Urinary Tract Infection Dr Shreedhar Paudel Urinary Tract









- Slides: 31

Urinary Tract Infection Dr. Shreedhar Paudel
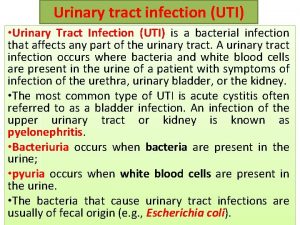
Urinary Tract Infection… • Incidence equal in girls and boys till infancy • Incidence in girls increases afterwards • Organisms: – Escherichia coli ( predominant periurethral flora) – Klebsiella – Proteus – Pseudomonas – enterococcus
Urinary Tract Infection… • Risk factors: – Female – Neurogenic bladder* – Vesicoureteral reflux * – Obstructive uropathy* – Urethral instrumentation – Wiping from back to front – Pinworm infestation – Voiding dysfunction * (30 -40 % of UTI in children)

Urinary Tract Infection… • Clinical features: – Neonates → features of sepsis with fever, vomiting diarrhea, poor weight gain and lethargy – Older infants → unexplained fever, frequent micturition – Distal UTI → dysuria, hypogastric pain, frequency and urgency of micturition
Urinary Tract Infection… • Clinical features: – Pyelonephritis → flank pain, fever with chills and rigors – Excessive crying or straining during voiding, dribbling, weak stream, palpable bladder → urinary obstruction
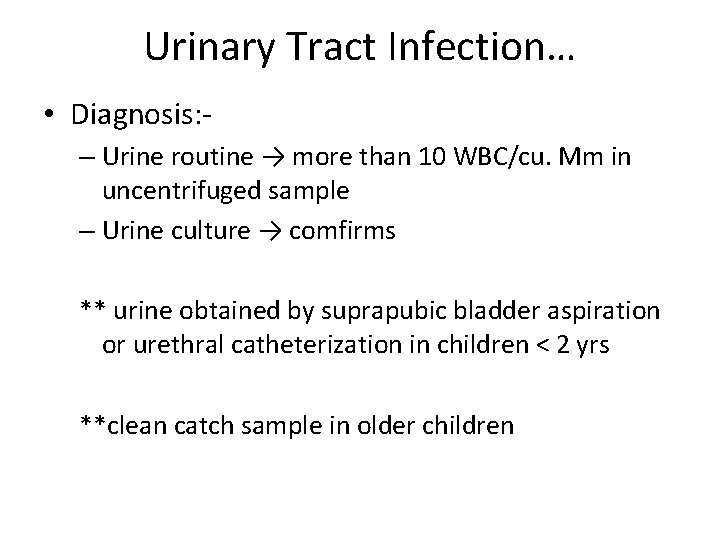
Urinary Tract Infection… • Diagnosis: – Urine routine → more than 10 WBC/cu. Mm in uncentrifuged sample – Urine culture → comfirms ** urine obtained by suprapubic bladder aspiration or urethral catheterization in children < 2 yrs **clean catch sample in older children
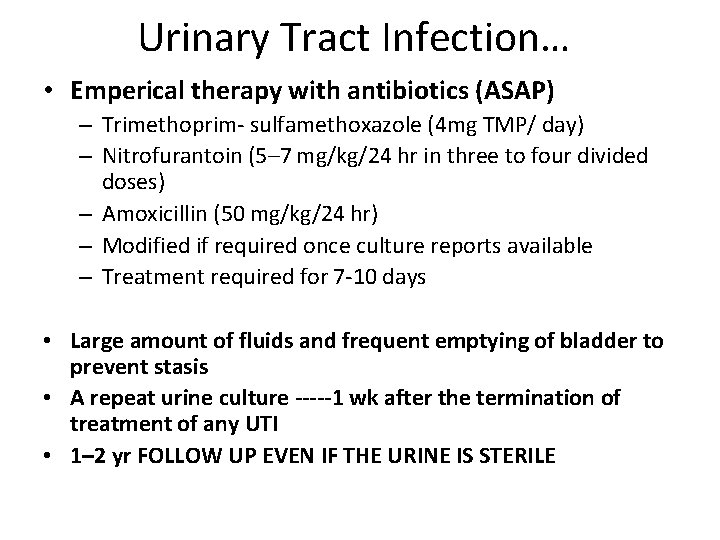
Urinary Tract Infection… • Emperical therapy with antibiotics (ASAP) – Trimethoprim- sulfamethoxazole (4 mg TMP/ day) – Nitrofurantoin (5– 7 mg/kg/24 hr in three to four divided doses) – Amoxicillin (50 mg/kg/24 hr) – Modified if required once culture reports available – Treatment required for 7 -10 days • Large amount of fluids and frequent emptying of bladder to prevent stasis • A repeat urine culture -----1 wk after the termination of treatment of any UTI • 1– 2 yr FOLLOW UP EVEN IF THE URINE IS STERILE

Vesicoureteral Reflux(VUR) • Retrograde flow of urine from the bladder to the upper urinary tract • Rise in intravesical pressure occuring during micturition is freely transmitted to ureter, renal pelvis, papillary collecting ducts and renal tubules • Pathogenic organism gain access to renal parenchyma → renal inflammation and scarring (Reflux nephropathy)
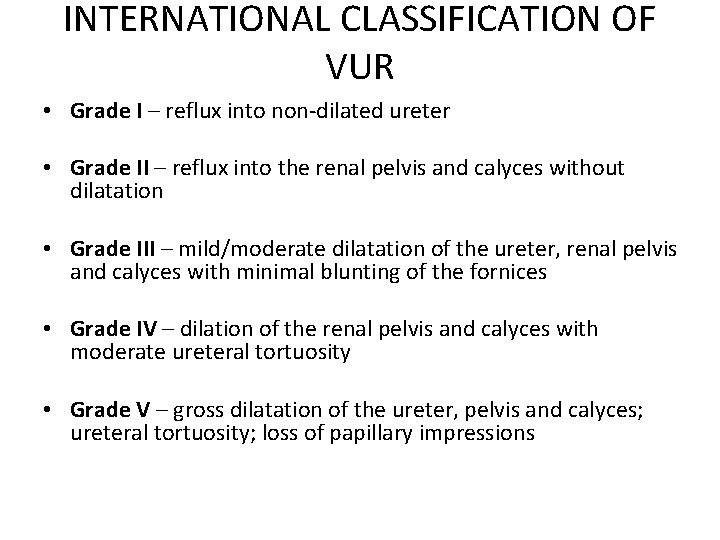
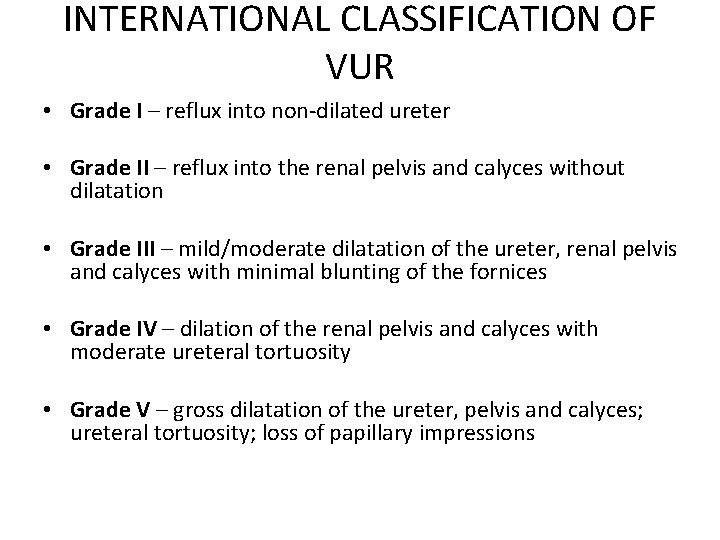
INTERNATIONAL CLASSIFICATION OF VUR • Grade I – reflux into non-dilated ureter • Grade II – reflux into the renal pelvis and calyces without dilatation • Grade III – mild/moderate dilatation of the ureter, renal pelvis and calyces with minimal blunting of the fornices • Grade IV – dilation of the renal pelvis and calyces with moderate ureteral tortuosity • Grade V – gross dilatation of the ureter, pelvis and calyces; ureteral tortuosity; loss of papillary impressions

INTERNATIONAL CLASSIFICATION OF VUR…. .
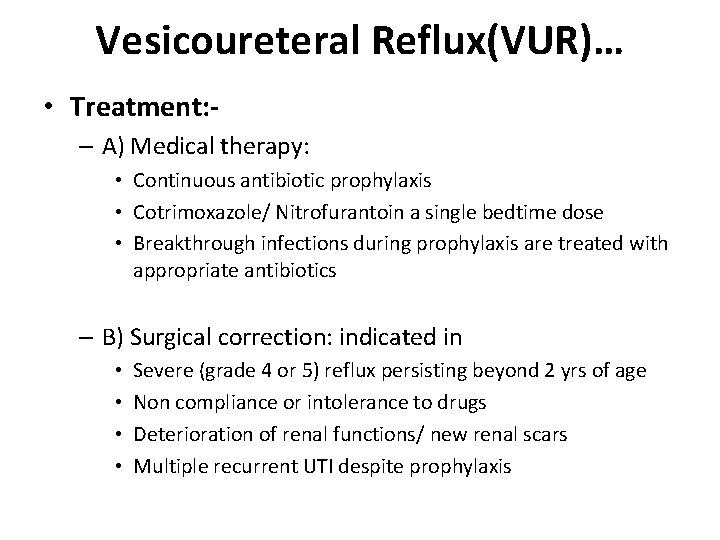
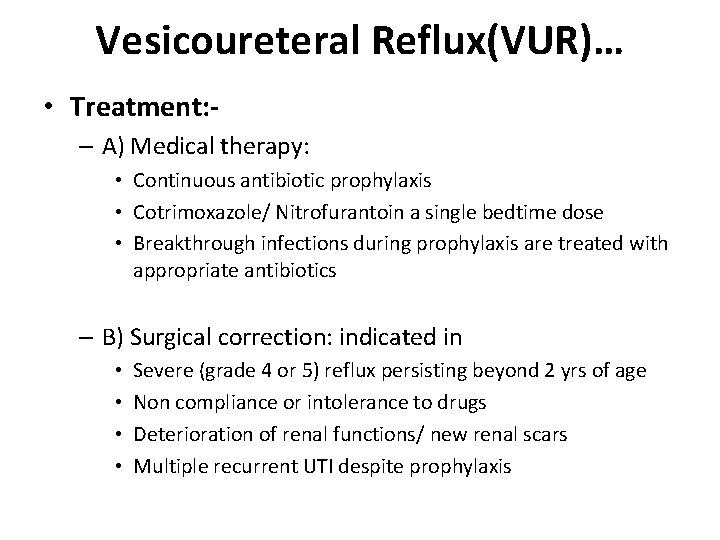
Vesicoureteral Reflux(VUR)… • Treatment: – A) Medical therapy: • Continuous antibiotic prophylaxis • Cotrimoxazole/ Nitrofurantoin a single bedtime dose • Breakthrough infections during prophylaxis are treated with appropriate antibiotics – B) Surgical correction: indicated in • • Severe (grade 4 or 5) reflux persisting beyond 2 yrs of age Non compliance or intolerance to drugs Deterioration of renal functions/ new renal scars Multiple recurrent UTI despite prophylaxis

Vesicoureteral Reflux(VUR)… • Treatment: – General measures: • Liberal fluid intake • Regular and complete bladder emptying • Constipation should be avoided

Vesicoureteral Reflux(VUR)… • LONGTERM ANTIBIOTICS PROPHYLAXIS indications: • < 3 yrs child who have received treatment for the first UTI and being investigated for underlying etiology • >3 UTI episode in a yr in a child with normal urinary tract and no VUR– prophylaxis continued for at least 6 mo after free of UTI • UTI with VUR--- prophylaxis till the child is free from reflux for 6 months

ARF • Life threatening situation with abrupt impairment of renal function resulting in ---retention of nitrogeneous wastes -- inappropriate regulation of fluid and electrolyte homeostatis • Oliguria ( urine flow less than 1 ml/kg/hr)– prominent feature
ARF • Causes: – Prerenal– hypoperfusion – Intrinsic/ renal – Post renal – mechanical obstruction in collecting system • Diagnostic approach: – Important task is to differentiate between prerenal and intrinsic renal failure
ARF • Diagnostic approach: – Pre-renal → intact renal tubular function so urine is highly concentrated with low sodium – Intrinsic → impaired tubular function leads to increased sodium excretion and failure to concentrate urine

ARF • Clinical features: – Anuria or severe oliguria • Investigations: – CBC – Serum urea, creatinine, electrolytes – EKG – to examine for evidence of hyperkalemia
ARF • Management: – Fluid and electrolytes • Fluid therapy guided by intake and output analysis, weight and serum sodium – Diet • Adequate nutritional support (as patients with ARF have increased metabolic needs – Treatment of complications • Early detection and management
ARF • Treatment of complications: • Fluid overload – Pulmonary edema and CHF should be treated with diuretics • Metabolic acidosis – Treated with sodium bicarbonate • HTN – Treated with antihypertensive drugs • Hyponatremia – Fluid restricition ( as hyponatremia is due to excessive fluid rather than salt loss)
ARF • Treatment of complications: • Hyperkalemia →Serious emergency -- its cardiotoxicity can cause sudden death – Calcium antagonizes the cardiotoxicity of hyperkalemia – Calcium gluconate IV (0. 5 -1 ml/kg of 10% calcium gluconate over 10 minutes) – Sodium bicarbonate -- increases the potassium uptake by the cells – Nebulised Salbutamol – IV Glucose with insulin – facilitates intracellular uptake of potassium – Calcium resonium – binds with potassium – Dialysis
ARF • Supportive care – Managed under intensive care – Daily intake and output chart maintainence – Prompt detection and treatment of infections • Dialysis – To remove endogeneous and exogenous toxin, maintain fluid, electrolyte and acid base balance until renal function recovers

CRF • Permanent severe decrease in renal function • End stage renal disease (ESRD) → decline of renal function to a degree when life can not be sustained without chronic dialyses or transplantation
CRF • Causes: – Glomerulonephritis – Reflux nephropathy – Obstructive uropathy – Developmental anomalies– renal hypoplasia, dysplasia – Others – amyloidosis, renal vein thrombosis, renal cortical necrosis
CRF • Management: – Diet – adequate calorie – HTN – be treated with B- blockers, CCB – Anemia – recombinant human erythropoietin – Infections – early detection and treatment
CRF • • RENAL REPALCEMENT THERAPY CHRONIC PERITONEAL DIALYSIS CHRONIC HEMODIALYSIS RENAL TRANSPLANTATION
Hemolytic-Uremic Syndrome (HUS) • • microangiopathic hemolytic anemia thrombocytopenia Uremia thrombotic thrombocytopenic purpura
HUS… • Etiology : • Diarrhea --Shiga toxin–producing Escherichia coli 0157: H 7 – D+ HUS • verotoxin • Shigella, Salmonella, Campylobacter, Streptococcus pneumoniae, Bartonella • viral (coxsackievirus, echovirus, influenza, varicella, HIV, Epstein-Barr) infections. • oral contraceptives, mitomycin, cyclosporine
HUS…. • Clinical Manifestations: – children younger than age 4 yr – onset usually preceded by a gastroenteritis characterized by fever, vomiting, abdominal pain, and diarrhea that is often bloody – Less commonly, patients may present after an upper respiratory tract infection.
HUS • Clinical Manifestations: – Sudden onset of pallor, irritability, weakness, lethargy, and oliguria usually occurs 5– 10 days after the initial gastrointestinal or respiratory illness – Physical examination may reveal dehydration, edema, petechiae, hepatosplenomegaly, and marked irritability
HUS • Investigations: – Blood film – broken and distorted red cells – Thrombocytopenia – Urine – microscopic hematuria, mild proteinuria – Serum urea and creatinine elevated
HUS • Treatment: – Is supportive – Proper nutriton – Plasmapheresis and infusion of FFP in some patients – Management of • • ARF HTN Dyselectrolytemia Correction of anemia
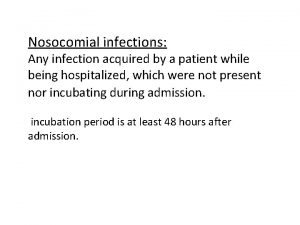
 ç
ç Uti symptoms men
Uti symptoms men Complicated urinary tract infection
Complicated urinary tract infection Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Nursing management for urinary tract infection
Nursing management for urinary tract infection Sunil paudel
Sunil paudel Conclusion of respiratory tract infection
Conclusion of respiratory tract infection Nursing management of reproductive tract infection
Nursing management of reproductive tract infection Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Tumor in the urinary tract
Tumor in the urinary tract Urinary tract obstruction
Urinary tract obstruction Urinary bladder
Urinary bladder Extrapyramidal vs pyramidal
Extrapyramidal vs pyramidal Dorsal reticulospinal tract
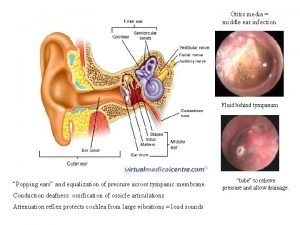
Dorsal reticulospinal tract Ear infection tympanic membrane
Ear infection tympanic membrane Infraorbital space infection
Infraorbital space infection Kidney infection
Kidney infection Active phagocytes that increase rapidly acute infection
Active phagocytes that increase rapidly acute infection Conclusion of infection
Conclusion of infection Why are viruses considered nonliving
Why are viruses considered nonliving Spirochete infection
Spirochete infection Infection control information
Infection control information Chain of infection
Chain of infection Wound infection continuum
Wound infection continuum Histoire
Histoire 15:4 observing standard precautions
15:4 observing standard precautions Thyroid eye disease
Thyroid eye disease Stages of infection
Stages of infection Streplococcus
Streplococcus Chapter 19 disease transmission and infection prevention
Chapter 19 disease transmission and infection prevention Conclusion of infection control
Conclusion of infection control History of dental radiology ppt
History of dental radiology ppt