Diarrhea Contd Dr Shreedhar Paudel 26032009 Dysentery Diarrhea




- Slides: 29

Diarrhea Contd…. Dr Shreedhar Paudel 26/03/2009
Dysentery • Diarrhea with visible blood in the stool • Important cause of mortality and morbidity associated with diarrhea • Around 10% of all diarrheal cases • 15% of all death attributed to diarrhea • More chance of developing persistent diarrhea • More chance of getting malnutrition
Dysentery… • Causes: – Shigella dysenteriae type 1 – S. flexneri – Campylobacter jejuni – Enteroinvasive E. coli
Clinical features • Bloody diarrhea—sometimes watery diarrhea will precede bloody one ± mucous • Fever/ subnormal temperature • Cramping abdominal pain • Tenesmus—pain in the rectum during defecation or attempting defecation
Investigations • Stool routine and microscopic examination • Stool culture and sensitivity • CBC • USG abdomen
Management of dysentery • Dysentery should be treated in the line of shigellosis unless proven otherwise • If diagnosed amoebic dysentery later—add antiamoebic therapy

Management… • Four key components of the treatment – Antimicrobials – Fluids – Feeding – Follow-up
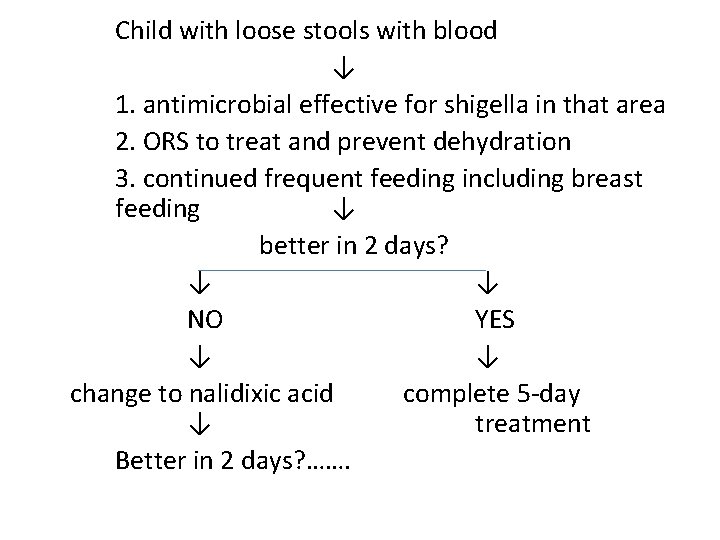
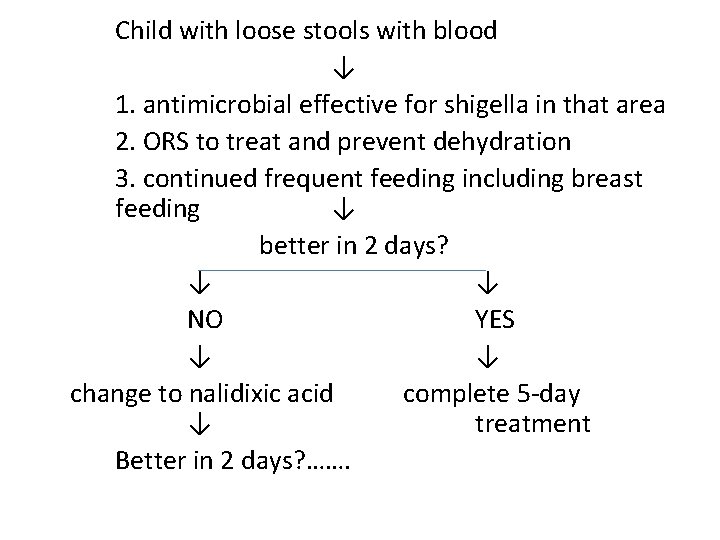
Child with loose stools with blood ↓ 1. antimicrobial effective for shigella in that area 2. ORS to treat and prevent dehydration 3. continued frequent feeding including breast feeding ↓ better in 2 days? ↓ ↓ NO YES ↓ ↓ change to nalidixic acid complete 5 -day ↓ treatment Better in 2 days? …….
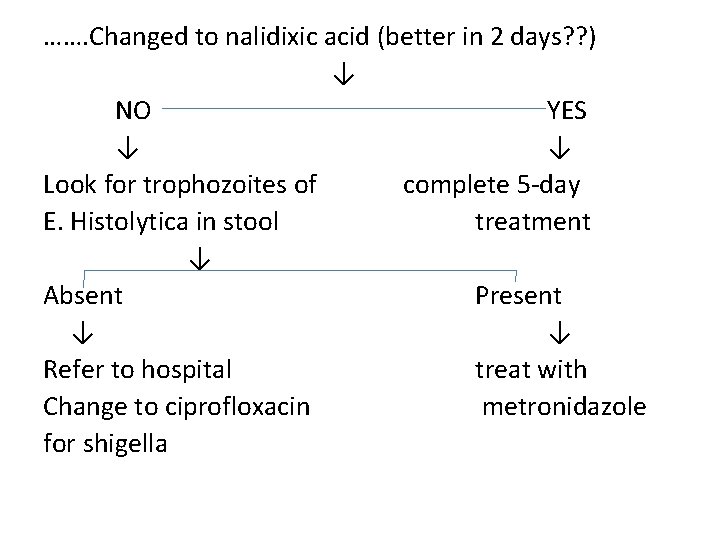
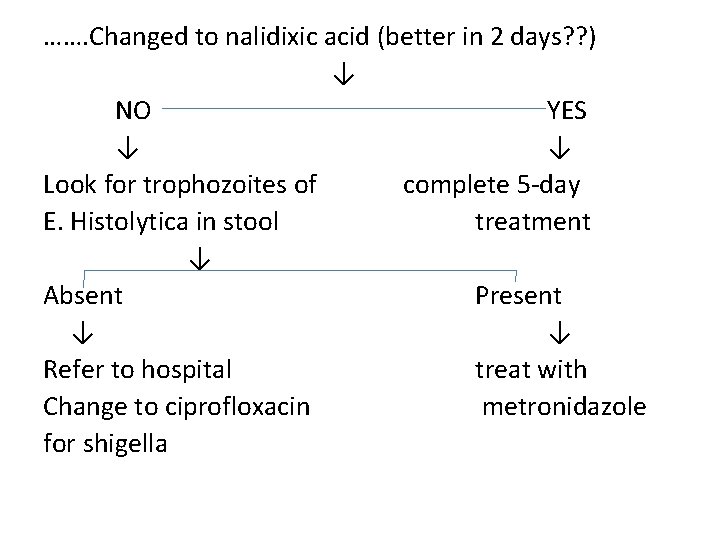
……. Changed to nalidixic acid (better in 2 days? ? ) ↓ NO YES ↓ ↓ Look for trophozoites of complete 5 -day E. Histolytica in stool treatment ↓ Absent Present ↓ ↓ Refer to hospital treat with Change to ciprofloxacin metronidazole for shigella
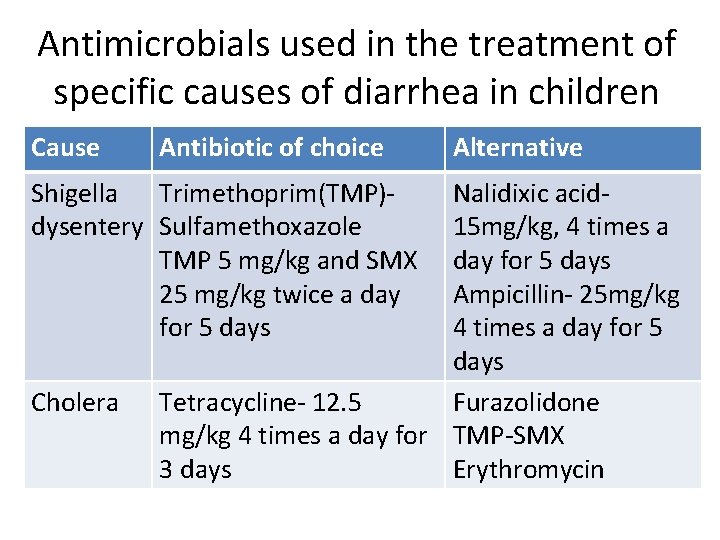
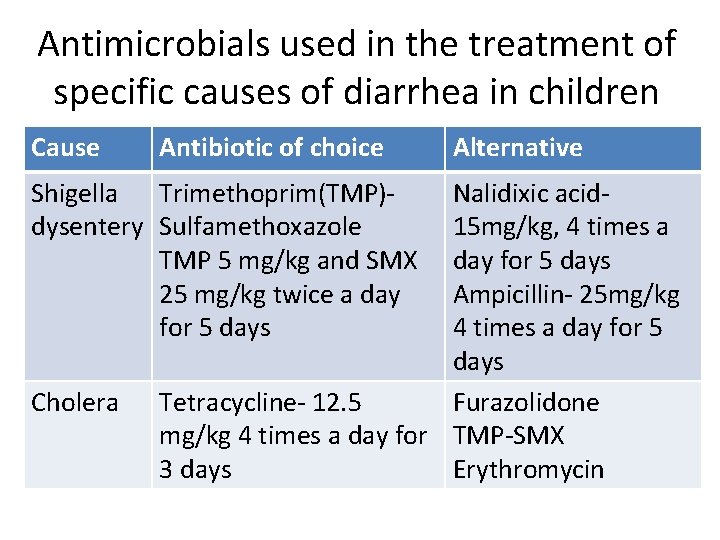
Antimicrobials used in the treatment of specific causes of diarrhea in children Cause Antibiotic of choice Shigella Trimethoprim(TMP)dysentery Sulfamethoxazole TMP 5 mg/kg and SMX 25 mg/kg twice a day for 5 days Cholera Alternative Nalidixic acid 15 mg/kg, 4 times a day for 5 days Ampicillin- 25 mg/kg 4 times a day for 5 days Tetracycline- 12. 5 Furazolidone mg/kg 4 times a day for TMP-SMX 3 days Erythromycin
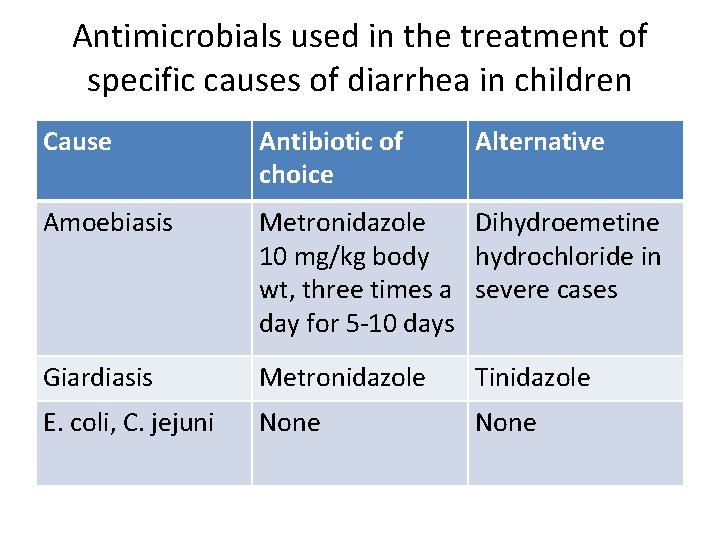
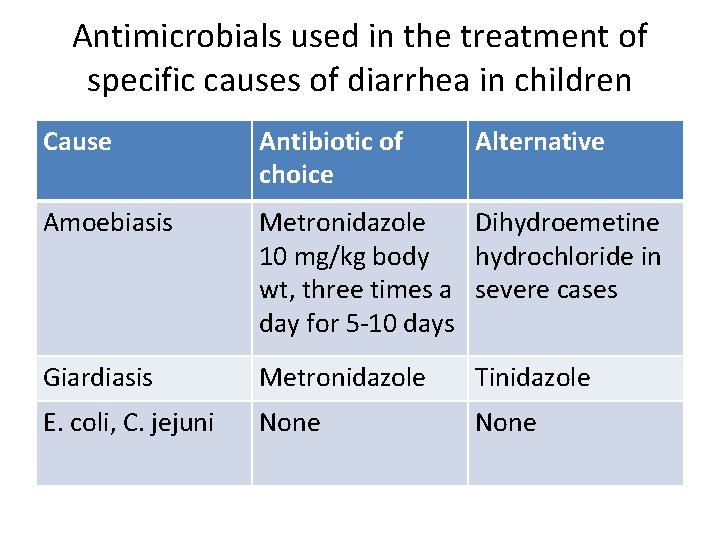
Antimicrobials used in the treatment of specific causes of diarrhea in children Cause Antibiotic of choice Alternative Amoebiasis Metronidazole Dihydroemetine 10 mg/kg body hydrochloride in wt, three times a severe cases day for 5 -10 days Giardiasis Metronidazole Tinidazole E. coli, C. jejuni None
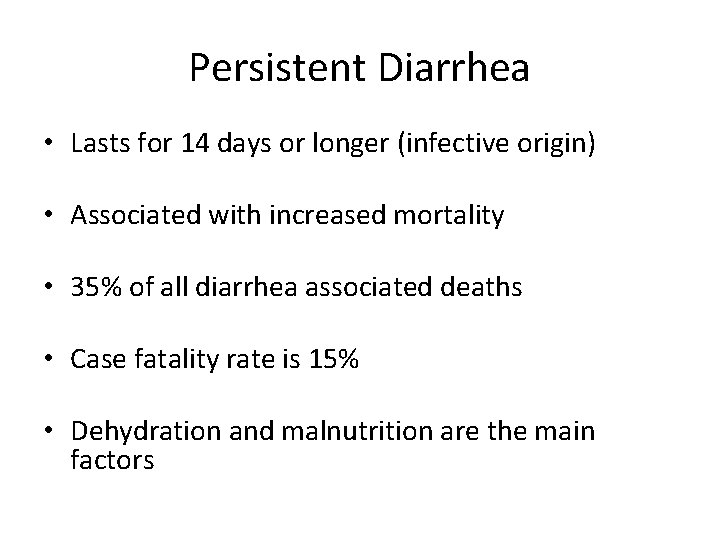
Persistent Diarrhea • Lasts for 14 days or longer (infective origin) • Associated with increased mortality • 35% of all diarrhea associated deaths • Case fatality rate is 15% • Dehydration and malnutrition are the main factors
Causes of Persistent Diarrhea • Mostly no single microbial cause: – Shigella – Salmonella – E. coli – Crysptosporidium and Cyclospora in case of immunocompromised patients – Unclear role of protozoal parasites
Risk factors for persistent diarrhea Malnutrition Recent introduction of animal milk or formula Young age Immunodeficiency status—HIV/AIDS, measles, malnourished child • Recent diarrhea • •
Persistent diarrhoea contd…. • Management: --2/3 rd of the patients can be treated in home --hospitalization required when: --age < 4 months and not breastfed --presence of dehydration --severe malnutrition --presence or suspicion of systemic infection
Persistent diarrhoea contd…. • Management: --assess the child for signs of dehydration and give fluids according to treatment Plan A, B, C (for acute diarrhoea) --dietary management—mainstay of therapy
Dietary management of persistent diarrhoea • Infants aged less than 6 months: • Encourage exclusive breast feeding • Reestablish lactation—who are not breast feeding • If only animal milk can be given—replace with curd/lactose free milk (with cup or spoon) • Cooked rice mixed with milk/curd/lactose free formula
Dietary management of persistent diarrhoea………. • Older infants and young children: -breastfeeding should be continued -optimal feeding of mixed diet is important • Diets: -Initial diet (Diet A) → reduced lactose diet-milk rice gruel, rice with curds -Second diet (Diet B)→ lactose free diet with reduced starch—milk protein is replaced by chicken/egg

Dietary management of persistent diarrhoea………. • Diets: -Third diet (Diet C) → monosaccharide based diet—only glucose and a protein source as egg white or chicken -supplemental vitamins and minerals— vit A, zinc
Chronic Diarrhoea/Malabsorption Syndromes • Chronic diarrhoea is the direct consequence of malabsorption • Malabsorption →malnutrition & failure to thrive • Associated with abnormal stools which continues over several months • Dehydration is rare ( common in persistent D)
Chronic Diarrhoea/Malabsorption Syndromes………. • Path physiologic categories: – Impaired intraluminal digestion → exocrine pancreatic insuffiency – Impaired intestinal malabsorption → celiac disease (total villous atrophy), partial villous atrophy (food protein sensitivity, malnutrition, giardia lamblia infestation) – Impaired fermentation →congenital deficiency of mucosal enzymes (liquid acidic stool)

Chronic Diarrhoea/Malabsorption Syndromes………. • Investigations: – Repeated stool examination especially for Giardia lamblia – Fecal fat excretion studies – Intestinal biopsy – Specific tests→ sweat chloride for cystic fibrosis; exocrine pancreatic function tests; serology for celiac disease; breath analysis for carbohydrate malabsorption
Chronic Diarrhoea/Malabsorption Syndromes………. • Management: – Of the underlying problem – Avoid allergic diets – Management of diarrhoea and dehydrationif present
Celiac Disease • Gluten sensitive enteropathy • Permanent intestinal intolerance to dietary wheat gliadin • Has strong genetic association • Immunologically mediated- cell damage
Celiac Disease……. . • Clinical features: – Chronic diarrhoea – Abdominal distension – Muscle wasting – Failure to thrive – Anorexia – Irritability – Vomiting ±
Celiac Disease……. . • H/O after initial normal course child starts having foul, greasy and bulky stool weeks to months after introduction of wheat into the diet • Weight gain stops • Child appears miserable • Short stature—prominent sign
Celiac Disease……. . • Diagnosis: • Intestinal biopsy—villous atrophy with hyperplasia of crypts • A full clinical and histological remission after withdrawal of gluten from the diet
Celiac Disease……. . • Management: – Strict gluten free diet—lifelong strict gluten free diet is mandatory for children with celiac disease 1) clinical response to gluten free diet is dramatic 2) growth velocity improves very rapidly 3) rice and maize are non toxic and act as wheat substitutes
Milk Protein Intolerance • Manifests—few weeks after the initial exposure to cow’s milk • C/F—diarrhoea – vomiting – abdominal colic – Irritability – failure to thrive – GI hemorrhage Usually subsides by the second year of life
 Sunil paudel
Sunil paudel Alliance future internetlapowskyprotocol
Alliance future internetlapowskyprotocol Die of dysentery
Die of dysentery Laboratory diagnosis of dysentery
Laboratory diagnosis of dysentery Swine dysentery
Swine dysentery Good protists
Good protists Swine dysentery
Swine dysentery Overflow diarrhea
Overflow diarrhea What is bile acid diarrhea
What is bile acid diarrhea Diarrhea chief complaint
Diarrhea chief complaint Chronic diarrhea
Chronic diarrhea Travelers diarrhea
Travelers diarrhea Optimental formula
Optimental formula Bile acid diarrhea
Bile acid diarrhea Diarrhea plan a
Diarrhea plan a Diarrhea dan
Diarrhea dan Dr ali azzam
Dr ali azzam Type of diarrhea
Type of diarrhea Pig diarrhea chart
Pig diarrhea chart Why does metformin cause gastrointestinal problems
Why does metformin cause gastrointestinal problems Diarrhoea introduction
Diarrhoea introduction Spinal reflexology chart
Spinal reflexology chart Imnci
Imnci Zinc diarrhea
Zinc diarrhea Tricomonase vaginalis
Tricomonase vaginalis Cholera
Cholera Overflow diarrhea
Overflow diarrhea Factitial diarrhea
Factitial diarrhea Radwan
Radwan What does hiv diarrhea look like
What does hiv diarrhea look like