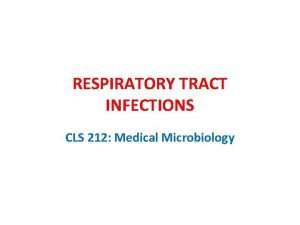
Upper and Lower Respiratory Infections URIs Upper Respiratory




- Slides: 81
Upper and Lower Respiratory Infections (URIs)
Upper Respiratory Infections (URIs) Objectives: 1. List 3 of the most common URIs in children. 2. Describe postoperative care of the child with a tonsillectomy. 3. Outline nursing care plan for a child with acute otitis media. 4. Outline nursing care plan for a child with acute otitis media.
Upper Respiratory Infections (URIs) Outlines: 1. The most common URIs in children. 2. Postoperative care of the child with a tonsillectomy. 3. Nursing care plan for a child with acute otitis media. 4. Nursing care plan for a child with acute otitis media.
Risk Factors n Age n Child’s health condition n Environmental factors e. g. pollution, overcrowding n Mother or care giver level of education n Culture n Nutritional status of the child 07/11/42 Dr. Afkar Ragab
Upper Respiratory Infections (URIs) Common upper of respiratory tract infections in children: q Tonsillitis. q Otitis media.
Tonsillitis The tonsils are masses of lymphoid tissue located in the pharyngeal cavity. Functions of tonsils: ü To filter and protect the respiratory and alimentary tracts for invasion by pathogenic organisms. ü They also may have a role in antibody formation.
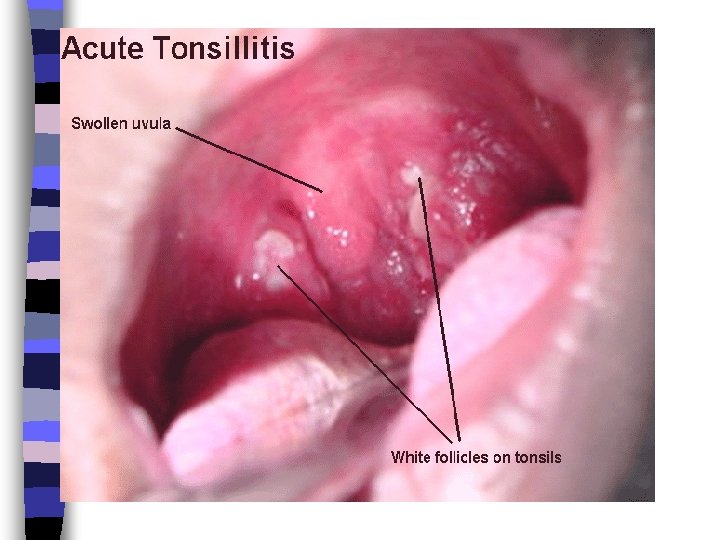
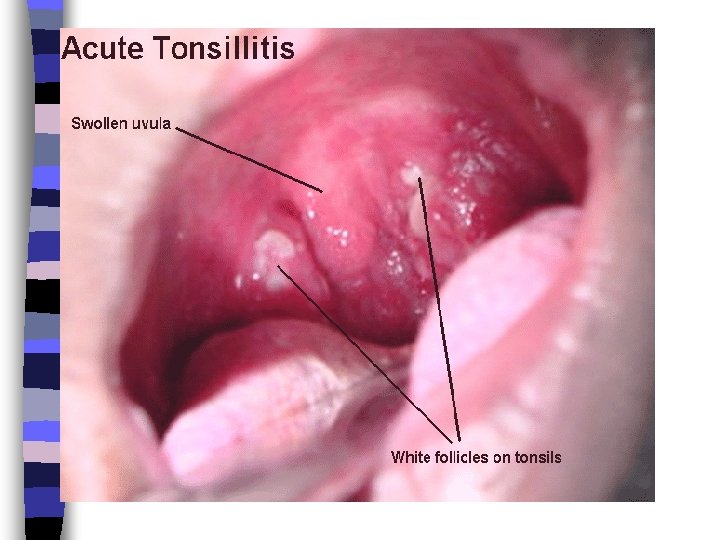
Tonsillitis is a swelling of the tonsils, which areas of lymphoid tissue on either side of the throat. Tonsils can become swollen when they are infected by bacteria or a virus. This is a common occurrence in children.

Symptoms of tonsillitis may include: n Ø Ø Ø Ø Sore throat. Difficult swallowing Fever. Headache. White patches in the throat or tonsils. Red, swollen tonsils. Pain when swallowing. Vomiting. Sore glands in the throat or jaw.
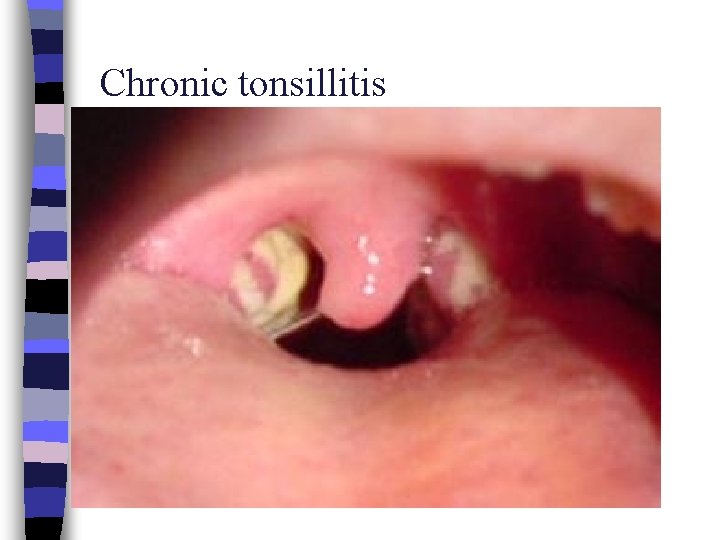
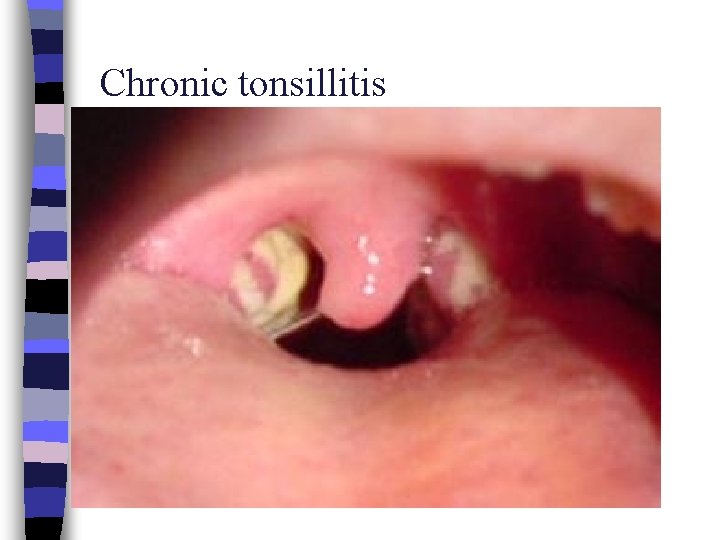
Chronic tonsillitis
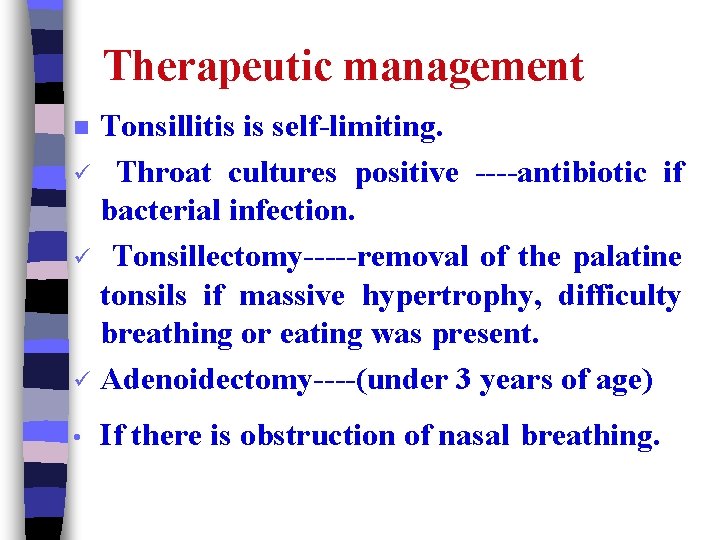
Therapeutic management Tonsillitis is self-limiting. ü Throat cultures positive ----antibiotic if bacterial infection. ü Tonsillectomy-----removal of the palatine tonsils if massive hypertrophy, difficulty breathing or eating was present. ü Adenoidectomy----(under 3 years of age) n • If there is obstruction of nasal breathing.
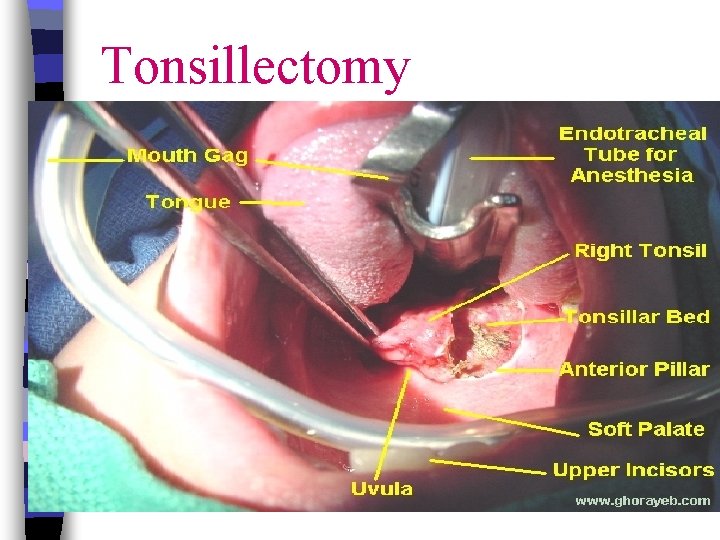
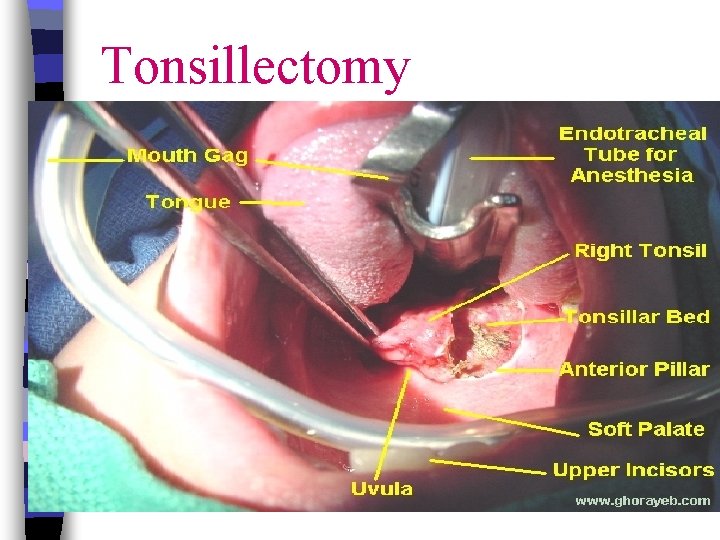
Tonsillectomy
Contraindications to either tonsillectomy or adenoidectomy § § § Cleft palate. Acute infections at the time of surgery. Local inflamed tissues increase the risk of bleeding. Uncontrolled systemic disease.
Nursing diagnoses with a tonsillectomy: § Impaired swallowing related to inflammation and discomfort. § § Pain related to surgery. Altered oral mucous membranes related to operative site. § High risk for injury.
Nursing diagnoses with a tonsillectomy: Anxiety/fear related to unfamiliar event, discomfort. §Altered family processes related to hospitalization of child. Ineffective airway clearance related to discomfort.
Nursing considerations with tonsillitis: ü Providing comfort. ü Soft liquid diet is generally preferred. ü cool mist. ü Warm salt gargles, throat lozenges.
Analgesic/antipyretic drugs as acetaminophen and codeine are useful to promote comfort (given rectally or IV. ). ü If surgery is needed: Care after tonsillectomy: üChildren are placed on the abdomen or side to facilitate drainage of secretions.
If the child need suctioning must be performed carefully to avoid trauma to the oropharynx. * Alert child the bed rest for the remainder of day. * Discourage child from coughing frequently and blowing their nose, clear their throat and activities that may aggravate the operative site.
üThe throat is very sore ---- Ice collar may provide relief. üPain medication for at least the first 24 hours. ü Cool water, crushed ice, fluids, diluted fruit juices is given first. * Avoid red or brown color fluids. * Citrus fluids or juices may cause discomfort.
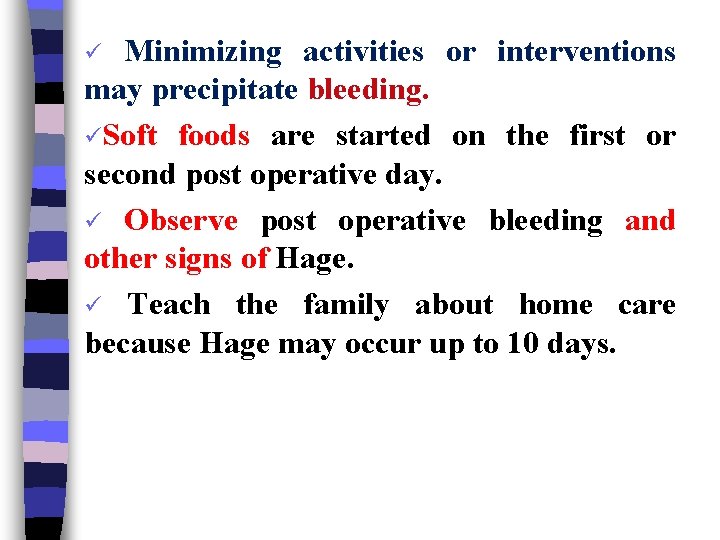
Minimizing activities or interventions may precipitate bleeding. üSoft foods are started on the first or second post operative day. ü Observe post operative bleeding and other signs of Hage. ü Teach the family about home care because Hage may occur up to 10 days. ü
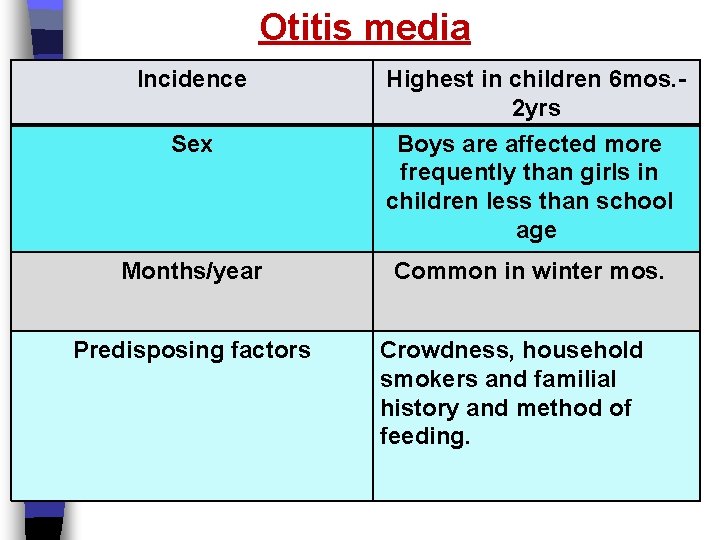
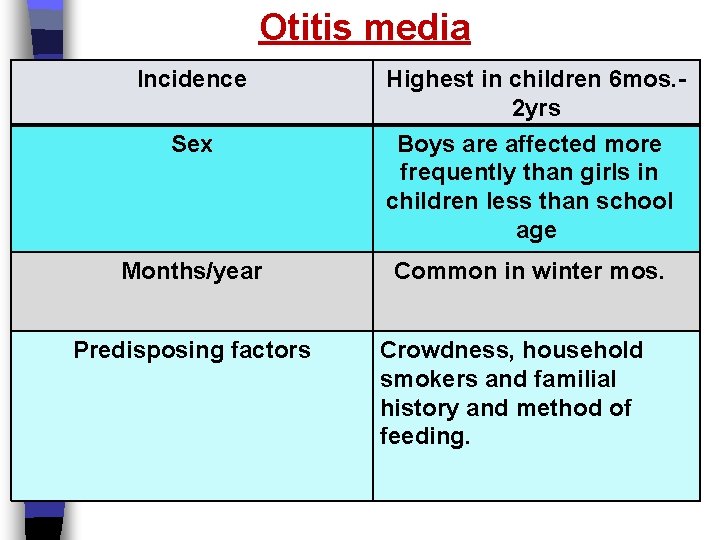
Otitis media Incidence Sex Highest in children 6 mos. 2 yrs Boys are affected more frequently than girls in children less than school age Months/year Common in winter mos. Predisposing factors Crowdness, household smokers and familial history and method of feeding.
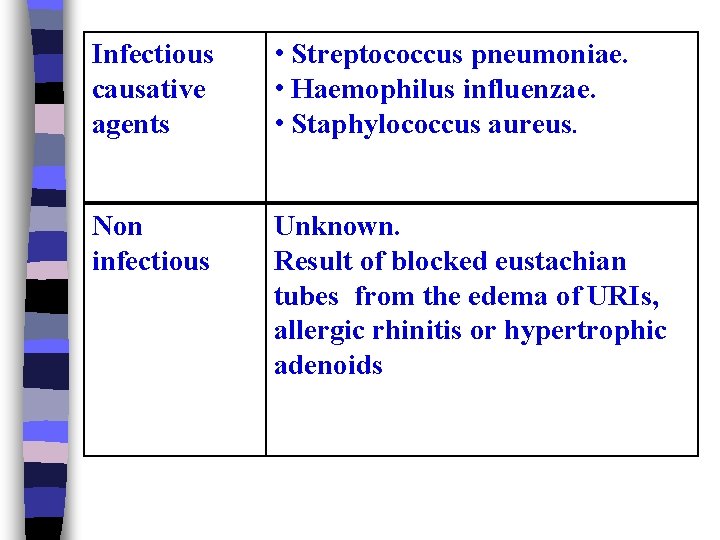
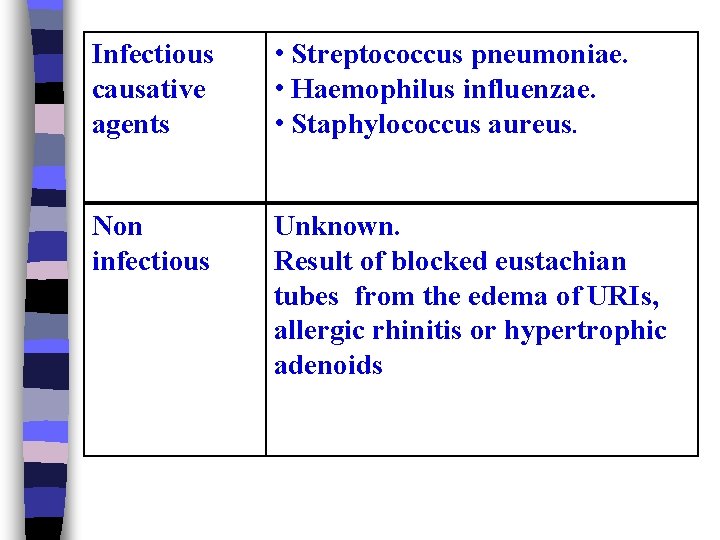
Infectious causative agents • Streptococcus pneumoniae. • Haemophilus influenzae. • Staphylococcus aureus. Non infectious Unknown. Result of blocked eustachian tubes from the edema of URIs, allergic rhinitis or hypertrophic adenoids
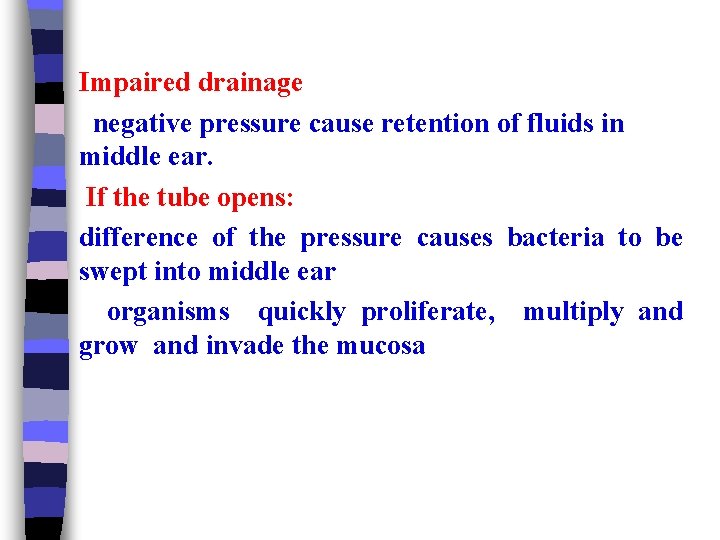
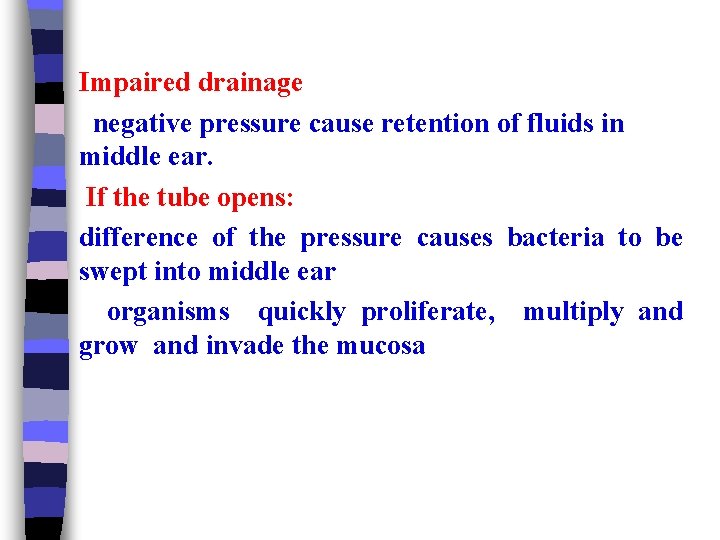
Impaired drainage negative pressure cause retention of fluids in middle ear. If the tube opens: difference of the pressure causes bacteria to be swept into middle ear organisms quickly proliferate, multiply and grow and invade the mucosa
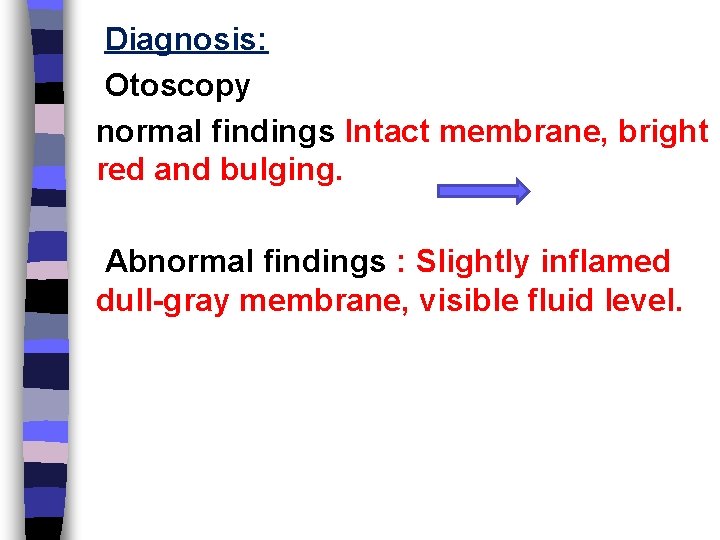
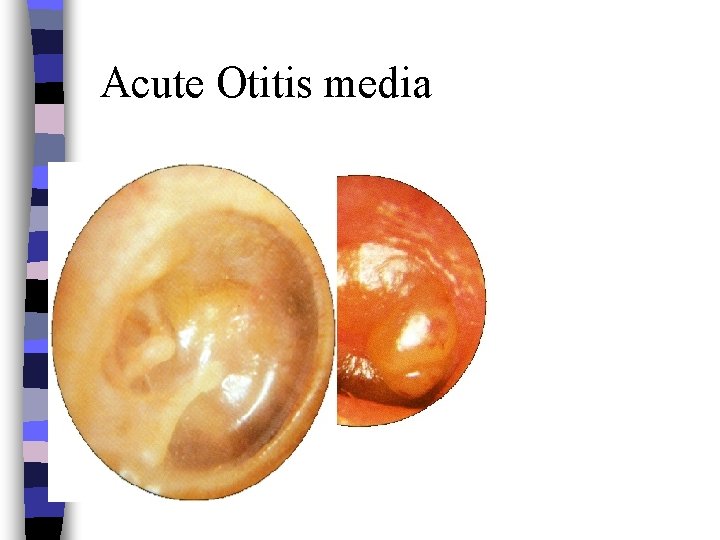
Diagnosis: Otoscopy normal findings Intact membrane, bright red and bulging. Abnormal findings : Slightly inflamed dull-gray membrane, visible fluid level.
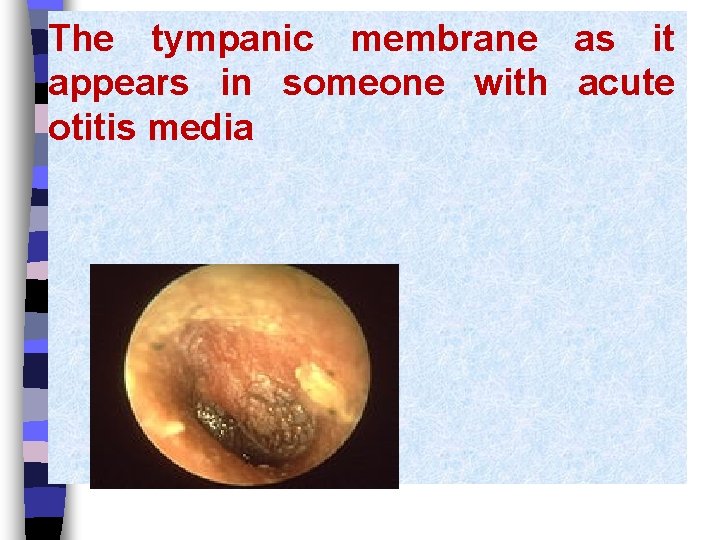
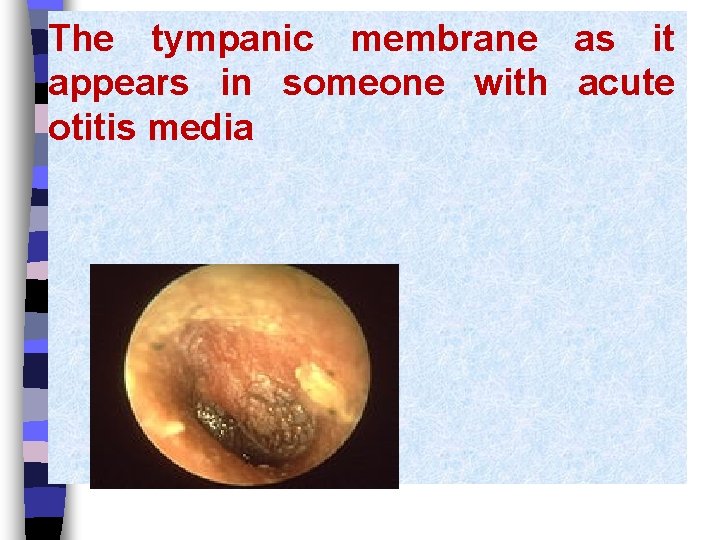
The tympanic membrane as it appears in someone with acute otitis media
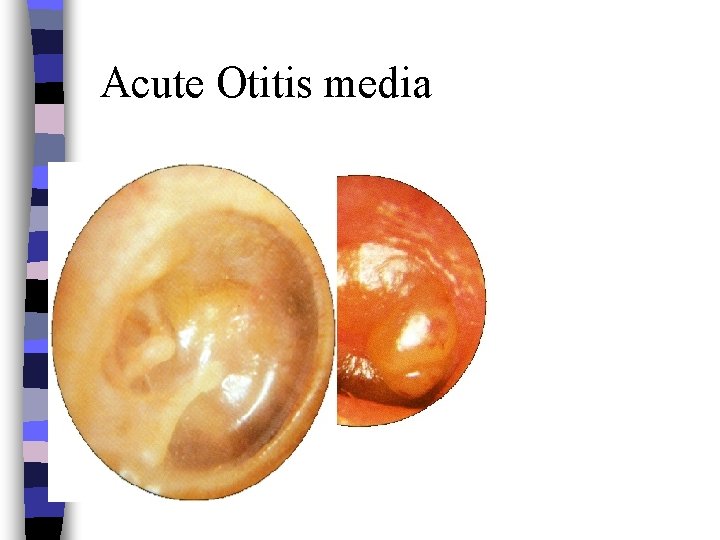
Acute Otitis media

Manifestations of otitis media: o. Follows o. Earache an upper respiratory infection (otalgia), pain that is more severe and continuous. o. Fever o of 39 °C. Purulent otorrhea. o. Perforation o of the ear drum. Infection of the mastoid space.
Infant or very young child: n Crying. n Fussy, restless, irritable. n Tendency to rub, hold, or pull affected ear n Rolls head side to side. n Difficulty comforting child. n Loss of appetite.
Older child: Ø Crying and/or verbalizes feelings of discomfort. Ø Irritability. Ø Lethargy. Ø Loss of appetite.
Chronic Otitis Media: q Hearing loss. q Difficulty communicating. q Feeling of fullness, tinnitus, vertigo (dizziness) may be present
Therapeutic management: Ø Administration of antibiotics child must improved within 48 -72 h. Ø Myringotomy (surgical incision of the eardrum) to relieve symptoms in some children. Ø After antibiotics child should be assessed for effectiveness of TT and to identify potential complications: -Effusion or hearing impairment.
Analgesic/ antipyretic are used to alleviate discomfort and reduce an elevated temperature. Tympanostomy tubes (pressure equalizer tubes or facilitate continued drainage of fluid and allow ventilation of the middle ear).

Trans-tympanic drainage
Nursing interventions: ü Analgesics/ antipyretics. ü The application of heat with a heating pad on low setting -----may reduce the discomfort, local heat over the ear with child lying on the affected side. ü This position facilitates drainage. ü An ice bag placed over the affected ear may also be beneficial ( reduces edema and pressure).
External ear canal may be cleaned with sterile cotton swabs soaked in hydrogen peroxide. ü üThe skin around the ear become excoriated from the exudates------this is prevented by frequent cleansing and application of zinc oxide.
Teach the parent for temporary hearing loss. ü Complete use of antibiotics. ü Avoid supine position during infant feeding. ü
LARYNGOTRACHOBRONCHITIS CROUP SYNDROME n . LTB is severe inflammation and partial obstruction of upper air way. It is also most often self-limited, but it occasionally is severe and, rarely, fatal. A barking cough, stridor, and fever are characteristic, and it is the most common cause of stridor in children
Etiology: • LTB usually results from viral infection; e. g. parainfluenza viruses, adenoviruses, respiratory syncytial virus, and measles viruses. • It also may be of bacterial origin (diphtheria or pertussis).
n Incidence: LTB affects boys more than girls, typically between ages 6 months and 3 years. Incidence peaks in the winter months.
Assessment Finding Health history and physical examination typically reveal one or more of the following. o Upper respiratory infection. o Substantial and suprasternal retractions. o Barking cough, hoarseness. o Pallor and cyanosis. o Irritability and restlessness. o Low-grade fever. o Crackles
Nursing Diagnosis n Ineffective airway clearance. n Anxiety and ineffective breathing pattern. n Altered family process. n High risk for fluid volume deficit. n High risk for injury. n Parents / mother knowledge deficit.
Planning and Implementation Assessment → assess obstruction by evaluating for air way respiratory status; color, respiratory effort, evidence of fatigue, and vital signs, keep emergency equipment at the bed side. Administer oxygen therapy, as ordered, to alleviate hypoxia. Administer IV fluids, as ordered, to ensure adequate hydration.
Planning and Implementation Administer prescribed medications which may include : Racemic epinephrine via neubilizer - Antibiotics if it is bacterial. - Corticosteroids to reduce inflammation. Maintain quiet environment and promote rest. Support parents by answering questions and explaining all treatments and procedures.
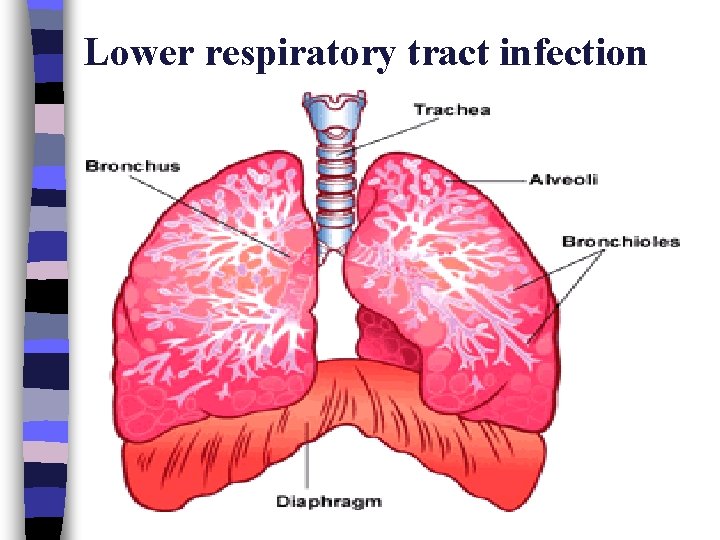
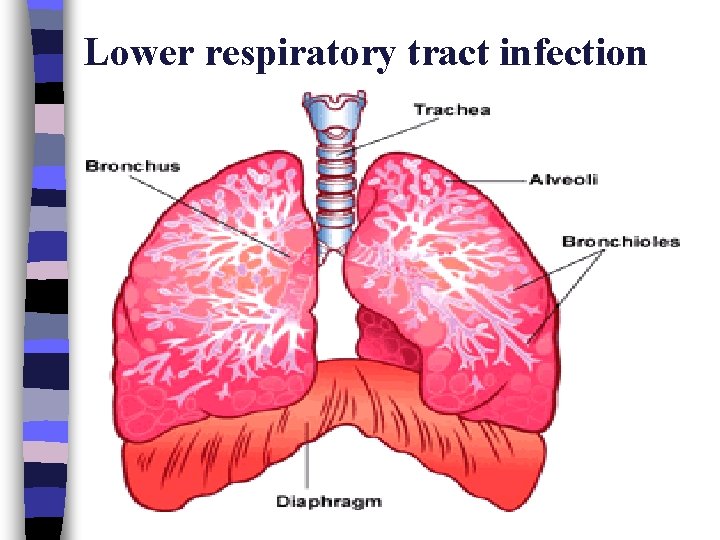
Lower respiratory tract infection
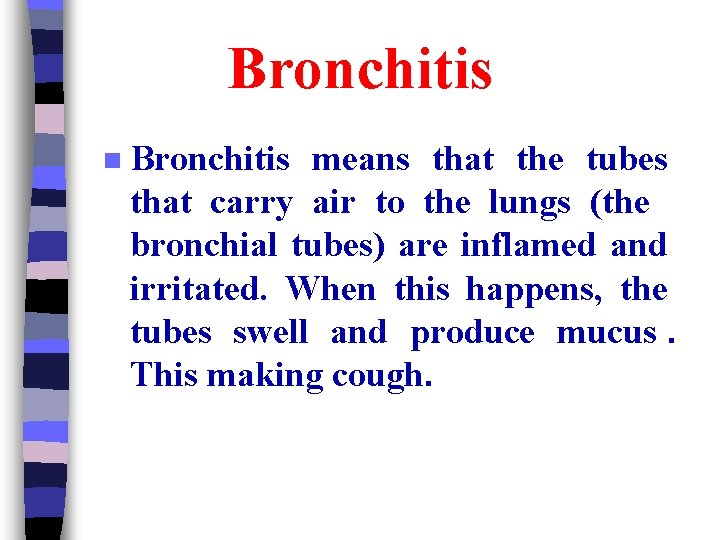
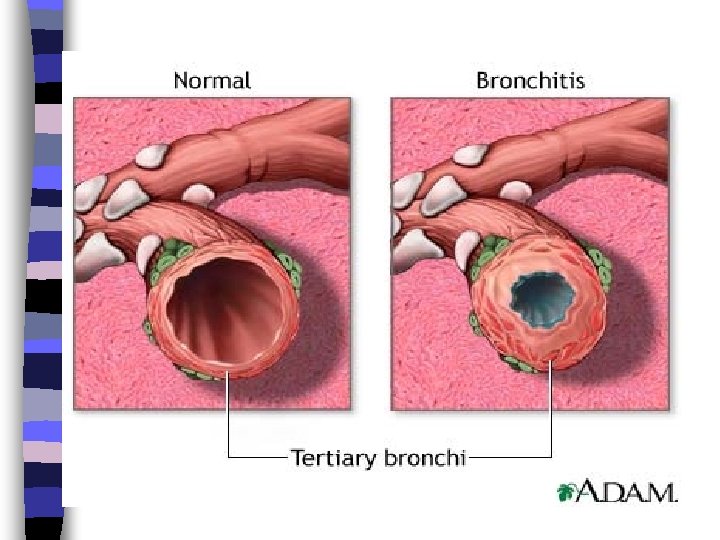
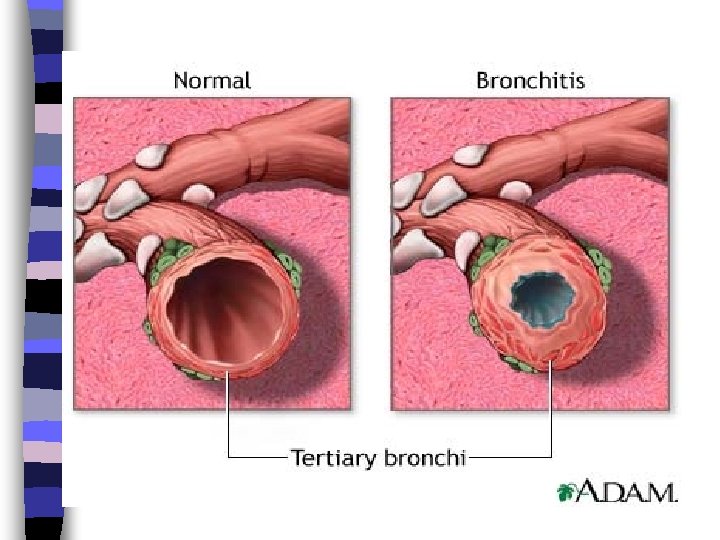
Bronchitis n Bronchitis means that the tubes that carry air to the lungs (the bronchial tubes) are inflamed and irritated. When this happens, the tubes swell and produce mucus. This making cough.
Bronchitis
Causes of Acute Bronchitis n virus. bronchitis after having an upper respiratory tract infection n bacteria In rare cases n breathing in things that irritate the bronchial tubes, such as smoke. n inhales food or vomit into the lungs.
Symptoms n. A cough, which is the main symptom of acute bronchitis. It may be dry at first (does not produce mucus (and after a few days may bring up mucus from the lungs (productive cough). The mucus may be clear, yellow, or green. Sometimes, small streaks of blood may be present.
n. A general feeling of tiredness. A sensation of tightness, burning, or dull pain in the chest under the breastbone that usually is worse when breathing deeply or coughing. n wheezing (when breathing, especially during physical exertion. n mild fever, usually less than (38. 3°C). n Hoarseness. n
Management n Drink more fluids. Water helps loosen mucus and soothe an irritated throat n Elevate head with extra pillows at night to ease a dry cough n Relieving a cough n Getting enough rest n Breathing moist air from a humidifier
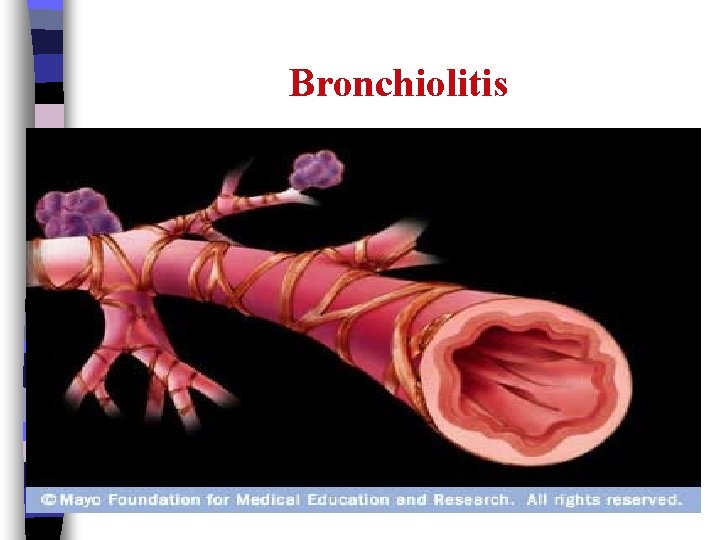
Bronchiolitis n A common infection of the lungs' airways, often caused by a virus. It most frequently occurs in infants, commonly between 3 and 6 months of age. Typically, Bronchiolitis occurs during the fall and winter
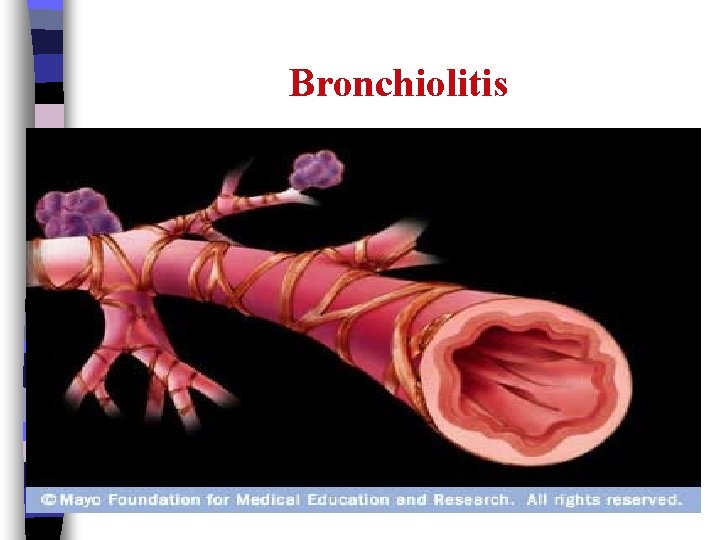
Bronchiolitis n
Causes n The respiratory syncytial virus (RSV), a common virus, causes most childhood Bronchiolitis cases
Symptoms n Runny nose n Stuffy nose n Slight fever (may or may not occur ( n After this, there may be two or three days of : n Wheezing — breathing seems more difficult or noisy when breathing out n Rapid or difficult breathing n Rapid heartbeat
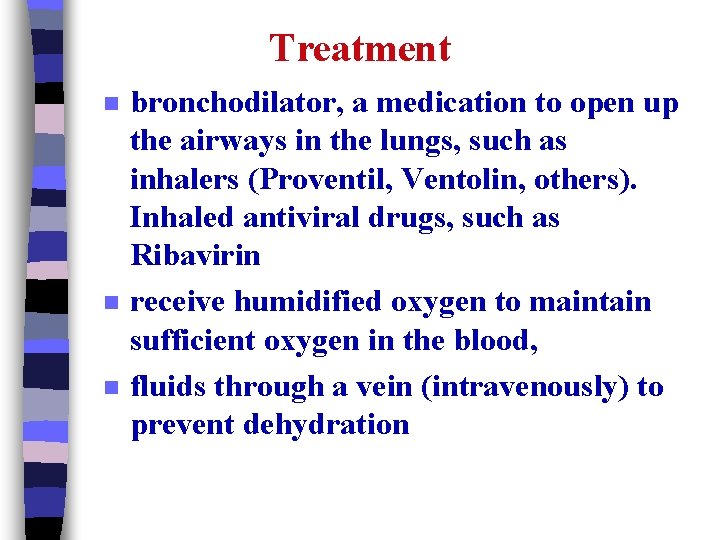
Treatment n n n bronchodilator, a medication to open up the airways in the lungs, such as inhalers (Proventil, Ventolin, others). Inhaled antiviral drugs, such as Ribavirin receive humidified oxygen to maintain sufficient oxygen in the blood, fluids through a vein (intravenously) to prevent dehydration
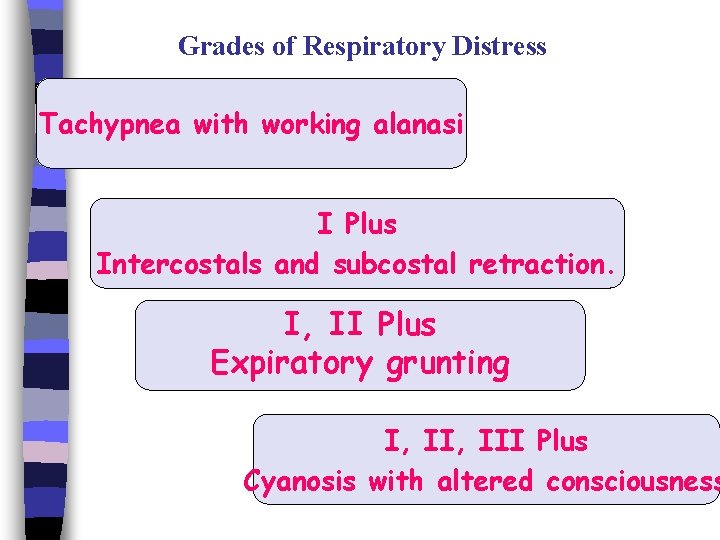
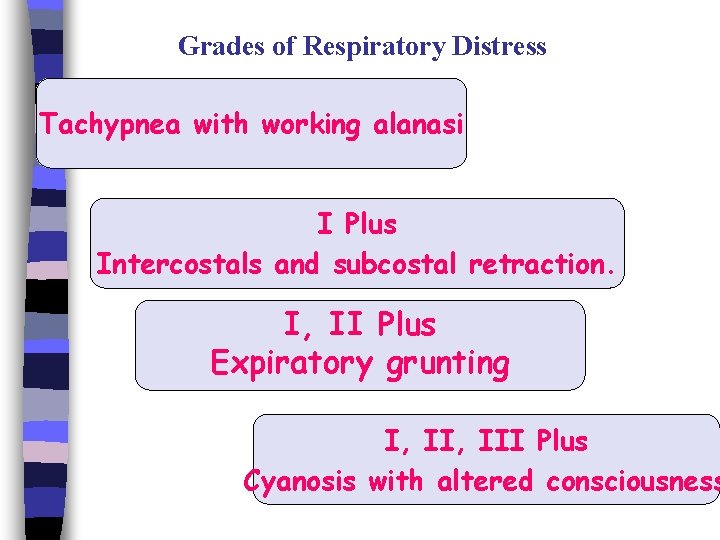
Grades of Respiratory Distress Tachypnea with working alanasi I Plus Intercostals and subcostal retraction. I, II Plus Expiratory grunting I, III Plus Cyanosis with altered consciousness
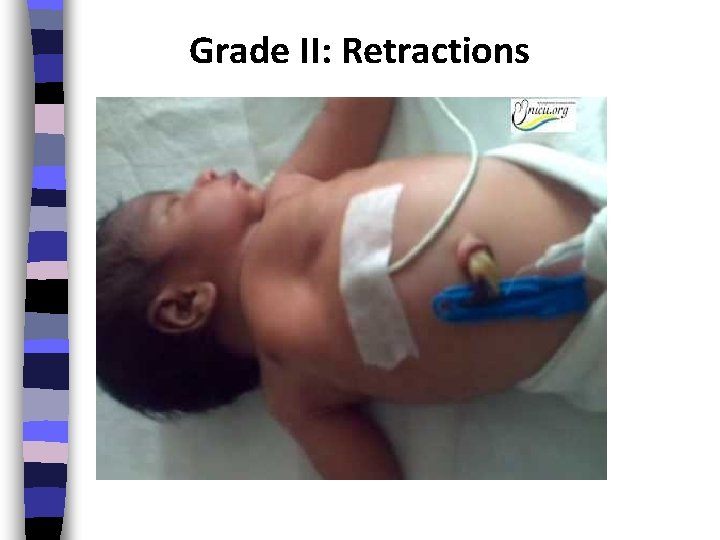
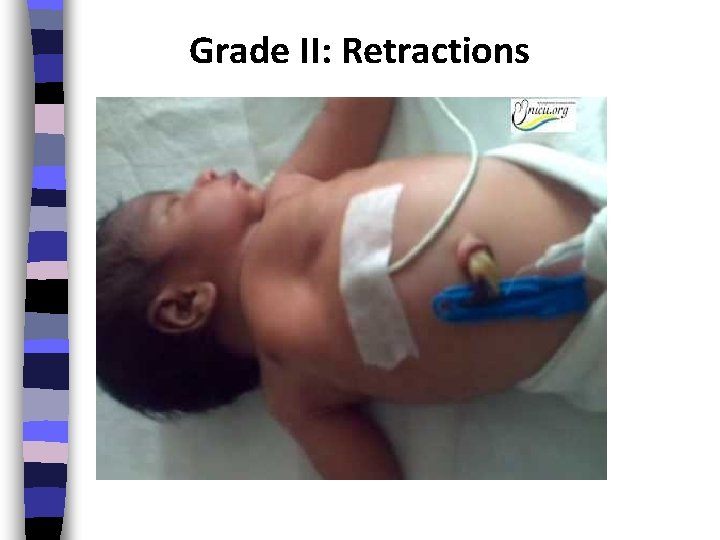
Grade II: Retractions
Pneumonia n Def : n Pneumonia is an acute inflammation of the lung parenchyma ( bronchioles, alveolar ducts and alveoli that impairs gas exchange n Occurs at a rate of 2 to 4 children in 100 and is most commonly seen during the late winter and early spring.

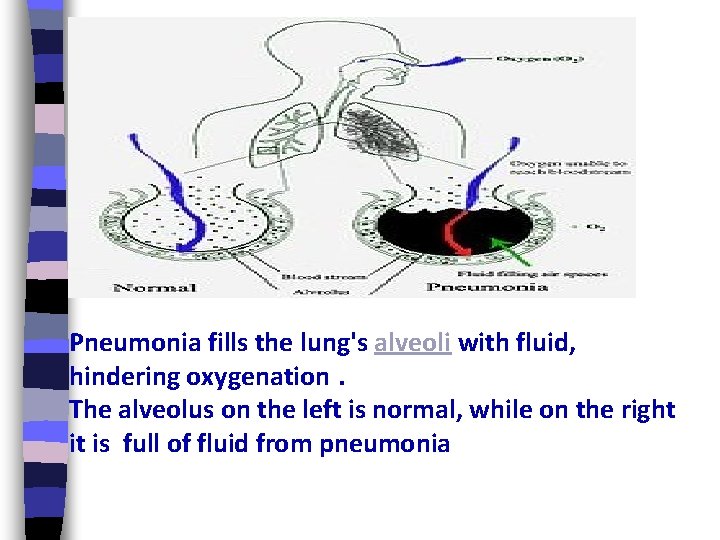
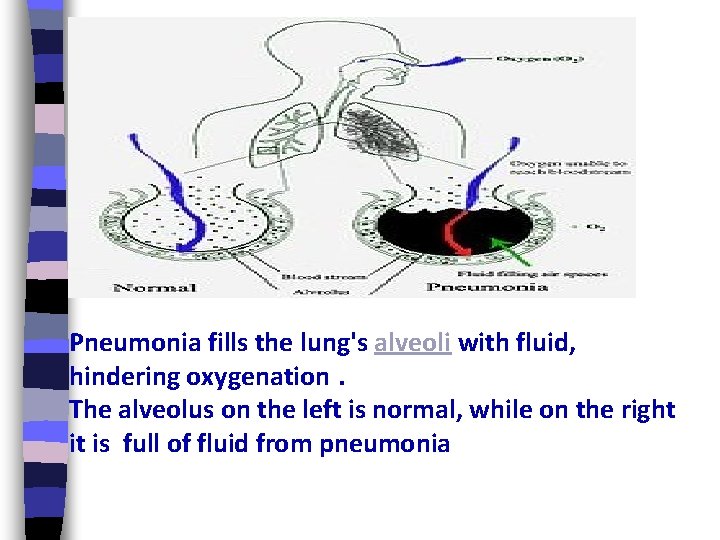
Pneumonia fills the lung's alveoli with fluid, hindering oxygenation. The alveolus on the left is normal, while on the right it is full of fluid from pneumonia
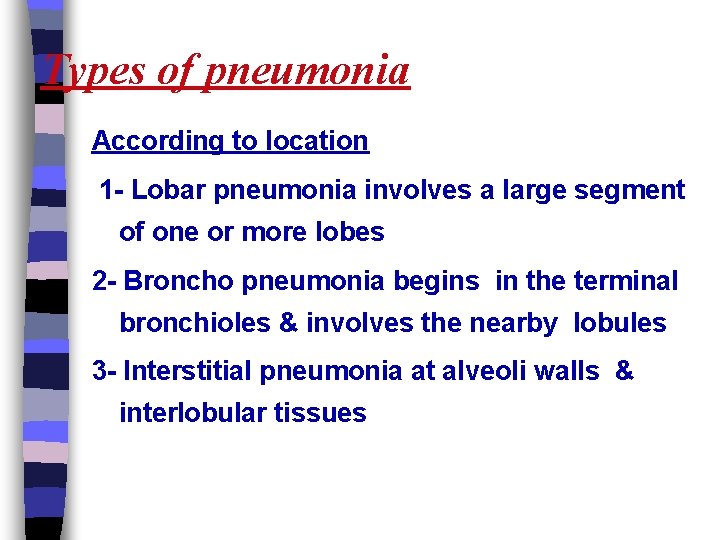
Types of pneumonia According to location 1 - Lobar pneumonia involves a large segment of one or more lobes 2 - Broncho pneumonia begins in the terminal bronchioles & involves the nearby lobules 3 - Interstitial pneumonia at alveoli walls & interlobular tissues
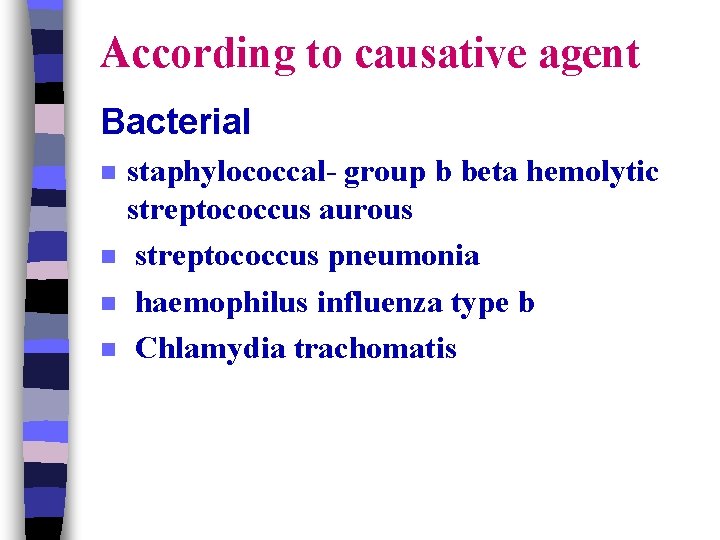
According to causative agent Bacterial n n staphylococcal- group b beta hemolytic streptococcus aurous streptococcus pneumonia haemophilus influenza type b Chlamydia trachomatis
Viral RSV n Para influenza virus n Adenoviruses Fungal Other agents (aspiration or ingestion of chemical agents ) n 07/11/42 Dr. Afkar Ragab
Causes of hospitalization in infants with pneumonia: 1 - Respiratory distress is severe 2 - Supplemental oxygen is needed 3 - Child is unable to tolerate oral fluids or medication because of respiratory distress or vomiting 4 - The infants are younger than 2 months of age. 5 - Underlying disease is present (e. g. Cardiac disease, sickle cell disease) 6 - The parents or care takers are unable to care for the child.
Symptoms n n n n n Cough, often producing mucus) sputum) from the lungs. may be rusty or green or tinged with blood. Fever Shaking, "teeth-chattering" chills (one time only or many times. ( Fast, often shallow, breathing and the feeling of being short of breath. Chest wall pain that is often made worse by coughing or breathing in. Fast heartbeat. Feeling very tired (fatigue) or feeling very weak (malaise. ( Nausea and vomiting. Diarrhea.
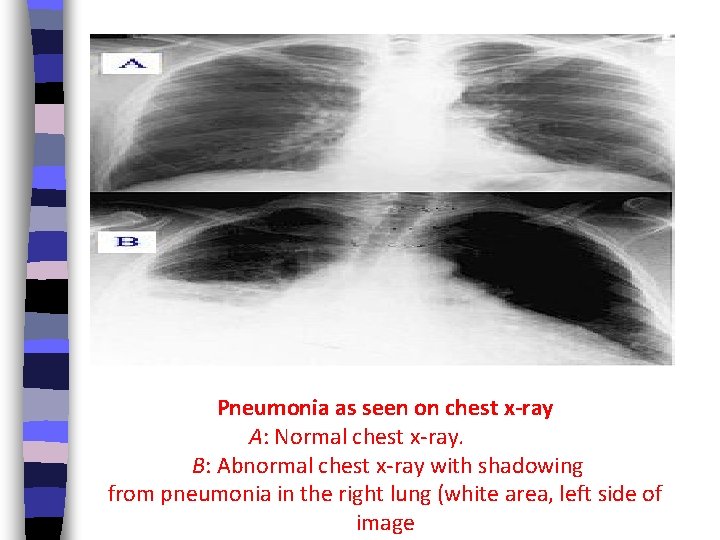
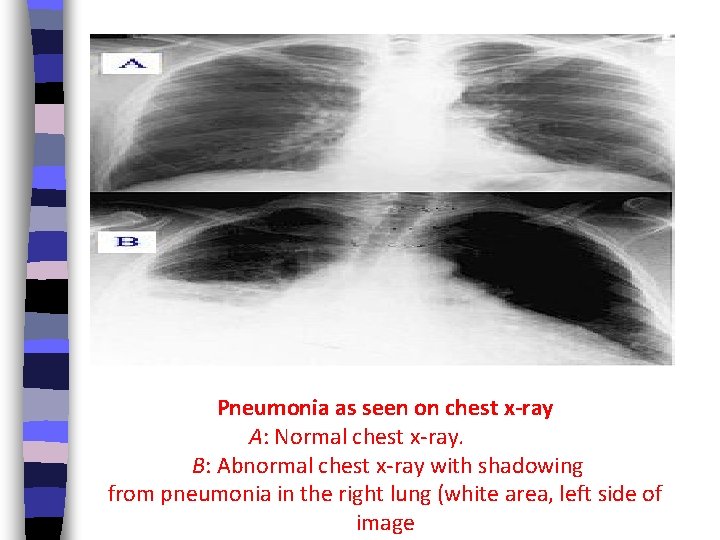
Pneumonia as seen on chest x-ray A: Normal chest x-ray. B: Abnormal chest x-ray with shadowing from pneumonia in the right lung (white area, left side of image
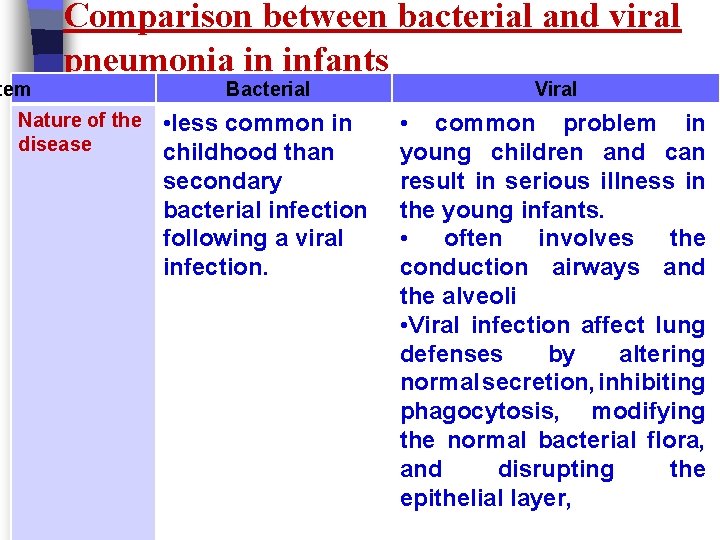
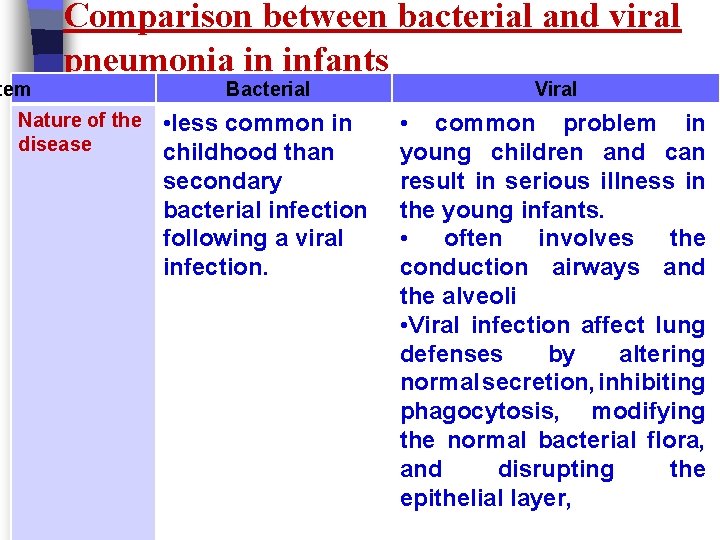
tem Comparison between bacterial and viral pneumonia in infants Nature of the disease Bacterial Viral • less common in childhood than secondary bacterial infection following a viral infection. • common problem in young children and can result in serious illness in the young infants. • often involves the conduction airways and the alveoli • Viral infection affect lung defenses by altering normal secretion, inhibiting phagocytosis, modifying the normal bacterial flora, and disrupting the epithelial layer,
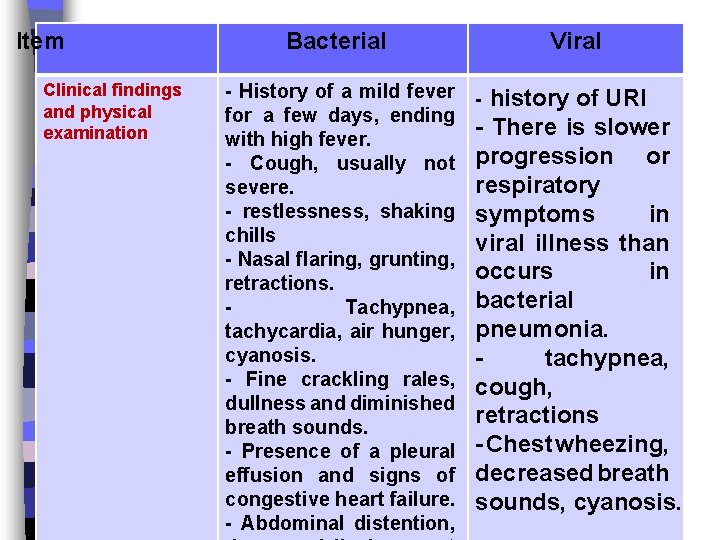
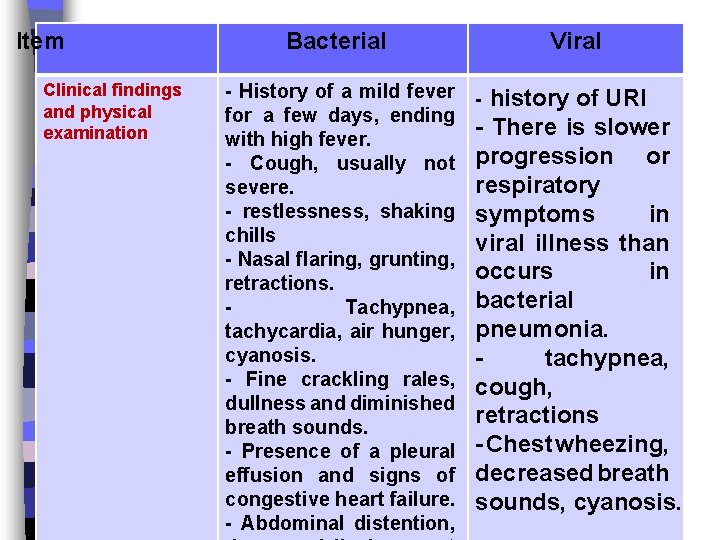
Item Clinical findings and physical examination Bacterial Viral - History of a mild fever - history of URI for a few days, ending - There is slower with high fever. or - Cough, usually not progression respiratory severe. - restlessness, shaking symptoms in chills viral illness than - Nasal flaring, grunting, occurs in retractions. Tachypnea, bacterial tachycardia, air hunger, pneumonia. cyanosis. tachypnea, - Fine crackling rales, cough, dullness and diminished retractions breath sounds. - Presence of a pleural - Chest wheezing, effusion and signs of decreased breath congestive heart failure. sounds, cyanosis. - Abdominal distention,
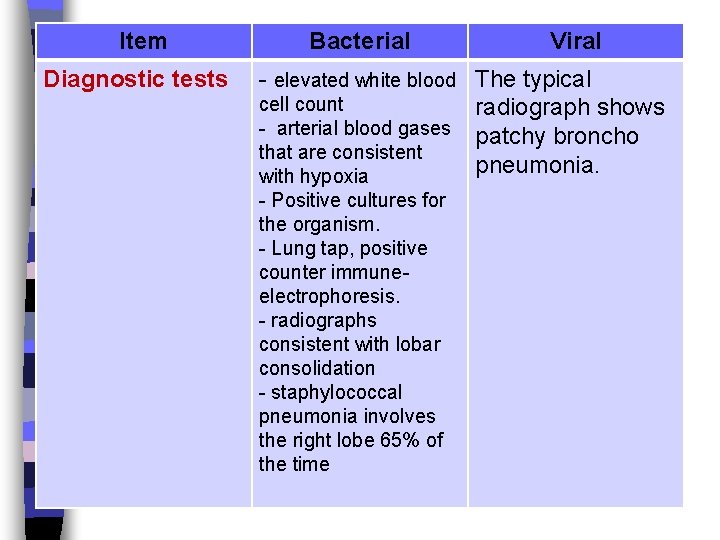
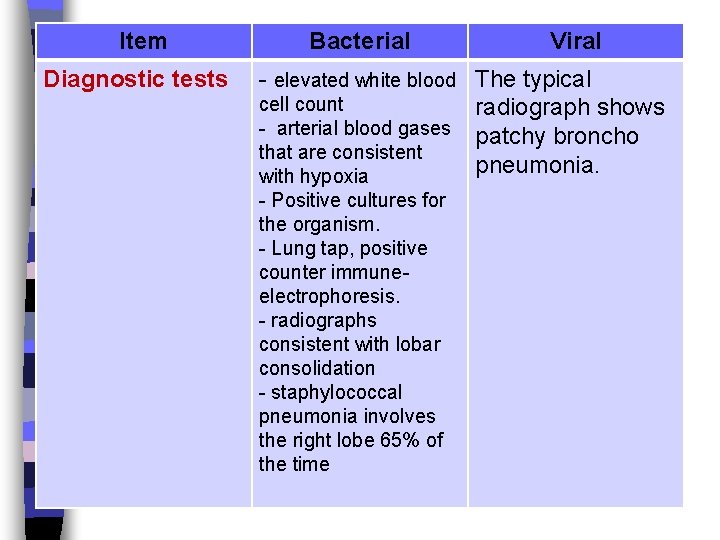
Item Diagnostic tests Bacterial Viral - elevated white blood The typical cell count radiograph shows - arterial blood gases patchy broncho that are consistent pneumonia. with hypoxia - Positive cultures for the organism. - Lung tap, positive counter immuneelectrophoresis. - radiographs consistent with lobar consolidation - staphylococcal pneumonia involves the right lobe 65% of the time
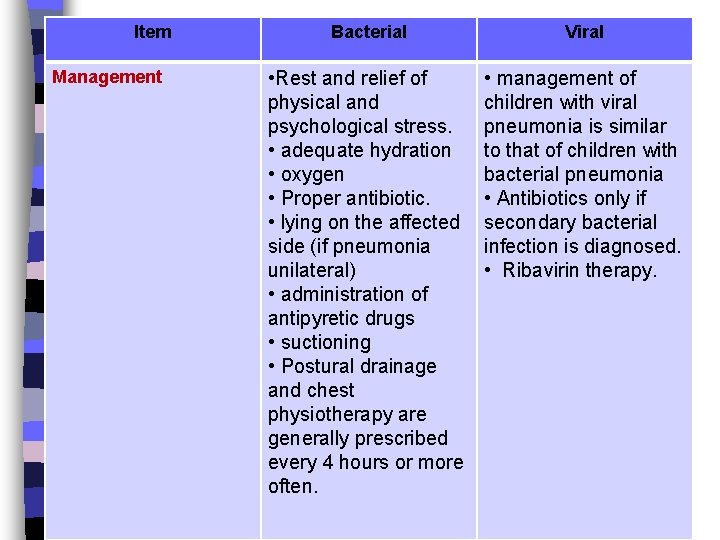
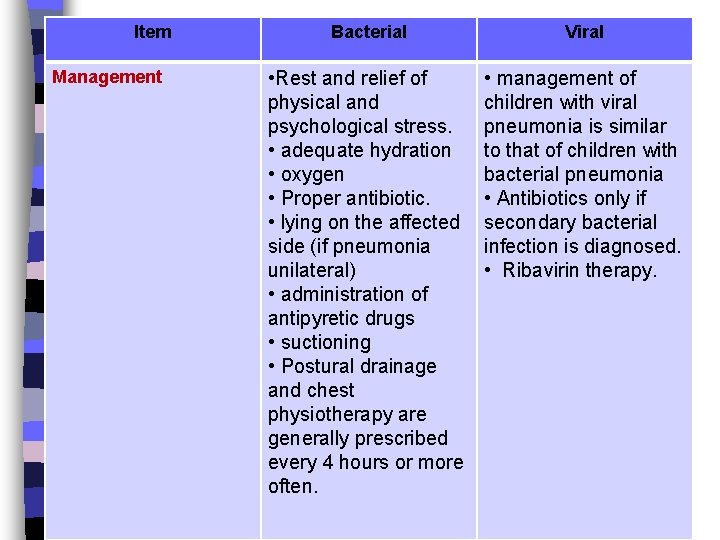
Item Management Bacterial Viral • Rest and relief of physical and psychological stress. • adequate hydration • oxygen • Proper antibiotic. • lying on the affected side (if pneumonia unilateral) • administration of antipyretic drugs • suctioning • Postural drainage and chest physiotherapy are generally prescribed every 4 hours or more often. • management of children with viral pneumonia is similar to that of children with bacterial pneumonia • Antibiotics only if secondary bacterial infection is diagnosed. • Ribavirin therapy.
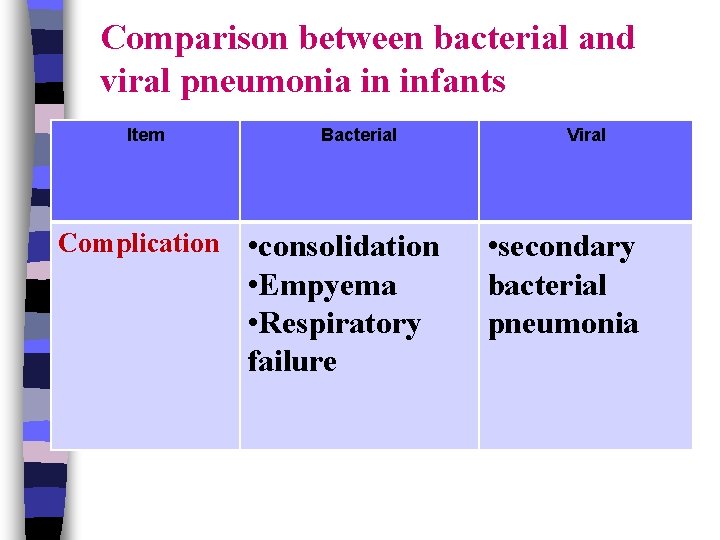
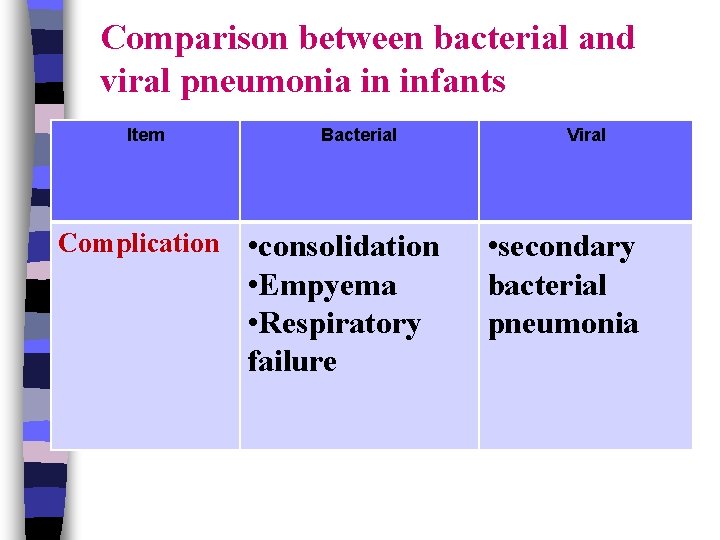
Comparison between bacterial and viral pneumonia in infants Item Bacterial Complication • consolidation • Empyema • Respiratory failure Viral • secondary bacterial pneumonia
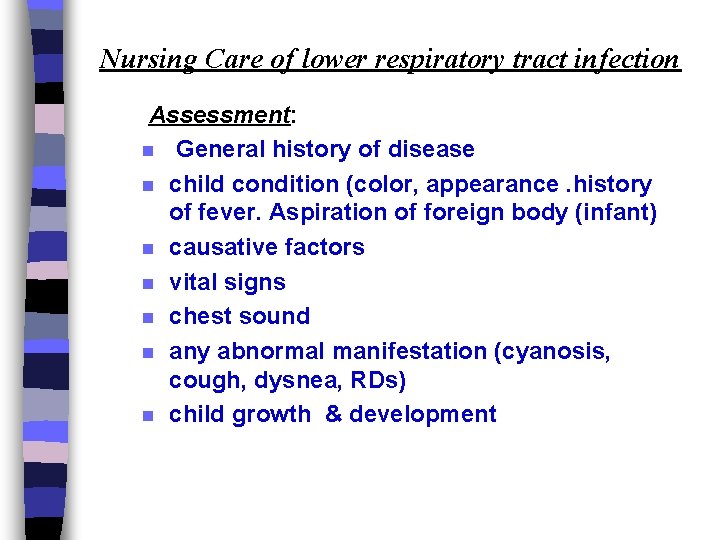
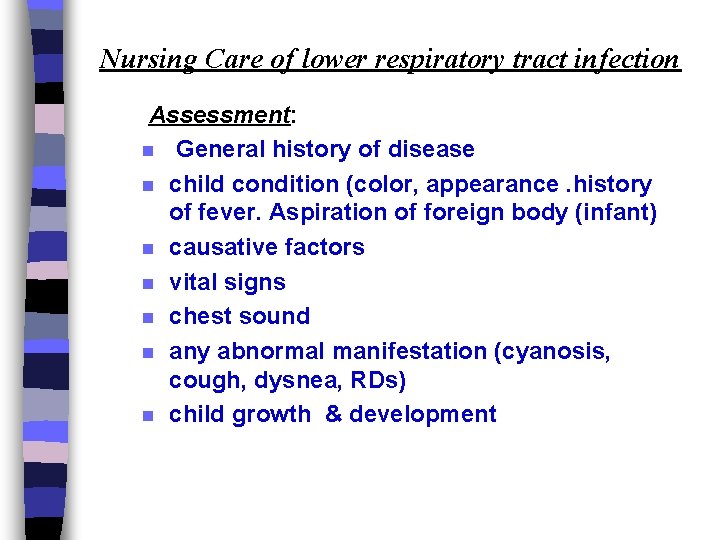
Nursing Care of lower respiratory tract infection Assessment: n General history of disease n child condition (color, appearance. history of fever. Aspiration of foreign body (infant) n causative factors n vital signs n chest sound n any abnormal manifestation (cyanosis, cough, dysnea, RDs) n child growth & development
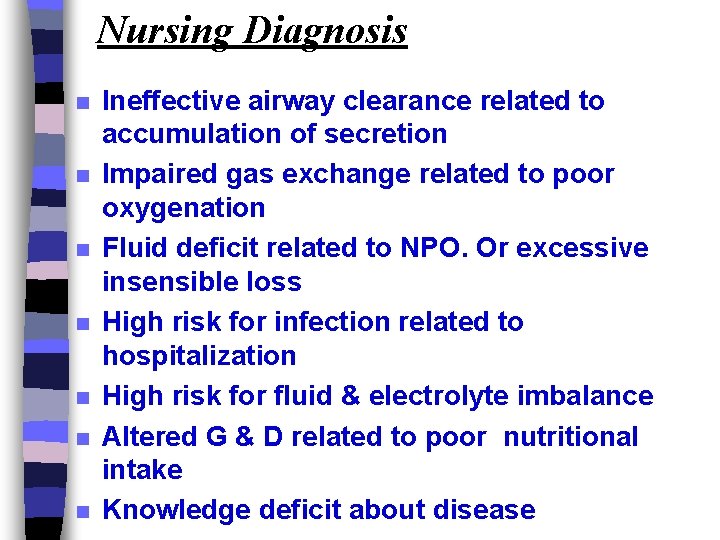
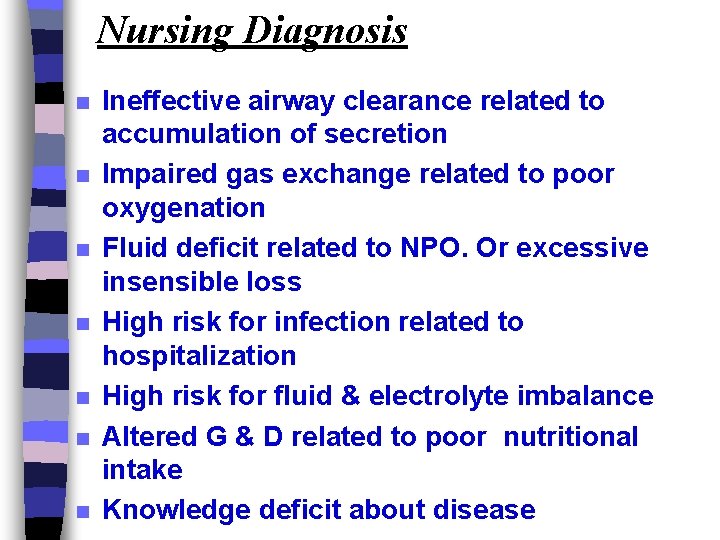
Nursing Diagnosis n n n n Ineffective airway clearance related to accumulation of secretion Impaired gas exchange related to poor oxygenation Fluid deficit related to NPO. Or excessive insensible loss High risk for infection related to hospitalization High risk for fluid & electrolyte imbalance Altered G & D related to poor nutritional intake Knowledge deficit about disease
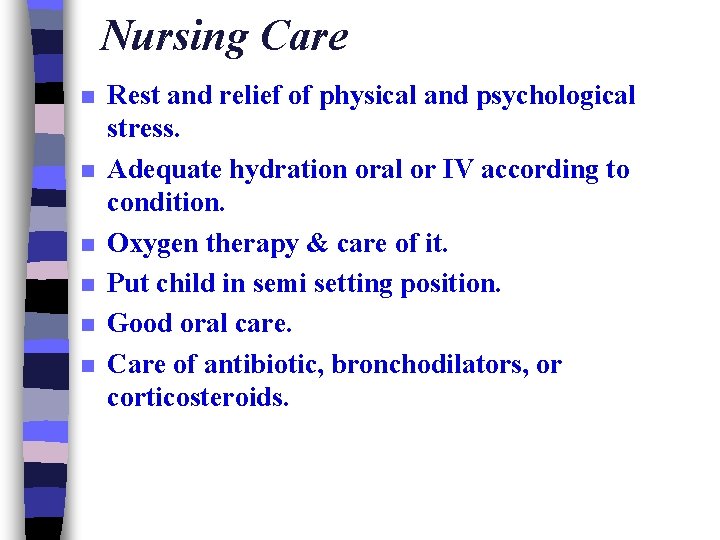
Nursing Care n n n Rest and relief of physical and psychological stress. Adequate hydration oral or IV according to condition. Oxygen therapy & care of it. Put child in semi setting position. Good oral care. Care of antibiotic, bronchodilators, or corticosteroids.
n Care of fever & administration of antipyretic drugs. n Chest physiotherapy. ( percussion , vibration , lying on the affected side (if pneumonia unilateral) , postural drainage and chest physiotherapy are generally prescribed every 4 hours or more often, coughing & breathing exercise if available )
Nursing Care of lower respiratory tract infection Assessment: n General history of disease n child condition (color, appearance. history of fever. Aspiration of foreign body (infant) n causative factors n vital signs n chest sound n any abnormal manifestation (cyanosis, cough, dysnea, RDs) n child growth & development
Nursing Diagnosis: Ineffective airway clearance related to accumulation of secretion n Impaired gas exchange related to poor oxygenation n Fluid deficit related to NPO. Or excessive insensible loss n High risk for infection related to hospitalization n High risk for fluid & electrolyte imbalance n Altered G & D related to poor nutritional intake n Knowledge deficit about disease
Nursing Care n Rest and relief of physical and psychological stress. n Adequate hydration oral or IV according to condition. n Oxygen therapy & care of it. n Put child in semi setting position. n Good oral care. n Care of antibiotic, bronchodilators, or corticosteroids.
Upper Respiratory Infections (URIs)
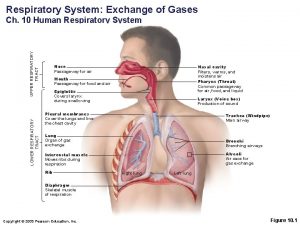
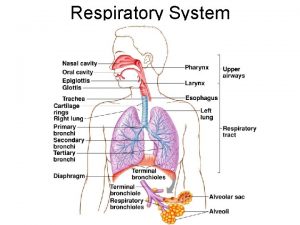
 Upper and lower respiratory tract
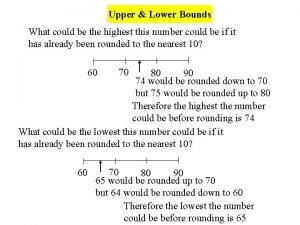
Upper and lower respiratory tract Nearest whole number upper and lower bounds
Nearest whole number upper and lower bounds Greatest lower bound and least upper bound
Greatest lower bound and least upper bound Physiology of respiration
Physiology of respiration Upper and lower bounds 3 significant figures
Upper and lower bounds 3 significant figures Upper and lower control limit formula
Upper and lower control limit formula Chuck allison
Chuck allison If lclp is negative number, we set the lclp = 0. why?
If lclp is negative number, we set the lclp = 0. why? Upper specification limit and lower specification limit
Upper specification limit and lower specification limit How to find upper and lower bounds
How to find upper and lower bounds Upper egypt and lower egypt
Upper egypt and lower egypt Lower and upper extremes
Lower and upper extremes Upper bound and lower bound in array
Upper bound and lower bound in array Laryngoscopy view grades
Laryngoscopy view grades Multiplication of diagonal matrix
Multiplication of diagonal matrix Abandon all hope ye who enter here
Abandon all hope ye who enter here Uti upper and lower
Uti upper and lower Upper and lower bounds of rounded numbers
Upper and lower bounds of rounded numbers Simple roof plan
Simple roof plan What divided upper and lower egypt
What divided upper and lower egypt Nearest whole number upper and lower bounds
Nearest whole number upper and lower bounds Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Johnson and johnson botnet infections
Johnson and johnson botnet infections Bone and joint infections
Bone and joint infections Methotrexate yeast infection
Methotrexate yeast infection Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Pneumonia classification
Pneumonia classification Lower respiratory system
Lower respiratory system Programme upper lower
Programme upper lower How to find the critical f value
How to find the critical f value Leaf tissues
Leaf tissues Upper lower bounds
Upper lower bounds Upper lower class
Upper lower class Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Storch infections
Storch infections Cryptosporidiose
Cryptosporidiose Bacterial vaginosis
Bacterial vaginosis Postpartum infections
Postpartum infections Genital infections
Genital infections Amber blumling
Amber blumling Opsonization
Opsonization Classification of acute gingival infections
Classification of acute gingival infections Respiratory zone
Respiratory zone External nose
External nose Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Ophthalmootorhinolaryngology
Ophthalmootorhinolaryngology Upper respiratory tract
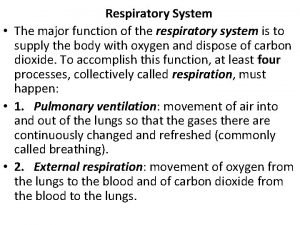
Upper respiratory tract What is the major function of the respiratory system
What is the major function of the respiratory system Broncheols
Broncheols Lesser saphenous vein
Lesser saphenous vein Lower delaware national wild and scenic river
Lower delaware national wild and scenic river Chapter 19 worksheet the ankle and lower leg
Chapter 19 worksheet the ankle and lower leg Chapter 15 the ankle and lower leg
Chapter 15 the ankle and lower leg Anterior tibial artery palpation
Anterior tibial artery palpation Sacral plexus
Sacral plexus Fraser valley health region map
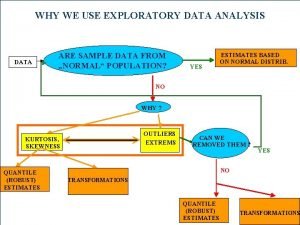
Fraser valley health region map Q-q graf
Q-q graf D2 flexion
D2 flexion The curve part of the head containing
The curve part of the head containing Pareto economist
Pareto economist Formation of a flood plain
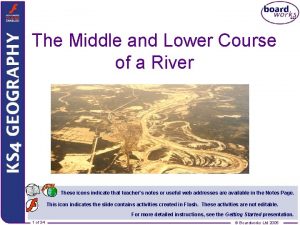
Formation of a flood plain Lower south colonies
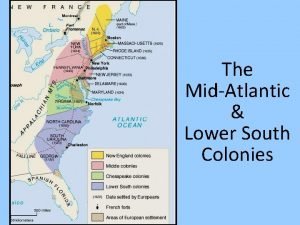
Lower south colonies Rosoideae
Rosoideae Vertical suspension
Vertical suspension Anatomical axis of lower limb
Anatomical axis of lower limb Left lower extremity
Left lower extremity Lower inner fence
Lower inner fence Lower jaw fracture
Lower jaw fracture Q1 formula for continuous series
Q1 formula for continuous series Cutaneous supply of lower limb
Cutaneous supply of lower limb Upper oblique occlusal radiograph
Upper oblique occlusal radiograph Lower gi 2ww pathway
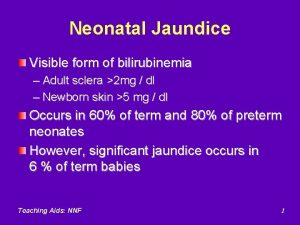
Lower gi 2ww pathway Hyperbilirubinemia workup
Hyperbilirubinemia workup Nz uniform lower hutt
Nz uniform lower hutt Nz uniform shop lower hutt
Nz uniform shop lower hutt Muscles of thigh cross section
Muscles of thigh cross section Western lower peninsula michigan
Western lower peninsula michigan Which principle
Which principle People as media vs people in media
People as media vs people in media