Upper Respiratory Tract Infections OTITIS MEDIA Otitis media












- Slides: 31

Upper Respiratory Tract Infections
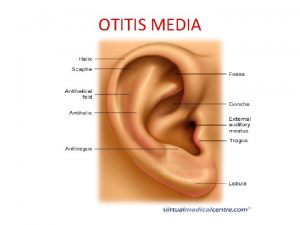
OTITIS MEDIA • Otitis media is an inflammation of the middle ear. • There are more than 709 million cases of otitis media worldwide each year; half of these cases occur in children under 5 years of age. • Otitis media is most common in infants and children. • The risk factors for amoxicillin resistant bacteria in acute otitis media include attendance at a child care center, recent receipt of antibiotic treatment (past 30 days), and age younger than 2 years.
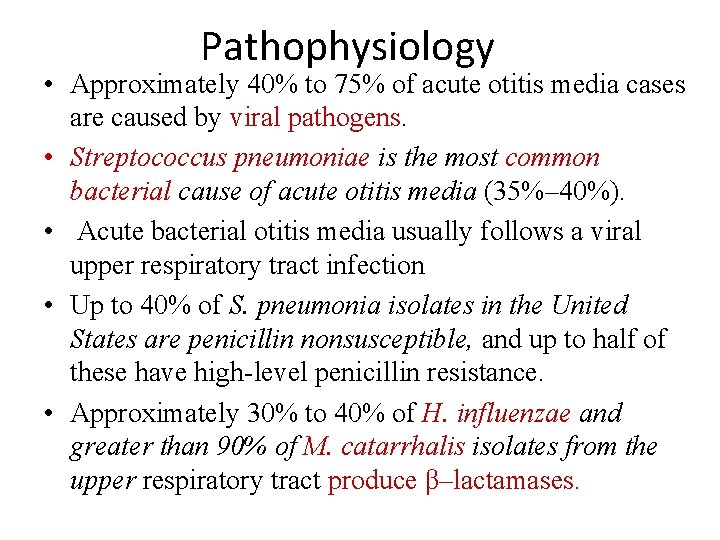
Pathophysiology • Approximately 40% to 75% of acute otitis media cases are caused by viral pathogens. • Streptococcus pneumoniae is the most common bacterial cause of acute otitis media (35%– 40%). • Acute bacterial otitis media usually follows a viral upper respiratory tract infection • Up to 40% of S. pneumonia isolates in the United States are penicillin nonsusceptible, and up to half of these have high-level penicillin resistance. • Approximately 30% to 40% of H. influenzae and greater than 90% of M. catarrhalis isolates from the upper respiratory tract produce β–lactamases.
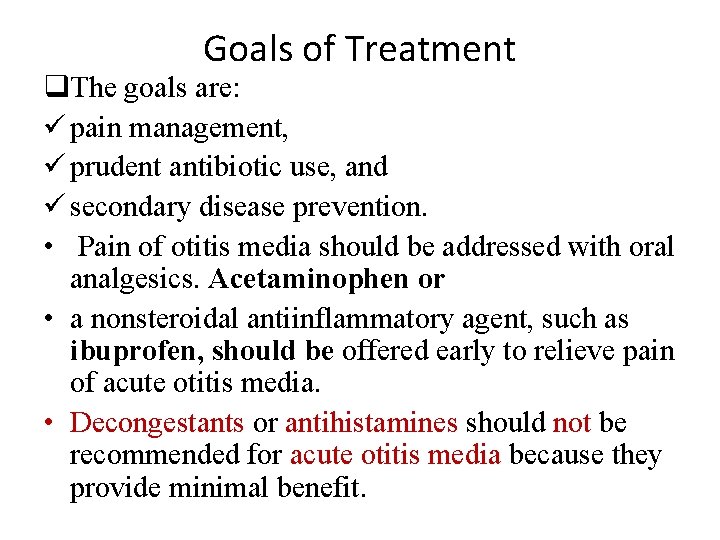
Goals of Treatment q. The goals are: ü pain management, ü prudent antibiotic use, and ü secondary disease prevention. • Pain of otitis media should be addressed with oral analgesics. Acetaminophen or • a nonsteroidal antiinflammatory agent, such as ibuprofen, should be offered early to relieve pain of acute otitis media. • Decongestants or antihistamines should not be recommended for acute otitis media because they provide minimal benefit.
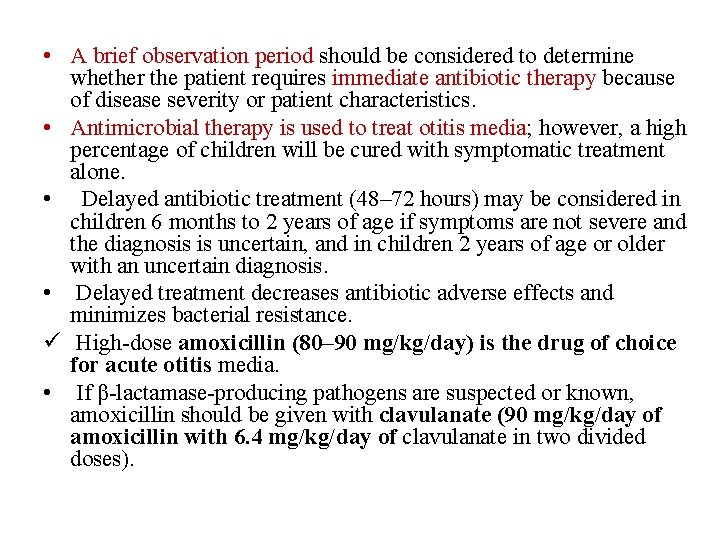
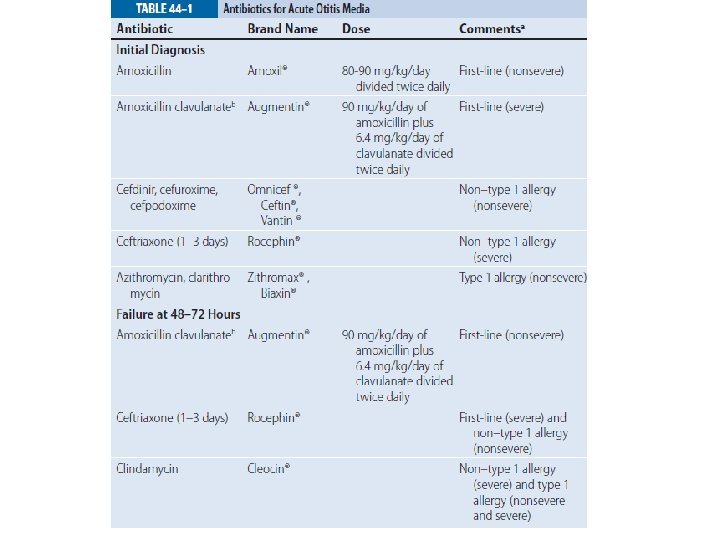
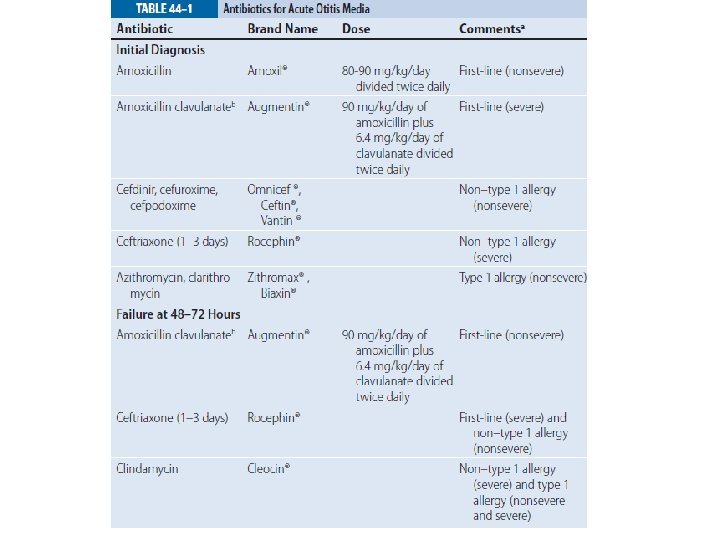
• A brief observation period should be considered to determine whether the patient requires immediate antibiotic therapy because of disease severity or patient characteristics. • Antimicrobial therapy is used to treat otitis media; however, a high percentage of children will be cured with symptomatic treatment alone. • Delayed antibiotic treatment (48– 72 hours) may be considered in children 6 months to 2 years of age if symptoms are not severe and the diagnosis is uncertain, and in children 2 years of age or older with an uncertain diagnosis. • Delayed treatment decreases antibiotic adverse effects and minimizes bacterial resistance. ü High-dose amoxicillin (80– 90 mg/kg/day) is the drug of choice for acute otitis media. • If β-lactamase-producing pathogens are suspected or known, amoxicillin should be given with clavulanate (90 mg/kg/day of amoxicillin with 6. 4 mg/kg/day of clavulanate in two divided doses).

PHARYNGITIS • Pharyngitis is an acute infection of the oropharynx or nasopharynx that results in 1% to 2% of all outpatient visits. • Although viral causes are most common, group A βhemolytic Streptococcus (GABHS), or Streptococcus pyogenes, is the primary bacterial cause. • Viruses (eg, rhinovirus, coronavirus, and adenovirus) cause most of the cases of acute pharyngitis. A bacterial etiology for acute pharyngitis is far less likely. • Of all of the bacterial causes, GABHS is the most common (15%– 30% of cases in pediatric patients and 5%– 15% in adults).
• Because pain is often the primary reason for visiting a physician, emphasis on analgesics such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) to aid in pain relief is strongly recommended. • Penicillin and amoxicillin are the treatments of choice. • Most cases of pharyngitis are self-limited; however, antimicrobial therapy will hasten resolution when given early to proven cases of GABHS. • Symptoms generally resolve by 3 or 4 days even without therapy.
ACUTE BACTERIAL RHINOSINUSITIS • Sinusitis is an inflammation and/or infection of the paranasal sinus mucosa. • The majority of these infections are viral in origin. • Acute bacterial sinusitis is most often caused by the same bacteria implicated in acute otitis media: S. pneumoniae and H. influenzae. • These organisms are responsible for ~50% to 70% of bacterial causes of acute sinusitis in both adults and children.
q. Goals of Treatment: ü Reduce signs and symptoms ü Limiting antimicrobial treatment to those who may benefit. ü Eradicating bacterial infection with appropriate antimicrobial therapy, ü Minimizing the duration of illness, ü Preventing complications, and ü Preventing progression from acute disease to chronic disease.
• Nasal decongestant sprays such as phenylephrine and oxymetazoline that reduce inflammation by vasoconstriction are often used in nonbacterial rhinosinusitis. • Use should be limited to the recommended duration of the product (no more than 3 days) to prevent rebound congestion. • Oral decongestants may also aid. • Irrigation of the nasal cavity with saline and steam inhalation may be used to increase mucosal moisture, and • mucolytics (eg, guaifenesin) may be used to decrease the viscosity of nasal secretions. • Antihistamines and oral decongestants should not be used for acute bacterial sinusitis in view of their anticholinergic effects that can dry mucosa and disturb clearance of mucosal secretions
• Amoxicillin is first-line treatment for acute bacterial sinusitis. • It is cost effective in acute uncomplicated disease, and • initial use of newer broad-spectrum agents is not justified.



Lower respiratory infections
BRONCHITIS • Acute Bronchitis: • Bronchitis refers to an inflammatory condition of the large elements of the tracheobronchial tree that is usually associated with a generalized respiratory infection. • The inflammatory process does not extend to include the alveoli. • The disease entity is frequently classified as either acute or chronic. • Acute bronchitis occurs in all ages, whereas chronic bronchitis primarily affects adults.
• Acute bronchitis most commonly occurs during the winter months. Cold, damp climates and/or the presence of high concentrations of irritating substances such as air pollution or cigarette smoke may precipitate attacks. • Respiratory viruses are by far the most common infectious agents associated with acute bronchitis. • The common cold viruses including rhinovirus and coronavirus and lower respiratory tract pathogens including influenza virus, adenovirus, and respiratory syncytial virus, account for the majority of cases. • Mycoplasma pneumoniae also appears to be a frequent cause of acute bronchitis. Other bacterial causes are Chlamydia pneumoniae and Bordetella pertussis.
• Infection of the trachea and bronchi causes hyperemic and edematous mucous membranes and an increase in bronchial secretions. • Destruction of respiratory epithelium can range from mild to extensive and may affect bronchial mucociliary function. • In addition, the increase in bronchial secretions, which can become thick and tenacious, further impairs mucociliary activity. • Recurrent acute respiratory infections may be associated with increased airway hyperreactivity and possibly the pathogenesis of chronic obstructive lung disease.
Clinical Presentation • Acute bronchitis usually begins as an upper respiratory infection. The patient typically has nonspecific complaints, such as malaise and headache, coryza, and sore throat. • Cough is the hallmark of acute bronchitis. It occurs early and will persist despite the resolution of nasal or nasopharyngeal complaints. • Frequently, the cough is initially nonproductive but progresses, yielding mucopurulent sputum.
• Goals of Therapy: Treatment ü The goal is to provide comfort to the patient and, in the unusually severe case, to treat associated dehydration and respiratory compromise. Ø The treatment of acute bronchitis is symptomatic and supportive in nature. ü Reassurance and antipyretics alone are often sufficient. ü Bed rest and mild analgesic antipyretic therapy are often helpful in relieving the associated lethargy, malaise, and fever. ü Patients should be encouraged to drink fluids to prevent dehydration and possibly decrease the viscosity of respiratory secretions. • Aspirin or acetaminophen (650 mg in adults or 10– 15 mg/kg per dose in children with a maximum daily adult dose of <4 g and 60 mg/kg for children) or ibuprofen.
• Mist therapy and/or the use of a vaporizer may further promote thinning and loosening of respiratory secretions. In otherwise healthy patients, no meaningful benefits have been described with the use of oral or aerosolized β 2 -receptor agonists and/or oral or aerosolized corticosteroids. • Persistent, mild cough, which may be bothersome, may be treated with dextromethorphan; more severe coughs may require intermittent codeine or other similar agents. • Routine use of antibiotics in the treatment of acute bronchitis is discouraged; however, in patients who exhibit persistent fever or respiratory symptomatology for more than 4 to 6 days, the possibility of a concurrent bacterial infection should be suspected. • When possible, antibiotic therapy is directed toward anticipated respiratory pathogen(s).
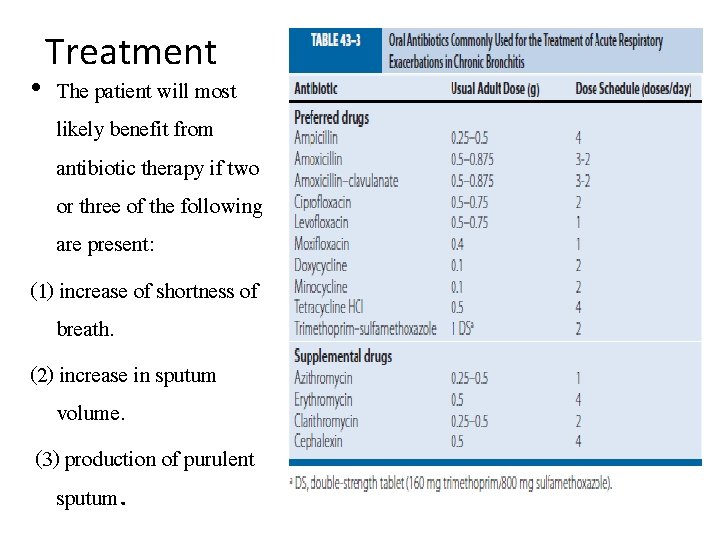
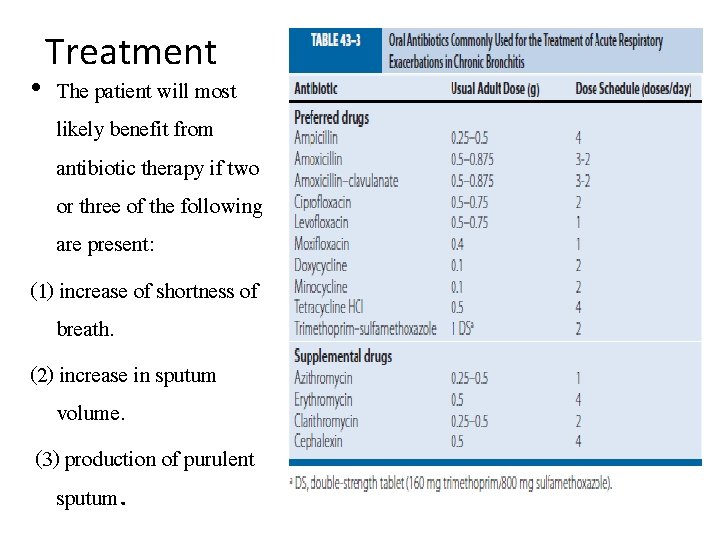
Treatment • The patient will most likely benefit from antibiotic therapy if two or three of the following are present: (1) increase of shortness of breath. (2) increase in sputum volume. (3) production of purulent sputum.

Pneumonia • Pneumonia is the most common infectious cause of death in the United States. • It occurs in persons of all ages, although the clinical manifestations are most severe in the very young, the elderly, and the chronically ill.

Pneumonia • Gram-Positive and Gram-Negative Bacterial Pneumonia • Anaerobic Pneumonia • Mycoplasma pneumoniae • Viral Pneumonia • Hospital-acquired Pneumonia
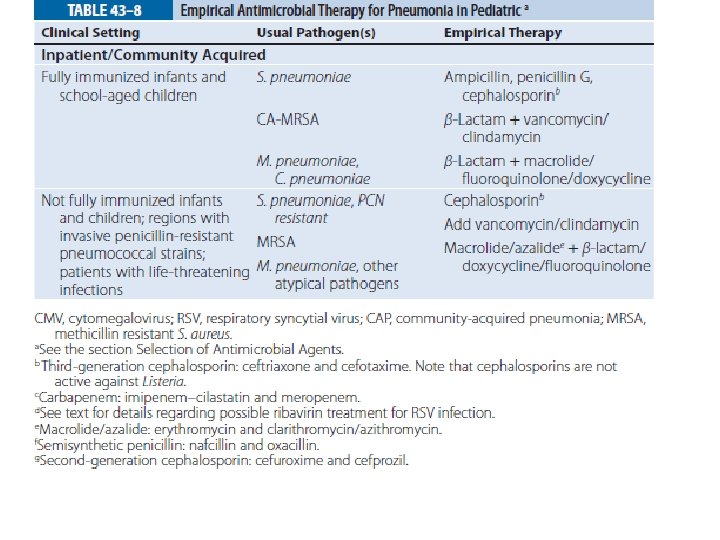
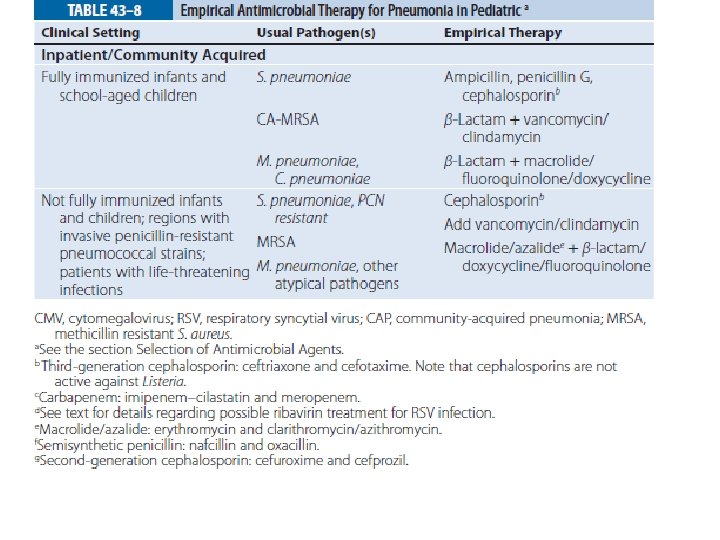
TREATMENT • Eradication of the offending organism and complete clinical cure are the primary objectives. • Associated morbidity should be minimized (eg, renal, pulmonary, or hepatic dysfunction). • The first priority on assessing the patient with pneumonia is to evaluate the adequacy of respiratory function and to determine whethere are signs of systemic illness, specifically dehydration, or sepsis with resulting circulatory collapse.





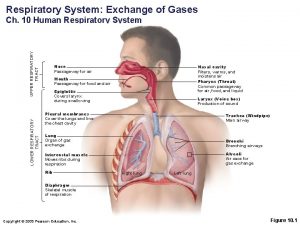
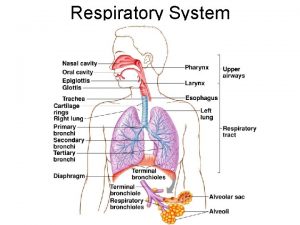
 Upper respiratory tract
Upper respiratory tract Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Upper respiratory tract anatomy
Upper respiratory tract anatomy Anatomy of upper respiratory tract
Anatomy of upper respiratory tract Hrpangina
Hrpangina Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Upper rti
Upper rti Upper and lower respiratory system
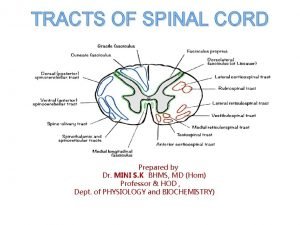
Upper and lower respiratory system Pyramidal vs extrapyramidal tract
Pyramidal vs extrapyramidal tract Dorsal reticulospinal tract
Dorsal reticulospinal tract Nose to lungs passage
Nose to lungs passage Classification of pneumonia
Classification of pneumonia Conclusion of respiratory tract infection
Conclusion of respiratory tract infection Normal flora of respiratory tract
Normal flora of respiratory tract Chassard lapine
Chassard lapine Conducting zone respiratory
Conducting zone respiratory Protective reflexes
Protective reflexes Tympanosclerosis
Tympanosclerosis Clasificación de la otitis media
Clasificación de la otitis media Otitis media ppt
Otitis media ppt Otitis media with effusion otoscopy
Otitis media with effusion otoscopy Serous vs mucoid
Serous vs mucoid Pediatr infect dis j
Pediatr infect dis j What does fluid in the ear look like
What does fluid in the ear look like Clasificación de la otitis media
Clasificación de la otitis media Nursing diagnosis for otitis media slideshare
Nursing diagnosis for otitis media slideshare Myringplasty
Myringplasty Otitis media ppt
Otitis media ppt Otitis media wiki
Otitis media wiki Ligamentos timpanomaleolares
Ligamentos timpanomaleolares Adhesive otitis media
Adhesive otitis media Classification of otitis media
Classification of otitis media