Pharmacy Refill Data plus Selfreport Adherence Improve Predictions



- Slides: 21

Pharmacy Refill Data plus Self-report Adherence Improve Predictions of LPV/rbased Regimen Failure in a Resource. Limited Setting Gert van Zyl, MBCh. B 1; Diederik Geboers, BS 1; Robert Gross, MD, MSc 2; Edward Mills, Ph. D 3; Lize van der Merwe, Ph. D 4; Jantjie Taljaard, MBCh. B 1; Gilles van Cutsem, MD, MPH 5; Hoang Nguyen, MD 7; David Bangsberg, MD, MPH 6; Jean B. Nachega, MD, Ph. D 1, 7. Stellenbosch University, Centre for Infectious Diseases 1, Cape Town, South Africa; Amsterdam Medical Centre, Amsterdam, The Netherlands; University of Pennsylvania, Philadelphia, PA, USA 2; University of British Columbia, Vancouver, Canada 3; South African Medical Research Council 4; Medecins Sans Frontieres, Cape Town, South Africa 5; Harvard Medical School, Boston, MA, USA 6; and Johns Hopkins University 7, Baltimore, MD, USA 6 th IAPAC-NIMH Adherence Conference, May 22 -24, 2011, Miami, FL. , USA, Ab. Or#70489 Project Funded by PEPFAR

Background • Adherence is the most important predictor of viral suppressions, drug resistance, and disease progression. • We have shown that pharmacy refill data is the most reliable and efficient method for monitoring adherence in RLS; performs better than CD 4 monitoring (Nachega et al. Ann Int Med 2007; Bisson et al. Plos Med 2008) • Other objective methods such as home pill counts or electronic monitoring are not always feasible in such settings
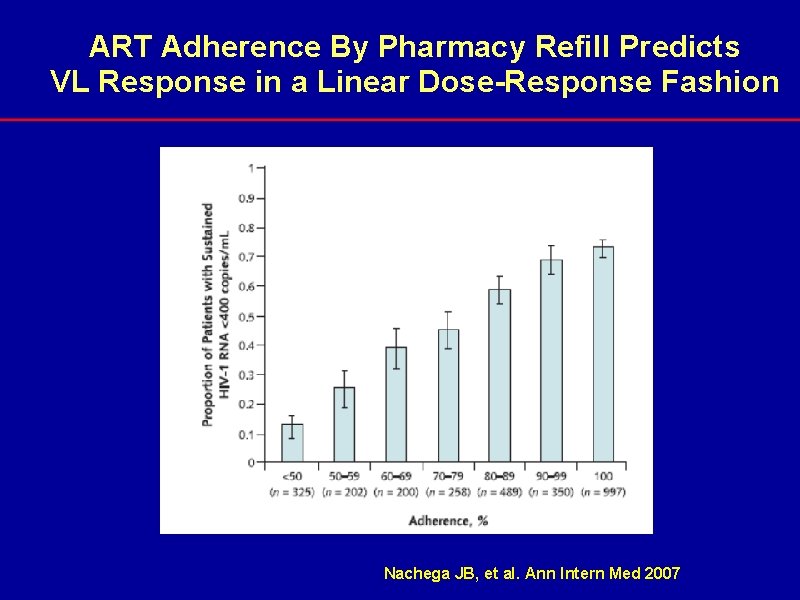
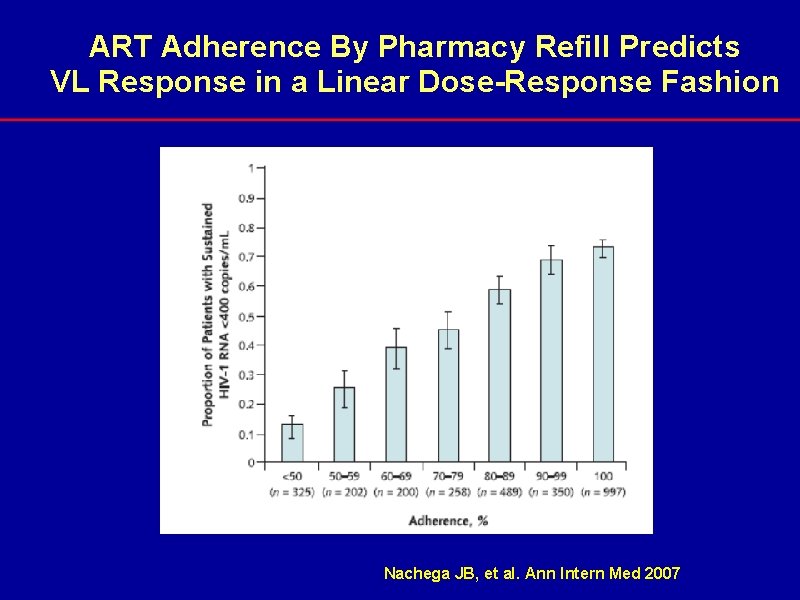
ART Adherence By Pharmacy Refill Predicts VL Response in a Linear Dose-Response Fashion Nachega JB, et al. Ann Intern Med 2007
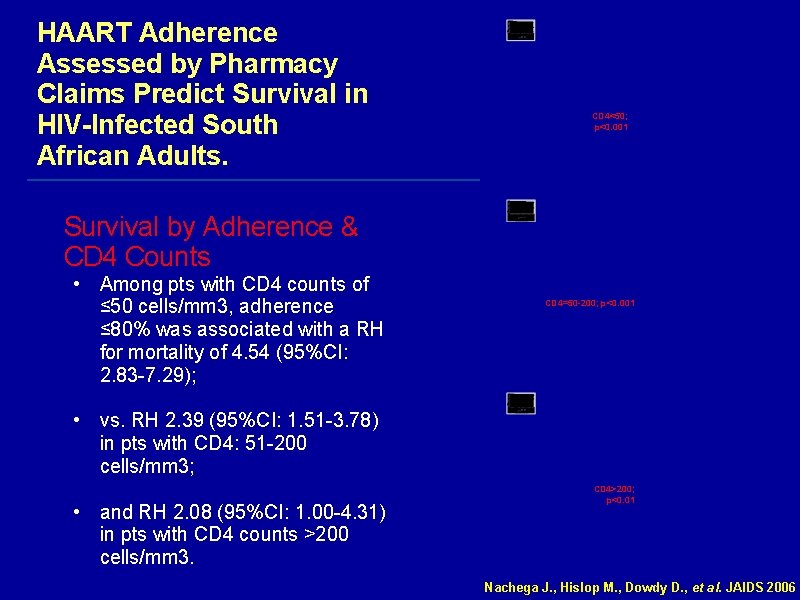
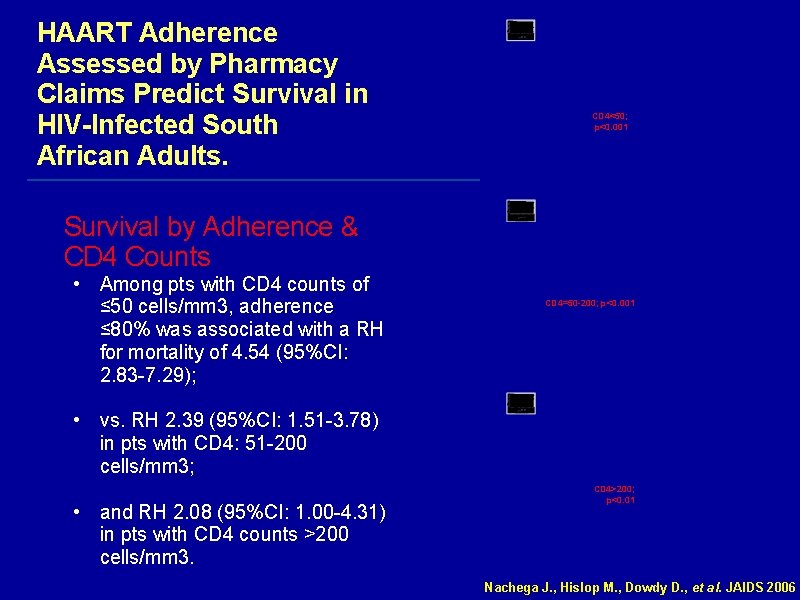
HAART Adherence Assessed by Pharmacy Claims Predict Survival in HIV-Infected South African Adults. CD 4<50; p<0. 001 Survival by Adherence & CD 4 Counts • Among pts with CD 4 counts of ≤ 50 cells/mm 3, adherence ≤ 80% was associated with a RH for mortality of 4. 54 (95%CI: 2. 83 -7. 29); CD 4=50 -200; p<0. 001 • vs. RH 2. 39 (95%CI: 1. 51 -3. 78) in pts with CD 4: 51 -200 cells/mm 3; • and RH 2. 08 (95%CI: 1. 00 -4. 31) in pts with CD 4 counts >200 cells/mm 3. CD 4>200; p<0. 01 Nachega J. , Hislop M. , Dowdy D. , et al. JAIDS 2006
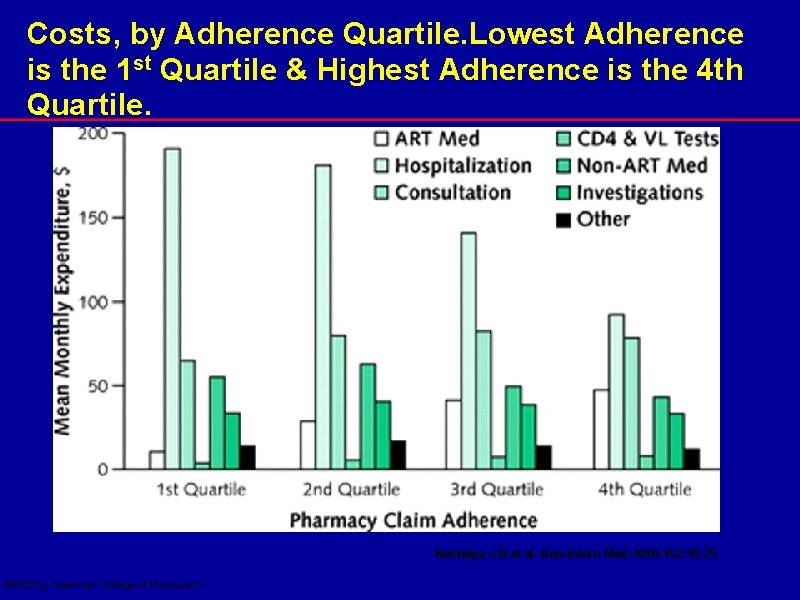
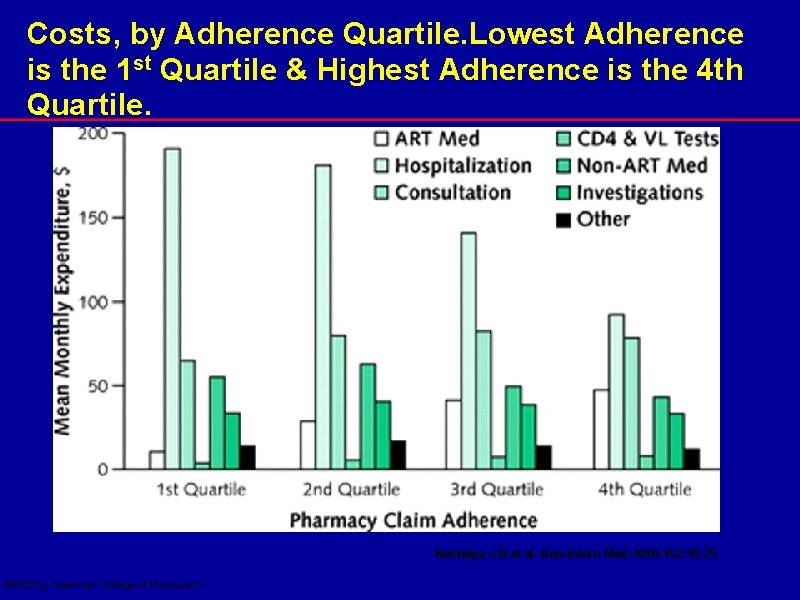
Costs, by Adherence Quartile. Lowest Adherence is the 1 st Quartile & Highest Adherence is the 4 th Quartile. Nachega J B et al. Ann Intern Med 2010; 152: 18 -25 © 2010 by American College of Physicians
Switching from 1 st line to 2 nd line ARV in RLS • Clinical and immunological criteria for switching • Viral Load not always available for monitoring the ARV therapy We are switching too late! 2
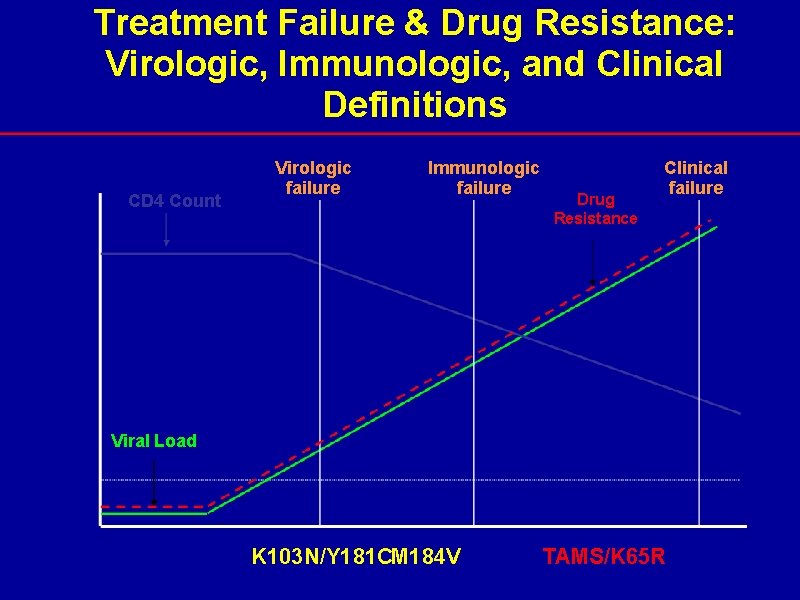
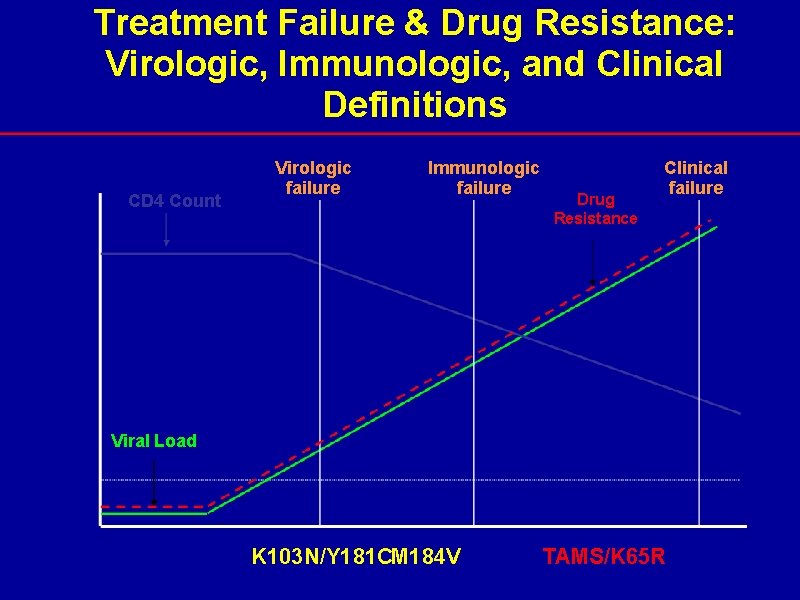
Treatment Failure & Drug Resistance: Virologic, Immunologic, and Clinical Definitions CD 4 Count Virologic failure Immunologic failure Drug Resistance Clinical failure Viral Load K 103 N/Y 181 CM 184 V TAMS/K 65 R
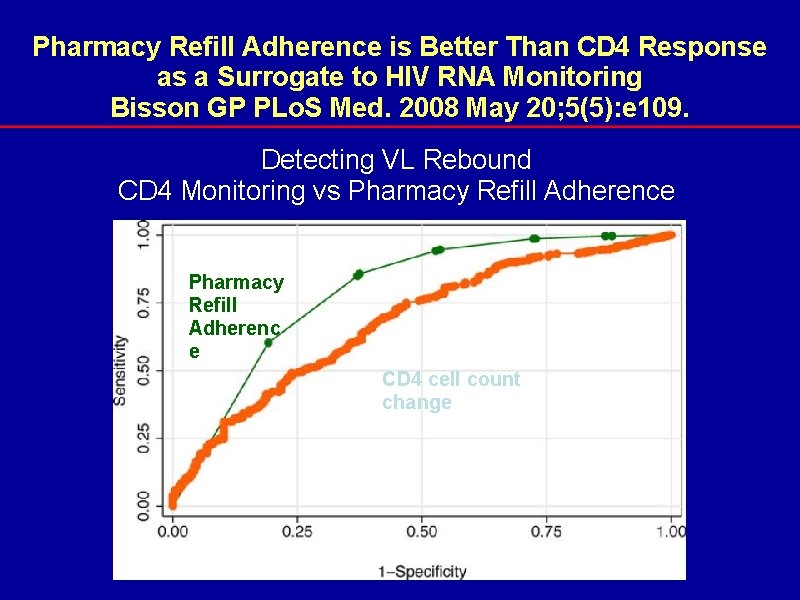
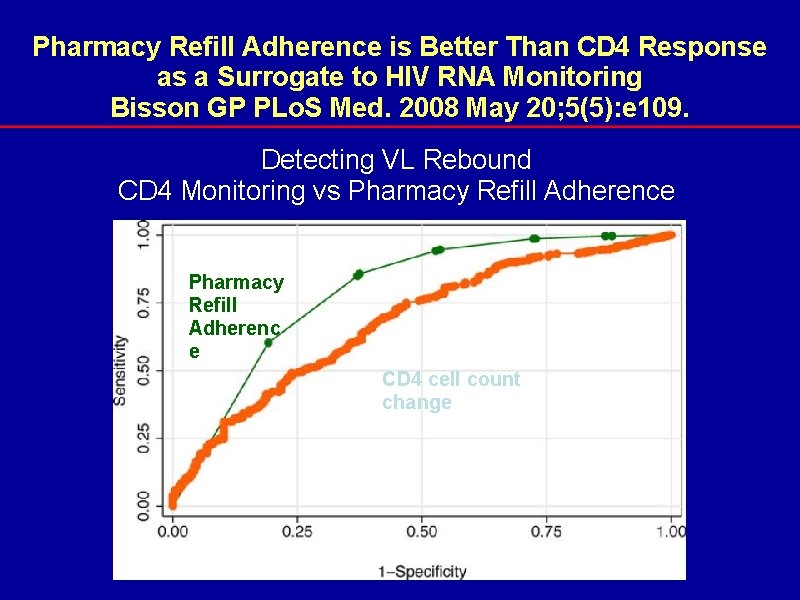
Pharmacy Refill Adherence is Better Than CD 4 Response as a Surrogate to HIV RNA Monitoring Bisson GP PLo. S Med. 2008 May 20; 5(5): e 109. Detecting VL Rebound CD 4 Monitoring vs Pharmacy Refill Adherence Pharmacy Refill Adherenc e CD 4 cell count change
Background (Cont’d) • Nonetheless, pharmacy refill monitoring remains a relatively coarse measure of adherence. • Ways to improve pharmacy refill monitoring include removing heterogeneity with respect to: o o o amount of medication dispensed (30, 60, 90 d), time since treatment initiation, and patients reported information with pattern of adherence of missed doses and treatment interruptions.
Background (Cont’d) • Studies evaluating the accuracy of simple, low-cost ART adherence monitoring tools such as pharmacy refill, pill count or self-report, used singly or in combination, to predict treatment success or failure are sketchy • This knowledge is critical for all patients, but even more in patients on second line antiretroviral therapy (ART), since it is last regimen option, available in the public sector of most resource-limited settings.
Objective To investigate whether accuracy of Pharmacy refill monitoring is improved by combining with pill count or patient reported information on adherence patterns increase predictions.
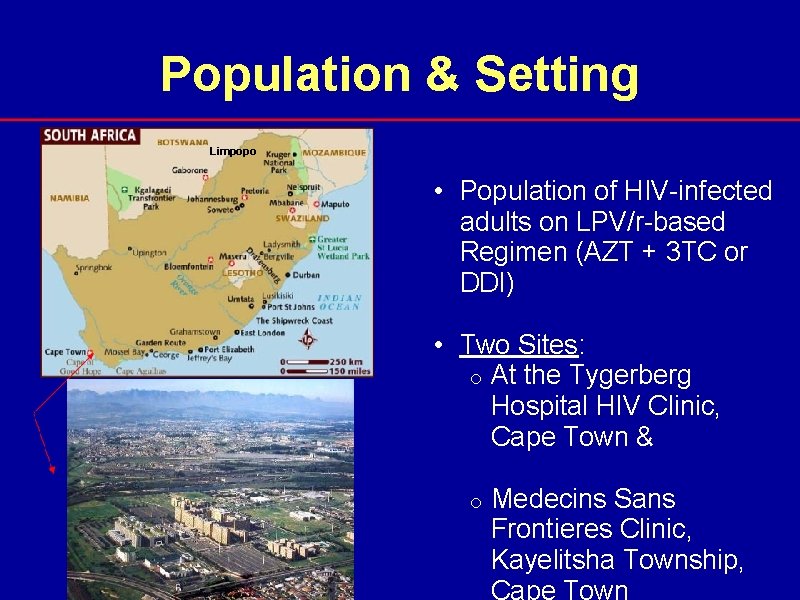
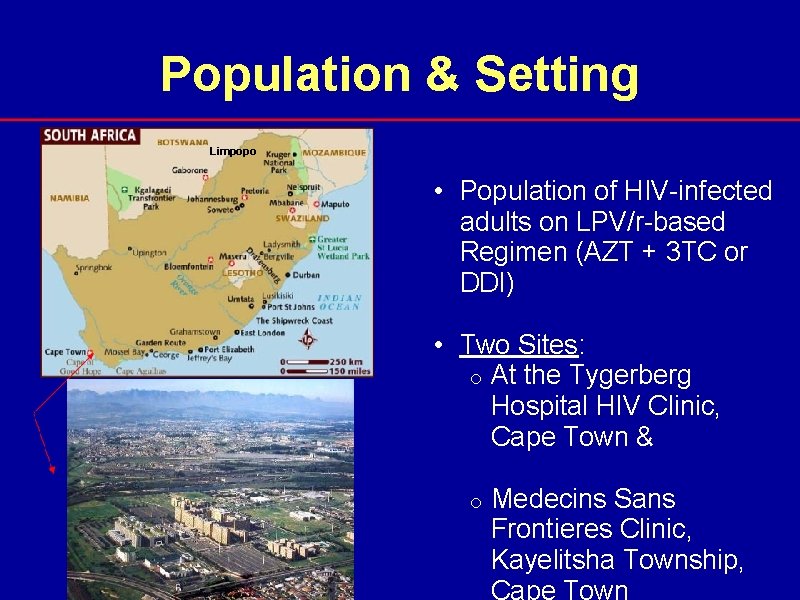
Population & Setting Limpopo • Population of HIV-infected adults on LPV/r-based Regimen (AZT + 3 TC or DDI) • Two Sites: o At the Tygerberg Hospital HIV Clinic, Cape Town & o Medecins Sans Frontieres Clinic, Kayelitsha Township, Cape Town
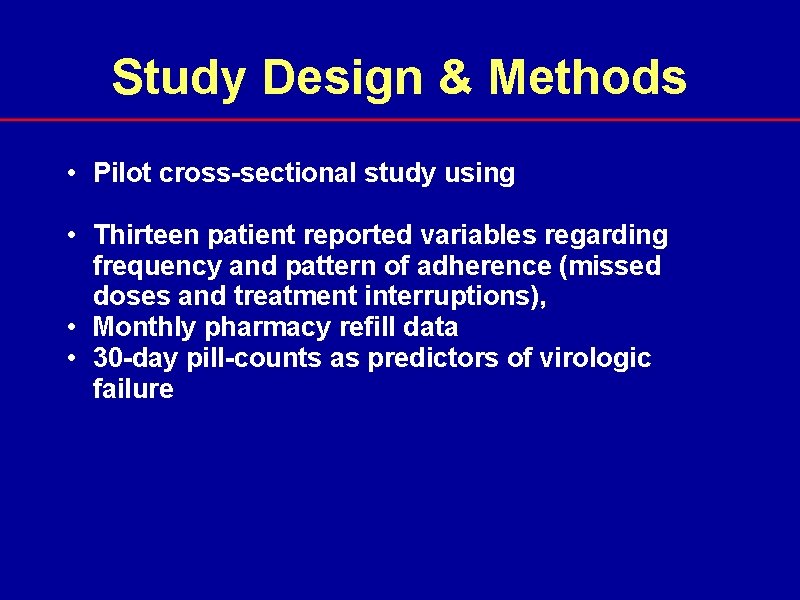
Study Design & Methods • Pilot cross-sectional study using • Thirteen patient reported variables regarding frequency and pattern of adherence (missed doses and treatment interruptions), • Monthly pharmacy refill data • 30 -day pill-counts as predictors of virologic failure
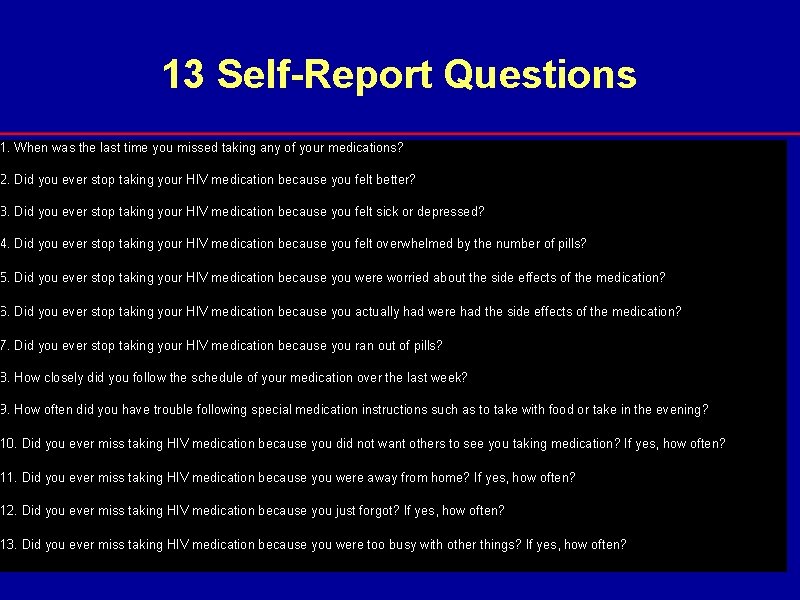
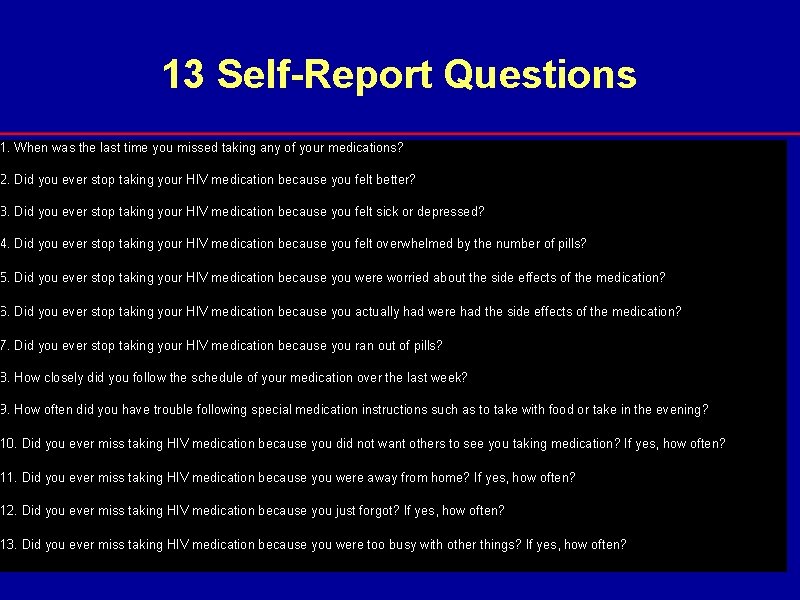
13 Self-Report Questions 1. When was the last time you missed taking any of your medications? 2. Did you ever stop taking your HIV medication because you felt better? 3. Did you ever stop taking your HIV medication because you felt sick or depressed? 4. Did you ever stop taking your HIV medication because you felt overwhelmed by the number of pills? 5. Did you ever stop taking your HIV medication because you were worried about the side effects of the medication? 6. Did you ever stop taking your HIV medication because you actually had were had the side effects of the medication? 7. Did you ever stop taking your HIV medication because you ran out of pills? 8. How closely did you follow the schedule of your medication over the last week? 9. How often did you have trouble following special medication instructions such as to take with food or take in the evening? 10. Did you ever miss taking HIV medication because you did not want others to see you taking medication? If yes, how often? 11. Did you ever miss taking HIV medication because you were away from home? If yes, how often? 12. Did you ever miss taking HIV medication because you just forgot? If yes, how often? 13. Did you ever miss taking HIV medication because you were too busy with other things? If yes, how often?
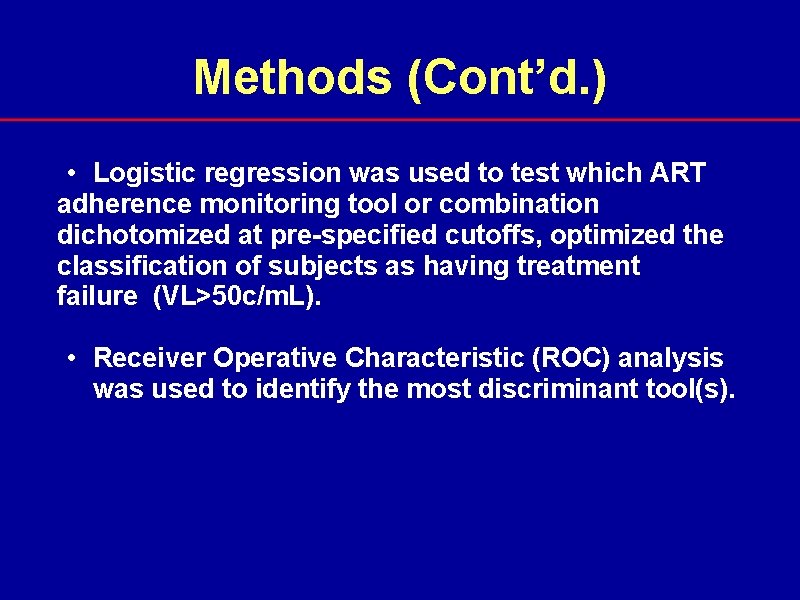
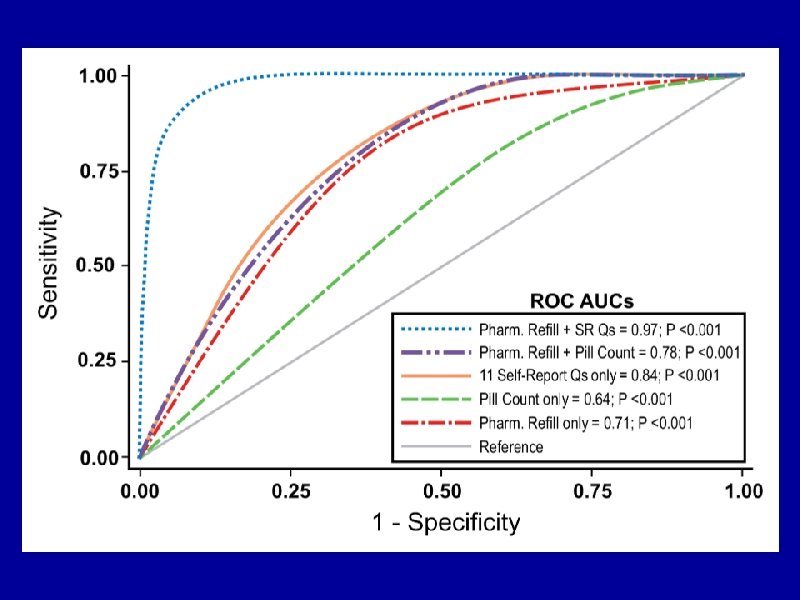
Methods (Cont’d. ) • Logistic regression was used to test which ART adherence monitoring tool or combination dichotomized at pre-specified cutoffs, optimized the classification of subjects as having treatment failure (VL>50 c/m. L). • Receiver Operative Characteristic (ROC) analysis was used to identify the most discriminant tool(s).
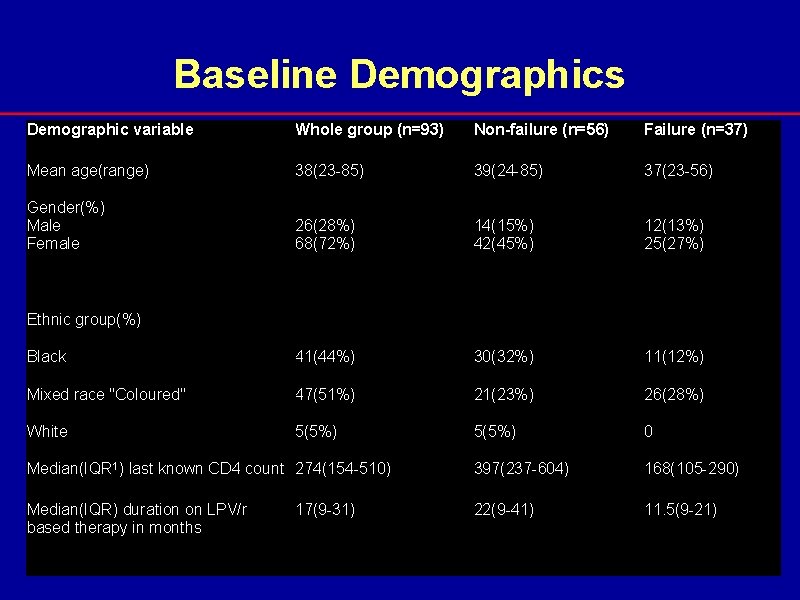
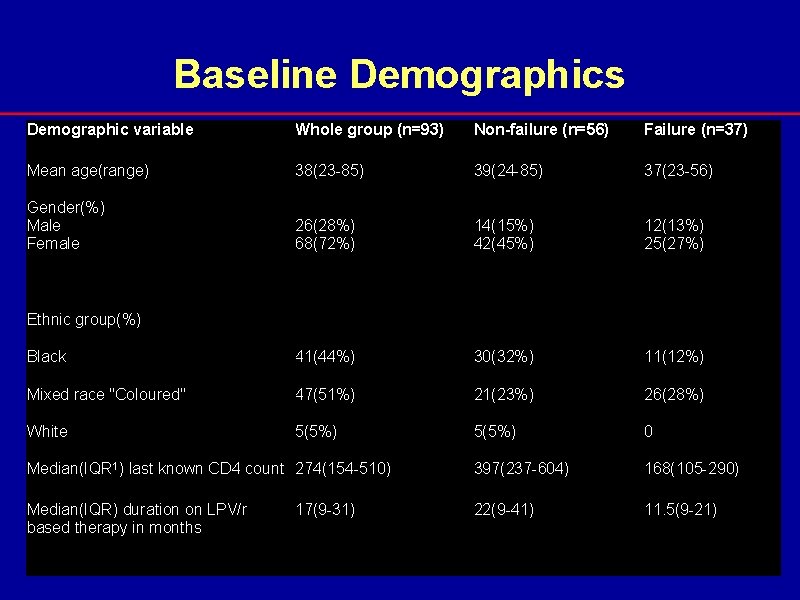
Baseline Demographics Demographic variable Whole group (n=93) Non-failure (n=56) Failure (n=37) Mean age(range) 38(23 -85) 39(24 -85) 37(23 -56) Gender(%) Male Female 26(28%) 68(72%) 14(15%) 42(45%) 12(13%) 25(27%) Black 41(44%) 30(32%) 11(12%) Mixed race "Coloured" 47(51%) 21(23%) 26(28%) White 5(5%) 0 Median(IQR 1) last known CD 4 count 274(154 -510) 397(237 -604) 168(105 -290) Median(IQR) duration on LPV/r based therapy in months 22(9 -41) 11. 5(9 -21) Ethnic group(%) 17(9 -31)

Adherence Tool Test Characteristic & 95% CI Adherence measure Sens 1 Spec 2 PPV 3 NPV 4 LR+5 LR-6 AUC 7 Pharmacy Refill* 56 (37– 73) 67 (47– 87) 70 (51– 88) 52 (33– 71) 1. 66 0. 67 0. 71 (0. 57– 0. 85) Pill count† 58 (41– 74) 74 (54– 93) 79 (63– 95) 50 (31– 69) 2. 19 0. 58 0. 64 (0. 50– 0. 79) 11 adherence Qs 73 (60– 85) 74 (61– 87) 76 (64– 88) 71 (58– 84) 2. 85 0. 36 0. 84 (0. 76– 0. 92) Refill + Pill Count 61 (43– 79) 72 (52– 93) 77 (60– 95) 54 (34– 74) 2. 19 0. 54 0. 78 (0. 65– 0. 91) Pill Count + 11 91 (81– 100) 83 (66– 100) ART adherence Qs 5. 44 0. 11 0. 91 (0. 83– 0. 99) Refill + 11 ART 93 (83– 100) 90 (77– 100) adherence Qs (Optimal) 9. 27 0. 08 0. 97 (0. 92– 1. 00) *ART adherence by pharmacy refill: optimal cut-off 95% (Test + by pharmacy refill, if ART adherence < 95%) †ART adherence by pill count: optimal cut-off 96% (Test + by pill count, if ART adherence <96%)
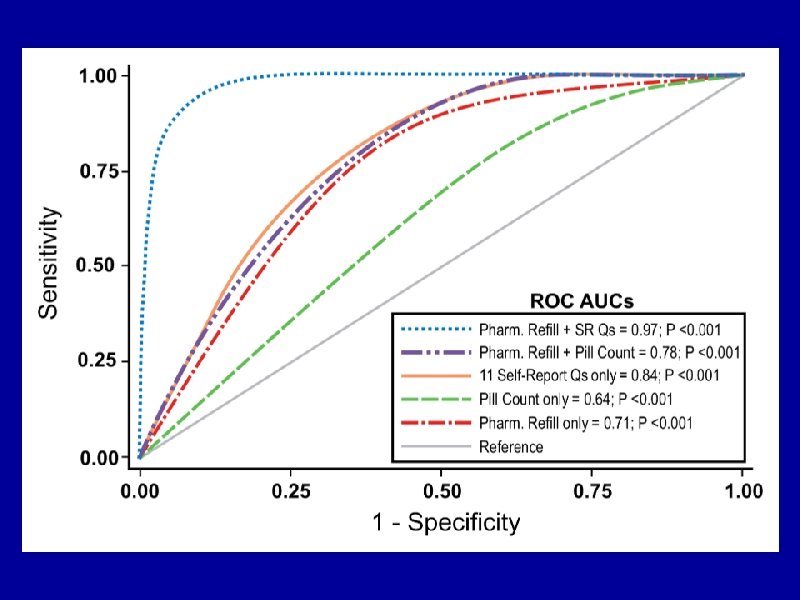
Conclusions • Pill Count performed poorly while the combination of pharmacy and self-report adherence questions had excellent diagnostic accuracy in this setting • This strategy could be used to limit VL monitoring to those at risk for VL rebound as well as guide adherence intervention with the following objectives • While promising, further validation of this simple, low cost, combination of ART adherence monitoring measures is warranted in large prospective studies
Acknowledgments • U. S. Federal Research Grant Support o NIAID/NIH, Division of AIDS § RO 1 AI 0055359 -01 § K 23 A 1068582 -01 • US PEPFAR Grant Award, T 84 HA 21652 -01 -00 for Medical Education Partnership Initiative (MEPI) through HRSA and NIH/FIC • European Developing Countries Clinical Trial Partnership (EDCTP) Senior Fellowship Award TA-08 -40200 -021 • Wellcome Trust Southern Africa Consortium for Excellence in Research Excellence (SACORE)
THANK YOU