Emergency Medical Responder First on Scene TENTH EDITION
















- Slides: 112

Emergency Medical Responder First on Scene TENTH EDITION CHAPTER 24 Caring for Infants and Children Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 1. Review the major stages of lifespan development for the pediatric patient (Chapter 4). 2. Define the following terms: a. b. c. d. Abuse Adolescent Croup Epiglottitis continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 2. Define the following terms: e. f. g. h. Febrile Infant Mandated reporter Neglect continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 2. Define the following terms: i. Pediatric Assessment Triangle (PAT) j. Retractions k. School age l. Shaken-baby syndrome m. Sudden Infant Death Syndrome (SIDS) n. Toddler o. Work of breathing continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 3. Explain various techniques that can be employed to maximize successful assessment of the pediatric patient. 4. Explain the components of the pediatric assessment triangle. 5. State the most common cause of cardiac arrest in the pediatric patient. 6. Describe the signs and symptoms of sudden infant death syndrome (SIDS). continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 7. Explain the appropriate steps for management of a suspected SIDS death. 8. Describe common signs and symptoms of abuse and neglect. 9. Explain the role of the Emergency Medical Responder in cases of suspected abuse and/or neglect. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 10. Explain the assessment and management of the following emergencies in pediatric patients: a. b. c. d. Upper airway obstruction Lower reactive airway disease Seizures Shock continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 11. Demonstrate the ability to properly assess and care for a pediatric patient. 12. Demonstrate various techniques that can be employed to maximize successful assessment of the pediatric patient. 13. Demonstrate the application of the pediatric assessment triangle. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 14. Demonstrate sensitivity for the feelings of the family while caring for an ill or injured pediatric patient. 15. Recognize the emotional impact that responding to pediatric patients can have on the Emergency Medical Responder. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Objectives 16. Value the role of the Emergency Medical Responder with respect to patient advocacy. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Media Directory Slide 22 EMS for Children Video Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Topics Caring for the Pediatric Patient Assessment of Infants and Children Managing Specific Medical Emergencies Managing Trauma Emergencies Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
CARING FOR THE PEDIATRIC PATIENT Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
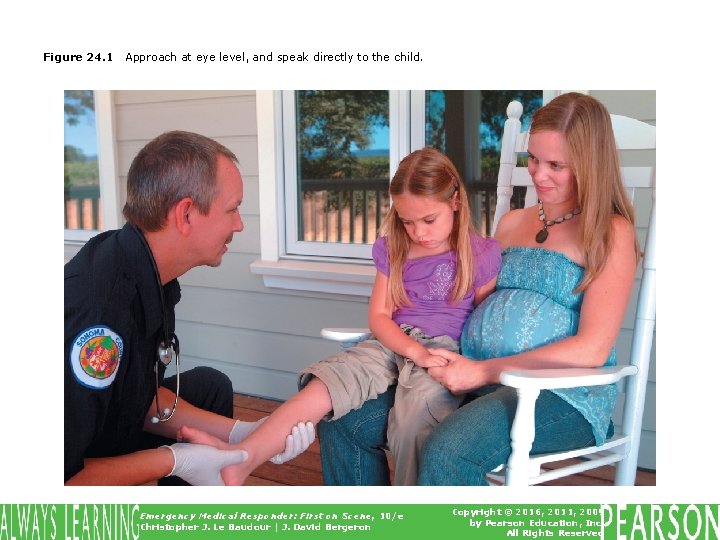
Caring for the Pediatric Patient • Characteristics of Infants and Children Approach them slowly. Establish eye contact. Ask permission to get closer. Let them know someone will call their parents. § Get down at eye level with child. § Let them see your face and expressions. § Speak directly to them. § § Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
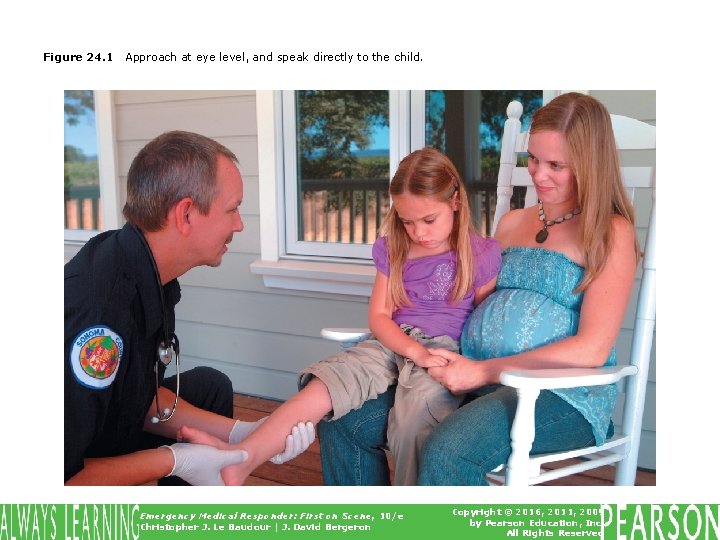
Figure 24. 1 Approach at eye level, and speak directly to the child. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Characteristics of Infants and Children § Pause to find out if child understands what you have said or asked. § Quickly determine and manage any lifethreatening problems. § Perform a toe-to-head assessment. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Characteristics of Infants and Children § Always tell children what you are going to do before each step of assessment. § Never lie to children. § Offer comfort by stroking their foreheads or holding their hands. § Do not direct all of your conversation to parents. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Characteristics of Infants and Children § Work with reactions of parents or primary caregivers. § Ask anxious caregivers to help you with tasks. § Parents will know how to manage any special pediatric medical equipment. § Help keep the parents calm. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Developmental Categories § Infants • Babies from birth to one year old § Toddlers • Child from one to three years old § Preschool • Child from three to six years old continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Developmental Categories § School age • Child between the ages of 6 and 12 years § Adolescent • Child between the ages of 12 and 18 years old Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Special Considerations § Child's head is proportionately larger and heavier than body. • Prone to head injuries § Handle head of newborn with caution because of fontanels (soft spots). • Sunken fontanel may indicate dehydration. • Bulging fontanel may indicate increased pressure in the skull. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
EMS for Children Video Click on the screenshot to view a video on the topic of emergency services for children. Back to Directory Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
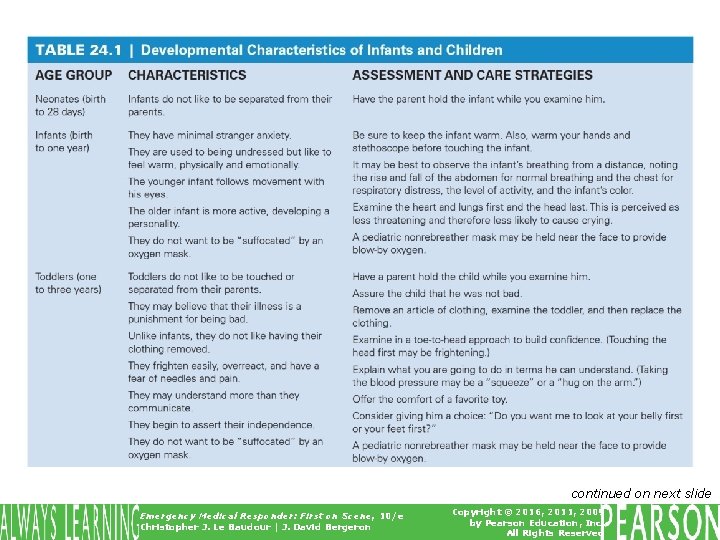
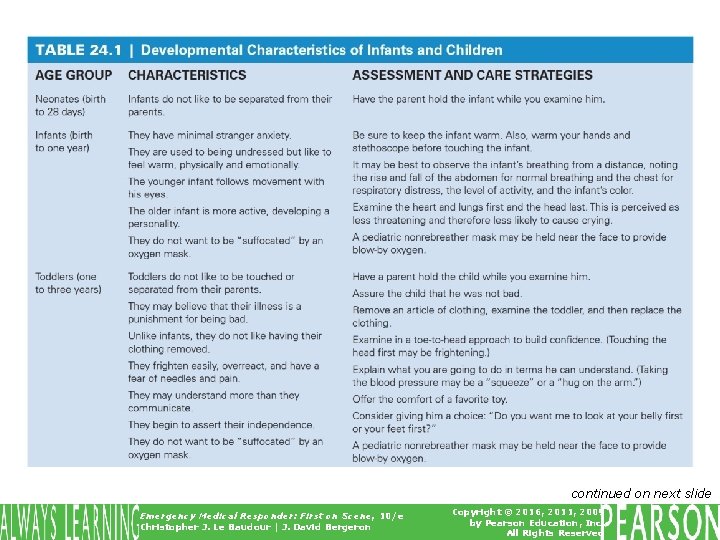
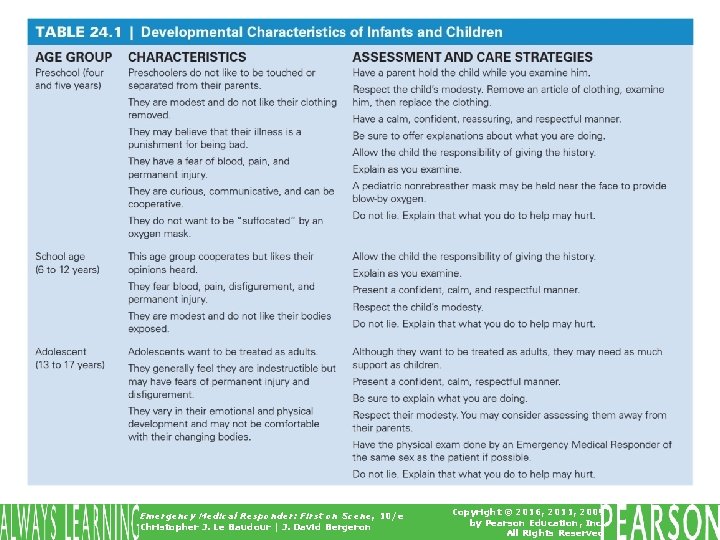
Table 24. 1 Developmental Characteristics of Infants and Children continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
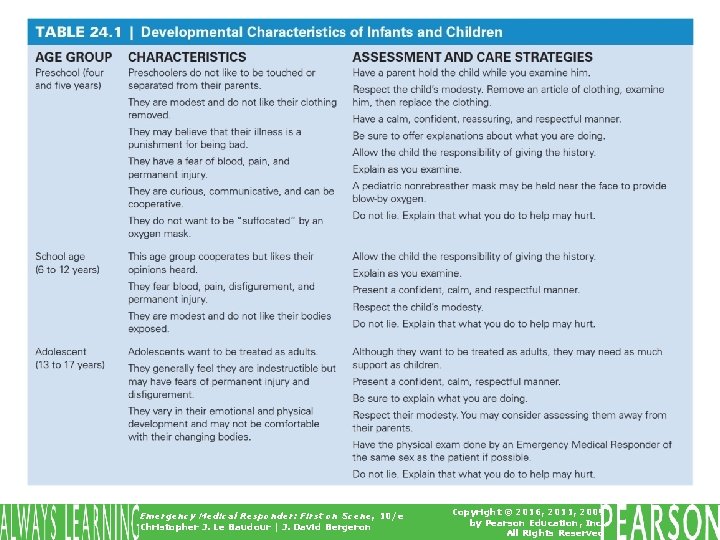
Table 24. 1 (continued) Developmental Characteristics of Infants and Children Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Special Considerations § Airway and respiratory systems of infant and child are not fully developed. § Infants are primarily nose breathers. § Overextending child's neck during airway management can cause trachea to collapse and obstruct airway. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
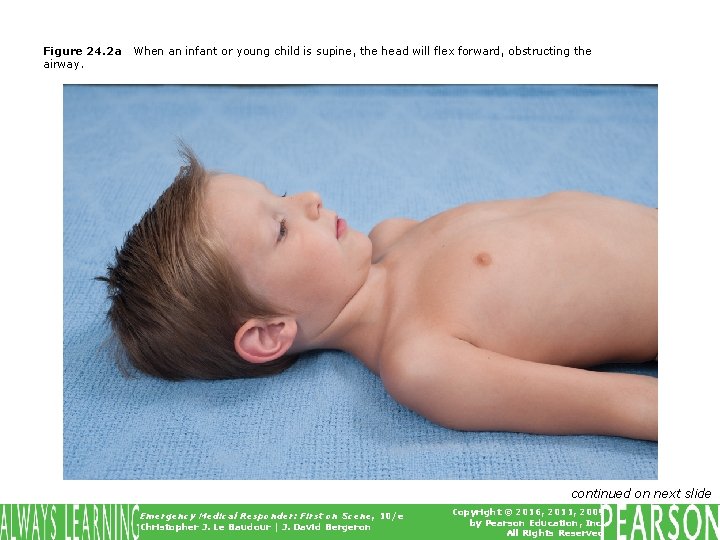
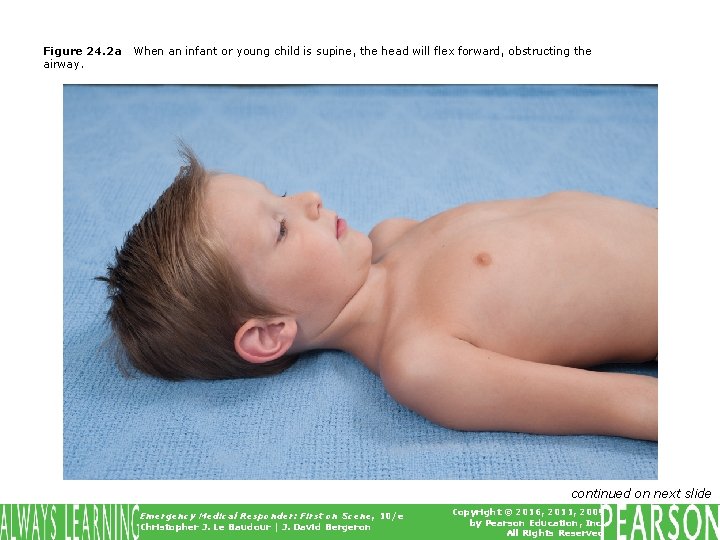
Figure 24. 2 a airway. When an infant or young child is supine, the head will flex forward, obstructing the continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
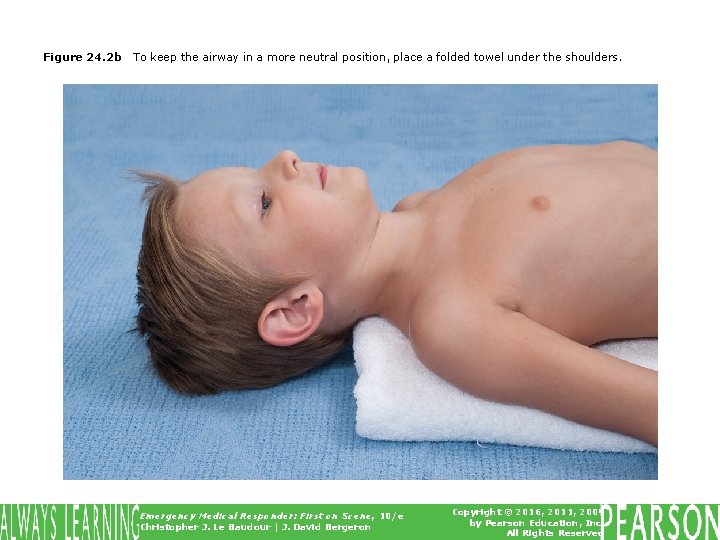
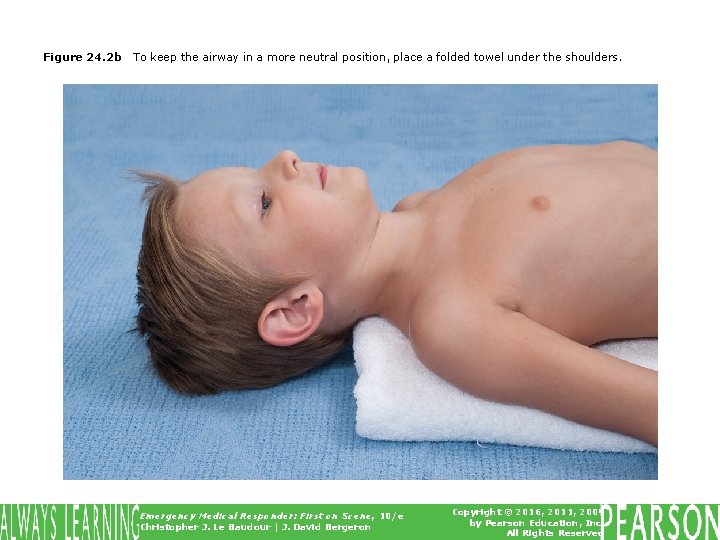
Figure 24. 2 b To keep the airway in a more neutral position, place a folded towel under the shoulders. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Caring for the Pediatric Patient • Special Considerations § Chest is more elastic. • Obvious chest movement with labored or distressed breathing • Look for loss of symmetry. • Unequal chest movement with breathing • Bruising over chest continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Caring for the Pediatric Patient • Special Considerations § Abdominal organs (liver and spleen) are large for size of cavity and more susceptible to injury. § Trauma to the pelvic girdle can result in large amounts of blood lost into the pelvic cavity. § Assess circulation, sensation, and motor function in distal extremities. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Caring for the Pediatric Patient • Special Considerations § Bones are less developed and more flexible. • Growth plate is developing tissue and weakest area of growing bone. § Infants and children have large amount of total surface area (skin) in proportion to total body mass. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
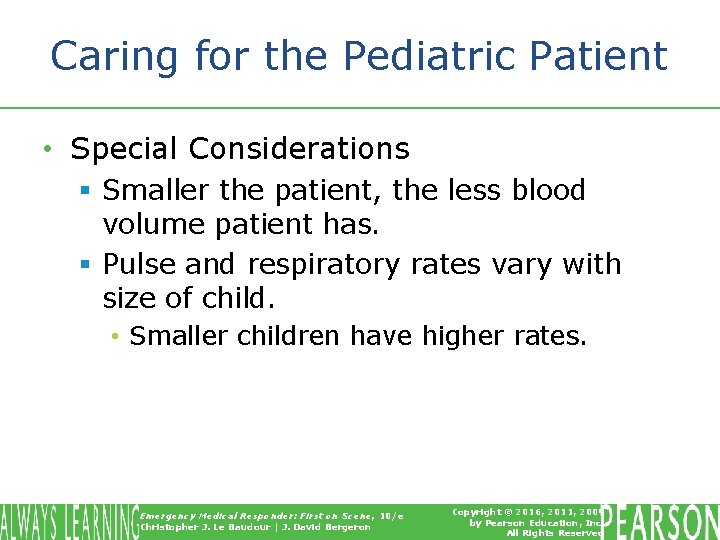
Caring for the Pediatric Patient • Special Considerations § Smaller the patient, the less blood volume patient has. § Pulse and respiratory rates vary with size of child. • Smaller children have higher rates. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
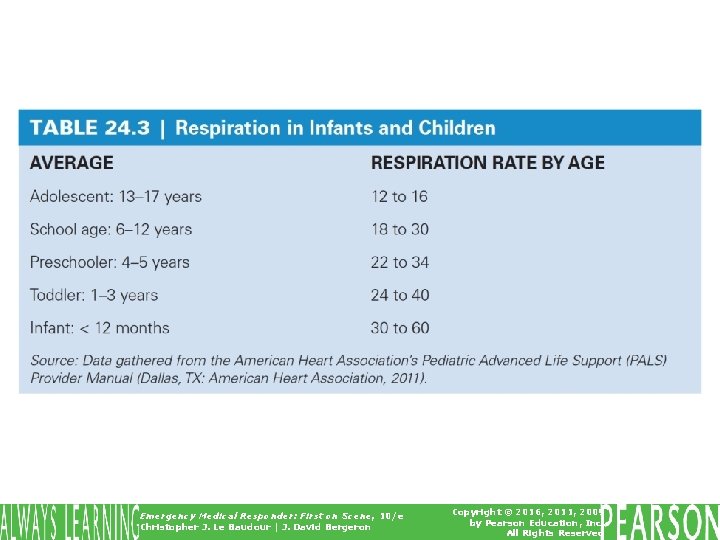
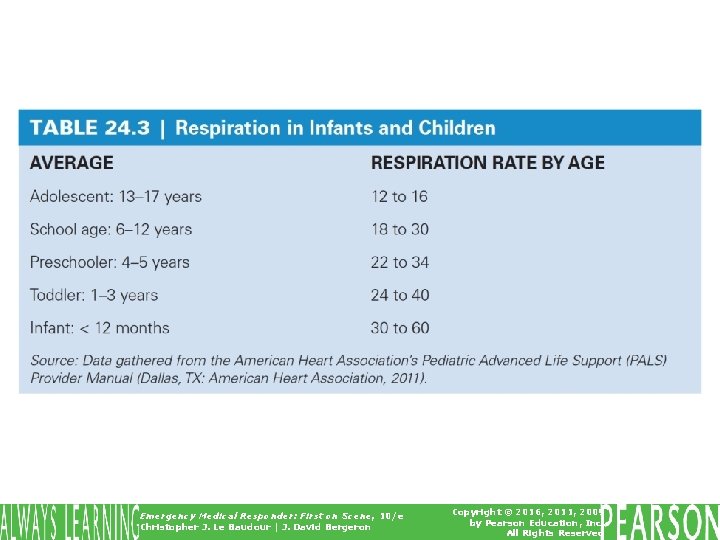
Table 24. 3 Respiration in Infants and Children Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Caring for the Pediatric Patient • Special Considerations § Blood pressure varies in children and depends on sex, age, and height. • • Time of day Physical activity Emotional moods or feelings Physical condition § Use appropriate size cuff. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Think About It • You respond to the home of a 9 -monthold female who began choking on a small toy and now cannot breathe. • How will you proceed? • While attempting to dislodge the obstruction, the baby becomes unresponsive. • What do you do next? Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

ASSESSMENT OF INFANTS AND CHILDREN Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Assessment of Infants and Children • Scene Size-up § Approach slowly so you do not frighten child. § Determine scene safety. § Determine number of patients involved. § Determine MOI or NOI. § Don PPE. § Call immediately if additional resources needed. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
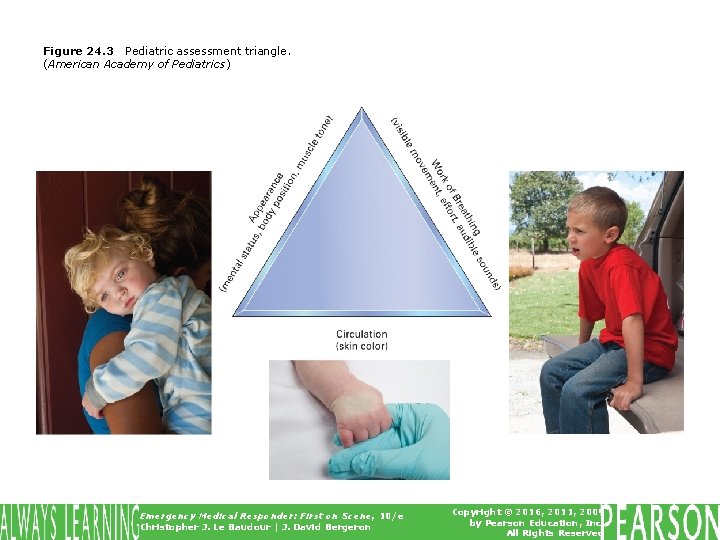
Assessment of Infants and Children • Primary Assessment § In children, general impression is important indicator of severity of illness. § Pediatric assessment triangle (PAT) • Tool used to determine general impression of pediatric patient • Appearance • Work of breathing • Circulation (perfusion) Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
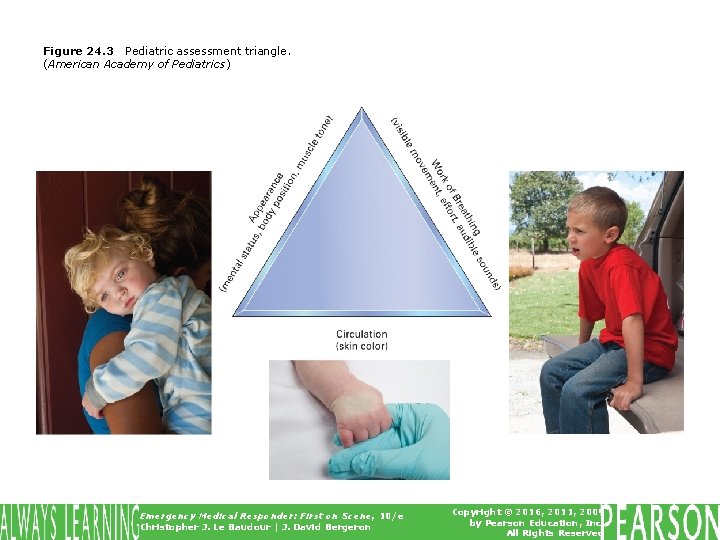
Figure 24. 3 Pediatric assessment triangle. (American Academy of Pediatrics) Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Assessment of Infants and Children • Primary Assessment § High priority infant or child Poor general impression Altered mental status Airway problem Respiratory distress or inadequate breathing • Developing shock • • continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
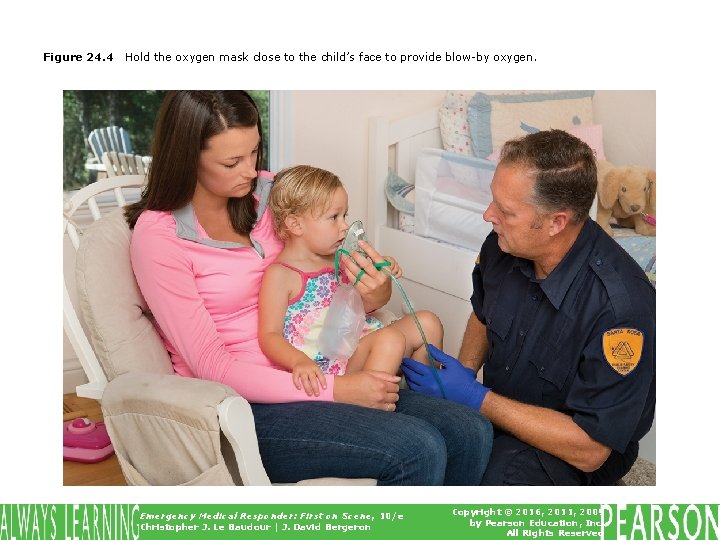
Assessment of Infants and Children • Primary Assessment § Airway first concern in care of any patient. § Infant's tongue can easily obstruct airway. § Do not perform blind finger sweeps. § Provide oxygen to children by using blow-by technique per local protocols. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
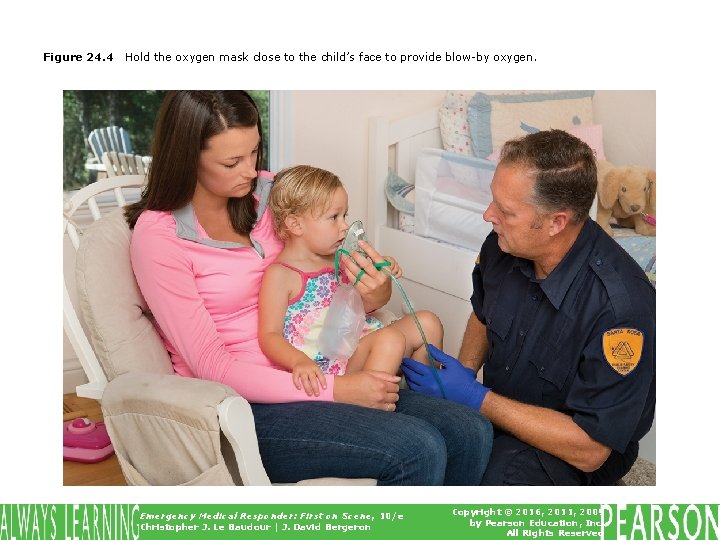
Figure 24. 4 Hold the oxygen mask close to the child’s face to provide blow-by oxygen. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Assessment of Infants and Children • Secondary Assessment § Focus on getting history and conducting physical exam. § For child who is seriously injured or sick, perform a rapid assessment. • Patient with significant MOI • Unresponsive patient continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Assessment of Infants and Children • Secondary Assessment § Child responding or acting normally. • Trauma patient with no significant MOI • Responsive medical patient § Physical exam similar to adult except, for frightened or crying infant or young child, perform in reverse order (toe to head). Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Assessment of Infants and Children • Reassessment § Status of child can change rapidly and frequently. § Reassess mental status, maintain airway, monitor breathing, check pulse, and reevaluate skin color, temperature, and condition. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Assessment of Infants and Children • Reassessment § Reassess vital signs • Every 5 minutes for unstable patients • Every 15 minutes for stable patients Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Think About It • You respond to an apartment to find a 7 -year-old female supine on a sofa. Her mother reports that she has been complaining of a sore throat for several days. She appears lethargic, her respirations are shallow, and her skin is very hot and flushed, even after taking a fever reducer. • How will you proceed? Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

MANAGING SPECIFIC MEDICAL EMERGENCIES Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Respiratory Emergencies § Most common cause of cardiac arrest in infants and children is respiratory arrest. § Review Chapter 8 for signs and symptoms and management of partial and complete airway obstruction for pediatric patients. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Respiratory Emergencies § Difficulty breathing • • Simple cold Respiratory infection Apnea Sleep apnea • SIDS continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Respiratory Emergencies § Croup • Acute respiratory condition common in infants and children • Barking type of cough or stridor § Epiglottitis • Swelling of epiglottis caused by bacterial infection • May cause airway obstruction Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
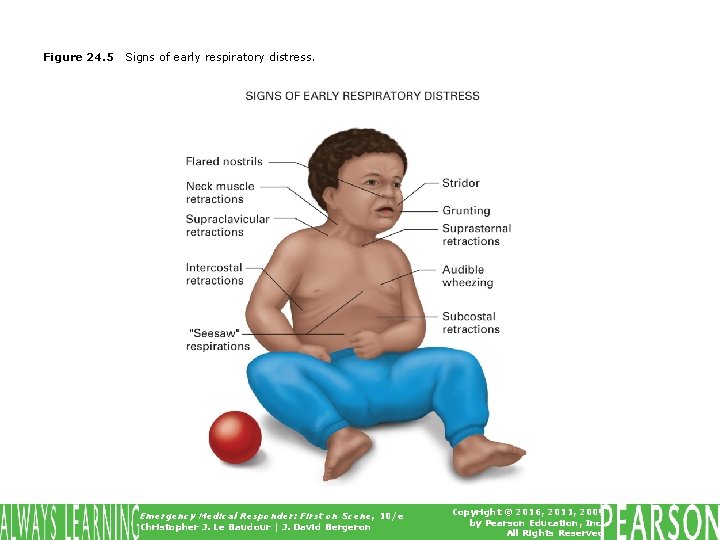
Managing Specific Medical Emergencies • Respiratory Distress Signs/Symptoms § Wheezing or high-pitched harsh noise, or grunting § Exhaling with abnormal effort § Abnormal or inadequate breathing patterns continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Managing Specific Medical Emergencies • Respiratory Distress Signs/Symptoms § § Use of accessory muscles to breathe Tripod position Drooling Nasal flaring continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Respiratory Distress Signs/Symptoms § Late Signs/Symptoms • • Cyanosis Capillary refill of more than two seconds Slow heart rate Altered mental status Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
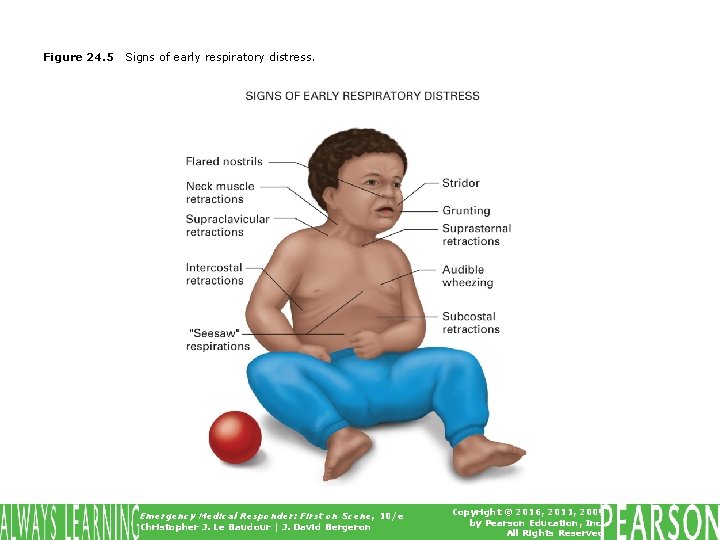
Figure 24. 5 Signs of early respiratory distress. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
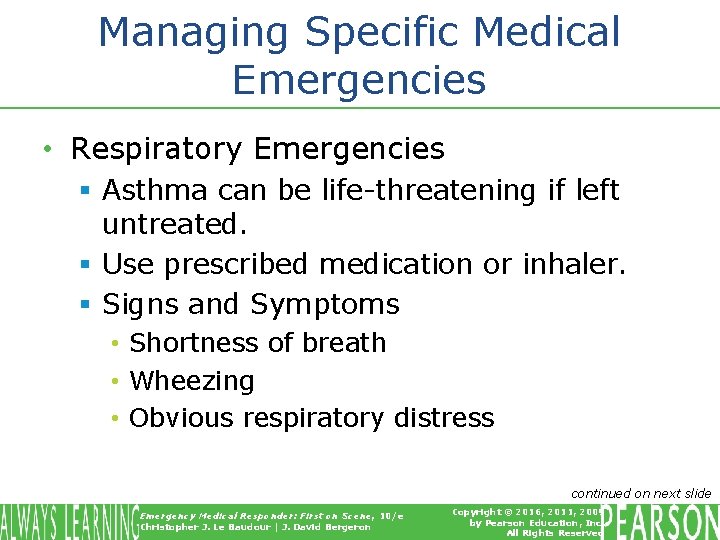
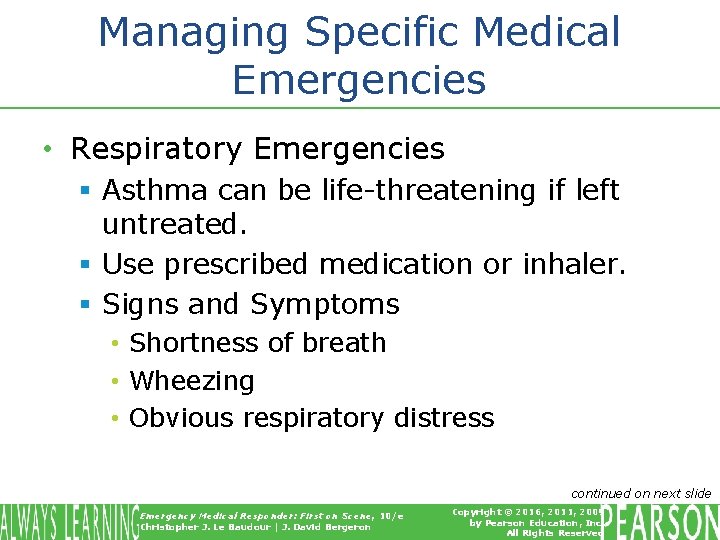
Managing Specific Medical Emergencies • Respiratory Emergencies § Asthma can be life-threatening if left untreated. § Use prescribed medication or inhaler. § Signs and Symptoms • Shortness of breath • Wheezing • Obvious respiratory distress continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Managing Specific Medical Emergencies • Respiratory Emergencies § Asthma Signs and Symptoms • • • Cough Faster than normal breathing rate Increased heart rate Sleepiness or slowed response Cyanosis continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
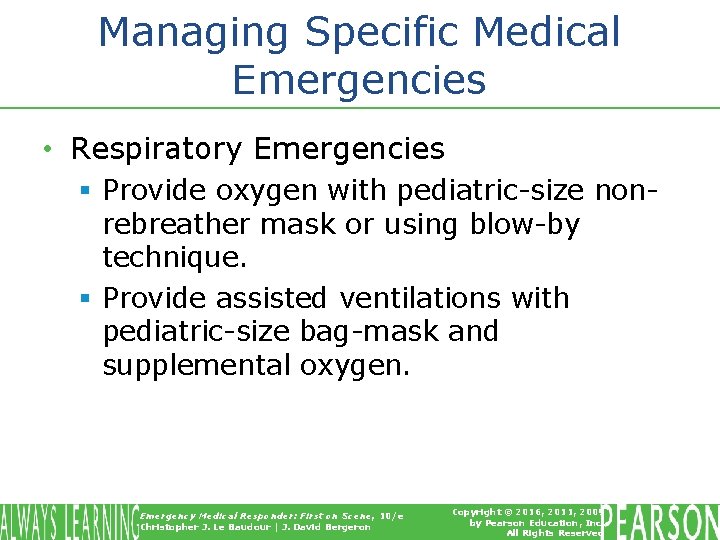
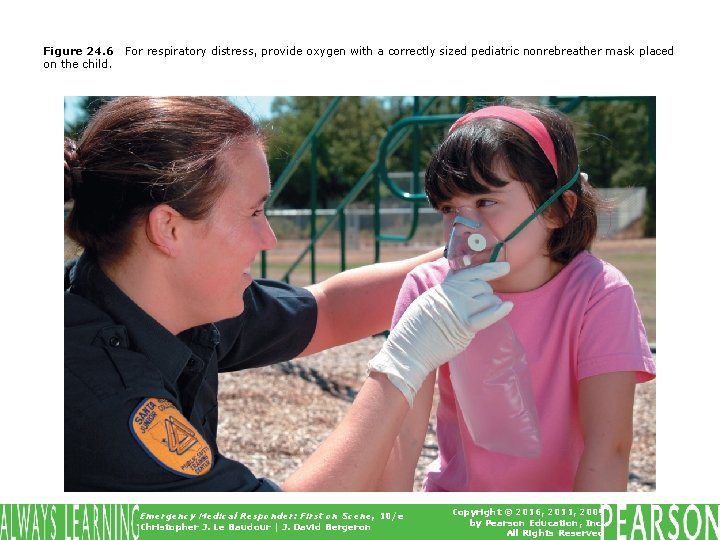
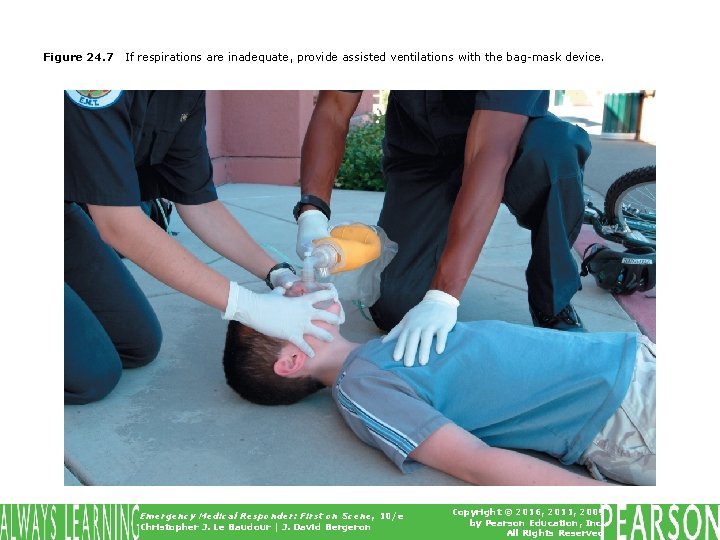
Managing Specific Medical Emergencies • Respiratory Emergencies § Provide oxygen with pediatric-size nonrebreather mask or using blow-by technique. § Provide assisted ventilations with pediatric-size bag-mask and supplemental oxygen. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
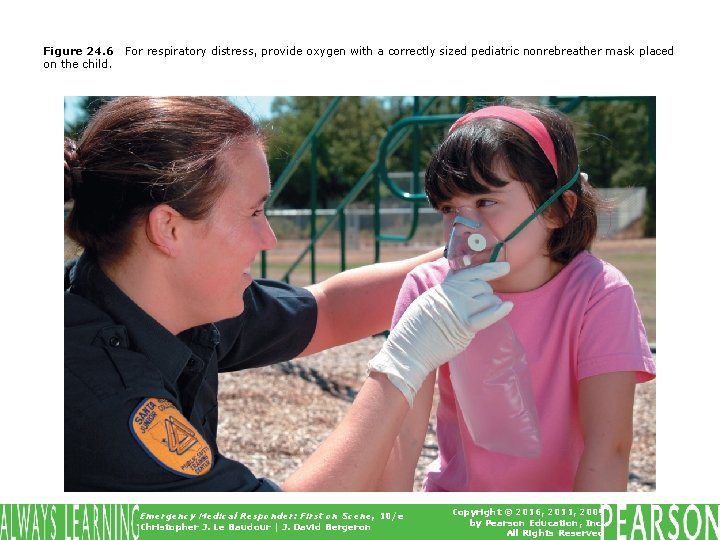
Figure 24. 6 on the child. For respiratory distress, provide oxygen with a correctly sized pediatric nonrebreather mask placed Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
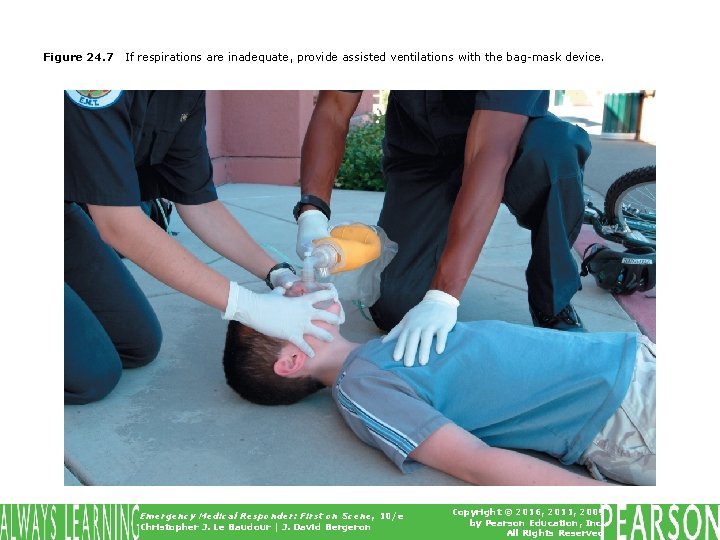
Figure 24. 7 If respirations are inadequate, provide assisted ventilations with the bag-mask device. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
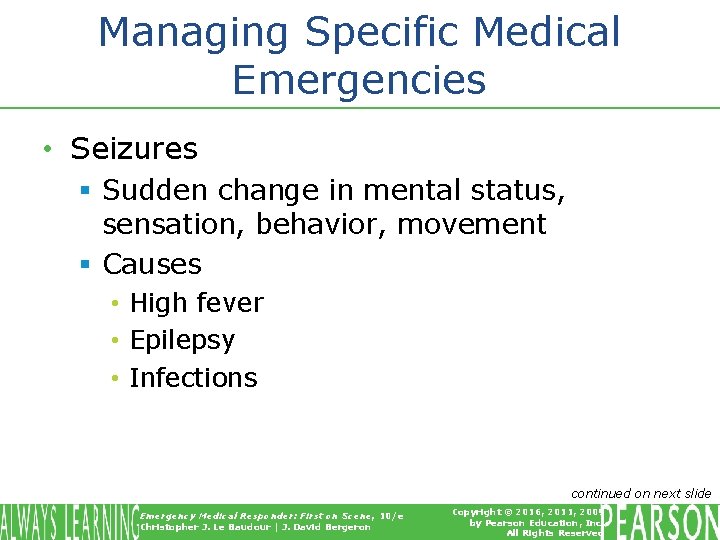
Managing Specific Medical Emergencies • Seizures § Sudden change in mental status, sensation, behavior, movement § Causes • High fever • Epilepsy • Infections continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Managing Specific Medical Emergencies • Seizures § Causes • Poisoning • Low blood sugar (hypoglycemia) • Head injury continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Seizures § Febrile seizures caused by fever should be taken seriously. § After seizure, normal for child to be either lethargic and difficult to arouse or agitated and combative. § Any child who has had a seizure must have a medical evaluation. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Altered Mental Status § § § § Low blood sugar (hypoglycemia) Poisoning Infection Head injury Decreased oxygen levels Shock Seizures Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Managing Specific Medical Emergencies • Shock § § § Dehydration from diarrhea and vomiting Blood loss Allergic reactions Poisoning Shock from fluid loss occurs quickly in infants and is a serious emergency. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Shock § Decompensated shock • Body's compensating mechanisms suddenly fail. • Rapid heart and respiratory rate • Weak or absent pulse • Delayed capillary refill • Decreased urine output Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Fever § Body's normal response to many childhood diseases and infections is high temperature or fever. § Additional causes • Heat exposure • Noninfectious disease • Childhood immunization shots continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Fever § Child with high fever will be flushed (red) and dry. § Potentially emergent situations • • Fever with rash Long bouts of diarrhea and vomiting Inadequate intake of fluids Sudden spike in temperature with or without seizure Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Hypothermia § Children lose body heat through their heads. § Children cannot conserve heat well. • Unable to regulate temperatures as well as adult bodies can • Can become chilled through environment, injury, or illness Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Diarrhea and Vomiting § Dehydration • Loss of large amounts of necessary body fluids through prolonged vomiting and diarrhea or decreased intake • Infants more susceptible to dehydration than adults continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Diarrhea and Vomiting § Dehydration • Balance of fluids-in to fluids-out needed to maintain muscle and organ function • Shock can result when large amounts of fluids are lost. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Poisoning § Potentially life-threatening condition that can affect any or all of body's systems § Drowning • Child submerged in water may still be alive or clinically dead (no breathing and no heartbeat) but not biologically dead (brain cells still alive). Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Specific Medical Emergencies • Sudden Infant Death Syndrome (SIDS) § Sudden unexplained death of apparently healthy baby during sleep § Most common first year of life but can occur in children as old as two years § Causes and theories still being investigated § Start emergency care as you would for any patient in cardiac arrest. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Think About It • You are treating an infant in respiratory distress. You notice that his respiratory rate begins to slow and that his pulse drops from 180 to 60 beats per minute. • What do these changes in vital signs indicate? • How will you proceed? Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
MANAGING TRAUMA EMERGENCIES Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
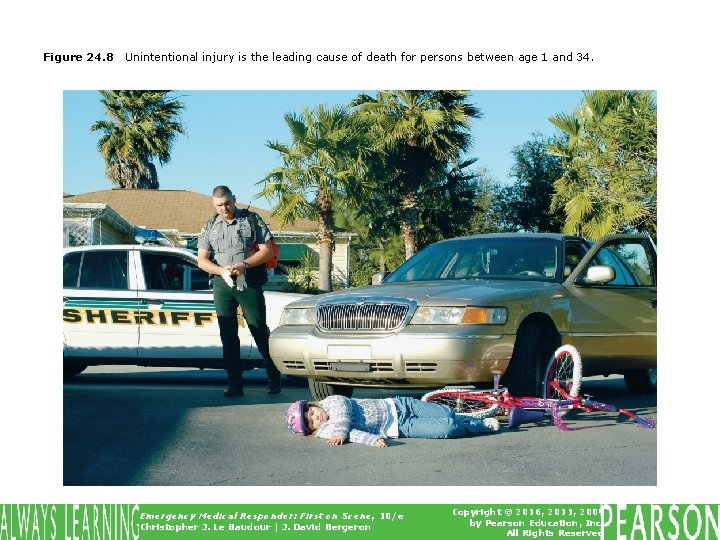
Managing Trauma Emergencies • Trauma number one cause of death in people 1 to 18 years of age § § Motor-vehicle crashes Drowning Burns Firearms continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Trauma Emergencies • Trauma number one cause of death in people 1 to 18 years of age § § Falls Abuse Entrapment Crushing Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
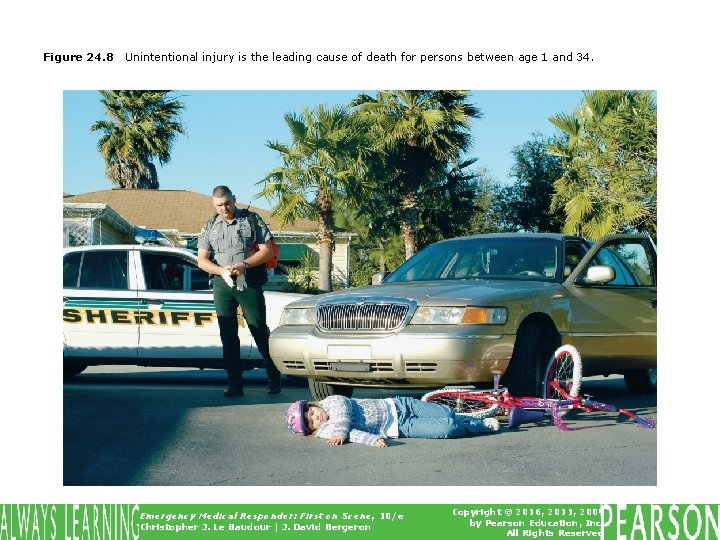
Figure 24. 8 Unintentional injury is the leading cause of death for persons between age 1 and 34. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
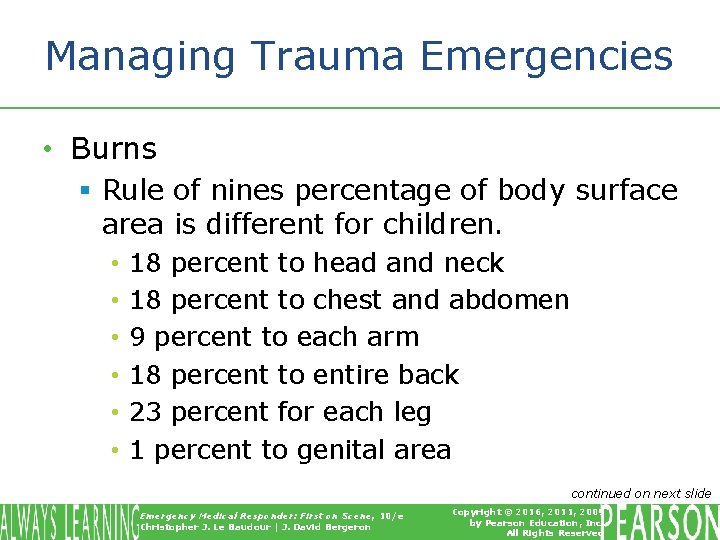
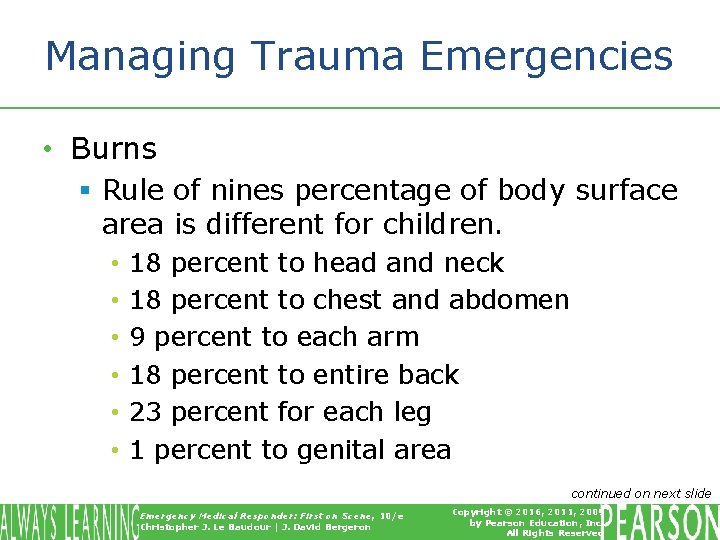
Managing Trauma Emergencies • Burns § Rule of nines percentage of body surface area is different for children. • • • 18 percent to head and neck 18 percent to chest and abdomen 9 percent to each arm 18 percent to entire back 23 percent for each leg 1 percent to genital area continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Managing Trauma Emergencies • Burns § Carefully and quickly care for burned area with dry, sterile, nonadherent dressings or sheets. § Follow local protocols. § Burns are excruciatingly painful. § Children are likely to be frantic. § Rapid transport is important. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
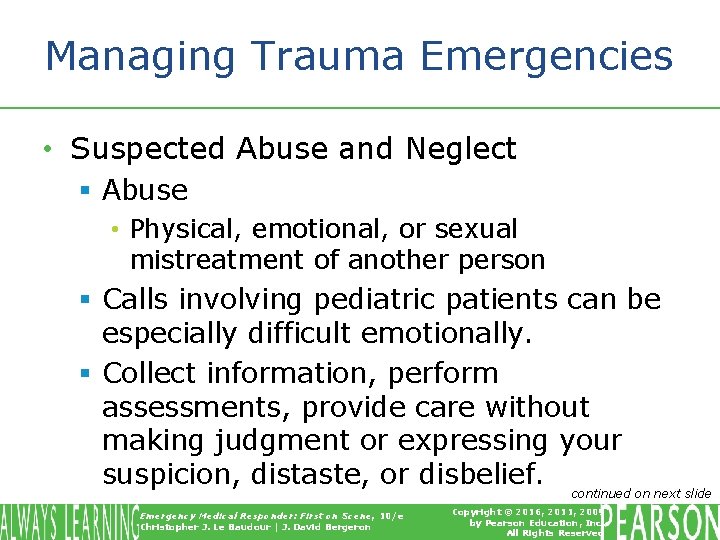
Managing Trauma Emergencies • Suspected Abuse and Neglect § Abuse • Physical, emotional, or sexual mistreatment of another person § Calls involving pediatric patients can be especially difficult emotionally. § Collect information, perform assessments, provide care without making judgment or expressing your suspicion, distaste, or disbelief. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Trauma Emergencies • Suspected Abuse and Neglect § Report concerns and impressions to ambulance personnel, medical direction, social services, health department, or law enforcement per local protocols. § Mandated reporters are those designated by law to report cases of suspected abuse or neglect. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Managing Trauma Emergencies • Suspected Abuse and Neglect § Psychological abuse • Emotional or verbal abuse that seriously affects child's positive emotional development, well-being, and selfesteem continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Trauma Emergencies • Suspected Abuse and Neglect § Neglect • Failure of parents/caregivers to adequately provide for person's basic physical, social, emotional, and medical needs continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Trauma Emergencies • Suspected Abuse and Neglect § Sexual abuse • Physical sexual contact or exposure and sexual exploitation by displaying or photographing children for sexual purposes or with sexual intent • Do not expect abuser to admit sexual abuse is reason for call. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Trauma Emergencies • Suspected Abuse and Neglect § Physical abuse • Any form of violent, harmful contact with a child or any disfiguring act performed on child • Child's relationship with parents or parent's attitude toward child or situation may be clue to abuse. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
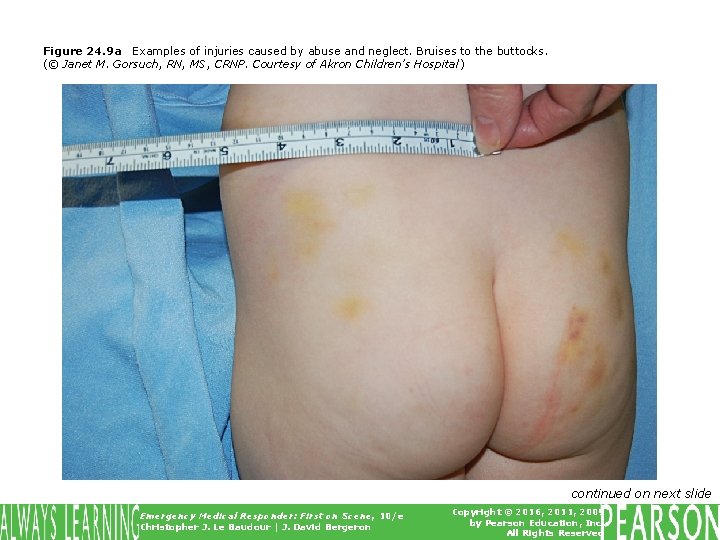
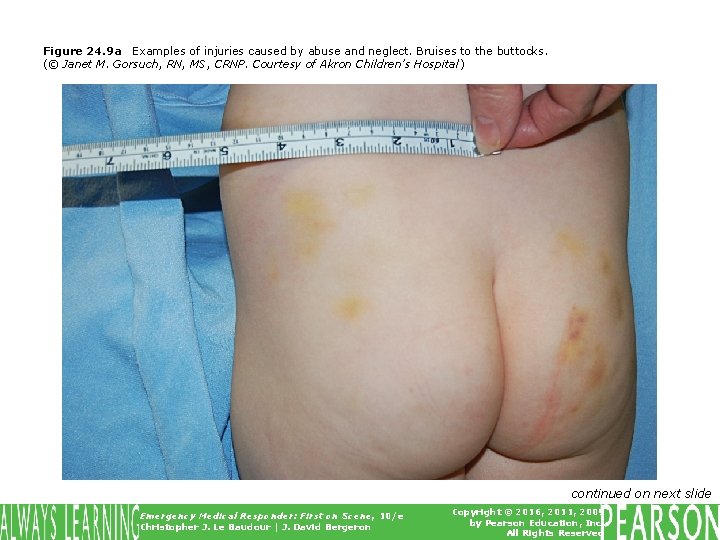
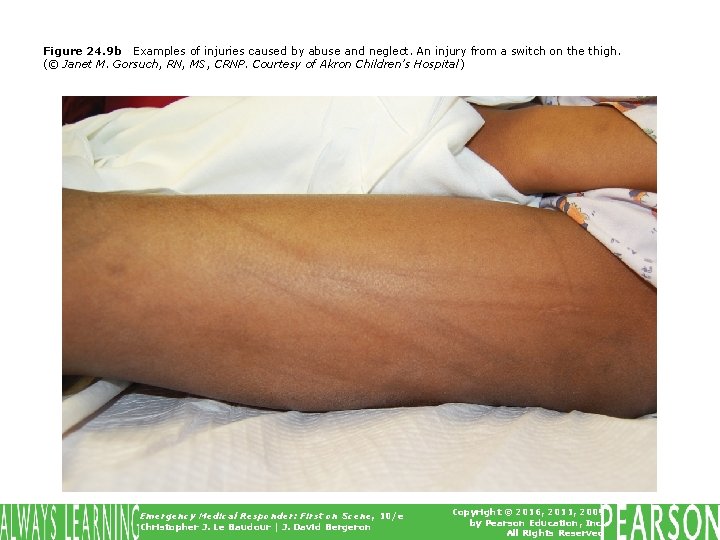
Figure 24. 9 a Examples of injuries caused by abuse and neglect. Bruises to the buttocks. (© Janet M. Gorsuch, RN, MS, CRNP. Courtesy of Akron Children’s Hospital) continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
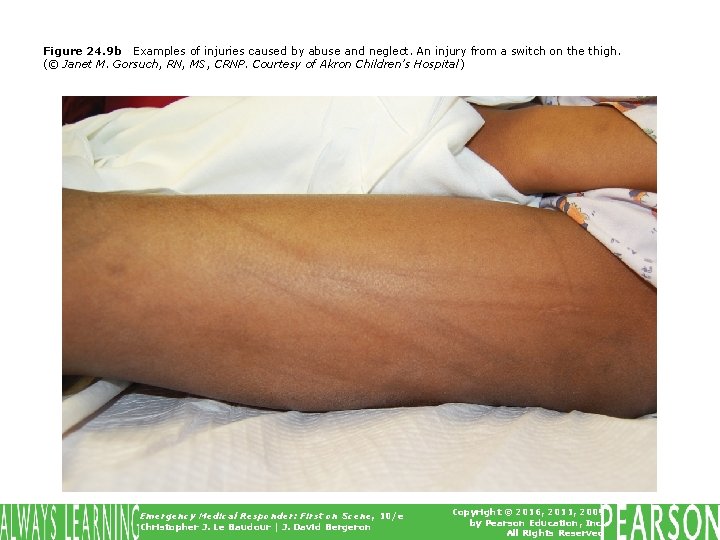
Figure 24. 9 b Examples of injuries caused by abuse and neglect. An injury from a switch on the thigh. (© Janet M. Gorsuch, RN, MS, CRNP. Courtesy of Akron Children’s Hospital) Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Trauma Emergencies • Suspected Abuse and Neglect § Shaken-baby syndrome • Abuser violently shakes infant or small child, creating whiplash-type motion that causes acceleration-deceleration injuries. • It is a serious emergency. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Managing Trauma Emergencies • Safety Seats § Many safety seats are not installed correctly. § Children are often not secured properly by safety straps/harnesses. § Any vehicle crash should lead you to suspect child has been injured. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

24. 1. 1 Rescuer 1 stabilizes car seat in upright position and applies manual head/neck stabilization. Rescuer 2 prepares equipment then loosens or cuts the seat straps and raises the front guard. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
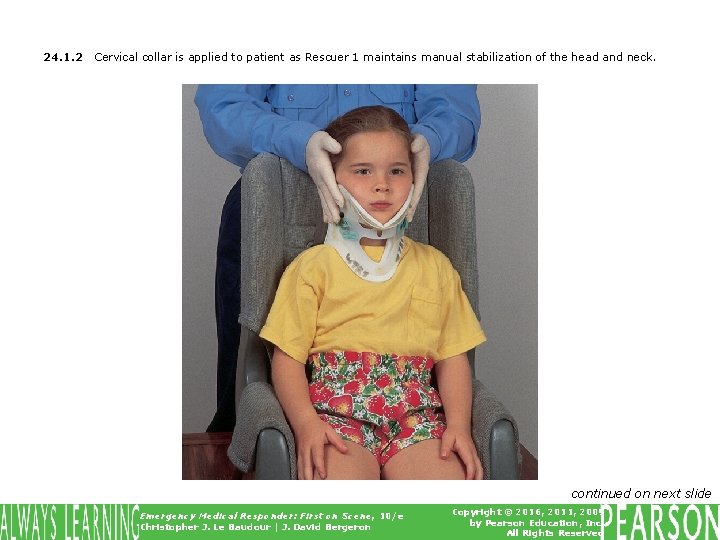
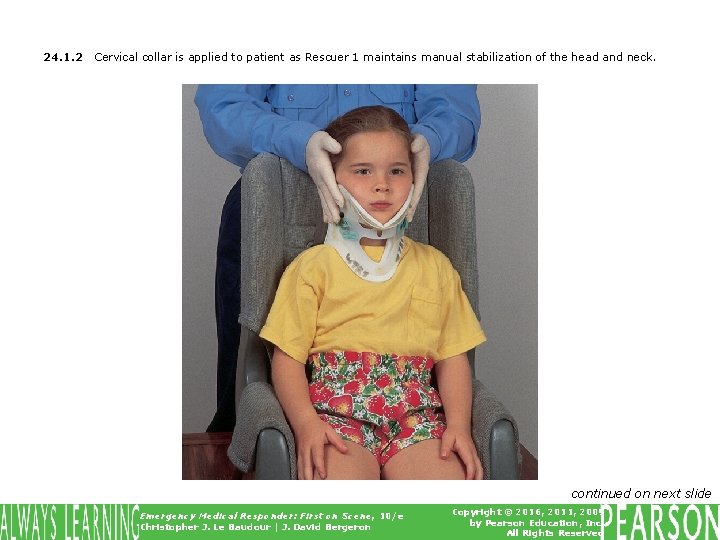
24. 1. 2 Cervical collar is applied to patient as Rescuer 1 maintains manual stabilization of the head and neck. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
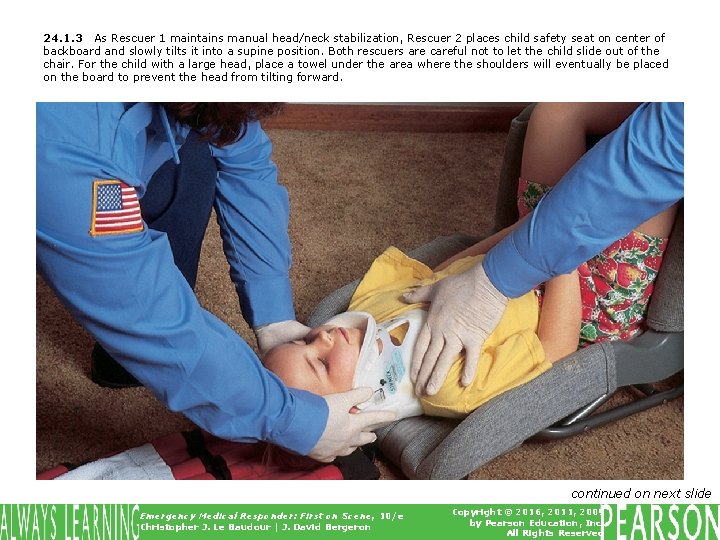
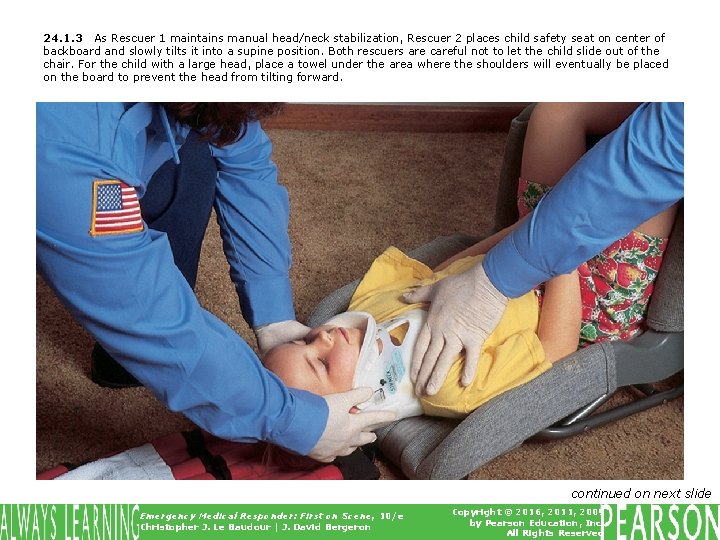
24. 1. 3 As Rescuer 1 maintains manual head/neck stabilization, Rescuer 2 places child safety seat on center of backboard and slowly tilts it into a supine position. Both rescuers are careful not to let the child slide out of the chair. For the child with a large head, place a towel under the area where the shoulders will eventually be placed on the board to prevent the head from tilting forward. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
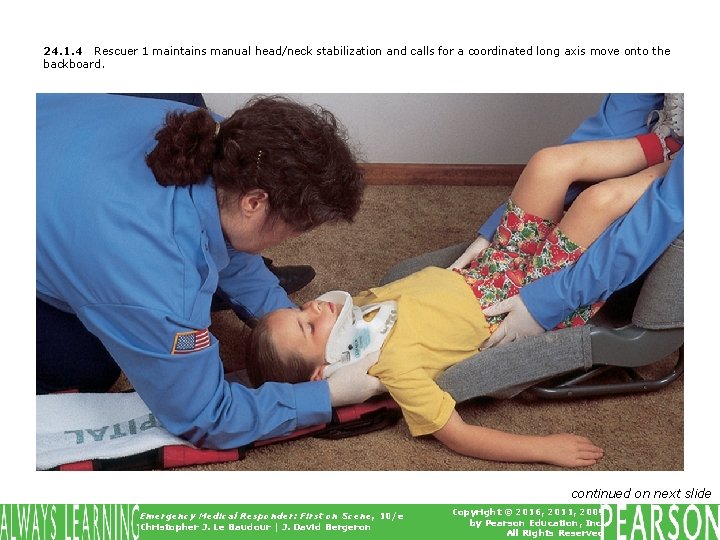
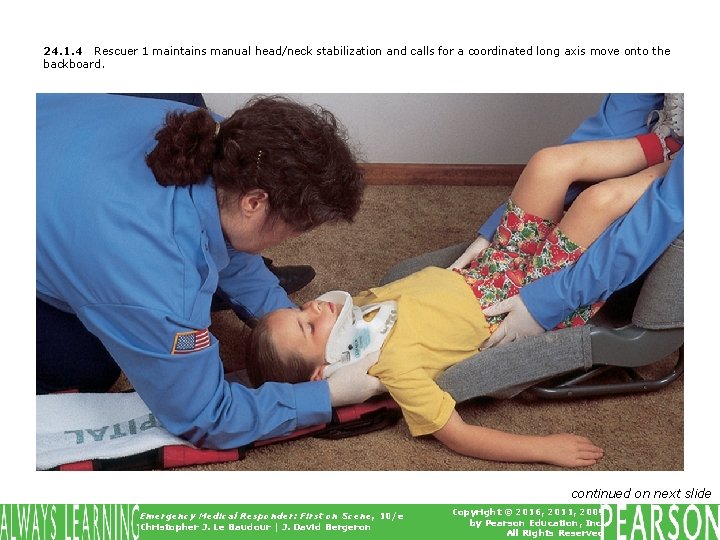
24. 1. 4 Rescuer 1 maintains manual head/neck stabilization and calls for a coordinated long axis move onto the backboard. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
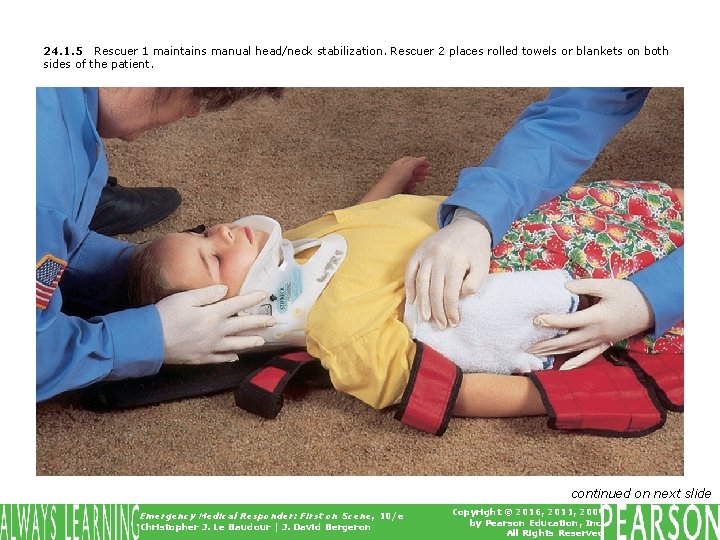
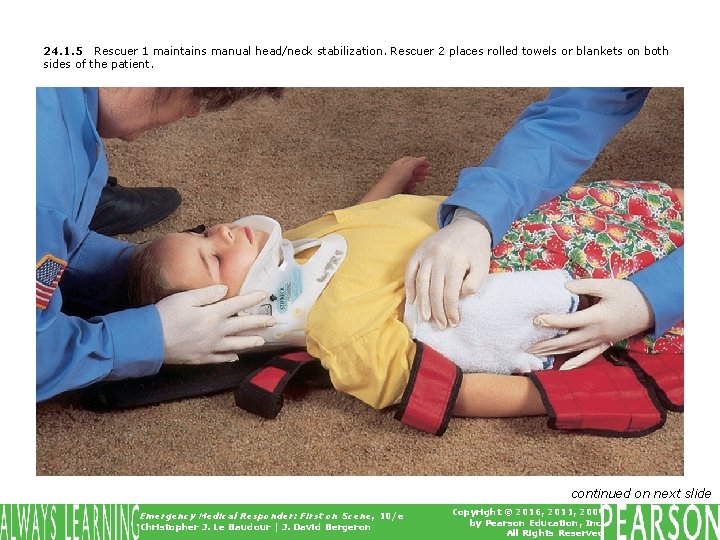
24. 1. 5 Rescuer 1 maintains manual head/neck stabilization. Rescuer 2 places rolled towels or blankets on both sides of the patient. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
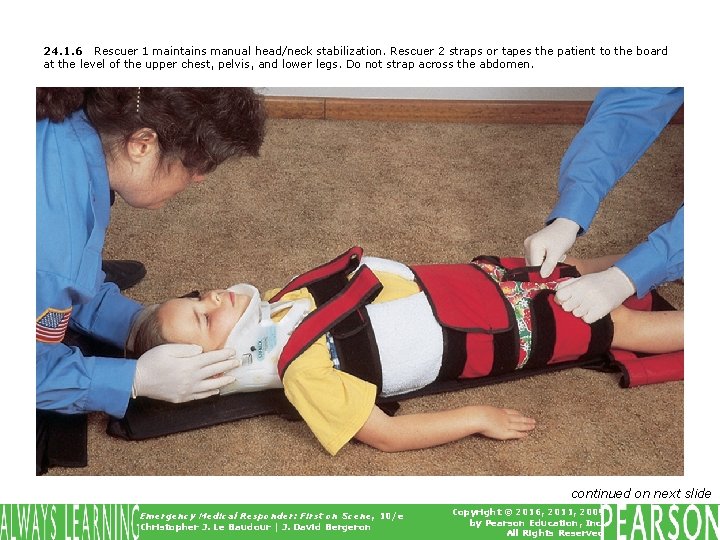
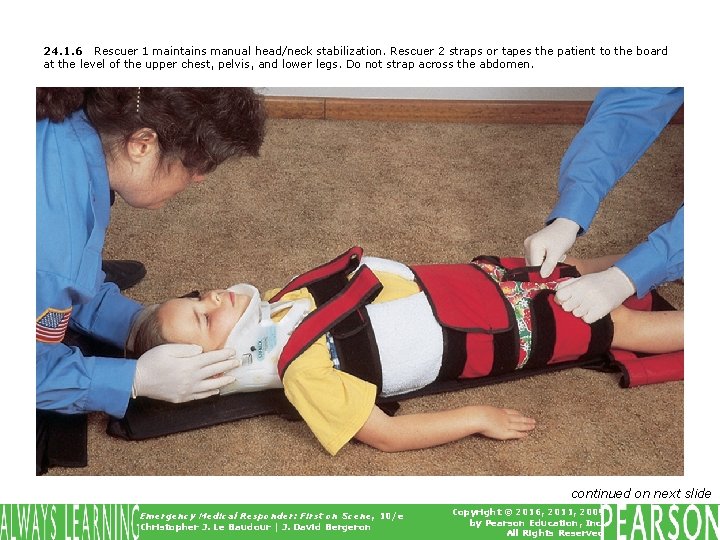
24. 1. 6 Rescuer 1 maintains manual head/neck stabilization. Rescuer 2 straps or tapes the patient to the board at the level of the upper chest, pelvis, and lower legs. Do not strap across the abdomen. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
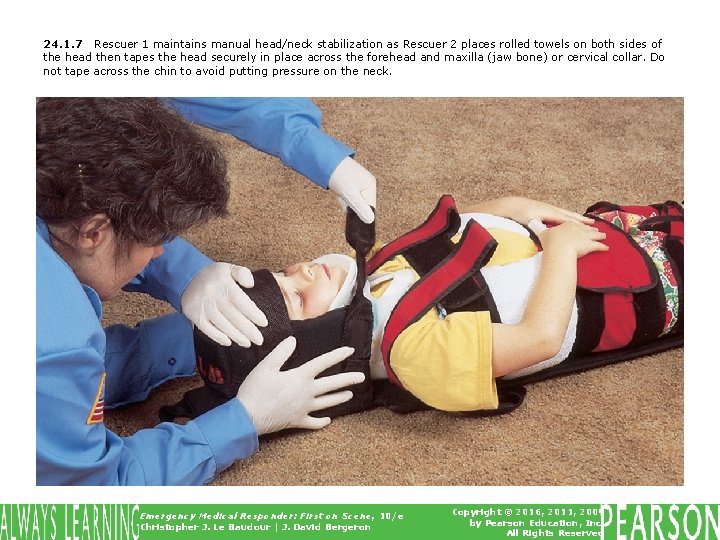
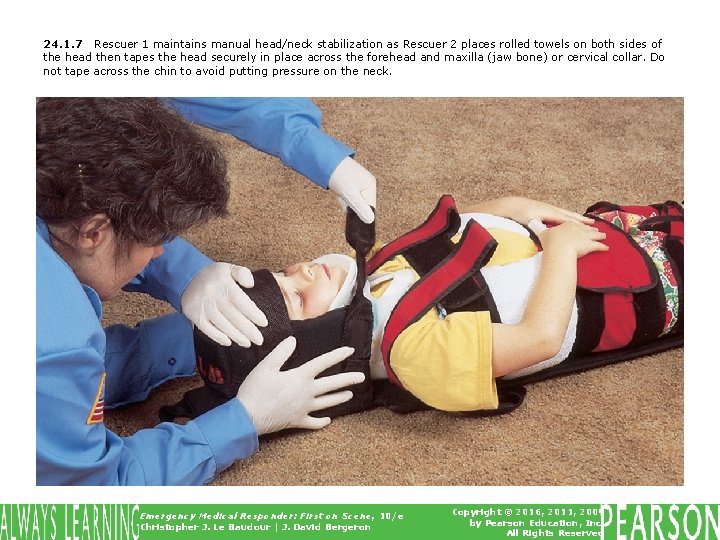
24. 1. 7 Rescuer 1 maintains manual head/neck stabilization as Rescuer 2 places rolled towels on both sides of the head then tapes the head securely in place across the forehead and maxilla (jaw bone) or cervical collar. Do not tape across the chin to avoid putting pressure on the neck. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Think About It • You respond to a 3 -year-old male who has been struck by a car. He is lying prone, crying, but not moving. • Why might his injuries be more extensive than those of a 30 -year-old who was hit by the same car? • How will you proceed? Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

SUMMARY Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • Assessment and emergency care of infants and children is same as adults. • Consider special characteristics of pediatric patient's anatomy, physiology, and emotional responses. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • Infants breathe through the nose. § If obstructed, they may not immediately open their mouths to breathe. • Be sure to clear nostrils of secretions. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • When managing airway of infant, make sure large head is in neutral position, neither hyperflexed nor hyperextended. • Place folded towel under infant's or child's shoulders to maintain spine and airway in neutral alignment. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • Care for respiratory distress in infants and children immediately. • For respiratory distress, provide oxygen with pediatric-size nonrebreather mask or by using blow-by technique. • Follow local protocols. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • For severe distress and respiratory arrest, provide assisted ventilations with appropriate device (pocket face mask or pediatric bag-mask device and supplemental oxygen). continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved

Summary • Children tolerate high fevers better than adults. § Fever that rises rapidly can cause seizures. § Arrange to transport feverish child. § Arrange to transport child who is vomiting and has diarrhea. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • Care for shock early. § In infant or child, signs and symptoms of shock mean it has progressed and is in the late stages. § If you suspect shock may result from the MOI or NOI, provide emergency care immediately. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • Infants and children are frequent victims of trauma because of their size, curiosity, and lack of fear due to their inexperience. • Keep in mind that their larger head size and weight make pediatric patients more prone to head and neck trauma. continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Summary • Be calm, professional, and discreet about suspicions of abuse or neglect in presence of caregivers. • Be an advocate for the child. • Remember your obligation to report any suspicions to proper authorities. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
REVIEW QUESTIONS Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Review Questions 1. What are the various techniques that can be used to help with the assessment of the pediatric patient? 2. What are the components of the pediatric assessment triangle? 3. What is the most common cause of cardiac arrest in the pediatric patient? 4. What are the signs and symptoms of sudden infant death syndrome (SIDS)? continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Review Questions 5. What are the appropriate steps for management of a suspected SIDS death? 6. What are common signs and symptoms of abuse and neglect? 7. What is the role of the Emergency Medical Responder in cases of suspected abuse and/or neglect? continued on next slide Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Review Questions 8. In treating the pediatric patient, how would you assess and manage: a. b. c. d. Upper airway obstruction? Lower reactive airway disease? Seizures? Shock? Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
Please visit www. bradybooks. com and follow the Resource Central links to access content for this text. Emergency Medical Responder: First on Scene, 10/e Christopher J. Le Baudour | J. David Bergeron Copyright © 2016, 2011, 2009 by Pearson Education, Inc. All Rights Reserved
 Emergency medical responder first on scene
Emergency medical responder first on scene Cardiopulmonary
Cardiopulmonary Emergency medical responder first on scene 11th edition
Emergency medical responder first on scene 11th edition Ac vein
Ac vein American red cross first responder
American red cross first responder Campbell biology tenth edition
Campbell biology tenth edition Campbell biology tenth edition
Campbell biology tenth edition Campbell biology tenth edition
Campbell biology tenth edition Elementary statistics tenth edition
Elementary statistics tenth edition Floyd digital fundamentals
Floyd digital fundamentals Corporate finance tenth edition
Corporate finance tenth edition Psychology tenth edition in modules
Psychology tenth edition in modules Human genetics concepts and applications 10th edition
Human genetics concepts and applications 10th edition Corporate finance tenth edition
Corporate finance tenth edition Corporate finance tenth edition
Corporate finance tenth edition Corporate finance tenth edition
Corporate finance tenth edition Corporate finance tenth edition
Corporate finance tenth edition Campbell biology tenth edition
Campbell biology tenth edition Biology tenth edition
Biology tenth edition Cloroplastos
Cloroplastos Biology tenth edition
Biology tenth edition Law enforcement first responder
Law enforcement first responder Prehospital emergency care 10th edition
Prehospital emergency care 10th edition Pre-hospital communication
Pre-hospital communication Emergency care 13th edition chapter 1
Emergency care 13th edition chapter 1 Outdoor emergency care 6th edition
Outdoor emergency care 6th edition Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Prehospital emergency care 11th edition study guide
Prehospital emergency care 11th edition study guide Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Using mis (10th edition) 10th edition
Using mis (10th edition) 10th edition Zulily case study
Zulily case study Introduction to emergency medical care
Introduction to emergency medical care Chapter 31 assisting in a medical emergency
Chapter 31 assisting in a medical emergency Define medical emergency chapter 31
Define medical emergency chapter 31 Medical emergency student lectures
Medical emergency student lectures Emergency medical dispatch guidecards
Emergency medical dispatch guidecards Medicaid transportation texas logisticare
Medicaid transportation texas logisticare Introduction to emergency medical care
Introduction to emergency medical care Introduction to emergency medical care
Introduction to emergency medical care Introduction to emergency medical care
Introduction to emergency medical care The tenth man graham greene summary
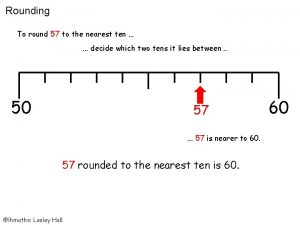
The tenth man graham greene summary Round 683 492 to the nearest hundred thousand
Round 683 492 to the nearest hundred thousand Round 74 to the nearest ten
Round 74 to the nearest ten Round off 37
Round off 37 How many hundredths are in one whole
How many hundredths are in one whole Greenspun's tenth rule
Greenspun's tenth rule Tuesday with morrie questions
Tuesday with morrie questions How to round off 25
How to round off 25 Tenth rib
Tenth rib Ubbl fire safety
Ubbl fire safety Lesson 2 volume of cones
Lesson 2 volume of cones Tenth may dawned bright and clear
Tenth may dawned bright and clear Tenth chapter wired
Tenth chapter wired Injuries first aid
Injuries first aid Chapter 8 emergency care first aid and disasters
Chapter 8 emergency care first aid and disasters Emancipated minors definition
Emancipated minors definition Medical law and ethics 5th edition
Medical law and ethics 5th edition Dragon medical network edition
Dragon medical network edition Medical law and ethics 5th edition
Medical law and ethics 5th edition Medical dosage calculations 10th edition
Medical dosage calculations 10th edition Buttock medical terminology
Buttock medical terminology Medical dosage calculations 10th edition
Medical dosage calculations 10th edition Macbeth act 1 summary scenes 1 7
Macbeth act 1 summary scenes 1 7 Macbeth act 4 summary
Macbeth act 4 summary Como enviar un correo formal
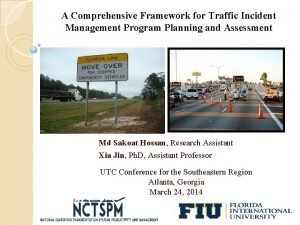
Como enviar un correo formal National tim responder training answers
National tim responder training answers Incident qualification system
Incident qualification system Responder las siguientes preguntas
Responder las siguientes preguntas Crisis responder
Crisis responder Esten siempre preparados para responder
Esten siempre preparados para responder Que responder a bienvenido
Que responder a bienvenido National tim responder training test answers
National tim responder training test answers Adveischool opiniones
Adveischool opiniones Lay responder
Lay responder Fdot mot training questions and answers
Fdot mot training questions and answers Responder las siguientes preguntas
Responder las siguientes preguntas Postergar en la biblia
Postergar en la biblia Prueba valanti resultados correcta
Prueba valanti resultados correcta Undernourished parents often raise
Undernourished parents often raise Kinder- und hausmärchen first edition
Kinder- und hausmärchen first edition Doctors license number
Doctors license number Greater baltimore medical center medical records
Greater baltimore medical center medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial cardiac rehab
Torrance memorial cardiac rehab Cartersville medical center medical records
Cartersville medical center medical records Maturity continuum model by stephen
Maturity continuum model by stephen State space search
State space search Sdl first vs code first
Sdl first vs code first Habit 3 lesson plans
Habit 3 lesson plans Put first things first meaning
Put first things first meaning Difference between code first and database first approach
Difference between code first and database first approach First to file vs first to invent
First to file vs first to invent First in first out
First in first out Dilakukan perintah top(push(b,s))
Dilakukan perintah top(push(b,s)) First in first out
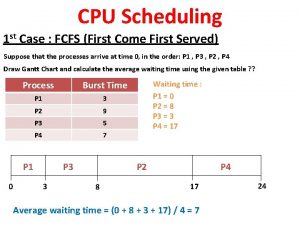
First in first out First come first serve
First come first serve Put first things first definition
Put first things first definition First come first serve calculator
First come first serve calculator Put first things first
Put first things first Habit number 3
Habit number 3 Put first things first video
Put first things first video Habit 3 activities
Habit 3 activities First aid merit badge first aid kit
First aid merit badge first aid kit Objective of first aid
Objective of first aid 7 habits promise
7 habits promise What is sems
What is sems Who emergency care system framework
Who emergency care system framework Svmc emergency room
Svmc emergency room Ucla
Ucla Pengertian shalat qashar
Pengertian shalat qashar Emergency purchasing
Emergency purchasing Eva tray in labour room
Eva tray in labour room