Acute diarrhea Diarrhea n Diarrhea is a clinical

- Slides: 47
Acute diarrhea
Diarrhea n Diarrhea is a clinical syndrome of diverse etiology associated with many influencing factors • In pediatrics, diarrhea is defined as an increase in the – Fluidity – Volume – Frequency of the stool Relative to the usual habits of each individual
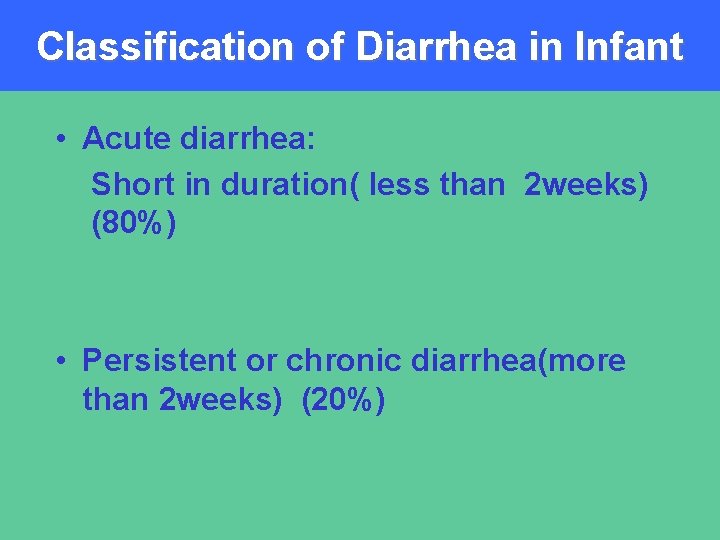
Classification of Diarrhea in Infant • Acute diarrhea: Short in duration( less than 2 weeks) (80%) • Persistent or chronic diarrhea(more than 2 weeks) (20%)
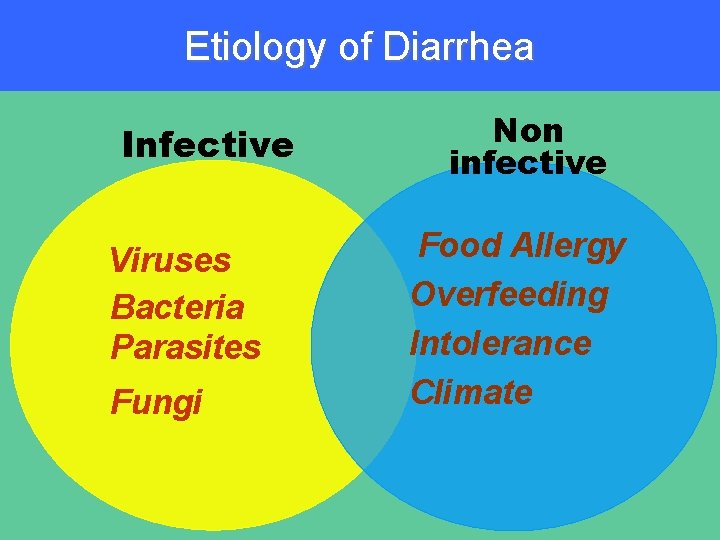
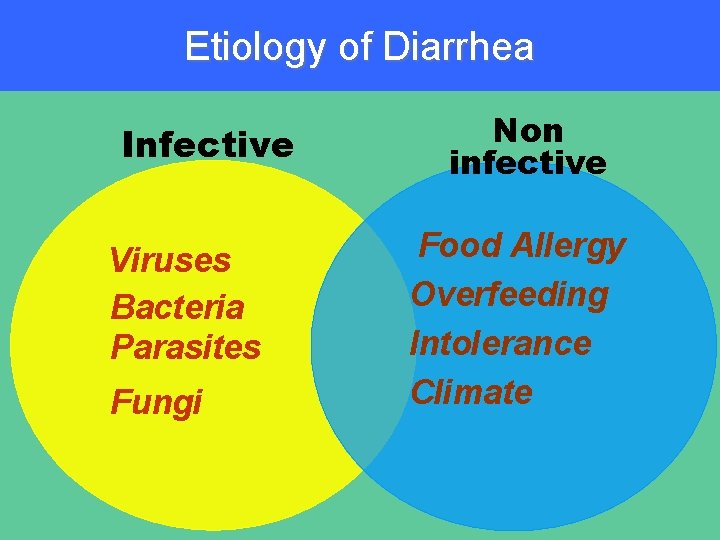
Etiology of Diarrhea Infective Viruses Bacteria Parasites Fungi Non infective Food Allergy Overfeeding Intolerance Climate
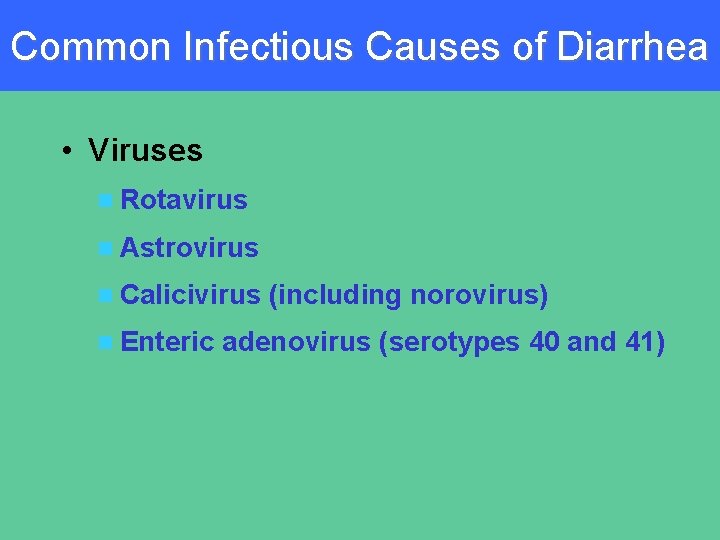
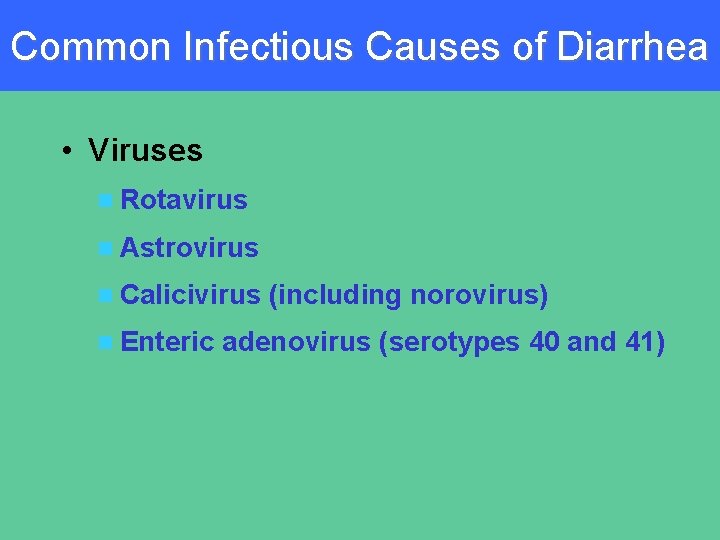
Common Infectious Causes of Diarrhea • Viruses n Rotavirus n Astrovirus n Calicivirus n Enteric (including norovirus) adenovirus (serotypes 40 and 41)
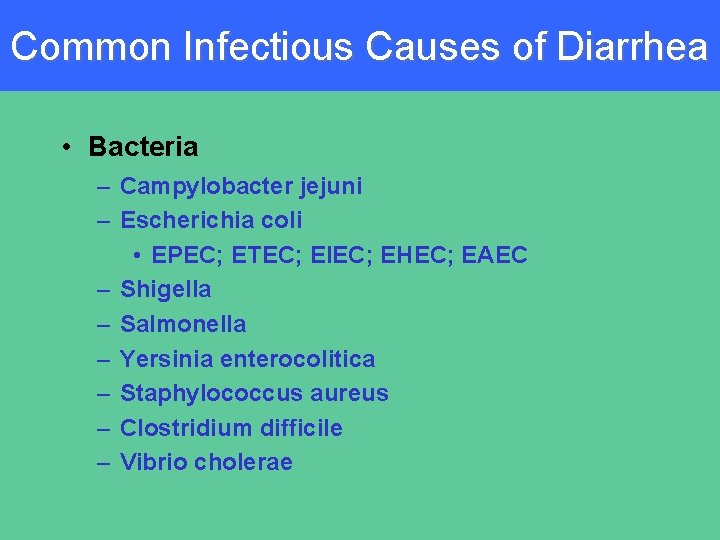
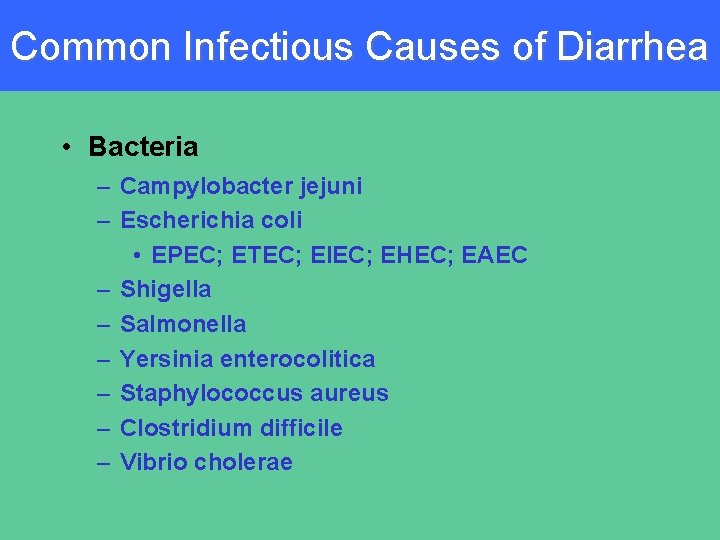
Common Infectious Causes of Diarrhea • Bacteria – Campylobacter jejuni – Escherichia coli • EPEC; ETEC; EIEC; EHEC; EAEC – Shigella – Salmonella – Yersinia enterocolitica – Staphylococcus aureus – Clostridium difficile – Vibrio cholerae
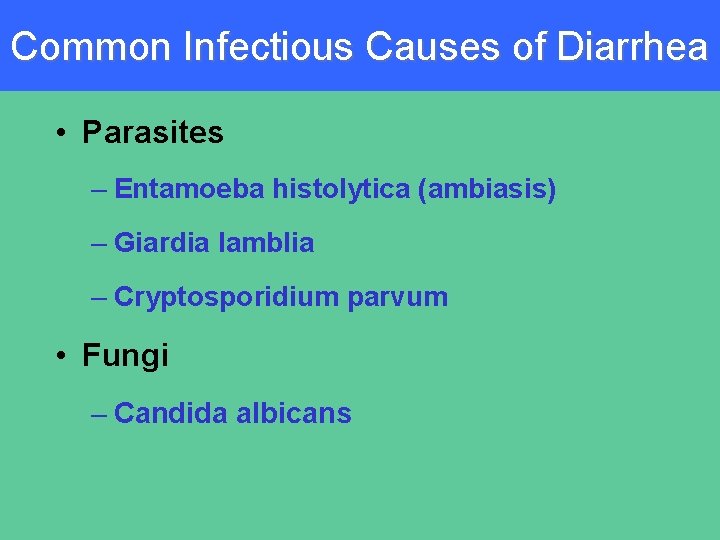
Common Infectious Causes of Diarrhea • Parasites – Entamoeba histolytica (ambiasis) – Giardia lamblia – Cryptosporidium parvum • Fungi – Candida albicans
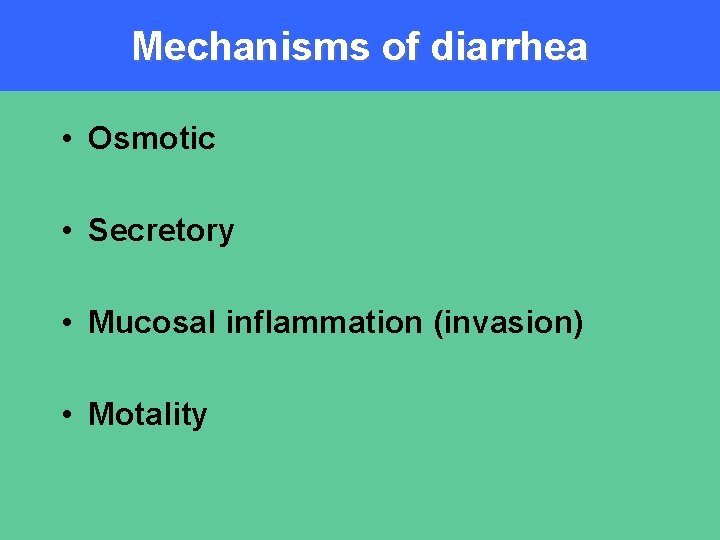
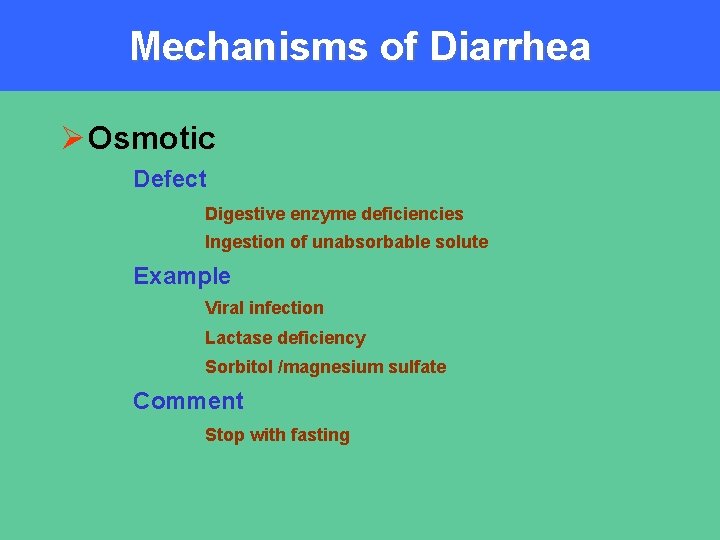
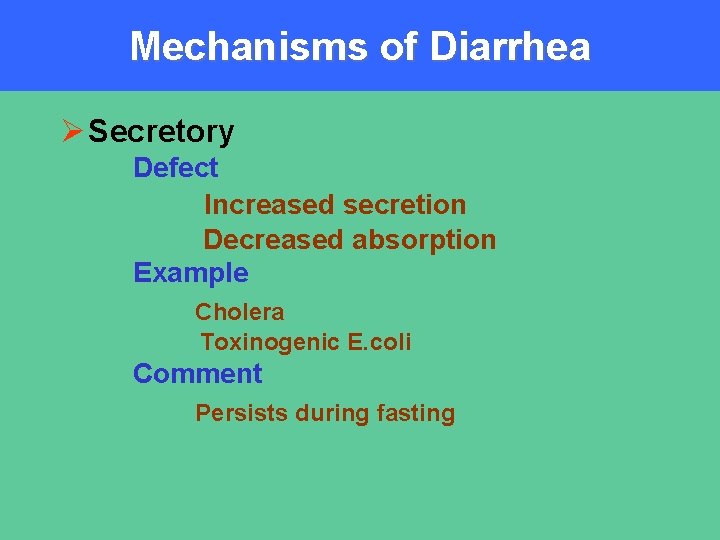
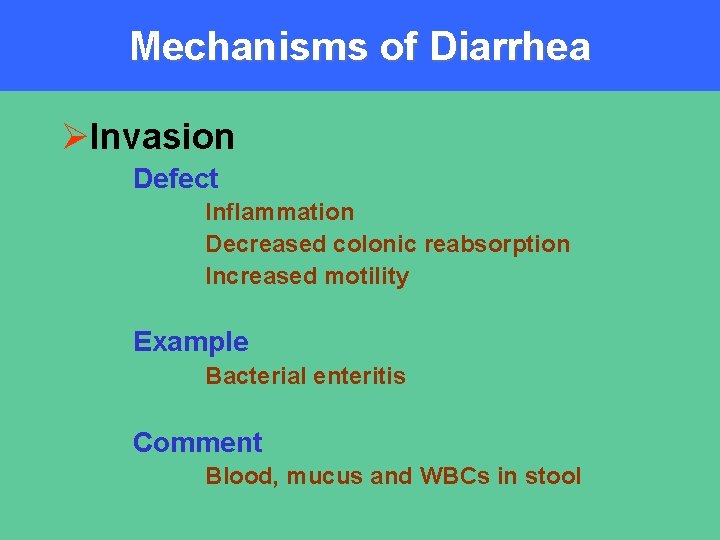
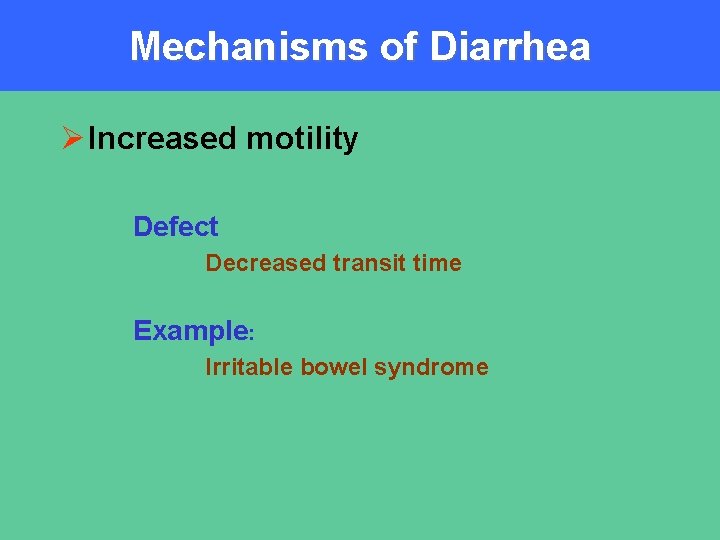
Mechanisms of diarrhea • Osmotic • Secretory • Mucosal inflammation (invasion) • Motality
Mechanisms of Diarrhea Ø Osmotic Defect Digestive enzyme deficiencies Ingestion of unabsorbable solute Example Viral infection Lactase deficiency Sorbitol /magnesium sulfate Comment Stop with fasting
Mechanisms of Diarrhea Ø Secretory Defect Increased secretion Decreased absorption Example Cholera Toxinogenic E. coli Comment Persists during fasting
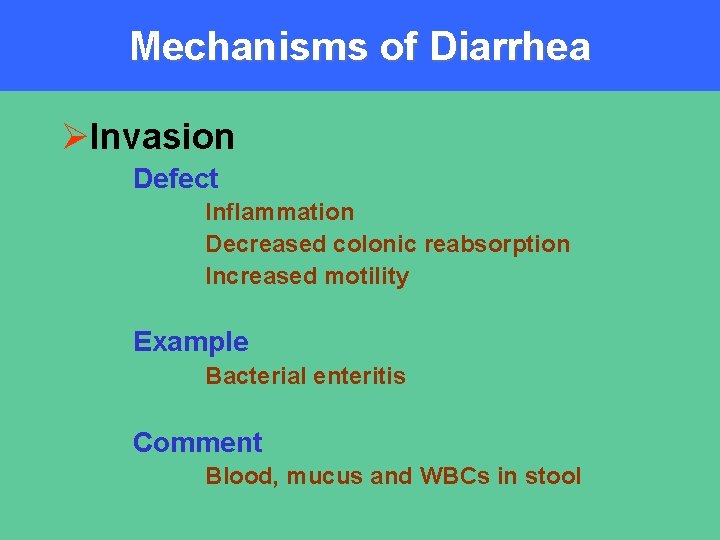
Mechanisms of Diarrhea ØInvasion Defect Inflammation Decreased colonic reabsorption Increased motility Example Bacterial enteritis Comment Blood, mucus and WBCs in stool
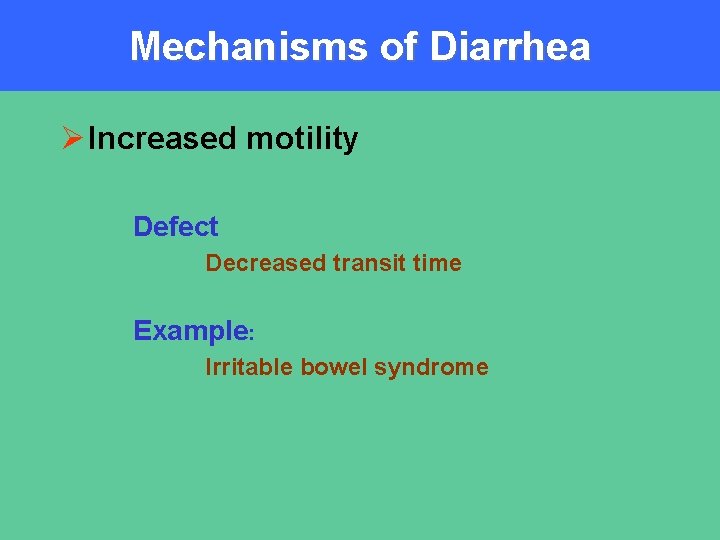
Mechanisms of Diarrhea Ø Increased motility Defect Decreased transit time Example: Irritable bowel syndrome
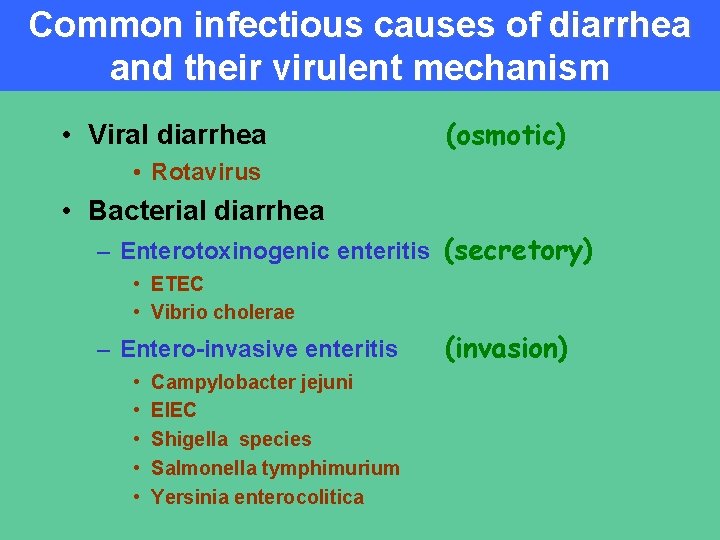
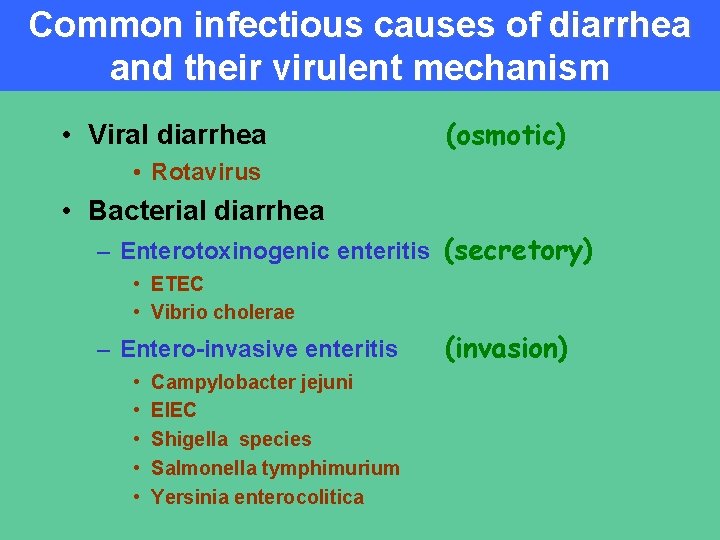
Common infectious causes of diarrhea and their virulent mechanism • Viral diarrhea (osmotic) • Rotavirus • Bacterial diarrhea – Enterotoxinogenic enteritis (secretory) • ETEC • Vibrio cholerae – Entero-invasive enteritis • • • Campylobacter jejuni EIEC Shigella species Salmonella tymphimurium Yersinia enterocolitica (invasion)
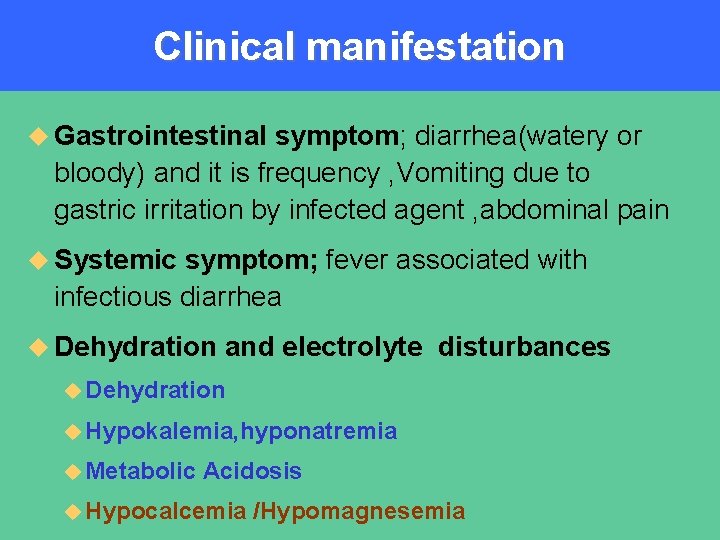
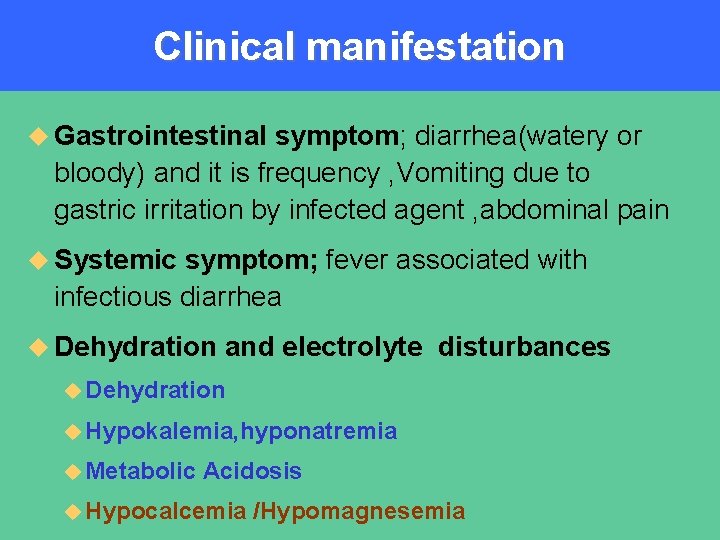
Clinical manifestation u Gastrointestinal symptom; diarrhea(watery or bloody) and it is frequency , Vomiting due to gastric irritation by infected agent , abdominal pain u Systemic symptom; fever associated with infectious diarrhea u Dehydration and electrolyte disturbances u Dehydration u Hypokalemia, hyponatremia u Metabolic Acidosis u Hypocalcemia /Hypomagnesemia
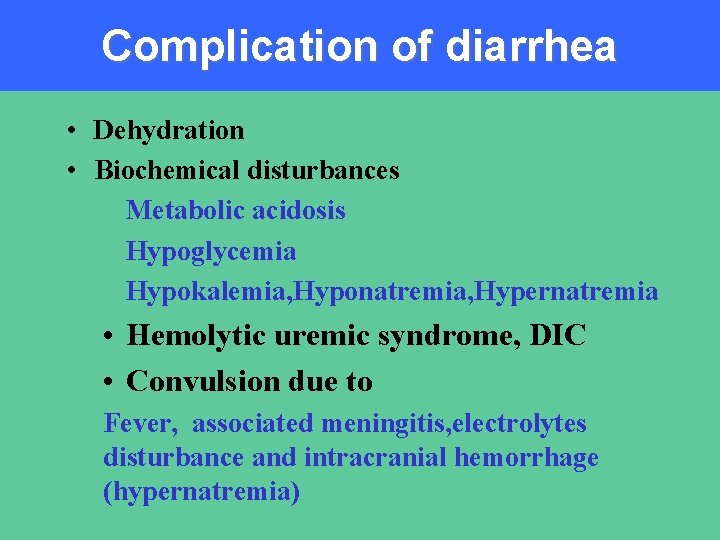
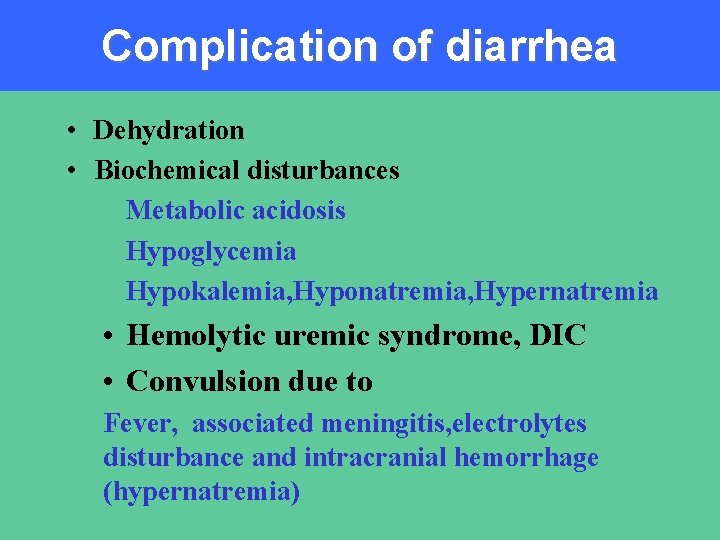
Complication of diarrhea • Dehydration • Biochemical disturbances Metabolic acidosis Hypoglycemia Hypokalemia, Hyponatremia, Hypernatremia • Hemolytic uremic syndrome, DIC • Convulsion due to Fever, associated meningitis, electrolytes disturbance and intracranial hemorrhage (hypernatremia)
Dehydration • Excessive loss of water, • especially loss of extracellular fluid
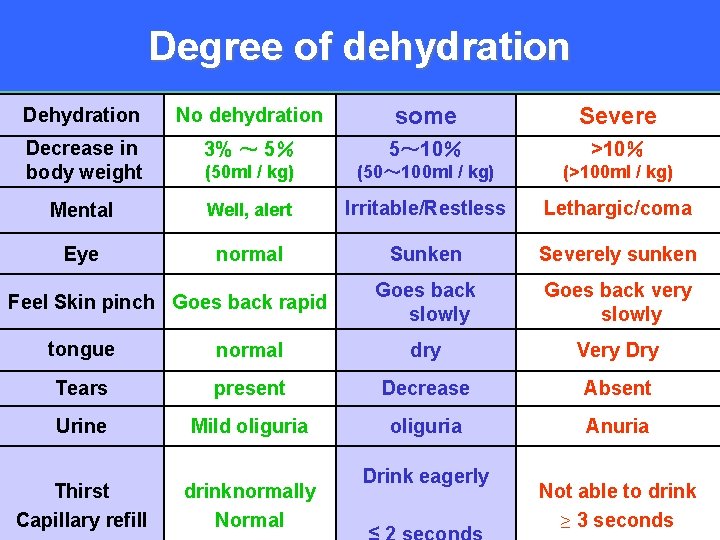
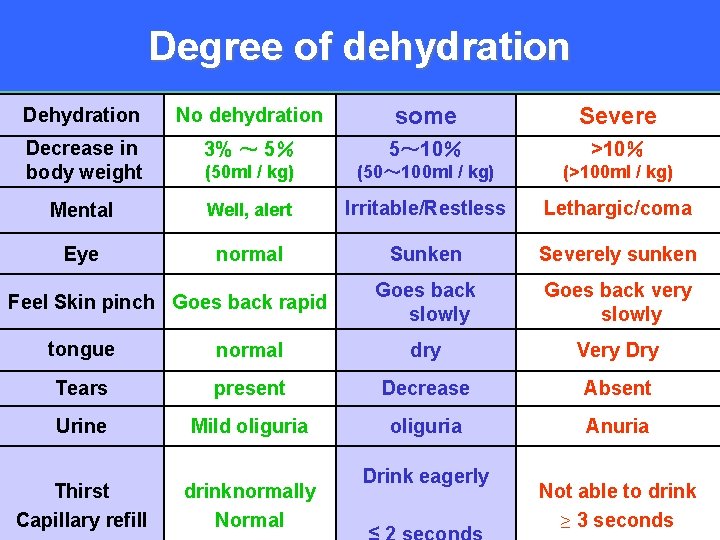
Degree of dehydration Dehydration No dehydration some Severe Decrease in body weight 3% ~ 5% 5~ 10% >10% (50 ml / kg) (50~ 100 ml / kg) (>100 ml / kg) Mental Well, alert Irritable/Restless Lethargic/coma Eye normal Sunken Severely sunken Goes back slowly Goes back very slowly Feel Skin pinch Goes back rapid tongue normal dry Very Dry Tears present Decrease Absent Urine Mild oliguria Anuria Thirst Capillary refill drinknormally Normal Drink eagerly Not able to drink ≥ 3 seconds
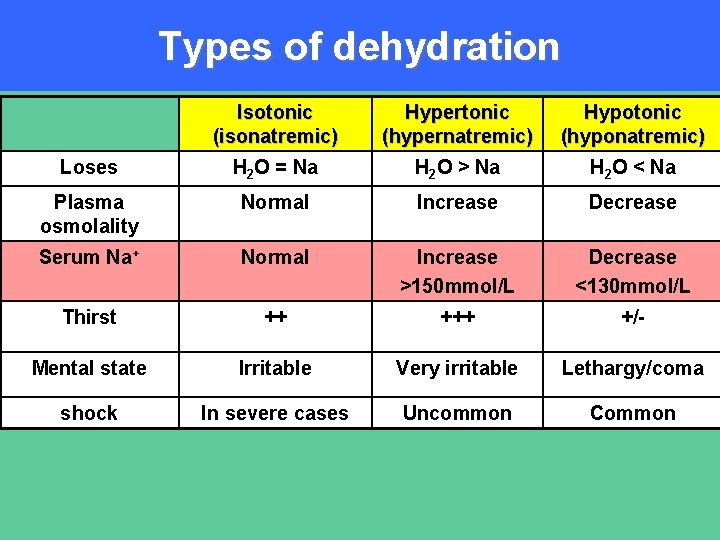
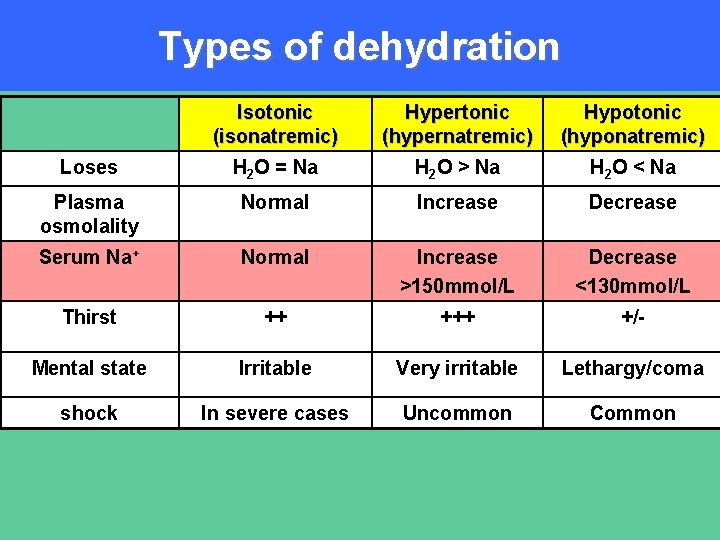
Types of dehydration Isotonic (isonatremic) Hypertonic (hypernatremic) Hypotonic (hyponatremic) Loses H 2 O = Na H 2 O > Na H 2 O < Na Plasma osmolality Normal Increase Decrease Serum Na+ Normal Increase >150 mmol/L Decrease <130 mmol/L Thirst ++ +/- Mental state Irritable Very irritable Lethargy/coma shock In severe cases Uncommon Common
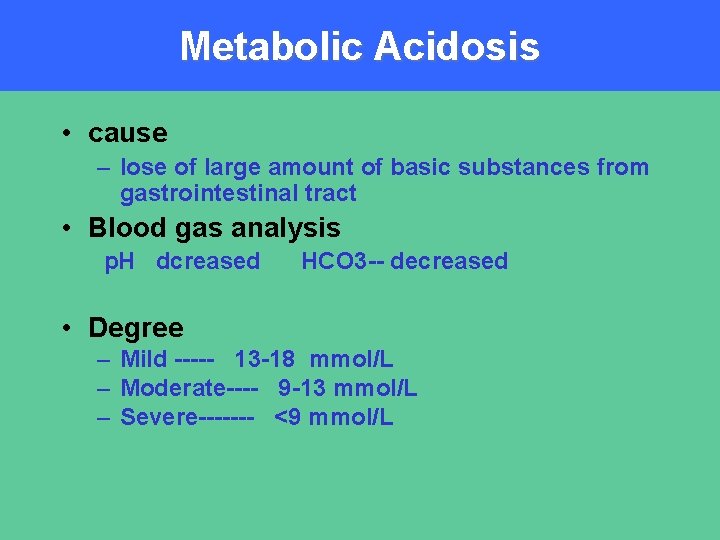
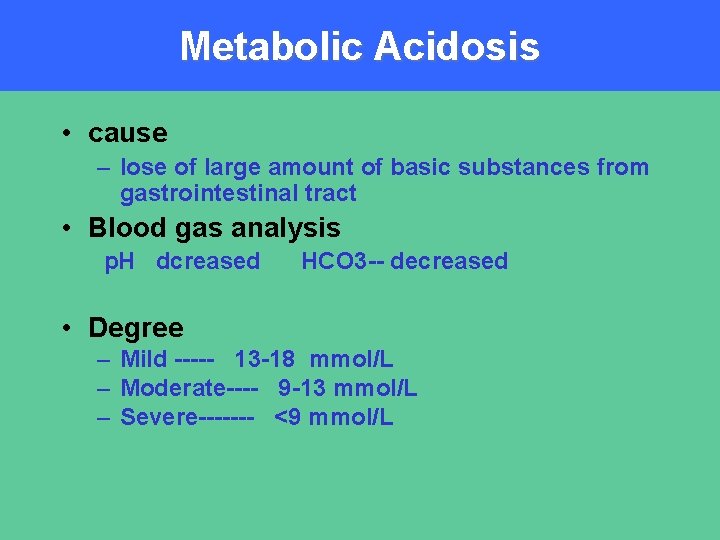
Metabolic Acidosis • cause – lose of large amount of basic substances from gastrointestinal tract • Blood gas analysis p. H dcreased HCO 3 -- decreased • Degree – Mild ----- 13 -18 mmol/L – Moderate---- 9 -13 mmol/L – Severe------- <9 mmol/L
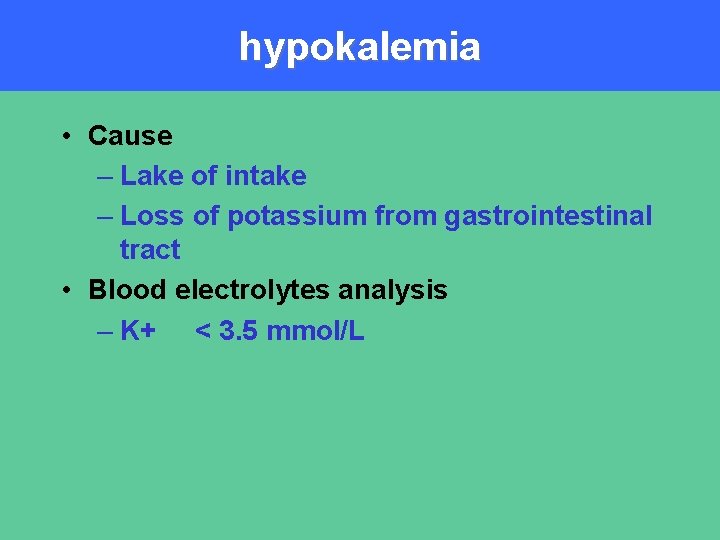
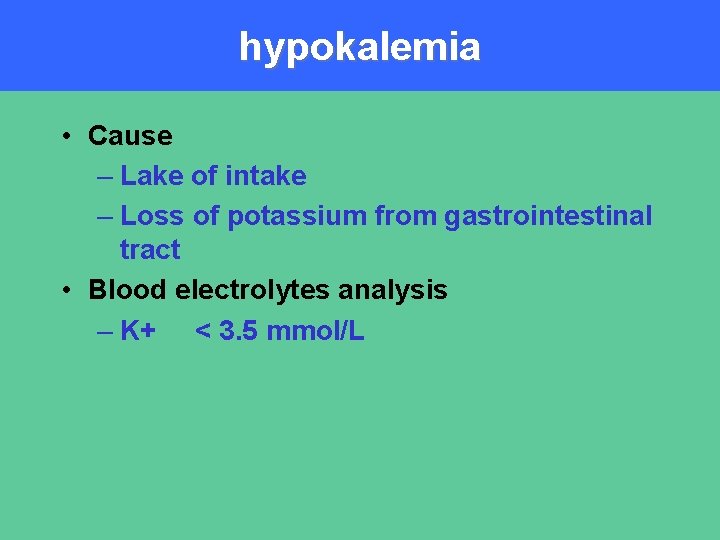
hypokalemia • Cause – Lake of intake – Loss of potassium from gastrointestinal tract • Blood electrolytes analysis – K+ < 3. 5 mmol/L
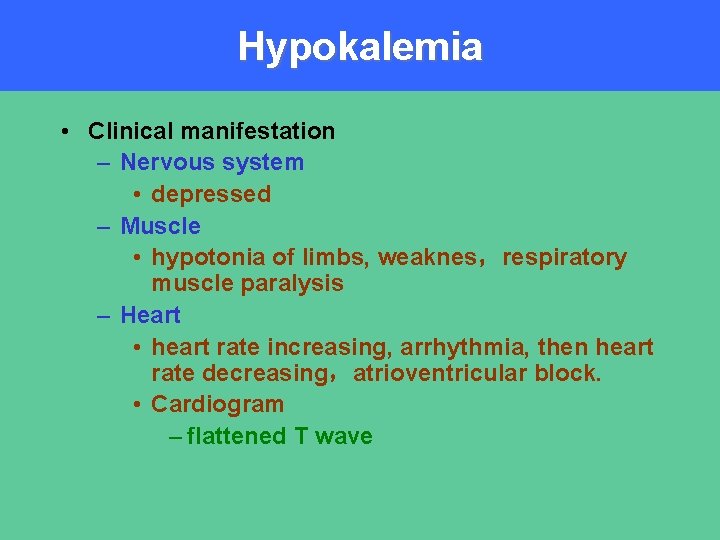
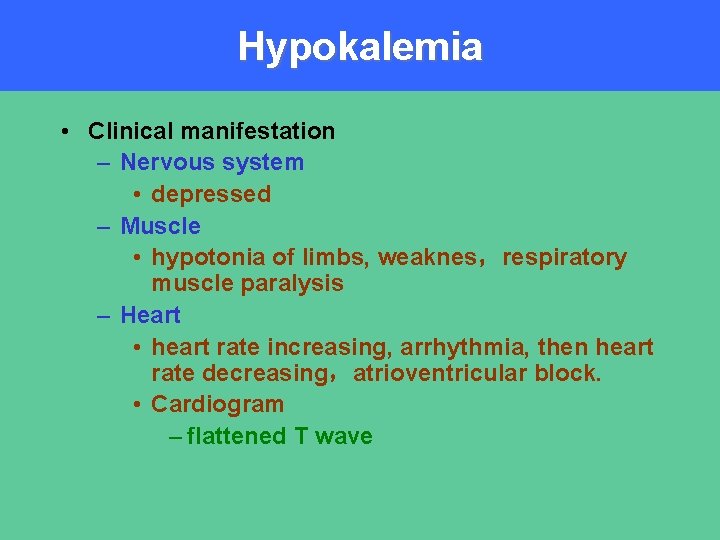
Hypokalemia • Clinical manifestation – Nervous system • depressed – Muscle • hypotonia of limbs, weaknes,respiratory muscle paralysis – Heart • heart rate increasing, arrhythmia, then heart rate decreasing,atrioventricular block. • Cardiogram – flattened T wave
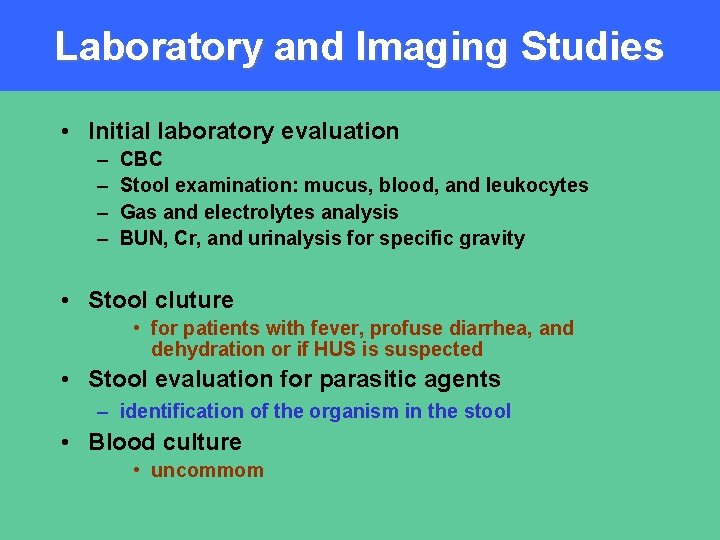
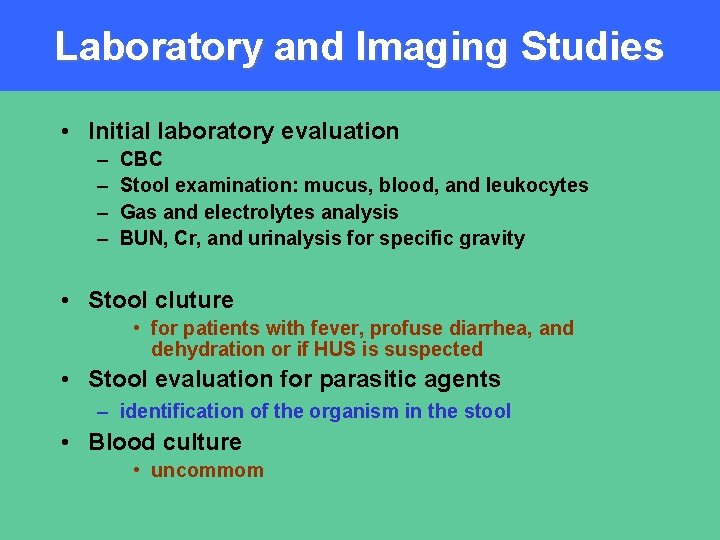
Laboratory and Imaging Studies • Initial laboratory evaluation – – CBC Stool examination: mucus, blood, and leukocytes Gas and electrolytes analysis BUN, Cr, and urinalysis for specific gravity • Stool cluture • for patients with fever, profuse diarrhea, and dehydration or if HUS is suspected • Stool evaluation for parasitic agents – identification of the organism in the stool • Blood culture • uncommom
Diagnosis & Differential Diagnosis
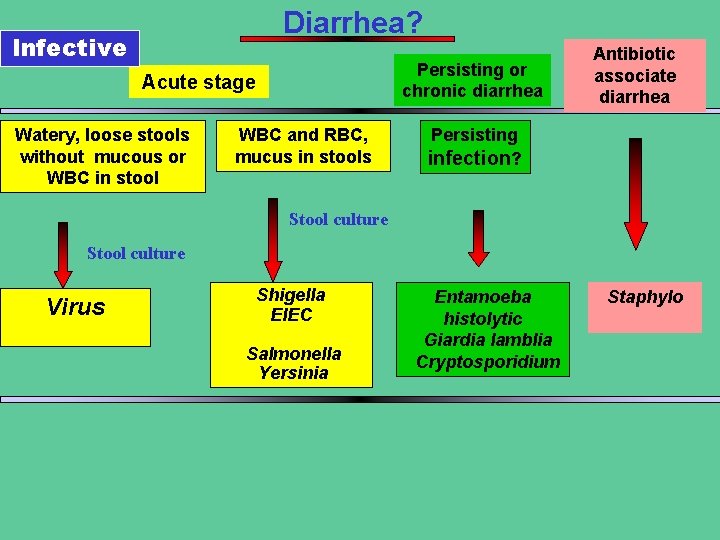
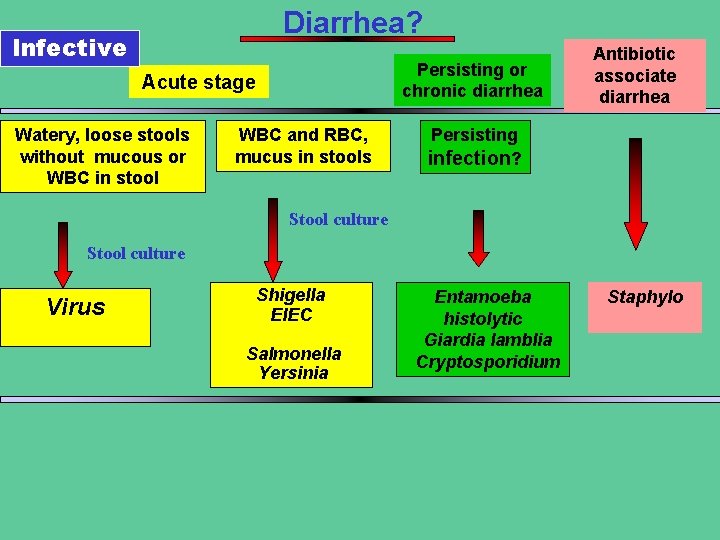
Diarrhea? Infective Persisting or chronic diarrhea Acute stage Watery, loose stools without mucous or WBC in stool WBC and RBC, mucus in stools Antibiotic associate diarrhea Persisting infection? Stool culture Virus Shigella EIEC Salmonella Yersinia Entamoeba histolytic Giardia lamblia Cryptosporidium Staphylo
Treatment • Primarily supportive – Fluid therapy • Rehydration • Correcting acidosis • Potassium supplement • Correcting ongoing loss – Managing secondary complication resulting from mucosa injury • Antibiotic treatment – for only some bacterial and parasitic causes of diarrhea • Start food as soon as possilble
Treatment of diarrhea with no dehydration Treatment of diarrhea at home: Is appropriate when the child have no signs of dehydration. Three important rules has to be explained to the mother: 1. Give the child more fluid than usual to prevent dehydration. The recommended home fluids include ORS, food based fluids ( soups, rice water, ), and water
Treatment of diarrhea with no dehydration Amount of ORS to be given after each loose stool is 50 – 100 ml. in children less than 2 years of age and 100 – 200 ml. in older child. Continue giving these fluids until diarrhea stops, ORS is given by cup and spoon 1 tsp/12 minutes
Treatment of diarrhea with no dehydration 2 -Give the child plenty of food to prevent malnutrition. • Continue to breast feed frequently and if the child is not breast fed give the usual milk. • If the child is 6 months or older - give cereal or another starchy food mixed vegetables and Add 1 -2 teaspoonful vegetable oil to each serving
Treatment of diarrhea with no dehydration 3 - Take the child to the health center if he does not get better in three days or develops - Many watery stools. - Repeated vomiting. - Marked thirst. - Eating or drinking poorly. - Blood in stools. - Fever
Treatment of diarrhea with some dehydration Some dehydration: • Can be treated in the ORS center where mothers can help with treatment and learn how to continue it at home. • Oral rehydration solution 75 ml/kg has to be given in the first four hours. It should be given by a cup and spoon. A teaspoonful every 1 – 2 minutes for infants and frequent sips from a cup for an older child.
Treatment of diarrhea with some dehydration • If the child vomits, wait 10 minutes and then continue giving ORS but more slowly. • Still persistent vomiting give ORS by NGT 20 ml/kg/hr for 6 hours • If the child eyelids become puffy stop ORS and give plain water or breast milk until the puffiness is gone. • After 4 hours carefully reassess the child’s hydration status; If the child has No signs of dehydration, the child can continue treatment at home by ORS and feeding.
Treatment of diarrhea with some dehydration • If there are signs of some dehydration continue giving the estimated volume of ORS again until the signs of dehydration disappear. If the child is passing watery stools frequently and the signs of severe dehydration appear ORS should be temporarily stopped and the child rehydrated intravenously
Treatment of diarrhea with sever dehydration Sever dehydration : The treatment of choice is Intravenous fluid. • Ringer’s lactate is the preferred solution. Normal saline or half normal saline in glucose may be used. • Infants should receive IV fluid at a rate of 30 ml. /kg in the first hour followed by 70 ml. /kg in the next 5 hours, thus providing 100 ml. /kg in 6 hours(<1 year)
Treatment of diarrhea with sever dehydration • Older children should be given 30 ml. /kg within 30 minutes followed by 70 ml. /kg in the next 2 and half hours, thus providing 100 ml. /kg in 3 hours. (>1 year) • After the first 30 ml/kg has been given a strong radial pulse should be readily palpable If it is very weak and rapid a second infusion of 30 ml. /kg should be given in the same rate; however, this is rarely necessary.
Treatment of diarrhea with sever dehydration • Small amounts of ORS( 5 ml/kg) should also be given by mouth as soon as the patient is able to drink to provide additional potassium and bicarbonate.
Treatment of diarrhea with sever dehydration • At the end of planned rehydration period ( usually 3 – 6 hours), the patient hydration state should be reassessed carefully. If signs of sever dehydration are still present rehydration should be continued by IV route, If there are signs of some dehydration shift to treatment of some dehydration
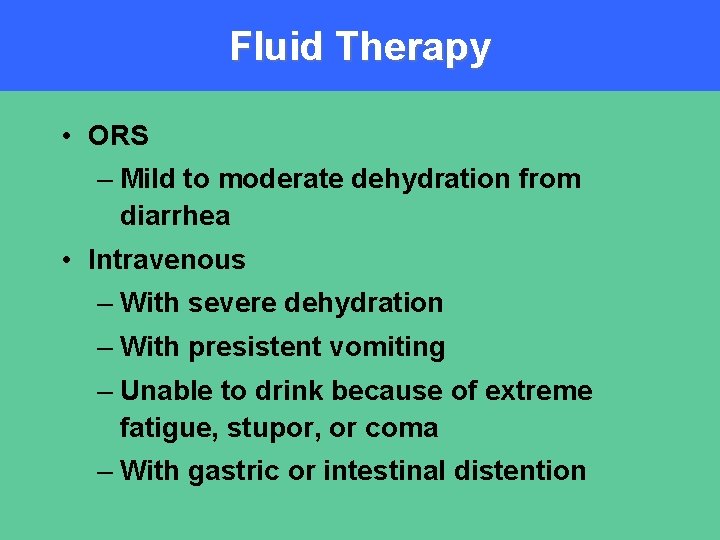
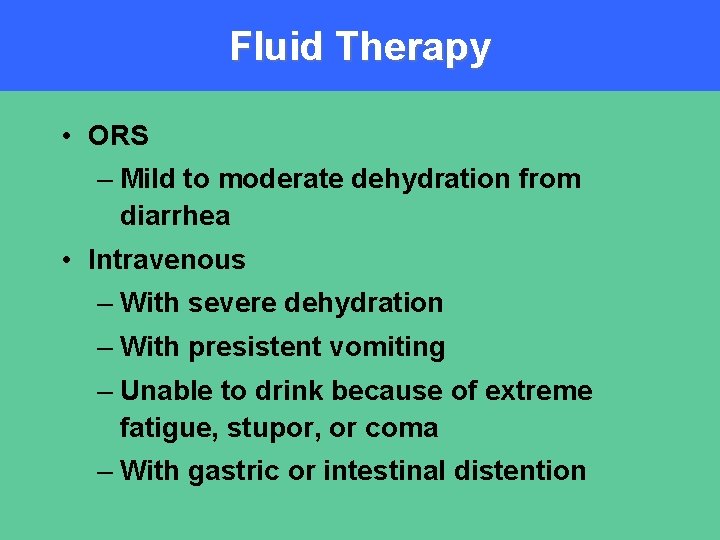
Fluid Therapy • ORS – Mild to moderate dehydration from diarrhea • Intravenous – With severe dehydration – With presistent vomiting – Unable to drink because of extreme fatigue, stupor, or coma – With gastric or intestinal distention
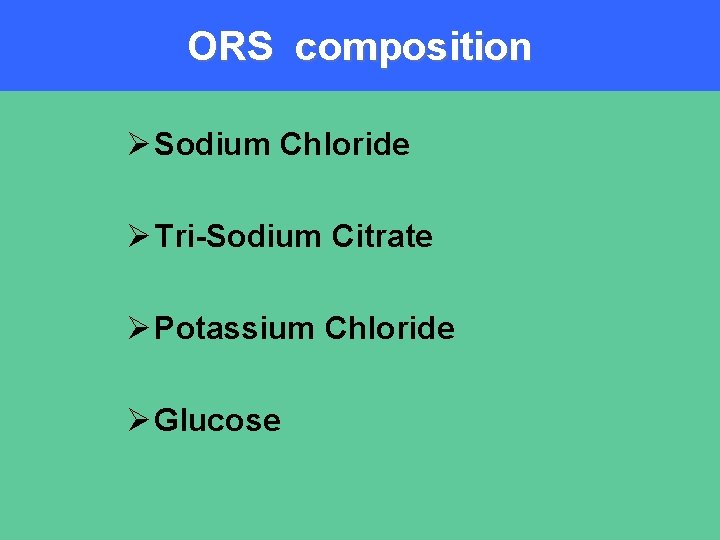
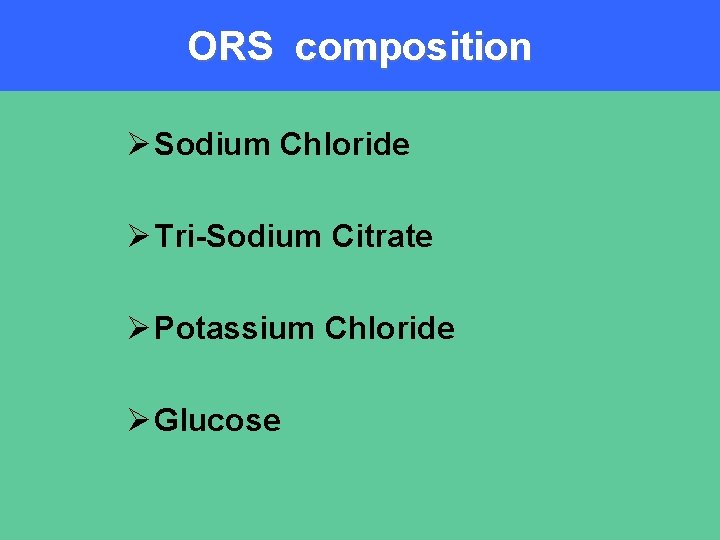
ORS composition Ø Sodium Chloride Ø Tri-Sodium Citrate Ø Potassium Chloride Ø Glucose
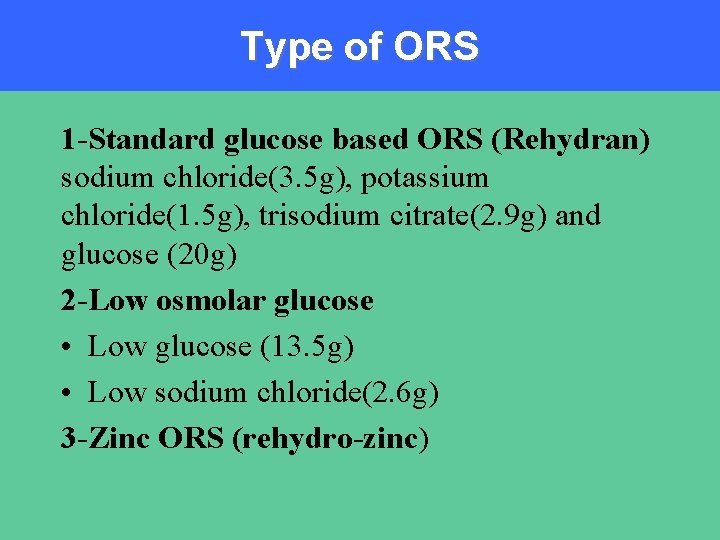
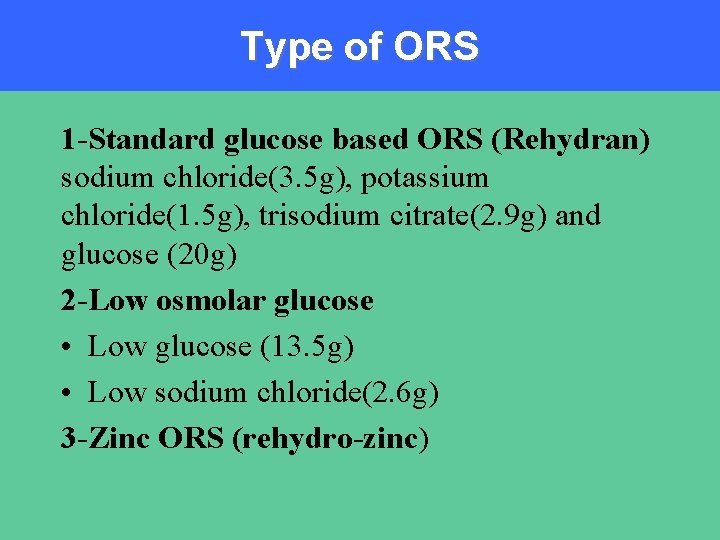
Type of ORS 1 -Standard glucose based ORS (Rehydran) sodium chloride(3. 5 g), potassium chloride(1. 5 g), trisodium citrate(2. 9 g) and glucose (20 g) 2 -Low osmolar glucose • Low glucose (13. 5 g) • Low sodium chloride(2. 6 g) 3 -Zinc ORS (rehydro-zinc)
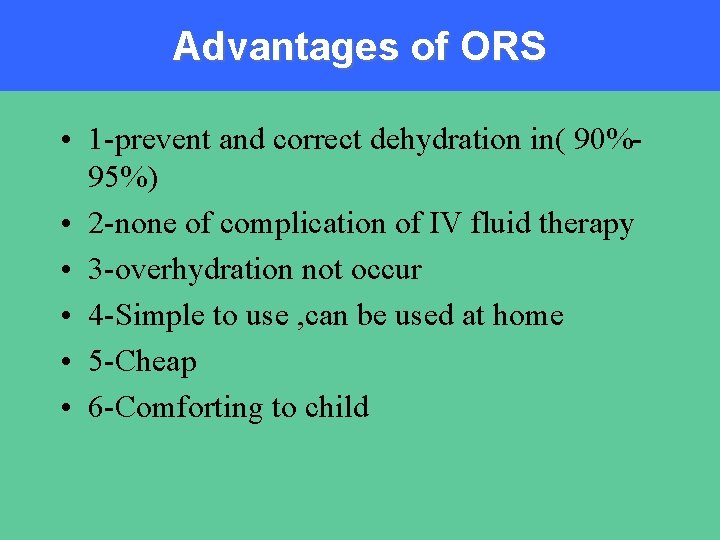
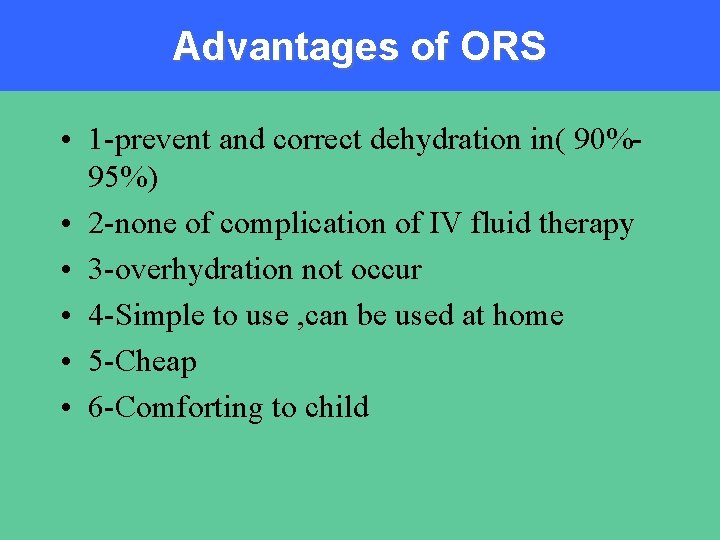
Advantages of ORS • 1 -prevent and correct dehydration in( 90%95%) • 2 -none of complication of IV fluid therapy • 3 -overhydration not occur • 4 -Simple to use , can be used at home • 5 -Cheap • 6 -Comforting to child
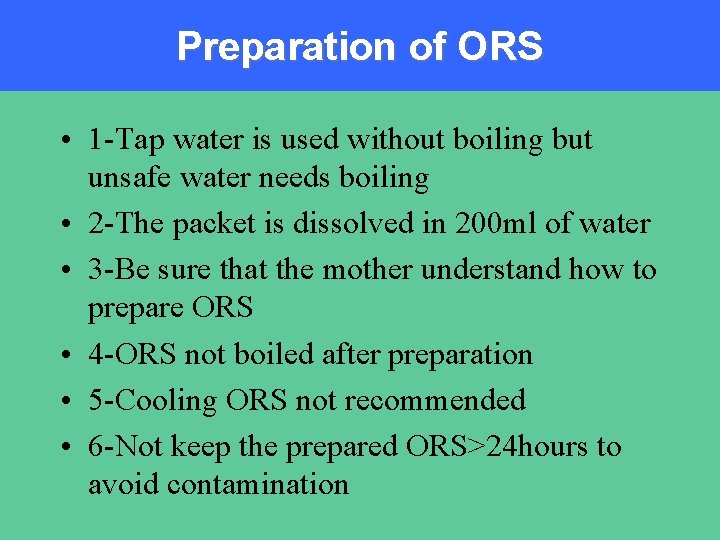
Preparation of ORS • 1 -Tap water is used without boiling but unsafe water needs boiling • 2 -The packet is dissolved in 200 ml of water • 3 -Be sure that the mother understand how to prepare ORS • 4 -ORS not boiled after preparation • 5 -Cooling ORS not recommended • 6 -Not keep the prepared ORS>24 hours to avoid contamination
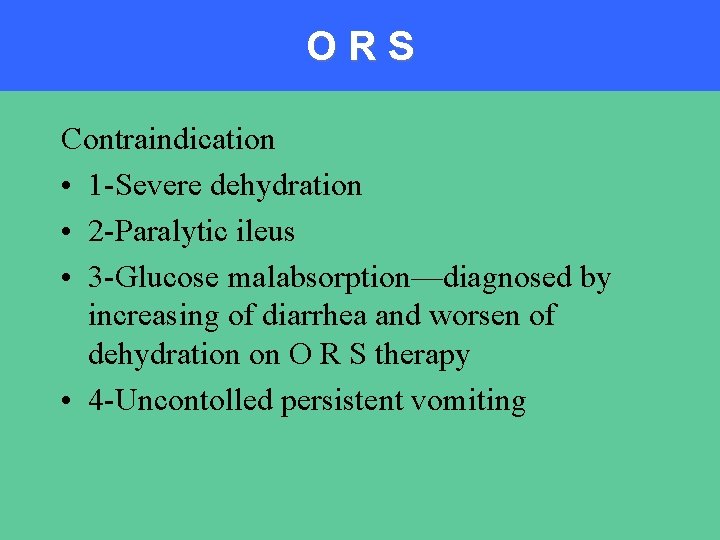
ORS Contraindication • 1 -Severe dehydration • 2 -Paralytic ileus • 3 -Glucose malabsorption—diagnosed by increasing of diarrhea and worsen of dehydration on O R S therapy • 4 -Uncontolled persistent vomiting
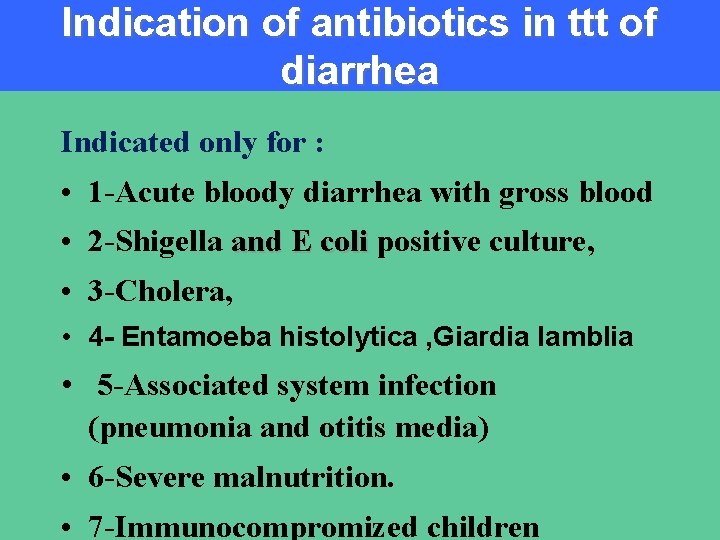
Indication of antibiotics in ttt of diarrhea Indicated only for : • 1 -Acute bloody diarrhea with gross blood • 2 -Shigella and E coli positive culture, • 3 -Cholera, • 4 - Entamoeba histolytica , Giardia lamblia • 5 -Associated system infection (pneumonia and otitis media) • 6 -Severe malnutrition. • 7 -Immunocompromized children
Role of zinc in ttt of diarrhea Zinc treatment is a simple, inexpensive, and new tool for treating diarrheal episodes. This important micronutrient becomes depleted during diarrhea, but recent studies suggest that treatment with zinc with a 10 - to 14 -day course of treatment can reduce the duration and severity of diarrheal episodes. WHO recommend daily 20 mg zinc supplements for 10 days for children with acute diarrhea and 10 mg per day for infants under six months old.
Antidiarrheal and antiemetic Antimotility agents (Diphenoxylate, Loperamide) adsorbants(Charcoal, Kaolin) and antiemetics including Chlorpromazine and should NOT be used in the treatment of diarrhea in children less than 5 years of age as non of these drugs has any proved practical benefits and some may have serious side effects
Prevention • Safe drinking water and food • Hand washing • Proper sanitation • Vaccines

THANK YOU
 Cholecystitis pathogenesis
Cholecystitis pathogenesis Acute apical periodontitis clinical features
Acute apical periodontitis clinical features Optimental enteral formula
Optimental enteral formula Diarrhea chief complaint
Diarrhea chief complaint Eluxodoline
Eluxodoline Nicholas seeliger, md flpen panama city beach fl
Nicholas seeliger, md flpen panama city beach fl Travelers diarrhea
Travelers diarrhea Pig diarrhea chart
Pig diarrhea chart Liemyosarcoma
Liemyosarcoma Bile acid diarrhea
Bile acid diarrhea Dan laufenberg
Dan laufenberg Metformin and constipation
Metformin and constipation Dr ali azzam
Dr ali azzam Vpims lucknow
Vpims lucknow Secretory diarrhea pathophysiology
Secretory diarrhea pathophysiology Flora git
Flora git Overflow diarrhea
Overflow diarrhea Imnci definition
Imnci definition Diarrhea types
Diarrhea types Factitial diarrhea
Factitial diarrhea Diarrhea
Diarrhea Osmotic diarrhea meaning
Osmotic diarrhea meaning Foot crunchies map
Foot crunchies map Diarrhea introduction
Diarrhea introduction Hiv stool color
Hiv stool color Cholera
Cholera Laxative effect
Laxative effect Diarrhea
Diarrhea Diarrhea
Diarrhea Constant diarrhea
Constant diarrhea Radwan
Radwan Ent
Ent Chapter 10 - sentence check 2 answer key
Chapter 10 - sentence check 2 answer key Paradoxical bronchospasm
Paradoxical bronchospasm Mcv4ue
Mcv4ue Trigonometr
Trigonometr Malnutrition case presentation
Malnutrition case presentation Acute defintion
Acute defintion Periradicular disease classification
Periradicular disease classification Acute suppurative appendicitis
Acute suppurative appendicitis Acute pericarditis
Acute pericarditis Acute cholecystitis treatment
Acute cholecystitis treatment Acute rheumatic fever
Acute rheumatic fever Treatments for acute renal failure
Treatments for acute renal failure Acute mi
Acute mi Difference between megaloblastic and pernicious anemia
Difference between megaloblastic and pernicious anemia Morphological patterns of inflammation
Morphological patterns of inflammation Acute confusion related to
Acute confusion related to