sharin Neetal D'souza 95
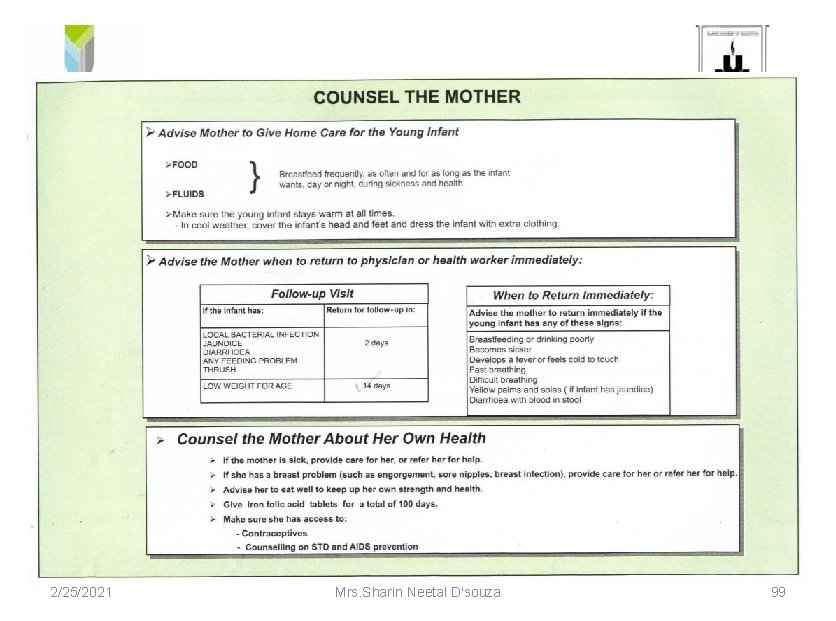
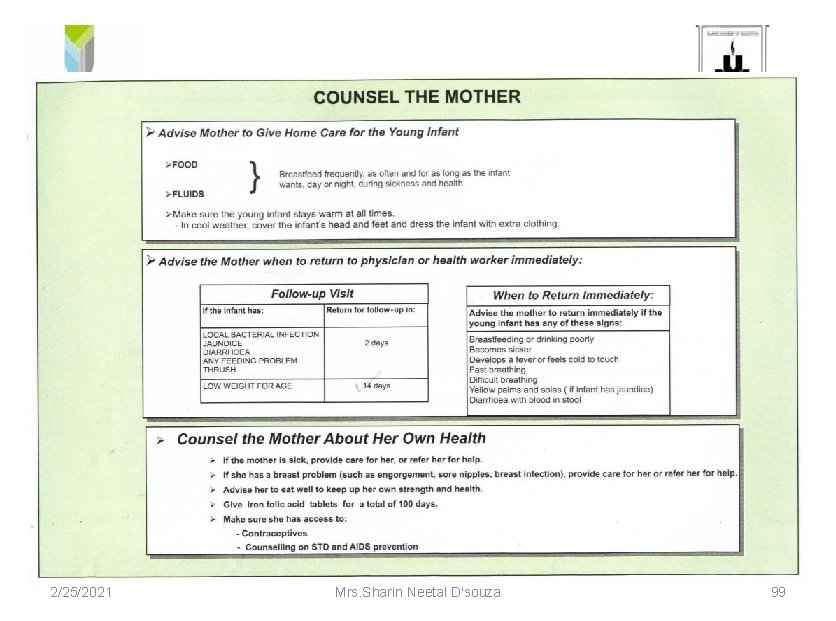
Counsel The Mother FOR HOME CARE Advice mother to give home care for the young infant: Ø Food and fluids Ø Breastfeed frequently as often and for as long as the infant wants. Ø Make sure the young infant stays warm at all times. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 96

Follow-Up Visit If the infant has Return for follow up in • Local bacterial infection • Jaundice • Diarrhea • Any feeding problem • Thrush • Low 2/25/2021 weight for age 2 days 14 days (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 97

When To Return Immediately • If the young infant has any of this signs: Ø Breastfeeding or drinking poorly Ø Becomes sicker Ø Develops a fever or feels cold to touch Ø Fast breathing Ø Difficult breathing Ø Yellow palms and soles Ø Diarrhoea with blood in stool. 2/25/2021 (IMNCI Module 2 WHO, UNICEF, MOHFW) Mrs. Sharin Neetal D'souza 98
2/25/2021 Mrs. Sharin Neetal D'souza 99
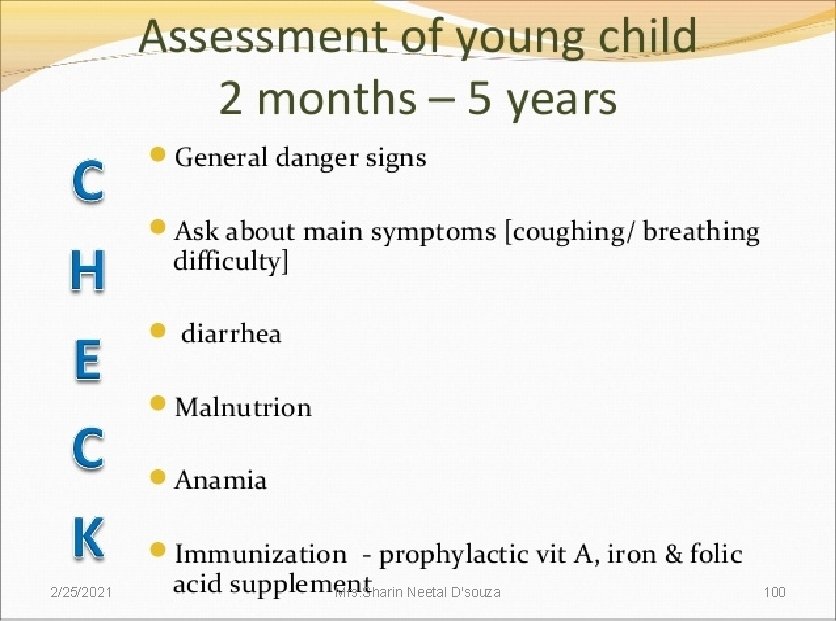
2/25/2021 Mrs. Sharin Neetal D'souza 100
2/25/2021 Mrs. Sharin Neetal D'souza 101
2/25/2021 Mrs. Sharin Neetal D'souza 102
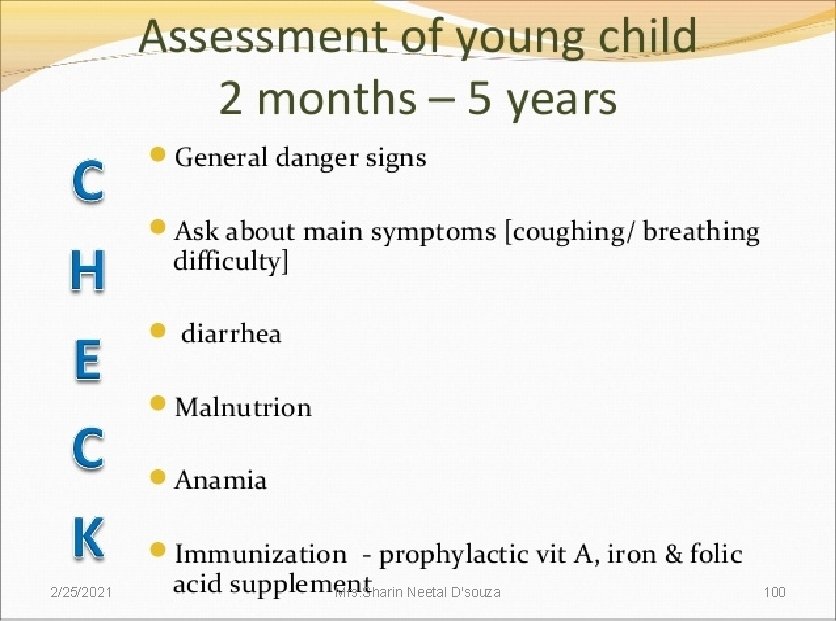
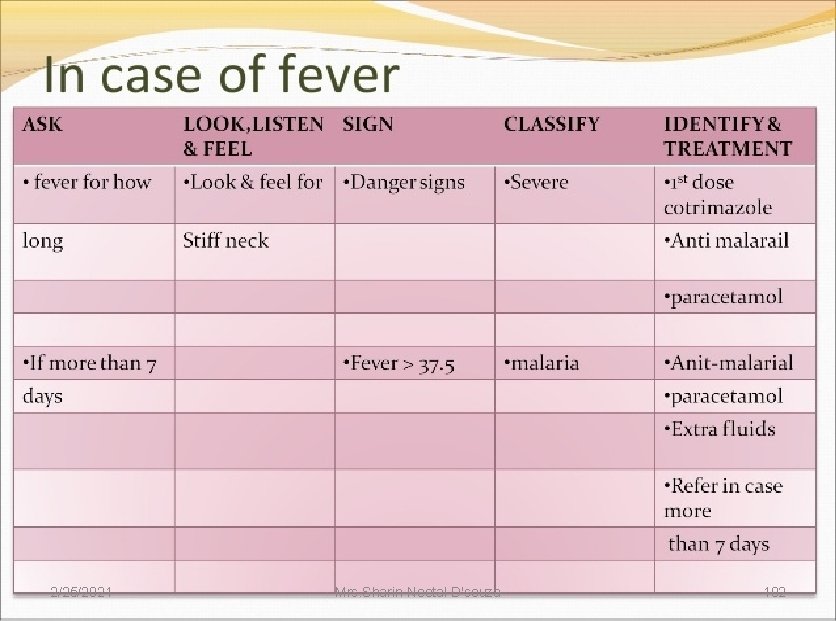
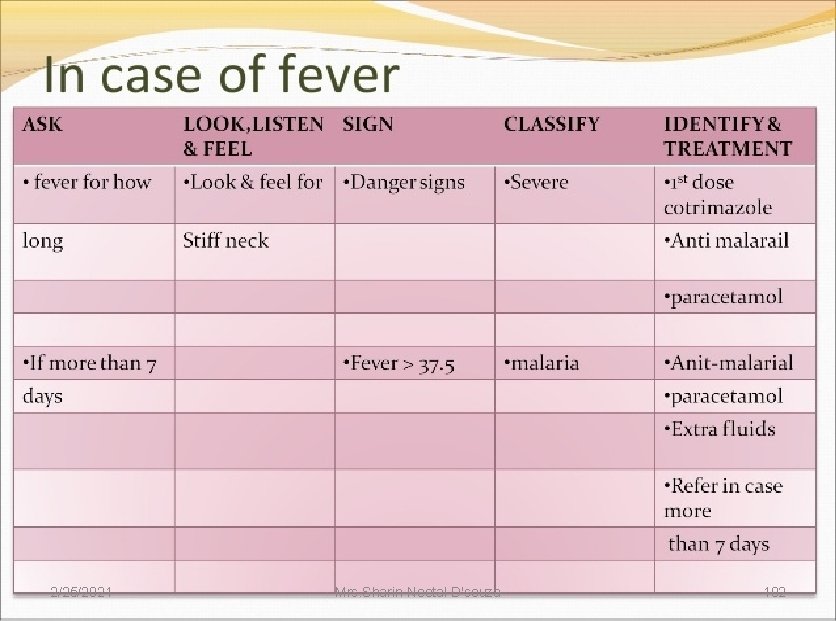
Fever Body temperature should be checked in all sick children brought to an outpatient clinic. 2/25/2021 Mrs. Sharin Neetal D'souza 103
• • • Child with fever should be assessed Risk for malaria Duration of fever Bulging fontanelle Stiff neck Runny nose Measles 2/25/2021 Mrs. Sharin Neetal D'souza 104
Classification of Fever • Any danger sign or • Stiff neck • Bulging fontanelle 2/25/2021 VERY SEVERE FEBRILE DISEASE Mrs. Sharin Neetal D'souza 105
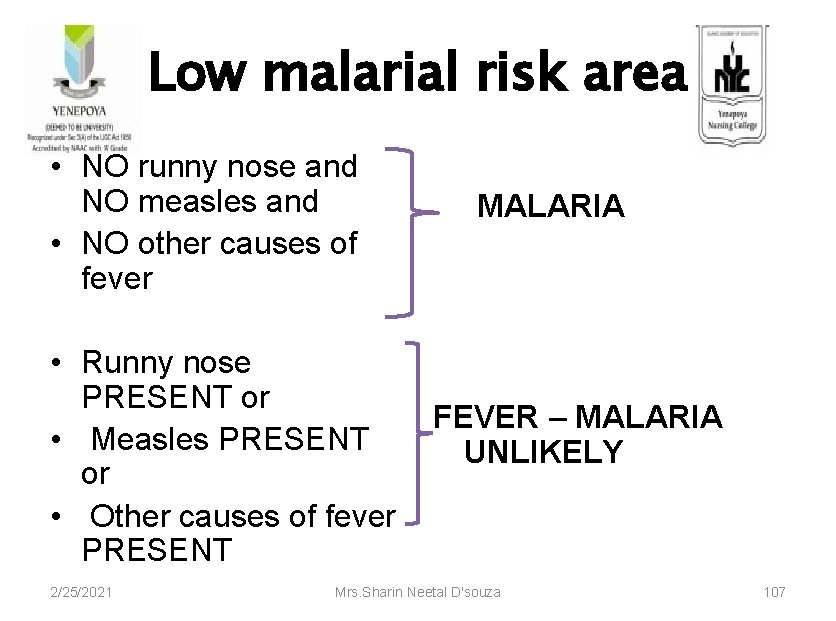
Depending on the level of malaria High malaria risk • Fever (by history or feels hot or • MALARIA • temperature 37. 5°C or above) 2/25/2021 Mrs. Sharin Neetal D'souza 106
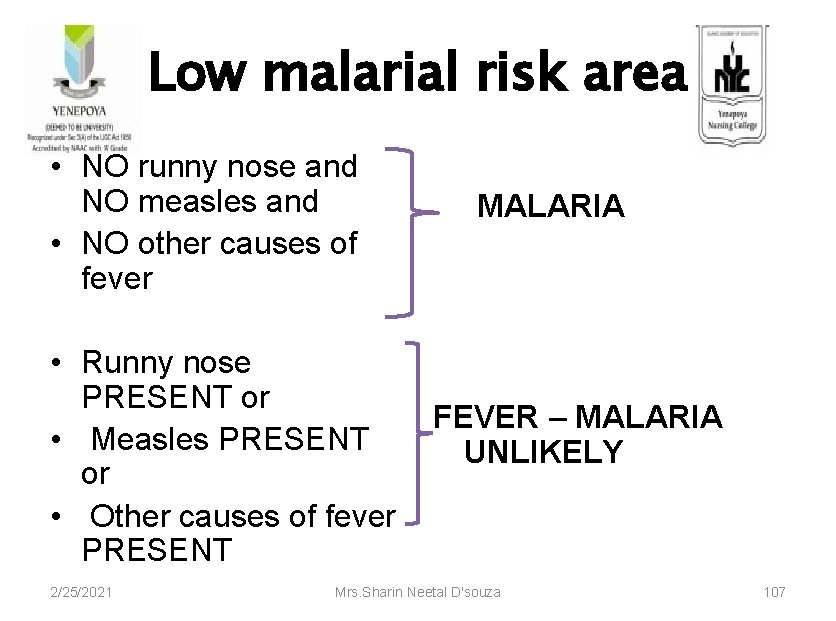
Low malarial risk area • NO runny nose and NO measles and • NO other causes of fever MALARIA • Runny nose PRESENT or FEVER – MALARIA • Measles PRESENT UNLIKELY or • Other causes of fever PRESENT 2/25/2021 Mrs. Sharin Neetal D'souza 107

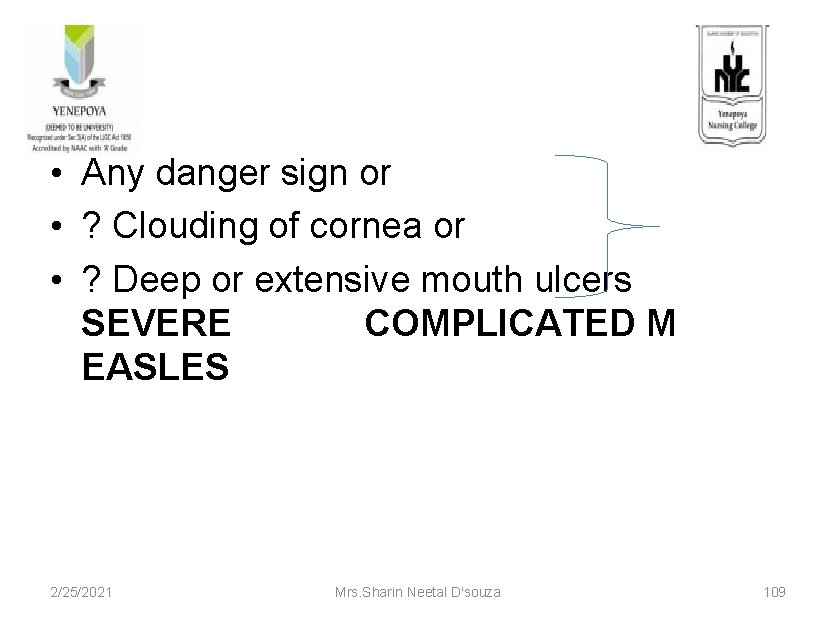
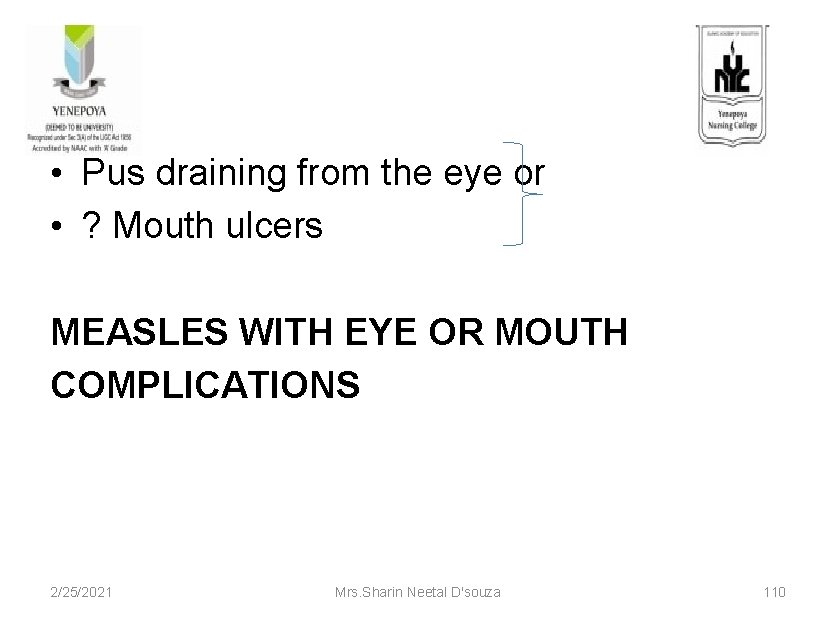
Classification of Measles • Severe complicated measles • Measles with eye or mouth complications • Measles 2/25/2021 Mrs. Sharin Neetal D'souza 108
• Any danger sign or • ? Clouding of cornea or • ? Deep or extensive mouth ulcers SEVERE COMPLICATED M EASLES 2/25/2021 Mrs. Sharin Neetal D'souza 109
• Pus draining from the eye or • ? Mouth ulcers MEASLES WITH EYE OR MOUTH COMPLICATIONS 2/25/2021 Mrs. Sharin Neetal D'souza 110

• Measles now or within the last three • months • MEASLES 2/25/2021 Mrs. Sharin Neetal D'souza 111
2/25/2021 Mrs. Sharin Neetal D'souza 112

2/25/2021 Mrs. Sharin Neetal D'souza 113
EAR PROBLEMS 2/25/2021 Mrs. Sharin Neetal D'souza 114
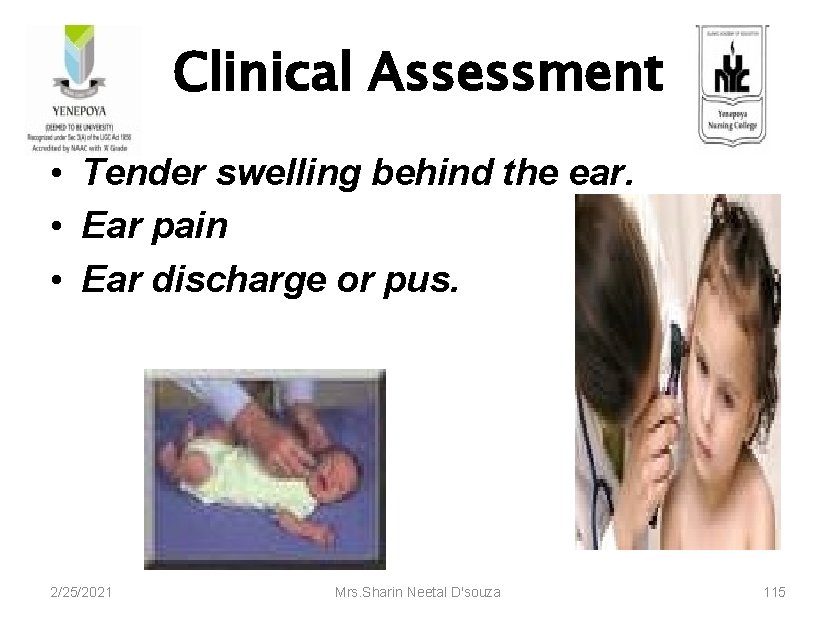
Clinical Assessment • Tender swelling behind the ear. • Ear pain • Ear discharge or pus. 2/25/2021 Mrs. Sharin Neetal D'souza 115

Classification of Ear Problems • Tender swelling behind the ear • MASTOIDITIS • Pus is seen draining from the ear and discharge is reported for less than 14 days or • Ear pain 2/25/2021 • ACUTE EAR INFECTION Mrs. Sharin Neetal D'souza 116

• Pus is seen draining from the ear and discharge is report for 14 days or more. • CHRONIC EAR INFECTION • NO ear pain and NO ear discharge seen draining from the ear • NO EAR INFECTION 2/25/2021 Mrs. Sharin Neetal D'souza 117
2/25/2021 Mrs. Sharin Neetal D'souza 118
2/25/2021 Mrs. Sharin Neetal D'souza 119
2/25/2021 Mrs. Sharin Neetal D'souza 120
2/25/2021 Mrs. Sharin Neetal D'souza 121
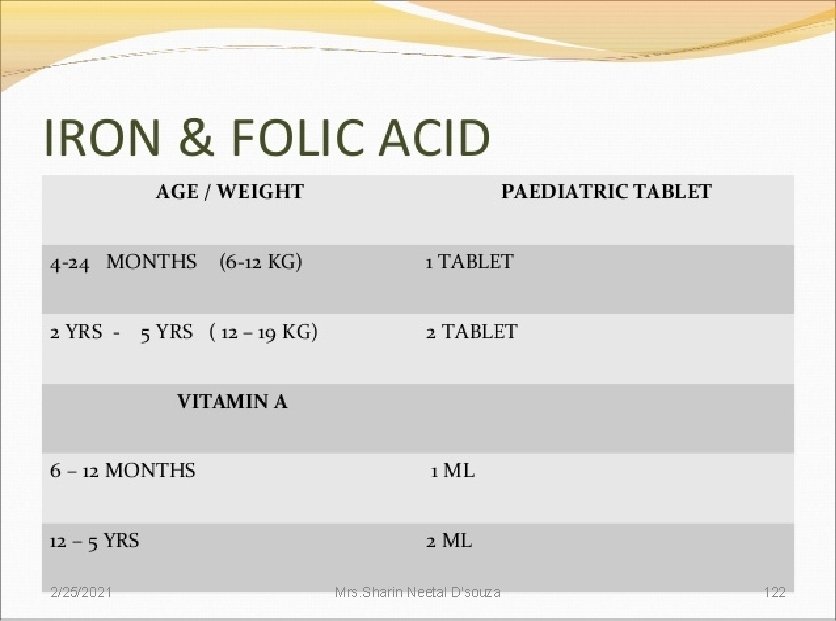
2/25/2021 Mrs. Sharin Neetal D'souza 122
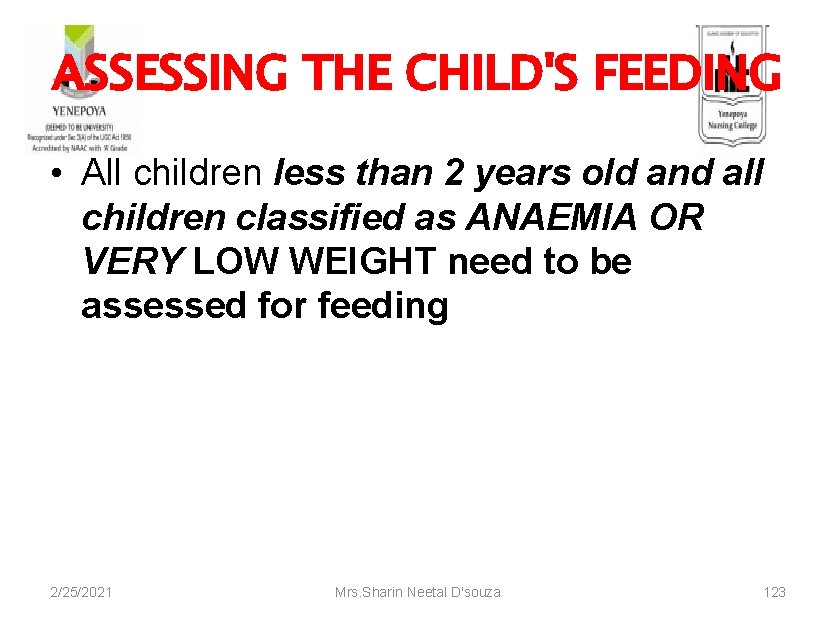
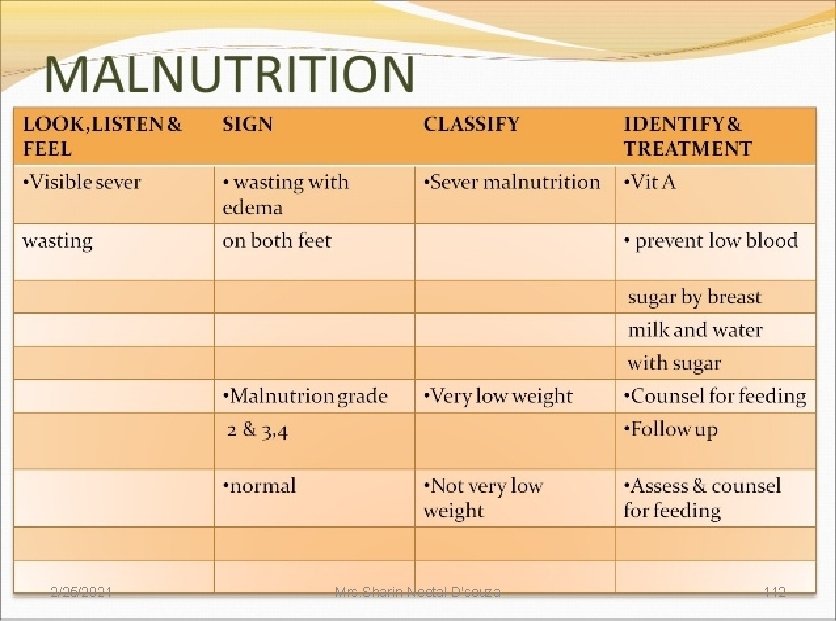
ASSESSING THE CHILD'S FEEDING • All children less than 2 years old and all children classified as ANAEMIA OR VERY LOW WEIGHT need to be assessed for feeding 2/25/2021 Mrs. Sharin Neetal D'souza 123
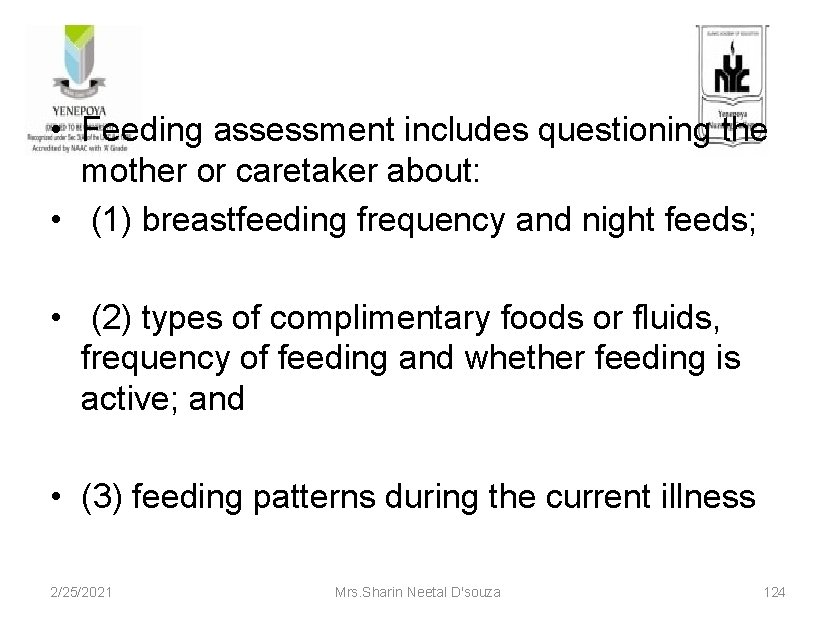
• Feeding assessment includes questioning the mother or caretaker about: • (1) breastfeeding frequency and night feeds; • (2) types of complimentary foods or fluids, frequency of feeding and whether feeding is active; and • (3) feeding patterns during the current illness 2/25/2021 Mrs. Sharin Neetal D'souza 124
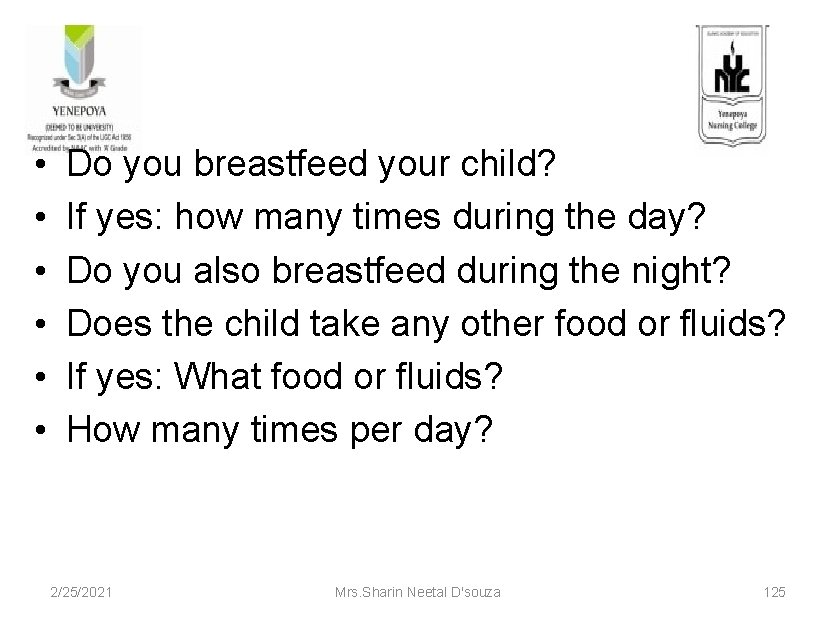
• • • Do you breastfeed your child? If yes: how many times during the day? Do you also breastfeed during the night? Does the child take any other food or fluids? If yes: What food or fluids? How many times per day? 2/25/2021 Mrs. Sharin Neetal D'souza 125
• What do you use to feed the child? • How large are servings? Does the child receive his own serving? • Who feeds the child and how? • During this illness, has the child’s feeding changed? If yes, how? 2/25/2021 Mrs. Sharin Neetal D'souza 126

Identify feeding problems CHILD’S ACTUAL FEEDING RECOMMENDED FEEDING A 3 -month-old is given sugar A 3 -month-old should be given only water as well breast milk and no another food or as breast milk. fluid. A 2 -year-old fed only 3 times A 2 -year-old should receive 2 extra each day. feedings between meals, as well as 3 meals a day. An 8 -month-old is still exclusively breastfed. 2/25/2021 A breastfed 8 -month-old should also be given adequate servings of a nutritious complementary food 3 times a day. Mrs. Sharin Neetal D'souza 127
Other common feeding problems • Difficulty breastfeeding • The mother may mention that breastfeeding is uncomfortable for her, or that her child seems to have difficulty breastfeeding. • You may find that infant’s positioning and attachment could be improved. 2/25/2021 Mrs. Sharin Neetal D'souza 128
• Use of feeding bottle • Feeding bottles should not be used • They are often dirty, and germs easily grow in them. • Also, sucking on a bottle may interfere with the child’s desire to breastfeed. 2/25/2021 Mrs. Sharin Neetal D'souza 129
• Lack of active feeding • Young children often need to be encouraged and assisted to eat. • If a young child is left to feed himself, or if he has to compete with siblings for food, he may not get enough to eat. By asking, • “Who feeds the child and how? ” you should be able to find out if the child is actively being encouraged to eat. 2/25/2021 Mrs. Sharin Neetal D'souza 130
• Not feeding well during illness • The child may be eating much less, or eating different foods during illness. • Children often lose their appetite during illness. • They should be offered their favorite nutritious foods, if possible, to encourage eating. 2/25/2021 Mrs. Sharin Neetal D'souza 131
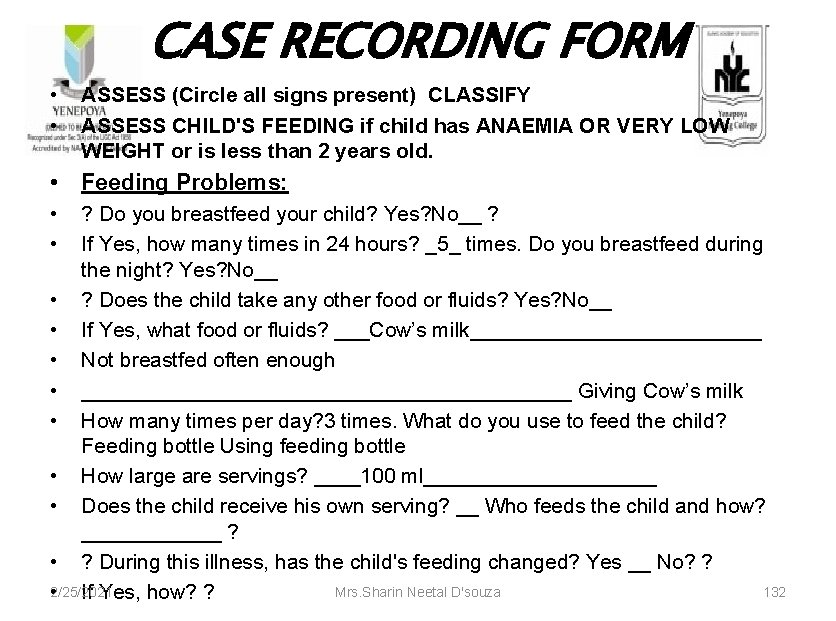
CASE RECORDING FORM • • ASSESS (Circle all signs present) CLASSIFY ASSESS CHILD'S FEEDING if child has ANAEMIA OR VERY LOW WEIGHT or is less than 2 years old. • Feeding Problems: • • ? Do you breastfeed your child? Yes? No__ ? If Yes, how many times in 24 hours? _5_ times. Do you breastfeed during the night? Yes? No__ • ? Does the child take any other food or fluids? Yes? No__ • If Yes, what food or fluids? ___Cow’s milk_____________ • Not breastfed often enough • _____________________ Giving Cow’s milk • How many times per day? 3 times. What do you use to feed the child? Feeding bottle Using feeding bottle • How large are servings? ____100 ml__________ • Does the child receive his own serving? __ Who feeds the child and how? ______ ? • ? During this illness, has the child's feeding changed? Yes __ No? ? Mrs. Sharin Neetal D'souza 132 • 2/25/2021 If Yes, how? ?
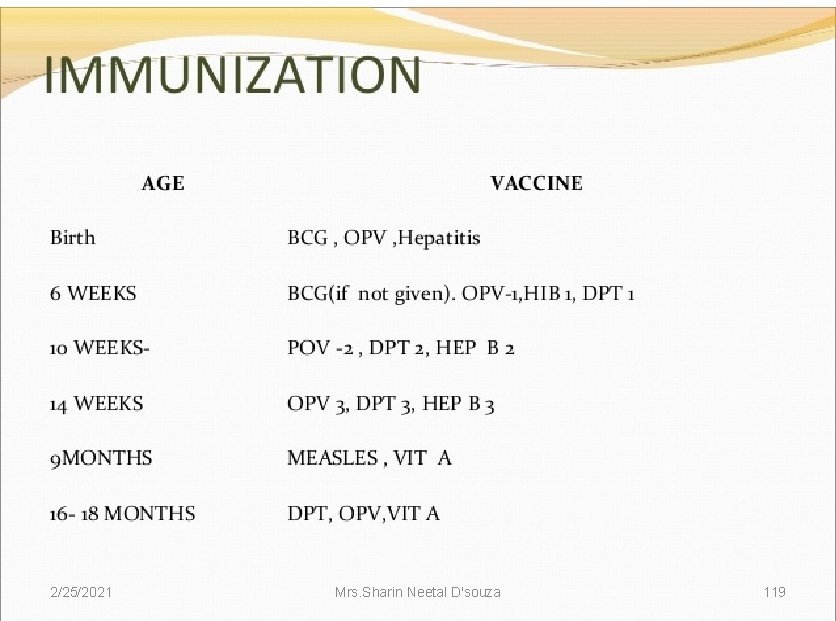
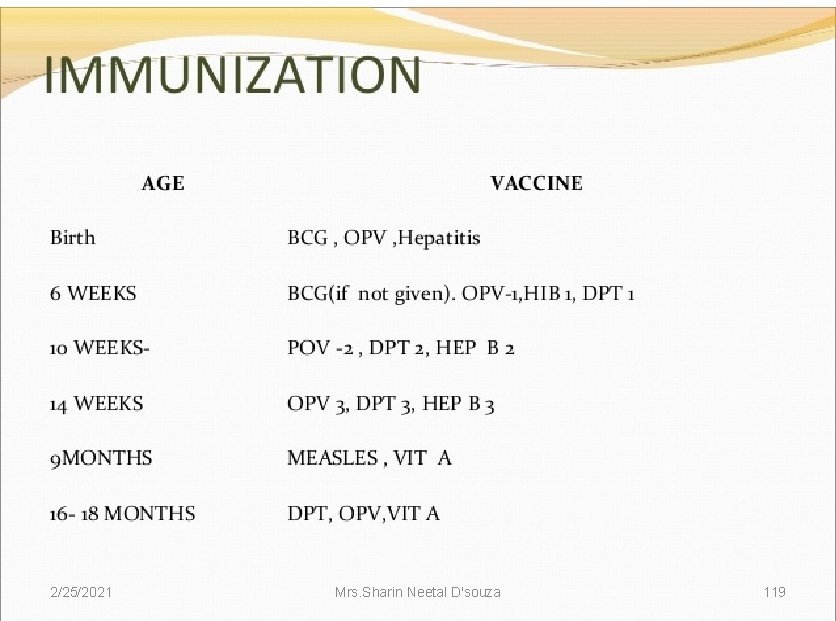
CHECKING IMMUNIZATION, VITAMIN -A AND FOLIC ACID SUPPLEMENTATION STATUS • The immunization status of every sick child brought to a health facility should be checked. • Illness is not a contraindication to immunization. • In practice, sick children may be even more in need of protection provided by immunization than well children. 2/25/2021 Mrs. Sharin Neetal D'souza 133
Four common situations that are contraindicated to immunization of sick children: • Children who are being referred urgently to the hospital should not be immunized. • There is no medical contraindication, but if the child dies, the vaccine may be incorrectly blamed for the death. 2/25/2021 Mrs. Sharin Neetal D'souza 134
• Live vaccines (BCG, measles, polio) should not be given to children with immunodeficiency diseases, or to children who are immuno suppressed due to malignant disease, therapy with immunosuppressive agents or irradiation. • However, all the vaccines, including BCG and yellow fever, can be given to children who have, or are suspected of having, HIV infection but are not yet symptomatic. BCG, if not given at birth, can be given in the next visit 2/25/2021 Mrs. Sharin Neetal D'souza 135
• DPT 2/ DPT 3 should not be given to children who have had convulsions or shock within three days of a previous dose of DPT. • DT can be administered instead of DPT. • DPT should not be given to children with recurrent convulsions or another active neurological disease of the central nervous system. 2/25/2021 Mrs. Sharin Neetal D'souza 136
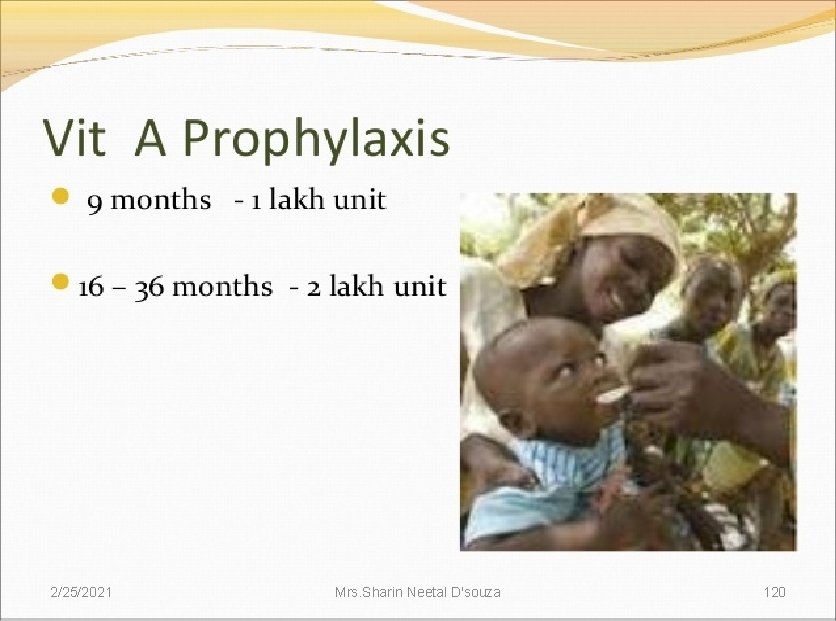
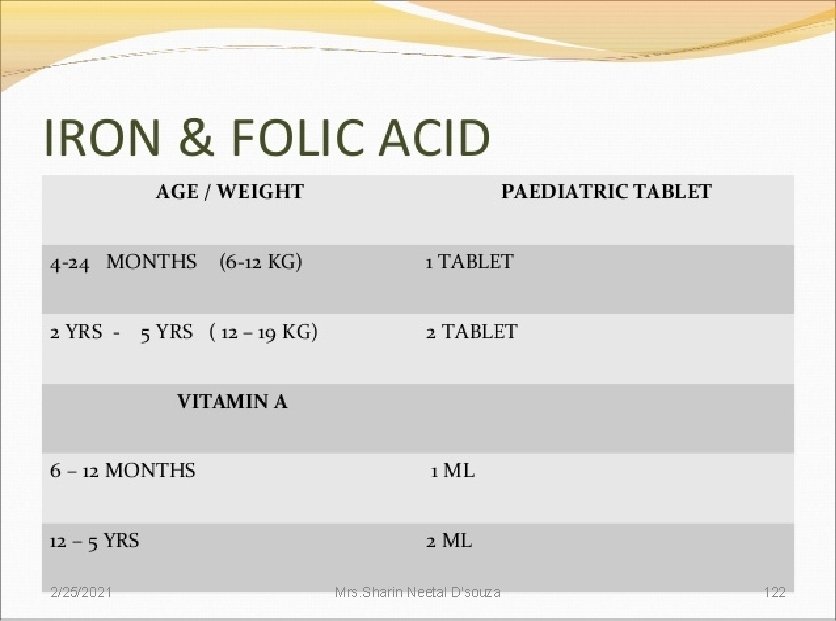
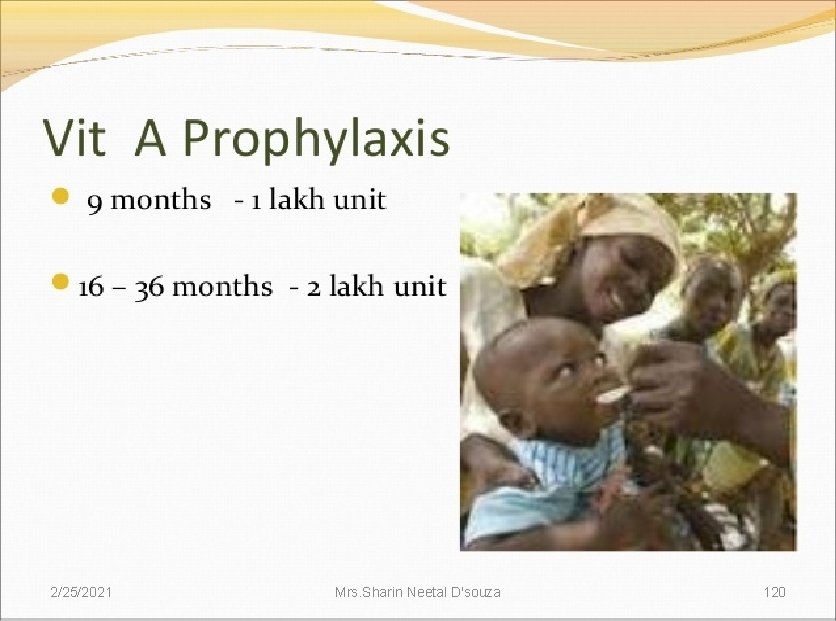
• After checking immunization status, determine if the child needs vitamin- A supplementation and/or prophylactic iron folic acid supplementation. 2/25/2021 Mrs. Sharin Neetal D'souza 137

• • Immunization status section of the case recording form. MANAGEMENT OF THE SICK CHILD AGE 2 MONTHS UP TO 5 YEARS Child's Name: _____Salim________ Age: 4 months Weight: 5. 5 kg Temperature: 36 ? C ASK: What are the child's problems? Cough Initial Visit? ? Follow-up Visit? __ ASSESS (Circle all signs present) CLASSIFY CHECK THE CHILD'S IMMUNIZATION STATUS Circle immunizations needed • today • __? __ ___? _ __________ • Return for next • BCG DPT 1 DPT 2 DPT 3 DPT(Booster) DT immunization on: • __? __ ___? _ _______ • OPV 0 OPV 1 OPV 2 OPV 3 Measles OPV • Measles at 9 • months age • _______ • 2/25/2021 HEP-B 2 HEP-B 3 Mrs. Sharin Neetal D'souza 138
ASSESSING OTHER PROBLEMS • The IMNCI clinical guidelines focus on five main symptoms (Cough or Difficult Breathing, Diarrhoea, Fever, Ear Problems). • In addition, the assessment steps within each main symptom take into account several other common problems. • For example, conditions such as meningitis, sepsis, tuberculosis, conjunctivitis, and different causes of fever such as ear infection and sore throat are routinely assessed within the IMNCI case management process. 2/25/2021 Mrs. Sharin Neetal D'souza 139
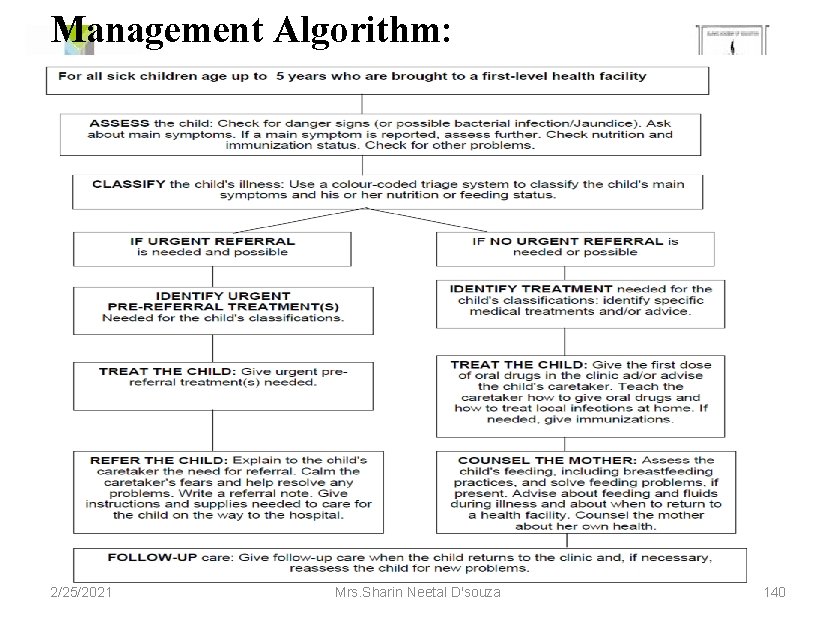
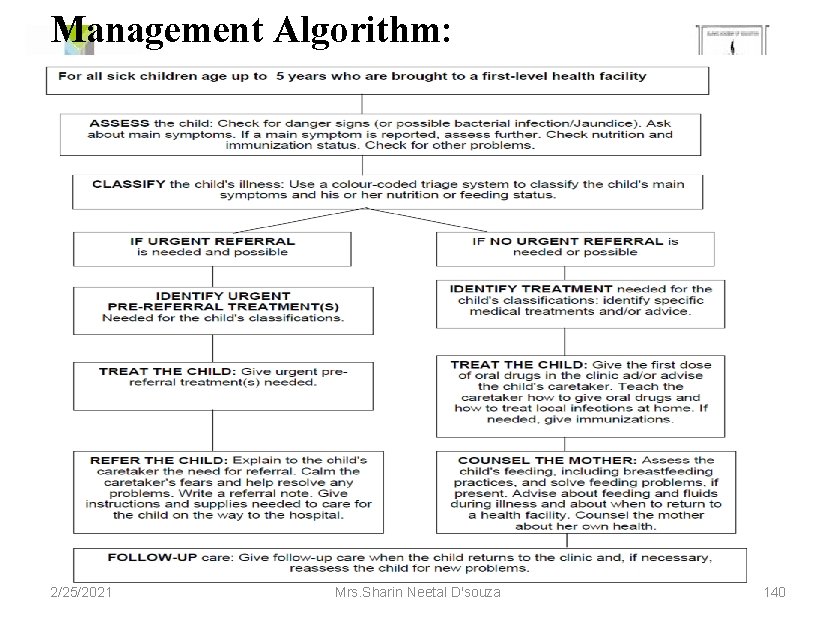
Management Algorithm: 2/25/2021 Mrs. Sharin Neetal D'souza 140
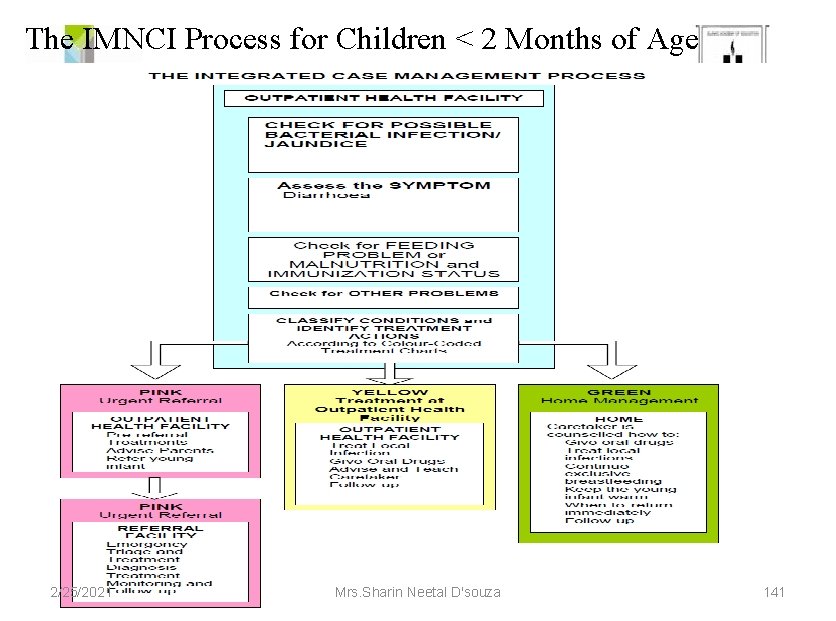
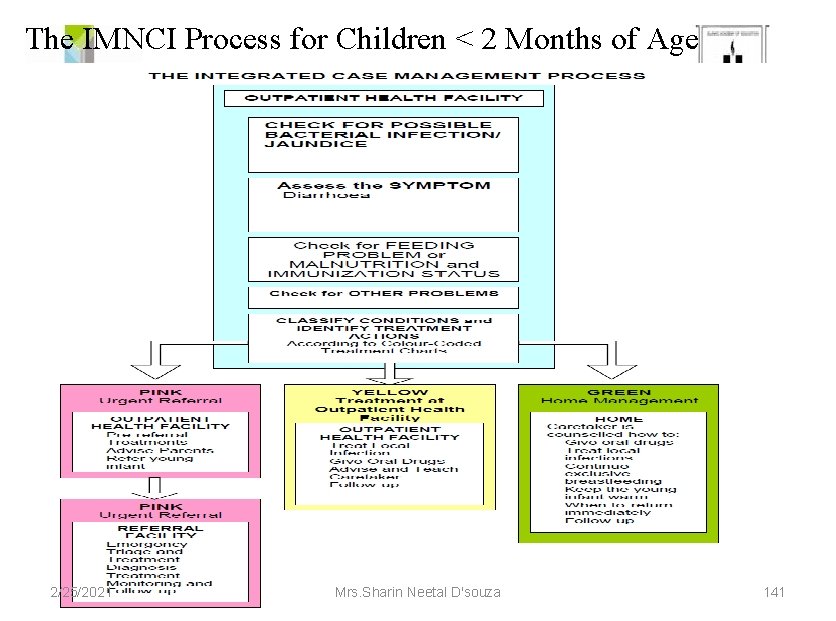
The IMNCI Process for Children < 2 Months of Age 2/25/2021 Mrs. Sharin Neetal D'souza 141
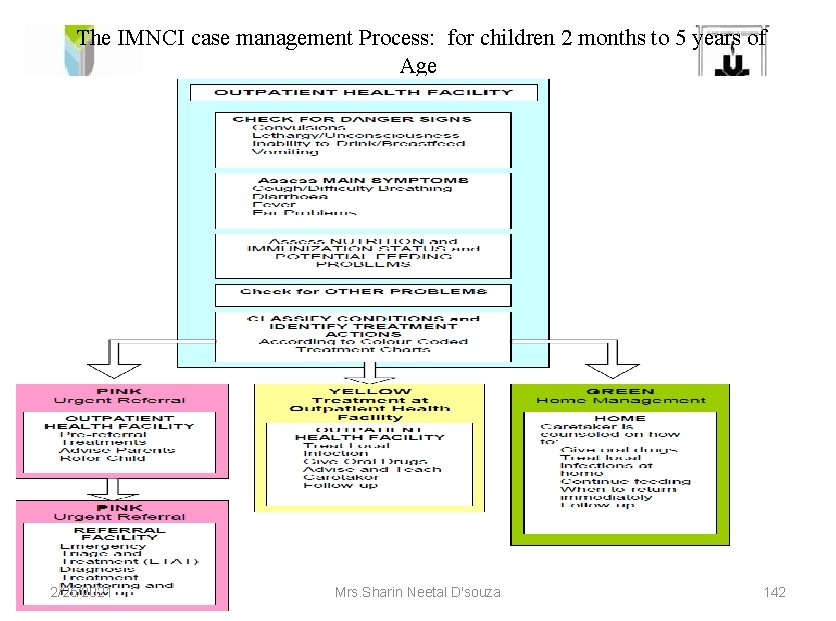
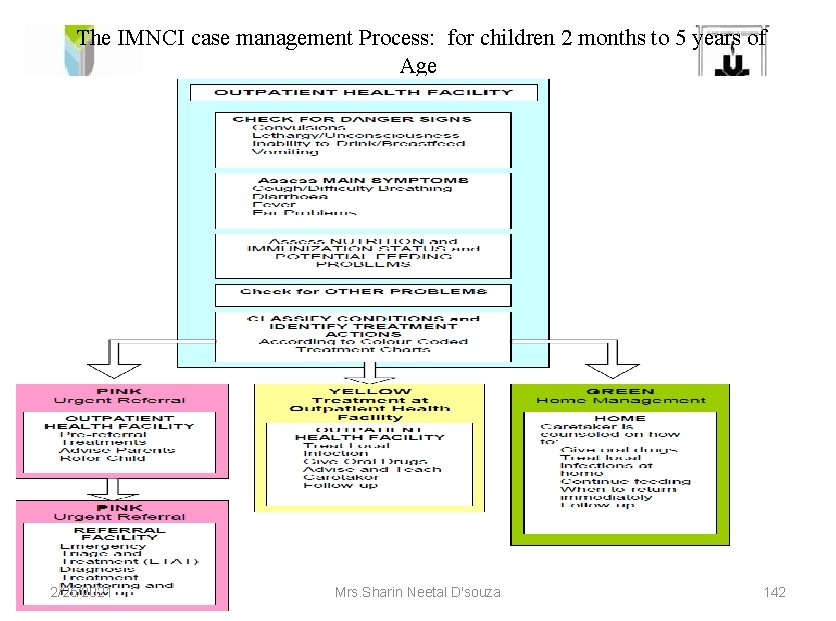
The IMNCI case management Process: for children 2 months to 5 years of Age 2/25/2021 Mrs. Sharin Neetal D'souza 142
Advantages Evidence-based management decisions. Eg: oral rehydration therapy for diarrhea. Focus on communication and counselling skills. Locally adapted recommendation for infant and young child feeding. 2/25/2021 Mrs. Sharin Neetal D'souza 143
Increased effectiveness of care and reduction in cost. Potential of lowering the burden on hospitals. Model for improving one aspect of service delivery that could be applied to other aspects of health care. 2/25/2021 Mrs. Sharin Neetal D'souza 144

What it does not address. . . • Not all major illnesses are included • Management of trauma / other emergencies not included. 2/25/2021 Mrs. Sharin Neetal D'souza 145
Challenges Feasibility Sustaining what is initiated through indicator-based monitoring Making home-based care of young infants operational by ANMs and AWWs 2/25/2021 Mrs. Sharin Neetal D'souza 146
Future aims To provide a comprehensive newborn and child care package at all levels of care: At the village/household level - AWWs. Sub-center level - through ANMs PHCs - doctors, nurses, and Lady Health Visitors; At First Referral Units – MOs and nurses 2/25/2021 Mrs. Sharin Neetal D'souza 147

Evaluation 1. According to IMNCI green colour refers 2. IMNCI focuses the age group of a. 2 -3 yrs b. 5 -9 yrs c. <2 months d. >10 yrs 3. What are the future plans of IMNCI 4. Which all conditions can be treated under IMNCI 2/25/2021 Mrs. Sharin Neetal D'souza 148
References • Wong’s essentials of pediatric nursing; 17 th edition • Marlow. Text book of paediatric nursing, 6 th edition • Rimple sharma. Text book of paediatric nursing • Parul Datta. Text book of child health nursing • 2/25/2021 Mrs. Sharin Neetal D'souza 149

2/25/2021 Mrs. Sharin Neetal D'souza 150
 Ready to eat tcs food
Ready to eat tcs food What is a common signal of sudden illness
What is a common signal of sudden illness Early and middle childhood
Early and middle childhood Imnci colour coding
Imnci colour coding Imnci colour coding system
Imnci colour coding system Newborn bilirubin chart
Newborn bilirubin chart Htig vs ats
Htig vs ats Imnci guidelines for diarrhoea
Imnci guidelines for diarrhoea Imnci guidelines for diarrhoea
Imnci guidelines for diarrhoea Dr sudhanshu mishra
Dr sudhanshu mishra Yorkshire and humber neonatal network
Yorkshire and humber neonatal network Advantages of integrated weed management
Advantages of integrated weed management Vasculopatía lenticuloestriada neonatal
Vasculopatía lenticuloestriada neonatal Circulação fetal
Circulação fetal Circulação neonatal
Circulação neonatal Tamiz neonatal
Tamiz neonatal Esfuerzo respiratorio neonatal
Esfuerzo respiratorio neonatal Neonatal ölüm hızı
Neonatal ölüm hızı Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis temprana
Sepsis temprana Fisiopatologia de ictericia neonatal
Fisiopatologia de ictericia neonatal Mortality rate formula
Mortality rate formula Poliglobulia
Poliglobulia Exaguinotransfusion
Exaguinotransfusion Phototherapy machine working principle
Phototherapy machine working principle Parâmetros iniciais ventilação mecânica neonatal
Parâmetros iniciais ventilação mecânica neonatal Dolorimeter
Dolorimeter Oxigenoterapia por halo
Oxigenoterapia por halo Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Suprasternal retraction
Suprasternal retraction Neonatarum
Neonatarum Neonatal sepsis
Neonatal sepsis Dope neonatal resuscitation
Dope neonatal resuscitation Iap ug teaching slides
Iap ug teaching slides Neonatal resuscitation definition
Neonatal resuscitation definition Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Niveles normales de bilirrubina en neonatos
Niveles normales de bilirrubina en neonatos Hemoglucotest en neonatos
Hemoglucotest en neonatos Escala de kramer modificada
Escala de kramer modificada Icterícia neonatal valores de referência
Icterícia neonatal valores de referência Diagnóstico de enfermería para ictericia adulto
Diagnóstico de enfermería para ictericia adulto Ascites veins
Ascites veins Qual o grau normal da icterícia
Qual o grau normal da icterícia Cuidados de enfermería en oxigenoterapia neonatal
Cuidados de enfermería en oxigenoterapia neonatal Circulação fetal
Circulação fetal Tetralogy of fallot heart sounds
Tetralogy of fallot heart sounds Hipernatremia neonatal
Hipernatremia neonatal Pacto pela redução da mortalidade materna e neonatal
Pacto pela redução da mortalidade materna e neonatal Credeização
Credeização Neonatal alloimmün trombositopeni
Neonatal alloimmün trombositopeni Neonatal sepsis symptoms
Neonatal sepsis symptoms Indication for exploratory laparotomy
Indication for exploratory laparotomy Neonatal cholestasis definition
Neonatal cholestasis definition Neonatal progeria
Neonatal progeria Icterícia neonatal tratamento
Icterícia neonatal tratamento Hoja de balance hidrico en enfermeria
Hoja de balance hidrico en enfermeria Physiopathologie de l'ictère néonatal
Physiopathologie de l'ictère néonatal Neonatal cholestasis naspghan
Neonatal cholestasis naspghan Clasificacion de ictericia neonatal
Clasificacion de ictericia neonatal Pathologic jaundice
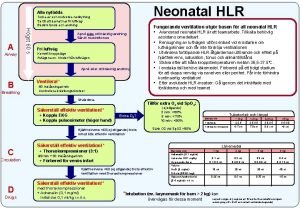
Pathologic jaundice Neonatal hlr
Neonatal hlr Vasculopatia lenticulo estriada
Vasculopatia lenticulo estriada Reflejos en el período neonatal
Reflejos en el período neonatal Clinical manifestation of hepatitis
Clinical manifestation of hepatitis Warm chain
Warm chain Differential diagnosis of jaundice in pediatrics
Differential diagnosis of jaundice in pediatrics Dr sneha sood
Dr sneha sood Indice infeccioso neonatal
Indice infeccioso neonatal Babinski reflex
Babinski reflex Rishika pandey
Rishika pandey Preterm classification
Preterm classification Organization of neonatal unit
Organization of neonatal unit Neonatal kolestaz
Neonatal kolestaz Neonatal jaundice physical examination
Neonatal jaundice physical examination Neonatal mortality rate formula
Neonatal mortality rate formula Neonatal reflexes
Neonatal reflexes Neurológica
Neurológica Glascow coma score
Glascow coma score Dope reanimacion neonatal
Dope reanimacion neonatal Hipocalcemia neonatal
Hipocalcemia neonatal The boy in the striped pajamas setting
The boy in the striped pajamas setting Integrated logistics management
Integrated logistics management Sinotrans-ksa
Sinotrans-ksa Hse risk management framework
Hse risk management framework Integrated watershed management
Integrated watershed management University management system dbms project
University management system dbms project Integrated talent management scorecards
Integrated talent management scorecards Integrated service management
Integrated service management Ipm integrated project management
Ipm integrated project management Pas 99
Pas 99 Enterprise wide quality integrated management software
Enterprise wide quality integrated management software Objectives of ipm
Objectives of ipm Integrated education
Integrated education Power management integrated circuits
Power management integrated circuits Integrated management information system imis
Integrated management information system imis Integrated clinical services management
Integrated clinical services management Advertising and integrated brand promotion 8th edition
Advertising and integrated brand promotion 8th edition Integrated engineering management system
Integrated engineering management system Avaya integrated management site administration
Avaya integrated management site administration Integrated project portfolio management
Integrated project portfolio management What is integrated safety management system
What is integrated safety management system Iqms tutorial
Iqms tutorial Ibm integrated risk management
Ibm integrated risk management Integrated health management system
Integrated health management system Pagba budget
Pagba budget Integrated financial management system
Integrated financial management system Integrated risk management consulting
Integrated risk management consulting Integrated nutrient management for sustainable agriculture
Integrated nutrient management for sustainable agriculture Integrated pest management
Integrated pest management Civil integrated management
Civil integrated management Integrated pest management
Integrated pest management Integrated pest management ____ than pesticides
Integrated pest management ____ than pesticides Iaea gsr part 2
Iaea gsr part 2 What is the third step in integrated pest management?
What is the third step in integrated pest management? Integrated logistics management
Integrated logistics management Integrated information management
Integrated information management Ifms integrated financial management system
Ifms integrated financial management system Building integrated management
Building integrated management Enterprise risk management integrated framework
Enterprise risk management integrated framework Integrated service management
Integrated service management Social development in infancy
Social development in infancy The developing person through childhood and adolescence
The developing person through childhood and adolescence Example of fast mapping
Example of fast mapping Late childhood
Late childhood Rockefeller college professional development program
Rockefeller college professional development program Early childhood education and care directorate
Early childhood education and care directorate Middle and late childhood
Middle and late childhood Ap psych schema
Ap psych schema Infancy and childhood psychology
Infancy and childhood psychology Social development in middle childhood
Social development in middle childhood Infancy and childhood physical development
Infancy and childhood physical development Early childhood of jose rizal
Early childhood of jose rizal Eating a balanced diet during childhood and adolescence
Eating a balanced diet during childhood and adolescence Chapter 11 childhood and neurodevelopmental disorders
Chapter 11 childhood and neurodevelopmental disorders Chapter 10 infancy and childhood
Chapter 10 infancy and childhood The developing person through childhood and adolescence
The developing person through childhood and adolescence Personality development in middle childhood
Personality development in middle childhood Chapter 10 infancy and childhood
Chapter 10 infancy and childhood Psychology chapter 10 infancy and childhood
Psychology chapter 10 infancy and childhood Middle childhood growth and development
Middle childhood growth and development Lesson quiz 3-2 infancy and childhood
Lesson quiz 3-2 infancy and childhood Middle and late childhood physical development
Middle and late childhood physical development Annunciation of the birth of jesus
Annunciation of the birth of jesus The developing person through childhood and adolescence
The developing person through childhood and adolescence Middle and late childhood
Middle and late childhood Childhood rivalry in bali and new guinea
Childhood rivalry in bali and new guinea Rovee-collier
Rovee-collier The crane center ohio
The crane center ohio Module 47 infancy and childhood cognitive development
Module 47 infancy and childhood cognitive development Top management middle management first line management
Top management middle management first line management Management pyramid
Management pyramid