Drugs for Coagulation Disorders Andrew N Schmelz Pharm









- Slides: 45
Drugs for Coagulation Disorders Andrew N. Schmelz, Pharm. D Post-Doctoral Teaching Fellow Purdue University October 8, 2008 anschmel@purdue. edu
Objectives n List important steps of hemostasis and fibrinolysis n Describe thromboembolic disorders that are indications for coagulation modifiers n Identify the primary mechanism for each coagulation modifying-drug discussed n Match specific coagulation-modifying drugs to lab tests with which they are appropriately monitored
Objectives (cont) n Categorize coagulation-modifying drugs based on their classification and mechanism of action n List important adverse effects for each coagulation-modifying drug discussed
Process of Hemostasis n Hemostasis: Protects the body from both external and internal injury n Injury to blood vessels causes: – Vessel spasms (causing constriction) – Platelet adherence to injury site – Platelets aggregate and form plug – Insoluble fibrin strands form and coagulate
Process of Hemostasis
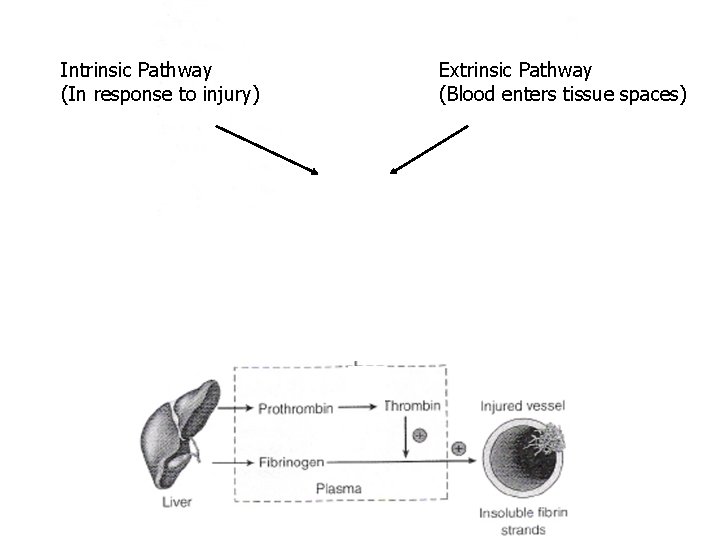
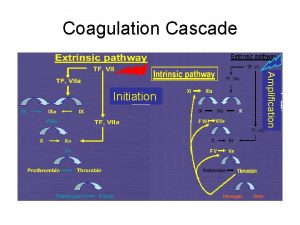
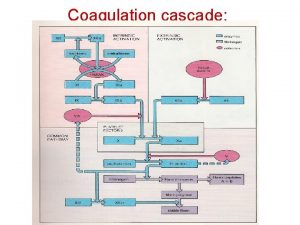
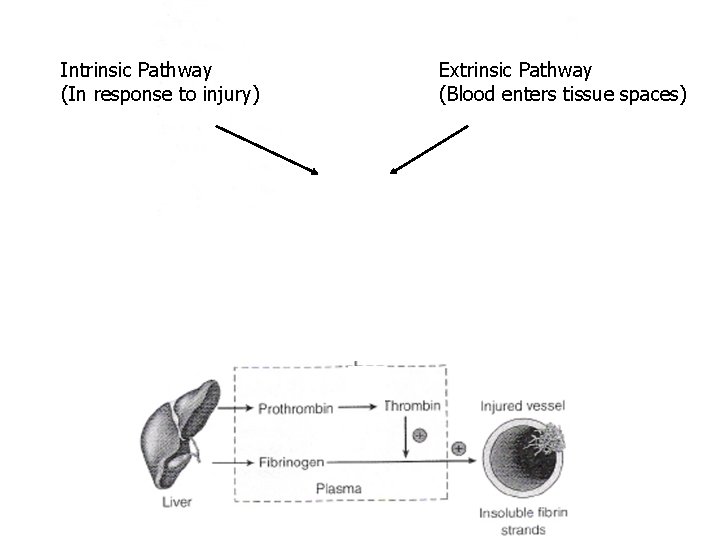
Intrinsic Pathway (In response to injury) (Factor Xa) Extrinsic Pathway (Blood enters tissue spaces)

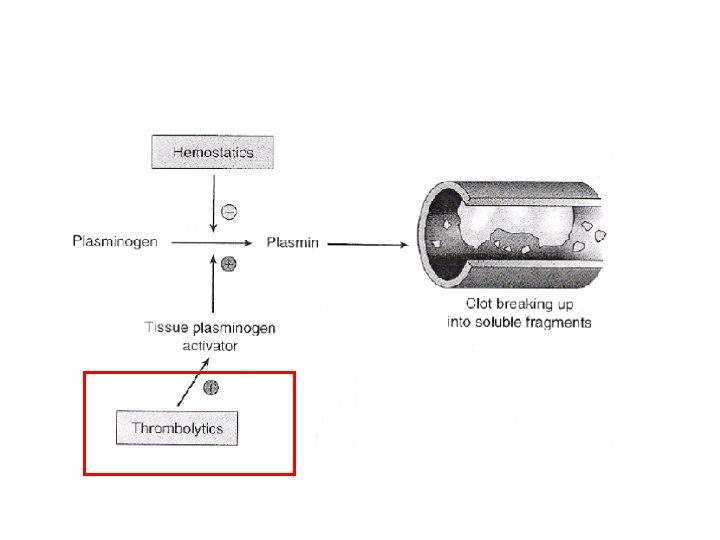
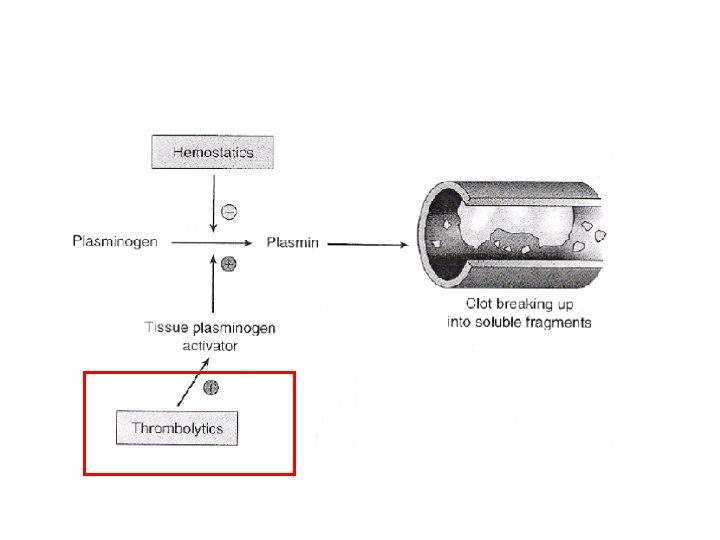
Removal of Blood Clots n Fibrinolysis: Removal of clot so that tissue can resume its normal activity
Diseases of Hemostasis n Thromboembolic CVA) disorders (MI and – Stationary clot (thrombus) grows and deprives specific areas of oxygen n Deep Vein Thrombosis (DVT) – Formation of clots in large veins (usually legs) n Embolus – Thrombus may break off and be carried by bloodstream to affect other areas

Diseases of Hemostasis (cont) n Thrombocytopenia – Low number of platelets, cannot properly form clots n Hemophilias – Genetic deficiencies of clotting factors
Mechanisms of Action n Anticoagulants – Inhibition of clotting factors n Antiplatelets – Inhibition of platelet function n Thrombolytics – Lyse thrombi n Hemostatics – Inhibition of fibrinolysis
Inhibition of Clotting Factors (Anticoagulants)

Heparin n Example: Heparin (Heplock®) n MOA: Enhances inhibitory effect of antithrombin III (inhibits factor Xa)
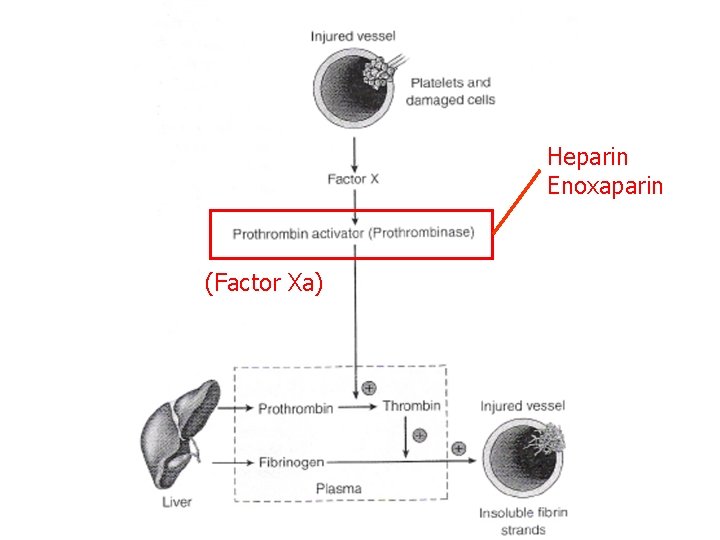
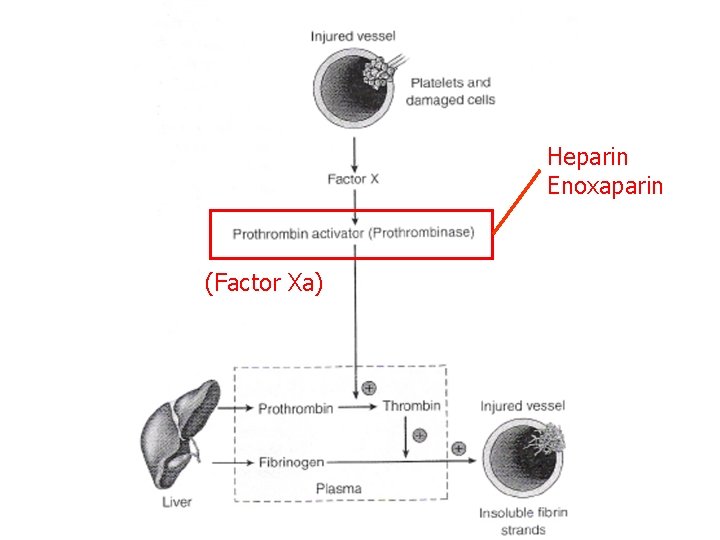
Heparin Enoxaparin (Factor Xa)
Heparin n Example: Heparin (Heplock®) n MOA: Enhances inhibitory effect of antithrombin III (inhibits factor Xa) n Route: IV (continuous infusion), SC n Monitoring: a. PTT (25 -40 s), platelets, s/sxs of hemorrhage n Adverse Effects: – Hemorrhage – Anaphylaxis – Thrombocytopenia (HIT)
Low-Molecular-Weight Heparins n Example: Enoxaparin (Lovenox®) n MOA: Enhances inhibitory effect of antithrombin III (inhibits factor Xa) n Route: SC n Monitoring: Anti-factor Xa, SCr, platelets n Adverse Effects: – Hemorrhage – Thrombocytopenia – Hypersensitivity (anaphylaxis)
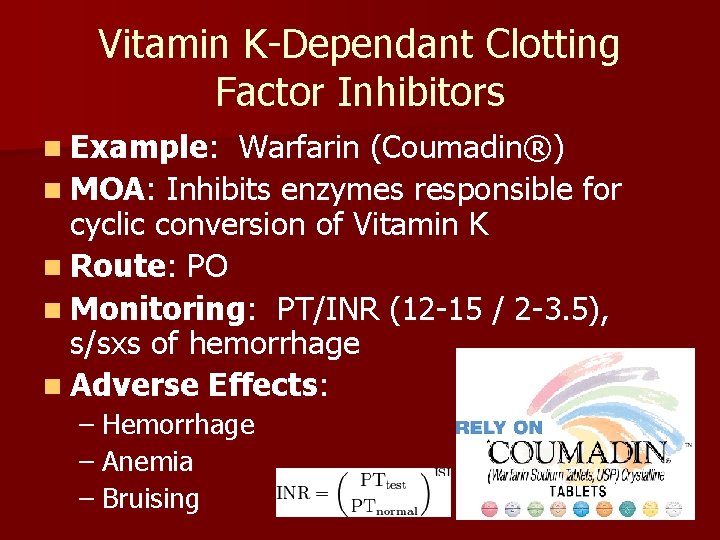
Vitamin K-Dependant Clotting Factor Inhibitors n Example: Warfarin (Coumadin®) n MOA: Inhibits enzymes responsible for cyclic conversion of Vitamin K n Route: PO n Monitoring: PT/INR (12 -15 / 2 -3. 5), s/sxs of hemorrhage n Adverse Effects: – Hemorrhage – Anemia – Bruising
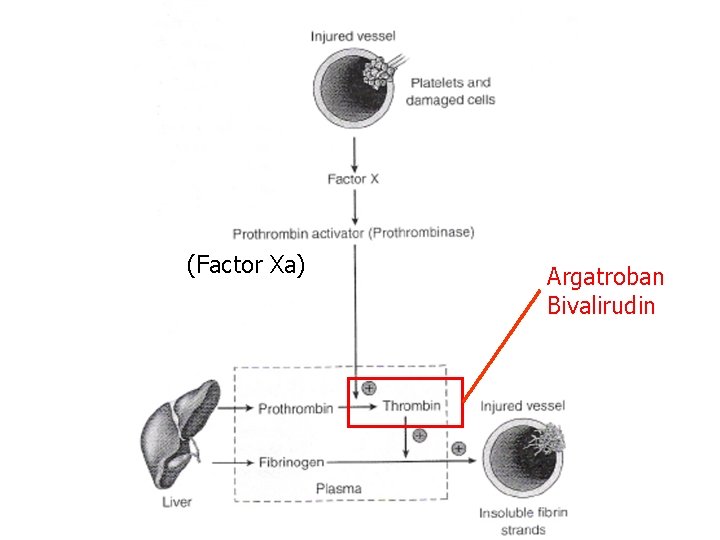
Direct Thrombin Inhibitors n Examples: Argatroban (Novastan®) Bivalirudin (Angiomax®) n MOA: Directly inhibit thrombin (preventing formation of fibrin clots)
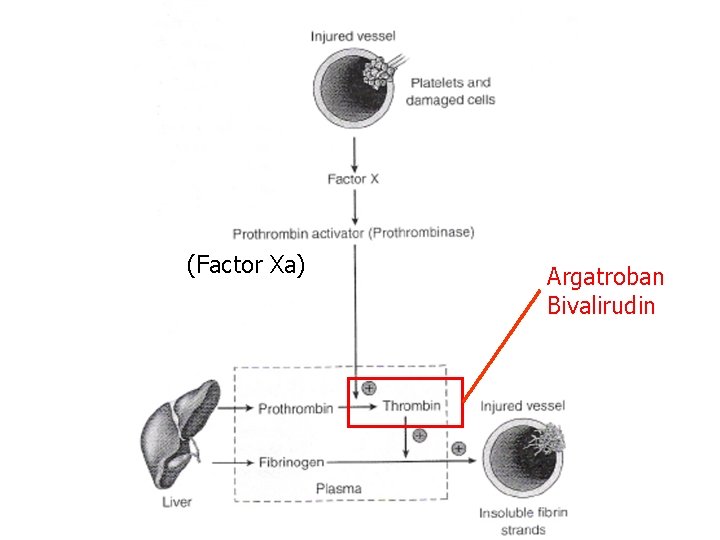
(Factor Xa) Argatroban Bivalirudin
Direct Thrombin Inhibitors n Examples: Argatroban (Novastan®) Bivalirudin (Angiomax®) n MOA: Directly inhibit thrombin (preventing formation of fibrin clots) n Route: IV n Monitoring: a. PTT (25 -40 s) n Adverse Effects: – Serious internal hemorrhage – Back pain (bivalirudin)
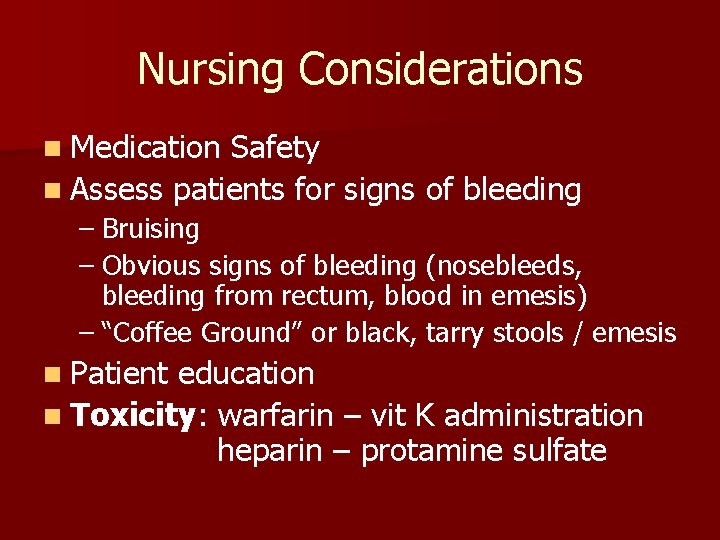
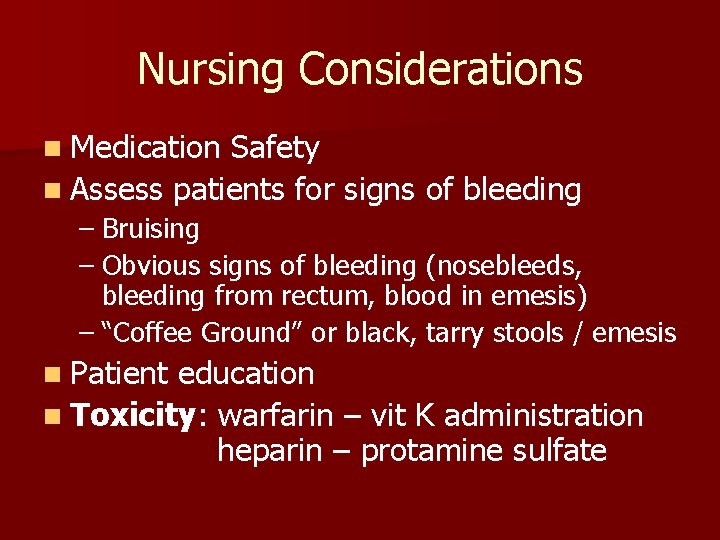
Nursing Considerations n Medication Safety n Assess patients for signs of bleeding – Bruising – Obvious signs of bleeding (nosebleeds, bleeding from rectum, blood in emesis) – “Coffee Ground” or black, tarry stools / emesis n Patient education n Toxicity: warfarin – vit K administration heparin – protamine sulfate
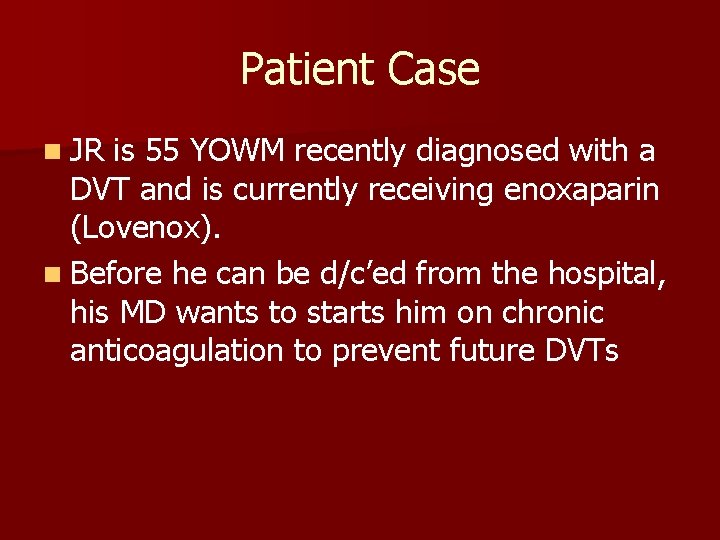
Patient Case n JR is 55 YOWM recently diagnosed with a DVT and is currently receiving enoxaparin (Lovenox). n Before he can be d/c’ed from the hospital, his MD wants to starts him on chronic anticoagulation to prevent future DVTs
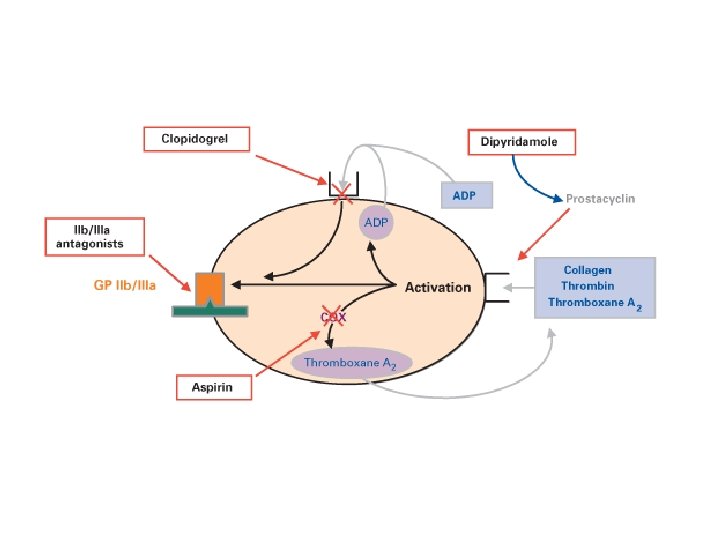
Inhibition of Platelet Function (Antiplatelets)

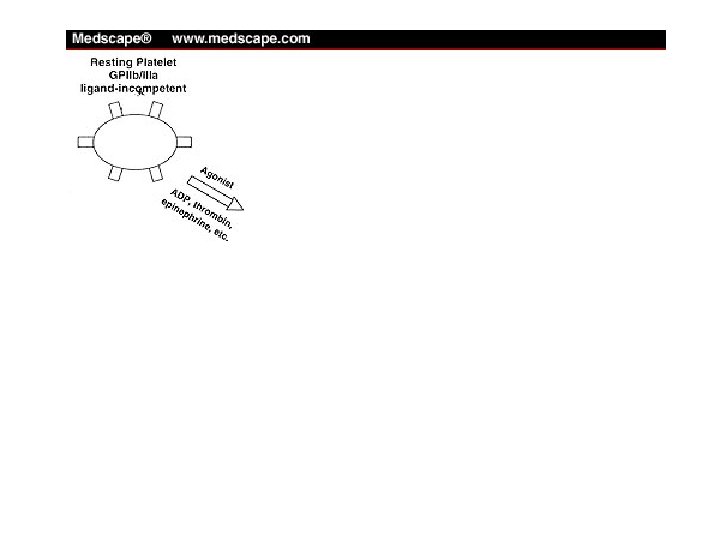
GP IIb/IIIa Antagonists n Example: Abciximab (Reo. Pro®) n MOA: Inhibit GP IIb/IIIa, enzyme necessary for platelet aggregation
GP IIb/IIIa Antagonists n Example: Abciximab (Reo. Pro®) n MOA: Inhibit GP IIb/IIIa, enzyme necessary for platelet aggregation n Route: IV n Monitoring: Platelets n Adverse Effects: – Hemorrhage – Thrombocytopenia
Aspirin (Ecotrin®) n Example: Aspirin (Ecotrin®) n MOA: Irreversibly binds to COX, inhibiting formation of thromboxane A 2

Aspirin (Ecotrin®) n Example: Aspirin (Ecotrin®) n MOA: Irreversibly binds to COX, inhibiting formation of thromboxane A 2 n Route: PO n Monitoring: S/sxs hemorrhage n Adverse Effects: – Increased clotting times – GI bleeding – Anaphylaxis
ADP Receptor Blockers n Example: Clopidogrel (Plavix®) n MOA: ADP-receptor blockers
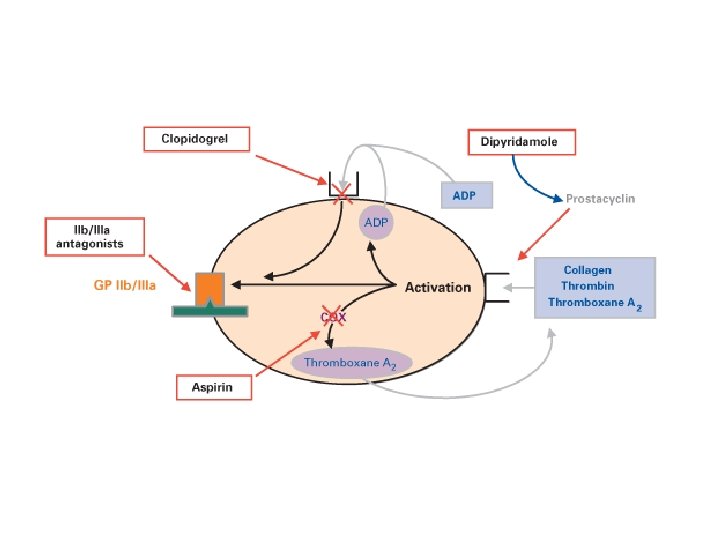
ADP Receptor Blockers n Example: Clopidogrel (Plavix®) n MOA: ADP-receptor blockers n Route: IV (loading dose), PO n Monitoring: S/sxs hemorrhage n Adverse Effects: – Increased clotting time – GI bleeding – Blood dyscrasias (TTP)

Agents for Intermittent Claudication n Example: Cilostazole (Pletal®) n MOA: PDE-3 inhibitor n Route: PO n Monitoring: S/sxs hemorrhage, heart n Adverse Effects: – Palpitation, tachycardia, – Nausea, vomitting
Nursing Considerations n Careful monitoring of patient condition (increased risk of bleeding) n Combination with anticoagulants – increased risk of bleeding n Injection / venipuncture sites will require prolonged pressure to control bleeding n Patient education

Pharmacotherapy with Thrombolytics
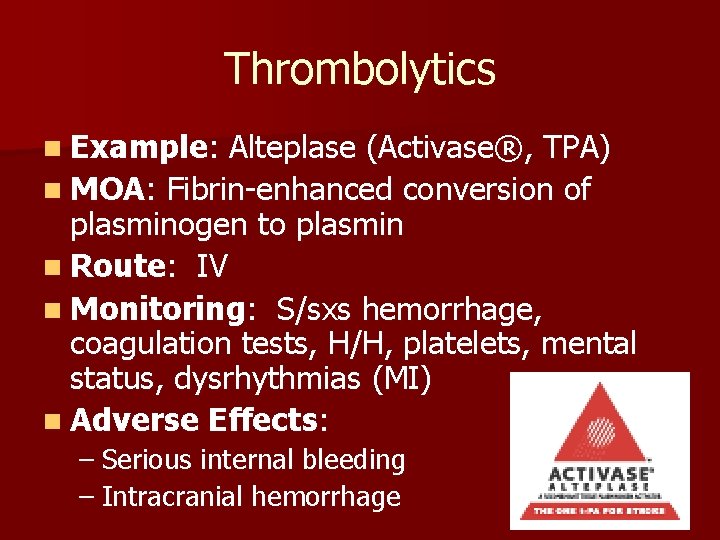
Thrombolytics n Example: Alteplase (Activase®, TPA) n MOA: Fibrin-enhanced conversion of plasminogen to plasmin
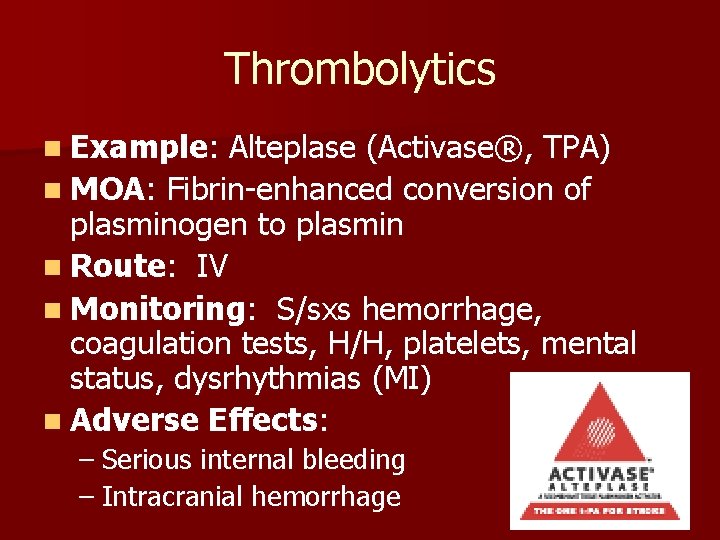
Thrombolytics n Example: Alteplase (Activase®, TPA) n MOA: Fibrin-enhanced conversion of plasminogen to plasmin n Route: IV n Monitoring: S/sxs hemorrhage, coagulation tests, H/H, platelets, mental status, dysrhythmias (MI) n Adverse Effects: – Serious internal bleeding – Intracranial hemorrhage
Nursing Considerations n Identify underlying conditions that exclude patient from receiving thrombolytics – Recent trauma, surgery, or biopsy – Arterial emboli – Recent cerebral embolism – Hemorrhage – Thrombocytopenia – Childbirth (within 10 days)
Pharmacotherapy with Hemostatics
Hemostatics n Example: Aprotinin (Trasylol®) n MOA: Inhibits fibrinolysis (affects multiple mediators)

Hemostatics n Example: Aprotinin (Trasylol®) n MOA: Inhibits fibrinolysis (affects multiple mediators) n Route: IV n Monitoring: Clotting, peripheral pulses, paresthesias, (+) Homans’ sign n Adverse Effects: – Clotting – Extravasation

Questions
Summary n Hemostasis protects the body from injury n Several pathologies may affect hemostasis n Four main drug categories are used to treat coagulation disorders n Nurses play an important role – Monitoring drug efficacy – Monitoring patient for adverse effects
Drugs for Coagulation Disorders Andrew N. Schmelz, Pharm. D Post-Doctoral Teaching Fellow Purdue University October 8, 2008 anschmel@purdue. edu
 Coagulation disorders
Coagulation disorders Dvt workbook
Dvt workbook Anabel schmelz
Anabel schmelz Lehre schmelz
Lehre schmelz Schmelz und erstarrungswärme
Schmelz und erstarrungswärme Pharm d means
Pharm d means Ambio pharm
Ambio pharm Pharm gkb
Pharm gkb What is the transport system of the body
What is the transport system of the body Klucel exf pharm
Klucel exf pharm Pharm 406
Pharm 406 Secur pharm
Secur pharm Library.med.utah.edu/kw/pharm/hyper heart.html
Library.med.utah.edu/kw/pharm/hyper heart.html Friciton
Friciton Bc bio-pharm
Bc bio-pharm Pharm degree
Pharm degree Purdue retail pharmacy
Purdue retail pharmacy Outfield pharm
Outfield pharm Pharm id
Pharm id Epharmacy
Epharmacy Pharm
Pharm Describe the mechanism of coagulation of blood
Describe the mechanism of coagulation of blood Primary hemostasis
Primary hemostasis Yolk composition
Yolk composition D'alessio
D'alessio Coagulation pathway made easy
Coagulation pathway made easy Flow chart of blood coagulation
Flow chart of blood coagulation Coagulation factors list
Coagulation factors list Coagulation profile test
Coagulation profile test Fulguration diathermy
Fulguration diathermy Protein denaturation definition
Protein denaturation definition Coagulation profile test
Coagulation profile test Hus dic
Hus dic Heat coagulation principle
Heat coagulation principle Fat
Fat Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Coagulation cascade
Coagulation cascade Nécrose de coagulation anapath
Nécrose de coagulation anapath Hemodynamic disorders pathology
Hemodynamic disorders pathology Principle of slide method of clotting time
Principle of slide method of clotting time Tidbok yrkesförare
Tidbok yrkesförare Mästar lärling modellen
Mästar lärling modellen Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? Orubbliga rättigheter
Orubbliga rättigheter Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Bamse för de yngsta
Bamse för de yngsta