Acquired coagulation disorders Acquired coagulation disorders They are
- Slides: 11
Acquired coagulation disorders
Acquired coagulation disorders: They are more common than the inherited disorders. Unlike the inherited disorders, multiple clotting factor deficiencies are usual.
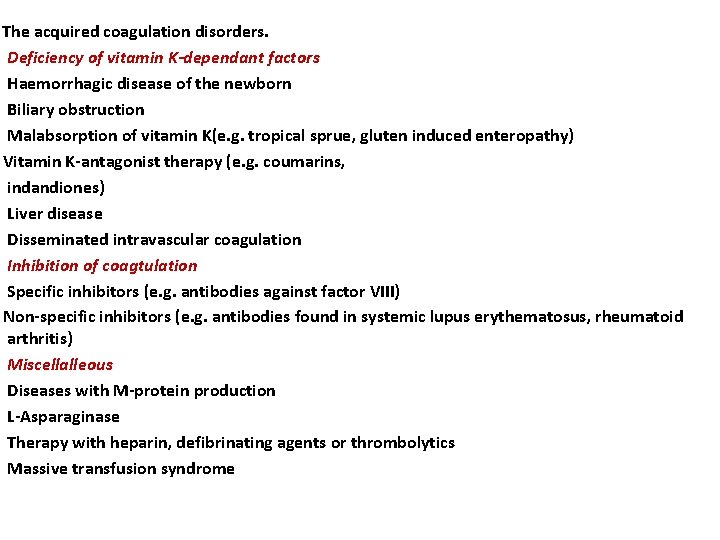
The acquired coagulation disorders. Deficiency of vitamin K-dependant factors Haemorrhagic disease of the newborn Biliary obstruction Malabsorption of vitamin K(e. g. tropical sprue, gluten induced enteropathy) Vitamin K-antagonist therapy (e. g. coumarins, indandiones) Liver disease Disseminated intravascular coagulation Inhibition of coagtulation Specific inhibitors (e. g. antibodies against factor VIII) Non-specific inhibitors (e. g. antibodies found in systemic lupus erythematosus, rheumatoid arthritis) Miscellalleous Diseases with M-protein production L-Asparaginase Therapy with heparin, defibrinating agents or thrombolytics Massive transfusion syndrome
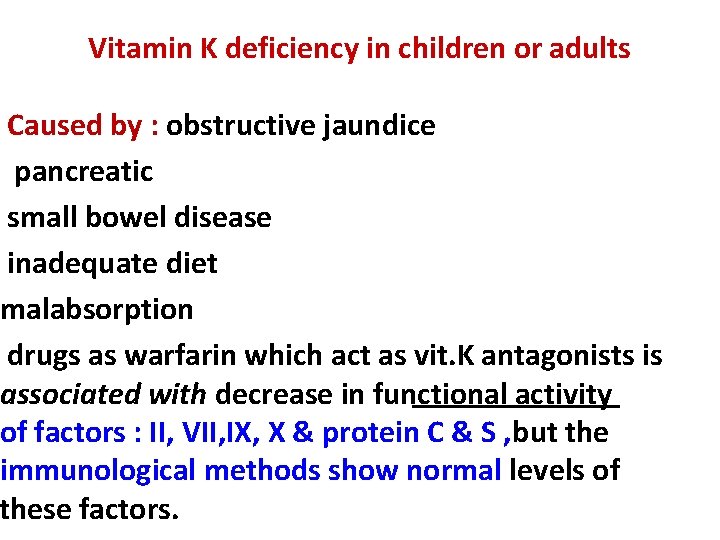
Vitamin K deficiency in children or adults Caused by : obstructive jaundice pancreatic small bowel disease inadequate diet malabsorption drugs as warfarin which act as vit. K antagonists is associated with decrease in functional activity of factors : II, VII, IX, X & protein C & S , but the immunological methods show normal levels of these factors.
Haemorrhagic disease of the newborn Vitamin K-dependent factors are low at birth and fall further in breast-fed infants in the first few days of life. Liver cell immaturity, lack of gut bacterial synthesis of the vitamin and low quantities in breast milk may all contribute to a deficiency which may cause haemorrhage, usually on the second to fourth day of life, but occasionally during the first 2 months
liver disease Multiple haemostatic abnormalities contribute to a bleeding tendency and may exacerbate haemorrhage from oesophageal varices, 1 Biliary obstruction results in impaired absorption of vitamin K and therefore decreased synthesis of factors II, VII, IX and X. 2 With severe hepatocellular disease, in addition to a deficiency of these factors, there are often reduced levels of factor V and fibrinogen and increased amounts of plasminogen activator
3 Functional abnormality of fibrinogen (dysfibrinogenaemia) 4 Decreased thrombopoietin production from the liver contributes to thrombocytopenia. 5 Hypersplenism associated with portal hypertension frequently results in thrombocytopenia. 6 Disseminated intravascular coagulation
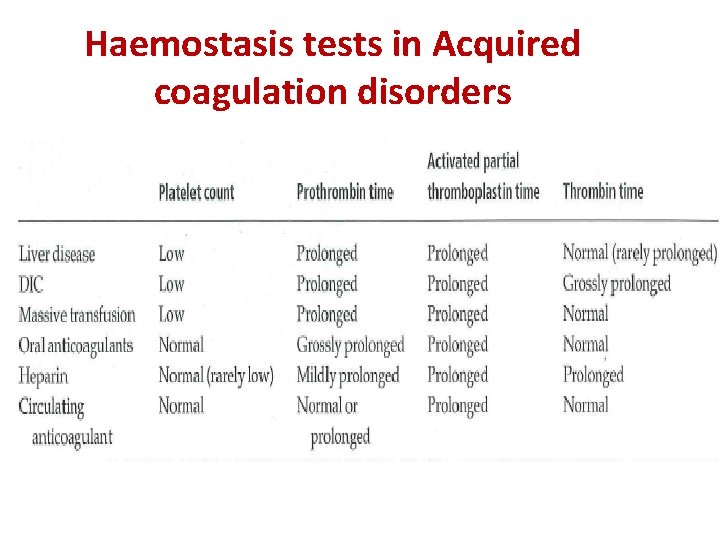
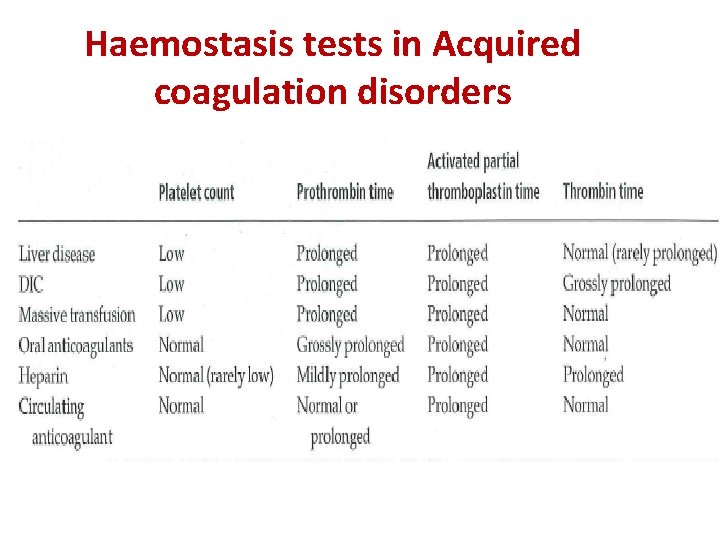
Haemostasis tests in Acquired coagulation disorders
DIC (disseminated intravascular coagulation). Wide spread intravascular deposition of fibrin with consumption of coagulation factors & platelets occur as consequence of many disorders which release procoagulant material into the circulation or cause wide spread endothelial damage or platelets aggregation. It may be associated with fulminant hemorrhagic syndrome or run less severe & more chronic course.
Coagulation deficiency caused by antibodies Circulating antibodies to coagulation factors are occasionally seen with an incidence of approximately 1 per millon per year. Alloantibodies to factor VIII occur in 5 -10% of haemophiliacs. Factor VIII autoantibodies may also result in a bleeding syndrome. These immunoglobulin G (Ig. G) antibodies occur rarely post-partum, in certain immunolological disorders (e. g. rheumatoid arthritis), in cancer and in old age. Treatment usually consists of a combination of immunosuppression and treatment with factor replacement
Massive transfusion syndrome Many factors may contribute to a bleeding disorder following massive transfusion, Blood loss results in reduced levels of platelets, coagulation factors and inhibitors, Further dilution of these factors occurs during replacement with red cells,