Disseminated Intravascular Coagulation DIC Coagulation hemostasis n Vessel



- Slides: 40
Disseminated Intravascular Coagulation (DIC)
Coagulation & hemostasis n Vessel wall n Platelets n Coagulation factors
Anticoagulation n Cellular system: Monocyte/ Macrophage n Anticoagulants in plasma(TFPI, ATⅢ, heparin co-factor II ) n Protein C system n Fibrinolytic system
Definition of DIC
Definition Disseminated intravascular coagulation (DIC) is a complex systemic thrombohemorrhagic disorder involving the generation of intravascular fibrin and the consumption of procoagulants and platelets. The resultant clinical condition is characterized by intravascular coagulation and hemorrhage.
Causes of DIC
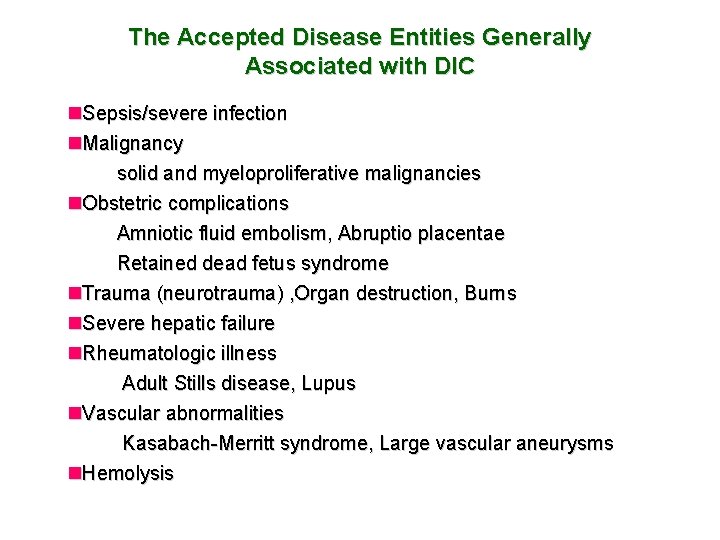
The Accepted Disease Entities Generally Associated with DIC n. Sepsis/severe infection n. Malignancy solid and myeloproliferative malignancies n. Obstetric complications Amniotic fluid embolism, Abruptio placentae Retained dead fetus syndrome n. Trauma (neurotrauma) , Organ destruction, Burns n. Severe hepatic failure n. Rheumatologic illness Adult Stills disease, Lupus n. Vascular abnormalities Kasabach-Merritt syndrome, Large vascular aneurysms n. Hemolysis
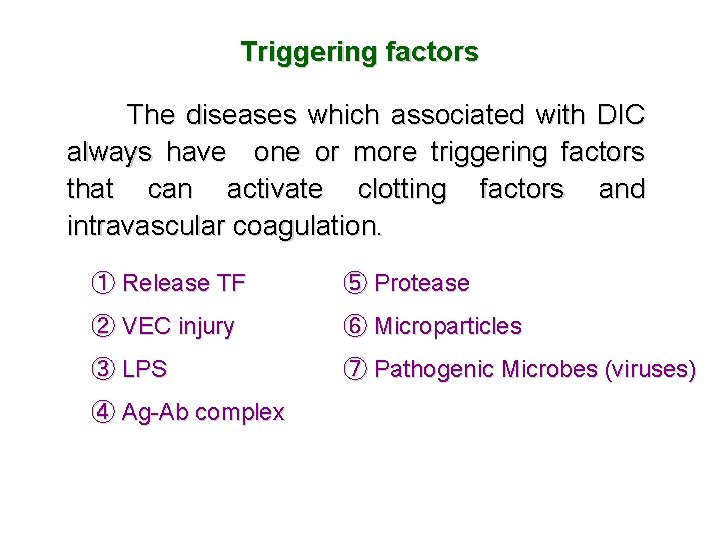
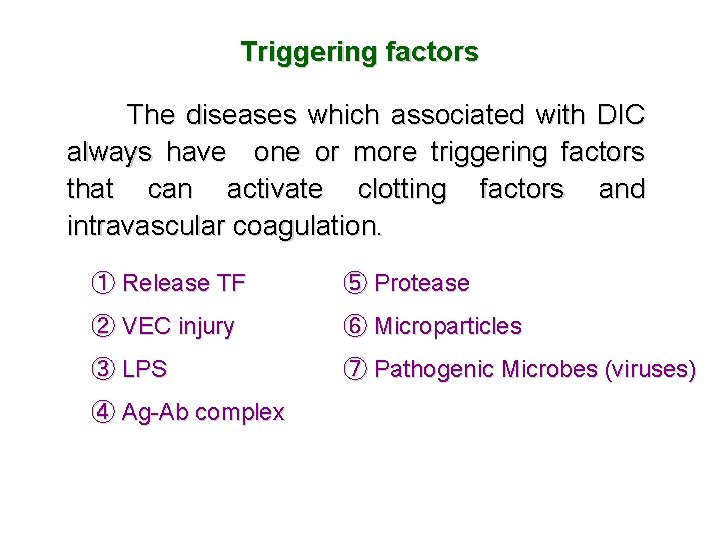
Triggering factors The diseases which associated with DIC always have one or more triggering factors that can activate clotting factors and intravascular coagulation. ① Release TF ⑤ Protease ② VEC injury ⑥ Microparticles ③ LPS ⑦ Pathogenic Microbes (viruses) ④ Ag-Ab complex
Pathogenesis of DIC
Pathophysiology n Activation of coagulation n Disabled anticoagulant mechanism n Impaired fibrinolysis
Activation of coagulation n Tissue damage n Endothelial disruption n Hemolysis n Leukemia n Other procoagulant molecules enter the vascular system
Suppression of anticoagulant pathways n Antithrombin activity is reduced n Protein C pathway is incapacitated n TFPI is another anticoagulant mechanism that is disabled
Impaired fibrinolysis n Experimental and clinical studies indicate that during DIC, the fibrinolytic system is largely suppressed at the time of maximal activation of coagulation. n This inhibition of fibrinolysis is caused by a sustained rise in the plasma level of plasminogen activator inhibitor-1 (PAI-1), the principal inhibitor of the fibrinolytic system.

Secondary Fibrinolysis Plasminogen Extrinic activators enzymes EC Pro-PA PAI-1 t-PA, u-PA Secretion Urine(UK,u-PA) Bile(bilokinase) PAI-3 Latex、saliva、tear Tissue lung、prostate、uterus Blood cell PAI-2 RBC, Platelet Exogenous activators Intrinic activators Coagulation Ⅺa Ⅱa Ⅻa Ⅻ KK VEC-HK Thrombolytic drugs Streptokinase (SK) Urokinase (UK) rt-PA Histidine-rich glycoprotein (HRG) PK Plasmin α 2 -plasmin inhibitor (α 2 -PI) α 2 - macroglobin (α 2 –MG) Proteolyses fibrinogen, fibronectin , laminin , thrombospondin;Activates collagenases.
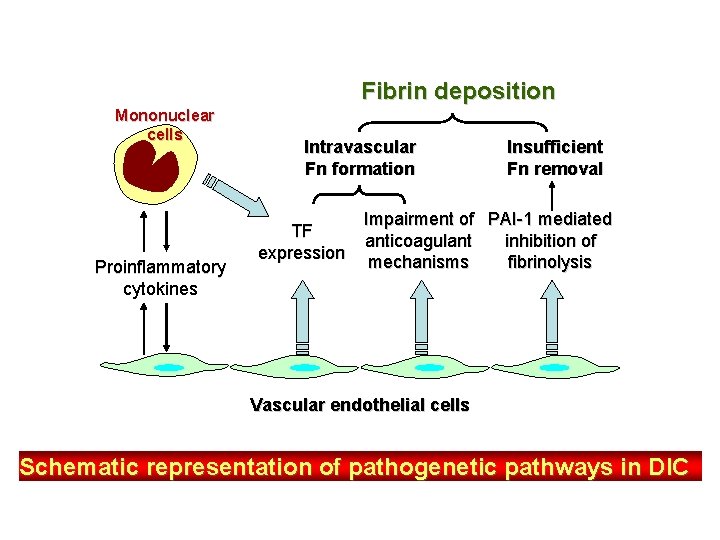
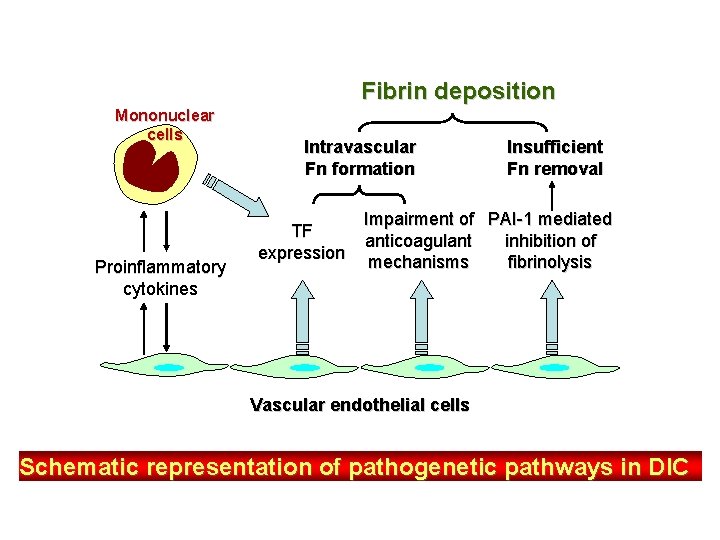
Fibrin deposition Mononuclear cells Proinflammatory cytokines Intravascular Fn formation TF expression Insufficient Fn removal Impairment of PAI-1 mediated anticoagulant inhibition of mechanisms fibrinolysis Vascular endothelial cells Schematic representation of pathogenetic pathways in DIC
Predisposing factors to DIC
Impairment of reticuloendothelial system n There is good evidence that most of the products of intravascular coagulation (free fibrin, prothrombinase, PF 3), as well as various initiators of the process (endotoxin, tissue fragments, antigen-antibody complexes, thromboplastins, red cell stroma) are removed from the circulation by the reticuloendothelial system. The hepatic cells are of primary importance in the clearance of activated coagulation factors (IXa, Xa and XIIa). It has been suggested that, in DIC, various substances saturate or block the clearance function of reticuloendothelial system in a manner comparable to that produced experimentally in the general Shwartzman reaction (GSR) in animals. n Reticuloendothelial system is suppressd by glucocorticoid or in the patients with liver diseases.
Hepatic dysfunction Hemostasis is intimately related to liver function, because most coagulation factors are synthesized by liver parenchymal cells and the liver's reticuloendothelial system serves an important role in the clearance of activation products. The extent of coagulation abnormalities depends upon the degree of disturbed liver function. n Acute or chronic hepatocellular diseases may display decreases in the vitamin K-dependent factors (prothrombin; factors VII, IX, and X; proteins C and S), whereas other parameters remain normal. n Patients with hepatic failure may present with the entire spectrum of factor deficiencies and may even develop DIC. n Patients with liver cirrhosis have a wide spectrum of abnormalities. Except for factor VIII: C and von Willebrand factor, all procoagulant and inhibitory factors are decreased, which is a reflection of impaired protein synthesis. Abnormal fibrinogen and prothrombin molecules can be identified. Platelets are quantitatively and qualitatively altered, and most patients develop DIC.
Hypercoagulable state It has been found that the platelet and several kinds of clotting factors (factor I, II, VIII, IX and X, etc. ) in blood are increased, while the substances with the action of anticoagulation and with the activity of fibrinolysis are deceased. For instance, the blood in pregnancy after 4 months bigins to increase coagulability, which is most marked in the terminal stage of pregnancy. Therefore the incidence of DIC is elevated in obstetrical accidents. In addition, acidosis, common in some patients, promotes the activation of clotting cascade by reducing the p. H of the blood.
Disorder of microcirculation Shock usually accompanies disorder of microcirculation which is manifested by stasis of blood flow, aggregation of blood cells and appearance of sludging, stasis of the microcirculation permits activated clotting factors to accumulated in one region making it easier to develop into a state of DIC. The stasis of blood in giant hemangioma may somehow contribute to the development of DIC.
Inhibition of fibrinolysis n Aging, smoking, pregnandiacy, diabetes. n Using antifibrinolytic agents like EACA and PAMBA

Main Features of DIC
Bleeding n. Include petechiae and purpura (found in most patients), hemorrhagic bullae, wound bleeding; especially oozing from a surgical or traumatic wound is common in patients who have undergone surgery or suffered trauma.
Bleeding n. The average patient with DIC usually bleeds from at least three unrelated sites and any combination may be seen.
Bleeding n. Bleeding causes: ▲Clotting factors consumption ▲ Activation of fibrinolytic system ▲ FDP generation ▲ Vessel damage
Shock n Excess bleeding n Thrombus formation results in a diminished return of venous blood to the heart n Activation of the kinin system leads to increased vascular permeability, hypotension, andshock n Creation of vasodilation FDP n Myocardial infarction result in enhanced
Organ damage / failure Pathogenesis n Impaired blood flow caused by microvascular thrombosis n Ischemia reperfusion injury n Systemic inflammatory response syndrom n Multiple organ dysfunction syndrome
Organ damage / failure l. Kidneys – renal damage seen in 25% of DIC cases in one series l. Liver – hepatic dysfunction in 19% l. Lungs – respiratory dysfunction in 16%
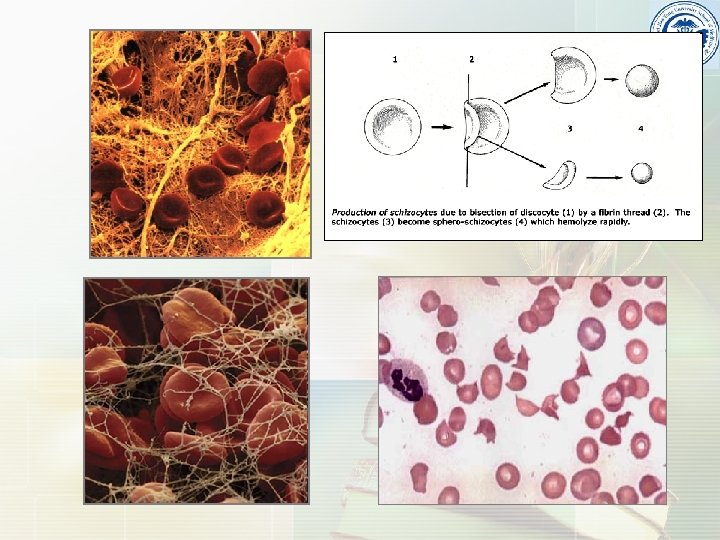
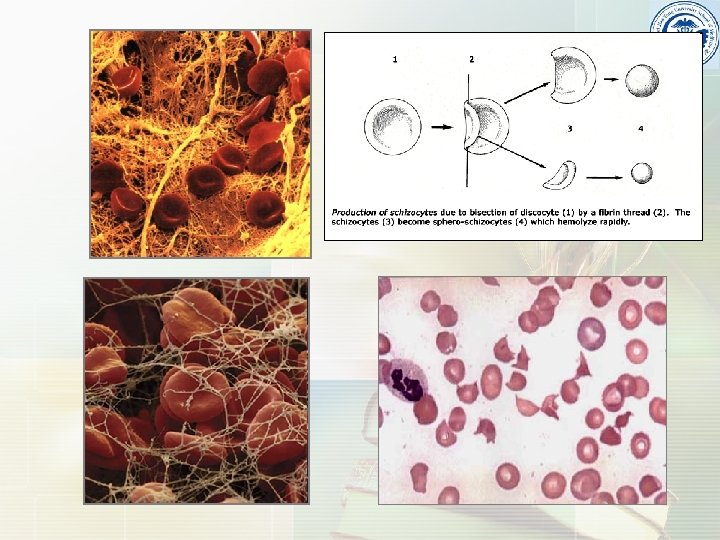
Microangiopathic hemolytic anemia n A disorder in which narrowing or obstruction of small blood vessels results in distortion and fragmentation of erythrocytes, hemolysis, and anemia. n It is identified by the finding of anaemia and schistocytes ("bite cells") on microscopy of the blood film.
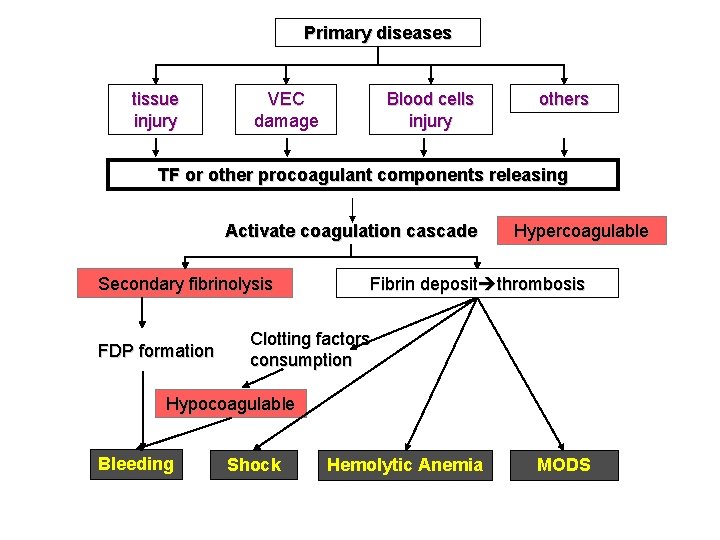
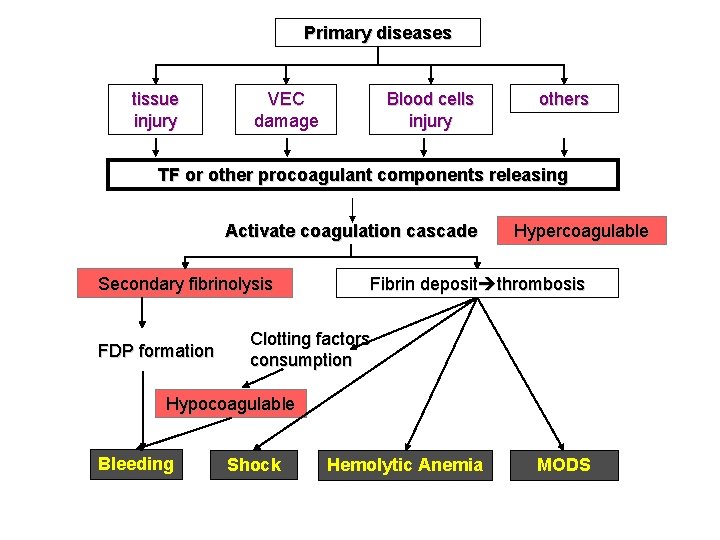
Primary diseases tissue injury VEC damage Blood cells injury others TF or other procoagulant components releasing Activate coagulation cascade Secondary fibrinolysis FDP formation Hypercoagulable Fibrin deposit thrombosis Clotting factors consumption Hypocoagulable Bleeding Shock Hemolytic Anemia MODS
Types and stages of DIC
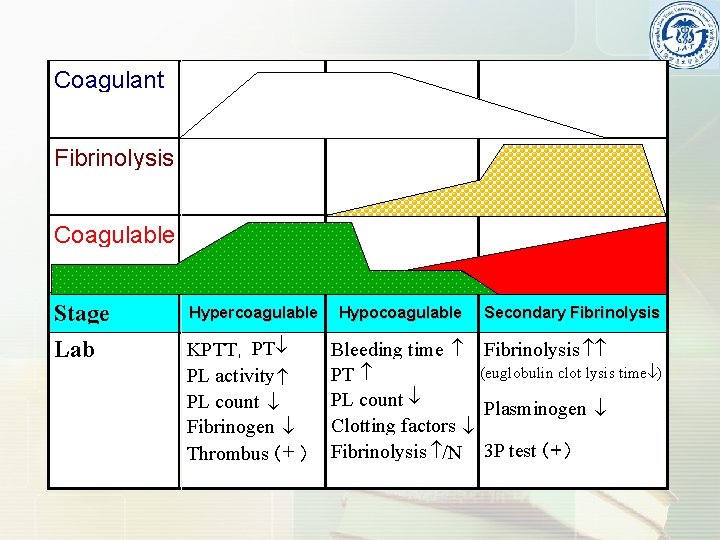
Stages n Hypercoagulable stage n Hypocoagulable stage n Secondary fibrinolytic stage
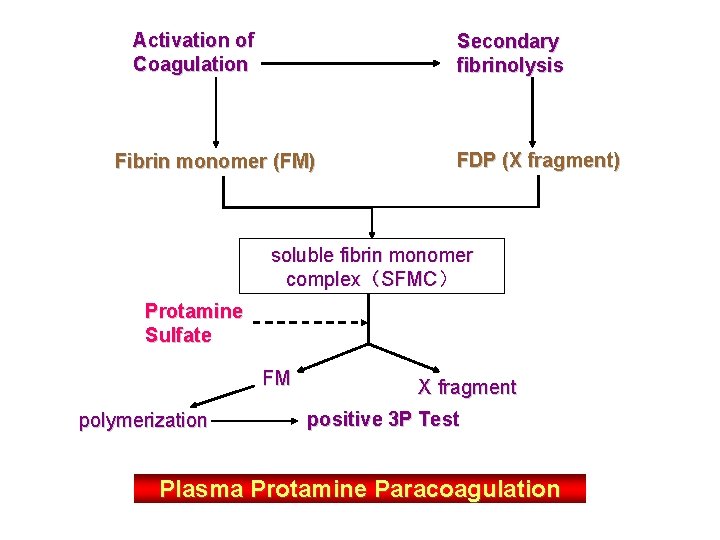
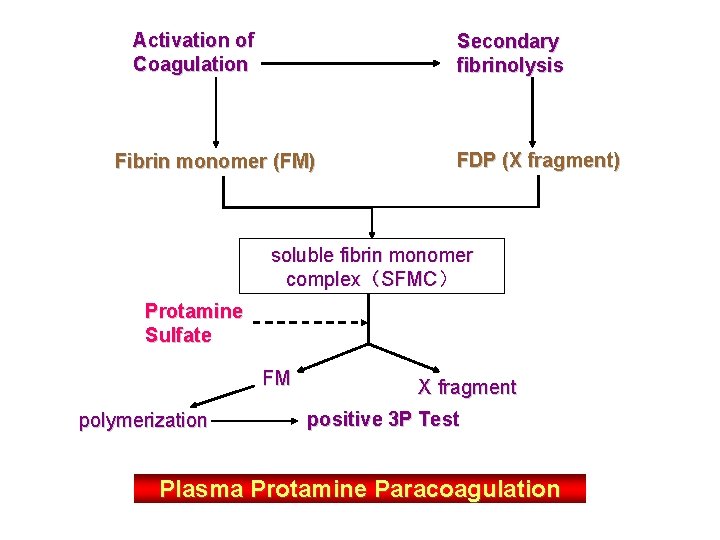
Activation of Coagulation Secondary fibrinolysis Fibrin monomer (FM) FDP (X fragment) soluble fibrin monomer complex(SFMC) Protamine Sulfate FM polymerization X fragment positive 3 P Test Plasma Protamine Paracoagulation
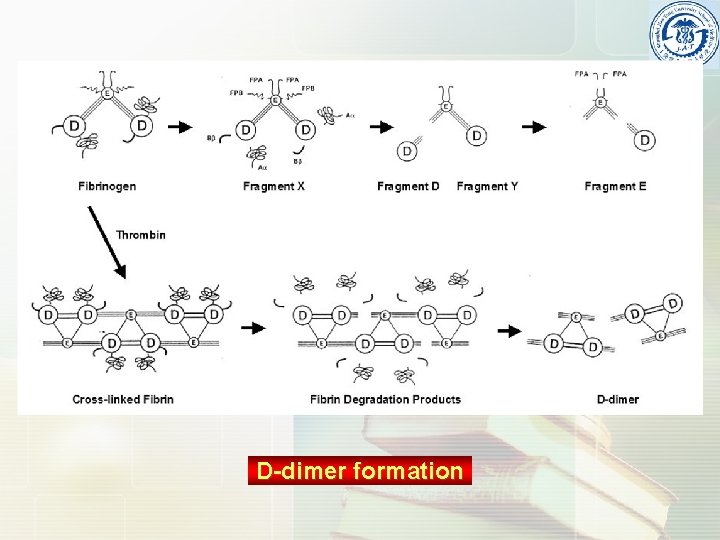
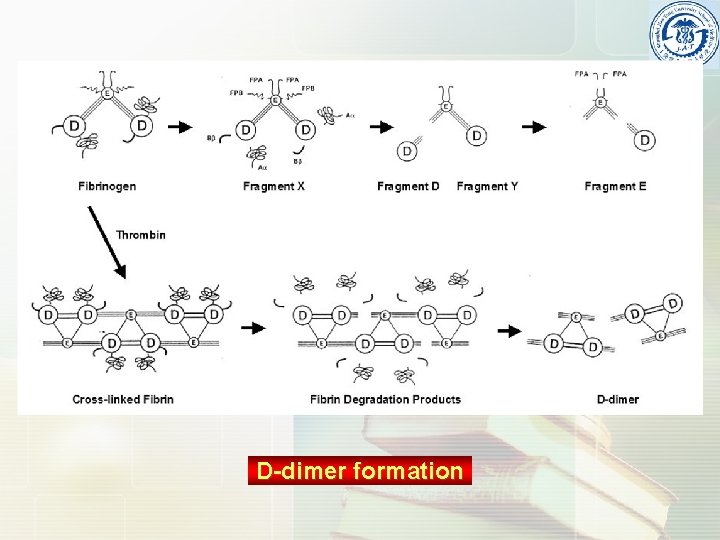
D-dimer formation
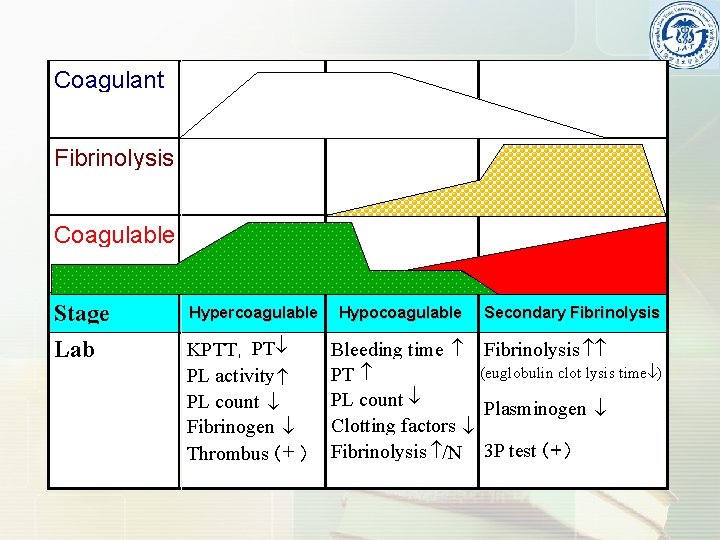
Coagulant Fibrinolysis Coagulable Stage Hypercoagulable Lab KPTT, PT PL activity PL count Fibrinogen Thrombus(+ ) Hypocoagulable Secondary Fibrinolysis Bleeding time Fibrinolysis (euglobulin clot lysis time ) PT PL count Plasminogen Clotting factors Fibrinolysis /N 3 P test(+)

Types The form of DIC depends on the rapidity and force of the initiating event, leading to the two primary forms of DIC: n Acute decompensated DIC n Chronic compensated DIC Compensated DIC: When the stimulus for coagulation is mild, the liver can increase production of clotting factors to up to 5 times the normal rate, in an effort to maintain plasma levels. Similarly, platelet production can increase up to 10 times. Thus, although coagulation and fibrinolysis are in progress, platelet counts and fibrinogen levels may be normal or only marpinally reduced. These patients rarely bleed spontaneously or from minor trauma, but have severe haemorrhage if subjected to surgery.
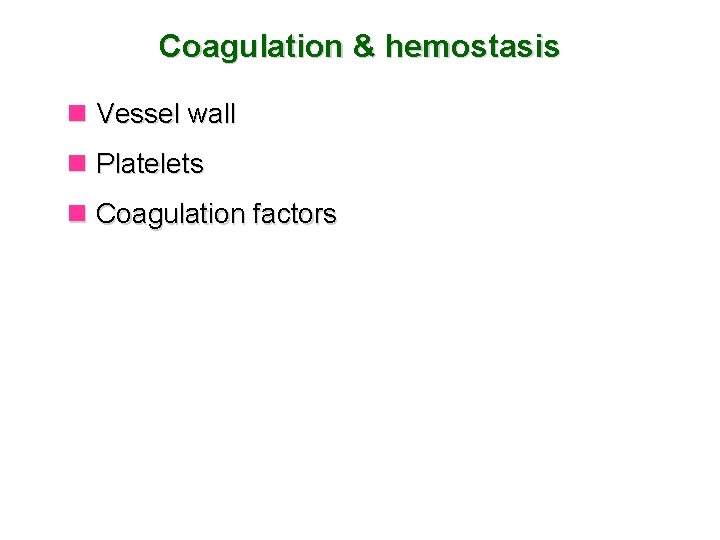
Treatment of DIC
Treatment of DIC n Cornerstone of management is the treatment of the underlying illness n Supportive management with ▲ Disruption of coagulation cascade using l “lower dose” heparin-treatment, l administration of ATIII and/or activated protein C (protein C infusion has shown to be the first intervention proven to be effective in reducing the mortality in septic patients ▲ If bleeding is the predominant symptom l Platelet infusion l Coagulation factor substitution with fresh frozen plasma