Cutting Edge Regulatory Strategies for Your IDG Regulatory

- Slides: 53
Cutting Edge Regulatory Strategies for Your IDG: Regulatory Requirements and IDT impacts on Organizational Compliance Jennifer Kennedy, MA, BSN, RN, CHC National Hospice and Palliative Care Organization September 2015
FY 2013 Medicare Part D Payments Outside Hospice Benefit • Medicare Part D spending: – FY 2013: $347. 1 million – CY 2012: $334. 9 million © National Hospice and Palliative Care Organization, 2015. All rights reserved. 2
Four case studies on frequent hospice diagnoses • Case studies presented for following diagnoses – – chronic airway obstruction congestive heart failure cerebral degeneration lung cancer • Citation of : – Typical symptoms – Evidence-based practice interventions/ recommendations • Comments on Medicare spending outside the hospice benefit © National Hospice and Palliative Care Organization, 2015. All rights reserved. 3
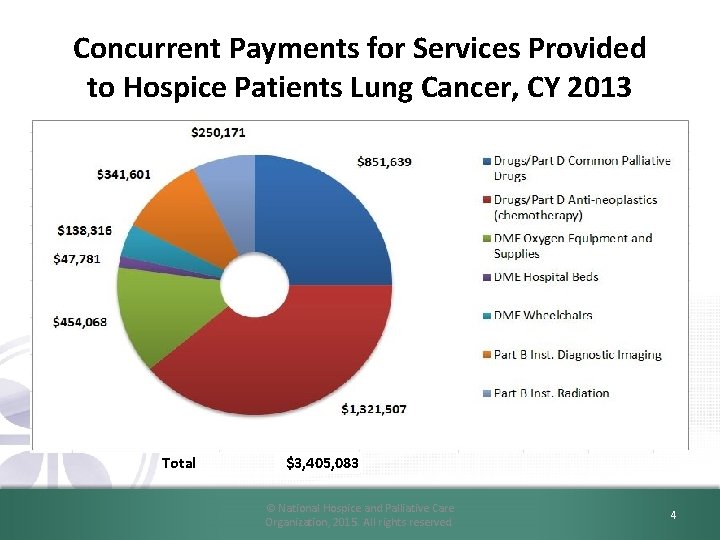
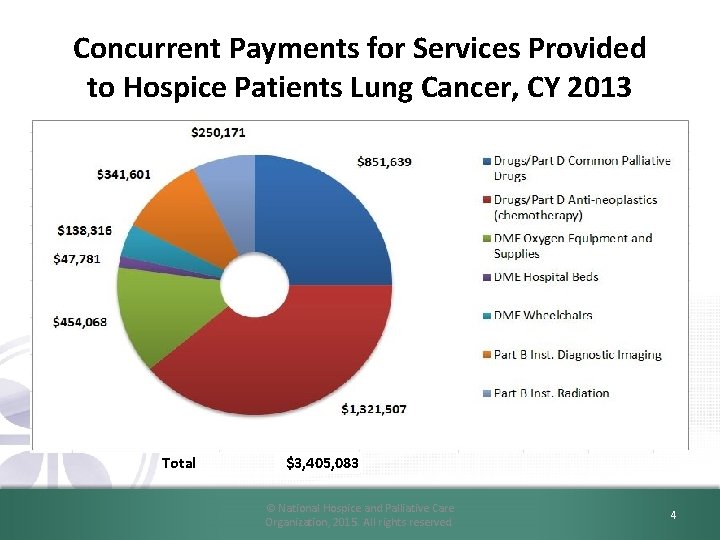
Concurrent Payments for Services Provided to Hospice Patients Lung Cancer, CY 2013 Total $3, 405, 083 © National Hospice and Palliative Care Organization, 2015. All rights reserved. 4
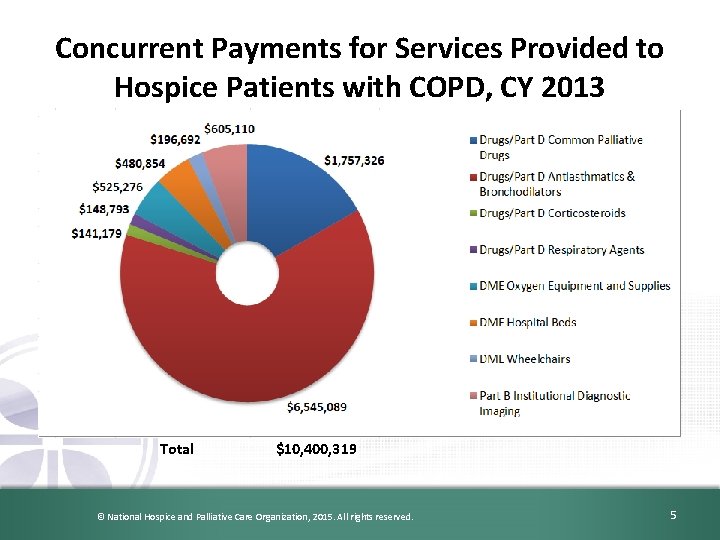
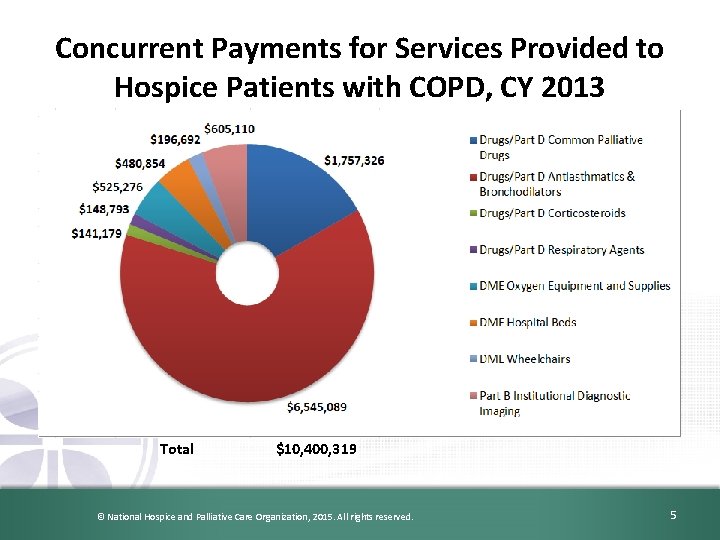
Concurrent Payments for Services Provided to Hospice Patients with COPD, CY 2013 Total $10, 400, 319 © National Hospice and Palliative Care Organization, 2015. All rights reserved. 5
CMS Concern • Analysis reveals: – Clinical based practices are not being covered under the Medicare hospice benefit. – Potential systematic unbundling of the Medicare hospice benefit – May be valuable analysis to inform policy stakeholders © National Hospice and Palliative Care Organization, 2015. All rights reserved. 6
NHPCO Comments to CMS • NHPCO is concerned that CMS is holding hospice providers alone solely responsible for all claims filed on behalf of beneficiaries who have elected hospice, and yet hospices often do not know, and are not in control of, whether or how other providers bill, and for what services, nor can hospices control whether and when a beneficiary sees a non-hospice provider. • We encourage CMS to establish systems in claims processing so that other providers are immediately aware of the patient’s hospice election and are guided to coordinate with the hospice and to bill appropriately. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 7
Assessment of Conditions and Comorbidities Required by Regulation • We (CMS) continue to state that those circumstances would be “exceptional and unusual” and that hospices continue to be required to provide virtually all the care that is needed by terminally ill patients. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 8
Assessment of Conditions and Comorbidities Required by Regulation • Comorbidities are recognized as important factors – Contributing to the overall status of an individual – Should be considered when determining terminal prognosis. • Mental health comorbidities must also be considered. – Not uncommon for terminally ill individuals to have underlying mental health conditions – Could contribute to their prognosis and/or affect the plan of care © National Hospice and Palliative Care Organization, 2015. All rights reserved. 9
NHPCO Comments to CMS • The cause and impact of a mental health (or any other) diagnosis has to be determined on a case by case basis, and expecting global adherence to general rules is unreasonable. • In addition, the impact of any comorbid diagnosis may vary based on the individual length of prognosis. • A hospice physician needs to make the determination of what is related to the terminal prognosis based on each individual patient’s clinical condition. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 10
NHPCO Comments to CMS • “Virtually all” – NHPCO strongly asserts that determinations of “relatedness” must be made on a case by case basis, as CMS has stated previously, and it is the role and responsibility of the hospice medical director or hospice physician to determine what is related to the terminal prognosis, and what is not. – We urge CMS to avoid blanket assertions or assumptions about which services are always related to a patient’s terminal prognosis. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 11
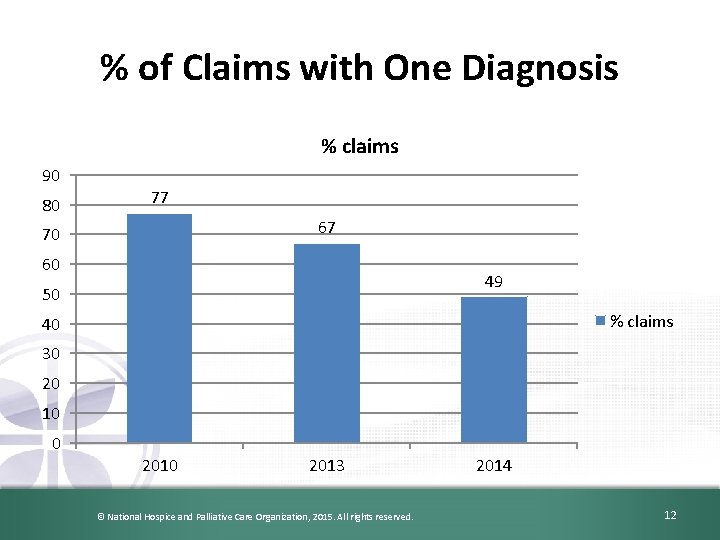
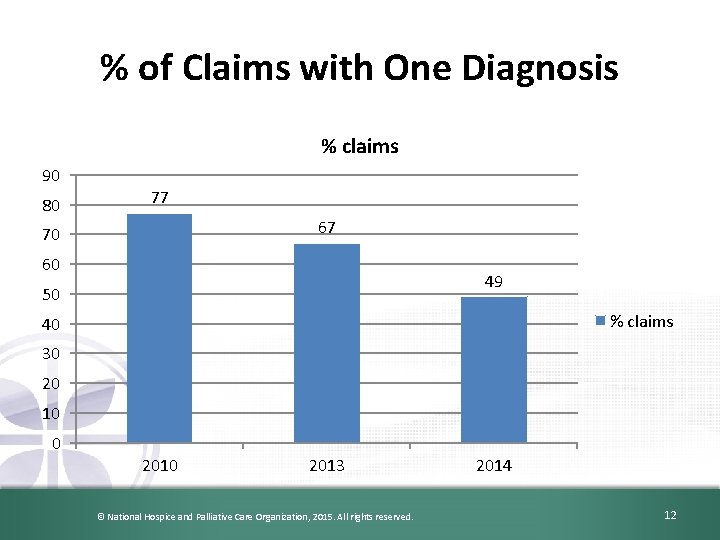
% of Claims with One Diagnosis % claims 90 80 77 67 70 60 49 50 % claims 40 30 20 10 0 2013 © National Hospice and Palliative Care Organization, 2015. All rights reserved. 2014 12
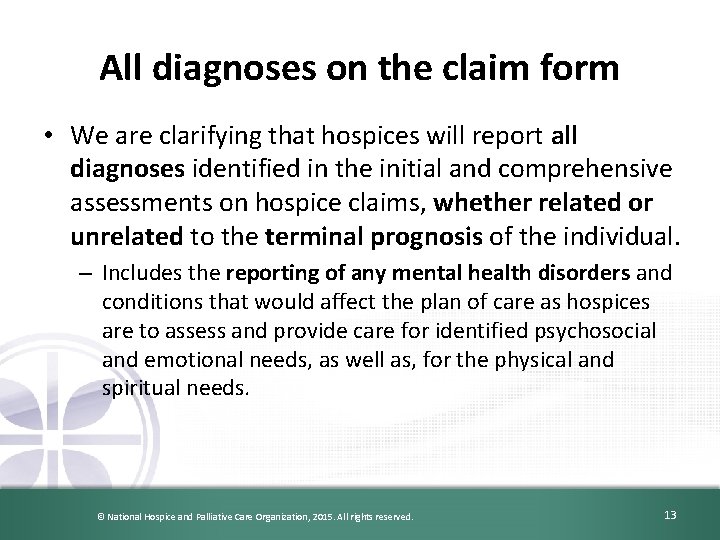
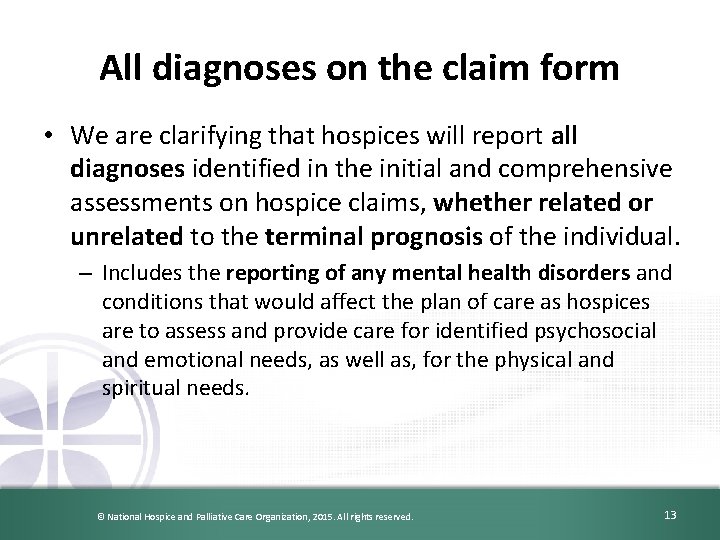
All diagnoses on the claim form • We are clarifying that hospices will report all diagnoses identified in the initial and comprehensive assessments on hospice claims, whether related or unrelated to the terminal prognosis of the individual. – Includes the reporting of any mental health disorders and conditions that would affect the plan of care as hospices are to assess and provide care for identified psychosocial and emotional needs, as well as, for the physical and spiritual needs. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 13
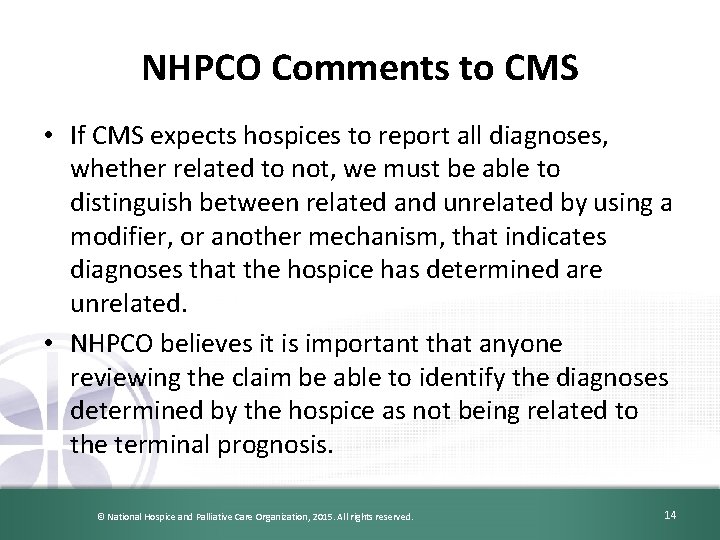
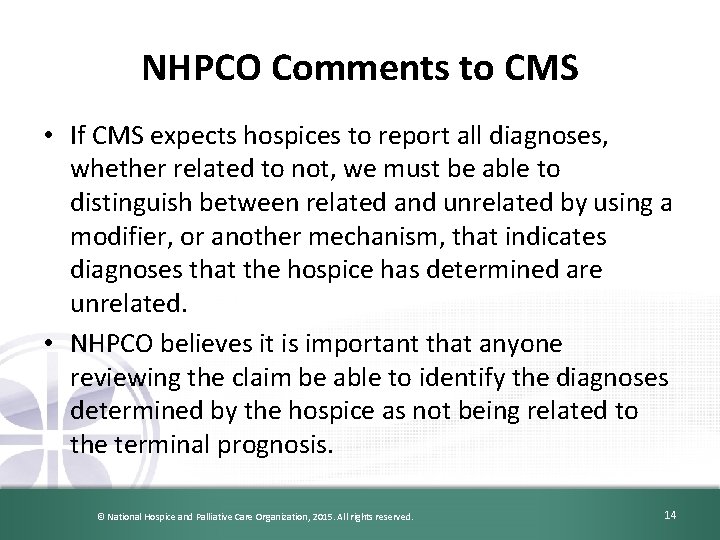
NHPCO Comments to CMS • If CMS expects hospices to report all diagnoses, whether related to not, we must be able to distinguish between related and unrelated by using a modifier, or another mechanism, that indicates diagnoses that the hospice has determined are unrelated. • NHPCO believes it is important that anyone reviewing the claim be able to identify the diagnoses determined by the hospice as not being related to the terminal prognosis. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 14
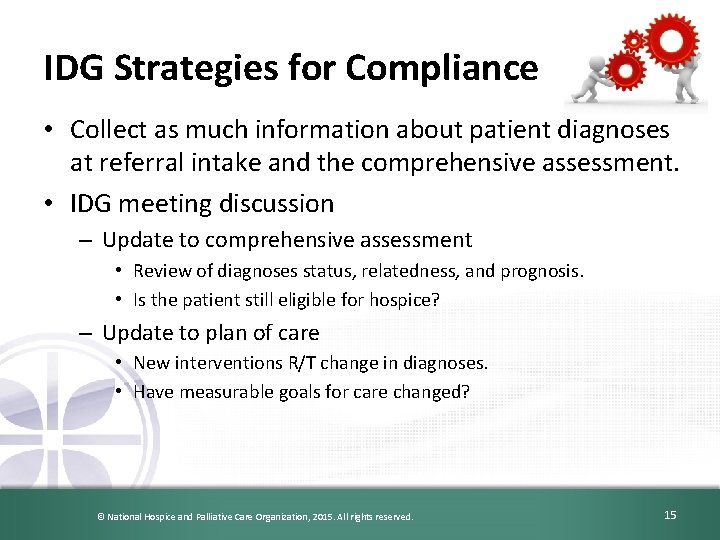
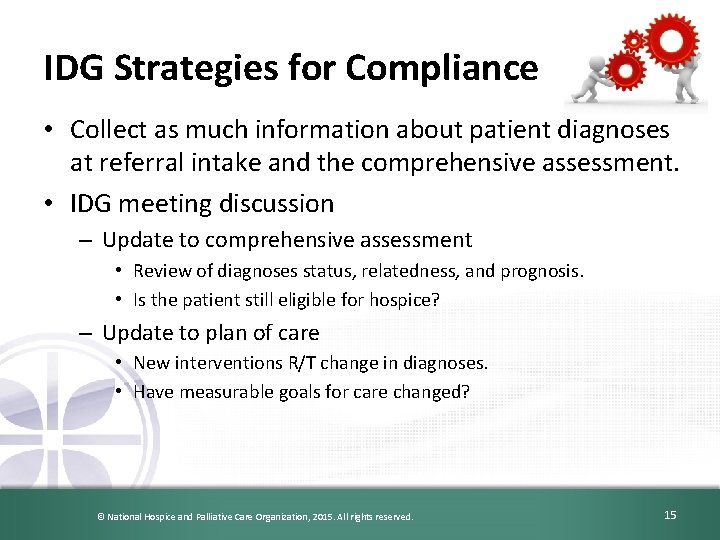
IDG Strategies for Compliance • Collect as much information about patient diagnoses at referral intake and the comprehensive assessment. • IDG meeting discussion – Update to comprehensive assessment • Review of diagnoses status, relatedness, and prognosis. • Is the patient still eligible for hospice? – Update to plan of care • New interventions R/T change in diagnoses. • Have measurable goals for care changed? © National Hospice and Palliative Care Organization, 2015. All rights reserved. 15
IDG Strategies for Compliance • Documentation – Is there hospice physician documentation in the clinical record that supports why a diagnosis, medication, treatment, etc… does not medically contribute to the terminal prognosis? – Is the documentation updated as the patient’s condition changes? – Does the IDG documentation support the hospice physician documentation? • I. e. : Communication with patient and family, communication with attending physician, … © National Hospice and Palliative Care Organization, 2015. All rights reserved. 16
Determining Relatedness © National Hospice and Palliative Care Organization, 2015. All rights reserved. 17
The Regulation § 418. 3 Definitions “Terminally ill means that the individual has a medical prognosis that his or her life expectancy is 6 months or less if the illness runs its normal course. ” © National Hospice and Palliative Care Organization, 2015. All rights reserved. 18
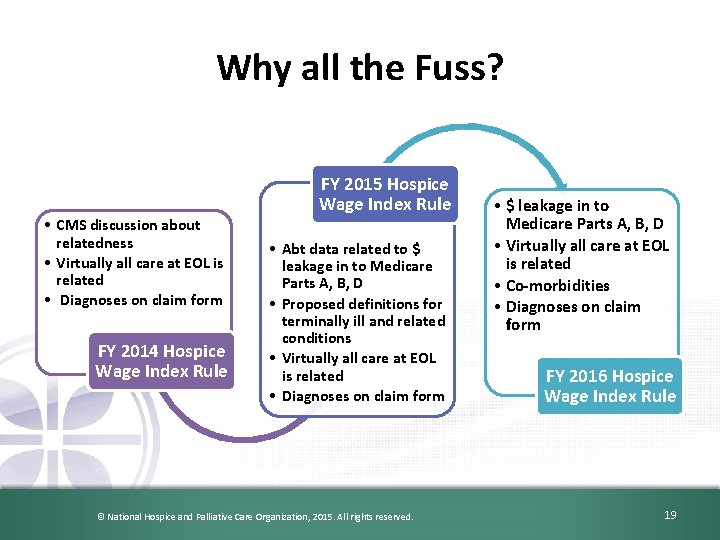
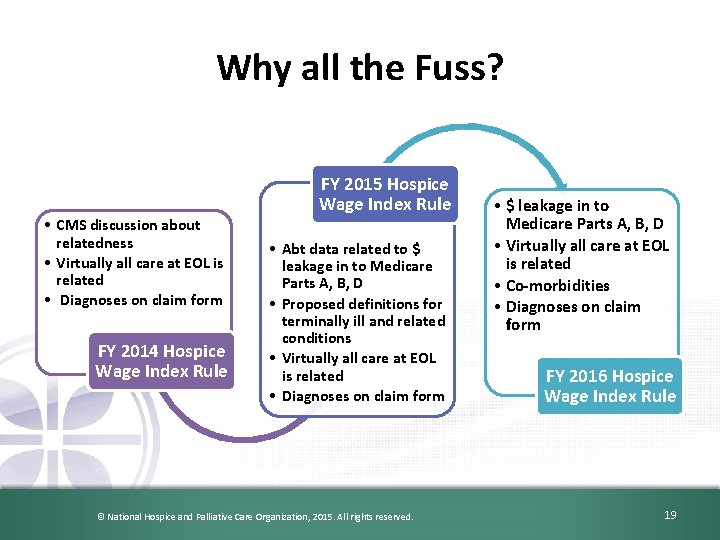
Why all the Fuss? • CMS discussion about relatedness • Virtually all care at EOL is related • Diagnoses on claim form FY 2014 Hospice Wage Index Rule FY 2015 Hospice Wage Index Rule • Abt data related to $ leakage in to Medicare Parts A, B, D • Proposed definitions for terminally ill and related conditions • Virtually all care at EOL is related • Diagnoses on claim form © National Hospice and Palliative Care Organization, 2015. All rights reserved. • $ leakage in to Medicare Parts A, B, D • Virtually all care at EOL is related • Co-morbidities • Diagnoses on claim form FY 2016 Hospice Wage Index Rule 19
NHPCO Relatedness Workgroup • A subcommittee of the NHPCO Regulatory Committee. • Formed in 2013 in response to FY 2014 proposed Hospice Wage Index Rule. • The group’s mission was to develop resources for the NHPCO membership that will assist in determining related diagnoses, treatments, medications, supplies, and equipment for a patient. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 20
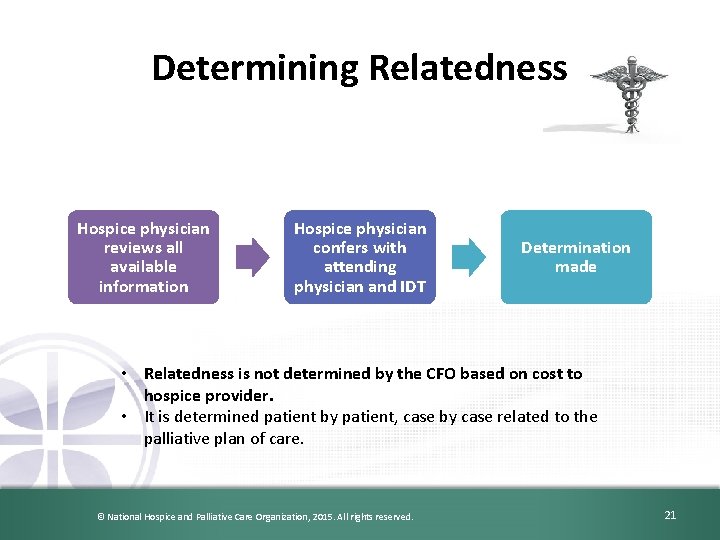
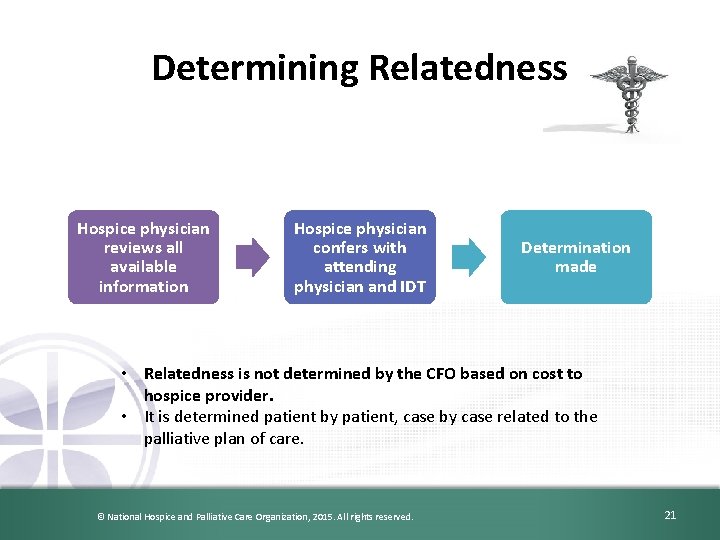
Determining Relatedness Hospice physician reviews all available information Hospice physician confers with attending physician and IDT Determination made • Relatedness is not determined by the CFO based on cost to hospice provider. • It is determined patient by patient, case by case related to the palliative plan of care. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 21
Role of the Nurse • Provision of clinical information to the hospice physician. – – Comprehensive assessment History and physical Discharge summary from hospital Clinical information from attending physician © National Hospice and Palliative Care Organization, 2015. All rights reserved. 22
Role of the Other IDT Members • Social worker, dietician, chaplain, … • Continuous provision of information to the hospice physician. – Updated to the comprehensive assessment © National Hospice and Palliative Care Organization, 2015. All rights reserved. 23
Role of the Hospice Physician • Determining the diagnoses is within the scope of practice of medicine – Formal diagnoses for the record vs. nursing diagnoses – Hospice physician can determine new diagnoses that are present but have not been previously designated formally – Example: Dementia is documented in the record, but does not state the etiology of the dementia © National Hospice and Palliative Care Organization, 2015. All rights reserved. 24
The Determination Process • Is the condition being considered a diagnosis or a symptom (or both)? – Diagnoses will need a determination of whether they are related or unrelated – Symptoms are almost automatically related (Coding guidelines state these do not need to be listed if they are a normal part of the diagnosis) – What if they are both diagnosis and symptom? (Example: Depression) © National Hospice and Palliative Care Organization, 2015. All rights reserved. 25
The Determination Process • Is there active pain or an active symptom? – Should be considered related • Is there a likelihood of pain or another symptom? – Should be considered related • Questions about: – Arthritis pain, Migraine prophylaxis, etc. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 26
The Determination Process • Is the diagnosis caused by or causing the terminal condition? • Some obvious examples include: – HIV AIDS – Ischemic heart disease Congestive heart failure – Cerebral atherosclerosis Vascular dementia • How far do you drill down? – Diabetes mellitus Diabetic nephropathy ESRD – HTN Hypertensive nephropathy ESRD DMT 2 © National Hospice and Palliative Care Organization, 2015. All rights reserved. 27
The Determination Process • Is the diagnosis in question stable? • If not requiring management – Does not need to listed – Example: Remote prostate cancer • If requiring management, does the treatment interact or potentially interact with the terminal illness? – Determined case by case © National Hospice and Palliative Care Organization, 2015. All rights reserved. 28
Other Considerations • All determinations must be done with consideration of the patient’s prognosis – If not eligible all the above is moot (Discharge (or do not admit) the patient) – If any DX (or TX for a DX) contributes to the terminal prognosis it is related • Is a TX under consideration still beneficial within the patient’s expected prognosis? – May still be related, but should be discontinued © National Hospice and Palliative Care Organization, 2015. All rights reserved. 29
Common Denominator • All the above determinations require medical judgment • The hospice physician must complete the documentation • Must have hospice physicians who can make such decisions – Must have adequate information on the patient’s status © National Hospice and Palliative Care Organization, 2015. All rights reserved. 30
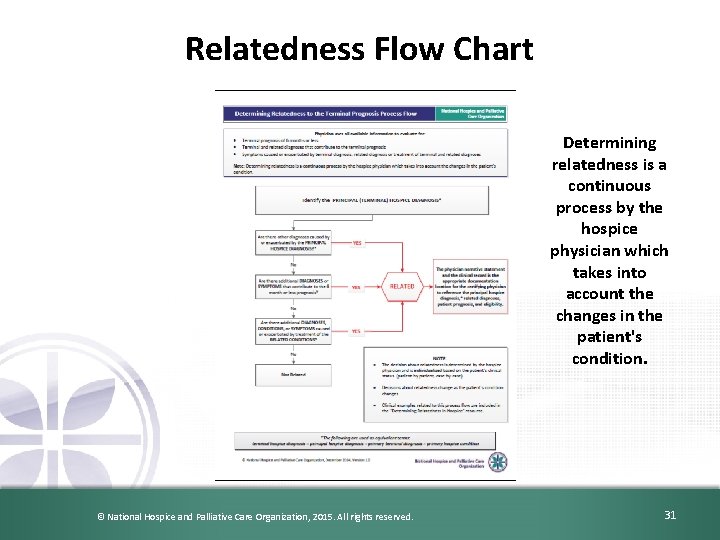
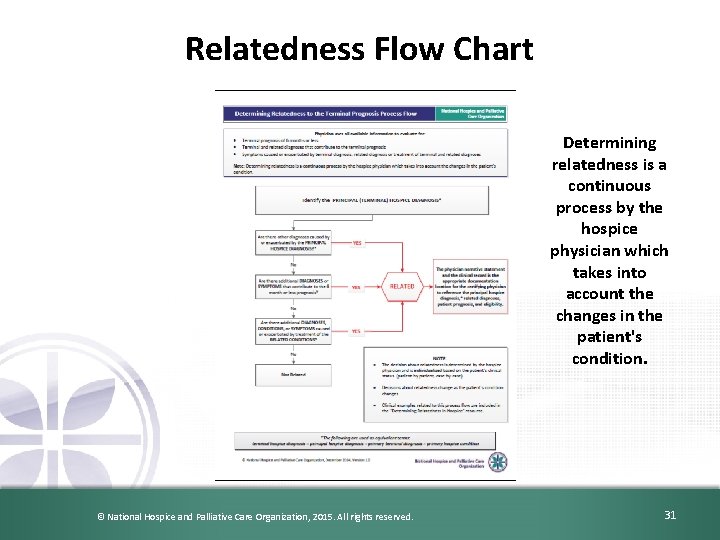
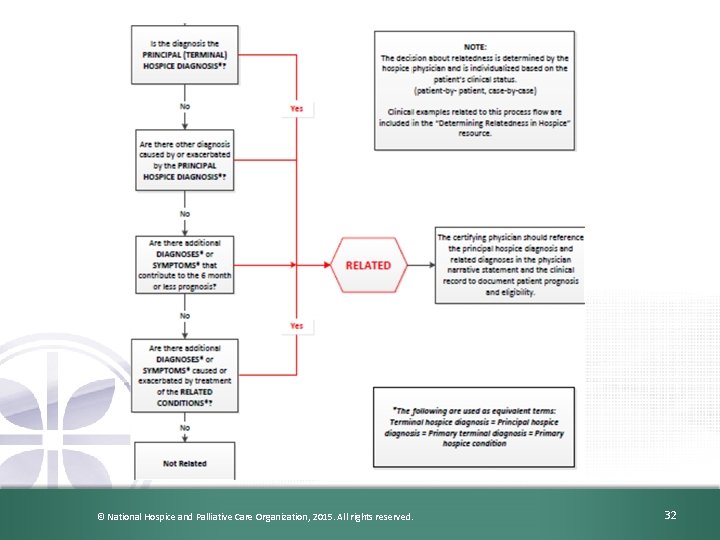
Relatedness Flow Chart Determining relatedness is a continuous process by the hospice physician which takes into account the changes in the patient's condition. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 31
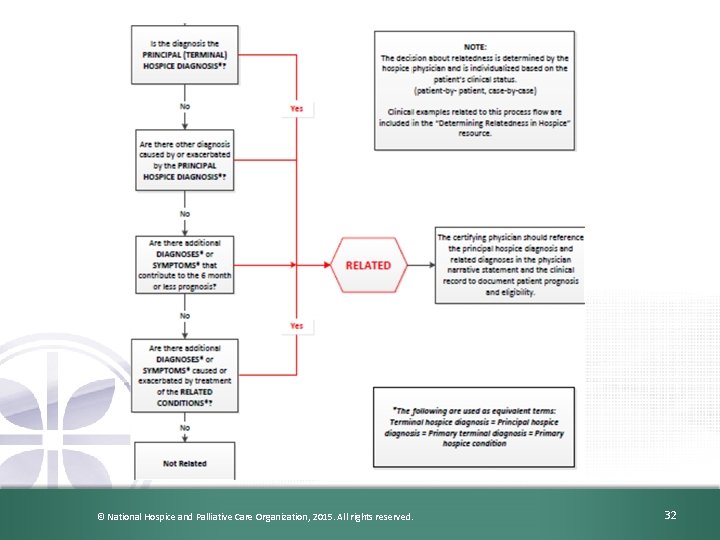
© National Hospice and Palliative Care Organization, 2015. All rights reserved. 32

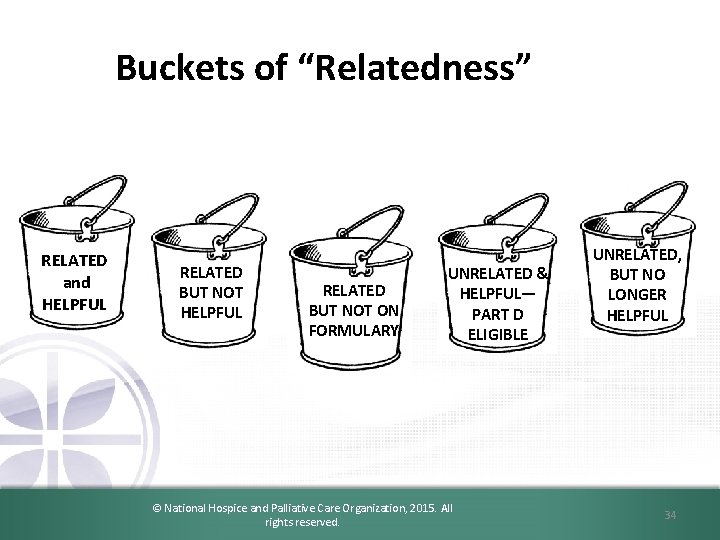
Coverage per the Regulations 418. 200 Requirements for coverage. – To be covered, hospice services … must be reasonable and necessary for the palliation or management of the terminal illness as well as related conditions. 418. 202 Covered services. – (f) Medical appliances and supplies, including drugs and biologicals. Only drugs … which are used primarily for the relief of pain and symptom control related to the individual's terminal illness are covered. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 33
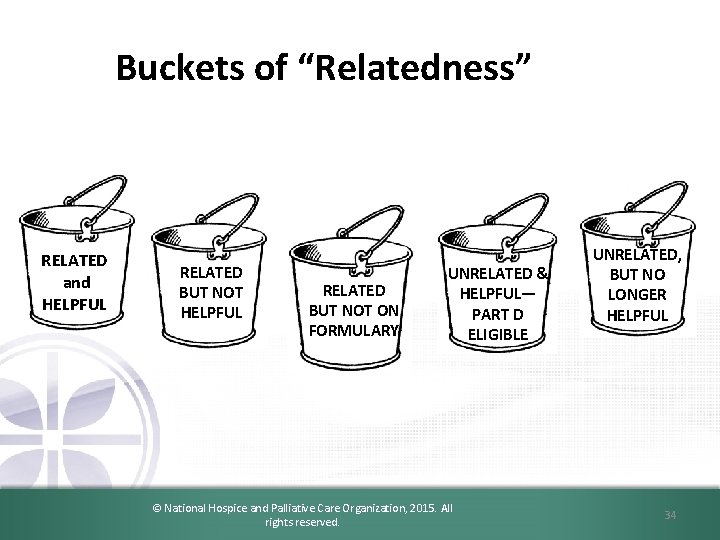
Buckets of “Relatedness” RELATED and HELPFUL RELATED BUT NOT ON FORMULARY UNRELATED & HELPFUL— PART D ELIGIBLE © National Hospice and Palliative Care Organization, 2015. All rights reserved. UNRELATED, BUT NO LONGER HELPFUL 34
Related vs. Unrelated • …, unless there is clear evidence that a condition is unrelated to the terminal prognosis; all services would be considered related. • It is also the responsibility of the hospice physician to document why a patient’s medical needs would be unrelated to the terminal prognosis. 78 Federal Register 152 (7 August 2013), p. 48236 -7 © National Hospice and Palliative Care Organization, 2015. All rights reserved. 35
Documenting “Un-relatedness” • It is the hospice physician’s responsibility to document what is unrelated • Where should that occur? – – In the certification narrative? Not the best place In a progress note? May be hard to locate In the med profile? Include non-med treatments? Stand-alone document? • EMR vs. Paper documentation concerns © National Hospice and Palliative Care Organization, 2015. All rights reserved. 36
Documenting “Unrelatedness” cont… • What does the hospice physician document? • CMS has providing varying guidance on this – Recent CMS Open Door Forum call: should be a brief narrative that is reasonable in explaining why the condition is unrelated © National Hospice and Palliative Care Organization, 2015. All rights reserved. 37
Examples of Unrelatedness • Two examples are repeatedly offered for unrelatedness – Neither has been validated by CMS 1. “Glaucoma is pathophysiologically unrelated to the patient’s lung cancer, and does not contribute to the terminal prognosis. ” 2. “Hypothyroidism is physiologically unrelated to the patient’s COPD, and since it is well managed, it does not contribute to a worsened prognosis. ” © National Hospice and Palliative Care Organization, 2015. All rights reserved. 38
Reasonable and Necessary • The Medicare Hospice Benefit requires the hospice to cover all reasonable and necessary palliative care related to the terminal prognosis and related conditions…. • Section 1862(a)(1)(C) of the Social Security Act (the Act) forbids payment for any items or services which are not reasonable and necessary for the palliation and management of the terminal illness. Services which are not needed. . . would not be reasonable and necessary. 78 Federal Register 152 (7 August 2013), p. 48236, 48274. © National Hospice and Palliative Care Organization, 2015. All rights reserved. 39
Discontinuation • When is the right time to discuss discontinuation? • What drives the determination of discontinuation? • Who determines discontinuation? • Does the patient have a choice? © National Hospice and Palliative Care Organization, 2015. All rights reserved. 40
IDG Strategies for Compliance • Process for determination of relatedness. – Do you have one? – Do IDG members know their role? – Is your physician skilled in determining relatedness? • Does he or she require training? – Are your staff trained to have the “discontinuation talk” with patient’s and family’s? – Does your documentation reflect your practice? – Is your clinical documentation defensible? © National Hospice and Palliative Care Organization, 2015. All rights reserved. 41
LIVE DISCHARGES © National Hospice and Palliative Care Organization, 2015. All rights reserved. 42
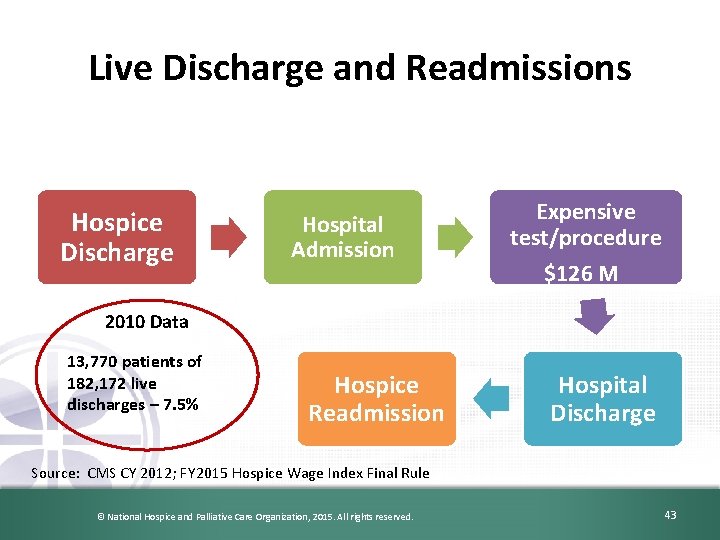
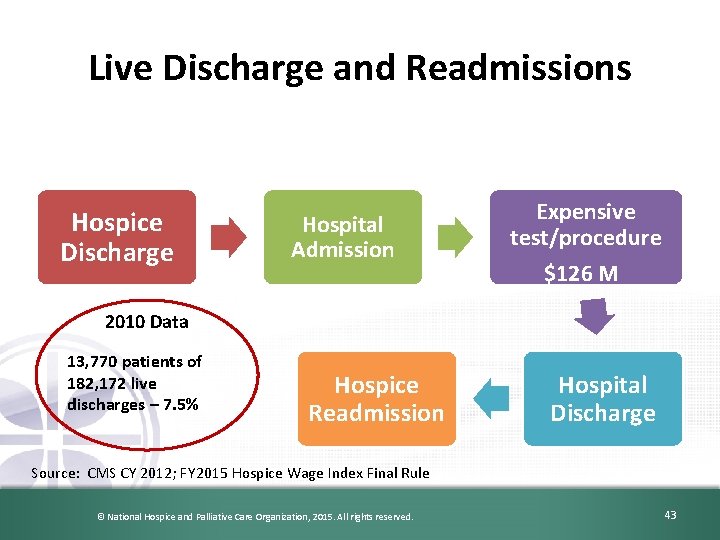
Live Discharge and Readmissions Hospice Discharge Hospital Admission Expensive test/procedure $126 M 2010 Data 13, 770 patients of 182, 172 live discharges – 7. 5% Hospice Readmission Hospital Discharge Source: CMS CY 2012; FY 2015 Hospice Wage Index Final Rule © National Hospice and Palliative Care Organization, 2015. All rights reserved. 43
IDG Strategies for Compliance • Live discharge practice in your organization. – What is your incidence of live discharge? • Last 12 months (includes revocation) – Why do you discharge live? – Are you collecting as much information as you should be? • Revocation • Reelection – Are patients/ families really understanding that hospice approval is required for all care related to the terminal prognosis? © National Hospice and Palliative Care Organization, 2015. All rights reserved. 44
Medications © National Hospice and Palliative Care Organization, 2015. All rights reserved. 45
46 If medication is deemed related… • Hospice covers the cost – Care (services, treatment, etc. …) – Medications – DME & supplies • Documentation should appear in the clinical record that it is related – Physician narrative – Plan of care – Medication profile © National Hospice and Palliative Care Organization, 2015. All rights reserved. 46
Related and NOT in Plan of Care • Not effective – not “supported by the evidence” or “truly necessary” • May be harmful for reasons not usually thought of by patients and families – “not free from harm” • Duplicate medications • Not on hospice formulary or preferred med list – And pt/family decline an equivalent medication that would be covered © National Hospice and Palliative Care Organization, 2015. All rights reserved. 47
If medication is deemed unrelated… • CMS expects that another health care professional would come to the same conclusion after reviewing the same data – Subject to MAC and auditor review – Subject to Part D plan sponsor review • Audits directed to start again with 2014 Part D claims • Documentation should appear in the clinical record that it is NOT related – Consistent, accessible location • “We expect drugs covered under Part D for hospice beneficiaries will be extremely rare. ” © National Hospice and Palliative Care Organization, 2015. All rights reserved. 48
IDG Strategies for Compliance • Do you have a process in place for assessing all medications and determining relatedness? – Does it work? • Are your staff trained to have the “discontinuation talk” with patient’s and family’s? • Does your documentation reflect your practice? • Is your clinical documentation defensible? © National Hospice and Palliative Care Organization, 2015. All rights reserved. 49
Questions NHPCO members enjoy unlimited access to Regulatory Assistance Feel free to email questions to regulatory@nhpco. org © National Hospice and Palliative Care Organization, 2015. All rights reserved. 50
Regulatory and Compliance Team at NHPCO Jennifer Kennedy, MA, BSN, RN, CHC Director, Regulatory and Compliance Judi Lund Person, MPH Vice President, Regulatory and Compliance Email us at: regulatory@nhpco. org © National Hospice and Palliative Care Organization, 2015. All rights reserved. 51
NHPCO Resources http: //www. nhp co. org/regulator y-compliancehospices/determ ining-terminalprognosis © National Hospice and Palliative Care Organization, 2015. All rights reserved. 52
References CMS Hospice Center �http: //www. cms. hhs. gov/center/hospice. asp �Conditions of Participation Hospice �Medicare Benefit Policy Manual; Chapter 9 - Coverage of Hospice Services NHPCO Regulatory Page http: //www. nhpco. org/resources/regulatory © National Hospice and Palliative Care Organization, 2015. All rights reserved. 53
 The appropriate cutting tool used in cutting fabrics
The appropriate cutting tool used in cutting fabrics Enamel hatchet formula
Enamel hatchet formula Modified palm and thumb grasp in dentistry
Modified palm and thumb grasp in dentistry Non cutting dental instruments
Non cutting dental instruments Flank wear
Flank wear Izharı lamı fiiliyye
Izharı lamı fiiliyye Mahreçleri aynı sıfatları farklı
Mahreçleri aynı sıfatları farklı Idğ
Idğ T-idg
T-idg New cutting edge starter
New cutting edge starter Open benefit sonoco
Open benefit sonoco Cutting edge graphics
Cutting edge graphics Teori cutting edge
Teori cutting edge Cutting edge peter moor
Cutting edge peter moor Cutting edge technology
Cutting edge technology Cutting edge technology
Cutting edge technology Moldflow
Moldflow Cutting edge
Cutting edge Cutting edge
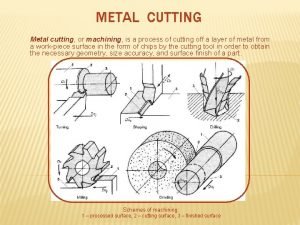
Cutting edge Three cutting tools
Three cutting tools Cutting edge bolus
Cutting edge bolus Rising edge and falling edge
Rising edge and falling edge Give us your hungry your tired your poor
Give us your hungry your tired your poor Don't put your cup on the edge of the table
Don't put your cup on the edge of the table Iso 22301 utbildning
Iso 22301 utbildning Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Returpilarna
Returpilarna Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Särskild löneskatt för pensionskostnader
Särskild löneskatt för pensionskostnader Personlig tidbok för yrkesförare
Personlig tidbok för yrkesförare Sura för anatom
Sura för anatom Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare Stig kerman
Stig kerman Debatt mall
Debatt mall Delegerande ledarstil
Delegerande ledarstil Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Arkimedes princip formel
Arkimedes princip formel Offentlig förvaltning
Offentlig förvaltning Urban torhamn
Urban torhamn Presentera för publik crossboss
Presentera för publik crossboss Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Bat mitza
Bat mitza Treserva lathund
Treserva lathund Fimbrietratt
Fimbrietratt Bästa kameran för astrofoto
Bästa kameran för astrofoto Cks
Cks Lågenergihus nyproduktion
Lågenergihus nyproduktion Mat för idrottare
Mat för idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering